Abstract
Purpose
Ulnar styloid fractures commonly occur in association with distal radius fractures. Ulnar styloid fractures that involve the insertion of the radioulnar ligaments can result in distal radioulnar joint (DRUJ) instability, and the literature suggests that these fractures should be treated with open reduction internal fixation (ORIF). However, in the absence of DRUJ instability, the effects of ulnar styloid fractures are not known. The purpose of this study is to evaluate the outcome of ulnar styloid fractures without DRUJ instability on patient-rated outcomes after distal radius fracture ORIF.
Materials and Methods
Between 2003 and 2008, a prospective cohort of distal radius fracture subjects treated with volar locking plating was enrolled. Patients with DRUJ instability treated at the time of distal radius ORIF were excluded. Radiographs were evaluated to identify ulnar styloid fractures, fracture size, amount of displacement, and evidence of healing. Patient-rated outcomes were measured at 6 weeks, 3 months, 6 months, and 12 months after surgery using the Michigan Hand Outcomes Questionnaire (MHQ). Physical examination, including a specific evaluation of the DRUJ, was performed at each postoperative visit. Regression analysis was performed to determine if the presence of an ulnar styloid fracture, the size or displacement of the ulnar styloid fracture, or the healing status of the ulnar styloid fracture (union versus non-union) was predictive of MHQ scores.
Results
One hundred forty-four patients were enrolled; 88 patients had associated ulnar styloid fractures, and 56 did not. During the collection period, three patients with ulnar styloid fractures had DRUJ instability found intraoperatively and underwent ulnar styloid ORIF. These patients were excluded. The remaining patients with a stable DRUJ after ORIF were included in the study, and maintained DRUJ stability postoperatively. The presence of an ulnar styloid fracture was not found to be an independent predictor of MHQ scores (p=0.55). In addition, neither the size of the ulnar styloid fracture (p=0.18), nor the degree of displacement (p=0.25) was found to be a significant independent predictor of MHQ scores. Furthermore, the healing status of the fracture (union versus non-union) was not predictive of MHQ scores (p=0.95).
Conclusion
In patients with a stable DRUJ after distal radius ORIF with a volar locking plate, the presence of an ulnar styloid fracture did not affect subjective outcomes as measured by the MHQ. Furthermore, neither the size of the ulnar styloid fracture, the degree of displacement, nor the presence or absence of radiographic union affected subjective outcomes as measured by the MHQ.
Keywords: distal radius fracture, ulnar styloid fracture, outcomes, the Michigan Hand Outcomes Questionnaire, Volar Locking Plating System
Distal radius fractures are common, representing 1 in 6 fractures that present to the emergency department.11,17,19,21,32 Ulnar styloid fractures are often associated with fractures of the distal radius, and are present in up to 50 to 65% of these fractures.15,27,31,34,40,4 The effects of ulnar styloid fractures in the setting of distal radius fractures are unclear, and the data from the literature are contradictory. Although some studies suggest that ulnar styloid fractures have little effect on radiographic or clinical outcomes,4,23,26,28,34,35,38,40 other studies showed that these fractures can contribute to poor results, including distal radioulnar joint (DRUJ) instability, ulnar sided wrist pain, stiffness, and weakness.1,18,22,27,31,39,41
The literature suggests that certain ulnar styloid fractures that result in DRUJ instability should be treated with open reduction internal fixation (ORIF) to stabilize the DRUJ.18,37,39 But in the absence of DRUJ instability, it is not known what impact concomitant ulnar styloid fractures have on outcomes after distal radius fracture ORIF. The purpose of this study is to examine the effect of ulnar styloid fractures on patient rated outcomes in patients with a stable DRUJ after distal radius ORIF.
Materials and Methods
Between 2003 and 2008, a prospective cohort of consecutive distal radius fracture subjects was recruited in an ongoing longitudinal study to evaluate the outcomes of distal radius fracture treatment. This is an ongoing cohort study and the data for 80% of the patients in this paper were presented in an outcomes study on using the volar locking plating system.13 After closed reduction of the fractures in the emergency department, radiographic indications for ORIF of the distal radius were dorsal angulation of greater than 10 degrees, radial inclination of less than 15 degrees, radial height of less than 10 mm, or an intra-articular step-off of 2 mm or greater. Ulnar variance was not used as a criterion for ORIF. Articular diastasis alone, without step-off, was not considered an indication for ORIF.
