Abstract
Patients want to be able to communicate with their physicians by e-mail. However, physicians are often concerned about the impact that such communications will have on their time, productivity, and reimbursement. Typically, physicians are not reimbursed for time spent communicating with patients electronically. But under federal meaningful-use criteria for information technology, physicians can receive a modest incentive for such communications. Little is known about trends in secure e-mail messaging between physicians and patients. To understand these trends, we analyzed the volume of messages in a large academic health care system’s patient portal in the period 2001–10. At the end of 2010, 49,778 patients (22.7 percent of all patients seen within the system) had enrolled in the portal, and 36.9 percent of enrolled patients (8.4 percent of all patients) had sent at least one message to a physician. Physicians in the aggregate saw a near tripling of e-mail messages during the study period. However, the number of messages per hundred patients per month stabilized between 2005 and 2010, at an average of 18.9 messages. As physician reimbursement moves toward global payments, physicians’ and patients’ participation in secure messaging will likely increase, and electronic communication should be considered part of physicians’ job descriptions.
Web-based patient portals that offer patients a view of their medical records were first introduced in 2000.[1] A cardinal feature of most patient portals is secure messaging, which allows patients and physicians to communicate electronically in an asynchronous fashion. Secure messaging offers patients a convenient way to contact their physicians outside of office visits. Surveys have shown that the vast majority of patients who are Internet users desire the ability to e-mail their physician.[2–5] However, only about 10 percent of these patients are able to do so. [6]
Despite patients’ interest, clinicians have been slow to incorporate secure messaging into their practices.[7,8] Recent data suggest that only 9 percent of doctors offered a patient portal that could allow for secure messaging.[9]
The convenience to patients is clear. However, large numbers of messages have the potential to burden busy physicians.[8,10–12] Like telephone calls with patients, secure messaging is generally not a reimbursed activity. Liability concerns may also arise, as physicians may be providing care via e-mail without actually examining the patient.[13] However, studies generally have reported high levels of satisfaction among physicians who communicate electronically with their patients.[14–19]
In the federal program to promote the meaningful use of electronic health records (EHRs)—which is administered by the Office of the National Coordinator for Health Information Technology—practitioners must meet certain criteria to receive incentive payments. These criteria include providing patients with online access to their data.” [20] In stage 2 of the meaningful-use program, physicians cannot qualify for incentives until 5 percent of their patients have sent them a secure message, a percentage that is assessed over a ninety-day period.[21]
Payment mechanisms such as global payments through accountable care organizations may allow providers to restructure their clinical days to handle some encounters via secure messaging or web conferencing instead of face-to-face visits.[8] However, most payers continue to use fee-for-service reimbursement systems that do not include compensation for time spent on patient e-mails, and this is unlikely to change in the foreseeable future. Moving forward, it will be important to understand the potential impact of messaging on physicians’ workflow.[22]
In this study, we report on the first decade of secure messaging at a large health care system that was among the first nationally to implement this technology. We focused on patient-physician messaging to determine whether patients increased their use of messaging over time and the extent to which the volume of messages to physicians grew over time.
Study Data And Methods
Setting
We analyzed patient portal use during the ten-year period 2001–10 within a single large academic health system with seventy participating clinical practices located in the Boston metropolitan area. Beth Israel Deaconess Medical Center launched its patient portal, PatientSite, in 2000 to enable secure electronic communication between patients and physicians and to allow patients to view aspects of their clinical chart electronically. Separate from the messaging function, patients can also request prescription refills and appointments through PatientSite.
Affiliated physicians who use the health system’s EHR are eligible to participate in PatientSite. Physicians receive no reimbursement for using secure messaging. Each participating practice can adopt its own workflow for using the portal. For example, most physicians receive messages directly, but a few practices have designated nurses to triage messages. All messages are archived as part of the patients’ permanent medical records.
Patients must enroll in PatientSite through a participating physician who is their established caregiver. To enroll, patients submit a web-based request, which is processed and approved by an administrator.
With the exception of the last six months of 2010, the study period predated the health system’s participation in the OpenNotes program, where patients could read their physicians’ visit notes through PatientSite.[23]
Definitions And Exclusions
Secure messages were defined as patient-initiated correspondence sent to an attending physician through the portal. Resident physicians participated only in the last year of the study period. Thus, we excluded them from our analysis.
