Abstract
Aim
To verify the reproducibility of patients irradiated after mastectomy on the immobilization system designed and manufactured for our hospital and to compare the Internal Protocol (IP) with the modified-No Action Level Protocol.
Background
Application of forward IMRT techniques requires a good reproducibility of patient positioning. To minimize the set-up error, an effective immobilization system is important.
Materials and methods
The study was performed for two groups of 65 each. In the first group, portal images for anterior field were taken in 1–3 fractions and, subsequently, three times a week. In this group, the mNAL protocol was used. In the second group, the IP was used. The portal images from the anterior field and from the gantry 0 were taken during the 1–3 and 10 fractions. In both groups, image registration was performed off-line. For each group the systematic and random errors and PTV margin were calculated.
Results
In the first group the value of the population systematic errors and random errors were 1.6 ± 1.6 mm for the left–right, and 1.5 ± 1.7 mm for the cranial–caudal directions, respectively, 1.7 ± 1.3 mm, and 1.9 ± 1.3 mm for the second group. The PTV margins for the left–right and cranial–caudal directions were 5.1 and 4.9 mm for the first group and 5.4 and 6.4 mm for the second group.
Conclusions
For patients immobilized with our support device treated according to the mNAL protocol or IP, a good set-up reproducibility was obtained. Implementation of IP limits the number of required images.
Keywords: Patient positioning, Systematic error, Random error
1. Background
Breast cancer is the most common malignant tumor among women. Different types of treatment are used for breast cancer patients. For some patients radiation therapy is applied after mastectomy. Some of them start with mastectomy followed by post-mastectomy radiotherapy.13 Post-mastectomy radiation is technically difficult due to complexity of the target volume and its close proximity to critical structures, including the heart, lung, brachial plexus and contralateral breast. Many different techniques have been proposed for post-mastectomy irradiation. Pierce12 described several commonly used treatment techniques: standard tangents, electron fields, reverse photon electron technique, photon electron mix technique. None of these is considered as the gold standard. Nowadays, more and more often, the state-of-the-art IMRT techniques are used.2,4,5
In order to ensure delivering the prescribed dose to the CTV throughout the entire course of irradiation, margins must be added. The ICRU9 recommends adding margins adequate to the chest wall, supraclavicular and axillary nodes in order to account for variations in the position, size and shape of the target (internal margin) and for uncertainties in patient positioning (set-up margin). To minimize the set-up errors, the effective immobilization systems, suitable for a given location, should be used. There are several commercially available immobilization systems designed for positioning of patients irradiated in the thorax region.
2. Aim
In this study, we evaluated the immobilization system designed in our hospital. We also compared two protocols of set-up correction: the modified-No Action Level (mNAL)7 and the Internal Protocol.
3. Materials and methods
3.1. Patients
Patients with T2–T3 breast cancer were included in the prospective study for evaluation of the immobilization system which was designed and manufactured for our hospital. We did not make any selection based on the tumor stage or body habitus. The study was performed for two groups of consecutive patients treated in our hospital. There were 65 patients in each group. In the first group (the mNAL group), the portal images were taken 12–17 times during the treatment. For the second group (the Internal Protocol group), the portal images were taken during the first three fractions and in the middle of the treatment.
3.2. Treatment techniques and patients’ set-up
For all patients, a treatment planning CT was made in the treatment position. The planning CT scans were acquired from the thyroid cartilage to 2 cm below the lower border of the healthy breast with 5-mm slice thickness in the spiral mode. Patients were treated with forward-IMRT Segmented Photon Beams Technique.14 Their radiotherapy plan consisted of 6 isocentric photon beams of 4 MV and 15 MV X-rays. There was one isocenter for all beams. Isocenter point was located near the top of the lung on the irradiated site.
Plans were prepared according to the International Commission on radiation Units and Measurements guidelines with the Precise Plan treatment planning system (version 2.15). Patients were irradiated on the Elekta Synergy accelerator equipped with the MLC and electronic portal imaging device (EPID). The total dose of 45 Gy in 20 fractions was administered. More details about the irradiation technique can be found elsewhere.14 After placing a patient on the immobilization system, the therapeutic position was achieved by aligning three skin tattoos with the laser system. Tattoos were made on the medial surface, on the left and right side of the thorax at the level of the sternum. An additional tattoo was always marked on the medial line in the infraclavicular area.
