Supplemental Digital Content is available in the text
Key Words: Belgium, health equity, immigration, leadership, social network, transcultural nursing
Abstract
Background
International migration is a global phenomenon challenging healthcare professionals to provide culturally competent care.
Objectives
The purpose of this study was to investigate the influence of leaders on the cultural competence of healthcare professionals.
Methods
A cross-sectional survey was conducted from 2010 to 2012 to obtain data for a social network analysis in 19 inpatient services and five primary care services in Belgium. The Competences in Ethnicity and Health questionnaire was used. A total of 507 healthcare professionals, including 302 nurses, identified their social relationships with other healthcare professionals working in their service. Highest in-degree centrality was used to identify the leaders within each health service. Multiple regressions with the Huber sandwich estimator were used to link cultural competence of leaders with the cultural competence of the rest of the healthcare staff.
Results
Cultural competence of the healthcare staff was associated with the cultural competence of the leaders. This association remained significant for two specific domains of cultural competence—mediation and paradigm—after controlling for contextual and sociodemographic variables. Interaction analysis suggested that the leadership effect varied with the degree of cultural competence of the leaders.
Discussion
Cultural competence among healthcare professionals is acquired partly through leadership. Social relationships and leadership effects within health services should be considered when developing and implementing culturally competent strategies. This requires a cautious approach as the most central individuals are not always the same persons as the formal leaders.
International migration is a global and complex phenomenon. Many European countries, including Belgium, are experiencing increasing population diversity arising from international immigration. Labor migrants, past colonial links, and, for some countries, their strategic position in the European Union are factors contributing to this diversity. Although labor immigration has decreased somewhat in recent years, migration flows still persist and asylum applications are still increasing in Europe (Laczko & Appave, 2013). In Belgium, around 12% of the population does not have Belgian nationality, but this proportion increases to 60% for those with a migrant background—especially in urban areas (Service Public Fédéral Economie, P.M.E., 2010). There is currently no clear definition of “ethnic minority” in the Belgian context, and overlaps exist between ethnic minorities and migrants (Jabobs & Rea, 2005), leading to an ethnically diverse population experiencing various life experiences.
Although the organization of health services and health systems varies from one country to another, migrants and ethnic minorities are more at risk of experiencing poor health outcomes when compared to the rest of the population. In Belgium, poor health outcomes have been reported for acute health problems, such as higher prevalence of tuberculosis or sexually transmitted infections (Sasse, Deblonde, & Van Beckhoven, 2013; van Heurck, Payen, De Wit, & Clumeck, 2013). Prevalence of Type 2 diabetes is higher in Moroccan women living in Belgium than native Belgian women (Vandenheede & Deboosere, 2009). Higher prevalence of mental health troubles, such as psychosis and anxiety syndromes, and a poorest perception of subjective health were found among Turks and Moroccans living in Belgium when compared to Belgians (Fossion et al., 2002; Levecque, Lodewyckx, & Vranken, 2007; Lorant, Van Oyen, & Thomas, 2008). Moreover, migrants and ethnic minorities have lower levels of access to health promotion facilities and health prevention (Ochieng, 2013; Wilson et al., 2012). Similar poor health outcomes and restricted access to healthcare services have been found in Europe (Nielsen & Krasnik, 2010; Sandhu et al., 2013; Stansbury, Jia, Williams, Vogel, & Duncan, 2005; Ujcic-Voortman, Baan, Seidell, & Verhoeff, 2012).
Consequently, in most European metropolitan areas, health services are required to provide culturally competent healthcare to ethnic minority patients in order to reduce health inequalities for these patients (Brach & Fraserirector, 2000; Ingleby, 2011). Betancourt, Green, Carrillo, and Ananeh-Firempong (2003) defined “culturally competent healthcare system as one that acknowledges and incorporates—at all levels—the importance of culture, assessment of cross-cultural relations, vigilance toward the dynamics that result from cultural differences, expansion of cultural knowledge, and adaptation of services to meet culturally unique needs. A culturally competent system is also built on an awareness of the integration and interaction of health beliefs and behaviors, disease prevalence and incidence, and treatment outcomes for different patient populations” (p. 294). Consequently, cultural competence encompasses a broad range of strategies ranging from the individual level to the political level (Anderson, Scrimshaw, Fullilove, Fielding, & Normand, 2003; Betancourt et al., 2003; Brach & Fraserirector, 2000) and is included in numerous training programs for health professionals (Beach et al., 2005; Campinha-Bacote, 2002; Seeleman, Suurmond, & Stronks, 2009; Wells, 2000). Among other examples, culturally competent interventions may include the development of culturally specific health services or ethnically sensitive health promotion campaigns, the deployment of interpreters and intercultural mediators in health facilities, as well as migrant-friendly health policies (Beach et al., 2006; Betancourt et al., 2003; Brach & Fraserirector, 2000). The Belgian healthcare system is also concerned about the adequate development of cultural competence, but specific actions and interventions remain limited (Dauvrin, Derluyn, Coune, Verrept, & Lorant, 2012).