Starting in 2004 the system automatically deleted patient accounts that had been inactive for two years or longer. When we calculated patient enrollment trends over time, we therefore restricted the analysis to enrolled patients who had accessed the web portal within the preceding two years.
To calculate the percentage of a physician’s patients who sent him or her messages during a calendar year, we considered the denominator to be the total number of unique patients seen by that physician in that year. Physicians who were not receiving messages through PatientSite in a given year were excluded from calculations for that year.
In determining the percentage of patients who either enrolled in or sent messages through PatientSite, we considered the denominator to be all patients who had an outpatient encounter within any clinic that was directly affiliated with the health care system during the calendar year.
Statistical Analyses
We evaluated message volumes and standardized them by hundred enrolled patients, as well as by the number of participating physicians, to account for growth in the number of users (both physicians and patients). To better understand the use of secure messaging, we reviewed characteristics such as the day and time that the message was sent.
To examine message variability as a function of clinical volume for primary care physicians, we estimated a physician’s clinical effort based on his or her total number of outpatient encounters during the calendar year. Using volume expectations from the largest participating primary care practice, we estimated that one full-time physician would have 2,200 or more patient encounters per year. We used this number of encounters to extrapolate what message volumes academic and part-time physicians with smaller patient panels would have had if they had been full-time.
The study was approved by the Beth Israel Deaconess Medical Center Institutional Review Board.
Limitations
Our study was subject to several limitations. We examined the experience of only one health care system, and our findings may not be generalizable to all settings.
In addition, we were limited in our ability to accurately control for disease burden in patients because of the limited availability of outpatient billing codes during the study period. Thus, we were not able to look for differences in messaging over time in patients with specific chronic diseases.
Furthermore, we did not include as secure messages patients’ requests for prescription refills and appointments that were sent outside of the messaging function. However, some patients may have sent such requests through that function. Thus, our number of secure messages may have included some of these requests.
Study Results
Enrollment And Participation
At the end of 2010, 49,778 patients of the seventy participating practices and their 272 participating physicians were enrolled in the patient portal. This represented 22.7 percent of the patients seen within the health care system in 2010 (Exhibit 1). Of those enrolled patients, 18,400 (36.9 percent of the enrolled patients and 8.4 percent of the health care system’s patients) sent at least one message to their physician in 2010.
EXHIBIT 1. Number Of Patients Enrolled In The PatientSite Portal, 2001–10.
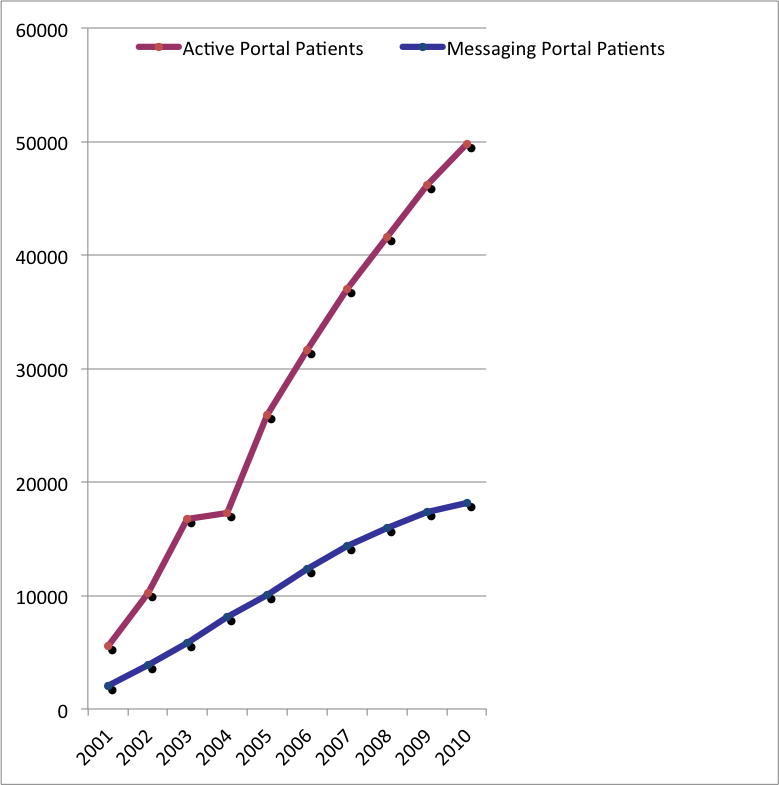
Source/Notes: SOURCE Authors’ analysis of PatientSite data.