Patients with inadequately-reduced distal radius fractures underwent ORIF using a volar locking plate (DVR® Anatomic Volar Plating System, DePuy Orthopaedics, Inc.).9,30 After fixation of the distal radius, the DRUJ was examined intra-operatively for stability. Examination of the DRUJ consisted of stabilization of the radiocarpal joint in neutral position, followed by passive dorsal and volar translation of the distal ulna. This test was performed with the forearm in neutral rotation, pronation, and supination. If there was a concern for instability, its level of stability was compared to the uninjured contralateral side. In some cases, if the contralateral DRUJ had not been carefully examined preoperatively, the surgeon changed out of gown and gloves to examine the contralateral side. If by comparison, the DRUJ of the repaired wrist was found to be unstable intraoperatively, the displaced ulnar styloid base fracture was treated with ORIF, and the triangular fibrocartilage complex (TFCC) was repaired if required. In the absence of DRUJ instability, ulnar styloid fractures were not treated, regardless of size or displacement. The patients who required ORIF of the ulnar styloid fracture because of DRUJ instability were excluded from the study.
Only patients within the prospective cohort who completed the Michigan Hand Outcomes Questionnaire (MHQ), thereby allowing an analysis of subjective outcomes, were included in this study. Exclusion criteria were pediatric age (less than 18 years of age), other concomitant upper extremity injuries, severe multi-system trauma, bilateral distal radius fractures, and fractures treated later than 2 weeks after injury. All aspects of the study were approved by the University’s institutional review board.
Post-operative rehabilitation
At one week after surgery, all patients began hand therapy as part of the standard volar locking plating system (VLPS) protocol by attending weekly sessions for 6 weeks. Therapy included edema control, active and passive finger range of motion (ROM), and active wrist ROM and forearm rotation. Patients were given a custom thermoplastic volar wrist splint and instructed to wear the splint at all times except for bathing and wrist exercises. Light activity while wearing the splint was allowed. At six weeks strengthening exercises were initiated. No distinction was made between the post- operative rehabilitation of patients with and without ulnar styloid fractures.
Radiographic measurements
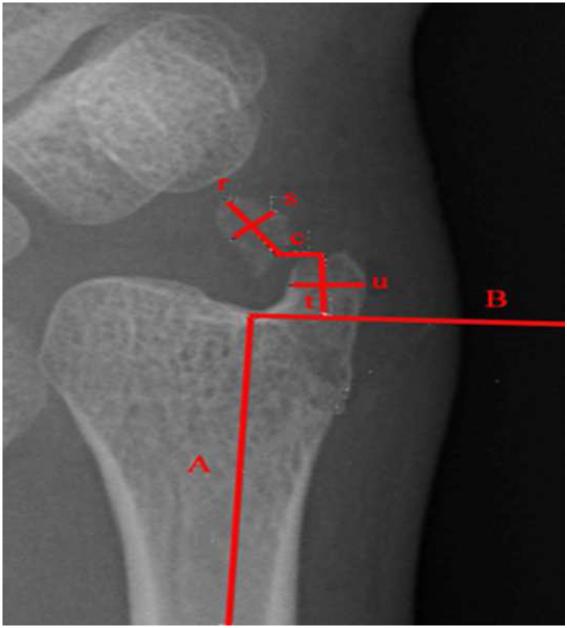
At the initial post-operative visit, posterior-anterior, lateral, and oblique wrist radiographs were taken. The presence or absence of an ulnar styloid fracture was documented. If present, the degree of displacement of the ulnar styloid fracture was measured to the nearest millimeter. In addition, the size of the fragment was measured to the nearest millimeter, and the percentage of the ulnar styloid involved with the fracture fragment was calculated. All measurements were made on the PA view of the wrist as described in Figure 1. Fracture displacement was categorized as 0 to 0.9 mm, 1 to 1.9 mm, and ≥ 2 mm. Lines s and u were drawn perpendicular to the long axes (lines r and t) at their mid-points. The size of the ulnar styloid fragment was then calculated by multiplying the lengths of lines s and r. The size of the intact remaining portion of the ulnar styloid was defined by multiplying the lengths of lines u and t. The percentage involvement of the ulnar styloid fracture was defined by the formula: 100(s × r) / [(s × r) + (u × t)]. Large fractures (those involving 75% to 100% of the ulnar styloid) were placed in one size category, and smaller fractures (those involving less than 75% of the ulnar styloid) were placed in a second size category.
Figure 1.
Measurement of ulnar styloid fracture displacement. Line A is drawn parallel to the long axis of the ulna. Line B is drawn perpendicular to line A, defining the base of the ulnar styloid. Lines t and r are drawn along the long axis of the ulnar styloid proximal and distal to the fracture respectively. Displacement is measured as the distance between the proximal end of the distal fragment, and the distal end of the proximal fragment, and is represented by line c. Lines s and u are drawn perpendicular to lines r and t at their mid-point. Fracture size is calculated by multiplying the length of lines s and r, and the size of the remaining portion of the styloid is calculated by multiplying lines u and t.
