Summary
Each year, the American Heart Association (AHA), in conjunction with the Centers for Disease Control and Prevention, the National Institutes of Health, and other government agencies, brings together the most up-to-date statistics on heart disease, stroke, other vascular diseases, and their risk factors and presents them in its Heart Disease and Stroke Statistical Update. The Statistical Update is a valuable resource for researchers, clinicians, healthcare policy makers, media professionals, the lay public, and many others who seek the best national data available on disease morbidity and mortality and the risks, quality of care, medical procedures and operations, and costs associated with the management of these diseases in a single document. Indeed, since 1999, the Statistical Update has been cited more than 8700 times in the literature (including citations of all annual versions). In 2009 alone, the various Statistical Updates were cited ≈1600 times (data from ISI Web of Science). In recent years, the Statistical Update has undergone some major changes with the addition of new chapters and major updates across multiple areas. For this year’s edition, the Statistics Committee, which produces the document for the AHA, updated all of the current chapters with the most recent nationally representative data and inclusion of relevant articles from the literature over the past year and added a new chapter detailing how family history and genetics play a role in cardiovascular disease (CVD) risk. Also, the 2011 Statistical Update is a major source for monitoring both cardiovascular health and disease in the population, with a focus on progress toward achievement of the AHA’s 2020 Impact Goals. Below are a few highlights from this year’s Update.
Death Rates From CVD Have Declined, Yet the Burden of Disease Remains High
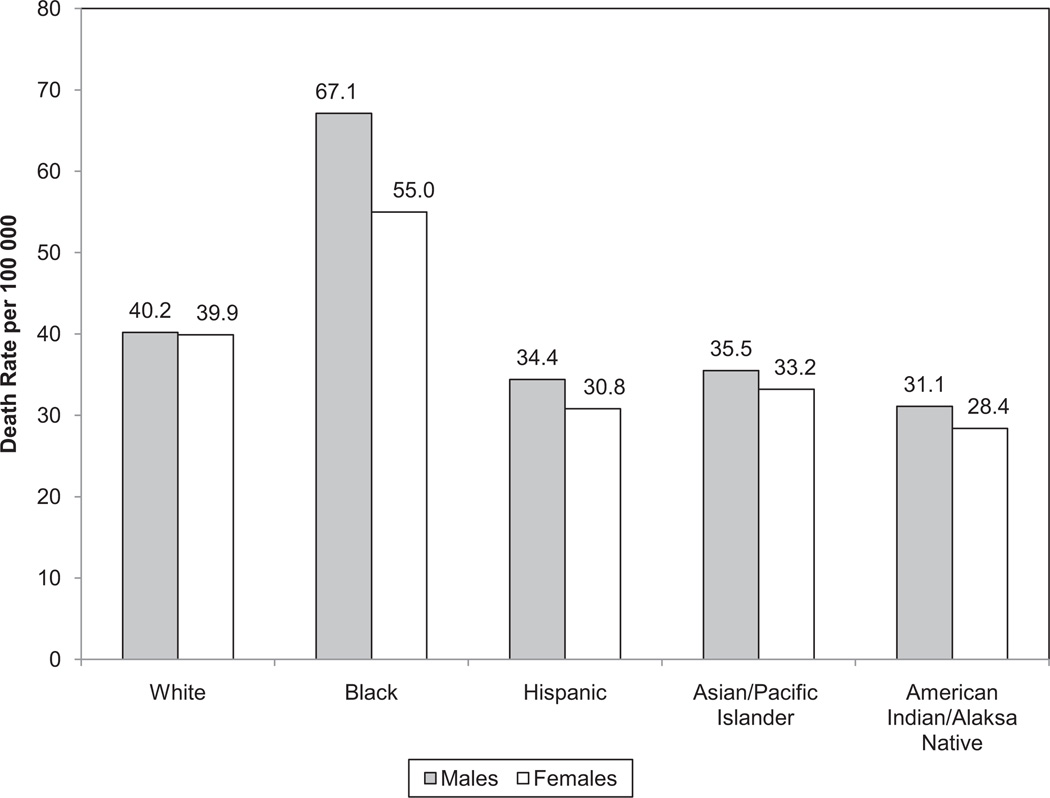
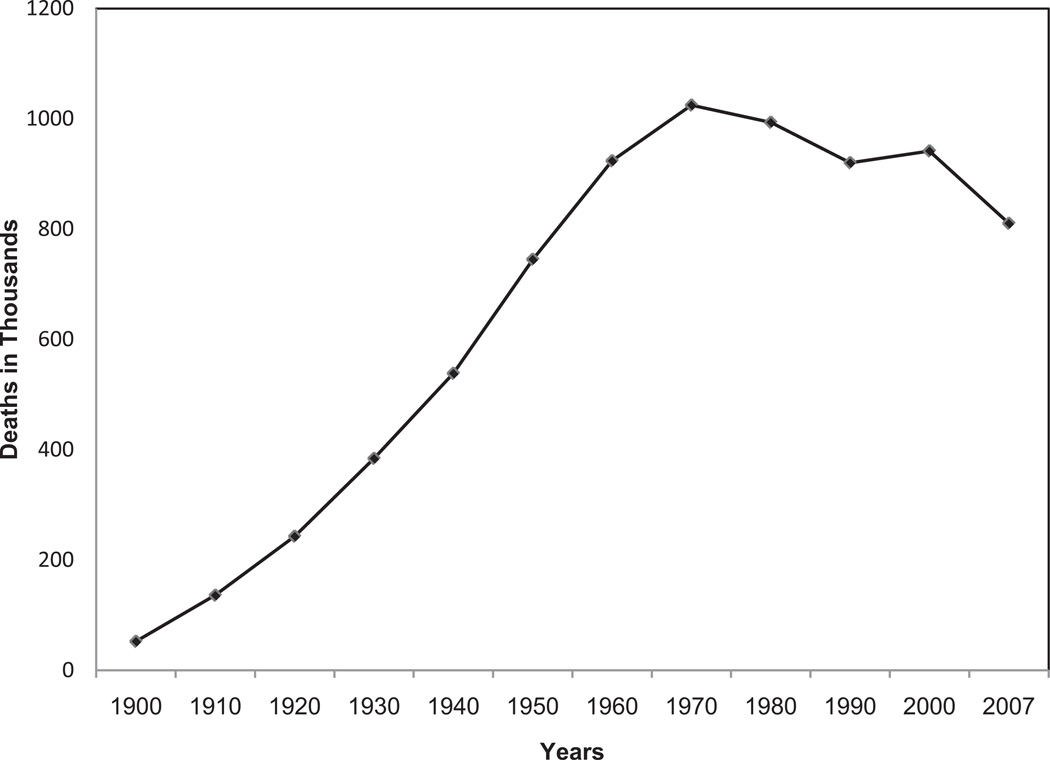
The 2007 overall death rate from CVD (International Classification of Diseases 10, I00–I99) was 251.2 per 100 000. The rates were 294.0 per 100 000 for white males, 405.9 per 100 000 for black males, 205.7 per 100 000 for white females, and 286.1 per 100 000 for black females. From 1997 to 2007, the death rate from CVD declined 27.8%. Mortality data for 2007 show that CVD (I00–I99; Q20–Q28) accounted for 33.6% (813 804) of all 2 243 712 deaths in 2007, or 1 of every 2.9 deaths in the United States.
On the basis of 2007 mortality rate data, more than 2200 Americans die of CVD each day, an average of 1 death every 39 seconds. More than 150 000 Americans killed by CVD (I00–I99) in 2007 were <65 years of age. In 2007, nearly 33% of deaths due to CVD occurred before the age of 75 years, which is well before the average life expectancy of 77.9 years.
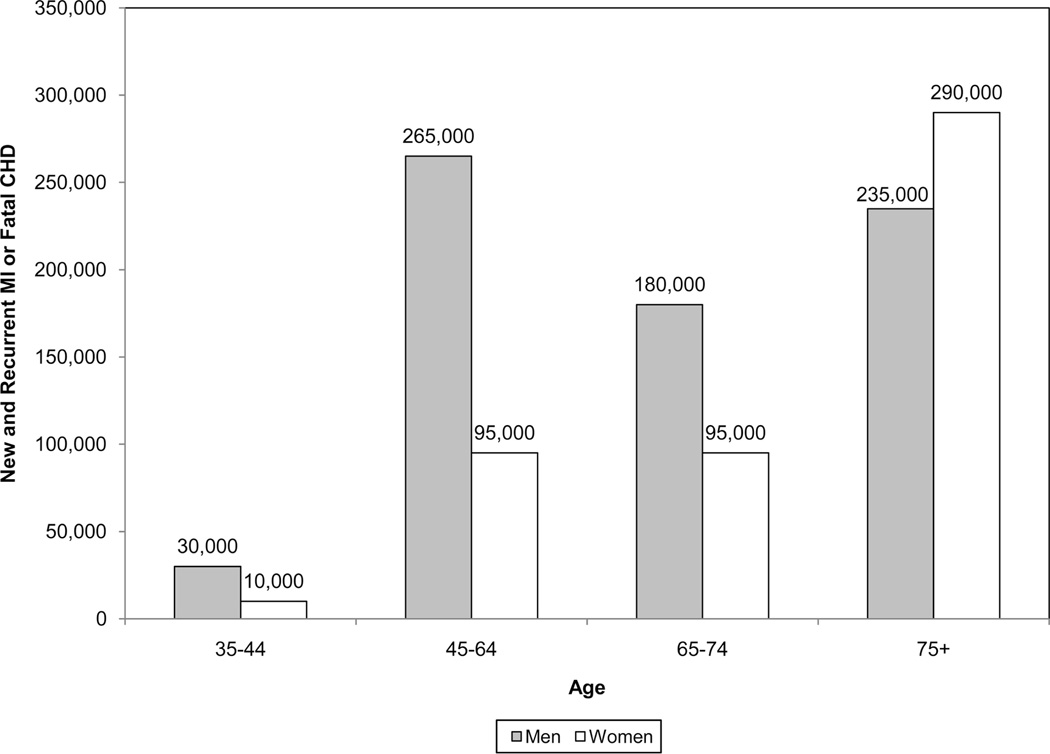
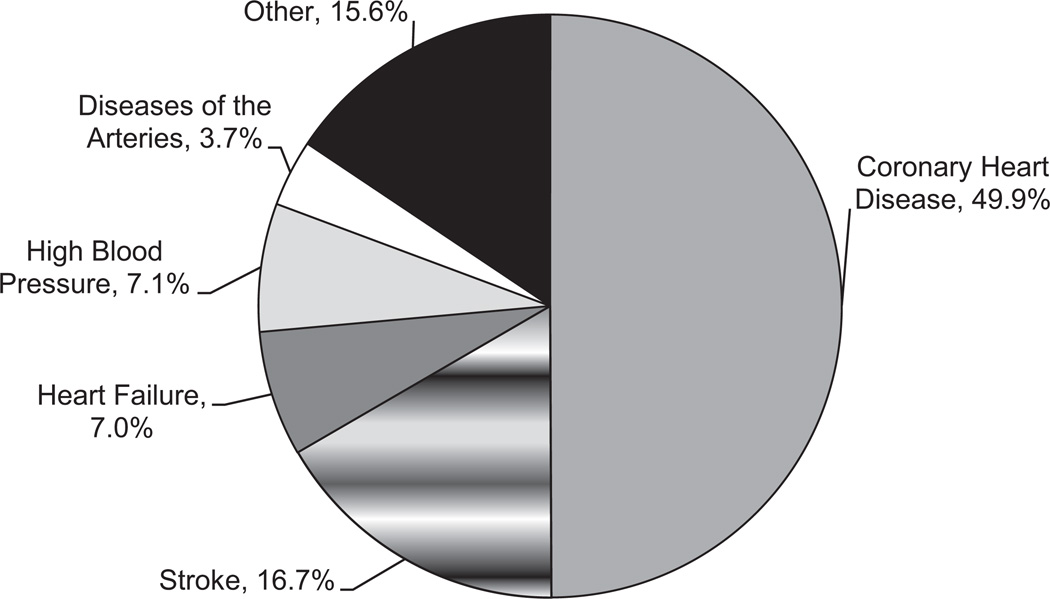
Coronary heart disease caused ≈1 of every 6 deaths in the United States in 2007. Coronary heart disease mortality in 2007 was 406 351. Each year, an estimated 785 000 Americans will have a new coronary attack, and ≈470 000 will have a recurrent attack. It is estimated that an additional 195 000 silent first myocardial infarctions occur each year. Approximately every 25 seconds, an American will have a coronary event, and approximately every minute, someone will die of one.
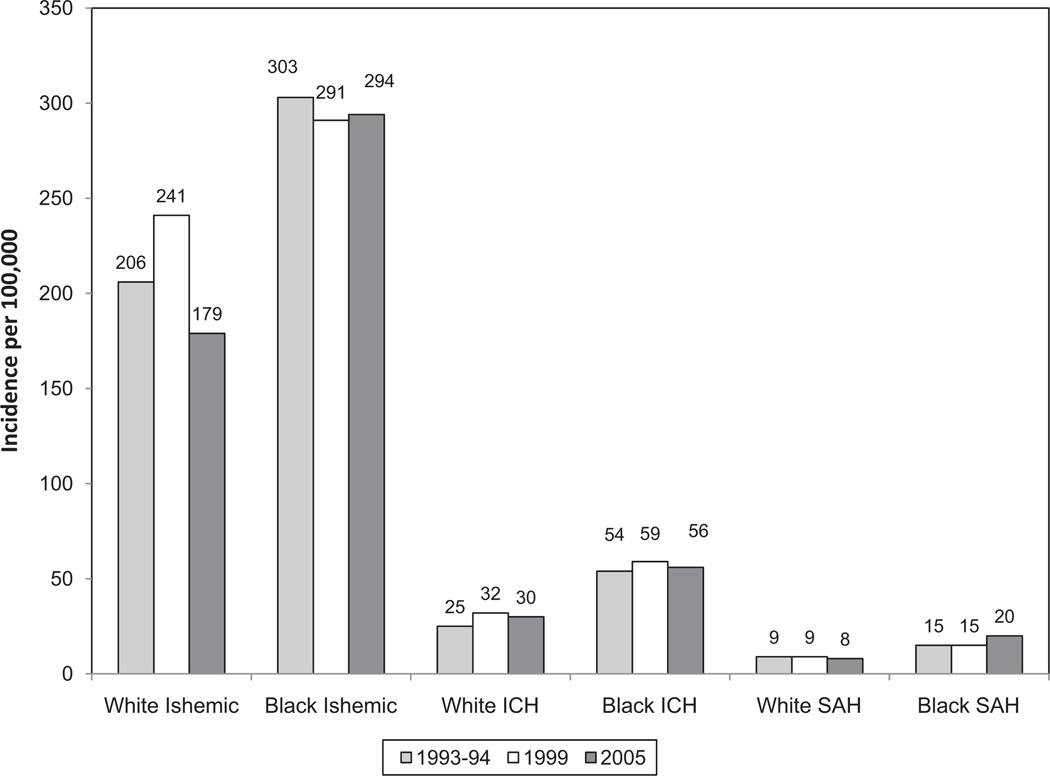
Each year, ≈795 000 people experience a new or recurrent stroke. Approximately 610 000 of these are first attacks, and 185 000 are recurrent attacks. Mortality data from 2007 indicate that stroke accounted for ≈1 of every 18 deaths in the United States. On average, every 40 seconds, someone in the United States has a stroke. From 1997 to 2007, the stroke death rate fell 44.8%, and the actual number of stroke deaths declined 14.7%.
In 2007, 1 in 9 death certificates (277 193 deaths) in the United States mentioned heart failure.
Prevalence and Control of Traditional Risk Factors Remains an Issue for Many Americans
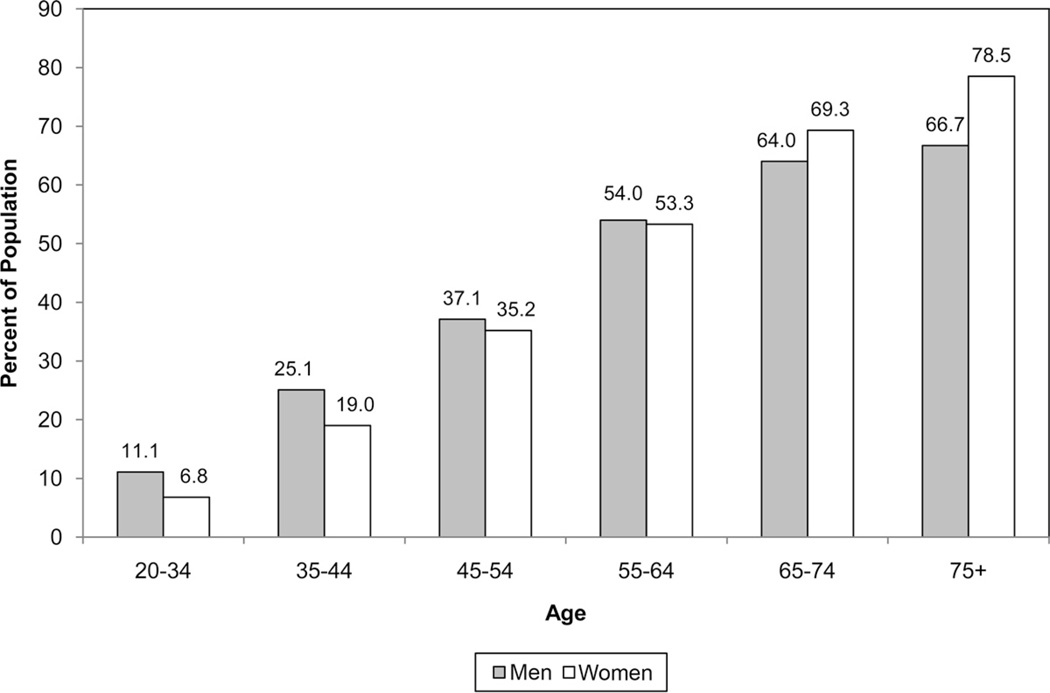
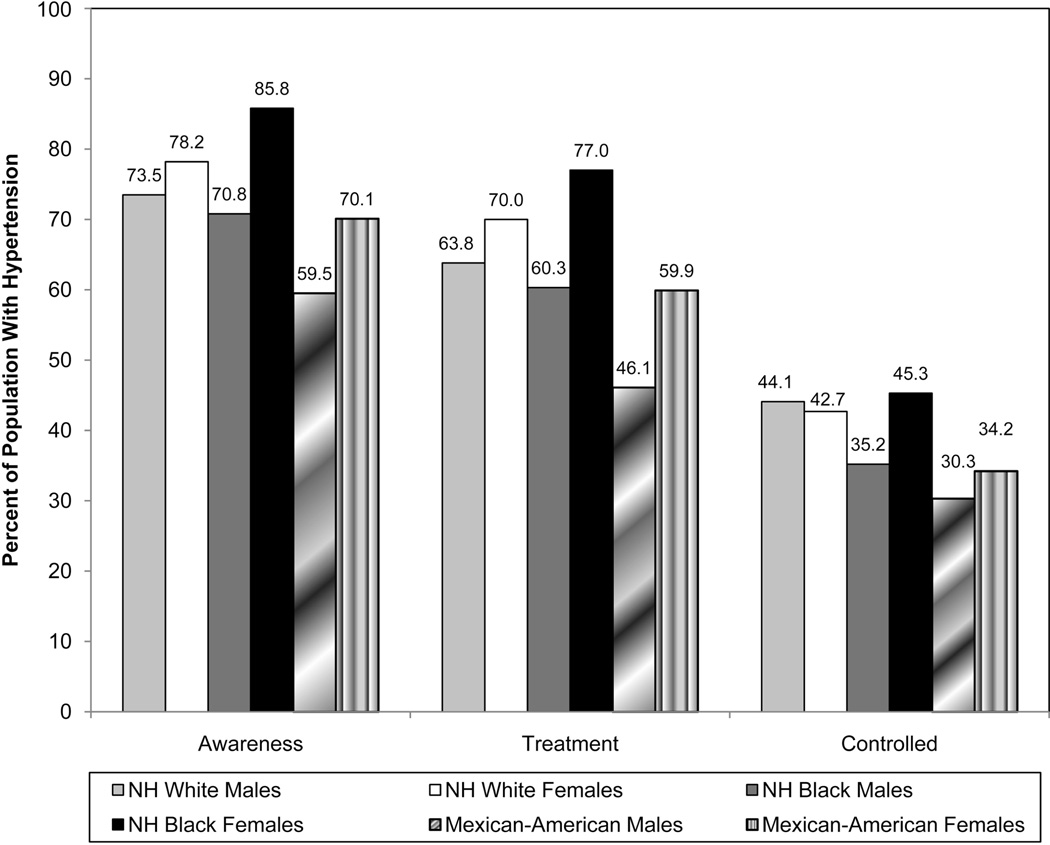
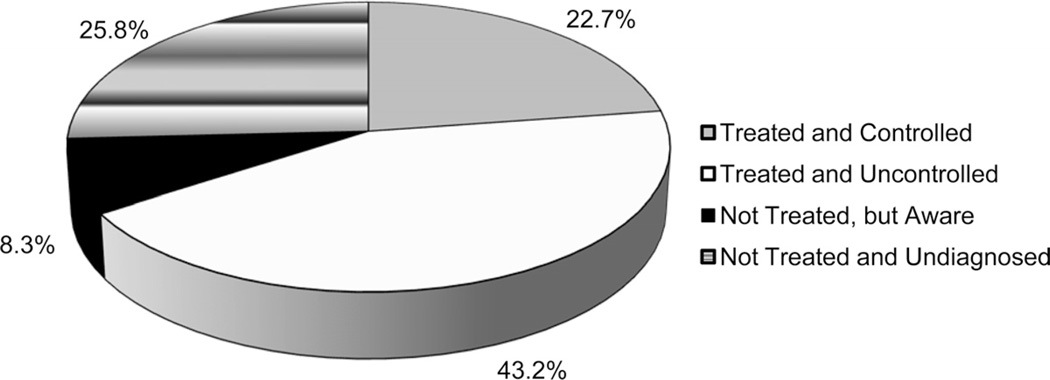
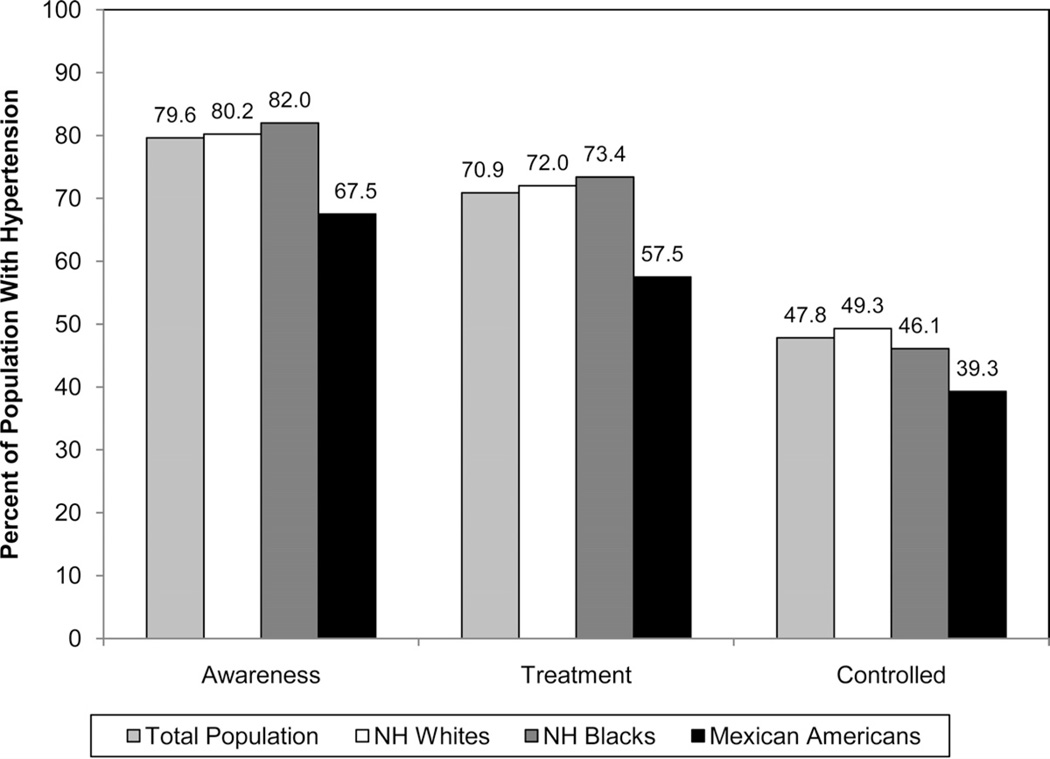
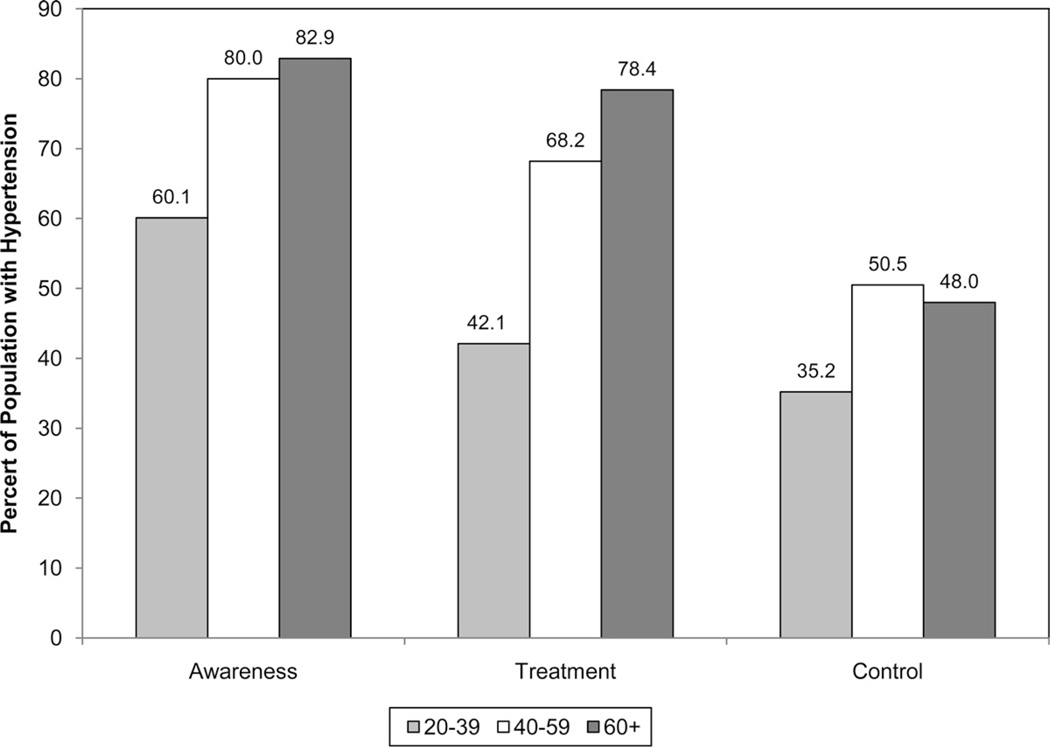
Data from the National Health and Nutrition Examination Survey (NHANES) 2005–2008 indicate that 33.5% of US adults ≥20 years of age have hypertension (Table 7-1). This amounts to an estimated 76 400 000 US adults with hypertension. The prevalence of hypertension is nearly equal between men and women. African American adults have among the highest rates of hypertension in the world, at 44%. Among hypertensive adults, ≈80% are aware of their condition, 71% are using antihypertensive medication, and only 48% of those aware that they have hypertension have their condition controlled.
Despite 4 decades of progress, in 2008, among Americans ≥18 years of age, 23.1% of men and 18.3% of women continued to be cigarette smokers. In 2009, 19.5% of students in grades 9 through 12 reported current tobacco use. The percentage of the nonsmoking population with detectable serum cotinine (indicating exposure to secondhand smoke) was 46.4% in 1999 to 2004, with declines occurring, and was highest for those 4 to 11 years of age (60.5%) and those 12 to 19 years of age (55.4%).
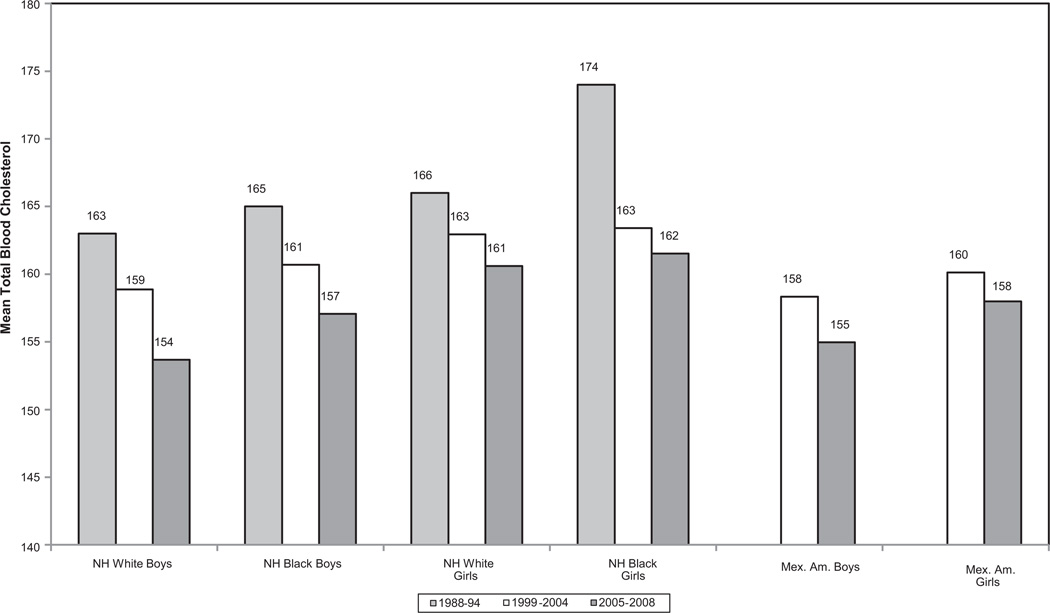
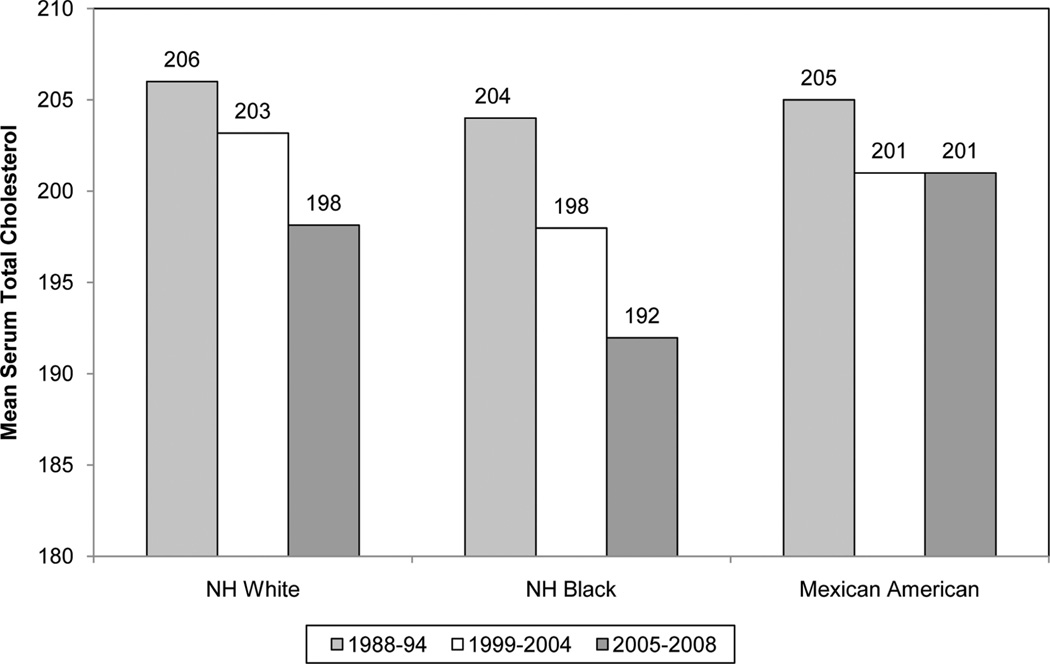
An estimated 33 600 000 adults ≥20 years of age have total serum cholesterol levels ≥240 mg/dL, with a prevalence of 15.0% (Table 13-1).
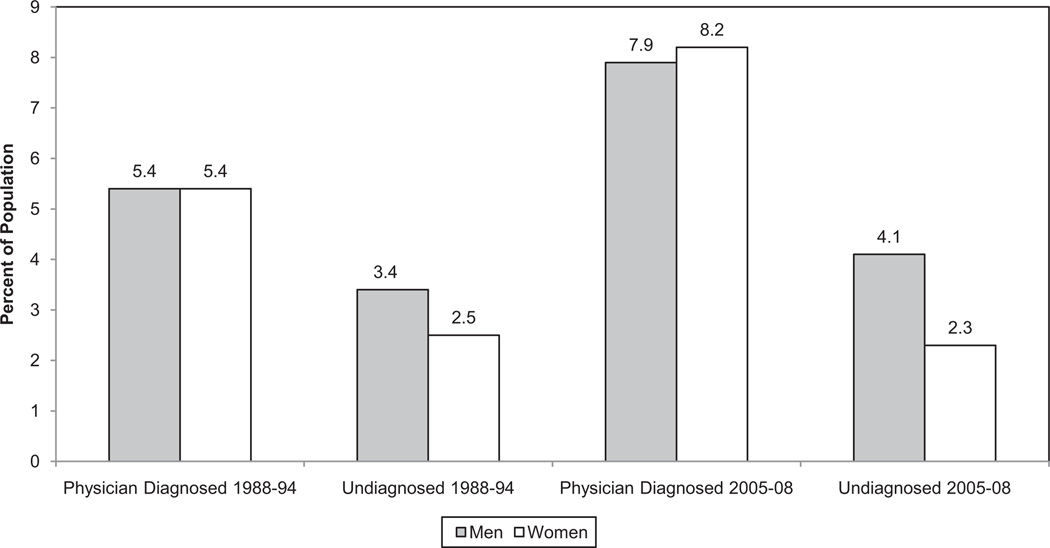
In 2008, an estimated 18 300 000 Americans had diagnosed diabetes mellitus, representing 8.0% of the adult population. An additional 7 100 000 had undiagnosed diabetes mellitus, and 36.8% had prediabetes, with abnormal fasting glucose levels. African Americans, Mexican Americans, Hispanic/Latino individuals, and other ethnic minorities bear a strikingly disproportionate burden of diabetes mellitus in the United States (Table 16-1).
The 2011 Update Expands Data Coverage of the Obesity Epidemic and Its Antecedents and Consequences
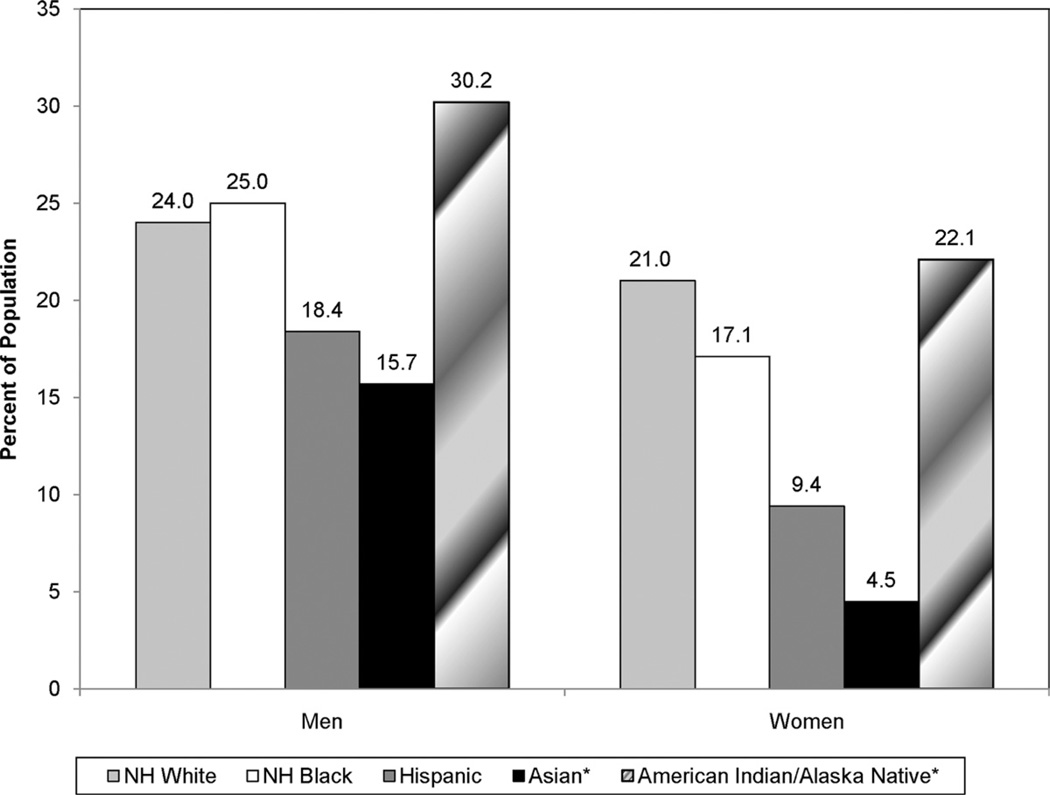
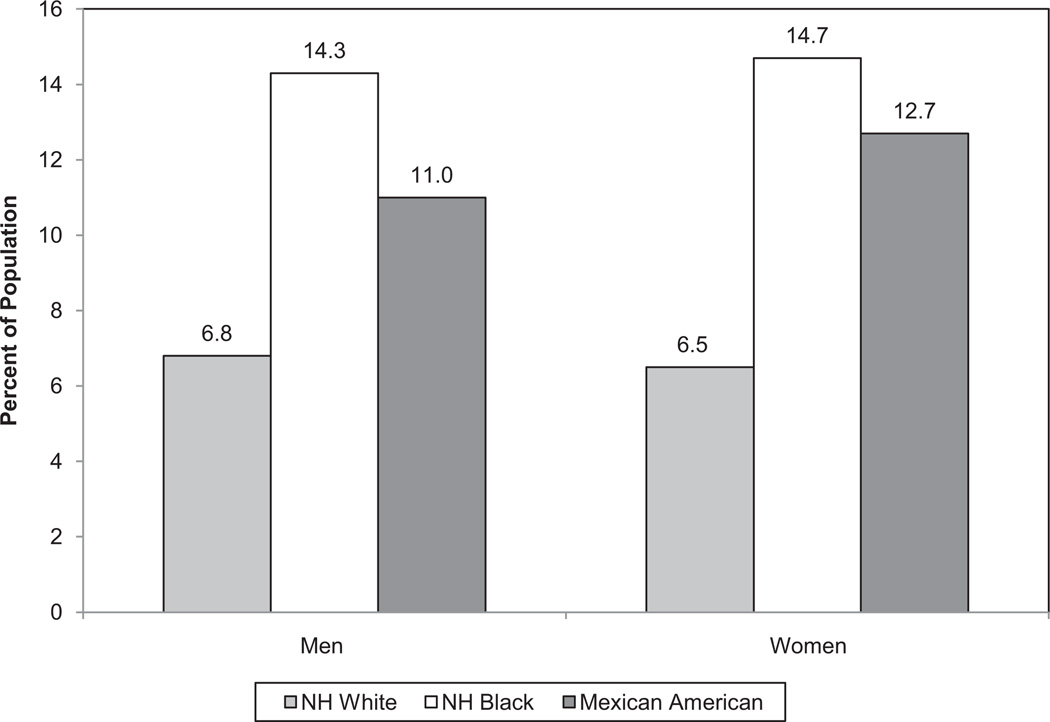
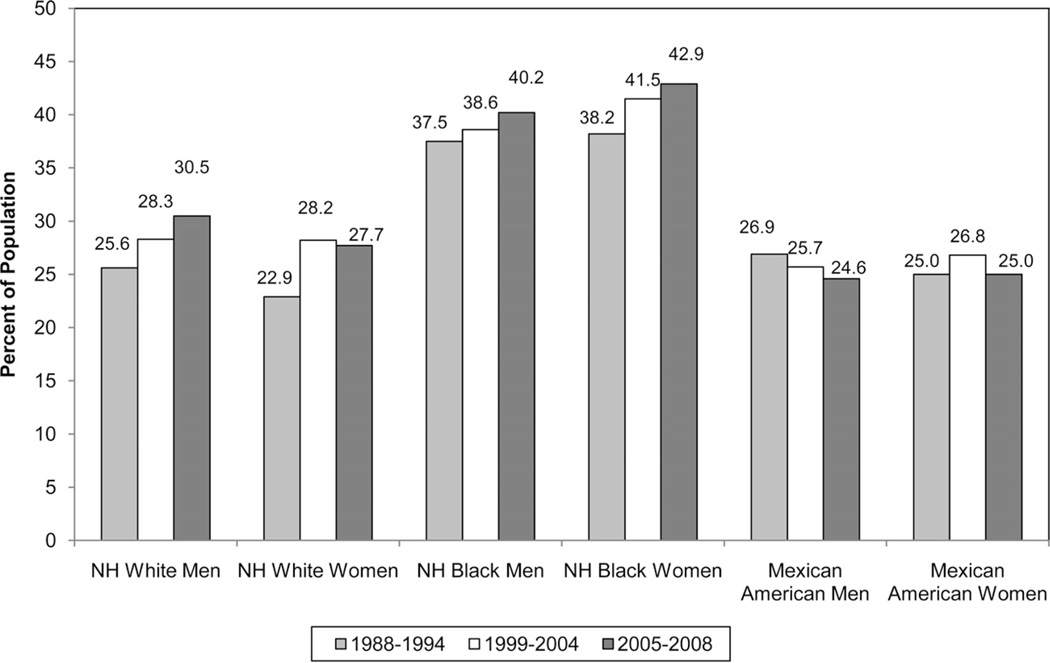
The estimated prevalence of overweight and obesity in US adults (≥20 years of age) is 149 300 000, which represents 67.3% of this group in 2008. Fully 33.7% of US adults are obese (body mass index ≥30 kg/m2). Men and women of all race/ethnic groups in the population are affected by the epidemic of overweight and obesity (Table 15-1).
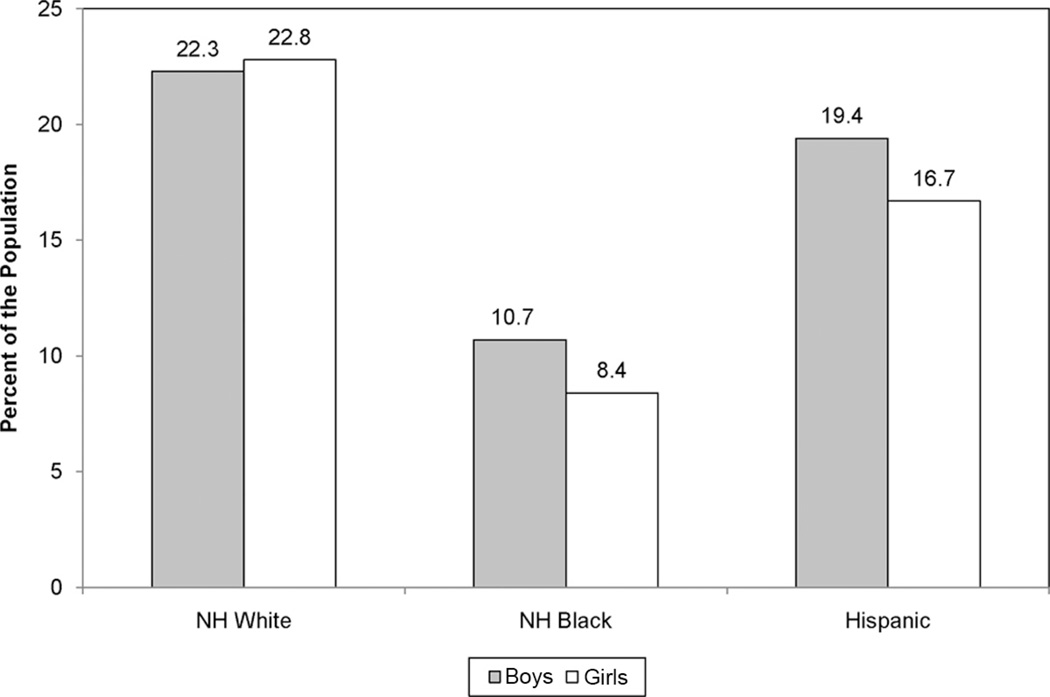
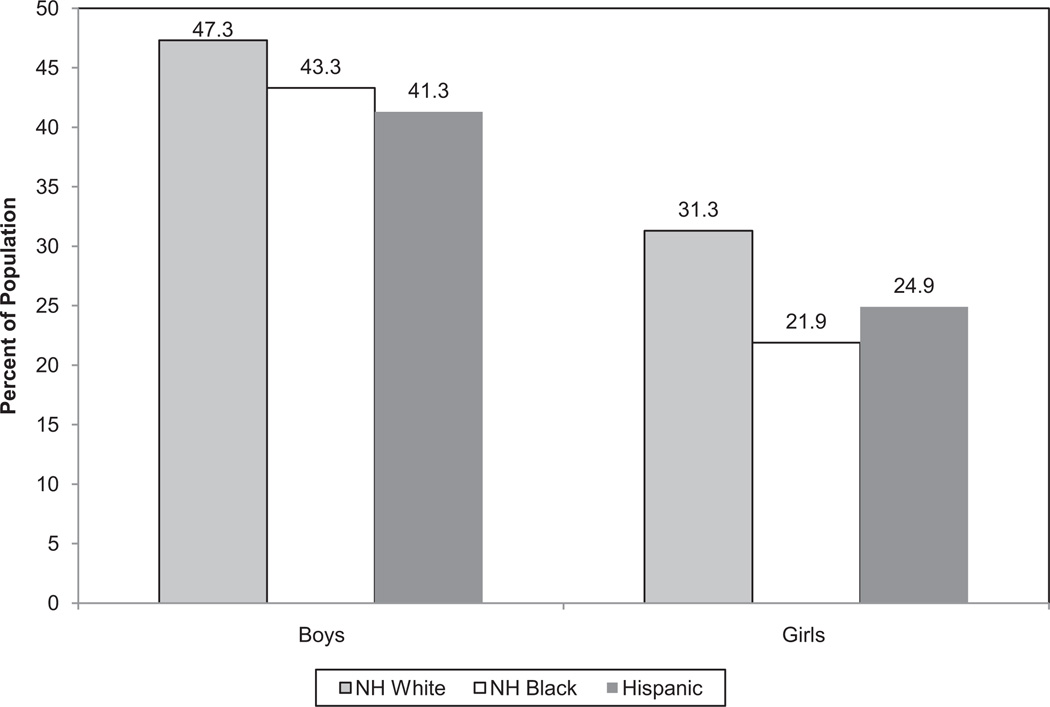
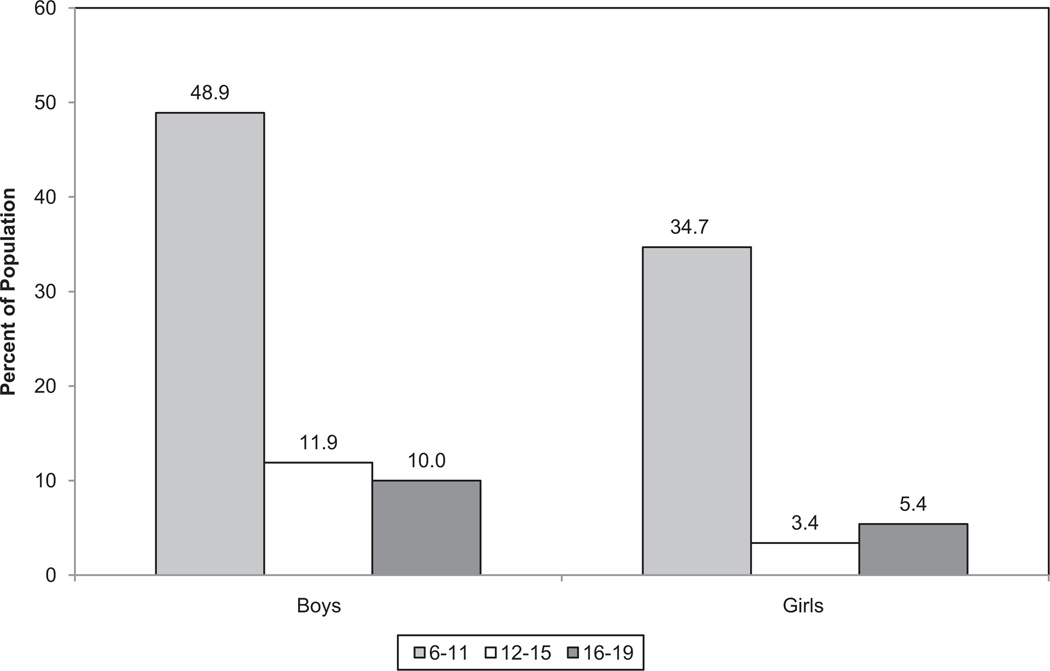
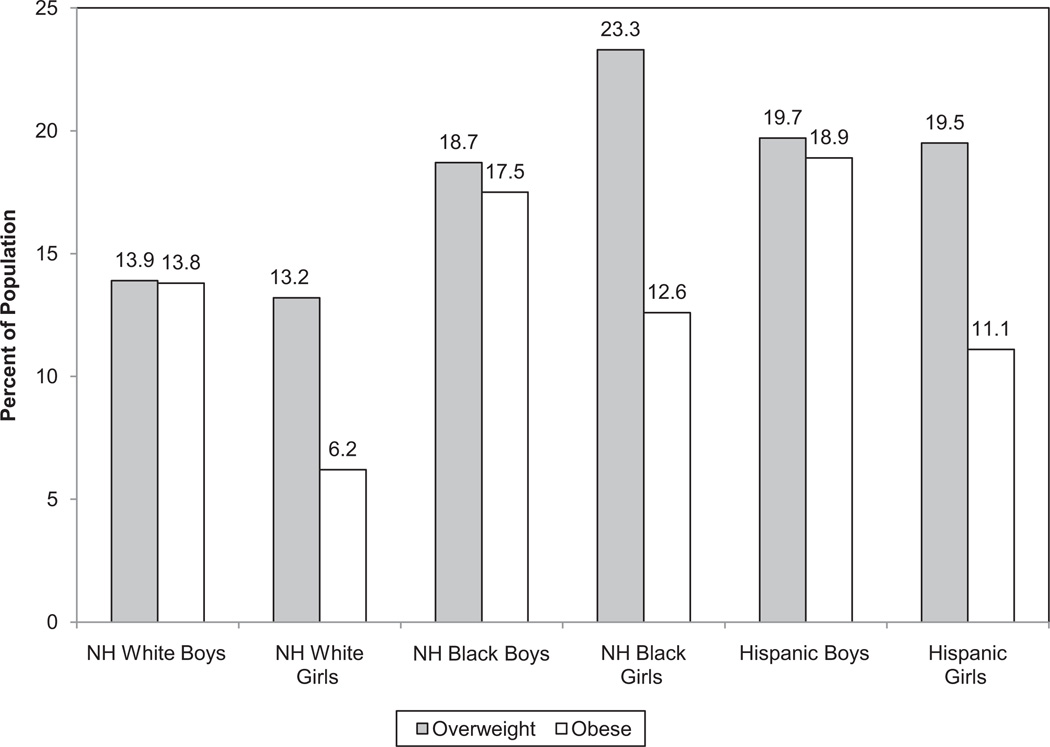
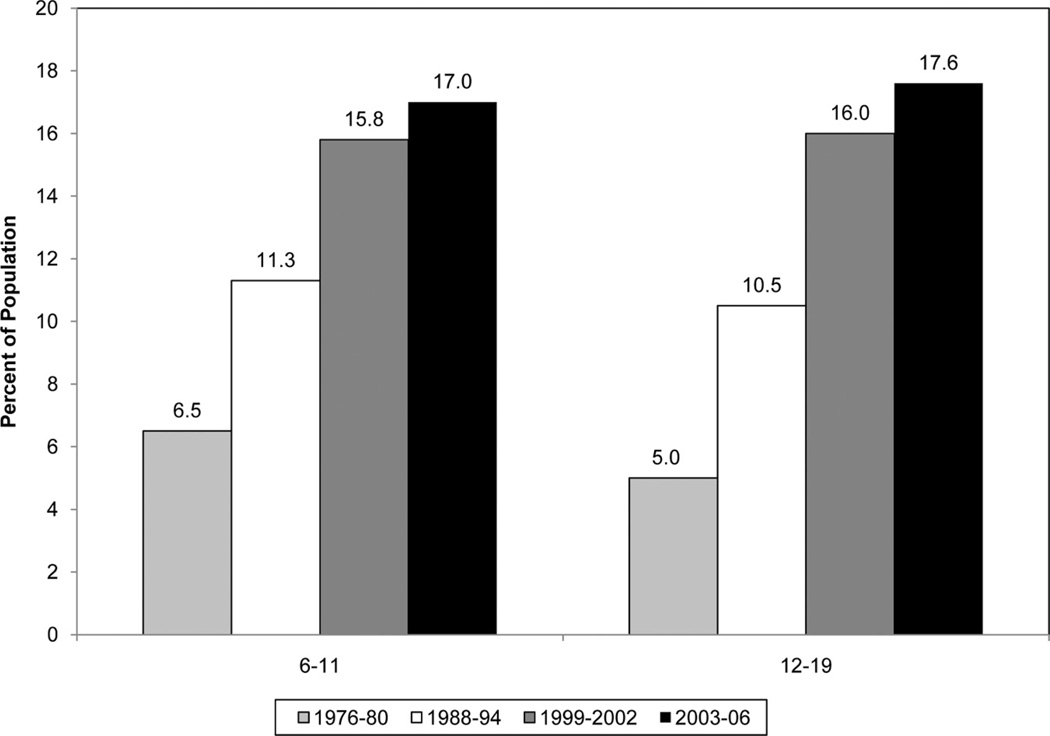
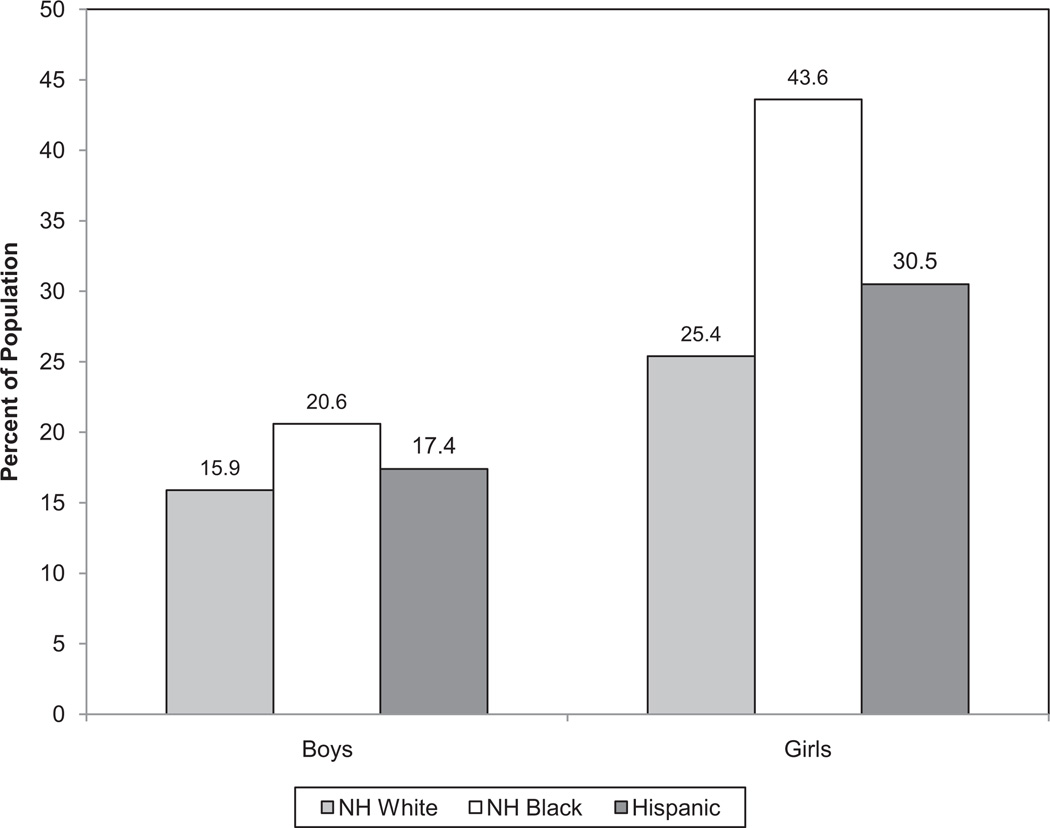
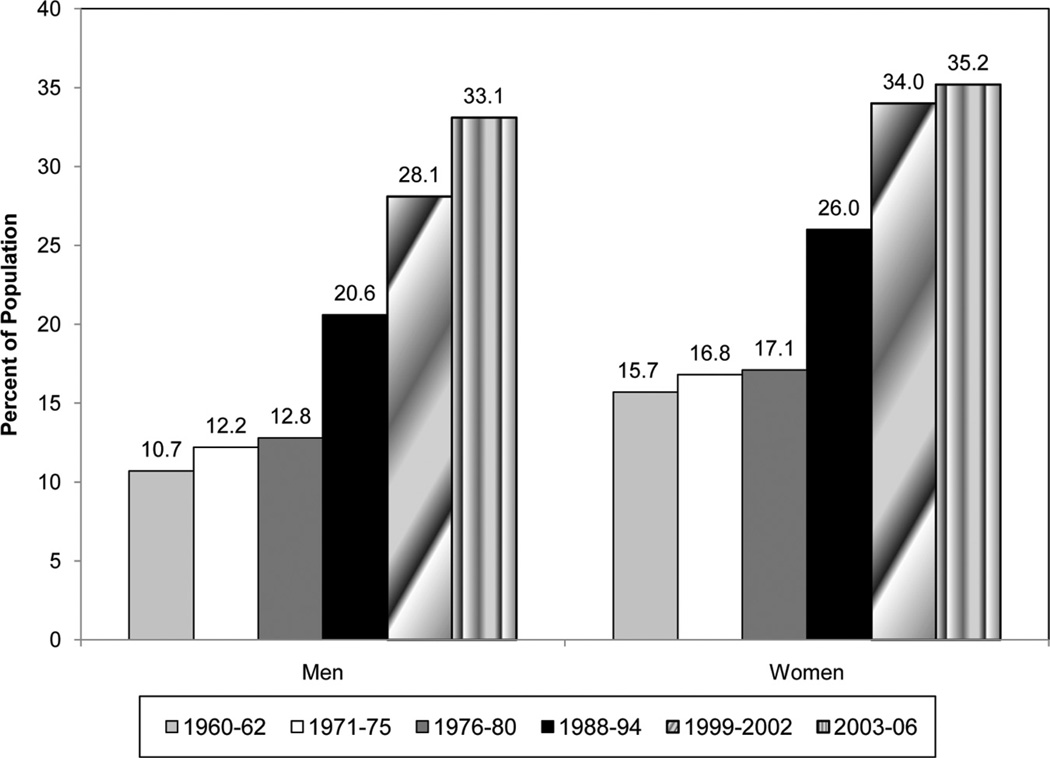
Among children 2 to 19 years of age, 31.9% are overweight and obese (which represents 23 500 000 children), and 16.3% are obese (12 000 000 children). Mexican American boys and girls and African American girls are disproportionately affected. Over the past 3 decades, the prevalence of obesity in children 6 to 11 years of age has increased from ≈4% to more than 20%.
Obesity (body mass index ≥30 kg/m2) is associated with marked excess mortality in the US population. Even more notable is the excess morbidity associated with overweight and obesity in terms of risk factor development and incidence of diabetes mellitus, CVD end points (including coronary heart disease, stroke, and heart failure), and numerous other health conditions, including asthma, cancer, degenerative joint disease, and many others.
The prevalence of diabetes mellitus is increasing dramatically over time, in parallel with the increases in prevalence of overweight and obesity.
On the basis of NHANES 2003–2006 data, the age-adjusted prevalence of metabolic syndrome, a cluster of major cardiovascular risk factors related to overweight/obesity and insulin resistance, is 34% (35.1% among men and 32.6% among women).
The proportion of youth (≤18 years of age) who report engaging in no regular physical activity is high, and the proportion increases with age. In 2007, among adolescents in grades 9 through 12, 29.9% of girls and 17.0% of boys reported that they had not engaged in 60 minutes of moderate-to-vigorous physical activity, defined as any activity that increased heart rate or breathing rate, even once in the previous 7 days, despite recommendations that children engage in such activity ≥5 days per week.
Thirty-six percent of adults reported engaging in no vigorous activity (activity that causes heavy sweating and a large increase in breathing or heart rate).
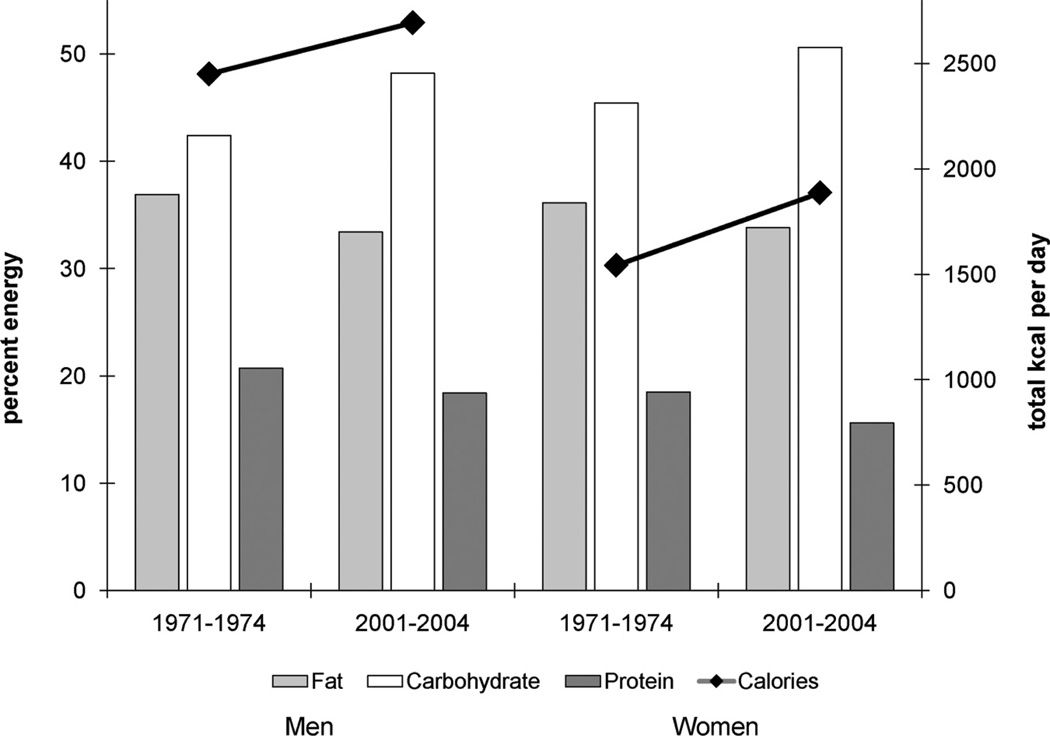
Data from NHANES indicate that between 1971 and 2004, average total energy consumption among US adults increased by 22% in women (from 1542 to 1886 kcal/d) and by 10% in men (from 2450 to 2693 kcal/d; see Chart 19-1).
The increases in calories consumed during this time period are attributable primarily to greater average carbohydrate intake, in particular, of starches, refined grains, and sugars. Other specific changes related to increased caloric intake in the United States include larger portion sizes, greater food quantity and calories per meal, and increased consumption of sugar-sweetened beverages, snacks, commercially prepared (especially fast food) meals, and higher energy-density foods.
The 2011 Update Provides Critical Data Regarding Cardiovascular Quality of Care, Procedure Utilization, and Costs
In light of the current national focus on healthcare utilization, costs, and quality, it is critical to monitor and understand the magnitude of healthcare delivery and costs, as well as the quality of healthcare delivery, related to CVDs. The Update provides these critical data in several sections.
Quality-of-Care Metrics for CVDs
Chapter 20 reviews many metrics related to the quality of care delivered to patients with CVDs, as well as healthcare disparities. In particular, quality data are available from the AHA’s “Get With The Guidelines” programs for coronary artery disease and heart failure and the American Stroke Association/ AHA’s “Get With the Guidelines” program for acute stroke. Similar data from the Veterans Healthcare Administration, national Medicare and Medicaid data and National Cardiovascular Data Registry Acute Coronary Treatment and Intervention Outcomes Network - “Get With The Guidelines” Registry data are also reviewed. These data show impressive adherence with guideline recommendations for many, but not all, metrics of quality of care for these hospitalized patients. Data are also reviewed on screening for cardiovascular risk factor levels and control.
Cardiovascular Procedure Utilization and Costs
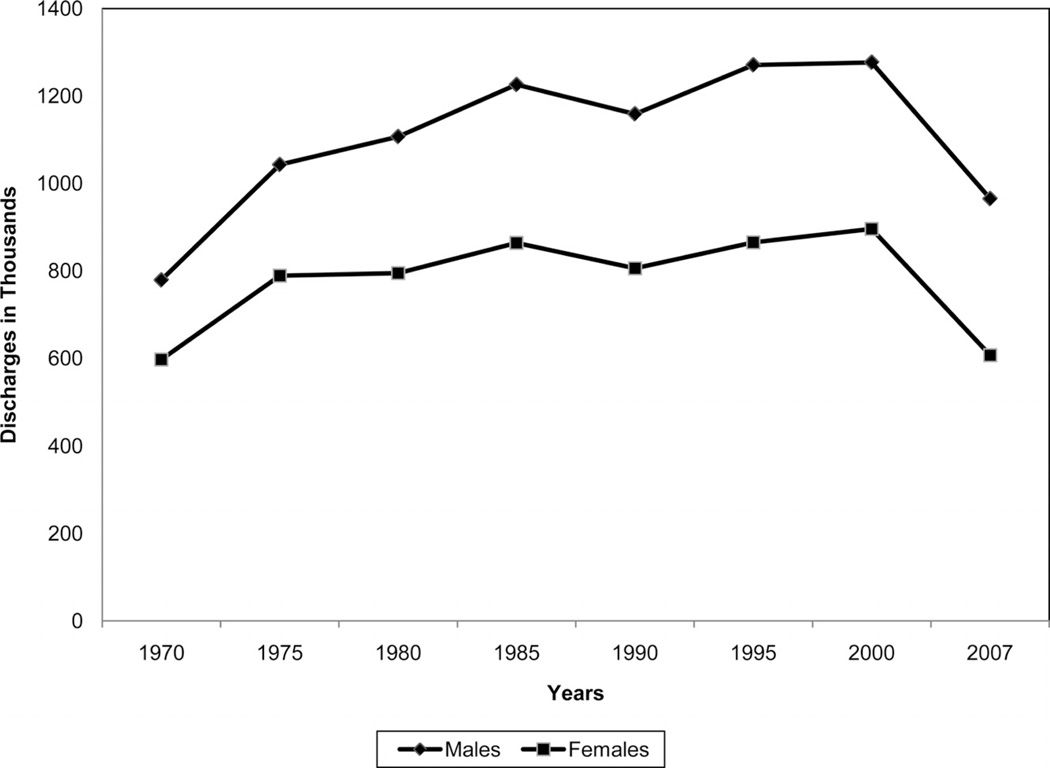
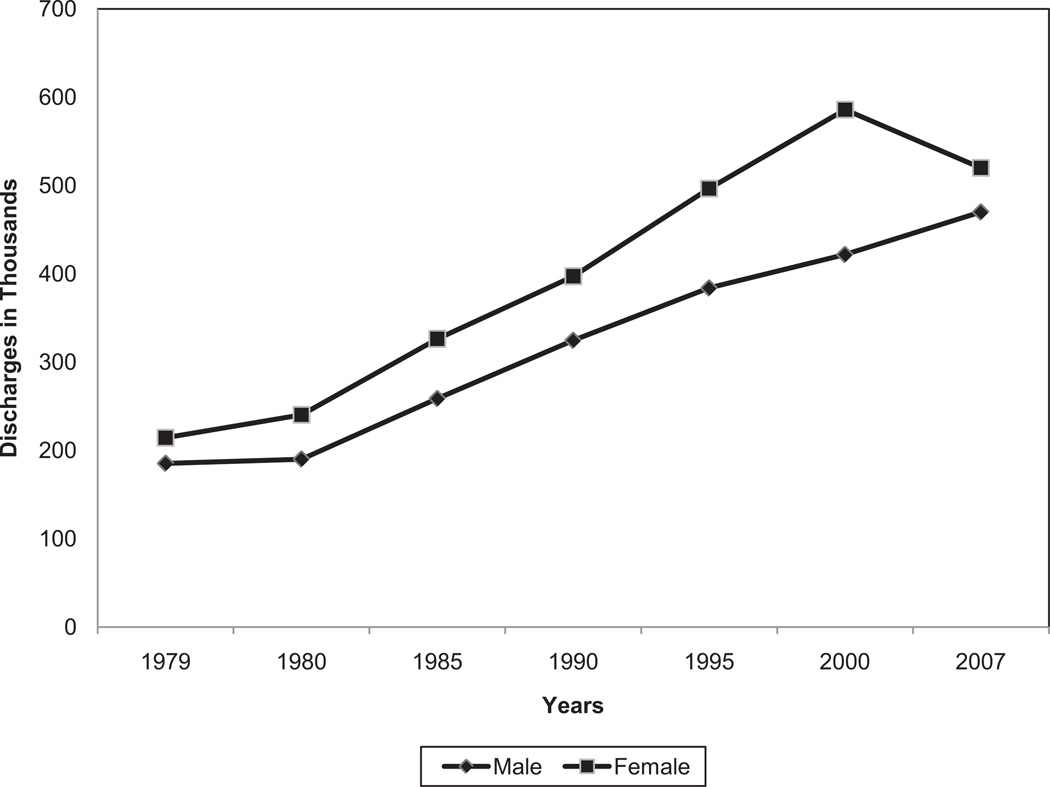
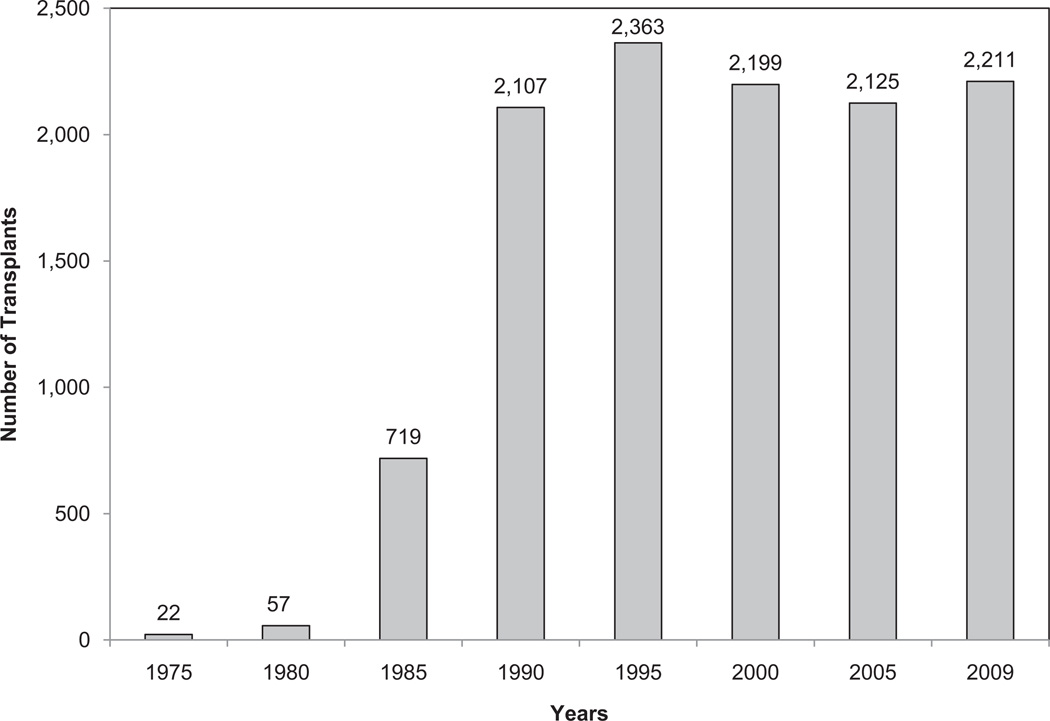
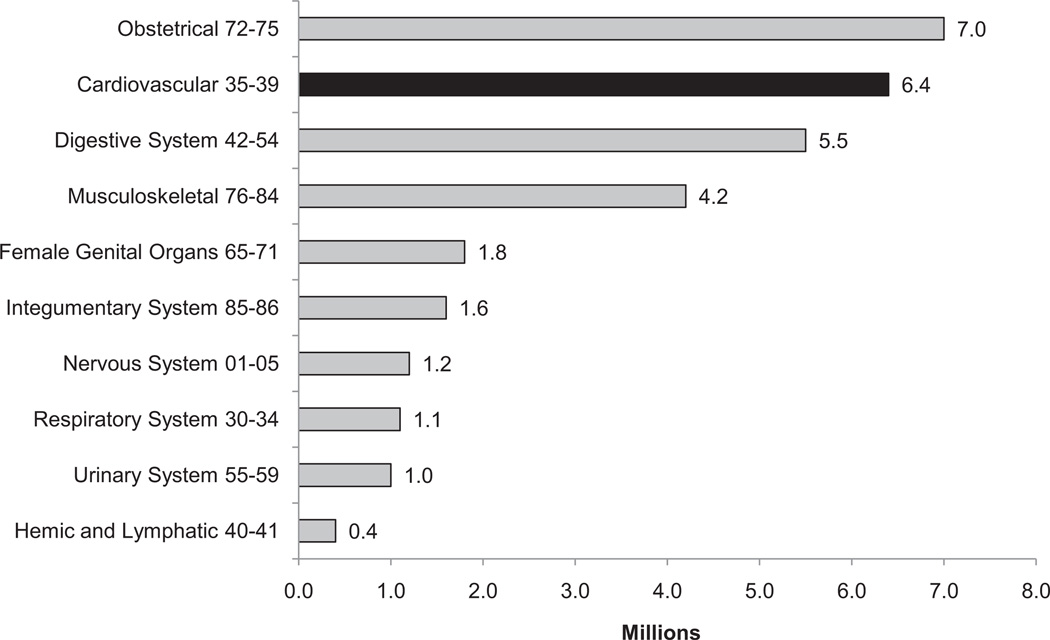
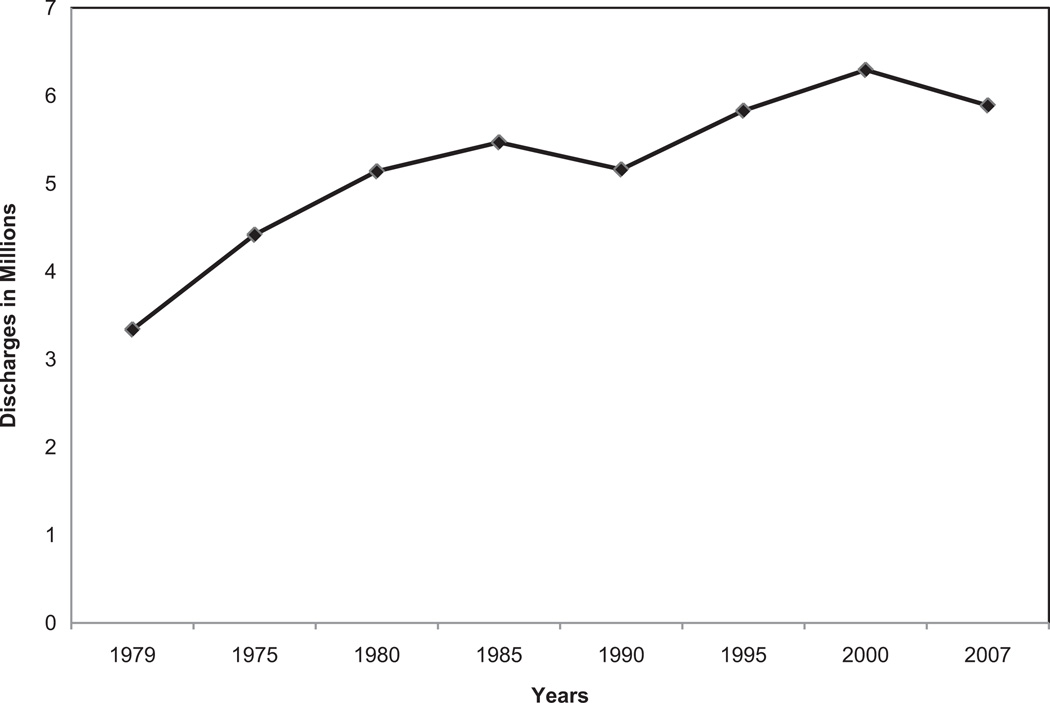
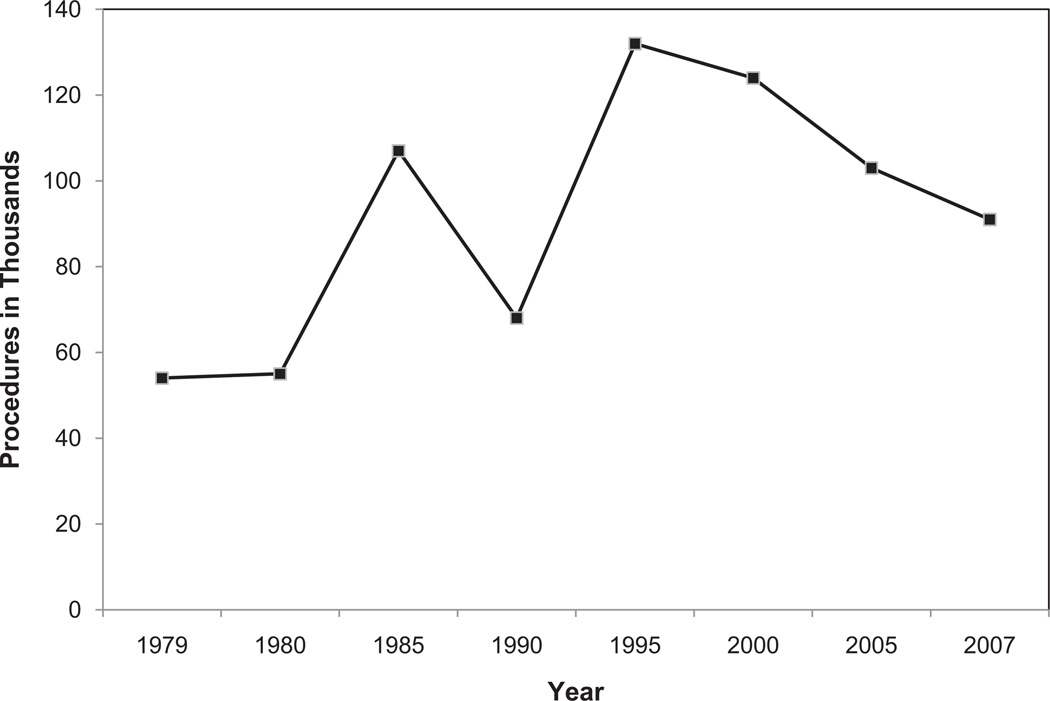
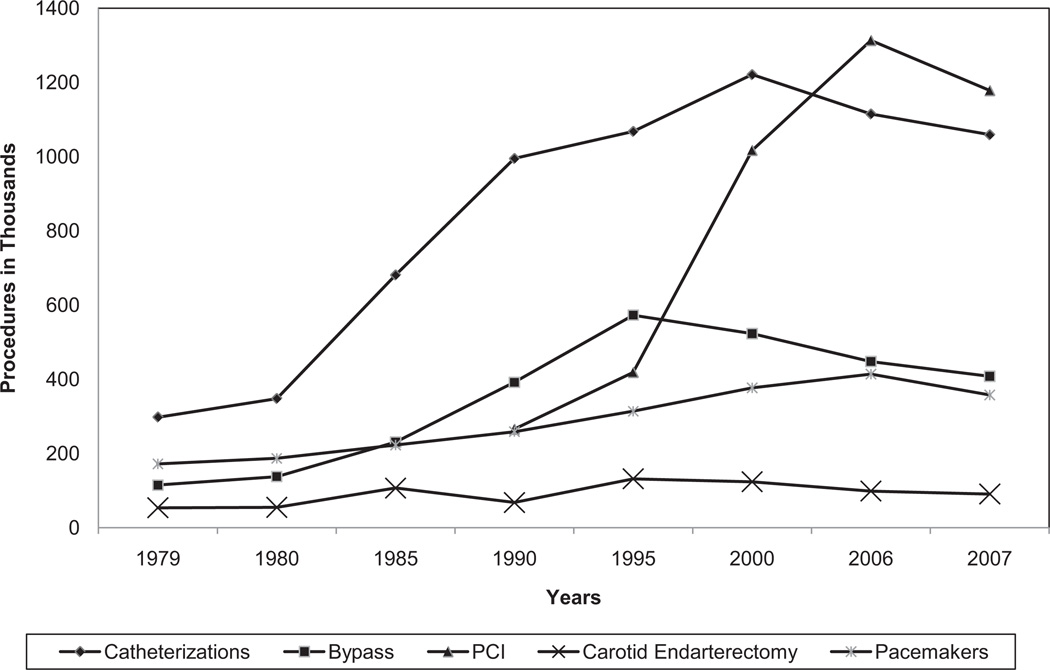
Chapter 21 provides data on trends and current usage of cardiovascular surgical and invasive procedures. For example, the total number of inpatient cardiovascular operations and procedures increased 27%, from 5 382 000 in 1997 to 6 846 000 in 2007 (National Heart, Lung, and Blood Institute computation based on National Center for Health Statistics annual data).
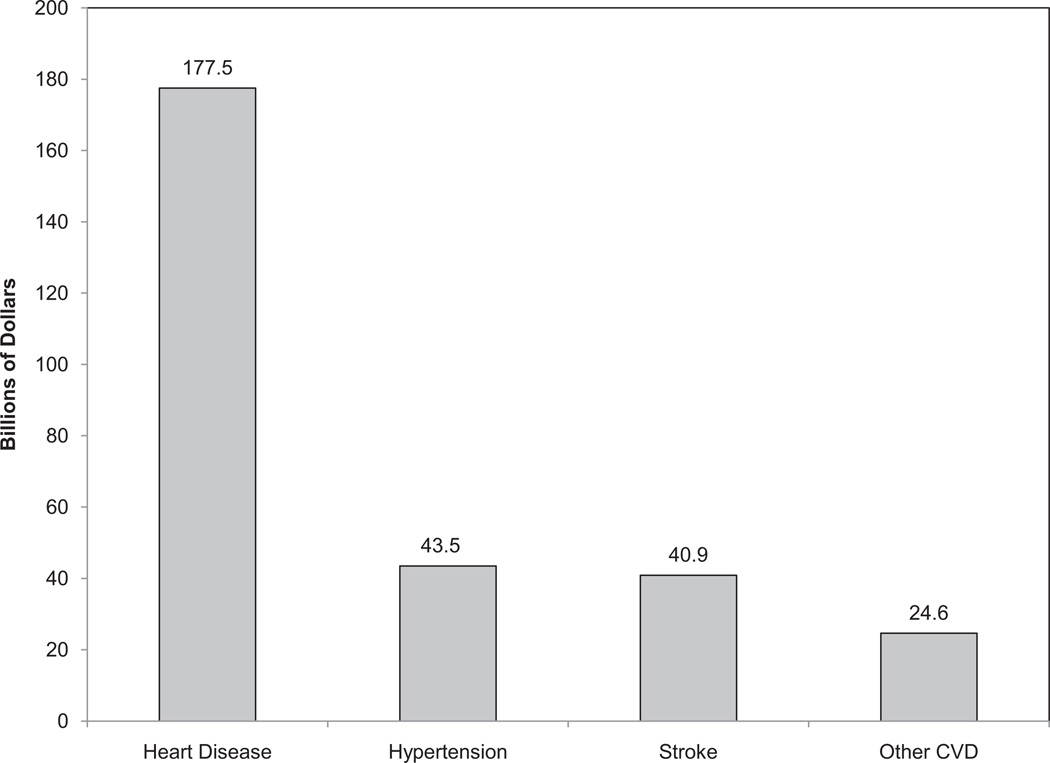
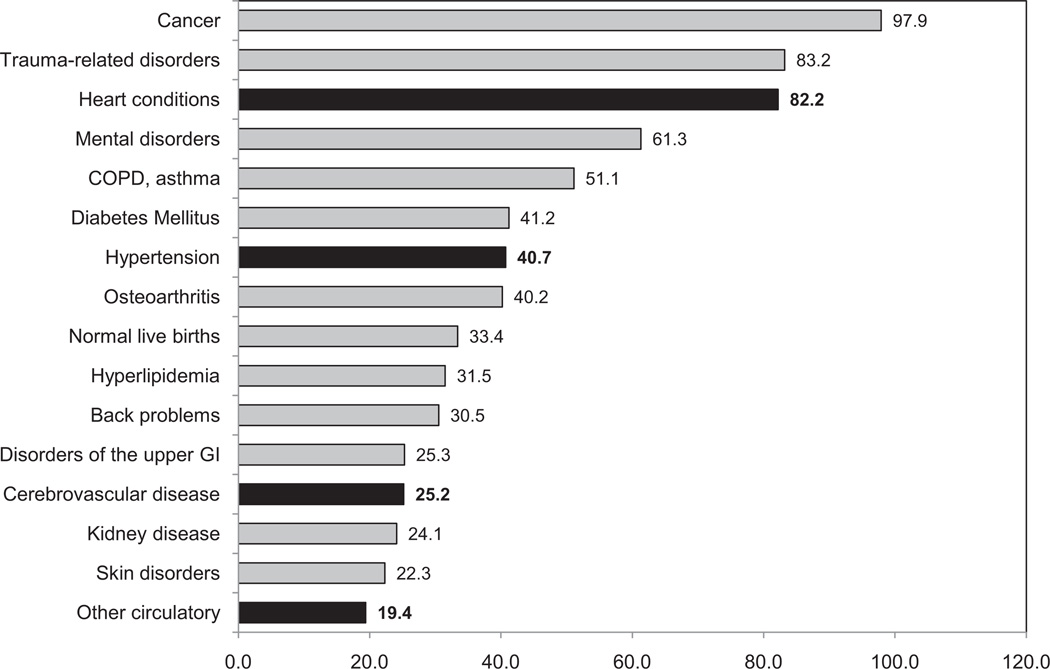
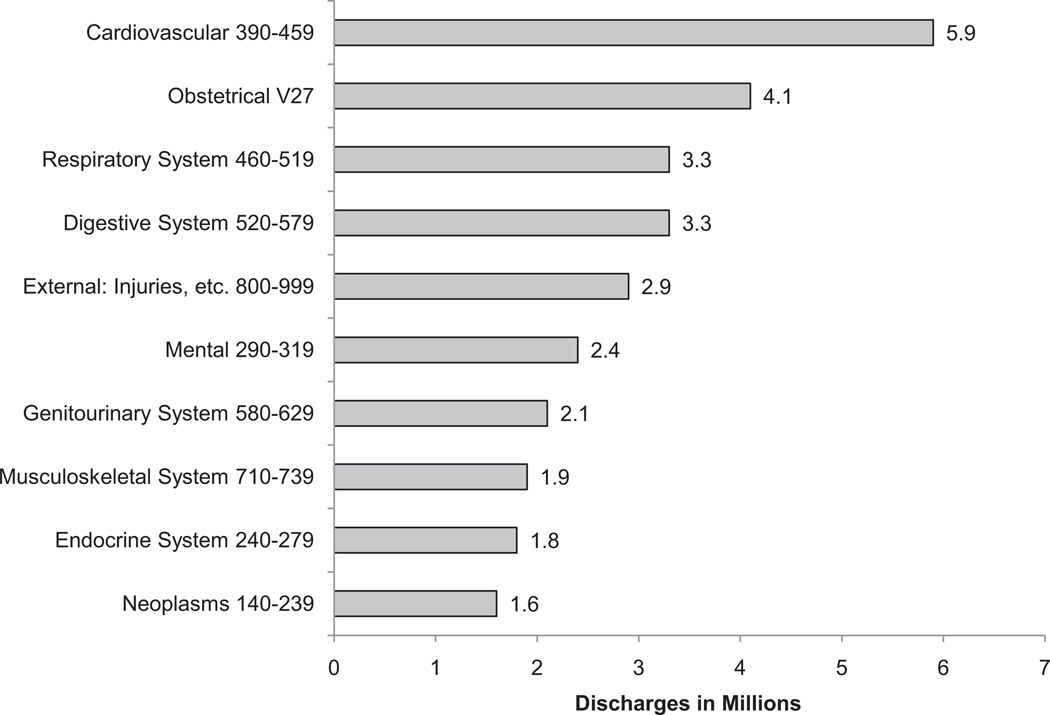
Chapter 22 reviews current estimates of direct and indirect healthcare costs related to CVDs, stroke, and related conditions using Medical Expenditure Panel Survey data. The total direct and indirect cost of CVD and stroke in the United States for 2007 is estimated to be $286 billion. This figure includes health expenditures (direct costs, which include the cost of physicians and other professionals, hospital services, prescribed medications, home health care, and other medical durables) and lost productivity resulting from mortality (indirect costs). By comparison, in 2008, the estimated cost of all cancer and benign neoplasms was $228 billion ($93 billion in direct costs, $19 billion in morbidity indirect costs, and $116 billion in mortality indirect costs). CVD costs more than any other diagnostic group.
The AHA, through its Statistics Committee, continuously monitors and evaluates sources of data on heart disease and stroke in the United States to provide the most current data available in the Statistics Update. The 2007 mortality data have been released. More information can be found at the National Center for Health Statistics Web site, http://www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_01.pdf.
Finally, it must be noted that this annual Statistical Update is the product of an entire year’s worth of effort by dedicated professionals, volunteer physicians and scientists, and outstanding AHA staff members, without whom publication of this valuable resource would be impossible. Their contributions are gratefully acknowledged.
-
Véronique L. Roger, MD, MPH, FAHA
Melanie B. Turner, MPH
On behalf of the American Heart Association Heart Disease and Stroke Statistics Writing Group
Note: Population data used in the compilation of NHANES prevalence estimates is for the latest year of the NHANES survey being used. Extrapolations for NHANES prevalence estimates are based on the census resident population for 2008 because this is the most recent year of NHANES data used in the Statistical Update.
Keywords: AHA Statistical Update, cardiovascular diseases, epidemiology, risk factors, statistics, stroke
1. About These Statistics
The American Heart Association (AHA) works with the Centers for Disease Control and Prevention’s (CDC’s) National Center for Health Statistics (NCHS); the National Heart, Lung, and Blood Institute (NHLBI); the National Institute of Neurological Disorders and Stroke (NINDS); and other government agencies to derive the annual statistics in this Update. This chapter describes the most important sources and the types of data we use from them. For more details, see Chapter 24 of this document, the Glossary.
The surveys used are:
Behavioral Risk Factor Surveillance System (BRFSS)— ongoing telephone health survey system
Greater Cincinnati/Northern Kentucky Stroke Study (GC-NKSS)— stroke incidence rates and outcomes within a biracial population
Medical Expenditure Panel Survey (MEPS)—data on specific health services that Americans use, how frequently they use them, the cost of these services, and how the costs are paid
National Health and Nutrition Examination Survey (NHANES)—disease and risk factor prevalence and nutrition statistics
National Health Interview Survey (NHIS)—disease and risk factor prevalence
National Hospital Discharge Survey (NHDS)—hospital inpatient discharges and procedures (discharged alive, dead, or status unknown)
National Ambulatory Medical Care Survey (NAMCS)—physician office visits
National Hospital Ambulatory Medical Care Survey (NHAMCS)—hospital outpatient and emergency department visits
National Inpatient Sample (NIS) of the Agency for Healthcare Research and Quality (AHRQ)—hospital inpatient discharges, procedures, and charges
National Nursing Home Survey (NNHS)—nursing home residents
National Vital Statistics System—national and state mortality data
World Health Organization (WHO)—mortality rates by country
Youth Risk Behavior Surveillance System (YRBSS) (CDC)—health-risk behaviors in youth and young adults
Disease Prevalence
Prevalence is an estimate of how many people have a disease at a given point or period in time. The NCHS conducts health examination and health interview surveys that provide estimates of the prevalence of diseases and risk factors. In this Update, the health interview part of the NHANES is used for the prevalence of cardiovascular diseases (CVDs). NHANES is used more than the NHIS because in NHANES, angina pectoris (AP) is based on the Rose Questionnaire; estimates are made regularly for heart failure (HF); hypertension is based on blood pressure (BP) measurements and interviews; and an estimate can be made for total CVD, including myocardial infarction (MI), AP, HF, stroke, and hypertension.
A major emphasis of this Update is to present the latest estimates of the number of people in the United States who have specific conditions to provide a realistic estimate of burden. Most estimates based on NHANES prevalence rates are based on data collected from 2005 to 2008 (in most cases, these are the latest published figure). These are applied to census population estimates for 2008. Differences in population estimates based on extrapolations of rates beyond the data collection period by use of more recent census population estimates cannot be used to evaluate possible trends in prevalence. Trends can only be evaluated by comparing prevalence rates estimated from surveys conducted in different years.
Risk Factor Prevalence
The NHANES 2005–2008 data are used in this Update to present estimates of the percentage of people with high lipid values, diabetes mellitus, overweight, and obesity. The NHIS is used for the prevalence of cigarette smoking and physical inactivity. Data for students in grades 9 through 12 are obtained from the YRBSS.
Incidence and Recurrent Attacks
An incidence rate refers to the number of new cases of a disease that develop in a population per unit of time. The unit of time for incidence is not necessarily 1 year, although we often discuss incidence in terms of 1 year. For some statistics, new and recurrent attacks or cases are combined. Our national incidence estimates for the various types of CVD are extrapolations to the US population from the Framingham Heart Study (FHS), the Atherosclerosis Risk in Communities (ARIC) study, and the Cardiovascular Health Study (CHS), all conducted by the NHLBI, as well as the GCNKSS, which is funded by the NINDS. The rates change only when new data are available; they are not computed annually. Do not compare the incidence or the rates with those in past editions of the Heart Disease and Stroke Statistics Update (also known as the Heart and Stroke Statistical Update for editions before 2005). Doing so can lead to serious misinterpretation of time trends.
Mortality
Mortality data are presented according to the underlying cause of death. “Any-mention” mortality means that the condition was nominally selected as the underlying cause or was otherwise mentioned on the death certificate. For many deaths classified as attributable to CVD, selection of the single most likely underlying cause can be difficult when several major comorbidities are present, as is often the case in the elderly population. It is useful, therefore, to know the extent of mortality due to a given cause regardless of whether it is the underlying cause or a contributing cause (ie, its “any-mention” status). The number of deaths in 2007 with any mention of specific causes of death was tabulated by the NHLBI from the NCHS public-use electronic files on mortality.
The first set of statistics for each disease in this Update includes the number of deaths for which the disease is the underlying cause. Two exceptions are Chapter 7 (High Blood Pressure) and Chapter 9 (Heart Failure). High BP, or hypertension, increases the mortality risks of CVD and other diseases, and HF should be selected as an underlying cause only when the true underlying cause is not known. In this Update, hypertension and HF death rates are presented in 2 ways: (1) as nominally classified as the underlying cause and (2) as any-mention mortality.
National and state mortality data presented according to the underlying cause of death were computed from the mortality tables of the NCHS World Wide Web site, the Health Data Interactive data system of the NCHS, or the CDC compressed mortality file. Any-mention numbers of deaths were tabulated from the electronic mortality files of the NCHS World Wide Web site and from Health Data Interactive.
Population Estimates
In this publication, we have used national population estimates from the US Census Bureau for 2008 in the computation of morbidity data. NCHS population estimates for 2007 were used in the computation of death rate data. The Census Bureau World Wide Web site1 contains these data, as well as information on the file layout.
Hospital Discharges and Ambulatory Care Visits
Estimates of the numbers of hospital discharges and numbers of procedures performed are for inpatients discharged from short-stay hospitals. Discharges include those discharged alive, dead, or with unknown status. Unless otherwise specified, discharges are listed according to the first-listed (primary) diagnosis, and procedures are listed according to all listed procedures (primary plus secondary). These estimates are from the NHDS of the NCHS unless otherwise noted. Ambulatory care visit data include patient visits to physician offices and hospital outpatient departments (OPDs) and emergency departments (EDs). Ambulatory care visit data reflect the first-listed (primary) diagnosis. These estimates are from NAMCS and NHAMCS of the NCHS.
International Classification of Diseases
Morbidity (illness) and mortality (death) data in the United States have a standard classification system: the International Classification of Diseases (ICD). Approximately every 10 to 20 years, the ICD codes are revised to reflect changes over time in medical technology, diagnosis, or terminology. Where necessary for comparability of mortality trends across the 9th and 10th ICD revisions, comparability ratios computed by the NCHS are applied as noted.2 Effective with mortality data for 1999, we are using the 10th revision (ICD-10). It will be a few more years before the 10th revision is used for hospital discharge data and ambulatory care visit data, which are based on the International Classification of Diseases, Clinical Modification, 9th Revision (ICD-9-CM).3
Age Adjustment
Prevalence and mortality estimates for the United States or individual states comparing demographic groups or estimates over time either are age specific or are age adjusted to the 2000 standard population by the direct method.4 International mortality data are age adjusted to the European standard.5 Unless otherwise stated, all death rates in this publication are age adjusted and are deaths per 100 000 population.
Data Years for National Estimates
In this Update, we estimate the annual number of new (incidence) and recurrent cases of a disease in the United States by extrapolating to the US population in 2008 from rates reported in a community- or hospital-based study or multiple studies. Age-adjusted incidence rates by sex and race are also given in this report as observed in the study or studies. For US mortality, most numbers and rates are for 2007. For disease and risk factor prevalence, most rates in this report are calculated from the 2005–2008 NHANES. Rates by age and sex are also applied to the US population in 2008 to estimate the numbers of people with the disease or risk factor in that year. Because NHANES is conducted only in the noninstitutionalized population, we extrapolated the rates to the total US population in 2008, recognizing that this probably underestimates the total prevalence, given the relatively high prevalence in the institutionalized population. The numbers and rates of hospital inpatient discharges for the United States are for 2007. Numbers of visits to physician offices, hospital EDs, and hospital OPDs are for 2007. Except as noted, economic cost estimates are for 2007.
Cardiovascular Disease
For data on hospitalizations, physician office visits, and mortality, CVD is defined according to ICD codes given in Chapter 24 of the present document. This definition includes all diseases of the circulatory system, as well as congenital CVD. Unless so specified, an estimate for total CVD does not include congenital CVD. Prevalence of CVD includes people with hypertension, heart disease, stroke, peripheral artery disease, and diseases of the veins.
Race
Data published by governmental agencies for some racial groups are considered unreliable because of the small sample size in the studies. Because we try to provide data for as many racial groups as possible, we show these data for informational and comparative purposes.
Contacts
If you have questions about statistics or any points made in this Update, please contact the AHA National Center, Office of Science & Medicine at statistics@heart.org or 214-706-1423. Direct all media inquiries to News Media Relations at inquiries@heart.org or 214-706-1173.
We do our utmost to ensure that this Update is error free. If we discover errors after publication, we will provide corrections at our World Wide Web site, http://www.americanheart.org/statistics, and in the journal Circulation.
Abbreviations Used in Chapter 1
- AHA
American Heart Association
- AHRQ
Agency for Healthcare Research and Quality
- AP
angina pectoris
- ARIC
Atherosclerosis Risk in Communities Study
- BP
blood pressure
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CHS
Cardiovascular Health Study
- CVD
cardiovascular disease
- ED
emergency department
- FHS
Framingham Heart Study
- GCNKSS
Greater Cincinnati/Northern Kentucky Stroke Study
- HF
heart failure
- ICD
International Classification of Diseases
- ICD-9-CM
International Classification of Diseases, Clinical Modification, 9th Revision
- MEPS
Medical Expenditure Panel Survey
- MI
myocardial infarction
- NAMCS
National Ambulatory Medical Care Survey
- NCHS
National Center for Health Statistics
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- NHANES
National Health and Nutrition Examination Survey
- NHDS
National Hospital Discharge Survey
- NHIS
National Health Interview Survey
- NHLBI
National Heart, Lung and Blood Institute
- NINDS
National Institute of Neurological Disorders and Stroke
- NIS
National Inpatient Sample
- NNHS
National Nursing Home Survey
- OPD
outpatient department
- WHO
World Health Organization
- YRBSS
Youth Risk Behavior Surveillance System
References
- 1.US Census Bureau population estimates. [Accessed September 27, 2010]; Available at: http://www.census.gov/popest/national/asrh/files/NC-EST2008-ALLDATA-R-File14.csv.
- 2.Health, United States, 2009, With Special Feature on Medical Technology. Hyattsville, Md: National Center for Health Statistics; 2010. [Accessed July 30, 2010]. National Center for Health Statistics. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. [PubMed] [Google Scholar]
- 3.International Classification of Diseases, Ninth Revision: Clinical Modification (ICD-9-CM) Hyattsville, Md: National Center for Health Statistics; 1978. National Center for Health Statistics, Centers for Medicare and Medicaid Services. [Google Scholar]
- 4.Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998;47:1–16. 20. [PubMed] [Google Scholar]
- 5.World Health Statistics Annual. Geneva, Switzerland: World Health Organization; 1998. World Health Organization. [Google Scholar]
2. American Heart Association’s 2020 Impact Goals
See Tables 2-1 through 2-3 and Charts 2-1 through 2-7.
Table 2-1.
Definitions of Poor, Intermediate, and Ideal Cardiovascular Health for Each Metric in the AHA 2020 Goals
| Level of Cardiovascular Health for Each Metric | |||
|---|---|---|---|
| Poor | Intermediate | Ideal | |
| Current smoking | |||
| Adults aged >20 y | Yes | Former ≤12 mo | Never or quit >12 mo |
| Children aged 12–19 y | Tried prior 30 d | … | Never tried; never smoked whole cigarette |
| BMI | |||
| Adults aged >20 y | ≥30 kg/m2 | 25–29.9 kg/m2 | <25 kg/m2 |
| Children aged 2–19 y | >95th percentile | 85th–95th percentile | <85th percentile |
| Physical activity | |||
| Adults aged >20 y | None | 1–149 min/wk moderate or 1–74 min/wk vigorous or 1–149 min/wk moderate+vigorous |
150+ min/wk moderate or 75+ min/wk vigorous or 150+ min/wk moderate+vigorous |
| Children aged 12–19 y | None | >0 and <60 min of moderate or vigorous every day |
60+ min of moderate or vigorous every day |
| Healthy diet score | |||
| Adults aged >20 y | 0–1 components | 2–3 components | 4–5 components |
| Children aged 5–19 y | 0–1 components | 2–3 components | 4–5 components |
| Total cholesterol | |||
| Adults aged >20 y | ≥240 mg/dL | 200–239 mg/dL or treated to goal | <200 mg/dL |
| Children aged 6–19 y | ≥200 mg/dL | 170–199 mg/dL | <170 mg/dL |
| Blood pressure | |||
| Adults aged >20 y | SBP ≥140 or DBP ≥90 mm Hg | SBP 120–139 or DBP 80–89 mm Hg or treated to goal |
<120/<80 mm Hg |
| Children aged 8–19 y | >95th percentile | 90th–95th percentile or SBP ≥120 or DBP ≥80 mm Hg |
<90th percentile |
| Fasting plasma glucose | |||
| Adults aged >20 y | ≥126 mg/dL | 100–125 mg/dL or treated to goal | <100 mg/dL |
| Children aged 12–19 y | ≥126 mg/dL | 100–125 mg/dL | <100 mg/dL |
… indicates no definition for this stratum;
AHA, American Heart Association; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Table 2-3.
Selected Secondary Metrics for Monitoring Cardiovascular Disease, NHANES 1999–2006
| N | Prevalence (%) | Standard Error | |
|---|---|---|---|
| Prevalence of CVD (Self-reported) | 16 786 | ||
| Coronary heart disease | 3.62 | 0.16 | |
| Stroke | 2.71 | 0.15 | |
| Congestive heart failure | 2.42 | 0.12 | |
| Acute MI heart attack | 3.61 | 0.20 | |
| Any self-reported history of CVD | 8.13 | 0.28 | |
| Risk factor control in the presence of CVD | 1728 | ||
| Current smoker or smokers who quit <12 mo ago | 1723 | 36.53 | 2.66 |
| Hypertension | |||
| Prevalence of BP >140/90 mm Hg or taking medications | 1596 | 40.56 | 2.35 |
| Awareness among hypertensives | 1129 | 84.97 | 4.39 |
| Treatment among hypertensives | 1129 | 79.63 | 4.37 |
| BP control among treated | 936 | 68.08 | 4.81 |
| Hypercholesterolemia | |||
| Prevalence of total cholesterol ≥240 mg/dL or taking medications | 1581 | 37.28 | 2.40 |
| Awareness among hypercholesterolemia | 806 | 68.53 | 4.32 |
| Treatment among hypercholesterolemia | 806 | 59.15 | 4.47 |
| Cholesterol control among treated | 639 | 80.09 | 6.57 |
| Overweight or Obese BMI ≥25.0 kg/m2 | 1625 | 78.10 | 2.91 |
| Obese BMI ≥30.0 kg/m2 | 45.35 | 3.63 | |
| Diabetes mellitus | |||
| Prevalence of fasting glucose ≥125 mg/dL or taking meds | 1028 | 17.59 | 22.81 |
| Awareness among diabetics | 502 | 56.35 | 5.39 |
| Treatment among diabetics | 502 | 36.52 | 5.48 |
| Blood glucose control among treated | 182 | 27.55 | 4.68 |
| Physical activity: intermediate or poor | 1728 | 68.59 | 2.88 |
| Moderate <150 min/wk AND | |||
| Vigorous <75 min/wk AND | |||
| Combined <150 min/wk | |||
| Physical activity: none | 44.99 | 3.44 | |
| Diet: intermediate or poor (2005–2006) | 430 | ||
| Total diet score 0–3 | 365 | 100.00 | 0.00 |
| Total diet score 0–1 | 80.80 | 4.69 |
NHANES indicates National Health and Nutrition Examination Survey; CVD, cardiovascular disease; MI, myocardial infarction; BP, blood pressure; BMI, body mass index.
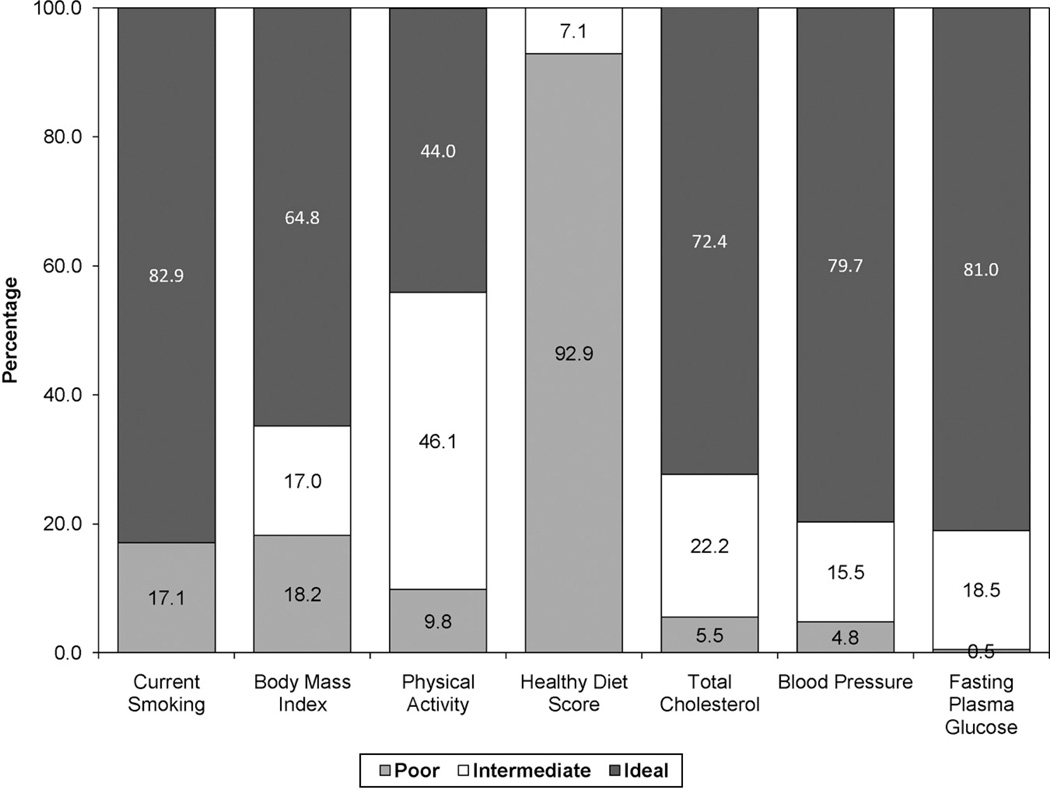
Chart 2-1.
Prevalence (unadjusted) estimates for poor, intermediate, and ideal cardiovascular health for each of the 7 metrics of cardiovascular health in the American Heart Association 2020 goals, US children aged 12 to 19 years, National Health and Nutrition Examination Survey (NHANES) 2005–2006 (baseline available data as of January 1, 2010).
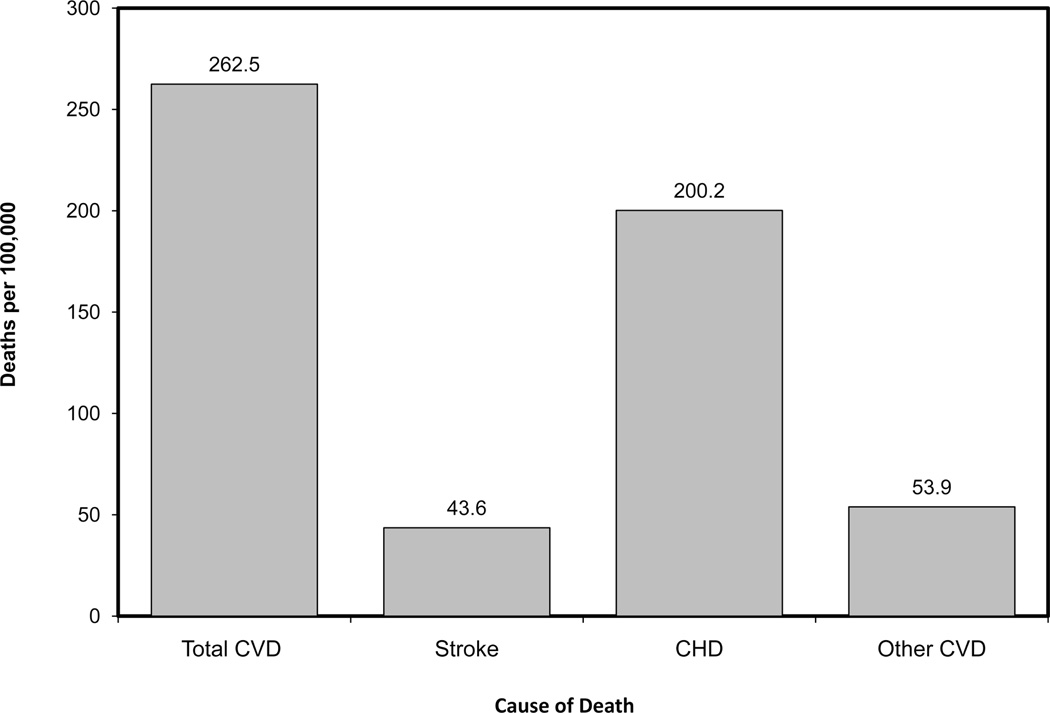
Chart 2-7.
Baseline US age-standardized death rates from cardiovascular diseases, 2006. Data derived from Heron et al.2
After achieving its major Impact Goals for 2010, the AHA recently created a new set of Impact Goals for the current decade.1 Specifically, the AHA committed to the following organizational goals:
By 2020, to improve the cardiovascular health of all Americans by 20%, while reducing deaths from cardiovascular disease and stroke by 20%.1
These goals include a novel concept, “cardiovascular health,” which encompasses 7 health behaviors and health factors (Table 2-1). “Ideal cardiovascular health” is defined by the absence of clinically manifest cardiovascular disease (CVD) and the simultaneous presence of optimal levels of all 7 health behaviors (lean body mass, avoidance of smoking, participation in physical activity, and healthy dietary intake consistent with a Dietary Approaches to Stop Hypertension [DASH]-like eating pattern) and health factors (untreated total cholesterol <200 mg/dL, untreated blood pressure <120/<80 mm Hg, and fasting blood glucose <100 mg/dL). Because the ideal cardiovascular health profile is known to be rare in the population, the entire spectrum of cardiovascular health can also be represented as being “ideal,” “intermediate,” or “poor” for each of the health behaviors and health factors, as shown in Table 2-1.1
Beginning in 2011, and recognizing the substantial time lag in the nationally representative data sets, the annual Statistical Update will begin to evaluate and publish metrics and information that gives AHA directional insights into progress and/or areas critical for greater concentration, to meet their 2020 goals. In this chapter, baseline data are presented that were derived from the existing national data available on January 20, 2010, the official announcement date of the 2020 Impact Goals.
Cardiovascular Health
Table 2-1 provides the specific definitions for ideal, intermediate, and poor cardiovascular health for each of the 7 health behaviors and health factors.
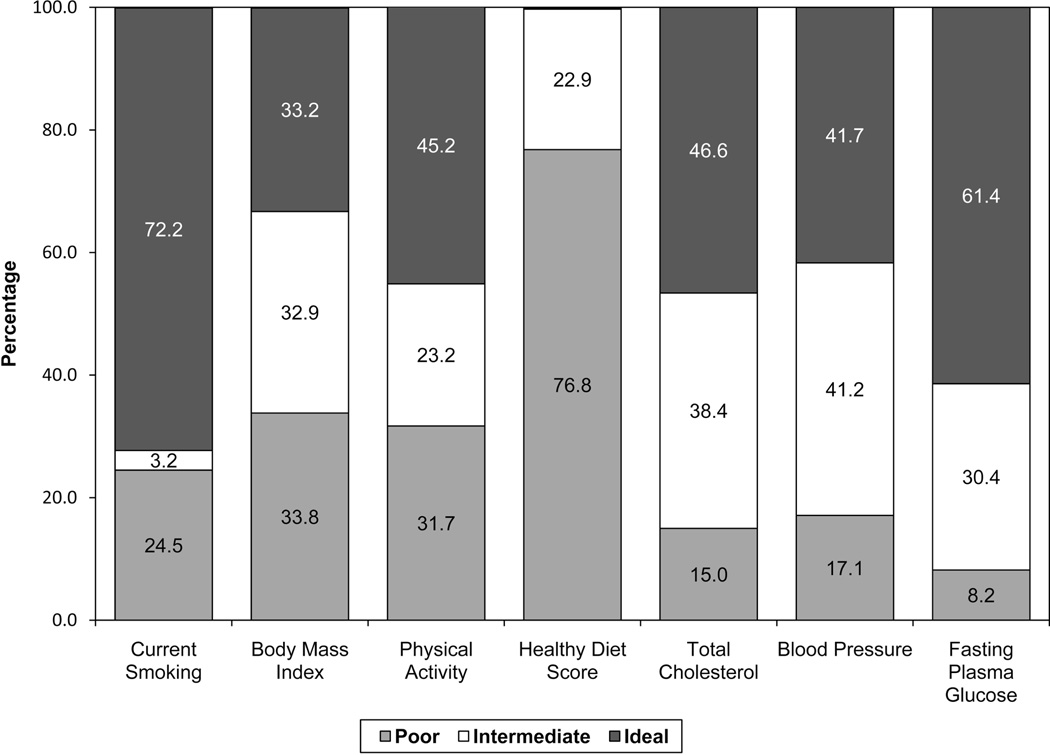
- The prevalences of ideal, intermediate, and poor levels of each of the 7 cardiovascular health metrics are shown in Chart 2-1 (for children) and Chart 2-2 (for adults).
-
—Among children (Chart 2-1), the prevalence (unadjusted) of ideal levels of cardiovascular health behaviors and factors currently varies from 0% for the healthy diet score (ie, essentially no children meet 4 or 5 of the 5 dietary components) to more than 80% for the smoking and fasting glucose metrics. More than 90% of US children meet 0 or only 1 of the 5 healthy dietary components.
-
—Among US adults (Chart 2-2), the age-standardized prevalence of ideal levels of cardiovascular health behaviors and factors currently varies from 0.2% for the healthy diet score up to 72% for the smoking metric (ie, 72% of US adults have never smoked or are current nonsmokers who have quit for more than 12 months).
-
—In general, the prevalence of ideal levels of health behaviors and health factors is higher in US children than in US adults.
-
—
Age-standardized and age-specific prevalence estimates for Ideal Cardiovascular Health and for ideal levels of each of its components are shown in Table 2-2.