Training models for cultural competence focus on developing the nontechnical skills of health professionals, such as empathy, openness, or kindness toward ethnic minorities (Seeleman et al., 2009). Besides, health professionals have to develop specific knowledge, attitudes, and skills in order to care for migrants and ethnic minorities, where “attitudes” refer to cognitive and evaluation components (Seeleman et al., 2009). In most training programs in cultural competence, the focus is on the individual healthcare professional rather than on groups. Training programs may, for example, target specific health professions, such as nurses (Jirwe, Gerrish, Keeney, & Emami, 2009; Purnell, 2002) or physicians (Mostow et al., 2010; Perloff, Bonder, Ray, Ray, & Siminoff, 2006). Some also concentrate on specific health services or specialties, such as psychiatry (Qureshi, Collazos, Ramos, & Casas, 2008) or health promotion (Kreuter, Lukwago, Bucholtz, Clark, & Sanders-Thompson, 2003).
However, despite promising results in terms of patient satisfaction, training in cultural competence has shown inconsistent effects on quality of care and on the health outcomes of the patients (Renzaho, Romios, Crock, & Sønderlund, 2013). More precisely, although these interventions are likely to increase short-term patient outcomes of satisfaction, their effects are not sustained on the long term. There may be insufficient evidence of a beneficial effect of cultural competence training on patient adherence and health outcomes as these programs mainly focus on one-time training and do not pay enough more attention to interdisciplinary interactions (Beach et al., 2005). Cultural competence should be considered as a longitudinal competency supported by lifelong learning (Betancourt & Green, 2010). Indeed, the effects of training on the practices of healthcare professionals tend to decrease over time, especially when these trainings do not rely on cases or clinical applications (Betancourt & Green, 2010) and when the work environment does not value or support the skills acquired through training (Barnes, Bullock, Bailey, Cowpe, & Karaharju-Suvanto, 2013). The importance of the support by organizations, leaders, or “champions” has been widely acknowledged (Chrisman, 2007; Yamada & Brekke, 2008), but so far, little evidence supports that leaders (influential health professionals) are more effective in being culturally competent. In fact, it seems that most models of cultural competence training programs neglect the fact that such competence should also be learned socially and shared in the workplace (Betancourt & Green, 2010).
Delivering healthcare is a multidisciplinary and collective activity, especially in hospitals and primary care services. The quality of care, including patient safety, depends on the efforts of the entire team and not just on a few individuals (Taylor et al., 2011). The relevant education paradigms focus on lapses and report behaviors that the healthcare professional should avoid. They fail to identify positive behaviors that may influence role-modeling of the healthcare professionals, particularly for nontechnical skills (Curry, Cortland, & Graham, 2011). Context, leadership, and colleagues are elements contributing to role-modeling and social learning of professional competence (Marsick & Watkins, 2007).
Moreover, being culturally competent is not, on its own, adequate. Each healthcare professional uses their own specific expertise to care for patients, and the combination of their complementary competences has positive effects on patient health outcomes (Cameron et al., 2013). Therefore, being a culturally competent nurse is not likely to make any difference to the quality of the service if the most central (or in other words, “the most popular”) nurse is not culturally competent (Zwarenstein, Goldman, & Reeves, 2009). In a group, a lone culturally competent health professional will suffer from trying to apply cultural competence that is not valued or acknowledged by colleagues (Fuller, Hester, Barnett, & Relyea, 2006). Moreover, poor teamwork and communication failure are commonly reported as the sources of most of the errors that occur in healthcare (Barrow, McKimm, & Gasquoine, 2011).