3.3. Immobilization system
Fig. 1 shows the immobilization system. Patients were placed supine with arms placed on acrylic supports with hands holding individually positioned hands grips and with their head placed on the commercially available head support (Orfit Industries). Our support device enables to carry out the planning computed tomography in the therapeutic position, even if the CT aperture is quite small. The support device is easy to handle, its weight being 2 kg only. Patients, who due to other coexisting diseases could not be positioned on the support device, were placed either on a Sinmed board or on a vac-lok mattress. These patients were excluded from this study.
Fig. 1.

The support device of our construction.
3.4. Set-up errors
Set-up errors were defined as a geometric difference between digitally reconstructed images and treatment fields position with respect to bony landmarks. For each patient, two DRRs were reconstructed. The first one was for the open field at gantry 0° with size covering all the irradiated regions. The other one was one of the main segments of the oblique fields at gantry angle of about 50°.
In Fig. 2, examples of these DRRs are shown. Bony structures used for image registration are marked in green. The set-up errors were measured for the left–right (l–r) and cranial–caudal (c–c) directions. For both groups of patients, the image for the oblique field was used to check if the anterior–posterior (a–p) direction was set correctly. The errors made in the a–p direction set lead to errors in dose delivery. The a–p direction error may be discovered from a comparison of the lateral displacement of the isocenter measured on the DRR at gantry 0° and from the one measured on the oblique field. Fig. 3 demonstrates the influence of the a–p direction error on a lateral displacement. In this figure, the error of placing the isocenter deeper than in the treatment plan is analyzed. After rotation of the gantry into the oblique position a different part of the thorax would be irradiated. The identical consequence of misalignment along the lateral direction might be obtained if the a–p direction was not set properly.
Fig. 2.
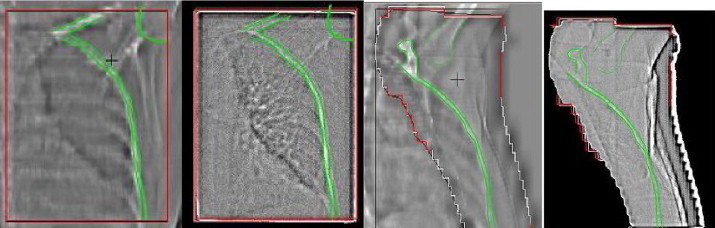
Portal images and DRRs for beams at gantry angle 0° and 50°.
Fig. 3.
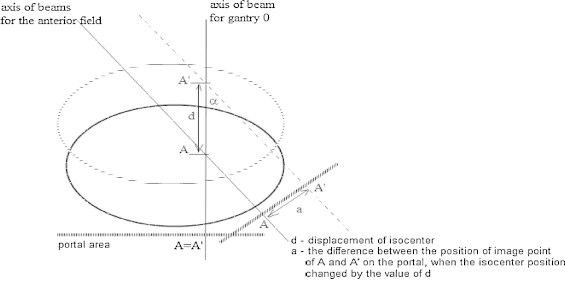
Horizontal displacement related to the changes in the anterior–posterior direction.
3.5. Analysis of errors
The data was analyzed in terms of systematic and random errors. Bijhold's1 convention was used. The probability density functions of set-up errors occurring in a patient population is described by the mean systematic error m, the dispersion of systematic errors ∑, and the mean value of random dispersions σp, mathematically defined by the following formulas:
| (f11) |
where
| (f12) |
index p denotes the patient's number, np is the number of images taken for a particular patient, N is the number of patients.
The value of random error is expressed by standard deviation over the mean value xp:
| (f13) |
The value of dispersion of systematic errors is calculated with the formula:
| (f14) |
The anterior–posterior direction error for the oblique anterior field was calculated with the formula:
| (f15) |
where d is the difference in the anterior–posterior direction, a is the difference between set-up errors along the left–right direction measured on the oblique portal field (see Fig. 3) with portal taken at 0°.
Further analysis of the displacements measured for the portal 0 and for the oblique anterior field allowed us to determine displacements in all three directions.