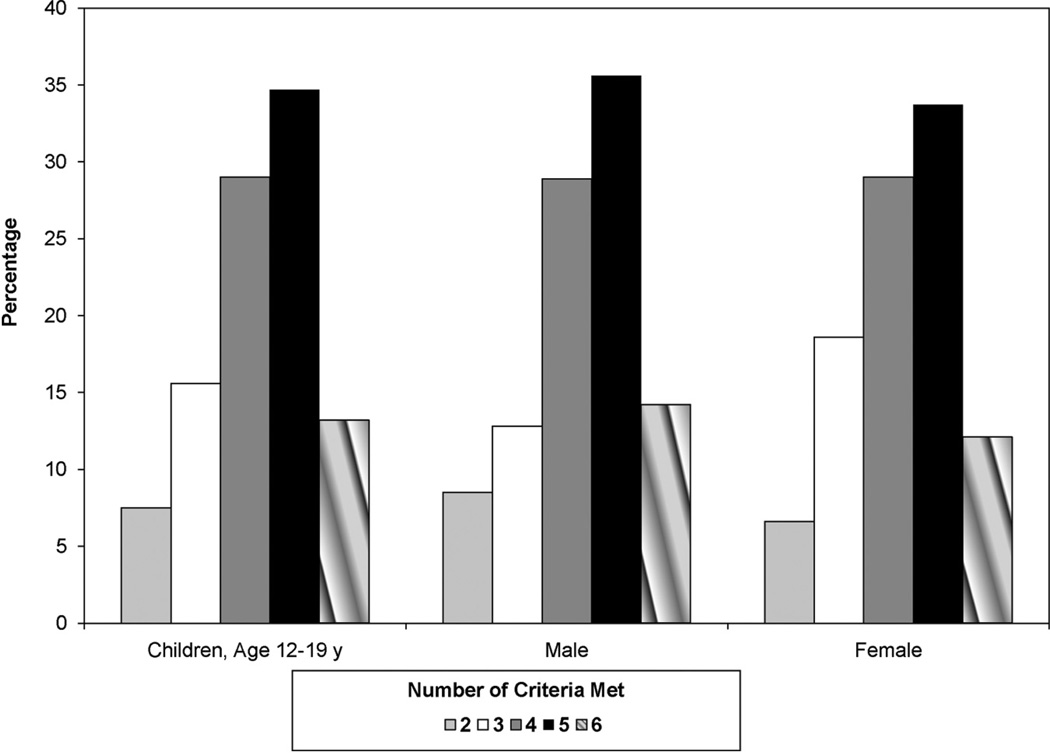
- Chart 2-3 displays the prevalence estimates for the population of US children meeting different numbers of criteria for Ideal Cardiovascular Health (out of 7 possible).
-
—Half of US children ages 12 to 19 years meet 4 or fewer criteria for Ideal Cardiovascular Health.
-
—The distributions are similar in boys and girls.
-
—
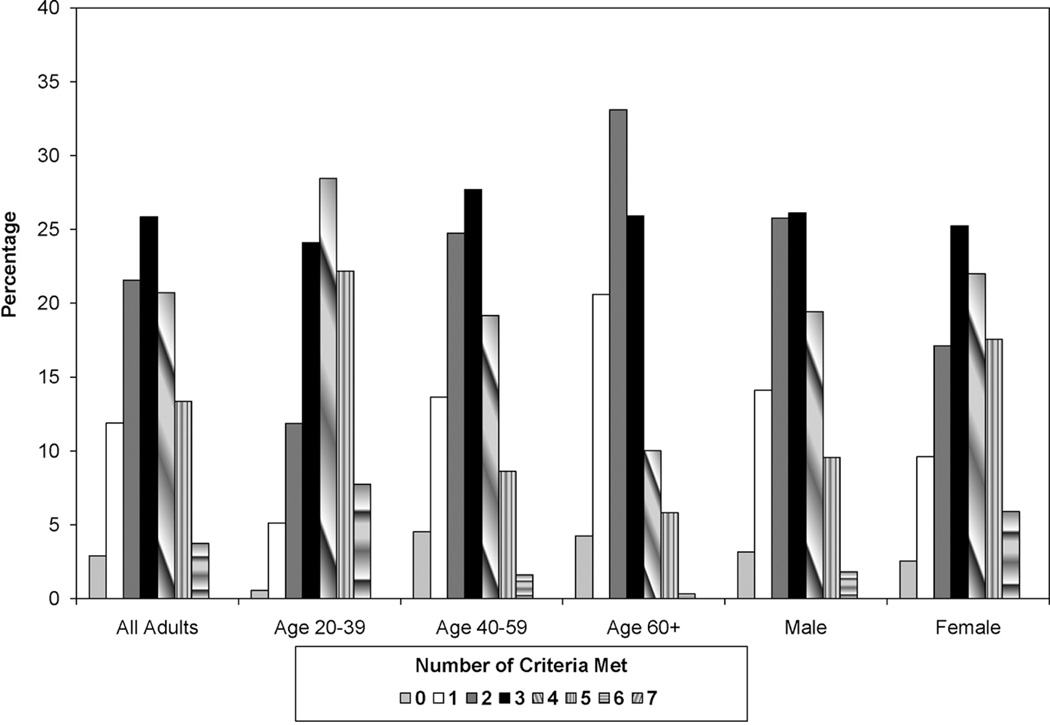
- Charts 2-4 and 2-5 display the age-standardized prevalence estimates for the population of US adults meeting different numbers of criteria for Ideal Cardiovascular Health (out of 7 possible), overall, and stratified by age groups, sex, and race.
-
—Approximately 3% of US adults have 0 of the 7 criteria at ideal levels, with ≈26% having 3 at ideal levels (Chart 2-4).
-
—Compared with younger adults, older adults tend to have fewer of the 7 metrics at ideal levels; more than half of those over age 60 years have only 2 or fewer at ideal levels (Chart 2-4).
-
—Women tend to have more metrics at ideal levels than do men (Chart 2-4).
-
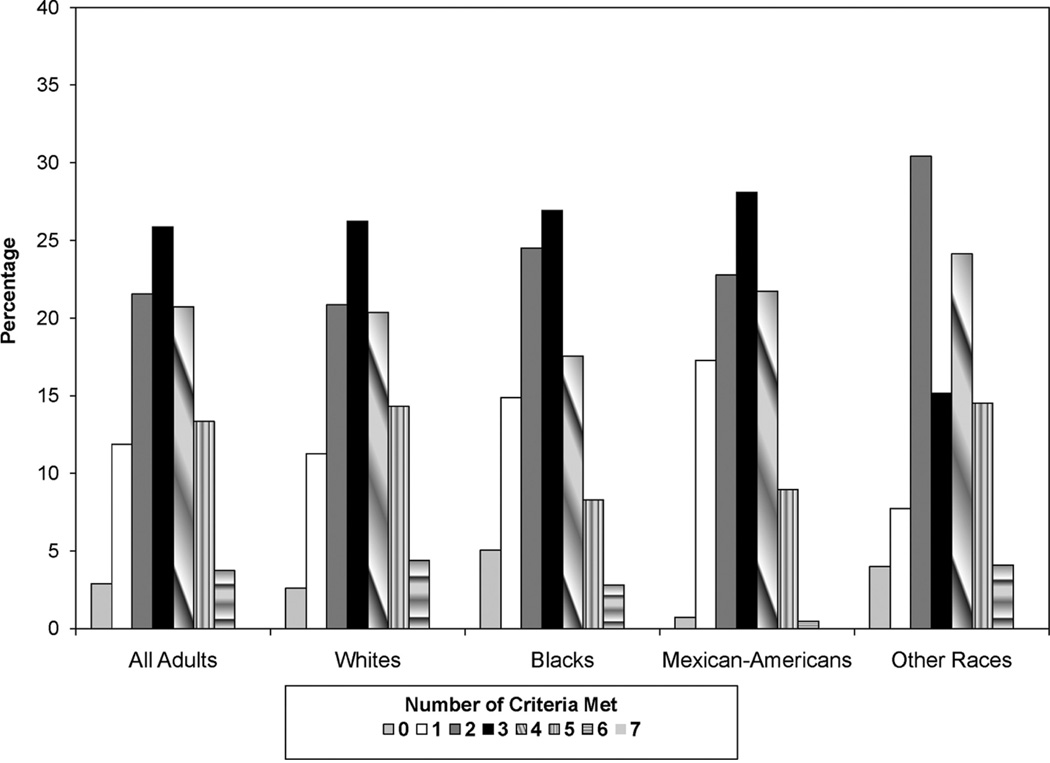
—Approximately 61% of white adults and 71% of black and Mexican American adults have 3 or fewer metrics (out of 7) at ideal levels (Chart 2-5).
-
—
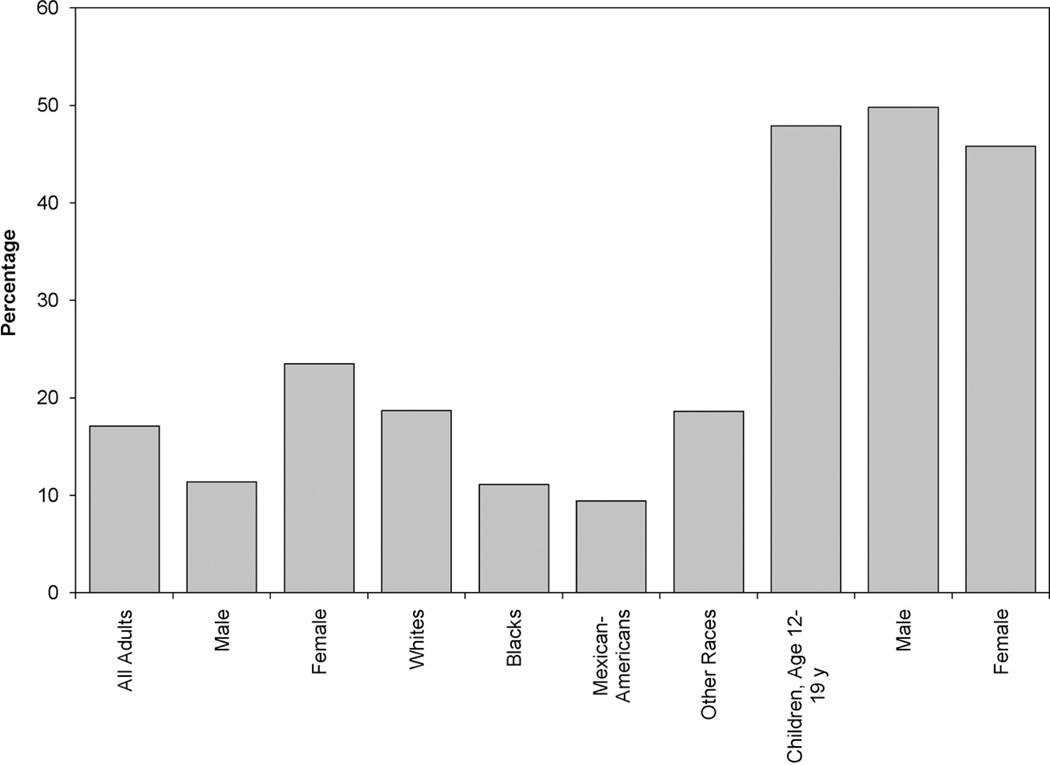
- Chart 2-6 displays the age-standardized percentages of US adults and percentages of children who have 5 or more of the metrics (out of 7 possible) at ideal levels.
-
—Almost 50% of US children aged 12 to 19 years have 5 or more metrics at ideal levels, including somewhat more boys than girls.
-
—However, only 17% of US adults have 5 or more metrics with ideal levels, including 11% of men and 24% of women.
-
—Whites have approximately twice the percentage of adults with 5 or more metrics with ideal levels, compared with Mexican Americans.
-
—
Chart 2-2.
Age-standardized prevalence estimates for poor, intermediate, and ideal cardiovascular health for each of the 7 metrics of cardiovascular health in the American Heart Association 2020 goals, among US adults aged >20 years, National Health and Nutrition Examination Survey (NHANES) 2005–2006 (baseline available data as of January 1, 2010).
Table 2-2.
Prevalence of US Population With Ideal Cardiovascular Health and With Components of Ideal Cardiovascular Health, Overall and in Selected Age Strata From NHANES 2005–2006 (Baseline Available Data as of January 1, 2010)
| Prevalence (%) | |||||
|---|---|---|---|---|---|
| Ages 12–19 y | Ages 20+ y | Ages 20–39 y | Ages 40–59 y | Ages 60+ y | |
| Ideal CV Health Profile (Composite–All 7) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Ideal Health Factors Index (Composite–All 4) | 40.8 | 13.0 | 24.8 | 7.0 | 2.1 |
| Individual components | |||||
| Total cholesterol <200 mg/dL (untreated) | 72.4 | 46.6 | 65.2 | 38.0 | 28.5 |
| SBP <120 and DBP <80 mm Hg (untreated) | 79.7 | 41.7 | 62.8 | 35.8 | 15.1 |
| Not current smoker (never or quit ≥12 mo) | 82.9 | 72.2 | 65.1 | 72.3 | 84.5 |
| Fasting blood glucose <100 mg/dL | 81.0 | 61.4 | 80.1 | 56.8 | 36.5 |
| Ideal Health Behaviors Index (Composite–All 4) | 0.00 | 0.1 | 0.0 | 0.1 | 0.3 |
| Individual components | |||||
| Physical activity at goal | 44.0 | 45.2 | 51.3 | 43.8 | 37.0 |
| Not current smoker (never or quit ≥12 mo) | 82.9 | 72.2 | 65.1 | 72.3 | 84.5 |
| BMI <25 kg/m2 | 64.8 | 33.2 | 39.9 | 28.6 | 29.3 |
| 4–5 diet goals met* | 0.0 | 0.2 | 0.0 | 0.5 | 0.3 |
| Fruits and vegetables ≥4.5 cups/d | 7.1 | 12.1 | 9.4 | 10.7 | 18.9 |
| Fish ≥2 3.5-oz servings/wk (preferably oily fish) | 11.3 | 21.8 | 16.5 | 25.5 | 25.0 |
| Sodium <1500 mg/d1 | 0.2 | 1.0 | 0.8 | 1.4 | 0.6 |
| Sugar-sweetened beverages ≤450 kcal/wk | 22.8 | 54.1 | 39.7 | 58.4 | 71.7 |
| Whole grains (1.1 g fiber in 10 g carb) ≥3 | 2.7 | 6.2 | 5.5 | 6.1 | 7.6 |
| 1-oz-equivalent servings per day | |||||
| Other dietary measures | |||||
| Nuts, legumes, seeds ≥4 servings/wk | 9.7 | 20.8 | 17.7 | 23.6 | 21.7 |
| Processed meats ≤2 servings/wk | 48.6 | 52.5 | 50.9 | 53.1 | 54.1 |
| Saturated fat <7% of total energy intake (kcal) | 4.4 | 9.1 | 9.6 | 8.6 | 9.3 |
NHANES indicates National Health and Nutrition Examination Survey; CV, cardiovascular; SBP, systolic blood pressure; DBP, diastolic blood pressure; BMI, body mass index.
Scaled for 2000 kcal/d, and in the context of intake with appropriate energy balance and a DASH-like eating plan.
Estimates for adults aged 20+ years are standardized to the US 2000 standard population.
Chart 2-3.
Proportion (unadjusted) of US children meeting different numbers of criteria for Ideal Cardiovascular Health, overall and by sex, National Health and Nutrition Examination Survey (NHANES) 2005–2006 (baseline available data as of January 1, 2010).
Chart 2-4.
Age-standardized prevalence estimates of US adults meeting different numbers of criteria for Ideal Cardiovascular Health, overall and by age and sex subgroups, National Health and Nutrition Examination Survey (NHANES) 2005–2006 (baseline available data as of January 1, 2010).
Chart 2-5.
Age-standardized prevalence estimates of US adults meeting different numbers of criteria for Ideal Cardiovascular Health, overall and in selected race subgroups from National Health and Nutrition Examination Survey (NHANES) 2005–2006 (baseline available data as of January 1, 2010).
Chart 2-6.
Prevalence estimates of meeting at least 5 criteria for Ideal Cardiovascular Health, US adults (age-standardized), overall and by sex and race, and US children (unadjusted), by sex, National Health and Nutrition Examination Survey (NHANES) 2005–2006 (baseline available data as of January 1, 2010).
Cardiovascular Disease
Data from NHANES 1999–2006 reveal that, overall, 8.1% of Americans self-reported having some type of CVD (Table 2-3).
- Among those with CVD, risk factor prevalence, awareness, treatment, and control were variable (Table 2-3).
-
—Nearly 37% were current smokers or had quit for less than 12 months.
-
—Awareness and treatment of hypertension were ≈80%, but only two-thirds of those who were treated were controlled to goal levels.
-
—Awareness and treatment of hypercholesterolemia were 60% and 68%, respectively, and 80% of treated individuals were at goal cholesterol levels.
-
—More than three fourths were overweight or obese, and 45% were obese.
-
—18% had diabetes mellitus.
-
—45% participated in no physical activity.
-
—100% of those with CVD met 3 or fewer of the 5 components of the healthy diet score.
-
—
Implications
- Taken together, these baseline data indicate the substantial progress that will need to occur for the AHA to achieve its 2020 Impact Goals over the next decade.
-
—To achieve improvements in cardiovascular health, all segments of the population will need to focus on improved cardiovascular health behaviors, in particular, with regard to diet and weight, as well as on an increase in physical activity and further reduction of the prevalence of smoking.
-
—More children, adolescents, and young adults will need to learn how to preserve their ideal levels of cardiovascular health factors and health behaviors into older ages.
-
—With regard to reducing the burden of CVD and stroke morbidity and mortality, renewed emphasis will be needed on treatment of acute events as well as secondary and primary prevention through treatment and control of risk factors.
-
—
Future issues of the Statistical Update will track progress toward these goals.
Abbreviations Used in Chapter 2
- AHA
American Heart Association
- BMI
body mass index
- BP
blood pressure
- CVD
cardiovascular disease
- DASH
Dietary Approaches to Stop Hypertension
- DBP
diastolic blood pressure
- mg/dL
milligrams per deciliter
- MI
myocardial infarction
- mm Hg
millimeter of mercury
- NHANES
National Health and Nutrition Examination Survey
- SBP
systolic blood pressure
References
- 1.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Grenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s Strategic Impact Goal Through 2020 and Beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 2.Heron MP, Hoyert DL, Murphy SL, Xu JQ, Kochanek KD, Tejada-Vera B. Deaths: Final Data for 2006. Hyattsville, Md: National Center for Health Statistics; 2009. National Vital Statistics Reports. Vol 57, No 14. [PubMed] [Google Scholar]
3. Cardiovascular Diseases
ICD-9 390–459, 745–747, ICD-10 I00 –I99, Q20–Q28; see Glossary (Chapter 24) for details and definitions. See Tables 3-1 through 3-4 and Charts 3-1 through 3-21.
Table 3-1.
Cardiovascular Disease
| Population Group | Prevalence, 2008 Age ≥20 y | Mortality, 2007 All Ages* | Hospital Discharges, 2007 All Ages | Cost, 2007 |
|---|---|---|---|---|
| Both sexes | 82 600 000 (36.2%) | 813 804 | 5 890 000 | $286.6 Billion |
| Males | 39 900 000 (37.4%) | 391 886 (48.2%)† | 3 016 000 | … |
| Females | 42 700 000 (35.0%) | 421 918 (51.8%)† | 2 874 000 | … |
| NH white males | 37.4% | 334 589 | … | … |
| NH white females | 33.8% | 362 762 | … | … |
| NH black males | 44.8% | 47 387 | … | … |
| NH black females | 47.3% | 50 015 | … | … |
| Mexican American males | 30.7% | … | … | … |
| Mexican American females | 30.9% | … | … | … |
Ellipses (…) indicate data not available; NH, non-Hispanic.
Mortality data are for whites and blacks and include Hispanics.
These percentages represent the portion of total cardiovascular disease mortality that is attributable to males versus females.
Sources: Prevalence: National Health and Nutrition Examination Survey 2005–2008, National Center for Health Statistics (NCHS) and National Heart, Lung, and Blood Institute (NHLBI). Percentages for racial/ethnic groups are age-adjusted for Americans ≥20 years of age. Age-specific percentages are extrapolated to the 2008 US population estimates. Mortality: NCHS. These data represent underlying cause of death only. Data include congenital cardiovascular disease mortality. Hospital discharges: National Hospital Discharge Survey, NCHS. Data include those inpatients discharged alive, dead, or of unknown status. Cost: NHLBI. Data include estimated direct and indirect costs for 2007.
Table 3-4.
Remaining Lifetime Risks for CVD and Other Diseases Among Men and Women Free of Disease at 40 and 70 Years of Age
| Remaining Lifetime Risk at Age 40 y |
Remaining Lifetime Risk at Age 70 y |
|||
|---|---|---|---|---|
| Diseases | Men | Women | Men | Women |
| Any CVD* | 2 in 3 | 1 in 2 | 1 in 2 | 1 in 2 |
| CHD5 | 1 in 2 | 1 in 3 | 1 in 3 | 1 in 4 |
| AF43 | 1 in 4 | 1 in 4 | 1 in 4 | 1 in 4 |
| CHF44 | 1 in 5 | 1 in 5 | 1 in 5 | 1 in 5 |
| Stroke45 | 1 in 6† | 1 in 5† | 1 in 6 | 1 in 5 |
| Dementia45 | … | … | 1 in 7 | 1 in 5 |
| Hip fracture57 | 1 in 20 | 1 in 6 | … | … |
| Breast cancer58,61 | 1 in 1000 | 1 in 8 | … | 1 in 14 |
| Prostate cancer58 | 1 in 6 | … | … | … |
| Lung cancer58 | 1 in 12 | 1 in 17 | … | … |
| Colon cancer58 | 1 in 16 | 1 in 17 | … | … |
| Diabetes62 | 1 in 3 | 1 in 3 | 1 in 9 | 1 in 7 |
| Hypertension63 | 9 in 10† | 9 in 10† | 9 in 10‡ | 9 in 10‡ |
| Obesity64 | 1 in 3 | 1 in 3 | … | … |
Ellipses (…) indicate not estimated.
CVD indicates cardiovascular disease; CHD, coronary heart disease; AF, atrial fibrillation; CHF, congestive heart failure.
Personal communication from Donald Lloyd-Jones, based on Framingham Heart Study data.
Age 55 years.
Age 65 years.
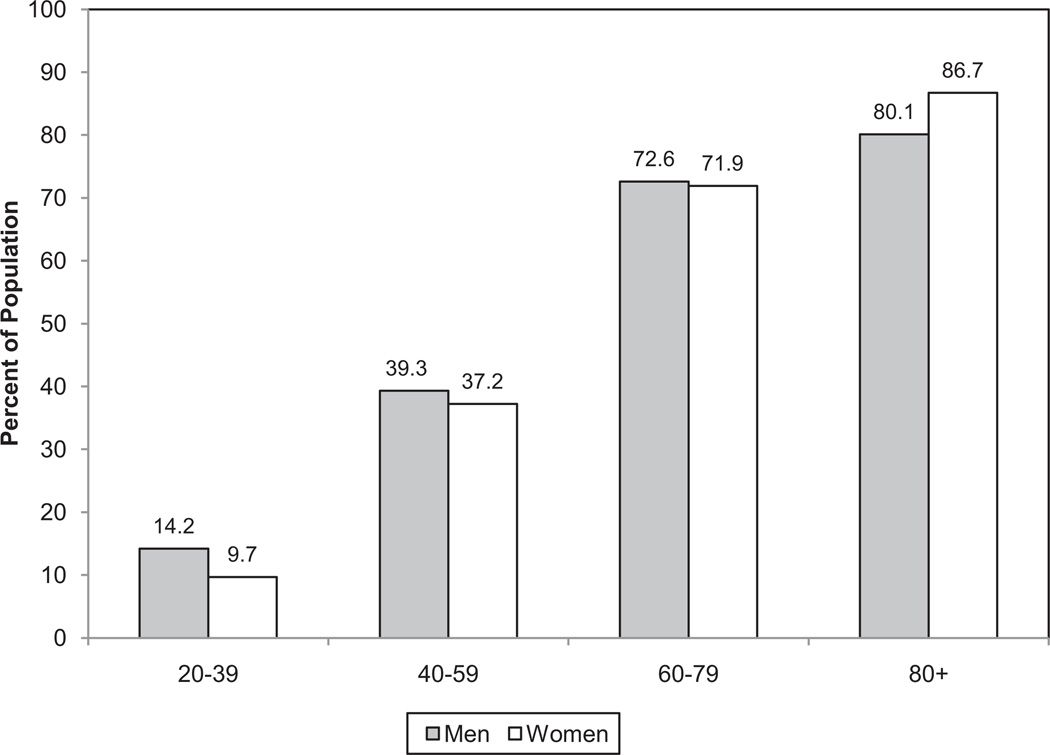
Chart 3-1.
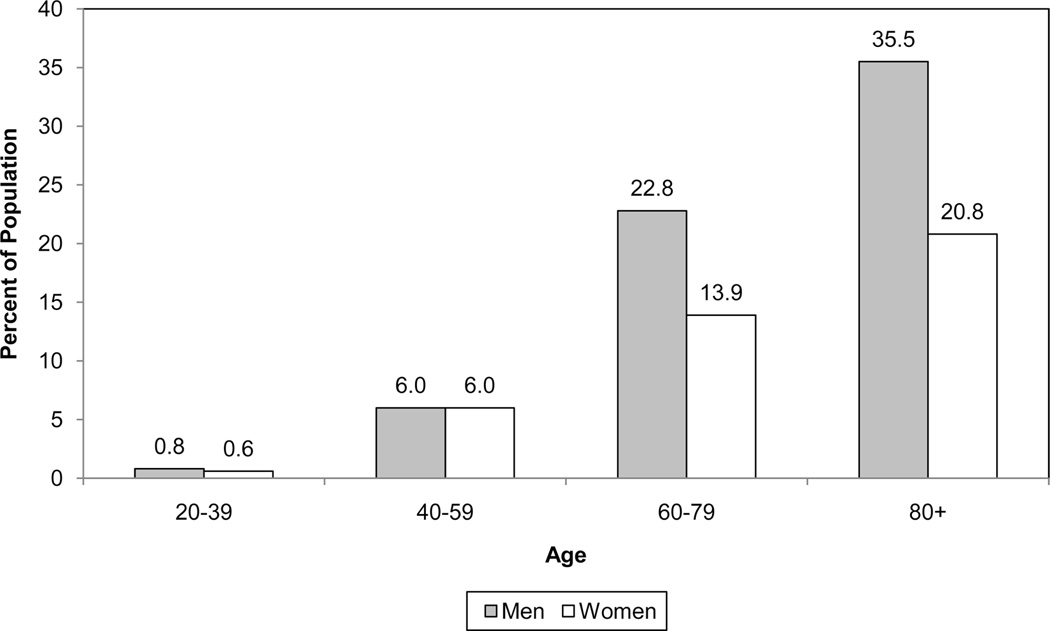
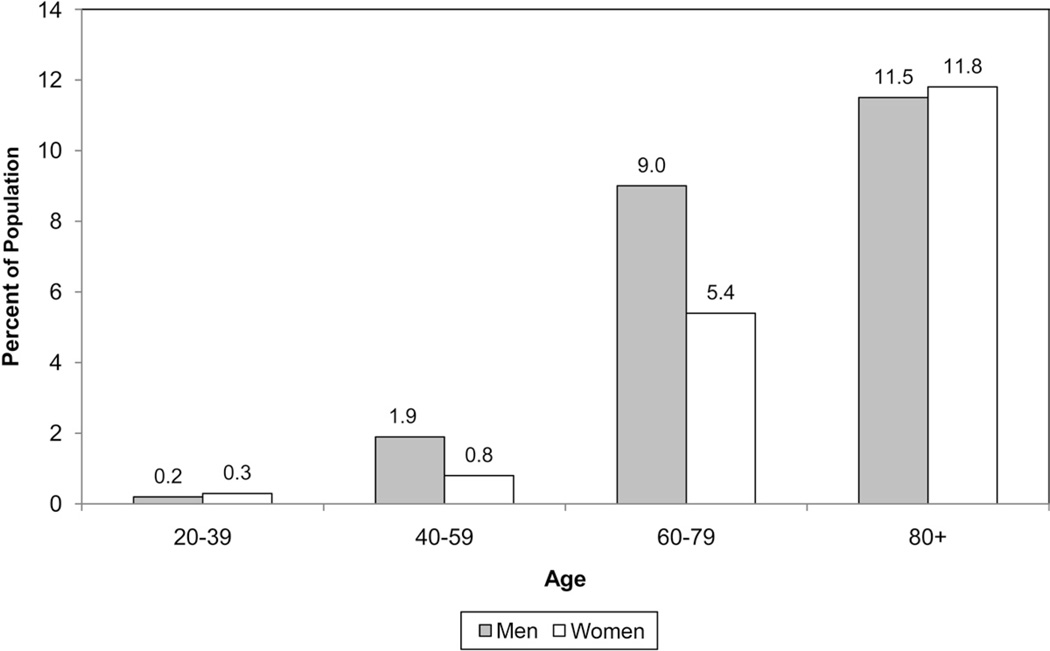
Prevalence of cardiovascular disease in adults ≥20 years of age by age and sex (National Health and Nutrition Examination Survey: 2005–2008). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute. These data include coronary heart disease, heart failure, stroke, and hypertension.
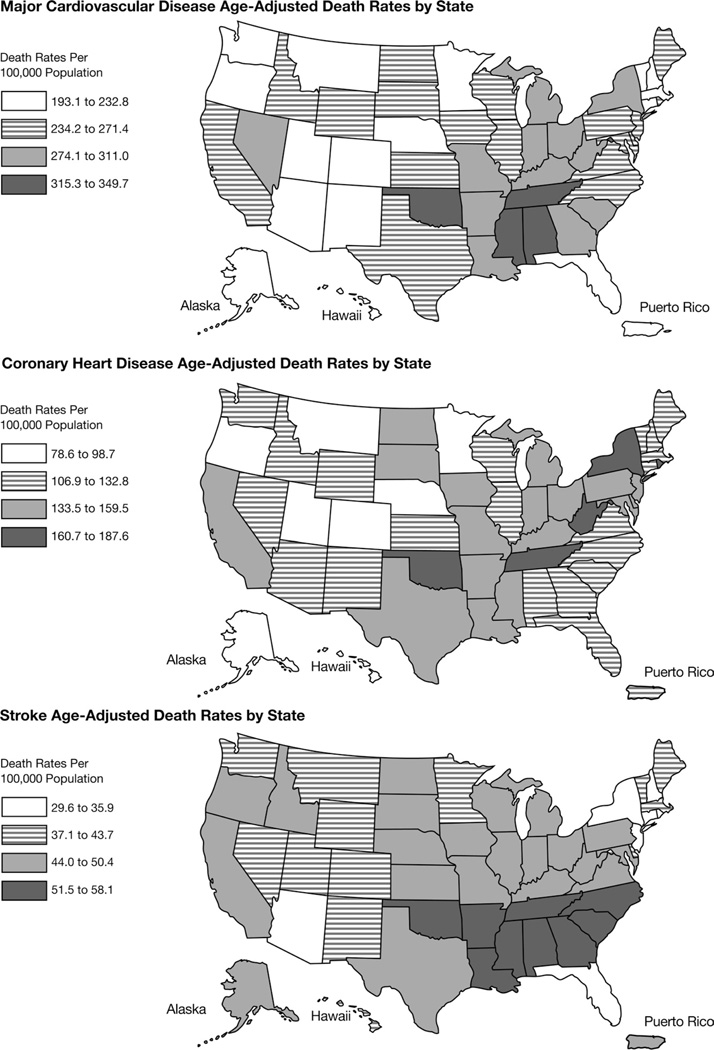
Chart 3-21.
US maps corresponding to state death rate statistics (including the District of Columbia).
Prevalence
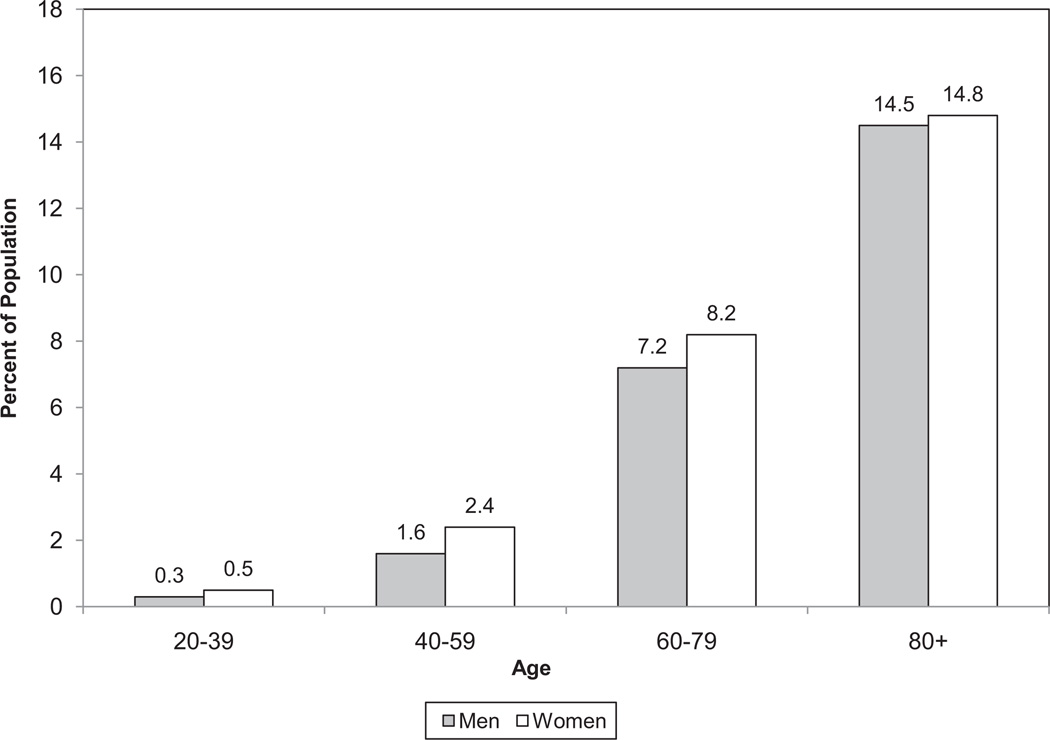
An estimated 82 600 000 American adults (>1 in 3) have 1 or more types of CVD. Of these, 40 400 000 are estimated to be ≥60 years of age. Total CVD includes diseases listed in the bullet points below, with the exception of congenital CVD. Because of overlap, it is not possible to add these conditions to arrive at a total.
High blood pressure (HBP)—76 400 000 (defined as systolic pressure ≥140 mm Hg and/or diastolic pressure ≥90 mm Hg, use of antihypertensive medication, or being told at least twice by a physician or other health professional that one has HBP).
- Coronary heart disease (CHD)—16 300 000
-
—MI (heart attack)— 7 900 000
-
—AP (chest pain)— 9 000 000
-
—
HF—5 700 000
Stroke— 7 000 000
Congenital cardiovascular defects— 650 000 to 1 300000
The following age-adjusted prevalence estimates from the NHIS, NCHS are for diagnosed conditions for people ≥18 years of age in 20091:
Among whites only, 11.9% have heart disease (HD), 6.4% have CHD, 23.0% have hypertension, and 2.5% have had a stroke.
Among blacks or African Americans, 11.2% have HD, 6.7% have CHD, 32.2% have hypertension, and 3.8% have had a stroke.
Among Hispanics or Latinos, 8.5% have HD, 5.8% have CHD, 21.5% have hypertension, and 2.0% have had a stroke.
Among Asians, 6.3% have HD, 3.9% have CHD, 19.4% have hypertension, and 1.3% have had a stroke.
Among American Indians or Alaska Natives, 8.0% have HD, 4.1% (figure considered unreliable) have CHD, and 21.8% have hypertension. An estimate for stroke is not reported because of its large relative standard error.
Among Native Hawaiians or other Pacific Islanders, HD, CHD, and stroke numbers are not reported because of large relative standard errors; 22.0% have hypertension, but the figure is considered unreliable.
Asian Indian adults (9%) are ≈2-fold more likely than Korean adults (4%) to have ever been told they have HD, based on data for 2004 to 2006.2
Incidence
- On the basis of the NHLBI’s FHS original and offspring cohort data from 1980 to 20033:
-
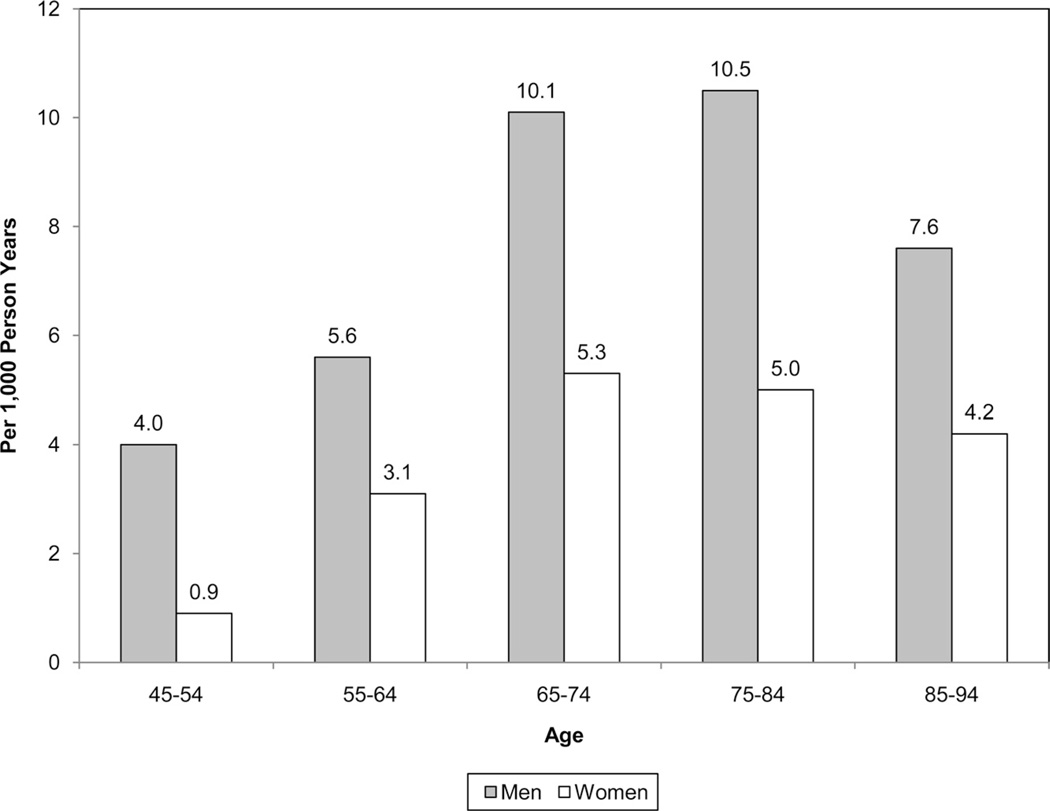
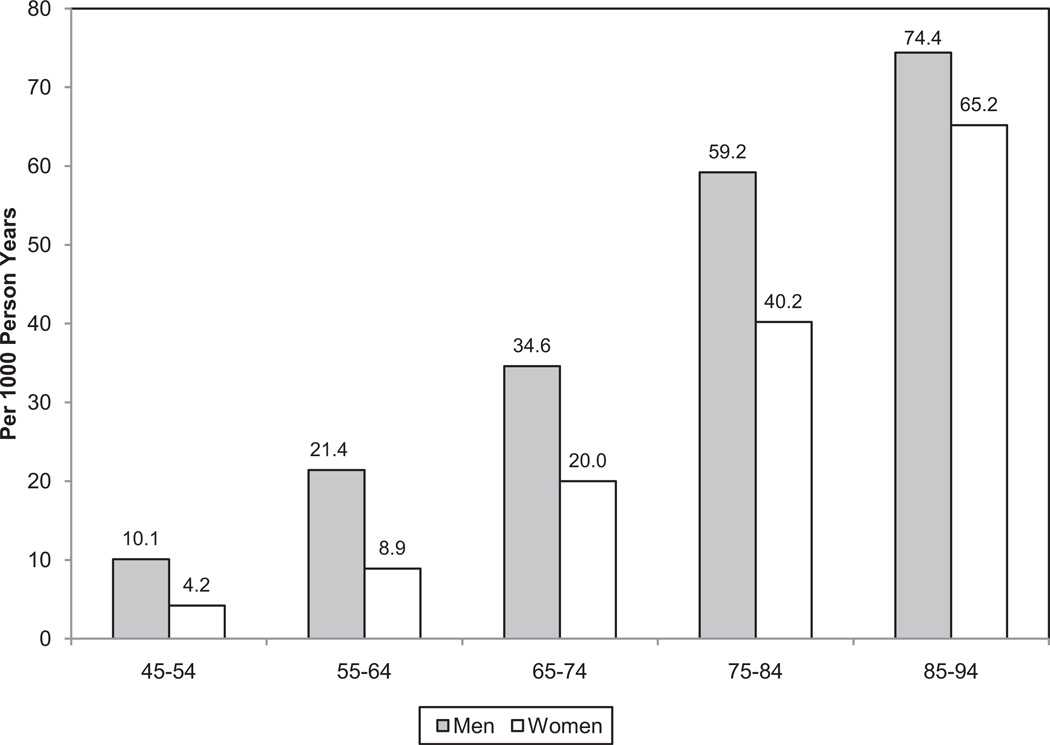
—The average annual rates of first cardiovascular events rise from 3 per 1000 men at 35 to 44 years of age to 74 per 1000 men at 85 to 94 years of age. For women, comparable rates occur 10 years later in life. The gap narrows with advancing age.
-
—Before 75 years of age, a higher proportion of CVD events due to CHD occur in men than in women, and a higher proportion of events due to stroke occur in women than in men.
-
—
Among American Indian men 45 to 74 years of age, the incidence of CVD ranges from 15 to 28 per 1000 population. Among women, it ranges from 9 to 15 per 1000.4
Data from the FHS indicate that the subsequent lifetime risk for all CVD in recipients starting free of known disease is 2 in 3 for men and >1 in 2 for women at 40 years of age (personal communication, Donald Lloyd-Jones, MD, Northwestern University, Chicago, Ill) (see Table 3-4).
Analysis of FHS data among participants free of CVD at 50 years of age showed the lifetime risk for developing CVD was 51.7% for men and 39.2% for women. Median overall survival was 30 years for men and 36 years for women.5
Mortality
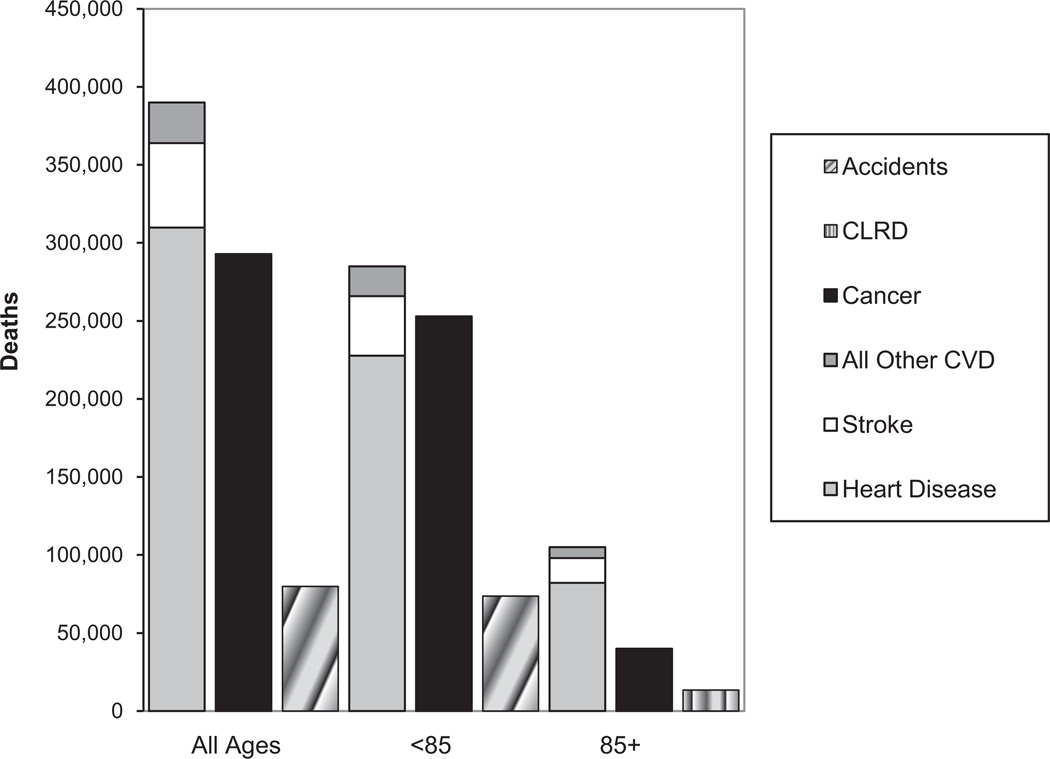
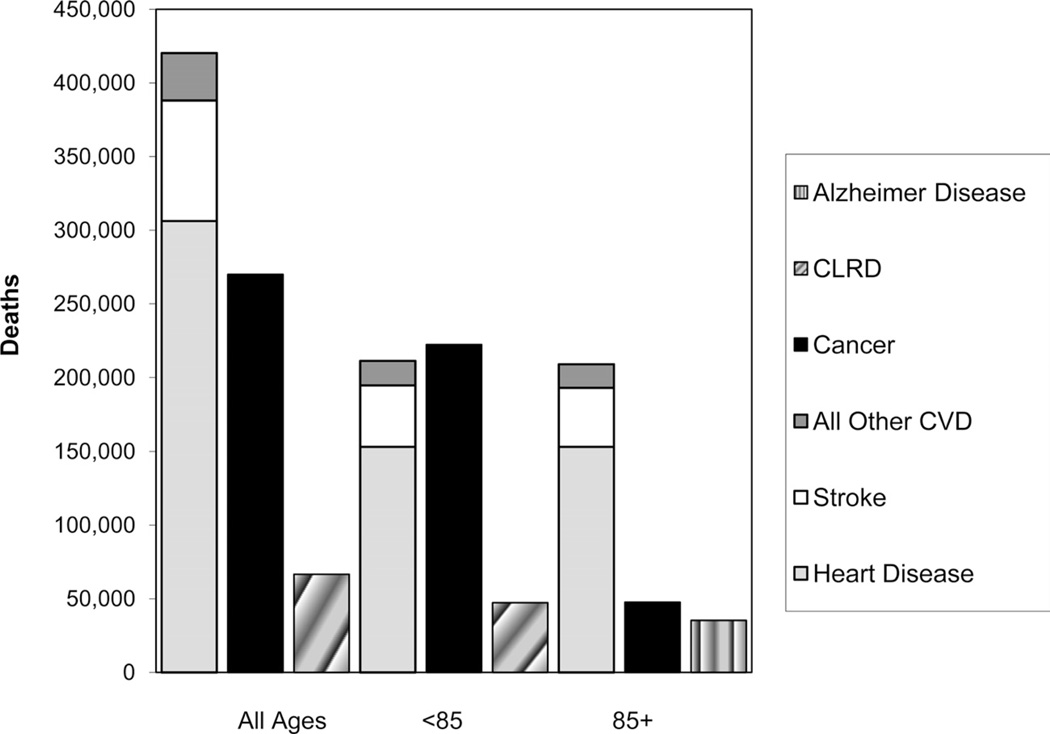
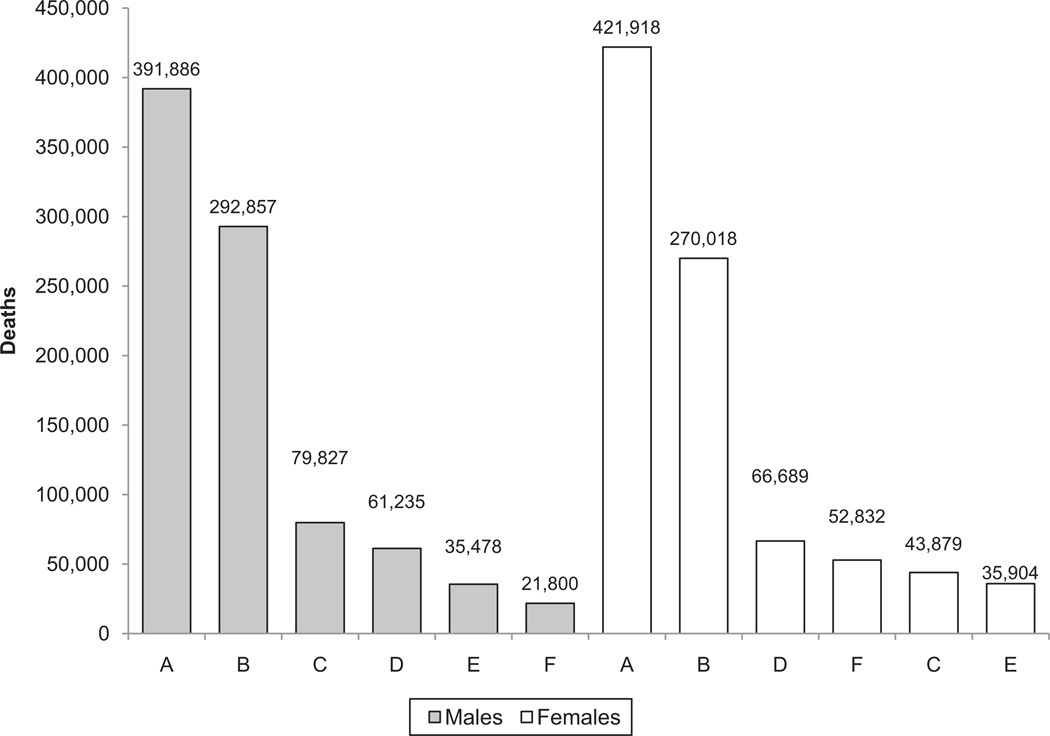
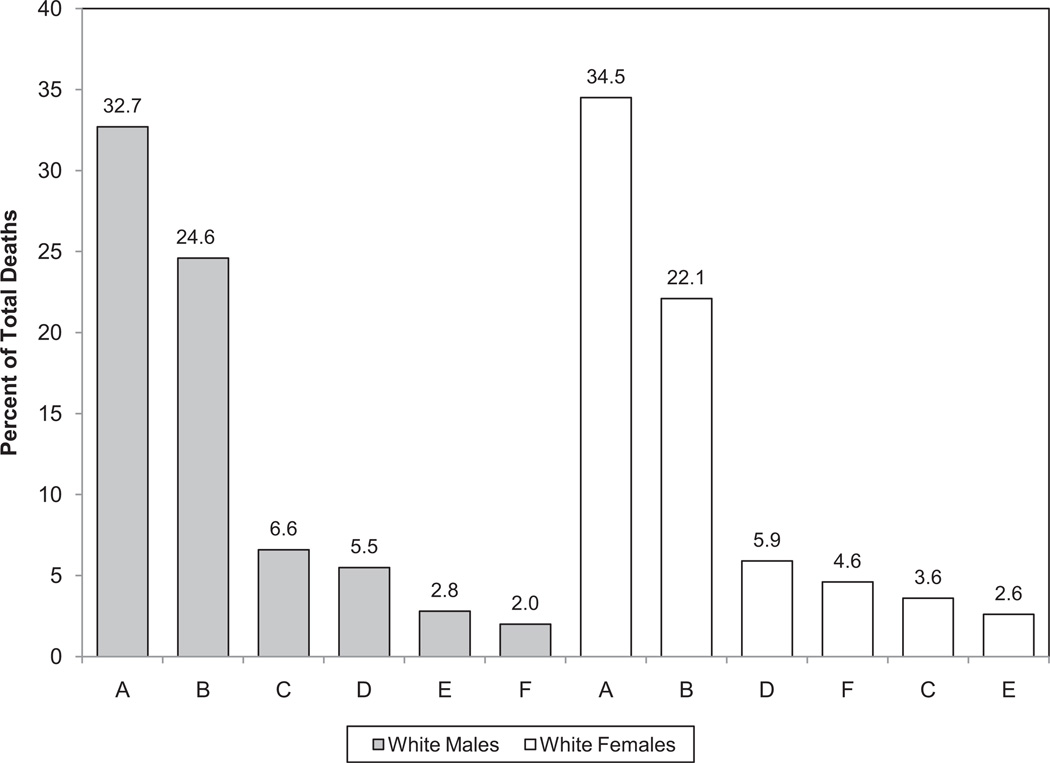
ICD-10 I00 –I99, Q20–Q28 for CVD (CVD mortality includes congenital cardiovascular defects); C00–C97 for cancer; C33–C34 for lung cancer; C50 for breast cancer; J40–J47 for chronic lower respiratory disease (CLRD); G30 for Alzheimer disease; E10–E14 for diabetes mellitus (DM); and V01–X59, Y85–Y86 for accidents.
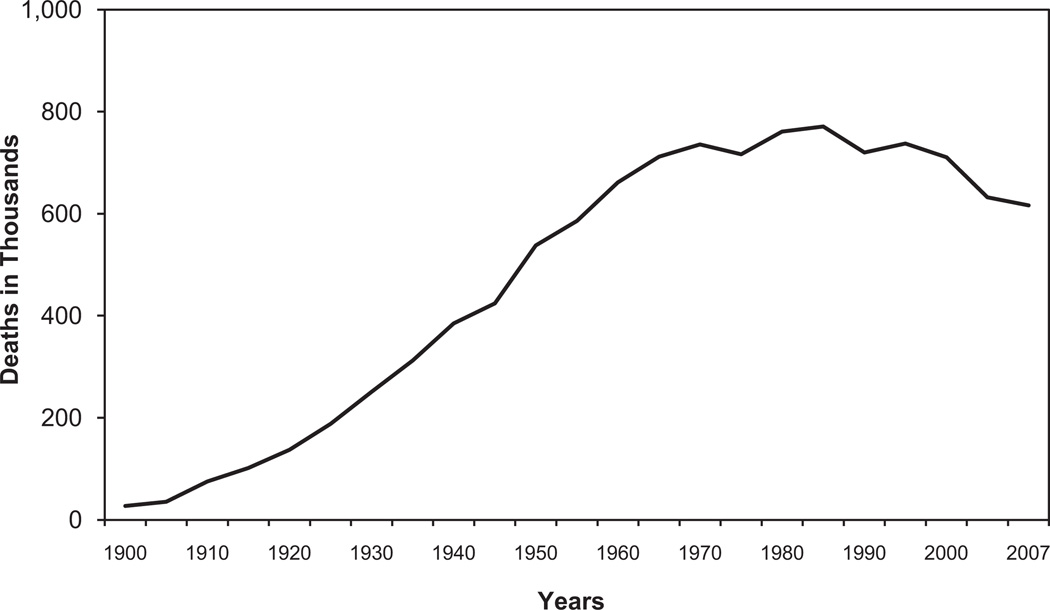
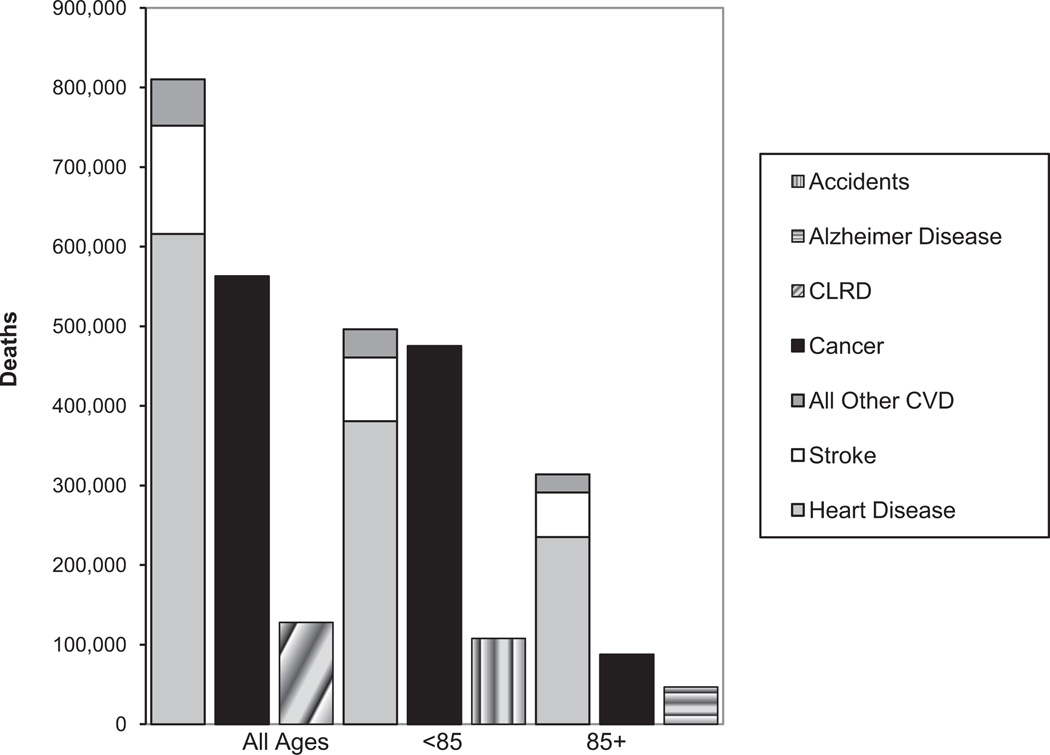
Mortality data show that CVD (I00 –I99, Q20–Q28) as the underlying cause of death (including congenital cardiovascular defects) accounted for 33.6% (813 804) of all 2 423 712 deaths in 2007, or 1 of every 3 deaths in the United States. CVD any-mentions (1 342 314 deaths in 2007) constituted 55.4% of all deaths that year (NHLBI; NCHS public-use data files).6 The 2007 death rate was 251.2 (excluding congenital cardiovascular defects) (NCHS).6 In every year since 1900 except 1918, CVD accounted for more deaths than any other major cause of death in the United States.7–10
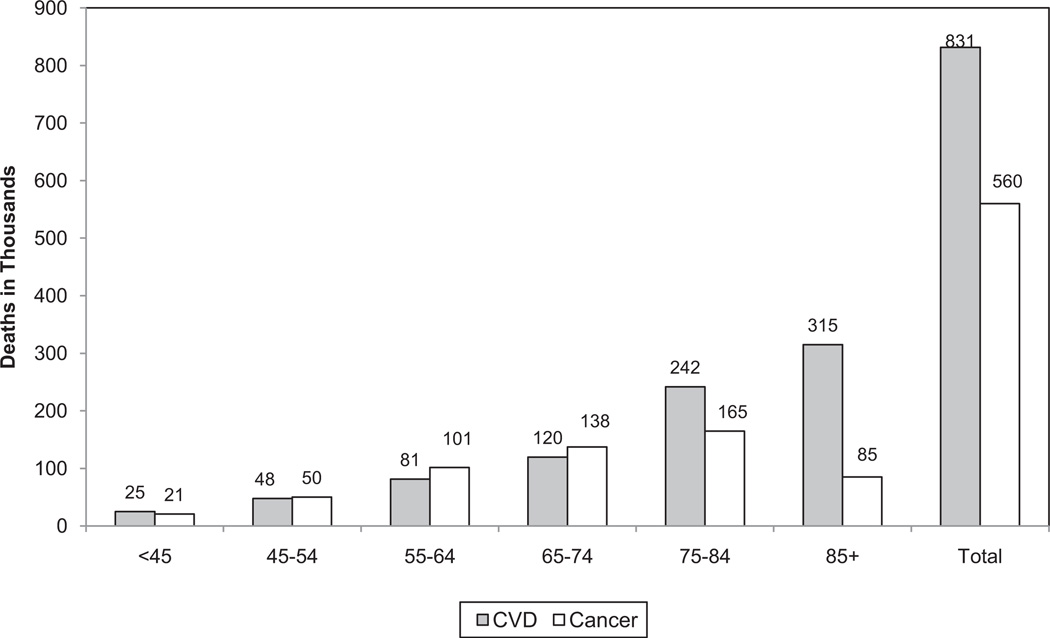
On average, >2200 Americans die of CVD each day, an average of 1 death every 39 seconds. CVD claims more lives each year than cancer, CLRD, and accidents combined.6
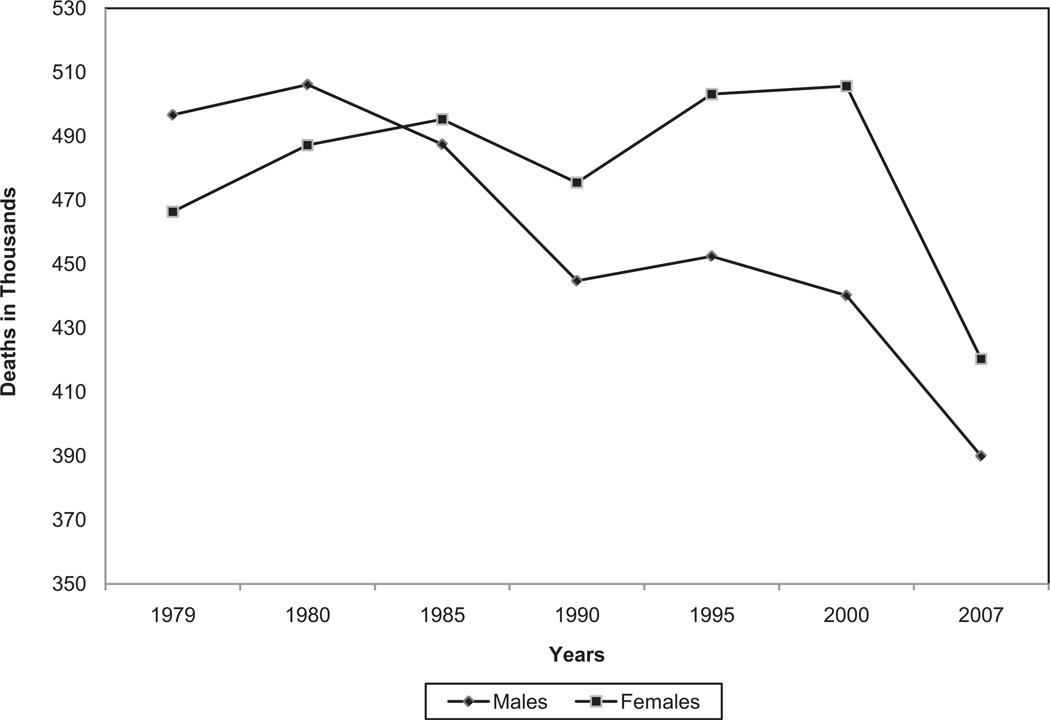
The 2007 overall death rate due to CVD (I00 –I99) was 251.2. The rates were 294.0 for white males, 405.9 for black males, 205.7 for white females, and 286.1 for black females. From 1997 to 2007, death rates due to CVD (ICD-10 I00 –I99) declined 27.8%. In the same 10-year period, the actual number of CVD deaths per year declined 14.2% (NHLBI tabulation).6 (Appropriate comparability ratios were applied.)
Among other causes of death in 2007, cancer caused 562 875 deaths; accidents, 123 706; Alzheimer disease, 74 632; and HIV/AIDS, 11 295.6
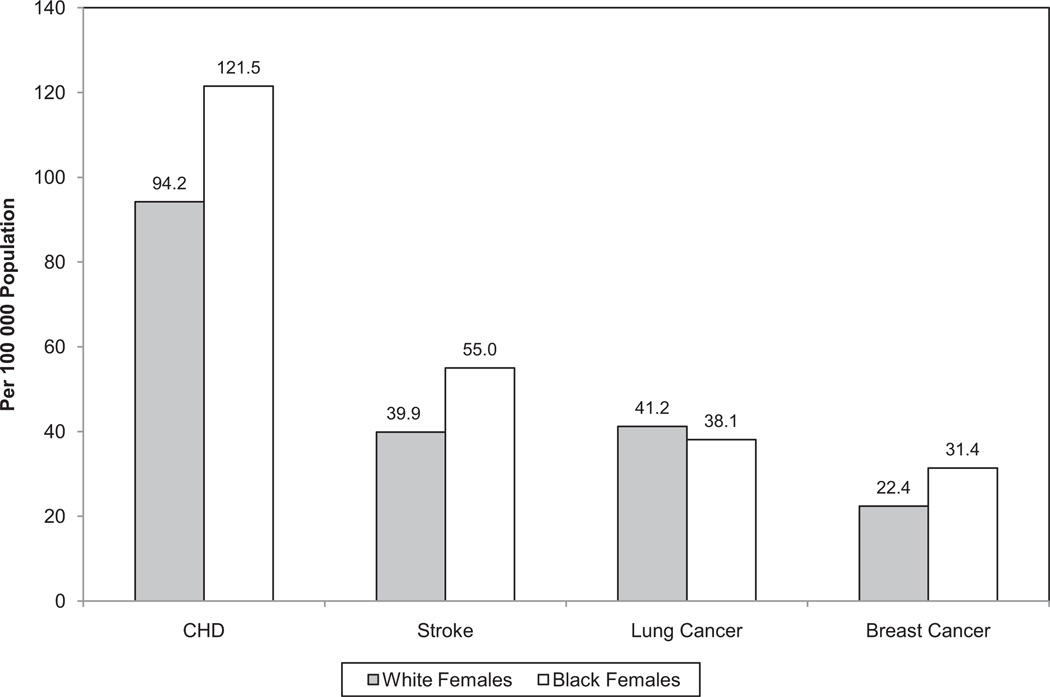
The 2007 CVD (I00 –I99) death rates were 300.3 for males and 211.6 for females. Death rates for cancer (malignant neoplasms) were 217.5 for males and 151.3 for females. Breast cancer claimed the lives of 40 599 females in 2007; lung cancer claimed 70 388. Death rates for females were 22.9 for breast cancer and 40.0 for lung cancer. One in 30 deaths in females was due to breast cancer, whereas 1 in 6.4 was due to CHD. For comparison, 1 in 4.5 females died of cancer, whereas 1 in 2.9 died of CVD (I00 –I99, Q20–Q28). On the basis of 2007 mortality data, CVD caused ≈1 death per minute among females, or 421 918 deaths in females in 2007. That represents more female lives than were claimed by cancer, CLRD, Alzheimer disease, and accidents combined (unpublished NHLBI tabulation).6
More than 150 000 Americans died of CVD (I00 –I99) in 2007 who were <65 years of age, and nearly 33% of deaths owing to CVD occurred before the age of 75 years, which is well before the average life expectancy of 77.9 years.6
In 2007, death rates for diseases of the heart in American Indians or Alaska Natives were 159.8 for males and 99.8 for females; for Asians or Pacific Islanders, they were 126.0 for males and 82.0 for females; and for Hispanics or Latinos, they were 165.0 for males and 111.8 for females.7
According to the NCHS, if all forms of major CVD were eliminated, life expectancy would rise by almost 7 years. If all forms of cancer were eliminated, the estimated gain would be 3 years. According to the same study, the probability at birth of eventually dying of major CVD (I00 –I78) is 47%, and the chance of dying of cancer is 22%. Additional probabilities are 3% for accidents, 2% for DM, and 0.7% for HIV.11
In 2007, the leading causes of death in women ≥65 years of age were diseases of the heart (No. 1), cancer (No. 2), stroke (No. 3), and CLRD (No. 4). In older men, they were diseases of the heart (No. 1), cancer (No. 2), CLRD (No. 3), and stroke (No. 4).6,10
A study of the decrease in US deaths due to CHD from 1980 to 2000 suggests that ≈47% of the decrease was attributable to increased use of evidence-based medical therapies and 44% to changes in risk factors in the population due to lifestyle and environmental changes.12
Analysis of data from NCHS was used to determine the number of disease-specific deaths attributable to all non-optimal levels of each risk factor exposure, by age and sex. In 2005, tobacco smoking and high BP were estimated to be responsible for 467 000 deaths, accounting for ≈1 in 5 or 6 deaths among US adults. Overweight/obesity and physical inactivity were each estimated to be responsible for nearly 1 in 10 deaths. High dietary salt, low dietary omega-3 fatty acids, and high dietary trans fatty acids were the dietary risks with the largest estimated mortality effects.13
Aftermath
Among an estimated 45 million people with functional disabilities in the United States, HD, stroke, and hypertension are among the 15 leading conditions that caused those disabilities. Disabilities were defined as difficulty with activities of daily living or instrumental activities of daily living, specific functional limitations (except vision, hearing, or speech), and limitation in ability to do housework or work at a job or business.14
Out-of-Hospital Cardiac Arrest
There is a wide variation in the reported incidence of and outcome for out-of-hospital cardiac arrest. These differences are due in part to differences in definition and ascertainment of cardiac arrest data, as well as differences in treatment after the onset of cardiac arrest. Cardiac arrest is defined as cessation of cardiac mechanical activity and is confirmed by the absence of signs of circulation.15
Extrapolation of the mortality rate observed in the Resuscitation Outcomes Consortium (ROC) to the total population of the United States suggests that each year, there are 295 000 (quasi confidence intervals 236 000 to 325 000) emergency medical services (EMS)-assessed out-of-hospital cardiac arrests in the United States.16
≈60% of out-of-hospital cardiac deaths are treated by EMS personnel.17
Only 33% of those with EMS-treated out-of-hospital cardiac arrest have symptoms within 1 hour of death.18
Among EMS-treated out-of-hospital cardiac arrests, 23% have an initial rhythm of ventricular fibrillation (VF), ventricular tachycardia (VT), or are shockable by automated external defibrillator (AED); 31% receive bystander cardiopulmonary resuscitation (CPR).16
The incidence of cardiac arrest with an initial rhythm of VF is decreasing over time; however, the incidence of cardiac arrest with any initial rhythm is not decreasing.19
Among ROC sites between December 2005 and May 2007, 32.0% of out-of-hospital cardiac arrests received layresponder CPR and only 2.1% had an AED applied before EMS arrival. Overall chance of surviving until hospital discharge was 7%, and AED application was associated with a moderately increased odds of survival.20
If bystander CPR is not provided, a sudden cardiac arrest victim’s chances of survival fall 7% to 10% for every minute of delay until defibrillation.21–25
The median survival rate to hospital discharge after EMS-treated out-of-hospital cardiac arrest with any first recorded rhythm is 7.9%.16
The median survival rate after VF is 21%.16
Extrapolation of data from ARIC, CHS, and Framingham suggests that there are 125 000 CHD deaths within 1 hour of symptom onset (NHLBI, written communication, July 13, 2010).
A study conducted in New York City found the age-adjusted incidence of out-of-hospital cardiac arrest per 10 000 adults was 10.1 among blacks, 6.5 among Hispanics, and 5.8 among whites. The age-adjusted survival to 30 days after discharge was more than twice as poor for blacks as for whites, and survival among Hispanics was also lower than among whites.26
In a systematic review of literature through 2008, the factors most correlated with survival to hospital discharge following out-of-hospital cardiac arrest were witness by a bystander, witness by EMS, receipt of bystander CPR, being found in VF or VT, and achieving return of spontaneous circulation.27
Out-of-Hospital Cardiac Arrest: Children
The reported incidence of out-of-hospital pediatric cardiac arrest varies widely (≈8 per 100 000).28
There are >74 million individuals <18 years of age in the United States29; this implies that there are about 5920 pediatric out-of-hospital cardiac arrests annually of all causes (including trauma, sudden infant death syndrome, respiratory causes, cardiovascular causes, and submersion).
Seven percent of EMS-treated pediatric cardiac arrest patients had an initial rhythm of VF, VT, or were shockable by AED; 35% received bystander CPR.28
Studies that document voluntary reports of deaths among high school athletes suggest that the incidence of out-of-hospital cardiac arrest ranges from 0.28 to 1.0 deaths per 100 000 high school athletes annually nationwide.30,31 Although incomplete, these numbers provide a basis for estimating the number of deaths in this age range.
One report describes the incidence of nontraumatic pediatric cardiac arrest (among students 3 to 18 years of age) that occurs in schools and estimates rates (per 100 000 person-school-years) for elementary, middle, and high schools to be 0.18, 0.19, and 0.15, respectively, for the geographic area (King County, WA) and time frame (January 1, 1990, to December 31, 2005) studied.32
The reported average rate of survival to hospital discharge after pediatric out-of-hospital cardiac arrest is 6%.
Most sudden deaths in athletes were attributable to CVD (56%). Of the cardiovascular deaths that occurred, 29% occurred in blacks, 54% in high school students, and 82% with physical exertion during competition/training, and only 11% occurred in females, although this proportion has increased over time.33
In-Hospital Cardiac Arrest
- A total of 287 facilities reported 18 817 events to the National Registry for Cardiopulmonary Resuscitation during 2009.
-
—The rates of survival to discharge after in-hospital cardiac arrest were 33% among children and 21% among adults. Of these, 95% were monitored or witnessed.
-
—Eighteen percent had VF or pulseless VT as the first recorded rhythm. Of these, 43% survived to discharge.
-
—
Awareness of CPR
Seventy-nine percent of the lay public are confident that they know what actions to take in a medical emergency; 98% recognize an AED as something that administers an electric shock to restore a normal heart beat among victims of sudden cardiac arrest; and 60% are familiar with CPR (Harris Interactive survey conducted on behalf of the AHA among 1132 US residents 18 years of age and older, January 8, 2008, through January 21, 2008).
Awareness of Warning Signs and Risk Factors for CVD
Surveys conducted by the AHA in 1997, 2000, 2003, and 2006 to evaluate trends in women’s awareness, knowledge, and perceptions related to CVD found that, in 2006, awareness of HD as the leading cause of death among women was 57%, significantly higher than in prior surveys. Awareness was lower among black and Hispanic women than among white women, and the racial/ethnic difference has not changed appreciably over time. In 2006, more than twice as many women felt uninformed about stroke compared with HD. Hispanic women were more likely than white women to report that there is nothing they can do to keep themselves from getting CVD. The majority of respondents reported confusion related to basic CVD prevention strategies.34
A nationally representative sample of women responded to a questionnaire about history of CVD risk factors, self-reported actions taken to reduce risk, and barriers to heart health. According to the study, published in 2006, the rate of awareness of CVD as the leading cause of death had nearly doubled since 1997, was significantly greater for whites than for blacks and Hispanics, and was independently correlated with increased physical activity (PA) and weight loss in the previous year. Fewer than half of the respondents were aware of healthy levels of risk factors. Awareness that their personal level was not healthy was positively associated with preventive action. Most women took steps to lower risk in family members and themselves.35
A total of 875 students in 4 Michigan high schools were given a survey to obtain data on the perception of risk factors and other knowledge-based assessment questions about CVD. Accidents were rated as the greatest perceived lifetime health risk (39%). Nearly 17% selected CVD as the greatest lifetime risk, which made it the third most popular choice after accidents and cancer. When asked to identify the greatest cause of death for each sex, 42% correctly recognized CVD for men, and 14% correctly recognized CVD for women; 40% incorrectly chose abuse/use behavior with a substance other than cigarettes as the most important CVD risk behavior.36
Risk Factors
Data from the 2003 CDC BRFSS survey of adults ≥18 years of age showed the prevalence of respondents who reported having ≥2 risk factors for HD and stroke was successively higher at higher age groups. The prevalence of having ≥2 risk factors was highest among blacks (48.7%) and American Indians/Alaska Natives (46.7%) and lowest among Asians (25.9%); prevalence was similar in women (36.4%) and men (37.8%). The prevalence of multiple risk factors ranged from 25.9% among college graduates to 52.5% among those with less than a high school diploma (or its equivalent). People reporting household income of ≥$50 000 had the lowest prevalence (28.8%), and those reporting household income of $10 000 had the highest prevalence (52.5%). Adults who reported being unable to work had the highest prevalence (69.3%) of ≥2 risk factors, followed by retired people (45.1%), unemployed adults (43.4%), homemakers (34.3%), and employed people (34.0%). Prevalence of ≥2 risk factors varied by state/territory and ranged from 27.0% (Hawaii) to 46.2% (Kentucky). Twelve states and 2 territories had a multiple-risk-factor prevalence of ≥40%: Alabama, Arkansas, Georgia, Indiana, Kentucky, Louisiana, Mississippi, North Carolina, Ohio, Oklahoma, Tennessee, West Virginia, Guam, and Puerto Rico.37
Data from the Chicago Heart Association Detection Project (1967 to 1973, with an average follow-up of 31 years) showed that in younger women (18 to 39 years of age) with favorable levels for all 5 major risk factors (BP, serum cholesterol, body mass index [BMI], DM, and smoking), future incidence of CHD and CVD is rare, and long-term and all-cause mortality are much lower than for those who have unfavorable or elevated risk factor levels at young ages. Similar findings applied to men in this study.38,39
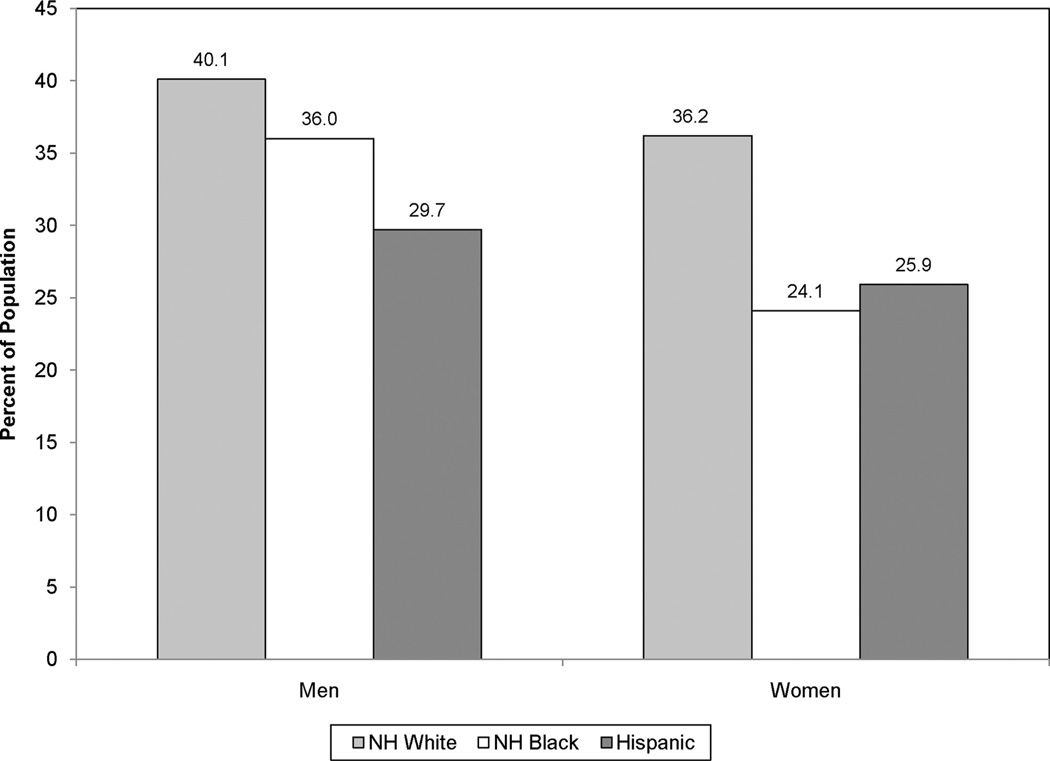
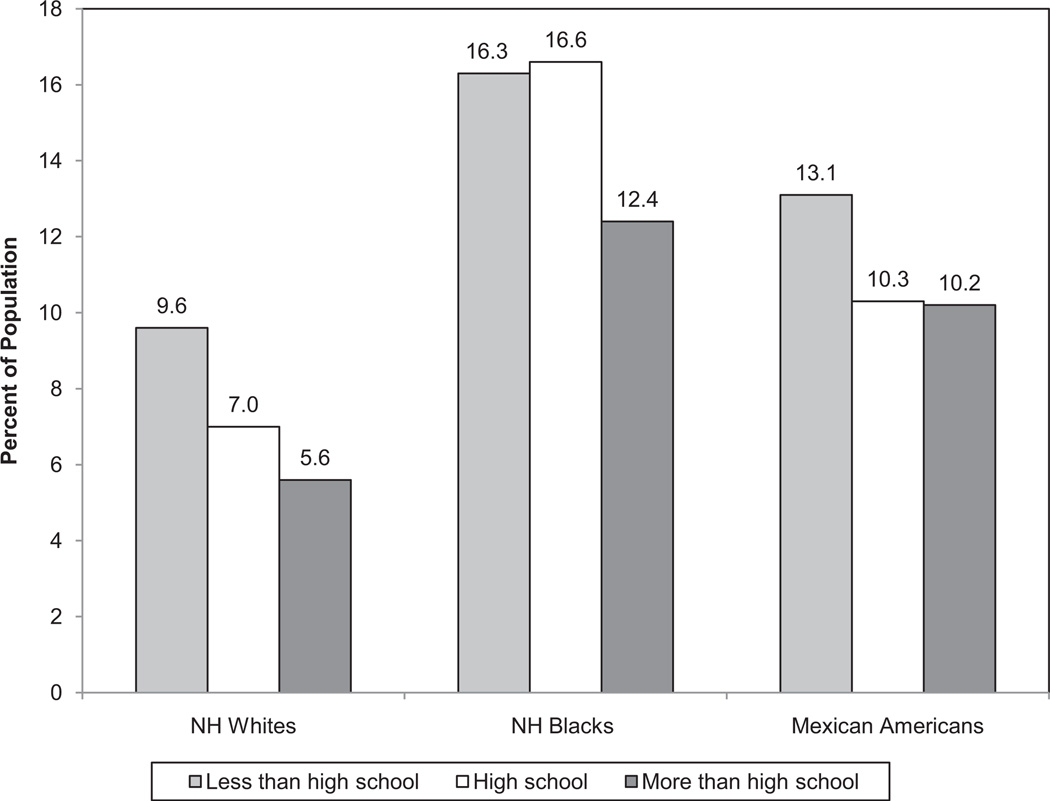
Analysis of several data sets by the CDC showed that in adults ≥18 years of age, disparities were common in all risk factors examined. In men, the highest prevalence of obesity (29.7%) was found in Mexican Americans who had completed a high school education. Black women with or without a high school education had a high prevalence of obesity (48.4%). Hypertension prevalence was high among blacks (41.2%) regardless of sex or educational status. Hypercholesterolemia was high among white and Mexican American men and white women regardless of educational status. CHD and stroke were inversely related to education, income, and poverty status. Hospitalization for total HD and acute MI was greater among men, but hospitalization for congestive heart failure (CHF) and stroke was greater among women. Among Medicare enrollees, CHF hospitalization was higher in blacks, Hispanics, and American Indians/Alaska Natives than among whites, and stroke hospitalization was highest in blacks. Hospitalizations for CHF and stroke were highest in the southeastern United States. Life expectancy remains higher in women than in men and in whites than in blacks by ≈5 years. CVD mortality at all ages tended to be highest in blacks.40
Analysis of 5 cross-sectional, nationally representative surveys from the National Health Examination Survey (NHES) 1960–1962 to the NHANES 1999–2000 showed that the prevalence of key risk factors (ie, high cholesterol, HBP, current smoking, and total DM) decreased over time across all BMI groups, with the greatest reductions observed among overweight and obese groups. Total DM prevalence was stable within BMI groups over time; however, the trend has leveled off or been reversed for some of the risk factors in more recent years.41
Data from BRFSS 2006–2008 demonstrated that during this 3-year period, 25.6% of non-Hispanic blacks, non-Hispanic whites, and Hispanics were obese, but prevalent obesity varied across groups: 35.7% for non-Hispanic blacks, 28.7% for Hispanics, and 23.7% for non-Hispanic whites.
Data from NHANES 2005–2006 showed that only 9.6% of US adults met their recommended target of daily dietary sodium intake.42
Analysis of >14 000 middle-aged subjects in the ARIC study sponsored by the NHLBI showed that >90% of CVD events in black subjects, compared with ≈70% in white subjects, appeared to be explained by elevated or borderline risk factors. Furthermore, the prevalence of participants with elevated risk factors was higher in black subjects; after accounting for education and known CVD risk factors, the incidence of CVD was identical in black and white subjects. Thus, the observed higher CVD incidence rate in black subjects appears to be largely attributable to a greater prevalence of elevated risk factors. These results suggest that the primary prevention of elevated risk factors might substantially impact the future incidence of CVD, and these beneficial effects would likely be applicable not only for white but also for black subjects.43
- Data from the MEPS 2004 Full-Year Data File showed that nearly 26 million US adults ≥18 years of age were told by a doctor that they had HD, stroke, or any other heart-related disease44:
-
—56.6% of those surveyed said they engaged in moderate-to-vigorous PA 3 times per week; 57.9% of those surveyed who had not been told they had HD engaged in regular PA, more than those who had been told they had HD (46.3%).
-
—38.6% maintained a healthy weight. Among those told that they had HD, 33.9% had a healthy weight compared with 39.3% who had never been told they had HD.
-
—78.8% did not currently smoke. Among those ever told that they had indicators of HD, 18.3% continued to smoke.
-
—More than 93% engaged in at least 1 recommended behavior for prevention of HD: 75.5% engaged in 1 or 2; 18% engaged in all 3; and 6.5% did not engage in any of the recommended behaviors.
-
—Age-based variations:
-
◦Moderate to vigorous PA ≥3 times per week varied according to age. Younger people (18 to 44 years of age) were more likely (59.9%) than those who were older (45 to 64 and ≥65 years of age, 55.3% and 48.5%, respectively) to engage in regular PA.
-
◦A greater percentage of those 18 to 44 years of age had a healthy weight (43.7%) than did those 45 to 64 years of age and ≥65 years of age (31.4% and 37.3%, respectively).
-
◦People ≥65 years of age were more likely to be current nonsmokers (89.7%) than were people 18 to 44 years of age and 45 to 64 years of age (76.1% and 77.7%, respectively).
-
◦
- — Race/ethnicity-based variations:
-
◦Non-Hispanic whites were more likely than Hispanics or non-Hispanic blacks to engage in moderate-to-vigorous PA (58.5% versus 51.4% and 52.5%, respectively).
-
◦Non-Hispanic whites were more likely to have maintained a healthy weight than were Hispanics or non-Hispanic blacks (39.8% versus 32.1% and 29.7%, respectively).
-
◦Hispanics were more likely to be nonsmokers (84.2%) than were non-Hispanic whites and non-Hispanic blacks (77.8% and 76.3%, respectively).
-
◦
-
—Sex-based variations:
-
◦Men were more likely to have engaged in moderate-to-vigorous PA ≥3 times per week than women (60.3% versus 53.1%, respectively).
-
◦Women were more likely than men to have maintained a healthy weight (45.1% versus 31.7%, respectively).
-
◦81.7% of women did not currently smoke, compared with 75.7% of men.
-
◦
-
—Variations based on education level:
-
◦A greater percentage of adults with at least some college education engaged in moderate-to-vigorous PA ≥3 times per week (60.8%) than did those with a high school education or less than a high school education (55.3% and 48.3%, respectively).
-
◦A greater percentage of adults with at least some college education had a healthy weight (41.2%) than did those with a high school or less than high school education (36.2% and 36.1%, respectively).
-
◦There was a greater percentage of nonsmokers among those with a college education (85.5%) than among those with a high school or less than high school education (73.8% and 69.9%, respectively).
-
◦
-
—
Participants (18 to 64 years of age at baseline) in the Chicago Heart Association Detection Project in Industry without a history of MI were investigated to determine whether traditional CVD risk factors were similarly associated with CVD mortality in black and white men and women. In general, the magnitude and direction of associations were similar by race. Most traditional risk factors demonstrated similar associations with mortality in black and white adults of the same sex. Small differences were primarily in the strength and not the direction of the association.45
A study of nearly 1500 participants in the Multi-Ethnic Study of Atherosclerosis (MESA) study found that Hispanics with hypertension, hypercholesterolemia, and/or DM who speak Spanish at home and/or have spent less than half a year in the United States have higher systolic BP, low-density lipoprotein (LDL) cholesterol, and fasting blood glucose, respectively, than Hispanics who speak English and who have lived a longer period of time in the United States.46
Family History of Premature-Onset CVD
There is consistent evidence from multiple large-scale prospective epidemiology studies for a strong and significant association of a reported family history of premature parental CHD with incident MI or CHD in offspring. In the FHS, the occurrence of a validated premature atherosclerotic CVD event in either a parent47 or a sibling48 was associated with an ≈2-fold elevated risk for CVD, independent of other traditional risk factors.
Addition of family history of premature CVD to a model that contained traditional risk factors provided modestly improved prognostic value in the FHS.47 Family history of premature MI is also an independent risk factor in other multivariable risk models that contain traditional risk factors in large cohorts of women50 and men.50
Parental history of premature CHD is associated with increased burden of atherosclerosis in the coronary arteries and the abdominal aorta.51,52
In the FHS, a parental history of validated HF is associated with a 1.7-fold higher risk of HF in offspring, after multivariable adjustment.53
A family history of early-onset sudden cardiac death in a first-degree relative is associated with a >2-fold higher risk for sudden cardiac death in offspring on the basis of available case-control studies.54
The 2004 HealthStyles survey of 4345 people in the United States indicated that most respondents believe that knowing their family history is important for their own health, but few are aware of the specific health information from relatives necessary to develop a family history.55
An accurate and complete family history may identify rare mendelian conditions such as hypertrophic cardiomyopathy, long-QT syndrome, or familial hypercholesterolemia. However, in most people with a family history of a CVD event, a known rare mendelian condition is not identified.
Studies are under way to determine genetic variants that may help identify people at increased risk of CVD.
Impact of Healthy Lifestyle and Low Risk Factor Levels
Much of the literature on CVD has focused on factors associated with increasing risk for CVD and on factors associated with poorer outcomes in the presence of CVD; however, in recent years, a number of studies have defined the potential beneficial effects of healthy lifestyle factors and lower CVD risk factor burden on CVD outcomes and longevity. These studies suggest that prevention of risk factor development at younger ages may be the key to “successful aging,” and they highlight the need for intensive prevention efforts at younger and middle ages once risk factors develop to increase the likelihood of healthy longevity.
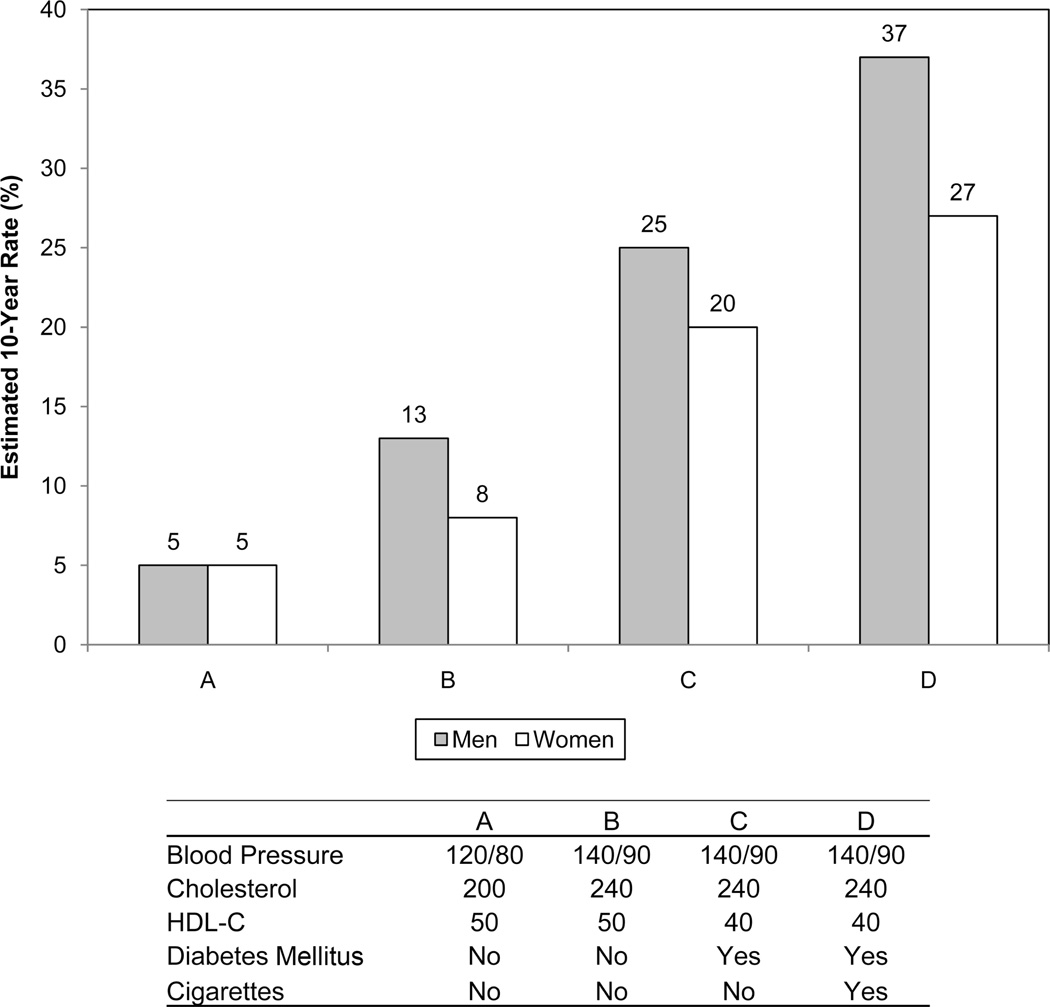
The lifetime risk for CVD and median survival were highly associated with risk factor presence and burden at 50 years of age among >7900 men and women from the FHS followed up for 111 000 person-years. In this study, optimal risk factor burden at 50 years of age was defined as BP <120/ 80 mm Hg, total cholesterol <180 mg/dL, absence of DM, and absence of smoking. Elevated risk factors were defined as stage 1 hypertension or borderline high cholesterol (200 to 239 mg/dL). Major risk factors were defined as stage 2 hypertension, elevated cholesterol (≥240 mg/dL), current smoking, and DM. Remaining lifetime risks for atherosclerotic CVD events were only 5.2% in men and 8.2% in women with optimal risk factors at 50 years of age compared with 68.9% in men and 50.2% in women with ≥2 major risk factors at age 50. In addition, men and women with optimal risk factors had a median life expectancy ≥10 years longer than those with ≥2 major risk factors at age 50 years.5
A recent study examined the association between low lifetime predicted risk for CVD (ie, having all optimal or near-optimal risk factor levels) and burden of subclinical atherosclerosis in younger adults in the Coronary Artery Risk Development in Young Adults (CARDIA) and MESA studies of the NHLBI. Among participants <50 years of age, nearly half had low and half had high predicted lifetime risks for CVD. Those with low predicted lifetime risk had lower prevalence and less severe amounts of coronary calcification and less carotid intima-media thickening, even at these younger ages, than those with high predicted lifetime risk. During follow-up, those with low predicted lifetime risk also had less progression of coronary calcium.56
- In another study, FHS investigators followed up 2531 men and women who were examined between the ages of 40 and 50 years and observed their overall rates of survival and survival free of CVD to 85 years of age and beyond. Low levels of the major risk factors in middle age was associated with overall survival and morbidity-free survival to 85 years of age or more.57
-
—Overall, 35.7% survived to the age of 85 years, and 22% survived to that age free of major morbidities.
-
—Factors associated with survival to the age of 85 years included female sex, lower systolic BP, lower total cholesterol, better glucose tolerance, absence of current smoking, and higher level of education attained. Factors associated with survival to the age of 85 years free of MI, unstable angina, HF, stroke, dementia, and cancer were nearly identical.
-
—When adverse levels of 4 of these factors were present in middle age, <5% of men and ≈15% of women survived to 85 years of age.
-
—
A study of 366 000 men and women from the Multiple Risk Factor Intervention Trial (MRFIT) and Chicago Heart Association Detection Project in Industry defined low-risk status as follows: serum cholesterol level <200 mg/dL, untreated BP 120/80 mm Hg, absence of current smoking, absence of DM, and absence of major electrocardiographic abnormalities. Compared with those who did not have low risk factor burden, those with low risk factor burden had between 73% and 85% lower relative risk (RR) for CVD mortality, 40% to 60% lower relative total mortality rates, and 6 to 10 years’ longer life expectancy.39
A study of 84 129 women enrolled in the Nurses’ Health Study identified 5 healthy lifestyle factors, including absence of current smoking, drinking half a glass or more of wine per day (or equivalent alcohol consumption), half an hour or more per day of moderate or vigorous PA, BMI <25 kg/m2, and dietary score in the top 40% (which included diets with lower amounts of trans fats, lower glycemic load, higher cereal fiber, higher marine omega-3 fatty acids, higher folate, and higher polyunsaturated to saturated fat ratio). When 3 of the 5 healthy lifestyle factors were present, the RR for CHD over a 14-year period was 57% lower; when 4 were present, RR was 66% lower; and when all 5 factors were present, RR was 83% lower.58 However, data from NHANES 1999–2002 showed that only about one third of adults complied with 6 or more of the recommended heart-healthy behaviors. Dietary recommendations, in general, and daily fruit intake recommendations, in particular, were least likely to be followed.59
In the Chicago Heart Association Detection Project in Industry, remaining lifetime risks for CVD death were noted to increase substantially and in a graded fashion according to the number of risk factors present in middle age (40 to 59 years of age). However, remaining lifetime risks for non-CVD death also increased dramatically with increasing CVD risk factor burden. These data help to explain the markedly greater longevity experienced by those who reach middle age free of major CVD risk factors.60
Among individuals 70 to 90 years of age, adherence to a Mediterranean-style diet and greater PA are associated with 65% to 73% relatively lower rates of all-cause mortality, as well as lower mortality rates due to CHD, CVD, and cancer.61
Seventeen-year mortality data from the NHANES II Mortality Follow-Up Study indicated that the RR for fatal CHD was 51% lower for men and 71% lower for women with none of 3 major risk factors (hypertension, current smoking, and elevated total cholesterol [≥ 240 mg/dL]) than for those with 1 or more risk factors. Had all 3 major risk factors not occurred, it is hypothesized that 64% of all CHD deaths among women and 45% of CHD deaths in men could have been avoided.62
- Investigators from the Chicago Heart Association Detection Project in Industry have also observed that risk factor burden in middle age is associated with better quality of life at follow-up in older age (≈25 years later) and lower average annual Medicare costs at older ages.
-
—The presence of a greater number of risk factors in middle age is associated with lower scores at older ages on assessment of social functioning, mental health, walking, and health perception in women, with similar findings in men.63
-
—Similarly, the existence of a greater number of risk factors in middle age is associated with higher average annual CVD-related and total Medicare costs (once Medicare eligibility is attained).64
-
—
Hospital Discharges, Ambulatory Care Visits, and Nursing Home Residents
From 1997 to 2007, the number of inpatient discharges from short-stay hospitals with CVD as the first-listed diagnosis decreased from 6 097 000 to 5 890 000 (NHDS, NCHS, and NHLBI). In 2007, CVD ranked highest among all disease categories in hospital discharges. (NHDS, NCHS, and NHLBI).
In 2008, there were 91 736 000 physician office visits with a primary diagnosis of CVD (NCHS, NAMCS).65 In 2008, there were 4 866 000 ED visits with a primary diagnosis of CVD (NCHS, National Hospital Ambulatory Medical Care Survey [NHAMCS]).66
In 2008, there were 8 795 000 hospital OPD visits with a primary diagnosis of CVD (NHAMCS).66 In 2005, ≈1 of every 6 hospital stays, or almost 6 million, resulted from CVD (AHRQ, NIS). The total inpatient hospital cost for CVD was $71.2 billion, approximately one fourth of the total cost of inpatient hospital care in the United States. The average cost per hospitalization was ≈41% higher than the average cost for all stays. Hospital admissions that originated in the ED accounted for 60.7% of all hospital stays for CVD. This was 41% higher than the overall rate of 43.1%; 3.3% of patients admitted to the hospital for CVD died in the hospital, which was significantly higher than the average in-hospital death rate of 2.1%.67
In 2004, coronary atherosclerosis was estimated to be responsible for 1.2 million hospital stays and was the most expensive condition treated. This condition resulted in >$44 billion in expenses. More than half of the hospital stays for coronary atherosclerosis were among patients who also received percutaneous coronary intervention or cardiac revascularization (coronary artery bypass graft; CABG) during their stay. Acute MI resulted in $31 billion of inpatient hospital charges for 695 000 hospital stays. The 1.1 million hospitalizations for CHF amounted to nearly $29 billion in hospital charges.69
In 2003, ≈48.3% of inpatient hospital stays for CVD were for women, who accounted for 42.8% of the national cost ($187 billion) associated with these conditions. Although only 40% of hospital stays for acute MI and coronary atherosclerosis were for women, more than half of all stays for nonspecific chest pain, CHF, and stroke were for women. There was no difference between men and women in hospitalizations for cardiac dysrhythmias.69
Circulatory disorders were the most frequent reason for admission to the hospital through the ED, accounting for 26.3% of all admissions through the ED. After pneumonia, the most common heart-related conditions (in descending order) were CHF, chest pain, hardening of the arteries, and heart attack, which together accounted for >15% of all admissions through the ED. Stroke and irregular heart beat ranked seventh and eighth, respectively.70
In 2004, nursing home residents had a primary diagnosis of CVD at admission (23.7%) and at the time of interview (25%). This was the leading primary diagnosis for these residents (NCHS, NNHS).67
Among current home health care patients in 2007, 18.3% had a primary diagnosis of CVD at admission and 62.9% had any diagnosis of CVD at the time of interview (NCHS, National Home and Hospice Care Survey [NHHCS] unpublished data).
Among patients discharged from hospice in 2007, 15.8% had a primary diagnosis of CVD at admission (NCHS, NHHCS unpublished data).
Operations and Procedures
In 2007, an estimated 6 846 000 inpatient cardiovascular operations and procedures were performed in the United States; 3.9 million were performed on males, and 2.9 million were performed on females (NHDS, NCHS, and NHLBI).
Cost
The estimated direct and indirect cost of CVD for 2007 is $286.6 billion (MEPS, AHRQ, and NHLBI).
In 2006, $32.7 billion in program payments were made to Medicare beneficiaries discharged from short-stay hospitals with a principal diagnosis of CVD. That was an average of $10 201 per discharge.71
Abbreviations Used in Chapter 3
- AED
automated external defibrillator
- AHA
American Heart Association
- AHRQ
Agency for Healthcare Research and Quality
- AIDS
acquired immune deficiency syndrome
- AP
angina pectoris
- ARIC
Atherosclerosis Risk in Communities study
- BMI
body mass index
- BP
blood pressure
- BRFSS
Behavioral Risk Factor Surveillance System
- CABG
cardiac revascularization (coronary artery bypass graft)
- CARDIA
Coronary Artery Risk Development in Young Adults
- CDC
Centers for Disease Control and Prevention
- CHD
coronary heart disease
- CHF
congestive heart failure
- CHS
Cardiovascular Health Study
- CLRD
chronic lower respiratory disease
- CPR
cardiopulmonary resuscitation
- CVD
cardiovascular disease
- DM
diabetes mellitus
- ED
emergency department
- EMS
emergency medical services
- FHS
Framingham Heart Study
- HBP
high blood pressure
- HD
heart disease
- HF
heart failure
- HIV
human immunodeficiency virus
- ICD-9
International Classification of Diseases, 9th Revision
- ICD-10
International Classification of Diseases, 10th Revision
- LDL
low-density lipoprotein
- MEPS
Medical Expenditure Panel Survey
- MESA
Multi-Ethnic Study of Atherosclerosis
- MI
myocardial infarction
- NAMCS
National Ambulatory Medical Care Survey
- NCHS
National Center for Health Statistics
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- NHANES
National Health and Nutrition Examination Survey
- NHDS
National Hospital Discharge Survey
- NHES
National Health Examination Survey
- NHIS
National Health Interview Survey
- NHHCS
National Home and Hospice Care Survey
- NHLBI
National Heart, Lung, and Blood Institute
- NIS
National Inpatient Sample
- NNHS
National Nursing Home Survey
- OPD
outpatient department
- PA
physical activity
- ROC
Resuscitation Outcomes Consortium
- RR
relative risk
- VF
ventricular fibrillation
- VT
ventricular tachycardia
References
- 1.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. [Accessed August 26, 2010];Vital Health Stat 10. 2010 (249) Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_249.pdf. [PubMed]
- 2.Barnes PM, Adams PF, Powell-Griner E. Advance Data From Vital and Health Statistics. 394. Hyattsville, Md: National Center for Health Statistics; 2008. Health Characteristics of the Asian Adult Population: United States, 200 –2006. [PubMed] [Google Scholar]
- 3.National Institutes of Health, National Heart, Lung, and Blood Institute. Incidence and Prevalence: 2006 Chart Book on Cardiovascular and Lung Diseases. Bethesda, Md: National Heart, Lung, and Blood Institute; 2006. [Accessed September 16, 2010]. Available at: http://www.nhlbi.nih.gov/resources/docs/06a_ip_chtbk.pdf. [Google Scholar]
- 4.Ali T, Jarvis B, O’Leary M. In: Strong Heart Study Data Book: A Report to American Indian Communities. Schaefer C, Fabsitz RR, editors. Rockville, Md: National Institutes of Health, National Heart, Lung, and Blood Institute; 2001. [Accessed September 27, 2010]. NIH publication 01-3285. Available at: http://www.nhlbi.nih.gov/resources/docs/shs_db.pdf. [Google Scholar]
- 5.Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PW, Wolf PA, Levy D. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 6.Xu J, Kochanek KD, Murphy S, Tejada-Vera B. Natl Vital Stat Rep. Vol. 58. Hyattsville, Md: National Center for Health Statistics; 2010. Deaths: final data for 2007; pp. 1–135. [PubMed] [Google Scholar]
- 7.National Center for Health Statistics. [Accessed July 12, 2010];Health Data Interactive. Available at: http://www.cdc.gov/nchs/hdi.htm.
- 8.National Center for Health Statistics. HIST290A: deaths for selected causes by 10-year age groups, race, and sex: death registration states, 1900–32, and United States, 1933–98. [Accessed September 27, 2010]; Available at: http://www.cdc.gov/nchs/nvss/mortality/hist290a.htm.
- 9.National Center for Health Statistics. GMWK292F: deaths for 358 selected causes by 5-year age groups, race, and sex: United States, 1999 –2007. [Accessed November 2, 2010]; Available at: http://www.cdc.gov/nchs/data/dvs/MortFinal2007_Worktable292F.pdf.
- 10.National Center for Health Statistics. Health, United States, 2009: With Special Feature on Medical Technology. Hyattsville, Md: National Center for Health Statistics; 2010. [Accessed August 30, 2010]. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. [PubMed] [Google Scholar]
- 11.Anderson RN. Hyattsville, Md: National Center for Health Statistics; 1999. [Accessed September 27, 2010]. U.S. Decennial Life Tables for 198–91, Vol. 1, No. 4: United States Life Tables Eliminating Certain Causes of Death. Available at: http://www.cdc.gov/nchs/data/lifetables/life89_1_4.pdf. [Google Scholar]
- 12.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980 –2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 13.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rhem J, Murray CJ, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Prevalence and most common causes of disability among adults—United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58:421–426. [PubMed] [Google Scholar]
- 15.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, Inter-American Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 16.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I Resuscitation Outcomes Consortium Investigators. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [published correction appears in JAMA. 2008;300:1763]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chugh SS, Jui J, Gunson K, Stecker EC, John BT, Thompson B, Ilias N, Vickers C, Dogra V, Daya M, Kron J, Zheng ZJ, Mensah G, McAnulty J. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate– based review in a large U.S. community. J Am Coll Cardiol. 2004;44:1268–1275. doi: 10.1016/j.jacc.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 18.Müller D, Agrawal R, Arntz HR. How sudden is sudden cardiac death? Circulation. 2006;114:1146–1150. doi: 10.1161/CIRCULATIONAHA.106.616318. [DOI] [PubMed] [Google Scholar]
- 19.Cobb LA, Fahrenbruch CE, Olsufka M, Copass MK. Changing incidence of out-of-hospital ventricular fibrillation, 1980–2000. JAMA. 2002;288:3008–3013. doi: 10.1001/jama.288.23.3008. [DOI] [PubMed] [Google Scholar]
- 20.Weisfeldt ML, Sitlani CM, Ornato JP, Rea T, Aufderheide TP, Davis D, Dreyer J, Hess EP, Jui J, Maloney J. Survival after application of automatic external defibrillators before arrival of the emergency medical system: evaluation in the resuscitation outcomes consortium population of 21 million. J Am Coll Cardiol. 2010;55:1713–1720. doi: 10.1016/j.jacc.2009.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Larsen MP, Eisenberg MS, Cummins RO, Hallstrom AP. Predicting survival from out-of-hospital cardiac arrest: a graphic model. Ann Emerg Med. 1993;22:1652–1658. doi: 10.1016/s0196-0644(05)81302-2. [DOI] [PubMed] [Google Scholar]
- 22.Valenzuela TD, Roe DJ, Cretin S, Spaite DW, Larsen MP. Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Circulation. 1997;96:3308–3313. doi: 10.1161/01.cir.96.10.3308. [DOI] [PubMed] [Google Scholar]
- 23.Swor RA, Jackson RE, Cynar M, Sadler E, Basse E, Boji B, Rivera-Rivera EJ, Maher A, Grubb W, Jacobson R. Bystander CPR, ventricular fibrillation, and survival in witnessed, unmonitored out-of-hospital cardiac arrest. Ann Emerg Med. 1995;25:780–784. doi: 10.1016/s0196-0644(95)70207-5. [DOI] [PubMed] [Google Scholar]
- 24.Holmberg M, Holmberg S, Herlitz J. Incidence, duration and survival of ventricular fibrillation in out-of-hospital cardiac arrest patients in Sweden. Resuscitation. 2000;44:7–17. doi: 10.1016/s0300-9572(99)00155-0. [DOI] [PubMed] [Google Scholar]
- 25.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O’Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y for the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics: 2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21–e181. doi: 10.1161/CIRCULATIONAHA.108.191261. [published correction appears in Circulation. 2009;119: e182]. [DOI] [PubMed] [Google Scholar]
- 26.Galea S, Blaney S, Nandi A, Silverman R, Vlahov D, Foltin G, Kusick M, Tunik M, Richmond N. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. Am J Epidemiol. 2007;166:534–543. doi: 10.1093/aje/kwm102. [DOI] [PubMed] [Google Scholar]
- 27.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 28.Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, Berg RA Resuscitation Outcomes Consortium Investigators. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009;119:1484–1491. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Annual Estimates of the Resident Population by Sex and Selected Age Groups for the United States: April 1, 2000 to July 1, 2009. [Accessed November 2, 2010];US Census data. Available at: http://www.census.gov/popest/national/asrh/NC-EST2009-sa.html.
- 30.Luckstead EF, Patel DR. Catastrophic pediatric sports injuries. Pediatr Clin North Am. 2002;49:581–591. doi: 10.1016/s0031-3955(02)00006-8. [DOI] [PubMed] [Google Scholar]
- 31.Maron BJ, Gohman TE, Aeppli D. Prevalence of sudden cardiac death during competitive sports activities in Minnesota high school athletes. J Am Coll Cardiol. 1998;32:1881–1884. doi: 10.1016/s0735-1097(98)00491-4. [DOI] [PubMed] [Google Scholar]
- 32.Lotfi K, White L, Rea T, Cobb L, Copass M, Yin L, Becker L, Eisenberg M. Cardiac arrest in schools. Circulation. 2007;116:1374–1379. doi: 10.1161/CIRCULATIONAHA.107.698282. [DOI] [PubMed] [Google Scholar]
- 33.Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009;119:1085–1092. doi: 10.1161/CIRCULATIONAHA.108.804617. [DOI] [PubMed] [Google Scholar]
- 34.Christian AH, Rosamond W, White AR, Mosca L. Nine-year trends and racial and ethnic disparities in women’s awareness of heart disease and stroke: an American Heart Association national study. J Womens Health (Larchmt) 2007;16:68–81. doi: 10.1089/jwh.2006.M072. [DOI] [PubMed] [Google Scholar]
- 35.Mosca L, Mochari H, Christian A, Berra K, Taubert K, Mills T, Burdick KA, Simpson SL. National study of women’s awareness, preventive action, and barriers to cardiovascular health. Circulation. 2006;113:525–534. doi: 10.1161/CIRCULATIONAHA.105.588103. [DOI] [PubMed] [Google Scholar]
- 36.Vanhecke TE, Miller WM, Franklin BA, Weber JE, McCullough PA. Awareness, knowledge, and perception of heart disease among adolescents. Eur J Cardiovasc Prev Rehabil. 2006;13:718–723. doi: 10.1097/01.hjr.0000214611.91490.5e. [DOI] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention. Racial/ethnic and socioeconomic disparities in multiple risk factors for heart disease and stroke: United States, 2003. MMWR Morb Mortal Wkly Rep. 2005;54:113–117. [PubMed] [Google Scholar]
- 38.Daviglus ML, Stamler J, Pirzada A, Yan LL, Garside DB, Liu K, Wang R, Dyer AR, Lloyd-Jones DM, Greenland P. Favorable cardiovascular risk profile in young women and long-term risk of cardiovascular and all-cause mortality. JAMA. 2004;292:1588–1592. doi: 10.1001/jama.292.13.1588. [DOI] [PubMed] [Google Scholar]
- 39.Stamler J, Stamler R, Neaton JD, Wentworth D, Daviglus ML, Garside D, Dyer AR, Liu K, Greenland P. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA. 1999;282:2012–2018. doi: 10.1001/jama.282.21.2012. [DOI] [PubMed] [Google Scholar]
- 40.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 41.Gregg EW, Cheng YJ, Cadwell BL, Imperatore G, Williams DE, Flegal KM, Narayan KM, Williamson DF. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293:1868–1874. doi: 10.1001/jama.293.15.1868. [published correction appears in JAMA. 2005;294: 182] [DOI] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. Sodium intake among adults—United States, 2005–2006. MMWR Morb Mortal Wkly Rep. 2010;59:746–749. [PubMed] [Google Scholar]
- 43.Hozawa A, Folsom AR, Sharrett AR, Chambless LE. Absolute and attributable risks of cardiovascular disease incidence in relation to optimal and borderline risk factors: comparison of African American with white subjects: Atherosclerosis Risk in Communities Study. Arch Intern Med. 2007;167:573–579. doi: 10.1001/archinte.167.6.573. [DOI] [PubMed] [Google Scholar]
- 44.Soni A. Personal Health Behaviors for Heart Disease Prevention Among the U.S. Adult Civilian Noninstitutionalized Population, 2004. Rockville, Md: Agency for Healthcare Research and Quality; 2007. Mar, [Accessed September 27, 2010]. MEPS Statistical Brief No. 165. Available at: http://meps.ahrq.gov/mepsweb/data_files/publications/st165/stat165.pdf. [Google Scholar]
- 45.Carnethon MR, Lynch EB, Dyer AR, Lloyd-Jones DM, Wang R, Garside DB, Greenland P. Comparison of risk factors for cardiovascular mortality in black and white adults. Arch Intern Med. 2006;166:1196–1202. doi: 10.1001/archinte.166.11.1196. [DOI] [PubMed] [Google Scholar]
- 46.Eamranond PP, Legedza AT, Diez-Roux AV, Kandula NR, Palmas W, Siscovick DS, Mukamal KJ. Association between language and risk factor levels among Hispanic adults with hypertension, hypercholesterolemia, or diabetes. Am Heart J. 2009;157:53–59. doi: 10.1016/j.ahj.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lloyd-Jones DM, Nam BH, D’Agostino RB, Sr, Levy D, Murabito JM, Wang TJ, Wilson PW, O’Donnell CJ. Parental cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults: a prospective study of parents and offspring. JAMA. 2004;291:2204–2211. doi: 10.1001/jama.291.18.2204. [DOI] [PubMed] [Google Scholar]
- 48.Murabito JM, Pencina MJ, Nam BH, D’Agostino RB, Sr, Wang TJ, Lloyd-Jones D, Wilson PW, O’Donnell CJ. Sibling cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults. JAMA. 2005;294:3117–3123. doi: 10.1001/jama.294.24.3117. [DOI] [PubMed] [Google Scholar]
- 49.Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA. 2007;297:611–619. doi: 10.1001/jama.297.6.611. [published correction appears in JAMA. 2007;297:1433] [DOI] [PubMed] [Google Scholar]
- 50.Assmann G, Cullen P, Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the Prospective Cardiovascular Münster (PROCAM) Study. Circulation. 2002;105:310–315. doi: 10.1161/hc0302.102575. [published correction appears in Circulation. 2002;105:900] [DOI] [PubMed] [Google Scholar]
- 51.Parikh NI, Hwang SJ, Larson MG, Cupples LA, Fox CS, Manders ES, Murabito JM, Massaro JM, Hoffmann U, O’Donnell CJ. Parental occurrence of premature cardiovascular disease predicts increased coronary artery and abdominal aortic calcification in the Framingham Offspring and Third Generation cohorts. Circulation. 2007;116:1473–1481. doi: 10.1161/CIRCULATIONAHA.107.705202. [DOI] [PubMed] [Google Scholar]
- 52.Nasir K, Budoff MJ, Wong ND, Scheuner M, Herrington D, Arnett DK, Szklo M, Greenland P, Blumenthal RS. Family history of premature coronary heart disease and coronary artery calcification: Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2007;116:619–626. doi: 10.1161/CIRCULATIONAHA.107.688739. [DOI] [PubMed] [Google Scholar]
- 53.Lee DS, Pencina MJ, Benjamin EJ, Wang TJ, Levy D, O’Donnell CJ, Nam BH, Larson MG, D’Agostino RB, Vasan RS. Association of parental heart failure with risk of heart failure in offspring. N Engl J Med. 2006;355:138–147. doi: 10.1056/NEJMoa052948. [DOI] [PubMed] [Google Scholar]
- 54.Friedlander Y, Siscovick DS, Arbogast P, Psaty BM, Weinmann S, Lemaitre RN, Raghunathan TE, Cobb LA. Sudden death and myocardial infarction in first degree relatives as predictors of primary cardiac arrest. Atherosclerosis. 2002;162:211–216. doi: 10.1016/s0021-9150(01)00701-8. [DOI] [PubMed] [Google Scholar]
- 55.Centers for Disease Control and Prevention (CDC) Awareness of family health history as a risk factor for disease: United States, 2004. MMWR Morb Mortal Wkly Rep. 2004;53:1044–1047. [PubMed] [Google Scholar]
- 56.Berry JD, Liu K, Folsom AR, Lewis CE, Carr JJ, Polak J, Shea SJ, Sidney S, O’Leary DH, Chan C, Lloyd-Jones DM. Prevalence and progression of subclinical atherosclerosis in younger adults with low short-term but high lifetime estimated risk for cardiovascular disease: the Coronary Artery Risk Development in Young Adults Study and Multi-Ethnic Study of Atherosclerosis. Circulation. 2009;119:382–389. doi: 10.1161/CIRCULATIONAHA.108.800235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Terry DF, Pencina MJ, Vasan RS, Murabito JM, Wolf PA, Hayes MK, Levy D, D’Agostino RB, Benjamin EJ. Cardiovascular risk factors predictive for survival and morbidity-free survival in the oldest-old Framingham Heart Study participants. J Am Geriatr Soc. 2005;53:1944–1950. doi: 10.1111/j.1532-5415.2005.00465.x. [DOI] [PubMed] [Google Scholar]
- 58.Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med. 2000;343:16–22. doi: 10.1056/NEJM200007063430103. [DOI] [PubMed] [Google Scholar]
- 59.Wright JD, Hirsch R, Wang CY. NCHS Data Brief 17. Hyattsville, Md: National Center for Health Statistics; 2009. One-third of U.S. adults embraced most heart healthy behaviors in 1999–2002. [PubMed] [Google Scholar]
- 60.Lloyd-Jones DM, Dyer AR, Wang R, Daviglus ML, Greenland P. Risk factor burden in middle age and lifetime risks for cardiovascular and non-cardiovascular death (Chicago Heart Association Detection Project in Industry) Am J Cardiol. 2007;99:535–540. doi: 10.1016/j.amjcard.2006.09.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, van Staveren WA. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004;292:1433–1439. doi: 10.1001/jama.292.12.1433. [DOI] [PubMed] [Google Scholar]
- 62.Mensah GA, Brown DW, Croft JB, Greenlund KJ. Major coronary risk factors and death from coronary heart disease: baseline and follow-up mortality data from the Second National Health and Nutrition Examination Survey (NHANES II) Am J Prev Med. 2005;29(suppl 1):68–74. doi: 10.1016/j.amepre.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 63.Daviglus ML, Liu K, Pirzada A, Yan LL, Garside DB, Feinglass J, Guralnik JM, Greenland P, Stamler J. Favorable cardiovascular risk profile in middle age and health-related quality of life in older age. Arch Intern Med. 2003;163:2460–2468. doi: 10.1001/archinte.163.20.2460. [DOI] [PubMed] [Google Scholar]
- 64.Daviglus ML, Liu K, Greenland P, Dyer AR, Garside DB, Manheim L, Lowe LP, Rodin M, Lubitz J, Stamler J. Benefit of a favorable cardiovascular risk-factor profile in middle age with respect to Medicare costs. N Engl J Med. 1998;339:1122–1129. doi: 10.1056/NEJM199810153391606. [DOI] [PubMed] [Google Scholar]
- 65.Centers for Disease Control and Prevention. National Center for Health Statistics. 2008 National Ambulatory Medical Care Survey. Hyattsville, Md: 2010. [Accessed August 31, 2010]. Unpublished data. For methodology, see National Center for Health Statistics. Public Use Data File Documentation: 2008 National Ambulatory Medical Care Survey. Available at: http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm. [Google Scholar]
- 66.Centers for Disease Control and Prevention. National Center for Health Statistics. 2008 National Hospital Ambulatory Medical Care Survey. Hyattsville, MD: 2010. [Accessed August 31, 2010]. Unpublished data. For methodology, see National Center for Health Statistics. Public Use Data File Documentation: 2008 National Hospital Ambulatory Medical Care Survey. Available at: http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm. [Google Scholar]
- 67.Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. The National Nursing Home Survey: 2004 overview. Vital Health Stat 13. 2009;(167):1–155. [PubMed] [Google Scholar]
- 68. Deleted post-production. [Google Scholar]
- 69.Russo CA, Andrews RM. Rockville, Md: Agency for Healthcare Research and Quality; 2006. Sep, [Accessed September 27, 2010]. The National Hospital Bill: The Most Expensive Conditions, by Payer 2004. HCUP Statistical Brief No. 13. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb13.pdf. [PubMed] [Google Scholar]
- 70.Elixhauser A, Jiang HJ. Rockville, Md: Agency for Healthcare Research and Quality; 2006. May, [Accessed September 27, 2010]. Hospitalizations for Women With Circulatory Disease, 2003. HCUP Statistical Brief No. 5. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb5.pdf. [PubMed] [Google Scholar]
- 71.Centers for Medicare & Medicaid Services. Health Care Financing Review: Medicare & Medicaid Statistical Supplement. Baltimore, Md: Centers for Medicare and Medicaid Services; 2005. [Accessed September 27, 2010]. Table 5.5: Discharges, Total Days of Care, and Program Payments for Medicare Beneficiaries Discharged from Short-Stay Hospitals, by Principal Diagnoses Within Major Diagnostic Classifications (MDCs): Calendar Year 2006. Available at: http://www.cms.hhs.gov/MedicareMedicaidStatSupp/downloads/2007Table5.5b.pdf. [Google Scholar]
- 72.D’Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
4. Subclinical Atherosclerosis
See Table 4-1 and Charts 4-1 through 4-6.