Being culturally competent can also be the result of existing norms among healthcare professionals (DiMaggio & Garip, 2012; Friedkin, 2001). These norms usually spread among healthcare professionals via the most influential individuals: the leaders (Friedkin, 2001). Normative influence is exerted through social side payments: both positive and negative norms can be spread among healthcare professionals (DiMaggio & Garip, 2012). Positive norms associated with cultural competence include a positive organizational leadership and value placed on diversity (Yamada & Brekke, 2008). In such a context, healthcare professionals with specific expertise in cultural competence will be more likely to integrate this competence into their daily practice. Negative norms, on the other hand, include a negative perception of intercultural care or poor appreciation of cultural competence. The risk of poor appreciation of cultural competence is even greater when the skills are nontechnical skills that are difficult to grasp. Normative influence by the leaders influences both the adoption of cultural competence and the prevention of harmful attitudes (DiMaggio & Garip, 2012).
For these three reasons (social learning, externalities, and norms), it is likely that cultural competence is spread through leadership. In this study, influence of leaders on the cultural competence of the rest of the healthcare staff was investigated through a social network analysis. Leaders were defined as those being the most central individual or the most popular within their network (Creswick, Westbrook, & Braithwaite, 2009; Valente, 2010). Social network analysis was previously used to identify how social relationships may shape the prescribing behaviors of physicians (Fattore, Frosini, Salvatore, & Tozzi, 2009) or the communication patterns in emergency departments (Creswick et al., 2009). The specific aims of this study were to (a) describe the cultural competence of the healthcare staff and leaders and (b) model the association between leader cultural competence and staff cultural competence using the framework depicted in Figure 1.
FIGURE 1.
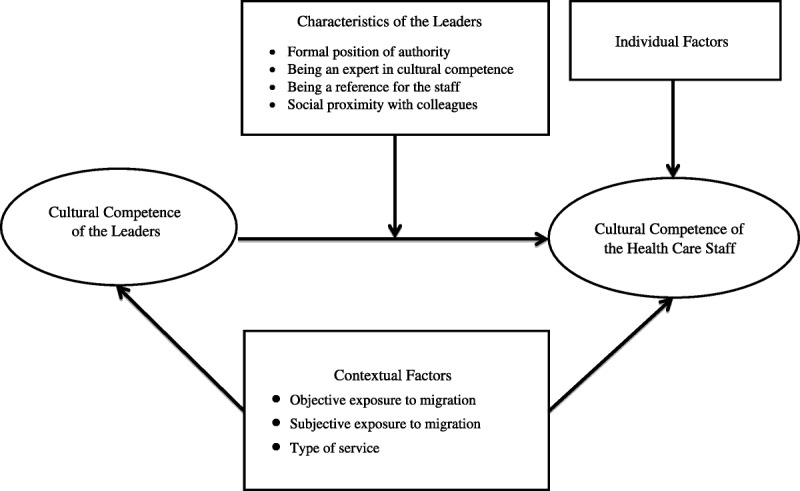
Leadership model of cultural competence.
METHODS
We conducted a quantitative social network analysis as part of a larger research project (Competences in Ethnicity and Health) aimed at evaluating and understanding the cultural competence of healthcare professionals in Belgium. Valente (2010) defined social network analysis as “a theoretical perspective and a set of techniques used to understand these relationships and how they affect behaviors” (Valente, 2010, p. 3). As stated by Anderson, Crabtree, Steele, and McDaniel (2005), “these measures might assist in describing relationship patterns. Relationships represent the ways in which work is carried out and are the conduits for understanding what is to be accomplished. Also, network analysis methods can characterize these patterns for each person in an organization and for the organization as a whole” (p. 678). For example, physicians who are highly connected to their colleagues are less likely to adopt evidence-based medicine, meaning that the cohesion between healthcare professionals was likely to prevent the diffusion of innovations (Mascia et al., 2013). The prescribing behavior of healthcare professionals in primary care services is influenced more by social influence than by social capital mechanisms (Fattore et al., 2009).
Setting
Cluster-based sampling was used to identify the social networks of healthcare professionals. Figure 2 shows the structure of the sample. First, three geographical zones were selected, reflecting numbers of non-national residents, in Brussels and Wallonia (Belgium; Service Public Fédéral Economie, P.M.E., 2010). These geographical zones were sorted into three categories according to the distribution of the foreign population: low exposure to migration, medium exposure to migration, and high exposure to migration. Within each geographical zone, the larger hospitals and the larger primary care services—based on the annual number of patients admitted per year—were identified. To ensure comparability between hospitals and health services, the same five services were selected when they were available: geriatrics, psychiatry, intensive care, oncology, and communicable diseases. Each service constituted a network for the analysis. Sample size was computed for each exposure group (low vs. medium–higher exposure to migration) with an assumed prevalence of cultural competence of 30%, a precision of 6%, and an alpha of 5% (Paez, Allen, Beach, Carson, & Cooper, 2009). Ignoring the number of clusters and the response rate, the total sample size should be constituted of at least 245 individuals. Assuming that each cluster will have an equal number of participants, on average 82 individuals should participate by cluster.