3.6. Data
Data was collected for two groups of 65 each. In the mNAL group, portal images for the anterior field were taken before 1–3 fraction and, subsequently, three times a week, and whenever a correction of a patient set-up was made. Portals were taken more frequently than required according to the mNAL protocol, in order to determine time trends. Additionally, the portal from the gantry angle 0° was taken during the 1° and 10° fraction. From the 4° fraction on, patients were set up using original tattoos and if the average value of the mean setup error (ɛx, ɛy, ɛz) in the first three fractions exceeded 5 mm the couch was shifted with −(ɛx, ɛy, ɛz). New correction value is calculated and used in the remaining part of treatment. Later, if in any treatment session the error exceeded 5 mm, the second portal was made in the next session. If the average value of errors obtained in these two sessions exceeded 5 mm, patient's position was corrected. Over the entire course of treatment (20 fractions), for each patient at least 14 portals were acquired. In total, 1080 images were analyzed for this group of patients.
Results of the first group were analysed in two ways:
-
-
the raw data was analyzed neglecting all corrections,
-
-
all corrections were taken into account.
In order to limit the number of portal controls made, the Internal Procedure was implemented. According to the procedure, the portal images from the oblique anterior field and from the gantry angle 0° were taken during the 1st, 2nd, 3rd and 10th fraction, and each time following any corrections. The corrections were made after the third fraction, if the mean value obtained from these three measurements exceeded 3 mm, or if the a–p direction required a change by at least 5 mm. Additional portal control was made in the11° fraction if in the 10° fraction the error in any direction exceeded 5 mm. The mean value of these two errors was calculated, and if the mean value exceed 3 mm, a set-up correction was undertaken. For patients from this group, 8–16 portals were acquired. For the Internal Protocol group, 520 portal images were taken and analysed. In both group image registration was performed offline.
3.7. Rotation
For patients from the mNAL group, the rotation was analyzed for portals taken at gantry angle 0 and for the anterior fields.
3.8. Time trends analysis3
For each patient in the mNAL group, the setup errors were analyzed as a function of the session number. The slope of the linear fit to the setup error for each direction was computed using regression analysis. A t-test was utilized to determine whether the slope was statistically different from zero.
3.9. Uncertainty of image registration
Intraobserver variability in image registration was used as a measure of image registration uncertainty. The difference in mean value and standard deviation of image registration results obtained by two experienced physicists were obtained.
4. Results
Table 1 shows the values of the population average systematic set-up errors, and the standard deviations of the systematic errors and random errors for the first group of patients. There are two sets of data. The first one if no mNAL protocol was used and the other one if the set-up was corrected according to the mNAL protocol.
Table 1.
Results of setup control obtained in the first group of patients.
| Directions | No correction |
Protocol mNAL |
||
|---|---|---|---|---|
| Left–right | Cranial–caudal | Left–right | Cranial–caudal | |
| m [mm] | −1.0 | −1.6 | −0.6 | 0.3 |
| ∑ [mm] | 2.4 | 2.8 | 1.6 | 1.5 |
| σp [mm] | 1.7 | 1.7 | 1.7 | 1.7 |
Implementation of the mNAL protocol considerably improves the reproducibility of irradiation. For both directions, the standard deviation of the systemic errors after mNAL implementation is significantly smaller than without this protocol (p < 0.05).
Table 2 shows the values of the population average systematic setup errors, and the standard deviations of the systematic and random errors for the second group of patients. There are two sets of data: the first one, when corrections were not required, and the second one, when corrections have been made. In the second case, all parameters were calculated for the first three fractions, without adjustments, and after the application of the Internal Procedure.
Table 2.
Results of setup control obtained in the second group of patients.
| Direction | Group without corrections 28 patients |
Group with corrections 37 patients |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| The first 3 fractions (no adjustements) |
After the Internal Procedure (adjustments) |
|||||||||||
| Angle 0° |
The anterior field |
Angle 0° |
The anterior field |
Angle 0° |
The anterior field |
|||||||
| l–r | c–c | l–r | c–c | l–r | c–c | l–r | c–c | l–r | c–c | l–r | c–c | |
| m [mm] | −0.3 | −0.72 | −0.1 | −0.6 | 0.5 | −1.2 | −1.1 | −2.2 | 0.1 | −0.5 | 0.8 | −0.7 |
| ∑ [mm] | 1.5 | 2.1 | 1.7 | 2.2 | 3.6 | 3.1 | 3.1 | 3.9 | 1.7 | 1.9 | 1.8 | 2.1 |
| σp [mm] | 1.5 | 1.5 | 1.3 | 1.6 | 1.6 | 1.3 | 1.7 | 1.7 | 1.3 | 1.3 | 1.3 | 1.3 |
l–r, left–right; c–c, cranial–caudal.