Patient-rated outcomes data collection
Patients were evaluated in clinic at 6 weeks, 3 months, 6 months, and 12 months post-operatively. Subjective outcomes were measured at each visit using the Michigan Hand Outcomes Questionnaire (MHQ).7,10 The MHQ is a patient-administered questionnaire used to evaluate the health-status domains that are important to patients with hand conditions. Its reliability and validity as well as responsiveness to clinical change have been established.7,10 It has been used to evaluate subjective outcomes in multiple disorders of the upper extremity, including distal radius fractures.6,8,9,12,24,36 The MHQ is scored on a scale from 0 to 100. The higher the score, the better the subject’s hand performance. In addition, demographic data including patient age, gender, income level, race, and level of education were recorded.6
Clinical exam
All patients were examined by their attending surgeon and by a hand-specialty physician’s assistant at 6 weeks, 3 months, 6 months, and 12 months post-operatively. The DRUJ was specifically evaluated for the presence of instability and pain. Examination included the piano key test, performed on both the injured and uninjured sides. The DRUJ was categorized as stable, lax but same as contralateral, lax, subluxable, and/or painful.
Statistical analysis
The student’s t-test was used to compare the mean patient age in the two cohorts, and the chi-square test was used to compare other demographic variables. Regression analysis was performed to test if patients with ulnar styloid fractures had different mean MHQ scores than those without ulnar styloid fractures, controlling for demographic characteristics previously found to be associated with outcomes after DRF. These potential confounders included age, gender, race (categorized into white and non-white), education level (categorized into no college, college, or professional/graduate degree), and income (categorized into $70,000 per year or $70,000 per year).
Next, ulnar styloid fractures were placed into one of two size categories (<75% of the ulnar styloid involved, and 75%-100% of the ulnar styloid involved). The fractures involving 75% or more of the ulnar styloid included those fractures at or near the base of the ulnar styloid. Fractures involving less than 75% of the ulnar styloid included those fractures distal to the base of the ulnar styloid. Regression analysis was performed to test if the size of the ulnar styloid fracture was an independent predictor of MHQ scores, controlling for the above potential confounders. Ulnar styloid fractures were then placed into one of three displacement categories (0-0.9 mm, 1-1.9 mm, and ≥2 mm). Regression analysis was performed to test if the amount of displacement was an independent predictor of MHQ scores, controlling for the above potential confounders. Finally, fractures were categorized as “radiographic union present” versus “no radiographic union” based upon their final available radiographs. Regression analysis was performed to test if the presence of ulnar styloid non-union had an effect on MHQ scores, controlling for the above potential confounders.
Power analysis was performed demonstrating sufficient power from this sample size to detect a 10-point difference between the MHQ means at 3 months (the time-point at which there was the greatest number of observations), with a power of 0.85. Statistical significance was set at a p-value of 0.05.
Results
Based upon the inclusion and exclusion criteria described above, 144 patients were included in the study. During the collection period 3 patients underwent ORIF of displaced ulnar styloid base fractures at the time of distal radius ORIF because of DRUJ instability. These patients were not included in the study. Eighty-eight of the 144 patients (61%) had associated ulnar styloid fractures, and 56 patients (39%) did not. The demographic and injury characteristics of the 144 study participants are provided in Tables I and II. At the 6-week follow-up point 40 of 144 patients were evaluated (28%). At the 3-month follow-up point 108 patients were evaluated (75%). At the 6-month follow-up point 91 patients were evaluated (63%), and at the 12-month follow-up point 59 patients were evaluated (41%). Initially, the follow-up appointments included the 3, 6, and 12 months points. However, we noted that patients reached 80 points on the MHQ at the 3 month time point. Because of the rapid improvement, we started to assess the patients at the 6 week time point to understand patients’ recovery pattern before the 3 month period. Therefore, 28% of the patients in this cohort were evaluated at 6 weeks. Over the course of the study, twenty-eight ulnar styloid fractures (32%) demonstrated radiographic evidence of union, with bridging trabeculae at the fracture site. None of the patients demonstrated instability of the DRUJ (other than laxity equal to the uninjured contralateral side) at any time-point post-operatively. One patient did have pain but no instability with testing of the DRUJ.
Table I.