FIGURE 2.
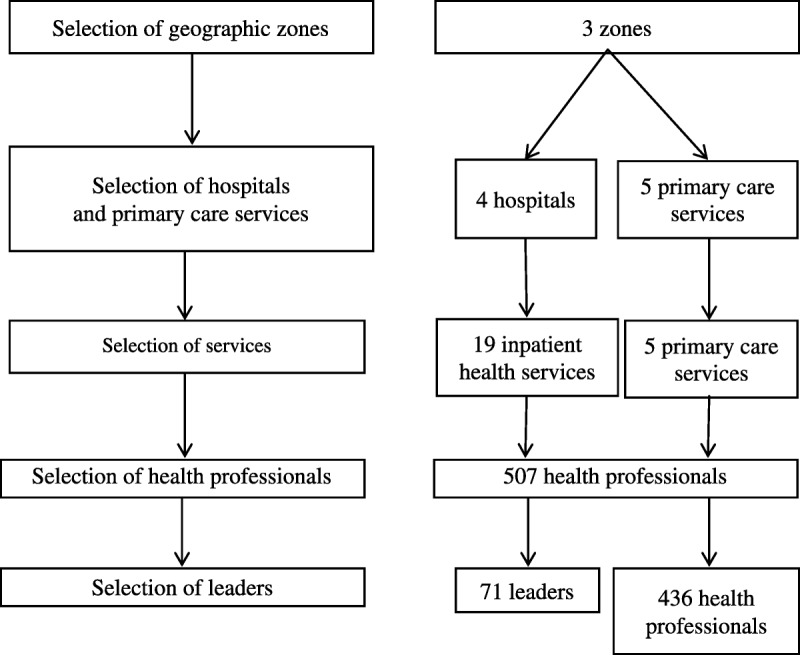
Structure of the sample.
During the recruitment process, two hospitals and one primary care service declined to participate in the project. Two of the participating hospitals did not have communicable diseases units. We therefore replaced these units with internal medicine units. In one hospital, the psychiatric unit declined to participate because of an internal reorganization at the time of the study. The final sample of services comprised 24 health services: five outpatient primary care services and 19 inpatient services recruited in four hospitals. The 19 inpatient health services included four geriatric units, four intensive care units, four oncology units, three psychiatric units, two communicable disease units, one palliative care unit, and one endocrinology unit. In one setting, the oncology unit also included patients with communicable diseases. The cluster “low exposure to migration” included two primary care services, one geriatric unit, one psychiatric unit, one oncology unit, one endocrinology unit, and one intensive care unit. The cluster “medium exposure to migration” included two primary care services, two oncology units (one of these units included patients suffering from communicable diseases), two psychiatric units, two intensive care units, two geriatric units, one communicable disease unit, and one palliative care unit. The cluster “high exposure to migration” included two primary care services, one oncology unit, one intensive care unit, one geriatric unit, and one communicable disease unit.
Data Collection
Initial consent was obtained from the management of each institution. All participants were then contacted by mail and through their head nurse of the doctor-in-chief. Posters reminding of the study were displayed in each health service. Every health professional working in each service was invited to participate in the research. Participants were free to withdraw their consent at any step of the data collection process. Data were collected from June 2010 to June 2012 using a self-administered questionnaire. Participants had 1 month to complete the questionnaire. Reminder e-mails were sent to the head nurse and the doctor-in-chief of each service every week during the 1-month data collection period. This study was approved by the Ethics Committee of the Université catholique de Louvain and the National Privacy Commission of Belgium (Ordinary Declaration No. 1304326281174). Each questionnaire received a unique randomly assigned identification code to protect anonymity of the data.
Measures
Individual Level: Cultural Competence of the Healthcare Staff The dependent variable was cultural competence of the healthcare staff (Figure 1). The Cultural Competence Scale of the Migrant Friendly Hospital project was adapted to the Belgian context and for all healthcare professionals (Krajic, Straßmayar, Karl-Trummer, Novak-Zezula, & Pelikan, 2005). Modifications concerned the terms used to describe specific situations. We tested the modified version of the questionnaire in a purposive sample of health professionals (n = 86) attending master training in public health sciences at the Université catholique de Louvain. The Cronbach’s alpha coefficient of the scale was .87 in pre- and postsurveys of the Migrant Friendly Hospital project (Krajic et al., 2005). The final scale consisted of 15 different items covering various aspects of cultural competence. Responses ranged from 1 (not at all competent) to 5 (entirely competent). We summed the 15 items to obtain a score reflecting total cultural competence. The scale was also divided into five different culturally competent domains: paradigm (aptitude to adapt to a different paradigm of care), communication (ability to provide information to the patients in clear language), specificity (ability to provide specific care for specific groups, such as migrants without a legal permit of residence), organization (ability to adapt the organization of the healthcare to the needs of the patients), and mediation (ability to negotiate with patients in case of trouble).