Correction considerably improved the quality of treatment. For both directions, the standard deviation of the systemic errors after correction is significantly smaller than before correction (p < 0.05). There is no significant difference between results obtained for the second group if correction has been implemented and for the first group irradiated according to the mNAL protocol (p > 0.05).
The results of time trends investigations are given in Table 3. No time trends were observed.
Table 3.
Time trends. Pearson's correlation coefficient for both directions.
| Correlation coefficient | Strength of correlation | Percent results |
|
|---|---|---|---|
| Left–right | Cranial–caudal | ||
| 0.0–0.2 | No correlation | 30 | 70 |
| 0.2–0.4 | Weak correlation | 20 | 80 |
For any patient, statistically significant (p < 0.05) slope of the linear fit to setup errors for both directions was obtained. For 85% of results the slopes of the linear fit were in the range from −0.25 mm to +0.25 mm per 1 fraction. For 6 patients, for at least one direction, those values were ±0.35 mm per fraction. For almost all patients these time trends may result in the overall patient's shift during the entire treatment of less than 5 mm.
In Fig. 4, a histogram of rotations is shown. Large rotations were noticed very seldom. The mean value of the rotation angle is close to zero. The standard deviation of the mean values of rotations obtained for single patients were close to 1 degree.
Fig. 4.
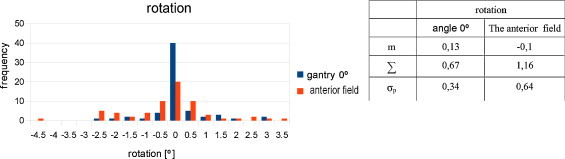
Histogram of rotations.
Result of differences obtained by two physicists.
The mean values for both the left–right and the cranial–caudal directions (0.2 and 0.3 respectively) were statistically not different from zero (p > 0.1). However, the standard deviations were quite large. The standard deviations for the left–right and the cranial–caudal directions were 2.5 and 3.2 mm, respectively.
5. Discussion
In order to evaluate the quality of our immobilization system for patients treated after mastectomy and to compare two protocols of setup corrections, we analyzed the magnitude of the systematic and random errors in two groups of patients. In the first group, the mNAL protocol supplemented with portal controls made in subsequent weeks of treatment was implemented. In the other group of patients, the Internal Protocol was used. Significantly smaller number of portal controls were made with the Internal Protocol than with the mNAL protocol: 520 and 1080 setup controls, respectively.
Different results of errors for the cranial–caudal direction obtained from portal at gantry 0° and for anterior oblique beams may be explained by rotations. Rotations make image registrations less accurate for anterior oblique portals.
Rotations which can be observed in the images for 0° are usually caused by patient setup deviation along the sagittal axis, which was easy to correct. The rotations observed in the images taken for the field at 50° are mainly caused by the changes in the shape of the chest wall associated with breathing and patient's body tension.
The setup errors were examined as a function of the number of treatment sessions. No statistically significant time trends were observed. Numerically, the population systematic errors for both directions are larger for the Internal Protocol than for the mNAL protocol (p > 0.05). However, the difference is statistically insignificant. The data obtained for the mNAL protocol as well as for the Internal Protocol are satisfactory. Similar results were obtained for patients treated with the Inverse Hockey Stique Technique.11 For this technique, the systematic errors for the left–right and cranial–caudal directions were 1.9 and 1.7 mm, respectively, and random errors were 2.0 and 2.5 mm, respectively. Results published in the cited article and in our article refer to patients positioned supine horizontally.
