Abstract
Hepatic Pulmonary Fusion is extremely rare with only 9 previous cases reported in the literature. In typical cases, the clinician should be alerted to the possibility of hepatic pulmonary fusion if the chest radiograph shows a large opacity on the right side without a contralateral mediastinal shift. The authors present a case of right sided diaphragmatic hernia and hepatic pulmonary fusion with associated contralateral mediastinal shift discovered beyond the neonatal period. The nine previous cases were retrospectively reviewed with special attention to mediastinal shift on preoperative chest radiograph, operative procedure and mortality. Only one previous case demonstrated a contralateral mediastinal shift. The most common procedure performed was partial separation of the hepatic pulmonary fusion and approximation of the diaphragmatic defect. Four of the previous 9 cases died. In our case, reduction of bowel and approximation of the diaphragmatic defect around the fused liver and lung has been successful.
Keywords: Diaphragmatic Hernia, Hepatic Pulmonary Fusion, Mediastinal Shift
Introduction
Approximately 15% of congenital diaphragmatic hernias (CDH) occur on the right side. [1] These patients often do not demonstrate respiratory distress, which likely accounts for their delayed presentation and diagnosis. [2] Liver parenchyma is the most common organ to herniate through the defect. In rare instances, fusion occurs between the liver and hypoplastic lung, known as hepatic pulmonary fusion and may be encountered at operative exploration of the right sided CDH. Only 9 previous cases of hepatic pulmonary fusion have been reported in the literature. [3–6] Chest radiographs show a right sided diaphragmatic hernia without mediastinal shift. [4] Repair of the defect with incorporation of the hepatic pulmonary fusion or diaphragm repair following separation of the fused organs have each been proposed to manage the condition. We describe a recent case of hepatic pulmonary fusion that presented beyond the neonatal period. We also present a meta-analysis of previous reports of hepatic pulmonary fusion in the literature with special attention to mediastinal shift, operative procedure and mortality.
Case Report
A full term infant boy presented at 3 months of age with a dry cough. A chest radiograph revealed a right-sided diaphragmatic hernia with bowel in the thorax and mediastinal shift to the contralateral side. (Figure 1a) Thoracoscopy was performed, however, after placement of a 5mm port in the right 4th intercostal space in the mid-axillary line, no intrapleural anatomy was identified. A second port was placed in the 5th intercostal space and a mesothelial lined cavity was seen, however we again found no identifiable lung tissue. A limited thoracotomy was performed through the 7th intercostal space. The diaphragm was identified laterally. The mesothelial cavity previously seen was entered without any lung tissue being identified. Frozen section of the mesothelial tissue revealed pulmonary parenchyma. The bowel was reduced into the abdomen and the diaphragmatic defect was closed with interrupted permanent suture. The patient had a smooth post-operative course and subsequently did well. Final pathology report described the mesothelial tissue as dysplastic lung with attached diaphragmatic hernia sac.
Figure 1.
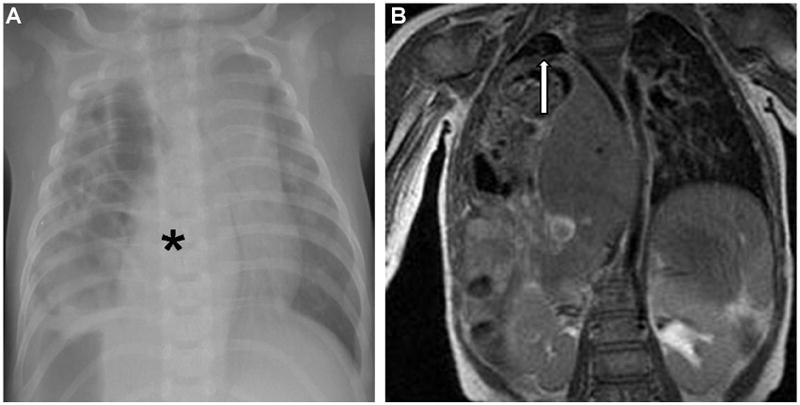
Figure 1A – Chest radiograph at time of presentation demonstrated a right sided diaphragmatic hernia with bowel in right chest and contralateral mediastinal shift. Black asterisk denotes liver in thorax.