Patient Demographics
| Parameter | US Fracture Present |
No US Fracture | P-value* |
|---|---|---|---|
| No. of patients enrolled |
88 | 56 | N/A |
| Age (range) | 49 (18-86) | 52 (18-83) | 0.28 |
| Male | 32 (36%) | 16 (29%) | 0.33 |
| Right hand dominant |
82 (93%) | 53 (95%) | 0.72 |
| Dominant hand injured |
44 (50%) | 21 (38%) | 0.14 |
| Caucasian | 80 (91%) | 51 (91%) | 0.97 |
| Education level** | 0.54 | ||
| No college | 19 (22%) | 9 (16%) | |
| College | 39 (44%) | 28 (50%) | |
| Graduate degree | 23 (26%) | 19 (34%) | |
| Income level** | 0.11 | ||
| <$70,000 | 46 (52%) | 24 (43%) | |
| ≥$70,000 | 30 (34%) | 28 (50%) |
N/A, not applicable
Based on student's t-test for age, and chi-square test for all other variables
Nine patients in the "US fracture present" cohort did not respond to the question regarding education level. Ten patients in the "US fracture present" cohort and 4 patients in the "no US fracture" cohort did not respond to the question regarding income level. This resulted in 13 patients in the "US fracture present" cohort and 4 patients in the "no US fracture" cohort with incomplete information on potential confounders. These patients were not included in regression analysis.
Table II.
Distal Radius Fracture Types
| AO Classification | Number of Patients | |
|---|---|---|
| No US Fracture | US Fracture Present | |
| Type A | 26 | 47 |
| Type B | 5 | 11 |
| Type C | 25 | 30 |
|
Sigmoid Notch
Involvement |
41 | 73 |
Although both cohorts demonstrated an improvement in mean MHQ scores over time, the presence of an ulnar styloid fracture was not found to be an independent predictor of MHQ scores, adjusting for other covariates (p=0.55). Table III provides the mean MHQ scores of both cohorts at each time-point.
Table III.
The Effect of Styloid Fractures
| US Fracture Present |
No. Patients |
MHQ Scores* | |||
|---|---|---|---|---|---|
| 6 weeks | 3 months | 6 months | 12 months | ||
| Yes | 75 | 66 ± 20 | 79 ± 16 | 83 ± 16 | 83 ± 18 |
| No | 52 | 61 ± 21 | 78 ± 17 | 83 ± 16 | 90 ± 11 |
Values given as mean ± standard deviation
Note: on regression analysis (n=127 patients), the presence of an ulnar styloid fracture was not a significant independent predictor of MHQ scores, adjusting for other covariates (p=0.55).
In patients with ulnar styloid fractures, the degree of displacement was not found to be an independent predictor of MHQ scores, adjusting for other covariates (p=0.25). Furthermore, fracture size was not found to be a significant independent predictor of MHQ scores, adjusting for other covariates (p=0.18). Tables IV and V provide the mean MHQ scores for each displacement category and size category over time. Finally, the healing status of the fracture (union versus nonunion) was not a significant independent predictor of MHQ scores (p=0.95).
Table IV.
Ulnar Styloid Fracture Displacement
| US Fracture Displacement |
No. Patients** |
MHQ Scores* | |||
|---|---|---|---|---|---|
| 6 weeks | 3 months | 6 months | 12 months | ||
| 0-0.9 mm | 19 | 56 ± 27 | 83 ± 12 | 80 ± 18 | 89 ± 12 |
| 1-1.9 mm | 21 | 71 ± 14 | 84 ± 13 | 88 ± 15 | 82 ± 25 |
| ≥2 mm | 26 | 72 ± 18 | 75 ± 18 | 82 ± 17 | 82 ± 15 |
Values given as mean ± standard deviation
In 9 patients, the degree of displacement could not be reliably measured
Note: on regression analysis (n=66), the degree of displacement was not a significant independent predictor of MHQ scores, adjusting for other covariates (p=0.25).
Table V.
Ulnar Styloid Fracture Size
| Percent of styloid involved |
No. Patients** | MHQ Scores* | |||
|---|---|---|---|---|---|
| 6 weeks | 3 months | 6 months | 12 months | ||
| <75% | 26 | 69 ± 14 | 80 ± 13 | 89 ± 10 | 85 ± 13 |
| 75 to 100% | 47 | 64 ± 24 | 79 ± 17 | 82 ± 17 | 82 ± 20 |
Values given as mean ± standard deviation
In 2 patients, the size of the fracture could not be reliably measured
Note: on regression analysis (n=73), fracture size was not a significant independent predictor of MHQ scores (p=0.18).
With the exception of income level, none of the potential confounders was a predictor of MHQ score. Those with an annual income of less than $70,000 were predicted to have a mean MHQ score 9 points lower than those with an annual income greater than $70,000 (p=0.0003). However, there was not a statistically significant difference in the income level categories of the two cohorts (Table I).