Indirectly, such good results indicate that our immobilization system used for our patients was properly designed. In our opinion the key points for good reproducibility are: the flat position of the patient and the possibility to always keep the hands in the same position. In most centers, different types of inclined wedge immobilization systems are used. The reason to use the inclined wedge was to keep the chest wall horizontal, which enables to avoid a collimator rotation. This was reasonable for 2D planning and for tangential fields. Nowadays, when more complicated techniques are used, with implementation of accelerators equipped with multileaf collimators, any comfortable position of a patient may be acceptable. The flat position is not only comfortable and quite stable but also leads to minimal tensions of the chest muscles. The arms are placed on wedge support with hands placed on the individually chosen rods. There is only one angle of the wedge support which, for some patients, may cause some problems, especially if physiotherapy performed after mastectomy was not performed properly. However, such situations happened very seldom.
Internal Procedure was introduced to evaluate the influence of errors made in the anterior–posterior direction set on the reproducibility of patients’ set-up. The data revealed that errors in the a–p direction setting of more than 5 mm are very rare. Only for 5 patients (7.5% of 65 patients), the anterior–posterior direction errors were larger than 5 mm. In this group (65 patients), after the 3° fraction, 37 corrections were made (56% of cases), with 21 (32%) in the left–right direction, 11 (17%) in the cranial–caudal direction.
Table 4 shows the set-up margins calculated with the Marcel van Herk formula16 if: (1) no correction, (2) mNAL protocol and (3) Internal Procedure would be applied. The smallest set-up margins are for the mNAL protocol but margins for the Internal Procedure, which takes less effort than mNAL, are not much larger. It should be noticed that in this location it is very likely that the largest uncertainty is introduced by doctor's delineation6 which, if accounted for in margin calculation,8,10,15–17 would make the difference negligible.
Table 4.
The set-up margins for: no correction, mNAL protocol and Internal Procedure.
| Protocol used | No correction |
mNAL |
Internal Procedure |
|||
|---|---|---|---|---|---|---|
| Analyzed the directions | Left–right | Cranial–caudal | Left–right | Cranial–caudal | Left–right | Cranial–caudal |
| Random errors σp | 1.7 | 1.7 | 1.7 | 1.7 | 1.7 | 1.7 |
| Systematic errors ∑ | 2.4 | 2.8 | 1.6 | 1.5 | 1.7 | 2.1 |
| Differences between operators | 0.2 | 0.3 | 0.2 | 0.3 | 0.2 | 0.3 |
| Margins [mm] | 7.2 | 8.2 | 5.1 | 4.9 | 5.4 | 6.4 |
Quite small rotations were observed. For the 0° field in 97% of portals, the error was smaller than 2°. For the oblique field, results were only a little worse. Errors smaller than 2° were observed in 87% of portals. These results confirmed the right decisions made in immobilization system designing. Our experience was that rotations were one of the most difficult problem in the set-up of patients with inclined systems.
Comparison of off-line image registration results performed by two experienced users revealed that image matching is not an easy task and is susceptible to subjectivity. One standard deviation of differences between results obtained by two users for the 0° field degree and the oblique field were 2.5 and 3.2 mm, respectively. These results make on-line corrections very difficult and unreliable. The off-line procedures of set-up control are more reliable.
6. Conclusions
Implementation of the mNAL protocol or our Internal Protocol for patients irradiated after mastectomy, immobilized with our immobilization system, enable a very good setup reproducibility. The Internal Protocol allows for checking if the SSD was properly set. The errors in the setting of the anterior–posterior direction exceeding 5 mm are quite rare.
Conflict of interest
None declared.
Financial disclosure
None declared.