Group Level: Identification of Leaders The exposure variable was the cultural competence of the leaders, that is, the most central persons in the health service. A social network design with a closed-network approach (also called “complete network data”) was used to identify leaders of each service. All the healthcare professionals identified the social relationships they had with their colleagues in a list containing the names of all the healthcare professionals working in the same service (roster method). We selected three relevant relationships in the professional context: problem-solving (who do I ask for help), advice-seeking (who do I ask for advice on the care of my patients), and socialization (who do I go to for informal moments of socialization, such as coffee breaks). Within each service, we computed indicators of centrality (the most cited person in the network) according to the in-degree in the advice-seeking relationship (Valente, 2010). In-degree centrality is defined as “the number of links (or ties) received by an individual.” The higher the in-degree is, the more central the individual is to the network. On the basis of the in-degree value, we then selected the three most central individuals (leaders) for each health service and computed their average level of cultural competence. We then removed these leaders from the database.
Confounding Variables: Contextual Factors The association between the cultural competence of healthcare staff and the cultural competence of the leaders could be due to confounding contextual factors (Chrisman, 2007; Johnstone & Kanitsaki, 2008). Contextual factors included objective exposure to migrant patients, subjective exposure to migrant patients, and service level factors. Objective exposure was measured by the location of the service in geographical zones with low, medium, or high exposure to migration. Subjective exposure was measured at the individual level by the frequency of exposure to intercultural situations as experienced by the healthcare professionals. We developed a specific scale adapted to the Belgian context. This scale was based on previous surveys in Belgium and Europe (Krajic et al., 2005). Service level factors were the type of service (intensive care, geriatrics, psychiatry, oncology [including palliative care and endocrinology units], communicable diseases, and primary care services) and the institution. Sociodemographic characteristics of the healthcare staff were also obtained.
Explanatory Variables: Cultural Competence and Characteristics of the Leaders For each leader, characteristics that might explain the relationship between the cultural competence of the leaders and the cultural competence of the healthcare staff were considered, including having a formal position of authority within the service (e.g., being the person officially in charge of the health service); having expertise in cultural competence (e.g., training in cultural competence, professional experience abroad as a health professional, and speaking English); being a reference because of their age (at least 40 years old) or professional experience (of at least 12 years); and being socially close to the rest of the healthcare staff (Northouse, 2009). Formal leaders play an important role in promoting learning in interdisciplinary teams within various contexts (Edmondson, 2003). The so-called Pygmalion effect, also known as “leadership of reference,” has a significant influence on the attitudes of healthcare professionals—particularly on the youngest members of health teams (Livingston, 1988). Similarly, leaders adopting a goal-oriented leadership are able to reinforce expected and productive attitudes among workers. Such leadership characteristics have been reported as improving the quality and safety of healthcare for patients (Kaplan et al., 2010) and as having a positive effect on the prevention of nosocomial infections (Ferguson, 2009), the implementation of a hand-washing culture (Roberts, Sieczkowski, Campbell, Balla, & Keenan, 2012), and on professional practices and healthcare outcomes (Flodgren et al., 2011).
On the basis of the network data, social proximity characteristics of closeness and betweenness of leaders and healthcare staff were measured. Closeness is “the average distance of an individual from all other individuals in the network”; high closeness indicates that the individual is socially close to the other individuals in the network (Valente, 2010). Betweenness is “the frequency with which an individual occurs on the shortest path that connects everyone else in the network”; a high level of betweenness indicates that the individual frequently lies between other individuals in the network (Valente, 2010).