Discussion
The ulnar styloid plays a crucial role in wrist biomechanics. The ulnar styloid base and the fovea are the insertion points for the primary stabilizers of the DRUJ, the superficial and deep portions of the palmar and dorsal radioulnar ligaments.20,29,33 In addition, the ulnar styloid functions as a strut, helping to stabilize the extensor carpi ulnaris (ECU), its sub-sheath, and the ulnocarpal ligaments.18 Because of its anatomic importance, the potential exists for ulnar styloid fractures to cause ulnar-sided wrist symptoms. However, the clinical significance of ulnar styloid fractures in association with distal radius fractures is not clear. Although some investigators have found no correlation between outcomes and the presence of ulnar styloid fractures,3,4,23,25,26,28,34,35,38,40 others have noted that ulnar styloid fractures can have a negative impact on outcomes after distal radius fracture.1,18,22,27,31,39,41
Early reports of distal radius fractures in the mid-1900’s suggested that concomitant ulnar styloid fractures did not affect outcomes,3,25 and many subsequent studies supported those conclusions. In 1985 Stewart et al. reviewed the outcomes of 235 patients with extra-articular distal radius fractures, and did not find a correlation between ulnar styloid fracture and function.38 In 1993, Roysam evaluated 170 patients with Colles’ fractures who were treated non-operatively. He was unable to detect a difference in functional outcomes in patients with concomitant ulnar styloid fractures to those without fractures.35 In 1997 Catalano et al. evaluated 21 patients with distal radius fractures at an average of 7.5 years follow-up. There was no difference in function between patients with ulnar styloid non-unions and those without, suggesting that the presence of an ulnar styloid non-union plays little role in functional outcomes after distal radius fracture.4 The same year, Richards et al. arthroscopically evaluated 118 distal radius fractures and found no correlation between ulnar styloid fractures and TFCC tears, suggesting that an ulnar styloid fracture is not a predictor of ligamentous injury.34 Further support for the benign nature of ulnar styloid fractures was provided in 2000 when Lindau et al. retrospectively evaluated 76 patients with distal radius fractures. They noted that although patients with DRUJ instability had worse objective and subjective wrist function than patients without instability, DRUJ instability did not correlate with the presence of an ulnar styloid fracture.26,28
However, over the same period of time, other investigators came to the opposite conclusion. In 1967 Frykman suggested that fractures of the ulnar styloid substantially affect the outcomes of distal radius fractures, and included the ulnar styloid in his distal radius fracture classification system.15 In 1988 Kaukonen et al. reported a series of 207 consecutive patients with distal radius fractures treated both operatively and non- operatively, and concluded that fractures of the ulnar styloid contributed to poor results.22,23 In 1997 Oskarsson et al. evaluated 158 patients with Colles’ fracture treated with cast immobilization, and found that a fracture of the ulnar styloid was a more important predictor of fracture stability and functional outcome than articular involvement.31
A number of authors have emphasized the correlation between ulnar styloid fractures and DRUJ instability. In 1996 Hauck et al. published an anatomic study of ulnar styloid non-unions. They noted that because the stabilizing ligaments of the DRUJ insert on the ulnar styloid base, two clinically distinct types of ulnar styloid fracture non- union can occur. In their classification system, a type I ulnar styloid fracture non-union is associated with a stable DRUJ, because it does not involve the insertion of the radioulnar ligaments. On the other hand, a type II fracture non-union (a large fracture at the ulnar styloid base) may result in DRUJ instability because the fracture fragment includes the insertion of the radioulnar ligaments. The authors emphasized the importance of examining all distal radius fractures for the presence of DRUJ instability, and recommended ORIF of the ulnar styloid in type II fracture non-unions.18 Similarly, Shaw et al. demonstrated that fixation of the ulnar styloid could successfully restore DRUJ stability in patients with TFCC-ulnar styloid avulsion fractures, and also recommended ORIF of displaced ulnar styloid fractures as a means of stabilizing the DRUJ.37 Later, Stoffelen et al. prospectively evaluated 272 distal radius fractures. In addition to concluding that ulnar styloid fractures correlate statistically with poor outcomes, they noted that all patients with DRUJ instability also had concomitant ulnar styloid fractures, further demonstrating the importance of the ulnar styloid in stabilizing the DRUJ.39
The findings of the above studies suggest that ulnar styloid fractures that result in DRUJ instability should be treated with ORIF. However, most ulnar styloid fractures do not result in DRUJ instability, and the clinical importance of an ulnar styloid fracture in the setting of a stable DRUJ remains unclear. Apart from DRUJ instability, ulnar styloid fractures can cause other problems. Non-union occurs in approximately 25 percent of ulnar styloid fractures.2 Although non-unions are asymptomatic the majority of the time,14,16 they can be a source of focal pain on the ulnar side of the wrist, resulting in clicking, grating, and pain to palpation.18 In addition, an ununited ulnar styloid fragment can act as an irritative loose body, resulting in stylocarpal impaction and focal chondromalacia of the triquetrum.5 Ulnar styloid malunions can be problematic as well. For example, a severely malunited ulnar styloid can impinge on the ECU subsheath,18 causing discomfort or tendonitis. Finally, some authors have suggested that the presence of an ulnar styloid fracture serves as a marker for more severe osseous and soft tissue injuries, and predicts worse radiographic and clinical outcomes.31
Clearly, some ulnar styloid fractures do result in DRUJ instability, and we believe that the literature supports treating these fractures with ORIF. The question we attempted to answer in this study was: if the DRUJ is stable, what effect, if any, does an ulnar styloid fracture have on subjective outcomes? The results of this study suggest that despite the potential problems associated with ulnar styloid fractures, in patients with a stable DRUJ, ulnar styloid fractures do not affect subjective outcomes after distal radius ORIF, regardless of size, displacement, or ulnar styloid healing status.