Table 4-1.
CAC Scores for the 75th Percentile of Men and Women of Different Race/Ethnic Groups, at Specified Ages
| 75th Percentile CAC Scores* | ||||
|---|---|---|---|---|
| Age, y | Black | Chinese | Hispanic | White |
| Women | ||||
| 45 | 0 | 0 | 0 | 0 |
| 55 | 0 | 2 | 0 | 1 |
| 65 | 26 | 45 | 19 | 54 |
| 75 | 138 | 103 | 116 | 237 |
| Men | ||||
| 45 | 0 | 3 | 0 | 0 |
| 55 | 15 | 34 | 27 | 68 |
| 65 | 95 | 121 | 141 | 307 |
| 75 | 331 | 229 | 358 | 820 |
CAC indicates coronary artery calcification.
The 75th percentile CAC score is the score at which 75% of people of the same age, sex, and race have a score at or below this level, and 25% of people of the same age, sex, and race have a higher score.
Source: MESA CAC Tools Web site: http://www.mesa-nhlbi.org/Calcium/input.aspx.
Chart 4-1.
Prevalence (%) of coronary calcium: US adults 33 to 45 years of age. P<0.0001 across race-sex groups. Data derived from Loria et al.4
Chart 5-2.
Annual number of adults having diagnosed heart attack or fatal coronary heart disease (CHD) by age and sex (Atherosclerosis Risk in Communities Surveillance: 1987–2004 and Cardiovascular Health Study: 1989–2004). These data include myocardial infarction (MI) and fatal coronary heart disease but not silent MI. Source: National Heart, Lung, and Blood Institute.
Atherosclerosis, a systemic disease process in which fatty deposits, inflammation, cells, and scar tissue build up within the walls of arteries, is the underlying cause of the majority of clinical cardiovascular events. Individuals who develop atherosclerosis tend to develop it in a number of different types of arteries (large and small arteries and those feeding the heart, brain, kidneys, and extremities), although they may have much more in some artery types than others. In recent decades, advances in imaging technology have allowed for improved ability to detect and quantify atherosclerosis at all stages and in multiple different vascular beds. Two modalities, computed tomography (CT) of the chest for evaluation of coronary artery calcification (CAC) and B-mode ultrasound of the neck for evaluation of carotid artery intima-media thickness (IMT), have been used in large studies with outcomes data and may help define the burden of atherosclerosis in individuals before they develop clinical events such as heart attack or stroke. Another commonly used method for detecting and quantifying atherosclerosis in the peripheral arteries is the ankle-brachial index, which is discussed in Chapter 10. Data on cardiovascular outcomes are starting to emerge for additional modalities for measuring subclinical disease, including brachial artery reactivity testing, aortic and carotid magnetic resonance imaging (MRI), and tonometric methods of measuring vascular compliance or microvascular reactivity. Further research may help to define the role of these techniques in cardiovascular risk assessment. Some guidelines have recommended screening for subclinical atherosclerosis, especially by CAC, or IMT may be appropriate in people at intermediate risk for heart disease (eg, 10-year estimated risk of 10% to 20%) but not for lower-risk general population screening or for people with preexisting HD, DM, or other high-risk conditions.1,2
Coronary Artery Calcification
Background
CAC is a measure of the burden of atherosclerosis in the heart arteries and is measured by CT. Other parts of the atherosclerotic plaque, including fatty (eg, cholesterol-rich components) and fibrotic components, often accompany CAC and may be present even in the absence of CAC.
The presence of any CAC, which indicates that at least some atherosclerotic plaque is present, is defined by an Agatston score >0. Clinically significant plaque, frequently an indication for more aggressive risk factor management, is often defined by a score ≥100 or a score ≥75th percentile for one’s age and sex. A score ≥400 has been noted to be an indication for further diagnostic evaluation (eg, exercise testing or myocardial perfusion imaging) for coronary artery disease (CAD).
Prevalence
The NHLBI’s FHS measured CAC in 3238 white adults from <45 years of age to ≥75 years of age.3
Overall, 32.0% of women and 52.9% of men had prevalent CAC, defined as age-specific cut points >90th percentile in a healthy referent sample.
Among FHS participants at intermediate risk, 58% of women and 64% of men had prevalent CAC.
- The NHLBI’s Coronary Artery Risk Development in Young Adults (CARDIA) study measured CAC in 3043 black and white adults 33 to 45 years of age (at the CARDIA year 15 examination).4
-
—Overall, 15.0% of men and 5.1% of women, 5.5% of those 33 to 39 years of age and 13.3% of those 40 to 45 years of age, had prevalent CAC. Overall, 1.6% of subjects had a score that exceeded 100.
-
—Chart 4-1 shows the prevalence of CAC by ethnicity and sex. The prevalence of CAC was lower in black men than in white men but was similar in black and white women at these ages.
-
—
- The NHLBI’s MESA study measured CAC in 6814 subjects 45 to 84 years of age, including white (n = 2619), black (n = 1898), Hispanic (n = 1494), and Chinese (n = 803) men and women.5
-
—Chart 4-2 shows the prevalence of CAC by sex and ethnicity.
-
—The prevalence and 75th percentile levels of CAC were highest in white men and lowest in black and Hispanic women. Significant ethnic differences persisted after adjustment for risk factors, with the RR of coronary calcium being 22% less in blacks, 15% less in Hispanics, and 8% less in Chinese than in whites.
-
—Table 4-1 shows the 75th percentile levels of CAC by sex and race at selected ages. These might be considered cut points above which more aggressive efforts to control risk factors (eg, elevated cholesterol or BP) could be implemented and/or at which treatment goals might be more aggressive (eg, LDL cholesterol <100 mg/dL instead of <130 mg/dL).
-
—
Chart 4-2.
Prevalence (%) of coronary calcium: US adults 45 to 84 years of age. P<0.0001 across ethnic groups in both men and women. Data derived from Bild et al.5
CAC and Incidence of Coronary Events
- The NHLBI’s MESA study recently reported on the association of CAC scores with first CHD events over a median follow-up of 3.9 years among a population-based sample of 6722 men and women (39% white, 27% black, 22% Hispanic, and 12% Chinese).6
-
—Chart 4-3 shows the relative risks (RRs) or hazard ratios (HRs) associated with CAC scores of 1 to 100, 101 to 300, and >300 compared with those without CAC (score=0), after adjustment for standard risk factors. People with CAC scores of 1 to 100 had ≈4 times greater risk and those with CAC scores >100 were 7 to 10 times more likely to experience a coronary event than those without CAC.
-
—CAC provided similar predictive value for coronary events in whites, Chinese, blacks, and Hispanics (HRs ranging from 1.15 to 1.39 for each doubling of coronary calcium).
-
—
In another report of a community-based sample, not referred for clinical reasons, the South Bay Heart Watch examined CAC in 1461 adults (average age 66 years) with coronary risk factors, with a median of 7.0 years of follow-up.7
Chart 4-4 shows the HRs associated with increasing CAC scores (relative to CAC=0 and <10% risk category) in low-risk (<10%), intermediate-risk (10% to 15% and 16% to 20%), and high-risk (>20%) Framingham Risk Score (FRS) categories of estimated risk for CHD in 10 years. Increasing CAC scores further predicted risk in intermediate- and high-risk groups.
In a study of healthy adults 60 to 72 years of age who were free of clinical CAD, predictors of the progression of CAC were assessed. Predictors tested included age, sex, race/ethnicity, smoking status, BMI, family history of CAD, C-reactive protein, several measures of DM, insulin levels, BP, and lipids. Insulin resistance, in addition to the traditional cardiac risk factors, independently predicts progression of CAC.8 Clinically, however, it is not yet recommended to conduct serial scanning of CAC to measure effects of therapeutic interventions.
It is noteworthy that, as recently demonstrated in the MESA study in 5878 subjects with a median of 5.8 years of follow-up, the addition of CAC to standard risk factors resulted in significant improvement of classification of risk for incident CHD events, placing 77% of people in the highest or lowest risk categories compared with 69% based on risk factors alone. Moreover, an additional 23% of those who experienced events were reclassified as high risk and 13% with events were reclassified as low risk.9
Chart 4-3.
Hazard ratios for coronary heart disease (CHD) events associated with coronary calcium scores: US adults 45 to 84 years of age (reference group coronary artery calcification = 0). All hazard ratios P<0.0001. Major CHD events included myocardial infarction and death due to CHD; any CHD events included major CHD events plus definite angina or definite or probable angina followed by revascularization. Data derived from Detrano et al.6
Chart 4-4.
Hazard ratios for coronary heart disease events associated with coronary calcium scores: US adults (reference group coronary artery calcification (CAC) = 0 and Framingham Risk Score <10%). Coronary heart disease events included nonfatal myocardial infarction and death due to coronary heart disease. Data derived from Greenland et al.7
Carotid IMT
Background
Carotid IMT measures the thickness of 2 layers (the intima and media) of the wall of the carotid arteries, the largest conduits of blood going to the brain. Carotid IMT is thought to be an even earlier manifestation of atherosclerosis than CAC, because thickening precedes the development of frank atherosclerotic plaque. Carotid IMT methods are still being refined, so it is important to know which part of the artery was measured (common carotid, internal carotid, or bulb) and whether near and far walls were both measured. This information can affect the average-thickness measurement that is usually reported.
Unlike CAC, everyone has some thickness to their arteries, but people who develop atherosclerosis have greater thickness. Ultrasound of the carotid arteries can also detect plaques and determine the degree of narrowing of the artery that they may cause. Epidemiological data, including the data discussed below, have indicated that high-risk levels might be considered as those in the highest quartile or quintile for one’s age and sex, or ≥1 mm.
Although ultrasound is commonly used to diagnose plaque in the carotid arteries in people who have had strokes or who have bruits (sounds of turbulence in the artery), guidelines are limited as to screening of asymptomatic people for carotid IMT to quantify atherosclerosis or predict risk. However, some organizations have recognized that carotid IMT measurement by B-mode ultrasonography may provide an independent assessment of coronary risk.10
Prevalence and Association With Incident Cardiovascular Events
- The Bogalusa Heart Study measured carotid IMT in 518 black and white men and women at a mean age of 32±3 years. These men and women were healthy but overweight.11
-
—The mean values of carotid IMT for the different segments are shown in Chart 4-5 by sex and race. Men had significantly higher carotid IMT in all segments than women, and blacks had higher common carotid and carotid bulb IMTs than whites.
-
—Even at this young age, after adjustment for age, race, and sex, carotid IMT was associated significantly and positively with waist circumference, SBP, DBP, and LDL cholesterol. Carotid IMT was inversely correlated with high-density lipoprotein (HDL) cholesterol levels. Participants with greater numbers of adverse risk factors (0, 1, 2, 3, or more) had stepwise increases in mean carotid IMT levels.
-
—
In a subsequent analysis, the Bogalusa investigators examined the association of risk factors measured since childhood with carotid IMT measured in these young adults.12 Higher BMI and LDL cholesterol levels measured at 4 to 7 years of age were associated with increased risk for being >75th percentile for carotid IMT in young adulthood. Higher SBP and LDL cholesterol and lower HDL cholesterol in young adulthood were also associated with having high carotid IMT. These data highlight the importance of adverse risk factor levels in early childhood and young adulthood in the early development of atherosclerosis.
Among both women and men in MESA, blacks had the highest common carotid IMT, but they were similar to whites and Hispanics in internal carotid IMT. Chinese participants had the lowest carotid IMT, in particular, in the internal carotid, of the 4 ethnic groups (Chart 4-6).
- The NHLBI’s CHS reported follow-up of 4476 men and women ≥65 years of age (mean age 72 years) who were free of CVD at baseline.13
-
—Mean maximal common carotid IMT was 1.03± 0.20 mm, and mean internal carotid IMT was 1.37±0.55 mm.
-
—After a mean follow-up of 6.2 years, those with maximal carotid IMT in the highest quintile had a 4- to 5-fold greater risk for incident heart attack or stroke than those in the bottom quintile. After adjustment for other risk factors, there was still a 2- to 3-fold greater risk for the top versus the bottom quintile.
-
—
More recently, the Atherosclerosis Risk in Communities Study has demonstrated in 13 145 subjects the addition of carotid IMT combined with identification of plaque presence or absence to traditional risk factors to reclassify risk in 23% of individuals overall, with a net reclassification improvement of 9.9% (with most classified to a lower risk group). There was a modest, but statistically significant improvement in the area under the receiver-operator characteristic curve from 0.742 to 0.755.14
Chart 4-5.
Mean values of carotid intima-media thickness (IMT) for different carotid artery segments in younger adults by race and sex (Bogalusa Heart Study). Data derived from Urbina et al.11
Chart 4-6.
Mean values of carotid intima-media thickness (IMT) for different carotid artery segments in older adults, by race. Data derived from Manolio et al.15
CAC and Carotid IMT
- In the NHLBI’s MESA study of white, black, Chinese, and Hispanic adults 45 to 84 years of age, carotid IMT and CAC were found to be commonly associated, but patterns of association differed somewhat by sex and race.15
- — Common and internal carotid IMT were greater in women and men who had CAC than in those who did not, regardless of ethnicity.
-
—Overall, CAC prevalence and scores were associated with carotid IMT, but associations were somewhat weaker in blacks than in other ethnic groups.
-
—In general, blacks had the thickest carotid IMT of all 4 ethnic groups, regardless of the presence of CAC.
-
—Common carotid IMT differed little by race/ethnicity in women with any CAC, but among women with no CAC, IMT was higher among blacks (0.86 mm) than in the other 3 groups (0.76 to 0.80 mm).
- In a more recent analysis from the NHLBI’s MESA study, the investigators reported on follow-up of 6698 men and women in 4 ethnic groups over 5.3 years and compared the predictive utility of carotid IMT and CAC.16
-
—CAC was associated more strongly than carotid IMT with the risk of incident CVD.
-
—After adjustment for each other (CAC score and IMT) and for traditional CVD risk factors, the HR for CVD increased 2.1-fold for each 1-standard deviation (SD) increment of log-transformed CAC score versus 1.3-fold for each 1-SD increment of the maximum carotid IMT.
-
—For CHD events, the HRs per 1-SD increment increased 2.5-fold for CAC score and 1.2-fold for IMT.
-
—A receiver operating characteristic curve analysis also suggested that CAC score was a better predictor of incident CVD than was IMT, with areas under the curve of 0.81 versus 0.78, respectively.
-
—Investigators from the NHLBI’s CARDIA and MESA studies examined the burden and progression of subclinical atherosclerosis among adults <50 years of age. Ten-year and lifetime risks for CVD were estimated for each participant, and the young adults were stratified into 3 groups: (1) those with low 10-year (<10%) and low lifetime (<39%) predicted risk for CVD; (2) those with low 10-year (<10%) but high lifetime (≥39%) predicted risk; and (3) those with high 10-year risk (>10%). The latter group had the highest burden and greatest progression of subclinical atherosclerosis. Given the young age of those studied, ≈90% of participants were at low 10-year risk, but of these, half had high predicted lifetime risk. Compared with those with low short-term/low lifetime predicted risks, those with low short-term/high lifetime predicted risk had significantly greater burden and progression of CAC and significantly greater burden of carotid IMT, even at these younger ages. These data confirm the importance of early exposure to risk factors for the onset and progression of subclinical atherosclerosis.17
-
—
Measures of Vascular Function and Incident CVD Events
Background
Measures of arterial tonometry (stiffness) are based on the concept that pulse pressure has shown to be an important risk factor for CVD. Arterial tonometry offers the ability to directly and noninvasively measure central pulse wave velocity in the thoracic and abdominal aorta.
Brachial flow-mediated dilation (FMD) is a marker for nitric oxide release from the endothelium that can be measured using ultrasound. Impaired FMD is an early marker of CVD.
Recommendations have not been specific, however, as to which, if any, measures of vascular function may be useful for CVD risk stratification in selected patient subgroups.
Arterial Tonometry and CVD
The Rotterdam Study measured arterial stiffness in 2835 elderly participants (mean age 71 years18). They found that as aortic pulse wave velocity increased, the risk of coronary heart disease was 1.72 (second versus first tertile) and 2.45 (third versus first tertile). Results remained robust even after accounting for carotid IMT, ankle-brachial index, and pulse pressure.
A study from Denmark measured 1678 individuals aged 40 to 70 years, and found that aortic pulse wave velocity increased CVD risk by 16% to 20%.19
The FHS measured several indices of arterial stiffness, including pulse wave velocity wave reflection and central pulse pressure.20 They found that not only was higher pulse wave velocity associated with a 48% increased risk of incident CVD events, but pulse wave velocity additionally improved CVD risk prediction (integrated discrimination index of 0.7%, P<0.05).
Flow-Mediated Dilation and CVD
The MESA study measured FMD in 3026 participants (mean age 61 years) that were free of CVD. As FMD increased (ie, improved brachial function), the risk of CVD was 16% lower.21 FMD also improved CVD risk prediction, compared with the FRS, by improving net reclassification by 29%.
Abbreviations Used in Chapter 4
- BMI
body mass index
- BP
blood pressure
- CAC
coronary artery calcification
- CAD
coronary artery disease
- CARDIA
Coronary Artery Risk Development in Young Adults
- CHD
coronary heart disease
- CHS
Cardiovascular Health Study
- CT
computed tomography
- CVD
cardiovascular disease
- DBP
diastolic blood pressure
- DM
diabetes mellitus
- FHS
Framingham Heart Study
- FMD
flow-mediated dilation
- FRS
Framingham Risk Score
- HDL
high-density lipoprotein
- HD
heart disease
- HR
hazard ratio
- IMT
intima-media thickness
- LDL
low-density lipoprotein
- MESA
Multi-Ethnic Study of Atherosclerosis
- mg/dL
milligrams per deciliter
- MRI
magnetic resonance imaging
- NHLBI
National Heart, Lung, and Blood Institute
- RR
relative risk
- SBP
systolic blood pressure
- SD
standard deviation
- 1.Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, Guerci AD, Lima JA, Rader DJ, Rubin GD, Shaw LJ, Wiegers SE. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 2.Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, Lauer MS, Post WS, Raggi P, Redberg RF, Rodgers GP, Shaw LJ, Taylor AJ, Weintraub WS. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) Circulation. 2007;115:402–426. doi: 10.1161/CIRCULATIONAHA..107.181425. [DOI] [PubMed] [Google Scholar]
- 3.Hoffmann U, Massaro JM, Fox CS, Manders E, O’Donnell CJ. Defining normal distributions of coronary artery calcium in women and men (from the Framingham Heart Study) Am J Cardiol. 2008;102:1136–1141. doi: 10.1016/j.amjcard.2008.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loria CM, Liu K, Lewis CE, Hulley SB, Sidney S, Schreiner PJ, Williams OD, Bild DE, Detrano R. Early adult risk factor levels and subsequent coronary artery calcification: the CARDIA Study. J Am Coll Cardiol. 2007;49:2013–2020. doi: 10.1016/j.jacc.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 5.Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, Ouyang P, Jackson S, Saad MF. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111:1313–1320. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 6.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 7.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 8.Lee KK, Fortmann SP, Fair JM, Iribarren C, Rubin GD, Varady A, Go AS, Quertermous T, Hlatky MA. Insulin resistance independently predicts the progression of coronary artery calcification. Am Heart J. 2009;157:939–945. doi: 10.1016/j.ahj.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 9.Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, Greenland P. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610–1616. doi: 10.1001/jama.2010.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith SC, Jr, Greenland P, Grundy SM. AHA Conference Proceedings. Prevention conference V: beyond secondary prevention: identifying the high-risk patient for primary prevention: executive summary. American Heart Association. Circulation. 2000;101:111–116. doi: 10.1161/01.cir.101.1.111. [DOI] [PubMed] [Google Scholar]
- 11.Urbina EM, Srinivasan SR, Tang R, Bond M, Kieltyka L, Berenson GS Bogalusa Heart Study. Impact of multiple coronary risk factors on the intima-media thickness of different segments of carotid artery in healthy young adults (The Bogalusa Heart Study) Am J Cardiol. 2002;90:953–958. doi: 10.1016/s0002-9149(02)02660-7. [DOI] [PubMed] [Google Scholar]
- 12.Li S, Chen W, Srinivasan SR, Bond MG, Tang R, Urbina EM, Berenson GS. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA. 2003;290:2271–2276. doi: 10.1001/jama.290.17.2271. [published correction appears in JAMA. 2003;290:2943]. [DOI] [PubMed] [Google Scholar]
- 13.O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 14.Nambi V, Chambless L, Folsom AR, He M, Hu Y, Mosley T, Volcik K, Boerwinkle E, Ballantyne CM. Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: the ARIC (Atherosclerosis Risk In Communities) study. J Am Coll Cardiol. 2010;55:1600–1607. doi: 10.1016/j.jacc.2009.11.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manolio TA, Arnold AM, Post W, Bertoni AG, Schreiner PJ, Sacco RL, Saad MF, Detrano RL, Szklo M. Ethnic differences in the relationship of carotid atherosclerosis to coronary calcification: the Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2008;197:132–138. doi: 10.1016/j.atherosclerosis.2007.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Folsom AR, Kronmal RA, Detrano RC, O’Leary DH, Bild DE, Bluemke DA, Budoff MJ, Liu K, Shea S, Szklo M, Tracy RP, Watson KE, Burke GL. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med. 2008;168:1333–1339. doi: 10.1001/archinte.168.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berry JD, Liu K, Folsom AR, Lewis CE, Carr JJ, Polak JF, Shea S, Sidney S, O’Leary DH, Chan C. Prevalence and progression of sub-clinical atherosclerosis in younger adults with low short-term but high lifetime estimated risk for cardiovascular disease: the coronary artery risk development in young adults study and multi-ethnic study of atherosclerosis. Circulation. 2009;119:382–389. doi: 10.1161/CIRCULATIONAHA.108.800235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mattace-Raso FU, van der Cammen TJ, Hofman A, van Popele NM, Bos ML, Schalekamp MA, Asmar R, Reneman RS, Hoeks AP, Breteler M, Witteman JC. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation. 2006;113:657–663. doi: 10.1161/CIRCULATIONAHA.105.555235. [DOI] [PubMed] [Google Scholar]
- 19.Willum Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, Jeppesen J. Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation. 2006;113:664–670. doi: 10.1161/CIRCULATIONAHA.105.579342. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D, Benjamin EJ. Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation. 2010;121:505–511. doi: 10.1161/CIRCULATIONAHA.109.886655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yeboah J, Folsom AR, Burke GL, Johnson C, Polak JF, Post W, Lima JA, Crouse JR, Herrington DM. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the Multi-Ethnic Study of Atherosclerosis. Circulation. 2009;120:502–509. doi: 10.1161/CIRCULATIONAHA.109.864801. [DOI] [PMC free article] [PubMed] [Google Scholar]
5. Coronary Heart Disease, Acute Coronary Syndrome, and Angina Pectoris
Coronary Heart Disease
ICD-9 410 to 414, 429.2; ICD-10 I20 to I25; see Glossary (Chapter 24) for details and definitions. See Tables 5-1 and 5-2. See Charts 5-1 through 5-8.
Table 5-1.
Coronary Heart Disease
| Population Group | Prevalence, CHD, 2008 Age ≥20 y |
Prevalence, MI, 2008 Age ≥20 y |
New and Recurrent MI and Fatal CHD, Age ≥35 y |
New and Recurrent MI, Age ≥35 y |
Mortality,* CHD, 2007, All Ages |
Mortality,* MI, 2007, All Ages |
Hospital Discharges, CHD, 2007, All Ages |
|---|---|---|---|---|---|---|---|
| Both sexes | 16 300 000 (7.0%) | 7 900 000 (3.1%) | 1 255 000 | 935 000 | 406 351 | 132 968 | 1 572 000 |
| Males | 8 800 000 (8.3%) | 4 800 000 (4.3%) | 740 000 | 565 000 | 216 050 (53.2%)† | 71 712 (53.9%)† | 965 000 |
| Females | 7 500 000 (6.1%) | 3 100 000 (2.2%) | 515 000 | 370 000 | 190 301 (46.8%)† | 61 256 (46.1%)† | 607 000 |
| NH white males | 8.5% | 4.3% | 675 000‡ | … | 189 056 | 63 011 | … |
| NH white females | 5.8% | 2.1% | 445 000‡ | … | 165 425 | 52 889 | … |
| NH black males | 7.9% | 4.3% | 70 000‡ | … | 21 768 | 6997 | … |
| NH black females | 7.6% | 2.2% | 65 000‡ | … | 20 911 | 7100 | … |
| Mexican American males | 6.3% | 3.0% | … | … | … | … | … |
| Mexican American females | 5.6% | 1.1% | … | … | … | … | … |
| Hispanic or Latino,§ age ≥18 y | 5.8% | … | … | … | … | … | … |
| Asian,§ age ≥18 y | 3.9% | … | … | … | 7414 | 2380 | … |
| American Indian/ Alaska Native,§ age ≥18 y | 4.1%‖ | … | … | … | 1777 | 591 | … |
CHD indicates coronary heart disease; MI, myocardial infarction; NH, non-Hispanic.
CHD includes people who responded “yes” to at least one of the questions in “Has a doctor or other health professional ever told you had coronary heart disease, angina or angina pectoris, heart attack, or myocardial infarction?” Those who answered “no” but were diagnosed with Rose angina are also included. Ellipses indicate data not available. Sources: Prevalence: National Health and Nutrition Examination Survey 2005–2008 (National Center for Health Statistics) and National Heart, Lung, and Blood Institute. Percentages for racial/ethnic groups are age-adjusted for Americans ≥20 years of age. Age-specific percentages are extrapolated to the 2008 US population estimates. These data are based on self-reports. Incidence: Atherosclerosis Risk in Communities study (1987–2004), National Heart, Lung, and Blood Institute. Mortality: National Center for Health Statistics (these data represent underlying cause of death only). Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics (data include those inpatients discharged alive, dead, or status unknown).
Mortality data are for whites and blacks and include Hispanics.
These percentages represent the portion of total CHD mortality that is for males versus females.
Estimates include Hispanics and non-Hispanics. Estimates for whites include other nonblack races.
National Health Interview Study, National Center for Health Statistics 2009; data are weighted percentages for Americans ≥18 years of age.1
Figure not considered reliable.
Table 5-2.
Angina Pectoris
| Population Group | Prevalence, 2008 Age ≥20 y |
Incidence of Stable AP, Age ≥45 y |
Hospital Discharges, 2007,* All Ages |
|---|---|---|---|
| Both sexes | 9 000 000 (3.9%) | 500 000 | 47 000 |
| Males | 4 000 000 (3.8%) | 320 000 | 28 000 |
| Females | 5 000 000 (4.0%) | 180 000 | 19 000 |
| NH white males | 3.8% | … | … |
| NH white females | 3.7% | … | … |
| NH black males | 3.3% | … | … |
| NH black females | 5.6% | … | … |
| Mexican American males | 3.6% | … | … |
| Mexican American females | 3.7% | … | … |
AP indicates angina pectoris; NH, non-Hispanic.
AP is chest pain or discomfort that results from insufficient blood flow to the heart muscle. Stable AP is predictable chest pain on exertion or under mental or emotional stress. The incidence estimate is for AP without myocardial infarction. Ellipses indicate data not available.
Sources: Prevalence: National Health and Nutrition Examination Survey 2005–2008 (National Center for Health Statistics) and National Heart, Lung, and Blood Institute; percentages for racial/ethnic groups are age adjusted for Americans ≥20 years of age. Angina pectoris includes persons who either answered “yes” to the question of ever having angina or angina pectoris of were diagnosed with Rose angina. Estimates from National Health and Nutrition Examination Survey 2005–2008 (National Center for Health Statistics) were applied to 2008 population estimates (≥20 years of age). Incidence: AP uncomplicated by a myocardial infarction or with no myocardial infarction (Framingham Heart Study 1980 to 2001–2003 of the original cohort and 1980 to 1998–2001 of the Offspring Cohort, National Heart, Lung, and Blood Institute). Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics; data include those inpatients discharged alive, dead, or status unknown.
There were 102 000 days of care for discharges with AP form short-stay hospitals in 2007.
Chart 5-1.
Prevalence of coronary heart disease by age and sex (National Health and Nutrition Examination Survey: 2005–2008). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 5-8.
Prevalence of low coronary heart disease risk, overall and by sex (National Health and Nutrition Examination Survey: 1971–2006). Low risk is defined as systolic blood pressure <120 mm Hg and diastolic blood pressure <80 mm Hg; cholesterol <200 mg/dL; body mass index <25 kg/m2; currently not smoking cigarettes and no prior myocardial infarction or diabetes mellitus. Source: Personal communication with the National Heart, Lung, and Blood Institute, June 28, 2007.
Prevalence
- On the basis of data from NHANES 2005 to 2008 (NCHS; unpublished NHLBI tabulation (Table 5-1; Chart 5-1), an estimated 16 300 000 Americans ≥20 years of age have CHD:
-
—Total CHD prevalence is 7.0% in US adults ≥20 years of age. CHD prevalence is 8.3% for men and 6.1% for women.
-
—Among non-Hispanic whites, CHD prevalence is 8.5% for men and 5.8% for women.
-
—Among non-Hispanic blacks, CHD prevalence is 7.9% for men and 7.6% for women.
-
—Among Mexican Americans, CHD prevalence is 6.3% for men and 5.6% for women.
-
—Among Hispanic or Latino individuals ≥18 years of age, CHD prevalence is 5.8% (2009 NHIS, NCHS).1
-
—Among American Indians/Alaska Natives ≥18 years of age, it is estimated that 4.1% have CHD (estimate considered unreliable), and among Asians ≥18 years of age, it is 3.9% (2009 NHIS, NCHS).1
-
—
- According to data from NHANES 2005 to 2008 (NCHS; unpublished NHLBI tabulation), the overall prevalence for MI is 3.1% in US adults ≥20 years of age. MI prevalence is 4.3% for men and 2.2% for women.
-
—Among non-Hispanic whites, MI prevalence is 4.3% for men and 2.1% for women.
-
—Among non-Hispanic blacks, MI prevalence is 4.3% for men and 2.2% for women.
-
—Among Mexican Americans, MI prevalence is 3.0% for men and 1.1% for women.
-
—
Data from 2009 from the BRFSS survey of the CDC found that 4.0% of respondents had been told that they had had an MI. The highest prevalence was in West Virginia (6.5%) and Kentucky (5.9%). The lowest prevalence was in the District of Columbia (1.9%). In the same survey, 3.8% of respondents were told that they had angina or CHD. The highest prevalence was in West Virginia (7.1%), and the lowest was in the District of Columbia (2.0%).2
Incidence
- On the basis of unpublished data from the ARIC and CHS studies of the NHLBI:
- —
-
—The estimated annual incidence of MI is 610 000 new attacks and 325 000 recurrent attacks.
-
—Average age at first MI is 64.5 years for men and 70.3 years for women.
- On the basis of the NHLBI-sponsored FHS:
-
—CHD makes up more than half of all cardiovascular events in men and women <75 years of age.3
-
—The lifetime risk of developing CHD after 40 years of age is 49% for men and 32% for women.5
-
—The incidence of CHD in women lags behind men by 10 years for total CHD and by 20 years for more serious clinical events such as MI and sudden death.3
-
—
In the NHLBI-sponsored ARIC study, in participants 45 to 64 years of age, the average age-adjusted CHD incidence rates per 1000 person-years were as follows: white men, 12.5; black men, 10.6; white women, 4.0; and black women, 5.1. Incidence rates excluding revascularization procedures were as follows: white men, 7.9; black men, 9.2; white women, 2.9; and black women, 4.9.6
Incidence rates for MI in the NHLBI-sponsored ARIC study are displayed in Charts 5–3 and 5–4, stratified by age, race, and sex. The annual age-adjusted rates per 1000 population of first MI (1987–2001) in ARIC Surveillance (NHLBI) were 4.2 in black men, 3.9 in white men, 2.8 in black women, and 1.7 in white women.7
Analysis of more than 40 years of physician-validated acute myocardial infarction (AMI) data in the FHS study of the NHLBI found that AMI rates diagnosed by ECG criteria declined ≈50% with a concomitant 2-fold increase in rates of AMI diagnosed by blood markers. These findings may explain the paradoxical stability of AMI rates in the United States despite concomitant improvements in CHD risk factors.8
Among American Indians 65 to 74 years of age, the annual rates per 1000 population of new and recurrent MIs were 7.6 for men and 4.9 for women.9 Analysis of data from NHANES III (1988 –1994) and NHANES 1999 to 2002 (NCHS) showed that in adults 20 to 74 years of age, the overall distribution of 10-year risk of developing CHD changed little during this time. Among the 3 racial/ethnic groups, blacks had the highest proportion of participants in the high-risk group.10
Based on data from the NHDS, since the mid-1990s, the rate of hospitalization for MI and in-hospital case fatality rates have decreased.11
From 2002 to 2007, the rates of hospitalization for MI decreased among Medicare beneficiaries. However, the degree of reduction was more significant in whites than African Americans.12
Chart 5-3.
Annual rate of first heart attacks by age, sex, and race (Atherosclerosis Risk in Communities Surveillance: 1987–2004). Source: National Heart, Lung, and Blood Institute.
Chart 5-4.
Incidence of myocardial infarction* by age, race, and sex (Atherosclerosis Risk in Communities Surveillance, 1987–2004). *Myocardial infarction diagnosis by expert committee based on review of hospital records. Source: Unpublished data from Atherosclerosis Risk in Communities study, National Heart, Lung, and Blood Institute.
Mortality
CHD caused ≈1 of every 6 deaths in the United States in 2007. CHD mortality was 406 351.13
CHD any-mention mortality was 571 402. MI mortality was 132 968. MI any-mention mortality was 172 538 (NHLBI tabulation; NCHS public-use data files). The 2007 CHD death rate was 126.0.13 CHD is the largest major killer of American males and females.13
Approximately every 25 seconds, an American will experience a coronary event, and approximately every minute, someone will die of one.
Approximately 34% of the people who experience a coronary attack in a given year will die of it, and ≈15% who experience a heart attack (MI) will die of it (AHA computation).
Approximately every 34 seconds, an American will have an MI.
The percentage of CHD deaths that occurred out of the hospital in 2007 was 70%. According to NCHS mortality data, 286 000 CHD deaths occur out of the hospital or in hospital EDs annually (2007, ICD-10 codes I20 to I25) (NHLBI tabulation of NCHS mortality data).
A study of 1275 health maintenance organization enrollees 50 to 79 years of age who had cardiac arrest showed that the incidence of out-of-hospital cardiac arrest was 6.0/1000 subject-years in subjects with any clinically recognized HD compared with 0.8/1000 subject-years in subjects without HD. In subgroups with HD, incidence was 13.6/1000 subject-years in subjects with prior MI and 21.9/1000 subject-years in subjects with HF.15
Temporal Trends in CHD Mortality
An analysis of FHS data (NHLBI) from 1950 to 1999 showed that overall CHD death rates decreased by 59%. Nonsudden CHD death decreased by 64%, and sudden cardiac death fell by 49%. These trends were seen in men and women, in subjects with and without a prior history of CHD, and in smokers and nonsmokers.16
The decline in CHD mortality rates partly reflects the shift in the pattern of clinical presentations of AMI. In the last decade, there has been a marked decline in ST-segment–elevation myocardial infarction (STEMI) (from 133 to 50 cases per 100 000 person-years).17
From 1997 to 2007, the annual death rate due to CHD declined 26.3%, and the actual number of deaths declined 12.9%. (Appropriate comparability ratios were applied.) In 2007, the overall CHD death rate was 126.0 per 100 000 population. The death rates were 165.6 for white males and 191.6 for black males; for white females, the rate was 94.2, and for black females, it was 121.5.13 Age-adjusted death rates for CHD were 122.3 for Hispanic or Latino males and 77.8 for females, 112.2 for American Indian or Alaska Native males and 65.6 for females, and 91.7 for Asian or Pacific Islander males and 55.0 for females.13
Approximately 81% of people who die of CHD are ≥65 years of age (NCHS; AHA computation).
The estimated average number of years of life lost because of an MI is 16.6 (NHLBI tabulation of NCHS mortality data).
- On the basis of data from the FHS of the NHLBI3:
-
—Fifty percent of men and 64% of women who die suddenly of CHD have no previous symptoms of this disease. Between 70% and 89% of sudden cardiac deaths occur in men, and the annual incidence is 3 to 4 times higher in men than in women; however, this disparity decreases with advancing age.
-
—People who have had an MI have a sudden death rate 4 to 6 times that of the general population.
-
—
- According to data from the National Registry of Myocardial Infarction18:
-
—From 1990 to 1999, in-hospital AMI mortality declined from 11.2% to 9.4%.
-
—Mortality rate increases for every 30 minutes that elapse before a patient with ST-segment elevation is recognized and treated.
-
—
- CHD death rates have fallen from 1968 to the present. Analysis of NHANES (NCHS) data compared CHD death rates between 1980 and 2000 to determine how much of the decline in deaths due to CHD over that period could be explained by the use of medical and surgical treatments versus changes in CVD risk factors (resulting from lifestyle/behavior). After 1980 and 2000 data were compared, it was estimated that ≈47% of the decrease in CHD deaths was attributable to treatments, including the following19:
-
—Secondary preventive therapies after MI or revascularization (11%).
-
—Initial treatments for AMI or unstable angina (UA; 10%).
-
—Treatments for HF (9%).
-
—Revascularization for chronic angina (5%). — Other therapies (12%), including antihypertensive and lipid-lowering primary prevention therapies.
-
—
- It was also estimated that a similar amount of the reduction in CHD deaths, ≈44%, was attributable to changes in risk factors, including the following19:
-
—Lower total cholesterol (24%).
-
—Lower SBP (20%).
-
—Lower smoking prevalence (12%).
-
—Decreased physical inactivity (5%).
-
—Nevertheless, these favorable improvements in risk factors were offset in part by increases in BMI and in diabetes mellitus prevalence, which accounted for an increased number of deaths (8% and 10%, respectively).
-
—
Between 1980 and 2002, death rates due to CHD among men and women ≥65 years of age fell by 52% in men and 49% in women. Among men, the death rate declined on average by 2.9% per year in the 1980s, 2.6% per year during the 1990s, and 4.4% per year from 2000 to 2002. Among women, death rates fell by 2.6%, 2.4%, and 4.4%, respectively. However, when stratified by age, among men 35 to 54 years of age, the average annual rate of death fell by 6.2%, 2.3%, and 0.5%, respectively. Among women 35 to 54 years of age, the average annual rate of death fell by 5.4% and 1.2% and then increased by 1.5%, respectively. This increase was not statistically significant; however, in even younger women (35 to 44 years of age), the rate of death has been increasing by an average of 1.3% annually between 1997 and 2002, which is statistically significant.20
An analysis of 28 studies published from 1977 to 2007 found that revascularization by coronary bypass surgery or percutaneous intervention in conjunction with medical therapy in patients with nonacute CAD is associated with significantly improved survival compared with medical therapy alone.21
A recent analysis of Centers for Medicare & Medicaid Services data suggest that between 1995 and 2006, the 30-day mortality rate from MI decreased, as has hospital variation in mortality from MI.22
Data from the Nationwide Inpatient Sample database suggest that mortality from MI have decreased since 1988.23
Risk Factors
Risk factors for CHD act synergistically to increase CHD risk, as shown in the example in Chart 5-6.
A study of men and women in 3 prospective cohort studies found that antecedent major CHD risk factor exposures were common among those who developed CHD. Approximately 90% of patients with CHD have prior exposure to at least 1 of these major risk factors, which include high total blood cholesterol levels or current medication with cholesterol-lowering drugs, hypertension or current medication with BP-lowering drugs, current cigarette use, and clinical report of diabetes mellitus.24
According to a case-control study of 52 countries (INTER-HEART), optimization of 9 easily measured and potentially modifiable risk factors could result in a 90% reduction in the risk of an initial AMI. The effect of these risk factors is consistent in men and women across different geographic regions and by ethnic group, which makes the study applicable worldwide. These 9 risk factors include cigarette smoking, abnormal blood lipid levels, hypertension, diabetes mellitus, abdominal obesity, a lack of PA, low daily fruit and vegetable consumption, alcohol overconsumption, and psychosocial index.25
A study of >3000 members of the FHS (NHLBI) Offspring Cohort without CHD showed that among men with 10-year predicted risk for CHD of 20%, both failure to reach target heart rate and ST-segment depression more than doubled the risk of an event, and each metabolic equivalent increment in exercise capacity reduced risk by 13%.26
A study of non-Hispanic white people 35 to 74 years of age in the FHS (NHLBI) and the NHANES III (NCHS) studies showed that 26% of men and 41% of women had at least 1 borderline risk factor in NHANES III. It is estimated that >90% of CHD events will occur in individuals with at least 1 elevated risk factor and that ≈8% will occur in people with only borderline levels of multiple risk factors. Absolute 10-year CHD risk exceeded 10% both in men >45 years of age who had 1 elevated risk factor and ≥4 borderline risk factors and in those who had ≥2 elevated risk factors. In women, absolute CHD risk was >10% only in those >55 years of age who had ≥3 elevated risk factors.27
A recent analysis examined the number and combination of risk factors necessary to exceed Adult Treatment Panel III (ATP III) treatment thresholds. In this analysis, relatively high risk factor levels were required to exceed ATP III treatment thresholds in men <45 years of age and women <65 years of age, which suggests that alternative means of risk prediction that focus on a longer time horizon than the 10 years captured by the traditional Framingham CHD risk score may be necessary to estimate risk in these individuals.28
Analysis of data from the CHS study (NHLBI) among participants ≥65 years of age at entry into the study showed that subclinical CVD is prevalent among older individuals, is independently associated with risk of CHD (even over a 10-year follow-up period), and substantially increases the risk of CHD among participants with hypertension or DM.29
On the basis of data from the CDC/BRFSS, it was found that patients with CHD are less likely to comply with PA recommendations than are subjects without CHD. Only 32% of CHD patients met moderate PA recommendations, 22% met vigorous PA recommendations, and 40% met total PA recommendations. In contrast, the percentage of subjects without CHD who met PA recommendations was significantly higher, and this percentage almost achieved the Healthy People 2010 objectives for PA.30
Analysis of data from the PREMIER trial (Prospective Registry Evaluating Myocardial Infarction: Events and Recovery), sponsored by the NHLBI, found that in people with prehypertension or stage 1 hypertension, 2 multicomponent behavioral interventions significantly reduced estimated 10-year CHD risk by 12% and 14%, respectively, compared with advice only.31
Chart 5-6.
Estimated 10-year coronary heart disease risk in adults 55 years of age according to levels of various risk factors (Framingham Heart Study). HDL-C indicates high density lipoprotein-cholesterol. Data derived from Wilson et al.53
Awareness of Warning Signs and Risk Factors for HD
Data from the Women Veterans Cohort showed that 42% of women ≥35 years of age were concerned about HD. Only 8% to 20% were aware that CAD is the major cause of death for women.32
Among people in 14 states and Washington, DC, participating in the 2005 BRFSS, only 27% were aware of 5 heart attack warning signs and symptoms (1, pain in jaw, neck, or back; 2, weak, lightheaded, or faint; 3, chest pain or discomfort; 4, pain or discomfort in arms or shoulder; and 5, shortness of breath) and indicated that they would first call 911 if they thought someone was having a heart attack or stroke. Awareness of all 5 heart attack warning signs and symptoms and the need to call 911 was higher among non-Hispanic whites (30.2%), women (30.8%), and those with a college education or more (33.4%) than among non-Hispanic blacks and Hispanics (16.2% and 14.3%, respectively), men (22.5%), and those with less than a high school education (15.7%), respectively. By state, awareness was highest in West Virginia (35.5%) and lowest in Washington, DC (16.0%).33
A 2004 national study of physician awareness and adherence to CVD prevention guidelines showed that fewer than 1 in 5 physicians knew that more women than men die each year of CVD.34
A recent community surveillance study in 4 US communities reported that in 2000, the overall proportion of people with delays of ≥4 hours from onset of AMI symptoms to hospital arrival was 49.5%. The study also reported that from 1987 to 2000, there was no statistically significant change in the proportion of patients whose delays were ≥4 hours, which indicates that there has been little improvement in the speed at which patients with MI symptoms arrive at the hospital after symptom onset. Although the proportion of patients with MI who arrived at the hospital by EMS increased over this period, from 37% in 1987% to 55% in 2000, the total time between onset and hospital arrival did not change appreciably.35
According to 2003 data from the BRFSS (CDC), 36.5% of all women surveyed had multiple risk factors for HD and stroke. The age-standardized prevalence of multiple risk factors was lowest in whites and Asians. After adjustment for age, income, education, and health coverage, the odds for multiple risk factors were greater in black and Native American women and lower for Hispanic women than for white women. Prevalence estimates and odds of multiple risk factors increased with age; decreased with education, income, and employment; and were lower in those with no health coverage. Smoking was more common in younger women, whereas older women were more likely to have medical conditions and to be physically inactive.36
Individuals with documented CHD have 5 to 7 times the risk of having a heart attack or dying as the general population. Survival rates improve after a heart attack if treatment begins within 1 hour; however, most patients are admitted to the hospital 2.5 to 3 hours after symptoms begin. More than 3500 patients surveyed with a history of CHD were asked to identify possible symptoms of heart attack. Despite their history of CHD, 44% had low knowledge levels. In this group, who were all at high risk of future AMI, 43% assessed their risk as less than or the same as others their age. More men than women perceived themselves as being at low risk, at 47% versus 36%, respectively.37
Data from Worcester, MA, indicate that the average time from symptom onset to hospital arrival has not improved and that delays in hospital arrival are associated with less receipt of guidelines-based care. Mean and median prehospital delay times from symptom onset to arrival at the hospital were 4.1 and 2.0 hours in 1986 and 4.6 and 2.0 hours in 2005. Compared with those arriving within 2 hours of symptom onset, those with prolonged prehospital delay were less likely to receive thrombolytic therapy and percutaneous coronary intervention (PCI) within 90 minutes of hospital arrival.38
In an analysis from ARIC, low neighborhood household income (odds ratio [OR] 1.46, 95% confidence interval [CI], 1.09 to 1.96) and being a Medicaid recipient (OR 1.87, 95% CI, 1.10 to 3.19) were associated with increased odds of having prolonged prehospital delays from symptom onset to hospital arrival for AMI compared with individuals with higher neighborhood household income and other insurance providers, respectively.39
Aftermath
Depending on their sex and clinical outcome, people who survive the acute stage of an MI have a chance of illness and death 1.5 to 15 times higher than that of the general population. Among these people, the risk of another MI, sudden death, AP, HF, and stroke—for both men and women—is substantial (FHS, NHLBI).3
A Mayo Clinic study found that cardiac rehabilitation after an MI is underused, particularly in women and the elderly. Women were 55% less likely than men to participate in cardiac rehabilitation, and older study patients were less likely to participate than younger participants. Only 32% of men and women ≥70 years of age participated in cardiac rehabilitation compared with 66% of those 60 to 69 years of age and 81% of those <60 years of age.40
- On the basis of pooled data from the FHS, ARIC, and CHS studies of the NHLBI, within 1 year after a first MI:
-
—At ≥45 years of age, 19% of men and 26% of women will die.
-
—At 45 to 64 years of age, 5% of white men, 9% of white women, 14% of black men, and 8% of black women will die.
-
—At ≥65 years of age, 25% of white men, 30% of white women, 25% of black men, and 30% of black women will die.
-
—In part because women have MIs at older ages than men, they are more likely to die of MIs within a few weeks.
-
—
- Within 5 years after a first MI:
-
—At ≥45 years of age, 36% of men and 47% of women will die.
-
—At 45 to 64 years of age, 11% of white men, 18% of white women, 22% of black men, and 28% of black women will die.
-
—At ≥65 years of age, 46% of white men, 53% of white women, 54% of black men, and 58% of black women will die.
-
—
- Of those who have a first MI, the percentage with a recurrent MI or fatal CHD within 5 years is:
-
—At 45 to 64 years of age, 15% of men and 22 of women.
-
—At ≥65 years of age, 22% of men and women.
-
—At 45 to 64 years of age, 14% of white men, 18% of white women, 22% of black men, and 28% of black women.
-
—At ≥65 years of age, 21% of white men and women, 33% of black men, and 26% of black women.
-
—
- The percentage of people with a first MI who will have HF in 5 years is:
-
—At 45 to 64 years of age, 8% of men and 18% of women.
-
—At ≥65 years of age, 20% of men and 23% of women.
-
—At 45 to 64 years of age, 7% of white men, 15% of white women, 13% of black men, and 25% of black women.
-
—At ≥65 years of age, 19% of white men, 23% of white women, 31% of black men, and 24% of black women.
-
—
- The percentage of people with a first MI who will have a stroke within 5 years is:
-
—At 45 to 64 years of age, 2% of men and 6% of women.
-
—At ≥65 years of age, 5% of men and 8% of women.
-
—At 45 to 64 years of age, 2% of white men, 4% of white women, 3% of black men, and 10% of black women.
-
—At ≥65 years of age, 5% of white men, 8% of white women, 9% of black men, and 10% of black women.
-
—
- The median survival time (in years) after a first MI is:
-
—At 55 to 64 years of age, 17.0 for men and 13.3 for women.
-
—At 65 to 74 years of age, 9.3 for men and 8.8 for women.
-
—At ≥75 years of age, 3.2 for men and 3.2 for women.
-
—
Among survivors of an MI, in 2005, 34.7% of BRFSS respondents participated in outpatient cardiac rehabilitation. The prevalence of cardiac rehabilitation was higher among older age groups (≥50 years of age), among men versus women, among Hispanics, among those who were married, among those with higher education, and among those with higher levels of household income.41
A recent analysis of Medicare claims data revealed that only 13.9% of Medicare beneficiaries enroll in cardiac rehabilitation after an AMI, and only 31% enroll after CABG. Older people, women, nonwhites, and individuals with comorbidities were less likely to enroll in cardiac rehabilitation programs.42
Hospital Discharges and Ambulatory Care Visits
(See Table 5-1 and Chart 5-7.)
Chart 5-7.
Hospital discharges for coronary heart disease by sex (United States: 1970–2007). Hospital discharges include people discharged alive, dead, and “status unknown.” Source: National Hospital Discharge Survey/National Center for Health Statistics and National Heart, Lung, and Blood Institute.
From 1997 to 2007, the number of inpatient discharges from short-stay hospitals with CHD as the first-listed diagnosis decreased from 2 090 000 to 1 572 000 (NHDS, NCHS, NHLBI).
In 2008, there were 16 251 000 ambulatory care visits with CHD as the first-listed diagnosis (NCHS, NAMCS, NHAMCS). The majority of these visits (62.2%) were for coronary atherosclerosis.43
Age-adjusted hospitalization rate for MI was 215 per 100 000 people in 1979 to 1981, increased to 342 in 1985 to 1987, stabilized for the next decade and then declined after 1996 to 242 in 2003 to 2005. Rates for men were almost twice that of women. Trends were similar for men and women. Hospitalization rates increased with age and were the highest among ≥85 years.11
Most hospitalized patients >65 years of age are women. For MI, 28.4% of hospital stays for people 45 to 64 years of age were for women, but 63.7% of stays for those ≥85 years of age were for women. Similarly, for coronary atherosclerosis, 32.7% of stays among people 45 to 64 years of age were for women; this figure increased to 60.7% of stays among those ≥85 years of age. For nonspecific chest pain, women were more numerous than men among patients <65 years of age. Approximately 54.4% of hospital stays among people 45 to 64 years of age were for women. Women constituted 73.9% of nonspecific chest pain stays among patients ≥85 years of age, higher than for any other condition examined. For AMI, one third more women than men died in the hospital: 9.3% of women died in the hospital compared with 6.2% of men.44
Operations and Procedures
In 2007, an estimated 1 178 000 inpatient PCI procedures, 408 000 inpatient bypass procedures, 1 061 000 inpatient diagnostic cardiac catheterizations, 111 000 inpatient implantable defibrillators, and 358 000 pacemaker procedures were performed for inpatients in the United States. (NHLBI, NCHS, unpublished tabulation).
Cost
The estimated direct and indirect cost of heart disease in 2007 is $177.5 billion. (MEPS, NHLBI tabulation).
In 2006, $11.7 billion was paid to Medicare beneficiaries for in-hospital costs when CHD was the principal diagnosis ($14 009 per discharge for AMI, $12 977 per discharge for coronary atherosclerosis, and $10 630 per discharge for other ischemic HD).37,45
Acute Coronary Syndrome
ICD-9 codes 410, 411.
The term acute coronary syndrome (ACS) is increasingly used to describe patients who present with either AMI or unstable angina (UA). (UA is chest pain or discomfort that is accelerating in frequency or severity and may occur while at rest but does not result in myocardial necrosis.) The discomfort may be more severe and prolonged than typical AP or may be the first time a person has AP. UA, non–ST-segment–elevation myocardial infarction (NSTEMI), and STEMI share common pathophysiological origins related to coronary plaque progression, instability, or rupture with or without luminal thrombosis and vasospasm.
A conservative estimate for the number of discharges with ACS from hospitals in 2007 is 671 000. Of these, an estimated 384 000 are males and 287 000 are females. This estimate is derived by adding the first-listed inpatient hospital discharges for MI (577 000) to those for UA (94 000; NHDS, NHLBI).
When secondary discharge diagnoses in 2007 were included, the corresponding number of inpatient hospital discharges was 1 172 000 unique hospitalizations for ACS; 667 000 were males, and 505 000 were females. Of the total, 731 000 were for MI alone, 431 000 were for UA alone, and 10 000 hospitalizations received both diagnoses (NHDS, NHLBI).
Decisions about medical and interventional treatments are based on specific findings noted when a patient presents with ACS. Such patients are classified clinically into 1 of 3 categories according to the presence or absence of ST-segment elevation on the presenting ECG and abnormal (“positive”) elevations of myocardial biomarkers such as troponins as follows:
STEMI
NSTEMI
UA
The percentage of ACS or MI cases with ST-segment elevation varies in different registries/databases and depends heavily on the age of patients included and the type of surveillance used. According to the National Registry of Myocardial Infarction 4 (NRMI-4), ≈29% of patients with MI are patients with STEMI.46 The AHA Get With The Guidelines project found that 32% of the patients with MI in the CAD module are patients with STEMI (personal communication from AHA Get With The Guidelines staff, October 1, 2007). The Global Registry of Acute Coronary Events (GRACE) study, which includes US patient populations, found that 38% of ACS patients have STEMI, whereas the second Euro Heart Survey on ACS (EHS-ACS-II) reported that ≈47% of patients with ACS have STEMI.47
In addition, the percentage of ACS or MI cases with ST-segment elevation appears to be declining. In an analysis of 46 086 hospitalizations for ACS in the Kaiser Permanente Northern California study, the percentage of MI cases with ST-segment elevation decreased from 48.5% to 24% between 1999 and 2008.17
Analysis of data from the GRACE multinational observational cohort study of patients with ACS found evidence of a change in practice for both pharmacological and interventional treatments in patients with either STEMI or NSTE ACS. These changes have been accompanied by significant decreases in the rates of in-hospital death, cardiogenic shock, and new MI among patients with non–ST-segment– elevation acute coronary syndromes (NSTE ACS). The use of evidence-based therapies and PCI interventions increased in the STEMI population. This increase was matched with a statistically significant decrease in the rates of death, cardiogenic shock, and HF or pulmonary edema.48
A study of patients with NSTE ACS treated at 350 US hospitals found that up to 25% of opportunities to provide American College of Cardiology (ACC)/AHA guideline–recommended care were missed in current practice. The composite guideline adherence rate was significantly associated with in-hospital mortality.48
A study of hospital process performance in 350 centers of nearly 65 000 patients enrolled in the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines) National Quality Improvement Initiative found that ACC/AHA guideline–recommended treatments were adhered to in 74% of eligible instances.49
After adjustment for clinical differences and the severity of CAD by angiogram, 30-day mortality after ACS is similar in men and women.50
Angina Pectoris
ICD-9 413; ICD-10 I20. See Table 5-2 and Chart 5-5.
Chart 5-5.
Incidence of angina pectoris* by age and sex (Framingham Heart Study 1980–2002/2003). *Angina pectoris uncomplicated based on physician interview of patient. (Rate for women 45–54 years of age considered unreliable.) Data derived from National Heart, Lung, and Blood Institute.7
Prevalence
A study of 4 national cross-sectional health examination studies found that among Americans 40 to 74 years of age, the age-adjusted prevalence of AP was higher among women than men. Increases in the prevalence of AP occurred for Mexican American men and women and African American women but were not statistically significant for the latter.51
Incidence
Only 18% of coronary attacks are preceded by longstanding AP (NHLBI computation of FHS follow-up since 1986).
The annual rates per 1000 population of new episodes of AP for nonblack men are 28.3 for those 65 to 74 years of age, 36.3 for those 75 to 84 years of age, and 33.0 for those ≥85 years of age. For nonblack women in the same age groups, the rates are 14.1, 20.0, and 22.9, respectively. For black men, the rates are 22.4, 33.8, and 39.5, and for black women, the rates are 15.3, 23.6, and 35.9, respectively (CHS, NHLBI).7
On the basis of 1987 to 2001 data from the ARIC study of the NHLBI, the annual rates per 1000 population of new episodes of AP for nonblack men are 8.5 for those 45 to 54 years of age, 11.9 for those 55 to 64 years of age, and 13.7 for those 65 to 74 years of age. For nonblack women in the same age groups, the rates are 10.6, 11.2, and 13.1, respectively. For black men, the rates are 11.8, 10.6, and 8.8, and for black women, the rates are 20.8, 19.3, and 10.0, respectively.7
Mortality
A small number of deaths resulting from CHD are coded as being due to AP. These are included as a portion of total deaths from CHD.
Cost
For women with nonobstructive CHD enrolled in the Women’s Ischemia Syndrome Evaluation (WISE) study of the NHLBI, the average lifetime cost estimate was ≈$770 000 and ranged from $1.0 to $1.1 million for women with 1-vessel to 3-vessel CHD.52
Abbreviations Used in Chapter 5
- ACC
American College of Cardiology
- ACS
acute coronary syndrome
- AHA
American Heart Association
- AMI
acute myocardial infarction
- AP
angina pectoris
- ARIC
Atherosclerosis Risk in Communities study
- ATP III
Adult Treatment Panel III
- BMI
body mass index
- BP
blood pressure
- BRFSS
Behavioral Risk Factor Surveillance System
- CABG
coronary artery bypass graft
- CAD
coronary artery disease
- CDC
Centers for Disease Control and Prevention
- CHD
coronary heart disease
- CHS
Cardiovascular Health Study
- CI
confidence interval
- CVD
cardiovascular disease
- DM
diabetes mellitus
- ECG
electrocardiogram
- EMS
emergency medical services
- FHS
Framingham Heart Study
- GRACE
Global Registry of Acute Coronary Events
- HD
heart disease
- HF
heart failure
- ICD
International Classification of Diseases
- INTERHEART
Interheart Study
- MEPS
Medical Expenditure Panel Survey
- MI
myocardial infarction
- NAMCS
National Ambulatory Medical Care Survey
- NCHS
National Center for Health Statistics
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- NHANES
National Health and Nutrition Examination Survey
- NHDS
National Hospital Discharge Survey
- NHIS
National Health Interview Study
- NHLBI
National Heart, Lung, and Blood Institute
- NRMI
National Registry of Myocardial Infarction
- NSTE ACS
non–ST-segment–elevation acute coronary syndromes
- NSTEMI
non–ST-segment–elevation myocardial infarction
- OR
odds ratio
- PA
physical activity
- PCI
percutaneous coronary intervention
- STEMI
ST-segment–elevation myocardial infarction
- UA
unstable angina
References
- 1.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. [Accessed August 26, 2010];Vital Health Stat 10. No. 249. 2010 Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_249.pdf. [PubMed]
- 2.CDC. 2009 Behavioral Risk Factor Surveillance System. [Accessed September 15, 2010]; Available at: http://www.cdc.gov/brfss.
- 3.Thom TJ, Kannel WB, Silbershatz H, D’Agostino RB., Sr . Cardiovascular diseases in the United States and prevention approaches. In: Fuster V, Alexander RW, Schlant RC, O’Rourke RA, Roberts R, Sonnenblick EH, editors. Hurst’s the Heart. 10th ed. New York, NY: McGraw-Hill; 2001. pp. 3–7. [Google Scholar]
- 4.Boland LL, Folsom AR, Sorlie PD, Taylor HA, Rosamond WD, Chambless LE, Cooper LS. Occurrence of unrecognized myocardial infarction in subjects aged 45 to 65 years (the ARIC Study) Am J Cardiol. 2002;90:927–931. doi: 10.1016/s0002-9149(02)02655-3. [DOI] [PubMed] [Google Scholar]
- 5.Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet. 1999;353:89–92. doi: 10.1016/S0140-6736(98)10279-9. [DOI] [PubMed] [Google Scholar]
- 6.Jones DW, Chambless LE, Folsom AR, Heiss G, Hutchinson RG, Sharrett AR, Szklo M, Taylor HA., Jr Risk factors for coronary heart disease in African Americans: the Atherosclerosis Risk in Communities Study, 1987–1997. Arch Intern Med. 2002;162:2565–2571. doi: 10.1001/archinte.162.22.2565. [DOI] [PubMed] [Google Scholar]
- 7.National Heart, Lung, and Blood Institute. Incidence and Prevalence: 2006 Chart Book on Cardiovascular and Lung Diseases. Bethesda, Md: National Institutes of Health; 2006. [Google Scholar]
- 8.Parikh NI, Gona P, Larson MG, Fox CS, Benjamin EJ, Murabito JM, O’Donnell CJ, Vasan RS, Levy D. Long-term trends in myocardial infarction incidence and case fatality in the National Heart, Lung, and Blood Institute’s Framingham Heart Study. Circulation. 2009;119:1203–1210. doi: 10.1161/CIRCULATIONAHA.108.825364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ali T, Jarvis B, O’Leary M. Strong Heart Study Data Book: A Report to American Indian Communities. Rockville, Md: National Institutes of Health, National Heart, Lung, and Blood Institute; 2001. [Google Scholar]
- 10.Ajani UA, Ford ES. Has the risk for coronary heart disease changed among U.S. adults? J Am Coll Cardiol. 2006;48:1177–1182. doi: 10.1016/j.jacc.2006.05.055. [DOI] [PubMed] [Google Scholar]
- 11.Fang J, Alderman MH, Keenan NL, Ayala C. Acute myocardial infarction hospitalization in the United States, 1979 to 2005. Am J Med. 2010;123:259–266. doi: 10.1016/j.amjmed.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 12.Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010;121:1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 13.Xu J, Kochanek KD, Murphy S, Tejada-Vera B. Deaths: Final Data for 2007. 19. Vol. 58. Hyattsville, Md: National Center for Health Statistics; 2010. National Vital Statistics Reports. [PubMed] [Google Scholar]
- 14.National Center for Health Statistics, Centers for Disease Control and Prevention Web site. Atlanta, Ga: Centers for Disease Control and Prevention; [Accessed September 27, 2010]. Compressed mortality file: underlying cause of death, 1979 to 2006. Available at: http://wonder.cdc.gov/mortSQL.html. [Google Scholar]
- 15.Rea TD, Pearce RM, Raghunathan TE, Lemaitre RN, Sotoodehnia N, Jouven X, Siscovick DS. Incidence of out-of-hospital cardiac arrest. Am J Cardiol. 2004;93:1455–1460. doi: 10.1016/j.amjcard.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Fox CS, Evans JC, Larson MG, Kannel WB, Levy D. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999: the Framingham Heart Study. Circulation. 2004;110:522–527. doi: 10.1161/01.CIR.0000136993.34344.41. [DOI] [PubMed] [Google Scholar]
- 17.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 18.National Registry of Myocardial Infarction. [Accessed September 27, 2010]; Available at: http://www.ncdr.com/WebNCDR/Common/. [Google Scholar]
- 19.Ford ES, Ajani UA, Croft JB, Critchley JA, LaBarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 20.Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol. 2007;50:2128–2132. doi: 10.1016/j.jacc.2007.05.056. [DOI] [PubMed] [Google Scholar]
- 21.Jeremias A, Kaul S, Rosengart T, Gruberg L, Brown D. The impact of revascularization on mortality in patients with nonacute coronary artery disease. Am J Med. 2009;122:152–161. doi: 10.1016/j.amjmed.2008.07.027. [DOI] [PubMed] [Google Scholar]
- 22.Krumholz HM, Wang Y, Chen J, Drye EE, Spertus JA, Ross JS, Curtis JP, Nallamothu BK, Lichtman JH, Havranek EP, Masoudi FA, Radford MJ, Han LF, Rapp MT, Straube BM, Normand SL. Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995–2006. JAMA. 2009;302:767–773. doi: 10.1001/jama.2009.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Movahed MR, John J, Hashemzadeh M, Jamal MM, Hashemzadeh M. Trends in the age adjusted mortality from acute ST segment elevation myocardial infarction in the United States (1988 –2004) based on race, gender, infarct location and comorbidities. Am J Cardiol. 2009;104:1030–1034. doi: 10.1016/j.amjcard.2009.05.051. [DOI] [PubMed] [Google Scholar]
- 24.Greenland P, Knoll MD, Stamler J, Neaton JD, Dyer AR, Garside DB, Wilson PW. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA. 2003;290:891–897. doi: 10.1001/jama.290.7.891. [DOI] [PubMed] [Google Scholar]
- 25.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L for the INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 26.Balady GJ, Larson MG, Vasan RS, Leip EP, O’Donnell CJ, Levy D. Usefulness of exercise testing in the prediction of coronary disease risk among asymptomatic persons as a function of the Framingham risk score. Circulation. 2004;110:1920–1925. doi: 10.1161/01.CIR.0000143226.40607.71. [DOI] [PubMed] [Google Scholar]
- 27.Vasan RS, Sullivan LM, Wilson PW, Sempos CT, Sundstrom J, Kannel WB, Levy D, D’Agostino RB. Relative importance of borderline and elevated levels of coronary heart disease risk factors. Ann Intern Med. 2005;142:393–402. doi: 10.7326/0003-4819-142-6-200503150-00005. [published correction appears in Ann Intern Med. 2005;142:681]. [DOI] [PubMed] [Google Scholar]
- 28.Cavanaugh-Hussey MW, Berry JD, Lloyd-Jones DM. Who exceeds ATP-III risk thresholds? Systematic examination of the effect of varying age and risk factor levels in the ATP-III risk assessment tool. Prev Med. 2008;47:619–623. doi: 10.1016/j.ypmed.2008.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kuller LH, Arnold AM, Psaty BM, Robbins JA, O’Leary DH, Tracy RP, Burke GL, Manolio TA, Chaves PH. 10-Year follow-up of subclinical cardiovascular disease and risk of coronary heart disease in the Cardiovascular Health Study. Arch Intern Med. 2006;166:71–78. doi: 10.1001/archinte.166.1.71. [DOI] [PubMed] [Google Scholar]
- 30.Zhao G, Ford ES, Li C, Mokdad AH. Are United States adults with coronary heart disease meeting physical activity recommendations? Am J Cardiol. 2008;101:557–561. doi: 10.1016/j.amjcard.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 31.Maruthur NM, Wang NY, Appel LJ. Lifestyle interventions reduce coronary heart disease risk: results from the PREMIER Trial. Circulation. 2009;119:2026–2031. doi: 10.1161/CIRCULATIONAHA.108.809491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Biswas MS, Calhoun PS, Bosworth HB, Bastian LA. Are women worrying about heart disease? Womens Health Issues. 2002;12:204–211. doi: 10.1016/s1049-3867(02)00136-6. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC) Disparities in adult awareness of heart attack warning signs and symptoms: 14 states, 2005. MMWR Morb Mortal Wkly Rep. 2008;57:175–179. [PubMed] [Google Scholar]
- 34.Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, Fabunmi RP, Kwan J, Mills T, Simpson SL. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111:499–510. doi: 10.1161/01.CIR.0000154568.43333.82. [DOI] [PubMed] [Google Scholar]
- 35.Jones DE, Weaver MT, Grimley D, Appel SJ, Ard J. Health belief model perceptions, knowledge of heart disease, and its risk factors in educated African-American women: an exploration of the relationships of socio-economic status and age. J Natl Black Nurses Assoc. 2006;17:13–23. [PubMed] [Google Scholar]
- 36.Hayes DK, Denny CH, Keenan NL, Croft JB, Sundaram AA, Greenlund KJ. Racial/ethnic and socioeconomic differences in multiple risk factors for heart disease and stroke in women: Behavioral Risk Factor Surveillance System, 2003. J Womens Health (Larchmt) 2006;15:1000–1008. doi: 10.1089/jwh.2006.15.1000. [DOI] [PubMed] [Google Scholar]
- 37.Dracup K, McKinley S, Doering LV, Riegel B, Meischke H, Moser DK, Pelter M, Carlson B, Aitken L, Marshall A, Cross R, Paul SM. Acute coronary syndrome: what do patients know? Arch Intern Med. 2008;168:1049–1054. doi: 10.1001/archinte.168.10.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saczynski JS, Yarzebski J, Lessard D, Spencer FA, Gurwitz JH, Gore JM, Goldberg RJ. Trends in prehospital delay in patients with acute myocardial infarction (from the Worcester Heart Attack Study) Am J Cardiol. 2008;102:1589–1594. doi: 10.1016/j.amjcard.2008.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Foraker RE, Rose KM, McGinn AP, Suchindran CM, Goff DC, Jr, Whitsel EA, Wood JL, Rosamond WD. Neighborhood income, health insurance, and prehospital delay for myocardial infarction: the Atherosclerosis Risk In Communities Study. Arch Intern Med. 2008;168:1874–1879. doi: 10.1001/archinte.168.17.1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Witt BJ, Jacobsen SJ, Weston SA, Killian JM, Meverden RA, Allison TG, Reeder GS, Roger VL. Cardiac rehabilitation after myocardial infarction in the community. J Am Coll Cardiol. 2004;44:988–996. doi: 10.1016/j.jacc.2004.05.062. [DOI] [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention (CDC) Receipt of outpatient cardiac rehabilitation among heart attack survivors—United States, 2005. MMWR Morb Mortal Wkly Rep. 2008;57:89–94. [PubMed] [Google Scholar]
- 42.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–1662. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention, National Center for Health Statistics. Unpublished data. For methodology, see National Center for Health Statistics, Public Use Data File Documentation: 2008 National Ambulatory Medical Care Survey and Public Use Data File Documentation: 2008 National Hospital Ambulatory Medical Care Survey. [Accessed August 31, 2010];2008 National Ambulatory Medical Care Survey and 2008 National Hospital Ambulatory Medical Care Survey. Available at: http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm.
- 44.Elixhauser A, Jiang HJ. Rockville, Md: Agency for Healthcare Research and Quality; 2006. May, [Accessed September 27, 2010]. Hospitalizations for Women With Circulatory Disease, 2003. HCUP Statistical Brief #5. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb5.pdf. [PubMed] [Google Scholar]
- 45.Centers for Medicare & Medicaid Services. Medicare & Medicaid Statistical Supplement. Baltimore, Md: Centers for Medicare & Medicaid Services; 2007. [Accessed September 27, 2010]. Table 5.5: Discharges, Total Days of Care, and Program Payments for Medicare Beneficiaries Discharged from Short-Stay Hospitals, by Principal Diagnoses Within Major Diagnostic Classifications (MDCs): Calendar Year 2006. Available at: http://www.cms.hhs.gov/MedicareMedicaidStatSupp/downloads/2007Table5.5b.pdf. [Google Scholar]
- 46.Roe MT, Parsons LS, Pollack CV, Jr, Canto JG, Barron HV, Every NR, Rogers WJ, Peterson ED for the National Registry of Myocardial Infarction Investigators. Quality of care by classification of myocardial infarction: treatment patterns for ST-segment elevation vs non-ST-segment elevation myocardial infarction. Arch Intern Med. 2005;165:1630–1636. doi: 10.1001/archinte.165.14.1630. [DOI] [PubMed] [Google Scholar]
- 47.Mandelzweig L, Battler A, Boyko V, Bueno H, Danchin N, Filippatos G, Gitt A, Hasdai D, Hasin Y, Marrugat J, Van de Werf F, Wallentin L, Behar S for the Euro Heart Survey Investigators. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006;27:2285–2293. doi: 10.1093/eurheartj/ehl196. [DOI] [PubMed] [Google Scholar]
- 48.Fox KAA, Steg PG, Eagle KA, Goodman SG, Anderson FA, Jr, Granger CB, Flather MD, Budaj A, Quill A, Gore JM GRACE Investigators. Decline in rates of death and heart failure in acute coronary syndromes, 1999–2006. JAMA. 2007;297:1892–1900. doi: 10.1001/jama.297.17.1892. [DOI] [PubMed] [Google Scholar]
- 49.Peterson ED, Roe MT, Mulgund J, DeLong ER, Lytle BL, Brindis RG, Smith SC, Jr, Pollack CV, Jr, Newby LK, Harrington RA, Gibler WB, Ohman EM. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006;295:1912–1920. doi: 10.1001/jama.295.16.1912. [DOI] [PubMed] [Google Scholar]
- 50.Berger JS, Elliott L, Gallup D, Roe M, Granger CB, Armstrong PW, Simes RJ, White HD, Van de Werf F, Topol EJ, Hochman JS, Newby LK, Harrington RA, Califf RM, Becker RC, Douglas PS. Sex differences in mortality following acute coronary syndromes. JAMA. 2009;302:874–882. doi: 10.1001/jama.2009.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ford ES, Giles WH. Changes in prevalence of nonfatal coronary heart disease in the United States from 1971–1994. Ethn Dis. 2003;13:85–93. [PubMed] [Google Scholar]
- 52.Shaw LJ, Merz CN, Pepine CJ, Reis SE, Bittner V, Kip KE, Kelsey SF, Olson M, Johnson BD, Mankad S, Sharaf BL, Rogers WJ, Pohost GM, Sopko G for the Women’s Ischemia Syndrome Evaluation (WISE) Investigators. The economic burden of angina in women with suspected ischemic heart disease: results from the National Institutes of Health–National Heart, Lung, and Blood Institute–sponsored Women’s Ischemia Syndrome Evaluation. Circulation. 2006;114:894–904. doi: 10.1161/CIRCULATIONAHA.105.609990. [DOI] [PubMed] [Google Scholar]
- 53.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
6. Stroke (Cerebrovascular Disease)
ICD-9 430 to 438, ICD-10 I60 to I69. See Tables 6-1 and 6-2 and Charts 6-1 through 6-8.
Table 6-1.
Stroke
| Population Group | Prevalence, 2008 Age ≥20 y |
New and Recurrent Attacks All Ages |
Mortality, 2007 All Ages* |
Hospital Discharges, 2007 All Ages |
Cost, 2007 |
|---|---|---|---|---|---|
| Both sexes | 7 000 000 (3.0%) | 795 000 | 135 952 | 829 000 | $40.9 billion |
| Males | 2 800 000 (2.7%) | 370 000 (46.5%)† | 54 111 (39.8%)† | 371 000 | |
| Females | 4 200 000 (3.3%) | 425 000 (53.5%)† | 81 841 (60.2%)† | 458 000 | |
| NH white males | 2.4% | 325 000‡ | 44 714 | ||
| NH white females | 3.3% | 365 000‡ | 69 981 | ||
| NH black males | 4.5% | 45 000‡ | 7549 | ||
| NH black females | 4.4% | 60 000‡ | 9536 | ||
| Mexican-American males | 2.0% | ||||
| Mexican-American females | 2.7% | ||||
| Hispanic or Latino, age ≥18 y | 2.0%§ | ||||
| Asian or Pacific Islander, age ≥18 y | 1.3%§ | 3586 | |||
| American Indian/ Alaska Native, age ≥18 y | … | 586 |
NH indicates non-Hispanic.
Ellipses (…) indicate data not available.
Mortality data are for whites and blacks and include Hispanics.
These percentages represent the portion of total stroke incidence or mortality that applies to males vs females.
Estimates include Hispanics and non-Hispanics. Estimates for whites include other nonblack races.
NHIS (2009), NCHS; data are weighted percentages for Americans ≥18 years of age.3
Sources: Prevalence: National Health and Nutrition Examination Survey 2005 to 2008, National Center for Health Statistics and National Heart, Lung, and Blood Institute. Percentages for racial/ethnic groups are age-adjusted for Americans ≥20 years of age. Age-specific percentages are extrapolated to the 2008 US population. Incidence: Greater Cincinnati/Northern Kentucky Stroke Study/National Institutes of Neurological Disorders and Stroke data for 1999 provided on August 1, 2007. US estimates compiled by National Heart, Lung, and Blood Institute. See also Kissela et al.142 Data include children. Mortality: National Center for Health Statistics. These data represent underlying cause of death only. Mortality data for white and black males and females include Hispanics. Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics. Data include those inpatients discharged alive, dead, or status unknown. Cost: National Heart, Lung, and Blood Institute. Data include estimated direct and indirect costs for 2007.
Table 6-2.
Modifiable Stroke Risk Factors
| Factor | Prevalence, % | Population- Attributable Risk, %* |
RR |
|---|---|---|---|
| CVD | |||
| CHD143 | |||
| Men | 8.4 | 5.8† | 1.73 (1.68–1.78)161 |
| Women | 5.6 | 3.9† | 1.55 (1.17–2.07)162 |
| Heart failure143 | |||
| Men | 2.6 | 1.4† | |
| Women | 2.1 | 1.1† | |
| Peripheral arterial disease | 4.9 | 3.0† | |
| Hypertension144 | |||
| Age 50 y | 20 | 40 | 4.0 |
| Age 60 y | 30 | 35 | 3.0 |
| Age 70 y | 40 | 30 | 2.0 |
| Age 80 y | 55 | 20 | 1.4 |
| Age 90 y | 60 | 0 | 1.0 |
| Cigarette smoking | 25 | 12–18 | 1.8 |
| Diabetes mellitus | 7.3 | 5–27 | 1.8–6 |
| Asymptomatic carotid stenosis | 2–8148–154 | 2–7‡ | 2.0162 |
| Atrial fibrillation (nonvalvular)145,146 | |||
| Age 50–59 y | 0.5 | 1.5 | 4.0 |
| Age 60–69 y | 1.8 | 2.8 | 2.6 |
| Age 70–79 y | 4.8 | 9.9 | 3.3 |
| Age 80–89 y | 8.8 | 23.5 | 4.5 |
| Sickle cell disease | 0.25 (of blacks)155 | 200–400163§ | |
| Dyslipidemia | |||
| High total cholesterol | 25156 | 15 | 2.0 for men and for women <55 y of age |
| Low HDL cholesterol | 25156 | 10 | 1.5–2.5 for men |
| Dietary factors | |||
| Na intake 2300 mg | 75–90 | Unknown | Unknown |
| K intake 4700 mg | 90–99157 | Unknown | Unknown |
| Obesity | 17.9158 | 12–20† | 1.75–2.37164,165 |
| Physical inactivity147 | 25 | 30 | 2.7‡ |
| Postmenopausal hormone therapy | 20159 (women 50–74 y of age)160 | 7 | 1.463 |
RR indicates relative risk; CVD, cardiovascular disease; CHD, coronary heart disease; HDL, high-density lipoprotein.
Data derived from Hart et al166,167 and van Walraven et al.168 Stroke includes both ischemic and hemorrhagic stroke. Cardiovascular disease includes coronary heart disease, heart failure, and peripheral arterial disease.
Population-attributable risk is the proportion of ischemic stroke in the population that can be attributed to a particular risk factor (see text for formula).
Calculated on the basis of point estimates of referenced data provided in the table. For peripheral arterial disease, calculation was based on average relative risk for men and women.
Calculated based on referenced data provided in the table or text.
Relative to stroke risk in children without sickle cell disease.
Adapted from Goldstein et al.169
Chart 6-1.
Prevalence of stroke by age and sex (National Health and Nutrition Examination Survey: 2005–2008). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 6-7.
Annual age-adjusted incidence of first-ever stroke by race. Hospital plus out-of-hospital ascertainment, 1993–1994 and 1999, 1999 and 2005. Data derived from Kleindorfer et al.171
Prevalence
An estimated 7 000 000 Americans ≥20 years of age have had a stroke (extrapolated to 2008 using NCHS/NHANES 2005 to 2008 data). Overall stroke prevalence during this period is an estimated 3.0% (see Table 6-1).
According to data from the 2005 BRFSS (CDC), 2.7% of men and 2.5% of women ≥18 years of age had a history of stroke. Of those with prevalent stroke, 2.3% were non-Hispanic white, 4.0% were non-Hispanic black, 1.6% were Asian/Pacific Islander, 2.6% were Hispanic (of any race), 6.0% were American Indian/Alaska Native, and 4.6% were admixed.1
Data from the 2009 survey of the CDC/BRFSS found that, overall, 2.4% of respondents had been told that they had a stroke. The highest prevalence was in Alabama and Oklahoma (3.9%) and the lowest was in Colorado (1.4%).2
Among blacks ≥18 years of age, the estimated prevalence of stroke based on the 2009 NHIS was 3.8%; among whites, it was 2.5%; and among Asians, it was 1.3%. Among American Indians/Alaska Natives, the prevalence of stroke is not reported due to its large relative standard error (NHIS, NCHS).3
The prevalence of silent cerebral infarction between 55 and 64 years of age is ≈11%. This prevalence increases to 22% between 65 and 69 years of age, 28% between 70 and 74 years of age, 32% between 75 and 79 years of age, 40% between 80 and 85 years of age, and 43% at ≥85 years of age. Application of these rates to 1998 US population estimates results in an estimated 13 million people with prevalent silent stroke.4,5
The prevalence of stroke-related symptoms was found to be relatively high in a general population free of a prior diagnosis of stroke or transient ischemic attack. On the basis of data from 18 462 participants enrolled in a national cohort study, 17.8% of the population >45 years of age reported at least 1 symptom. Stroke symptoms were more likely among blacks than whites, among those with lower income and lower educational attainment, and among those with fair to poor perceived health status. Symptoms also were more likely in participants with higher Framingham stroke risk score (Reasons for Geographic and Racial Differences in Stroke study [REGARDS], National Institutes of Neurological Disorders and Stroke [NINDS]).6
Incidence
Each year, ≈795 000 people experience a new or recurrent stroke. Approximately 610 000 of these are first attacks, and 185 000 are recurrent attacks (GCNKSS, NINDS, and NHLBI; GCNKSS and NINDS data for 1999 provided July 9, 2008; estimates compiled by NHLBI). Of all strokes, 87% are ischemic, 10% are intracerebral hemorrhage, and 3% are subarachnoid hemorrhage strokes (GCNKSS, NINDS, 1999).7
On average, every 40 seconds, someone in the United States has a stroke (AHA computation based on latest available data).
Analysis of data from the FHS study of the NHLBI suggest that stroke incidence is declining over time. In this largely white cohort, data from 1950 to 1977, 1978 to 1989, and 1990 to 2004, showed that the age-adjusted incidence of first stroke per 1000 person-years in each of the 3 periods was 7.6, 6.2, and 5.3 in men and 6.2, 5.8, and 5.1 in women, respectively. Lifetime risk for incident stroke at 65 years of age decreased significantly in the latest data period compared with the first, from 19.5% to 14.5% in men and from 18.0% to 16.1% in women. Age-adjusted stroke severity did not vary across periods; however, 30-day mortality rate decreased significantly in men (from 23% to 14%), but not in women (from 21% to 20%).8
As compared with the 1990s, when incidence rates of stroke were stable, data from 2005 showed that stroke incidence was decreasing for whites but not blacks (GCNKSS 2005). Blacks continue to have a higher stroke incidence than whites, especially among young adults (GCNKSS 1999, 2005).
Blacks have a risk of first-ever stroke that is almost twice that of whites. The age-adjusted stroke incidence rates in people 45 to 84 years of age are 6.6 per 1000 population in black men, 3.6 in white men, 4.9 in black women, and 2.3 in white women (ARIC, NHLBI).7 On the basis of 1987 to 2001 data from the ARIC study sponsored by the NHLBI, stroke/ transient ischemic attack (TIA) incidence rates (per 1000 person-years) are 2.4 for white men 45 to 54 years of age, 6.1 for white men 55 to 64 years of age, and 12.2 for white men 65 to 74 years of age. For white women in the same age groups, the rates are 2.4, 4.8, and 9.8, respectively. For black men in the same age groups, the rates are 9.7, 13.1, and 16.2, and for black women, the rates are 7.2, 10.0, and 15.0, respectively.7
A study of nearly 18 000 middle-aged, predominantly white male participants in the Physicians’ Health Study found that the Southeast and Midwest had higher crude and age-standardized major CVD, total stroke, ischemic stroke, coronary revascularization, and CVD death incidence rates compared with the Northeast.9
Each year, ≈55 000 more women than men have a stroke (GCNKSS, NINDS).
National statistics from death certificate data have long shown an increase in deaths attributed to stroke for blacks because of a higher stroke incidence compared with whites, although the case-fatality rate is similar between the 2 racial groups. This racial disparity in stroke incidence does not seem to be changing over time. Community socioeconomic status appeared to explain 39% of the excess stroke incidence risk in blacks in this study.10
The BASIC project (NINDS) demonstrated an increased incidence of stroke among Mexican Americans compared with non-Hispanic whites in this community. The crude 3-year cumulative incidence was 168 per 10 000 in Mexican Americans and 136 per 10 000 in non-Hispanic whites. Specifically, Mexican Americans have a higher cumulative incidence for ischemic stroke at younger ages (45 to 59 years of age: RR 2.04; 95% CI, 1.55 to 2.69; 60 to 74 years of age: RR 1.58; 95% CI, 1.31 to 1.91), but not at older ages (≥75 years of age: RR 1.12; 95% CI, 0.94 to 1.32). Mexican Americans also have a higher incidence of intra-cerebral hemorrhage and subarachnoid hemorrhage than non-Hispanic whites, adjusted for age.11
Among 4507 American Indian participants without a prior stroke in the Strong Heart Study in 1989 to 1992, the age-and sex-adjusted incidence of stroke through 2004 was 6.79 per 100 person-years, with 86% of incident strokes being ischemic.12
The age-adjusted incidence of first ischemic stroke per 100 000 was 88 in whites, 191 in blacks, and 149 in Hispanics, according to data from the Northern Manhattan Study (NOMAS) (NINDS). Among blacks, compared with whites, the relative rate of intracranial atherosclerotic stroke was 5.85; extracranial atherosclerotic stroke, 3.18; lacunar stroke, 3.09; and cardioembolic stroke, 1.58. Among Hispanics (primarily Cuban and Puerto Rican), compared with whites, the relative rate of intracranial atherosclerotic stroke was 5.00; extracranial atherosclerotic stroke, 1.71; lacunar stroke, 2.32; and cardioembolic stroke, 1.42.13
Analysis of black and white patients in the Warfarin–Aspirin Symptomatic Intracranial Disease (WASID) trial found that blacks were significantly more likely to have an ischemic stroke, brain hemorrhage or vascular death, or ischemic stroke alone than whites.14
A review of published studies and data from clinical trials found that hospital admissions for intracerebral hemorrhage have increased by 18% in the past 10 years, probably because of increases in the number of elderly people, many of whom lack adequate blood pressure control, and the increasing use of anticoagulants, thrombolytics, and antiplatelet agents. Mexican Americans, Latin Americans, blacks, Native Americans, Japanese people, and Chinese people have higher incidences than do white Americans.15
In the GCNKSS, the annual incidence of anticoagulant-associated intracerebral hemorrhage (AAICH) per 100 000 people was 0.8 (95% CI, 0.3 to 1.3) in 1988, 1.9 (95% CI, 1.1 to 2.7) in 1993/1994, and 4.4 (95% CI, 3.2 to 5.5) in 1999 (P<0.001 for trend). Among people aged ≥80, the AAICH rate increased from 2.5 (95% CI, 0 to 7.4) in 1988 to 45.9 (95% CI, 25.6 to 66.2) in 1999 (P<0.001 for trend). Incidence rates of cardioembolic ischemic stroke were similar in 1993/1994 and 1999 (31.1 versus 30.4, P=0.65). Warfarin distribution in the United States quadrupled on a per-capita basis between 1988 and 1999.16
Transient Ischemic Attack
The number of TIAs in the United States has been estimated to be ≈200 000 to 500 000 per year, with a population prevalence of 2.3%, which translates into ≈5 million people.17
The prevalence of TIA increases significantly with older age.18
In population-based studies, the age- and sex-adjusted incidence rates for TIA range from 68.2 to 83.0 per 100 000. Men, blacks and Mexican Americans have higher rates of TIA.11,19,
Meta-analyses of cohorts of patients with TIA have shown the short-term risk of stroke after TIA to be ≈3% to 10% at 2 days and 9% to 17% at 90 days.20,21
In the North American Symptomatic Carotid Endarterectomy Trial, patients with a first-ever hemispheric TIA had a 90-day stroke risk of 20%. The risk of stroke after TIA exceeded the risk after hemispheric stroke.22
Individuals who have a TIA have a 10-year stroke risk of roughly 19% and a combined 10-year stroke, MI, or vascular death risk of 43% (4%/year).23
Approximately 15% of all strokes are heralded by a TIA.18
Within 1 year of TIA, about 12% to 13% of patients will die.24,25
Approximately half of all patients who experience a TIA fail to report it to their healthcare providers.26
One third of episodes characterized as TIAs according to the classic definition (ie, focal neurological deficits that resolve within 24 hours) would be considered infarctions on the basis of diffusion-weighted MRI findings.27
Mortality
On average, every 4 minutes, someone dies of a stroke (NCHS, NHLBI).28
Stroke accounted for ≈1 of every 18 deaths in the United States in 2007.28
When considered separately from other CVDs, stroke ranks No. 3 among all causes of death, behind diseases of the heart and cancer (NCHS mortality data). Preliminary data from the CDC released on December 9, 2010, suggest that, using the 10th version of the International Classification of Diseases (ICD-10) and reclassification of some respiratory diseases, cerebrovascular disease may now rank No. 4 among all causes of death, after diseases of the heart, cancer, and chronic lower respiratory diseases.28a
Stroke mortality in 2007 was 135 952; any-mention mortality in 2007 was 227 215 and the death rate was 42.2.28 See Chart 6-2 for sex/race comparison.
From 1997 to 2007, the annual stroke death rate decreased 34.3%, and the actual number of stroke deaths declined 18.8% (appropriate comparability ratios were applied) (NCHS Health Data Interactive Web site http://www.cdc.gov/nchs/hdi.htm accessed on July 15, 2010).
- Conclusions about changes in stroke death rates from 1980 to 2005:
-
—There was a greater decline in stroke death rates in men than in women, with a male-to-female ratio decreasing from 1.11 to 1.03 (age-adjusted).
-
—There were greater declines in stroke death rates in men than in women among people ≥65 years of age compared with younger ages.29
-
—
Approximately 54% of stroke deaths in 2007 occurred out of the hospital (unpublished NHLBI tabulation of NCHS 2007 Mortality Data Set).
Among people 45 to 64 years of age, 8% to 12% of ischemic strokes and 37% to 38% of hemorrhagic strokes result in death within 30 days, according to the ARIC study of the NHLBI.30
In a study of people ≥65 years of age recruited from a random sample of Health Care Financing Administration Medicare Part B eligibility lists in 4 US communities, the 1-month case fatality rate was 12.6% for all strokes, 8.1% for ischemic strokes, and 44.6% for hemorrhagic strokes.31
More women than men die of stroke each year due to the larger number of elderly women. Women accounted for 60.6% of US stroke deaths in 2007.
From 1995 to 1998, age-standardized mortality rates for ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage were higher among blacks than whites. Death rates from intracerebral hemorrhage also were higher among Asians/Pacific Islanders than among whites. All minority populations had higher death rates from subarachnoid hemorrhage than did whites. Among adults 25 to 44 years of age, blacks and American Indians/Alaska Natives had higher risk ratios than did whites for all 3 stroke subtypes.32
In 2002, death certificate data showed that the mean age at stroke death was 79.6 years; however, males had a younger mean age at stroke death than females. Blacks, American Indians/Alaska Natives, and Asians/Pacific Islanders had younger mean ages than whites, and the mean age at stroke death was also younger among Hispanics than non-Hispanics.33
Age-adjusted stroke mortality rates began to level off in the 1980s and stabilized in the 1990s for both men and women, according to the Minnesota Heart Study. Women had lower rates of stroke mortality than did men throughout the period. Some of the improvement in stroke mortality may be the result of improved acute stroke care, but most is thought to be the result of improved detection and treatment of hypertension.34
A report released by the CDC in collaboration with the Center for Medicare & Medicaid Services (CMS), the Atlas of Stroke Hospitalizations Among Medicare Beneficiaries, found that in Medicare beneficiaries, 30-day mortality rate varied by age: 9% in patients 65 to 74 years of age, 13.1% in those 74 to 84 years of age, and 23% in those ≥85 years of age.35
There are substantial geographic disparities in stroke mortality with higher rates in the southeastern US known as the “stroke belt.” This area is usually defined to include the eight southern states of North Carolina, South Carolina, Georgia, Tennessee, Mississippi, Alabama, Louisiana, and Arkansas. These geographic differences have existed since at least 194036 and despite some minor shifts,37 they still persist.38–40 Within the stroke belt, a “buckle” region along the coastal plain of North Carolina, South Carolina, and Georgia has been identified with even a higher stroke mortality rate than the remainder of the stroke belt.41 The overall average stroke mortality is ≈20% higher in the stroke belt than in the rest of the nation and ≈40% higher in the stroke buckle.
Chart 6-2.
Age-adjusted death rates for stroke by sex and race/ethnicity, 2007. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Stroke Risk Factors
(See Table 6-2 for data on modifiable stroke risk factors.)
TIAs confer a substantial short-term risk of stroke, hospitalization for CVD events, and death. Of 1707 TIA patients evaluated in the ED of Kaiser Permanente Northern California, a large integrated healthcare delivery system, 180 (10%) experienced a stroke within 90 days. Ninety-one patients (5%) had a stroke within 2 days. Predictors of stroke included age >60 years, DM, focal symptoms of weakness or speech impairment, and TIA that lasted >10 minutes.42
BP is a powerful determinant of risk for both ischemic stroke and intercranial hemorrhage. Subjects with BP <120/80 mm Hg have approximately half the lifetime risk of stroke of subjects with hypertension. The treatment and lowering of blood pressure among hypertensive individuals was associated with a significant reduction in stroke risk.43
In REGARDS (NINDS), black participants were more aware than whites of their hypertension and more likely to be undergoing treatment if aware of their diagnosis, but among those treated for hypertension, they were less likely than whites to have their BP controlled. There was no evidence of a difference between the stroke belt and other regions in awareness of hypertension, but there was a trend for better treatment and BP control in the stroke belt region. The lack of substantial geographic differences in hypertension awareness and the trend toward better treatment and control in the stroke belt suggest that differences in hypertension management may not be a major contributor to the geographic disparity in stroke mortality.44
Impaired glucose tolerance nearly doubled the stroke risk as compared with patients with normal glucose levels and tripled the risks for patients with diabetes mellitus.45
Atrial fibrillation (AF) is a powerful risk factor for stroke, independently increasing risk ≈5-fold throughout all ages. The percentage of strokes attributable to AF increases steeply from 1.5% at 50 to 59 years of age to 23.5% at 80 to 89 years of age.46,47
As AF is often asymptomatic48,49 and likely frequently clinically undetected,50 the stroke risk attributed to AF may be substantially underestimated.51 Therefore, although AF is an important stroke risk factor, both patients and treating physicians may be unaware of its presence. A related point is that no strategy to pursue normal sinus rhythm, including cardioversion, antiarrhythmic drug therapy and/ or ablation, has definitively been shown to reduce the risk of stroke.
The risk of ischemic stroke associated with current cigarette smoking has been shown to be approximately double that of nonsmokers after adjustment for other risk factors (FHS, CHS, Honolulu Heart Program [HHP], NHLBI).
Age-specific incidence rates and rate ratios show that diabetes increases ischemic stroke incidence at all ages, but this risk is most prominent before 55 years of age in blacks and before 65 years of age in whites. Ischemic stroke patients with DM are younger, more likely to be black, and more likely to have hypertension, MI, and high cholesterol than nondiabetic patients.52
In a recent ARIC/NHLBI study of a biracial population 45 to 64 years of age, with an average follow-up of 13.4 years, researchers found that blacks had a 3-fold higher multivariate- adjusted risk ratio of lacunar stroke than whites. In this middle-aged population, the top 3 risk factors based on the population-attributable fraction for lacunar stroke were hypertension (population-attributable fraction, 33.9%), DM (26.3%), and current smoking (22.0%).53
In the Framingham Offspring Study, 2040 individuals free of clinical stroke had an MRI scan to detect silent cerebral infarct (SCI). Prevalent SCI was associated with the Framingham Stroke Risk Profile score (OR 1.27; 95% CI, 1.10 to 1.46), hypertension (OR 1.56; 95% CI, 1.15 to 2.11), elevated plasma homocysteine (OR 2.23; 95% CI, 1.42 to 3.51), AF (OR 2.16; 95% CI, 1.07 to 4.40), carotid stenosis >25% (OR 1.62; 95% CI, 1.13 to 2.34), and increased carotid intimal-medial thickness (OR 1.65; 95% CI, 1.22 to 2.24).54
In the FHS of the NHLBI, in participants <65 years of age, the risk of developing stroke/TIA was 4.2-fold higher in those with symptoms of depression. After adjustment for components of the Framingham Stroke Risk Profile and education, similar results were obtained. In subjects ≥65 years of age, use of antidepressant medications did not alter the risk associated with depressive symptoms. Identification of depressive symptoms at younger ages may have an impact on the primary prevention of stroke.55
Data from the HHP/NHLBI found that in Japanese men 71 to 93 years of age, low concentrations of HDL cholesterol were more likely to be associated with a future risk of thromboembolic stroke than were high concentrations.56
Risk Factor Issues Specific to Women
Analysis of NHANES 1999 to 2004 data found that women 45 to 54 years of age are more than twice as likely as men to have had a stroke. Women in the 45- to 54-year age group had a >4-fold higher likelihood of having had a stroke than women 35 to 44 years of age.57
Women are older at stroke onset compared with men (75 years compared with 71 years).58
Women have lower age-adjusted stroke incidence than men; however, sex differences in stroke risk are modified by age. Data from Framingham demonstrate that compared with white men, white women 45 to 84 years have lower stroke risk than men, but this association is reversed in older ages such that women greater than 85 years have elevated risk compared with men.58 Similarly, a population-based study in Sweden found stroke incidence to be 60% lower for women than men at ages 55 to 64 years, but by 75 years of age this association reversed and women had a 50% higher incidence than men.59 The Oxford Vascular Study also showed lower stroke incidence for women than men aged 55 to 74 years, but higher incidence for women aged 85 years and older.60
Lifetime risk of stroke is greater in women compared with men because of their greater life expectancy and the fact that stroke rates increase substantially with age.61
Overall, randomized clinical trial data indicate that the use of estrogen plus progestin, as well as estrogen alone, increases stroke risk in postmenopausal, generally healthy women and provides no protection for women with established HD.62,63
Among postmenopausal women who were generally healthy, the Women’s Health Initiative (WHI), a randomized trial of 16 608 women (95% of whom had no preexisting CVD), found that estrogen plus progestin increased ischemic stroke risk by 44%, with no effect on hemorrhagic stroke. The excess risk was apparent in all age groups, in all categories of baseline stroke risk, and in women with and without hypertension or prior history of CVD.62
In the WHI trial, among 10 739 women with hysterectomy, it was found that conjugate equine estrogen alone increased the risk of ischemic stroke by 55% and that there was no significant effect on hemorrhagic stroke. The excess risk of total stroke conferred by estrogen alone was 12 additional strokes per 10 000 person-years.64
In postmenopausal women with known CHD, the Heart and Estrogen/Progestin Replacement Study (HERS), a secondary CHD prevention trial, found that a combination of estrogen plus progestin (conjugated equine estrogen [0.625 mg] and medroxyprogesterone acetate [2.5 mg]) hormone therapy did not reduce stroke risk.65
The Women’s Estrogen for Stroke Trial (WEST) found that estrogen alone (1 mg of 17β-estradiol) in women with a mean age of 71 years also had no significant overall effect on recurrent stroke or fatality, but there was an increased rate of fatal stroke and an early increase in overall stroke rate in the first 6 months of therapy.66
Analysis of data from the FHS found that women with menopause at 42 to 54 years of age and at ≥55 years of age had lower stroke risk compared with those with menopause <42 years of age, even after adjustment for potential confounders. Women with menopause before 42 years of age had twice the stroke risk compared with all other women in different age groups.67
The preponderance of evidence supports an increased risk of ischemic stroke among users of low-estrogen oral contraception.68–70 An increased relative risk of 1.93 (95% CI, 1.35 to 2.74) was found for low-estrogen preparations in population-based studies that controlled for smoking and hypertension. This translates to an additional 4.1 ischemic strokes per 100 000 nonsmoking, normotensive women using low-estrogen oral contraceptives, or 1 additional ischemic stroke per year per 24 000 such women.69
The risk of ischemic stroke or intracerebral hemorrhage during pregnancy and the first 6 weeks postpartum was 2.4 times greater than for nonpregnant women of similar age and race, according to the Baltimore-Washington Cooperative Young Stroke Study. The risk of ischemic stroke during pregnancy was not increased during pregnancy per se but was increased 8.7-fold during the 6 weeks postpartum. Intracerebral hemorrhage showed a small RR of 2.5 during pregnancy but increased dramatically to an RR of 28.3 in the 6 weeks postpartum. The excess risk of stroke (all types except subarachnoid hemorrhage) attributable to the combined pregnancy/postpregnancy period was 8.1 per 100 000 pregnancies.71
In the US Nationwide Inpatient Sample from 2000 to 2001, the rate of events per 100 000 pregnancies was 9.2 for ischemic stroke, 8.5 for intracerebral hemorrhage, 0.6 for cerebral venous thrombosis, and 15.9 for the ill-defined category of pregnancy-related cerebrovascular events, for a total rate of 34.2 per 100 000, not including subarachnoid hemorrhage. The risk was increased in blacks and among older women. Death occurred during hospitalization in 4.1% of women with these events and in 22% of survivors after discharge to a facility other than home.72
Preeclampsia is a risk factor for ischemic stroke remote from pregnancy.73 The subsequent stroke risk of preeclampsia may be mediated by a 3.6 to 6.1-fold higher later risk of hypertension and a 3.1 to 3.7-fold higher later risk of diabetes mellitus, depending on whether the preeclampsia was mild or severe.74
Physical Inactivity as a Risk Factor for Stroke
Higher levels of physical activity are associated with lower stroke risk. This relationship has been consistently demonstrated in prospective and case-control studies conducted in the United States as well as in a variety of other populations.
Results from the Physicians’ Health Study showed a 14% lower RR of stroke associated with vigorous exercise (exercise ≥5 times per week) among men.75
The Harvard Alumni Study showed that men who were highly physically active had an 18% lower RR of total stroke.76
In the Women’s Health Study, a dose-response relationship between level of leisure-time walking time and pace and risk of stroke was demonstrated, with higher levels of activity associated with 20% to 40% reduction in risk.77
In NOMAS, a prospective cohort that included white, black, and Hispanic men and women in an urban setting who were followed for a median of 9 years, baseline physical activity was associated with an overall 35% reduction in risk of ischemic stroke.78
In this analysis, an interaction between sex and activity intensity was seen, with moderate to heavy activity associated with a 60% reduction in risk of ischemic stroke in men, but no association was seen in women.78
The NOMAS study found that only moderate to vigorous intensity exercise was associated with reduced stroke incidence, whereas light exercise (such as walking) showed no benefit.78
In a subanalysis of data from the ARIC study, blacks reporting sports-related activity had a 40% reduced risk of subclinical MRI-detected cerebral infarct after 6 years of follow-up.79
In contrast to studies showing little or no benefit at lower levels of exercise,78,81–82 several reports indicate a protective effect of relatively light exposure. After a median of 16 years of follow-up in the Nord-Trøndelag Health Study (HUNT),83 a single weekly episode of vigorous exercise was associated with a 50% reduction in the risk of dying from stroke in men, with no additional benefit seen with more frequent exercise. Recent findings from the Women’s Health Study77 also demonstrated an inverse association between stroke incidence and walking, but no clear relationship with vigorous-intensity activity.
Timing of physical activity in relation to stroke onset has also been examined in several studies. In a hospital-based case-control study from Heidelberg, Germany, recent activity (within the prior months) was associated with reduced odds of having a stroke or transient ischemic attack, whereas sports activity during young adulthood that was not continued showed no benefit.84 In a Danish case-control study, ischemic stroke patients were less physically active in the week preceding the stroke compared with age-and sex-matched controls, with the highest activity scores associated with greatest reduction in odds of stroke.85
Awareness of Stroke Warning Signs and Risk Factors
Correct knowledge of at least 1 stroke warning sign increased from 48% in 1995 to 68% in 2000, with no significant improvement to 2005 (68%) based on a telephone survey conducted in a biracial population in the greater Cincinnati/Northern Kentucky region. Knowledge of 3 correct warning signs was low, but increased over time; 5.4% in 1995, 12.0% in 2000, and 15.7% in 2005. Knowledge of at least 1 stroke risk factor increased from 59% in 1995% to 71% in 2000, but there was not improvement to 2005 (71%). Only 3.6% of those surveyed were able to independently identify tissue-type plasminogen activator (tPA) as an available drug therapy and only 9% of these were able to identify a window of <3 hours for treatment.86
In the 2005 BRFSS among respondents in 14 states, 38.1% were aware of 5 stroke warning symptoms and would first call 9-1-1 if they thought that someone was having a heart attack or stroke. Awareness of all 5 stroke warning symptoms and calling 9-1-1 was higher among whites versus blacks and Hispanics (41.3%, 29.5%, and 26.8%, respectively), women versus men (41.5% versus 34.5%), and people with higher versus lower educational attainment (47.6% for people with a college degree or more versus 22.5% for those who had not received a high school diploma). Among states, the same measure ranged from 27.9% (Oklahoma) to 49.7% (Minnesota).87
A study was conducted of patients admitted to an ED with possible stroke to determine their knowledge of the signs, symptoms, and risk factors of stroke. Of the 163 patients able to respond, 39% did not know a single sign or symptom. Patients ≥65 years of age were less likely than those <65 years old to know a sign or symptom of stroke (28% versus 47%), and 43% did not know a single risk factor. Overall, almost 40% of patients did not know the signs, symptoms, and risk factors of stroke.88
Among patients recruited from the Academic Medical Center Consortium, the CHS, and United HealthCare, only 41% were aware of their increased risk for stroke. Approximately 74% recalled being told of their increased stroke risk by a physician, compared with 28% who did not recall this. Younger patients, depressed patients, those in poor current health, and those with a history of TIA were most likely to be aware of their risk.89
An AHA-sponsored random-digit dialing telephone survey was conducted in mid-2003. Only 26% of women >65 years of age reported being well informed about stroke. Correct identification of the warning signs of stroke was low among all age and racial/ethnic groups.90
Among participants in a study by the National Stroke Association, 2.3% reported having been told by a physician that they had had a TIA. Of those with a TIA, only 64% saw a physician within 24 hours of the event, only 8.2% correctly related the definition of TIA, and 8.6% could identify a typical symptom. Men, people of color, and those with lower income and fewer years of education were less likely to be knowledgeable about TIA.19
In 2004, 800 adults ≥45 years of age were surveyed to assess their perceived risk for stroke and their history of stroke risk factors. Overall, 39% perceived themselves to be at risk. Younger age, current smoking, a history of DM, high BP, high cholesterol, HD, and stroke/TIA were independently associated with perceived risk for stroke. Respondents with AF were no more likely to report being at risk than were respondents without AF. Perceived risk for stroke increased as the number of risk factors increased; however, 46% of those with ≥3 risk factors did not perceive themselves to be at risk.91
A study of patients who have had a stroke found that only 60.5% were able to accurately identify 1 stroke risk factor and that 55.3% were able to identify 1 stroke symptom. Patients’ median delay time from onset of symptoms to admission in the ED was 16 hours, and only 31.6% accessed the ED in <2 hours. Analysis showed that the appearance of nonmotor symptoms as the primary symptom and nonuse of the 9-1-1 system were significant predictors of delay >2 hours. Someone other than the patient made the decision to seek treatment in 66% of the cases.92
Spanish-speaking Hispanics are less likely to know all stroke symptoms than English-speaking Hispanics, non-Hispanic blacks, and non-Hispanic whites. Lack of English proficiency is strongly associated with lack of stroke knowledge among Hispanics.93
Aftermath
Stroke is a leading cause of serious, long-term disability in the United States (Survey of Income and Program Participation, a survey of the US Bureau of the Census).94
Data from the BRFSS (CDC) 2005 survey on stroke survivors in 21 states and the District of Columbia found that 30.7% of stroke survivors received outpatient rehabilitation. The findings indicated that the prevalence of stroke survivors receiving outpatient stroke rehabilitation was lower than would be expected if clinical practice guideline recommendations for all stroke patients had been followed.
- On the basis of pooled data from the FHS, ARIC, and CHS studies of the NHLBI:
-
—The proportions of patients dead 1 year after a first stroke were as follows:
-
◦At ≥45 years of age: 28% of men and 32% of women
-
◦At 45 to 64 years of age: 16% of white men, 21% of white women, 19% of black men, and 19% of black women
-
◦At ≥65 years of age: 31% of white men, 35% of white women, 27% of black men, and 29% of black women
-
◦
-
—The proportions of patients dead within 5 years after a first stroke were as follows:
-
◦At ≥45 years of age: 52% of men and 56% of women
-
◦At 45 to 64 years of age: 27% of white men, 31% of white women, 36% of black men, and 42% of black women
-
◦At ≥65 years of age: 58% of white men, 61% of white women, 52% of black men, and 53% of black women
-
◦
-
—Of those who have a first stroke, the proportions with a recurrent stroke in 5 years were as follows:
-
◦At 45 to 64 years of age: 10% of men and 20% of women
-
◦At ≥65 years of age: 20% of men and 25% of women
-
◦At 45 to 64 years of age: 13% of white men, 15% of white women, 6% of black men, and 23% of black women
-
◦At ≥65 years of age: 21% of white men, 25% of white women, 12% of black men, and 23% of black women
-
◦
-
—The median survival times after a first stroke were:
-
◦At 55 to 64 years of age: 13.1 years for men and 7.8 years for women
-
◦At 65 to 74 years of age: 6.2 years for men and 7.7 years for women
-
◦At ≥75 years of age: 2.1 years for men and 2.3 years for women
-
◦
-
—
The length of time to recover from a stroke depends on its severity. Between 50% and 70% of stroke survivors regain functional independence, but 15% to 30% are permanently disabled, and 20% require institutional care at 3 months after onset.96
- In the NHLBI’s FHS, among ischemic stroke survivors who were ≥65 years of age, these disabilities were observed at 6 months after stroke97:
-
—50% had some hemiparesis
-
—30% were unable to walk without some assistance
-
—26% were dependent in activities of daily living (ADLs)
-
—19% had aphasia
-
—35% had depressive symptoms
-
—26% were institutionalized in a nursing home
-
—
Black stroke survivors had greater activity limitations than did white stroke survivors, according to data from the NHIS (2000 to 2001, NCHS) as analyzed by the CDC.98
After stroke, women have greater disability than men. A Michigan-based stroke registry found that 33% of women had moderate to severe disability (modified Rankin score ≥4) at discharge, compared with 27% of men. In a study of 108 stroke survivors from FHS, 34% of women were disabled at 6 months (Barthel Index [BI] <60), compared with 16% of men. In the Kansas City Stroke Study, women had a 30% lower probability of achieving independence (BI ≥95) by 6 months compared with men. In the Michigan registry, women had a 63% lower probability of achieving ADL independence (BI ≥95) 3 months after discharge.97,99–101
Hospital Discharges/Ambulatory Care Visits
From 1997 to 2007, the number of inpatient discharges from short-stay hospitals with stroke as the first listed diagnosis declined from 1 018 000 to 829 000 (NHDS, NCHS). Most of the decrease was observed in men and women ≥65 years of age. (NHLBI tabulation, NHDS, NCHS)
In 2005, there was a hospitalization rate of 77.3 stays per 10 000 people >45 years of age for cerebrovascular disease. There has been a decline in the hospitalization rate for different types of cerebrovascular disease between 1997 and 2005, with the exception of hemorrhagic stroke. Between 1997 and 2005, the hospitalization rate for ischemic stroke decreased by 34%, from 54.4 to 35.9 stays per 10 000 people. The hospitalization rate for transient cerebral ischemia also decreased ≈23% during this period. Similarly, the hospitalization rate for occlusion or stenosis of precerebral arteries steadily decreased by 30% between 1997 and 2005, from 18.4 to 12.8 stays per 10 000 people. In contrast, the hospitalization rate for hemorrhagic stroke remained relatively stable during this period.102
Data from 2007 from the Hospital Discharge Survey of the NCHS showed that the average length of stay for discharges with stroke as the first-listed diagnosis was 5.3 days.