Analysis
The analysis had two aims. First, cultural competence of the leaders and the cultural competence of the rest of the healthcare staff were described. Second, the association between leader cultural competence and healthcare staff cultural competence was modeled. A nominal p value of .05 was used. In Model 1 (bivariate regression), we performed a regression on the cultural competence of the healthcare staff against the cultural competence of the leaders. In Model 2 (multivariate regression), individual and contextual factors were controlled: subjective exposure, objective exposure, type of service, profession, gender, age, and professional experience. The control variables were selected in a stepwise regression. The stepwise regression captured the confounding variables likely to be correlated with both the cultural competence of the healthcare staff and that of the leaders. To account for with-service clustering, we used the Huber sandwich estimator (Freedman, 2006). In Model 3 (interaction model), interactions between leader cultural competence and possible intermediary factors, such as formal leader position (yes/no), expertise in cultural competence (low/high), reference position (yes/no), and social proximity, were tested. The interaction variables were also selected using stepwise regression. These three models were tested for the total cultural competence and for each domain of cultural competence.
Data were checked before estimating the regression models (Eekhout, de Boer, Twisk, de Vet, & Heymans, 2012). We compared the sociodemographic and contextual data on the nonrespondents with those of the nonrespondents, but we did not observe significant differences between respondents and nonrespondents. We assessed whether the respondents were “straight liners,” that is, providing the same response whatever the item is (Laveault & Grégoire, 2002). Overall, a minority of the respondents were straight liners. We also assessed the existence of response bias. Indeed, in a questionnaire of social network using a roster method, the first persons on the list may be more cited than the last ones. However, we did not observe such bias in our data.
Statistical analyses were conducted using SAS 9.2 software, and computations of centrality measures were done using UCINET 6.416 software (Borgatti, Everett, & Freeman, 2002).
RESULTS
Participant Description
We contacted 876 members of staff in the 24 participating services and received 576 replies, yielding an overall participation rate of 66%. After data cleaning, 507 questionnaires were eligible for social network analysis. Among these 507 respondents, 71 individuals were identified as the leaders (most central individuals according to the in-degree centrality). These 71 individuals are referred to as “leaders,” and the healthcare professionals who were not leaders are called “healthcare staff.” Overall, we found a low percentage of nonresponses (less than 10%). The percentage of straight lining was also low (less than 1%).
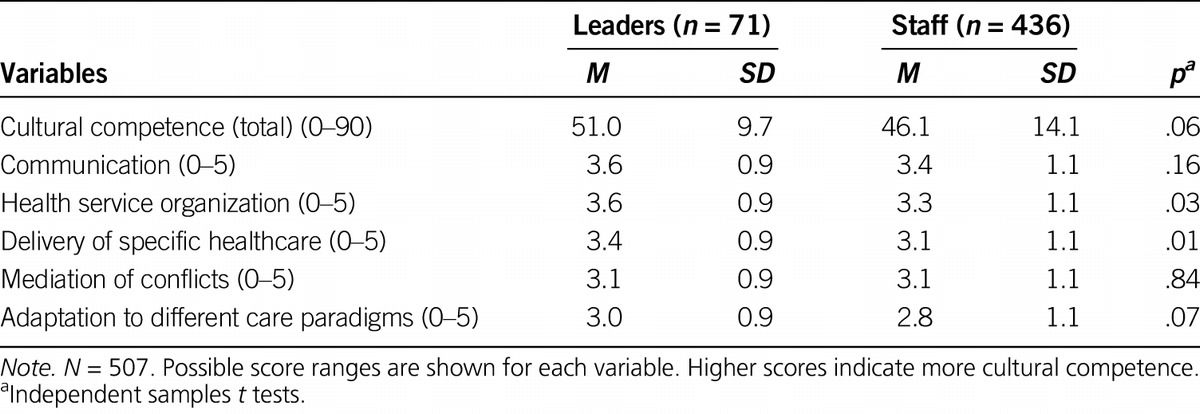
Table 1 presents descriptive characteristics of the leaders and healthcare staff. Respondents were mostly nurses and care assistants (59.6%). The mean professional experience as a health professional was 12 years (SD = 8.94). Twenty-five percent of health professionals reported previous training in cultural competence. Among the 71 leaders identified through social network analysis, 15 individuals were formal leaders such as head nurses. The mean cultural competence of the leaders and the mean cultural competence of the healthcare staff appear in Table 2. Overall, leaders showed a higher level of cultural competence than the healthcare staff. Leaders had a mean score of 3.6 (SD = 0.9) for communication competence, whereas healthcare staff had a mean score of 3.4 (SD = 1.1). However, leaders and healthcare staff showed fairly similar scores for adaptation to different healthcare paradigms (3.0, SD = 0.9 vs. 2.8, SD = 1.1, respectively).
Table 1.