This study has some potential limitations. Data were not collected beyond 12 months after surgery. It is possible that significant changes in MHQ scores would have occurred after one year had these patients been followed for a longer period of time. However, the mean MHQ scores approached the normal range and appeared relatively stable by one year after surgery, suggesting that further significant changes were unlikely. Another potential limitation is that although the study is powered to detect a 10-point difference in MHQ scores at 3 months post-operatively, it may have insufficient power to detect this difference at other time points, or to detect smaller differences in MHQ scores. However, because a difference in MHQ scores of less than 10 points is not clinically significant, this is likely not a substantial limitation. In addition, it should be noted that the findings of this study are limited to patients who have a stable DRUJ after distal radius fracture ORIF with a volar locking plate. The findings of this study may not be generalizable to patients treated non-operatively, or to patients treated by other surgical techniques such as external fixation, percutaneous pinning, or dorsal plating. The findings are also not applicable to patients with instability of the DRUJ after distal radius ORIF.
Another important question is whether the MHQ is an appropriate instrument for measuring subjective outcomes in patients with distal radius fractures. The MHQ has been specifically evaluated for use in the treatment of distal radius fractures, and along with physical tests (grip, pinch, Jebsen-Taylor test, range-of-motion) has been found to be a responsive measure of outcomes (in other words was able to detect meaningful differences and changes, when compared to other physical measurements).(28) Although the use of the MHQ for evaluating ulnar sided wrist problems has not been specifically evaluated, we believe that it is an appropriate instrument for the purpose of the study, which was to evaluate patient rated outcomes after distal radius fracture ORIF.
In patients who have a stable DRUJ after distal radius fracture ORIF with a volar locking plate, associated ulnar styloid fractures do not affect subjective outcomes as measured by the MHQ, regardless of ulnar styloid fracture size, degree of displacement, or the presence or absence of non-union.
Table VI.
Ulnar Styloid Union
| Union | No. Patients | MHQ Scores* | |||
|---|---|---|---|---|---|
| 6 weeks | 3 months | 6 months | 12 months | ||
| Yes | 24 | 54 ± 19 | 80 ± 14 | 83 ± 16 | 84 ± 17 |
| No | 51 | 73 ± 18 | 78 ± 17 | 84 ± 16 | 83 ± 19 |
Values given as mean ± standard deviation
Note: on regression analysis (n=75), union was not a significant independent predictor of MHQ scores (p=0.95).
