Abstract
An 80-year-old woman with longstanding hemifacial spasm had a 1 cm × 1.5 cm internal carotid artery terminus aneurysm treated with endovascularly delivered bare metal coils. Follow-up imaging revealed an expansile perianeurysmal cyst that coincided with development of contralateral dopa-responsive hemiparkinsonism. This is the first report of perianeurysmal cyst expansion causing levodopa-responsive hemiparkinsonism.
Introduction
Perianeurysmal edema and cyst formation following endovasuclar coil treatment of unruptured basilar or internal carotid artery aneurysms [1, 2] is rare. There is a single report of damage isolated to the nigrostriatal pathway after coiling a ruptured aneurysm. This damage caused only mild contralateral hemiparesis that persisted after two aspiration attempts and intracavitary phosphorus-32 radioisotype injection. [3] There are no reported cases of parkinsonism secondary to perianeurysmal cystic expansion following coiling.
Control of cyst expansion has been attempted with a couple of approaches. Repeat surgical interventions provided complete neurologic recovery in only one patient. [1, 2, 4] Intravenous corticosteroids reduced perianeurysmal edema and a postprocedural cyst associated with chemical meningitis developing a few days after second-generation endovascular coiling for ruptured aneurysm of the posterior cerebral artery. [5] There are no additional reports of medical therapy geared at symptomatic treatment of cystic expansion after aneurysm coiling.
Aneurysms involving the middle cerebral artery, vertebral artery, [6] or posterior cerebral arteries [7] can cause secondary parkinsonism, but benefit from optimized medical therapy remains unknown. Structural lesions that impair the nigrostriatal pathway rarely produce dopa-responsive parkinsonism [8] but more commonly this type of parkinsonism has little, [9] if any, response to levodopa. [10] Here, we report a case of levodopa-responsive hemiparkinsonism resulting from midbrain compression after expansion of a coiled aneurysm with perianeurysmal cyst formation.
Case Presentation
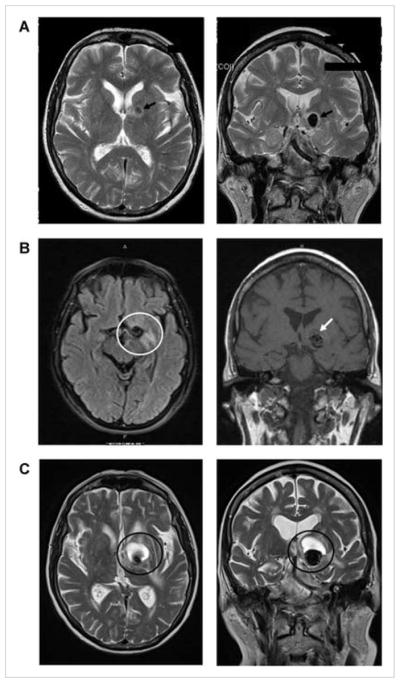
An 80-year-old right-handed woman with atrial fibrillation was examined and treated in a movement disorders clinic with botulinum injections every 3 months over 9 years for left hemifacial spasm. Development of transient roaring and reduced hearing in the left ear prompted magnetic resonance imaging (MRI; Fig 1A). A 1 cm × 1.5 cm internal carotid artery terminus aneurysm projected superiorly at the A1 location. Embolization with platinum coils (Target Therapeutics, Fremont, CA) produced a good angiographic result (Fig 2A). Routine follow-up magnetic resonance angiography (MRA) at 6 and 12 months demonstrated a stable result.
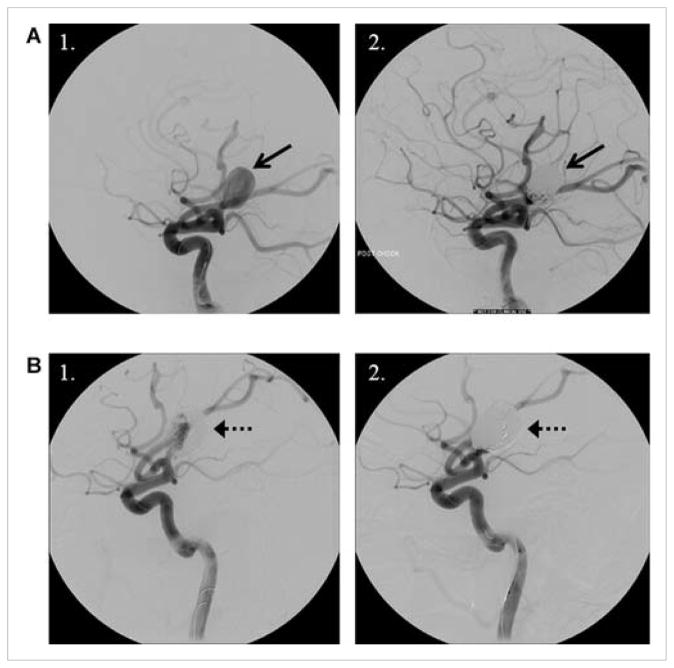
Figure 1.