Participant Characteristics
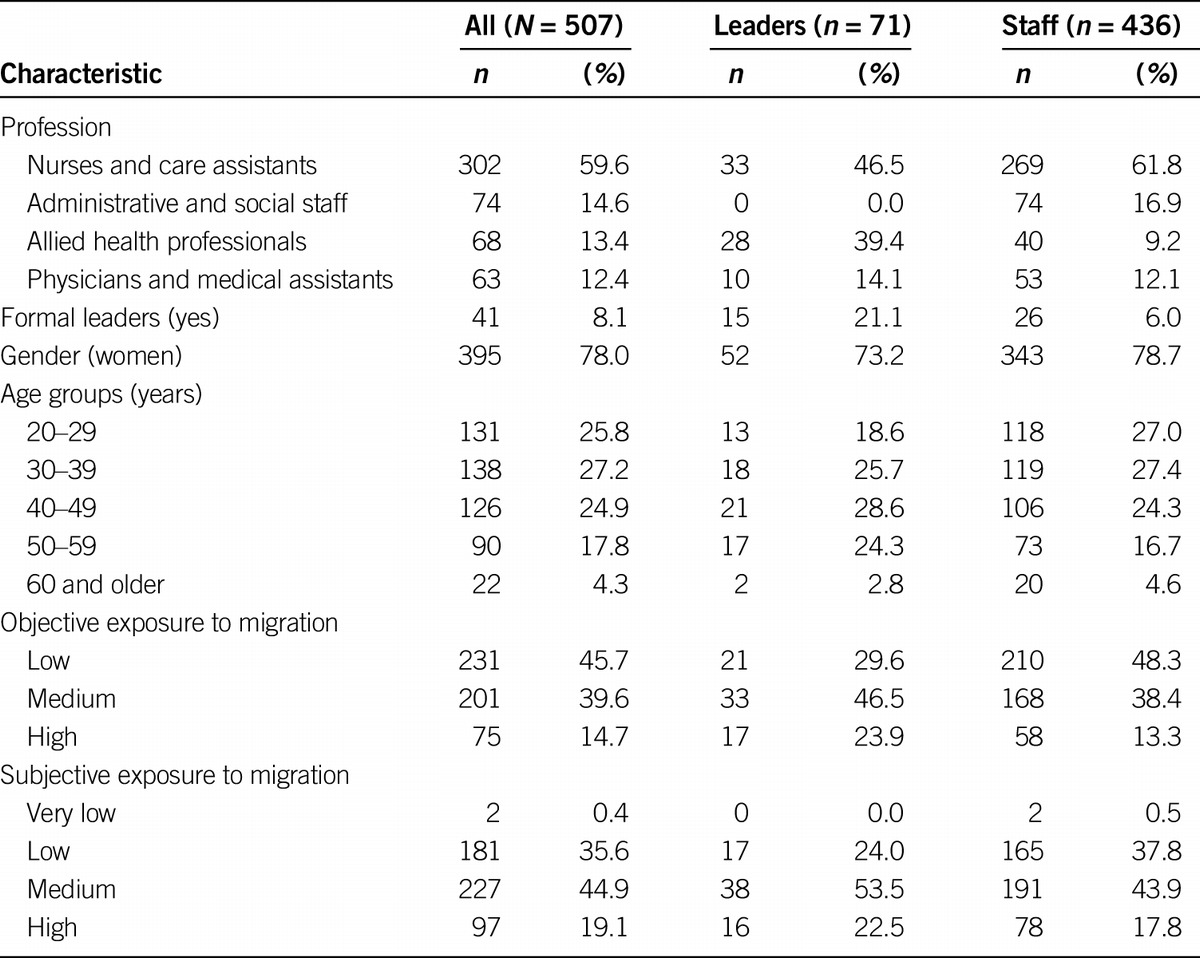
Table 2.
Cultural Competence: Differences Between Leaders and Staff
Correlations
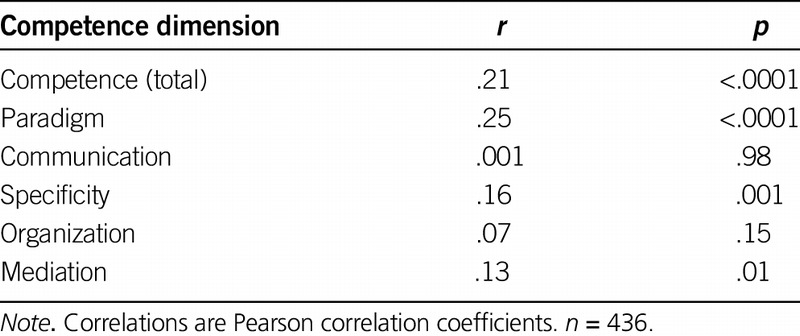
The Pearson correlation coefficients between the cultural competence of the leaders and that of the healthcare staff appear in Table 3. There was a slight positive correlation (r = .21, p < .001) between the cultural competence of the leaders (n = 71) and that of the healthcare staff (n = 436). Among the domains of cultural competence, paradigm competence had the strongest correlation (r = .25, p < .0001), followed by specificity competence (r = .16, p = .0009), and mediation competence (r = .13, p = .007). The communication competence (r = .001, p = .98) and organization competence (r = .07, p = .15) of the leaders and the healthcare staff were not significant.