In 2003, men and women accounted for roughly the same number of hospital stays for stroke in the 18- to 44-year age group. After 65 years of age, women were the majority. Among people 65 to 84 years of age, 54.5% of stroke patients were women, whereas among the oldest age group, women constituted 69.7% of all stroke patients.103
A first-ever county-level Atlas of Stroke Hospitalizations Among Medicare Beneficiaries was released in 2008 by the CDC in collaboration with the CMS. It found that the stroke hospitalization rate for blacks was 27% higher than for the US population in general, 30% higher than for whites, and 36% higher than for Hispanics. In contrast to whites and Hispanics, the highest percentage of strokes in blacks (42.3%) occurred in the youngest Medicare age group (65 to 74 years of age).35
In 2008, the number of ambulatory care visits with stroke as the first-listed diagnosis was 3 726 000 (NAMCS, NHAMCS/NCHS).104
Stroke in Children
On the basis of pathogenic differences, pediatric strokes are typically classified as either perinatal, occurring at ≤28 days of life and including in utero strokes, or (later) childhood.
Recent estimates of the overall annual incidence of stroke in US children are 6.4 per 100 000 children (0 to 15 years) in 1999 in GCNKSS105 and 4.6 per 100 000 children (0 to 19 years) from 1997 to 2003 Kaiser Permanente of Northern California (KPNC), a large integrated healthcare delivery system.106 Approximately half of incident childhood strokes are hemorrhagic.107
The prevalence of perinatal strokes is 29 per 100 000 live births, or one per 3500 live births in the 1997 to 2003 KPNC population.106
A history of infertility, preeclampsia, prolonged rupture of membranes, and chorioamnionitis were found to be independent risk factors for perinatal arterial ischemic stroke in KPNC. The RR of perinatal stroke increased ≈25-fold, with an absolute risk of 1 per 200 deliveries, when ≥3 of antenatally determined risk factors were present.108
Although children with sickle cell disease and congenital HD are at high risk for ischemic stroke, the most common cause in a previously healthy child is a cerebral arteriopathy, found in approximately two thirds of cases.109
Thrombophilias (genetic and acquired) are risk factors for childhood stroke, with summary ORs ranging from 1.6 to 8.8 in a recent meta-analysis.110
From 1979 to 1998 in the United States, childhood mortality resulting from stroke declined by 58% overall, with reductions in all major subtypes.111
The incidence of stroke in children has been stable over the past 10 years, whereas the 30-day case fatality rates were 18% in 1988 to 1989, 9% in 1993 to 1994, and 9% in 1999 in the GCNKSS population. The previously reported nationwide decrease in overall stroke mortality in children might be due to decreasing case fatality after stroke and not decreasing stroke incidence.105
Compared with girls, boys have a 1.28-fold higher risk of stroke.112 Compared with white children, black children have a 2-fold risk of both incident stroke and death from stroke.111,112 The increased risk among blacks is not fully explained by the presence of sickle cell disease, nor is the excess risk among boys fully explained by trauma.112
At a mean follow-up time of 2.1 years, 37% of 123 childhood ischemic stroke survivors had full recovery, 20% had mild deficits, 26% had moderate deficits, and 16% had severe deficits.113 Concomitant involvement of the basal ganglia, cerebral cortex, and posterior limb of the internal capsule predicts a persistent hemiparesis.114
After adjusting for routine healthcare costs, the average 5-year cost of a neonatal stroke was $51 719 and of a childhood stroke was $135 161. Costs in children with stroke continued to exceed that in age-matched control children even in the fifth year by an average of $2016.115
Despite current treatment, 1 of 10 children with ischemic or hemorrhagic stroke will have a recurrence within 5 years.116,117 The 5-year recurrence risk is as high as 60% among children with cerebral arteriopathy. The recurrence risk after perinatal stroke, however, is negligible.118
Sickle cell disease is the most important cause of ischemic stroke among black children. The Stroke Prevention Trial in Sickle Cell Anemia (STOP), reported in 1998, demonstrated the efficacy (reduction of stroke from 10% per year to <1%) of blood transfusions for primary stroke prevention in high-risk children with sickle cell disease identified by transcranial Doppler. First-admission rates for stroke in California among children with sickle cell disease showed a dramatic decline subsequent to the publication of the STOP study.119
A second randomized clinical trial, STOP II, demonstrated that stopping transfusions after 30 months of treatment was associated with a high risk of stroke.120
Barriers to Stroke Care
Based on NHIS data, the inability to afford medications among stroke survivors increased significantly from 8.1% to 12.7% between 1997 to 2004, totaling 76 000 US stroke survivors in 2004. Compared with stroke survivors able to afford medications, those unable more frequently reported lack of transportation, no health insurance, no usual place of care, income <$20 000 and out-of-pocket medical expenses ≥$2000.121
In 2002, ≈21% of US counties did not have a hospital, 31% lacked a hospital with an ED, and 77% did not have a hospital with neurological services.122
Of patients with ischemic stroke in the California Acute Stroke Pilot Registry, 23.5% arrived at the ED within 3 hours of symptom onset, and 4.3% received thrombolysis. If all patients had called 9-1-1 immediately, the expected overall rate of thrombolytic treatment within 3 hours would have increased to 28.6%. If all patients with known onset had arrived within 1 hour and had been optimally treated, 57% could have received thrombolytic treatment.123
Data from the Paul Coverdell National Acute Stroke Registry were analyzed from the 142 hospitals that participated in the 4 registry states. More patients were transported by ambulance than by other means (43.6%). Time of stroke symptom onset was recorded for 44.8% of the patients. Among these patients, 48% arrived at the ED within 2 hours of symptom onset. Significantly fewer blacks (42.4%) arrived within 2 hours of symptom onset than did whites (49.5%), and significantly fewer nonambulance patients (36.2%) arrived within 2 hours of symptom onset than did patients transported by ambulance (58.6%). The median arrival time for all patients with known time of onset was 2.0 hours. Sixty-five percent of patients who arrived at the ED within 2 hours of onset received imaging within 1 hour of ED arrival. Significantly fewer women (62%) received imaging within 1 hour of ED arrival than men.124
A comprehensive statewide survey of hospital-based stroke prevention and treatment capabilities conducted in all emergent stroke care hospitals in North Carolina in 1998, 2003, and 2008 found that the proportion of hospitals offering certain stroke-related diagnostic tests increased over the 10-year period, with significant increases in CT angiography and diffusion-weighted MRI, but not catheter angiography. Sixteen hospitals received Joint Commission certification as Primary Stroke Centers, servicing 41% of the state’s population based on county of residence. In 2008, 96% of hospitals provided CT imaging, 59% provided diffusion-weighted MRI, 57% had a neurologist on staff, 69% had a tPA protocol, and 27% had a stroke team. Despite increases in the accessibility of specific diagnostic tests and improvements in hospitals’ organizational features, there were no major differences in hospitals’ offerings of stroke education programs in their communities.125
NHIS data from 1998 to 2002 found that younger stroke survivors (45 to 64 years) self-reported worse access to physician care and medication affordability than older stroke survivors. Compared with older patients, younger stroke survivors were more likely to be male (47% versus 52%), black (10% versus 19%), and to lack health insurance (0.4% versus 11%). Lack of health insurance was associated with reduced access to care.126
Data from 142 hospitals participating in the Paul Coverdell National Acute Stroke Registry found that fewer than 48% of stroke patients arrived at the ED within 2 hours of symptom onset in 2005 to 2006. Blacks were less likely to arrive within the 2-hour window compared with whites (42.4% versus 49.5%). Among those arriving within 2 hours, 65.2% received imaging within 1 hour of ED arrival; significantly fewer women received imaging within 1 hour as compared with men (62.9% versus 67.6%), but no differences were observed by racial group.127
Results from the Brain Attack Surveillance in Corpus Christi (BASIC) project found that women were less likely to arrive at the ED within 3 hours of stroke symptom onset than men (OR 0.7; 95% CI, 0.5 to 0.9). Mexican Americans were 40% less likely to arrive by EMS than non-Hispanic whites, even after adjustment for age, National Institutes of Health Stroke Scale (NIHSS), education, history of stroke, and insurance status. Language fluency was not associated with time to hospital arrival or use of EMS. The receipt of tPA was low (1.5%), but did not differ by sex or race.128
A national study of Academic Medical Centers found no change in the proportion of patients with stroke arriving at hospitals within 2 hours of symptom onset between 2001 and 2004 (37% versus 38%); however, the rate of IV tPA use increased over this time period (14% to 38%), suggesting system-level improvements in the organization of in-hospital care. In risk-adjusted analyses, black patients were 45% less likely to arrive within 2 hours compared with white patients.129
Receipt of time-sensitive interventions such as fibrinolytic therapy for acute stroke is contingent on access to an appropriately staffed emergency department. In 2003, 71% of the US population had access to an ED within 30 minutes, and 98% within 60 minutes. Access to teaching hospitals was more limited (16% within 30 minutes, 44% within 60 minutes). Although the majority of the US population had access to an ED within 60 minutes, rural states had lower access to all types of EDs, indicating geographic heterogeneity in rapid access to emergency care; 30-minute access ranged from 48% in Vermont to 86% in the District of Columbia.130
A study of 55 094 US veterans with ischemic stroke from 1990 to 1997 found substantial geographic variation in inpatient and outpatient healthcare utilization and outcomes. Patients in the Northeast and West were 30% more likely than those in the Midwest and South to have a neurology and/or general medicine clinic visit within 60 days of discharge and were also more likely to have both neurology and general medicine follow-up within 1 year. Mortality was lower in regions where more patients had early outpatient care after stroke.131
Patients with a discharge diagnosis of ischemic stroke were identified in 7 California hospitals participating in the California Acute Stroke Pilot Registry. Six points of care were tracked: thrombolysis, receipt of antithrombotic medications within 48 hours, prophylaxis for deep vein thrombosis, smoking cessation counseling, and prescription of lipid-lowering and antithrombotic medications at discharge. Overall, rates of optimal treatment improved for patients treated in year 2 versus year 1, with 63% receiving a perfect score in year 2 versus 44% in year 1. Rates improved significantly in 4 of the 6 hospitals and for 4 of the 6 interventions. A seventh hospital that participated in the registry but did not implement standardized orders showed no improvement in optimal treatment.132
Operations and Procedures
Among stroke or TIA patients with high-grade carotid stenosis, carotid endarterectomy has been the recommended treatment for the prevention of stroke, whereas carotid stenting has been proposed as a therapeutic option for patients at high risk for surgical revascularization.
In 2005, a total of 66 698 eligible Medicare beneficiaries underwent carotid endarterectomy and 7357 underwent carotid stenting.
There is substantial geographic variation in the age-adjusted rates of carotid endarterectomy, with a nearly nine-fold difference between the highest rate and the lowest rate.
The rate of carotid endarterectomy decreased slightly from 2003 (3.2 per 1000 person-years) to 2006 (2.7 per 1000 person-years).
From 2001 to 2006, there was a significant increase in the use of carotid imaging among Medicare beneficiaries, along with a concurrent decrease in the use of carotid revascularization procedures.
In 2007, an estimated 91 000 inpatient endarterectomy procedures were performed in the United States. Carotid endarterectomy is the most frequently performed surgical procedure to prevent stroke. (NHDS, NCHS, NHLBI tabulation).
Although rates of carotid endarterectomy in the Medicare population slightly decreased between 1998 and 2004, the use of carotid artery stenting dramatically increased.133 (see Chart 6-8)
The randomized Carotid Revascularization Endarterectomy versus Stenting Trial (CREST) compared carotid endarterectomy and stenting for symptomatic and asymptomatic carotid stenosis. There was no overall difference in the primary end point of stroke, myocardial infarction, or death. However, carotid endarterectomy showed superiority with increasing age, with the crossover point at approximately age 70, and was associated with fewer strokes, which had a greater impact on quality of life than MI.134
Cost
The direct and indirect cost of stroke in 2007 was $40.9 billion. (MEPS, NHLBI tabulation)
The estimated direct medical cost of stroke for 2007 is $25.2 billion. This includes hospital outpatient or officebased provider visits, hospital inpatient stays, emergency room visits, prescribed medicines, and home health.134
The mean expenses per person for stroke care in the United States in 2007 was estimated at $7657.135
The mean lifetime cost of ischemic stroke in the United States is estimated at $140 048. This includes inpatient care, rehabilitation, and follow-up care necessary for lasting deficits. (All numbers were converted to 1999 dollars by use of the medical component of the Consumer Price Index.)136
The estimated cost of acute pediatric stoke in the United Sates is $42 million in 2003. The mean cost of short-term hospital care was $20 927 per discharge.137
In a study of stroke costs within 30 days of an acute event between 1987 to 1989 in the Rochester Stroke Study, the average cost was $13 019 for mild ischemic strokes and $20 346 for severe ischemic strokes (4 or 5 on the Rankin Disability Scale).138
Inpatient hospital costs for an acute stroke event account for 70% of first-year poststroke costs.106
The largest components of short-term-care costs were room charges (50%), medical management (21%), and diagnostic costs (19%).139
Death within 7 days, subarachnoid hemorrhage, and stroke while hospitalized for another condition are associated with higher costs in the first year. Lower costs are associated with mild cerebral infarctions or residence in a nursing home before the stroke.138
Demographic variables (age, sex, and insurance status) are not associated with stroke cost. Severe strokes (NIHSS score >20) cost twice as much as mild strokes, despite similar diagnostic testing. Comorbidities such as ischemic HD and AF predict higher costs.139,140
The total cost of stroke from 2005 to 2050, in 2005 dollars, is projected to be $1.52 trillion for non-Hispanic whites, $313 billion for Hispanics, and $379 billion for blacks. The per capita cost of stroke estimates is highest in blacks ($25 782), followed by Hispanics ($17 201) and non-Hispanic whites ($15 597). Loss of earnings is expected to be the highest cost contributor in each race/ethnic group.141
Abbreviations Used in Chapter 6
- AAICH
anticoagulant-associated intracerebral hemorrhage
- AF
atrial fibrillation
- ADL
activities of daily living
- AHA
American Heart Association
- ARIC
Atherosclerosis Risk in Communities study
- BASIC
Brain Attack Surveillance in Corpus Christi
- BI
Barthel Index
- BMI
body mass index
- BP
blood pressure
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CHD
coronary heart disease
- CHS
Cardiovascular Health Study
- CI
confidence interval
- CMS
Center for Medicare & Medicaid Services
- CREST
Carotid Revascularization Endarterectomy versus Stenting Trial
- CVD
cardiovascular disease
- DM
diabetes mellitus
- ED
emergency department
- FHS
Framingham Heart Study
- GCNKSS
Greater Cincinnati/Northern Kentucky Stroke Study
- HD
heart disease
- HDL
high-density lipoprotein
- HERS
Heart and Estrogen/Progestin Replacement Study
- HHP
Honolulu Heart Program
- HUNT
Nord-Trøndelag Health Study
- ICD
International Classification of Diseases
- KPNC
Kaiser Permanente of Northern California
- MEPS
Medical Expenditure Panel Survey
- MI
myocardial infarction
- mm Hg
millimeters of mercury
- MRI
magnetic resonance imaging
- NAMCS
National Ambulatory Medical Care Survey
- NCHS
National Center for Health Statistics
- NH
non-Hispanic
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- NHANES
National Health and Nutrition Examination Survey
- NHDS
National Hospital Discharge Survey
- NHIS
National Health Interview Survey
- NHLBI
National Heart, Lung, and Blood Institute
- NIHSS
National Institutes of Health Stroke Scale
- NINDS
National Institutes of Neurological Disorders and Stroke
- NOMAS
Northern Manhattan Study
- OR
odds ratio
- REGARDS
Reasons for Geographic and Racial Differences in Stroke study
- RR
relative risk
- SCI
silent cerebral infarct
- STOP
Stroke Prevention Trial in Sickle Cell Anemia
- TIA
transient ischemic attack
- tPA
tissue-type plasminogen activator
- WASID
Warfarin–Aspirin Symptomatic Intracranial Disease Trial
- WEST
Women’s Estrogen for Stroke Trial
- WHI
Women’s Health Initiative
- 1.Centers for Disease Control and Prevention (CDC) Prevalence of stroke: United States, 2005. MMWR Morb Mortal Wkly Rep. 2007;56:469–474. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Data. Atlanta, Ga: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2009. [Accessed September 15, 2010]. Prevalence and trends data. Available at: http://apps.nccd.cdc.gov/brfss/index.asp. [Google Scholar]
- 3.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. [Accessed August 26, 2010];Vital Health Stat 10. 2010 (247) Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_247.pdf. [PubMed]
- 4.Howard G, Wagenknecht LE, Cai J, Cooper L, Kraut MA, Toole JF. Cigarette smoking and other risk factors for silent cerebral infarction in the general population. Stroke. 1998;29:913–917. doi: 10.1161/01.str.29.5.913. [DOI] [PubMed] [Google Scholar]
- 5.Bryan RN, Wells SW, Miller TJ, Elster AD, Jungreis CA, Poirier VC, Lind BK, Manolio TA. Infarctlike lesions in the brain: prevalence and anatomic characteristics at MR imaging of the elderly: data from the Cardiovascular Health Study. Radiology. 1997;202:47–54. doi: 10.1148/radiology.202.1.8988191. [DOI] [PubMed] [Google Scholar]
- 6.Howard VJ, McClure LA, Meschia JF, Pulley L, Orr SC, Friday GH. High prevalence of stroke symptoms among persons without a diagnosis of stroke or transient ischemic attack in a general population: the REasons for Geographic And Racial Differences in Stroke (REGARDS) Study. Arch Intern Med. 2006;166:1952–1958. doi: 10.1001/archinte.166.18.1952. [DOI] [PubMed] [Google Scholar]
- 7.Incidence and Prevalence: 2006 Chart Book on Cardiovascular and Lung Diseases. Bethesda, Md: National Heart, Lung, and Blood Institute; 2006. [Google Scholar]
- 8.Carandang R, Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Kannel WB, Wolf PA. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. JAMA. 2006;296:2939–2946. doi: 10.1001/jama.296.24.2939. [DOI] [PubMed] [Google Scholar]
- 9.Rich DQ, Gaziano JM, Kurth T. Geographic patterns in overall and specific cardiovascular disease incidence in apparently healthy men in the United States. Stroke. 2007;38:2221–2227. doi: 10.1161/STROKEAHA.107.483719. [DOI] [PubMed] [Google Scholar]
- 10.Kleindorfer D. Sociodemographic groups at risk: race/ethnicity. Stroke. 2009;40(suppl):S75–S78. doi: 10.1161/STROKEAHA.108.534909. [DOI] [PubMed] [Google Scholar]
- 11.Morgenstern LB, Smith MA, Lisabeth LD, Risser JM, Uchino K, Garcia N, Longwell PJ, McFarling DA, Akuwumi O, Al-Wabil A, Al-Senani F, Brown DL, Moyé LA. Excess stroke in Mexican Americans compared with non-Hispanic Whites: the Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol. 2004;160:376–383. doi: 10.1093/aje/kwh225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Y, Galloway JM, Welty TK, Wiebers DO, Whisnant JP, Devereux RB, Kizer JR, Howard BV, Cowan LD, Yeh J, Howard WJ, Wang W, Best L, Lee ET. Incidence and risk factors for stroke in American Indians: The Strong Heart Study. Circulation. 2008;118:1577–1584. doi: 10.1161/CIRCULATIONAHA.108.772285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.White H, Boden-Albala B, Wang C, Elkind MS, Rundek T, Wright CB, Sacco RL. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005;111:1327–1331. doi: 10.1161/01.CIR.0000157736.19739.D0. [DOI] [PubMed] [Google Scholar]
- 14.Waddy SP, Cotsonis G, Lynn MJ, Frankel MR, Chaturvedi S, Williams JE, Chimowitz M. Racial differences in vascular risk factors and outcomes of patients with intracranial atherosclerotic arterial stenosis. Stroke. 2009;40:719–725. doi: 10.1161/STROKEAHA.108.526624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qureshi AI, Mendelow AD, Hanley DF. Intracerebral haemorrhage. Lancet. 2009;373:1632–1644. doi: 10.1016/S0140-6736(09)60371-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flaherty ML, Kissela B, Woo D, Kleindorfer D, Alwell K, Sekar P, Moomaw CJ, Haverbusch M, Broderick JP. The increasing incidence of anticoagulant-associated intracerebral hemorrhage. Neurology. 2007;68:116–121. doi: 10.1212/01.wnl.0000250340.05202.8b. [DOI] [PubMed] [Google Scholar]
- 17.Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldman E, Hatsukami TS, Higashida RT, Johnston SC, Kidwell CS, Lutsep HL, Miller E, Sacco RL. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. Stroke. 2009;40:2276–2293. doi: 10.1161/STROKEAHA.108.192218. [DOI] [PubMed] [Google Scholar]
- 18.Hankey GJ. Impact of treatment of people with transient ischemic attack on stroke incidence and public health. Cerebrovasc Dis. 1996;6(suppl 1):26–33. [Google Scholar]
- 19.Hill MD, Yiannakoulias N, Jeerakathil T, Tu JV, Svenson LW, Schopflocher DP. The high risk of stroke immediately after transient ischemic attack: a population-based study. Neurology. 2004;62:2015–2020. doi: 10.1212/01.wnl.0000129482.70315.2f. [DOI] [PubMed] [Google Scholar]
- 20.Wu CM, McLaughlin K, Lorenzetti DL, Hill MD, Manns BJ, Ghali WA. Early risk of stroke after transient ischemic attack: a systematic review and meta-analysis. Arch Intern Med. 2007;167:2417–2422. doi: 10.1001/archinte.167.22.2417. [DOI] [PubMed] [Google Scholar]
- 21.Giles MF, Rothwell PM. Risk of stroke early after transient ischaemic attack: a systematic review and meta-analysis. Lancet Neurol. 2007;6:1063–1072. doi: 10.1016/S1474-4422(07)70274-0. [DOI] [PubMed] [Google Scholar]
- 22.Eliasziw M, Kennedy J, Hill MD, Buchan AM, Barnett HJ North American Symptomatic Carotid Endarterectomy Trial Group. Early risk of stroke after a transient ischemic attack in patients with internal carotid artery disease. CMAJ. 2004;170:1105–1109. doi: 10.1503/cmaj.1030460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark TG, Murphy MF, Rothwell PM. Long term risks of stroke, myocardial infarction, and vascular death in “low-risk” patients with a non-recent transient ischaemic attack. J Neurol Neurosurg Psychiatry. 2003;74:577–580. doi: 10.1136/jnnp.74.5.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kleindorfer D, Panagos P, Pancioli A, Khoury J, Kissela B, Woo D, Schneider A, Alwell K, Jauch E, Miller R, Moomaw C, Shukla R, Broderick JP. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke. 2005;36:720–723. doi: 10.1161/01.STR.0000158917.59233.b7. [DOI] [PubMed] [Google Scholar]
- 25.Sherman DG. Reconsideration of TIA diagnostic criteria. Neurology. 2004;62(suppl 6):S20–S21. doi: 10.1212/wnl.62.8_suppl_6.s20. [DOI] [PubMed] [Google Scholar]
- 26.Johnston SC, Fayad PB, Gorelick PB, Hanley DF, Shwayder P, van Husen D, Weiskopf T. Prevalence and knowledge of transient ischemic attack among US adults. Neurology. 2003;60:1429–1434. doi: 10.1212/01.wnl.0000063309.41867.0f. [DOI] [PubMed] [Google Scholar]
- 27.Ovbiagele B, Kidwell CS, Saver JL. Epidemiological impact in the United States of a tissue-based definition of transient ischemic attack. Stroke. 2003;34:919–924. doi: 10.1161/01.STR.0000064323.65539.A7. [DOI] [PubMed] [Google Scholar]
- 28.Xu J, Kochanek KD, Murphy S, Tejada-Vera B. Deaths: Final Data for 2007. Natl Vital Stat Rep. 2010:58. Also available at: http://www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_19.pdf. [PubMed]
- 28a.Minino AM, Xu J, Kochanek KD. Hyattsville, MD: National Center for Health Statistics; 2010. [Accessed December 9, 2010]. Deaths: Preliminary Data for 2008. National Vital Statistics Reports, Vol 59, No 2. Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_02.pdf. [PubMed] [Google Scholar]
- 29.National Center for Health Statistics. NCHS Health Data Interactive web site. [Accessed July 15, 2010]; Available at: http://www.cdc.gov/nchs/hdi.htm.
- 30.Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, Copper LS, Shahar E. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerotic Risk in Communities (ARIC) cohort. Stroke. 1999;30:736–743. doi: 10.1161/01.str.30.4.736. [DOI] [PubMed] [Google Scholar]
- 31.El-Saed A, Kuller LH, Newman AB, Lopez O, Costantino J, McTigue K, Cushman M, Kronmal R. Geographic variations in stroke incidence and mortality among older populations in four US communities. Stroke. 2006;37:1975–1979. doi: 10.1161/01.STR.0000231453.98473.67. [DOI] [PubMed] [Google Scholar]
- 32.Ayala C, Greenlund KJ, Croft JB, Keenan NL, Donehoo RS, Giles WH, Kittner SJ, Marks JS. Racial/ethnic disparities in mortality by stroke subtype in the United States, 1995–1998. Am J Epidemiol. 2001;154:1057–1063. doi: 10.1093/aje/154.11.1057. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC) Disparities in deaths from stroke among persons aged <75 years: United States, 2002. MMWR Morb Mortal Wkly Rep. 2005;54:477–481. [PubMed] [Google Scholar]
- 34.Luepker RV, Arnett DK, Jacobs DR, Jr, Duval SJ, Folsom AR, Armstrong C, Blackburn H. Trends in blood pressure, hypertension control, and stroke mortality: the Minnesota Heart Survey. Am J Med. 2006;119:42–49. doi: 10.1016/j.amjmed.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 35.Casper ML, Nwaise IA, Croft JB, Nilasena DS. Atlas of Stroke Hospitalizations Among Medicare Beneficiaries. Atlanta, Ga: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 36.Lanska DJ. Geographic distribution of stroke mortality in the United States: 1939–1941 to 1979–1981. Neurology. 1993;43:1839–1851. doi: 10.1212/wnl.43.9.1839. [DOI] [PubMed] [Google Scholar]
- 37.Casper ML, Wing S, Anda RF, Knowles M, Pollard RA. The shifting stroke belt. Changes in the geographic pattern of stroke mortality in the United States, 1962 to 1988. Stroke. 1995;26:755–760. doi: 10.1161/01.str.26.5.755. [DOI] [PubMed] [Google Scholar]
- 38.Howard G, Evans GW, Pearce K, Howard VJ, Bell RA, Mayer EJ, Burke GL. Is the stroke belt disappearing? An analysis of racial, temporal, and age effects. Stroke. 1995;26:1153–1158. doi: 10.1161/01.str.26.7.1153. [DOI] [PubMed] [Google Scholar]
- 39.Perry HM, Roccella EJ. Conference report on stroke mortality in the southeastern United States. Hypertension. 1998;31:1206–1215. doi: 10.1161/01.hyp.31.6.1206. [DOI] [PubMed] [Google Scholar]
- 40.Casper ML, Barnett E, Williams GI, Jr, Halverson JA, Braham VE, Greenlund KJ. Atlas of Stroke Mortality: Racial, Ethnic, and Geographic Disparities in the United States. Atlanta, Ga: Department of Health and Human Services, Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 41.Howard G, Anderson R, Johnson NJ, Sorlie P, Russell G, Howard VJ. Evaluation of social status as a contributing factor to the stroke belt region of the United States. Stroke. 1997;28:936–940. doi: 10.1161/01.str.28.5.936. [DOI] [PubMed] [Google Scholar]
- 42.Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA. 2000;284:2901–2906. doi: 10.1001/jama.284.22.2901. [DOI] [PubMed] [Google Scholar]
- 43.ACCORD Study Group. Cushman WC, Evans GW, Byington RP, Goff DC, Jr, Grimm RH, Jr, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Howard G, Prineas R, Moy C, Cushman M, Kellum M, Temple E, Graham A, Howard V. Racial and geographic differences in awareness, treatment, and control of hypertension: the REasons for Geographic And Racial Differences in Stroke Study. Stroke. 2006;37:1171–1178. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]
- 45.Vermeer SE, Sandee W, Algra A, Koudstaal PJ, Kappelle LJ, Dippel DW Dutch TIA Trial Study Group. Impaired glucose tolerance increases stroke risk in nondiabetic patients with transient ischemic attack or minor ischemic stroke. Stroke. 2006;37:1413–1417. doi: 10.1161/01.STR.0000221766.73692.0b. [DOI] [PubMed] [Google Scholar]
- 46.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–988. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 47.Wang TJ, Massaro JM, Levy D, Vasan RS, Wolf PA, D’Agostino RB, Larson MG, Kannel WB, Benjamin EJ. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA. 2003;290:1049–1056. doi: 10.1001/jama.290.8.1049. [DOI] [PubMed] [Google Scholar]
- 48.Page RL, Wilkinson WE, Clair WK, McCarthy EA, Pritchett EL. Asymptomatic arrhythmias in patients with symptomatic paroxysmal atrial fibrillation and paroxysmal supraventricular tachycardia. Circulation. 1994;89:224–227. doi: 10.1161/01.cir.89.1.224. [DOI] [PubMed] [Google Scholar]
- 49.Strickberger SA, Ip J, Saksena S, Curry K, Bahnson TD, Ziegler PD. Relationship between atrial tachyarrhythmias and symptoms. Heart Rhythm. 2005;2:125–131. doi: 10.1016/j.hrthm.2004.10.042. [DOI] [PubMed] [Google Scholar]
- 50.Tayal AH, Tian M, Kelly KM, Jones SC, Wright DG, Singh D, Jarouse J, Brillman J, Murali S, Gupta R. Atrial fibrillation detected by mobile cardiac outpatient telemetry in cryptogenic TIA or stroke. Neurology. 2008;71:1696–1701. doi: 10.1212/01.wnl.0000325059.86313.31. [DOI] [PubMed] [Google Scholar]
- 51.Elijovich L, Josephson SA, Fung G, Smith WS. Intermittent atrial fibrillation may account for a large proportion of otherwise cryptogenic stroke: a study of 30-day cardiac event monitors. J Stroke Cerebrovasc Dis. 2009;18:185–189. doi: 10.1016/j.jstrokecerebrovasdis.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 52.Kissela BM, Khoury J, Kleindorfer D, Woo D, Schneider A, Alwell K, Miller R, Ewing I, Moomaw CJ, Szaflarski JP, Gebel J, Shukla R, Broderick JP. Epidemiology of ischemic stroke in patients with diabetes: the greater Cincinnati/Northern Kentucky Stroke Study. Diabetes Care. 2005;28:355–359. doi: 10.2337/diacare.28.2.355. [DOI] [PubMed] [Google Scholar]
- 53.Ohira T, Shahar E, Chambless LE, Rosamond WD, Mosley TH, Jr, Folsom AR. Risk factors for ischemic stroke subtypes: the Atherosclerosis Risk in Communities study. Stroke. 2006;37:2493–2498. doi: 10.1161/01.STR.0000239694.19359.88. [DOI] [PubMed] [Google Scholar]
- 54.Das RR, Seshadri S, Beiser AS, Kelly-Hayes M, Au R, Himali JJ, Kase CS, Benjamin EJ, Polak JF, O’Donnell CJ, Yoshita M, D’Agostino RB, Sr, DeCarli C, Wolf PA. Prevalence and correlates of silent cerebral infarcts in the Framingham Offspring Study. Stroke. 2008;39:2929–2935. doi: 10.1161/STROKEAHA.108.516575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Salaycik KJ, Kelly-Hayes M, Beiser A, Nguyen AH, Brady SM, Kase CS, Wolf PA. Depressive symptoms and risk of stroke: the Framingham Study. Stroke. 2007;38:16–21. doi: 10.1161/01.STR.0000251695.39877.ca. [DOI] [PubMed] [Google Scholar]
- 56.Curb JD, Abbott RD, Rodriguez BL, Masaki KH, Chen R, Popper JS, Petrovitch H, Ross GW, Schatz IJ, Belleau GC, Yano K. High density lipoprotein cholesterol and the risk of stroke in elderly men: the Honolulu Heart Program. Am J Epidemiol. 2004;160:150–157. doi: 10.1093/aje/kwh177. [DOI] [PubMed] [Google Scholar]
- 57.Towfighi A, Saver JL, Engelhardt R, Ovbiagele B. A midlife surge among women in the United States. Neurology. 2007;69:1898–1904. doi: 10.1212/01.wnl.0000268491.89956.c2. [DOI] [PubMed] [Google Scholar]
- 58.Petrea RE, Beiser AS, Seshadri S, Kelly-Hayes M, Kase CS, Wolf PA. Gender differences in stroke incidence and poststroke disability in the Framingham Heart Study. Stroke. 2009;40:1032–1037. doi: 10.1161/STROKEAHA.108.542894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Löfmark U, Hammarström A. Evidence for age-dependent education-related differences in men and women with first-ever stroke. Results from a community-based incidence study in northern Sweden. Neuroepidemiology. 2007;28:135–141. doi: 10.1159/000102141. [DOI] [PubMed] [Google Scholar]
- 60.Rothwell PM, Coull AJ, Silver LE, Fairhead JF, Giles MF, Lovelock CE, Redgrave JN, Bull LM, Welch SJ, Cuthbertson FC, Binney LE, Gutnikov SA, Anslow P, Banning AP, Mant D, Mehta Z Oxford Vascular Study. Population-based study of event-rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study) Lancet. 2005;366:1773–1783. doi: 10.1016/S0140-6736(05)67702-1. [DOI] [PubMed] [Google Scholar]
- 61.Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, Khatiwoda A, Lisabeth L. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7:915–926. doi: 10.1016/S1474-4422(08)70193-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wassertheil-Smoller S, Hendrix SL, Limacher M, Heiss G, Kooperberg C, Baird A, Kotchen T, Curb JD, Black H, Rossouw JE, Aragaki A, Safford M, Stein E, Laowattana S, Mysiw WJ WHI Investigators. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative: a randomized trial. JAMA. 2003;289:2673–2684. doi: 10.1001/jama.289.20.2673. [DOI] [PubMed] [Google Scholar]
- 63.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 64.Hendrix SL, Wassertheil-Smoller S, Johnson KC, Howard BV, Kooperberg C, Rossouw JE, Trevisan M, Aragaki A, Baird AE, Bray PF, Buring JE, Criqui MH, Herrington D, Lynch JK, Rapp SR, Torner J WHI Investigators. Effects of conjugated equine estrogen on stroke in the Women’s Health Initiative. Circulation. 2006;113:2425–2434. doi: 10.1161/CIRCULATIONAHA.105.594077. [DOI] [PubMed] [Google Scholar]
- 65.Simon JA, Hsia J, Cauley JA, Richards C, Harris F, Fong J, Barrett-Connor E, Hulley SB. Postmenopausal hormone therapy and risk of stroke: the Heart and Estrogen-Progestin Replacement Study (HERS) Circulation. 2001;103:638–642. doi: 10.1161/01.cir.103.5.638. [DOI] [PubMed] [Google Scholar]
- 66.Viscoli CM, Brass LM, Kernan WN, Sarrel PM, Suissa S, Horwitz RI. A clinical trial of estrogen-replacement therapy after ischemic stroke. N Engl J Med. 2001;345:1243–1249. doi: 10.1056/NEJMoa010534. [DOI] [PubMed] [Google Scholar]
- 67.Lisabeth LD, Beiser AS, Brown DL, Murabito JM, Kelly-Hayes M, Wolf PA. Age at natural menopause and risk of ischemic stroke: the Framingham Heart Study. Stroke. 2009;40:1044–1049. doi: 10.1161/STROKEAHA.108.542993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ischaemic stroke and combined oral contraceptives: results of an international, multicentre, case-control study: WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Lancet. 1996;348:498–505. [PubMed] [Google Scholar]
- 69.Gillum LA, Johnston SC. Ischemic stroke risk with oral contraceptives. JAMA. 2000;284:72–78. doi: 10.1001/jama.284.1.72. [DOI] [PubMed] [Google Scholar]
- 70.Gillum LA, Johnston SC. Oral contraceptives and stroke risk: the debate continues. Lancet Neurol. 2004;3:453–454. doi: 10.1016/S1474-4422(04)00819-1. [DOI] [PubMed] [Google Scholar]
- 71.Kittner SJ, Stern BJ, Feeser BR, Hebel R, Nagey DA, Buchholz DW, Earley CJ, Johnson CJ, Macko RF, Sloan MA, Wityk RJ, Wozniak MA. Pregnancy and the risk of stroke. N Engl J Med. 1996;335:768–774. doi: 10.1056/NEJM199609123351102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.James AH, Bushnell CD, Jamison MG, Myers ER. Incidence and risk factors for stroke in pregnancy and the puerperium. Obstet Gynecol. 2005;106:509–516. doi: 10.1097/01.AOG.0000172428.78411.b0. [DOI] [PubMed] [Google Scholar]
- 73.Brown DW, Dueker N, Jamieson DJ, Cole JW, Wozniak MA, Stern BJ, Giles WH, Kittner SJ. Preeclampsia and the risk of ischemic stroke among young women: results from the Stroke Prevention in Young Women Study. Stroke. 2006;37:1055–1059. doi: 10.1161/01.STR.0000206284.96739.ee. [DOI] [PubMed] [Google Scholar]
- 74.Lykke JA, Langhoff-Roos J, Sibai BM, Funai EF, Triche EW, Paidas MJ. Hypertensive pregnancy disorders and subsequent cardiovascular morbidity and type 2 diabetes mellitus in the mother. Hypertension. 2009;53:944–951. doi: 10.1161/HYPERTENSIONAHA.109.130765. [DOI] [PubMed] [Google Scholar]
- 75.Lee IM, Hennekens CH, Berger K, Buring JE, Manson JE. Exercise and risk of stroke in male physicians. Stroke. 1999;30:1–6. doi: 10.1161/01.str.30.1.1. [DOI] [PubMed] [Google Scholar]
- 76.Lee IM, Paffenbarger RS., Jr Physical activity and stroke incidence: the Harvard Alumni Health Study. Stroke. 1998;29:2049–2054. doi: 10.1161/01.str.29.10.2049. [DOI] [PubMed] [Google Scholar]
- 77.Sattelmair JR, Kurth T, Buring JE, Lee I. Physical activity and risk of stroke in women. Stroke. 2010;41:1243–1250. doi: 10.1161/STROKEAHA.110.584300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Willey JZ, Xu Q, Boden-Albala B, Paik MC, Moon YP, Sacco RL, Elkind MS. Lipid profile components and risk of ischemic stroke: The Northern Manhattan Study (NOMAS) Arch Neurol. 2009;66:1400–1406. doi: 10.1001/archneurol.2009.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dubbert PM, Penman AD, Evenson KR, Reeves RR, Mosley TH., Jr Physical activity and subclinical MRI cerebral infarcts: The ARIC Study. J Neurol Sci. 2009;284:135–139. doi: 10.1016/j.jns.2009.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Williams PT. Reduction in incident stroke risk with vigorous physical activity: evidence from 7.7-year follow-up of the National Runners’ Health Study. Stroke. 2009;40:1921–1923. doi: 10.1161/STROKEAHA.108.535427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liang W, Lee AH, Binns CW, Zhou A, Huang R, Hu D. Habitual physical activity reduces the risk of ischemic stroke: a case-control study in southern China. Cerebrovasc Dis. 2009;28:454–459. doi: 10.1159/000235990. [DOI] [PubMed] [Google Scholar]
- 82.Boone-Heinonen J, Evenson KR, Taber DR, Gordon-Larsen P. Walking for prevention of cardiovascular disease in men and women: a systematic review of observational studies. Obes Rev. 2009;10:204–217. doi: 10.1111/j.1467-789X.2008.00533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wisløff U, Nilsen TIL, Drøyvold B, Mørkved S, Slørdahl SA, Vatten LJ. A single weekly bout of exercise may reduce cardiovascular mortality: how little pain for cardiac gain? ‘The HUNT study, Norway.’. Eur J Cardiovasc Prev Rehabil. 2006;13:798–804. doi: 10.1097/01.hjr.0000216548.84560.ac. [DOI] [PubMed] [Google Scholar]
- 84.Grau AJ, Barth C, Geletneky B, Ling P, Palm F, Lichy C, Becher H, Buggle F. Association between recent sports activity, sports activity in young adulthood, and stroke. Stroke. 2009;40:426–431. doi: 10.1161/STROKEAHA.108.527978. [DOI] [PubMed] [Google Scholar]
- 85.Krarup LH, Truelsen T, Pedersen A, Lerke H, Lindahl M, Hansen L, Schnohr P, Boysen G. Level of physical activity in the week preceding an ischemic stroke. Cerebrovasc Dis. 2007;24:296–300. doi: 10.1159/000105683. [DOI] [PubMed] [Google Scholar]
- 86.Kleindorfer D, Khoury J, Broderick JP, Rademacher E, Woo D, Flaherty ML, Alwell K, Moomaw CJ, Schneider A, Pancioli A, Miller R, Kissela BM. Temporal trends in public awareness of stroke: warning signs, risk factors, and treatment. Stroke. 2009;40:2502–2506. doi: 10.1161/STROKEAHA.109.551861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Centers for Disease Control and Prevention (CDC) Awareness of stroke warning symptoms: 13 states and the District of Columbia, 2005. MMWR Morb Mortal Wkly Rep. 2008;57:481–485. [PubMed] [Google Scholar]
- 88.Kothari R, Sauerbeck L, Jauch E, Broderick J, Brott T, Khoury J, Liu T. Patient’s awareness of stroke signs, symptoms, and risk factors. Stroke. 1997;28:1871–1875. doi: 10.1161/01.str.28.10.1871. [DOI] [PubMed] [Google Scholar]
- 89.Samsa GP, Cohen SJ, Goldstein LB, Bonito AJ, Duncan PW, Enarson C, DeFriese GH, Horner RD, Matchar DB. Knowledge of risk among patients at increased risk for stroke. Stroke. 1997;28:916–921. doi: 10.1161/01.str.28.5.916. [DOI] [PubMed] [Google Scholar]
- 90.Ferris A, Robertson RM, Fabunmi R, Mosca American Heart Association and American Stroke Association national survey of stroke risk awareness among women. Circulation. 2005;111:1321–1326. doi: 10.1161/01.CIR.0000157745.46344.A1. [DOI] [PubMed] [Google Scholar]
- 91.Harwell TS, Blades LL, Oser CS, Dietrich DW, Okon NJ, Rodriguez DV, Burnett AM, Russell JA, Allen MJ, Fogle CC, Helgerson SD, Gohdes D. Perceived risk for developing stroke among older adults. Prev Med. 2005;41:791–794. doi: 10.1016/j.ypmed.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 92.Zerwic J, Hwang SY, Tucco L. Interpretation of symptoms and delay in seeking treatment by patients who have had a stroke: exploratory study. Heart Lung. 2007;36:25–34. doi: 10.1016/j.hrtlng.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 93.DuBard CA, Garrett J, Gizlice Z. Effect of language on heart attack and stroke awareness among U.S. Hispanics. Am J Prev Med. 2006;30:189–196. doi: 10.1016/j.amepre.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 94.Centers for Disease Control and Prevention (CDC) Prevalence of disabilities and associated health conditions among adults: United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50:120–125. [PubMed] [Google Scholar]
- 95.Centers for Disease Control and Prevention (CDC) Outpatient rehabilitation among stroke survivors: 21 states and the District of Columbia, 2005. MMWR Morb Mortal Wkly Rep. 2007;56:504–507. [PubMed] [Google Scholar]
- 96.Asplund K, Stegmayr B, Peltonen M. From the twentieth to the twenty-first century: a public health perspective on stroke. In: Ginsberg MD, Bogousslavsky J, editors. Cerebrovascular Disease Pathophysiology, Diagnosis, and Management. Malden, Mass: Blackwell Science; 1998. p. 2. [Google Scholar]
- 97.Kelly-Hayes M, Beiser A, Kase CS, Scaramucci A, D’Agostino RB, Wolf PA. The influence of gender and age on disability following ischemic stroke: the Framingham study. J Stroke Cerebrovasc Dis. 2003;12:119–126. doi: 10.1016/S1052-3057(03)00042-9. [DOI] [PubMed] [Google Scholar]
- 98.Centers for Disease Control and Prevention (CDC) Differences in disability among black and white stroke survivors: United States, 2000–2001. MMWR Morb Mortal Wkly Rep. 2005;54:3–6. [PubMed] [Google Scholar]
- 99.Roquer J, Campello AR, Gomis M. Sex differences in first-ever acute stroke. Stroke. 2003;34:1581–1585. doi: 10.1161/01.STR.0000078562.82918.F6. [DOI] [PubMed] [Google Scholar]
- 100.Gargano JW, Reeves MJ Paul Coverdell National Acute Stroke Registry Michigan Prototype Investigators. Sex differences in stroke recovery and stroke-specific quality of life: results from a statewide stroke registry. Stroke. 2007;38:2541–2548. doi: 10.1161/STROKEAHA.107.485482. [DOI] [PubMed] [Google Scholar]
- 101.Lai SM, Duncan PW, Dew P, Keighley J. Sex differences in stroke recovery. Prev Chronic Dis. 2005;2:A13. [PMC free article] [PubMed] [Google Scholar]
- 102.Russo CA, Andrews RM. Hospital Stays for Stroke and Other Cerebrovascular Diseases, 2005. Rockville, Md: Agency for Healthcare Research and Quality; 2008. May, [Accessed September 15, 2010]. HCUP Statistical Brief No. 51. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb51.pdf. [PubMed] [Google Scholar]
- 103.Elixhauser A, Jiang HJ. Hospitalizations for Women With Circulatory Disease, 2003. Rockville, Md: Agency for Healthcare Research and Quality; 2006. May, HCUP Statistical Brief No. 5. [PubMed] [Google Scholar]
- 104.Centers for Disease Control and Prevention. National Center for Health Statistics. Unpublished data. For methodology, see National Center for Health Statistics, Public Use Data File Documentation: 2008 National Ambulatory Medical Care Survey and Public Use Data File Documentation: 2008 National Hospital Ambulatory Medical Care Survey. [Accessed August 31, 2010];2008 National Ambulatory Medical Care Survey and 2008 National Hospital Ambulatory Medical Care Survey. http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm.
- 105.Kleindorfer D, Khoury J, Kissela B, Alwell K, Woo D, Miller R, Schneider A, Moomaw C, Broderick JP. Temporal trends in the incidence and case fatality of stroke in children and adolescents. J Child Neurol. 2006;21:415–418. doi: 10.1177/08830738060210050301. [DOI] [PubMed] [Google Scholar]
- 106.Agrawal N, Johnston SC, Wu YW, Sidney S, Fullerton HJ. Imaging data reveal a higher pediatric stroke incidence than prior US estimates. Stroke. 2009;40:3415–3421. doi: 10.1161/STROKEAHA.109.564633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Broderick J, Brott T, Kothari R, Miller R, Khoury J, Pancioli A, Gebel J, Mills D, Minneci L, Shukla R. The Greater Cincinnati/Northern Kentucky Stroke Study: preliminary first-ever and total incidence rates of stroke among blacks. Stroke. 1998;29:415–421. doi: 10.1161/01.str.29.2.415. [DOI] [PubMed] [Google Scholar]
- 108.Lee J, Croen LA, Backstrand KH, Yoshida CK, Henning LH, Lindan C, Ferriero DM, Fullerton HJ, Barkovich AJ, Wu YW. Maternal and infant characteristics associated with perinatal arterial stroke in the infant. JAMA. 2005;293:723–729. doi: 10.1001/jama.293.6.723. [DOI] [PubMed] [Google Scholar]
- 109.Ganesan V, Prengler M, McShane M, Wade A, Kirkham F. Investigation of risk factors in children with arterial ischemic stroke. Ann Neurol. 2003;53:167–173. doi: 10.1002/ana.10423. [DOI] [PubMed] [Google Scholar]
- 110.Kenet G, Lütkhoff LK, Albisetti M, Bernard T, Bonduel M, Brandao L, Chabrier S, Chan A, deVeber G, Fiedler B, Fullerton HJ, Goldenberg NA, Grabowski E, Günther G, Heller C, Holzhauer S, Iorio A, Journeycake J, Junker R, Kirkham FJ, Kurnik K, Lynch JK, Male C, Manco-Johnson M, Mesters R, Monagle P, van Ommen CH, Raffini L, Rostásy K, Simioni P, Sträter RD, Young G, Nowak-Göttl U. Impact of thrombophilia on risk of arterial ischemic stroke or cerebral sinovenous thrombosis in neonates and children: a systematic review and meta-analysis of observational studies. Circulation. 2010;121:1838–1847. doi: 10.1161/CIRCULATIONAHA.109.913673. [DOI] [PubMed] [Google Scholar]
- 111.Fullerton HJ, Chetkovich DM, Wu YW, Smith WS, Johnston SC. Deaths from stroke in US children, 1979 to 1998. Neurology. 2002;59:34–39. doi: 10.1212/wnl.59.1.34. [DOI] [PubMed] [Google Scholar]
- 112.Fullerton HJ, Wu YW, Zhao S, Johnston SC. Risk of stroke in children: ethnic and gender disparities. Neurology. 2003;61:189–194. doi: 10.1212/01.wnl.0000078894.79866.95. [DOI] [PubMed] [Google Scholar]
- 113.deVeber GA, MacGregor D, Curtis R, Mayank S. Neurologic outcome in survivors of childhood arterial ischemic stroke and sinovenous thrombosis. J Child Neurol. 2000;15:316–324. doi: 10.1177/088307380001500508. [DOI] [PubMed] [Google Scholar]
- 114.Boardman JP, Ganesan V, Rutherford MA, Saunders DE, Mercuri E, Cowan F. Magnetic resonance image correlates of hemiparesis after neonatal and childhood middle cerebral artery stroke. Pediatrics. 2005;115:321–326. doi: 10.1542/peds.2004-0427. [DOI] [PubMed] [Google Scholar]
- 115.Gardner MA, Hills NK, Sidney S, Johnston SC, Fullerton HJ. The 5-year direct medical cost of neonatal and childhood stroke in a population-based cohort. Neurology. 2010;74:372–378. doi: 10.1212/WNL.0b013e3181cbcd48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sträter R, Becker S, von Eckardstein A, Heinecke A, Gutsche S, Junker R, Kurnik K, Schobess R, Nowak-Göttl U. Prospective assessment of risk factors for recurrent stroke during childhood: a 5-year follow-up study. Lancet. 2002;360:1540–1545. doi: 10.1016/S0140-6736(02)11520-0. [DOI] [PubMed] [Google Scholar]
- 117.Fullerton HJ, Wu YW, Sidney S, Claiborne Johnston S. Recurrent hemorrhagic stroke in children: a population-based cohort study. Stroke. 2007;38:2658–2662. doi: 10.1161/STROKEAHA.107.481895. [DOI] [PubMed] [Google Scholar]
- 118.Fullerton HJ, Wu YW, Sidney S, Johnston SC. Risk of recurrent childhood arterial ischemic stroke in a population-based cohort: the importance of cerebrovascular imaging. Pediatrics. 2007;119:495–501. doi: 10.1542/peds.2006-2791. [DOI] [PubMed] [Google Scholar]
- 119.Fullerton HJ, Adams RJ, Zhao S, Johnston SC. Declining stroke rates in Californian children with sickle cell disease. Blood. 2004;104:336–339. doi: 10.1182/blood-2004-02-0636. [DOI] [PubMed] [Google Scholar]
- 120.Adams RJ, Brambilla D Optimizing Stroke Prevention in Sickle Cell Anemia Investigative Team (STOP 2) Discontinuing prophylactic transfusions used to prevent stroke in sickle cell disease. N Engl J Med. 2005;353:2769–2778. doi: 10.1056/NEJMoa050460. [DOI] [PubMed] [Google Scholar]
- 121.Levine DA, Kiefe CI, Howard G, Howard VJ, Williams OD, Allison JJ. Reduced medication access: a marker for vulnerability in US stroke survivors. Stroke. 2007;38:1557–1564. doi: 10.1161/STROKEAHA.106.478545. [DOI] [PubMed] [Google Scholar]
- 122.Centers for Disease Control and Prevention. First-ever county level report on stroke hospitalizations. [Accessed September 27, 2010];CDC Press Release. 2008 Mar 28; http://www.cdc.gov/media/pressrel/2008/r080328.htm.
- 123.California Acute Stroke Pilot Registry (CASPR) Investigators. Prioritizing interventions to improve rates of thrombolysis for ischemic stroke. Neurology. 2005;64:654–659. doi: 10.1212/01.WNL.0000151850.39648.51. [DOI] [PubMed] [Google Scholar]
- 124.Centers for Disease Control and Prevention (CDC) Prehospital and hospital delays after stroke onset: United States, 2005–2006. MMWR Morb Mortal Wkly Rep. 2007;56:474–478. [PubMed] [Google Scholar]
- 125.Goldstein LB. Statewide hospital-based stroke services in north carolina: changes over 10 years. Stroke. 2010;41:778–783. doi: 10.1161/STROKEAHA.109.572750. [DOI] [PubMed] [Google Scholar]
- 126.Levine DA, Kiefe CI, Houston TK, Allison JJ, McCarthy EP, Ayanian JZ. Younger stroke survivors have reduced access to physician care and medications: National Health Interview Survey from years 1998 to 2002. Arch Neurol. 2007;64:37–42. doi: 10.1001/archneur.64.1.noc60002. [DOI] [PubMed] [Google Scholar]
- 127.Centers for Disease Control and Prevention (CDC) Prehospital and hospital delays after stroke onset: United States, 2005–2006. MMWR Morb Mortal Wkly Rep. 2007;56:474–478. [PubMed] [Google Scholar]
- 128.Smith MA, Lisabeth LD, Bonikowski F, Morgenstern LB. The role of ethnicity, sex, and language on delay to hospital arrival for acute ischemic stroke. Stroke. 2010;41:905–909. doi: 10.1161/STROKEAHA.110.578112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lichtman JH, Watanabe E, Allen NB, Jones SB, Dostal J, Goldstein LB. Hospital arrival time and intravenous t-PA use in US academic medical centers, 2001–2004. Stroke. 2009;40:3845–3850. doi: 10.1161/STROKEAHA.109.562660. [DOI] [PubMed] [Google Scholar]
- 130.Carr BG, Branas CC, Metlay JP, Sullivan AF, Camargo CA Access to emergency care in the United States. Ann Emerg Med. 2009;54:261–269. doi: 10.1016/j.annemergmed.2008.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Williams LS, Eckert GJ, L’italien GJ, Lapuerta P, Weinberger M. Regional variation in health care utilization and outcomes in ischemic stroke. J Stroke Cerebrovasc Dis. 2003;12:259–265. doi: 10.1016/j.jstrokecerebrovasdis.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 132.California Acute Stroke Pilot Registry Investigators. The impact of standardized stroke orders on adherence to best practices. Neurology. 2005;65:360–365. doi: 10.1212/01.wnl.0000171706.68756.b7. [DOI] [PubMed] [Google Scholar]
- 133.Goodney PP, Lucas FL, Travis LL, Likosky DS, Malenka DJ, Fisher ES. Changes in the use of carotid revascularization among the medicare population. Arch Surg. 2008;143:170–173. doi: 10.1001/archsurg.2007.43. [DOI] [PubMed] [Google Scholar]
- 134.Brott TG, Hobson RW, 2nd, Howard G, Roubin GS, Clark WM, Brooks W, Mackey A, Hill MD, Leimgruber PP, Sheffet AJ, Howard VJ, Moore WS, Voeks JH, Hopkins LN, Cutlip DE, Cohen DJ, Popma JJ, Ferguson RD, Cohen SN, Blackshear JL, Silver FL, Mohr JP, Lal BK, Meschia JF CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010;363:11–23. doi: 10.1056/NEJMoa0912321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Medical Expenditure Panel Survey (MEPS) of the Agency for Healthcare Research and Quality (AHRQ) Household component summary data table. [Accessed July 31, 2010]; Available at: http://www.meps.ahrq.gov/mepsweb/data_stats/tables_compendia_hh_interactive.jsp?_SERVICE=MEPSSocket0&_PROGRAM=MEPSPGM.TC.SAS&File=HCFY2007& Table=HCFY2007_CNDXP_C&_Debug=.
- 136.Taylor TN, Davis PH, Torner JC, Holmes J, Meyer JW, Jacobson MF. Lifetime cost of stroke in the United States. Stroke. 1996;27:1459–1466. doi: 10.1161/01.str.27.9.1459. [DOI] [PubMed] [Google Scholar]
- 137.Perkins E, Stephens J, Xiang H, Lo W. The cost of pediatric stroke acute care in the United States. Stroke. 2009;40:2820–2827. doi: 10.1161/STROKEAHA.109.548156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Leibson CL, Hu T, Brown RD, Hass SL, O’Fallon WM, Whisnant JP. Utilization of acute care services in the year before and after first stroke: a population-based study. Neurology. 1996;46:861–869. [PubMed] [Google Scholar]
- 139.Diringer MN, Edwards DF, Mattson DT, Akins PT, Sheedy CW, Hsu CY, Dromerick AW. Predictors of acute hospital costs for treatment of ischemic stroke in an academic center. Stroke. 1999;30:724–728. doi: 10.1161/01.str.30.4.724. [DOI] [PubMed] [Google Scholar]
- 140.Metz R. Cost-effective, risk-free, evidence-based medicine. Arch Intern Med. 2003;163:2795. doi: 10.1001/archinte.163.22.2795-a. [DOI] [PubMed] [Google Scholar]
- 141.Brown DL, Boden-Albala B, Langa KM, Lisabeth LD, Fair M, Smith MA, Sacco RL, Morgenstern LB. Projected costs of ischemic stroke in the United States. Neurology. 2006;67:1390–1395. doi: 10.1212/01.wnl.0000237024.16438.20. [DOI] [PubMed] [Google Scholar]
- 142.Kissela B, Schneider A, Kleindorfer D, Khoury J, Miller R, Alwell K, Woo D, Szaflarski J, Gebel J, Moomaw C, Pancioli A, Jauch E, Shukla R, Broderick J. Stroke in a biracial population: the excess burden of stroke among blacks. Stroke. 2004;35:426–431. doi: 10.1161/01.STR.0000110982.74967.39. [DOI] [PubMed] [Google Scholar]
- 143.Howard G, Wagenknecht LE, Burke GL, Diez-Roux A, Evans GW, McGovern P, Nieto FJ, Tell GS. Cigarette smoking and progression of atherosclerosis: the Atherosclerosis Risk in Communities (ARIC) Study. JAMA. 1998;279:119–124. doi: 10.1001/jama.279.2.119. [DOI] [PubMed] [Google Scholar]
- 144.Whisnant JP, Wiebers DO, O’Fallon WM, Sicks JD, Frye RL. A population-based model of risk factors for ischemic stroke: Rochester, Minnesota. Neurology. 1996;47:1420–1428. doi: 10.1212/wnl.47.6.1420. [DOI] [PubMed] [Google Scholar]
- 145.Bonow RO, Carabello B, de Leon AC, Jr, Edmunds LH, Jr, Fedderly BJ, Freed MD, Gaasch WH, McKay CR, Nishimura RA, O’Gara PT, O’Rourke RA, Rahimtoola SH, Ritchie JL, Cheitlin MD, Eagle KA, Gardner TJ, Garson A, Jr, Gibbons RJ, Russell RO, Ryan TJ, Smith SC., Jr ACC/AHA guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients With Valvular Heart Disease) J Am Coll Cardiol. 1998;32:1486–1588. doi: 10.1016/s0735-1097(98)00454-9. [DOI] [PubMed] [Google Scholar]
- 146.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 147.Sacco RL, Gan R, Boden-Albala B, Lin IF, Kargman DE, Hauser WA, Shea S, Paik MC. Leisure-time physical activity and ischemic stroke risk: the Northern Manhattan Stroke Study. Stroke. 1998;29:380–387. doi: 10.1161/01.str.29.2.380. [DOI] [PubMed] [Google Scholar]
- 148.O’Leary DH, Polak JF, Kronmal RA, Kittner SJ, Bond MG, Wolfson SK, Jr, Bommer W, Price TR, Gardin JM, Savage PJ. Distribution and correlates of sonographically detected carotid artery disease in the Cardiovascular Health Study: the CHS Collaborative Research Group. Stroke. 1992;23:1752–1760. doi: 10.1161/01.str.23.12.1752. [DOI] [PubMed] [Google Scholar]
- 149.Fine-Edelstein JS, Wolf PA, O’Leary DH, Poehlman H, Belanger AJ, Kase CS, D’Agostino RB. Precursors of extracranial carotid atherosclerosis in the Framingham Study. Neurology. 1994;44:1046–1050. doi: 10.1212/wnl.44.6.1046. [DOI] [PubMed] [Google Scholar]
- 150.Yin D, Carpenter JP. Cost-effectiveness of screening for asymptomatic carotid stenosis. J Vasc Surg. 1998;27:245–255. doi: 10.1016/s0741-5214(98)70355-6. [DOI] [PubMed] [Google Scholar]
- 151.Colgan MP, Strode GR, Sommer JD, Gibbs JL, Sumner DS. Prevalence of asymptomatic carotid disease: results of duplex scanning in 348 unselected volunteers. J Vasc Surg. 1988;8:674–678. doi: 10.1067/mva.1988.avs0080674. [DOI] [PubMed] [Google Scholar]
- 152.Prati P, Vanuzzo D, Casaroli M, Di Chiara A, De Biasi F, Feruglio GA, Touboul PJ. Prevalence and determinants of carotid atherosclerosis in a general population. Stroke. 1992;23:1705–1711. doi: 10.1161/01.str.23.12.1705. [DOI] [PubMed] [Google Scholar]
- 153.Pujia A, Rubba P, Spencer MP. Prevalence of extracranial carotid artery disease detectable by echo-Doppler in an elderly population. Stroke. 1992;23:818–822. doi: 10.1161/01.str.23.6.818. [DOI] [PubMed] [Google Scholar]
- 154.Ramsey DE, Miles RD, Lambeth A, Sumner DS. Prevalence of extracranial carotid artery disease: a survey of an asymptomatic population with noninvasive techniques. J Vasc Surg. 1987;5:584–588. doi: 10.1067/mva.1987.avs0050584. [DOI] [PubMed] [Google Scholar]
- 155.Ahmed A, Adams RJ. Sickle cell disorders and cerebrovascular disease. In: Gillum RF, Gorelick PB, Cooper ES, editors. Stroke in Blacks: A Guide to Management and Prevention. Basel, Switzerland: Karger; 1999. pp. 62–69. [Google Scholar]
- 156.National Institutes of Health. Adult Treatment Panel III: Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Bethesda, Md: National Institutes of Health; 2002. [Google Scholar]
- 157.Institute of Medicine. Dietary Reference Intakes: Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: National Academies Press; 2004. [Google Scholar]
- 158.Boushey CJ, Beresford SA, Omenn GS, Motulsky AG. A quantitative assessment of plasma homocysteine as a risk factor for vascular disease: probable benefits of increasing folic acid intakes. JAMA. 1995;274:1049–1057. doi: 10.1001/jama.1995.03530130055028. [DOI] [PubMed] [Google Scholar]
- 159.Majumdar SR, Almasi EA, Stafford RS. Promotion and prescribing of hormone therapy after report of harm by the Women’s Health Initiative. JAMA. 2004;292:1983–1988. doi: 10.1001/jama.292.16.1983. [DOI] [PubMed] [Google Scholar]
- 160.Haas JS, Kaplan CP, Gerstenberger EP, Kerlikowske K. Changes in the use of postmenopausal hormone therapy after the publication of clinical trial results. Ann Intern Med. 2004;140:184–188. doi: 10.7326/0003-4819-140-3-200402030-00009. [DOI] [PubMed] [Google Scholar]
- 161.D’Agostino RB, Wolf PA, Belanger AJ, Kannel WB. Stroke risk profile: adjustment for antihypertensive medication: the Framingham Study. Stroke. 1994;25:40–43. doi: 10.1161/01.str.25.1.40. [DOI] [PubMed] [Google Scholar]
- 162.Wilterdink JL, Easton JD. Vascular event rates in patients with atherosclerotic cerebrovascular disease. Arch Neurol. 1992;49:857–863. doi: 10.1001/archneur.1992.00530320089016. [DOI] [PubMed] [Google Scholar]
- 163.Adams RJ, McKie VC, Hsu L, Files B, Vichinsky E, Pegelow C, Abboud M, Gallagher D, Kutlar A, Nichols FT, Bonds DR, Brambilla D. Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial Doppler ultrasonography. N Engl J Med. 1998;339:5–11. doi: 10.1056/NEJM199807023390102. [DOI] [PubMed] [Google Scholar]
- 164.Welin L, Svärdsudd K, Wilhelmsen L, Larsson B, Tibblin G. Analysis of risk factors for stroke in a cohort of men born in 1913. N Engl J Med. 1987;317:521–526. doi: 10.1056/NEJM198708273170901. [DOI] [PubMed] [Google Scholar]
- 165.Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986–1998. JAMA. 2001;286:2845–2848. doi: 10.1001/jama.286.22.2845. [DOI] [PubMed] [Google Scholar]
- 166.Hart RG, Benavente O, McBride R, Pearce LA. Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta-analysis. Ann Intern Med. 1999;131:492–501. doi: 10.7326/0003-4819-131-7-199910050-00003. [DOI] [PubMed] [Google Scholar]
- 167.Hart RG. Intensity of anticoagulation to prevent stroke in patients with atrial fibrillation. Ann Intern Med. 1998;128:408. doi: 10.7326/0003-4819-128-5-199803010-00012. [DOI] [PubMed] [Google Scholar]
- 168.van Walraven C, Hart RG, Singer DE, Laupacis A, Connolly S, Petersen P, Koudstaal PJ, Chang Y, Hellemons B. Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta-analysis. JAMA. 2002;288:2441–2448. doi: 10.1001/jama.288.19.2441. [DOI] [PubMed] [Google Scholar]
- 169.Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, Culebras A, DeGraba TJ, Gorelick PB, Guyton JR, Hart RG, Howard G, Kelly-Hayes M, Nixon JVI, Sacco RL. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Stroke. 2006;37:1583–1633. doi: 10.1161/01.STR.0000223048.70103.F1. [DOI] [PubMed] [Google Scholar]
- 170.Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke. 1991;22:312–318. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- 171.Kleindorfer DO, Khoury J, Moomaw CJ, Alwell K, Woo D, Flaherty ML, Khatri P, Adeoye O, Ferioli S, Broderick JP. Stroke incidence is decreasing in whites but not in blacks: a population-based estimate of temporal trends in stroke incidence from the Greater Cincinnati/Northern Kentucky Stroke Study. Stroke. 2010;41:1326–1331. doi: 10.1161/STROKEAHA.109.575043. [DOI] [PMC free article] [PubMed] [Google Scholar]
7. High Blood Pressure
ICD-9 401 to 404, ICD-10 I10 to I15. See Tables 7-1 and 7-2 and Charts 7-1 through 7-5.
Table 7-1.
High Blood Pressure
| Population Group | Prevalence, 2008, Age ≥20 y |
Mortality,* 2007, All Ages |
Hospital Discharges, 2007, All Ages |
Estimated Cost, 2007 |
|---|---|---|---|---|
| Both sexes | 76 400 000 (33.5%) | 57 732 | 568 000 | $43.5 billion |
| Males | 36 500 000 (34.1%) | 24 984 (43.3%)† | 241 000 | … |
| Females | 39 900 000 (32.7%) | 32 748 (56.7%)† | 327 000 | … |
| NH white males | 33.9% | 18 179 | … | … |
| NH white females | 31.3% | 25 406 | … | … |
| NH black males | 43.0% | 6060 | … | … |
| NH black females | 45.7% | 6513 | … | … |
| Mexican American males | 27.8% | … | … | … |
| Mexican American females | 28.9% | … | … | … |
| Hispanic or Latino‡ ≥18 y | 21.5% | … | … | … |
| Asian or Pacific Islander‡ ≥18 y | 19.4% | 1323 | ||
| American Indians/Alaska Natives‡ ≥18 y | 21.8% | 251 | … | … |
Ellipses (…) indicate data not available;
NH indicates non-Hispanic.
Mortality data are for whites and blacks and include Hispanics.
These percentages represent the portion of total high blood pressure mortality that is for males versus females.
National Health Interview Survey (2009), National Center for Health Statistics; data are weighted percentages for Americans ≥18 years of age. Data derived from Pleis et al.16
Sources: Prevalence: National Health and Nutrition Examination Survey (2005–2008, National Center for Health Statistics) and National Heart, Lung, and Blood Institute. Percentages for racial/ethnic groups are age-adjusted for Americans ≥20 years of age. Age-specific percentages are extrapolated to the 2008 US population estimates. Mortality: National Center for Health Statistics. These data represent underlying cause of death only. Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics; data include those discharged alive, dead, or status unknown.
Cost: Medical Expenditure Panel Survey data include estimated direct costs for 2007; indirect costs calculated by National Heart, Lung, and Blood Institute for 2007.
Hypertension is defined in terms of National Health and Nutrition Examination Survey blood pressure measurements and health interviews. A subject was considered hypertensive if systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90, said “yes” to taking antihypertensive medication, or was told on 2 occasions of having hypertension.
Table 7-2.
Hypertension Awareness, Treatment, and Control: NHANES 1988–1994 and 1999–2008, by Race and Sex
| Awareness, % | Treatment, % | Control, % | ||||
|---|---|---|---|---|---|---|
| 1988 –1994 | 1999 –2008 | 1988 –1994 | 1999 –2008 | 1988 –1994 | 1999 –2008 | |
| NH white males | 63.0 | 73.5 | 46.2 | 63.8 | 22.0 | 44.1 |
| NH white females | 74.7 | 78.2 | 61.6 | 70.0 | 32.2 | 42.7 |
| NH black males | 62.5 | 70.8 | 42.3 | 60.3 | 16.6 | 35.2 |
| NH black females | 77.8 | 85.8 | 64.6 | 77.0 | 30.0 | 45.3 |
| Mexican American males | 47.8 | 59.5 | 30.9 | 46.1 | 13.5 | 30.3 |
| Mexican American females | 69.3 | 70.1 | 47.8 | 59.9 | 19.4 | 34.2 |
NH indicates non-Hispanic; NHANES indicates National Health and Nutrition Examination Survey.
Sources: NHANES (1988 –1994), (1999 –2008) and National Heart, Lung, and Blood Institute.
Chart 7-1.
Prevalence of high blood pressure in adults ≥20 years of age by age and sex (National Health and Nutrition Examination Survey: 2005–2008). Hypertension is defined as systolic blood pressure 140 mm Hg or diastolic blood pressure 90 mm Hg, taking antihypertensive medication, or being told twice by a physician or other professional that one has hypertension. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 7-5.
Extent of awareness, treatment, and control of high blood pressure by race/ethnicity and sex (National Health and Nutrition Examination Survey: 1999–2008). NH indicates non-Hispanic. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Prevalence
- HBP is defined as:
-
—SBP ≥140 mm Hg or DBP ≥90 mm Hg or taking antihypertensive medicine, or
-
—Having been told at least twice by a physician or other health professional that one has HBP.
-
—
One in 3 US adults has HBP.1
Data from NHANES 1999 to 2006 found that ≈8% of US adults have undiagnosed hypertension.2
An estimated 76 400 000 adults ≥20 years of age have HBP, extrapolated to 2008 with NHANES 2005 to 2008 data (Table 7-1).
NHANES data show that a higher percentage of men than women have hypertension until 45 years of age. From 45 to 54 and from 55 to 64 years of age, the percentages of men and women with hypertension are similar. After that, a higher percentage of women have hypertension than men.3
HBP is 2 to 3 times more common in women taking oral contraceptives, especially among obese and older women, than in women not taking them.4
Data from NHANES 2005 to 2006 found that 29% of US adults ≥18 years of age were hypertensive. The prevalence of hypertension was nearly equal between men and women; 7% of adults had HBP but had never been told that they had hypertension. Among hypertensive adults, 78% were aware of their condition, 68% were using antihypertensive medication, and 64% of those treated had their hypertension controlled.5
Data from the 2009 BRFSS/CDC indicate that the percentage of adults ≥18 years of age who had been told that they had HBP ranged from 21.6% in Minnesota to 37.6% in West Virginia. The median percentage was 28.7%.6
Older Adults
In 2007 to 2008, diagnosed chronic conditions that were more prevalent among older women than men included hypertension (58% for women, 53% for men). Ever-diagnosed conditions that were more prevalent among older men than older women included HD (38% for men, 27% for women) and DM (20% for men, 18% for women) based on data from NHIS/NCHS.7
The age-adjusted prevalence of hypertension (both diagnosed and undiagnosed) in 2003 to 2006 was 75% for older women and 65% for older men on the basis of data from NHANES/NCHS.8
Children and Adolescents
Analysis of NHES, Hispanic Health and Nutrition Examination Survey (HHANES), and NHANES/NCHS surveys of the NCHS (1963–2002) found that the BP, pre-HBP, and HBP trends in children and adolescents 8 to 17 years of age moved downward from 1963 to 1988 and upward thereafter. Pre-HBP and HBP increased 2.3% and 1%, respectively, between 1988 and 1999. Increased obesity (more so abdominal obesity than general obesity) partially explained the HBP and pre-HBP rise from 1988 to 1999. BP and HBP reversed their downward trends 10 years after the increase in the prevalence of obesity. In addition, an ethnic and sex gap appeared in 1988 for pre-HBP and in 1999 for HBP: Non-Hispanic blacks and Mexican Americans had a greater prevalence of HBP and pre-HBP than non-Hispanic whites, and the prevalence was greater in boys than in girls. In that study, HBP in children and adolescents was defined as SBP or DBP that was, on repeated measurement, ≥95th percentile.9
A study in Ohio of >14 000 children and adolescents 3 to 18 years of age who were observed at least 3 times between 1999 and 2006 found that 3.6% had hypertension. Of these, 26% had been diagnosed and 74% were undiagnosed. In addition, 3% of those with hypertension had stage 2 hypertension, and 41% of those with stage 2 hypertension were undiagnosed. Criteria for prehypertension were met by 485 children. Of these, 11% were diagnosed. In this study, HBP in children and adolescents was defined as SBP or DBP that was, on repeated measurement, ≥95th percentile.10
A study from 1988 to 1994 through 1999 to 2000 of children and adolescents 8 to 17 years of age showed that among non-Hispanic blacks, mean SBP levels increased by 1.6 mm Hg among girls and by 2.9 mm Hg among boys compared with non-Hispanic whites. Among Mexican Americans, girls’ SBP increased 1.0 mm Hg and boys’ SBP increased 2.7 mm Hg compared with non-Hispanic whites.11
Analysis of data from the Search for Diabetes in Youth Study (SEARCH), which included children 3 to 17 years of age with type 1 and type 2 DM, found the prevalence of elevated BP among those with type 1 DM to be 5.9% and the prevalence of elevated BP among those with type 2 DM to be 23.7%.12
Race/Ethnicity and HBP
The prevalence of hypertension in blacks in the United States is among the highest in the world, and it is increasing. From 1988 to 1994 through 1999 to 2002, the prevalence of HBP in adults increased from 35.8% to 41.4% among blacks, and it was particularly high among black women at 44.0%. Prevalence among whites also increased, from 24.3% to 28.1%.13
Compared with whites, blacks develop HBP earlier in life, and their average BPs are much higher. As a result, compared with whites, blacks have a 1.3-times greater rate of nonfatal stroke, a 1.8-times greater rate of fatal stroke, a 1.5-times greater rate of death due caused by HD, and a 4.2-times greater rate of end-stage kidney disease (Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure 5 and 6).
- Within the black community, rates of hypertension vary substantially.13,14
-
—Those with the highest rates are more likely to be middle-aged or older, less educated, overweight or obese, and physically inactive and are more likely to have DM.
-
—Those with the lowest rates are more likely to be younger but also overweight or obese.
-
—Those with uncontrolled HBP who are not taking antihypertensive medication tend to be male, to be younger, and to have infrequent contact with a physician.
-
—
Analysis from the REGARDS study of the NINDS suggests that efforts to raise awareness of prevalent hypertension among blacks apparently have been successful (31% greater odds in blacks relative to whites), and efforts to communicate the importance of receiving treatment for hypertension have been successful (69% greater odds among blacks relative to whites); however, substantial racial disparities remain with regard to the control of BP (SBP <140 mm Hg, DBP <90 mm Hg), with the odds of control being 27% lower in blacks than whites. In contrast, geographic disparities in hypertension awareness, treatment, and control were minimal.15
Data from the 2009 NHIS showed that black adults ≥18 years of age were more likely (32.2%) to have been told on ≥2 occasions that they had hypertension than American Indian/Alaska Native adults (21.8%), white adults (23.0%), and Asian adults (19.4%).16
The CDC analyzed death certificate data from 1995 to 2002 (any-mention mortality; ICD-9 codes 401 to 404 and ICD-10 codes I10 to I13). The results indicated that Puerto Rican Americans had a consistently higher hypertension-related death rate than all other Hispanic subpopulations and non-Hispanic whites. The age-standardized hypertension-related mortality rate was 127.2 per 100 000 population for all Hispanics, similar to that of non-Hispanic whites (135.9). The age-standardized rate for Hispanic females (118.3) was substantially lower than that observed for Hispanic males (135.9). Hypertension-related mortality rates for males were higher than rates for females for all Hispanic subpopulations. Puerto Rican Americans had the highest hypertension-related death rate among all Hispanic subpopulations (154.0); Cuban Americans had the lowest (82.5).17
Some studies suggest that Hispanic Americans have rates of HBP similar to or lower than those of non-Hispanic white Americans. Findings from a new analysis of combined data from the NHIS of 2000 to 2002 point to a health disparity between black and white adults of Hispanic descent. Black Hispanics were at slightly greater risk than white Hispanics, although non-Hispanic black adults had by far the highest rate of HBP. The racial disparity among Hispanics also was evident in the fact that higher-income, better-educated black Hispanics still had a higher rate of HBP than lower-income, less-educated white Hispanics.18 Data from the NHLBI’s ARIC study found that hypertension was a particularly powerful risk factor for CHD in black people, especially black women.19
Data from MESA found that being born outside the United States, speaking a language other than English at home, and living fewer years in the United States were each associated with a decreased prevalence of hypertension.20
Filipino (27%) and Japanese (25%) adults were more likely than Chinese (17%) or Korean (17%) adults to have ever been told that they had hypertension.21
Mortality
HBP mortality in 2007 was 57 732. Any-mention mortality in 2007 was 336 353 (NHLBI tabulation of NCHS mortality data). The 2007 death rate was 17.8.22
From 1997 to 2007, the death rate caused by HBP increased 9.0%, and the actual number of deaths rose 35.6% (NCHS and NHLBI; appropriate comparability ratios were applied).
The 2007 overall death rate resulting from HBP was 17.8. Death rates were 15.7 for white males, 49.2 for black males, 14.3 for white females, and 37.0 for black females. When any-mention mortality for 2007 was used, the overall death rate was 108.5. Death rates were 108.6 for white males, 228.8 for black males, 90.7 for white females, and 174.8 for black females (NHLBI tabulation of NCHS mortality data).
Risk Factors
Numerous risk factors and markers for development of hypertension, including age, ethnicity, family history of hypertension and genetic factors, lower education and socioeconomic status, greater weight, lower physical activity, tobacco use, psychosocial stressors, sleep apnea, and dietary factors (including dietary fats, higher sodium intake, lower potassium intake, and excessive alcohol intake), have been identified.
A study of related individuals in the NHLBI’s FHS estimated that when measured at a single examination, BP levels are ≈40% heritable; when measured across multiple examinations, long-term BP trends are ≈55% heritable.23
Recent data from the Nurses’ Health Study suggest that a large proportion of incident hypertension in women can be prevented by controlling dietary and lifestyle risk factors.24
Aftermath
Approximately 69% of people who have a first heart attack, 77% of those who have a first stroke, and 74% of those who have CHF have BP >140/90 mm Hg (NHLBI unpublished estimates from ARIC, CHS, and FHS Cohort and Offspring studies).
Data from FHS/NHLBI indicate that recent (within the past 10 years) and remote antecedent BP levels may be an important determinant of risk over and above the current BP level.25
- Data from the FHS/NHLBI indicate that hypertension is associated with shorter overall life expectancy, shorter life expectancy free of CVD, and more years lived with CVD.26
-
—Total life expectancy was 5.1 years longer for normotensive men and 4.9 years longer for normotensive women than for hypertensives of the same sex at 50 years of age.
-
—Compared with hypertensive men at 50 years of age, men with untreated BP <140/90 mm Hg survived on average 7.2 years longer without CVD and spent 2.1 fewer years of life with CVD. Similar results were observed for women.
-
—
Hospital Discharges/Ambulatory Care Visits
From 1997 to 2007, the number of inpatient discharges from short-stay hospitals with HBP as the first-listed diagnosis increased from 422 000 to 568 000 (NCHS, NHDS). The number of all-listed discharges increased from 6 629 000 to 10 645 000 (NHLBI, unpublished data from the NHDS, 2007).
Data from ambulatory medical care utilization estimates for 2007 showed that the number of visits for essential hypertension was 46 284 000.27
In 2007, there were 349 000 hospitalizations with a first-listed diagnosis of essential hypertension (ICD-9-CM code 401), but essential hypertension was listed as either a primary or a secondary diagnosis 8 784 000 times for hospitalized inpatients (NHLBI, unpublished data from the NHDS, 2007).
Awareness, Treatment, and Control
Data from NHANES/NCHS 2005 to 2008 showed that of those with hypertension who were ≥20 years of age, 79.6% were aware of their condition, 70.9% were under current treatment, 47.8% had their hypertension under control, and 52.2% did not have it controlled (NHLBI tabulation, NCHS, NHANES data).
Data from NHANES 1999 to 2006 showed that 11.2% of adults ≥20 years of age had treated and controlled BP levels.28
Analysis of NHANES/NCHS data from 1999 to 2004 through 2005 to 2006 found that there were substantial increases in awareness and treatment rates of hypertension. The control rates increased in both sexes, in non-Hispanic blacks, and in Mexican Americans. Among the group ≥60 years of age, awareness, treatment, and control rates of hypertension increased significantly.5,29
In NHANES/NCHS 2005 to 2006, rates of control were lower in Mexican Americans (35.2%) than in non-Hispanic whites (46.1%) and non-Hispanic blacks (46.5%).5
The awareness, treatment, and control of HBP among those ≥65 years of age in the CHS/NHLBI improved during the 1990s. The percentages of those aware of and treated for HBP were higher among blacks than among whites. Prevalences with HBP under control were similar. For both groups combined, the control of BP to <140/90 mm Hg increased from 37% in 1990 to 49% in 1999. Improved control was achieved by an increase in antihypertensive medications per person and by an increase in the proportion of the CHS population treated for hypertension from 34.5% to 51.1%.30
- Data from the FHS of the NHLBI show that:
-
—Among those ≥80 years of age, only 38% of men and 23% of women had BPs that met targets set forth in the National High Blood Pressure Education Program’s clinical guidelines. Control rates in men <60, 60 to 79, and ≥80 years of age were 38%, 36%, and 38%, respectively; for women in the same age groups, they were 38%, 28%, and 23%, respectively.31
-
—
Data from the Women’s Health Initiative Observational Study of nearly 100 000 postmenopausal women across the country enrolled between 1994 and 1998 indicate that although prevalence rates ranged from 27% of women 50 to 59 years of age to 41% of women 60 to 69 years of age to 53% of women 70 to 79 years of age, treatment rates were similar across age groups: 64%, 65%, and 63%, respectively. Despite similar treatment rates, hypertension control is especially poor in older women, with only 29% of hypertensive women 70 to 79 years of age having clinic BPs <140/90 mm Hg compared with 41% and 37% of those 50 to 59 and 60 to 69 years of age, respectively.32
A study of >300 women in Wisconsin showed a need for significant improvement in BP and LDL levels. Of the screened participants, 35% were not at BP goal, 32.4% were not at LDL goal, and 53.5% were not at both goals.33
In 2005, a survey of people in 20 states conducted by the BRFSS of the CDC found that 19.4% of respondents had been told on 2 or more visits to a health professional that they had HBP. Of these, 70.9% reported changing their eating habits; 79.5% reduced the use of or were not using salt; 79.2% reduced the use of or eliminated alcohol; 68.8% were exercising; and 73.4% were taking antihypertensive medication.34
On the basis of NHANES 2003 to 2004 data, it was found that nearly three fourths of adults with CVD comorbidities have hypertension. Poor control rates of systolic hypertension remain a principal problem that further compromises their already high CVD risk.35
Cost
The estimated direct and indirect cost of HBP for 2007 is $43.5 billion (MEPS, NHLBI tabulation).
Prehypertension
Prehypertension is untreated SBP of 120 to 139 mm Hg or untreated DBP of 80 to 89 mm Hg and not having been told on 2 occasions by a physician or other health professional that one has hypertension.
Data from NHANES 1999 to 2006 estimate 29.7% of adults ≥20 years of age have prehypertension.28
Follow-up of 9845 men and women in the FHS/NHLBI who attended examinations from 1978 to 1994 revealed that at 35 to 64 years of age, the 4-year incidence of hypertension was 5.3% for those with baseline BP <120/80 mm Hg, 17.6% for those with SBP of 120 to 129 mm Hg or DBP of 80 to 84 mm Hg, and 37.3% for those with SBP of 130 to 139 mm Hg or DBP of 85 to 89 mm Hg. At 65 to 94 years of age, the 4-year incidences of hypertension were 16.0%, 25.5%, and 49.5% for these BP categories, respectively.36
Data from FHS/NHLBI also reveal that prehypertension is associated with elevated relative and absolute risks for CVD outcomes across the age spectrum. Compared with normal BP (<120/80 mm Hg), prehypertension was associated with a 1.5- to 2-fold risk for major CVD events in those <60, 60 to 79, and ≥80 years of age. Absolute risks for major CVD associated with prehypertension increased markedly with age: 6-year event rates for major CVD were 1.5% in prehypertensive people <60 years of age, 4.9% in those 60 to 79 years of age, and 19.8% in those ≥80 years of age.31
In a study of NHANES 1999 to 2000 (NCHS), people with prehypertension were more likely than those with normal BP levels to have above-normal cholesterol levels, overweight/obesity, and DM, whereas the probability of currently smoking was lower. People with prehypertension were 1.65 times more likely to have 1 or more of these adverse risk factors than were those with normal BP.37
Abbreviations Used in Chapter 7
- ARIC
Atherosclerosis Risk in Communities Study
- BP
blood pressure
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CHD
coronary heart disease
- CHF
congestive heart failure
- CHS
Cardiovascular Health Study
- CVD
cardiovascular disease
- DBP
diastolic blood pressure
- DM
diabetes mellitus
- FHS
Framingham Heart Study
- HBP
high blood pressure
- HD
heart disease
- HHANES
Hispanic Health and Nutrition Examination Survey
- ICD
International Classification of Diseases
- LDL
low-density lipoprotein
- MEPS
Medical Expenditure Panel Survey
- MESA
Multi-Ethnic Study of Atherosclerosis
- mm Hg
millimeters of mercury
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- NHDS
National Hospital Discharge Survey
- NHES
National Health Examination Survey
- NHIS
National Health Interview Survey
- NHLBI
National Heart, Lung, and Blood Institute
- NINDS
National Institute of Neurological Disorders and Stroke
- SBP
systolic blood pressure
- SEARCH
Search for Diabetes in Youth Study
References
- 1.Fields LE, Burt VL, Cutler JA, Hughes J, Roccella EJ, Sorlie P. The burden of adult hypertension in the United States 1999–2000: a rising tide. Hypertension. 2004;44:398–404. doi: 10.1161/01.HYP.0000142248.54761.56. [DOI] [PubMed] [Google Scholar]
- 2.Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD. Hypertension, high serum total cholesterol, and diabetes: racial and ethnic prevalence differences in U.S. adults, 1999–2006. NCHS Data Brief. 2010:1–8. [PubMed] [Google Scholar]
- 3.National Center for Health Statistics. Health, United States-2009: With Special Feature on Medical Technology. Hyattsville, Md: National Center for Health Statistics; 2010. [Accessed September 15, 2010]. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. [PubMed] [Google Scholar]
- 4.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, National Heart, Lung, and Blood Institute, National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 5.Ostchega Y, Yoon SS, Hughes J, Louis T. Hypertension Awareness, Treatment, and Control—Continued Disparities in Adults: United States, 2005–2006. Hyattsville, Md: National Center for Health Statistics; 2008. NCHS Data Brief No. 3. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Data. Atlanta, Ga: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2009. [Accessed September 2, 2010]. Prevalence and trends data. Available at: http://apps.nccd.cdc.gov/brfss/index.asp. [Google Scholar]
- 7.Older Americans 2010 Key Indicators of Well-Being: Federal Interagency Forum on Aging-Related Statistics. Washington, DC: US Government Printing Office; 2010. Jul, [Accessed September 27, 2010]. Federal Interagency Forum on Aging-Related Statistics. Available at: http://www.agingstats.gov. [Google Scholar]
- 8.Crescioni M, Gorina Y, Bilheimer L, Gillum R. National Health Statistics Reports No. 24. Hyattsville, Md: National Center for Health Statistics; 2010. Trends in health status and health care use among older men. [PubMed] [Google Scholar]
- 9.Din-Dzietham R, Liu Y, Bielo M-V, Shamsa F. High blood pressure trends in children and adolescents in national surveys 1963 to 2002. Circulation. 2007;116:1488–1496. doi: 10.1161/CIRCULATIONAHA.106.683243. [DOI] [PubMed] [Google Scholar]
- 10.Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298:874–879. doi: 10.1001/jama.298.8.874. [DOI] [PubMed] [Google Scholar]
- 11.Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. Trends in blood pressure among children and adolescents. JAMA. 2004;291:2107–2113. doi: 10.1001/jama.291.17.2107. [DOI] [PubMed] [Google Scholar]
- 12.Rodriguez BL, Dabelea D, Liese AD, Fujimoto W, Waitzfelder B, Liu L, Bell R, Talton J, Snively BM, Kershnar A. Prevalence and correlates of elevated blood pressure in youth with diabetes mellitus: the Search for Diabetes in Youth Study. J Pediatr. 2010;157:245–251. doi: 10.1016/j.jpeds.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 13.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness and management. Arch Intern Med. 2005;165:2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 14.Collins R, Winkleby MA. African American women and men at high and low risk for hypertension: a signal detection analysis of NHANES III, 1988–1994. Prev Med. 2002;35:303–312. doi: 10.1006/pmed.2002.1081. [DOI] [PubMed] [Google Scholar]
- 15.Howard G, Prineas R, Moy C, Cushman M, Kellum M, Temple E, Graham A, Howard V. Racial and geographic differences in awareness, treatment, and control of hypertension: the Reasons for Geographic and Racial Differences in Stroke Study. Stroke. 2006;37:1171–1178. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]
- 16.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey 2009. [Accessed August 26, 2010];Vital Health Stat 10. 2010 No. 249. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_249.pdf. [PubMed]
- 17.Centers for Disease Control and Prevention (CDC) Hypertension-related mortality among Hispanic subpopulations: United States, 1995–2002. MMWR Morb Mortal Wkly Rep. 2006;55:177–180. [PubMed] [Google Scholar]
- 18.Borrell LN. Self-reported hypertension and race among Hispanics in the National Health Interview Survey. Ethn Dis. 2006;16:71–77. [PubMed] [Google Scholar]
- 19.Jones DW, Chambless LE, Folsom AR, Heiss G, Hutchinson RG, Sharrett AR, Szklo M, Taylor HA., Jr Risk factors for coronary heart disease in African Americans: the Atherosclerotic Risk in Communities Study, 1987–1997. Arch Intern Med. 2002;162:2565–2571. doi: 10.1001/archinte.162.22.2565. [DOI] [PubMed] [Google Scholar]
- 20.Moran A, Roux AV, Jackson SA, Kramer H, Manolio T, Shrager S, Shea S. Acculturation is associated with hypertension in a multiethnic sample. Am J Hypertens. 2007;20:354–363. doi: 10.1016/j.amjhyper.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 21.Barnes PM, Adams PF, Powell-Griner E. Health Characteristics of the Asian Adult Population: United States, 2004–2006. Hyattsville, Md: National Center for Health Statistics; 2008. Advance data from Vital and Health Statistics; No. 394. [PubMed] [Google Scholar]
- 22.Xu J, Kochanek KD, Murphy S, Tejada-Vera B. Deaths: Final Data for 2007. 19. Vol. 58. Hyattsville, Md: National Center for Health Statistics; 2010. National Vital Statistics Reports. [PubMed] [Google Scholar]
- 23.Levy D, DeStefano AL, Larson MG, O’Donnell CJ, Lifton RP, Gavras H, Cupples LA, Myers RH. Evidence for a gene influencing blood pressure on chromosome 17: genome scan linkage results for longitudinal blood pressure phenotypes in subjects from the Framingham Heart Study. Hypertension. 2000;36:477–483. doi: 10.1161/01.hyp.36.4.477. [DOI] [PubMed] [Google Scholar]
- 24.Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009;302:401–411. doi: 10.1001/jama.2009.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vasan RS, Massaro JM, Wilson PW, Seshadri S, Wolf PA, Levy D, D’Agostino RB Framingham Heart Study. Antecedent blood pressure and risk of cardiovascular disease: the Framingham Heart Study. Circulation. 2002;105:48–53. doi: 10.1161/hc0102.101774. [DOI] [PubMed] [Google Scholar]
- 26.Franco OH, Peeters A, Bonneux L, de Laet C. Blood pressure in adulthood and life expectancy with cardiovascular disease in men and women: life course analysis. Hypertension. 2005;46:280–286. doi: 10.1161/01.HYP.0000173433.67426.9b. [DOI] [PubMed] [Google Scholar]
- 27.Schappert SM, Rechsteiner EA. ambulatory medical care utilization estimates for 2006. Natl Health Stat Report. 2008;6:1–29. [PubMed] [Google Scholar]
- 28.Ogunniyi MO, Croft JB, Greenlund KJ, Giles WH, Mensah GA. Racial/ethnic differences in microalbuminuria among adults with prehypertension and hypertension: National Health and Nutrition Examination Survey (NHANES), 1999–2006. Am J Hypertens. 2010;23:859–864. doi: 10.1038/ajh.2010.77. [DOI] [PubMed] [Google Scholar]
- 29.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 30.Psaty BM, Manolio TA, Smith NL, Heckbert SR, Gottdiener JS, Burke GL, Weissfeld J, Enright P, Lumley T, Powe N, Furberg CD Cardiovascular Health Study. Time trends in high blood pressure control and the use of antihypertensive medications in older adults: the Cardiovascular Health Study. Arch Intern Med. 2002;162:2325–2332. doi: 10.1001/archinte.162.20.2325. [DOI] [PubMed] [Google Scholar]
- 31.Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294:466–472. doi: 10.1001/jama.294.4.466. [DOI] [PubMed] [Google Scholar]
- 32.Wassertheil-Smoller S, Anderson G, Psaty BM, Black HR, Manson J, Wong N, Francis J, Grimm R, Kotchen T, Langer R, Lasser N. Hypertension and its treatment in postmenopausal women: baseline data from the Women’s Health Initiative. Hypertension. 2000;36:780–789. doi: 10.1161/01.hyp.36.5.780. [DOI] [PubMed] [Google Scholar]
- 33.Sanchez RJ, Khalil L. Badger Heart Program: health screenings targeted to increase cardiovascular awareness in women at four northern sites in Wisconsin. WMJ. 2005;104:24–29. [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention (CDC) Prevalence of actions to control high blood pressure 20 states, 2005. MMWR Morb Mortal Wkly Rep. 2007;56:420–423. [PubMed] [Google Scholar]
- 35.Wong ND, Lopez VA, L’Italien G, Chen R, Kline SE, Franklin SS. Inadequate control of hypertension in US adults with cardiovascular disease comorbidities in 2003–2004. Arch Intern Med. 2007;167:2431–2436. doi: 10.1001/archinte.167.22.2431. [DOI] [PubMed] [Google Scholar]
- 36.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–1686. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 37.Greenlund KJ, Croft JB, Mensah GA. Prevalence of heart disease and stroke risk factors in persons with prehypertension in the United States, 1999–2000. Arch Intern Med. 2004;164:2113–2118. doi: 10.1001/archinte.164.19.2113. [DOI] [PubMed] [Google Scholar]
8. Congenital Cardiovascular Defects
ICD-9 745 to 747, ICD-10 Q20 to Q28. See Tables 8-1 through 8-4.
Table 8-1.
Congenital Cardiovascular Defects
| Population Group | Estimated Prevalence, Adults |
Mortality, 2007, All Ages |
Hospital Discharges, 2007, All Ages |
|---|---|---|---|
| Both sexes | 650 000 to 1.3 million2 | 3547 | 67 000 |
| Males | … | 1935 (54.6%)* | 31 000 |
| Females | … | 1612 (45.4%)* | 36 000 |
| NH white males | … | 1506 | … |
| NH white females | … | 1226 | … |
| NH black males | … | 341 | … |
| NH black females | … | 309 | … |
Ellipses (…) indicate data not available;
NH, non-Hispanic.
These percentages represent the portion of total congenital cardiovascular mortality that is for males versus females.
Sources: Mortality: National Center for Health Statistics. These data represent underlying cause of death only; data for white and black males and females include Hispanics. Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics; data include those inpatients discharged alive, dead, or status unknown.
Table 8-4.
Surgery for Congenital Heart Disease
| Sample | Population, Weighted |
|
|---|---|---|
| Surgery for congenital heart disease, n | 14 888 | 25 831 |
| Deaths, n | 736 | 1253 |
| Mortality rate, % | 4.9 | 4.8 |
| By sex (81 missing in sample) | ||
| Males | 8127 | 14 109 |
| Deaths, n | 420 | 714 |
| Mortality rate, % | 5.2 | 5.1 |
| Females | 6680 | 11 592 |
| Deaths, n | 315 | 539 |
| Mortality rate, % | 4.7 | 4.6 |
| By type of surgery | ||
| ASD secundum surgery, n | 834 | 1448 |
| Deaths, n | 3 | 6 |
| Mortality rate, % | 0.4 | 0.4 |
| Norwood procedure for HPLHS, n | 161 | 286 |
| Deaths, n | 42 | 72 |
| Mortality rate, % | 26.1 | 25.2 |
ASD indicates atrial septal defect; HPLHS, hypoplastic left heart syndrome.
In 2003, 25 000 cardiovascular operations for congenital cardiovascular defects were performed on children <20 years of age. Inpatient mortality rate after all types of cardiac surgery was 4.8%. Nevertheless, mortality risk varies substantially for different defect types, from 0.4% for ASD repair to 25.2% for first-stage palliation for HPLHS. Fifty-five percent of operations were performed in males. In unadjusted analysis, mortality after cardiac surgery was somewhat higher for males than for females (5.1% versus 4.6%).
Source: Analysis of 2003 Kids’ Inpatient Database, HCUPnet, Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality (http://www.hcup-us.ahrq.gov), and personal communication with Kathy Jenkins, MD, Children’s Hospital of Boston, October 1, 2006.
Congenital cardiovascular defects, also known as congenital heart defects, are structural problems that arise from abnormal formation of the heart or major blood vessels. ICD-9 lists 25 congenital heart defects codes, of which 21 designate specified anatomic and/or hemodynamic lesions.
Defects range in severity from tiny pinholes between chambers, which are nearly irrelevant and often resolve spontaneously, to major malformations that can require multiple surgical procedures before school age and may result in death in utero, in infancy, or in childhood. The common complex defects include:
Tetralogy of Fallot (TOF; 9% to 14%)
Transposition of the great arteries (TGA; 10% to 11%)
Atrioventricular septal defects (4% to 10%)
Coarctation of the aorta (8% to 11%)
Hypoplastic left heart syndrome (HPLHS; 4% to 8%)
Ventricular septal defects (VSDs)
Although VSDs may close spontaneously, these lesions are the most prevalent in childhood and still account for 14% to 16% of defects that require an invasive procedure within the first year of life.1 Atrial septal defects (ASDs) are the most common defects seen in adults.2
Prevalence
The estimated number of adults with congenital heart defects ranges from 650 000 to 1.3 million.1,2 From 1940 to 2002, ≈2 million patients with congenital cardiovascular defects were born in the United States, ≈1 million with simple lesions and 0.5 million each with moderate and complex lesions. Using available data to estimate the prevalence of congenital cardiovascular defects at birth and in adults in the year 2000, the survival of these patients is estimated to be 2000 assuming no treatment (the low estimate) and full treatment (the high estimate). If all were treated, there would be 750 000 survivors with simple lesions, 400 000 with moderate lesions, and 180 000 with complex lesions; in addition, there would be 3 million subjects alive with bicuspid aortic valves. Without treatment, the number of survivors in each group would be 400 000, 220 000, and 30 000, respectively. The actual numbers surviving are projected to be between these 2 sets of estimates.2 The 32nd Bethesda Conference estimated that the total number of adults living with congenital heart disease in the United States in 2000 was 787 800.3 In the United States, 1 in 150 adults is expected to have some form of congenital heart disease.4
Currently, no measured data are available in the United States for the prevalence of congenital cardiovascular defects in adults. Population data from Quebec, Canada, measured a prevalence of congenital cardiac defects of 11.89 per 1000 children and 4.09 per 1000 adults.5 The most common types of defects in children are as follows: VSD, 620 000 people; ASD, 235 000 people; valvular pulmonary stenosis, 185 000 people; and patent ductus arteriosus, 173 000 people.2 The most common lesions seen in adults are ASD and TOF.3
Incidence
As of 2002, the most commonly reported incidence of congenital cardiovascular defects in the United States is between 4 and 10 per 1000, clustering around 8 per 1000 live births.6 Major defects are usually apparent in the neonatal period, but minor defects may not be detected until adulthood. Thus, true measures of the incidence of congenital heart disease would need to record new cases of defects that present any time in fetal life through adulthood; however, estimates are available only for new cases detected between birth and 30 days of life, known as birth prevalence, or for new cases detected in the first year of life only. Both of these are typically reported as cases per 1000 live births per year and do not distinguish between tiny defects that resolve without treatment and major malformations. To distinguish more serious defects, some studies also report new cases of sufficient severity to require an invasive procedure or that result in death within the first year of life. Despite the absence of a true incidence figure, some data are available and are provided in Table 8-1.
According to the CDC, 1 in every 110 infants in the metropolitan Atlanta, GA, area is born with a congenital heart defect, including some infants with tiny defects that resolve without treatment. Some defects occur more commonly in boys or girls or in whites or blacks.6
Eight (8.0) defects per 1000 live births, or 36 000 affected infants per year, are expected in the United States. Of these, several studies suggest that 9200, or 2.3 per 1000 live births, require invasive treatment or result in death in the first year of life.1
Estimates also are available for bicuspid aortic valves, which occur in 13.7 per 1000 people; these defects may not require treatment in infancy but can cause problems later in adulthood.7
Some studies suggest that as many as 5% of newborns, or 200 000 per year, are born with tiny muscular VSDs, almost all of which close spontaneously.8,9 These defects almost never require treatment, so they are not included in Table 8-1.
Data collected by the National Birth Defects Prevention Network from 11 states from 1999 to 2001 showed the average prevalence of 18 selected major birth defects. These data indicated that there are >6500 estimated annual cases of 5 cardiovascular defects: truncus arteriosus, TGA, TOF, atrioventricular septal defect, and HPLHS.10
Risk Factors
Numerous intrinsic and extrinsic nongenetic risk factors contribute to CHD.11
Attributable risks or fractions have been shown to include paternal anesthesia in TOF (3.6%), sympathomimetic medication for coarctation of the aorta (5.8%), pesticides for VSD (5.5%), and solvents for HPLHS (4.6%).12
A study of infants born with heart defects unrelated to genetic syndromes who were included in the National Birth Defects Prevention Study found that women who reported smoking in the month before becoming pregnant or in the first trimester were more likely to give birth to a child with a septal defect. Compared with the infants of mothers who did not smoke during pregnancy, infants of mothers who were heavy smokers (≥25 cigarettes daily) were twice as likely to have a septal defect.13
Associations between exposure to air pollutants during first-trimester pregnancy and risks of congenital heart defects were documented from 1986 to 2003 by the Metropolitan Atlanta Congenital Defects Program that related carbon monoxide, nitrogen dioxide, and sulfur dioxide measurements to the risk of ASD, VSD, TGA, and TOF.14
The results of a population-based study examining pregnancy obesity found a weak to moderate positive association of maternal obesity with 7 of 16 categories of birth defects.15
Although folic acid supplementation is recommended during pregnancy to potentially reduce the risk of congenital heart defects,11 there has been only 1 US population-based case-control study, performed with the Baltimore-Washington Infant Study between 1981 and 1989, that showed an inverse relationship between folic acid use and the risk of TGA.16 A study from Quebec that analyzed 1.3 million births from 1990 to 2005 found a significant 6%/y reduction in severe congenital heart defects using a time-trend analysis before and after public health measures were instituted that mandated folic acid fortification of grain and flour products in Canada.17
Pregestational DM was significantly associated with cardiac defects, both isolated and multiple. Gestational DM was associated with a limited group of birth defects.18
Mortality
Congenital cardiovascular defects mortality in 2007 was 3547. Any-mention mortality related to congenital cardiovascular defects in 2007 was 5643.
Congenital cardiovascular defects are the most common cause of infant death resulting from birth defects; >24% of infants who die of a birth defect have a heart defect.19
The 2007 death rate for congenital cardiovascular defects was 1.2. Death rates were 1.3 for white males, 1.5 for black males, 1.0 for white females, and 1.4 for black females. Crude infant mortality rates (<1 year of age) were 35.5 for white infants and 51.7 for black infants.20
In 2007, 189 000 life-years were lost before 55 years of age because of deaths resulting from congenital cardiovascular defects. This is almost as many as the life-years lost from leukemia and asthma combined (NHLBI tabulation of NCHS mortality data).
The mortality rate attributable to congenital defects has been declining. From 1979 to 1997, age-adjusted death rates resulting from all defects declined 39%, and deaths tended to occur at progressively older ages. Nevertheless, 45% of deaths still occurred in infants <1 year of age. The mortality rate varies considerably according to type of defect.21
From 1997 to 2007, death rates for congenital cardiovascular defects declined 33.3%, whereas the actual number of deaths declined 23.8%.19
Data from the Pediatric Heart Network conducted in 15 North American centers revealed that even in lesions associated with the highest mortality among congenital lesions such as HPLHS, aggressive palliation can lead to 12-month survival from 64% to 74%.22
Data analysis from the Society of Thoracic Surgeons, a voluntary registry with self-reported data for a 4-year cycle (2004 to 2007) from 68 centers performing congenital heart surgery (67 from the United States and 1 from Canada), showed that of 61 410 total operations, the overall aggregate hospital discharge mortality rate was 3.7%; specifically, for neonates (0 to 30 days of age), the mortality rate was 10.7%; for infants (31 days to 1 year of age), it was 2.6%; for children (>1 year to 18 years of age), it was 1.2%; and for adults (>18 years of age), it was 1.9%.23
Using the Nationwide Inpatient Sample 1988 to 2003, mortality was examined for 12 congenital heart defects procedures. A total of 30 250 operations were identified, which yielded a national estimate of 152 277±7875 operations. Of these, 27% were performed in patients ≥18 years of age. The overall in-hospital mortality rate for adult patients with congenital heart defects was 4.71% (95% CI, 4.19 to 5.23), with a significant reduction in mortality observed when surgery was performed on adult patients with congenital heart defects by pediatric versus nonpediatric heart surgeons (1.87% versus 4.84%; P<0.0001).24
Hospitalizations
In 2004, birth defects accounted for >139 000 hospitalizations, representing 47.4 stays per 100 000 people. Cardiac and circulatory congenital anomalies, which include ASDs and VSDs, accounted for more than one third of all hospital stays for birth defects and had the highest in-hospital mortality rate. Between 1997 and 2004, hospitalization rates increased by 28.5% for cardiac and circulatory congenital anomalies. For almost 86 300 hospitalizations, ASD was noted as the principal reason for the hospital stay or as a coexisting or secondary condition.25
Cost
From 2003 data from the Healthcare Cost and Utilization Project 2003 Kids’ Inpatient Database (KID) and information on birth defects in the Congenital Malformations Surveillance Report, it was found that the most expensive average neonatal hospital charges were for 2 congenital heart defects: HPLHS ($199 597) and common truncus arteriosus ($192 781). Two other cardiac defects, coarctation of the aorta and TGA, were associated with average hospital charges in excess of $150 000. For the 11 selected cardiovascular congenital defects (of 35 birth defects considered), there were 11 578 hospitalizations in 2003 and 1550 in-hospital deaths (13.4%). Estimated total hospital charges for these 11 conditions were $1.4 billion.26
In 2004, hospital costs for congenital cardiovascular defect conditions totaled $2.6 billion. The highest aggregate costs were for stays related to cardiac and circulatory congenital anomalies, which accounted for ≈$1.4 billion, more than half of all hospital costs for birth defects.25
Abbreviations Used in Chapter 8
- ASD
atrial septal defect
- CDC
Centers for Disease Control and Prevention
- CHD
coronary heart disease
- CI
confidence interval
- DM
diabetes mellitus
- HPLHS
hypoplastic left heart syndrome
- ICD
International Classification of Diseases
- KID
Kids’ Inpatient Database
- NCHS
National Center for Health Statistics
- NHLBI
National Heart, Lung, and Blood Institute
- TGA
transposition of the great arteries
- TOF
tetralogy of Fallot
- VSD
ventricular septal defect
References
- 1.Moller JH. Perspectives in Pediatric Cardiology: Surgery of Congenital Heart Disease: Pediatric Cardiac Care Consortium, 1984–1995. Vol. 6. Armonk, NY: Futura Publishing Co; 1998. Prevalence and incidence of cardiac malformation; pp. 19–26. [Google Scholar]
- 2.Hoffman JI, Kaplan S, Liberthson RR. Prevalence of congenital heart disease. Am Heart J. 2004;147:425–439. doi: 10.1016/j.ahj.2003.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Warnes CA, Liberthson R, Danielson GK, Dore A, Harris L, Hoffman JI, Somerville J, Williams RG, Webb GD. Task Force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. 2001;37:1170–1175. doi: 10.1016/s0735-1097(01)01272-4. [DOI] [PubMed] [Google Scholar]
- 4.Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, del Nido P, Fasules JW, Graham TP, Jr, Hijazi ZM. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease): developed in collaboration with the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2008;118:e714–e833. [Google Scholar]
- 5.Marelli AJ, Mackie AS, Ionescu-Ittu R, Rahme E, Pilote L. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation. 2007;115:163–172. doi: 10.1161/CIRCULATIONAHA.106.627224. [DOI] [PubMed] [Google Scholar]
- 6.Botto LD, Correa A, Erickson JD. Racial and temporal variations in the prevalence of heart defects. Pediatrics. 2001;107:E32. doi: 10.1542/peds.107.3.e32. [DOI] [PubMed] [Google Scholar]
- 7.Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890–1900. doi: 10.1016/s0735-1097(02)01886-7. [DOI] [PubMed] [Google Scholar]
- 8.Roguin N, Du ZD, Barak M, Nasser N, Hershkowitz S, Milgram E. High prevalence of muscular ventricular septal defect in neonates. J Am Coll Cardiol. 1995;26:1545–1548. doi: 10.1016/0735-1097(95)00358-4. [DOI] [PubMed] [Google Scholar]
- 9.Sands AJ, Casey FA, Craig BG, Dornan JC, Rogers J, Mulholland HC. Incidence and risk factors for ventricular septal defect in “low risk” neonates. Arch Dis Child Fetal Neonatal Ed. 1999;81:F61–F63. doi: 10.1136/fn.81.1.f61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Improved national prevalence estimates for 18 selected major birth defects: United States, 1999–2001. MMWR Morb Mortal Wkly Rep. 2006;54:1301–1305. [PubMed] [Google Scholar]
- 11.Jenkins KJ, Correa A, Feinstein JA, Botto L, Britt AE, Daniels SR, Elixson M, Warnes CA, Webb CL. Noninherited risk factors and congenital cardiovascular defects: current knowledge: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young. Circulation. 2007;115:2995–3014. doi: 10.1161/CIRCULATIONAHA.106.183216. [DOI] [PubMed] [Google Scholar]
- 12.Wilson PD, Loffredo CA, Correa-Villaseñor A, Ferencz C. Attributable fraction for cardiac malformations. Am J Epidemiol. 1998;148:414–423. doi: 10.1093/oxfordjournals.aje.a009666. [DOI] [PubMed] [Google Scholar]
- 13.Malik S, Cleves MA, Honein MA, Romitti PA, Botto LD, Yang S, Hobbs CA National Birth Defects Prevention Study. Maternal smoking and congenital heart defects. Pediatrics. 2008;121:e810–e816. doi: 10.1542/peds.2007-1519. [DOI] [PubMed] [Google Scholar]
- 14.Strickland MJ, Klein M, Correa A, Reller MD, Mahle WT, Riehle-Colarusso TJ, Botto LD, Flanders WD, Mulholland JA, Siffel C, Marcus M, Tolbert PE. Ambient air pollution and cardiovascular malformations in Atlanta, Georgia, 1986–2003. Am J Epidemiol. 2009;169:1004–1014. doi: 10.1093/aje/kwp011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waller DK, Shaw GM, Rasmussen SA, Hobbs CA, Canfield MA, Siega-Riz AM, Gallaway MS, Correa A National Birth Defects Prevention Study. Prepregnancy obesity as a risk factor for structural birth defects. Arch Pediatr Adolesc Med. 2007;161:745–750. doi: 10.1001/archpedi.161.8.745. [DOI] [PubMed] [Google Scholar]
- 16.Scanlon KS, Ferencz C, Loffredo CA, Wilson PD, Correa-Villaseñor A, Khoury MJ, Willett WC Baltimore-Washington Infant Study Group. Preconceptional folate intake and malformations of the cardiac outflow tract. Epidemiology. 1998;9:95–98. [PubMed] [Google Scholar]
- 17.Ionescu-Ittu R, Marelli AJ, Mackie AS, Pilote L. Prevalence of severe congenital heart disease after folic acid fortification of grain products: time trend analysis in Quebec, Canada. BMJ. 2009;338:b1673. doi: 10.1136/bmj.b1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Correa A, Gilboa SA, Besser LM, Botto LD, Moore CA, Hobbs CA, Cleves MA, Riehle-Colarusso TJ, Waller DK, Reece EA. Diabetes mellitus and birth defects. Am J Obstet Gynecol. 2008;199:237.e1–237.e9. doi: 10.1016/j.ajog.2008.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Center for Health Statistics. Health data interactive: final mortality data for 2004 –2006. [Accessed July 15, 2010]; Available at: http://www.cdc.gov/nchs/hdi.htm.
- 20.Centers for Disease Control and Prevention. Compressed mortality file: underlying cause of death, 1979 to 2007. [Accessed December 7, 2010]; Available at: http://wonder.cdc.gov/mortSQL.html.
- 21.Boneva RS, Botto LD, Moore CA, Yang Q, Correa A, Erickson JD. Mortality associated with congenital heart defects in the United States: trends and racial disparities, 1979 –1997. Circulation. 2001;103:2376–2381. doi: 10.1161/01.cir.103.19.2376. [DOI] [PubMed] [Google Scholar]
- 22.Ohye RG, Sleeper LA, Mahony L, Newburger JW, Pearson GD, Lu M, Goldberg CS, Tabbutt S, Frommelt PC, Ghanayem NS. Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N Engl J Med. 2010;362:1980–1992. doi: 10.1056/NEJMoa0912461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jacobs JP, Jacobs ML, Mavroudis C, Lacour-Gayet F, Tchervenkov CI. STS congenital heart surgery data summary, 2007–2007 procedures, all patients. [Accessed September 27, 2010]; Available at: http://www.sts.org/documents/pdf/ndb/Spring_2008_STSCONG-ALLPatientsSUMMARY.pdf. [Google Scholar]
- 24.Karamlou T, Diggs BS, Person T, Ungerleider RM, Welke KF. National practice patterns for management of adult congenital heart disease operation by pediatric heart surgeons decreases in-hospital death. Circulation. 2008;118:2345–2352. doi: 10.1161/CIRCULATIONAHA.108.776963. [DOI] [PubMed] [Google Scholar]
- 25.Russo CA, Elixhauser A. Hospitalizations for Birth Defects, 2004. Rockville, Md: US Agency for Healthcare Research and Quality; 2007. Jan, [Accessed October 23, 2007]. HCUP Statistical Brief No. 24. Available at: http://www.hcupdoc.net/reports/statbriefs/sb24.pdf. [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Hospital stays, hospital charges, and in-hospital deaths among infants with selected birth defects: United States, 2003. MMWR Morb Mortal Wkly Rep. 2007;56:25–29. [PubMed] [Google Scholar]
- 27.Larson EW, Edwards WD. Risk factors for aortic dissection: a necropsy study of 161 cases. Am J Cardiol. 1984;53:849–855. doi: 10.1016/0002-9149(84)90418-1. [DOI] [PubMed] [Google Scholar]
9. Cardiomyopathy and Heart Failure
See Table 9-1 and Charts 9-1 through 9-3.
Table 9-1.