Figure 1B – Coronal magnetic resonance image of patient’s chest. In right chest, liver is seen herniating and area of fusion to underdeveloped right lung is denoted by white arrow.
Due to concern that the mesothelial tissue was a congenital cystic adenomatoid malformation or a pulmonary sequestration, a magnetic resonance image (MRI) of the chest was obtained. This revealed right lobe of the liver and loops of bowel herniated into the right chest along with a minimal amount of right lung parenchyma. (Figure 1b)
The patient was returned to the operating room for definitive repair at age 11 months. A right subcostal incision was used and a large postero-lateral defect in the diaphragm was identified. A portion of transverse colon protruded through the defect into the chest. Once the bowel was reduced it became apparent that the right lobe of the liver was adherent to the inferior portion of the lung remnant. (Figure 2a) A polytetraflouroethylene (PTFE) patch was used to repair the defect laterally except in the area that the liver was fused to the lung. A strip of polyester fiber mesh was then sewn from the PTFE patch to the capsule of the liver. (Figure 2b) The post-operative course was uneventful. He was discharged on post-operative day #3, tolerating a regular diet. Follow up at 7 months found him to be asymptomatic. (Figure 3)
Figure 2.
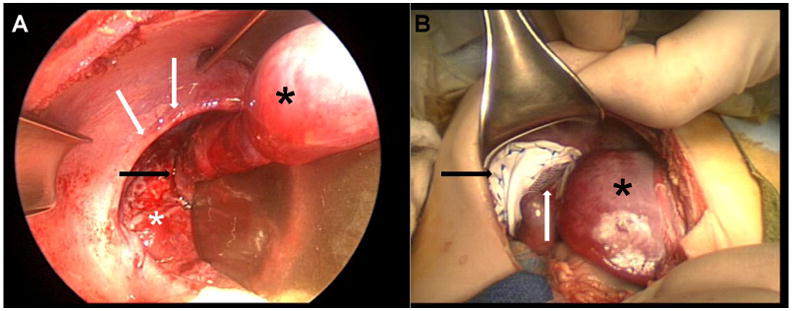
Figure 2A – View from abdomen. Black arrow denotes site of hepatic pulmonary fusion. White arrows show border of diaphragmatic defect. White asterisk on lung and black asterisk on liver. Retractor is seen at right side of image.
Figure 2B – After approximation of diaphragmatic defect. Black asterisk is liver, black arrow is PTFE mesh and white arrow is polyester fiber mesh connecting liver to the PTFE patch.
Figure 3.
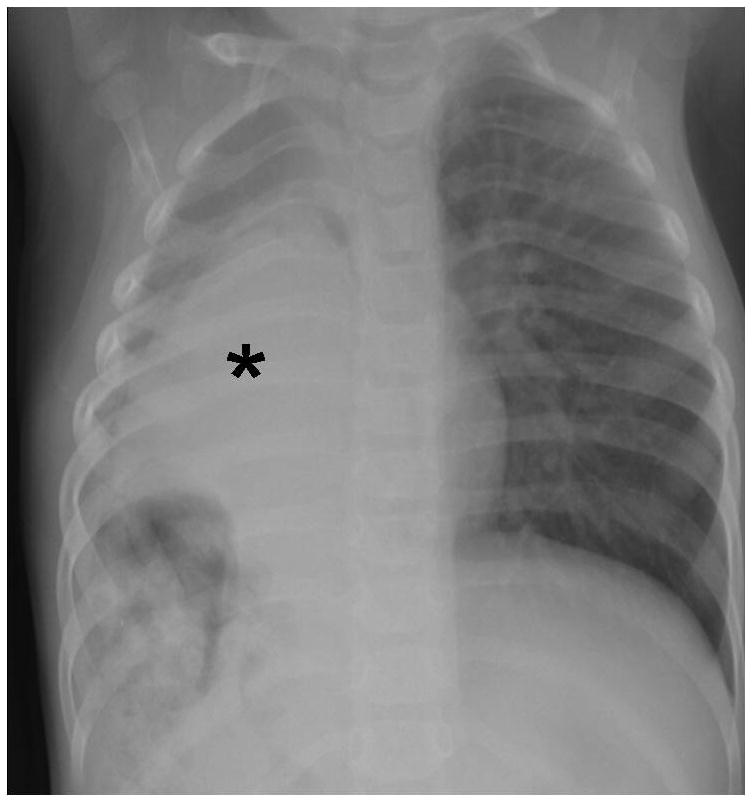
Post operative chest radiograph demonstrating bowel contents reduced into the abdomen. Black asterisk denotes liver persistently in right chest.