References
- 1.Bijhold J., Lebesque J.V., Hart A.A.M. Maximizing setup accuracy using portal images as applied to conformal boost technique for prostatic cancer. Radiother Oncol. 1992;24:261–271. doi: 10.1016/0167-8140(92)90233-k. [DOI] [PubMed] [Google Scholar]
- 2.Caudrelier J.-M., Morgan S.C., Montgomery L. Helical tomotherapy for locoregional irradiation including mammary chain in left-side breast cancer: dosimetric evaluation. Radiother Oncol. 2009;90:99–105. doi: 10.1016/j.radonc.2008.09.028. [DOI] [PubMed] [Google Scholar]
- 3.Dąbrowski A., Kukołowicz P.F., Paczkowski N. Trendy czasowe odtwarzalność ułożenia pacjentów leczonych z powodu nowotworów piersi po mastektomii, ginekologicznych i prostaty. Rep Pract Oncol Radiother. 2004;9(Suppl. 2):S287–S288. [Google Scholar]
- 4.Gaffney D.K., Leavitt D.D., Tsodikov A. Electron arc irradiation of the postmastectomy chestwall with ct treatment planning: 20-year experience. Int J Radiat Oncol Biol Phys. 2001;51:994–1001. doi: 10.1016/s0360-3016(01)01726-6. [DOI] [PubMed] [Google Scholar]
- 5.Gauer T., Engel K., Kiesel A. Comparison of electron IMRT to helical photon IMRT and conventional photon irradiation of breast and chest wall tumours. Radiother Oncol. 2010;94:313–318. doi: 10.1016/j.radonc.2009.12.037. [DOI] [PubMed] [Google Scholar]
- 6.Dobbs H.J., Greener A.G., Driver A.M. The British Institute of Radiology; 2003. Geometric uncertainties in radiotherapy; pp. 63–64. [chapter 3] [Google Scholar]
- 7.de Boer H.C.J., Heijmen B.J.M. eNAL: an extensional of the NAL setup correction protocol for effective use of weekly follow-up measurements. Int J Radiat Oncol Biol Phys. 2007;67:1586–1595. doi: 10.1016/j.ijrobp.2006.11.050. [DOI] [PubMed] [Google Scholar]
- 8.Hurkmans C.W., Remeijer P., Lebesque J.V. Set-up verification using portal imaging; review of current clinical practice. Radiother Oncol. 2001;58:105–120. doi: 10.1016/s0167-8140(00)00260-7. [DOI] [PubMed] [Google Scholar]
- 9.ICRU; Bethesda, MD: 1995. International commission on radiation units and measurments ICRU report 62 prescribing, recording and reporting photon beam therapy (supplement + IDRU report 50) [Google Scholar]
- 10.McKenzie A., Van Herk M., Mijnheer B. Margins for geometric uncertainty organs at risk in radiotherapy. Radiother Oncol. 2002;62:299–307. doi: 10.1016/s0167-8140(02)00015-4. [DOI] [PubMed] [Google Scholar]
- 11.Kukołowicz P.F., Dąbrowski A., Gut P. Evaluation of set-up deviations during the irradiation of patients suffering from breast cancer treated with two different technique. Radiother Oncol. 2005;75:22–27. doi: 10.1016/j.radonc.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 12.Pierce L.J., Butler J.B., Martel M.K. Postmastectomy radiotherapy of the chest wall: dosimetric comparison of common techniques. Int J Radiat Oncol Biol Phys. 2002;52:1220–1230. doi: 10.1016/s0360-3016(01)02760-2. [DOI] [PubMed] [Google Scholar]
- 13.Ragaz J., Jackson S.M., Le N. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med. 1997;337:956–962. doi: 10.1056/NEJM199710023371402. [DOI] [PubMed] [Google Scholar]
- 14.Semaniak A., Jodkiewicz Z., Skowrońska-Gardas A. Segmented photon beams technique for irradiation of postmastectomy patients. Rep Pract Oncol Radiother. 2011;17(2):85–92. doi: 10.1016/j.rpor.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stroom J.C., Heijmen Ben J.M. Geometrical uncertainties, radiotherapy planning margins, and the ICRU-62 report. Radiother Oncol. 2002;64:75–83. doi: 10.1016/s0167-8140(02)00140-8. [DOI] [PubMed] [Google Scholar]
- 16.Van Herk M., Remeijer P., Rasch C. The probability of correct target dosage: dose-population histograms for deriving treatment margins in radiotherapy. Int J Radiat Oncol Biol Phys. 2000;47:1121–1135. doi: 10.1016/s0360-3016(00)00518-6. [DOI] [PubMed] [Google Scholar]
- 17.Yang D.S., Yoon W.S., Chung S.Y. Set-up uncertainty during breast radiotherapy. Image-guided radiotherapy for patients with initial extensive variation. Strahlenther Onkol. 2013;189:315–320. doi: 10.1007/s00066-012-0271-4. [DOI] [PubMed] [Google Scholar]