Heart Failure
| Population Group | Prevalence, 2008, Age ≥20 y |
Incidence (New Cases), Age ≥45 y |
Mortality, 2007, All Ages* |
Hospital Discharges, 2007, All Ages |
|---|---|---|---|---|
| Both sexes | 5 700 000 (2.4%) | 670 000 | 56 565 | 990 000 |
| Males | 3 100 000 (3.0%) | 350 000 | 22 914 (40.5%)† | 470 000 |
| Females | 2 600 000 (2.0%) | 320 000 | 33 651 (59.5%)† | 520 000 |
| NH white males | 2.7% | … | 20 262 | … |
| NH white females | 1.8% | … | 30 105 | … |
| NH black males | 4.5% | … | 2341 | … |
| NH black females | 3.8% | … | 3156 | … |
| Mexican American males | 2.3% | … | … | … |
| Mexican American females | 1.3% | … | … | … |
NH indicates non-Hispanic.
Heart failure includes persons who answered “yes” to the question of ever having congestive heart failure.
Ellipses (…) indicate data not available.
Mortality data are for whites and blacks and include Hispanics.
These percentages represent the portion of total HF mortality that is for males vs females.
Sources: Prevalence: National Health and Nutrition Examination Survey 2005–2008 (National Center for Health Statistics) and National Heart, Lung, and Blood Institute. Percentages are age adjusted for Americans ≥20 years of age. Age-specific percentages are extrapolated to the 2008 US population estimates. These data are based on self-reports. Incidence: Framingham Heart Study, 1980–2003 from National Heart, Lung, and Blood Institute Incidence and Prevalence Chart Book, 2006. Mortality: National Center for Health Statistics.
Chart 9-1.
Prevalence of heart failure by sex and age (National Health and Nutrition Examination Survey: 2005–2008). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 9-3.
Hospital discharges for heart failure by sex (United States: 1979–2007). Note: Hospital discharges include people discharged alive, dead, and status unknown. Source: National Hospital Discharge Survey/National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Cardiomyopathy
ICD-9 425; ICD-10 I42.
Mortality—24 703. Any-mention mortality—48 579. Hospital discharges—55 000.
Mortality from cardiomyopathy is highest in older people, men, and blacks.
Tachycardia-induced cardiomyopathy develops slowly and appears reversible, but recurrent tachycardia causes rapid decline in left ventricular function and development of HF. Sudden death is possible.1
- Since 1996, the NHLBI-sponsored Pediatric Cardiomyopathy Registry has collected data on all children with newly diagnosed cardiomyopathy in New England and the Central Southwest (Texas, Oklahoma, and Arkansas).2
-
—The overall incidence of cardiomyopathy is 1.13 cases per 100 000 in children <18 years of age.
-
—In children <1 year of age, the incidence is 8.34, and in children 1 to 18 years of age, it is 0.70 per 100 000.
-
—The annual incidence is lower in white than in black children, higher in boys than in girls, and higher in New England (1.44 per 100 000) than in the Central Southwest (0.98 per 100 000).
-
—
Studies show that 36% of young athletes who die suddenly have probable or definite hypertrophic cardiomyopathy.3
Hypertrophic cardiomyopathy is the leading cause of sudden cardiac death in young people, including trained athletes. Hypertrophic cardiomyopathy is the most common inherited heart defect, occurring in 1 of 500 individuals. In the United States, ≈500 000 people have hypertrophic cardiomyopathy, yet most are unaware of it.4
In a recent report of the Pediatric Cardiomyopathy Registry, the overall annual incidence of hypertrophic cardiomyopathy in children was 4.7 per 1 million children. There was a higher incidence in the New England than in the Central Southwest region, in boys than in girls, and in children diagnosed at <1 year of age than in older children.5
Dilated cardiomyopathy is the most common form of cardiomyopathy. The Pediatric Cardiomyopathy Registry recently reported an annual incidence of dilated cardiomyopathy in children <18 years of age of 0.57 per 100 000 per year overall. The annual incidence was higher in boys than in girls (0.66 versus 0.47 cases per 100 000), in blacks than in whites (0.98 versus 0.46 cases per 100 000), and in infants (<1 year of age) than in children (4.40 versus 0.34 cases per 100 000). The majority of children (66%) had idiopathic disease. The most common known causes were myocarditis (46%) and neuromuscular disease (26%).6
Heart Failure
ICD-9 428, ICD-10 I50.
Incidence
- Data from the NHLBI-sponsored FHS7 indicate that:
-
—HF incidence approaches 10 per 1000 population after 65 years of age.
-
—Seventy-five percent of HF cases have antecedent hypertension.
-
—At 40 years of age, the lifetime risk of developing HF for both men and women is 1 in 5. At 80 years of age, remaining lifetime risk for development of new HF remains at 20% for men and women, even in the face of a much shorter life expectancy.
-
—At 40 years of age, the lifetime risk of HF occurring without antecedent MI is 1 in 9 for men and 1 in 6 for women.
-
—The lifetime risk for people with BP >160/90 mm Hg is double that of those with BP <140/90 mm Hg.
-
—
The annual rates per 1000 population of new HF events for white men are 15.2 for those 65 to 74 years of age, 31.7 for those 75 to 84 years of age, and 65.2 for those ≥85 years of age. For white women in the same age groups, the rates are 8.2, 19.8, and 45.6, respectively. For black men, the rates are 16.9, 25.5, and 50.6,* and for black women, the estimated rates are 14.2, 25.5, and 44.0,* respectively (CHS, NHLBI).8
In MESA, African Americans had the highest risk of developing HF, followed by Hispanic, white, and Chinese Americans (4.6, 3.5, 2.4, and 1.0 per 1000 person-years, respectively). This higher risk reflected differences in the prevalence of hypertension, DM, and socioeconomic status. African Americans had the highest proportion of incident HF not preceded by clinical myocardial infarction (75%).9
In Olmsted County, MN, the incidence of HF did not decline between 1979 and 2000.10
In the ARIC study of the NHLBI, the age-adjusted incidence rate per 1000 person-years was 3.4 for white women, less than all other groups—that is, white men (6.0), black women (8.1), and black men (9.1). The 30-day, 1-year, and 5-year case fatality rates after hospitalization for HF were 10.4%, 22%, and 42.3%, respectively. Blacks had a greater 5-year case fatality rate than whites (P<0.05). HF incidence rates in black women were more similar to those of men than of white women. The greater HF incidence in blacks than in whites is explained largely by blacks’ greater levels of atherosclerotic risk factors.11
Data from Kaiser Permanente indicated an increase in the incidence of HF among the elderly, with the effect being greater in men.12
Data from hospitals in Worcester, MA, indicate that during 2000, the incidence and attack rates for HF were 219 per 100 000 and 897 per 100 000, respectively. HF was more frequent in women and the elderly. The hospital fatality rate was 5.1%.13
In the CARDIA study, HF before 50 years of age is more common among blacks than whites. Hypertension, obesity, and systolic dysfunction are important risk factors that may be targets for prevention.14
Risk Factors
In the NHLBI-sponsored FHS, hypertension is a common risk factor for HF followed closely by antecedent MI.15
In a study of 2763 postmenopausal women with coronary disease, DM was the strongest risk factor for HF.16
The prevalence of DM is increasing among older people with HF. Between 1979 and 1999, among subjects in Olmsted County, MN, with a first diagnosis of HF, the prevalence of DM increased 3.8% every year. The odds of having DM for those first diagnosed with HF in 1999 were nearly 4 times higher than for those diagnosed 20 years earlier.17
In the Framingham Offspring Study, among 2739 participants, increased circulating concentrations of resistin were associated with incident HF, independently of prevalent coronary disease, obesity, insulin resistance, and inflammation.18
Among 20 900 male physicians in the Physicians Health Study, the lifetime risk of HF at 40 years of age was 13.8%. Lifetime risk of HF was higher in men with hypertension; healthy lifestyle factors (normal weight, not smoking, regular exercise, moderate alcohol intake, consumption of breakfast cereals, and consumption of fruits and vegetables) were related to lower risk of HF.19
Among 2934 participants in the Health Aging, Body and Composition (ABC) study, the incidence of HF was 13.6 per 1000 person-years. Men and black participants were more likely to develop HF. Coronary disease (population-attributable risk [PAR], 23.9% for white participants, 29.5% for black participants) and uncontrolled BP (PAR, 21.3% for white participants, 30.1% for black participants) had the highest PARs in both races. There was a higher overall proportion of HF attributable to modifiable risk factors in black participants versus white participants (67.8% versus 48.9%). Hospitalizations were higher among black participants.20
Left Ventricular Function
- Data from Olmsted County, MN, indicate that:
-
—Among asymptomatic individuals, the prevalence of left ventricular diastolic dysfunction was 21% for mild diastolic dysfunction and 7% for moderate or severe diastolic dysfunction. The prevalence of systolic dysfunction was 6%. The presence of any left ventricular dysfunction (systolic or diastolic) was associated with an increased risk of developing overt HF, and diastolic dysfunction was predictive of all-cause death.21
-
—Among individuals with symptomatic HF, the prevalence of left ventricular diastolic dysfunction was 6% for mild diastolic dysfunction and 75% for moderate or severe diastolic dysfunction.22 The proportion of people with HF and preserved ejection fraction (EF) increased over time. Survival improved over time among individuals with reduced EF but not among those with preserved EF.23
-
—
Mortality
In 2007, HF any-mention mortality was 277 193 (121 684 males and 155 509 females). HF was mentioned on 277 193 US death certificates and was the underlying cause in 56 565 of those deaths in 2007 (NCHS, NHLBI). Table 9-1 contains the numbers of these deaths that are coded for HF as the underlying cause.
The 2007 overall any-mention death rate for HF was 85.4. Any-mention death rates were 99.2 for white males, 104.2 for black males, 76.7 for white females, and 82.5 for black females (NCHS, NHLBI).
One in 9 deaths has HF mentioned on the death certificate (NCHS, NHLBI).
The number of any-mention deaths from HF was about as high in 1995 (287 000) as it was in 2006 (283 000) (NCHS, NHLBI).
Survival after HF diagnosis has improved over time as shown by data from the FHS24 and Olmsted County Study.10 However, the death rate remains high: ≈50% of people diagnosed with HF will die within 5 years.10,24
In the elderly, data from Kaiser Permanente indicate that survival after the onset of HF also improved.12
Hospital Discharges/Ambulatory Care Visits
Hospital discharges for HF were essentially unchanged from 1997 to 2007 with first listed discharges of 966 000 and 990 000, respectively (unpublished data from the NHDS 2007, NCHS, NHLBI).
Data from Ambulatory Medical Care Utilization Estimates for 2007 showed that the number of visits for HF was 3 434 000.25
Among 1077 patients with HF in Olmsted County, MN, hospitalizations were common after HF diagnosis, with 83% patients hospitalized at least once and 43% hospitalized at least 4 times. More than one half of hospitalizations were related to noncardiovascular causes.26
Abbreviations Used in Chapter 9
- ABC
Aging, Body and Composition
- ARIC
Atherosclerosis Risk in Communities Study
- BMI
body mass index
- BP
blood pressure
- CARDIA
Coronary Artery Risk Development in Young Adults Study
- CDC
Centers for Disease Control and Prevention
- CHD
coronary heart disease
- CHS
Cardiovascular Health Study
- DM
diabetes mellitus
- EF
ejection fraction
- FHS
Framingham Heart Study
- HF
heart failure
- ICD
International Classification of Diseases
- MESA
Multi-Ethnic Study of Atherosclerosis
- MI
myocardial infarction
- mm Hg
millimeters of mercury
- NCHS
National Center for Health Statistics
- NH
non-Hispanic
- NHANES
National Health and Nutrition Examination Survey
- NHDS
National Hospital Discharge Survey
- NHLBI
National Heart, Lung, and Blood Institute
- PAR
population-attributable risk
References
- 1.Nerheim P, Birger-Botkin S, Piracha L, Olshansky B. Heart failure and sudden death in patients tachycardia-induced cardiomyopathy and recurrent tachycardia. Circulation. 2004;110:247–252. doi: 10.1161/01.CIR.0000135472.28234.CC. [DOI] [PubMed] [Google Scholar]
- 2.Lipshultz SE, Sleeper LA, Towbin JA, Lowe AM, Orav EJ, Cox GF, Lurie PR, McCoy KL, McDonald MA, Messere JE, Colan SD. The incidence of pediatric cardiomyopathy in two regions of the United States. N Engl J Med. 2003;348:1647–1655. doi: 10.1056/NEJMoa021715. [DOI] [PubMed] [Google Scholar]
- 3.Maron BJ, Shirani J, Poliac LC, Mathenge R, Roberts WC, Mueller FO. Sudden death in young competitive athletes: clinical, demographic, and pathological profiles. JAMA. 1996;276:199–204. [PubMed] [Google Scholar]
- 4.Maron BJ, McKenna WJ, Danielson GK, Kappenberger LJ, Kuhn HJ, Seidman CE, Shah PM, Spencer WH, III, Spirito P, Ten Cate FJ, Wigle ED. American College of Cardiology/European Society of Cardiology clinical expert consensus document on hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines. J Am Coll Cardiol. 2003;42:1687–1713. doi: 10.1016/s0735-1097(03)00941-0. [DOI] [PubMed] [Google Scholar]
- 5.Colan SD, Lipshultz SE, Lowe AM, Sleeper LA, Messere J, Cox GF, Lurie PR, Orav EJ, Towbin JA. Epidemiology and cause-specific outcome of hypertrophic cardiomyopathy in children: findings from the Pediatric Cardiomyopathy Registry. Circulation. 2007;115:773–781. doi: 10.1161/CIRCULATIONAHA.106.621185. [DOI] [PubMed] [Google Scholar]
- 6.Towbin JA, Lowe AM, Colan SD, Sleeper LA, Orav EJ, Clunie S, Messere J, Cox GF, Lurie PR, Hsu D, Canter C, Wilkinson JD, Lipshultz SE. Incidence, causes, and outcomes of dilated cardiomyopathy in children. JAMA. 2006;296:1867–1876. doi: 10.1001/jama.296.15.1867. [DOI] [PubMed] [Google Scholar]
- 7.Lloyd-Jones DM, Larson MG, Leip EP, Beiser A, D’Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJ, Levy D Framingham Heart Study. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002;106:3068–3072. doi: 10.1161/01.cir.0000039105.49749.6f. [DOI] [PubMed] [Google Scholar]
- 8.Incidence and Prevalence: 2006 Chart Book on Cardiovascular and Lung Diseases. Bethesda, Md: National Heart, Lung, and Blood Institute; 2006. [Google Scholar]
- 9.Bahrami H, Kronmal R, Bluemke DA, Olson J, Shea S, Liu K, Burke GL, Lima JAC. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med. 2008;168:2138–2145. doi: 10.1001/archinte.168.19.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, Jacobsen SJ. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004;292:344–350. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 11.Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities study) Am J Cardiol. 2008;101:1016–1022. doi: 10.1016/j.amjcard.2007.11.061. [DOI] [PubMed] [Google Scholar]
- 12.Barker WH, Mullooly JP, Getchell W. Changing incidence and survival for heart failure in a well-defined older population 1970–1974 and 1990–1994. Circulation. 2006;113:799–805. doi: 10.1161/CIRCULATIONAHA.104.492033. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg RJ, Spencer FA, Farmer C, Meyer TE, Pezzella S. Incidence and hospital death rates associated with heart failure: a community-wide perspective. Am J Med. 2005;118:728–734. doi: 10.1016/j.amjmed.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 14.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–1562. [PubMed] [Google Scholar]
- 16.Bibbins-Domingo K, Lin F, Vittinghoff E, Barrett-Connor E, Hulley SB, Grady D, Shlipak MG. Predictors of heart failure among women with coronary disease. Circulation. 2004;110:1424–1430. doi: 10.1161/01.CIR.0000141726.01302.83. [DOI] [PubMed] [Google Scholar]
- 17.From AM, Leibson CL, Bursi F, Redfield MM, Weston SA, Jacobsen SJ, Rodeheffer RJ, Roger VL. Diabetes in heart failure: prevalence and impact on outcome in the population. Am J Med. 2006;119:591–599. doi: 10.1016/j.amjmed.2006.05.024. [DOI] [PubMed] [Google Scholar]
- 18.Frankel DS, Vasan RS, D’Agostino RB, Sr, Benjamin EJ, Levy D, Wang TJ, Meigs JB. Resistin, adiponectin, and risk of heart failure: the Framingham Offspring Study. J Am Coll Cardiol. 2009;53:754–762. doi: 10.1016/j.jacc.2008.07.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Djousse L, Driver JA, Gaziano JM. Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA. 2009;302:394–400. doi: 10.1001/jama.2009.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalogeropoulos A, Georgiopoulou V, Kritchevsky SB, Psaty BM, Smith NL, Newman AB, Rodondi N, Satterfield S, Bauer DC, Bibbins-Domingo K, Smith AL, Wilson PWF, Vasan RS, Harris TB, Butler J. Epidemiology of incident heart failure in a contemporary elderly cohort: the health, aging, and body composition study. Arch Intern Med. 2009;169:708–715. doi: 10.1001/archinternmed.2009.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Redfield MM, Jacobsen SJ, Burnett JC, Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289:194–202. doi: 10.1001/jama.289.2.194. [DOI] [PubMed] [Google Scholar]
- 22.Bursi F, Weston SA, Redfield MM, Jacobsen SJ, Pakhomov S, Nkomo VT, Meverden RA, Roger VL. Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–2216. doi: 10.1001/jama.296.18.2209. [DOI] [PubMed] [Google Scholar]
- 23.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 24.Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, Murabito JM, Vasan RS. Long-term trends in the incidence and survival with heart failure. N Engl J Med. 2002;347:1397–1402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 25.Schappert SM, Rechtsteiner EA. Ambulatory Medical Care Utilization Estimates for 2007. Hyattsville, Md: National Center for Health Statistics; Natl Health Stat Rep. In press. [PubMed] [Google Scholar]
- 26.Dunlay SM, Redfield MM, Weston SA, Therneau TM, Hall Long K, Shah ND, Roger VL. Hospitalizations after heart failure diagnosis a community perspective. J Am Coll Cardiol. 2009;54:1695–1702. doi: 10.1016/j.jacc.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
10. Other Cardiovascular Diseases
See Table 10-1.
Table 10-1.
Rheumatic Fever/Rheumatic Heart Disease
| Population Group | Mortality, 2007: All Ages* |
Hospital Discharges, 2007: All Ages |
|---|---|---|
| Both sexes | 3201 | 61 000 |
| Males | 1026 (32.1%)† | 22 000 |
| Females | 2175 (67.9%)† | 39 000 |
| NH white males | 907 | … |
| NH white females | 1946 | … |
| NH black males | 84 | … |
| NH black females | 161 | … |
Ellipses (…) indicate that data are not available.
NH indicates non-Hispanic.
Mortality data are for whites and blacks and include Hispanics.
These percentages represent the portion of total mortality that is for males versus females.
Sources: Mortality: National Center for Health Statistics; data represent underlying cause of death only. Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics, and National Heart, Lung, and Blood Institute; data include those inpatients discharged alive, dead, or of unknown status.
Mortality and any-mention mortality in this section are for 2007. “Mortality” is the number of deaths in 2007 for the given underlying cause. Prevalence data are for 2006. Hospital discharge data are from the NHDS/NCHS; data include inpatients discharged alive, dead, or status unknown. Hospital discharge data for 2007 are based on ICD-9 codes.
Valvular Heart Disease
ICD-9 424; ICD-10 I34 to I38.
Mortality—23 313. Any-mention mortality—44 149. Hospital discharges—98 000.
Echocardiographic data from the CARDIA Study (n=4351), the ARIC Study (n=2435), and the CHS (n=5125) were pooled to assess the prevalence of valve disease. The prevalence increased with age, from 0.7% (95% CI 0.5% to 1.0%) in participants 18 to 44 years of age to 13.3% (95% CI 11.7% to 15.0%) in participants ≥75 years of age (P<0.0001). The prevalence of valve disease, adjusted to the US 2000 population, was 2.5% (95% CI 2.2% to 2.7%). The adjusted mortality risk ratio associated with valve disease was 1.36 (95% CI 1.15 to 1.62; P=0.0005).1
Doppler echocardiography data in 1696 men and 1893 women (54±10 years of age) attending a routine examination at the Framingham Study were used to assess the prevalence of valvular regurgitation. Mitral regurgitation and tricuspid regurgitation of more than or equal to mild severity were seen in 19.0% and 14.8% of men and 19.1% and 18.4% of women, respectively. Aortic regurgitation of more than or equal to trace severity was present in 13.0% of men and 8.5% of women.2
Aortic Valve Disorders
ICD-9 424.1; ICD-10 I35.
Mortality—15 183. Any-mention mortality—28 191. Hospital discharges—48 000.
Calcific aortic stenosis on a trileaflet valve or bicuspid aortic valve is the most common cause of aortic stenosis.3
In the MESA, a study of 5880 participants 45 to 84 years of age, aortic valve calcium was quantified with serial CT images. During a mean follow-up of 2.4 years, 210 subjects (4.1%) had a mean incidence rate of progression of 1.7% per year, which increased significantly with age. The incident aortic valve calcium risk was associated with several traditional cardiovascular risk factors, specifically age, male sex, BMI, and smoking.4
In the Euro Heart Survey, which included 4910 patients in more than 25 countries, aortic stenosis was the most frequent lesion, accounting for 43% of all patients who had valvular heart disease.5
Among men and women ≥65 years of age enrolled in the CHS who underwent echocardiography, the aortic valve was normal in 70% of cases, sclerotic without outflow obstruction in 29%, and stenotic in 2%. Aortic sclerosis was associated with an increase of ≈50% in the risk of death due to cardiovascular causes and the risk of MI.6 Clinical factors associated with aortic sclerosis and stenosis were similar to risk factors for atherosclerosis.7 These data largely exclude patients with congenital heart disease, a group that is expected to increasingly contribute to the prevalence of valve disease.
Mitral Valve Disorders
ICD-9 424.0; ICD-10 I34.
Mortality—2644. Any-mention mortality—5608. Hospital discharges—42 000.
Prevalence
In pooled data from the CARDIA, ARIC, and CHS studies, mitral valve disease was the most common valvular lesion. At least moderate mitral regurgitation occurred at a frequency of 1.7% as adjusted to the US adult population of 2000, increasing from 0.5% to 9.3% between 18 and ≥75 years of age.1
Isolated mitral stenosis is more common in women and occurs in 40% of all patients presenting with rheumatic HD.8
The NHLBI-sponsored FHS reports that among people 26 to 84 years of age, the prevalence of mitral valve disorders is ≈1% to 2% and equal between women and men.9
The prevalence of mitral valve prolapse in the general population was evaluated with the use of echocardiograms of 1845 women and 1646 men who participated in the fifth examination of the Offspring Cohort of the FHS. The prevalence of mitral valve prolapse was 2.4%. The frequencies of chest pain, dyspnea, and electrocardiographic abnormalities were similar among subjects with prolapse and those without prolapse.9
Pulmonary Valve Disorders
ICD-9 424.3; ICD-10 I37.
Mortality—15. Any-mention mortality—43.
Tricuspid Valve Disorders
ICD-9 424.2; ICD-10 I36.
Mortality—23. Any-mention mortality—97.
Rheumatic Fever/Rheumatic HD
ICD-9 390 to 398; ICD-10 I00 to I09.
Mortality—3201. Any-mention mortality—5838.
The incidence of acute rheumatic fever has decreased in the United States.10
Although localized outbreaks have occurred, the overall incidence of acute rheumatic fever remains very low in most areas of the United States.11,12
The incidence of rheumatic fever remains high in blacks, Puerto Ricans, Mexican Americans, and American Indians.13
In 1950, ≈15 000 Americans (adjusted for changes in ICD codes) died of rheumatic fever/rheumatic HD compared with ≈3300 today (NCHS/NHLBI).
From 1996 to 2006, the death rate for rheumatic fever/rheumatic HD fell 8.3%, and actual deaths declined 26.2% (NCHS/NHLBI).
The 2006 overall death rate for rheumatic fever/rheumatic HD was 1.1. Death rates were 0.8 for white males, 0.7 for black males, 1.3 for white females, and 0.9 for black females (NCHS/NHLBI).
Immune risk factors have been linked with rheumatic HD. Human leukocyte antigen (HLA) typing was performed in 120 black patients with severe chronic rheumatic HD requiring cardiac surgery; the HLA-DR 1 antigen was present in 12.6% of patients compared with 2.7% of normal control subjects, and the HLA-DRw6 antigen was present in 31.1% of patients compared with 15% of control subjects, which suggests that genetically determined immune response factors may play a role in the pathogenesis of severe chronic rheumatic HD.14
Bacterial Endocarditis
ICD-9 421.0; ICD-10 I33.0.
Any-mention mortality—2419. Hospital discharges—27 000, primary plus secondary diagnoses.
The 2007 AHA Guidelines on Prevention of Infective Endocarditis15 state that infective endocarditis (IE) is thought to result from the following sequence of events: (1) Formation of nonbacterial thrombotic endocarditis on the surface of a cardiac valve or elsewhere that endothelial damage occurs; (2) bacteremia; and (3) adherence of the bacteria in the bloodstream to nonbacterial thrombotic endocarditis and proliferation of bacteria within a vegetation. Viridans group streptococci are part of the normal skin, oral, respiratory, and gastrointestinal tract flora, and they cause ≥50% of cases of community-acquired nativevalve IE not associated with intravenous drug use.16
Transient bacteremia is common with manipulation of the teeth and periodontal tissues, and reported frequencies of bacteremia because of dental procedures vary widely: Tooth extraction, 10% to 100%; periodontal surgery, 36% to 88%; scaling and root planing, 8% to 80%; teeth cleaning, up to 40%; rubber dam matrix/wedge placement, 9% to 32%; and endodontic procedures, up to 20%. Transient bacteremia also occurs frequently during routine daily activities unrelated to dental procedures: Tooth brushing and flossing, 20% to 68%; use of wooden toothpicks, 20% to 40%; use of water-irrigation devices, 7% to 50%; and chewing food, 7% to 51%. When it is considered that the average person living in the United States has <2 dental visits per year, the frequency of bacteremia from routine daily activities is far greater than that associated with dental procedures.1
- Although the absolute risk for IE from a dental procedure is impossible to measure precisely, the best available estimates are as follows: If dental treatment causes 1% of all cases of viridans group streptococcal IE annually in the United States, the overall risk in the general population is estimated to be as low as 1 case of IE per 14 million dental procedures. The estimated absolute risk rates for IE from a dental procedure in patients with underlying cardiac conditions are as follows15:
-
—Mitral valve prolapse: 1 per 1.1 million procedures
-
—CHD: 1 per 475 000
-
—Rheumatic HD: 1 per 142 000
-
—Presence of a prosthetic cardiac valve: 1 per 114 000
-
—Previous IE: 1 per 95 000 dental procedures
-
—
Although these calculations of risk are estimates, it is likely that the number of cases of IE that result from a dental procedure is exceedingly small. Therefore, the number of cases that could be prevented by antibiotic prophylaxis, even if prophylaxis were 100% effective, is similarly small. One would not expect antibiotic prophylaxis to be near 100% effective, however, because of the nature of the organisms and choice of antibiotics.15
Endocarditis, Valve Unspecified
ICD-9 424.9; ICD-10 I38.
Mortality—5448. Any-mention mortality—10 469.
Kawasaki Disease
ICD-9 446.1; ICD-10 M30.3.
Mortality—4. Any-mention mortality—7. Hospital discharges—5000 (figure considered unreliable), primary plus secondary diagnoses.
Kawasaki disease (KD) is more prevalent in the United States than in Japan, where outbreaks occurred in 1979, 1982, and 1986 and where the majority of cases occurred in those under the age of 2 years and predominantly in boys.17
An estimated 4248 hospitalizations for KD occurred in the United States in 2000, with a median patient age of 2 years. Race-specific incidence rates indicate that KD is most common among Americans of Asian and Pacific Island descent (32.5 per 100 000 children <5 years of age), occurs with intermediate frequency in non-Hispanic blacks (16.9 per 100 000 children <5 years of age) and Hispanics (11.1 per 100 000 children <5 years of age), and is least common in whites (9.1 per 100 000 children <5 years of age).18 In the United States, KD is more common during the winter and early spring months; boys with KD outnumber girls by ≈1.5:1 to 1.7:1; and 76% of children with KD are <5 years of age.19
Venous Thromboembolism Epidemiology (Including Deep Vein Thrombosis and Pulmonary Embolism)20
Pulmonary Embolism
ICD-9 415.1; ICD-10 I26.
Mortality—7097. Any-mention mortality—27 824. Hospital discharges—146 000.
Deep Vein Thrombosis
ICD-9 451.1; ICD-10 I80.2.
Mortality—2381. Any-mention mortality—12 018.
Incidence
Venous thromboembolism (VTE) consists of deep vein thrombosis (DVT), which typically involves deep veins of the leg or pelvis, and its complication, pulmonary embolism (PE).
The average incidence of VTE among whites is 108 per 100 000 person-years, with ≈250 000 incident cases occurring annually among US whites.
VTE incidence appears to be similar or higher among African Americans and lower among Asian Americans and Native Americans.
With adjustment for the different age and sex distributions of African Americans, VTE incidence is ≈78 per 100 000, which suggests 27 000 incident VTE cases occur annually among US African Americans.
Modeling suggests that more than 900 000 incident or recurrent VTE events occur annually in the United States, of which approximately one third are fatal.
VTE incidence has not changed significantly over the last 25 years.
Incidence rates increase exponentially with age for both males and females for both DVT and PE.
Incidence rates are higher in women during childbearing years, whereas incidence rates after age 45 years are higher in men.
PE accounts for an increasing proportion of VTE with increasing age for both sexes.
Survival
Observed survival after VTE is significantly worse than expected survival for age and sex, and survival after PE is much worse than after DVT alone.
For almost one quarter of patients with PE, the initial clinical presentation is sudden death.
Thirty-day VTE survival is 74.8% (DVT alone, 96.2%; PE with or without DVT, 59.1%).21
PE is an independent predictor of reduced survival for up to 3 months.
Because most PE deaths are sudden and are usually attributed to underlying disease (eg, cancer; other chronic heart, lung, or renal disease), secular trends in VTE survival are confounded by autopsy rates.
Recurrence
VTE is a chronic disease with episodic recurrence; ≈30% of patients develop recurrence within the next 10 years.
The hazard of recurrence varies with the time since the incident event and is highest within the first 6 to 12 months.
Independent predictors of recurrence include increasing patient age and BMI; neurological disease with leg paresis; active cancer; lupus anticoagulant or antiphospholipid antibody, antithrombin, protein C, or protein S deficiency; and persistently increased plasma fibrin D-dimer.
Complications
VTE complications include venous stasis syndrome (VSS) (or postthrombotic syndrome), venous ulcer, and chronic thromboembolic pulmonary hypertension (CTEPH).
The 20-year cumulative VSS and venous ulcer incidence after proximal DVT is ≈40% and 3.7%, respectively.
CTEPH incidence is 6.5 per million person-years; ≈1400 incident CTEPH cases occur annually among US whites.
Risk Factors
Independent VTE risk factors include increasing patient age, surgery, trauma/fracture, hospital or nursing home confinement, active cancer, central vein catheterization or transvenous pacemaker, prior superficial vein thrombosis, varicose veins, and neurological disease with leg paresis, and among women, oral contraceptive use, pregnancy/ postpartum status, and hormone therapy.
Together, these risk factors account for >75% of all incident VTE that occurs in the community.
Compared with residents in the community, hospitalized residents have a >130-fold higher incidence of VTE (71 versus 9605 cases per 100 000 person-years).22
Hospitalization and nursing home residence together account for almost 60% of incident VTE events that occur in the community.
Pregnancy-associated VTE incidence is 200 per 100 000 woman-years; compared with nonpregnant women of childbearing age, the RR is increased ≈4-fold.
VTE risk during the postpartum period is ≈5-fold higher than during pregnancy.
VTE is highly heritable and follows a complex mode of inheritance that involves environmental interaction.
Inherited thrombophilias (eg, inherited antithrombin, protein C, or protein S deficiency; factor V Leiden; prothrombin G20210A; ABO blood type non-O) interact with such clinical risk factors (ie, environmental “exposures”) as oral contraceptives, pregnancy, hormone therapy, and surgery to compound VTE risk.
Similarly, genetic interaction compounds the risk of incident and recurrent VTE.
Peripheral Arterial Disease
Peripheral arterial disease (PAD) affects ≈8 million Americans and is associated with significant morbidity and mortality.23 Prevalence increases dramatically with age, and PAD disproportionately affects blacks.23
PAD affects 12% to 20% of Americans ≥65 years of age.24 Despite its prevalence and cardiovascular risk implications, only ≈70% to 80% of patients with PAD undergo recommended antiplatelet therapy or lipid-lowering therapy.25
In the general population, only ≈10% of people with PAD have the classic symptom of intermittent claudication. Approximately 40% do not complain of leg pain, whereas the remaining 50% have a variety of leg symptoms different from classic claudication.26,27 In an older, disabled population of women, however, as many as two thirds of individuals with PAD had no exertional leg symptoms.28
The risk factors for PAD are similar but not identical to those for CHD. DM and cigarette smoking are stronger risk factors for PAD than for CHD.29 ORs for associations of DM and smoking with symptomatic PAD are ≈3.0 to 4.0. Most studies suggest that the prevalence of PAD is similar in men and women.30
Pooled data from 11 studies in 6 countries found that PAD is a marker for systemic atherosclerotic disease. The ageand sex-adjusted RR of all-cause death was 2.35; for CVD mortality, it was 3.34; and for CHD fatal and nonfatal events combined, it was 2.13. The findings for stroke were slightly weaker but still significant, with a pooled RR of 1.86 for fatal and nonfatal events combined.31
A recent meta-analysis of 24 955 men and 23 339 women demonstrated that the association of the ankle brachial index (ABI) with mortality has a reverse J-shaped distribution in which participants with an ABI of 1.11 to 1.40 are at lowest risk for mortality.32 Furthermore, an ABI <0.90 added meaningfully to the Framingham Risk Score in predicting 10-year risk of total mortality, cardiovascular mortality, and major coronary events. An ABI <0.90 approximately doubled the risk of total mortality, cardiovascular mortality, and major coronary events in each Framingham Risk Score category.32
Among 508 patients (449 men) identified from 2 vascular laboratories in San Diego, CA, a decline in ABI of >0.15 within a 10-year period was associated with a subsequent increased risk of all-cause mortality (RR 2.4) and CVD mortality (RR of 2.8) at 3 years’ follow-up.33
Among 440 patients with PAD, male sex and smoking were more associated with aortoiliac (proximal) disease than infrailiac (distal) disease. In addition, aortoiliac disease was associated with an increased risk of mortality or cardiovascular events compared with infrailiac disease (adjusted HR 3.28, 95% CI 1.87 to 5.75).34
Men and women with PAD have higher levels of inflammatory biomarkers than individuals without PAD. Elevated levels of C-reactive protein were associated with an increased risk of developing PAD among men in the Physicians’ Health Study.35 The OR for developing PAD 5 years after C-reactive protein measurement was 2.1 for those in the highest versus lowest baseline quartile of C-reactive protein. Among participants in the Women’s Health Study, 12 years after soluble intercellular adhesion molecule-1 measurement, women in the highest baseline tertile for levels of soluble intercellular adhesion molecule-1 had a 2-fold increased risk of developing PAD compared with women in the lowest baseline tertile.36 Among individuals with PAD, higher levels of inflammatory biomarkers are associated with increased all-cause and cardiovascular mortality rates and increased risk of failure of lower-extremity revascularization procedures.37–39
Data from the NHANES 1999 to 2004 cohort demonstrated an inverse association between bilirubin levels and prevalence of PAD. A 0.1-mg/dL higher level of bilirubin was associated with a 6% reduction in the odds of PAD (OR 0.94, 95% CI 0.90 to 0.98) after adjustment for PAD risk factors.40
People with PAD have impaired function and quality of life. This is true even for people who do not report leg symptoms. Furthermore, patients with PAD, including those who are asymptomatic, experience a significant decline in lower-extremity functioning over time.41–43
Data from NHANES 1999 to 2000 (NCHS) show that high blood levels of lead and cadmium are associated with an increased prevalence of PAD. Exposure to these 2 metals can occur through cigarette smoke. The risk was 2.8 for high levels of cadmium and 2.9 for high levels of lead. The OR of PAD for current smokers was 4.13 compared with people who had never smoked.44
Results from NHANES 1999 to 2000 (NCHS) and the CHS showed a remarkably high prevalence of PAD among patients with renal insufficiency.45,46 In addition, chronic kidney disease is common among community-dwelling older men and women with a high ABI.46
Available evidence suggests that the prevalence of PAD in people of Hispanic origin is similar to or slightly higher than that in non-Hispanic whites.23,47
Among patients with established PAD, higher physical activity levels during daily life are associated with better overall survival rate, a lower risk of death because of CVD, and slower rates of functional decline.48,49 In addition, better 6-minute walk performance and faster walking speed are associated with lower rates of all-cause mortality, cardiovascular mortality, and mobility loss.50,51
A cross-sectional, population-based telephone survey of >2500 adults ≥50 years of age, with oversampling of blacks and Hispanics, found that 26% expressed familiarity with PAD. Of these, half were not aware that diabetes mellitus and smoking increase the risk of PAD. One in 4 knew that PAD is associated with increased risk of heart attack and stroke, and only 14% were aware that PAD could lead to amputation. All knowledge domains were lower in individuals with lower income and education levels.52
Arrhythmias (Disorders of Heart Rhythm)
ICD-9 426, 427; ICD-10 I46 to I49.
Mortality—40 759. Any-mention mortality—461 872. Hospital discharges—881 000.
In 2006, $3.1 billion ($7783 per discharge) was paid to Medicare beneficiaries for cardiac dysrhythmias.53
Atrial Fibrillation and Flutter
ICD-9 427.3; ICD-10 I48.
Mortality—14 490. Any-mention mortality—93 594. Prevalence—>2.2 million, projected to 2.66 million in 2010.54,55 Incidence—>75 000.55 Hospital discharges—529 000.
Participants in the NHLBI-sponsored FHS study were followed up from 1968 to 1999. At 40 years of age, remaining lifetime risks for AF were 26.0% for men and 23.0% for women. At 80 years of age, lifetime risks for AF were 22.7% for men and 21.6% for women. In further analysis, counting only those who had development of AF without prior or concurrent HF or MI, lifetime risk for AF was ≈16%.56
Data from a large community-based population suggest that AF is less prevalent in blacks than in whites, both overall and in the setting of congestive heart failure.54,57
- Data from the NHDS/NCHS (1996 –2001) on cases that included AF as a primary discharge diagnosis found the following58:
-
—Approximately 44.8% of patients were men.
-
—The mean age for men was 66.8 years versus 74.6 years for women.
-
—The racial breakdown for admissions was 71.2% white, 5.6% black, and 2.0% other races (20.8% were not specified).
-
—Black patients were much younger than patients of other races.
-
—The incidence in men ranged from 20.58 per 100 000 people per year for patients between 15 and 44 years of age to 1077.39 per 100 000 people per year for patients ≥85 years of age. In women, the incidence ranged from 6.64 per 100 000 people per year for patients between 15 and 44 years of age to 1203.7 per 100 000 people per year for those ≥85 years of age.
-
—From 1996 to 2001, hospitalizations with AF as the first-listed diagnosis increased by 34%.
-
—
- In 1999, the CDC analyzed data from national and state multiple-cause mortality statistics and Medicare hospital claims for people with AF. The most common disease listed as the primary diagnosis for people hospitalized with AF was HF (11.8%), followed by AF (10.9%), CHD (9.9%), and stroke (4.9%).59 In Olmsted County, MN, the age-adjusted incidence of clinically recognized AF in a white population increased by 12.6% between 1980 and 2000.60,61
-
—The incidence of AF was greater in men (incidence ratio for men over women 1.86) and increased markedly with older age.60
-
—If incidence estimates are applied to US population projections from the Census Bureau, the projected number of people with AF may exceed 12 million by 2050.60
-
—Among Medicare patients ≥65 years of age, AF prevalence increased from 3.2% in 1992 to 6.0% in 2002, with higher prevalence in older subsets of the study population. Stroke rates per 1000 patient-years declined in AF patients on anticoagulants from 46.7 in 1992 to 19.5 in 2002 for ischemic stroke but remained fairly steady for hemorrhagic stroke (1.6 to 2.9).62
-
—AF independently increases the risk of ischemic stroke by 4- to 5-fold.63
-
—AF is responsible for at least 15% to 20% of all ischemic strokes.55
-
—Paroxysmal, persistent, and permanent AF all appear to increase the risk of ischemic stroke to a similar degree.64
-
—AF is also an independent risk factor for ischemic stroke severity and recurrence. In 1 study, people who had AF and were not treated with anticoagulants had a 2.1-fold increase in risk for recurrent stroke and a 2.4-fold increase in risk for recurrent severe stroke.65
- —
-
—
A study of >4600 patients diagnosed with first AF showed that risk of death within the first 4 months after the AF diagnosis was high. The most common causes of CVD death were CAD, HF, and ischemic stroke, accounting for 22%, 14%, and 10% respectively, of the early deaths (within the first 4 months) and 15%, 16%, and 7%, respectively, of the late deaths.61
Other Arrhythmias
Tachycardia
ICD-9 427.0, 1, 2; ICD-10 I47.0, 147.1, 147.2, 147.9.
Mortality—601. Any-mention mortality—5921. Hospital discharges—75 000.
Paroxysmal Supraventricular Tachycardia
ICD-9 427.0; ICD-10 I47.1.
Mortality—140. Any-mention mortality—1262. Hospital discharges—27 000.
Ventricular Fibrillation
ICD-9 427.4; ICD-10 I49.0.
Mortality—1024. Any-mention mortality—9297. Hospital discharges—7000.
VF is listed as the cause of relatively few deaths, but the overwhelming majority of sudden cardiac deaths due to coronary disease (estimated at ≈310 000 per year) are thought to be due to ventricular fibrillation.
- In Olmsted County, MN, the incidence of out-of-hospital treated VF decreased from 1985 to 200268:
-
—1985 to 1989: 26.3 per 100 000 (95% CI 21.0 to 32.6)
-
—1990 to 1994: 18.2 per 100 000 (95% CI 14.1 to 23.1)
-
—1995 to 1999: 13.8 per 100 000 (95% CI 10.4 to 17.9)
-
—2000 to 2002: 7.7 per 100 000 (95% CI 4.7 to 11.9)
-
—
Arteries, Diseases of
ICD-9 440 to 448; ICD-10 I70–I79. Includes PAD.
Mortality—30 172. Any-mention mortality—92 168. Hospital discharges—268 000.
Aortic Aneurysm
ICD-9 441; ICD-10 I71.
Mortality—12 986. Any-mention mortality—18 346. Hospital discharges—55 000.
Although the definition varies somewhat by age and body surface area, generally an abdominal aortic aneurysm (AAA) is considered to be present when the anteroposterior diameter of the aorta reaches 3.0 cm.29
The prevalence of AAAs 2.9 to 4.9 cm in diameter ranges from 1.3% in men 45 to 54 years of age to 12.5% in men 75 to 84 years of age. For women, the prevalence ranges from 0% in the youngest to 5.2% in the oldest age groups.29
Factors associated with increased prevalence of AAA include older age, male sex, family history of AAA, tobacco use, hypertension, and manifest atherosclerotic disease in other vascular beds, including the coronary and peripheral arteries.29,69 The association of dyslipidemia with AAA is mixed.70
Patients with DM are approximately half as likely as patients without DM to have an AAA.71,72
Male sex, older age, and smoking are important risk factors for incident AAA in the next 7 years.73
- Large AAAs tend to expand more rapidly than small AAAs, and large AAAs are at substantially higher risk for rupture.29
-
—Average annual expansion rates are ≈1 to 4 mm for aneurysms <4.0 cm in diameter, 4 to 5 mm for AAAs 4.0 to 6.0 cm in diameter, and as much as 7 to 8 mm for AAAs >6.0 cm in diameter.
-
—Absolute risk for eventual rupture is ≈20% for AAAs >5.0 cm, ≈40% for AAAs >6.0 cm, and >50% for AAAs >7.0 cm in diameter.
-
—Rupture of an AAA may be associated with death rates as high as 90%.
-
—
Atherosclerosis
ICD-9 440; ICD-10 I70.
Mortality—8232. Any-mention mortality—46 962. Hospital discharges—123 000.
Atherosclerosis is a process that leads to a group of diseases characterized by a thickening of artery walls. Atherosclerosis causes many deaths due to heart attack and stroke and accounts for nearly three fourths of all deaths because of CVD (FHS, NHLBI).
Analysis of data from the Reduction of Atherothrombosis for Continued Health (REACH) Registry74 showed that atherothrombosis (CAD, CVD, and PAD) is associated with the main causes of death on a worldwide scale. Despite decreases in age-adjusted death rates, the absolute number of deaths attributable to these conditions continues to increase, and prevalence is increasing sharply in other parts of the world. Atherothrombotic diseases are projected to be the leading cause of death worldwide in 2020. In the REACH study, outpatients with established atherosclerotic arterial disease or at risk of atherothrombosis experienced relatively high annual cardiovascular event rates. Multiple disease locations increased the 1-year risk of cardiovascular events.75
Other Diseases of Arteries
ICD-9 442 to 448; ICD-10 I72 to I78.
Mortality—8954. Any-mention mortality—30 727. Hospital discharges—90 000.
Abbreviations Used in Chapter 10
- AAA
abdominal aortic aneurysm
- ABI
ankle brachial index
- AF
atrial fibrillation
- AHA
American Heart Association
- ARIC
Atherosclerosis Risk In Communities
- BMI
body mass index
- CAD
coronary artery disease
- CARDIA
Coronary Artery Risk Development in Young Adults
- CDC
Centers for Disease Control and Prevention
- CHD
coronary heart disease
- CHS
Cardiovascular Health Study
- CI
confidence interval
- CT
computed tomography
- CTEPH
chronic thromboembolic pulmonary hypertension
- CVD
cardiovascular disease
- DM
diabetes mellitus
- DVT
deep vein thrombosis
- FHS
Framingham Heart Study
- HD
heart disease
- HF
heart failure
- HLA
human leukocyte antigen
- HR
hazard ratio
- ICD-9
International Classification of Diseases, 9th Revision
- ICD-10
International Classification of Diseases, 10th Revision
- IE
infective endocarditis
- KD
Kawasaki disease
- MESA
Multi-Ethnic Study of Atherosclerosis
- MI
myocardial infarction
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- NHDS
National Hospital Discharge Survey
- NHLBI
National Heart, Lung, and Blood Institute
- OR
odds ratio
- PAD
peripheral arterial disease
- PE
pulmonary embolism
- REACH
Reduction of Atherothrombosis for Continued Health
- RR
relative risk
- VF
ventricular fibrillation
- VSS
venous stasis syndrome
- VTE
venous thromboembolism
References
- 1.Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368:1005–1011. doi: 10.1016/S0140-6736(06)69208-8. [DOI] [PubMed] [Google Scholar]
- 2.Singh JP, Evans JC, Levy D, Larson MG, Freed LA, Fuller DL, Lehman B, Benjamin EJ. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study) Am J Cardiol. 1999;83:897–902. doi: 10.1016/s0002-9149(98)01064-9. [published correction appears in Am J Cardiol. 1999;84:1143]. [DOI] [PubMed] [Google Scholar]
- 3.Roberts WC, Ko JM. Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation. 2005;111:920–925. doi: 10.1161/01.CIR.0000155623.48408.C5. [DOI] [PubMed] [Google Scholar]
- 4.Owens DS, Katz R, Takasu J, Kronmal R, Budoff MJ, O’Brien KD. Incidence and progression of aortic valve calcium in the Multi-Ethnic Study of Atherosclerosis (MESA) Am J Cardiol. 2010;105:701–708. doi: 10.1016/j.amjcard.2009.10.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, Tornos P, Vanoverschelde JL, Vermeer F, Boersma E, Ravaud P, Vahanian A. A prospective survey of patients with valvular heart disease in Europe: the Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003;24:1231–1243. doi: 10.1016/s0195-668x(03)00201-x. [DOI] [PubMed] [Google Scholar]
- 6.Otto CM, Lind BK, Kitzman DW, Gersh BJ, Siscovick DS. Association of aortic-valve sclerosis with cardiovascular mortality and morbidity in the elderly. N Engl J Med. 1999;341:142–147. doi: 10.1056/NEJM199907153410302. [DOI] [PubMed] [Google Scholar]
- 7.Stewart BF, Siscovick D, Lind BK, Gardin JM, Gottdiener JS, Smith VE, Kitzman DW, Otto CM. Clinical factors associated with calcific aortic valve disease: Cardiovascular Health Study. J Am Coll Cardiol. 1997;29:630–634. doi: 10.1016/s0735-1097(96)00563-3. [DOI] [PubMed] [Google Scholar]
- 8.Rowe JC, Bland EF, Sprague HB, White PD. The course of mitral stenosis without surgery: ten- and twenty-year perspective. Ann Intern Med. 1960;52:741–749. doi: 10.7326/0003-4819-52-4-741. [DOI] [PubMed] [Google Scholar]
- 9.Freed LA, Levy D, Levine RA, Larson MG, Evans JC, Fuller DL, Lehman B, Benjamin EJ. Prevalence and clinical outcome of mitral-valve prolapse. N Engl J Med. 1999;341:1–7. doi: 10.1056/NEJM199907013410101. [DOI] [PubMed] [Google Scholar]
- 10.Lee GM, Wessels MR. Changing epidemiology of acute rheumatic fever in the United States. Clin Infect Dis. 2006;42:448–450. doi: 10.1086/499817. [DOI] [PubMed] [Google Scholar]
- 11.Miyake CY, Gauvreau K, Tani LY, Sundel RP, Newburger JW. Characteristics of children discharged from hospitals in the United States in 2000 with the diagnosis of acute rheumatic fever. Pediatrics. 2007;120:503–508. doi: 10.1542/peds.2006-3606. [DOI] [PubMed] [Google Scholar]
- 12.Gerber MA, Baltimore RS, Eaton CB, Gewitz M, Rowley AH, Shulman ST, Taubert KA. Prevention of rheumatic fever and diagnosis and treatment of acute streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology, and the Interdisciplinary Council on Quality of Care and Outcomes Research. Circulation. 2009;119:1541–1551. doi: 10.1161/CIRCULATIONAHA.109.191959. [DOI] [PubMed] [Google Scholar]
- 13.Thom TJ, Kannel WB, Silbershatz H, D’Agostino RB., Sr . Cardiovascular diseases in the United States and prevention approaches. In: Fuster V, Alexander RW, O’Rourke RA, editors. Hurst’s The Heart. 10th ed. New York, NY: McGraw-Hill; 2001. pp. 3–18. [Google Scholar]
- 14.Maharaj B, Hammond MG, Appadoo B, Leary WP, Pudifin DJ. HLA-A, B, DR, and DQ antigens in black patients with severe chronic rheumatic heart disease. Circulation. 1987;76:259–261. doi: 10.1161/01.cir.76.2.259. [DOI] [PubMed] [Google Scholar]
- 15.Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, Bolger A, Cabell CH, Takahashi M, Baltimore RS, Newburger JW, Strom BL, Tani LY, Gerber M, Bonow RO, Pallasch T, Shulman ST, Rowley AH, Burns JC, Ferrieri P, Gardner T, Goff D, Durack DT. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007;116:1736–1754. doi: 10.1161/CIRCULATIONAHA.106.183095. [published correction appears in Circulation. 2007;116:e376–e377]. [DOI] [PubMed] [Google Scholar]
- 16.Fowler VG, Scheld WM, Bayer AS. Endocarditis and intravascular infections. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and Practices of Infectious Diseases. 6th ed. New York, NY: Elsevier; 2005. pp. 975–1021. [Google Scholar]
- 17.Hata A, Onouchi Y. Susceptibility genes for Kawasaki disease: toward implementation of personalized medicine. J Hum Genet. 2009;54:67–73. doi: 10.1038/jhg.2008.9. [DOI] [PubMed] [Google Scholar]
- 18.Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, Shulman ST, Bolger AF, Ferrieri P, Baltimore RS, Wilson WR, Baddour LM, Levison ME, Pallasch TJ, Falace DA, Taubert KA. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2004;110:2747–2771. doi: 10.1161/01.CIR.0000145143.19711.78. [DOI] [PubMed] [Google Scholar]
- 19.Chang RK. The incidence of Kawasaki disease in the United States did not increase between 1988 and 1997. Pediatrics. 2003;111(pt 1):1124–1125. doi: 10.1542/peds.111.5.1124. [DOI] [PubMed] [Google Scholar]
- 20.Heit JA. The epidemiology of venous thromboembolism in the community. Arterioscler Thromb Vasc Biol. 2008;28:370–372. doi: 10.1161/ATVBAHA.108.162545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heit JA, Silverstein MD, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ., III Predictors of survival after deep vein thrombosis and pulmonary embolism: a population-based, cohort study. Arch Intern Med. 1999;159:445–453. doi: 10.1001/archinte.159.5.445. [DOI] [PubMed] [Google Scholar]
- 22.Heit JA, Melton LJ, III, Lohse CM, Petterson TM, Silverstein MD, Mohr DN, O’Fallon WM. Incidence of venous thromboembolism in hospitalized patients versus community residents. Mayo Clin Proc. 2001;76:1102–1110. doi: 10.4065/76.11.1102. [DOI] [PubMed] [Google Scholar]
- 23.Allison MA, Ho E, Denenberg JO, Langer RD, Newman AB, Fabsitz RR, Criqui MH. Ethnic-specific prevalence of peripheral arterial disease in the United States. Am J Prev Med. 2007;32:328–333. doi: 10.1016/j.amepre.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 24.Ostchega Y, Paulose-Ram R, Dillon CF, Gu Q, Hughes JP. Prevalence of peripheral arterial disease and risk factors in people aged 60 and older: data from the National Health and Nutrition Examination Survey 1999–2004. J Am Geriatr Soc. 2007;55:583–589. doi: 10.1111/j.1532-5415.2007.01123.x. [DOI] [PubMed] [Google Scholar]
- 25.Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL, Goto S, Liau CS, Richard AJ, Röther J, Wilson PW REACH Registry Investigators. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA. 2006;295:180–189. doi: 10.1001/jama.295.2.180. [DOI] [PubMed] [Google Scholar]
- 26.Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW, Krook SH, Hunninghake DB, Comerota AJ, Walsh ME, McDermott MM, Hiatt WR. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286:1317–1324. doi: 10.1001/jama.286.11.1317. [DOI] [PubMed] [Google Scholar]
- 27.McDermott MM, Greenland P, Liu K, Guralnik JM, Criqui MH, Dolan NC, Chan C, Celic L, Pearce WH, Schneider JR, Sharma L, Clark E, Gibson D, Martin GJ. Leg symptoms in peripheral arterial disease: associated clinical characteristics and functional impairment. JAMA. 2001;286:1599–1606. doi: 10.1001/jama.286.13.1599. [DOI] [PubMed] [Google Scholar]
- 28.McDermott MM, Fried L, Simonsick E, Ling S, Guralnik JM. Asymptomatic peripheral arterial disease is independently associated with impaired lower extremity functioning: the Women’s Health and Aging Study. Circulation. 2000;101:1007–1012. doi: 10.1161/01.cir.101.9.1007. [published correction appears in Circulation. 2001;104:504] [DOI] [PubMed] [Google Scholar]
- 29.Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, Rosenfield KA, Sacks D, Stanley JC, Taylor LM, Jr, White CJ, White J, White RA, Antman EM, Smith SC, Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Hunt SA, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) Circulation. 2006;113:e463–e654. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]
- 30.Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG TASC II Working Group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) J Vasc Surg. 2007;45(suppl S):S5–S67. doi: 10.1016/j.jvs.2006.12.037. [DOI] [PubMed] [Google Scholar]
- 31.Heald CL, Fowkes FG, Murray GD, Price JF Ankle Brachial Index Collaboration. Risk of mortality and cardiovascular disease associated with the ankle-brachial index: systematic review. Atherosclerosis. 2006;189:61–69. doi: 10.1016/j.atherosclerosis.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 32.Ankle Brachial Index Collaboration. Fowkes FG, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE, Folsom AR, Hirsch AT, Dramaix M, deBacker G, Wautrecht JC, Kornitzer M, Newman AB, Cushman M, Sutton-Tyrrell K, Fowkes FG, Lee AJ, Price JF, d’Agostino RB, Murabito JM, Norman PE, Jamrozik K, Curb JD, Masaki KH, Rodríguez BL, Dekker JM, Bouter LM, Heine RJ, Nijpels G, Stehouwer CD, Ferrucci L, McDermott MM, Stoffers HE, Hooi JD, Knottnerus JA, Ogren M, Hedblad B, Witteman JC, Breteler MM, Hunink MG, Hofman A, Criqui MH, Langer RD, Fronek A, Hiatt WR, Hamman R, Resnick HE, Guralnik J, McDermott MM. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA. 2008;300:197–208. doi: 10.1001/jama.300.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Criqui MH, Ninomiya JK, Wingard DL, Ji M, Fronek A. Progression of peripheral arterial disease predicts cardiovascular disease morbidity and mortality. J Am Coll Cardiol. 2008;52:1736–1742. doi: 10.1016/j.jacc.2008.07.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aboyans V, Desormais I, Lacroix P, Salazar J, Criqui MH, Laskar M. The general prognosis of patients with peripheral arterial disease differs according to the disease localization. J Am Coll Cardiol. 2010;55:898–903. doi: 10.1016/j.jacc.2009.09.055. [DOI] [PubMed] [Google Scholar]
- 35.Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Plasma concentration of C-reactive protein and risk of developing peripheral vascular disease. Circulation. 1998;97:425–428. doi: 10.1161/01.cir.97.5.425. [DOI] [PubMed] [Google Scholar]
- 36.Pradhan AD, Shrivastava S, Cook NR, Rifai N, Creager MA, Ridker PM. Symptomatic peripheral arterial disease in women: nontraditional biomarkers of elevated risk. Circulation. 2008;117:823–831. doi: 10.1161/CIRCULATIONAHA.107.719369. [DOI] [PubMed] [Google Scholar]
- 37.Owens CD, Ridker PM, Belkin M, Hamdan AD, Pomposelli F, Logerfo F, Creager MA, Conte MS. Elevated C-reactive protein levels are associated with postoperative events in patients undergoing lower extremity vein bypass surgery. J Vasc Surg. 2007;45:2–9. doi: 10.1016/j.jvs.2006.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vidula H, Tian L, Liu K, Criqui MH, Ferrucci L, Pearce WH, Greenland P, Green D, Tan J, Garside DB, Guralnik J, Ridker PM, Rifai N, McDermott MM. Biomarkers of inflammation and thrombosis as predictors of near-term mortality in patients with peripheral arterial disease: a cohort study. Ann Intern Med. 2008;148:85–93. doi: 10.7326/0003-4819-148-2-200801150-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Criqui MH, Ho LA, Denenberg J, Ridker PM, Wassel CL, McDermott MM. Biomarkers in peripheral arterial disease patients and near- and longer-term mortality. J Vasc Surg. 2010;52:85–90. doi: 10.1016/j.jvs.2010.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Perlstein TS, Pande RL, Beckman JA, Creager MA. Serum total bilirubin level and prevalent lower-extremity peripheral arterial disease: National Health and Nutrition Examination Survey (NHANES) 1999 to 2004. Arterioscler Thromb Vasc Biol. 2008;28:166–172. doi: 10.1161/ATVBAHA.107.153262. [DOI] [PubMed] [Google Scholar]
- 41.McDermott MM, Greenland P, Liu K, Guralnik JM, Celic L, Criqui MH, Chan C, Martin GJ, Schneider J, Pearce WH, Taylor LM, Clark E. The ankle brachial index is associated with leg function and physical activity: the Walking and Leg Circulation Study. Ann Intern Med. 2002;136:873–883. doi: 10.7326/0003-4819-136-12-200206180-00008. [published correction appears in Ann Intern Med. 2003;139:306]. [DOI] [PubMed] [Google Scholar]
- 42.McDermott MM, Liu K, Greenland P, Guralnik JM, Criqui MH, Chan C, Pearce WH, Schneider JR, Ferrucci L, Celic L, Taylor LM, Vonesh E, Martin GJ, Clark E. Functional decline in peripheral arterial disease: associations with the ankle brachial index and leg symptoms. JAMA. 2004;292:453–461. doi: 10.1001/jama.292.4.453. [DOI] [PubMed] [Google Scholar]
- 43.McDermott MM, Guralnik JM, Tian L, Liu K, Ferrucci L, Liao Y, Sharma L, Criqui MH. Associations of borderline and low normal ankle-brachial index values with functional decline at 5-year follow-up: the WALCS (Walking and Leg Circulation Study) J Am Coll Cardiol. 2009;53:1056–1062. doi: 10.1016/j.jacc.2008.09.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Navas-Acien A, Selvin E, Sharrett AR, Calderon-Aranda E, Silbergeld E, Guallar E. Lead, cadmium, smoking, and increased risk of peripheral arterial disease. Circulation. 2004;109:3196–3201. doi: 10.1161/01.CIR.0000130848.18636.B2. [DOI] [PubMed] [Google Scholar]
- 45.O’Hare AM, Glidden DV, Fox CS, Hsu CY. High prevalence of peripheral arterial disease in persons with renal insufficiency: results from the National Health and Nutrition Examination Survey 1999–2000. Circulation. 2004;109:320–323. doi: 10.1161/01.CIR.0000114519.75433.DD. [DOI] [PubMed] [Google Scholar]
- 46.Ix JH, Katz R, De Boer IH, Kestenbaum BR, Allison MA, Siscovick DS, Newman AB, Sarnak MJ, Shlipak MG, Criqui MH. Association of chronic kidney disease with the spectrum of ankle brachial index: the CHS (Cardiovascular Health Study) J Am Coll Cardiol. 2009;54:1176–1184. doi: 10.1016/j.jacc.2009.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Criqui MH, Vargas V, Denenberg JO, Ho E, Allison M, Langer RD, Gamst A, Bundens WP, Fronek A. Ethnicity and peripheral arterial disease: the San Diego Population Study. Circulation. 2005;112:2703–2707. doi: 10.1161/CIRCULATIONAHA.105.546507. [DOI] [PubMed] [Google Scholar]
- 48.Garg PK, Tian L, Criqui MH, Liu K, Ferrucci L, Guralnik JM, Tan J, McDermott MM. Physical activity during daily life and mortality in patients with peripheral arterial disease. Circulation. 2006;114:242–248. doi: 10.1161/CIRCULATIONAHA.105.605246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garg PK, Liu K, Tian L, Guralnik JM, Ferrucci L, Criqui MH, Tan J, McDermott MM. Physical activity during daily life and functional decline in peripheral arterial disease. Circulation. 2009;119:251–260. doi: 10.1161/CIRCULATIONAHA.108.791491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McDermott MM, Guralnik JM, Tian L, Ferrucci L, Liu K, Liao Y, Criqui MH. Baseline functional performance predicts the rate of mobility loss in persons with peripheral arterial disease. J Am Coll Cardiol. 2007;50:974–982. doi: 10.1016/j.jacc.2007.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McDermott MM, Tian L, Liu K, Guralnik JM, Ferrucci L, Tan J, Pearce WH, Schneider JR, Criqui MH. Prognostic value of functional performance for mortality in patients with peripheral artery disease. J Am Coll Cardiol. 2008;51:1482–1489. doi: 10.1016/j.jacc.2007.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hirsch AT, Murphy TP, Lovell MB, Twillman G, Treat-Jacobson D, Harwood EM, Mohler ER, 3rd, Creager MA, Hobson RW, Jr, Robertson RM, Howard WJ, Schroeder P, Criqui MH Peripheral Arterial Disease Coalition. Gaps in public knowledge of peripheral arterial disease: the first national PAD public awareness survey. Circulation. 2007;116:2086–2094. doi: 10.1161/CIRCULATIONAHA.107.725101. [DOI] [PubMed] [Google Scholar]
- 53.Centers for Medicare and Medicaid Services. Health Care Financing Review: Medicare &; Medicaid Statistical Supplement. Baltimore, Md: Centers for Medicare and Medicaid Services; 2005. [Accessed September 27, 2010]. Table 5.5: Discharges, Total Days of Care, and Program Payments for Medicare Beneficiaries Discharged from Short-Stay Hospitals, by Principal Diagnoses Within Major Diagnostic Classifications (MDCs): Calendar Year 2006. Available at: http://www.cms.hhs.gov/MedicareMedicaidStatSupp/downloads/2007Table5.5b.pdf. [Google Scholar]
- 54.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors In Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 55.Go AS. The epidemiology of atrial fibrillation in elderly persons: the tip of the iceberg. Am J Geriatr Cardiol. 2005;14:56–61. doi: 10.1111/j.1076-7460.2005.02278.x. [DOI] [PubMed] [Google Scholar]
- 56.Lloyd-Jones DM, Wang TJ, Leip EP, Larson MG, Levy D, Vasan RS, D’Agostino RB, Massaro JM, Beiser A, Wolf PA, Benjamin EJ. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004;110:1042–1046. doi: 10.1161/01.CIR.0000140263.20897.42. [DOI] [PubMed] [Google Scholar]
- 57.Ruo B, Capra AM, Jensvold NG, Go AS. Racial variation in the prevalence of atrial fibrillation among patients with heart failure: the Epidemiology, Practice, Outcomes, and Costs of Heart Failure (EPOCH) study. J Am Coll Cardiol. 2004;43:429–435. doi: 10.1016/j.jacc.2003.09.035. [DOI] [PubMed] [Google Scholar]
- 58.Khairallah F, Ezzedine R, Ganz LI, London B, Saba S. Epidemiology and determinants of outcome of admissions for atrial fibrillation in the United States from 1996 to 2001. Am J Cardiol. 2004;94:500–504. doi: 10.1016/j.amjcard.2004.04.068. [DOI] [PubMed] [Google Scholar]
- 59.Centers for Disease Control and Prevention (CDC) Atrial fibrillation as a contributing cause of death and Medicare hospitalization: United States, 1999. MMWR Morb Mortal Wkly Rep. 2003;52:128, 130–131. [PubMed] [Google Scholar]
- 60.Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward JB, Tsang TS. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–125. doi: 10.1161/CIRCULATIONAHA.105.595140. [published correction appears in Circulation. 2006;114:e498] [DOI] [PubMed] [Google Scholar]
- 61.Miyasaka Y, Barnes ME, Bailey KR, Cha SS, Gersh BJ, Seward JB, Tsang TS. Mortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-based study. J Am Coll Cardiol. 2007;49:986–992. doi: 10.1016/j.jacc.2006.10.062. [DOI] [PubMed] [Google Scholar]
- 62.Lakshminarayan K, Solid CA, Collins AJ, Anderson DC, Herzog CA. Atrial fibrillation and stroke in the general Medicare population: a 10-year perspective (1992 to 2002) Stroke. 2006;37:1969–1974. doi: 10.1161/01.STR.0000230607.07928.17. [DOI] [PubMed] [Google Scholar]
- 63.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–988. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 64.Hart RG, Pearce LA, Rothbart RM, McAnulty JH, Asinger RW, Halperin JL Stroke Prevention in Atrial Fibrillation Investigators. Stroke with intermittent atrial fibrillation: incidence and predictors during aspirin therapy. J Am Coll Cardiol. 2000;35:183–187. doi: 10.1016/s0735-1097(99)00489-1. [DOI] [PubMed] [Google Scholar]
- 65.Penado S, Cano M, Acha O, Hernández JL, Riancho JA. Atrial fibrillation as a risk factor for stroke recurrence. Am J Med. 2003;114:206–210. doi: 10.1016/s0002-9343(02)01479-1. [DOI] [PubMed] [Google Scholar]
- 66.Halligan SC, Gersh BJ, Brown RD, Jr, Rosales AG, Munger TM, Shen WK, Hammill SC, Friedman PA. The natural history of lone atrial flutter. Ann Intern Med. 2004;140:265–268. doi: 10.7326/0003-4819-140-4-200402170-00008. [DOI] [PubMed] [Google Scholar]
- 67.Seidl K, Hauer B, Schwick NG, Zellner D, Zahn R, Senges J. Risk of thromboembolic events in patients with atrial flutter. Am J Cardiol. 1998;82:580–583. doi: 10.1016/s0002-9149(98)00419-6. [DOI] [PubMed] [Google Scholar]
- 68.Bunch TJ, White RD, Friedman PA, Kottke TE, Wu LA, Packer DL. Trends in treated ventricular fibrillation out-of-hospital cardiac arrest: a 17-year population-based study. Heart Rhythm. 2004;1:255–259. doi: 10.1016/j.hrthm.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 69.Baumgartner I, Hirsch AT, Abola MT, Cacoub PP, Poldermans D, Steg PG, Creager MA, Bhatt DL. Cardiovascular risk profile and outcome of patients with abdominal aortic aneurysm in outpatients with atherothrombosis: data from the Reduction of Atherothrombosis for Continued Health (REACH) Registry. J Vasc Surg. 2008;48:808–814. doi: 10.1016/j.jvs.2008.05.026. [DOI] [PubMed] [Google Scholar]
- 70.Diehm N, Baumgartner I. Determinants of aneurysmal aortic disease. Circulation. 2009;119:2134–2135. doi: 10.1161/CIRCULATIONAHA.109.850180. [DOI] [PubMed] [Google Scholar]
- 71.Lederle FA, Johnson GR, Wilson SE, Chute EP, Littooy FN, Bandyk D, Krupski WC, Barone GW, Acher CW, Ballard DJ for the Aneurysm Detection and Management (ADAM) Veterans Affairs Cooperative Study Group. Prevalence and associations of abdominal aortic aneurysm detected through screening. Ann Intern Med. 1997;126:441–449. doi: 10.7326/0003-4819-126-6-199703150-00004. [DOI] [PubMed] [Google Scholar]
- 72.Vega de Céniga M, Gómez R, Estallo L, Rodríguez L, Baquer M, Barba A. Growth rate and associated factors in small abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2006;31:231–236. doi: 10.1016/j.ejvs.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 73.Forsdahl SH, Singh K, Solberg S, Jacobsen BK. Risk factors for abdominal aortic aneurysms: a 7-year prospective study: the Tromsø Study, 1994–2001. Circulation. 2009;119:2202–2208. doi: 10.1161/CIRCULATIONAHA.108.817619. [DOI] [PubMed] [Google Scholar]
- 74.Healthcare Cost and Utilization Project. Overview of the Kids’ Inpatient Database (KID) [Accessed September 28, 2010]; http://www.hcup-us.ahrq.gov/kidoverview.jsp.
- 75.Steg PG, Bhatt DL, Wilson PW, D’Agostino R, Jr, Ohman EM, Röther J, Liau CS, Hirsch AT, Mas JL, Ikeda Y, Pencina MJ, Goto S REACH Registry Investigators. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297:1197–1206. doi: 10.1001/jama.297.11.1197. [DOI] [PubMed] [Google Scholar]
11. Family History and Genetics
Prevalence
Family History of HD
- Among adults ≥20 years of age, 13.3% reported a parent or sibling with a heart attack or angina before the age of 50 years (NHANES question MCQ300a, combined for 2005 to 2008). The racial/ethnic breakdown is as follows:
-
—For non-Hispanic whites, 14.9% for men, 16.7% for women
-
—For non-Hispanic blacks, 10.0% for men, 12.4% for women
-
—For Mexican Americans, 8.8% for men, 12.3% for women
-
—For other races, 11.4% for men, 13.6% for women
-
—
- HD occurs as people age, and those without a family history of HD may survive longer, so the prevalence of family history will vary depending on the age at which it is assessed. The breakdown of reported family history of heart attack by age in the US population, as measured by NHANES, is as follows:
-
—Age 20 to 39 years, 10.3% for men, 11.6% for women
-
—Age 40 to 59 years, 14.1% for men, 18.4% for women
-
—Age 60 to 79 years, 12.4% for men, 15.5% for women
-
—Age ≥80 years, 11.2% for men, 9.2% for women
-
—
In the multigenerational FHS, only 75% of participants with a documented parental history of a heart attack before 55 years of age reported that history when asked.1
Impact of Family History
Genetics
The increased risk of HD seen in people with a family history of a heart attack is likely due in part to shared genetics. The full genetic basis for CVD has not yet been determined, and genetic markers discovered thus far have not been shown to add to existing cardiovascular risk prediction tools.5
- The most consistently replicated genetic marker for HD is located at 9p21.3. At this single nucleotide polymorphism (SNP), ≈27% of the white population is estimated to have 0 risk alleles, 50% is estimated to have 1 risk allele, and the remaining 23% is estimated to have 2 risk alleles.6
-
—The 10-year HD risk for a 65-year-old man with 2 alleles and no other traditional risk factors is ≈13.2%, whereas a similar man with 0 alleles would have a 10-year risk of ≈9.2%. The 10-year HD risk for a 40-year-old woman with 2 alleles and no other traditional risk factors is ≈2.4%, whereas a similar man with 0 alleles would have a 10-year risk of ≈1.7%.6
-
—The biological function of the 9p21.3 SNP is not yet known.
-
—
Abbreviations Used in Chapter 11
- CVD
cardiovascular disase
- FHS
Framingham Heart Study
- HD
heart disase
- NHANES
National Health and Nutrition Examination Survey
- SNP
single nucleotide polymorphism
References
- 1.Murabito JM, Nam BH, D’Agostino RB, Sr, Lloyd-Jones DM, O’Donnell CJ, Wilson PWF. Accuracy of offspring reports of parental cardiovascular disease history: the Framingham Offspring Study. Ann Intern Med. 2004;140:434–440. doi: 10.7326/0003-4819-140-6-200403160-00010. [DOI] [PubMed] [Google Scholar]
- 2.Lloyd-Jones DM, Nam BH, D’Agostino RB, Sr, Levy D, Murabito JM, Wang TJ, Wilson PW, O’Donnell CJ. Parental cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults: a prospective study of parents and offspring. JAMA. 2004;291:2204–2211. doi: 10.1001/jama.291.18.2204. [DOI] [PubMed] [Google Scholar]
- 3.Sesso HD, Lee I, Gaziano JM, Rexrode KM, Glynn RJ, Buring JE. Maternal and paternal history of myocardial infarction and risk of cardiovascular disease in men and women. Circulation. 2001;104:393–398. doi: 10.1161/hc2901.093115. [DOI] [PubMed] [Google Scholar]
- 4.Murabito JM, Pencina MJ, Nam BH, D’Agostino RB, Sr, Wang TJ, Lloyd-Jones D, Wilson PW, O’Donnell CJ. Sibling cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults. JAMA. 2005;294:3117–3123. doi: 10.1001/jama.294.24.3117. [DOI] [PubMed] [Google Scholar]
- 5.Paynter NP, Chasman DI, Paré G, Buring JE, Cook NR, Miletich JP, Ridker PM. Association between a literature-based genetic risk score and cardiovascular events in women. JAMA. 2010;303:631–637. doi: 10.1001/jama.2010.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palomaki GE, Melillo S, Bradley LA. Association between 9p21 genomic markers and heart disease: a meta-analysis. JAMA. 2010;303:648–656. doi: 10.1001/jama.2010.118. [DOI] [PubMed] [Google Scholar]
12. Risk Factor: Smoking/Tobacco Use
See Table 12-1 and Charts 12-1 and 12-2.
Table 12-1.
Cigarette Smoking
| Population Group | Prevalence, 2009 Age ≥18 y* |
Cost15 |
|---|---|---|
| Both sexes | 46 600 000 (20.6%) | $193 billion per year |
| Men | 25 700 000 (23.1%) | … |
| Women | 21 100 000 (18.1%) | … |
| NH white men | 25.0% | … |
| NH white women | 20.7% | … |
| NH black men | 22.9% | … |
| NH black women | 18.8% | … |
| Hispanic or Latino men | 17.6% | … |
| Hispanic or Latino women | 9.4% | … |
| Asian only (both sexes) | 11.6% | … |
| American Indian/Alaska Native only (both sexes) | 19.0% | … |
Ellipses (…) indicate data not available;
NH indicates non-Hispanic.
Percentages are age-adjusted. Estimates for Asian only, and American/Alaska Native only include non-Hispanic and Hispanic persons.
Data derived from Centers for Disease Control and Prevention/National Center for Health Statistics/National Health Interview Survey.7
Chart 12-1.
Prevalence (%) of students in grades 9 to 12 reporting current cigarette use by sex and race/ethnicity (Youth Risk Behavior Surveillance System, 2009). NH indicates non-Hispanic. Data derived from MMWR: Morbidity and Mortality Weekly Report.1
Chart 12-2.
Prevalence (%) of current smoking for adults >18 years of age by race/ethnicity and sex (National Health Interview Survey: 2006–2008). All percentages are age-adjusted. NH indicates non-Hispanic. *Includes both Hispanics and non-Hispanics. Data derived from Centers for Disease Control and Prevention/National Center for Health Statistics, Health Data Interactive.11
Prevalence
Youth
In 2009, in grades 9 through 12, 19.5% of students reported current cigarette use (on at least 1 day during the 30 days before the survey), 14.0% of students reported current cigar use, and 8.9% of students reported current smokeless tobacco use. Overall, 26.0% of students reported any current tobacco use (YRBSS).1
In 2009, in grades 9 to 12, male and female students were equally likely to report current cigarette use (19.8% compared with 19.1%); however, male students were more likely than female students to report current cigar use (18.6% compared with 8.8%) and current smokeless tobacco use (15.0% compared with 2.2%; YRBSS).1
In 2009, in grades 9 through 12, non-Hispanic white students were more likely than Hispanic or non-Hispanic black students to report any current tobacco use, which includes cigarettes, cigars, or smokeless tobacco (30.3% compared with 20.8% for Hispanic students and 16.2% for non-Hispanic black students; YRBSS).1
Among youths 12 to 17 years of age in 2008, 2.8 million (11.4%) used a tobacco product (cigarettes, cigars, or smokeless tobacco) in the past month, and 2.3 million (9.1%) used cigarettes, a decrease compared with 2007. Cigarette use in the past month in the age group declined from 13.0% in 2002 to 9.1% in 2008 (National Survey on Drug Use and Health [NSDUH]).2,3
- Data from the YRBSS4 for students in grades 9 to 12 indicated the following:
-
—The percentage of students who reported ever trying cigarettes remained stable from 1991 to 1999 and then declined from 70.4% in 1999 to 46.3% in 2009.
-
—The percentage who reported current cigarette use (on at least 1 day in the 30 days before the survey) increased between 1991 and 1997 and then declined from 36.4% in 1997 to 19.5% in 2009.
-
—The percentage who reported current frequent cigarette use (smoked on ≥20 of the 30 days before the survey) increased from 1991 to 1999 and then declined from 16.8% in 1999 to 7.3% in 2009.
-
—
In 2007, 60.9% of students in grades 9 to 12 who ever smoked cigarettes daily tried to quit smoking cigarettes. The prevalence of this behavior did not vary by grade but was higher among female students (67.3%) than male students (55.5%) and higher among black students (68.1%) than Hispanic students (54.1%). No other differences were found by race/ethnicity. Overall, 12.2% of students who ever smoked cigarettes daily tried to quit smoking cigarettes and were successful (YRBSS).5
Adults
From 1998 to 2009, the percentage of US adults ≥18 years of age who were current cigarette smokers declined from 24.1% to 20.6%; however, the percentage who were current smokers did not change significantly from 2005 to 2009 (NHIS).6,7
In 2009, among Americans ≥18 years of age, 23.1% of men and 18.1% of women were current cigarette smokers, putting them at increased risk of heart attack and stroke (NHIS).8
From 1998 to 2007, cigarette smoking prevalence among adults ≥18 years of age decreased in 44 states, the District of Columbia, and Puerto Rico. Six states had no substantial changes in prevalence after controlling for age, sex, and race/ethnicity. However, only Utah and the US Virgin Islands met the Healthy People 2010 target for reducing adult smoking prevalence to 12% (BRFSS).9
In 2009, among adults ≥18 years of age, the state with the highest percentage of current cigarette smokers was West Virginia (25.5%), and the state with the lowest percentage was Utah (9.8%; BRFSS).10
In 2006 to 2008, Asian adults ≥18 years of age (men 15.7%, women 4.5%) and Hispanic adults (men 18.4%, women 9.4%) were less likely to be current cigarette smokers than American Indian or Alaska Native adults (men 30.2%, women 22.1%), non-Hispanic white adults (men 24.0%, women 21.0%), and non-Hispanic black adults (men 25.0%, women 17.1%), on the basis of age-adjusted estimates (NHIS).11
In 2004 to 2006 data, adult cigarette smoking varied among Asian subgroups. Most Asian adults had never smoked, with rates ranging from 65% of Korean adults to 84% of Chinese adults. Korean adults (22%) were ≈2 to 3 times as likely to be current smokers as Japanese (12%), Asian Indian (7%), or Chinese (7%) adults on the basis of age-adjusted estimates (NHIS).12
In 2008, among people ≥65 years of age, 9.8% of men and 8.5% of women were current smokers. In this age group, men were more likely than women to be former smokers (54.3% compared with 28.9%) on the basis of age-adjusted estimates (NHIS).13
Among women 15 to 44 years of age, combined data for 2007 and 2008 indicated that the rate of past-month cigarette use was lower among those who were pregnant (16.4%) than among those who were not pregnant (27.3%). This pattern was evident among women 18 to 25 years of age (22.1% versus 32.3% for pregnant and nonpregnant women, respectively) and among women 26 to 44 years of age (12.6% versus 27.4%, respectively). Among those 15 to 17 years of age, the difference in the rate of cigarette smoking between pregnant and nonpregnant women was not statistically significant (NSDUH).2
In 2008, an estimated 70.9 million Americans ≥12 years of age were current (past month) users of a tobacco product (cigarettes, cigars, smokeless tobacco, or tobacco in pipes). The rate of current use of any tobacco product in this age range remained steady from 2007 to 2008 (28.6% and 28.4%, respectively; NSDUH).2
Incidence
In 2008, ≈2.4 million people ≥12 years of age smoked cigarettes for the first time within the past 12 months, which was similar to the estimate in 2007 (2.2 million). The 2008 estimate averages out to ≈6600 new cigarette smokers every day. Most new smokers (58.8%) in 2008 were <18 years of age when they first smoked cigarettes (NSDUH).2
Data from 2002 to 2004 suggest that ≈1 in 5 nonsmokers 12 to 17 years of age is likely to start smoking. Youths in the Mexican subpopulations were significantly more susceptible (28.8%) to start smoking than those in non- Hispanic white (20.8%), non-Hispanic black (23.0%), Cuban (16.4%), Asian Indian (15.4%), Chinese (15.3%), and Vietnamese (13.8%) subpopulations. There was no significant difference in susceptibility to start smoking between boys and girls in any of the major populations or subpopulations (NSDUH).14
Approximately 80% of people who use tobacco began at <18 years of age, according to a report from the Surgeon General of the United States. The most common age of initiation is 14 to 15 years.15
Mortality
During 2000 to 2004, cigarette smoking resulted in an estimated 443 000 premature deaths each year due to smoking-related illnesses, and ≈49 000 of these deaths were due to secondhand smoke (SHS). In adults ≥35 years of age, a total of 32.7% of these deaths were related to CVD.16
Each year from 2000 to 2004, smoking caused 3.1 million years of potential life lost for males and 2.0 million years for females, excluding deaths due to smoking-attributable residential fires and adult deaths due to SHS.16
From 2000 to 2004, smoking during pregnancy resulted in an estimated 776 infant deaths annually.16
During 2000 to 2004, cigarette smoking resulted in an estimated 269 655 deaths annually among males and 173 940 deaths annually among females.16
On average, male smokers die 13.2 years earlier than male nonsmokers, and female smokers die 14.5 years earlier than female nonsmokers.17
Current cigarette smoking is a powerful independent predictor of cardiac arrest in patients with CHD.18
After up to 14.5 years of follow-up of participants in the Lung Health Study of the NHLBI, the all-cause death rate among participants in a smoking-cessation intervention was significantly lower (15%) than among those given usual care.19
Secondhand Smoke
The national prevalence of households with smoke-free home rules increased from 43.2% during 1992 to 1993 to 72.2% in 2003 on the basis of data from the “Tobacco Use Supplement” to the “Current Population Survey.” During this period, the prevalence of such rules increased from 9.6% to 31.8% among households with at least 1 smoker and from 56.8% to 83.5% among households with no smokers. Approximately 126 million children and nonsmoking adults were still exposed to SHS in the United States as of 1999 to 2002.20
In 2008, data from 11 states showed that the majority of people surveyed in each state reported having smoke-free home rules, ranging from 68.8% in West Virginia to 85.6% in Arizona (BRFSS).21
The percentage of the US nonsmoking population with detectable serum cotinine declined from 52.5% in 1999 to 2000 to 40.1% in 2007 to 2008, with declines occurring for children and adults. During 2007 to 2008, the percentage of nonsmokers with detectable serum cotinine was higher for those 3 to 11 years of age (53.6%) and those 12 to 19 years of age (46.5%) than for those ≤20 years of age (36.7%); the percentage was also higher for non-Hispanic blacks (55.9%) than for non-Hispanic whites (40.1%) and Mexican Americans (28.5%; NHANES).22
- Data from a 2006 report of the US Surgeon General on the consequences of involuntary exposure to tobacco smoke23 indicate the following:
-
—Nonsmokers who are exposed to SHS at home or at work increase their risk of developing CHD by 25% to 30%.
-
—Short exposures to SHS can cause blood platelets to become stickier, damage the lining of blood vessels, and decrease coronary flow velocity reserves, potentially increasing the risk of an acute MI.
-
—
Aftermath
Among ever-smokers who had 1 circulatory disorder, 52.1% were current smokers, and among those who reported that they had ≥3 circulatory disorders, 28% were current smokers at the time of the interview. The adjusted odds of being a current smoker were lower for individuals who had ≥2 central circulatory disorders, such as MI, HF, or stroke, than for those without a central circulatory disorder.24
- The CDC’s “Health Effects of Cigarette Smoking” fact sheet25 provides the following information:
-
—Cigarette smokers are 2 to 4 times more likely to develop CHD than nonsmokers.
-
—Cigarette smoking approximately doubles a person’s risk for stroke.
-
—Cigarette smokers are >10 times as likely as nonsmokers to develop peripheral vascular disease.
-
—Smoking increases the risk of abdominal aortic aneurysm.
-
—
In 2006, 62.9% of adult current smokers 18 to 64 years of age with a checkup during the preceding year reported that they had been advised to quit, about the same percentage as in 2002 (63.5%; MEPS).26
Cost
Direct medical costs ($96 billion) and lost productivity costs ($97 billion) associated with smoking totaled an estimated $193 billion per year between 2000 and 2004.16
Abbreviations Used in Chapter 12
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CHD
coronary heart disease
- CVD
cardiovascular disease
- HF
heart failure
- MEPS
Medical Expenditure Panel Survey
- MI
myocardial infarction
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- NHIS
National Health Interview Survey
- NHLBI
National Heart, Lung, and Blood Institute
- NSDUH
National Survey on Drug Use and Health
- SHS
secondhand smoke
- YRBSS
Youth Risk Behavior Surveillance System
References
- 1.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Lim C, Whittle L, Brener ND, Wechsler H Centers for Disease Control and Prevention (CDC) Youth risk behavior surveillance: United States, 2009. MMWR Surveill Summ. 2010;59:1–142. [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration. Results From the 2008 National Survey on Drug Use and Health: National Findings. Rockville, Md: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2009. NSDUH series H-36, HHS publication No. SMA 09-4434. [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health: national findings, detailed tables. [Accessed June 11, 2010]; Available at: http://oas.samhsa.gov/NSDUH/2K8NSDUH/tabs/toc.htm.
- 4.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion. Healthy Youth! YRBBS: national trends in risk behaviors. [Accessed June 7, 2010]; Available at: http://www.cdc.gov/HealthyYouth/yrbs/trends.htm.
- 5.Centers for Disease Control and Prevention (CDC) High school students who tried to quit smoking cigarettes: United States, 2007. MMWR Morb Mortal Wkly Rep. 2009;58:428–431. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults and trends in smoking cessation: United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:1227–1232. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) Vital signs: current cigarette smoking among adults aged ≥18 years: United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:1135–1140. [PubMed] [Google Scholar]
- 8.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. [Accessed August 26, 2010];Vital Health Stat 10. 2010 No. 249. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_249.pdf. [PubMed]
- 9.Centers for Disease Control and Prevention (CDC) State-specific prevalence and trends in adult cigarette smoking: United States, 1998–2007. MMWR Morb Mortal Wkly Rep. 2009;58:221–226. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System survey data. Atlanta, Ga: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2009. [Accessed June 7, 2010]. Prevalence and trends data, tobacco use. Available at: http://www.cdc.gov/brfss. [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC) National Center for Health Statistics. Health Data Interactive. [Accessed June 11, 2010]; Available at: http://www.cdc.gov/nchs/hdi.htm.
- 12.Barnes PM, Adams PF, Powell-Griner E. Advance Data From Vital and Health Statistics. No. 394. Hyattsville, Md: National Center for Health Statistics; 2008. Health characteristics of the Asian Adult population: United States, 2004 –2006. [PubMed] [Google Scholar]
- 13.Crescioni M, Gorina Y, Bilheimer L, Gillum RF. Hyattsville, Md: National Center for Health Statistics; 2010. [Accessed June 11, 2010]. Trends in health status and health care use among older men. National Health Statistics Report No. 24. Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr024.pdf. [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention (CDC) Racial/ethnic differences among youths in cigarette smoking and susceptibility to start smoking: United States, 2002–2004. MMWR Morb Mortal Wkly Rep. 2006;55:1275–1277. [PubMed] [Google Scholar]
- 15.US Department of Health and Human Services. Atlanta, Ga: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1994. Preventing Tobacco Use Among Young People: A Report of the Surgeon General: Executive Summary. [Google Scholar]
- 16.Centers for Disease Control and Prevention (CDC) Smoking-attributable mortality, years of potential life lost, and productivity losses: United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57:1226–1228. [PubMed] [Google Scholar]
- 17.US Department of Health and Human Services. Atlanta, Ga: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. [Accessed September 28, 2010]. 2004 Surgeon General’s Report: The Health Consequences of Smoking. Available at: http://www.cdc.gov/tobacco/data_statistics/sgr/2004/index.htm. [Google Scholar]
- 18.Goldenberg I, Jonas M, Tenenbaum A, Boyko V, Matetzky S, Shotan A, Behar S, Reicher-Reiss H Bezafibrate Infarction Prevention Study Group. Current smoking, smoking cessation, and the risk of sudden cardiac death in patients with coronary artery disease. Arch Intern Med. 2003;163:2301–2305. doi: 10.1001/archinte.163.19.2301. [DOI] [PubMed] [Google Scholar]
- 19.Anthonisen NR, Skeans MA, Wise RA, Manfreda J, Kanner RE, Connett JE Lung Health Study Research Group. The effects of a smoking cessation intervention on 14.5-year mortality: a randomized clinical trial. Ann Intern Med. 2005;142:233–239. doi: 10.7326/0003-4819-142-4-200502150-00005. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) State-specific prevalence of smoke-free home rules: United States, 1992–2003. MMWR Morb Mortal Wkly Rep. 2007;56:501–504. [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention (CDC) State-specific secondhand smoke exposure and current cigarette smoking among adults: United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:1232–1235. [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC) Vital signs: non-smokers’ exposure to secondhand smoke: United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2010;59:1141–1146. [PubMed] [Google Scholar]
- 23.US Department of Health and Human Services. Atlanta, Ga: US Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. [Google Scholar]
- 24.John U, Meyer C, Hanke M, Völzke H, Schumann A. Relation between awareness of circulatory disorders and smoking in a general population health examination. BMC Public Health. 2006;6:48. doi: 10.1186/1471-2458-6-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.US Department of Health and Human Services. Atlanta, Ga: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; [Accessed June 8, 2010]. Fact sheet: health effects of cigarette smoking. updated December 2009. Available at: http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/. [Google Scholar]
- 26.Agency for Healthcare Research and Quality. Rockville, Md: US Department of Health and Human Services, Agency for Healthcare Research and Quality; 2010. 2009 National Healthcare Quality & Disparities Reports. [Google Scholar]
13. Risk Factor: High Blood Cholesterol and Other Lipids
See Table 13-1 and Charts 13-1 through 13-3.
Table 13-1.
High Total and LDL Cholesterol and Low HDL Cholesterol
| Population Group | Prevalence of Total Cholesterol ≥200 mg/dL, 2008 Age ≥20 y |
Prevalence of Total Cholesterol ≥240 mg/dL, 2008 Age ≥20 y |
Prevalence of LDL Cholesterol ≥130 mg/dL, 2008 Age ≥20 y |
Prevalence of HDL Cholesterol <40 mg/dL, 2008 Age ≥20 y |
|---|---|---|---|---|
| Both sexes* | 98 800 000 (44.4%) | 33 600 000 (15.0%) | 71 300 000 (31.9%) | 41 800 000 (18.9%) |
| Men* | 45 000 000 (41.8%) | 14 600 000 (13.5%) | 35 300 000 (32.5%) | 30 800 000 (28.6%) |
| Women* | 53 800 000 (46.3%) | 19 000 000 (16.2%) | 36 000 000 (31.0%) | 11 000 000 (9.7%) |
| NH white men, % | 41.2 | 13.7 | 30.5 | 29.5 |
| NH white women, % | 47.0 | 16.9 | 32.0 | 10.1 |
| NH black men, % | 37.0 | 9.7 | 34.4 | 16.6 |
| NH black women, % | 41.2 | 13.3 | 27.7 | 6.6 |
| Mexican-American men, % | 50.1 | 16.9 | 41.9 | 31.7 |
| Mexican-American women, % | 46.5 | 14.0 | 31.6 | 12.2 |
LDL indicates low-density lipoprotein; HDL, high-density lipoprotein; and NH, non-Hispanic.
Prevalence of total cholesterol ≥200 mg/dL includes people with total cholesterol ≥240 mg/dL. In adults, levels of 200 to 239 mg/dL are considered borderline high. Levels of ≥240 mg/dL are considered high.
Total data for total cholesterol are for Americans ≥20 years of age. Data for LDL cholesterol, HDL cholesterol, and all racial/ethnic groups are age adjusted for age ≥20 years.
Source for total cholesterol ≥200 mg/dL, ≥240 mg/dL, LDL, and HDL: National Health and Nutrition Examination Survey (2005–2008), National Center for Health Statistics, and National Heart, Lung, and Blood Institute. Estimates from National Health and Nutrition Examination Survey 2005–2008 (National Center for Health Statistics) applied to 2008 population estimates.
Chart 13-1.
Trends in mean total serum cholesterol among adolescents 12 to 17 years of age by race, sex, and survey year (National Health and Nutrition Examination Survey: 1988–1994,* 1999–2004, and 2005–2008). Values are in mg/dL. NH indicates non-Hispanic; Mex. Am., Mexican American. *Data for Mexican Americans not available. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 13-3.
Age-adjusted trends in the prevalence of total serum cholesterol ≥200 mg/dL in adults ≥20 years of age by sex, race/ethnicity, and survey year (National Health and Nutrition Examination Survey 2003–2004, 2005–2006, and 2007–2008). NH indicates non-Hispanic; Mex. Am., Mexican American.
Prevalence
For information on dietary cholesterol, total fat, saturated fat, and other factors that affect blood cholesterol levels, see Chapter 19 (Nutrition).
Youth
- Among children 4 to 11 years of age, the mean total blood cholesterol level is 164.5 mg/dL. For boys, it is 163.8 mg/dL; for girls, it is 165.2 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2005–2008, NCHS and NHLBI; unpublished analysis):
-
—For non-Hispanic whites, 163.9 mg/dL for boys and 165.6 mg/dL for girls
-
—For non-Hispanic blacks, 165.7 mg/dL for boys and 162.3 mg/dL for girls
-
—For Mexican Americans, 160.7 mg/dL for boys and 161.5 mg/dL for girls
-
—
- Among adolescents 12 to 19 years of age, the mean total blood cholesterol level is 159.2 mg/dL. For boys, it is 156.3 mg/dL; for girls, it is 162.3 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2005–2008, NCHS and NHLBI; unpublished analysis):
-
—For non-Hispanic whites, 155.9 mg/dL for boys and 162.3 mg/dL for girls
-
—For non-Hispanic blacks, 157.7 mg/dL for boys and 163.6 mg/dL for girls
-
—For Mexican Americans, 156.9 mg/dL for boys and 161.3 mg/dL for girls
-
—
The prevalence of abnormal lipid levels among youths 12 to 19 years of age is 20.3%; 14.2% of normal-weight youths, 22.3% of overweight youths, and 42.9% of obese youths have at least 1 abnormal lipid level (NHANES 1999–2006, NCHS).1
Approximately 8.5% of adolescents 12 to 19 years of age have total cholesterol levels ≥200 mg/dL (NHANES 2005–2008, NCHS and NHLBI; unpublished analysis).
Fewer than 1% of adolescents are eligible for pharmacological treatment.1,2
Adults
An estimated 33 500 000 adults ≥20 years of age have total serum cholesterol levels ≥240 mg/dL (extrapolated to 2008 by use of NCHS/NHANES 2005–2008 data), with a prevalence of 16.2% (Table 13-1; NCHS and NHLBI, unpublished analysis).
Data from NHANES 1999–2006 showed that ≈8% of adults ≥20 years of age have undiagnosed hypercholesterolemia.3
Data from the BRFSS study of the CDC in 2009 showed that the percentage of adults who had been screened for high blood cholesterol in the preceding 5 years ranged from 67.5% in Utah to 85.3% in the District of Columbia. The median percentage among all 50 states was 77.0%.4
The percentage of adults who reported having had a cholesterol check increased from 68.6% during 1999–2000 to 74.8% during 2005–2006.5
A10% (population-wide) decrease in total cholesterol levels may result in an estimated 30% reduction in the incidence of CHD.6
Data from NHANES 1999–2002 (NCHS) showed that overall, 63.3% of participants whose test results indicated high blood cholesterol or who were taking a cholesterol-lowering medication had been told by a professional that they had high cholesterol. Women were less likely than men to be aware of their condition; blacks and Mexican Americans were less likely to be aware of their condition than were whites. Fewer than half of Mexican Americans with high cholesterol were aware of their condition.7
Between the periods 1988–1994 and 1999–2002 (NHANES/NCHS), the age-adjusted mean total serum cholesterol level of adults ≥20 years of age decreased from 206 to 203 mg/dL, and LDL cholesterol levels decreased from 129 to 123 mg/dL.8
Data from NHANES 2003–2006 (NCHS) showed the serum total crude mean cholesterol level in adults ≥20 years of age was 198 mg/dL for men and 202 mg/dL for women.9
Data from the Minnesota Heart Survey (1980–1982 to 2000– 2002) showed a decline in age-adjusted mean total cholesterol concentrations from 5.49 and 5.38 mmol/L for men and women, respectively, in 1980–1982 to 5.16 and 5.09 mmol/L, respectively, in 2000–2002; however, the decline was not uniform across all age groups. Middle-aged to older people have shown substantial decreases, but younger people have shown little overall change and recently had increased total cholesterol values. Lipid-lowering drug use rose significantly for both sexes among those 35 to 74 years of age. Awareness, treatment, and control of hypercholesterolemia have increased; however, more than half of those at borderline-high risk remain unaware of their condition.10
Data from the BRFSS (CDC) survey in 2009 showed that among adults screened for high blood cholesterol, the percentage who had been told that they had high blood cholesterol ranged from 32.9% in Tennessee to 41.8% in South Carolina. The median percentage among states was 37.5%.4
Among adults with hypercholesterolemia, the percentage who had been told that they had high cholesterol increased from 42.0% during 1999–2000 to 50.4% during 2005–2006.5
According to data from NHANES 2005–2006, between the periods 1999–2000 and 2005–2006, mean serum total cholesterol levels in adults ≥20 years of age declined from 204 to 199 mg/dL. This decline was observed for men ≥40 years of age and for women ≥60 years of age. There was little change over this time period for other sex/age groups. In 2005–2006, ≈65% of men and 70% of women had been screened for high cholesterol in the past 5 years, and 16% of adults had serum total cholesterol levels of 240 mg/dL or higher.11
Self-reported use of cholesterol-lowering medications increased from 8.2% during 1999–2000 to 14.0% during 2005–2006.5
According to data from NHANES, from 1999 to 2006, the prevalence of elevated LDL cholesterol levels in adults >20 years of age has decreased by ≈33%.12
Adherence
Youth
Analysis of data from NHANES 1999–2006 showed that the overall prevalence of abnormal lipid levels among youths 12 to 19 years of age was 20.3%.1
Adults
- On the basis of data from the Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults13:
-
—Fewer than half of all people who qualify for any kind of lipid-modifying treatment for CHD risk reduction are receiving it.
-
—Fewer than half of even the highest-risk people (those with symptomatic CHD) are receiving lipid-lowering treatment.
-
—Only about one third of treated patients are achieving their LDL goal; <20% of patients with CHD are at their LDL goal.
-
—
Data from NHANES 2005–2006 indicate that among those with elevated LDL cholesterol levels, 35.5% had not been screened previously, 24.9% were screened but not told they had elevated cholesterol, and 39.6% were treated inadequately.12
Lipid Levels
LDL (Bad) Cholesterol
Youth
- Among adolescents 12 to 19 years of age, the mean LDL cholesterol level is 88.5 mg/dL. For boys, it is 87.1 mg/dL, and for girls, it is 89.9 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2005–2008, NCHS and NHLBI; unpublished analysis):
-
—Among non-Hispanic whites, 87.6 mg/dL for boys and 89.8 mg/dL for girls
-
—Among non-Hispanic blacks, 88.8 mg/dL for boys and 92.6 mg/dL for girls
-
—Among Mexican Americans, 88.4 mg/dL for boys and 88.8 mg/dL for girls
-
—
High levels of LDL cholesterol occurred in 8.4% of male adolescents and 6.8% of female adolescents during 1999–2006.1
Adults
The mean level of LDL cholesterol for American adults ≥20 years of age was 115.2 mg/dL in 2008.12 Levels of 130 to 159 mg/dL are considered borderline high, levels of 160 to 189 mg/dL are classified as high, and levels of ≥190 mg/dL are considered very high.
- According to NHANES 2005–2008 (NCHS and NHLBI; unpublished data):
-
—Among non-Hispanic whites, mean LDL cholesterol levels were 114.5 mg/dL for men and 115.8 mg/dL for women.
-
—Among non-Hispanic blacks, mean LDL cholesterol levels were 114.6 mg/dL for men and 111.5 mg/dL for women.
-
—Among Mexican Americans, mean LDL cholesterol levels were 121.2 mg/dL for men and 113.6 mg/dL for women.
-
—
The age-adjusted prevalence of high LDL cholesterol in US adults was 26.6% in 1988–1994 and 25.3% in 1999–2004 (NHANES/NCHS). Between 1988–1994 and 1999–2004, awareness increased from 39.2% to 63.0%, and use of pharmacological lipid-lowering treatment increased from 11.7% to 40.8%. LDL cholesterol control increased from 4.0% to 25.1% among those with high LDL cholesterol. In 1999–2004, rates of LDL cholesterol control were lower among adults 20 to 49 years of age than among those ≥65 years of age (13.9% versus 30.3%, respectively), among non-Hispanic blacks and Mexican Americans than among non-Hispanic whites (17.2% and 16.5% versus 26.9%, respectively), and among men than among women (22.6% versus 26.9%, respectively).14
Mean levels of LDL cholesterol decreased from 126.1 mg/dL during 1999–2000 to 114.8 mg/dL during 2005–2006. The prevalence of high LDL cholesterol decreased from 31.5% during 1999–2000 to 21.2% during 2005–2006.12
HDL (Good) Cholesterol
Youth
- Among children 4 to 11 years of age, the mean HDL cholesterol level is 54.7 mg/dL. For boys, it is 55.6 mg/dL, and for girls, it is 53.6 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2005–2008, NCHS and NHLBI; unpublished analysis):
-
—Among non-Hispanic whites, 54.7 mg/dL for boys and 52.8 mg/dL for girls
-
—Among non-Hispanic blacks, 61.4 mg/dL for boys and 58.1 mg/dL for girls
-
—Among Mexican Americans, 53.6 mg/dL for boys and 51.1 mg/dL for girls
-
—
- Among adolescents 12 to 19 years of age, the mean HDL cholesterol level is 51.6 mg/dL. For boys, it is 49.3 mg/dL, and for girls, it is 54.0 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2005–2008, NCHS and NHLBI; unpublished analysis):
-
—Among non-Hispanic whites, 48.1 mg/dL for boys and 53.3 mg/dL for girls
-
—Among non-Hispanic blacks, 54.6 mg/dL for boys and 56.9 mg/dL for girls
-
—Among Mexican Americans, 48.3 mg/dL for boys and 53.5 mg/dL for girls
-
—
Low levels of HDL cholesterol occurred in 11% of male adolescents and 4% of female adolescents during 1999–2006.1
Adults
An HDL cholesterol level below 40 mg/dL in adults is considered low and is a risk factor for HD and stroke. The mean level of HDL cholesterol for American adults ≥20 years of age is 53.3 mg/dL (NHANES 2005–2008, NCHS and NHLBI; unpublished analysis).
- According to NHANES 2005–2008 (NCHS and NHLBI; unpublished analysis):
-
—Among non-Hispanic whites, mean HDL cholesterol levels were 47.2 mg/dL for men and 58.8 mg/dL for women.
-
—Among non-Hispanic blacks, mean HDL cholesterol levels were 52.3 mg/dL for men and 61.3 mg/dL for women.
-
—Among Mexican Americans, mean HDL cholesterol levels were 46.0 mg/dL for men and 54.2 mg/dL for women.
-
—
Triglycerides
Youth
- Among adolescents 12 to 19 years of age, the mean triglyceride level is 87.8 mg/dL. For boys, it is 87.2 mg/dL, and for girls, it is 88.5 mg/dL. The racial/ethnic breakdown is as follows (NHANES 2005–2008, NCHS and NHLBI; unpublished analysis):
-
—Among non-Hispanic whites, 92.7 mg/dL for boys and 90.9 mg/dL for girls
-
—Among non-Hispanic blacks, 68.8 mg/dL for boys and 63.0 mg/dL for girls
-
—Among Mexican Americans, 94.5 mg/dL for boys and 90.2 mg/dL for girls
-
—
High levels of triglycerides occurred in 11.4% of male adolescents and 8.8% of female adolescents during 1999–2006.1
Adults
- A triglyceride level >150 mg/dL in adults is considered elevated and is a risk factor for HD and stroke. The mean level of triglycerides for American adults ≥20 years of age is 137.6 mg/dL (NHANES 2005–2008, NCHS and NHLBI; unpublished analysis).
-
—Among men, the mean triglyceride level is 149.9 mg/dL (NHANES 2005–2008, NCHS and NHLBI; unpublished analysis). The racial/ethnic breakdown is as follows:
-
◦150.2 mg/dL for white men
-
◦120.1 mg/dL for black men
-
◦169.4 mg/dL for Mexican American men
-
◦
-
—Among women, the mean triglyceride level is 125.5 mg/dL, with the following racial/ethnic breakdown:
-
◦128.8 mg/dL for white women
-
◦97.0 mg/dL for black women
-
◦139.0 mg/dL for Mexican American women
-
◦
-
—
Approximately 33% of adults ≥20 years of age had a triglyceride level ≥150 mg/dL during 1999–2004.15
Fewer than 3% of adults with a triglyceride level ≥150 mg/dL received pharmacological treatment during 1999 –2004.15
Abbreviations Used in Chapter 13
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CHD
coronary heart disease
- HD
heart disease
- HDL
high-density lipoprotein
- LDL
low-density lipoprotein
- mg/dL
milligrams per deciliter
- mmol/L
millimoles per liter
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- NHLBI
National Heart, Lung, and Blood Institute
References
- 1.Centers for Disease Control and Prevention (CDC); Prevalence of abnormal lipid levels among youths: United States, 1999–2006. MMWR Morb Mortal Wkly Rep. 2010;59:29–33. [published correction appears in MMWR Morb Mortal Wkly Rep. 2010;59:78]. [PubMed] [Google Scholar]
- 2.Ford ES, Li C, Zhao G, Mokdad AH. Concentrations of low-density lipoprotein cholesterol and total cholesterol among children and adolescents in the United States. Circulation. 2009;119:1108–1115. doi: 10.1161/CIRCULATIONAHA.108.816769. [DOI] [PubMed] [Google Scholar]
- 3.Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD. Hypertension, high serum total cholesterol, and diabetes: racial and ethnic prevalence differences in U.S. adults, 1999–2006. NCHS Data Brief. 2010;36:1–8. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Web site. Behavioral Risk Factor Surveillance System: prevalence and trends data. [Accessed September 15, 2010]; Available at: http://apps.nccd.cdc.gov/brfss/index.asp.
- 5.Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. 2010;140:226–235. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) State-specific cholesterol screening trends: United States, 1991–1999. MMWR Morb Mortal Wkly Rep. 2000;49:750–755. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC) Disparities in screening for and awareness of high blood cholesterol: United States, 1999–2002. MMWR Morb Mortal Wkly Rep. 2005;54:117–119. [PubMed] [Google Scholar]
- 8.Carroll MD, Lacher DA, Sorlie PD, Cleeman JI, Gordon DJ, Wolz M, Grundy SM, Johnson CL. Trends in serum lipids and lipoproteins of adults, 1960–2002. JAMA. 2005;294:1773–1781. doi: 10.1001/jama.294.14.1773. [DOI] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics. Health, United States, 2009: With Special Feature on Medical Technology. Hyattsville, Md: National Center for Health Statistics; 2010. [Accessed September 15, 2010]. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. [PubMed] [Google Scholar]
- 10.Arnett DK, Jacobs DR, Jr, Luepker RV, Blackburn H, Armstrong C, Claas SA. Twenty-year trends in serum cholesterol, hypercholesterolemia, and cholesterol medication use: the Minnesota Heart Survey, 1980–1982 to 2000–2002. Circulation. 2005;112:3884–3891. doi: 10.1161/CIRCULATIONAHA.105.549857. [DOI] [PubMed] [Google Scholar]
- 11.Schober SE, Carroll MD, Lacher DA, Hirsch R. High Serum Total Cholesterol: An Indicator for Monitoring Cholesterol Lowering Efforts: U.S. Adults, 2005–2006. Hyattsville, Md: National Center for Health Statistics; 2007. Division of Health and Nutrition Examination Surveys. NCHS Data Brief No. 2. [PubMed] [Google Scholar]
- 12.Kuklina EV, Yoon PW, Keenan NL. Trends in high levels of low-density lipoprotein cholesterol in the United States, 1999–2006. JAMA. 2009;302:2104–2110. doi: 10.1001/jama.2009.1672. [DOI] [PubMed] [Google Scholar]
- 13.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 14.Hyre AD, Muntner P, Menke A, Raggi P, He J. Trends in ATP-III-defined high blood cholesterol prevalence, awareness, treatment and control among U.S. adults. Ann Epidemiol. 2007;17:548–555. doi: 10.1016/j.annepidem.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 15.Ford ES, Li C, Zhao G, Pearson WS, Mokdad AH. Hypertriglyceridemia and its pharmacologic treatment among US adults. Arch Intern Med. 2009;169:572–578. doi: 10.1001/archinternmed.2008.599. [DOI] [PubMed] [Google Scholar]
14. Risk Factor: Physical Inactivity
See Table 14-1 and Charts 14-1 through 14-4.
Table 14-1.
Regular Leisure-Time Physical Activity
| Population Group | Prevalence, 2008 (Age ≥18 y), % |
|---|---|
| Both sexes | 34.9 |
| Men | 37.4 |
| Women | 32.7 |
| NH white only | 38.1 |
| NH black only | 29.3 |
| Hispanic or Latino | 27.8 |
| American Indian/Alaska Native only | 34.0 |
| Asian only | 28.3 |
NH indicates non-Hispanic.
Regular leisure-time physical activity is defined as light to moderate activity for ≥30 minutes, 5 times per week, or vigorous activity for ≥20 minutes, ≥3 times per week.
Data are age adjusted for adults ≥18 years of age.
Source: National Health Interview Survey 2009 (National Center for Health Statistics).7
Chart 14-1.
Prevalence of students in grades 9–12 who met currently recommended levels of physical activity during the past 7 days by race/ethnicity and sex (Youth Risk Behavior Surveillance: 2009). “Currently recommended levels” was defined as activity that increased their heart rate and made them breathe hard some of the time for a total of at least 60 minutes per day on 5 of the 7 days preceding the survey. NH indicates non-Hispanic. Data derived from MMWR Surveillance Summaries.1
Chart 14-4.
Prevalence of children 6 to 19 years of age who attained sufficient moderate to vigorous physical activity to meet public health recommendations (≥60 minutes per day on ≥5 of the 7 days preceding the survey), by sex and age (National Health and Nutrition Examination Survey: 2003–2004). Data derived from Troiano et al.3
Prevalence
Youth
Inactivity
The proportion of adolescents (12 to 19 years old) who report engaging in no regular PA is high and varies by sex and race.1
Nationwide, 23.1% of adolescents were inactive during the previous 7 days, indicated by their response that they did not participate in ≥60 minutes of any kind of PA that increased their heart rate and made them breathe hard on any 1 of the previous 7 days.1
Girls were more likely than boys to report inactivity (29.9% versus 17.0%).1
The prevalence of inactivity was highest in black (43.6%) and Hispanic (30.5%) girls, followed by white girls (25.4%), black boys (20.6%), Hispanic boys (17.4%), and white boys (15.9%; CDC).1
Nationwide, 24.9% of adolescents used a computer for activities other than school work (eg, videogames or other computer games) for ≥3 hours per day on an average school day.1
A greater proportion of black and Hispanic students used computers or watched television >3 hours per day than white students.2
Activity Recommendations
The proportion of students who met activity recommendations declined from 9th (39.7%) to 12th (31.6%) grades, and at each grade level, the proportion was higher in boys than in girls.1
More adolescent boys (45.6%) than girls (27.7%) self-reported having been physically active at least 60 minutes per day on 5 or more days; self-reported rates of activity were higher in white (39.9%) than in black (32.6%) or Hispanic (33.1%) adolescents.1
There was a marked discrepancy between the proportion of youth (ages 6 to 11 years) who reported engaging in ≥60 minutes of moderate-to-vigorous physical activity (MVPA) on most days of the week and those who actually engaged in MVPA for ≥60 minutes when activity was measured objectively with accelerometers (ie, portable motion censors that record and quantify the duration and intensity of movements) in the NHANES 2003–2004 survey.3
On the basis of accelerometer counts per minute >2020, 42% of 6- to 11-year-olds accumulated ≥60 minutes of MVPA on 5 of 7 days per week, whereas only 8% of 12- to 15-year-olds and 7.6% of 16- to 19-year-olds achieved similar counts.3
More boys than girls met PA recommendations (≥60 minutes of moderate to vigorous activity on most days of the week) as measured by accelerometry.3
Fewer than 50% of adolescents (14 to 17 years of age) met PA guideline recommendations; 57% of boys met recommendations versus 40% of girls.4
Structured Activity Participation
Despite recommendations from the National Association for Sport and Physical Education that schools should require daily physical education for students in kindergarten through 12th grade, only 33.3% of students attended physical education classes in school daily (34.6% of boys and 31.9% of girls).1,5
Physical education class participation declined from the 9th through the 12th grades among boys and girls.2
Among children 9 to 13 years old, 61.5% do not participate in any organized PA during nonschool hours and 22.6% do not engage in any free-time PA, according to 2002 data from the Youth Media Campaign Longitudinal Study of the CDC.6
Little more than half (58.3%) of all students played on at least 1 school or community sports team in the previous year; however, the prevalence declined with increasing grade level, from 61.6% in the 9th grade to 51.1% in the 12th grade.1
Adults
Inactivity
Thirty-three percent of adults (>18 years of age) do not engage in leisure-time PA according to 2009 data from the NHIS (“no leisure-time physical activity/inactivity” refers to no sessions of light/moderate or vigorous PA of at least 10 minutes’ duration).7
Inactivity in 2009 was higher among women than men (34.5% versus 30.3%, age adjusted) and increased with age from 27.7% to 33.3%, 38.2%, and 55.3% among adults 18 to 44, 45 to 64, 65 to 74, and ≥75 years of age, respectively.7
Non-Hispanic black and Hispanic adults were more likely to report inactivity (0.8.7% and 44.0%, respectively) than were non-Hispanic white adults (28.4%), based on age-adjusted estimates from the 2009 NHIS.7
Fifty-six percent of adults who responded to the 2009 NHIS survey reported engaging in no vigorous activity (activity that causes heavy sweating and a large increase in breathing or heart rate).7
Women (60.1%) were more likely than men (50.3%) to report never engaging in vigorous PA, based on age-adjusted estimates from the 2009 NHIS.7
The proportion of respondents who did not participate in any vigorous activity increased with age from 45.7% in 18- to 44-year-olds to 86.8% in adults ≥75 years of age in the 2009 NHIS.7
American Indians/Alaska Natives (61.7%), blacks (61.6%), and Asians (61.4%) were more likely to report not engaging in any vigorous activity than whites (54.1%), and Hispanic/Latino adults were more likely not to engage in any vigorous activity (66.9%) than non-Hispanic/non-Latino adults (53.3%) according to age-adjusted estimates from the 2009 NHIS.7
The probability of not engaging in any vigorous activity was inversely associated with education; participants with no high school diploma (77.6%), a high school diploma (66.2%), some college (54.0%), or bachelor’s degree or higher (39.3%), respectively, reported that they did not engage in any vigorous PA, based on the 2009 NHIS.7
Activity Recommendations
The proportion of adults reporting levels of PA consistent with the Healthy People 2010 objectives remains low and decreases with age.8
Thirty-three percent of respondents in a study examining awareness of current US PA guidelines had direct knowledge of the recommended dosage of PA (ie, frequency/duration).9
The age-adjusted proportion of adults 18 years and older who reported engaging in regular moderate or vigorous PA as defined by the Healthy People 2010 objective 22-2 was 32%, based on the 2008 NHIS (CDC, Data2010; available at http://wonder.cdc.gov/data2010/).