NOTES In 2004 and beyond, the system removed patients who had not logge into the system within two years. “Messaging patients” are those who sent a secure message in a given calendar year.
Physician participation plateaued in the period 2008–2010, with a net increase of only twelve physicians during that time period. Nearly all of the participating physicians (97.1 percent) received at least one message in the study period. Primary care physicians, who represented approximately 20 percent of all eligible physicians, accounted for 48 percent of those who participated in secure messaging. Enrolled patients were mostly female (61 percent), white (73 percent), and commercially insured (87 percent). The mean age at enrollment in the patient portal was forty-three years.
Messaging Trends Over Time
The growth in the number of enrolled patients over time has largely been linear, despite a plateau in the number of participating physicians. During the study period, physicians in the aggregate saw a near tripling of messages, from 11.9 (standard deviation: 1.5) messages per month in 2001 to 32.9 (SD: 3.1) per month in 2010 (Exhibit 2). This change was largely driven by increasing patient enrollment. These numbers were not adjusted for clinical effort—that is they are inclusive of academic and other clinically part-time physicians and were not standardized based on expected message volume of full-time clinicians.
EXHIBIT 2. Number Of Messages Per 100 Patients And Per Physician Sent Through The PatientSite Portal, 2001–10.
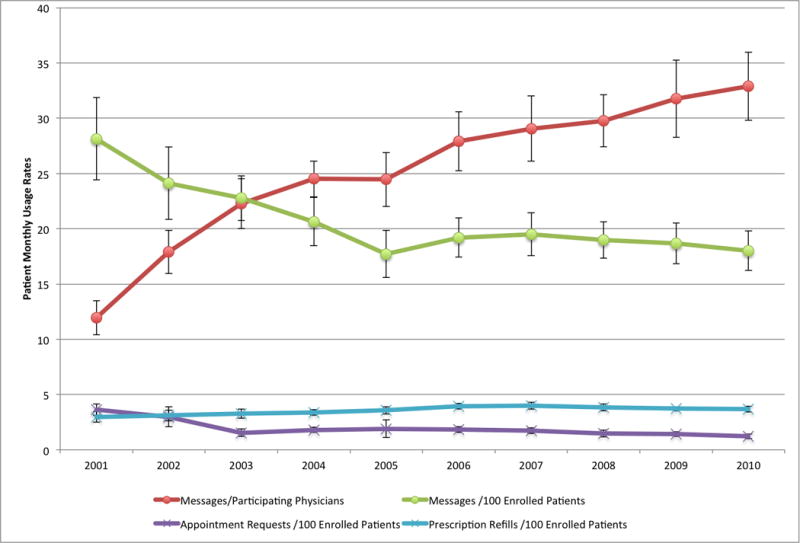
Source/Notes: SOURCE Authors’ analysis of PatientSite message tables and user data. NOTES “Messages per 100 patients” is the average number of messages sent per hundred enrolled patients per month. “Messages per physician” is the average number of messages received by each physician (the number of messages divided by the number of participating physicians) per month. “Appointment requests” and “Rx refill requests” are the average numbers of requests for appointments and prescription refills, respectively, sent per hundred enrolled patients per month through a separate portal functionality from messaging. Whisker marks denote standard deviations.
The average number of messages per hundred enrolled patients per month decreased between 2001 and 2005 (Exhibit 2). The number then stabilized at an average of 18.9 (SD: 2.0) messages per month between 2005 and 2010.
Patients tended to send most messages in the morning. However, they sent 37.5 percent of their messages during “off hours”—that is, outside of weekday business hours—with 10 percent of their messages sent on weekends.
Messaging Variability
Messaging to primary care physicians accounted for 85 percent of all secure messages sent by patients. Message volumes per physician were highly variable. The median number of messages per primary care physician per year was 197, with an interquartile range of 55–521 (Exhibit 3). There was a maximum of 14,439 messages in a year for a single very high volume physician user (approximately 58 messages per work day).