Acknowledgments
The authors would like to thank Ann Haas, MPH for her contributions to the statistical analysis in this project. This project is supported in part by a Midcareer Investigator Award in Patient- Oriented Research (K24 AR053120), and an Exploratory/Developmental Research Grant Award (R21 AR056988) (To Dr. Kevin C. Chung)
References
- 1.af Ekenstam F, Jakobsson OP, Wadin K. Repair of the triangular ligament in Colles' fracture. No effect in a prospective randomized study. Acta Orthop Scand. 1989;60(4):393–6. doi: 10.3109/17453678909149304. [DOI] [PubMed] [Google Scholar]
- 2.Bacorn RW, Kurtzke JF. Colles' fracture; a study of two thousand cases from the New York State Workmen's Compensation Board. J Bone Joint Surg Am. 1953;35-A(3):643–58. [PubMed] [Google Scholar]
- 3.Castaing J. [Recent Fractures of the Lower Extremity of the Radius in Adults.] Rev Chir Orthop Reparatrice Appar Mot. 1964;50:581–696. [PubMed] [Google Scholar]
- 4.Catalano LW, 3rd, Cole RJ, Gelberman RH, Evanoff BA, Gilula LA, Borrelli J., Jr. Displaced intra-articular fractures of the distal aspect of the radius. Long-term results in young adults after open reduction and internal fixation. J Bone Joint Surg Am. 1997;79(9):1290–302. doi: 10.2106/00004623-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Cerezal L, del Pinal F, Abascal F, Garcia-Valtuille R, Pereda T, Canga A. Imaging findings in ulnar-sided wrist impaction syndromes. Radiographics. 2002;22(1):105–21. doi: 10.1148/radiographics.22.1.g02ja01105. [DOI] [PubMed] [Google Scholar]
- 6.Chung KC. Website title: Michigan Hand Outcomes Questionnaire. University of Michigan Department of Surgery; 2006. URL: http://sitemaker.umich.edu/mhq/overview. [Google Scholar]
- 7.Chung KC, Hamill JB, Walters MR, Hayward RA. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999;42(6):619–22. doi: 10.1097/00000637-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Chung KC, Kotsis SV, Kim HM. Predictors of functional outcomes after surgical treatment of distal radius fractures. J Hand Surg [Am] 2007;32(1):76–83. doi: 10.1016/j.jhsa.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Chung KC, Petruska EA. Treatment of unstable distal radial fractures with the volar locking plating system. Surgical technique. J Bone Joint Surg Am. 2007;89(Suppl 2):256–66. doi: 10.2106/JBJS.G.00283. Pt.2. [DOI] [PubMed] [Google Scholar]
- 10.Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg [Am] 1998;23(4):575–87. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 11.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg [Am] 2001;26(5):908–15. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 12.Chung KC, Squitieri L, Kim HM. Comparative outcomes study using the volar locking plating system for distal radius fractures in both young adults and adults older than 60 years. J Hand Surg [Am] 2008;33(6):809–19. doi: 10.1016/j.jhsa.2008.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg. 2006;88A(12):2687–94. doi: 10.2106/JBJS.E.01298. [DOI] [PubMed] [Google Scholar]
- 14.Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg [Am] 1991;16(3):375–84. doi: 10.1016/0363-5023(91)90001-r. [DOI] [PubMed] [Google Scholar]
- 15.Frykman G. Fracture of the distal radius including sequelae--shoulder-hand- finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function. A clinical and experimental study. Acta Orthop Scand: Suppl. 1967;108:1–155. doi: 10.3109/ort.1967.38.suppl-108.01. [DOI] [PubMed] [Google Scholar]
- 16.Geissler WB, Fernandez DL, Lamey DM. Distal radioulnar joint injuries associated with fractures of the distal radius. Clin Orthop Relat Res, . 1996;(327):135–46. doi: 10.1097/00003086-199606000-00018. [DOI] [PubMed] [Google Scholar]
- 17.Golden GN. Treatment and prognosis of Colles' fracture. Lancet. 1963;1(7280):511–5. doi: 10.1016/s0140-6736(63)91321-7. [DOI] [PubMed] [Google Scholar]
- 18.Hauck RM, Skahen J, 3rd, Palmer AK. Classification and treatment of ulnar styloid nonunion. J Hand Surg [Am] 1996;21(3):418–22. doi: 10.1016/S0363-5023(96)80355-8. [DOI] [PubMed] [Google Scholar]
- 19.Hollingsworth R, Morris J. The importance of the ulnar side of the wrist in fractures of the distal end of the radius. Injury. 1976;7(4):263–6. doi: 10.1016/s0020-1383(75)80004-0. [DOI] [PubMed] [Google Scholar]
- 20.Ishii S, Palmer AK, Werner FW, Short WH, Fortino MD. An anatomic study of the ligamentous structure of the triangular fibrocartilage complex. J Hand Surg [Am] 1998;23(6):977–85. doi: 10.1016/S0363-5023(98)80003-8. [DOI] [PubMed] [Google Scholar]