Materials and Methods
A PubMed and Medline search was performed using the terms “hepatic pulmonary fusion” and “hepatiocopulmonary fusion”. The papers were examined for mediastinal shift on the chest radiograph, surgical procedure and outcome.
Results
Four articles with a total of 9 cases of hepatic pulmonary fusion were discovered. (Table 1) Six of 7 cases (85%) reported either an ipsilateral or no mediastinal shift. The most common operative procedure (77%) was a partial separation of the fused organs and approximation of the diaphragmatic defect. Overall mortality was 44%. We were unable to determine mortality by surgical procedure, as the article by Slovis et al., did not individually specify the surgical procedure in each of its 6 cases.
Table 1.
| Paper | # of patients | Mediastinal Shift | Operation | Mortality |
|---|---|---|---|---|
| Katz et al., 1998 | 1 | Not indicated | Partial seperation, approximation of defect | 100% |
| Slovis et al., 2000 | 6 | 4 towards ipsilateral side, 1 without shift, 1 towards contralateral side | 4 with seperation and repair 2 without seperation |
33% |
| Keller et al., 2002 | 1 | No shift | Partial Lung resection | 0% |
| Robertson et al., 2006 | 1 | Not indicated | Partial seperation, approximation of defect | 100% |
Discussion
Liver parenchyma may be located above the diaphragm in three instances: a right sided CDH with liver protruding through the defect, an ectopic liver nodule connected to the main body of the liver or an interspersion of the supradiaphragmatic liver and lung, known as hepatic pulmonary fusion. [4]
Development of hepatic pulmonary fusion in-utero is not well understood. Failure of formation of the embryonic diaphragm allows the liver to herniate into the thorax during the 10th week of gestation. Later in development, the liver may then fuse to the primitive lung. Conversely, hepatic pulmonary fusion may be a primary anomaly which then “prevents” the diaphragm from forming properly. [5]
The lung on the fused side is usually hypoplastic and systemic arterial and venous vessels will often be seen supplying and draining the fused lung tissue. [4] Because of this observation, some authors have suggested that hepatic pulmonary fusion may have a relationship to pulmonary sequestration. [4]
All 9 previously reported patients with hepatic pulmonary fusion presented in the neonatal period. In contrast, our patient was asymptomatic until 3 months of age. The most common presenting symptom reported was respiratory distress. [3–6]
Postnatal diagnosis of CDH is made on chest radiograph, but hepatic pulmonary fusion may be difficult to recognize on a plain film. The diagnosis of hepatic pulmonary fusion should be considered if the patient has a large opacity in the right hemithorax without a mediastinal shift to the contralateral side. This is believed due to the concomitant pulmonary hypoplasia on the affected side. [4] The difficulty in making the correct diagnosis in the present case was that the chest radiograph demonstrated a mediastinal shift to the contralateral side. The size of the diaphragmatic defect may contribute to the mediastinal shift. Only one other case in the Slovis et al series of patients with hepatic pulmonary fusion had a contralateral mediastinal shift and in that instance, the defect was reported to be large. [4] In our case, there was a significant amount of bowel in the chest with a relatively large diaphragmatic defect. Although this was noted in only 2 cases, it suggests that the size of the defect and possibly the amount of herniated bowel may then cause contralateral mediastinal shift, despite hepatic pulmonary fusion being present.
MRI has been suggested as a useful diagnostic imaging technique in instances of hepatic pulmonary fusion. Keller et al, described a case in which tissue that resembled atelectatic lung conformed to the shape of the liver contour. The lung parenchyma had venous drainage to the intrahepatic inferior vena cava. The authors suggested that this finding may be diagnostic of hepatic pulmonary fusion. [5] In our case, the MRI did not reveal systemic drainage, but the hypoplastic lung was seen in close proximity of the herniated liver. When a CDH is discovered on a prenatal ultrasound study, it is now more common that a fetal MRI is also performed. Perhaps increased use of this modality will be able to identify instances of hepatic pulmonary fusion prior to postnatal operative exploration. The finding of hepatic veins draining directly into the right atrium as seen on echocardiography may also be diagnostic of hepatic pulmonary fusion.