EXHIBIT 3. Variability In Number Of Messages Sent To Physicians Through The PatientSite Portal In 2010, By Specialty.
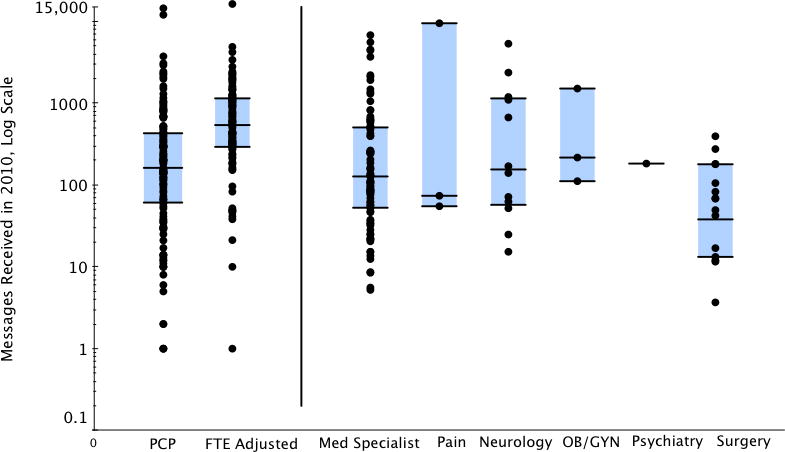
Source/Notes: SOURCE Authors’ analysis of PatientSite data and Beth Israel Deaconess Medical Center scheduling data. NOTES The center line in each shaded box represents the median, and the box represents the interquartile range (with the top line indicating the seventy-fifth percentile and the bottom line the twenty-fifth percentile). For psychiatry, only one physician used the system in 2010, and thus no interquartile range is provided. The dots indicate all observations. “FTE adjusted” represents extrapolation of message volumes that academic and other part-time primary care physicians with less than full-time clinical effort would have if they practiced full time.
After we adjusted the results for full-time clinical effort, we estimated that primary care physicians would have received a median of 539 messages (interquartile range: 292–1,145) per year. Specialists demonstrated similar variability.
Achieving Meaningful Use
In 2010 primary care physicians had a median of 11 percent of their patients sending secure messages (Exhibit 4). Across the entire health care system, 8.4 percent of outpatients sent at least one secure message in 2010. This is over the 5 percent threshold for meeting stage 2 criteria for meaningful use.
EXHIBIT 4. Estimated Growth In Secure Messaging Within Primary Care Physician Panels, 2001–10.
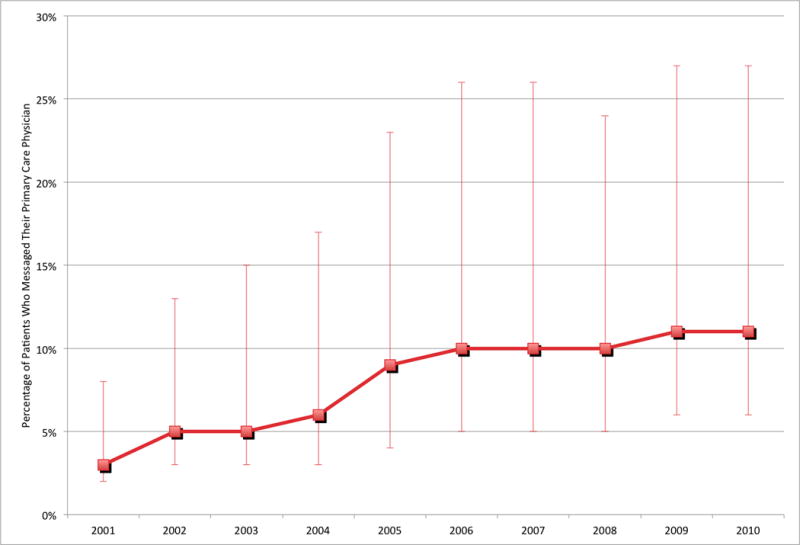
Source/Notes: SOURCE Authors’ analysis of PatientSite data and Beth Israel Deaconess Medical Center scheduling data.