- 21.Jupiter JB, Lipton H. The operative treatment of intraarticular fractures of the distal radius. Clin Orthop Relat Res, . 1993;(292):48–61. [PubMed] [Google Scholar]
- 22.Kaukonen JP, Karaharju EO, Porras M, Luthje P, Jakobsson A. Functional recovery after fractures of the distal forearm. Analysis of radiographic and other factors affecting the outcome. Ann Chir Gynaecol. 1988;77(1):27–31. [PubMed] [Google Scholar]
- 23.Kaukonen JP, Porras M, Karaharju E. Anatomical results after distal forearm fractures. Ann Chir Gynaecol. 1988;77(1):21–6. [PubMed] [Google Scholar]
- 24.Kotsis SV, Lau FH, Chung KC. Responsiveness of the Michigan Hand Outcomes Questionnaire and physical measurements in outcome studies of distal radius fracture treatment. J Hand Surg [Am] 2007;32(1):84–90. doi: 10.1016/j.jhsa.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 25.Lidstrom A. Fractures of the distal end of the radius. A clinical and statistical study of end results. Acta Orthop Scand Suppl. 1959;41:1–118. [PubMed] [Google Scholar]
- 26.Lindau T, Adlercreutz C, Aspenberg P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg [Am] 2000;25(3):464–8. doi: 10.1053/jhsu.2000.6467. [DOI] [PubMed] [Google Scholar]
- 27.Lindau T, Arner M, Hagberg L. Intraarticular lesions in distal fractures of the radius in young adults. A descriptive arthroscopic study in 50 patients. J Hand Surg [Br] 1997;22(5):638–43. doi: 10.1016/s0266-7681(97)80364-6. [DOI] [PubMed] [Google Scholar]
- 28.Lindau T, Hagberg L, Adlercreutz C, Jonsson K, Aspenberg P. Distal radioulnar instability is an independent worsening factor in distal radial fractures. Clin Orthop Relat Res, . 2000;(376):229–35. doi: 10.1097/00003086-200007000-00031. [DOI] [PubMed] [Google Scholar]
- 29.Mikic ZD. Detailed anatomy of the articular disc of the distal radioulnar joint. Clin Orthop Relat Res. 1989;(245):123–32. [PubMed] [Google Scholar]
- 30.Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg [Am] 2002;27(2):205–15. doi: 10.1053/jhsu.2002.32081. [DOI] [PubMed] [Google Scholar]
- 31.Oskarsson GV, Aaser P, Hjall A. Do we underestimate the predictive value of the ulnar styloid affection in Colles fractures? Arch Orthop Trauma Surg. 1997;116(6-7):341–4. doi: 10.1007/BF00433986. [DOI] [PubMed] [Google Scholar]
- 32.Owen RA, Melton LJ, 3rd, Johnson KA, Ilstrup DM, Riggs BL. Incidence of Colles' fracture in a North American community. Am J Public Health. 1982;72(6):605–7. doi: 10.2105/ajph.72.6.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Palmer AK, Werner FW. The triangular fibrocartilage complex of the wrist--anatomy and function. J Hand Surg [Am] 1981;6(2):153–62. doi: 10.1016/s0363-5023(81)80170-0. [DOI] [PubMed] [Google Scholar]
- 34.Richards RS, Bennett JD, Roth JH, Milne K., Jr. Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg [Am] 1997;22(5):772–6. doi: 10.1016/S0363-5023(97)80068-8. [DOI] [PubMed] [Google Scholar]
- 35.Roysam GS. The distal radio-ulnar joint in Colles' fractures. J Bone Joint Surg Br. 1993;75(1):58–60. doi: 10.1302/0301-620X.75B1.8421035. [DOI] [PubMed] [Google Scholar]
- 36.Sammer DM, Kawamura K, Chung KC. Outcomes using an internal osteotomy and distraction device for corrective osteotomy of distal radius malunions requiring correction in multiple planes. J Hand Surg [Am] 2006;31(10):1567–77. doi: 10.1016/j.jhsa.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 37.Shaw JA, Bruno A, Paul EM. Ulnar styloid fixation in the treatment of posttraumatic instability of the radioulnar joint: a biomechanical study with clinical correlation. J Hand Surg [Am] 1990;15(5):712–20. doi: 10.1016/0363-5023(90)90142-e. [DOI] [PubMed] [Google Scholar]
- 38.Stewart HD, Innes AR, Burke FD. Factors affecting the outcome of Colles' fracture: an anatomical and functional study. Injury. 1985;16(5):289–95. doi: 10.1016/0020-1383(85)90126-3. [DOI] [PubMed] [Google Scholar]
- 39.Stoffelen D, De Smet L, Broos P. The importance of the distal radioulnar joint in distal radial fractures. J Hand Surg [Br] 1998;23(4):507–11. doi: 10.1016/s0266-7681(98)80134-4. [DOI] [PubMed] [Google Scholar]
- 40.Tsukazaki T, Iwasaki K. Ulnar wrist pain after Colles' fracture. 109 fractures followed for 4 years. Acta Orthop Scand. 1993;64(4):462–4. doi: 10.3109/17453679308993668. [DOI] [PubMed] [Google Scholar]
- 41.Villar RN, Marsh D, Rushton N, Greatorex RA. Three years after Colles' fracture. A prospective review. J Bone Joint Surg Br. 1987;69(4):635–8. doi: 10.1302/0301-620X.69B4.3611172. [DOI] [PubMed] [Google Scholar]