Axial (left column) and coronal (right column) T2 weighted (A, C) and fluid attenuated inversion recovery (FLAIR) MRI images (B) demonstrating aneurysm evolution: (A) prior to intervention, a 12-mm left internal carotid artery terminus aneurysm (black arrows) anterior and superior to the left cerebral peduncle; (B) 14 months after endovascular coil embolization with parenchymal T2 signal hyperintensity around the left callosal and pericallosal regions of the coiled aneurysm site (white circle) and some low signal at the aneurysm apex (white arrow), above the coil mass (represented as area of signal loss) on the coronal view. Low signal is inconsistent with blood product and likely represents developing cyst (T2 images not obtained); (C) 15 months after repeat endovascular coil embolization with enlarged aneurysm and superior expansion of a cystic mass compressing internal capsule, pallidum, and some caudate (dark circles).
Figure 2.
Digital subtraction lateral projection cerebral angiography of the left common carotid artery (A) before placement of coils (1) and after successful initial coil embolization (2), and (B) before retreatment showing compaction of coils at base (1) and successful repeat coil embolization with dense packing at the neck (2). Neck remodeling was performed with a balloon across the neck during placement of coils. Microcatheter is visible in the internal carotid artery in all images. Arrows reference the aneurysm in both image sets.
Two years after coiling, repeat MRA demonstrated coil compaction, expansion of the aneurysm, and a new cystic lesion extending in the superior-medial direction. Repeat coil embolization (MicroVention, Inc., Orange, CA) provided excellent angiographic outcome (Fig 2B).
MRA 6 months following repeat coiling demonstrated stable coils, but the cystic component enlarged with inferior displacement of the aneurysm. At this time, she developed small handwriting, intermittent right foot dragging, and occasional stumbling without falls. Fifteen months after repeat coiling, she developed right-hand rest tremor. New examination findings included 5-Hz right arm resting and postural tremor, rigidity, and bradykinesia of the right upper- and lower extremities with reduced right arm swing. MRI demonstrated increased cyst volume with direct compression of the internal capsule, pallidum and some caudate, and inferior displacement of the coiled aneurysm into the ventro-lateral cerebral peduncle (Fig 1B). Carbidopa-levodopa 25–100 mg, .5 tablets TID provided dramatic improvement of parkinsonism. Symptoms progressed over 15 months along with cyst enlargement and compression of the cerebral peduncle (Fig 1C), yet increased levodopa provided additional benefit.
Discussion
The onset and progression of levodopa-responsive parkinsonism in this patient developed in conjunction with progressive perivascular cystic expansion following endovascular coil treatment of an unruptured aneurysm. The unilateral nature of the parkinsonism and temporal and spatial relationship with cystic expansion supports a causal relationship of perianeurysmal cystic expansion as opposed to idiopathic Parkinson disease. We found no other report of isolated parkinsonism secondary to development of a perianeurysmal cyst. Development of coincident idiopathic Parkinson disease beginning just at the time of the cyst expansion seems much less likely. Parkinsonism secondary to unruptured giant aneurysms is rare, but may respond to surgical excision. [11] We found no other reports of levodopa-responsive parkinsonism secondary to aneurysms.
Cystic expansion of coiled aneurysms is uncommon and may result from coil extension outside the aneurysm wall. [2] Here, we report cystic expansion of a coiled aneurysm with progressive inferior displacement of a coiled aneurysm into the ventral-lateral cerebral peduncle. Several mechanisms might contribute to parkinsonism in the current case, including altered perfusion or anatomic distortion of the striatum, cerebral peduncle, or both. Gradual symptom progression makes it less likely that the terminal portion of the aneurysm or the coiling intervention disrupted blood flow with subsequent direct injury to striatum. Postsynaptic targets of the nigrostriatal pathway were not likely the primary source of injury since she was dopa-responsive. This implies disruption of the nigrostriatal pathway with functional dopamine receptors on postsynaptic neurons.