NOTES Each dot represents the median for physicians’ panels. Whisker marks denote the twenty-fifth and seventy-fifth percentiles. The denominator is the number of unique patients seen by each physician.
Discussion
In this study, we analyzed the first decade of experience with a patient portal embedded within a large health care system. Nearly 50,000 patients enrolled in the portal.
Our study produced several important findings for health care systems and clinicians who adopt secure messaging. First, physicians saw an increase in their message volume over time that was related to increasing numbers of patients enrolling in the portal. The average number of messages per provider nearly tripled.
Second, the average number of secure messages per patient per month decreased over time and plateaued after five years. This likely represents an “early adopter” effect that waned over time as additional patients enrolled.
Finally, 23 percent of patients across the health system were enrolled. This yielded an active participation rate of 8 percent, just over the 5 percent federal threshold for eligibility for stage 2 meaningful-use incentives. Much of this growth was driven by communication between patients and their primary care physician.
As health care systems consider enabling electronic communication between patients and physicians, some physicians have expressed concerns that this will lead patients to develop a lower threshold for contacting their physician, potentially overwhelming busy providers with messages.[15,24] Instead, our analysis found that the volume of secure messaging per patient has remained stable since 2005.
If patients were to rely increasingly on this type of messaging, even for minor concerns, we would expect to see messaging per patient increasing instead of decreasing over time. Based on our data, the principal driver of increased messages was the increasing number of enrolled patients, and not an increasing volume of messages per patient over time.
Primary care physicians represented only half of the physicians participating in PatientSite. However, 85 percent of messages were directed to them. This likely reflects the clinical needs of patients and the usefulness of e-mail for first-contact questions related to new problems or other questions that are best directed to primary care physicians. But it may also be the case that secure messaging may be more comfortable for patients and physicians alike when relationships are longitudinal in nature, as they often are in primary care.
Regardless of the clinical domain, we observed wide variability in message volume across physicians. This may represent differences in physicians’ preferences and comfort levels with technology. Alternatively, it could be a function of the patients seen by various providers, since older and less affluent patients might be expected to be slower to enroll in a portal and use it.[25]
The nature of the patient-physician relationship likely also influences messaging. Patients who are more comfortable with their physician in general may also be more comfortable sending that physician a secure message.
Cultural norms and structural differences in physician practices, such as practice workflow and staffing resources, also may explain variability seen across physicians. In many practices, physicians received secure messages directly, without a nurse or assistant triaging messages. Other physicians, such as those in the Beth Israel Deaconess Medical Center’s multiple sclerosis clinic, conducted most of their non-visit related patient contact with secure messages through PatientSite as opposed to more typical telephone calls, and utilized a central staff member to manage inbound messages. This made it easier for physicians to balance revenue-generating clinical activity such as office visits with nonreimbursed services such as secure messaging.[26] Jonathan Wald has demonstrated that practice-level approaches and leadership weigh heavily in patients’ rates of adoption of secure messaging.[27]
Policy And Practice Implications
Innovative reimbursement models that are based on global payments, such as those in accountable care organizations, may provide the necessary incentives to physicians to use secure messaging with patients. Electronic communication has the potential to better meet patients’ needs in a timely and efficient manner than telephone or postal mail, and to substitute for more expensive office visits when appropriate. As physicians begin to manage patients outside of visits, electronic communication with patients and family members may enhance care coordination, enable physicians to use their time more efficiently, and allow for more delegation and team-based care.
As the use of secure messaging becomes more prevalent, a mechanism for reimbursing physicians and accounting for the workload of electronic messaging will be important.[28] For instance, if physician reimbursement systems move toward fixed population-based payments, instead of visit-based payments, physicians will be better able to incorporate telephone and e-mail time into their workdays.
Conclusion
We have reported results from the first longitudinal study of patient messaging during the first decade of use of a robust patient portal. We demonstrated that the principal driver of increased messaging was the rising number of patients who enrolled in the patient portal, and not a tendency for those who were enrolled to send more messages.
As more practices embrace this technology, understanding the variability in physician participation will be helpful. Reimbursement models and clinic structures that allow time for secure messaging will be important for physicians. Given that secure messaging is becoming more prevalent and is incentivized through meaningful-use criteria, future studies should seek to determine how patients and clinicians can best use messaging to improve the quality and efficiency of care.