The percentage of adults reporting regular moderate or vigorous PA decreased with age from 38% for adults 18 to 24 years of age to 18% for those ≥75 years, based on the 2008 NHIS (CDC, Data2010; available at http://wonder.cdc.gov/data2010/).
- In 2008, 27% of adults participated in leisure-time strengthening activities, an important component of overall physical fitness.
-
—The percentage of men who engaged in leisure-time strengthening activities decreased with age, from 47% at age 18 to 24 years to 16% at age ≥75 years. The percentage of women who engaged in leisure-time strengthening activities also decreased with age, from 28% at age 18 to 24 years to 11% at age ≥75 years.10
-
—
The proportion of adults reporting regular leisure-time activity (30 minutes of light or moderate activity ≥5 times per week or 20 minutes of vigorous activity ≥3 times per week) in the 2009 NHIS was positively associated with education level: 46.0% of people with a college degree or higher were regularly active compared with 21.4% of adults with less than a high school diploma.7
- Adherence to PA recommendations was much lower when based on PA measured by accelerometer in NHANES 2003–20043:
-
—Among adults 20 to 59 years of age, 3.8% of men and 3.2% of women met recommendations to engage in MVPA (accelerometer counts >2020/min) for 30 minutes (in sessions of ≥10 minutes) on ≥5 of 7 days.
-
—Among people ≥60 years of age, adherence was 2.5% in men and 2.3% in women.
-
—
- In a review examining self-reported versus actual measured PA (eg, accelerometers, pedometers, indirect calorimetry, double-labeled water, heart rate monitor), 60% of respondents self-reported higher values of activity than what was measured by use of direct methods.
-
—Among men, self-reported PA was 44% greater than actual measured values; among women, self-reported activity was 138% greater than actual measured PA.11
-
—
Trends
Youth
- A study of 3068 youths between the ages of 14 and 24 years from 1999 to 2006 found that the prevalence of inactivity went up with age in both boys and girls.
Adults
Between NHANES III (1988 –1994) and NHANES 2001–2006, the proportion of adults who engaged in >12 bouts of PA per month declined from 57% to 43% in men and from 49% to 43% in women.
In non-Hispanic whites, the activity level has decreased from 55.3% to 45.2%; for non-Hispanic blacks, it has decreased from 41.2% to 34.6%; and for Hispanics, the decline has been from 40.9% to 36.2%.14
CHD Risk Factors
Youth
More girls (67.9%) than boys (55.7%) reported having exercised to lose weight or to keep from gaining weight.
White girls (72.2%) were more likely than black (54.2%) and Hispanic (66.3%) girls to report exercising to lose weight or to keep from gaining weight.1
Total and vigorous PA are inversely correlated with body fat and the prevalence of obesity.15
Physical inactivity was positively correlated with CHD risk factors (eg, mean arterial pressure, triglycerides, LDL, HDL, and fasting plasma glucose) in youths. Findings were similar for boys and girls.16
Adults
Participants in the Diabetes Prevention Project randomized trial who met the PA goal of 150 minutes of PA per week were 44% less likely to develop DM, even if they did not meet the weight-loss target.17
As a weight-loss intervention, exercise alone was associated with significant reductions in DBP (−2 mm Hg, 95% CI −4 to −1 mm Hg), triglycerides (−0.2 mmol/L, 95% CI −0.3 to −0.1 mmol/L), and fasting glucose (−0.2 mmol/L, 95% CI −0.3 to −0.1 mmol/L).18
A total of 120 to 150 minutes per week of moderate-intensity activity can reduce the risk of developing metabolic syndrome and its individual components (ie, abdominal adiposity, high BP, low HDL cholesterol, high triglycerides, or high glucose).19
CHD Events and Mortality
- The PA guidelines for adults cite evidence that ≈150 minutes a week of moderate-intensity aerobic activity can reduce the risk of CVD.20
-
—The RR of CHD associated with physical inactivity ranges from 1.5 to 2.4.21
-
—Physical inactivity is responsible for 12.2% of the global burden of MI after accounting for other CVD risk factors such as cigarette smoking, DM, hypertension, abdominal obesity, lipid profile, no alcohol intake, and psychosocial factors.22
-
—A 2.3% decline in physical inactivity between 1980 and 2000 prevented or postponed ≈17 445 deaths (≈5%) due to CHD in the United States.23
-
—The Nurse’s Health Study of >72 000 female nurses indicated that moderate-intensity PA, such as walking, is associated with a substantial reduction in risk of total and ischemic stroke.24
-
—
- Longitudinal studies commonly report a graded, inverse association of PA amount and duration (ie, dose) with incident CHD and stroke.25
-
—In the Health Professionals Follow-Up Study, PA “dose” was inversely associated with the incidence of CHD over time, with rates declining from 46.3, 39.3, 35.9, 32.2, and 25.8 cases per 10 000 person years according to quintiles of activity. The adjusted HR comparing the uppermost quintile of activity with the lowest was 0.72 (95% CI 0.61 to 0.85).26
-
—Metabolic equivalent tasks (MET) levels >6 were associated with a statistically significantly lower RR (RR 0.83, 95% CI 0.74 to 0.97 versus MET intensity of 1 to 3.9) of developing incident CHD in the Health Professionals Follow-Up Study of men.26
-
—In a meta-analysis of longitudinal studies among women, RRs of incident CHD were 0.83 (95% CI 0.69 to 0.99), 0.77 (95% CI 0.64 to 0.92), 0.72 (95% CI 0.59 to 0.87), and 0.57 (95% CI 0.41 to 0.79) across increasing quintiles of PA compared with the lowest quintile.27
-
—A 2003 meta-analysis of 23 studies on the association of PA with stroke indicated that compared with low levels of activity, high (RR 0.79, 95% CI 0.69 to 0.91) and moderate (RR 0.91, 95% CI 0.80 to 1.05) levels of activity were inversely associated with the likelihood of developing total stroke (ischemic and hemorrhagic).28
-
—
Secondary Prevention
PA improves inflammatory markers in people with existing stable CHD. After a 6-week training session, C-reactive protein levels declined by 23.7% (P<0.001), and plasma vascular cell adhesion molecule-1 levels declined by 10.23% (P<0.05); there was no difference in leukocyte count or levels of intercellular adhesion molecule-1.29
In a randomized trial of patients with PAD, supervised treadmill exercise training and lower-extremity resistance training were each associated with significant improvements in functional performance and quality of life compared with a usual-care control group. Exercise training was additionally associated with improved brachial artery flow-mediated dilation, whereas resistance training was associated with better stair-climbing ability versus control.30
The benefit of intense exercise training for cardiac rehabilitation in people with HF was tested in a trial of 27 patients with stable, medically treated HF. Intense activity (an aerobic interval-training program 3 times per week for 12 weeks) was associated with a significant 35% improvement in left ventricular EF and decreases in pro– brain natriuretic peptide (40%), left ventricular end-diastolic volume (18%), and left ventricular end-systolic volume (25%) compared with control and endurance-training groups.31
Costs
The economic consequences of physical inactivity are substantial. In a summary of WHO data sources, the economic costs of physical inactivity were estimated to account for 1.5% to 3.0% of total direct healthcare expenditures in developed countries such as the United States.32
The 1996 MEPS was linked to self-reported activity in the 1995 NHIS. On the basis of a self-reported prevalence of inactivity of 47.5% and a prevalence of CVD of 21.5%, the direct expenditures for CVD associated with inactivity were estimated to be $23.7 billion in 2001.33
Abbreviations Used in Chapter 14
- BP
blood pressure
- CDC
Centers for Disease Control and Prevention
- CHD
coronary heart disease
- CI
confidence interval
- CVD
cardiovascular disease
- DBP
diastolic blood pressure
- DM
diabetes mellitus
- EF
ejection fraction
- HDL
high-density lipoprotein
- HF
heart failure
- HR
hazard ratio
- LDL
low-density lipoprotein
- MEPS
Medical Expenditure Panel Survey
- MET
metabolic equivalent tasks
- MI
myocardial infarction
- MVPA
moderate-to-vigorous physical activity
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- NHIS
National Health Interview Survey
- PA
physical activity
- PAD
peripheral arterial disease
- RR
relative risk
- WHO
World Health Organization
References
- 1.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Lim C, Whittle L, Brener ND, Wechsler H. Centers for Disease Control and Prevention. Youth risk behavior surveillance: United States, 2009. MMWR Surveill Summ. 2010;59:1–142. [PubMed] [Google Scholar]
- 2.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Lim C, Brener ND, Wechsler H. Centers for Disease Control and Prevention (CDC). Youth risk behavior surveillance: United States, 2007. MMWR Surveill Summ. 2008;57:1–131. [PubMed] [Google Scholar]
- 3.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 4.Butcher K, Sallis JF, Mayer JA, Woodruff S. Correlates of physical activity guideline compliance for adolescents in 100 U.S. cities. J Adolesc Health. 2008;42:360–368. doi: 10.1016/j.jadohealth.2007.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Association for Sport and Physical Education. Moving Into the Future: National Standards for Physical Education. 2nd ed. Reston, Va: National Association for Sport and Physical Education; 2004. [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) Physical activity levels among children aged 9–13 years: United States, 2002. MMWR Morb Mortal Wkly Rep. 2003;52:785–788. [PubMed] [Google Scholar]
- 7.Pleis JR, Ward BW, Lucas JW. Vital and Health Statistics, Series 10, No. 249. Hyattsville, Md: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2010. [Accessed August 26, 2010]. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. DHHS publication No. (PHS) 2011-1577. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_249.pdf. [PubMed] [Google Scholar]
- 8.Pleis J, Lucas J. Summary Health Statistics for US Adults: National Health Interview Survey 2007. Hyattsville, Md: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2010. Vital and Health Statistics, Series 10, No. 249. DHHS publication No. 2009-1568. [Google Scholar]
- 9.Bennett GG, Wolin KY, Puleo EM, Mâsse LC, Atienza A. Awareness of national physical activity recommendations for health promotion among US adults. Med Sci Sports Exerc. 2009;41:1849–1855. doi: 10.1249/MSS.0b013e3181a52100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. QuickStats: percentage of adults aged ≥18 years who engaged in leisure-time strengthening activities, by age group and sex: National Health Interview Survey, United States, 2008. MMWR Weekly. 2009;58:955. [Google Scholar]
- 11.Prince SA, Adamo KB, Hamel ME, Hardt J, Gorber SC, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zimmermann-Sloutskis D, Wanner M, Zimmermann E, Martin BW. Physical activity levels and determinants of change in young adults: a longitudinal panel study. Int J Behav Nutr Phys Act. 2010;7:2. doi: 10.1186/1479-5868-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kahn JA, Huang B, Gillman MW, Field AE, Austin SB, Colditz GA, Frazier AL. Patterns and determinants of physical activity in U.S. adolescents. J Adoles Health. 2008;42:369–377. doi: 10.1016/j.jadohealth.2007.11.143. [DOI] [PubMed] [Google Scholar]
- 14.King DE, Mainous AG, III, Carnemolla M, Everett CJ. Adherence to healthy lifestyle habits in US adults, 1988–2006. Am J Med. 2009;122:528–534. doi: 10.1016/j.amjmed.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 15.Kim Y, Lee S. Physical activity and abdominal obesity in youth. Appl Physiol Nutr Metab. 2009;34:571–581. doi: 10.1139/H09-066. [DOI] [PubMed] [Google Scholar]
- 16.Katzmarzyk PT, Malina RM, Bouchard C. Physical activity, physical fitness, and coronary heart disease risk factors in youth: the Québec Family Study. Prev Med. 1999;29:555–562. doi: 10.1006/pmed.1999.0592. [DOI] [PubMed] [Google Scholar]
- 17.Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, Hoskin M, Kriska AM, Mayer-Davis EJ, Pi-Sunyer X, Regensteiner J, Venditti B, Wylie-Rosett J. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29:2102–2107. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaw KA, Gennat HC, O’Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev. 2006;(4):CD003817. doi: 10.1002/14651858.CD003817.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Department of Health and Human Services, Centers for Disease Control and Prevention. Physical activity for everyone: physical activity and health: the benefits of physical activity. [Accessed September 16, 2009]; Available at: http://www.cdc.gov/physicalactivity/everyone/health/index.html#ReduceCardiovascularDisease.
- 20.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 21.Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Heath GW, King AC, Kriska A, Leon AS, Marcus BH, Morris J, Paffenbarger RS, Jr, Patrick K, Pollock ML, Rippe JM, Sallis J, Wilmore JH. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 22.Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L. INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 23.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 24.Hu FB, Stampfer MJ, Colditz GA, Ascherio A, Rexrode KM, Willett WC, Manson JE. Physical activity and risk of stroke in women. JAMA. 2000;283:2961–2967. doi: 10.1001/jama.283.22.2961. [DOI] [PubMed] [Google Scholar]
- 25.Carnethon MR. Physical activity and cardiovascular disease: how much is enough? Am J Lifestyle Med. 2009;3(suppl):44S–49S. doi: 10.1177/1559827609332737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. JAMA. 2002;288:1994–2000. doi: 10.1001/jama.288.16.1994. [DOI] [PubMed] [Google Scholar]
- 27.Oguma Y, Shinoda-Tagawa T. Physical activity decreases cardiovascular disease risk in women: review and meta-analysis. Am J Prev Med. 2004;26:407–418. doi: 10.1016/j.amepre.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 28.Lee CD, Folsom AR, Blair SN. Physical activity and stroke risk: a meta-analysis. Stroke. 2003;34:2475–2481. doi: 10.1161/01.STR.0000091843.02517.9D. [DOI] [PubMed] [Google Scholar]
- 29.Ranković G, Milicić B, Savić T, Dindić B, Mancev Z, Pesić G. Effects of physical exercise on inflammatory parameters and risk for repeated acute coronary syndrome in patients with ischemic heart disease. Vojnosanit Pregl. 2009;66:44–48. doi: 10.2298/vsp0901044r. [DOI] [PubMed] [Google Scholar]
- 30.McDermott MM, Ades P, Guralnik JM, Dyer A, Ferrucci L, Liu K, Nelson M, Lloyd-Jones D, Van Horn L, Garside D, Kibbe M, Domanchuk K, Stein JH, Liao Y, Tao H, Green D, Pearce WH, Schneider JR, McPherson D, Laing ST, McCarthy WJ, Shroff A, Criqui MH. Treadmill exercise and resistance training in patients with peripheral arterial disease with and without intermittent claudication: a randomized controlled trial. JAMA. 2009;301:165–174. doi: 10.1001/jama.2008.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wisløff U, Støylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram PM, Tjønna AE, Helgerud J, Slørdahl SA, Lee SJ, Videm V, Bye A, Smith GL, Najjar SM, Ellingsen Ø, Skjaerpe T. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115:3086–3094. doi: 10.1161/CIRCULATIONAHA.106.675041. [DOI] [PubMed] [Google Scholar]
- 32.Oldridge NB. Economic burden of physical inactivity: healthcare costs associated with cardiovascular disease. Eur J Cardiovasc Prev Rehabil. 2008;15:130–139. doi: 10.1097/HJR.0b013e3282f19d42. [DOI] [PubMed] [Google Scholar]
- 33.Wang G, Pratt M, Macera CA, Zheng ZJ, Heath G. Physical activity, cardiovascular disease, and medical expenditures in U.S. adults. Ann Behav Med. 2004;28:88–94. doi: 10.1207/s15324796abm2802_3. [DOI] [PubMed] [Google Scholar]
15. Risk Factor: Overweight and Obesity
See Table 15-1 and Charts 15-1 through 15-3.
Table 15-1.
Overweight and Obesity
| Population Group | Prevalence of Overweight and Obesity in Adults, 2005–2008 Age ≥20 y |
Prevalence of Obesity in Adults, 2005–2008 Age ≥20 y |
Prevalence of Overweight and Obesity in Children, 2007–2008 Ages 2–19 y |
Prevalence of Obesity in Children, 2007–2008 Ages 2–19 y |
Cost, 2008* |
|---|---|---|---|---|---|
| Both sexes, n (%) | 149 300 000 (67.3) | 75 000 000 (33.7) | (31.7) | (16.9) | $147 billion |
| Males, n (%) | 78 000 000 (72.4) | 34 900 000 (32.4) | (32.1) | (17.8) | … |
| Females, n (%) | 71 300 000 (62.3) | 40 100 000 (35.2) | (31.3) | (15.9) | … |
| NH white males, % | 72.3 | 32.1 | 29.5 | 15.7 | … |
| NH white females, % | 59.3 | 32.8 | 29.2 | 14.9 | … |
| NH black males, % | 70.8 | 37.0 | 33.0 | 17.3 | … |
| NH black females, % | 77.7 | 51.0 | 39.0 | 22.7 | … |
| Mexican American males, % | 77.5 | 31.4 | 41.7 | 24.9 | … |
| Mexican American females, % | 75.1 | 43.4 | 36.1 | 16.5 | … |
NH indicates non-Hispanic.
Ellipses (…) indicate data not available.
Data for white and black males and females are for non-Hispanics. Overweight and obesity in adults is body mass index ≥25 kg/m2. Obesity in adults is ≥ body mass index 30 kg/m2. In children, overweight and obesity are based on body mass index -for-age values ≥85th percentile of the 2000 Centers for Disease Control and Prevention growth charts. In children, obesity is based on body mass index -for-age values ≥95th percentile of the Centers for Disease Control and Prevention growth charts.
In January 2007, the American Medical Association’s Expert Task Force on Childhood Obesity recommended new definitions for overweight and obesity in children and adolescents (available at http://www.ama-assn.org/ama1/pub/upload/mm/433/ped_obesity_recs.pdf). However, statistics based on this new definition are not yet available.
Data from Health Affairs.40
Sources: age-adjusted National Health and Nutrition Examination Survey 2005–2008 (National Center for Health Statistics), National Heart, Lung, and Blood Institute, and unpublished data. Estimates from National Health and Nutrition Examination Survey 2005–2008 (National Center for Health Statistics) were applied to 2008 population estimates. In children, age-adjusted National Health and Nutrition Examination Survey 2007–2008 data were applied to 2006 population estimates (JAMA. 2010;303:235–241; and JAMA. 2010;303:242–249).
Chart 15-1.
Prevalence of overweight and obesity among students in grades 9 through 12 by sex and race/ethnicity. NH indicates non-Hispanic. Data derived from Youth Risk Behavior Surveillance—United States, 2009, Table 90.43
Chart 15-3.
Trends in the prevalence of overweight among US children and adolescents by age and survey year (National Health and Nutrition Examination Survey: 1976–1980, 1988–1994, 1999–2002, and 2003–2006). Data derived from Health, United States, 2009 (National Center for Health Statistics).44
Prevalence
Youth
The prevalence of overweight and obesity in children 2 to 5 years of age, based on a BMI-for-age value ≥85th percentile of the 2000 CDC growth charts, was 16% for non-Hispanic white boys and 20% for non-Hispanic white girls, 28% for non-Hispanic black boys and 24% for non-Hispanic black girls, and 32% for Mexican American boys and 23% for Mexican American girls according to 2007 to 2008 data from NHANES (NCHS). In children 6 to 11 years of age, the prevalence was 35% for non-Hispanic white boys and 34% for non-Hispanic white girls, 36% for non-Hispanic black boys and 39% for non-Hispanic black girls, and 44% for Mexican American boys and 39% for Mexican American girls. In children 12 to 19 years of age, the prevalence was 33% for non-Hispanic white boys and 30% for non-Hispanic white girls, 33% for non-Hispanic black boys and 46% for non-Hispanic black girls, and 46% for Mexican American boys and 42% for Mexican American girls.1
The prevalence of obesity in children 2 to 5 years of age, based on BMI-for-age values ≥95th percentile of the 2000 CDC growth charts, was 7% for non-Hispanic white boys and 12% for non-Hispanic white girls, 11% for non-Hispanic black boys and 12% for non-Hispanic black girls, and 19% for Mexican American boys and 8% for Mexican American girls according to 2007 to 2008 data from NHANES (NCHS). In children 6 to 11 years of age, the prevalence was 21% for non-Hispanic white boys and 17% for non-Hispanic white girls, 18% for non-Hispanic black boys and 21% for non-Hispanic black girls, and 27% for Mexican American boys and 22% for Mexican American girls. In children 12 to 19 years of age, the prevalence was 17% for non-Hispanic white boys and 15% for non-Hispanic white girls, 20% for non-Hispanic black boys and 29% for non-Hispanic black girls, and 27% for Mexican American boys and 17% for Mexican American girls.1
Overall, 19% of US children and adolescents 6 to 19 years of age have BMI-for-age values ≥95th percentile of the 2000 CDC growth charts for the United States (NHANES [2007–2008], NCHS).1
NHANES 2003 to 2006 found that 11.3% of children and adolescents 2 to 19 years of age were at or above the 97th percentile of the 2000 BMI-for-age growth chart, 16.3% were ≥95th percentile, and 31.9% were ≥85th percentile.2
- Data from the NHANES in the 2008 National Healthcare Quality Report found that3:
-
—During 2003 to 2006, 39.4% of overweight (≥95th percentile of the 2000 BMI-for-age growth chart) children and teens 2 to 19 years of age were told by a doctor or health professional that they were overweight.
-
—During 2003 to 2006, overweight children 2 to 5 years of age (22.3%) and 6 to 11 years of age (35.70%) were less likely than overweight children 12 to 19 years of age (47.5%) to be told by a provider that they were overweight.
-
—
A study of >8500 4-year-olds in the Early Childhood Longitudinal Study, Birth Cohort (National Center for Education Statistics) found that 1 in 5 are obese. Almost 13% of Asian children, 16% of white children, nearly 21% of black children, 22% of Hispanic children, and 31% of American Indian children were obese. Children were considered obese if their BMI was ≥95th percentile, based on CDC BMI growth charts. For 4-year-olds, that would be a BMI of ≈18 kg/m2. Researchers did not examine reasons for the disparities.4
Overweight adolescents have a 70% chance of becoming overweight adults. This increases to 80% if 1 or both parents are overweight or obese.5
Childhood sociodemographic factors may contribute to sex disparities in obesity prevalence. A study of data from the National Longitudinal Study of Adolescent Health found that parental education consistently modified sex disparity in blacks. The sex gap was largest in those with low parental education (16.7% of men compared with 45.4% of women were obese) and smallest in those with high parental education (28.5% of men compared with 31.4% of women were obese). In whites, there was little overall sex difference in obesity prevalence.6
The obesity epidemic is disproportionally more rampant among children living in low-income, low-education, and higher-unemployment households according to data from the National Survey of Children’s Health.7
Adults
Overall, 68% of US adults were overweight or obese (72% of men and 64% of women).8
Among men, Mexican-Americans (80%) and non-Hispanic whites (73%) were more likely to be overweight or obese than non-Hispanic blacks (69%) according to NHANES 2007 to 2008.8
Among women, non-Hispanic blacks (78%) and Mexican-Americans (77%) were more likely to be overweight or obese than non-Hispanic whites (61%).8
Of US adults, 34% were obese (32% of men and 36% of women) according to NHANES 2007 to 2008.8
Among men, non-Hispanic blacks (37%) and Mexican-Americans (36%) were more likely to be obese than non-Hispanic whites (32%).8
Among women, non-Hispanic blacks (50%) and Mexican-Americans (45%) were more likely to be obese than non-Hispanic whites (33%).8
When estimates were based on self-reported height and weight in the BRFSS/CDC survey in 2008, the prevalence of obesity ranged from 19.1% in Colorado to 33.3% in Mississippi. The median percentage by state was 26.6%. Additionally, no state met the Healthy People 2010 goal of reducing obesity to 15% of adults.9
The county-level prevalence of obesity in the United States ranged from 12.4% to 43.7% with a median of 28.4% according to BRFSS/CDC 2007.10
In 1998 and 1999, surveys of people in 8 states and the District of Columbia by the BRFSS study of the CDC indicated that obesity rates were significantly higher among people with disabilities, especially blacks and those 45 to 64 years of age.11
Blacks ≥18 years of age (27.6%), American Indians or Alaska Natives (29.1%), and whites (35.9%) were less likely than Asians (53.4%) to be at a healthy weight based on self-reported height and weight data from the 2009 NHIS.12
Based on self-reported weights and heights, data showed that blacks ≥18 years of age (37.6%) and American Indians or Alaska Natives (34.4%) were more likely to be obese than were whites (26.6%) and Asians (9.0%) according to 2009 data from the NHIS.12
Most adults in Asian subgroups were in the healthy weight range, with rates ranging from 51% for Filipino adults to 68% for Chinese adults. Although the prevalence of obesity is low within the Asian adult population, Filipino adults (14%) were more than twice as likely to be obese (BMI ≥30 kg/m2) as Asian Indian (6%), Vietnamese (5%), or Chinese (4%) adults.13
From 1999 to 2004, obese adults 45 to 64 years of age (73%) and ≥65 years of age (73.6%) were more likely than those 20 to 44 years of age (59.5%) to be told by a doctor or health professional that they were overweight. Obese adults 45 to 64 years of age and ≥65 years of age were more likely to receive advice about exercise than those 18 to 44 years of age.3
Approximately 64.8% of obese adults were told by a doctor or health professional that they were overweight according to the 2008 National Healthcare Disparities Report (based on NHANES 2003 to 2006).14
The proportion of obese adults told that they were overweight was significantly lower for non-Hispanic blacks (60.5%) and Mexican Americans (57.1%) than for non-Hispanic whites (66.4%), for middle-income people than for high-income people (62.4% versus 70.6%), and for adults with less than a high school education than for those with any college education (59.2% versus 70.3%).14
A large proportion of white, black, and Hispanic participants were overweight (60% to 85%) or obese (30% to 50%), whereas fewer Chinese American participants were overweight (33%) or obese (5%), as judged by an analysis of data from MESA. These findings may be indicators of potential future increases in vascular disease burden and healthcare costs associated with the obesity epidemic.15
Trends
Youth
The prevalence of BMI-for-age values ≥95th percentile of the 2000 CDC growth charts in children 6 to 11 years of age was 20% in 2007 to 2008 compared with 4.0% in 1971 to 1974. The prevalence of BMI-for-age values ≥95th percentile in adolescents 12 to 19 years of age was 18% in 2007 to 2008 compared with 6% in 1971 to 1974 in NHANES. No statistically significant linear trends in high weight for recumbent length or high BMI were found over the time periods 1999 to 2000, 2001 to 2002, 2003 to 2004, 2005 to 2006, and 2007 to 2008 among girls and boys except among the very heaviest 6- through 19-year-old boys.1
Among infants and children between 6 and 23 months years of age, the prevalence of high weight for age was 7% in 1976 to 1980 and 12% in 2003 to 2006 (NHANES, NCHS).16
The obesity epidemic in children continues to grow on the basis of recent data from the Bogalusa Heart Study. Compared with 1973 to 1974, the proportion of children 5 to 17 years of age who were obese was 5 times higher in 2008 to 2009.17
Adults
Analysis of the FHS, 1971 to 2001 (NHLBI), showed that among normal-weight white adults between 30 and 59 years of age, the 4-year rates of developing overweight varied from 14% to 19% in women and from 26% to 30% in men. The 30-year risk was similar for both sexes, with some variation by age. Overall, the 30-year risk for “overweight or more” exceeded 1 in 2 people, 1 in 4 for obesity, and 1 in 10 for stage II obesity (BMI ≥35 kg/m2) across different age groups. The 30-year estimates correspond to the lifetime risk for “overweight or more” or obesity for participants 50 years of age.18
The age-adjusted prevalence of obesity among adults increased between 1976 to 1980 and 1988 to 1994 and again between 1988 to 1994 and 1999 to 2000 based on NHANES data. Over the 10-year period of 1999 to 2008, obesity showed no significant trend among women. For men, there was a significant linear trend. Obesity prevalence for men was 28% in NHANES 1999 to 2000 (NCHS) and 32% in NHANES 2007 to 2008; for women, obesity prevalence was 33% in 1999 to 2000 and 36% in 2007 to 2008.8
Thirty-five percent of noninstitutionalized women 65 to 74 years of age and 27% of women ≥75 years of age were obese on the basis of NHANES/NCHS data in 2007 to 2008. This is an increase from 1988 to 1994, when 27% of women 65 to 74 years of age and 19% of women ≥75 years of age were obese. For men, from 1988 to 1994, 24% of those 65 to 74 years of age and 13% of those ≥75 years of age were obese compared with 40% of those 65 to 74 years of age and 26% of those ≥75 years of age in 2007 to 2008.19
The prevalence of obesity increased by 5.6% or ≈2.7 million from 1997 to 2002 in Medicare beneficiaries. By 2002, 21.4% of beneficiaries and 39.3% of disabled beneficiaries were obese compared with 16.4% and 32.5%, respectively, in 1997. The rise in obesity, along with expansions in treatment coverage, could greatly increase obesity-related Medicare spending.20
The WHO estimates that by 2015, the number of overweight people globally will increase to 2.3 billion, and 700 million will be obese. Globally, at least 20 million children <5 years of age were overweight in 2005. Once considered a problem only in high-income countries, overweight and obesity are now dramatically on the rise in low- and middle-income countries, particularly in urban settings.21
Morbidity
- Overweight children and adolescents are at increased risk for future adverse health effects, including22:
-
—Increased prevalence of traditional cardiovascular risk factors such as hypertension, hyperlipidemia, and DM.
-
—Poor school performance, tobacco use, alcohol use, premature sexual behavior, poor diet, and DM.
-
—Other associated health conditions such as asthma, hepatic steatosis, sleep apnea, stroke, some cancers (breast, colon, and kidney), musculoskeletal disorders, and gallbladder disease.
-
—
The increasing prevalence of obesity is driving an increased incidence of type 2 DM. Data from the FHS indicate a doubling in the incidence of DM over the past 30 years, most dramatically during the 1990s and primarily among individuals with a BMI >30 kg/m2.23
Obesity was the most powerful predictor of DM in the Nurses’ Health Study. Women with a BMI of ≥35 kg/m2 had an RR for DM of 38.8 compared with women with a BMI of <23 kg/m2.24
Overweight and obesity were associated with increased risk for cardiovascular disease in the FHS. The age-adjusted relative risk for CVD was increased by 21% in men and 20% in women among those who were overweight and 46% in men and 64% in women among those who were obese.25
Abdominal obesity is an independent risk factor for ischemic stroke in all race/ethnic groups. This effect is larger for those <65 years of age (OR, 4.4) than for those >65 years of age (OR, 2.2; NOMAS, NINDS).26
A recent comparison of risk factors in both the Honolulu Heart Program and FHS (NHLBI) showed that a BMI increase of ≈3 kg/m2 raised the risk of hospitalized thromboembolic stroke by 10% to 30%.27
Obesity is also a strong predictor of sleep-disordered breathing, itself strongly associated with the development of CVD, as well as with myriad other health conditions, including numerous cancers, nonalcoholic fatty liver disease, gallbladder disease, musculoskeletal disorders, and reproductive abnormalities.28
Mortality
Elevated childhood BMIs in the highest quartile were associated with premature death as an adult in a cohort of 4857 American Indian children during a median follow-up of 23.9 years.29
Among adults, obesity was associated with nearly 112 000 excess deaths (95% CI, 53 754 to 170 064) relative to normal weight in 2000. Grade I obesity (BMI, 30 to <35 kg/m2) was associated with almost 30 000 of these excess deaths (95% CI, 8534 to 68 220) and grade II to III obesity (BMI ≥35 kg/m2) with >82 000 (95% CI, 44 843 to 119 289). Underweight was associated with nearly 34 000 excess deaths (95% CI, 15 726 to 51). As other studies have found,30 overweight (BMI, 25 to <30 kg/m2) was not associated with excess deaths.31
Overweight was associated with significantly increased mortality resulting from DM or kidney disease and was not associated with increased mortality resulting from cancer or CVD in an analysis of 2004 data from NHANES. Obesity was associated with significantly increased mortality caused by CVD, some cancers, and DM or kidney disease. Obesity was associated with 13% of CVD deaths in 2004.32
Data from NHANES 1988 to 1994 were studied to determine estimates of excess deaths associated with BMI and other anthropometric variables. Estimates for all-cause mortality, obesity-related causes of death, and other causes of death showed no statistically significant or systematic differences between BMI and other variables.33
In a collaborative analysis of data from almost 900 000 adults in 57 prospective studies, mostly in Western Europe and North America, overall mortality was lowest at ≈22.5 to 25 kg/m2 in both sexes and at all ages, after exclusion of early follow-up and adjustment for smoking status. Above this range, each 5-kg/m2-higher BMI was associated with ≈30% higher all-cause mortality, and no specific cause of death was inversely associated with BMI. Below 22.5 to 25 kg/m2, the overall inverse association with BMI was due predominantly to strong inverse associations for smoking-related respiratory disease, and the only clearly positive association was for ischemic heart disease.34
Overweight and obesity were associated with large decreases in life expectancy in an analysis of data from FHS (NHLBI). Forty-year-old female nonsmokers lost 3.3 years and 40-year-old male nonsmokers lost 3.1 years of life expectancy because of overweight. In 40-year-old nonsmokers, women lost 7.1 years and men lost 5.8 years because of obesity. Obese female smokers lost 7.2 years and obese male smokers lost 6.7 years compared with normal-weight nonsmokers.35
Recent calculations based on NHANES data from 1978 to 2006 suggest that the gains in life expectancy from smoking cessation are beginning to be outweighed by the loss of life expectancy from obesity.36
As a result of the increasing prevalence of obesity, the number of quality-adjusted life years lost as a result of obesity is similar to or greater than that lost as a result of smoking based on data from the BRFSS.37
Recent estimates suggest that reductions in smoking, cholesterol, BP, and PA levels resulted in a gain of 2 770 500 life-years. However, these gains were reduced by a loss of 715 000 life-years owing to the increased prevalence of obesity and DM.38
Cost
Among children and adolescents, annual hospital costs related to obesity were $127 million between 1997 and 1999.39
According to 1 study, overall estimates show that the annual medical burden of obesity has increased to almost 10% of all medical spending and could amount to $147 billion per year in 2008 (in 2008 dollars).40
If current trends in the growth of obesity continue, total healthcare costs attributable to obesity could reach $861 to $957 billion by 2030, which would account for 16% to 18% of US health expenditures.41
The total excess cost related to the current prevalence of adolescent overweight and obesity is estimated to be $254 billion, $208 billion in lost productivity secondary to premature morbidity and mortality, and $46 billion in direct medical costs.42
Abbreviations Used in Chapter 15
- BMI
body mass index
- BP
blood pressure
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CI
confidence interval
- CVD
cardiovascular disease
- DM
diabetes mellitus
- FHS
Framingham Heart Study
- kg/m2
kilograms per square meter
- MESA
Multi-Ethnic Study of Atherosclerosis
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- NHIS
National Health Interview Survey
- NHLBI
National Heart, Lung, and Blood Institute
- NINDS
National Institute of Neurological Disorders and Stroke
- NOMAS
Northern Manhattan Study
- OR
odds ratio
- PA
physical activity
- RR
relative risk
- WHO
World Health Organization
References
- 1.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 3.2008 National Healthcare Quality Report. Rockville, Md: US Department of Health and Human Services, Agency for Healthcare Research and Quality; 2009. Agency for Healthcare Research and Quality. AHRQ publication No. 09–0001. [Google Scholar]
- 4.Anderson SE, Whitaker RC. Prevalence of obesity among US preschool children in different racial and ethnic groups. Arch Pediatr Adolesc Med. 2009;163:344–348. doi: 10.1001/archpediatrics.2009.18. [DOI] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent Overweight and Obesity: Overweight in Children and Adolescents. Washington, DC: US Department of Health and Human Services; 2007. [Accessed September 28, 2010]. Available at: http://www.surgeongeneral.gov/topics/obesity/calltoaction/fact_adolescents.htm. [Google Scholar]
- 6.Robinson WR, Gordon-Larsen P, Kaufman JS, Suchindran CM, Stevens J. The female-male disparity in obese prevalence among black American young adults: contributions of sociodemographic characteristics of the childhood family. Am J Clin Nutr. 2009;89:1204–1212. doi: 10.3945/ajcn.2007.25751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003–2007. Ann Epidemiol. 2010;20:40–52. doi: 10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 8.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC) State-specific prevalence of obesity among adults: United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57:765–768. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Estimated County-Level Prevalence of Diabetes and Obesity: United States, 2007. MMWR Morb Mortal Wkly Rep. 2009;58:1259–1263. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC) State-specific prevalence of obesity among adults with disabilities: eight states and the District of Columbia, 1998–1999. MMWR Morb Mortal Wkly Rep. 2002;51:805–808. [PubMed] [Google Scholar]
- 12.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. [Accessed August 26, 2010];Vital Health Stat 10. 2010 No. 249. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_249.pdf. [PubMed]
- 13.Barnes PM, Adams PF, Powell-Griner E. Health Characteristics of the Asian Adult Population: United States, 2004–2006. Hyattsville, Md: National Center for Health Statistics; [January 22, 2008]. Advance Data From Vital and Health Statistics, No. 394. [PubMed] [Google Scholar]
- 14.Agency for Healthcare Research and Quality. 2008 National Healthcare Disparities Report. Rockville, Md: US Department of Health and Human Services, Agency for Healthcare Research and Quality; 2009. Mar, AHRQ publication No. 09–0002. [Google Scholar]
- 15.Burke GL, Bertoni AG, Shea S, Tracy R, Watson KE, Blumenthal RS, Chung H, Carnethon MR. The impact of obesity on cardiovascular disease risk factors and subclinical vascular disease: the Multi-Ethnic Study of Atherosclerosis. Arch Intern Med. 2008;168:928–935. doi: 10.1001/archinte.168.9.928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prevalence of Overweight, Infants and Children Less Than 2 Years of Age: United States, 2003–2004. Hyattsville, Md: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2007. [Accessed September 28, 2010]. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Available at: http://www.cdc.gov/nchs/data/hestat/overweight/overweight_child_under02.htm. [Google Scholar]
- 17.Broyles S, Katzmarzyk PT, Srinivasan SR, Chen W, Bouchard C, Freedman DS, Berenson GS. The pediatric obesity epidemic continues unabated in Bogalusa, Louisiana. Pediatrics. 2010;125:900–905. doi: 10.1542/peds.2009-2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vasan RS, Pencina MJ, Cobain M, Freiberg MS, D’Agostino RB. Estimated risks for developing obesity in the Framingham Heart Study. Ann Intern Med. 2005;143:473–480. doi: 10.7326/0003-4819-143-7-200510040-00005. [DOI] [PubMed] [Google Scholar]
- 19.Older Americans 2010 Key Indicators of Well-Being: Federal Interagency Forum on Aging-Related Statistics. Washington DC: US Government Printing Office; 2010. Jul, [Accessed September 28, 2010]. The Federal Interagency Forum on Aging-Related Statistics. Available at: http://www.agingstats.gov. [Google Scholar]
- 20.Doshi JA, Polsky D, Chang VW. Prevalence and trends in obesity among aged and disabled U.S. Medicare beneficiaries, 1997–2002. Health Aff (Millwood) 2007;26:1111–1117. doi: 10.1377/hlthaff.26.4.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization. Obesity and Overweight. Geneva, Switzerland: World Health Organization; 2006. Sep, [Accessed September 28, 2010]. Fact Sheet No. 311. Available at: http://www.who.int/mediacentre/factsheets/fs311/en/print.html/. [Google Scholar]
- 22.Daniels SR, Jacobson MS, McCrindle BW, Eckel RH, Sanner BM. American Heart Association Childhood Obesity Research Summit: executive summary. Circulation. 2009;119:2114–2123. doi: 10.1161/CIRCULATIONAHA.109.192215. [DOI] [PubMed] [Google Scholar]
- 23.Fox CS, Pencina MJ, Meigs JB, Vasan RS, Levitzky YS, D’Agostino RB., Sr Trends in the incidence of type 2 diabetes mellitus from the 1970s to the 1990s: the Framingham Heart Study. Circulation. 2006;113:2914–2918. doi: 10.1161/CIRCULATIONAHA.106.613828. [DOI] [PubMed] [Google Scholar]
- 24.Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, Willett WC. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001;345:790–797. doi: 10.1056/NEJMoa010492. [DOI] [PubMed] [Google Scholar]
- 25.Wilson PW, D’Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk: the Framingham Experience. Arch Intern Med. 2002;162:1867–1872. doi: 10.1001/archinte.162.16.1867. [DOI] [PubMed] [Google Scholar]
- 26.Suk SH, Sacco RL, Boden-Albala B, Cheun JF, Pittman JG, Elkind MS, Paik MC Northern Manhattan Stroke Study. Abdominal obesity and risk of ischemic stroke: the Northern Manhattan Stroke Study. Stroke. 2003;34:1586–1592. doi: 10.1161/01.STR.0000075294.98582.2F. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez BL, D’Agostino R, Abbott RD, Kagan A, Burchfiel CM, Yano K, Ross GW, Silbershatz H, Higgins MW, Popper J, Wolf PA, Curb JD. Risk of hospitalized stroke in men enrolled in the Honolulu Heart Program and the Framingham Study: a comparison of incidence and risk factor effects. Stroke. 2002;33:230–236. doi: 10.1161/hs0102.101081. [DOI] [PubMed] [Google Scholar]
- 28.Brown WV, Fujioka K, Wilson PW, Woodworth KA. Obesity: why be concerned? Am J Med. 2009;122:S4–S11. doi: 10.1016/j.amjmed.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 29.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McGee DL Diverse Populations Collaboration. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol. 2005;15:87–97. doi: 10.1016/j.annepidem.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 31.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 32.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298:2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 33.Flegal KM, Graubard BI. Estimates of excess deaths associated with body mass index and other anthropometric variables. Am J Clin Nutr. 2009;89:1213–1219. doi: 10.3945/ajcn.2008.26698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prospective Studies Collaboration. Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun A, Bonneux L NEDCOM, the Netherlands Epidemiology and Demography Compression of Morbidity Research Group. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med. 2003;138:24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 36.Stewart ST, Cutler DM, Rosen AB. Forecasting the effects of obesity and smoking on US life expectancy. N Engl J Med. 2009;361:2252–2260. doi: 10.1056/NEJMsa0900459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jia H, Lubetkin EI. Trends in quality-adjusted life-years lost contributed by smoking and obesity. Am J Prev Med. 2010;38:138–144. doi: 10.1016/j.amepre.2009.09.043. [DOI] [PubMed] [Google Scholar]
- 38.Capewell S, Hayes DK, Ford ES, Critchley JA, Croft JB, Greenlund KJ, Labarthe DR. Life-years gained among US adults from modern treatments and changes in the prevalence of 6 coronary heart disease risk factors between 1980 and 2000. Am J Epidemiol. 2009;170:229–236. doi: 10.1093/aje/kwp150. [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Preventing Obesity and Chronic Diseases Through Good Nutrition and Physical Activity. Atlanta, Ga: Centers for Disease Control and Prevention; [Accessed September 28, 2010]. Revised 2008. Available at: http://www.cdc.gov/nccdphp/publications/factsheets/prevention/pdf/obesity.pdf. [Google Scholar]
- 40.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff (Millwood) 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 41.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring) 2008;16:2323–2330. doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]
- 42.Lightwood J, Bibbins-Domingo K, Coxson P, Wang YC, Williams L, Goldman L. Forecasting the future economic burden of current adolescent overweight: an estimate of the Coronary Heart Disease Policy Model. Am J Public Health. 2009;99:2230–2237. doi: 10.2105/AJPH.2008.152595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Lim C, Whittle L, Brener ND, Wechsler H Centers for Disease Control and Prevention. Youth risk behavior surveillance: United States, 2009. MMWR Surveill Summ. 2010;59:1–142. [PubMed] [Google Scholar]
- 44.National Center for Health Statistics. Health, United States, 2009: With Special focus on Young Adults. Hyattsville, Md: National Center for Health Statistics; 2010. [Accessed September 23, 2010]. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. [Google Scholar]
16. Risk Factor: Diabetes Mellitus
ICD-9 250; ICD-10 E10–E14. See Table 16-1 and Charts 16-1 through 16-4.
Table 16-1.
Diabetes Mellitus
| Population Group | Prevalence of Physician-Diagnosed DM, 2008, Age ≥20 y |
Prevalence of Undiagnosed DM, 2008, Age ≥20 y |
Prevalence of Prediabetes, 2008, Age ≥20 y |
Incidence of Diagnosed DM, Age ≥20 y |
Mortality (DM), 2007,* All Ages |
Hospital Discharges, 2007, All Ages |
Cost, 2007† |
|---|---|---|---|---|---|---|---|
| Both sexes | 18 300 000 (8.0%) | 7 100 000 (3.1%) | 81 500 000 (36.8%) | 1 600 000† | 71 382 | 626 000 | $174 billion |
| Males | 8 300 000 (7.9%) | 4 400 000 (4.1%) | 48 100 000 (44.9%) | 35 478 (49.7%)‡ | 322 000 | ||
| Females | 10 000 000 (8.2%) | 2 700 000 (2.3%) | 33 400 000 (28.8%) | 35 904 (50.3%)‡ | 304 000 | ||
| NH white males | 6.8% | 3.9% | 45.4% | 28 744 | |||
| NH white females | 6.5% | 1.9% | 27.9% | 27 646 | |||
| NH black males | 14.3% | 4.8% | 31.6% | 5493 | |||
| NH black females | 14.7% | 4.0% | 27.1% | 6966 | |||
| Mexican American males | 11.0% | 6.3% | 44.9% | ||||
| Mexican American females | 12.7% | 3.8% | 34.3% |
Ellipses (…) indicate data not available;
NH indicates non-Hispanic; DM, diabetes mellitus.
Undiagnosed DM is defined as those whose fasting glucose is ≥126 mg/dL but who did not report being told by a healthcare provider that they had DM. Prediabetes is a fasting blood glucose of 100 to <126 mg/dL (impaired fasting glucose). Prediabetes includes impaired glucose tolerance.
Mortality data are for whites and blacks and include Hispanics.
Centers for Disease Control and Prevention; National Diabetes Fact Sheet, 2007. Accessed June 24, 2008.
These percentages represent the portion of total DM mortality that is for males versus females.
Sources: Prevalence: Prevalence of diagnosed and undiagnosed diabetes: National Health and Nutrition Examination Survey 2005–2008, National Center for Health Statistics, and National Heart, Lung, and Blood Institute. Percentages for racial/ethnic groups are age-adjusted for Americans ≥20 years of age. Age-specific percentages are extrapolations to the 2008 US population estimates. Incidence: National Institute of Diabetes and Digestive and Kidney Diseases estimates. Mortality: National Center for Health Statistics. These data represent underlying cause of death only. Hospital discharges: National Hospital Discharge Survey, National Center for Health Statistics; data include those inpatients discharged alive, dead, or status unknown.
Chart 16-1.
Age-adjusted prevalence of physician-diagnosed diabetes mellitus in adults ≥20 years of age by race/ethnicity and sex (National Health and Nutrition Examination Survey: 2005–2008). NH indicates non-Hispanic. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 16-4.
Diabetes mellitus awareness, treatment, and control (National Health and Nutrition Examination Survey: 2005–2008). Source: National Heart, Lung, and Blood Institute.
Prevalence
Youth
In SEARCH, the prevalence of DM in youths <20 years of age in 2001 in the United States was 1.82 cases per 1000 youths (0.79 per 1000 among youths 0 to 9 years of age and 2.80 per 1000 among youths 10 to 19 years of age). Non-Hispanic white youths had the highest prevalence (1.06 per 1000) in the younger group. Among youths 10 to 19 years of age, black youths (3.22 per 1000) and non-Hispanic white youths (3.18 per 1000) had the highest rates, followed by American Indian youths (2.28 per 1000), Hispanic youths (2.18 per 1000), and Asian/Pacific Islander youths (1.34 per 1000). Among younger children, type 1 DM accounted for ≥80% of DM; among older youths, the proportion of type 2 DM ranged from 6% (0.19 per 1000 for non-Hispanic white youths) to 76% (1.74 per 1000 for American Indian youths). This translates to 154 369 youths with physician-diagnosed DM in 2001 in the United States, for an overall prevalence estimate for DM in children and adolescents of ≈0.18%.1
Approximately 186 000 people <20 years of age have DM. Each year, ≈15 000 people <20 years of age are diagnosed with type 1 DM. Healthcare providers are finding more and more children with type 2 DM, a disease usually diagnosed in adults ≥40 years of age. Children who develop type 2 DM are typically overweight or obese and have a family history of the disease. Most are American Indian, black, Asian, or Hispanic/Latino.2
Among adolescents 10 to 19 years of age diagnosed with DM, 57.8% of blacks were diagnosed with type 2 versus type 1 DM compared with 46.1% of Hispanic and 14.9% of white youths.3
According to the Bogalusa Heart Study, a long-term follow-up study of youths aging into adulthood, youths who were prediabetic or who had DM are more likely to have a constellation of metabolic disorders in young adulthood (19 to 44 years of age), including obesity, hypertension, dyslipidemia, and metabolic syndrome, all of which predispose to CHD.4
Adult
On the basis of data from NHANES 2005 to 2008 (NCHS; unpublished NHLBI tabulation) (Table 16-1), an estimated 18 300 000 Americans ≥20 years of age have physician-diagnosed DM. An additional 7 100 000 adults have undiagnosed DM and about 81 500 000 adults have prediabetes (eg, fasting blood glucose of 100 to <126 mg/dL). The prevalence of prediabetes in the US adult population is nearly 37%.
Data from NHANES 2005 to 2006 (NCHS) showed the prevalence of diagnosed DM in adults ≥65 years of age to be 17.0%. The prevalence of undiagnosed DM was 14.6% (based on fasting glucose or oral glucose tolerance testing).5
Among Americans ≥20 years of age, 7.7% have diagnosed DM. Women ≥20 years of age have a slightly higher prevalence (8.3%) than men (7.2%) (NHANES) (NCHS).5
Data from NHANES (NCHS) show a disproportionately high prevalence of DM in non-Hispanic blacks compared with non-Hispanic whites.5
After adjustment for population age differences, 2004 to 2006 national survey data for people ≥20 years of age indicate that 6.6% of non-Hispanic whites, 7.5% of Asian Americans, 10.4% of Hispanics, and 11.8% of non-Hispanic blacks had diagnosed DM.6
In 2004 to 2006, the prevalence of diagnosed DM was more than twice as high for Asian Indian adults (14%) as for Chinese (6%) or Japanese (5%) adults.7
Type 2 DM accounts for 90% to 95% of all diagnosed cases of DM in adults.8 In Framingham, MA, 99% of DM is type 2.9
The prevalence of DM increased by 8.2% from 2000 to 2001. From 1990 to 2001, the prevalence of those diagnosed with DM increased 61%.10
On the basis of 2009 BRFSS (CDC) data, the prevalence of adults who reported ever having been told by a physician that they had DM ranged from 5.8% in Alaska and Colorado to 12.4% in West Virginia. The median percentage among states was 8.3%.11
The CDC analyzed data from 1994 to 2004 collected by the Indian Health Service that indicated that the age-adjusted prevalence per 1000 population of DM increased 101.2% among American Indian/Alaska Native adults <35 years of age (from 8.5% to 17.1%). During this time period, the prevalence of diagnosed DM was greater among females than males in all age groups.12
The prevalence of DM for all age groups worldwide was estimated to be 2.8% in 2000 and is projected to be 4.4% in 2030. The total number of people with DM is projected to rise from 171 million in 2000 to 366 million in 2030.13
On the basis of projections from NHANES/NCHS studies between 1984 and 2004, the total prevalence of DM in the United States is expected to more than double from 2005 to 2050 (from 5.6% to 12.0%) in all age, sex, and race/ethnicity groups. Increases are projected to be largest for the oldest age groups (for instance, increasing by 220% among those 65 to 74 years of age and by 449% among those ≥75 years of age). DM prevalence is projected to increase by 99% among non-Hispanic whites, by 107% among non-Hispanic blacks, and by 127% among Hispanics. The age/race/ethnicity group with the largest increase is expected to be blacks ≥75 years of age (increase of 606%).14
Incidence
Youths
In the SEARCH study, the incidence of DM in youths overall was 24.3 per 100 000 person-years. Among children <10 years of age, most had type 1 DM, regardless of race/ethnicity. The highest rates of incident type 1 DM were observed in non-Hispanic white youths (18.6, 28.1, and 32.9 per 100 000 person-years for age groups of 0 to 4, 5 to 9, and 10 to 14 years, respectively). Overall, type 2 DM was relatively infrequent, with the highest rates (17.0 to 49.4 per 100 000 person-years) seen among 15- to 19-yearold minority groups.3
Adults
A total of 1 600 000 new cases of DM were diagnosed in people ≥20 years of age in 2006.6
Data from Framingham, MA, indicate a doubling in the incidence of DM over the past 30 years, most dramatically during the 1990s. Among adults 40 to 55 years of age in each decade of the 1970s, 1980s, and 1990s, the age-adjusted 8-year incidence rates of DM were 2.0%, 3.0%, and 3.7% among women and 2.7%, 3.6%, and 5.8% among men, respectively. Compared with the 1970s, the age- and sex-adjusted OR for DM was 1.40 in the 1980s and 2.05 in the 1990s (P for trend = 0.0006). Most of the increase in absolute incidence of DM occurred in individuals with a BMI ≥30 kg/m2 (P for trend = 0.03).15
DM incidence in adults also varies markedly by race. Over 5 years of follow-up in 45- to-84-year-olds in the MESA, 8.2% of the cohort developed DM. The cumulative incidence was highest in Hispanics (11.3%), followed by black (9.5%), Chinese (7.7%), and white (6.3%) participants.16
Mortality
DM mortality in 2007 was 71 382. Any-mention mortality in 2007 was 231 402 (NHLBI tabulation of NCHS mortality data).
The 2007 overall underlying-cause death rate owing to DM was 22.5. Death rates per 100 000 people were 24.6 for white males, 45.9 for black males, 17.2 for white females, and 40.2 for black females (NCHS, Health Data Interactive Web site http://www.cdc.gov/nchs/hdi; accessed July 19, 2010).
- According to data from the National Diabetes Information Clearinghouse, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), and the National Institutes of Health (NIH):
-
—At least 65% of people with DM die of some form of HD or stroke.
-
—HD death rates among adults with DM are 2 to 4 times higher than the rates for adults without DM.17
-
—
FHS/NHLBI data show that having DM significantly increased the risk of developing CVD (HR, 2.5 for women and 2.4 for men) and of dying when CVD was present (HR, 2.2 for women and 1.7 for men). Diabetic men and women ≥50 years of age lived an average of 7.5 and 8.2 years less than their nondiabetic equivalents. The differences in life expectancy free of CVD were 7.8 and 8.4 years, respectively.18
Analysis of data from NHANES 1971 to 2000 found that men with DM experienced a 43% relative reduction in the age-adjusted mortality rate, which is similar to that of nondiabetic men. Among women with DM, however, mortality rates did not decrease, and the difference in mortality rates between diabetic and nondiabetic women doubled.19
During 1979 to 2004, DM death rates for black youths 1 to 19 years of age were approximately twice those for white youths. During 2003 to 2004, the annual average DM death rate per 1 million youths was 2.46 for black youths and 0.91 for white youths.20
Analysis of data from the FHS from 1950 to 2005 found reductions in all-cause and CVD mortality among men and women with and without DM. However, all-cause and CVD mortality rates among individuals with DM remain ≈2-fold higher compared with individuals without DM.21
Awareness
The NIDDK estimates that 23.6 million Americans (7.8% of the population) have DM.6
Analysis of NHANES/NCHS data from 1988 to 1994 to 1999 to 2005 to 2006 in adults ≥20 years of age showed that 40% of those with DM did not know they had it.5 Although the prevalence of diagnosed DM has increased significantly over the past decade, the prevalences of undiagnosed DM and impaired fasting glucose have remained relatively stable. Minority groups remain disproportionately affected.22
Analysis of NHANES/NCHS data collected during 2005 to 2008 indicated that the prevalence of DM was 8.2% among people ≥20 years of age. Prevalence of DM was defined as people who were told by a physician or other health professional that they have DM. Of the estimated 18 300 adults with DM, 73.3% were told or were on treatment and 26.7% (5.7 million) were unaware of the diagnosis. Of 7 895 000 people being treated (37.3% of the diabetic population), one third of them (2 604 000) were controlled (ie, on treatment with fasting plasma glucose <126 mg/dL) and 25.0% (5 300 000) were treated and uncontrolled (fasting plasma glucose ≥126 mg/dL). An estimated 13 300 000 individuals with DM are not treated. The untreated and unaware population (5 600 000) was 26.7% of the diabetic population (NHLBI tabulation of NHANES 2003 to 2006) (see Chart 16-4).
Aftermath
Although the exact date of DM onset can be difficult to determine, duration of DM appears to affect CVD risk. Longitudinal data from Framingham, MA, suggest that the risk factor–adjusted relative risk of CHD was 1.38 (95% CI, 0.99 to 1.92) times higher and the risk for CHD death was 1.86 (95% CI, 1.17 to 2.93) times higher for each 10-year increase in duration of DM.23
DM increases the risk of stroke, with the RR ranging from 1.8 to almost 6.0.24
Ischemic stroke patients with DM are younger, more likely to be black, and more likely to have hypertension, MI, and high cholesterol than nondiabetic patients. DM increases ischemic stroke incidence at all ages, but this risk is most prominent before 55 years of age in blacks and before 65 years of age in whites.25
- On the basis of data from the NCHS/NHIS, 1997 to 2005:26
-
—During 1997 to 2005, the estimated number of people ≥35 years of age with DM with a self-reported cardiovascular condition increased 36%, from 4.2 million in 1997 to 5.7 million in 2005. However, the age-adjusted prevalence of self-reported CVD conditions among people with diagnosed DM ≥35 years of age decreased 11.2%, from 36.6% in 1997 to 32.5% in 2005.
-
—During 1997 to 2005, age-adjusted CVD prevalence was higher among men than women, among whites than blacks, and among non-Hispanics than Hispanics. Among women, the age-adjusted prevalence decreased by 11.2%; among men, it did not decrease significantly. Among blacks, the age-adjusted prevalence of self-reported CVD decreased by 25.3%; among whites, no significant decrease occurred; among non-Hispanics, the rate decreased by 12%. No clear trends were detected among Hispanics. If the total number of people with DM and self-reported CVD increased over this period but proportions with self-reported CVD declined, the data suggest that the mean age at which people have been diagnosed is decreasing, or the higher CVD mortality rate among older diabetic individuals is removing them from ability to self-report CVD. These and other data show a consistent increase over time in the United States of the number of people with DM and CVD.
-
—
Statistical modeling of the use and effectiveness of specific cardiac treatments and of changes in risk factors between 1980 and 2000 among US adults 25 to 84 years of age showed that the age-adjusted death rate for CHD decreased from 543 to 267 deaths per 100 000 population among men and from 263 to 134 deaths per 100 000 population among women. Approximately 47% of this decrease was attributed to treatments, and ≈44% was attributed to changes in risk factors, although reductions were offset in part by increases in BMI and the prevalence of DM, which accounted for an increased number of deaths (8% and 10%, respectively).27 An analysis from the Cooper Clinic in Dallas, TX, of exercise electrocardiographic responses and CVD mortality in 2854 men with DM reported 441 deaths (210 CVD and 133 CHD) over a follow-up of 16 years. That analysis showed that equivocal and abnormal exercise electrocardiographic responses were associated with higher risk of all-cause, CVD, and CHD mortality. Across normal, equivocal, and abnormal exercise electrocardiographic groups, age- and examination year–adjusted CHD mortality rates per 10 000 person-years were 23.0, 48.6, and 69.0, respectively (P for trend <0.001), and risk factor–adjusted HRs were 1.00, 1.68 (95% CI, 1.01 to 2.77), and 2.21 (95% CI, 1.41 to 3.46; P for trend <0.001), respectively.28
A subgroup analysis was conducted of patients with DM enrolled in randomized clinical trials that evaluated ACS therapies. The data included 62 036 patients from TIMI studies (46 577 with STEMI and 15 459 with unstable angina/non-STEMI [UA/NSTEMI]). Of these, 17.1% had DM. Modeling showed that mortality at 30 days was significantly higher among patients with DM than among those without DM who presented with UA/NSTEMI (2.1% versus 1.1%; P≤0.001) and STEMI (8.5% versus 5.4%; P = 0.001), with adjusted risks for 30-day mortality in DM versus no DM of 1.78 for UA/NSTEMI (95% CI, 1.24 to 2.56) and 1.40 (95% CI, 1.24 to 1.57) for STEMI. DM was also associated with significantly higher mortality 1 year after UA/NSTEMI or STEMI. By 1 year after ACS, patients with DM presenting with UA/NSTEMI had a risk of death that approached that of patients without DM presenting with STEMI (7.2% versus 8.1%).29
Data from the ARIC study of the NHLBI found that DM was a weaker predictor of CHD in blacks than in whites.30
- Data from Framingham, MA, show that despite improvements in CVD morbidity and mortality, DM continues to elevate CVD risk. Participants 45 to 64 years of age from the FHS original and offspring cohorts who attended examinations in 1950 to 1966 (“earlier” time period) and 1977 to 1995 (“later” time period) were followed up for incident MI, CHD death, and stroke. Among participants with DM, the age- and sex-adjusted CVD incidence rate was 286.4 per 10 000 person-years in the earlier period and 146.9 per 10 000 person-years in the later period, a 35.4% decline. HRs for DM as a predictor of incident CVD were not significantly different in the earlier (risk factor–adjusted HR, 2.68; 95% CI, 1.88 to 3.82) versus later (HR, 1.96; 95% CI, 1.44 to 2.66) periods.31 Thus, although there was a 50% reduction in the rate of incident CVD events among adults with DM, the absolute risk of CVD remained 2-fold greater than among people without DM.31
-
—Data from these earlier and later time periods in Framingham also suggest that the increasing prevalence of DM is leading to an increasing rate of CVD, resulting in part from CVD risk factors that commonly accompany DM. The age- and sex-adjusted HR for DM as a CVD risk factor was 3.0 in the earlier time period and 2.5 in the later time period. Because the prevalence of DM has increased over time, the population-attributable risk for DM as a CVD risk factor increased from 5.4% in the earlier time period to 8.7% in the later time period (attributable risk ratio, 1.62; P = 0.04). Adjustment for CVD risk factors (age, sex, hypertension, current smoking, high cholesterol, and obesity) weakened this attributable risk ratio to 1.5 (P = 0.12).32
-
—Other data from Framingham show that over 30 years, CVD among women with DM was 54.8% among normal-weight women but 78.8% among obese women. Among normal-weight men with DM, the lifetime risk of CVD was 78.6%, whereas it was 86.9% among obese men.33
-
—
Other studies show that the increased prevalence of DM is being followed by an increasing prevalence of CVD morbidity and mortality. New York City death certificate data for 1989 to 1991 and 1999 to 2001 and hospital discharge data for 1988 to 2002 show increases in all-cause and cause-specific mortality between 1990 and 2000, as well as in annual hospitalization rates for DM and its complications among patients hospitalized with AMI and/or DM. During this decade, all-cause and cause-specific mortality rates declined, although not for patients with DM; rates increased 61% and 52% for diabetic men and women, respectively, as did hospitalization rates for DM and its complications. The percentage of all AMIs occurring in patients with DM increased from 21% to 36%, and the absolute number more than doubled, from 2951 to 6048. Although hospital days for AMI fell overall, for those with DM, they increased 51% (from 34 188 to 51 566). These data suggest that increases in DM rates threaten the long-established nationwide trend toward reduced coronary artery events.34
In an analysis of provincial health claims data for adults living in Ontario, Canada, between 1992 and 2000, the rate of patients admitted for AMI and stroke decreased to a greater extent in the diabetic than the nondiabetic population (AMI, −15.1% versus −9.1%, P = 0.0001; stroke, −24.2% versus −19.4%, P = 0.0001). Diabetic patients experienced reductions in case fatality rates related to AMI and stroke similar to those without DM (−44.1% versus −33.2%, P = 0.1; −17.1% versus −16.6%, P = 0.9, respectively) and similarly comparable decreases in all-cause mortality. Over the same period, the number of DM cases increased by 165%, which translates to a marked increase in the proportion of CVD events occurring among patients with DM: AMI, 44.6%; stroke, 26.1%; AMI deaths, 17.2%; and stroke deaths, 13.2%.35
In the same data set, the transition to a high-risk category (an event rate equivalent to a 10-year risk of 20% or an event rate equivalent to that associated with previous MI) occurred at a younger age for men and women with DM than for those without DM (mean difference, 14.6 years). For the outcome of AMI, stroke, or death resulting from any cause, diabetic men and women entered the high-risk category at 47.9 and 54.3 years of age, respectively. The data suggest that DM confers a risk equivalent to aging 15 years. In North America, diverse data show lower rates of CVD among diabetic people, but as the prevalence of DM has increased, so has the absolute burden of CVD, especially among middle-aged and older individuals.36
HbA1c levels ≥6.5% can be used to diagnose DM.37 In the population-based ARIC study, HbA1c levels ≥6.5% had a 14-year follow-up, multivariable-adjusted HR for diagnosed DM of 16.5 (95% CI, 14.2 to 19.1) and for CHD of 1.95 (95% CI, 1.53 to 2.48) relative to those with HbA1c <5.0%.38
Risk Factors
- Data from the 2004 National Healthcare Disparities Report (AHRQ, US Department of Health and Human Services) found that only approximately one third of adults with DM received all 5 interventions to reduce risk factors recommended for comprehensive DM care in 2001. The proportion receiving all 5 interventions was lower among blacks than whites and among Hispanics than non-Hispanic whites.39
-
—In multivariate models that controlled for age, sex, income, education, insurance, and residence location, blacks were 38% less likely and Hispanics were 33% less likely than their respective comparison groups to receive all recommended risk factor interventions in 2001.39
-
—
Between NHANES III 1988 to 1994 (NCHS) and NHANES 1999 to 2002 (NCHS), considerable differences were found among ethnic groups in glycemic control rates among adults with type 2 DM. Among non-Hispanic whites, the control rates were 43.8% in 1988 to 1994 and 48.4% in 1999 to 2002. For non-Hispanic blacks, the rates were 41.2% and 36.5%, respectively. For Mexican Americans, the respective rates were 34.5% and 34.2%.40
- In 1 large academic medical center, outpatients with type 2 DM were observed during an 18-month period for proportions of patients who had HbA1c levels, BP, or total cholesterol levels measured; who had been prescribed any drug therapy if HbA1c levels, SBP, or LDL cholesterol levels exceeded recommended treatment goals; and who had been prescribed greater-than-starting-dose therapy if these values were above treatment goals. Patients were less likely to have cholesterol levels measured (76%) than HbA1c levels (92%) or BP (99%; P<0.0001 for either comparison). The proportion of patients who received any drug therapy was greater for above-goal HbA1c (92%) than for above-goal SBP (78%) or LDL cholesterol (38%; P<0.0001 for each comparison). Similarly, patients whose HbA1c levels were above the treatment goal (80%) were more likely to receive greater-than-starting-dose therapy than were those who had above-goal SBP (62%) and LDL cholesterol levels (13%; P<0.0001).41
-
—Data from the same academic medical center also showed that CVD risk factors among women with DM were managed less aggressively than among men with DM. Women were less likely than men to have HbA1c <7% (without CHD: adjusted OR for women versus men, 0.84, P = 0.005; with CHD: 0.63, P<0.0001). Women without CHD were less likely than men to be treated with lipid-lowering medication (0.82; P = 0.01) or, when treated, to have LDL cholesterol levels <100 mg/dL (0.75; P = 0.004) and were less likely than men to be prescribed aspirin (0.63; P<0.0001). Women with DM and CHD were less likely than men to be prescribed aspirin (0.70, P<0.0001) and, when treated for hypertension or hyperlipidemia, were less likely to have BP levels <130/80 mm Hg (0.75; P<0.0001) or LDL cholesterol levels <100 mg/dL (0.80; P = 0.006).42
-
—
In 2001 to 2002, among adults ≥18 years of age with DM, 50.2% were not at goal for HbA1c (<7%), 64.6% were not at goal for LDL cholesterol (<100 mg/dL), and 53% were not at goal for BP (<130/80 mm Hg). Moreover, 48.6% were not at recommended levels of triglycerides (<150 mg/dL in women). Only 5.3% of men and 12.7% of women were simultaneously at goal for HbA1c, LDL cholesterol, and BP.43
Analysis of data from the CHS study of the NHLBI found that lifestyle risk factors, including physical activity level, dietary habits, smoking habits, alcohol use, and adiposity measures, assessed late in life, were each independently associated with risk of new-onset DM. Participants whose PA level and dietary, smoking, and alcohol habits were all in the low-risk group had an 82% lower incidence of DM compared with all other participants. When absence of adiposity was added to the other 4 low-risk lifestyle factors, incidence of DM was 89% lower.44
Aggressive treatment of hypertension is recommended for adults with DM to prevent cardiovascular complications. Between NHANES III (1984 to 1992) and NHANES 1999 to 2004, the proportion of patients with DM whose BP was treated increased from 76.5% to 87.8%, and the proportion whose BP was controlled nearly doubled (15.9% to 29.6%).45
Hospitalizations
Youth
National Inpatient Sample data from 1993 to 2004 were analyzed for individuals 0 to 29 years of age with a diagnosis of DM. Rates of hospitalizations increased by 38%. Hospitalization rates were higher for females (42%) than for males (29%). Inflation-adjusted total charges for DM hospitalizations increased 130%, from $1.05 billion in 1993 to $2.42 billion in 2004.46
Cost
In 2007, the direct ($116 billion) and indirect ($58 billion) cost attributable to DM was $174 billion.6 These estimates include not just DM as a primary diagnosis but also DM-related long-term complications that are attributed to DM.47
A study of data from NHANES 2003 to 2006, Ingenix Research DataMart, 2003 to 2005 National Ambulatory Medical Care Survey, the 2003 to 2005 National Hospital Ambulatory Medical Care Survey, the 2004 to 2005 Nationwide Inpatient Sample, and the 2003 to 2005 Medical Expenditure Panel Survey found that the estimated economic cost of undiagnosed DM in 2007 was $18 billion, including medical costs of $11 billion and indirect costs of $7 billion.48
Abbreviations Used in Chapter 16
- ACS
acute coronary syndrome
- AHRQ
Agency for Healthcare Research and Quality
- AMI
acute myocardial infarction
- ARIC
Atherosclerosis Risk in Communities study
- BMI
body mass index
- BP
blood pressure
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CHD
coronary heart disease
- CHS
Cardiovascular Health Study
- CI
confidence interval
- CVD
cardiovascular disease
- DM
diabetes mellitus
- FHS
Framingham Heart Study
- HbA1c
glycosylated hemoglobin
- HD
heart disease
- HR
hazard ratio
- ICD
International Classification of Diseases
- kg/m2
kilograms per square meter
- LDL
low-density lipoprotein
- mg/dL
milligrams per deciliter
- MESA
Multi-Ethnic Study of Atherosclerosis
- MI
myocardial infarction
- mm Hg
millimeter of mercury
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- NHDS
National Hospital Discharge Survey
- NHIS
National Health Interview Survey
- NHLBI
National Heart, Lung, and Blood Institute
- NIDDK
National Institute of Diabetes and Digestive and Kidney Diseases
- NIH
National Institutes of Health
- NINDS
National Institute of Neurological Disorders and Stroke
- NSTEMI
non–ST-segment–elevation myocardial infarction
- OR
odds ratio
- PA
physical activity
- RR
relative risk
- SBP
systolic blood pressure
- SEARCH
Search for Diabetes in Youth Study
- STEMI
ST-segment–elevation myocardial infarction
- TIMI
Thrombolysis in Myocardial Infarction
- UA
unstable angina
References
- 1.SEARCH for Diabetes in Youth Study Group. Liese AD, D’Agostino RB, Jr, Hamman RF, Kilgo PD, Lawrence JM, Liu LL, Loots B, Linder B, Marcovina S, Rodriguez B, Standiford D, Williams DE. The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006;118:1510–1518. doi: 10.1542/peds.2006-0690. [DOI] [PubMed] [Google Scholar]
- 2.Liu LL, Yi JP, Beyer J, Mayer-Davis EJ, Dolan LM, Dabelea DM, Lawrence JM, Rodriguez BL, Marcovina SM, Waitzfelder BE, Fujimoto WY SEARCH for Diabetes in Youth Study Group. Type 1 and Type 2 diabetes in Asian and Pacific Islander US. youth: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2009;32(suppl 2):S133–S140. doi: 10.2337/dc09-S205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Writing Group for the SEARCH for Diabetes in Youth Study Group. Dabelea D, Bell RA, D’Agostino RB, Jr, Imperatore G, Johansen JM, Linder B, Liu LL, Loots B, Marcovina S, Mayer-Davis EJ, Pettitt DJ, Waitzfelder B. Incidence of diabetes in youth in the United States. JAMA. 2007;297:2716–2724. doi: 10.1001/jama.297.24.2716. [published correction appears in JAMA. 2007;298:627] [DOI] [PubMed] [Google Scholar]
- 4.Nguyen QM, Srinivasan SR, Xu JH, Chen W, Berenson GS. Changes in risk variables of metabolic syndrome since childhood in pre-diabetic and type 2 diabetic subjects: the Bogalusa Heart Study. Diabetes Care. 2008;31:2044–2049. doi: 10.2337/dc08-0898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cowie CC, Rust KF, Ford ES, Eberhardt MS, Byrd-Holt DD, Li C, Williams DE, Gregg EW, Bainbridge KE, Saydah SH. Full accounting of diabetes and pre-diabetes in the US population in 1988–1994 and 2005–2006. Diabetes Care. 2009;32:287–294. doi: 10.2337/dc08-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics, 2007 Fact Sheet. Bethesda, Md: US Department of Health and Human Services, National Institutes of Health; 2008. [Google Scholar]
- 7.Barnes PM, Adams PF, Powell-Griner E. Health Characteristics of the Asian Adult Population: United States, 2004–2006. Hyattsville, Md: National Center for Health Statistics; 2008. Jan 22, Advance Data From Vital and Health Statistics; No. 394. [PubMed] [Google Scholar]
- 8.National Diabetes Information Clearinghouse. National diabetes statistics. [Accessed September 28, 2010]; Available at: http://www.diabetes.niddk.nih.gov/dm/pubs/statistics/index.htm.
- 9.Meigs JB, Cupples LA, Wilson PW. Parental transmission of type 2 diabetes mellitus: the Framingham Offspring Study. Diabetes. 2000;49:2201–2207. doi: 10.2337/diabetes.49.12.2201. [DOI] [PubMed] [Google Scholar]
- 10.Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Data. Atlanta, Ga: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2009. [Accessed September 15, 2010]. Prevalence and trends data. Available at: http://apps.nccd.cdc.gov/brfss/index.asp. [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC) Diagnosed diabetes among American Indians and Alaska Natives aged <35 years: United States, 1994–2002. MMWR Morb Mortal Wkly Rep. 2006;55:1201–1203. [PubMed] [Google Scholar]
- 13.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 14.Narayan KM, Boyle JP, Geiss LS, Saaddine JB, Thompson TJ. Impact of recent increase in incidence on future diabetes burden: U.S., 2005–2050. Diabetes Care. 2006;29:2114–2116. doi: 10.2337/dc06-1136. [DOI] [PubMed] [Google Scholar]
- 15.Fox CS, Pencina MJ, Meigs JB, Vasan RS, Levitzky YS, D’Agostino RB., Sr Trends in the incidence of type 2 diabetes mellitus from the 1970s to the 1990s: the Framingham Heart Study. Circulation. 2006;113:2914–2918. doi: 10.1161/CIRCULATIONAHA.106.613828. [DOI] [PubMed] [Google Scholar]
- 16.Nettleton JA, Steffen LM, Ni H, Liu K, Jacobs DR. Dietary patterns and risk of incident type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA) Diabetes Care. 2008;31:1777–1782. doi: 10.2337/dc08-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Diabetes Information Clearinghouse (a service of the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health) [Accessed September 28, 2010];Diabetes Across the United States. Available at: http://www.diabetes.niddk.nih.gov/populations/index.htm.
- 18.Franco OH, Steyerberg EW, Hu FB, Mackenbach J, Nusselder W. Associations of diabetes mellitus with total life expectancy and life expectancy with and without cardiovascular disease. Arch Intern Med. 2007;167:1145–1151. doi: 10.1001/archinte.167.11.1145. [DOI] [PubMed] [Google Scholar]
- 19.Gregg EW, Gu Q, Cheng YJ, Narayan KM, Cowie CC. Mortality trends in men and women with diabetes, 1971 to 2000. Ann Intern Med. 2007;147:149–155. doi: 10.7326/0003-4819-147-3-200708070-00167. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) Racial disparities in diabetes mortality among persons aged 1–19 years: United States, 1979–2004. MMWR Morb Mortal Wkly Rep. 2007;56:1184–1187. [PubMed] [Google Scholar]
- 21.Preis SR, Hwang SJ, Coady S, Pencina MJ, D’Agostino RB, Sr, Savage PJ, Levy D, Fox CS. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation. 2009;119:1728–1725. doi: 10.1161/CIRCULATIONAHA.108.829176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, Engelgau MM, Saydah SH, Williams DE, Geiss LS, Gregg EW. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health and Nutrition Examination Survey 1999–2002. Diabetes Care. 2006;29:1263–1268. doi: 10.2337/dc06-0062. [DOI] [PubMed] [Google Scholar]
- 23.Fox CS, Sullivan L, D’Agostino RB, Sr, Wilson PW Framingham Heart Study. The significant effect of diabetes duration on coronary heart disease mortality: the Framingham Heart Study. Diabetes Care. 2004;27:704–708. doi: 10.2337/diacare.27.3.704. [DOI] [PubMed] [Google Scholar]
- 24.Goldstein LB, Adams R, Becker K, Furberg CD, Gorelick PB, Hademenos G, Hill M, Howard G, Howard VJ, Jacobs B, Levine SR, Mosca L, Sacco RL, Sherman DG, Wolf PA, del Zoppo GJ. Primary prevention of ischemic stroke: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke. 2001;32:280–299. doi: 10.1161/01.str.32.1.280. [DOI] [PubMed] [Google Scholar]
- 25.Kissela BM, Khoury J, Kleindorfer D, Woo D, Schneider A, Alwell K, Miller R, Ewing I, Moomaw CJ, Szaflarski JP, Gebel J, Shukla R, Broderick JP. Epidemiology of ischemic stroke in patients with diabetes: the greater Cincinnati/Northern Kentucky Stroke Study. Diabetes Care. 2005;28:355–359. doi: 10.2337/diacare.28.2.355. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC) Prevalence of self-reported cardiovascular disease among persons aged ≥35 years with diabetes: United States, 1997–2005. MMWR Morb Mortal Wkly Rep. 2007;56:1129–1132. [PubMed] [Google Scholar]
- 27.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 28.Lyerly GW, Sui X, Church TS, Lavie CJ, Hand GA, Blair SN. Maximal exercise electrocardiography responses and coronary heart disease mortality among men with diabetes mellitus. Circulation. 2008;117:2734–2742. doi: 10.1161/CIRCULATIONAHA.107.729277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Donahoe SM, Stewart GC, McCabe CH, Mohanavelu S, Murphy SA, Cannon CP, Antman EM. Diabetes and mortality following acute coronary syndromes. JAMA. 2007;298:765–775. doi: 10.1001/jama.298.7.765. [DOI] [PubMed] [Google Scholar]
- 30.Jones DW, Chambless LE, Folsom AR, Heiss G, Hutchinson RG, Sharrett AR, Szklo M, Taylor HA., Jr Risk factors for coronary heart disease in African Americans: the Atherosclerotic Risk in Communities Study, 1987–1997. Arch Intern Med. 2002;162:2565–2571. doi: 10.1001/archinte.162.22.2565. [DOI] [PubMed] [Google Scholar]
- 31.Fox CS, Coady S, Sorlie PD, Levy D, Meigs JB, D’Agostino RB, Sr, Wilson PW, Savage PJ. Trends in cardiovascular complications of diabetes. JAMA. 2004;292:2495–2499. doi: 10.1001/jama.292.20.2495. [DOI] [PubMed] [Google Scholar]
- 32.Fox CS, Coady S, Sorlie PD, D’Agostino RB, Sr, Pencina MJ, Vasan RS, Meigs JB, Levy D, Savage PJ. Increasing cardiovascular disease burden due to diabetes mellitus: the Framingham Heart Study. Circulation. 2007;115:1544–1550. doi: 10.1161/CIRCULATIONAHA.106.658948. [DOI] [PubMed] [Google Scholar]
- 33.Fox CS, Pencina MJ, Wilson PW, Paynter NP, Vasan RS, D’Agostino RB., Sr Lifetime risk of cardiovascular disease among individuals with and without diabetes stratified by obesity status in the Framingham Heart Study. Diabetes Care. 2008;31:1582–1584. doi: 10.2337/dc08-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fang J, Alderman MH. Impact of the increasing burden of diabetes on acute myocardial infarction in New York City: 1990–2000. Diabetes. 2006;55:768–773. doi: 10.2337/diabetes.55.03.06.db05-1196. [DOI] [PubMed] [Google Scholar]
- 35.Booth GL, Kapral MK, Fung K, Tu JV. Recent trends in cardiovascular complications among men and women with and without diabetes. Diabetes Care. 2006;29:32–37. doi: 10.2337/diacare.29.01.06.dc05-0776. [DOI] [PubMed] [Google Scholar]
- 36.Booth GL, Kapral MK, Fung K, Tu JV. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort study. Lancet. 2006;368:29–36. doi: 10.1016/S0140-6736(06)68967-8. [DOI] [PubMed] [Google Scholar]
- 37.American Diabetes Association. Position Statement: Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2010;33:S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Selvin E, Steffes MW, Zhu H, Matsushita K, Wagenknecht L, Pankow J, Coresh J, Brancati FL. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med. 2010;362:800–811. doi: 10.1056/NEJMoa0908359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.National Healthcare Disparities Report, 2004. Rockville, Md: Agency for Healthcare Research and Quality; 2004. [Accessed September 28, 2010]. US Department of Health and Human Services, Agency for Healthcare Research and Quality. AHRQ publication No. 05– 0014. Available at: http://www.ahrq.gov/qual/nhdr04/nhdr04.htm. [Google Scholar]
- 40.Fan T, Koro CE, Fedder DO, Bowlin SJ. Ethnic disparities and trends in glycemic control among adults with type 2 diabetes in the U.S. from 1988 to 2002. Diabetes Care. 2006;29:1924–1925. doi: 10.2337/dc05-2238. [DOI] [PubMed] [Google Scholar]
- 41.Grant RW, Cagliero E, Murphy-Sheehy P, Singer DE, Nathan DM, Meigs JB. Comparison of hyperglycemia, hypertension, and hypercholesterolemia management in patients with type 2 diabetes. Am J Med. 2002;112:603–609. doi: 10.1016/s0002-9343(02)01103-8. [DOI] [PubMed] [Google Scholar]
- 42.Wexler DJ, Grant RW, Meigs JB, Nathan DM, Cagliero E. Sex disparities in treatment of cardiac risk factors in patients with type 2 diabetes. Diabetes Care. 2005;28:514–520. doi: 10.2337/diacare.28.3.514. [DOI] [PubMed] [Google Scholar]
- 43.Malik S, Lopez V, Chen R, Wu W, Wong ND. Undertreatment of cardiovascular risk factors among persons with diabetes in the United States. Diabetes Res Clin Pract. 2007;77:126–133. doi: 10.1016/j.diabres.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 44.Mozaffarian D, Kamineni A, Carnethon M, Djoussé L, Mukamal KJ, Siscovick D. Lifestyle risk factors and new-onset diabetes mellitus in older adults: the Cardiovascular Health Study. Arch Intern Med. 2009;169:798–807. doi: 10.1001/archinternmed.2009.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Suh DC, Kim CM, Choi IS, Plauschinat CA, Barone JA. Trends in blood pressure control and treatment among type 2 diabetes with comorbid hypertension in the United States: 1988–2004. J Hypertens. 2009;27:1908–1916. doi: 10.1097/HJH.0b013e32832d4aee. [DOI] [PubMed] [Google Scholar]
- 46.Lee JM, Okumura MJ, Freed GL, Menon RK, Davis MM. Trends in hospitalizations for diabetes among children and young adults: United States, 1993–2004. Diabetes Care. 2007;30:3035–3039. doi: 10.2337/dc07-0769. [DOI] [PubMed] [Google Scholar]
- 47.American Diabetic Association. Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31:596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- 48.Zhang Y, Dall TM, Mann SE, Chen Y, Martin J, Moore V, Baldwin A, Reidel VA, Quick WW. The economic costs of undiagnosed diabetes. Popul Health Manage. 2009;12:95–101. doi: 10.1089/pop.2009.12202. [DOI] [PubMed] [Google Scholar]
17. End-Stage Renal Disease and Chronic Kidney Disease
ICD-10 N18.0. See Tables 17-1 through 17-3.
Table 17-1.
Blood Pressure and the Adjusted Risk of End-Stage Renal Disease Among 316 675 Adults Without Evidence of Baseline Kidney Disease
| JNC V BP Category | Adjusted RR (95% CI) |
|---|---|
| Optimal | 1.00 (Reference) |
| Normal, not optimal | 1.62 (1.27–2.07) |
| High normal | 1.98 (1.55–2.52) |
| Hypertension | |
| Stage 1 | 2.59 (2.07–3.25) |
| Stage 2 | 3.86 (3.00–4.96) |
| Stage 3 | 3.88 (2.82–5.34) |
| Stage 4 | 4.25 (2.63–6.86) |
JNC V indicates fifth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; RR, relative risk; CI, confidence interval.
Table 17–3.
Adjusted Hazard Ratio for Death Resulting From Any Cause, Cardiovascular Events, and Hospitalization Among 1 120 295 Ambulatory Adults According to the Estimated Glomerular Filtration Rate*
| Adjusted Hazard Ratio (95% CI) | |||
|---|---|---|---|
| Estimated GFR, mL · min−1 · 1.73 m−2 |
Death Resulting From Any Cause |
Any Cardiovascular Event |
Any Hospitalization |
| ≥60† | 1.00 | 1.00 | 1.00 |
| 45–59 | 1.2 (1.1–1.2) | 1.4 (1.4–1.5) | 1.1 (1.1–1.1) |
| 30–44 | 1.8 (1.7–1.9) | 2.0 (1.9–2.1) | 1.5 (1.5–1.5) |
| 15–29 | 3.2 (3.1–3.4) | 2.8 (2.6–2.9) | 2.1 (2.0–2.2) |
| <15 | 5.9 (5.4–6.5) | 3.4 (3.1–3.8) | 3.1 (3.0–3.3) |
GFR indicates glomerular filtration rate; CI, confidence interval.
The analyses were adjusted for age, sex, income, education, use or nonuse of dialysis, and presence or absence of prior coronary heart disease, prior chronic heart failure, prior ischemic stroke or transient ischemic attack, prior peripheral arterial disease, diabetes mellitus, hypertension, dyslipidemia, a serum albumin level of ≤3.5 g/dL, dementia, cirrhosis or chronic liver disease, chronic lung disease, documented proteinuria, and prior hospitalizations.
This group served as the reference group.
End-stage renal disease is a condition that is most commonly associated with DM and/or HBP, occurs when the kidneys are functioning at a very low level, and is currently defined as the receipt of chronic renal replacement treatment such as hemodialysis, peritoneal dialysis, or kidney transplantation. The end-stage renal disease (ESRD) population is increasing in size and cost as those with chronic kidney disease (CKD) transition to ESRD and as a result of changing practice patterns in the United States.
Data from the 2009 annual report of the US Renal Data System (USRDS) showed that in 2007, the prevalence of ESRD was 527 282, with 65% of these prevalent cases being treated with hemodialysis.1
In 2007, 110 996 new cases of ESRD were reported.1
In 2007, mortality rates for those who were receiving dialysis were 6.7 to 8.5 times greater than those of the general US population.1
In 2007, 17 513 kidney transplants were performed.2
Data from a large cohort of insured patients found that in addition to established risk factors for ESRD, lower hemoglobin levels, higher serum uric acid levels, self-reported history of nocturia, and family history of kidney disease are independent risk factors for ESRD.3
Data from a large insured population revealed that among adults with a glomerular filtration rate (GFR) >60 mL · min−1 · 1.73 m−2 and no evidence of proteinuria or hematuria at baseline, risks for ESRD increased dramatically with higher baseline BP level, and in this same patient population, BP-associated risks were greater in men than in women and in blacks than in whites4 (see Table 17-1).
Compared with white patients with similar levels of kidney function, black patients are much more likely to progress to ESRD and are on average 10 years younger when they reach ESRD.5,6
Results from a large community-based population showed that higher BMI also independently increased the risk of ESRD. The higher risk of ESRD with overweight and obesity was consistent across age, sex, and race and in the presence or absence of DM, hypertension, or known baseline kidney disease7 (see Table 17-2).
Table 17–2.
Multivariable Association Between Body Mass Index and Risk of End-Stage Renal Disease Among 320 252 Adults
| BMI, kg/m2 | Adjusted RR (95% CI) |
|---|---|
| 18.5–24.9 (Normal weight) | 1.00 (Reference) |
| 25.0–29.9 (Overweight) | 1.87 (1.64–2.14) |
| 30.0–34.9 (Class I obesity) | 3.57 (3.05–4.18) |
| 35.0–39.9 (Class II obesity) | 6.12 (4.97–7.54) |
| ≥40.0 (Extreme obesity) | 7.07 (5.37–9.31) |
BMI indicates body mass index; RR, relative risk; CI, confidence interval.
Age, Sex, Race, and Ethnicity
The median age of the population with ESRD in 2007 varied across different racial/ethnic groups: 57.1 years for blacks, 57.9 years for Native American, 59.1 years for Asians, and 60.3 years for whites.1
Treatment of ESRD is more common in men than in women.1
Blacks, Hispanics, Asian Americans, and Native Americans have significantly higher rates of ESRD than do white/Europeans. Blacks represent nearly 28% of treated patients with ESRD.1
Chronic Kidney Disease
Prevalence
CKD, defined as reduced GFR and/or excess urinary protein excretion, is a serious health condition and a worldwide public health problem. The incidence and prevalence of CKD are increasing in the United States and are associated with poor outcomes and a high cost to the US healthcare system. Controversy exists about whether CKD itself independently causes incident CVD, but it is clear that people with CKD, as well as those with ESRD, represent a population at very high risk for CVD events. In fact, individuals with CKD are more likely to die of CVD than to transition to ESRD. The USRDS estimates that by 2020, >700 000 Americans will have ESRD, with >500 000 requiring dialysis and >250 000 receiving a transplant.1
- The National Kidney Foundation (NKF) Kidney Disease Outcome Quality Initiative (K/DOQI) developed guidelines in 2002 that provided a standardized definition for CKD. Prevalence estimates may differ depending on assumptions used in obtaining estimates, including which equation is used to estimate GFR and methods for measuring proteinuria.8 The most recent US prevalence estimates of CKD, with the use of K/DOQI guidelines, come from NHANES 1999 to 2004 (NCHS) in adults ≥20 years of age9:
- —
-
—The prevalence of GFR ≥90 mL · min−1 · 1.73 m−2 with kidney damage (ie, presence of albuminuria) is 5.7%.
-
—The prevalence of stage II CKD (estimated glomerular filtration rate (eGFR), 60 to 89 mL · min−1 · 1.73 m−2 with kidney damage) is 5.4%.
-
—The prevalence of stage III CKD (eGFR, 30 to 59 mL · min−1 · 1.73 m−2) is 5.4%.
-
—The prevalence of stages IV and V CKD (eGFR <29 mL · min−1 · 1.73 m−2) is 0.4%.
Nearly 26 million people (13%) in the United States have CKD, and most are undiagnosed.11 Another 20 million are at increased risk for CKD.2
Demographics
- Using current definitions, the prevalence of CKD is higher with older age:1
-
—5.7% for those 20 to 39 years of age;
-
—5.7% for those 40 to 59 years of age; and
-
—37.8% for those ≥60 years of age.
-
—
CKD prevalence was greater among those with DM (43.7%) and hypertension (28.0%) than among those without these chronic conditions.1
The prevalence of CKD was slightly higher among Mexican Americans (18.7%) and non-Hispanic blacks (19.9%) than among non-Hispanic whites (16.1%). This disparity was most evident for those with stage I CKD; non-Hispanic whites had a CKD prevalence of 4.2% compared with prevalences among Mexican Americans and non-Hispanic blacks of 10.2% and 9.4%, respectively.9
Risk Factors
Many traditional CVD risk factors are also risk factors for CKD, including older age, male sex, hypertension, DM, smoking, and family history of CVD.
Other risk factors include systemic conditions such as autoimmune diseases, systemic infections, and drug exposure, as well as anatomically local conditions such as urinary tract infections, urinary stones, lower urinary tract obstruction, and neoplasia. Even after adjustment for these risk factors, excess CVD risk remains.12
Many clinical risk factors for CKD are the same as those for CVD.
Proteinuria is a strong independent risk factor for a decline in eGFR, regardless of DM status, and is associated with many of the same risk factors for CVD as for CKD.13,14
ESRD/CKD and CVD
- CVD is the leading cause of death among those with ESRD, although the specific cardiovascular cause of death may be more likely to be arrhythmic compared with an acute myocardial infarction, end-stage heart failure, or stroke.
Studies from a broad range of cohorts demonstrate an association between reduced eGFR and elevated risk of CVD, CVD outcomes, and all-cause death17,19–25 that appears to be largely independent of other known major CVD risk factors.
- Any degree of albuminuria, starting below the microalbuinuria cut point, has been shown to be an independent risk factor for cardiovascular events, CHF hospitalization, PAD, and all-cause death in a wide variety of cohorts.26–31
-
—A recent meta-analysis of 21 published studies of albuminuria involving 105 872 participants (730 577 person-years) from 14 studies with urine albumin/creatinine ratio (ACR) measurements and 1 128 310 participants (4 732 110 person-years) from 7 studies with urine dipstick measurements showed that excess albuminuria or proteinuria is independently associated with a higher risk of CVD and all-cause mortality.32
-
—People with both albuminuria/proteinuria and reduced eGFR are at particularly high risk for CVD, CVD outcomes, and death.33
-
—The exact reasons why CKD and ESRD increase the risk of CVD have not been completely delineated but are clearly multifactorial and likely involve pathological alterations in multiple organ systems and pathways.
-
—
Cost–ESRD
The total annual cost of treating ESRD in the United States was ≈$24 billion in 2007, representing nearly 6% of the total Medicare budget.1
The total annual cost associated with CKD has not been accurately determined to date.
Cystatin C: Kidney Function and CVD
Serum cystatin C, another marker of kidney function, has been proposed to be a more sensitive indicator of kidney function than serum creatinine and creatinine-based estimating formulas at higher levels of GFR. It is a low-molecular-weight protein produced at a constant rate by all nucleated cells and appears not to be affected significantly across age, sex, and levels of muscle mass. Cystatin C is excreted by the kidneys, filtered through the glomerulus, and nearly completely reabsorbed by proximal tubular cells.34 Several equations have been proposed using cystatin C alone and in combination with serum creatinine to estimate kidney function.35,36
All-Cause Mortality
Elevated levels of cystatin C have been shown to be associated with increased risk for all-cause mortality in studies from a broad range of cohorts.37–39
Cardiovascular Disease
Data from a large national cohort found higher values of cystatin C to be associated with prevalent stroke, angina, and MI,40 as well as higher BMI.41
Elevated cystatin C was an independent risk factor for HF,42,43 PAD events,44 clinical atherosclerosis, and subclin- ical measures of CVD in older adults,45 as well as for cardiovascular events among those with CHD.37,46
In several diverse cohorts, elevated cystatin C has been found to be associated with CVD-related mortality,39,47,48 including sudden cardiac death.49
Abbreviations Used in Chapter 17
- ACR
albumin/creatinine ratio
- BMI
body mass index
- BP
blood pressure
- CHD
coronary heart disease
- CHF
congestive heart failure
- CKD
chronic kidney disease
- CVD
cardiovascular disease
- DM
diabetes mellitus
- eGFR
estimated glomerular filtration rate
- ESRD
end-stage renal disease
- GFR
glomerular filtration rate
- HBP
high blood pressure
- HF
heart failure
- kg/m2
kilograms per square meter
- K/DOQI
Kidney Disease Outcome Quality Initiative
- mL · min−1 · 1.73 m−2
first morning urine protein/creatinine ratio
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- NHDS
National Hospital Discharge Survey
- NKF
National Kidney Foundation
- PAD
peripheral arterial disease
- RR
relative risk
- USRDS
US Renal Data System
References
- 1.United States Renal Data System. USRDS 2009 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease. Bethesda, Md: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2009. [Accessed August 1, 2010]. Available at: http://www.usrds.org/adr.htm. [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Hospitalization discharge diagnoses for kidney disease: United States, 1980–2005. MMWR Morb Mortal Wkly Rep. 2008;57:309–312. [PubMed] [Google Scholar]
- 3.Hsu CY, Iribarren C, McCulloch CE, Darbinian J, Go AS. Risk factors for end-stage renal disease: 25-year follow-up. Arch Intern Med. 2009;169:342–350. doi: 10.1001/archinternmed.2008.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsu CY, McCulloch CE, Darbinian J, Go AS, Iribarren C. Elevated blood pressure and risk of end-stage renal disease in subjects without baseline kidney disease. Arch Intern Med. 2005;165:923–928. doi: 10.1001/archinte.165.8.923. [DOI] [PubMed] [Google Scholar]
- 5.Hsu CY, Lin F, Vittinghoff E, Shlipak MG. Racial differences in the progression from chronic renal insufficiency to end-stage renal disease in the United States. J Am Soc Nephrol. 2003;14:2902–2907. doi: 10.1097/01.asn.0000091586.46532.b4. [DOI] [PubMed] [Google Scholar]
- 6.Choi AI, Rodriguez RA, Bacchetti P, Bertenthal D, O’Hare AM. White/black racial differences in risk of end-stage renal disease and death. Am J Med. 2009;122:672–678. doi: 10.1016/j.amjmed.2008.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsu CY, McCulloch CE, Iribarren C, Darbinian J, Go AS. Body mass index and risk for end-stage renal disease. Ann Intern Med. 2006;144:21–28. doi: 10.7326/0003-4819-144-1-200601030-00006. [DOI] [PubMed] [Google Scholar]
- 8.Snyder JJ, Foley RN, Collins AJ. Prevalence of CKD in the United States: a sensitivity analysis using the National Health and Nutrition Examination Survey (NHANES) 1999–2004. Am J Kidney Dis. 2009;53:218–228. doi: 10.1053/j.ajkd.2008.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC) Prevalence of chronic kidney disease and associated risk factors: United States, 1999–2004. MMWR Morb Mortal Wkly Rep. 2007;56:161–165. [PubMed] [Google Scholar]
- 10.Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G National Kidney Foundation. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139:137–147. doi: 10.7326/0003-4819-139-2-200307150-00013. [published correction appears in Ann Intern Med. 2003;139:605]. [DOI] [PubMed] [Google Scholar]
- 11.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 12.Coresh J, Astor B, Sarnak MJ. Evidence for increased cardiovascular disease risk in patients with chronic kidney disease. Curr Opin Nephrol Hypertens. 2004;13:73–81. doi: 10.1097/00041552-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Sarnak MJ, Coronado BE, Greene T, Wang SR, Kusek JW, Beck GJ, Levey AS. Cardiovascular disease risk factors in chronic renal insufficiency. Clin Nephrol. 2002;57:327–335. doi: 10.5414/cnp57327. [DOI] [PubMed] [Google Scholar]
- 14.Bianchi S, Bigazzi R, Campese VM. Microalbuminuria in essential hypertension: significance, pathophysiology, and therapeutic implications. Am J Kidney Dis. 1999;34:973–995. doi: 10.1016/S0272-6386(99)70002-8. [DOI] [PubMed] [Google Scholar]
- 15.Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, McCullough PA, Kasiske BL, Kelepouris E, Klag MJ, Parfrey P, Pfeffer M, Raij L, Spinosa DJ, Wilson PW. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108:2154–2169. doi: 10.1161/01.CIR.0000095676.90936.80. [DOI] [PubMed] [Google Scholar]
- 16.Weiner DE, Tabatabai S, Tighiouart H, Elsayed E, Bansal N, Griffith J, Salem DN, Levey AS, Sarnak MJ. Cardiovascular outcomes and all-cause mortality: exploring the interaction between CKD and cardiovascular disease. Am J Kidney Dis. 2006;48:392–401. doi: 10.1053/j.ajkd.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 17.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 18.Weiner DE, Tighiouart H, Stark PC, Amin MG, MacLeod B, Griffith JL, Salem DN, Levey AS, Sarnak MJ. Kidney disease as a risk factor for recurrent cardiovascular disease and mortality. Am J Kidney Dis. 2004;44:198–206. doi: 10.1053/j.ajkd.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 19.Mann JF, Gerstein HC, Pogue J, Bosch J, Yusuf S. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: the HOPE randomized trial. Ann Intern Med. 2001;134:629–636. doi: 10.7326/0003-4819-134-8-200104170-00007. [DOI] [PubMed] [Google Scholar]
- 20.Fried LF, Shlipak MG, Crump C, Bleyer AJ, Gottdiener JS, Kronmal RA, Kuller LH, Newman AB. Renal insufficiency as a predictor of cardiovascular outcomes and mortality in elderly individuals. J Am Coll Cardiol. 2003;41:1364–1372. doi: 10.1016/s0735-1097(03)00163-3. [DOI] [PubMed] [Google Scholar]
- 21.Shlipak MG, Fried LF, Cushman M, Manolio TA, Peterson D, Stehman-Breen C, Bleyer A, Newman A, Siscovick D, Psaty B. Cardiovascular mortality risk in chronic kidney disease: comparison of traditional and novel risk factors. JAMA. 2005;293:1737–1745. doi: 10.1001/jama.293.14.1737. [DOI] [PubMed] [Google Scholar]
- 22.Ruilope LM, Salvetti A, Jamerson K, Hansson L, Warnold I, Wedel H, Zanchetti A. Renal function and intensive lowering of blood pressure in hypertensive participants of the Hypertension Optimal Treatment (HOT) study. J Am Soc Nephrol. 2001;12:218–225. doi: 10.1681/ASN.V122218. [DOI] [PubMed] [Google Scholar]
- 23.Manjunath G, Tighiouart H, Ibrahim H, MacLeod B, Salem DN, Griffith JL, Coresh J, Levey AS, Sarnak MJ. Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol. 2003;41:47–55. doi: 10.1016/s0735-1097(02)02663-3. [DOI] [PubMed] [Google Scholar]
- 24.Hailpern SM, Cohen HW, Alderman MH. Renal dysfunction and ischemic heart disease mortality in hypertensive population. J Hypertens. 2005;23:1809–1816. doi: 10.1097/01.hjh.0000183120.92455.2a. [DOI] [PubMed] [Google Scholar]
- 25.Culleton BF, Larson MG, Wilson PW, Evans JC, Parfrey PS, Levy D. Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int. 1999;56:2214–2219. doi: 10.1046/j.1523-1755.1999.00773.x. [DOI] [PubMed] [Google Scholar]
- 26.Arnlöv J, Evans JC, Meigs JB, Wang TJ, Fox CS, Levy D, Benjamin EJ, D’Agostino RB, Vasan RS. Low-grade albuminuria and incidence of cardiovascular disease events in nonhypertensive and nondiabetic individuals: the Framingham Heart Study. Circulation. 2005;112:969–975. doi: 10.1161/CIRCULATIONAHA.105.538132. [DOI] [PubMed] [Google Scholar]
- 27.Klausen K, Borch-Johnsen K, Feldt-Rasmussen B, Jensen G, Clausen P, Scharling H, Appleyard M, Jensen JS. Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension, and diabetes. Circulation. 2004;110:32–35. doi: 10.1161/01.CIR.0000133312.96477.48. [DOI] [PubMed] [Google Scholar]
- 28.Gerstein HC, Mann JF, Yi Q, Zinman B, Dinneen SF, Hoogwerf B, Hallé JP, Young J, Rashkow A, Joyce C, Nawaz S, Yusuf S HOPE Study Investigators. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA. 2001;286:421–426. doi: 10.1001/jama.286.4.421. [DOI] [PubMed] [Google Scholar]
- 29.Yuyun MF, Adler AI, Wareham NJ. What is the evidence that microalbuminuria is a predictor of cardiovascular disease events? Curr Opin Nephrol Hypertens. 2005;14:271–276. doi: 10.1097/01.mnh.0000165895.90748.3b. [DOI] [PubMed] [Google Scholar]
- 30.Wattanakit K, Folsom AR, Criqui MH, Kramer HJ, Cushman M, Shea S, Hirsch AT. Albuminuria and peripheral arterial disease: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Atherosclerosis. 2008;201:212–216. doi: 10.1016/j.atherosclerosis.2007.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brantsma AH, Bakker SJ, Hillege HL, de Zeeuw D, de Jong PE, Gansevoort RT PREVEND Study Group. Cardiovascular and renal outcome in subjects with K/DOQI stage 1–3 chronic kidney disease: the importance of urinary albumin excretion. Nephrol Dial Transplant. 2008;23:3851–3858. doi: 10.1093/ndt/gfn356. [DOI] [PubMed] [Google Scholar]
- 32.Chronic Kidney Disease Prognosis Consortium. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375:2073–2081. doi: 10.1016/S0140-6736(10)60674-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hemmelgarn BR, Manns BJ, Lloyd A, James MT, Klarenbach S, Quinn RR, Wiebe N, Tonelli M. Relation between kidney function, proteinuria, and adverse outcomes. JAMA. 2010;303:423–429. doi: 10.1001/jama.2010.39. [DOI] [PubMed] [Google Scholar]
- 34.Filler G, Bokenkamp A, Hofmann W, Le Bricon T, Martínez-Brú C, Grubb A. Cystatin C as a marker of GFR: history, indications, and future research. Clin Biochem. 2005;38:1–8. doi: 10.1016/j.clinbiochem.2004.09.025. [DOI] [PubMed] [Google Scholar]
- 35.Stevens LA, Coresh J, Schmid CH, Feldman HI, Froissart M, Kusek J, Rossert J, Van Lente F, Bruce RD, III, Zhang YL, Greene T, Levey AS. Estimating GFR using serum cystatin C alone and in combination with serum creatinine: a pooled analysis of 3,418 individuals with CKD. Am J Kidney Dis. 2008;51:395–406. doi: 10.1053/j.ajkd.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20:629–637. doi: 10.1681/ASN.2008030287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ix JH, Shlipak MG, Chertow GM, Whooley MA. Association of cystatin C with mortality, cardiovascular events, and incident heart failure among persons with coronary heart disease: data from the Heart and Soul Study. Circulation. 2007;115:173–179. doi: 10.1161/CIRCULATIONAHA.106.644286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fried LF, Katz R, Sarnak MJ, Shlipak MG, Chaves PH, Jenny NS, Stehman-Breen C, Gillen D, Bleyer AJ, Hirsch C, Siscovick D, Newman AB. Kidney function as a predictor of noncardiovascular mortality. J Am Soc Nephrol. 2005;16:3728–3735. doi: 10.1681/ASN.2005040384. [DOI] [PubMed] [Google Scholar]
- 39.Shlipak MG, Wassel Fyr CL, Chertow GM, Harris TB, Kritchevsky SB, Tylavsky FA, Satterfield S, Cummings SR, Newman AB, Fried LF. Cystatin C and mortality risk in the elderly: the Health, Aging, and Body Composition Study. J Am Soc Nephrol. 2006;17:254–261. doi: 10.1681/ASN.2005050545. [DOI] [PubMed] [Google Scholar]
- 40.Muntner P, Mann D, Winston J, Bansilal S, Farkouh ME. Serum cystatin C and increased coronary heart disease prevalence in US adults without chronic kidney disease. Am J Cardiol. 2008;102:54–57. doi: 10.1016/j.amjcard.2008.02.098. [DOI] [PubMed] [Google Scholar]
- 41.Muntner P, Winston J, Uribarri J, Mann D, Fox CS. Overweight, obesity, and elevated serum cystatin C levels in adults in the United States. Am J Med. 2008;121:341–348. doi: 10.1016/j.amjmed.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Djoussé L, Kurth T, Gaziano JM. Cystatin C and risk of heart failure in the Physicians’ Health Study (PHS) Am Heart J. 2008;155:82–86. doi: 10.1016/j.ahj.2007.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sarnak MJ, Katz R, Stehman-Breen CO, Fried LF, Jenny NS, Psaty BM, Newman AB, Siscovick D, Shlipak MG Cardiovascular Health Study. Cystatin C concentration as a risk factor for heart failure in older adults. Ann Intern Med. 2005;142:497–505. doi: 10.7326/0003-4819-142-7-200504050-00008. [DOI] [PubMed] [Google Scholar]
- 44.O’Hare AM, Newman AB, Katz R, Fried LF, Stehman-Breen CO, Seliger SL, Siscovick DS, Shlipak MG. Cystatin C and incident peripheral arterial disease events in the elderly: results from the Cardiovascular Health Study. Arch Intern Med. 2005;165:2666–2670. doi: 10.1001/archinte.165.22.2666. [DOI] [PubMed] [Google Scholar]
- 45.Shlipak MG, Katz R, Kestenbaum B, Fried LF, Siscovick D, Sarnak MJ. Clinical and subclinical cardiovascular disease and kidney function decline in the elderly. Atherosclerosis. 2009;204:298–303. doi: 10.1016/j.atherosclerosis.2008.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koenig W, Twardella D, Brenner H, Rothenbacher D. Plasma concentrations of cystatin C in patients with coronary heart disease and risk for secondary cardiovascular events: more than simply a marker of glomerular filtration rate. Clin Chem. 2005;51:321–327. doi: 10.1373/clinchem.2004.041889. [DOI] [PubMed] [Google Scholar]
- 47.Keller T, Messow CM, Lubos E, Nicaud V, Wild PS, Rupprecht HJ, Bickel C, Tzikas S, Peetz D, Lackner KJ, Tiret L, Münzel TF, Blankenberg S, Schnabel RB. Cystatin C and cardiovascular mortality in patients with coronary artery disease and normal or mildly reduced kidney function: results from the AtheroGene study. Eur Heart J. 2009;30:314–320. doi: 10.1093/eurheartj/ehn598. [DOI] [PubMed] [Google Scholar]
- 48.Deo R, Fyr CL, Fried LF, Newman AB, Harris TB, Angleman S, Green C, Kritchevsky SB, Chertow GM, Cummings SR, Shlipak MG Health ABC Study. Kidney dysfunction and fatal cardiovascular disease: an association independent of atherosclerotic events: results from the Health, Aging, and Body Composition (Health ABC) study. Am Heart J. 2008;155:62–68. doi: 10.1016/j.ahj.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 49.Deo R, Sotoodehnia N, Katz R, Sarnak MJ, Fried LF, Chonchol M, Kestenbaum B, Psaty BM, Siscovick DS, Shlipak MG. Cystatin C and sudden cardiac death risk in the elderly. Circ Cardiovasc Qual Outcomes. 2010;3:159–164. doi: 10.1161/CIRCOUTCOMES.109.875369. [DOI] [PMC free article] [PubMed] [Google Scholar]
18. Metabolic Syndrome
- Metabolic syndrome refers to a cluster of risk factors for CVD and type 2 DM. Although several different definitions for metabolic syndrome have been proposed, the International Diabetes Federation, NHLBI, AHA, and others recently proposed a harmonized definition for metabolic syndrome.1 By this definition, metabolic syndrome is diagnosed when ≥3 of the following 5 risk factors are present:
-
—Fasting plasma glucose ≥100 mg/dL or undergoing drug treatment for elevated glucose.
-
—HDL cholesterol <40 mg/dL in men or <50 mg/dL in women or undergoing drug treatment for reduced HDL cholesterol.
-
—Triglycerides ≥150 mg/dL or undergoing drug treatment for elevated triglycerides.
-
—Waist circumference ≥102 cm in men or ≥88 cm in women in the United States.
-
—BP ≥130 mm Hg systolic or ≥85 mm Hg diastolic or undergoing drug treatment for hypertension or antihypertensive drug treatment in a patient with a history of hypertension.
-
—
Adults
Prevalence of metabolic syndrome varies by the definition used, with definitions such as the International Diabetes Federation that suggest lower thresholds for defining central obesity resulting in higher prevalence estimates.2
On the basis of NHANES 2003 to 2006 data and National Cholesterol Education Program (NCEP)/ATP III guidelines, ≈34% of adults ≥20 years of age met the criteria for metabolic syndrome.3
- Also based on NHANES 2003 to 2006 data3:
-
—The age-adjusted prevalence was 35.1% for men and 32.6% for women.
-
—Among men, the age-specific prevalence ranged from 20.3% among people 20 to 39 years of age to 40.8% for people 40 to 59 years of age and 51.5% for people ≥60 years of age. Among women, the age-specific prevalence ranged from 15.6% among people 20 to 39 years of age to 37.2% for people 40 to 59 years of age and 54.4% for those ≥60 years of age.
-
—The age-adjusted prevalences of people with metabolic syndrome were 37.2%, 25.3%, and 33.2% for non-Hispanic white, non-Hispanic black, and Mexican American men, respectively. Among women, the percentages were 31.5%, 38.8%, and 40.6%, respectively.
-
—The age-adjusted prevalence was ≈53% higher among non-Hispanic black women than among non-Hispanic black men and ≈22% higher among Mexican American women than among Mexican American men.
-
—
The prevalence of metabolic syndrome is also high among immigrant Asian Indians, ranging between 26.8% and 38.2%, depending on the definition used.4
The prevalence of metabolic syndrome among pregnant women increased to 26.5% during 1999 to 2004 from 17.8% during 1988 to 1994.5
However, the public’s recognition of metabolic syndrome is limited.6
Children/Adolescents
An AHA scientific statement about metabolic syndrome in children and adolescents was released in 2009.7
Metabolic syndrome should be diagnosed with caution in children and adolescents because metabolic syndrome categorization in adolescents is not stable. Approximately half of the 1098 adolescent participants in the Princeton School District Study diagnosed with pediatric ATP III metabolic syndrome lost the diagnosis over 3 years of follow-up.8
Additional evidence of the instability of the diagnosis of metabolic syndrome in children exists. In children 6 to 17 years of age participating in research studies in a single clinical research hospital, the diagnosis of metabolic syndrome was unstable in 46% of cases after a mean of 5.6 years of follow-up.9
On the basis of NHANES 1999 to 2002 data, the prevalence of metabolic syndrome in adolescents 12 to 19 years of age was 9.4%, which represents ≈2.9 million people. It was 13.2% in boys, 5.3% in girls, 10.7% in whites, 5.2% in blacks, and 11.1% in Mexican Americans.10
In 1999 to 2004, ≈4.5% of US adolescents 12 to 17 years of age had metabolic syndrome according to the definition developed by the International Diabetes Federation.11 In 2006, this prevalence would have represented ≈1.1 million adolescents 12 to 17 years of age with metabolic syndrome. It increased from 1.2% among those 12 to 13 years of age to 7.1% among those 14 to 15 years of age and was higher among boys (6.7%) than girls (2.1%). Furthermore, 4.5% of white adolescents, 3.0% of black adolescents, and 7.1% of Mexican American adolescents had metabolic syndrome. The prevalence of metabolic syndrome remained relatively stable during successive 2-year periods: 4.5% for 1999 to 2000, 4.4% to 4.5% for 2001 to 2002, and 3.7% to 3.9% for 2003 to 2004.
In 1999 to 2002, among overweight or obese adolescents, 44% had metabolic syndrome.10 In 1988 to 1994, two thirds of all adolescents had at least 1 metabolic abnormality.12
Of 31 participants in the NHLBI Lipid Research Clinics Princeton Prevalence Study and the Princeton Follow-Up Study who had metabolic syndrome at baseline, 21 (68%) had metabolic syndrome 25 years later.13 After adjustment for age, sex, and race, the baseline status of metabolic syndrome was significantly associated with an increased risk of having metabolic syndrome during adulthood (OR, 6.2; 95% CI, 2.8 to 13.8).
In the Bogalusa Heart Study, 4 variables (BMI, homeostasis model assessment of insulin resistance, ratio of triglycerides to HDL cholesterol, and mean arterial pressure) considered to be part of the metabolic syndrome clustered together in blacks and whites and in children and adults.14 The degree of clustering was stronger among adults than children. The clustering of rates of change in the components of the metabolic syndrome in blacks exceeded that in whites.
Cardiovascular abnormalities are associated with metabolic syndrome in children and adolescents.15,16
Risk
Adults
Consistent with 2 earlier meta-analyses, a recent meta-analysis of prospective studies concluded that metabolic syndrome increased the risk of developing CVD (summary RR, 1.78; 95% CI, 1.58 to 2.00).17 The risk of CVD tended to be higher in women (summary RR, 2.63) than in men (summary RR, 1.98; P=0.09). On the basis of results from 3 studies, metabolic syndrome remained a predictor of cardiovascular events after adjustment for the individual components of the syndrome (summary RR, 1.54; 95% CI, 1.32 to 1.79).
Several studies suggest that the FRS is a better predictor of incident CVD than metabolic syndrome.18–20 In the San Antonio Heart Study, the area under the receiver-operating characteristic curve (aROC) was 0.816 for the FRS and 0.811 for the FRS plus the metabolic syndrome.18 Furthermore, the sensitivity for CVD at a fixed specificity was significantly higher for the FRS than for the metabolic syndrome. In ARIC, metabolic syndrome did not improve the risk prediction achieved by the FRS.19 In the British Regional Heart Study, the aROC for the FRS was 0.73 for incident CHD during 10 years of follow-up, and the aROC for the number of metabolic syndrome components was 0.63.20 For CHD events during 20 years of follow-up, the aROCs were 0.68 for the FRS and 0.59 for the number of metabolic syndrome components.