The objectives of surgical repair in a patient with CDH are to reduce abdominal contents and repair the diaphragmatic defect. Of the 9 cases reported, 4 had separation of the lung and liver, 1 other case had attempted separation of the organs with a Ligasure® device (Valley Lab, Boulder, CO) and in another case, attempted blunt dissection created a large air leak. [3, 4] Slovis et al. described two cases in whom the defect was repaired without separation of the fused tissue. [4] In our case, the defect was approximated around the hepatic pulmonary fusion. We chose to use polyester fiber mesh on the liver capsule with the hope that this would result in an inflammatory reaction that might incorporate the patch more securely than would occur with a PTFE mesh. The patient has had neither significant complications from the repair nor evidence of respiratory symptoms.
Of the 9 cases described in the literature, four died, but the mortality does not appear to relate to the type of operative repair. The 4 reported deaths were attributed to complications of a congenital cardiac lesion, severe pulmonary hypertension, persistent fetal circulation and an unknown reason immediately post-operatively. [3–6] Long term consequences of this condition are not known, but it is reasonable to assume that these children may develop scoliosis due to the pulmonary hypoplasia on the affected side.
Hepatic pulmonary fusion is a rare finding associated with a right sided CDH. In most instances it is diagnosed in newborns that have respiratory symptoms. Our patient indicates that it may also be discovered beyond the neonatal period when the patient presents with delayed onset of symptoms. The diagnosis should be considered if there is a right sided chest opacity without a contralateral mediastinal shift. However, as noted in the present case, hepatic pulmonary fusion can occasionally occur with a mediastinal shift. MRI is a useful diagnostic imaging technique. With increased use of fetal MRI, hepatic pulmonary fusion may be identified prior to repair. Operative exploration with intent to separate the organs may result in bleeding and injury to pulmonary parenchyma. Reduction of bowel and creation of 2 separate cavities is the primary surgical goal when separation of the fused tissues cannot be achieved without undue risk. The surgeon should be aware that division of hepatic pulmonary fusion to achieve complete separation of the thoracic and abdominal cavity adds risk to the procedure and may not be necessary. Reduction of bowel and approximation of the diaphragmatic defect around the fused liver and lung was successfully employed in the present case. However, long term follow up is necessary to be sure that this technique is enduring.
Supplementary Material
References
- 1.Fisher JC, Jefferson RA, Arkovitz MS, et al. Redefining outcomes in right congenital diaphragmatic hernia. J Pediatr Surg. 2008;43:373–9. doi: 10.1016/j.jpedsurg.2007.10.049. [DOI] [PubMed] [Google Scholar]
- 2.Weber TR, Tracy T, Bailey PV, et al. Congenital diaphragmatic hernia beyond infancy. Am J Surg. 1991;162:643–6. doi: 10.1016/0002-9610(91)90127-y. [DOI] [PubMed] [Google Scholar]
- 3.Robertson DJ, Harmon CM, Goldberg S. Right congenital diaphragmatic hernia associated with fusion of the liver and the lung. J Pediatr Surg. 2006;41:9–10. doi: 10.1016/j.jpedsurg.2006.02.031. [DOI] [PubMed] [Google Scholar]
- 4.Slovis TL, Farmer DL, Berdon WE, et al. Hepatic Pulmonary Fusion in Neonates. AJR. 2000;174:229–33. doi: 10.2214/ajr.174.1.1740229. [DOI] [PubMed] [Google Scholar]
- 5.Keller RL, Aaroz PA, Hawgood S, et al. MR Imaging of Hepatic Pulmonary Fusion in Neonates. AJR. 2003;180:438–40. doi: 10.2214/ajr.180.2.1800438. [DOI] [PubMed] [Google Scholar]
- 6.Katz S, Kidron D, Litmanovitz I, et al. Fibrous fusion between the liver and the lung: an unusual complication of right congenital diaphragmatic hernia. J Pediatr Surg. 1998;33:766–7. doi: 10.1016/s0022-3468(98)90214-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