Acknowledgments
Bradley Crotty was supported by an Institutional National Research Service Award (No. T32HP12706) and by the and the Ryoichi Sasakawa Fellowship Fund. Yonas Tamrat was funded through support from the National Library of Medicine (Grant No. T15LM007092). The authors gratefully acknowledge the assistance of Margaret Jeddry and Jing Ji, as well as George Silva in the Beth Israel Deaconess Medical Center’s Center for Healthcare Delivery Science, for help with data acquisition. Crotty had full access to the data and takes full responsibility for the integrity and accuracy of the data analysis.
Biographies
Bradley H. Crotty (bcrotty@bidmc.harvard.edu) is the director of patient portals in the Division of Clinical Informatics, Beth Israel Deaconess Medical Center, and an instructor in medicine at Harvard Medical School in Boston, Massachusetts.
Yonas Tamrat is a primary care internist at Johnson Health Center, in Lynchburg, Virginia.
Arash Mostaghimi is an instructor in dermatology at Brigham and Women’s Hospital, in Boston.
Charles Safran is chief of the Division of Clinical Informatics, Beth Israel Deaconess Medical Center and an associate professor of medicine at Harvard Medical School.
Bruce E. Landon is a professor of health care policy at Harvard Medical School, in Boston.
Contributor Information
Bradley H. Crotty, Division of Clinical Informatics, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Yonas Tamrat, Johnson Health Center, Lynchburg, VA.
Arash Mostaghimi, Department of Dermatology, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA.
Charles Safran, Division of Clinical Informatics, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA.
Bruce E. Landon, Department of Health Care Policy, Harvard Medical School, Boston, MA
Notes
- 1.Halamka JD, Mandl KD, Tang PC. Early experiences with personal health records. J Am Med Inform Assoc. 2008;15(1):1–7. doi: 10.1197/jamia.M2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ye J, Rust G, Fry-Johnson Y, Strothers H. E-mail in patient-provider communication: a systematic review. Patient Educ Couns. 2010;80(2):266–73. doi: 10.1016/j.pec.2009.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moyer CA, Stern DT, Dobias KS, Cox DT, Katz SJ. Bridging the electronic divide: patient and provider perspectives on e-mail communication in primary care. Am J Manag Care. 2002;8(5):427–33. [PubMed] [Google Scholar]
- 4.Virji A, Yarnall KS, Krause KM, Pollak KI, Scannell MA, Grandison M, et al. Use of email in family practice setting: opportunities and challenges in patient-and physician-initiated communication. BMC Med. 2006;4:18. doi: 10.1186/1741-7015-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kleiner KD, Akers R, Burke BL, Werner EJ. Parent and physician attitudes regarding electronic communication in pediatric practices. Pediatrics. 2002;109(5):740–4. doi: 10.1542/peds.109.5.740. [DOI] [PubMed] [Google Scholar]
- 6.Beckjord EB, Finney Rutten LJ, Squiers L, Arora NK, Volckmann L, Moser RP, et al. Use of the internet to communicate with health care providers in the United States: estimates from the 2003 and 2005 Health Information National Trends Surveys (HINTS) J Med Internet Res. 2007;9(3):e20. doi: 10.2196/jmir.9.3.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zickmund SL, Hess R, Bryce CL, McTigue K, Olshansky E, Fitzgerald K, et al. Interest in the use of computerized patient portals: role of the providerpatient relationship. J Gen Intern Med. 2008;23(Suppl 1):20–6. doi: 10.1007/s11606-007-0273-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bishop TF, Press MJ, Mendelsohn JL, Casalino LP. Electronic communication improves access, but barriers to its widespread adoption remain. Health Aff (Millwood) 2013;32(8):1361–7. doi: 10.1377/hlthaff.2012.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Markle Foundation. Markle Survey on Health in a Networked Life 2010 [Internet] New York (NY): Markle Foundation; 2011. Jan, [cited 2014 Aug 11]. Available from: http://www.markle.org/sites/default/files/20110110_HINLSurveyBrief_0.pdf. [Google Scholar]