Estimates of relative risk for CVD generally increase as the number of components of metabolic syndrome increases.20,21 Compared with men without an abnormal component in the Framingham Offspring Study, the HRs for CVD were 1.48 (95% CI, 0.69 to 3.16) for men with 1 or 2 components and 3.99 (95% CI, 1.89 to 8.41) for men with ≥3 components.21 Among women, the HRs were 3.39 (95% CI, 1.31 to 8.81) for 1 or 2 components and 5.95 (95% CI, 2.20 to 16.11) for ≥3 components. Compared with men without a metabolic abnormality in the British Regional Heart Study, the HRs were 1.74 (95% CI, 1.22 to 2.39) for 1 component, 2.34 (95% CI, 1.65 to 3.32) for 2 components, 2.88 (95% CI, 2.02 to 4.11) for 3 components, and 3.44 (95% CI, 2.35 to 5.03) for 4 or 5 components.20
The cardiovascular risk associated with the metabolic syndrome varies on the basis of the combination of metabolic syndrome components present. Of all possible ways to have 3 metabolic syndrome components, the combination of central obesity, elevated BP, and hyperglycemia had the greatest risk for CVD (HR, 2.36; 95% CI, 1.54 to 3.61) and mortality (HR, 3.09; 95% CI, 1.93 to 4.94) in the Framingham Offspring Study.22
Data from the Aerobics Center Longitudinal Study indicate that risk for CVD mortality is increased in men without DM who have metabolic syndrome (HR, 1.8; 95% CI, 1.5 to 2.0). However, among those with metabolic syndrome, the presence of DM is associated with even greater risk for CVD mortality (HR, 2.1; 95% CI, 1.7 to 2.6).23
Analysis of data from NCHS was used to determine the number of disease-specific deaths attributable to all non-optimal levels of each risk factor exposure by age and sex. The results of the analysis of dietary, lifestyle, and metabolic risk factors show that targeting a handful of risk factors has large potential to reduce mortality in the United States.24
In addition to CVD, the metabolic syndrome has also been associated with incident atrial fibrillation25 and HF.26
The metabolic syndrome is associated with increased healthcare use and healthcare–related costs among individuals with and without DM. Overall, healthcare costs increase by ≈24% for each additional metabolic syndrome component present.27
Children
Few prospective pediatric studies have examined the future risk for CVD or DM according to baseline metabolic syndrome status. Data from 771 participants 6 to 19 years of age from the NHLBI’s Lipid Research Clinics Princeton Prevalence Study and the Princeton Follow-Up Study showed that the risk of developing CVD was substantially higher among those with metabolic syndrome than among those without this syndrome (OR, 14.6; 95% CI, 4.8 to 45.3) who were followed up for 25 years.13
Another analysis of 814 participants of this cohort showed that those 5 to 19 years of age who had metabolic syndrome at baseline had an increased risk of having DM 25 to 30 years later compared with those who did not have the syndrome at baseline (OR, 11.5; 95% CI, 2.1 to 63.7).28
Additional data from the Princeton Follow-Up Study, the Fels Longitudinal Study, and the Muscatine Study suggest that the absence of components of the metabolic syndrome in childhood had a high negative predictive value for the development of metabolic syndrome or DM in adulthood.29
Risk Factors
In prospective or retrospective cohort studies, the following factors have been reported as being directly associated with incident metabolic syndrome, defined by one of the major definitions: age,28,30–32 low educational attainment,30,33 low socioeconomic status,34 smoking,33–36 low levels of PA,33–39 low levels of physical fitness,37,40–42 intake of soft drinks,43 intake of diet soda,44 magnesium intake,45 energy intake,39 carbohydrate intake,30,35,46 total fat intake,30,46 Western dietary pattern,44 meat intake,44 intake of fried foods,44 heavy alcohol consumption,47 abstention from alcohol use,30 parental history of DM,28 long-term stress at work,48 pediatric metabolic syndrome,28 obesity or BMI,30,31,35,39,49 childhood obesity,50 waist circumference,32,46,51–54 intra-abdominal fat,55 gain in weight or BMI,30,56 change in weight or BMI,32,35,57 weight fluctuation,58 BP,32,46,53,59 heart rate,60 homeostasis model assessment,51,61 fasting insulin,51 2-hour insulin,51 proinsulin,51 fasting glucose or hyperglycemia,32,51,53 2-hour glucose,51 impaired glucose tolerance,51 triglycerides,32,46,49,51–53 low HDL cholesterol,32,46,50,51,53 oxidized LDL,61 uric acid,57,62 γ–glutamyltransferase,57,63,64 alanine transaminase,57,63,65,66 plasminogen activator inhibitor-1,67 aldosterone,67 leptin,68 C-reactive protein,69,70 adipocyte–fatty acid binding protein,71 and free testosterone index.72
The following factors have been reported as being inversely associated with incident metabolic syndrome, defined by one of the major definitions, in prospective or retrospective cohort studies: muscular strength,73 change in PA or physical fitness,35,40 alcohol intake,33,39 Mediterranean diet,74 dairy consumption,44 insulin sensitivity,51 ratio of aspartate aminotransferase to alanine transaminase,65 total testosterone,72,75,76 sex hormone– binding globulin,72,75,76 and Δ5-desaturase activity.77
Furthermore, men were more likely than women to develop metabolic syndrome,30,32 and blacks were shown to be less likely to develop metabolic syndrome than whites.30
Abbreviations Used in Chapter 18
- AHA
American Heart Association
- ARIC
Atherosclerosis Risk in Communities
- aROC
area under the receiver-operating characteristic curve
- ATP III
Adult Treatment Panel III
- BMI
body mass index
- BP
blood pressure
- CHD
coronary heart disease
- CI
confidence interval
- cm
centimeter
- CVD
cardiovascular disease
- DM
diabetes mellitus
- FRS
Framingham Risk Score
- HDL
high-density lipoprotein
- HR
hazard ratio
- HF
heart failure
- mg/dL
milligrams per deciliter
- mm Hg
millimeters of mercury
- NCEP
National Cholesterol Education Program
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- NHLBI
National Heart, Lung, and Blood Institute
- OR
odds ratio
- PA
physical activity
- RR
relative risk
References
- 1.Alberti K, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WPT, Loria CM, Smith SC., Jr Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 2.Brown TM, Voeks JH, Bittner V, Safford MM. Variations in prevalent cardiovascular disease and future risk by metabolic syndrome classification in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. Am Heart J. 2010;159:385–391. doi: 10.1016/j.ahj.2009.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ervin RB. National Health Statistics Reports; No. 13. Hyattsville, Md: National Center for Health Statistics; 2009. [Accessed September 28, 2010]. Prevalence of metabolic syndrome among adults 20 years of age and over by sex age, race and ethnicity, and body mass index: United States, 2003–2006. Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr013.pdf. [PubMed] [Google Scholar]
- 4.Misra R, Patel T, Kotha P, Raji A, Ganda O, Banerji MA, Shah V, Vijay K, Mudaliar S, Iyer D. Prevalence of diabetes, metabolic syndrome, and cardiovascular risk factors in US Asian Indians: results from a national study. J Diabetes Complications. 2009;24:145–153. doi: 10.1016/j.jdiacomp.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Ramos RG, Olden K. The prevalence of metabolic syndrome among US women of childbearing age. Am J Public Health. 2008;98:1122–1127. doi: 10.2105/AJPH.2007.120055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewis SJ, Rodbard HW, Fox KM, Grandy S SHIELD Study Group. Self-reported prevalence and awareness of metabolic syndrome: findings from SHIELD. Int J Clin Pract. 2008;62:1168–1176. doi: 10.1111/j.1742-1241.2008.01770.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steinberger J, Daniels SR, Eckel RH, Hayman L, Lustig RH, McCrindle B, Mietus-Snyder ML. Progress and challenges in metabolic syndrome in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young, Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing; and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2009;119:628–647. doi: 10.1161/CIRCULATIONAHA.108.191394. [DOI] [PubMed] [Google Scholar]
- 8.Goodman E, Daniels SR, Meigs JB, Dolan LM. Instability in the diagnosis of metabolic syndrome in adolescents. Circulation. 2007;115:2316–2322. doi: 10.1161/CIRCULATIONAHA.106.669994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gustafson JK, Yanoff LB, Easter BD, Brady SM, Keil MF, Roberts MD, Sebring NG, Han JC, Yanovski SZ, Hubbard VS. The stability of metabolic syndrome in children and adolescents. J Clin Endocrinol Metab. 2009;94:4828–4834. doi: 10.1210/jc.2008-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cook S, Auinger P, Li C, Ford ES. Metabolic syndrome rates in United States adolescents, from the National Health and Nutrition Examination Survey, 1999–2002. J Pediatr. 2008;152:165–170. doi: 10.1016/j.jpeds.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Ford ES, Li C, Zhao G, Pearson WS, Mokdad AH. Prevalence of metabolic syndrome among U.S. adolescents using the definition from the International Diabetes Federation. Diabetes Care. 2008;31:587–589. doi: 10.2337/dc07-1030. [DOI] [PubMed] [Google Scholar]
- 12.de Ferranti SD, Gauvreau K, Ludwig DS, Neufeld EJ, Newburger JW, Rifai N. Prevalence of the metabolic syndrome in American adolescents: findings from the Third National Health and Nutrition Examination Survey. Circulation. 2004;110:2494–2497. doi: 10.1161/01.CIR.0000145117.40114.C7. [DOI] [PubMed] [Google Scholar]
- 13.Morrison JA, Friedman LA, Gray-McGuire C. Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: the Princeton Lipid Research Clinics Follow-Up Study. Pediatrics. 2007;120:340–345. doi: 10.1542/peds.2006-1699. [DOI] [PubMed] [Google Scholar]
- 14.Chen W, Srinivasan SR, Li S, Xu J, Berenson GS. Clustering of long-term trends in metabolic syndrome variables from childhood to adulthood in blacks and whites: the Bogalusa Heart Study. Am J Epidemiol. 2007;166:527–533. doi: 10.1093/aje/kwm105. [DOI] [PubMed] [Google Scholar]
- 15.Chinali M, de Simone G, Roman MJ, Best LG, Lee ET, Russell M, Howard BV, Devereux RB. Cardiac markers of pre-clinical disease in adolescents with the metabolic syndrome: the Strong Heart Study. J Am Coll Cardiol. 2008;52:932–938. doi: 10.1016/j.jacc.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Toledo-Corral CM, Ventura EE, Hodis HN, Weigensberg MJ, Lane CJ, Li Y, Goran MI. Persistence of the metabolic syndrome and its influence on carotid artery intima media thickness in overweight Latino children. Atherosclerosis. 2009;206:594–598. doi: 10.1016/j.atherosclerosis.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–414. doi: 10.1016/j.jacc.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 18.Stern MP, Williams K, González-Villalpando C, Hunt KJ, Haffner SM. Does the metabolic syndrome improve identification of individuals at risk of type 2 diabetes and/or cardiovascular disease [published correction appears in Diabetes Care. 2005;28:238]? Diabetes Care. 2004;27:2676–2681. doi: 10.2337/diacare.27.11.2676. [DOI] [PubMed] [Google Scholar]
- 19.McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, Ballantyne CM, Heiss G. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the Atherosclerosis Risk in Communities study. Diabetes Care. 2005;28:385–390. doi: 10.2337/diacare.28.2.385. [DOI] [PubMed] [Google Scholar]
- 20.Wannamethee SG, Shaper AG, Lennon L, Morris RW. Metabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med. 2005;165:2644–2650. doi: 10.1001/archinte.165.22.2644. [DOI] [PubMed] [Google Scholar]
- 21.Wilson PW, D’Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066–3072. doi: 10.1161/CIRCULATIONAHA.105.539528. [DOI] [PubMed] [Google Scholar]
- 22.Franco OH, Massaro JM, Civil J, Cobain MR, O’Malley B, D’Agostino RB., Sr Trajectories of entering the metabolic syndrome: the Framingham Heart Study. Circulation. 2009;120:1943–1950. doi: 10.1161/CIRCULATIONAHA.109.855817. [DOI] [PubMed] [Google Scholar]
- 23.Church TS, Thompson AM, Katzmarzyk PT, Sui X, Johannsen N, Earnest CP, Blair SN. Metabolic syndrome and diabetes, alone and in combination, as predictors of cardiovascular disease mortality among men. Diabetes Care. 2009;32:1289–1294. doi: 10.2337/dc08-1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJL, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chamberlain AM, Agarwal SK, Ambrose M, Folsom AR, Soliman EZ, Alonso A. Metabolic syndrome and incidence of atrial fibrillation among blacks and whites in the Atherosclerosis Risk in Communities (ARIC) Study. Am Heart J. 2010;159:850–856. doi: 10.1016/j.ahj.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Horwich TB, Fonarow GC. Glucose, obesity, metabolic syndrome, and diabetes: relevance to incidence of heart failure. J Am Coll Cardiol. 2010;55:283–293. doi: 10.1016/j.jacc.2009.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boudreau DM, Malone DC, Raebel MA, Fishman PA, Nichols GA, Feldstein AC, Boscoe AN, Ben-Joseph RH, Magid DJ, Okamoto LJ. Health care utilization and costs by metabolic syndrome risk factors. Metab Syndr Relat Disord. 2009;7:305–314. doi: 10.1089/met.2008.0070. [DOI] [PubMed] [Google Scholar]
- 28.Morrison JA, Friedman LA, Wang P, Glueck CJ. Metabolic syndrome in childhood predicts adult metabolic syndrome and type 2 diabetes mellitus 25 to 30 years later. J Pediatr. 2008;152:201–206. doi: 10.1016/j.jpeds.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 29.Schubert CM, Sun SS, Burns TL, Morrison JA, Huang TTK. Predictive ability of childhood metabolic components for adult metabolic syndrome and type 2 diabetes. J Pediatr. 2009;155:S6.e1–S6.e7. doi: 10.1016/j.jpeds.2009.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carnethon MR, Loria CM, Hill JO, Sidney S, Savage PJ, Liu K Coronary Artery Risk Development in Young Adults Study. Risk factors for the metabolic syndrome: the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1985–2001. Diabetes Care. 2004;27:2707–2715. doi: 10.2337/diacare.27.11.2707. [DOI] [PubMed] [Google Scholar]
- 31.Albareda M, Caballero A, Badell G, Rodríguez-Espinosa J, Ordóñez-Llanos J, de Leiva A, Corcoy R. Metabolic syndrome at follow-up in women with and without gestational diabetes mellitus in index pregnancy. Metabolism. 2005;54:1115–1121. doi: 10.1016/j.metabol.2005.03.017. [DOI] [PubMed] [Google Scholar]
- 32.Cheung BM, Wat NM, Tam S, Thomas GN, Leung GM, Cheng CH, Woo J, Janus ED, Lau CP, Lam TH, Lam KS. Components of the metabolic syndrome predictive of its development: a 6-year longitudinal study in Hong Kong Chinese. Clin Endocrinol (Oxf) 2008;68:730–737. doi: 10.1111/j.1365-2265.2007.03110.x. [DOI] [PubMed] [Google Scholar]
- 33.Wilsgaard T, Jacobsen BK. Lifestyle factors and incident metabolic syndrome: the Tromsø Study 1979–2001. Diabetes Res Clin Pract. 2007;78:217–224. doi: 10.1016/j.diabres.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 34.Chichlowska KL, Rose KM, Diez-Roux AV, Golden SH, McNeill AM, Heiss G. Life course socioeconomic conditions and metabolic syndrome in adults: the Atherosclerosis Risk in Communities (ARIC) Study. Ann Epidemiol. 2009;19:875–883. doi: 10.1016/j.annepidem.2009.07.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wannamethee SG, Shaper AG, Whincup PH. Modifiable lifestyle factors and the metabolic syndrome in older men: effects of lifestyle changes. J Am Geriatr Soc. 2006;54:1909–1914. doi: 10.1111/j.1532-5415.2006.00974.x. [DOI] [PubMed] [Google Scholar]
- 36.Holme I, Tonstad S, Sogaard AJ, Larsen PG, Haheim LL. Leisure time physical activity in middle age predicts the metabolic syndrome in old age: results of a 28-year follow-up of men in the Oslo study. BMC Public Health. 2007;7:154. doi: 10.1186/1471-2458-7-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Laaksonen DE, Lakka HM, Salonen JT, Niskanen LK, Rauramaa R, Lakka TA. Low levels of leisure-time physical activity and cardiorespiratory fitness predict development of the metabolic syndrome. Diabetes Care. 2002;25:1612–1618. doi: 10.2337/diacare.25.9.1612. [DOI] [PubMed] [Google Scholar]
- 38.Ekelund U, Brage S, Franks PW, Hennings S, Emms S, Wareham NJ. Physical activity energy expenditure predicts progression toward the metabolic syndrome independently of aerobic fitness in middle-aged healthy Caucasians: the Medical Research Council Ely Study. Diabetes Care. 2005;28:1195–1200. doi: 10.2337/diacare.28.5.1195. [DOI] [PubMed] [Google Scholar]
- 39.Ferreira I, Twisk JW, van Mechelen W, Kemper HC, Stehouwer CD. Development of fatness, fitness, and lifestyle from adolescence to the age of 36 years: determinants of the metabolic syndrome in young adults: the Amsterdam Growth and Health Longitudinal Study. Arch Intern Med. 2005;165:42–48. doi: 10.1001/archinte.165.1.42. [DOI] [PubMed] [Google Scholar]
- 40.Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Jr, Liu K. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA. 2003;290:3092–3100. doi: 10.1001/jama.290.23.3092. [DOI] [PubMed] [Google Scholar]
- 41.LaMonte MJ, Barlow CE, Jurca R, Kampert JB, Church TS, Blair SN. Cardiorespiratory fitness is inversely associated with the incidence of metabolic syndrome: a prospective study of men and women. Circulation. 2005;112:505–512. doi: 10.1161/CIRCULATIONAHA.104.503805. [DOI] [PubMed] [Google Scholar]
- 42.Ferreira I, Henry RM, Twisk JW, van Mechelen W, Kemper HC, Stehouwer CD Amsterdam Growth and Health Longitudinal Study. The metabolic syndrome, cardiopulmonary fitness, and subcutaneous trunk fat as independent determinants of arterial stiffness: the Amsterdam Growth and Health Longitudinal Study. Arch Intern Med. 2005;165:875–882. doi: 10.1001/archinte.165.8.875. [DOI] [PubMed] [Google Scholar]
- 43.Dhingra R, Sullivan L, Jacques PF, Wang TJ, Fox CS, Meigs JB, D’Agostino RB, Gaziano JM, Vasan RS. Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community [published correction appears in Circulation. 2007;116:e557] Circulation. 2007;116:480–488. doi: 10.1161/CIRCULATIONAHA.107.689935. [DOI] [PubMed] [Google Scholar]
- 44.Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation. 2008;117:754–761. doi: 10.1161/CIRCULATIONAHA.107.716159. [DOI] [PubMed] [Google Scholar]
- 45.He K, Liu K, Daviglus ML, Morris SJ, Loria CM, Van Horn L, Jacobs DR, Jr, Savage PJ. Magnesium intake and incidence of metabolic syndrome among young adults. Circulation. 2006;113:1675–1682. doi: 10.1161/CIRCULATIONAHA.105.588327. [DOI] [PubMed] [Google Scholar]
- 46.Mirmiran P, Noori N, Azizi F. A prospective study of determinants of the metabolic syndrome in adults. Nutr Metab Cardiovasc Dis. 2008;18:567–573. doi: 10.1016/j.numecd.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 47.Baik I, Shin C. Prospective study of alcohol consumption and metabolic syndrome. Am J Clin Nutr. 2008;87:1455–1463. doi: 10.1093/ajcn/87.5.1455. [DOI] [PubMed] [Google Scholar]
- 48.Chandola T, Brunner E, Marmot M. Chronic stress at work and the metabolic syndrome: prospective study. BMJ. 2006;332:521–525. doi: 10.1136/bmj.38693.435301.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lim HS, Lip GY, Beevers DG, Blann AD. Factors predicting the development of metabolic syndrome and type II diabetes against a background of hypertension. Eur J Clin Invest. 2005;35:324–329. doi: 10.1111/j.1365-2362.2005.01495.x. [DOI] [PubMed] [Google Scholar]
- 50.Sun SS, Liang R, Huang TT, Daniels SR, Arslanian S, Liu K, Grave GD, Siervogel RM. Childhood obesity predicts adult metabolic syndrome: the Fels Longitudinal Study. J Pediatr. 2008;152:191–200. doi: 10.1016/j.jpeds.2007.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Palaniappan L, Carnethon MR, Wang Y, Hanley AJ, Fortmann SP, Haffner SM, Wagenknecht L Insulin Resistance Atherosclerosis Study. Predictors of the incident metabolic syndrome in adults: the Insulin Resistance Atherosclerosis Study. Diabetes Care. 2004;27:788–793. doi: 10.2337/diacare.27.3.788. [DOI] [PubMed] [Google Scholar]
- 52.Morrison JA, Friedman LA, Harlan WR, Harlan LC, Barton BA, Schreiber GB, Klein DJ. Development of the metabolic syndrome in black and white adolescent girls: a longitudinal assessment. Pediatrics. 2005;116:1178–1182. doi: 10.1542/peds.2004-2358. [DOI] [PubMed] [Google Scholar]
- 53.Sheu WH, Chuang SY, Lee WJ, Tsai ST, Chou P, Chen CH. Predictors of incident diabetes, metabolic syndrome in middle-aged adults: a 10-year follow-up study from Kinmen, Taiwan. Diabetes Res Clin Pract. 2006;74:162–168. doi: 10.1016/j.diabres.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 54.Onat A, Uyarel H, Hergenc G, Karabulut A, Albayrak S, Can G. Determinants and definition of abdominal obesity as related to risk of diabetes, metabolic syndrome and coronary disease in Turkish men: a prospective cohort study. Atherosclerosis. 2007;191:182–190. doi: 10.1016/j.atherosclerosis.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 55.Tong J, Boyko EJ, Utzschneider KM, McNeely MJ, Hayashi T, Carr DB, Wallace TM, Zraika S, Gerchman F, Leonetti DL, Fujimoto WY, Kahn SE. Intra-abdominal fat accumulation predicts the development of the metabolic syndrome in non-diabetic Japanese-Americans. Diabetologia. 2007;50:1156–1160. doi: 10.1007/s00125-007-0651-y. [DOI] [PubMed] [Google Scholar]
- 56.Lloyd-Jones DM, Liu K, Colangelo LA, Yan LL, Klein L, Loria CM, Lewis CE, Savage P. Consistently stable or decreased body mass index in young adulthood and longitudinal changes in metabolic syndrome components: the Coronary Artery Risk Development in Young Adults Study. Circulation. 2007;115:1004–1011. doi: 10.1161/CIRCULATIONAHA.106.648642. [DOI] [PubMed] [Google Scholar]
- 57.Ryu S, Song J, Choi BY, Lee SJ, Kim WS, Chang Y, Kim DI, Suh BS, Sung KC. Incidence and risk factors for metabolic syndrome in Korean male workers, ages 30 to 39. Ann Epidemiol. 2007;17:245–252. doi: 10.1016/j.annepidem.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 58.Vergnaud AC, Bertrais S, Oppert JM, Maillard-Teyssier L, Galan P, Hercberg S, Czernichow S. Weight fluctuations and risk for metabolic syndrome in an adult cohort. Int J Obes (Lond) 2008;32:315–321. doi: 10.1038/sj.ijo.0803739. [DOI] [PubMed] [Google Scholar]
- 59.Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniels SR. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119:237–246. doi: 10.1542/peds.2006-2543. [DOI] [PubMed] [Google Scholar]
- 60.Tomiyama H, Yamada J, Koji Y, Yambe M, Motobe K, Shiina K, Yamamoto Y, Yamashina A. Heart rate elevation precedes the development of metabolic syndrome in Japanese men: a prospective study. Hypertens Res. 2007;30:417–426. doi: 10.1291/hypres.30.417. [DOI] [PubMed] [Google Scholar]
- 61.Holvoet P, Lee DH, Steffes M, Gross M, Jacobs DR., Jr Association between circulating oxidized low-density lipoprotein and incidence of the metabolic syndrome. JAMA. 2008;299:2287–2293. doi: 10.1001/jama.299.19.2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sui X, Church TS, Meriwether RA, Lobelo F, Blair SN. Uric acid and the development of metabolic syndrome in women and men. Metabolism. 2008;57:845–852. doi: 10.1016/j.metabol.2008.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.André P, Balkau B, Vol S, Charles MA, Eschwege E DESIR Study Group. Gamma-glutamyltransferase activity and development of the metabolic syndrome (International Diabetes Federation Definition) in middle-aged men and women: data from the Epidemiological Study on the Insulin Resistance Syndrome (DESIR) cohort. Diabetes Care. 2007;30:2355–2361. doi: 10.2337/dc07-0440. [DOI] [PubMed] [Google Scholar]
- 64.Lee DS, Evans JC, Robins SJ, Wilson PW, Albano I, Fox CS, Wang TJ, Benjamin EJ, D’Agostino RB, Vasan RS. Gamma glutamyl transferase and metabolic syndrome, cardiovascular disease, and mortality risk: the Framingham Heart Study. Arterioscler Thromb Vasc Biol. 2007;27:127–133. doi: 10.1161/01.ATV.0000251993.20372.40. [DOI] [PubMed] [Google Scholar]
- 65.Hanley AJ, Williams K, Festa A, Wagenknecht LE, D’Agostino RB, Jr, Haffner SM. Liver markers and development of the metabolic syndrome: the Insulin Resistance Atherosclerosis study. Diabetes. 2005;54:3140–3147. doi: 10.2337/diabetes.54.11.3140. [DOI] [PubMed] [Google Scholar]
- 66.Schindhelm RK, Dekker JM, Nijpels G, Stehouwer CD, Bouter LM, Heine RJ, Diamant M. Alanine aminotransferase and the 6-year risk of the metabolic syndrome in Caucasian men and women: the Hoorn Study. Diabet Med. 2007;24:430–435. doi: 10.1111/j.1464-5491.2007.02100.x. [DOI] [PubMed] [Google Scholar]
- 67.Ingelsson E, Pencina MJ, Tofler GH, Benjamin EJ, Lanier KJ, Jacques PF, Fox CS, Meigs JB, Levy D, Larson MG, Selhub J, D’Agostino RB, Sr, Wang TJ, Vasan RS. Multimarker approach to evaluate the incidence of the metabolic syndrome and longitudinal changes in metabolic risk factors: the Framingham Offspring Study. Circulation. 2007;116:984–992. doi: 10.1161/CIRCULATIONAHA.107.708537. [DOI] [PubMed] [Google Scholar]
- 68.Galletti F, Barbato A, Versiero M, Iacone R, Russo O, Barba G, Siani A, Cappuccio FP, Farinaro E, della Valle E, Strazzullo P. Circulating leptin levels predict the development of metabolic syndrome in middle-aged men: an 8-year follow-up study. J Hypertens. 2007;25:1671–1677. doi: 10.1097/HJH.0b013e3281afa09e. [DOI] [PubMed] [Google Scholar]
- 69.Laaksonen DE, Niskanen L, Nyyssönen K, Punnonen K, Tuomainen TP, Valkonen VP, Salonen R, Salonen JT. C-reactive protein and the development of the metabolic syndrome and diabetes in middle-aged men. Diabetologia. 2004;47:1403–1410. doi: 10.1007/s00125-004-1472-x. [DOI] [PubMed] [Google Scholar]
- 70.Hassinen M, Lakka TA, Komulainen P, Gylling H, Nissinen A, Rauramaa R. C-reactive protein and metabolic syndrome in elderly women: a 12-year follow-up study. Diabetes Care. 2006;29:931–932. doi: 10.2337/diacare.29.04.06.dc05-2508. [DOI] [PubMed] [Google Scholar]
- 71.Xu A, Tso AW, Cheung BM, Wang Y, Wat NM, Fong CH, Yeung DC, Janus ED, Sham PC, Lam KS. Circulating adipocyte–fatty acid binding protein levels predict the development of the metabolic syndrome: a 5-year prospective study. Circulation. 2007;115:1537–1543. doi: 10.1161/CIRCULATIONAHA.106.647503. [DOI] [PubMed] [Google Scholar]
- 72.Rodriguez A, Muller DC, Metter EJ, Maggio M, Harman SM, Blackman MR, Andres R. Aging, androgens, and the metabolic syndrome in a longitudinal study of aging. J Clin Endocrinol Metab. 2007;92:3568–3572. doi: 10.1210/jc.2006-2764. [DOI] [PubMed] [Google Scholar]
- 73.Jurca R, Lamonte MJ, Barlow CE, Kampert JB, Church TS, Blair SN. Association of muscular strength with incidence of metabolic syndrome in men. Med Sci Sports Exerc. 2005;37:1849–1855. doi: 10.1249/01.mss.0000175865.17614.74. [DOI] [PubMed] [Google Scholar]
- 74.Tortosa A, Bes-Rastrollo M, Sanchez-Villegas A, Basterra-Gortari FJ, Nuñez-Cordoba JM, Martinez-Gonzalez MA. Mediterranean diet inversely associated with the incidence of metabolic syndrome: the SUN prospective cohort. Diabetes Care. 2007;30:2957–2959. doi: 10.2337/dc07-1231. [DOI] [PubMed] [Google Scholar]
- 75.Laaksonen DE, Niskanen L, Punnonen K, Nyyssönen K, Tuomainen TP, Valkonen VP, Salonen R, Salonen JT. Testosterone and sex hormone-binding globulin predict the metabolic syndrome and diabetes in middle-aged men. Diabetes Care. 2004;27:1036–1041. doi: 10.2337/diacare.27.5.1036. [DOI] [PubMed] [Google Scholar]
- 76.Kupelian V, Page ST, Araujo AB, Travison TG, Bremner WJ, McKinlay JB. Low sex hormone-binding globulin, total testosterone, and symptomatic androgen deficiency are associated with development of the metabolic syndrome in nonobese men. J Clin Endocrinol Metab. 2006;91:843–850. doi: 10.1210/jc.2005-1326. [DOI] [PubMed] [Google Scholar]
- 77.Warensjö E, Risérus U, Vessby B. Fatty acid composition of serum lipids predicts the development of the metabolic syndrome in men. Diabetologia. 2005;48:1999–2005. doi: 10.1007/s00125-005-1897-x. [DOI] [PubMed] [Google Scholar]
19. Nutrition
See Tables 19-1 and 19-2 and Charts 19-1 through 19-3.
Table 19-1.
Dietary Consumption in 2005 to 2006 Among US Adults (>20 Years of Age) of Selected Foods and Nutrients Related to Cardiometabolic Health104–109
| NH White Men | NH White Women | NH Black Men | NH Black Women | Mexican American Men | Mexican American Women | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
|
| Foods | ||||||||||||
| Whole grains, servings/d |
0.7±0.6 | 4.6 | 0.7±0.6 | 5.0 | 0.5±0.3 | 3.6 | 0.5±0.6 | 4.4 | 2.2±1.6 | 28.2 | 1.6±1.5 | 22.0 |
| Fruits, servings/d |
1.2±1.3 | 7.5 | 1.6±1.5 | 11.0 | 1.2±1.3 | 8.6 | 1.1±1.3 | 5.8 | 1.3±1.5 | 5.9 | 1.8±1.3 | 10.2 |
| Fruits including 100% juices, servings/d |
2.0±1.8 | 16.0 | 2.1±1.6 | 17.0 | 2.3±1.8 | 21.9 | 2.1±1.6 | 14.3 | 2.0±1.8 | 13.8 | 2.8±2.1 | 23.7 |
| Vegetables, servings/d |
1.8±1.1 | 10.7 | 2.1±1.1 | 14.3 | 1.3±0.8 | 5.1 | 1.7±1.2 | 9.5 | 1.2±0.6 | 3.6 | 1.4±0.7 | 4.6 |
| Vegetables including juices/sauces, servings/d |
2.0±1.2 | 13.4 | 2.2±1.2 | 16.0 | 1.4±0.7 | 5.2 | 1.8±1.2 | 10.2 | 1.4±0.6 | 4.3 | 1.6±0.6 | 5.5 |
| Fish and shellfish, servings/wk |
1.6±1.4 | 22.3 | 1.4±1.1 | 19.7 | 1.7±1.2 | 24.2 | 1.7±1.1 | 24.4 | 1.7±2.0 | 18.5 | 1.5±1.1 | 19.2 |
| Nuts, legumes, and seeds, servings/wk |
2.5±1.6 | 18.2 | 2.3±1.6 | 18.2 | 2.2±0.4 | 16.6 | 1.5±0.6 | 14.0 | 7.6±6.9 | 45.9 | 5.9±3.7 | 36.2 |
| Processed meats, servings/wk |
3.2±1.8 | 46.3 | 1.9±1.1 | 61.2 | 3.7±1.9 | 42.3 | 2.2±1.3 | 56.6 | 1.9±1.1 | 66.8 | 1.5±1.1 | 69.8 |
| Sugar- sweetened beverages, servings/wk |
10.5±11.4 | 48.7 | 6.0±10.2 | 68.2 | 15.6±8.6 | 23.8 | 12.5±8.2 | 35.6 | 17.7±10.8 | 21.8 | 10.6±8.2 | 38.9 |
| Sweets and bakery desserts, servings/wk |
7.6±4.9 | 33.1 | 7.3±3.7 | 34.9 | 7.1±4.9 | 41.0 | 7.2±1.8 | 40.5 | 4.3±2.9 | 50.6 | 6.6±3.0 | 47.3 |
| Nutrients | ||||||||||||
| Total calories, kcal/d |
2587±667 | NA | 1750±454 | NA | 2425±608 | NA | 1742±603 | NA | 2441±692 | NA | 1853±546 | NA |
| EPA DHA, g/d | 0.126±0.134 | 5.8 | 0.124±0.134 | 5.8 | 0.164±0.168 | 7.6 | 0.153±0.125 | 6.7 | 0.138±0.134 | 7.4 | 0.123±0.134 | 5.5 |
| ALA, g/d | 1.34±0.27 | 25.4 | 1.54±0.51 | 72.1 | 1.28±0.34 | 20.1 | 1.43±0.44 | 67.2 | 1.17±0.26 | 15.6 | 1.27±0.32 | 57.9 |
| n-6 PUFA, % energy |
7.0±1.2 | NA | 7.4±1.6 | NA | 7.2±1.4 | NA | 7.5±2.0 | NA | 6.5±1.1 | NA | 6.6±1.7 | NA |
| Saturated fat, % energy |
11.5±2.3 | 32.7 | 11.5±2.3 | 33.5 | 11.0±1.9 | 36.4 | 10.6±2.3 | 40.1 | 9.9±2.1 | 54.1 | 10.3±1.7 | 49.3 |
| Dietary cholesterol, mg/d |
270±91 | 68.8 | 279±93 | 67.7 | 298±108 | 65.1 | 308±91 | 59.2 | 304±138 | 62.7 | 280±97 | 65.5 |
| Total fat, % energy |
34.1±5.3 | 55.4 | 34.1±4.9 | 55.2 | 34.1±4.8 | 46.3 | 33.2±5.4 | 52.9 | 31.2±5.2 | 66.4 | 31.2±5.3 | 66.1 |
| Carbohydrate, % energy |
47.3±7.7 | NA | 49.0±6.6 | NA | 48.8±6.2 | NA | 51.1±6.7 | NA | 50.9±6.9 | NA | 53.6±6.8 | NA |
| Dietary fiber, g/d |
14.8±4.6 | 3.2 | 17.1±5.7 | 6.8 | 12.9±3.8 | 2.0 | 14.0±5.0 | 3.3 | 18.0±6.7 | 11.7 | 19.1±4.6 | 10.7 |
| Sodium, g/d | 3.3±0.8 | 13.1 | 3.6±0.5 | 7.2 | 3.2±0.4 | 10.2 | 3.4±0.6 | 8.7 | 3.0±0.8 | 24.4 | 3.2±0.6 | 17.4 |
NH indicates non-Hispanic; EPA, eicosapentaenoic acid; DHA docosahexaenoic acid; ALA, α-linoleic acid; n-6 PUFA, omega-6 polyunsaturated fatty acid; NA, not available.
Based on data from National Health and Nutrition Examination Survey 2005 to 2006 (two 24-hour dietary recalls per person, with SDs adjusted for within- and between-person variation). All values are energy adjusted, and for comparability, means and proportions are reported for a 2000-kcal/d diet. To obtain actual mean consumption levels, multiply group means by group-specific total caloric consumption divided by 2000.
Guidelines adjusted to a 2000-kcal/d diet. Whole grains (characterized as minimum 1.1 g fiber per 10 g carbohydrate), 3 or more 1-oz equivalent (1 oz bread; 1 cup dry cereal; 1/2 cup cooked rice, pasta, or cereal) servings per day (Dietary Guidelines for Americans); fish or shellfish, 2 or more 100-g (3.5-oz) servings per week106; fruits, 4 or more 1/2-cup servings per day108; vegetables, 5 or more 1/2-cup servings per day, including up to 3 cups per week of starchy vegetables107; nuts, legumes, and seeds, 4 or more 50-g servings per week106; processed meats (bacon, hot dogs, sausage, processed deli meats), 2 or fewer 100-g (3.5-oz) servings per week (1/4 of discretionary calories)107; sugar-sweetened beverages (defined as ≥50 cal/8 oz, excluding whole juices), 36 oz or less per week (≈1/4 of discretionary calories)106,107; sweets and bakery desserts, 2.5 or fewer 50-g servings per week (≈1/4 of discretionary calories)106,107; EPA DHA, ≥0.5 g/d108; ALA, ≥1.6/1.1 g/d (men/women)109; saturated fat, <10% energy107; dietary cholesterol, <300 mg/d107; total fat, 20% to 35% energy107; dietary fiber, ≥28/d107; and sodium, <2.3 g/d.107
Table 19-2.
Dietary Consumption in 2005 to 2006 Among US Children and Teenagers of Selected Foods and Nutrients Related to Cardiometabolic Health
| Boys (5–9 y) | Girls (5–9 y) | Boys (10–14 y) | Girls (10–14 y) | Boys (15–19 y) | Girls (15–19 y) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
Average Consumption (Mean±SD) |
% Meeting Guidelines* |
|
| Foods | ||||||||||||
| Whole grains, servings/d |
0.5±0.4 | 0.9 | 0.5±0.2 | 0.8 | 0.5±0.5 | 4.0 | 0.5±0.4 | 2.6 | 0.4±0.4 | 2.0 | 0.5±0.4 | 2.5 |
| Fruits, servings/d |
1.5±0.6 | 6.2 | 1.3±0.8 | 6.2 | 1.3±0.4 | 8.4 | 1.3±0.4 | 5.9 | 0.8±0.6 | 3.2 | 0.8±0.8 | 4.2 |
| Fruits including 100% juices, servings/d |
2.6±1.6 | 18.7 | 2.3±1.3 | 17.7 | 2.0±1.1 | 15.6 | 2.2±1.1 | 15.8 | 1.7±1.4 | 14.2 | 1.7±1.3 | 10.3 |
| Vegetables, servings/d |
0.8±0.5 | 1.4 | 1.9±0.6 | 2.1 | 0.8±0.5 | 2.2 | 0.9±0.5 | 2.2 | 0.8±0.5 | 1.2 | 0.9±0.5 | 2.3 |
| Vegetables including juices/sauces, servings/d |
0.9±0.5 | 1.8 | 1.0±0.6 | 1.7 | 0.9±0.8 | 2.2 | 1.0±0.5 | 2.3 | 1.0±0.8 | 1.5 | 1.0±0.5 | 2.4 |
| Fish and shellfish, servings/wk |
0.6±0.3 | 11.7 | 0.8±0.3 | 13.8 | 1.1±0.4 | 15.2 | 0.4±0.4 | 9.2 | 0.6±0.4 | 10.3 | 0.7±0.4 | 12.2 |
| Nuts, legumes, and seeds, servings/wk |
1.5±2.8 | 13.0 | 1.7±2.8 | 12.9 | 1.4±2.3 | 8.8 | 1.5±2.3 | 11.2 | 1.2±2.1 | 9.2 | 1.0±1.8 | 8.7 |
| Processed meats, servings/wk |
2.2±1.0 | 60.0 | 2.1±1.1 | 59.0 | 2.5±1.1 | 57.0 | 2.3±1.2 | 54.8 | 3.4±1.7 | 41.8 | 2.3±1.7 | 58.6 |
| Sugar- sweetened beverages, servings/wk |
7.8±5.5 | 40.6 | 8.0±3.7 | 39.7 | 14.2±6.2 | 19.9 | 10.9±5.6 | 31.6 | 22.5±8.7 | 12.9 | 15.3±8.7 | 27.2 |
| Sweets and bakery desserts, servings/wk |
10.2±4.1 | 18.2 | 9.8±4.1 | 18.4 | 9.5±4.1 | 24.0 | 8.4±4.0 | 28.0 | 6.5±3.3 | 41.2 | 8.5±1.5 | 32.6 |
| Nutrients | ||||||||||||
| Total calories, kcal/d |
2010±278 | NA | 1777±292 | NA | 2210±423 | NA | 1901±483 | NA | 2809±477 | NA | 1901±457 | NA |
| EPA DHA, g/d | 0.048±0.025 | NA | 0.063±0.025 | NA | 0.081±0.030 | NA | 0.044±0.030 | NA | 0.064±0.022 | NA | 0.068±0.021 | NA |
| ALA, g/d | 1.14±0.17 | 11.1 | 1.13±0.25 | 42.6 | 1.13±0.17 | 11.2 | 1.23±0.25 | 49.4 | 1.12±0.20 | 12.5 | 1.33±0.20 | 56.7 |
| n-6 PUFA, % energy |
6.4±0.8 | NA | 6.3±1.0 | NA | 6.5±0.8 | NA | 6.9±1.0 | NA | 6.3±1.1 | NA | 6.9±1.1 | NA |
| Saturated fat, % energy |
11.9±1.5 | 21.9 | 12.0±1.1 | 20.2 | 11.7±1.7 | 24.3 | 11.5±1.5 | 28.6 | 11.8±1.2 | 25.6 | 11.7±2.0 | 29.5 |
| Dietary cholesterol, mg/d |
220±72 | 85.0 | 250±72 | 75.2 | 230±86 | 79.2 | 218±115 | 85.1 | 239±48 | 75.7 | 222±64 | 81.4 |
| Total fat, % energy |
33.3±3.5 | 63.8 | 33.3±2.5 | 67.9 | 33.4±3.3 | 61.9 | 33.3±4.1 | 62.3 | 33.5±3.0 | 57.6 | 33.4±5.6 | 56.8 |
| Carbohydrate, % energy |
54.0±4.7 | NA | 53.9±3.5 | NA | 53.1±4.9 | NA | 53.8±5.0 | NA | 51.5±3.6 | NA | 53.0±4.2 | NA |
| Dietary fiber, g/d |
13.6±2.1 | 0.1 | 13.7±2.2 | 1.3 | 13.0±3.6 | 1.8 | 13.8±3.2 | 0.8 | 11.5±2.3 | 0.7 | 12.8±1.9 | 0.7 |
| Sodium, g/d | 3.0±0.3 | 10.4 | 3.2±0.4 | 6.8 | 3.2±0.4 | 8.4 | 3.4±0.4 | 6.1 | 3.2±0.4 | 12.4 | 3.3±0.4 | 10.0 |
EPA indicates eicosapentaenoic acid; DHA docosahexaenoic acid; ALA, α-linoleic acid; n-6 PUFA, omega-6 polyunsaturated fatty acid; NA, not available.
Based on data from National Health and Nutrition Examination Survey 2005 to 2006 (two 24-hour dietary recalls per person, with SDs adjusted for within- and between-person variation). All values are energy adjusted, and for comparability, means and proportions are reported for a 2000-kcal/d diet. To obtain actual mean consumption levels, multiply group means by group-specific total caloric consumption divided by 2000. Each of these guidelines is age-appropriately adjusted to a 2000-kcal/d diet, as for adults.
See Table 19-1 for food group, serving size, and guideline definitions.
Chart 19-1.
Age-adjusted trends in macronutrients and total calories consumed by US adults (20 to 74 years of age), 1971–2004. Data derived from National Center for Health Statistics. Health, United States 2007, With Chartbook on Trends in the Health of Americans.14
Chart 19-3.
Total US food expenditures away from home and at home, 1977 and 2007. Data derived from US Department of Agriculture Economic Research Service.57
This chapter of the update highlights national nutritional intake data, focusing on foods, nutrients, dietary patterns, and other dietary factors that are related to cardiometabolic health. It is intended to examine current intakes, trends and changes in intakes, and estimated effects on disease to support and further stimulate efforts to monitor and improve dietary habits in relation to cardiovascular health.
Prevalence
Foods and Nutrients: Adults
See Table 19-1; NHANES 2005 to 2006; personal communication with D. Mozaffarian (December 2008).
The dietary consumption by US adults of selected foods and nutrients related to cardiometabolic health is detailed in Table 19-1 according to sex and ethnic subgroups:
Average consumption of whole grains by white and black men and women was between 0.5 and 0.7 servings per day, with only between 3% and 5% of white and black adults consuming ≥3 servings per day. Average whole grain consumption by Mexican Americans was ≈2 servings per day, with 22% to 28% consuming ≥3 servings per day.
Average fruit consumption ranged from 1.1 to 1.8 servings per day in these sex and ethnic subgroups; 8% to 11% of whites, 6% to 9% of blacks, and 6% to 10% of Mexican Americans consumed ≥4 servings per day. When 100% fruit juices were included, the number of servings consumed and the proportions of adults consuming ≥4 servings per day approximately doubled.
Average vegetable consumption ranged from 1.2 to 2.1 servings per day; 11% to 14% of whites, 5% to 10% of blacks, and 3% to 5% of Mexican Americans consumed ≥5 servings per day. The inclusion of vegetable juices and sauces generally produced little change in these consumption patterns.
Average consumption of fish and shellfish was lowest among white women (1.4 servings per week) and highest among black and Mexican American men (1.7 servings per week); between 75% and >80% of adults in each sex and ethnic subgroup consumed <2 servings per week. Approximately 6% of whites, 7% of blacks, and 6% to 7% of Mexican Americans consumed ≥500 mg/d of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
Average consumption of nuts, legumes, and seeds was ≈2 servings per week among black women, black men, and white women; 3 servings per week among white men; and 6 and 8 servings per week among Mexican American women and men, respectively. Approximately 18% of whites, 14% to 17% of blacks, and 36% to 46% of Mexican Americans consumed ≥4 servings per week.
Average consumption of processed meats was lowest among Mexican American women (1.5 servings per week) and highest among black men (3.7 servings per week). Between 40% (Mexican American women) and 68% (black men) of adults consumed ≥1 serving per week.
Average consumption of sugar-sweetened beverages ranged from ≈6 servings per week among white women to 18 servings per week among Mexican American men. Approximately 51% and 32% of white men and women, 76% and 66% of black men and women, and 78% and 61% of Mexican American men and women, respectively, consumed >36 oz (4.5 eight-oz servings) per week.
Average consumption of sweets and bakery desserts ranged from ≈4 servings per day (Mexican American men) to 8 servings per day (white men). Approximately two thirds of white and black men and women and half of all Mexican American men and women consumed >25 servings per week.
Between 33% and 54% of adults in each sex and ethnic subgroup consumed <10% of total calories from saturated fat, and between 59% and 69% consumed <300 mg of dietary cholesterol per day.
Only 3% to 7% of whites, 2% to 3% of blacks, and 11% to 12% of Mexican Americans consumed ≥28 g of dietary fiber per day.
Only 7% to 13% of whites, 9% to 10% of blacks, and 17% to 24% of Mexican Americans consumed <2.3 g of sodium per day. In 2005, the US Department of Health and Human Services (DHHS) and US Department of Agriculture (USDA) recommended that adults in specific groups, including people with hypertension, all middle-aged and older adults, and all blacks, should consume no more than 1.5 g of sodium per day. Overall in 2005 to 2006, the majority (69.2%) of US adults belonged to 1 or more of these specific groups in whom sodium consumption should be 1.5 g/d.1
Foods and Nutrients: Children and Teenagers
See Table 19-2; NHANES 2005 to 2006; personal communication with D. Mozaffarian (December 2008).
The dietary consumption by US children and teenagers of selected foods and nutrients related to cardiometabolic health is detailed in Table 19-2:
Average whole grain consumption was low, ranging from 0.4 to 0.5 servings per day, with 4% of children in different age and sex subgroups consuming ≥3 servings per day.
Average fruit consumption was low: 1.5 and 1.3 servings per day in younger boys and girls (5 to 9 years of age), 1.3 servings per day in adolescent boys and girls (10 to 14 years of age), and 0.8 servings per day in teenage boys and girls (15 to 19 years of age). The proportion consuming ≥4 servings per day was low and decreased with age: 6% in those 5 to 9 years of age, 6% to 8% in those 10 to 14 years of age, and 3% to 4% in those 15 to 19 years of age. When 100% fruit juices were included, the number of servings consumed approximately doubled or tripled, and proportions consuming ≥4 servings per day were 18% to 19% of those 5 to 9 years of age, 16% of those 10 to 14 years of age, and 10% to 14% of those 15 to 19 years of age.
Average vegetable consumption was low, ranging from 0.8 to 0.9 servings per day, with only up to 2% of children in different age and sex subgroups consuming ≥5 servings per day.
Average consumption of fish and shellfish was low, ranging between 0.6 and 0.8 servings per week in 5- to 9-year-olds, 0.4 to 1.1 servings per week in 10- to 14-year-olds, and 0.6 to 0.7 servings per week in 15- to 19-year-olds. Among all ages, 15% of children and teenagers consumed ≥2 servings per week.
Average consumption of nuts, legumes, and seeds ranged from 1.0 to 1.2 servings per week among 15- to 19-year-olds to 1.4 to 1.7 servings per week at younger ages. Between 9% and 13% of children in different age and sex subgroups consumed ≥4 servings per week.
Average consumption of processed meats ranged from 2.1 to 3.4 servings per week; was uniformly higher than the average consumption of nuts, legumes, and seeds; and was up to 6 times higher than the average consumption of fish and shellfish. Between 42% and 60% of children consumed ≥2 servings per week.
Average consumption of sugar-sweetened beverages was higher in boys than in girls and was ≈8 servings per week in 5- to 9-year-olds, 11 to 14 servings per week in 10- to 14-year-olds, and 15 to 23 servings per week in 15- to 19-year-olds. This was generally considerably higher than the average consumption of whole grains, fruits, vegetables, fish and shellfish, or nuts, legumes, and seeds. Only between 13% (boys 15 to 19 years of age) and 40% (boys and girls 5 to 9 years of age) of children consumed 4.5 servings per week.
Average consumption of sweets and bakery desserts was ≈10 servings per week in 5- to 9-year-olds and 10- to 14-year-olds and 6 to 9 servings per week in 15- to 19-year-olds. From 82% (5 to 9 years of age) to 59% (15 to 19 years of age) of youths consumed >2.5 servings per week.
Average consumption of EPA and DHA was low, ranging from ≈40 to 80 mg/d in boys and girls at all ages. Only between 0.4% and 2.5% of children and teenagers at all ages consumed ≥500 mg/d.
Average consumption of saturated fat was between 11% and 12% of calories, and average consumption of dietary cholesterol was ≈230 mg/d. Approximately one fifth to one third of children consumed <10% energy from saturated fat, and ≈80% consumed <300 mg of dietary cholesterol per day.
Average consumption of dietary fiber ranged from 11 to 14 g/d. Less than 2% of children in different age and sex subgroups consumed ≥28 g/d.
Average consumption of sodium ranged from 3.0 to 3.4 g/d. Between 6% and 12% of children in different age and sex subgroups consumed <2.3 g/d.
Energy Balance
Energy balance, or consumption of total calories appropriate for needs, is determined by the balance of average calories consumed versus expended, with this balance depending on multiple factors, including calories consumed, PA, body size, age, sex, and underlying basal metabolic rate. Thus, one individual may consume relatively high calories but have negative energy balance (as a result of even greater calories expended), whereas another individual may consume relatively few calories but have positive energy balance (because of low calories expended). Given such variation, the most practical and reasonable method to assess energy balance in populations is to assess changes in weight over time (see the Trends section below).
Average daily caloric intake in the United States is ≈2500 calories in adult men and 1800 calories in adult women (Table 19-1). In children and teenagers, average caloric intake is higher in boys than in girls and increases with age in boys (Table 19-2). Trends in energy balance are described below.
Individual nutritional determinants of positive energy balance (more calories consumed than expended), as determined by adiposity or weight gain, include larger portion sizes,2,3 higher intake of sugar-sweetened beverages,4,5 and greater consumption of fast food and commercially prepared meals.6–10
Each of these dietary factors has multiple influences; for example, preferences for portion size are associated with BMI, socioeconomic status, eating in fast food restaurants, and television watching.11,12 Portion sizes are larger at fast food restaurants than at home or at other restaurants.13
In 1999 to 2000, 41% of US adults consumed ≥3 commercially prepared meals per week.7 Between 1999 and 2004, 53% of Americans consumed an average of 1 to 3 restaurant meals per week, and 23% consumed ≥4 restaurant meals per week.14 Spending on food away from home, including restaurant meals, catered foods, and food eaten during out-of-town trips, increased from 26% of average annual food expenditures in 1970% to 42% in 2004.14
Macronutrient composition of the diet such as percent calories from total fat or total carbohydrate does not appear to be strongly associated with energy balance as ascertained by weight gain or loss.15–17 Preliminary evidence suggests that aspects of dietary quality rather than composition such as extent of processing of carbohydrates consumed,17 consumption of trans fat,18–20 and energy density21–23 may be associated with energy imbalance as assessed by changes in adiposity or weight, but such data are still emerging. Randomized controlled trials in obese individuals generally show modestly greater weight loss with low-carbohydrate versus low-fat diets at 6 months, but at 1 year, such differences diminish, and a diet that focuses on dietary quality and whole foods may be most successful.24–26
A comparison of BRFSS data in 1996 and 2003 suggested a shift in self-reported dietary strategies to lose weight, with the proportion focusing on energy restriction increasing from 11.3% to 24.9%, and the proportion focusing on restricting fat consumption decreasing from 41.6% to 29.1%.27
Other individual factors associated with positive energy balance (weight gain) include greater television watching (particularly as related to greater food consumption)28–33 and lower average sleep duration, particularly among children.34
A 2007 to 2008 national survey of 1082 retail stores in 19 US cities found that energy-dense snack foods/beverages were present in 96% of pharmacies, 94% of gas stations, 22% of furniture stores, 16% of apparel stores, and 29% to 65% of other types of stores.35
Societal and environmental factors independently associated with energy imbalance (weight gain), via either increased caloric consumption or decreased expenditure, include education, income, race/ethnicity, and local conditions such as availability of grocery stores, types of restaurants, safety, parks and open spaces, and walking or biking paths.36–38 PA is covered in a separate chapter of this update.
Dietary Patterns
In addition to individual foods and nutrients, overall dietary patterns can be used to assess more global dietary quality. Different dietary patterns have been defined, including the Healthy Eating Index (HEI), Alternative Health Eating Index, Western versus prudent dietary patterns, Mediterranean dietary pattern, and DASH-type diet.
In 1999 to 2004, only 19.4% of hypertensive US adults were following a DASH-type diet (based on intake of fiber, magnesium, calcium, sodium, potassium, protein, total fat, saturated fat, and cholesterol). This represented a decrease from 26.7% of hypertensive US adults in 1988 to 1994.39
Among older US adults (≥60 years of age) in 1999 to 2002, 72% met guidelines for dietary cholesterol intake, but only between 18% and 32% met guidelines for the HEI food groups (meats, dairy, fruits, vegetables, and grains). On the basis of the HEI score, only 17% of older US adults consumed a good-quality diet. Higher HEI scores were seen in white adults and individuals with greater education; lower HEI scores were seen in black adults and smokers.40
Nearly 75 000 women 38 to 63 years of age in the Nurses’ Health Study without a history of CVD or DM were followed up from 1984 to 2004. It was found that a greater adherence to the Mediterranean diet, as reflected by a higher Alternate Mediterranean Diet Score, was associated with a lower risk of incident CHD and stroke in women.41
Dietary Supplements
Use of dietary supplements is common in the United States among both adults and children:
Half (53%) of US adults in 2001 to 2004 used dietary supplements, with the most common supplement being multivitamins and multiminerals (67% of supplement users). Most supplements were taken daily and for at least 2 years. Supplement use was associated with older age, higher education, greater PA, wine intake, lower BMI, and white race.14,42
One third (32%) of US children (birth to 18 years of age) used dietary supplements in 1999 to 2002, with the highest use (48.5%) occurring among 4- to 8-year-olds. The most common supplements were multivitamins and multiminerals (58% of supplement users). The primary nutrients supplemented (either by multivitamins and/or individual vitamins) included vitamin C (29% of US children), vitamin A (26%), vitamin D (26%), calcium (21%), and iron (19%). Supplement use was associated with higher family income, a smoke-free home environment, lower child BMI, and less screen time (television, video games, or computers).43
In a 2005 to 2006 telephone survey of US adults, 41.3% were making or had made in the past a serious weight-loss attempt. Of these, one third (33.9%) had used a dietary supplement for weight loss, with such use being more common in women (44.9%) than in men (19.8%) and in blacks (48.7%) or Hispanics (41.6%) than in whites (31.2%); in those with high school education or less (38.4%) than in those with some college or more (31.1%); and in those with household income less than $40 000 per year (41.8%) than in those with higher incomes (30.3%).44
Multiple trials of most dietary supplements, including folate, vitamin C, and vitamin E, have generally shown no significant effect on CVD risk. The major exceptions are long-chain omega-3 fatty acids, for which 3 large randomized controlled trials that included populations with and without established HD have shown significant reductions in risk of CVD events at doses of 1 to 2 g/d (Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico [GISSI]-Prevenzione, Japan EPA Lipid Intervention Study, and GISSI-HF).45–47 Another multicenter randomized trial conducted in a population with diabetic nephropathy found that B vitamin supplementation containing folic acid (2.5 mg/d), vitamin B6 (25 mg), and vitamin B12 (1 mg/d) resulted in a greater decrease in glomerular filtration rate and an increase in myocardial infarction and stroke compared with placebo.48
Trends
Energy Balance
Energy balance, or consumption of total calories appropriate for needs, has been steadily worsening in the United States over the past several decades, as evidenced by the dramatic increases in overweight and obesity among both children and adults across broad cross sections of sex, race/ethnicity, geographic residence, and socioeconomic status.49,50
Although trends in total calories consumed are difficult to quantify exactly because of differing methods of serial national dietary surveys over time, multiple lines of evidence indicate that average total energy consumption has increased by at least 200 kcal/d per person in the past 3 decades.
Data from NHANES indicate that between 1971 and 2004, average total energy consumption among US adults increased by 22% in women (from 1542 to 1886 kcal/d) and by 10% in men (from 2450 to 2693 kcal/d; Chart 19-1). These increases are supported by data from the Nationwide Food Consumption Survey (1977–1978) and the Continuing Surveys of Food Intake (1989 –1998).13
The increases in calories consumed during this time period are attributable primarily to greater average carbohydrate intake, particularly of starches, refined grains, and sugars (see the Foods and Nutrients section below). Other specific changes related to increased caloric intake in the United States include larger portion sizes, greater food quantity and calories per meal, and increased consumption of sugar-sweetened beverages, snacks, commercially prepared (especially fast food) meals, and higher-energy-density foods.7,13,51–55
Between 1977 to 1978 and 1994 to 1996, the average portion sizes for nearly all foods increased at fast food outlets, other restaurants, and home. These included a 33% increase in the average portion of Mexican food (from 408 to 541 calories), a 34% increase in the average portion of cheeseburgers (from 397 to 533 calories), a 36% increase in the average portion of French fries (from 188 to 256 calories), and a 70% increase in the average portion of salty snacks such as crackers, potato chips, pretzels, puffed rice cakes, and popcorn (from 132 to 225 calories).13
Among US children 2 to 7 years of age, an estimated energy imbalance of only 110 to 165 kcal/d (the equivalent of one 12- to 16-oz bottle of soda/cola) was sufficient to account for the excess weight gain between 1988 to 1994 and 1999 to 2002.56
Foods and Nutrients
Several changes in foods and nutrients have occurred over time. Selected changes are highlighted:
Macronutrients
Starting in 1977 and continuing until the most recent dietary guidelines revision in 2005, a major focus of US dietary guidelines was reduction of total dietary fat.55 During this time, average total fat consumption declined as a percent of calories from 36.9% to 33.4% in men and from 36.1% to 33.8% in women (Chart 19-1).
Dietary guidelines during this time also emphasized carbohydrate consumption (eg, as the base of the Food Guide Pyramid),57 which increased from 42.4% to 48.2% of calories in men and from 45.4% to 50.6% of calories in women (Chart 19-1). Evaluated as absolute intakes, the increase in total calories consumed during this period was attributable primarily to the greater consumption of carbohydrates, both as foods (starches and grains) and as beverages.58,59
Sugar-Sweetened Beverages
Between 1965 and 2002, the average percentage of total calories consumed from beverages in the United States increased from 11.8% to 21.0% of energy, which represents an overall absolute increase of 222 cal/d per person.54 This increase was due largely to increased consumption of sugar-sweetened beverages and alcohol: Average consumption of fruit juices went from 20 to 39 kcal/d; of milk, from 125 to 94 kcal/d; of alcohol, from 26 to 99 kcal/d; of sweetened fruit drinks, from 13 to 38 kcal/d; and of soda/cola, from 35 to 143 kcal/d (Chart 19-2).
In addition to increased overall consumption, the average portion size of a single sugar-sweetened beverage increased by >50% between 1977 and 1996, from 13.1 to 19.9 fl oz.13
Among children and teenagers (2 to 19 years of age), the largest increases in consumption of sugar-sweetened beverages between 1988 to 1994 and 1999 to 2004 were seen among black and Mexican American youths compared with white youths.55
Chart 19-2.
Per-capita calories consumed from different beverages by US adults (≥19 years of age), 1965–2002. Data derived from Nationwide Food Consumption Surveys (1965, 1977–1978), National Health and Nutrition Examination Survey (1988–1994, 1999–2002), and Duffey and Popkin.54
Fruits and Vegetables
Between 1994 and 2005, the average consumption of fruits and vegetables declined slightly, from a total of 3.4 to 3.2 servings per day. The proportions of men and women consuming combined fruits and vegetables ≥5 times per day were low (≈20% and 29%, respectively) and did not change during this period.60
Morbidity and Mortality
Effects on Cardiovascular Risk Factors
In randomized controlled trials, dietary habits affect multiple cardiovascular risk factors, including both established risk factors (SBP, DBP, LDL cholesterol levels, HDL cholesterol levels, glucose levels, and obesity/weight gain) and novel risk factors (eg, inflammation, cardiac arrhythmias, endothelial cell function, triglyceride levels, lipoprotein(a) levels, and heart rate):
A DASH dietary pattern with low sodium reduced SBP by 7.1 mm Hg in adults without hypertension and by 11.5 mm Hg in adults with hypertension.61
Compared with the low-fat DASH diet, DASH-type diets that increased consumption of either protein or unsaturated fat had similar or greater beneficial effects on CVD risk factors. Compared with a baseline usual diet, each of the DASH-type diets, which included various percentages (27% to 37%) of total fat and focused on whole foods such as fruits, vegetables, whole grains, and fish, as well as potassium and other minerals and low sodium, reduced SBP by 8 to 10 mm Hg, DBP by 4 to 5 mm Hg, and LDL cholesterol by 12 to 14 mg/dL. The diets that had higher levels of protein and unsaturated fat also lowered triglyceride levels by 16 and 9 mg/dL, respectively.62
In a meta-analysis of randomized controlled trials, consumption of 1% of calories from trans fat in place of saturated fat, monounsaturated fat, or polyunsaturated fat increased the ratio of total to HDL cholesterol by 0.031, 0.054, and 0.67; increased apolipoprotein (apo) B levels by 3, 10, and 11 mg/L; decreased apoA-1 levels by 7, 5, and 3 mg/L; and increased lipoprotein(a) levels by 3.8, 1.4, and 1.1 mg/L, respectively.63
In meta-analyses of randomized controlled trials, consumption of EPA and DHA for ≥12 weeks lowered SBP by 2.1 mm Hg64 and resting heart rate by 2.5 bpm.65
A review of cross-sectional and prospective cohort studies suggests that higher intake of sugar-sweetened beverages is associated with greater visceral fat and higher risk of type 2 DM.66 In the PREMIER study, a prospective analysis of the 810 participants indicated that a reduction in sugar-sweetened beverages of 1 serving per day was associated with a reduction in SBP of 1.8 mm Hg (95% CI, 1.2 to 2.4) and in DBP of 1.1 mm Hg (95% CI, 0.7 to 1.4).67
In a randomized controlled trial, compared with a low-fat diet, 2 Mediterranean dietary patterns that included either virgin olive oil or mixed nuts lowered SBP by 5.9 and 7.1 mm Hg, plasma glucose by 7.0 and 5.4 mg/dL, fasting insulin by 16.7 and 20.4 pmol/L, the homeostasis model assessment (HOMA) index by 0.9 and 1.1, and the ratio of total to HDL cholesterol by 0.38 and 0.26 and raised HDL cholesterol by 2.9 and 1.6 mg/dL, respectively. The Mediterranean dietary patterns also lowered levels of C-reactive protein, interleukin-6, intercellular adhesion molecule-1, and vascular cell adhesion molecule-1.68
Effects on Cardiovascular Outcomes
Because dietary habits affect a broad range of established and novel risk factors, estimation of the impact of nutritional factors on cardiovascular health by considering only a limited number of pathways (eg, only effects on lipids, BP, and obesity) will systematically underestimate or even misconstrue the actual total impact on health. Randomized controlled trials and prospective observational studies can better quantify the total effects of dietary habits on clinical outcomes:
In the WHI randomized clinical trial, n = 48 835), reduction of total fat consumption from 37.8% energy (baseline) to 24.3% energy (at 1 year) and 28.8% energy (at 6 years) had no effect on incidence of CHD (RR, 0.98; 95% CI, 0.88 to 1.09), stroke (RR, 1.02; 95% CI, 0.90 to 1.15), or total CVD (RR, 0.98; 95% CI, 0.92 to 1.05) over a mean of 8.1 years.69 This was consistent with null results of 4 prior randomized clinical trials (see below) and multiple large prospective cohort studies (see below) that indicated little effect of total fat consumption on risk of CVD.70–79
In 3 separate meta-analyses of prospective cohort studies, the largest including 21 studies with up to 2 decades of follow-up, saturated fat consumption overall had no significant association with incidence of CHD, stroke, or total CVD.80–82 However, in a pooled individual-level analysis of 11 prospective cohort studies, the specific exchange of polyunsaturated fat consumption in place of saturated fat was associated with lower CHD risk, with 13% lower risk for a 5% energy exchange (RR, 0.87; 95% CI, 0.70 to 0.97).83 These findings are consistent with a meta-analysis of randomized controlled trials in which increased polyunsaturated fat consumption in place of saturated fat reduced CHD risk, with 10% lower risk for a 5% energy exchange (RR, 0.90; 95% CI, 0.83 to 0.97).84
In a pooled analysis of individual-level data from 11 prospective cohort studies in the United States, Europe, and Israel that included 344 696 participants, each 5% energy of carbohydrate consumption in place of saturated fat was associated with a 7% higher risk of CHD (RR 1.07, 95% CI 1.01 to 1.14).83 Each 5% energy of monounsaturated fat consumption in place of saturated fat was not significantly associated with CHD risk.83
In a meta-analysis of prospective cohort studies, each 2% of calories from trans fat was associated with a 23% higher risk of CHD (RR, 1.23; 95% CI, 1.11 to 1.37).85
In meta-analyses of prospective cohort studies, each daily serving of fruits or vegetables was associated with a 4% lower risk of CHD (RR, 0.96; 95% CI, 0.93 to 0.99) and a 5% lower risk of stroke (RR, 0.95; 95% CI, 0.92 to 0.97).86,87
In a meta-analysis of prospective cohort studies, greater whole grain intake (2.5 compared with 0.2 servings per day) was associated with a 21% lower risk of CVD events (RR, 0.79; 95% CI, 0.73 to 0.85), with similar estimates for specific CVD outcomes (HD, stroke, fatal CVD) and in sex-specific analyses. In contrast, refined grain intake was not associated with lower risk of CVD (RR, 1.07; 95% CI, 0.94 to 1.22).88
In a meta-analysis of 16 prospective cohort studies including 326 572 generally healthy individuals in Europe, the United States, China, and Japan, fish consumption was associated with significantly lower risk of CHD mortality.89 Compared with no consumption, an estimated 250 mg/d of long-chain omega-3 fatty acids was associated with 35% lower risk of CHD death (P<0.001).
Higher estimated consumption of dietary sodium was not associated with lower CVD mortality in NHANES,90 although such findings may be limited by changes in behaviors that result from underlying risk (reverse causation). In a posthoc analysis of the Trials of Hypertension Prevention, participants randomized to low-sodium interventions had a 25% lower risk of CVD (RR, 0.75; 95% CI, 0.57 to 0.99) after 10 to 15 years of follow-up after the original trials.91
Among 88 520 generally healthy women in the Nurses’ Health Study who were 34 to 59 years of age in 1980 and were followed up from 1980 to 2004, regular consumption of sugar-sweetened beverages was independently associated with higher incidence of CHD, with 23% and 35% higher risk with 1 and ≥2 servings per day, respectively, compared with <1 per month.92 Among the 15 745 participants in Atherosclerosis Risk in Communities Study, the odds ratio for developing chronic kidney disease was 2.59 for participants who had a serum uric acid level >9.0 mg/dL and who drank >1 sugar-sweetened soda per day.93
In a cohort of 380 296 US men and women, greater versus lower adherence to a Mediterranean dietary pattern, characterized by higher intakes of vegetables, legumes, nuts, fruits, whole grains, fish, and unsaturated fat and lower intakes of red and processed meat, was associated with a 22% lower cardiovascular mortality (RR, 0.78; 95% CI, 0.69 to 0.87).94 In a cohort of 72 113 US female nurses, a dietary pattern characterized by higher intakes of vegetables, fruits, legumes, fish, poultry, and whole grains was associated with a 28% lower cardiovascular mortality (RR, 0.72; 95% C,I 0.60 to 0.87), whereas a dietary pattern characterized by higher intakes of processed meat, red meat, refined grains, French fries, and sweets/desserts was associated with a 22% higher cardiovascular mortality (RR, 1.22; 95% CI, 1.01 to 1.48).95 Similar findings have been seen in other cohorts and for other outcomes, including development of DM and metabolic syndrome.96–100
In one report that used consistent and comparable risk assessment methods and nationally representative data, the mortality effects in the United States of 12 modifiable dietary, lifestyle, and metabolic risk factors were assessed. High dietary salt consumption was estimated to be responsible for 102 000 annual deaths, low dietary omega-3 fatty acids for 84 000 annual deaths, high dietary trans fatty acids for 82 000 annual deaths, and low consumption of fruits and vegetables for 55 000 annual deaths.101
Cost
The USDA forecast that the Consumer Price Index for all food would increase 4.5% to 5.5% in 2008 as retailers continued to pass on higher commodity and energy costs to consumers in the form of higher retail prices. The Consumer Price Index for food increased 4.0% in 2007, the highest annual increase since 1990. Prices for foods eaten at home increased 4.2% in 2007, whereas prices for foods eaten away from home increased by 3.6%.55
The proportion of total US food expenditures for meals outside the home, as a share of total food dollars, increased from 25% in 1957 to 38% in 1977 to 49% in 200757 (Chart 19-3).
The proportion of sales of meals and snacks from fast food restaurants compared with total meals and snacks away from home increased from 5% in 1958 to 28% in 1977 to 37% in 2007.102
As a proportion of income, food has become less expensive over time in the United States. As a share of personal disposable income, average (mean) total food expenditures by families and individuals have decreased from 23.5% (1947) to 18.4% (1957) to 13.4% (1977) to 9.8% (2007). For any given year, the share of disposable income spent on food is inversely proportional to absolute income; the share increases as absolute income levels decline.102
Among 154 forms of fruits and vegetables priced with ACNielsen Homescan data, more than half were estimated to cost 25 cents per serving. Consumers could meet a recommendation of 3 servings of fruits and 4 servings of vegetables daily for a total cost of 64 cents per day.102
An overview of the costs of various strategies for primary prevention of CVD determined that the estimated costs per year of life gained were between $9800 and $18 000 for statin therapy, $1500 or more for nurse screening and lifestyle advice, $500 to $1250 for smoking cessation, and $20 to $900 for population-based healthy eating.103
Each year, more than $33 billion in medical costs and $9 billion in lost productivity resulting from HD, cancer, stroke, and DM are attributed to poor nutrition.104–109
Abbreviations Used in Chapter 19
- apo
apolipoprotein
- BMI
body mass index
- BP
blood pressure
- bpm
beats per minute
- BRFSS
Behavioral Risk Factor Surveillance System
- Cal/d
calories per day
- CHD
coronary heart disease
- CI
confidence interval
- CVD
cardiovascular disease
- DASH
Dietary Approaches to Stop Hypertension
- DBP
diastolic blood pressure
- DHA
docosahexaenoic acid
- DHHS
US Department of Health and Human Services
- DM
diabetes mellitus
- EPA
eicosapentaenoic acid
- g
grams
- GISSI
Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico
- HD
heart disease
- HDL
high-density lipoprotein
- HEI
Healthy Eating Index
- HOMA
homeostasis model assessment
- kCal
kilocalories
- LDL
low-density lipoprotein
- mg
milligrams
- mg/dL
milligrams per deciliter
- mg/L
milligrams per liter
- mm Hg
millimeters of mercury
- NHANES
National Health and Nutrition Examination Survey
- PA
physical activity
- pmol
picomoles per liter
- RR
relative risk
- SBP
systolic blood pressure
- SD
standard deviation
- USDA
US Department of Agriculture
- WHI
Women’s Health Initiative
References
- 1.Centers for Disease Control and Prevention. Application of lower sodium intake recommendations to adults: United States, 1999–2006. MMWR Morb Mortal Wkly Rep. 2009;58:281–283. [PubMed] [Google Scholar]
- 2.Ello-Martin JA, Ledikwe JH, Rolls BJ. The influence of food portion size and energy density on energy intake: implications for weight management. Am J Clin Nutr. 2005;82(suppl):236S–241S. doi: 10.1093/ajcn/82.1.236S. [DOI] [PubMed] [Google Scholar]
- 3.Fisher JO, Kral TV. Super-size me: portion size effects on young children’s eating. Physiol Behav. 2008;94:39–47. doi: 10.1016/j.physbeh.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr. 2006;84:274–288. doi: 10.1093/ajcn/84.1.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sichieri R, Paula Trotte A, de Souza RA, Veiga GV. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr. 2009;11:197–202. doi: 10.1017/S1368980008002644. [DOI] [PubMed] [Google Scholar]
- 6.Bowman Vinyard BT. Fast food consumption of U.S. adults: impact on energy and nutrient intakes and overweight status. J Am Coll Nutr. 2004;23:163–168. doi: 10.1080/07315724.2004.10719357. [DOI] [PubMed] [Google Scholar]
- 7.Kant AK, Graubard BI. Eating out in America, 1987–2000: trends and nutritional correlates. Prev Med. 2004;38:243–249. doi: 10.1016/j.ypmed.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Duerksen SC, Elder JP, Arredondo EM, Ayala GX, Slymen DJ, Campbell NR, Baquero B. Family restaurant choices are associated with child and adult overweight status in Mexican-American families. J Am Diet Assoc. 2007;107:849–853. doi: 10.1016/j.jada.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 9.Duffey KJ, Gordon-Larsen P, Jacobs DR, Jr, Williams OD, Popkin BM. Differential associations of fast food and restaurant food consumption with 3-y change in body mass index: the Coronary Artery Risk Development in Young Adults Study. Am J Clin Nutr. 2007;85:201–208. doi: 10.1093/ajcn/85.1.201. [DOI] [PubMed] [Google Scholar]
- 10.Rosenheck R. Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obes Rev. 2008;9:535–547. doi: 10.1111/j.1467-789X.2008.00477.x. [DOI] [PubMed] [Google Scholar]
- 11.Burger KS, Kern M, Coleman KJ. Characteristics of self-selected portion size in young adults. J Am Diet Assoc. 2007;107:611–618. doi: 10.1016/j.jada.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Colapinto CK, Fitzgerald A, Taper LJ, Veugelers PJ. Children’s preference for large portions: prevalence, determinants, and consequences. J Am Diet Assoc. 2007;107:1183–1190. doi: 10.1016/j.jada.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 13.Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977–1998. JAMA. 2003;289:450–453. doi: 10.1001/jama.289.4.450. [DOI] [PubMed] [Google Scholar]
- 14.Health, United States 2007, With Chartbook on Trends in the Health of Americans. Hyattsville, Md: National Center for Health Statistics; 2007. National Center for Health Statistics. [PubMed] [Google Scholar]
- 15.Willett WC, Leibel RL. Dietary fat is not a major determinant of body fat. Am J Med. 2002;113(suppl 9B):47S–59S. doi: 10.1016/s0002-9343(01)00992-5. [DOI] [PubMed] [Google Scholar]
- 16.Brehm BJ, D’Alessio DA. Weight loss and metabolic benefits with diets of varying fat and carbohydrate content: separating the wheat from the chaff. Nat Clin Pract Endocrinol Metab. 2008;4:140–146. doi: 10.1038/ncpendmet0730. [DOI] [PubMed] [Google Scholar]
- 17.van Dam RM, Seidell JC. Carbohydrate intake and obesity. Eur J Clin Nutr. 2007;61(suppl 1):S75–S99. doi: 10.1038/sj.ejcn.1602939. [DOI] [PubMed] [Google Scholar]
- 18.Koh-Banerjee P, Chu NF, Spiegelman D, Rosner B, Colditz G, Willett W, Rimm E. Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16 587 US men. Am J Clin Nutr. 2003;78:719–727. doi: 10.1093/ajcn/78.4.719. [DOI] [PubMed] [Google Scholar]
- 19.Field AE, Willett WC, Lissner L, Colditz GA. Dietary fat and weight gain among women in the Nurses’ Health Study. Obesity (Silver Spring) 2007;15:967–976. doi: 10.1038/oby.2007.616. [DOI] [PubMed] [Google Scholar]
- 20.Kavanagh K, Jones KL, Sawyer J, Kelley K, Carr JJ, Wagner JD, Rudel LL. Trans fat diet induces abdominal obesity and changes in insulin sensitivity in monkeys. Obesity (Silver Spring) 2007;15:1675–1684. doi: 10.1038/oby.2007.200. [DOI] [PubMed] [Google Scholar]
- 21.Rolls BJ, Roe LS, Beach AM, Kris-Etherton PM. Provision of foods differing in energy density affects long-term weight loss. Obes Res. 2005;13:1052–1060. doi: 10.1038/oby.2005.123. [DOI] [PubMed] [Google Scholar]
- 22.Ledikwe JH, Rolls BL, Smiciklas-Wright H, Mitchell DC, Ard JD, Champagne C, Karanja N, Lin PH, Stevens VJ, Appel LJ. Reductions in dietary energy density are associated with weight loss in overweight and obese participants in the PREMIER trial. Am J Clin Nutr. 2007;85:1212–1221. doi: 10.1093/ajcn/85.5.1212. [DOI] [PubMed] [Google Scholar]
- 23.Ello-Martin JA, Roe LS, Ledikwe JH, Beach AM, Rolls BJ. Dietary energy density in the treatment of obesity: a year-long trial comparing 2 weight-loss diets. Am J Clin Nutr. 2007;85:1465–1477. doi: 10.1093/ajcn/85.6.1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nordmann AJ, Nordmann A, Briel M, Keller U, Yancy WS, Jr, Brehm BJ, Bucher HC. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials [published correction appears in Arch Intern Med. 2006;166:285–293] Arch Intern Med. 2006;166:285–293. doi: 10.1001/archinte.166.3.285. [DOI] [PubMed] [Google Scholar]
- 25.Gardner CD, Kiazand A, Alhassan S, Kim S, Stafford RS, Balise RR, Kraemer HC, King AC. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial [published correction appears in JAMA. 2007;298:178] JAMA. 2007;297:969–977. doi: 10.1001/jama.297.9.969. [DOI] [PubMed] [Google Scholar]
- 26.Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, Golan R, Fraser D, Bolotin A, Vardi H, Tangi-Rozental O, Zuk-Ramot R, Sarusi B, Brickner D, Schwartz Z, Sheiner E, Marko R, Katorza E, Thiery J, Fiedler GM, Blüher M, Stumvoll M, Stampfer MJ Dietary Intervention Randomized Controlled Trial (DIRECT) Group. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008;359:229–241. doi: 10.1056/NEJMoa0708681. [DOI] [PubMed] [Google Scholar]
- 27.Andreyeva T, Long MW, Henderson KE, Grode GM. Trying to lose weight: diet strategies among Americans with overweight or obesity in 1996 and 2003. J Am Diet Assoc. 2010;110:535–542. doi: 10.1016/j.jada.2009.12.029. [DOI] [PubMed] [Google Scholar]
- 28.Gortmaker SL, Must A, Sobol AM, Peterson K, Colditz GA, Dietz WH. Television viewing as a cause of increasing obesity among children in the United States, 1986–1990. Arch Pediatr Adolesc Med. 1996;150:356–362. doi: 10.1001/archpedi.1996.02170290022003. [DOI] [PubMed] [Google Scholar]
- 29.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 30.Gable S, Chang Y, Krull JL. Television watching and frequency of family meals are predictive of overweight onset and persistence in a national sample of school-aged children. J Am Diet Assoc. 2007;107:53–61. doi: 10.1016/j.jada.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 31.Temple JL, Giacomelli AM, Kent KM, Roemmich JN, Epstein LH. Television watching increases motivated responding for food and energy intake in children. Am J Clin Nutr. 2007;85:355–361. doi: 10.1093/ajcn/85.2.355. [DOI] [PubMed] [Google Scholar]
- 32.Dubois L, Farmer A, Girard M, Peterson K. Social factors and television use during meals and snacks is associated with higher BMI among pre-school children. Public Health Nutr. 2008;11:1267–1279. doi: 10.1017/S1368980008002887. [DOI] [PubMed] [Google Scholar]
- 33.Epstein LH, Roemmich JN, Robinson JL, Paluch RA, Winiewicz DD, Fuerch JH, Robinson TN. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med. 2008;162:239–245. doi: 10.1001/archpediatrics.2007.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16:643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Farley TA, Baker ET, Futrell L, Rice JC. The ubiquity of energy-dense snack foods: a national multicity study. Am J Public Health. 2010;100:306–311. doi: 10.2105/AJPH.2009.178681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumanyika S, Grier S. Targeting interventions for ethnic minority and low-income populations. Future Child. 2006;16:187–207. doi: 10.1353/foc.2006.0005. [DOI] [PubMed] [Google Scholar]
- 37.Sallis JF, Glanz K. The role of built environments in physical activity, eating, and obesity in childhood. Future Child. 2006;16:89–108. doi: 10.1353/foc.2006.0009. [DOI] [PubMed] [Google Scholar]
- 38.Li F, Harmer PA, Cardinal BJ, Bosworth M, Acock A, Johnson-Shelton D, Moore JM. Built environment, adiposity, and physical activity in adults aged 50–75. Am J Prev Med. 2008;35:38–46. doi: 10.1016/j.amepre.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mellen PB, Gao SK, Vitolins MZ, Goff DC., Jr Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988–1994 and 1999–2004. Arch Intern Med. 2008;168:308–314. doi: 10.1001/archinternmed.2007.119. [DOI] [PubMed] [Google Scholar]
- 40.Ervin RB. Healthy Eating Index Scores Among Adults, 60 Years of Age and Over, by Sociodemographic and Health Characteristics: United States, 1999–2002. Hyattsville, Md: National Center for Health Statistics; 2008. Advance Data From Vital and Health Statistics No. 395. [PubMed] [Google Scholar]
- 41.Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women [published correction appears in Circulation. 2009;119:e379] Circulation. 2009;119:1093–1100. doi: 10.1161/CIRCULATIONAHA.108.816736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Radimer K, Bindewald B, Hughes J, Ervin B, Swanson C, Picciano MF. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999–2000. Am J Epidemiol. 2004;160:330–349. doi: 10.1093/aje/kwh207. [DOI] [PubMed] [Google Scholar]
- 43.Picciano MF, Dwyer JT, Radimer KL, Wilson DH, Fisher KD, Thomas PR, Yetley EA, Moshfegh AJ, Levy PS, Nielsen SJ, Marriott BM. Dietary supplement use among infants, children, and adolescents in the United States, 1999–2002. Arch Pediatr Adolesc Med. 2007;161:978–985. doi: 10.1001/archpedi.161.10.978. [DOI] [PubMed] [Google Scholar]
- 44.Pillitteri JL, Shiffman S, Rohay JM, Harkins AM, Burton SL, Wadden TA. Use of dietary supplements for weight loss in the United States: results of a national survey. Obesity (Silver Spring) 2008;16:790–796. doi: 10.1038/oby.2007.136. [DOI] [PubMed] [Google Scholar]
- 45.Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial [published corrections appear in Lancet. 2001;357:642 and Lancet. 2007;369:106] Lancet. 1999;354:447–455. [PubMed] [Google Scholar]
- 46.Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, Oikawa S, Sasaki J, Hishida H, Itakura H, Kita T, Kitabatake A, Nakaya N, Sakata T, Shimada K, Shirato K, Japan EPA Lipid Intervention Study (JELIS) Investigators. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis [published correction appears in Lancet. 2007;370:220] Lancet. 2007;369:1090–1098. doi: 10.1016/S0140-6736(07)60527-3. [DOI] [PubMed] [Google Scholar]
- 47.GISSI-HF Investigators. Tavazzi L, Maggioni AP, Marchioli R, Barlera S, Franzosi MG, Latini R, Lucci D, Nicolosi GL, Porcu M, Tognoni G. Effect of n-3 polyunsaturated fatty acids in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372:1223–1230. doi: 10.1016/S0140-6736(08)61239-8. [DOI] [PubMed] [Google Scholar]
- 48.House AA, Eliasziw M, Cattran DC, Churchill DN, Oliver MJ, Fine A, Dresser GK, Spence JD. Effect of B-vitamin therapy on progression of diabetic nephropathy: a randomized controlled trial. JAMA. 2010;303:1603–1609. doi: 10.1001/jama.2010.490. [DOI] [PubMed] [Google Scholar]
- 49.Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. The spread of the obesity epidemic in the United States, 1991–1998. JAMA. 1999;282:1519–1522. doi: 10.1001/jama.282.16.1519. [DOI] [PubMed] [Google Scholar]
- 50.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 51.Briefel RR, Johnson CL. Secular trends in dietary intake in the United States. Annu Rev Nutr. 2004;24:401–431. doi: 10.1146/annurev.nutr.23.011702.073349. [DOI] [PubMed] [Google Scholar]
- 52.Kant AK, Graubard BI. Secular trends in patterns of self-reported food consumption of adult Americans: NHANES 1971–1975 to NHANES 1999–2002. Am J Clin Nutr. 2006;84:1215–1223. doi: 10.1093/ajcn/84.5.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Popkin BM, Armstrong LE, Bray GM, Caballero B, Frei B, Willett WC. A new proposed guidance system for beverage consumption in the United States [published correction appears in Am J Clin Nutr. 2007;86:525] Am J Clin Nutr. 2006;83:529–542. doi: 10.1093/ajcn.83.3.529. [DOI] [PubMed] [Google Scholar]
- 54.Duffey KJ, Popkin BM. Shifts in patterns and consumption of beverages between 1965 and 2002. Obesity (Silver Spring) 2007;15:2739–2747. doi: 10.1038/oby.2007.326. [DOI] [PubMed] [Google Scholar]
- 55.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988 –2004. Pediatrics. 2008;121:e1604–e1614. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 56.Wang YC, Gortmaker SL, Sobol AM, Kuntz KM. Estimating the energy gap among US children: a counterfactual approach. Pediatrics. 2006;118:e1721–e1733. doi: 10.1542/peds.2006-0682. [DOI] [PubMed] [Google Scholar]
- 57.Davis C, Saltos E. Dietary recommendations and how they have changed over time. In: Frazao E, editor. America’s Eating Habits: Changes and Consequences. Washington, DC: US Department of Agriculture, Economic Research Service, Food and Rural Economics Division; 1999. [Accessed September 28, 2010]. Agriculture Information Bulletin No. AIB750. Available at: http://www.ers.usda.gov/publications/aib750/aib750b.pdf. [Google Scholar]
- 58.Centers for Disease Control and Prevention (CDC) Trends in intake of energy and macronutrients: United States, 1971–2000. MMWR Morb Mortal Wkly Rep. 2004;53:80–82. [PubMed] [Google Scholar]
- 59.Egan SK, Bolger PM, Carrington CD. Update of US FDA’s Total Diet Study food list and diets. J Expo Sci Environ Epidemiol. 2007;17:573–582. doi: 10.1038/sj.jes.7500554. [DOI] [PubMed] [Google Scholar]
- 60.Blanck HM, Gillespie C, Kimmons JE, Seymour JD, Serdula MK. Trends in fruit and vegetable consumption among U.S. men and women, 1994–2005. Prev Chronic Dis. 2008;5:A35. [PMC free article] [PubMed] [Google Scholar]
- 61.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, III, Simons-Morton DG, Karanja N, Lin PH DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet: DASH–Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 62.Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER, III, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, Charleston J, McCarron P, Bishop LM Omni Heart Collaborative Research Group. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA. 2005;294:2455–2464. doi: 10.1001/jama.294.19.2455. [DOI] [PubMed] [Google Scholar]
- 63.Uauy R, Aro A, Clarke R, Ghafoorunissa R, L’Abbe M, Mozaffarian D, Skeaff M, Stender S, Tavella M. WHO Scientific Update on trans fatty acids: summary and conclusions. Eur J Clin Nutr. 2009;63:S68–S75. [Google Scholar]
- 64.Geleijnse JM, Giltay EJ, Grobbee DE, Donders AR, Kok FJ. Blood pressure response to fish oil supplementation: metaregression analysis of randomized trials. J Hypertens. 2002;20:1493–1499. doi: 10.1097/00004872-200208000-00010. [DOI] [PubMed] [Google Scholar]
- 65.Mozaffarian D, Geelen A, Brouwer IA, Geleijnse JM, Zock PL, Katan MB. Effect of fish oil on heart rate in humans: a meta-analysis of randomized controlled trials. Circulation. 2005;112:1945–1952. doi: 10.1161/CIRCULATIONAHA.105.556886. [DOI] [PubMed] [Google Scholar]
- 66.Hu FB, Malik VS. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav. 2010;100:47–54. doi: 10.1016/j.physbeh.2010.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen L, Caballero B, Mitchell DC, Loria C, Lin PH, Champagne CM, Elmer PJ, Ard JD, Batch BC, Anderson CAM. Reducing consumption of sugar-sweetened beverages is associated with reduced blood pressure: a prospective study among United States adults. Circulation. 2010;121:2398–2406. doi: 10.1161/CIRCULATIONAHA.109.911164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, Fiol M, Gómez-Gracia E, López-Sabater MC, Vinyoles E, Arós F, Conde M, Lahoz C, Lapetra J, Sáez G, Ros E PREDIMED Study Investigators. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med. 2006;145:1–11. doi: 10.7326/0003-4819-145-1-200607040-00004. [DOI] [PubMed] [Google Scholar]
- 69.Howard BV, Van Horn L, Hsia J, Manson JE, Stefanick ML, Wassertheil-Smoller S, Kuller LH, LaCroix AZ, Langer RD, Lasser NL, Lewis CE, Limacher MC, Margolis KL, Mysiw WJ, Ockene JK, Parker LM, Perri MG, Phillips L, Prentice RL, Robbins J, Rossouw JE, Sarto GE, Schatz IJ, Snetselaar LG, Stevens VJ, Tinker LF, Trevisan M, Vitolins MZ, Anderson GL, Assaf AR, Bassford T, Beresford SA, Black HR, Brunner RL, Brzyski RG, Caan B, Chlebowski RT, Gass M, Granek I, Greenland P, Hays J, Heber D, Heiss G, Hendrix SL, Hubbell FA, Johnson KC, Kotchen JM. Low-fat dietary pattern and risk of cardiovascular disease: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:655–666. doi: 10.1001/jama.295.6.655. [DOI] [PubMed] [Google Scholar]
- 70.Research Committee to the Medical Research Council. Low-fat diet in myocardial infarction: a controlled trial. Lancet. 1965;2:501–504. [PubMed] [Google Scholar]
- 71.World Health Organisation European Collaborative Group. European collaborative trial of multifactorial prevention of coronary heart disease: final report on the 6-year results. Lancet. 1986;1:869–872. [PubMed] [Google Scholar]
- 72.Multiple Risk Factor Intervention Trial Research Group. Mortality rates after 10.5 years for participants in the Multiple Risk Factor Intervention Trial: findings related to a priori hypotheses of the trial [published correction appears in JAMA. 1990;263:3151] JAMA. 1990;263:1795–1801. doi: 10.1001/jama.1990.03440130083030. [DOI] [PubMed] [Google Scholar]
- 73.Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM, Elwood PC, Deadman NM. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: Diet and Reinfarction Trial (DART) Lancet. 1989;2:757–761. doi: 10.1016/s0140-6736(89)90828-3. [DOI] [PubMed] [Google Scholar]
- 74.Ascherio A, Rimm EB, Giovannucci EL, Spiegelman D, Stampfer M, Willett WC. Dietary fat and risk of coronary heart disease in men: cohort follow up study in the United States. BMJ. 1996;313:84–90. doi: 10.1136/bmj.313.7049.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pietinen P, Ascherio A, Korhonen P, Hartman AM, Willett WC, Albanes D, Virtamo J. Intake of fatty acids and risk of coronary heart disease in a cohort of Finnish men: the Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study. Am J Epidemiol. 1997;145:876–887. doi: 10.1093/oxfordjournals.aje.a009047. [DOI] [PubMed] [Google Scholar]
- 76.Gillman MW, Cupples LA, Millen BE, Ellison RC, Wolf PA. Inverse association of dietary fat with development of ischemic stroke in men. JAMA. 1997;278:2145–2150. [PubMed] [Google Scholar]
- 77.Hu FB, Stampfer MJ, Manson JE, Rimm E, Colditz GA, Rosner BA, Hennekens CH, Willett WC. Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med. 1997;337:1491–1499. doi: 10.1056/NEJM199711203372102. [DOI] [PubMed] [Google Scholar]
- 78.He K, Merchant A, Rimm EB, Rosner BA, Stampfer MJ, Willett WC, Ascherio A. Dietary fat intake and risk of stroke in male US healthcare professionals: 14 year prospective cohort study. BMJ. 2003;327:777–782. doi: 10.1136/bmj.327.7418.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Oh K, Hu FB, Manson JE, Stampfer MJ, Willett WC. Dietary fat intake and risk of coronary heart disease in women: 20 years of follow-up of the Nurses’ Health Study. Am J Epidemiol. 2005;161:672–679. doi: 10.1093/aje/kwi085. [DOI] [PubMed] [Google Scholar]
- 80.Skeaff CM, Miller J. Dietary fat and coronary heart disease: summary of evidence from prospective cohort and randomised controlled trials. Ann Nutr Metab. 2009;55:173–201. doi: 10.1159/000229002. [DOI] [PubMed] [Google Scholar]
- 81.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169:659–669. doi: 10.1001/archinternmed.2009.38. [DOI] [PubMed] [Google Scholar]
- 82.Siri-Tarino P, Sun Q, Hu F, Krauss R. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr. 2010;91:535–546. doi: 10.3945/ajcn.2009.27725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jakobsen MU, O’Reilly EJ, Heitmann BL, Pereira MA, Bälter K, Fraser GE, Goldbourt U, Hallmans G, Knekt P, Liu S, Pietinen P, Spiegelman D, Stevens J, Virtamo J, Willett WC, Ascherio A. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr. 2009;89:1425–1432. doi: 10.3945/ajcn.2008.27124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7:e1000252. doi: 10.1371/journal.pmed.1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC. Trans fatty acids and cardiovascular disease. N Engl J Med. 2006;354:1601–1613. doi: 10.1056/NEJMra054035. [DOI] [PubMed] [Google Scholar]
- 86.Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr. 2006;136:2588–2593. doi: 10.1093/jn/136.10.2588. [DOI] [PubMed] [Google Scholar]
- 87.Dauchet L, Amouyel P, Dallongeville J. Fruit and vegetable consumption and risk of stroke: a meta-analysis of cohort studies. Neurology. 2005;65:1193–1197. doi: 10.1212/01.wnl.0000180600.09719.53. [DOI] [PubMed] [Google Scholar]
- 88.Mellen PB, Walsh TF, Herrington DM. Whole grain intake and cardiovascular disease: a meta-analysis. Nutr Metab Cardiovasc Dis. 2008;18:283–290. doi: 10.1016/j.numecd.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 89.Harris WS, Mozaffarian D, Lefevre M, Toner CD, Colombo J, Cunnane SC, Holden JM, Klurfeld DM, Morris MC, Whelan J. Towards establishing dietary reference intakes for eicosapentaenoic and docosahexaenoic acids. J Nutr. 2009;139:804S–819S. doi: 10.3945/jn.108.101329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cohen HW, Hailpern SM, Alderman MH. Sodium intake and mortality follow-up in the Third National Health and Nutrition Examination Survey (NHANES III) J Gen Intern Med. 2008;23:1297–1302. doi: 10.1007/s11606-008-0645-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, Appel LJ, Whelton PK. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the Trials of Hypertension Prevention (TOHP) BMJ. 2007;334:885–888. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fung TT, Malik V, Rexrode KM, Manson JE, Willett WC, Hu FB. Sweetened beverage consumption and risk of coronary heart disease in women. Am J Clin Nutr. 2009;89:1037–1042. doi: 10.3945/ajcn.2008.27140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bomback AS, Derebail VK, Shoham DA, Anderson CA, Steffen LM, Rosamond WD, Kshirsagar AV. Sugar-sweetened soda consumption, hyperuricemia, and kidney disease. Kidney Int. 2010;77:609–616. doi: 10.1038/ki.2009.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mitrou PN, Kipnis V, Thiébaut AC, Reedy J, Subar AF, Wirfält E, Flood A, Mouw T, Hollenbeck AR, Leitzmann MF, Schatzkin A. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH-AARP Diet and Health Study. Arch Intern Med. 2007;167:2461–2468. doi: 10.1001/archinte.167.22.2461. [DOI] [PubMed] [Google Scholar]
- 95.Heidemann C, Schulze MB, Franco OH, van Dam RM, Mantzoros CS, Hu FB. Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation. 2008;118:230–237. doi: 10.1161/CIRCULATIONAHA.108.771881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Osler M, Heitmann BL, Gerdes LU, Jørgensen LM, Schroll M. Dietary patterns and mortality in Danish men and women: a prospective observational study. Br J Nutr. 2001;85:219–225. doi: 10.1079/bjn2000240. [DOI] [PubMed] [Google Scholar]
- 97.van Dam RM, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Dietary patterns and risk for type 2 diabetes mellitus in U.S. men. Ann Intern Med. 2002;136:201–209. doi: 10.7326/0003-4819-136-3-200202050-00008. [DOI] [PubMed] [Google Scholar]
- 98.Heidemann C, Hoffmann K, Spranger J, Klipstein-Grobusch K, Möhlig M, Pfeiffer AF, Boeing H. European Prospective Investigation Into Cancer and Nutrition (EPIC)–Potsdam Study Cohort. A dietary pattern protective against type 2 diabetes in the European Prospective Investigation Into Cancer and Nutrition (EPIC)–Potsdam Study cohort. Diabetologia. 2005;48:1126–1134. doi: 10.1007/s00125-005-1743-1. [DOI] [PubMed] [Google Scholar]
- 99.Brunner EJ, Mosdøl A, Witte DR, Martikainen P, Stafford M, Shipley MJ, Marmot MG. Dietary patterns and 15-y risks of major coronary events, diabetes, and mortality. Am J Clin Nutr. 2008;87:1414–1421. doi: 10.1093/ajcn/87.5.1414. [DOI] [PubMed] [Google Scholar]
- 100.Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation. 2008;117:754–761. doi: 10.1161/CIRCULATIONAHA.107.716159. [DOI] [PubMed] [Google Scholar]
- 101.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.United States Department of Agriculture. Food CPI and expenditures. [Accessed September 28, 2010]; Available at: http://www.ers.usda.gov/Briefing/CPIFoodAndExpendi-tures/Data/.
- 103.Brunner E, Cohen D, Toon L. Cost effectiveness of cardiovascular disease prevention strategies: a perspective on EU food based dietary guidelines. Public Health Nutr. 2001;4:711–715. doi: 10.1079/phn2001161. [DOI] [PubMed] [Google Scholar]
- 104.Centers for Disease Control and Prevention. Preventing Chronic Diseases: Investing Wisely in Health: Preventing Obesity and Chronic Diseases Through Good Nutrition and Physical Activity. Atlanta, Ga: US Department of Health and Human Services; [Accessed September 28, 2010]. Revised 2008. Available at: http://www.cdc.gov/nccdphp/publications/factsheets/prevention/pdf/obesity.pdf. [Google Scholar]
- 105.The Power of Prevention. Rockville, Md: US Department of Health and Human Services, Office of Public Health and Science, Office of Disease Prevention and Health Promotion; 2003. [Accessed September 28, 2010]. Steps to a Healthier US Cooperative Agreement Program. Available at: http://www.healthierus.gov/steps/summit/prevportfolio/power/index.html. [Google Scholar]
- 106.Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Franklin B, Kris-Etherton P, Harris WS, Howard B, Karanja N, Lefevre M, Rudel L, Sacks F, Van Horn L, Winston M, Wylie-Rosett J. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee [published corrections appear in Circulation. 2006; 114:e629 and Circulation. 2006;114:e27] Circulation. 2006;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 107.US Department of Health and Human Services. [Accessed September 28, 2010];Dietary Guidelines for Americans. Available at: http://www.health.gov/dietaryguidelines/dga2005/report/.
- 108.Recommendations for Dietary Intake of Polyunsaturated Fatty Acids in Healthy Adults. Devon, UK: International Society for the Study of Fatty Acids and Lipids; 2004. International Society for the Study of Fatty Acids and Lipids. [Google Scholar]
- 109.Dietary Reference Intakes for Energy, Carbohydrate, Fiber Fat Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) Washington, DC: Institute of Medicine, National Academies Press; 2005. Food and Nutrition Board, Institute of Medicine. [Google Scholar]
20. Quality of Care
See Tables 20-1 through 20-11.
Table 20-1.
Acute Coronary Syndrome Quality-of-Care Measures, 2009
| Quality-of-Care Measure | VHA* | National Medicare and Medicaid† |
AHA GWTG- CAD‡ |
ACTION/GWTG- STEMI§ |
ACTION/GWTG- NSTEMI§ |
|---|---|---|---|---|---|
| Aspirin within 24 h of admission | 99 | 98 | 91‖ | 99 | 97 |
| Aspirin at discharge | 99 | 98 | 96‖ | 99 | 97 |
| β-blockers within 24 h of admission among AMI and angina patients | 97 | 95 | NM | NM | NM |
| β-blockers at discharge | 99 | 98 | 95‖ | 97 | 95 |
| Lipid-lowering medication at discharge | 92 | NM | 87 | 98 | 97 |
| Lipid therapy at discharge if LDL >100 mg/dL | 97¶ | NM | 93‖ | NM | NM |
| ARB/ACEI at discharge for patients with LVEF <40% | 96 | 95 | 92‖ | 88 | 84 |
| ACEI at discharge for AMI patients | 75 | NM | 66‖ | NM | NM |
| Adult smoking cessation advice/counseling | 99 | 99 | 98‖ | 98 | 97 |
| Cardiac rehabilitation referral for AMI patients | NM | NM | 49 | 84 | 74 |
VHA indicates Veterans Health Administration; AHA GWTG-CAD, American Heart Association’s Get With The Guidelines–Coronary Artery Disease; ACTION/GWTG-STEMI, Acute Coronary Treatment and Intervention Outcomes Network/Get With The Guidelines–ST-Elevation Myocardial Infarction; ACTION/GWTG-NSTEMI, Acute Coronary Treatment and Intervention Outcomes Network/Get With The Guidelines–Non–ST-Elevation Myocardial Infarction; AMI, acute myocardial infarction; NM, not measured; LDL, low-density lipoprotein; ARB, angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; LVEF, left ventricular ejection fraction.
Values are percentages.
VHA: AMI patients.
National Medicare and Medicaid: AMI patients.
AHA GWTG-CAD: Patients admitted with a cardiovascular event. In the GWTG-CAD registry, the in-hospital mortality rate was 4.5% (excludes transfer-out patients; if discharge status was missing, it was assumed to be “no.”). The mean length of hospital stay was 5.0 days (median 3.0 days).
ACTION Registry: STEMI and NSTEMI patients were reported separately. Patients must have been admitted with acute ischemic symptoms within the previous 24 hours, typically reflected by a primary diagnosis of STEMI or NSTEMI. Patients who were admitted for any other clinical condition were not eligible.
Indicates the 7 key achievement measures targeted in GWTG-CAD. The composite quality-of-care measure for 2009 was 94.4%. The composite quality-of-care measure indicates performance on the provision of several elements of care. It is computed by summing the numerators for each key performance measure across the population of interest to create a composite numerator (all the care that was given), summing the denominators for each measure to form a composite denominator (all the care that should have been given), and reporting the ratio (the percentage of all the needed care that was given).
Lipid-lowering therapy among patients with LDL >130 mg/dL.
Table 20-11.
Quality of Care by Race/Ethnicity and Sex in the GWTG-Stroke Program, 2009
| Race/Ethnicity | Sex | |||||
|---|---|---|---|---|---|---|
| Quality-of-Care Measure | Overall | White | Black | Hispanic | Male | Female |
| IV tPA in patients who arrived <2 h after symptom onset* | 73.1 | 73.2 | 72.7 | 73.0 | 74.6 | 71.7 |
| IV tPA in patients who arrived <3 h after symptom onset | 67.1 | 67.0 | 67.6 | 66.9 | 69.0 | 65.4 |
| No IV-tPA (contraindicated/warning) | 82.4 | 82.6 | 82.1 | 80.4 | 83.0 | 81.9 |
| Thrombolytic complications: IV tPA and life-threatening, serious systemic hemorrhage | 15.1 | 15.1 | 13.7 | 16.2 | 14.3 | 16.0 |
| Antithrombotics <48 h after admission* | 96.2 | 96.4 | 95.8 | 95.3 | 96.6 | 95.8 |
| DVT prophylaxis by second hospital day* | 92.7 | 92.8 | 92.9 | 91.7 | 93.0 | 92.4 |
| Antithrombotics at discharge* | 97.8 | 97.9 | 97.3 | 96.9 | 98.1 | 97.5 |
| Anticoagulation for atrial fibrillation at discharge* | 93.5 | 93.8 | 91.9 | 91.3 | 93.9 | 93.2 |
| Therapy at discharge if LDL >100 mg/dL or LDL not measured or on therapy at admission* | 86.2 | 86.0 | 86.7 | 86.7 | 88.8 | 84.0 |
| Counseling for smoking cessation* | 96.2 | 96.5 | 96.5 | 94.8 | 96.4 | 96.1 |
| Lifestyle changes recommended for BMI >25 kg/m2 | 57.3 | 56.6 | 58.7 | 62.6 | 57.5 | 57.1 |
| Composite quality-of-care measure† | 93.3 | 93.3 | 93.4 | 92.6 | 94.1 | 92.5 |
GWTG-Stroke indicates Get With The Guidelines–Stroke; IV tPA, intravenous tissue-type plasminogen activator; DVT, deep venous thrombosis; LDL, low-density lipoprotein; BMI, body mass index.
Values are percentages.
In-hospital mortality for the 2009 patient population was 6.9%, and mean length of hospital stay was 5.3 days (median 3.0 days).
Indicates the 7 key performance measures targeted in GWTG-Stroke.
The composite quality-of-care measure indicates performance on the provision of several elements of care. It is computed by summing the numerators for each key achievement measure across the population of interest to create a composite numerator (all the care that was given), summing the denominators for each measure to form a composite denominator (all the care that should have been given), and reporting the ratio (the percentage of all the needed care that was given).
The Institute of Medicine (IOM) defines quality of care as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.”1 The IOM has defined 6 specific domains for improving health care, including care that is safe, effective, patient-centered, timely, efficient, and equitable.
In the following sections, data on quality of care will be presented based on the 6 domains of quality as defined by the IOM. This is intended to highlight current care and to stimulate efforts to improve the quality of cardiovascular care nationally. Where possible, data are reported from recently published literature or standardized quality indicators from quality improvement registries (ie, those consistent with the methods for quality performance measures endorsed by the ACC and the AHA).2 Additional data on aspects of quality of care, such as adherence to ACC/AHA clinical practice guidelines, are also included to provide a spectrum of quality-of care data. The data selected are meant to provide examples of the current quality of care as reflected by the IOM domain and are not meant to be comprehensive given the sheer number of publications yearly.
- The safety domain has been defined as avoiding injuries to patients from the care that is intended to help them. The following are several publications that have focused on safety issues:
-
—In a small, single-center study conducted over a 2-month period in the cardiac care unit (CCU) of a tertiary center, Rahim et al1 demonstrated that iatrogenic adverse events were common (99 of 194 patients), of which bleeding (27%) was the most common preventable iatrogenic adverse event.
-
—Using the National Cardiovascular Data Registry CathPCI registry, Tsai et al2 found that almost one fourth of dialysis patients undergoing PCI (n=22 778) received a contraindicated antithrombotic agent, specifically enoxaparin, eptifibatide, or both. Patients who received a contraindicated antithrombotic agent had an increased risk of in-hospital bleeding (OR 1.63, 95% CI 1.35 to 1.98) and a trend toward increased mortality (OR 1.15, 95% CI 0.97 to 1.36).2
-
—In a random sample of medical and surgical long-term care adult patients in Massachusetts hospitals, López et al3 assessed the association between disclosure of an adverse event and patients’ perception of quality of care. Overall, only 40% of adverse events were disclosed. Higher quality ratings were associated with disclosure of an adverse event. Conversely, lower patient perception of quality of care was associated with events that were preventable and with events that caused discomfort.3
-
—The AHA published a scientific statement4 about medication errors in acute cardiovascular and stroke patients and classified medication errors into the following categories:
-
◦Improper dosing or timing, or delivery of an incorrect or unnecessary medication.
-
◦Administration to the wrong patient (errors of omission).
-
◦Failure to prescribe appropriate medication therapy or needed monitoring of medication therapy (errors of omission).
-
◦
-
—The following recommendations were made to improve medication safety in long-term cardiovascular care:
-
◦An accurate patient weight should be obtained on admission.
-
◦Estimated creatinine clearance should be calculated with the Cockcroft-Gault formula on admission and as changes in creatinine occur.
-
◦Medication dosage adjustments and heightened surveillance for adverse medication events are recommend owing to age-related changes in pharmacodynamics, pharmacokinetics, and renal function.
-
◦Order forms and protocols for anticoagulation should be standardized.
-
◦Pharmacists and nurses should be integrated within the cardiovascular care teams in the ED, intensive care unit (ICU), CCU, and inpatient wards to enhance communication and medication safety.
-
◦Computerized order entry, medication bar-coding technology, and smart infusion pumps should be implemented throughout all inpatient wards, including the ED.
-
◦Staff should be educated about high-alert medication, safe medication administration techniques, medication reconciliation procedures, and automated dispensing-device technologies.
-
◦An organizational culture of safety should be cultivated that promotes no-fault internal and external medication error reporting and an interdisciplinary quality improvement review process to reduce the frequency and impact of medication errors.4
-
◦
-
—
- Effective care has been defined as providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit. There are many quality improvement registries that have been developed for inpatient cardiovascular/stroke care, and the data on these are provided in subsequent tables. Similar efforts are under way for quality-of-care registries in the outpatient setting.
-
—In the CRUSADE registry, >7% of patients with STEMI without a reperfusion contraindication did not have reperfusion therapy administered, and this was associated with greater in-hospital mortality. One in 10 patients (10.3%) had a documented contraindication to reperfusion. Primary reasons for contraindications were identified as absence of an ischemic indication (53.8%), bleeding risk (16.7%), patient-related reasons (25.3%), and other (4.2%).5
-
—According to data from NHANES 1988–1994 and 1999–2008, rates of hypertension have increased from 23.9% in 1988–1994 to 29.0% between 2007 and 2008, and hypertension control has increased from 27.3% in 1988–1994 to 50.1% in 2007–2008. In addition, among patients with hypertension, BP has decreased from 143.0/80.4 to 135.2/74.1 mm Hg.6
-
—The National Quality Forum (NQF) is a nonprofit organization that aims to improve the quality of healthcare for all Americans through fulfillment of its 3-part mission: (1) Setting national priorities and goals for performance improvement; (2) endorsing national consensus standards for measuring and publicly reporting on performance; and (3) promoting the attainment of national goals through education and outreach programs. Recognizing that adherence can impact the effectiveness of therapies, NQF has adopted several performance measures related to medication adherence/ persistence, including angiotensin-converting enzyme inhibitor (ACEI)/angiotensin receptor blocker (ARB) use and persistence among patients with CAD who are at high risk for coronary events, persistence of β-blocker treatment after a heart attack for patients with AMI, and adherence to lipid-lowering medication.7
-
—Inpatient ACS, HF, and stroke quality-of-care measures data, including trends in care data, where available from national registries, are given in Tables 20-1 to 20-6.
-
—Selected outpatient quality-of-care measures from the National Committee for Quality Assurance for 2009 appear in Table 20-7.
-
—
- Patient-centered care has been defined as the provision of care that is respectful of and responsive to individual patient preferences, needs, and values and that ensures that patient values guide all clinical decisions. Dimensions of patient-centered care include the following: (1) Respect for patients’ values, preferences, and expressed needs; (2) coordination and integration of care; (3) information, communication, and education; (4) physical comfort; (5) emotional support; and (6) involvement of family and friends. Studies focusing on some of these aspects of patient-centered care are highlighted below:
-
—The Clinical Outcomes Utilizing Revascularization and AGgressive drug Evaluation (COURAGE) trial,8 which investigated a strategy of PCI plus optimal medical therapy versus optimal medical therapy alone, demonstrated that both groups had significant improvement in health status during follow-up. By 3 months, health status scores had increased in the PCI group compared with the medical therapy group to 76±24 versus 72±23 for physical limitation (P=0.004), 77±28 versus 73±27 for angina stability (P=0.002), 85±22 versus 80±23 for angina frequency (P<0.001), 92±12 versus 90±14 for treatment satisfaction (P<0.001), and 73±22 versus 68±23 for quality of life (P<0.001). The PCI plus optimal medical therapy group had a small but significant incremental benefit compared with the optimal medical therapy group early on, but this benefit disappeared by 36 months.
-
—In the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT)9 of single-lead ICD versus amiodarone for moderately symptomatic HF, patients with ICDs had improvement in quality of life compared with medical therapy patients at 3 and 12 months but not at 30 months. ICD shocks in the month preceding a scheduled assessment were associated with a decrease in quality of life in multiple domains. The authors concluded that the presence of a single-lead ICD was not associated with any detectably adverse quality of life during 30 months of follow-up.
-
—Peikes et al10 reported on 15 care-coordination programs as a part of a Medicare demonstration project for patients with coronary HF, CAD, and DM. Thirteen of the 15 programs did not show a difference in hospitalization rates, and none of the programs demonstrated a net savings. The interventions tested varied significantly, but the majority of the interventions included patient education to improve adherence to medication, diet, exercise, and self-care regimens and improving care coordination through various approaches. These programs overall had favorable effects on none of the adherence measures and only a few of the many quality-of-care indicators examined. The authors concluded that programs with substantial in-person contact that target moderately to severely ill patients can be cost-neutral and improve some aspects of care.
-
—Hernandez et al11 showed that patients with outpatient follow-up within 7 days of discharge for an HF hospitalization were less likely to be readmitted within 30 days in the Get With The Guidelines (GWTG)-HF registry of patients who were ≥65 years of age. The median length of stay was 4 days (interquartile range, 2 to 6 days), and 21.3% of patients were readmitted within 30 days. At the hospital level, the median percentage of patients who had early follow-up after discharge from the index hospitalization was 38.3% (interquartile range, 32.4% to 44.5%).
-
—Smolderen et al12 assessed whether health insurance status affects decisions to seek care for AMI. Uninsured and insured patients with financial concerns were more likely to delay seeking care during AMI and had prehospital delays of more than 6 hours (48.6% of uninsured patients and 44.6% of insured patients with financial concerns compared with only 39.3% of insured patients without financial concerns). Lack of health insurance and financial concerns about accessing care among those with health insurance were each associated with delays in seeking emergency care for AMI.
-
—Using a cohort (n=192) nested within a randomized trial at a university-affiliated ambulatory practice, Murray et al13 demonstrated that refill adherence of <40% was associated with a 3-fold higher incidence of hospitalization for HF than a refill adherence of ≥80% (P=0.002). In multivariable analysis, prescription label–reading skills were associated with a lower incidence of HF-specific emergency care (incidence rate ratio 0.76, 95% CI, 0.19 to 0.69), and participants with adequate health literacy had a lower risk of hospitalization for HF (incidence rate ratio 0.34, 95% CI, 0.15 to 0.76).