Hemifacial spasm does not increase risk of Parkinson disease [12] although some report increased risk of hemifacial spasm in those with Parkinson disease. [13] There are no reported cases of hemifacial spasm in relation to aneurysms involving the anterior circulation, and it is unlikely the aneurysm of the anterior circulation in the current case contributed to longstanding symptomatology.
Although parkinsonism is a rare complication of aneurysm, it is important to recognize it as potentially treatable. This case adds to growing evidence that parkinsonism secondary to structural lesions involving the midbrain may respond to levodopa. Thus, therapeutic trials are warranted prior to surgical intervention in select cases. Neuro-interventionalists, neurosurgeons, neurologists, and radiologists should be aware of rare cyst expansion following aneurysm coiling, which in this case contributed to hemiparkinsonism. Previous reports of continued perianeurysmal cystic expansion indicates the need for close monitoring in this and other patients despite successful medical therapy.
References
- 1.Friedman JA, McIver JI, Collignon FP, et al. Development of a pontine cyst after endovascular coil occlusion of a basilar artery trunk aneurysm: case report. Neurosurgery. 2003;52(3):694–699. doi: 10.1227/01.neu.0000048480.41325.17. discussion 698–699. [DOI] [PubMed] [Google Scholar]
- 2.Konig M, Bakke SJ, Scheie D, et al. Reactive expansive intracerebral process as a complication of endovascular coil treatment of an unruptured intracranial aneurysm: case report. Neurosurgery. 2011;68(5):E1468–E1473. doi: 10.1227/NEU.0b013e318210c7c0. discussion E1473–1474. [DOI] [PubMed] [Google Scholar]
- 3.Grandhi R, Miller RA, Zwagerman NT, et al. J Neuroimag. Wiley Online Library; 2013. Perianeursymal cyst development after endovascular treatment of a ruptured giant aneurysm. [DOI] [PubMed] [Google Scholar]
- 4.Marcoux J, Roy D, Bojanowski MW. Acquired arachnoid cyst after a coil-ruptured aneurysm. Case illustration. J Neurosurg. 2002;97(3):722. doi: 10.3171/jns.2002.97.3.0722. [DOI] [PubMed] [Google Scholar]
- 5.Meyers PM, Lavine SD, Fitzsimmons BF, et al. Chemical meningitis after cerebral aneurysm treatment using two second-generation aneurysm coils: report of two cases. Neurosurgery. 2004;55(5):1222–1227. doi: 10.1227/01.neu.0000140987.71791.df. [DOI] [PubMed] [Google Scholar]
- 6.Bossi L, Caffaratti E. Juvenile parkinsonian hemi-syndrome in a case of extracranial arteriovenous aneurysm of the vertebral artery. Clinical and radiological study. Minerva Radiologica. 1967;12(12):533–538. [PubMed] [Google Scholar]
- 7.Bhattacharjee S, Kumar H, Tiwari M, et al. Hemiparkinsonism due to coiled posterior cerebral artery aneurysm. Can J Neurologic Sci. 2013;40(1):101–103. doi: 10.1017/s0317167100013056. [DOI] [PubMed] [Google Scholar]
- 8.Ling MJ, Aggarwal A, Morris JG. Dopa-responsive parkinsonism secondary to right temporal lobe haemorrahage. Movement Disord. 2002;17(2):402–404. doi: 10.1002/mds.10081. [DOI] [PubMed] [Google Scholar]
- 9.Lhermitte F, Agid Y, Serdaru M, et al. Parkinson syndrome, frontal tumor and L-dopa. Revue Neurolog. 1984;140(2):138–139. [PubMed] [Google Scholar]
- 10.Cicarelli G, Pellecchia MT, Maiuri F, et al. Brain stem cystic astrocytoma presenting with “pure” parkinsonism. Movement Disord. 1999;14(2):364–366. doi: 10.1002/1531-8257(199903)14:2<364::aid-mds1028>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 11.Sibon I, Rajabally Y, Tison F. Parkinsonism as a result of a giant aneurysm. Movement Disord. 1999;14(1):159–161. doi: 10.1002/1531-8257(199901)14:1<159::aid-mds1029>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 12.Tan EK, Chan LL. Exploring the relationship between Parkinson’s disease and hemifacial spasm. Acta Neurologica Scandinavica. 2006;113(5):350–352. doi: 10.1111/j.1600-0404.2006.00581.x. [DOI] [PubMed] [Google Scholar]
- 13.Miwa H, Yoritaka A, Mizuno Y. Hemifacial spasm in Parkinson’s disease. Movement Disord. 1999;14(2):358–359. doi: 10.1002/1531-8257(199903)14:2<358::aid-mds1026>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]