- 10.Delbanco T, Sands DZ. Electrons in flight—e-mail between doctors and patients. N Engl J Med. 2004;350(17):1705–7. doi: 10.1056/NEJMp038209. [DOI] [PubMed] [Google Scholar]
- 11.Hobbs J, Wald J, Jagannath YS, Kittler A, Pizziferri L, Volk LA, et al. Opportunities to enhance patient and physician e-mail contact. Int J Med Inform. 2003;70(1):1–9. doi: 10.1016/s1386-5056(03)00007-8. [DOI] [PubMed] [Google Scholar]
- 12.Archer N, Fevrier-Thomas U, Lokker C, McKibbon KA, Straus SE. Personal health records: a scoping review. J Am Med Inform Assoc. 2011;18(4):515–22. doi: 10.1136/amiajnl-2011-000105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Houston T, Sands DZ, Nash BR, Ford DE. Experiences of physicians who frequently use e-mail with patients. Health Commun. 2003;15(4):515–25. doi: 10.1207/S15327027HC1504_08. [DOI] [PubMed] [Google Scholar]
- 14.Nazi KM. The personal health record paradox: health care professionals’ perspectives and the information ecology of personal health record systems in organizational and clinical settings. J Med Internet Res. 2013;15(4):e70. doi: 10.2196/jmir.2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kittler AF, Carlson GL, Harris C, Lippincott M, Pizziferri L, Volk LA, et al. Primary care physician attitudes towards using a secure web-based portal designed to facilitate electronic communication with patients. Inform Prim Care. 2004;12(3):129–38. doi: 10.14236/jhi.v12i3.118. [DOI] [PubMed] [Google Scholar]
- 16.Byrne JM, Elliott S, Firek A. Initial experience with patient-clinician secure messaging at a VA medical center. J Am Med Inform Assoc. 2009;16(2):267–70. doi: 10.1197/jamia.M2835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaster B, Knight CL, DeWitt DE, Sheffield JV, Assefi NP, Buchwald D. Physicians’ use of and attitudes toward electronic mail for patient communication. J Gen Intern Med. 2003;18(5):385–9. doi: 10.1046/j.1525-1497.2003.20627.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liederman EM, Morefield CS. Web messaging: a new tool for patient-physician communication. J Am Med Inform Assoc. 2003;10(3):260–70. doi: 10.1197/jamia.M1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anand SG, Feldman MJ, Geller DS, Bisbee A, Bauchner H. A content analysis of e-mail communication between primary care providers and parents. Pediatrics. 2005;115(5):1283–8. doi: 10.1542/peds.2004-1297. [DOI] [PubMed] [Google Scholar]
- 20.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–4. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Medicare and Medicaid Services. Stage 2 overview tipsheet [Internet] Baltimore (MD): CMS; [last updated 2012 Aug; cited 2014 Aug 11]. Available from: http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/Stage2Overview_Tipsheet.pdf. [Google Scholar]
- 22.Bodenheimer T, Grumbach K. Electronic technology: a spark to revitalize primary care? JAMA. 2003;290(2):259–64. doi: 10.1001/jama.290.2.259. [DOI] [PubMed] [Google Scholar]
- 23.Delbanco T, Walker J, Darer JD, Elmore JG, Feldman HJ, Leveille SG, et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010;153(2):121N5. doi: 10.7326/0003-4819-153-2-201007200-00008. [DOI] [PubMed] [Google Scholar]
- 24.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–6. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yamin CK, Emani S, Williams DH, Lipsitz SR, Karson AS, Wald JS, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med. 2011;171(6):568–74. doi: 10.1001/archinternmed.2011.34. [DOI] [PubMed] [Google Scholar]
- 26.Nielsen AS, Halamka JD, Kinkel RP. Internet portal use in an academic multiple sclerosis center. J Am Med Inform Assoc. 2012;19(1):128–33. doi: 10.1136/amiajnl-2011-000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wald JS. Variations in patient portal adoption in four primary care practices. AMIA Annu Symp Proc. 2010;2010:837–41. [PMC free article] [PubMed] [Google Scholar]
- 28.Landon BE. Keeping score under a global payment system. N Engl J Med. 2012;366(5):393–5. doi: 10.1056/NEJMp1112637. [DOI] [PubMed] [Google Scholar]