-
—
- The timely care domain relates to reducing waits and sometimes harmful delays for both those who receive and those who give care. Timeliness is an important characteristic of any service and is a legitimate and valued focus of improvement in healthcare and other industries.
-
—Chan et al14 demonstrated significant variation in timely defibrillation (<2 minutes) for in-hospital cardiac arrest among 200 hospitals participating in the National Registry of Cardiopulmonary Resuscitation (NRCPR). Adjusted rates of delayed defibrillation varied from 2.4% to 50.9% of in-hospital cardiac arrests. The variations in defibrillation rates were largely unexplained by traditional hospital factors.
-
—Bradley et al15 demonstrated that participation in the Door-to-Balloon (D2B) Alliance led to a reduction in D2B time to within 90 minutes for patients with STEMI. By March 2008, >75% of patients had D2B times of ≤90 minutes compared with only approximately one fourth of patients in April 2005.
-
—From data submitted to GWTG-Resuscitation in 2009:
-
◦Among children who experienced in-hospital cardiac arrests with an initial shockable rhythm, 74% received a defibrillation attempt within 3 minutes.
-
◦Among adults in similar situations, 80% received a defibrillation attempt within 3 minutes.
-
◦
-
—Thirty-one percent of adults treated for out-of-hospital cardiac arrest received bystander CPR.16
-
—Data on time to reperfusion for STEMI or ischemic stroke are provided from national registries in Table 20-8.
-
—
- Efficiency has been defined as avoiding waste, in particular waste of equipment, supplies, ideas, and energy. In an efficient healthcare system, resources are used to get the best value for the money spent.
-
—The AHA and ACC have jointly developed a scientific statement that outlines standards for measures to be used for public reporting of efficiency in health care. The group identified 4 standards important to the development of any efficiency performance measure, including (1) integration of quality and cost, (2) valid cost measurement and analysis, (3) no or minimal incentive to provide poor-quality care, and (4) no or proper attribution of the measure. In the statement, 4 examples were provided of hospital-based efficiency measures, as well as information on how each of the measures fared within the 4 domains recommended. The examples were length of stay, 30-day readmission, hospitalization costs, and nonrecommended imaging tests.
-
—At an urban, tertiary-care, academic medical center ED, elements of departmental work flow were redesigned to streamline patient throughput before implementation of a fully integrated ED information system with patient tracking, computerized charting and order entry, and direct access to patient historical data from the hospital data repository. Increasing the clinical information available at the bedside and improving departmental work flow through ED information system implementation and process redesign led to decreased patient throughput times and improved ED efficiency (eg, the length of stay for all patients [from arrival to time patient left ED] decreased by 1.94 hours, from 6.69 [n=508] before the intervention to 4.75 [n=691] after the intervention; P<0.001).17
-
—Himmelstein et al18 analyzed whether more-computerized hospitals had lower costs of care or administration or better quality to address a common belief that computerization improves healthcare quality, reduces costs, and increases administrative efficiency. They found that hospitals that increased computerization faster had more rapid administrative cost increases (P=0.0001); however, higher overall computerization scores correlated weakly with better quality scores for AMI (r=0.07, P=0.003) but not for HF, pneumonia, or the 3 conditions combined. In multivariate analyses, more-computerized hospitals had slightly better quality. The authors concluded that hospital computing might modestly improve process measures of quality but does not reduce administrative or overall costs.
-
—
- Equitable care means the provision of care that does not vary in quality because of personal characteristics such as sex, ethnicity, geographic location, and socioeconomic status. The aim of equity is to secure the benefits of quality health care for all the people of the United States. With regard to equity in caregiving, all individuals rightly expect to be treated fairly by local institutions, including healthcare organizations.
-
—Chan et al19 demonstrated that rates of survival to discharge were lower for black patients (25.2%) than for white patients (37.4%). Lower rates of survival to discharge for blacks reflected lower rates of both successful resuscitation (55.8% versus 67.4%) and postresuscitation survival (45.2% versus 55.5%). Adjustment for the hospital site at which patients received care explained a substantial portion of the racial differences in successful resuscitation (adjusted RR 0.92; 95% CI, 0.88 to 0.96; P<0.001) and eliminated the racial differences in postresuscitation survival (adjusted RR 0.99; 95% CI, 0.92 to 1.06; P=0.68). The authors concluded that much of the racial difference was associated with the hospital center in which black patients received care.
-
—Cohen et al20 demonstrated that among hospitals engaged in a national quality monitoring and improvement program, evidence-based care for AMI appeared to improve over time for patients irrespective of race/ethnicity, and differences in care by race/ethnicity care were reduced or eliminated. They analyzed 142 593 patients with AMI (121 528 whites, 10 882 blacks, and 10 183 Hispanics) at 443 hospitals participating in the GWTG-CAD program. Overall, defect-free care was 80.9% for whites, 79.5% for Hispanics (adjusted OR versus whites 1.00; 95% CI, 0.94 to 1.06; P=0.94), and 77.7% for blacks (adjusted OR versus whites 0.93; 95% CI, 0.87 to 0.98; P=0.01). A significant gap in defect-free care was observed for blacks during the first half of the study but was no longer present during the remainder of the study. Overall, progressive improvements in defect-free care were observed regardless of race/ethnic groups.
-
—According to NHANES 1999 to 2006, 45% of adults had at least 1 of 3 chronic conditions (hypertension, hypercholesterolemia, or DM), 13% had 2 of these conditions, and 3% of adults had all 3 conditions. Non-Hispanic black people were more likely than non-Hispanic white and Mexican-American people to have at least 1 of the 3 conditions. In 15% of US adults, 1 or more of the 3 conditions is undiagnosed.21
-
—GWTG data by race, sex, and ethnicity are provided in Tables 20-9 through 20-11
-
—
Table 20-6.
Additional ACTION-GWTG Quality-of-Care Metrics for ACS Care, 2009
| Quality Metrics | Overall | STEMI | NSTEMI |
|---|---|---|---|
| ECG within 10 min of arrival | 59.1 | 70.4 | 53.7 |
| Aspirin within 24 h of arrival | 94.4 | 96.3 | 93.2 |
| Anticoagulant within 24 h of arrival for NSTEMI | 87.9 | NA | 87.9 |
| Excessive initial UFH dose | 60.2 | 61.7 | 58.7 |
| Excessive initial enoxaparin dose | 12.0 | 11.5 | 12.1 |
| Excessive GP IIb/IIIa dose | 8.5 | 8.6 | 8.4 |
| ADP receptor within 24 h of arrival for STEMI | 92.9 | 92.9 | NA |
| ADP receptor on discharge for revascularized AMI population | 91.5 | 95.2 | 87.8 |
| ADP receptor on discharge for medically treated AMI population | 59.8 | 65.0 | 59.1 |
| Aldosterone-blocking agents on discharge | 6.0 | 6.3 | 5.8 |
| Documentation of LDL-C level in hospital record | 82.9 | 84.4 | 81.5 |
ACTION indicates Acute Coronary Treatment and Intervention Outcomes Network; GWTG, Get With The Guidelines; ACS, acute coronary syndrome; STEMI, ST-elevation myocardial infarction; NSTEMI, non–ST-elevation myocardial infarction; ECG, electrocardiogram; NA, not applicable; UFH, unfractionated heparin; GP, glycoprotein; ADP, adenosine triphosphate; AMI, acute myocardial infarction; LDL-C, low-density lipoprotein cholesterol.
Table 20-7.
National Committee for Quality Assurance Health Plan Employer Data and Information Set Measures of Care
| Commercial, % |
Medicare, % |
Medicaid, % |
|
|---|---|---|---|
| Acute MI | |||
| β-blocker persistence* | 75.0 | 79.7 | 73.6 |
| Cholesterol management for patients with CAD | |||
| Cholesterol screening | 88.9 | 88.6 | 79.6 |
| LDL control (<100 mg/dL) | 59.7 | 56.7 | 40.1 |
| Hypertension | |||
| BP <140/90 mm Hg | 63.4 | 58.5 | 55.8 |
| DM | |||
| HbA1c testing | 89.0 | 88.3 | 80.5 |
| HbA1c >9.0% | 28.4 | 29.4 | 44.8 |
| Eye examination performed | 56.5 | 60.8 | 52.8 |
| LDL cholesterol screening | 84.8 | 86.3 | 74.1 |
| LDL cholesterol <100 mg/dL | 45.5 | 48.7 | 33.8 |
| Monitoring nephropathy | 82.4 | 87.9 | 76.6 |
| BP <130/80 mm Hg | 33.4 | 31.8 | 30.7 |
| BP <140/90 mm Hg | 65.6 | 59.5 | 56.9 |
| Advising smokers to quit | 76.7 | N/A | 69.3 |
MI indicates myocardial infarction; CAD, coronary artery disease; LDL, low-density lipoprotein; BP, blood pressure; DM, diabetes mellitus; HbA1c, glycosylated hemoglobin.
β-blocker persistence: Received persistent β-blocker treatment for 6 months after hospital discharge for acute MI.
Table 20-8.
Timely Reperfusion for ACS and Stroke
| Quality-of-Care Measure |
VHA* | National Medicare and Medicaid* |
GWTG- CAD† |
ACTION- GWTG STEMI‡ |
GWTG- Stroke |
|---|---|---|---|---|---|
| ACS | |||||
| tPA within 30 min | 73 | 52 | 27 | 69 | N/A |
| PCI within 90 min | 55 | 86 | 78 | 90 | N/A |
| Stroke | |||||
| IV tPA in patients who arrived <2h after symptom onset§ | NA | NA | NA | NA | 73.1 |
| IV tPA in patients who arrived <3h after symptom onset | NA | NA | NA | NA | 67.1 |
| No IV tPA (contraindicated/warning) | NA | NA | NA | NA | 82.4 |
ACS indicates acute coronary syndrome; VHA, Veterans Health Administration; GWTG-CAD, Get With The Guidelines–Coronary Artery Disease; ACTIONGWTG-STEMI, Acute Coronary Treatment and Intervention Outcomes Network/Get With The Guidelines–ST-elevation myocardial infarction; tPA, tissue-type plasminogen activator; NA, not applicable; PCI, percutaneous coronary intervention; IV, intravenous.
Values are percentages.
Acute myocardial infarction patients.
GWTG-CAD: Patients admitted with a cardiovascular event. In the GWTGCAD registry, the in-hospital mortality rate was 4.5% (excludes transfer-out patients; if discharge status was missing, it was assumed to be “no.”). The mean length of hospital stay was 5.0 days (median 3.0 days).
ACTION Registry: STEMI and NSTEMI patients were reported separately. Patients must have been admitted with acute ischemic symptoms within the previous 24 hours, typically reflected by a primary diagnosis of ST-elevation myocardial infarction or non–ST-elevation myocardial infarction. Patients who were admitted for any other clinical condition were not eligible.
Indicates 1 of the 7 key performance measures targeted in GWTG-Stroke.
Table 20-9.
Quality of Care by Race/Ethnicity and Sex in the GWTG-CAD Program, 2009
| Race/Ethnicity | Sex | ||||
|---|---|---|---|---|---|
| Quality-of-Care Measure | White | Black | Hispanic | Men | Women |
| Aspirin at admission* | 98.0 | 98.2 | 97.9 | 97.9 | 97.5 |
| Aspirin at discharge* | 96.1 | 96.3 | 93.5 | 96.7 | 94.5 |
| β-Blockers at discharge* | 96.0 | 97.0 | 94.2 | 96.4 | 94.5 |
| ACEI at discharge | 62.7 | 68.6 | 68.2 | 65.4 | 59.5 |
| ACEI at discharge for AMI patients | 64.6 | 70.1 | 71.1 | 67.3 | 61.7 |
| ACEI in LVSD patients | 84.8 | 83.1 | 82.4 | 84.4 | 81.6 |
| ACEI/ARB for LVSD patients at discharge* | 93.4 | 93.0 | 93.0 | 92.6 | 92.1 |
| Lipid therapy at discharge | 87.5 | 85.9 | 79.4 | 88.5 | 82.6 |
| Lipid therapy at discharge if LDL >100 mg/dL* | 93.5 | 90.7 | 91.5 | 95.2 | 88.2 |
| Patients with last BP <140/90 mm Hg | 80.6 | 72.8 | 79.8 | 81.6 | 76.9 |
| Smoking cessation counseling* | 98.5 | 98.7 | 99.0 | 98.3 | 98.1 |
| Referral to cardiac rehabilitation for AMI patients | 51.5 | 46.2 | 52.6 | 49.6 | 48.3 |
| Composite quality-of-care measure† | 96.4 | 96.5 | 94.8 | 96.7 | 94.9 |
GWTG-CAD indicates Get With the Guidelines–Coronary Artery Disease; ACEI, angiotensin-converting enzyme inhibitor; AMI inhibitor, acute myocardial infarction; LVSD, left ventricular systolic dysfunction; ARB, angiotensin receptor blocker; LDL, low-density lipoprotein; BP, blood pressure.
Values are percentages.
Indicates the 6 key achievement measures targeted in GWTG-CAD.
The composite quality-of-care measure indicates performance on the provision of several elements of care. It is computed by summing the numerators for each key achievement measure across the population of interest to create a composite numerator (all the care that was given), summing the denominators for each measure to form a composite denominator (all the care that should have been given), and reporting the ratio (the percentage of all the needed care that was given).
Abbreviations Used in Chapter 20
- ACC
American College of Cardiology
- ACEI
angiotensin-converting enzyme inhibitor
- ACS
acute coronary syndrome
- AHA
American Heart Association
- AMI
acute myocardial infarction
- ARB
angiotensin receptor blocker
- BP
blood pressure
- CAD
coronary artery disease
- CCU
cardiac care unit
- CI
confidence interval
- COURAGE
Clinical Outcomes Utilizing Revascularization and AGgressive drug Evaluation trial
- CPR
cardiopulmonary resuscitation
- CRUSADE
Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines
- D2B
door-to-balloon
- ED
emergency department
- GWTG
Get With The Guidelines
- HF
heart failure
- ICD
implantable cardioverter-defibrillator
- ICU
intensive care unit
- IOM
Institute of Medicine
- NHANES
National Health and Nutrition Examination Survey
- NQF
National Quality Forum
- NRCPR
National Registry of Cardiopulmonary Resuscitation
- NSTEMI
non–ST-elevation myocardial infarction
- OR
odds ratio
- PCI
percutaneous coronary intervention
- RR
relative risk
- SCD-HeFT
Sudden Cardiac Death in Heart Failure Trial
- STEMI
ST-elevation myocardial infarction
- VHA
Veterans Health Administration
References
- 1.Rahim SA, Mody A, Pickering J, Devereaux PJ, Yusuf S. Iatrogenic adverse events in the coronary care unit. Circ Cardiovasc Qual Outcomes. 2009;2:437–442. doi: 10.1161/CIRCOUTCOMES.108.846493. [DOI] [PubMed] [Google Scholar]
- 2.Tsai TT, Maddox TM, Roe MT, Dai D, Alexander KP, Ho PM, Messenger JC, Nallamothu BK, Peterson ED, Rumsfeld JS. Contraindicated medication use in dialysis patients undergoing percutaneous coronary intervention. JAMA. 2009;302:2458–2464. doi: 10.1001/jama.2009.1800. [DOI] [PubMed] [Google Scholar]
- 3.López L, Weissman JS, Schneider EC, Weingart SN, Cohen AP, Epstein AM. Disclosure of hospital adverse events and its association with patients’ ratings of the quality of care. Arch Intern Med. 2009;169:1888–1894. doi: 10.1001/archinternmed.2009.387. [DOI] [PubMed] [Google Scholar]
- 4.Michaels AD, Spinler SA, Leeper B, Ohman EM, Alexander KP, Newby LK, Ay H, Gibler WB. on behalf of the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology, Council on Quality of Care and Outcomes Research; Council on Cardiopulmonary, Critical Care, Perioperative, and Resuscitation; Council on Cardiovascular Nursing; and Stroke Council Medication errors in acute cardiovascular and stroke patients: a scientific statement from the American Heart Association. Circulation. 2010;121:1664–1682. doi: 10.1161/CIR.0b013e3181d4b43e. [DOI] [PubMed] [Google Scholar]
- 5.Gharacholou SM, Alexander KP, Chen AY, Wang TY, Melloni C, Gibler WB, Pollack CV, Jr, Ohman EM, Peterson ED, Roe MT. Implications and reasons for the lack of use of reperfusion therapy in patients with ST-segment elevation myocardial infarction: findings from the CRUSADE initiative. Am Heart J. 2010;159:757–763. doi: 10.1016/j.ahj.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 6.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 7.National Quality Forum. About NQF. [Accessed July 22, 2010]; Available at: http://www.qualityforum.org/About_NQF/About_NQF.aspx. [Google Scholar]
- 8.Weintraub WS, Spertus JA, Kolm P, Maron DJ, Zhang Z, Jurkovitz C, Zhang W, Hartigan PM, Lewis C, Veledar E, Bowen J, Dunbar SB, Deaton C, Kaufman S, O’Rourke RA, Goeree R, Barnett PG, Teo KK, Boden WE for the COURAGE Trial Research Group. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med. 2008;359:677–687. doi: 10.1056/NEJMoa072771. [DOI] [PubMed] [Google Scholar]
- 9.Mark DB, Anstrom KJ, Sun JL, Clapp-Channing NE, Tsiatis AA, Davidson-Ray L, Lee KL, Bardy GH Sudden Cardiac Death in Heart Failure Trial Investigators. Quality of life with defibrillator therapy or amiodarone in heart failure. N Engl J Med. 2008;359:999–1008. doi: 10.1056/NEJMoa0706719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301:603–618. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- 11.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, Peterson ED, Curtis LH. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 12.Smolderen KG, Spertus JA, Nallamothu BK, Krumholz HM, Tang F, Ross JS, Ting HH, Alexander KP, Rathore SS, Chan PS. Health care insurance, financial concerns in accessing care, and delays to hospital presentation in acute myocardial infarction. JAMA. 2010;303:1392–1400. doi: 10.1001/jama.2010.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murray MD, Tu W, Wu J, Morrow D, Smith F, Brater DC. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther. 2009;85:651–658. doi: 10.1038/clpt.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan PS, Nichol G, Krumholz HM, Spertus JA, Nallamothu BK American Heart Association National Registry of Cardiopulmonary Resuscitation (NRCPR) Investigators. Hospital variation in time to defibrillation after in-hospital cardiac arrest. Arch Intern Med. 2009;169:1265–1273. doi: 10.1001/archinternmed.2009.196. [DOI] [PubMed] [Google Scholar]
- 15.Bradley EH, Nallamothu BK, Herrin J, Ting HH, Stern AF, Nembhard IM, Yuan CT, Green JC, Kline-Rogers E, Wang Y, Curtis JP, Webster TR, Masoudi FA, Fonarow GC, Brush JE, Jr, Krumholz HM. National efforts to improve door-to-balloon time results from the Door-to-Balloon Alliance. J Am Coll Cardiol. 2009;54:2423–2429. doi: 10.1016/j.jacc.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I Resuscitation Outcomes Consortium Investigators. Regional variation in out-of-hospital cardiac arrest incidence and outcome [published correction appears in JAMA. 2008;300:1763] JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baumlin KM, Shapiro JS, Weiner C, Gottlieb B, Chawla N, Richardson LD. Clinical information system and process redesign improves emergency department efficiency. Jt Comm J Qual Patient Saf. 2010;36:179–185. doi: 10.1016/s1553-7250(10)36030-2. [DOI] [PubMed] [Google Scholar]
- 18.Himmelstein DU, Wright A, Woolhandler S. Hospital computing and the costs and quality of care: a national study. Am J Med. 2010;123:40–46. doi: 10.1016/j.amjmed.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Chan PS, Nichol G, Krumholz HM, Spertus JA, Jones PG, Peterson ED, Rathore SS, Nallamothu BK American Heart Association National Registry of Cardiopulmonary Resuscitation (NRCPR) Investigators. Racial differences in survival after in-hospital cardiac arrest. JAMA. 2009;302:1195–1201. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen MG, Fonarow GC, Peterson ED, Moscucci M, Dai D, Hernandez AF, Bonow RO, Smith SC., Jr Racial and ethnic differences in the treatment of acute myocardial infarction: findings from the Get With the Guidelines-Coronary Artery Disease program. Circulation. 2010;121:2294–2301. doi: 10.1161/CIRCULATIONAHA.109.922286. [DOI] [PubMed] [Google Scholar]
- 21.Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD. Hypertension, high serum total cholesterol, and diabetes: racial and ethnic prevalence differences in U.S. adults, 1999–2006. NCHS Data Brief. 2010 Apr;:1–8. [PubMed] [Google Scholar]
21. Medical Procedures
See Tables 21-1 and 21-2 and Charts 21-1 through 21-3.
- The total number of inpatient cardiovascular operations and procedures increased 27%, from 5 382 000 in 1997 to 6 846 000 in 2007 (NHLBI computation based on NCHS annual data). Data from the NHDS were examined for trends from 1990 to 2004 for use of PCI and CABG and in-hospital mortality rate due to PCI and CABG by sex.1
-
—Discharge rates (per 10 000 population) for PCI increased 58%, from 37.2 in 1990–1992 to 59.2 in 2002–2004.
-
—Discharge rates for CABG increased from 34.1 in 1990–1992 to 38.6 in 1996–1998, then declined to 25.2 in 2002–2004.
-
—In 1990–1992, discharge rates for CABG were 53.5 for males and 18.1 for females; these rates increased through 1996–1998, then declined to 38.8 and 13.6, respectively, in 2002–2004. The magnitude of these declines decreased by age decile and were essentially flat for both men and women 75 years of age.
-
—PCI discharge rates increased from 54.5 for males and 23.0 for females to 83.0 and 38.7 over the 15-year time interval. In 2002–2004, discharge rates for men and women 65 to 74 years of age were 135.1 and 64.0, respectively. For those 75 years of age, the rates were 128.7 and 69.0, respectively.
-
—In-hospital mortality rate (deaths per 100 CABG discharges) declined from 4.3 to 3.5 in 2002 to 2004 despite an increase in Charlson comorbidity index. The mortality rate declined in all age and sex subsets, but especially in women.
-
—PCI mortality remained stable over the 15-year interval.
-
—
- Data from the Acute Care Tracker database were used to estimate the population-based rates per 100 000 population for PCI and CABG procedures from 2002 to 2005, standardized to the 2005 US population2:
-
—Adjusted for age and sex, the overall rate for coronary revascularization declined from 382 to 358 per 100 000. PCI rates during hospitalization increased from 264 to 267 per 100 000, whereas CABG rates declined from 121 to 94.
-
—
- Data from men and women enrolled in Medicare from 1992 to 2001 suggest that efforts to eliminate racial disparities in the use of high-cost cardiovascular procedures (PCI, CABG, and carotid endarterectomy) were unsuccessful.3
-
—In 1992, among women, the age-standardized rates of carotid endarterectomy were 1.59 per 1000 enrollees for whites and 0.64 per 1000 enrollees for blacks. By 2002, the rates were 2.42 per 1000 enrollees among white women and 1.15 per 1000 enrollees among black women. For men, the difference in rates between whites and blacks remained the same. In 1992, the rates were 3.13 per 1000 enrollees among white men and 0.82 per 1000 enrollees among black men; in 2001, the rates were 4.42 and 1.44, respectively.
-
—
Table 21-1.
2008 National Healthcare Cost and Utilization: Project Statistics: Mean Hospital Charges and In-Hospital Death: Rates for Various Procedures
| Procedure | Mean Hospital Charges, $ |
In-Hospital Death Rate, % |
|---|---|---|
| Total vascular and cardiac surgery and procedures | 62 509 | 3.04 |
| CABG | 117 094 | 1.89 |
| PCI | 56 015 | 0.87 |
| Diagnostic cardiac catheterization | 34 198 | 0.86 |
| Pacemaker | 57 633 | 1.29 |
| Implantable defibrillator | 124 901 | 0.61 |
| Endarterectomy | 30 588 | 0.30 |
| Valves | 164 238 | 4.89 |
CABG indicates coronary artery bypass graft; PCI, percutaneous coronary intervention.
Data derived from the Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project.10
Table 21-2.
Estimated* Inpatient Cardiovascular Operations, Procedures, and Patient Data by Sex and Age: United States, 2007 (in Thousands)
| Sex | Age, y | |||||||
|---|---|---|---|---|---|---|---|---|
| Operation/Procedure/Patients | ICD-9-CM Code(s) | All | Males | Females | <15 | 15–44 | 45–64 | ≥65 |
| Valves | 35.1, 35.2, 35.99 | 106 | 64 | 41 | † | 7† | 27 | 68 |
| Angioplasty | 36.0, 00.66 | 1179 | 787 | 392 | † | 66 | 502 | 610 |
| PCI (patients) | 36.06, 36.07, 00.66 (Any) | 622 | 414 | 208 | † | 34 | 263 | 324 |
| PCI | 00.66 | 618 | 410 | 208 | † | 35 | 263 | 320 |
| PCI with stents | 36.06, 36.07 | 560 | 376 | 183 | † | 31 | 238 | 290 |
| Cardiac revascularization (bypass)§ | 36.1–36.3 | 408 | 293 | 115 | … | 9† | 167 | 233 |
| Cardiac revascularization (bypass) (patients) | 36.1–36.3 (Any) | 232 | 164 | 68 | … | 5† | 90 | 137 |
| Cardiac catheterization | 37.21–37.23 | 1059 | 638 | 420 | 6† | 92 | 453 | 517 |
| Pacemakers | 37.7, 37.8, 00.50, 00.53 | 358 | 180 | 178 | † | 11 | 58 | 287 |
| Pacemaker devices | (37.8, 00.53) | 160 | 78 | 82 | † | † | 21 | 134 |
| Pacemaker leads | (37.7, 00.50) | 198 | 102 | 96 | † | 7† | 37 | 153 |
| Implantable defibrillators | 37.94–37.99, 00.51, 00.54 | 111 | 78 | 32 | † | 6† | 38 | 66 |
| Endarterectomy | 38.12 | 91 | 53 | 38 | … | † | 24 | 66 |
| Total vascular and cardiac surgery and procedures‖¶ | 35–39, 00.50–00.51, 00.53–00.55, 00.61–00.66 | 6846 | 3912 | 2934 | 77 | 726 | 2517 | 3526 |
ICD-9-CM indicates International Classification of Diseases, 9th Revision, Clinical Modification; PCI, percutaneous coronary intervention.
Ellipses (…) indicate data not available.
These data do not reflect any procedures performed on an outpatient basis. Many more procedures are being performed on an outpatient basis. Some of the lower numbers in this table compared with 2006 probably reflect this trend.
Breakdowns are not available for some procedures, so entries for some categories do not add to totals. These data include codes for which the estimated number of procedures is <5000. Categories of such small numbers are considered unreliable by NCHS and in some cases may have been omitted.
Estimate should be used with caution because it may be unreliable or does not meet standards of reliability or precision.
Because ≥1 procedure codes are required to describe the specific bypass procedure performed, it is impossible from these (mixed) data to determine the average number of grafts per patient.
Totals include procedures not shown here.
This estimate includes angioplasty and stent insertions for noncoronary arteries.
Data derived from the National Hospital Discharge Survey/National Center for Health Statistics, 2007. Estimates are based on a sample of inpatient records from short-stay hospitals in the United States.
Chart 21-1.
Trends in heart transplantations (United Network for Organ Sharing : 1975–2009). Source: United Network for Organ Sharing (UNOS), scientific registry data.
Chart 21-3.
Number of surgical procedures in the 10 leading diagnostic groups, United States: 2007. Source: National Hospital Discharge Survey/National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Cardiac Catheterization and PCI
From 1997 to 2007, the number of cardiac catheterizations decreased slightly, from 1 112 000 to 1 059 000 annually.
In 2007, an estimated 622 000 patients underwent PCI (previously referred to as percutaneous transluminal coronary angioplasty, or PTCA) procedures in the United States (NHLBI tabulation, NHDS, NCHS).
In 2007, ≈67% of PCI procedures were performed on men, and ≈51% were performed on people ≥65 years of age (NHDS, NCHS).
The mortality rate for PCI has remained stable despite an increase in risk.1
In 2006, ≈76% of stents implanted during PCI were drug-eluting stents compared with 24% that were bare-metal stents.4
In a study of nontransferred patients with STEMI treated with primary PCI from July 2006 to March 2008, there was significant improvement over time in the percentage of patients receiving PCI within 90 minutes, from 54.1% from July to September 2006 to 74.1% from January to March 2008 among hospitals participating in the GWTG-CAD program. This improvement was seen whether or not hospitals joined the D2B Alliance during that period.5
Cardiac Open Heart Surgery
The NHDS (NCHS) estimates that in 2007, in the United States, 232 000 patients underwent a total of 408 000 coronary artery bypass procedures (defined by procedure codes). CABG volumes have declined nationally since 1998. Risk-adjusted mortality for CABG has declined significantly over the past decade:
Data from the Society of Thoracic Surgeons’ National Adult Cardiac Database (STS NCD), which voluntarily collects data from ≈80% of all hospitals that perform CABG in the United States, indicate that a total of 163 149 procedures involved CABG in 2009.6
Data from the STS NCD document a 50% decline in the risk-adjusted mortality rate despite a significant increase in preoperative surgical risk.7
Congenital Heart Surgery, 2005 to 2008 (From the Society of Thoracic Surgeons [STS])
There were 91 639 procedures performed from July 2005 to June 2009. The in-hospital mortality rate was 3.4% in 2009. The 5 most common diagnoses were the following: Patent ductus arteriosus (7.8%); hypoplastic left heart syndrome (7.0%); ventricular septal defect, type 2 (5.7%); tetralogy of Fallot (5.3%); and cardiac, other (4.7%).8
Congenital Heart Surgery, 1998 to 2002 (From STS)
There were 16 920 procedures performed from 1998 to 2002 at 18 centers. In 2002, there were 4208 procedures performed. The in-hospital mortality ranged from 5.7% in 1998 to 4.3% in 2002. Of these procedures, ≈46% were performed in children >1 year old, ≈32% in infants between 29 days and 1 year of age, and ≈22% in neonates (<29 days old). The conditions for which these procedures were most commonly performed were the following: Patent ductus arteriosus (6.5%), ventricular septal defect (6.4%), and TOF (6.0%).
Heart Transplantations
In 2009, 2211 heart transplantations were performed in the United States. There are 249 transplant hospitals in the United States, 127 of which perform heart transplantations (United Network for Organ Sharing, Web site accessed June 24, 2010).
Of the recipients, 72.1% are male, and 67.6% are white; 19.0% are black, whereas 9.1% are Hispanic; 25.5% are <35 years of age, 17.9% are 35 to 49 years of age, and 56.6% are ≥50 years of age.
As of June 25, 2010, for transplants that occurred between 1997 and 2004, the 1-year survival rate for males was 88.0%, and for females, it was 86.2%; the 3-year rates were 79.3% for males and 77.2% for females; and the 5-year rates were 73.1% for males and 69.0% for females. The 1-, 3-, and 5-year survival rates for white cardiac transplant patients were 87.1%, 79.2%, and 72.5%, respectively. For black patients, they were 85.5%, 71.9%, and 62.3%, respectively. For Hispanic patients, they were 88.7%, 77.6%, and 72.1%, respectively.
As of June 25, 2010, 3153 patients were on the transplant waiting list for a heart transplant and 80 patients were on the list for a heart/lung transplant.
Cardiovascular Healthcare Expenditures
An analysis of claims and enrollment data from the Continuous Medicare History Sample and from physician claims from 1995 to 2004 was used to evaluate the conditions that contributed to the most expensive 5% of Medicare beneficiaries.9
Ischemic HD, CHF, and cerebrovascular disease, respectively, constituted 13.8%, 5.9%, and 5.7% of the conditions of all beneficiaries in 2004. In patients in the top 5% overall for all expenditures, the respective figures were 39.1%, 32.7%, and 22.3% for these cardiovascular conditions.
Abbreviations Used in Chapter 21
- AHA
American Heart Association
- CABG
coronary artery bypass graft
- CHF
congestive heart failure
- D2B
door-to-balloon
- GWTG-CAD
Get With The Guidelines–Coronary Artery Disease
- HD
heart disease
- NCHS
National Center for Health Statistics
- NHDS
National Hospital Discharge Survey
- NHLBI
National Heart, Lung, and Blood Institute
- PCI
percutaneous coronary intervention
- PTCA
percutaneous transluminal coronary angioplasty
- STEMI
ST-elevation myocardial infarction
- STS
Society of Thoracic Surgeons
- STS NCD
Society of Thoracic Surgeons’ National Adult Cardiac Database
- TOF
tetralogy of Fallot
References
- 1.Holmes JS, Kozak LJ, Owings MF. Use and in-hospital mortality associated with two cardiac procedures, by sex and age: national trends, 1990–2004. Health Aff (Millwood) 2007;26:169–177. doi: 10.1377/hlthaff.26.1.169. [DOI] [PubMed] [Google Scholar]
- 2.Nallamothu BK, Young J, Gurm HS, Pickens G, Safavi K. Recent trends in hospital utilization for acute myocardial infarction and coronary revascularization in the United States. Am J Cardiol. 2007;99:749–753. doi: 10.1016/j.amjcard.2006.10.029. [DOI] [PubMed] [Google Scholar]
- 3.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353:683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 4.US Food and Drug Administration. Circulatory System Devices Panel. Meeting minutes. Washington, DC: 2006. Dec 8, [Accessed September 28, 2010]. Available at: http://www.fda.gov/ohrms/dockets/ac/06/transcripts/2006-4253t2.rtf. [Google Scholar]
- 5.Nallamothu BK, Krumholz HM, Peterson ED, Pan W, Bradley E, Stern AF, Masoudi FA, Janicke DM, Hernandez AF, Cannon CP, Fonarow GC. D2B Alliance and the American Heart Association Get-With-The-Guidelines Investigators. Door-to-balloon times in hospitals within the Get-With-The-Guidelines registry after initiation of the Door-To-Balloon (D2B) Alliance. Am J Cardiol. 2009;103:1051–1055. doi: 10.1016/j.amjcard.2008.12.030. [DOI] [PubMed] [Google Scholar]
- 6.STS Adult Cardiac Surgery Database: period ending 12/31/2009: executive summary contents. [Accessed July 7, 2010]; Available at: http://www.sts.org/documents/pdf/ndb2010/1stHarvestExecutiveSummary%5B1%5D.pdf. [Google Scholar]
- 7.Ferguson TB, Jr, Hammill BG, Peterson ED, DeLong ER, Grover FL. STS National Database Committee. A decade of change: risk profiles and outcomes for isolated coronary artery bypass grafting procedures, 1990–1999: a report from the STS National Database Committee and the Duke Clinical Research Institute. Ann Thorac Surg. 2002;73:480–489. doi: 10.1016/s0003-4975(01)03339-2. [DOI] [PubMed] [Google Scholar]
- 8.STS congenital heart surgery data summary: July 2005–June 2009 procedures, all patients. [Accessed July 7, 2010]; Available at: http://www.sts.org/documents/pdf/ndb/STSCONG-AllPatientsSummary_Fall2009.pdf. [Google Scholar]
- 9.Riley GF. Long-term trends in the concentration of Medicare spending. Health Aff (Millwood) 2007;26:808–816. doi: 10.1377/hlthaff.26.3.808. [DOI] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project. [Accessed June 7, 2010];HCUPnet. Available at: http://www.hcup.ahrq.gov/HCUPnet.jsp. [PubMed]
22. Economic Cost of Cardiovascular Disease
See Tables 22-1 and 22-2 and Charts 22-1 and 22-2.
Table 22-1.
Estimated Direct and Indirect Costs (in Billions of Dollars) of Cardiovascular Disease and Stroke: United States, 2007 (Based on New Data Sources and Estimation Methods)
| Heart Disease* |
Stroke | Hypertensive Disease† |
Other Circulatory Conditions |
Total Cardiovascular Disease |
|
|---|---|---|---|---|---|
| Direct costs‡ | |||||
| Hospital inpatient stays | 49.8 | 17.9 | 6.2 | 11.8 | 85.7 |
| Hospital emergency room visits | 3.9 | 0.6 | 0.6 | 0.2 | 5.3 |
| Hospital outpatient or office-based provider visits | 13.7 | 2.5 | 9.8 | 5.0 | 31.0 |
| Home health care | 6.3 | 2.9 | 3.6 | 1.1 | 13.9 |
| Prescribed medicines | 8.5 | 1.3 | 20.4 | 1.2 | 31.4 |
| Total expenditures | 82.2 | 25.2 | 40.6 | 19.3 | 167.4 |
| Indirect costs§ | |||||
| Lost productivity/mortality‖ | 95.3 | 15.7 | 2.9 | 5.3 | 119.2 |
| Grand totals | 177.5 | 40.9 | 43.5 | 24.6 | 286.6 |
Numbers do not add to total due to rounding.
This category includes coronary heart disease, heart failure, part of hypertensive disease, cardiac dysrhythmias, rheumatic heart disease, cardiomyopathy, pulmonary heart disease, and other or ill-defined heart diseases.
Costs due to hypertensive disease are limited to hypertension without heart disease.
Medical Expenditure Panel Survey healthcare expenditures are estimates of direct payments for care of a patient with the given disease provided during the year, including out-of-pocket payments and payments by private insurance, Medicaid, Medicare, and other sources. Payments for over-the-counter drugs are not included. These estimates of direct costs do not include payments attributed to comorbidities. Total cardiovascular disease costs are the sum of costs for the 4 diseases but with some duplication.
The Statistics Committee agreed to suspend presenting estimates of lost productivity due to morbidity until a better estimating method can be developed.
Earnings of persons who died in 2007, discounted at 3%.
Sources: Estimates from the Household Component of the Medical Expenditure Panel Survey of the Agency for Healthcare Research and Quality for direct costs (2007).1 Indirect mortality costs are based on 2007 counts of deaths by the National Center for Health Statistics and an estimated present value of lifetime earnings furnished for 2005 by Wendy Max (Institute for Health and Aging, University of California, San Francisco, 2009) and inflated to 2007 from mean earnings values reported by the US Census Bureau.4,5
All estimates prepared by Thomas Thom and Michael Mussolino, National Heart, Lung, and Blood Institute.
Table 22-2.
Costs of Total CVD in Billions of Dollars by Age and Sex: United States, 2007
| Sex | Age, y | ||||
|---|---|---|---|---|---|
| Total | Males | Females | <65 | ≥65 | |
| Direct costs | 167.4 | 86.4 | 81.0 | 74.6 | 92.8 |
| Indirect mortality | 119.2 | 91.3 | 27.9 | 103.0 | 16.2 |
| Total | 286.6 | 177.7 | 108.9 | 177.6 | 109.0 |
CVD indicates cardiovascular disease.
Numbers may not add due to rounding.
Source: Medical Expenditure Panel Survey. All estimates prepared by Thomas Thom and Michael Mussolino, National Heart, Lung, and Blood Institute.
Chart 22-1.
Direct and indirect costs (in billions of dollars) of major cardiovascular diseases (CVD) and stroke (United States: 2007). Source: National Heart, Lung, and Blood Institute.
Chart 22-2.
The 16 leading diagnoses for direct health expenditures, United States, 2007 (in billions of dollars). COPD indicates chronic obstructive pulmonary disease; GI, gastrointestinal. Source: National Heart, Lung, and Blood Institute; estimates are from the Medical Expenditure Panel Survey and exclude nursing home costs.
The total direct and indirect cost of CVD and stroke in the United States for 2007 is an estimated $286 billion (Table 22-1; Chart 22-1). This figure includes $167 billion in expenditures (direct costs, which include the cost of physicians and other professionals, hospital services, prescribed medications, and home health care) and $119 billion in lost productivity resulting from premature mortality (indirect costs).
The $286 billion is substantially lower than the estimate in the 2010 Statistical Update. Previously, annual estimates were based on the assumption that the proportion of CVD costs to total costs for physician services, hospital care, drugs, etc that were reported in a major study of 1995 direct costs were still valid in the current year. Each year, the 1995 proportions were applied to current National Health Expenditure Accounts (NHEA) of aggregate personal healthcare expenditures from the CMS to estimate direct costs.1 Because the assumption becomes weaker each year, the decision was made to use another data source.
The previous estimates of indirect morbidity costs of CVD were also unsatisfactory because they were based on extrapolations from 1980 data and were only corrected for annual inflation. In addition, the estimates for the specific CVDs were based on crude assumptions that used data for bed disability days. The true indirect morbidity costs of lost productivity due to CVD illnesses are probably large, but data to estimate them are inadequate.
Thus, the following changes were made:
The annual direct cost estimates are available on the Web site of the nationally representative MEPS of the AHRQ.1
The estimates of indirect morbidity costs will be discontinued until adequate estimates can be made.
Estimates of all direct costs and indirect mortality costs are limited to the latest year for which MEPS data are available, 2007, rather than projecting costs to 2011.
The advantages of using data from MEPS are as follows:
MEPS is designed to estimate healthcare utilization and expenditures linked to specific medical conditions for the US civilian noninstitutionalized population, and the estimates are based on person-level survey data directly linked to patient care events.2
The estimates are available annually on the MEPS Web site and can be customized by age, sex, and race/ethnicity.1
MEPS data have been used extensively in scientific publications and reports.2
Some disadvantages of using data from MEPS are as follows:
MEPS cost estimates cover a narrower population and a narrower range of healthcare expenditures than the NHEA estimates.3 For example, costs of nursing home care are not included.
The MEPS data are based on household reports, which are subject to underreporting and misreporting of individual medical events and to annual fluctuation.2
The $286 billion estimate includes some double counting of costs for individuals classified in more than 1 of the 4 CVD groups.
Direct costs for CHD and HF are not included in the list of conditions on the MEPS Web site.
Direct costs for hypertension exclude costs for hypertensive HD, which are included in the HD costs. There is no estimate for total hypertension.
There is no change in the way mortality costs are estimated except to limit estimates to the same year (2007) as for direct costs (personal communication [unpublished table of present value of lifetime earnings by age and sex, United States, 2005] from Wendy Max, PhD, University of California at San Francisco, and data from the National Center for Health Statistics4 and the US Census Bureau5).
Most Costly Diseases
CVD and stroke accounted for 15% of the total health expenditures in 2007.2,6 The total cost and the indirect mortality cost estimates for CVD are higher than for any other major diagnostic group.1 By way of comparison, CVD total direct and indirect costs shown in Table 22-1 are higher than the official National Cancer Institute estimates for cancer and benign neoplasms in 2010, which were cited as $264 billion total, $103 billion direct, $21 billion indirect morbidity, and $140 billion indirect cost of mortality.7
Table 22-2 shows direct and indirect costs for CVD by sex and by 2 broad age groups. Chart 22-2 shows total direct costs for the 13 leading chronic diseases in the MEPS list.
Abbreviations Used in Chapter 22
- AHRQ
Agency for Healthcare Research and Quality
- CHD
coronary heart disease
- CMS
Centers for Medicare & Medicaid Services
- CVD
cardiovascular disease
- HD
heart disease
- HF
heart failure
- MEPS
Medical Expenditure Panel Survey
- NHEA
National Health Expenditure Accounts
References
- 1.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. Table 3: Total expenses for selected conditions by type of service: United States, 2007. [Accessed September 7, 2010]; Available at: http://www.meps.ahrq.gov/mepsweb/data_stats/quick_tables.jsp.
- 2.Cohen JW, Cohen SB, Banthin JS. The Medical Expenditure Panel Survey: a national information resource to support healthcare cost research and inform policy and practice. Med Care. 2009;47(suppl 1):S44–S50. doi: 10.1097/MLR.0b013e3181a23e3a. [DOI] [PubMed] [Google Scholar]
- 3.Rosen AB, Cutler DM. Challenges in building disease-based national health accounts. Med Care. 2009;47(suppl 1):S7–S13. doi: 10.1097/MLR.0b013e3181a23e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Center for Health Statistics. Public use data sets for final U.S. 2007 mortality tabulated by the National Heart, Lung, and Blood Institute, Mortality multiple cause files. [Accessed June 2010]; Available at: http://www.cdc.gov/nchs/data_access/Vitalstatsonline.htm.
- 5.US Census Bureau. Historical income tables: people. Table P-37: full-time year-round workers age 15 and over by mean earnings and sex, 1955 to 2009. [Accessed September 28, 2010]; Available at: http://www.census.gov/hhes/www/income/data/historical/people/index.html.
- 6.Kashihara D, Carper K. Medical Expenditure Panel Survey, Statistical Brief No. 272. Rockville, Md: Agency for Healthcare Research and Quality; 2009. Dec, National health care expenditures in the U.S. civilian noninstitutionalized population, 2007. [Google Scholar]
- 7.American Cancer Society. Cancer facts and figures. [Accessed November 29, 2010]; Available at: http://www.cancer.org/Research/CancerFactsFigures/Cancer FactsFigures/cancer-facts-and-figures-2010. [Google Scholar]
23. At-a-Glance Summary Tables
See Tables 23-1 through 23-4.
Table 23-1.
Males and CVD: At-a-Glance Table
| Diseases and Risk Factors | Both Sexes | Total Males | White Males | Black Males | Mexican American Males |
|---|---|---|---|---|---|
| Total CVD | |||||
| Prevalence, 2008* | 82.6 M (36.2%) | 39.9 M (37.4%) | 37.4% | 44.8% | 30.7% |
| Mortality, 2007† | 813.8 K | 391.9 K | 334.6 K | 47.4 K | NA |
| CHD | |||||
| Prevalence, CHD, 2008* | 16.3 M (7.0%) | 8.8 M (8.3%) | 8.5% | 7.9% | 6.3% |
| Prevalence, MI, 2008* | 7.9 M (3.1%) | 4.8 M (4.3%) | 4.3% | 4.3% | 3.0% |
| Prevalence, AP, 2008* | 9.0 M (3.9%) | 4.0 M (3.8%) | 3.8% | 3.3% | 3.6% |
| New and recurrent CHDठ| 1.26 M | 740.0 K | 675.0 K | 70.0 K | NA |
| New and recurrent MI§ | 935.0 K | 565.0 K | NA | NA | NA |
| Incidence of AP (stable angina)‖ | 500.0 K | 320.0 K | NA | NA | NA |
| Mortality, 2007 CHD† | 406.4 K | 216.1 K | 189.1 K | 21.8 K | NA |
| Mortality, 2007 MI† | 133.0 K | 71.7 K | 63.0 K | 6.9 K | NA |
| Stroke | |||||
| Prevalence, 2008* | 7.0 M (3.0%) | 2.8 M (2.7%) | 2.4% | 4.5% | 2.0% |
| New and recurrent strokes† | 795.0 K | 370.0 K | 325.0 K | 45.0 K | NA |
| Mortality, 2007† | 136.0 K | 54.1 K | 44.7 K | 7.5 K | NA |
| HBP | |||||
| Prevalence, 2008* | 76.4 M (33.5%) | 36.5 M (34.1%) | 33.9% | 43.0% | 27.8% |
| Mortality, 2007† | 57.7 K | 25.0 K | 18.2 K | 6.1 K | NA |
| HF | |||||
| Prevalence, 2008* | 5.7 M (2.4%) | 3.1 M (3.0%) | 2.7% | 4.5% | 2.3% |
| Mortality, 2007† | 56.6 K | 22.9 K | 20.3 K | 2.3 K | NA |
| Smoking | |||||
| Prevalence, 2009¶ | 46.6 M (20.6%) | 25.7 M (23.1%) | 25.0% | 22.9% | NA |
| Blood cholesterol | |||||
| Prevalence, 2008 | |||||
| Total cholesterol ≥200 mg/dL* | 98.8 M (44.4%) | 45.0 M (41.8%) | 41.2% | 37.0% | 50.1% |
| Total cholesterol ≥240 mg/dL* | 33.6 M (15.0%) | 14.6 M (13.5%) | 13.7% | 9.7% | 16.9% |
| LDL-C ≥130 mg/dL* | 71.3 M (31.9%) | 35.3 M (32.5%) | 30.5% | 34.4% | 41.9% |
| HDL-C <40 mg/dL* | 41.8 M (18.9%) | 30.8 M (28.6%) | 29.5% | 16.6% | 31.7% |
| PA# | |||||
| Prevalence, 2009¶ | 34.9% | 37.4% | 40.1% | 36.0% | NA |
| Overweight and obesity | |||||
| Prevalence, 2008 | |||||
| Overweight and obesity, BMI ≥25.0 kg/m2* | 149.3 M (67.3%) | 78.0 M (72.4%) | 72.3% | 70.8% | 77.5% |
| Obesity, BMI ≥30.0 kg/m2* | 75.0 M (33.7%) | 34.9 M (32.4%) | 32.1% | 37.0% | 31.4% |
| DM | |||||
| Prevalence, 2008 | |||||
| Physician-diagnosed DM* | 18.3 M (8.2%) | 8.3 M (7.7%) | 6.8% | 14.3% | 11.0% |
| Undiagnosed DM* | 7.1 M (3.2%) | 4.4 M (4.2%) | 3.9% | 4.8% | 6.3% |
| Prediabetes* | 81.5 M (36.8%) | 48.1 M (44.7%) | 45.4% | 31.6% | 44.9% |
| Incidence, diagnosed DM* | 1.6 M | NA | NA | NA | NA |
| Mortality, 2007† | 71.4 K | 35.5 K | 28.7 K | 5.5 K | NA |
CVD indicates cardiovascular disease; M, millions; K, thousands; NA, data not available; CHD, coronary heart disease (includes heart attack, angina pectoris chest pain, or both); MI, myocardial infarction (heart attack); AP, angina pectoris (chest pain); mg/dL, milligrams per deciliter; HBP, high blood pressure; HF, heart failure; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; PA, physical activity; BMI, body mass index; kg/m2, kilograms per square meter; DM, diabetes mellitus.
Age ≥20 years.
All ages.
New and recurrent MI and fatal CHD.
Age ≥35 years.
Age ≥45 years.
Age ≥18 years.
Regular leisure-time PA.
Sources: See summary tables for each chapter in this Update.
Table 23-4.
Children, Youth, and CVD: At-a-Glance Table
| NH Whites | NH Blacks | Mexican Americans |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Diseases and Risk Factors | Both Sexes | Total Males | Total Females | Males | Females | Males | Females | Males | Females |
| Congenital cardiovascular defects | |||||||||
| Mortality, 2007* | 3.5 K | 1.9 K | 1.6 K | 1.5 K | 1.2 K | 0.3 K | 0.3 K | NA | NA |
| Smoking, % | |||||||||
| High school students, grades 9–12 | |||||||||
| Current cigarette smoking, 2009 | 19.5 | 19.8 | 19.1 | 22.3 | 22.8 | 10.7 | 8.4 | 19.4† | 16.7† |
| Current cigar smoking, 2009 | 14.0 | 18.6 | 8.8 | 21.0 | 8.0 | 13.9 | 11.5 | 15.8† | 9.5† |
| Blood cholesterol | |||||||||
| Mean total cholesterol, mg/dL | |||||||||
| Ages 4–11 y | 164.5 | 163.8 | 165.2 | 163.9 | 165.6 | 165.7 | 162.3 | 160.7 | 161.5 |
| Ages 12–19 y | 159.2 | 156.3 | 162.3 | 155.9 | 162.3 | 157.7 | 163.6 | 156.9 | 161.3 |
| Mean HDL-C, mg/dL | |||||||||
| Ages 4–11 y | 54.7 | 55.6 | 53.6 | 54.7 | 52.8 | 61.4 | 58.1 | 53.6 | 51.1 |
| Ages 12–19 y | 51.6 | 49.3 | 54.0 | 48.1 | 53.3 | 54.6 | 56.9 | 48.3 | 53.5 |
| Mean LDL-C, mg/dL | |||||||||
| Ages 12–19 y | 88.5 | 87.1 | 89.9 | 87.6 | 89.8 | 88.8 | 92.6 | 88.4 | 88.8 |
| PA‡ | |||||||||
| Prevalence, grades 9–12, 2009§ | |||||||||
| Met currently recommended levels of PA, % | 37.0 | 45.6 | 27.7 | 47.3 | 31.3 | 43.3 | 21.9 | 41.3† | 24.9† |
| Overweight and obesity | |||||||||
| Prevalence, 2008 | |||||||||
| Children and adolescents, ages 2–19 y (overweight or obese) | 23.5 M (31.9%) | 12.3 M (32.7%) | 11.2 M (31.0%) | 31.9% | 29.5% | 30.8% | 39.2% | 40.8% | 35.0% |
| Students in grades 9–12§ (overweight only) | 15.8% | 15.1% | 9.6% | 15.7% | 12.8% | 16.6% | 21.4% | 18.3%† | 17.9%† |
CVD indicates cardiovascular disease; K, thousands; NA, data not available; mg/dL, milligrams per deciliter; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; PA, physical activity; M, millions.
Overweight indicates a body mass index in the 95th percentile of the Centers for Disease Control and Prevention 2000 growth chart.
All ages.
Hispanic.
Regular leisure-time physical activity.
Centers for Disease Control and Prevention.1
Sources: See summary tables in related chapters in this Update. For more data on congenital defects, see Chapter 8.
References
- 1.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Lim C, Whittle L, Brener ND, Wechsler H Centers for Disease Control and Prevention (CDC) Youth risk behavior surveillance: United States, 2009. MMWR Surveill Summ. 2010;59:1–142. [PubMed] [Google Scholar]
Chart 3-2.
Incidence of cardiovascular disease* by age and sex (FHS, 1980–2003). *Coronary heart disease, heart failure, stroke, or intermittent claudication. Does not include hypertension alone. Source: National Heart, Lung, and Blood Institute.3
Chart 3-3.
Deaths due to diseases of the heart (United States: 1900–2007). See Glossary (Chapter 24) for an explanation of “diseases of the heart.” Note: In the years 1900–1920, the International Classification of Diseases codes were 77–80; for 1925, 87–90; for 1930–1945, 90–95; for 1950–1960, 402–404, 410–443; for 1965, 402–404, 410–443; for 1970–1975, 390–398, 404–429; for 1980–1995, 390–398, 402, 404–429; for 2000–2007, I00 –I09, I11, I13, I20 –I51. Source: National Center for Health Statistics.
Chart 3-4.
Deaths due to cardiovascular disease (United States: 1900–2007). Cardiovascular disease does not include congenital. Source: National Center for Health Statistics.
Chart 3-5.
Percentage breakdown of deaths due to cardiovascular disease (United States: 2007). Source: National Heart, Lung, and Blood Institute from National Center for Health Statistics reports and data sets. *Not a true underlying cause. With any mention deaths, heart failure accounts for 34 percent of cardiovascular disease deaths. Total may not add to 100 because of rounding.
Chart 3-6.
Cardiovascular disease (CVD) deaths versus cancer deaths by age (United States: 2007). Source: National Center for Health Statistics.
Chart 3-7.
Cardiovascular disease (CVD) and other major causes of death: total, <85 years of age, and ≥85 years of age. Deaths among both sexes, United States, 2007. CLRD indicates chronic lower respiratory disease. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 3-8.
Cardiovascular disease (CVD) and other major causes of death: total, <85 years of age and ≥85 years of age. Deaths among males, United States, 2007. CLRD indicates chronic lower respiratory disease. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 3-9.
Cardiovascular disease (CVD) and other major causes of death: total, <85 years of age, and ≥85 years of age. Deaths among females, United States, 2007. CLRD indicates chronic lower respiratory disease. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 3-10.
Cardiovascular disease and other major causes of death for all males and females (United States: 2007). A indicates cardiovascular disease plus congenital cardiovascular disease; B, cancer; C, accidents; D, chronic lower respiratory disease; E, diabetes mellitus; F, Alzheimer disease. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 3-11.
Cardiovascular disease and other major causes of death for white males and females (United States: 2007). A indicates cardiovascular disease plus congenital cardiovascular disease; B, cancer; C, accidents; D, chronic lower respiratory disease; E, diabetes mellitus; F, Alzheimer disease. Source: National Center for Health Statistics.
Chart 3-12.
Cardiovascular disease and other major causes of death for black males and females (United States: 2007). A indicates cardiovascular disease plus congenital cardiovascular disease; B, cancer; C, accidents; D, assault (homicide); E, diabetes mellitus; F, nephritis. Source: National Center for Health Statistics.
Chart 3-13.
Cardiovascular disease and other major causes of death for Hispanic or Latino males and females (United States: 2007). A indicates diseases of the heart and stroke; B, cancer; C, accidents; D, diabetes mellitus; E, assault (homicide); F, chronic lower respiratory disease. Source: National Center for Health Statistics.
Chart 3-14.
Cardiovascular disease and other major causes of death for Asian or Pacific Islander males and females (United States: 2007). “Asian or Pacific Islander” is a heterogeneous category that includes people at high cardiovascular disease risk (eg, South Asian) and people at low cardiovascular disease risk (eg, Japanese). More specific data on these groups are not available. A indicates cardiovascular disease (I00 –I99); B, cancer; C, accidents; D, diabetes mellitus; E, chronic lower respiratory disease; F, influenza and pneumonia. Source: National Center for Health Statistics.
Chart 3-15.
Cardiovascular disease and other major causes of death for American Indian or Alaska Native males and females (United States: 2007). A indicates cardiovascular disease (I00 –I99); B, cancer; C, accidents; D, chronic liver disease; E, diabetes mellitus; F, chronic lower respiratory disease. Source: National Center for Health Statistics.
Chart 3-16.
Age-adjusted death rates for coronary heart disease (CHD), stroke, and lung and breast cancer for white and black females (United States: 2007). Source: National Center for Health Statistics.
Chart 3-17.
Cardiovascular disease mortality trends for males and females (United States: 1979–2007). The overall comparability for cardiovascular disease between the International Classification of Diseases, 9th Revision (1979–1998) and International Classification of Diseases, 10th Revision (1999–2007) is 0.9962. No comparability ratios were applied. Source: National Center for Health Statistics.
Chart 3-18.
Hospital discharges for cardiovascular disease (United States: 1970–2007). Hospital discharges include people discharged alive, dead, and “status unknown.” Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 3-19.
Hospital discharges for the 10 leading diagnostic groups (United States: 2007). Source: National Hospital Discharge Survey/National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 3-20.
Estimated average 10-year cardiovascular disease risk in adults 50 to 54 years of age according to levels of various risk factors (Framingham Heart Study). HDL indicates high-density lipoprotein; BP, blood pressure. Data derived from D’Agostino et al72 with permission of the publisher. Copyright © 2008, American Heart Association.
Chart 6-3.
Annual rate of first cerebral infarction by age, sex, and race (Greater Cincinnati/Northern Kentucky Stroke Study: 1999). Rates for black men and women 45 to 54 years of age and for black men ≥75 years of age are considered unreliable. An estimated 15 000 people have first cerebral infarctions before 45 years of age. Source: Unpublished data from the Greater Cincinnati/Northern Kentucky Stroke Study.
Chart 6-4.
Annual rate of all first-ever strokes by age, sex, and race (Greater Cincinnati/Northern Kentucky Stroke Study: 1999). Rates for black men and women 45 to 54 years of age and for black men ≥75 years of age are considered unreliable.
Chart 6-5.
Estimated 10-year stroke risk in adults 55 years of age according to levels of various risk factors (Framingham Heart Study). AF indicates atrial fibrillation; CVD, cardiovascular disease. Data derived from Wolf et al170 with permission of the publisher. Copyright © 1991, American Heart Association.
Chart 6-6.
Trends in carotid endarterectomy procedures (United States: 1979–2007). Source: National Hospital Discharge Survey/National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 6-8.
Trends in carotid revascularization procedures. MCBE indicates Medicare beneficiaries; CEA, carotid endarterectomy; CAS, carotid artery stenting. Reproduced with permission from Goodney et al.133 Copyright © 2008, American Medical Association. All rights reserved.
Chart 7-2.
Age-adjusted prevalence trends for high blood pressure in adults ≥20 years of age by race/ethnicity, sex, and survey (National Health and Nutrition Examination Survey: 1988–1994, 1999–2004, and 2005–2008). NH indicates non-Hispanic. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 7-3.
Extent of awareness, treatment, and control of high blood pressure by race/ethnicity (National Health and Nutrition Examination Survey: 2005–2008). NH indicates non-Hispanic. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 7-4.
Extent of awareness, treatment and control of high blood pressure by age (National Health and Nutrition Examination Survey: 2005–2008). Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 9-2.
Incidence of heart failure (heart failure based on physician review of medical records and strict diagnostic criteria) by age and sex (Framingham Heart Study: 1980–2003). Source: National Heart, Lung, and Blood Institute.
Chart 13-2.
Trends in mean total serum cholesterol among adults ages ≥20 years old by race and survey year (National Health and Nutrition Examination Survey: 1988–1994, 1999–2004, and 2005–2008). Values are in mg/dL. NH indicates non-Hispanic. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 14-2.
Prevalence of regular leisure-time physical activity among adults >18 years of age by race/ethnicity and sex (National Health Interview Survey: 2009). Percentages are age-adjusted. “Regular leisure-time physical activity” was defined as ≥3 sessions per week of vigorous activity lasting at least 20 minutes or ≥5 sessions per week of light or moderate activity lasting at least 30 minutes. NH indicates non-Hispanic. Data derived from Pleis et al.7
Chart 14-3.
Prevalence of students in grades 9 to 12 who did not participate in at least 60 minutes of physical activity on any day by race/ethnicity and sex (Youth Risk Behavior Surveillance: 2009). NH indicates non-Hispanic. Data derived from MMWR Surveillance Summaries.1
Chart 15-2.
Age-adjusted prevalence of obesity in adults 20 to 74 years of age by sex and survey year (National Health Examination Survey: 1960–1962; National Health and Nutrition Examination Survey: 1971–1975, 1976–1980, 1988–1994, 1999–2002, and 2003–2006). Obesity is defined as a body mass index of ≥30.0 kg/m2. Data derived from Health, United States, 2009 (National Center for Health Statistics).44
Chart 16-2.
Age-adjusted prevalence of physician-diagnosed type 2 diabetes mellitus in adults ≥20 years of age by race/ethnicity and years of education (National Health and Nutrition Examination Survey: 2005–2008). NH indicates non-Hispanic. Source: National Center for Health Statistics and National Heart, Lung, and Blood Institute.
Chart 16-3.
Trends in diabetes mellitus prevalence in adults ≥20 years of age by sex (National Health and Nutrition Examination Survey: 1988–1994 and 2005–2008). Source: National Center for Health Statistics, National Heart, Lung, and Blood Institute.
Chart 21-2.
Trends in cardiovascular procedures, United States: 1979–2007. PCI indicates percutaneous coronary intervention. Note: In-hospital procedures only. Source: National Hospital Discharge Survey, National Center for Health Statistics, and National Heart, Lung, and Blood Institute.
Table 3-2.
Age-Adjusted Death Rates per 100 000 Population for CVD, CHD, and Stroke by State; 2005–2007
| CVD* | CHD† | Stroke‡ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| State | Rank§ | Death Rate |
% Change 1999–2001 to 2005–2007 |
Rank§ | Death Rate |
% Change 1999–2001 to 2005–2007 |
Rank§ | Death Rate |
% Change 1999–2001 to 2005–2007 |
| Alabama | 51 | 326.9 | −16.0 | 20 | 116.6 | −28.9 | 50 | 56.3 | −19.3 |
| Alaska | 6 | 221.6 | −22.3 | 4 | 87.9 | −31.7 | 35 | 48.1 | −26.1 |
| Arizona | 5 | 217.0 | −24.3 | 25 | 121.5 | −25.7 | 4 | 35.3 | −32.8 |
| Arkansas | 45 | 307.4 | −19.5 | 46 | 159.5 | −14.8 | 51 | 58.0 | −24.8 |
| California | 27 | 252.9 | −23.0 | 33 | 136.3 | −28.7 | 29 | 44.9 | −29.4 |
| Colorado | 4 | 216.1 | −21.8 | 7 | 98.2 | −23.9 | 11 | 40.1 | −29.6 |
| Connecticut | 14 | 229.6 | −23.4 | 14 | 110.1 | −31.4 | 5 | 35.7 | −29.4 |
| Delaware | 28 | 262.2 | −21.8 | 39 | 143.1 | −28.1 | 14 | 41.3 | −21.3 |
| District of Columbia | 50 | 325.6 | −13.4 | 52 | 187.6 | −7.2 | 18 | 42.5 | −11.5 |
| Florida | 12 | 227.7 | −26.4 | 27 | 128.5 | −32.1 | 6 | 35.7 | −27.7 |
| Georgia | 41 | 287.6 | −23.8 | 10 | 107.9 | −33.6 | 44 | 51.5 | −28.5 |
| Hawaii | 2 | 206.0 | −24.3 | 3 | 82.0 | −28.4 | 20 | 43.0 | −31.1 |
| Idaho | 19 | 234.4 | −21.2 | 11 | 108.9 | −26.3 | 38 | 48.9 | −24.8 |
| Illinois | 31 | 264.8 | −23.9 | 29 | 132.8 | −30.8 | 30 | 45.2 | −26.6 |
| Indiana | 39 | 284.7 | −21.6 | 32 | 136.2 | −27.4 | 37 | 48.6 | −28.9 |
| Iowa | 24 | 247.6 | −21.8 | 37 | 140.8 | −24.5 | 25 | 44.5 | −25.7 |
| Kansas | 25 | 252.7 | −20.9 | 15 | 112.4 | −27.4 | 34 | 46.8 | −23.4 |
| Kentucky | 44 | 304.5 | −22.3 | 42 | 149.6 | −25.5 | 42 | 49.6 | −26.7 |
| Louisiana | 47 | 311.0 | −17.9 | 36 | 139.6 | −26.0 | 45 | 52.6 | −19.8 |
| Maine | 18 | 234.2 | −24.3 | 16 | 113.5 | −30.9 | 16 | 41.8 | −27.7 |
| Maryland | 33 | 269.2 | −21.2 | 40 | 144.9 | −23.9 | 22 | 44.0 | −29.6 |
| Massachusetts | 9 | 224.1 | −22.6 | 9 | 106.9 | −27.2 | 10 | 37.9 | −24.7 |
| Michigan | 42 | 293.2 | −20.9 | 45 | 158.0 | −25.4 | 32 | 45.5 | −26.3 |
| Minnesota | 1 | 193.1 | −25.9 | 2 | 80.5 | −33.2 | 12 | 40.1 | −28.8 |
| Mississippi | 52 | 349.7 | −19.3 | 41 | 147.2 | −29.4 | 46 | 53.3 | −25.4 |
| Missouri | 43 | 293.9 | −21.0 | 44 | 154.2 | −25.1 | 43 | 50.4 | −21.6 |
| Montana | 11 | 226.6 | −20.9 | 6 | 97.6 | −21.5 | 19 | 42.7 | −29.2 |
| Nebraska | 17 | 232.8 | −23.0 | 5 | 94.4 | −29.2 | 28 | 44.8 | −22.8 |
| Nevada | 40 | 287.4 | −16.8 | 21 | 117.4 | −29.1 | 17 | 42.3 | −26.8 |
| New Hampshire | 13 | 229.1 | −26.9 | 24 | 120.9 | −33.9 | 2 | 35.2 | −36.8 |
| New Jersey | 25 | 252.2 | −23.7 | 38 | 141.1 | −29.0 | 7 | 35.9 | −23.8 |
| New Mexico | 7 | 222.1 | −19.8 | 17 | 114.7 | −25.0 | 9 | 37.7 | −26.2 |
| New York | 37 | 278.6 | −21.1 | 51 | 182.1 | −23.6 | 1 | 29.6 | −27.1 |
| North Carolina | 34 | 270.4 | −24.4 | 28 | 128.7 | −29.9 | 47 | 53.4 | −30.0 |
| North Dakota | 22 | 241.3 | −20.3 | 30 | 133.5 | −19.6 | 24 | 44.2 | −26.1 |
| Ohio | 38 | 283.2 | −22.0 | 43 | 151.4 | −25.3 | 33 | 46.5 | −23.3 |
| Oklahoma | 49 | 322.4 | −20.6 | 50 | 176.2 | −23.5 | 49 | 54.4 | −20.5 |
| Oregon | 15 | 230.6 | −22.1 | 8 | 98.7 | −26.8 | 40 | 49.3 | −33.1 |
| Pennsylvania | 35 | 271.4 | −22.1 | 34 | 137.9 | −28.0 | 26 | 44.6 | −22.6 |
| Puerto Rico‖ | 8 | 223.5 | −15.9 | 13 | 109.4 | −15.8 | 23 | 44.1 | −15.5 |
| Rhode Island | 29 | 260.4 | −16.8 | 48 | 170.6 | −19.0 | 3 | 35.2 | −26.7 |
| South Carolina | 36 | 274.1 | −25.2 | 23 | 119.8 | −32.3 | 48 | 53.7 | −33.1 |
| South Dakota | 20 | 238.1 | −21.2 | 35 | 137.9 | −17.5 | 31 | 45.4 | −21.9 |
| Tennessee | 48 | 315.3 | −19.4 | 49 | 171.1 | −22.3 | 52 | 58.1 | −23.7 |
| Texas | 32 | 266.9 | −24.0 | 31 | 134.9 | −30.5 | 41 | 49.3 | −25.1 |
| Utah | 3 | 213.2 | −21.3 | 1 | 78.6 | −30.8 | 13 | 40.4 | −34.0 |
| Vermont | 10 | 226.3 | −24.0 | 26 | 121.6 | −26.0 | 8 | 37.1 | −31.2 |
| Virginia | 28 | 254.7 | −23.1 | 19 | 114.8 | −27.4 | 36 | 48.3 | −28.4 |
| Washington | 16 | 232.4 | −22.6 | 22 | 117.5 | −26.0 | 21 | 43.7 | −36.8 |
| West Virginia | 46 | 309.1 | −22.0 | 47 | 160.7 | −27.1 | 39 | 49.2 | −19.9 |
| Wisconsin | 23 | 242.6 | −24.0 | 18 | 114.7 | −29.9 | 27 | 44.7 | −30.3 |
| Wyoming | 21 | 238.7 | −19.4 | 13 | 109.3 | −25.1 | 15 | 41.4 | −29.2 |
| Total United States | 262.7 | −22.6 | 135.1 | −27.7 | 44.1 | −26.9 | |||
Cardiovascular disease (CVD) is defined here as International Classification of Diseases (ICD)-10 I00–I78.
Coronary heart disease (CHD) is defined here as ICD-10 I20–I25.
Stroke is defined here as ICD-10 I60–I69.
Rank is lowest to highest.
Percentage changes for Puerto Rico are for 2000 to 2005–2007.
Source: Health Data Interactive, 2005–2007. Data provided by personal communication with National Heart, Lung, and Blood Institute.
The Agency for Healthcare Research and Quality has released state-level data for heart disease for all 50 states and the District of Columbia. The data are taken from the Congressionally mandated National Healthcare Quality Report (NHQR), available at http://statesnapshots.ahrq.gov/snaps07/index.jsp. In addition, the Women’s Health and Mortality Chartbook of the National Center for Health Statistics has state-related data for women available at http://www.cdc.gov/nchs/data/healthywomen/womenschartbook_aug2004.pdf. Also, at http://apps.nccd.cdc.gov/brfss-smart/index.asp, Metropolitan/Micropolitan Area Risk (MMSA) data are available for 500 such areas nationwide. Behavioral Risk Factor Surveillance System data are also collected within each state (http://www.cdc.gov/brfss). The Centers for Disease Control and Prevention (CDC) has the Geographic Information Systems (GIS), which provides mortality rates down to the county level, by sex and ethnicity, available at http://www.cdc.gov/gis/. The 2008 Atlas of Stroke Hospitalizations Among Medicare Beneficiaries (CDC, 2008) is a new resource that provides data down to the county level, by sex and race (available at http://www.cdc.gov/dhdsp/library/stroke_hospitalization_atlas.htm).
Table 3-3.
International Death Rates (Revised 2010): Death Rates (Per 100 000 Population) for Total CVD, CHD, Stroke, and Total Deaths in Selected Countries (Most Recent Year Available)
| ICD Revision 9 or 10 |
CVD Deaths |
CHD Deaths |
Stroke Deaths |
Total Deaths |
|
|---|---|---|---|---|---|
| Men, ages 35–74 y | |||||
| Russian Federation (2006) | 10 | 1299.2 | 706.0 | 351.4 | 2683.4 |
| Bulgaria (2006) | 10 (new) | 899.5 | 253.5 | 239.8 | 1635.2 |
| Hungary (2005) | 10 | 709.7 | 384.7 | 140.8 | 1818.0 |
| Romania (2008) | 10 | 682.6 | 283.5 | 204.3 | 1560.2 |
| Argentina (1996) | 9 | 531.0 | 140.3 | 115.7 | 1344.3 |
| Poland (2007) | 10 | 503.1 | 190.8 | 103.2 | 1448.1 |
| Colombia (1994) | 9 | 397.1 | 189.6 | 90.0 | 1166.1 |
| Czech Republic (2008) | 10 | 396.6 | 209.7 | 64.1 | 1098.8 |
| China - Urban (2000) | 9 | 374.8 | 108.3 | 160.1 | 976.8 |
| Scotland (2007) | 10 | 294.8 | 195.3 | 46.1 | 936.1 |
| Finland (2008) | 10 | 290.9 | 173.6 | 44.1 | 845.9 |
| Mexico (1995) | 9 | 273.3 | 136.8 | 60.5 | 1172.0 |
| China - Rural (2000) | 9 | 265.3 | 41.6 | 364.5 | 828.0 |
| Greece (2008) | 9 | 262.2 | 135.9 | 55.1 | 733.8 |
| United States (2007) | 10 | 262.8 | 153.3 | 31.6 | 868.9 |
| Portugal (2003) | 10 | 252.8 | 96.6 | 96.1 | 966.5 |
| Germany (2006) | 10 | 242.1 | 125.3 | 34.5 | 788.5 |
| Northern Ireland (2007) | 10 | 232.4 | 161.9 | 29.6 | 781.2 |
| Ireland (2007) | 10 (new) | 227.6 | 152.5 | 25.7 | 701.3 |
| Belgium (2004) | 10 | 222.6 | 106.5 | 37.6 | 825.0 |
| England/Wales (2007) | 10 | 219.7 | 138.3 | 32.7 | 702.2 |
| New Zealand (2005) | 10 | 206.8 | 138.4 | 3 30. | 646.3 |
| Denmark (2006) | 10 | 206.6 | 84.8 | 45.6 | 865.6 |
| Canada (2004) | 10 | 198.3 | 130.8 | 24.2 | 705.3 |
| Sweden (2007) | 10 | 193.9 | 115.6 | 30.6 | 602.5 |
| Spain (2005) | 10 | 191.2 | 92.1 | 39.2 | 786.3 |
| Austria (2008) | 10 | 184.7 | 105.9 | 27.1 | 708.2 |
| Norway (2007) | 10 | 177.3 | 95.9 | 29.0 | 633.8 |
| Republic of Korea (2006) | 10 | 175.6 | 51.4 | 93.1 | 895.1 |
| Netherlands (2008) | 10 | 162.5 | 66.2 | 26.6 | 637.3 |
| Italy (2007) | 10 | 160.6 | 75.6 | 29.9 | 625.8 |
| Switzerland (2007) | 10 | 150.4 | 78.2 | 16.6 | 587.5 |
| Japan (2008) | 10 | 149.9 | 47.6 | 54.4 | 619.6 |
| Israel (2006) | 10 | 147.8 | 78.7 | 31.2 | 650.5 |
| France (2007) | 10 | 145.1 | 58.4 | 26.5 | 775.3 |
| Australia (2006) | 10 | 141.3 | 88.9 | 22.0 | 553.4 |
| Women, ages 35–74 y | |||||
| Russian Federation (2006) | 10 | 521.4 | 237.1 | 189.2 | 1001.8 |
| Bulgaria (2006) | 10 (new) | 420.4 | 86.7 | 137.5 | 750.7 |
| Romania (2008) | 10 | 332.3 | 112.9 | 122.6 | 705.6 |
| Hungary (2005) | 10 | 291.1 | 144.6 | 67.0 | 780.4 |
| Colombia (1994) | 9 | 286.1 | 110.2 | 83.8 | 747.7 |
| China - Urban (2000) | 9 | 258.9 | 71.9 | 103.1 | 637.7 |
| Argentina (1996) | 9 | 227.2 | 39.4 | 63.2 | 642.3 |
| Mexico (1995) | 9 | 196.5 | 73.2 | 52.4 | 773.1 |
| Poland (2007) | 10 | 186.9 | 54.9 | 52.5 | 579.2 |
| China–Rural (2000) | 9 | 184.6 | 29.1 | 239.1 | 528.1 |
| Czech Republic (2008) | 10 | 163.4 | 70.7 | 35.0 | 518.5 |
| Scotland (2007) | 10 | 130.9 | 67.5 | 33.0 | 590.0 |
| United States (2007) | 10 | 131.5 | 60.4 | 24.3 | 546.3 |
| Portugal (2003) | 10 | 123.2 | 34.8 | 54.6 | 448.7 |
| Northern Ireland (2007) | 10 | 101.4 | 51.5 | 28.1 | 470.7 |
| Greece (2008) | 9 | 101.0 | 34.1 | 30.9 | 330.3 |
| Denmark (2006) | 10 | 100.0 | 32.4 | 32.1 | 557.8 |
| Germany (2006) | 10 | 97.8 | 38.2 | 20.1 | 402.4 |
| England/Wales (2007) | 10 | 97.1 | 43.4 | 25.4 | 450.4 |
| New Zealand (2005) | 10 | 97.0 | 47.2 | 27.1 | 425.3 |
| Ireland (2007) | 10 (new) | 96.2 | 48.6 | 21.1 | 434.9 |
| Belgium (2004) | 10 | 95.3 | 32.1 | 26.6 | 430.9 |
| Republic of Korea (2006) | 10 | 89.0 | 20.0 | 50.8 | 359.3 |
| Finland (2008) | 10 | 84.8 | 39.9 | 22.1 | 380.4 |
| Canada (2004) | 10 | 83.1 | 42.8 | 17.3 | 432.7 |
| Sweden (2007) | 10 | 79.5 | 36.4 | 20.6 | 382.2 |
| Netherlands (2008) | 10 | 76.3 | 22.8 | 19.2 | 425.0 |
| Austria (2008) | 10 | 73.8 | 33.0 | 16.2 | 358.8 |
| Spain (2005) | 10 | 73.5 | 22.9 | 21.0 | 325.9 |
| Norway (2007) | 10 | 69.3 | 27.7 | 19.2 | 394.7 |
| Israel (2006) | 10 | 69.0 | 26.9 | 18.7 | 391.7 |
| Italy (2007) | 10 | 67.3 | 22.2 | 18.2 | 326.0 |
| Australia (2006) | 10 | 60.4 | 26.8 | 16.3 | 327.5 |
| Japan (2008) | 10 | 57.9 | 13.8 | 24.4 | 277.1 |
| Switzerland (2007) | 10 | 54.1 | 19.4 | 12.4 | 327.6 |
| France (2007) | 10 | 51.3 | 12.2 | 14.0 | 346.2 |
Rates are adjusted to the European Standard population. For countries using International Classification of Diseases (ICD)-9, the ICD-9 codes are 390–459 for CVD, 410–414 for coronary heart disease (CHD), and 430–438 for stroke. ICD-10 codes are I00–I99 for cardiovascular disease (CVD), I20 –I25 for CHD, and I60–I69 for stroke.
Sources: The World Health Organization, National Center for Health Statistics, and National Heart, Lung, and Blood Institute.
Table 8-2.
| Type of Presentation | Rate per 1000 Live Births |
n |
|---|---|---|
| Fetal loss | Unknown | Unknown |
| Invasive procedure during the first year | 2.3 | 9200 |
| Detected during first year* | 9 | 36 000 |
| Bicuspid aortic valve | 13.7 | 54 800 |
| Other defects detected after first year | Unknown | Unknown |
| Total | Unknown | Unknown |
Includes stillbirths and pregnancy termination at <20 weeks’ gestation; includes some defects that resolve spontaneously or do not require treatment.
Table 8-3.
Estimated Prevalence of Congenital Cardiovascular Defects and Percent Distribution by Type, United States, 2002* (in Thousands)
| Prevalence, n | Percent of Total | |||||
|---|---|---|---|---|---|---|
| Type | Total | Children | Adults | Total | Children | Adults |
| Total | 994 | 463 | 526 | 100 | 100 | 100 |
| VSD† | 199 | 93 | 106 | 20.1 | 20.1 | 20.1 |
| ASD | 187 | 78 | 109 | 18.8 | 16.8 | 20.6 |
| Patent ductus arteriosus | 144 | 58 | 86 | 14.2 | 12.4 | 16.3 |
| Valvular pulmonic stenosis | 134 | 58 | 76 | 13.5 | 12.6 | 14.4 |
| Coarctation of aorta | 76 | 31 | 44 | 7.6 | 6.8 | 8.4 |
| Valvular aortic stenosis | 54 | 25 | 28 | 5.4 | 5.5 | 5.2 |
| TOF | 61 | 32 | 28 | 6.1 | 7 | 5.4 |
| Atrioventricular septal defect | 31 | 18 | 13 | 3.1 | 3.9 | 2.5 |
| TGA | 26 | 17 | 9 | 2.6 | 3.6 | 1.8 |
| Hypoplastic right heart syndrome | 22 | 12 | 10 | 2.2 | 2.5 | 1.9 |
| Double-outlet right ventricle | 9 | 9 | 0 | 0.9 | 1.9 | 0.1 |
| Single ventricle | 8 | 6 | 2 | 0.8 | 1.4 | 0.3 |
| Anomalous pulmonary venous connection | 9 | 5 | 3 | 0.9 | 1.2 | 0.6 |
| Truncus arteriosus | 9 | 6 | 2 | 0.7 | 1.3 | 0.5 |
| HPLHS | 3 | 3 | 0 | 0.3 | 0.7 | 0 |
| Other | 22 | 12 | 10 | 2.1 | 2.6 | 1.9 |
VSD indicates ventricular septal defect; ASD, atrial septal defect; TOF, tetralogy of Fallot; TGA, transposition of the great arteries; HPLHS, hypoplastic left heart syndrome.
Excludes an estimated 3 million bicuspid aortic valve prevalence (2 million in adults and 1 million in children).
Small VSD, 117 000 (65 000 adults and 52 000 children); large VSD, 82 000 (41 000 adults and 41 000 children).
Table 20-2.
Heart Failure Quality-of-Care Measures, 2009
| Quality-of-Care Measure | National Medicare and Medicaid |
AHA- GWTG-HF |
VHA |
|---|---|---|---|
| LVEF assessment | 97 | 98* | 100 |
| ARB/ACEI at discharge for patients with left ventricular systolic dysfunction | 93 | 93* | 96 |
| Complete discharge instructions | 85 | 91* | 96 |
| Adult smoking cessation advice/counseling | 98 | 98* | 98 |
| β-blockers at discharge for patients with LVSD, no contraindications | NM | 93* | 90 |
| Anticoagulation for AF or atrial flutter, no contraindications | NM | 69 | 94 |
AHA GWTG-HF indicates American Heart Association Get With The Guidelines–Heart Failure; VHA, Veterans Health Administration; LVEF, left ventricular ejection fraction; ARB, angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; LVSD, left ventricular systolic dysfunction; NM, not measured; AF, atrial fibrillation.
Values are percentages.
In the GWTG registry, mechanical ventilation was required in 3.0% of patients. In-hospital mortality rate was 3.0%, and mean length of hospital stay was 5.5 days (median 4.0 days).
Indicates the 5 key performance measures targeted in GWTG-HF. The composite quality-of-care measure for 2009 was 94.5%. The composite quality-of-care measure indicates performance on the provision of several elements of care. It is computed by summing the numerators for each key performance measure across the population of interest to create a composite numerator (all the care that was given), summing the denominators for each measure to form a composite denominator (all the care that should have been given), and reporting the ratio (the percentage of all the needed care that was given).
Table 20-3.
Time Trends in GWTG-CAD Acute Coronary Syndrome Quality-of-Care Measures, 2006–2009
| Quality-of-Care Measure | 2006 | 2007 | 2008 | 2009 |
|---|---|---|---|---|
| Aspirin within 24 h of admission* | 94.7 | 92.8 | 91.2 | 90.9 |
| Aspirin at discharge* | 94.4 | 95.8 | 94.9 | 95.5 |
| β-blockers at discharge* | 92.8 | 94.6 | 94.5 | 94.9 |
| Lipid-lowering medication at discharge | 84.5 | 85.6 | 81.6 | 86.8 |
| Lipid therapy at discharge if LDL >100 mg/dL* | 89.1 | 90.7 | 91.9 | 92.5 |
| ARB/ACEI at discharge for patients with left ventricular ejection fraction <40%* | 87.3 | 91.1 | 91.9 | 91.9 |
| ACEI at discharge for AMI patients | 72.6 | 71.0 | 66.6 | 65.9 |
| Adult smoking cessation advice/counseling* | 94.3 | 97.4 | 98.4 | 98.4 |
| Cardiac rehabilitation referral for AMI patients | 71.1 | 63.6 | 52.0 | 49.1 |
GWTG indicates Get With The Guidelines; LDL, low-density lipoprotein cholesterol; ARB, angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; AMI, acute myocardial infarction.
Values are percentages.
GWTG-CAD: Patients admitted with cardiovascular event. In the GWTG-CAD registry. The in-hospital mortality was 4.5% (excludes transfer-out patients; if discharge status was missing, it was assumed to be “no”), and mean length of hospital stay was 5.0 days (median 3.0 days).
Table 20-4.
Time Trends in GWTG-HF Quality-of-Care Measures, 2006–2009
| Quality of Care Measure | 2006 | 2007 | 2008 | 2009 |
|---|---|---|---|---|
| Left ventricular ejection fraction assessment* | 93.8 | 96.2 | 96.8 | 98.2 |
| ARB/ACEI at discharge for patients with left ventricular systolic dysfunction* | 85.5 | 89.1 | 91.6 | 93.0 |
| Complete discharge instructions* | 78.8 | 84.8 | 88.5 | 90.9 |
| Adult smoking cessation advice/counseling* | 90.8 | 94.7 | 97.1 | 97.6 |
| β-blockers at discharge for patients with LVSD, no contraindications* | 89.9 | 90.2 | 92.5 | 92.7 |
| Anticoagulation for atrial fibrillation or atrial flutter, no contraindications | 62.9 | 61.6 | 60.7 | 68.9 |
GWTG-HF indicates Get With The Guidelines–Heart Failure; ARB, angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; LVSD, left ventricular systolic dysfunction.
Values are percentages.
In the GWTG registry, mechanical ventilation was required in 3.0% of patients. In-hospital mortality was 3.0%, and mean length of hospital stay was 5.5 days (median 4.0 days).
Indicates the 5 key achievement measures targeted in GWTG-HF. The composite quality of care measure for 2009 was 94.5%. The composite quality-of-care measure indicates performance on the provision of several elements of care. It is computed by summing the numerators for each key achievement measure across the population of interest to create a composite numerator (all the care that was given), summing the denominators for each measure to form a composite denominator (all the care that should have been given), and reporting the ratio (the percentage of all the needed care that was given).
Table 20-5.
Time Trends in GWTG-Stroke Quality-of-Care Measures, 2006–2009
| Quality of Care Measure | 2006 | 2007 | 2008 | 2009 |
|---|---|---|---|---|
| Thrombolytic complications: IV tPA and life-threatening, serious systemic hemorrhage | 20.8 | 17.3 | 16.1 | 15.1 |
| Antithrombotics <48 h after admission* | 94.8 | 95.8 | 96.0 | 96.2 |
| DVT prophylaxis by second hospital day* | 85.3 | 88.9 | 92.2 | 92.7 |
| Antithrombotics at discharge* | 94.1 | 95.1 | 97.0 | 97.8 |
| Anticoagulation for atrial fibrillation at discharge* | 88.2 | 89.5 | 93.1 | 93.5 |
| Therapy at discharge if LDL >100 mg/dL or LDL not measured or on therapy at admission* | 70.3 | 76.3 | 82.1 | 86.2 |
| Counseling for smoking cessation* | 86.1 | 92.2 | 94.3 | 96.2 |
| Lifestyle changes recommended for BMI >25 kg/m2 | 42.5 | 45.7 | 51.7 | 57.3 |
| Composite quality-of-care measure† | 85.9 | 88.9 | 91.7 | 93.3 |
GWTG indicates Get With The Guidelines; IV, intravenous; tPA, tissue-type plasminogen activator; DVT, deep venous thrombosis; LDL, low-density lipoprotein; BMI, body mass index.
Values are percentages. In-hospital mortality for the 2009 patient population was 6.9%, and mean length of hospital stay was 5.3 days (median 3.0 days).
Indicates key performance measures targeted in GWTG-Stroke.
The composite quality-of-care measure indicates performance on the provision of several elements of care. It is computed by summing the numerators for each key achievement measure across the population of interest to create a composite numerator (all the care that was given), summing the denominators for each measure to form a composite denominator (all the care that should have been given), and reporting the ratio (the percentage of all the needed care that was given).
Table 20-10.
Quality of Care by Race/Ethnicity and Sex in the GWTG-HF Program, 2009
| Race/Ethnicity | Sex | ||||
|---|---|---|---|---|---|
| Quality-of-Care Measure | White | Black | Hispanic | Men | Women |
| Complete set of discharge instructions* | 90.8 | 91.7 | 91.4 | 91.3 | 90.2 |
| Measure of LV function* | 98.3 | 98.9 | 97.3 | 98.4 | 98.0 |
| ACEI or ARB at discharge for patients with LVSD, no contraindications* | 92.0 | 94.2 | 94.0 | 92.8 | 93.0 |
| Smoking cessation counseling, current smokers* | 96.6 | 99.1 | 96.7 | 97.8 | 97.1 |
| β-Blockers at discharge for patients with LVSD, no contraindications* | 92.8 | 92.0 | 91.2 | 93.2 | 92.0 |
| Hydralazine/nitrates at discharge for patients with LVSD, no contraindications | NM | 12.2 | NM | 13.1† | 10.1† |
| Anticoagulation for atrial fibrillation or atrial flutter, no contraindications | 69.2 | 67.2 | 72.3 | 71.6 | 66.1 |
| Composite quality-of-care measure‡ | 94.4 | 95.1 | 94.0 | 94.7 | 94.2 |
GWTG-HF indicates Get With The Guidelines–Heart Failure; LV, left ventricular; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; LVSD, left ventricular systolic dysfunction; NM, not measured.
Values are percentages.
Indicates the 5 key achievement measures targeted in GWTG-HF.
For black patients only.
The composite quality-of-care measure indicates performance on the provision of several elements of care. It is computed by summing the numerators for each key achievement measure across the population of interest to create a composite numerator (all the care that was given), summing the denominators for each measure to form a composite denominator (all the care that should have been given), and reporting the ratio (the percentage of all the needed care that was given).
Table 23-2.
Females and CVD: At-a-Glance Table
| Diseases and Risk Factors | Both Sexes | Total Females | White Females | Black Females | Mexican American Females |
|---|---|---|---|---|---|
| Total CVD | |||||
| Prevalence, 2008* | 82.6 M (36.2%) | 42.7 M (35.0%) | 33.8% | 47.3% | 30.9% |
| Mortality, 2007† | 813.8 K | 421.9 K | 362.8 K | 50.0 K | NA |
| CHD | |||||
| Prevalence, CHD, 2008* | 16.3 M (7.0%) | 7.5 M (6.1%) | 5.8% | 7.6% | 5.6% |
| Prevalence, MI, 2008* | 7.9 M (3.1%) | 3.1 M (2.2%) | 2.1% | 2.2% | 1.1% |
| Prevalence, AP, 2008* | 9.0 M (3.9%) | 5.0 M (4.0%) | 3.7% | 5.6% | 3.7% |
| New and recurrent CHDठ| 1.26 M | 515.0 K | 445.0 K | 65.0 K | NA |
| New and recurrent MI§ | 935.0 K | 370.0 K | NA | NA | NA |
| Incidence of AP (stable angina)‖ | 500.0 K | 180.0 K | NA | NA | NA |
| Mortality, 2007 CHD† | 406.4 K | 190.3 K | 165.4 K | 20.9 K | NA |
| Mortality, 2007 MI† | 133.0 K | 61.3 K | 52.9 K | 7.1 K | NA |
| Stroke | |||||
| Prevalence, 2008* | 7.0 M (3.0%) | 4.2 M (3.3%) | 3.3% | 4.4% | 2.7% |
| New and recurrent strokes† | 795.0 K | 425.0 K | 365.0 K | 60.0 K | NA |
| Mortality, 2007† | 136.0 K | 81.8 K | 70.0 K | 9.5 K | NA |
| HBP | |||||
| Prevalence, 2008* | 76.4 M (33.5%) | 39.9 M (32.7%) | 31.3% | 45.7% | 28.9% |
| Mortality, 2007† | 57.7 K | 32.7 K | 25.4 K | 6.5 K | NA |
| HF | |||||
| Prevalence, 2008* | 5.7 M (2.4%) | 2.6 M (2.0%) | 1.8% | 3.8% | 1.3% |
| Mortality, 2007† | 56.6 K | 33.7 K | 30.1 K | 3.2 K | NA |
| Smoking | |||||
| Prevalence, 2009¶ | 46.6 M (20.6%) | 21.0 M (18.3%) | 20.7% | 18.8% | NA |
| Blood cholesterol | |||||
| Prevalence, 2008 | |||||
| Total cholesterol ≥200 mg/dL* | 98.8 M (44.4%) | 53.8 M (46.3%) | 47.0% | 41.2% | 46.5% |
| Total cholesterol ≥240 mg/dL* | 33.6 M (15.0%) | 19.0 M (16.2%) | 16.9% | 13.3% | 14.0% |
| LDL-C ≥130 mg/dL* | 71.3 M (31.9%) | 36.0 M (31.0%) | 32.0% | 27.7% | 31.6% |
| HDL-C <40 mg/dL* | 41.8 M (18.9%) | 11.0 M (9.7%) | 10.1% | 6.6% | 12.2% |
| PA# | |||||
| Prevalence, 2009¶ | 34.9% | 32.7% | 36.2% | 24.1% | NA |
| Overweight and obesity | |||||
| Prevalence, 2008 | |||||
| Overweight and obesity, BMI ≥25.0 kg/m2* | 149.3 M (67.3%) | 71.3 M (62.3%) | 59.3% | 77.7% | 75.1% |
| Obesity, BMI ≥30.0 kg/m2* | 75.06 M (33.7%) | 40.1 M (35.2%) | 35.2% | 51.0% | 43.4% |
| DM | |||||
| Prevalence, 2008 | |||||
| Physician-diagnosed DM* | 18.3 M (8.2%) | 10.0 M (8.7%) | 6.5% | 14.7% | 12.7% |
| Undiagnosed DM* | 6.7 M (3.2%) | 2.7 M (2.3%) | 1.9% | 4.0% | 3.8% |
| Prediabetes* | 81.5 M (36.8%) | 25.7 M (22.2%) | 27.9% | 27.1% | 34.3% |
| Incidence, diagnosed DM* | 1.6 M | NA | NA | NA | NA |
| Mortality, 2007† | 71.4 K | 35.9 K | 27.6 K | 7.0 K | NA |
Abbreviations as in Table 23-1.
Age ≥20 years.
All ages.
New and recurrent MI and fatal CHD.
Age ≥35 years.
Age ≥45 years.
Age ≥18 years.
Regular leisure-time physical activity.
Sources: See summary tables for each chapter in this Update.
Table 23-3.
Ethnic Groups and CVD: At-a-Glance Table
| Diseases and Risk Factors | Both Sexes | Whites | Blacks | Mexican Americans |
Hispanics/ Latinos |
Asians, Both Sexes |
American Indians/ Alaska Natives, Both Sexes |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | Males | Females | ||||
| Total CVD | |||||||||||
| Prevalence, 2008* | 82.6 M (36.2%) | 37.4% | 33.8% | 44.8% | 47.3% | 30.7% | 30.9% | NA | NA | NA | NA |
| Mortality, 2007† | 813.8 K | 334.6 K | 362.8 K | 47.4 K | 50.0 K | NA | NA | NA | NA | NA | NA |
| CHD | |||||||||||
| Prevalence, CHD, 2008* | 16.3 M (7.0%) | 8.5% | 5.8% | 7.9% | 7.6% | 6.3% | 5.6% | NA | NA | NA | NA |
| Prevalence, MI, 2008* | 7.9 M (3.1%) | 4.3% | 2.1% | 4.3% | 2.2% | 3.0% | 1.1% | NA | NA | NA | NA |
| Prevalence, AP, 2008* | 9.0 M (3.9%) | 3.8% | 3.7% | 3.3% | 5.6% | 3.6% | 3.7% | NA | NA | NA | NA |
| New and recurrent CHDठ| 1.26 M | 675.0 K | 445.0 K | 70.0 K | 65.0 K | NA | NA | NA | NA | NA | NA |
| Mortality, CHD, 2007† | 406.4 K | 189.1 K | 165.4 K | 21.8 K | 20.9 K | NA | NA | NA | NA | NA | NA |
| Mortality, MI, 2007† | 133.0 K | 63.0 K | 52.9 K | 7.0 K | 7.1 K | NA | NA | NA | NA | NA | NA |
| Stroke | |||||||||||
| Prevalence, 2008* | 7.0 M (3.0%) | 2.4% | 3.3% | 4.5% | 4.4% | 2.0% | 2.7% | NA | NA | NA | NA |
| New and recurrent strokes† | 795.0 K | 325.0 K | 365.0 K | 45.0 K | 60.0 K | NA | NA | NA | NA | NA | NA |
| Mortality, 2007† | 136.0 K | 44.7 K | 70.0 K | 7.5 K | 9.5 K | NA | NA | NA | NA | NA | NA |
| HBP | |||||||||||
| Prevalence, 2008* | 76.4 M (33.5%) | 33.9% | 31.3% | 43.0% | 45.7% | 27.8% | 28.9% | NA | NA | NA | NA |
| Mortality, 2007† | 57.7 K | 18.2 K | 25.4 K | 6.1 K | 6.5 K | NA | NA | NA | NA | NA | NA |
| HF | |||||||||||
| Prevalence, 2008* | 5.7 M (2.4%) | 2.7% | 1.8% | 4.5% | 3.8% | 2.3% | 1.3% | NA | NA | NA | NA |
| Mortality, 2007† | 56.6 K | 20.3 K | 30.1 K | 2.3 K | 3.2 K | NA | NA | NA | NA | NA | NA |
| Smoking | |||||||||||
| Prevalence, 2009‖ | 46.6 M (20.6%) | 25.0% | 20.7% | 22.9% | 18.8% | 13.2% | 17.6% | 9.4% | 11.6% | 19.0% | |
| Blood cholesterol | |||||||||||
| Prevalence, 2008 | |||||||||||
| Total cholesterol ≥200 mg/dL* | 98.8 M (44.4%) | 41.2% | 47.0% | 37.0% | 41.2% | 50.1% | 46.5% | NA | NA | NA | NA |
| Total cholesterol ≥240 mg/dL* | 33.6 M (15.0%) | 13.7% | 16.9% | 9.7% | 13.3% | 16.9% | 14.0% | NA | NA | NA | NA |
| LDL-C ≥130 mg/dL* | 71.3 M (31.9%) | 30.5% | 32.0% | 34.4% | 27.7% | 41.9% | 31.6% | NA | NA | NA | NA |
| HDL-C <40 mg/dL* | 41.8 M (18.9%) | 29.5% | 10.1% | 16.6% | 6.6% | 31.7% | 12.2% | NA | NA | NA | NA |
| PA¶ | |||||||||||
| Prevalence, 2009‖ | 34.9% | 37.4% | 29.3% | NA | NA | 27.8% | 28.3% | 34.0% | |||
| Overweight and obesity | |||||||||||
| Prevalence, 2008 | |||||||||||
| Overweight and obesity, BMI ≥25.0 kg/m2* | 149.3 M (67.3%) | 72.3% | 59.3% | 70.8% | 77.7% | 77.5% | 75.1% | NA | NA | NA | NA |
| Obesity, BMI ≥30.0 kg/m2* | 75.0 M (33.7%) | 32.1% | 32.8% | 37.0% | 51.0% | 31.4% | 43.4% | NA | NA | NA | NA |
| DM | |||||||||||
| Prevalence, 2008 | |||||||||||
| Physician-diagnosed DM* | 18.3 M (8.0%) | 6.8% | 6.5% | 14.3% | 14.7% | 11.0% | 12.7% | NA | NA | NA | NA |
| Undiagnosed DM* | 7.1 M (3.1%) | 3.9% | 1.9% | 4.8% | 4.0% | 6.3% | 3.8% | NA | NA | NA | NA |
| Prediabetes* | 81.5 M (36.8%) | 45.4% | 27.9% | 31.6% | 27.1% | 44.9% | 34.3% | NA | NA | NA | NA |
| Incidence, diagnosed DM* | 1.6 M | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Mortality, 2007† | 71.4 K | 28.7 K | 27.6 K | 5.5 K | 7.0 K | NA | NA | NA | NA | NA | NA |
Abbreviations as in Table 23-1.
Age ≥20 years.
All ages.
New and recurrent MI and fatal CHD.
Age ≥35 years.
Age ≥18 years.
Regular leisure-time physical activity.
Sources: See summary tables for each chapter in this Update.
Acknowledgments
We wish to thank Thomas Thom, Jonathan Pool, Michael Wolz, and Sean Coady for their valuable comments and contributions. We would like to acknowledge Karen Modesitt for her administrative assistance.
Glossary
- Age-adjusted rates
Used mainly to compare the rates of ≥2 communities or population groups or the nation as a whole over time. The American Heart Association (AHA) uses a standard population (2008), so these rates are not affected by changes or differences in the age composition of the population. Unless otherwise noted, all death rates in this publication are age adjusted per 100 000 population and are based on underlying cause of death.
- Agency for Healthcare Research and Quality (AHRQ)
A part of the US Department of Health and Human Services, this is the lead agency charged with supporting research designed to improve the quality of healthcare, reduce the cost of healthcare, improve patient safety, decrease the number of medical errors, and broaden access to essential services. AHRQ sponsors and conducts research that provides evidence-based information on healthcare outcomes, quality, cost, use, and access. The information helps healthcare decision makers (patients, clinicians, health system leaders, and policy makers) make more informed decisions and improve the quality of healthcare services.
- Bacterial endocarditis
An infection of the heart’s inner lining (endocardium) or of the heart valves. The bacteria that most often cause endocarditis are streptococci, staphylococci, and enterococci.
- Body mass index (BMI)
A mathematical formula to assess body weight relative to height. The measure correlates highly with body fat. It is calculated as weight in kilograms divided by the square of the height in meters (kg/m2).
- Centers for Disease Control and Prevention/National Center for Health Statistics (CDC/NCHS)
- An agency within the US Department of Health and Human Services. The CDC conducts the Behavioral Risk Factor Surveillance System (BRFSS), an ongoing study. The NCHS also conducts or has conducted these studies (among others):
-
—National Health Examination Survey (NHES I, 1960 to 1962; NHES II, 1963 to 1965; NHES III, 1966 to 1970)
-
—National Health and Nutrition Examination Survey I (NHANES I, 1971 to 1974)
-
—National Health and Nutrition Examination Survey II (NHANES II, 1976 to 1980)
-
—National Health and Nutrition Examination Survey III (NHANES III, 1988 to 1994)
-
—National Health and Nutrition Examination Survey (NHANES, 1999 to …) (ongoing)
-
—National Health Interview Survey (NHIS) (ongoing)
-
—National Home and Hospice Care Survey (periodic)
-
—National Hospital Discharge Survey (NHDS) (ongoing)
-
—National Nursing Home Survey (periodic)
-
—
- Centers for Medicare & Medicaid Services (CMS), formerly Health Care Financing Administration (HCFA)
The federal agency that administers the Medicare, Medicaid, and Child Health Insurance programs.
- Comparability ratio
Provided by the NCHS to allow time-trend analysis from one International Classification of Diseases (ICD) revision to another. It compensates for the “shifting” of deaths from one causal code number to another. Its application to mortality based on one ICD revision means that mortality is “comparability modified” to be more comparable to mortality coded to the other ICD revision.
- Coronary heart disease (CHD) (ICD-10 codes I20–I25)
This category includes acute myocardial infarction (I21–I22), other acute ischemic (coronary) heart disease (I24), angina pectoris (I20), atherosclerotic cardiovascular disease (I25.0), and all other forms of chronic ischemic CHD (I25.1–I25.9).
- Death rate
The relative frequency with which death occurs within some specified interval of time in a population. National death rates are computed per 100 000 population. Dividing the total number of deaths by the total population gives a crude death rate for the total population. Rates calculated within specific subgroups, such as age-specific or sex-specific rates, are often more meaningful and informative. They allow well-defined subgroups of the total population to be examined. Unless otherwise stated, all death rates in this publication are age adjusted and are per 100 000 population.
- Diseases of the circulatory system (ICD codes I00–I99)
Included as part of what the AHA calls “cardiovascular disease.” (See “Total cardiovascular disease” in this Glossary.)
- Diseases of the heart
Classification the NCHS uses in compiling the leading causes of death. Includes acute rheumatic fever/chronic rheumatic heart diseases (I00–I09), hypertensive heart disease (I11), hypertensive heart and renal disease (I13), coronary heart disease (I20 –I25), pulmonary heart disease and diseases of pulmonary circulation (I26 –I28), heart failure (I50), and other forms of heart disease (I29 –I49, I50.1–I51). “Diseases of the heart” are not equivalent to “total cardiovascular disease,” which the AHA prefers to use to describe the leading causes of death.
- Health Care Financing Administration (HCFA)
See Centers for Medicare & Medicaid Services (CMS).
- Hispanic origin
In US government statistics, “Hispanic” includes people who trace their ancestry to Mexico, Puerto Rico, Cuba, Spain, the Spanish-speaking countries of Central or South America, the Dominican Republic, or other Spanish cultures, regardless of race. It does not include people from Brazil, Guyana, Suriname, Trinidad, Belize, or Portugal, because Spanish is not the first language in those countries. Most of the data in this update are for Mexican Americans or Mexicans, as reported by government agencies or specific studies. In many cases, data for all Hispanics are more difficult to obtain.
- Hospital discharges
The number of inpatients discharged from short-stay hospitals for whom some type of disease was the first-listed diagnosis. Discharges include those discharged alive, dead, or “status unknown.”
- International Classification of Diseases (ICD) codes
A classification system in standard use in the United States. The International Classification of Diseases is published by the World Health Organization. This system is reviewed and revised approximately every 10 to 20 years to ensure its continued flexibility and feasibility. The 10th revision (ICD-10) began with the release of 1999 final mortality data. The ICD revisions can cause considerable change in the number of deaths reported for a given disease. The NCHS provides “comparability ratios” to compensate for the “shifting” of deaths from one ICD code to another. To compare the number or rate of deaths with that of an earlier year, the “comparability-modified” number or rate is used.
- Incidence
An estimate of the number of new cases of a disease that develop in a population, usually in a 1-year period. For some statistics, new and recurrent attacks, or cases, are combined. The incidence of a specific disease is estimated by multiplying the incidence rates reported in community- or hospital-based studies by the US population. The rates in this report change only when new data are available; they are not computed annually.
- Major cardiovascular diseases
Disease classification commonly reported by the NCHS; represents ICD codes I00 –I78. The AHA does not use “major cardiovascular diseases” for any calculations. See “Total cardiovascular disease” in this Glossary.
- Metabolic syndrome
-
The metabolic syndrome is defined* as the presence of any 3 of the following 5 diagnostic measures: Elevated waist circumference (≥102 cm in men or ≥88 cm in women), elevated triglycerides (≥150 mg/dL [1.7 mmol/L] or drug treatment for elevated triglycerides), reduced high-density lipoprotein (HDL) cholesterol (<40 mg/dL [0.9 mmol/L] in men, <50 mg/dL [1.1 mmol/L] in women, or drug treatment for reduced HDL cholesterol), elevated blood pressure (≥130 mm Hg systolic blood pressure, ≥85 mm Hg diastolic blood pressure, or drug treatment for hypertension), and elevated fasting glucose (≥100 mg/dL or drug treatment for elevated glucose).
*According to criteria established by the American Heart Association/National Heart, Lung, and Blood Institute and published in Circulation (Circulation. 2005;112:2735–2752).
- Morbidity
Incidence and prevalence rates are both measures of morbidity (ie, measures of various effects of disease on a population).
- Mortality
Mortality data for states can be obtained from the NCHS Web site (http://cdc.gov/nchs/), by direct communication with the CDC/NCHS, or from the AHA on request. The total number of deaths due to a given disease in a population during a specific interval of time, usually a year, are reported. These data are compiled from death certificates and sent by state health agencies to the NCHS. The process of verifying and tabulating the data takes ≈2 years.
- National Heart, Lung, and Blood Institute (NHLBI)
- An institute in the National Institutes of Health in the US Department of Health and Human Services. The NHLBI conducts such studies as the following:
-
—Framingham Heart Study (FHS) (1948 to …) (ongoing)
-
—Honolulu Heart Program (HHP) (1965 to 1997)
-
—Cardiovascular Health Study (CHS) (1988 to …) (ongoing)
-
—Atherosclerosis Risk in Communities (ARIC) study (1985 to …) (ongoing)
-
—Strong Heart Study (SHS) (1989 to 1992; 1991 to 1998)
-
—The NHLBI also published reports of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure and the Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III, or ATP III).
-
—
- National Institute of Neurological Disorders and Stroke (NINDS)
- An institute in the National Institutes of Health of the US Department of Health and Human Services. The NINDS sponsors and conducts research studies such as these:
-
—Greater Cincinnati/Northern Kentucky Stroke Study (GCNKSS)
-
—Rochester (Minnesota) Stroke Epidemiology Project
-
—Northern Manhattan Study (NOMAS)
-
—Brain Attack Surveillance in Corpus Christi (BASIC) Project
-
—
- Prevalence
An estimate of the total number of cases of a disease existing in a population during a specified period. Prevalence is sometimes expressed as a percentage of population. Rates for specific diseases are calculated from periodic health examination surveys that government agencies conduct. Annual changes in prevalence as reported in this statistical update reflect changes in the population size. Changes in rates can be evaluated only by comparing prevalence rates estimated from surveys conducted in different years.
Note
In the data tables, which are located in the different disease and risk factor categories, if the percentages shown are age adjusted, they will not add to the total.
- Race and Hispanic origin
Race and Hispanic origin are reported separately on death certificates. In this publication, unless otherwise specified, deaths of people of Hispanic origin are included in the totals for whites, blacks, American Indians or Alaska Natives, and Asian or Pacific Islanders according to the race listed on the decedent’s death certificate. Data for Hispanic people include all people of Hispanic origin of any race. See “Hispanic origin” in this Glossary.
- Stroke (ICD-10 codes I60–I69)
This category includes subarachnoid hemorrhage (I60); intracerebral hemorrhage (I61); other nontraumatic intracranial hemorrhage (I62); cerebral infarction (I63); stroke, not specified as hemorrhage or infarction (I64); occlusion and stenosis of precerebral arteries not resulting in cerebral infarction (I65); occlusion and stenosis of cerebral arteries not resulting in cerebral infarction (I66); other cerebrovascular diseases (I67); cerebrovascular disorders in diseases classified elsewhere (I68); and sequelae of cerebrovascular disease (I69).
- Total cardiovascular disease (ICD-10 codes I00–I99, Q20– Q28)
This category includes rheumatic fever/rheumatic heart disease (I00 –I09); hypertensive diseases (I10 –I15); ischemic (coronary) heart disease (I20 –I25); pulmonary heart disease and diseases of pulmonary circulation (I26 –I28); other forms of heart disease (I30 –I52); cerebrovascular disease (stroke) (I60 –I69); atherosclerosis (I70); other diseases of arteries, arterioles, and capillaries (I71–I79); diseases of veins, lymphatics, and lymph nodes not classified elsewhere (I80 –I89); and other and unspecified disorders of the circulatory system (I95–I99). When data are available, we include congenital cardiovascular defects (Q20–Q28).
- Underlying cause of death or any-mention cause of death
These terms are used by the NCHS when defining mortality. Underlying cause of death is defined by the World Health Organization as “the disease or injury which initiated the train of events leading directly to death, or the circumstances of the accident or violence which produced the fatal injury.” Contributing cause of death would be any other disease or condition that the decedent may also have had.
Footnotes
The American Heart Association makes every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
A copy of the statement is available at http://www.americanheart.org/presenter.jhtml?identifier_3003999 by selecting either the “topic list” link or the “chronological list” link (No. KB-0111). To purchase additional reprints, call 843-216-2533 or e-mail kelle.ramsay@wolterskluwer.com.
Expert peer review of AHA Scientific Statements is conducted at the AHA National Center. For more on AHA statements and guidelines development, visit http://www.americanheart.org/presenter.jhtml?identifier_3023366.
Disclosures
| Writing Group Member | Employment | Research Grant | Other Research Support |
Speakers’ Bureau/Honoraria |
Expert Witness | Ownership Interest |
Consultant/Advisory Board |
Other |
|---|---|---|---|---|---|---|---|---|
| Véronique L. Roger | Mayo Clinic | None | None | None | None | None | None | None |
| Robert J. Adams | Medical University of South Carolina | NHLBI† | None | Boehringer Ingelheim†; Genentech* | None | None | Boehringer Ingelheim†; Novartis* | None |
| Jarett D. Berry | UT Southwestern Medical School | AHA†; NHLBI† | None | Merck† | None | None | None | None |
| Todd M. Brown | University of Alabama at Birmingham | NIH† | None | None | None | None | None | None |
| Mercedes R. Carnethon | Northwestern University | None | None | None | None | None | None | None |
| Shifan Dai | Centers for Disease Control and Prevention | None | None | None | None | None | None | None |
| Giovanni de Simone | Federico II University of Naples | None | None | None | None | None | None | None |
| Earl S. Ford | Centers for Disease Control and Prevention | None | None | None | None | None | None | None |
| Caroline S. Fox | NHLBI | None | None | None | None | None | None | None |
| Heather J. Fullerton | University of California, San Francisco | None | None | None | None | None | None | None |
| Cathleen Gillespie | Centers for Disease Control and Prevention | None | None | None | None | None | None | None |
| Alan S. Go | The Permanente Medical Group | Johnson & Johnson†; GlaxoSmithKline† | None | None | None | None | None | None |
| Kurt J. Greenlund | Centers for Disease Control and Prevention | None | None | None | None | None | None | None |
| Susan M. Hailpern | Northern Westchester Hospital | None | None | None | None | None | None | None |
| John A. Heit | Mayo Clinic | None | None | None | None | None | None | None |
| P. Michael Ho | Denver VA Medical Center | None | None | None | None | None | Wellpoint Inc.* | None |
| Virginia J. Howard | University of Alabama at Birmingham | NIH/NINDS† | None | None | None | None | None | None |
| Brett M. Kissela | University of Cincinnati | NIH/NCRR†; NIH/NINDS† | None | None | Expert witness for defense in 1 stroke-related case in 2010† | None | Allergan† | None |
| Steven J. Kittner | University of Maryland School of Medicine | None | None | None | None | None | None | None |
| Daniel T. Lackland | Medical University of South Carolina | None | None | None | None | None | None | None |
| Judith H. Lichtman | Yale School of Medicine | None | None | None | None | None | None | None |
| Lynda D. Lisabeth | University of Michigan | None | None | None | None | None | None | None |
| Donald M. Lloyd-Jones | Northwestern | None | None | None | None | None | None | None |
| Diane M. Makuc | National Center for Health Statistics, CDC | None | None | None | None | None | None | None |
| Gregory M. Marcus | UCSF | None | None | None | None | None | None | None |
| Ariane Marelli | McGill University Health Center | None | None | None | None | None | None | None |
| David B. Matchar | Duke-NUS Graduate Medical School | None | None | None | None | None | Boehringer Ingelheim* | None |
| Mary M. McDermott | Northwestern University’s Feinberg School of Medicine | None | None | None | None | None | None | Contributing Editor for JAMA |
| James B. Meigs | Massachusetts General Hospital | None | None | None | None | None | None | None |
| Claudia S. Moy | National Institutes of Health | None | None | None | None | None | None | None |
| Dariush Mozaffarian | Harvard School of Public Health | NIH†; Harvard†; Gates Foundation/World Health Organization†; Searle Funds at the Chicago Community Trust† | None | Aramark*; International Life Sciences Institute*; SPRIM*; Unilvever*; US Food and Drug Administration*; World Health Organization* | None | Royalties from UpToDate for an online chapter* | Nutrition Impact*` | None |
| Michael E. Mussolino | National Heart, Lung, and Blood Institute | None | None | None | None | None | None | None |
| Graham Nichol | University of Washington | Asmund S Laerdal Foundation for Acute Medicine†; Medtronic Inc. †; NHLBI†; NIH† | None | None | None | None | Gambro Renal Inc*; Lifebridge Medizintechnik AG*; Sotera Wireless* | None |
| Nina P. Paynter | Brigham and Women’s Hospital | F. Hoffman LaRoche Ltd. † | None | None | None | None | None | None |
| Wayne D. Rosamond | University of North Carolina | None | None | None | None | None | None | None |
| Paul D. Sorlie | National Heat, Lung and Blood Institute, NIH | None | None | None | None | None | None | None |
| Randall S. Stafford | Stanford University | None | None | None | None | None | None | None |
| Tanya N. Turan | Medical University of South Carolina | Applied Clinical Intelligence*; NIH/NINDS† | None | None | None | None | None | AAN Clinical Research Fellowship† |
| Melanie B. Turner | American Heart Association | None | None | None | None | None | None | None |
| Nathan D. Wong | University of California, Irvine | Bristol-Myers Squibb†; Forest†; Novartis Pharmaceuticals† | None | None | None | None | None | None |
| Judith Wylie-Rosett | Albert Einstein College of Medicine | Kraft via subcontract from Provident* | None | None | None | None | None | None |