Table 3.
Correlations: Leader and Staff Cultural Competence
Regression Models
Bivariate Models Table 4 shows estimates of the regression coefficients for the bivariate models for cultural competence, paradigm competence, specificity competence, and mediation competence. In the bivariate models, cultural competence of the healthcare staff increased with the cultural competence of the leaders. Paradigm competence had the highest coefficient ( = .35, p < .001).
= .35, p < .001).
Table 4.
Bivariate Regressions: Staff Cultural Competence on Leader Cultural Competence
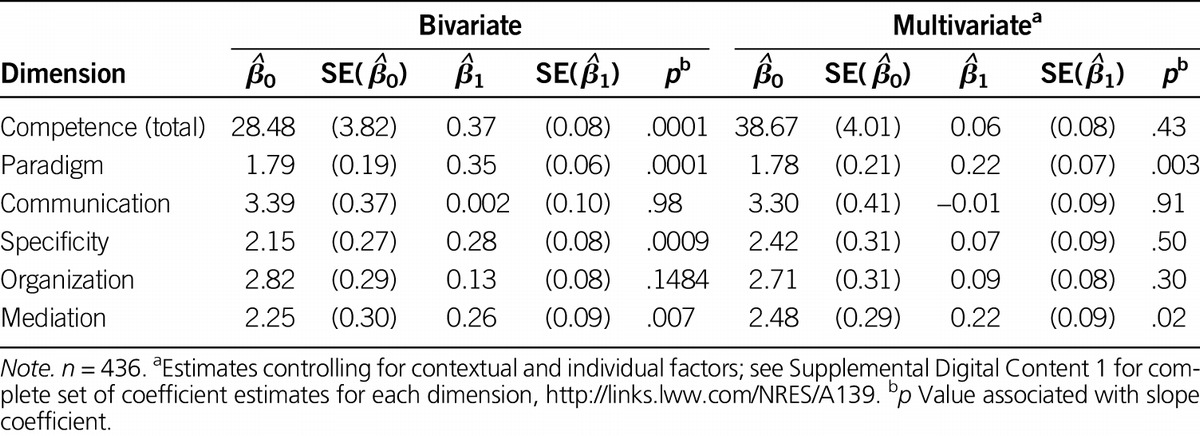
Multivariate Models Detailed results for the multivariate models are available in Supplemental Digital Content 1, http://links.lww.com/NRES/A139; estimated intercepts and coefficients for the regression of healthcare staff on leader (controlling for contextual and individual factors) are also shown in Table 4 for each of the competence dimensions. The effect of leader cultural competence on that of healthcare staff was nonsignificant when contextual variables (objective and subjective exposure to migration and type of service) and individual factors (gender, profession, or age) were controlled  = .06, p < .43). However, leader competence predicted paradigm competence (
= .06, p < .43). However, leader competence predicted paradigm competence ( = 0.22, p = .003), and mediation competence of the healthcare staff remained positively associated with the leaders’ competence (
= 0.22, p = .003), and mediation competence of the healthcare staff remained positively associated with the leaders’ competence ( = 0.22, p = .03). A nonsignificant result was found for specificity competence (
= 0.22, p = .03). A nonsignificant result was found for specificity competence ( = 0.07, p = .50).
= 0.07, p = .50).
Interaction Models Interactions were computed to analyze the intermediary mechanisms for paradigm competence and mediation competence. Detailed results are available in Supplemental Digital Content 1, http://links.lww.com/NRES/A139. In the interaction model for paradigm competence, interaction of language of the leader (especially if the leader language was English), leader training in cultural competence, and age (especially if 40 years old or older) with leader paradigm competence were significant predictors of staff paradigm competence. In the interaction model for mediation competence, interactions of leader language (especially if English), leader training in cultural competence, and social proximity of the leader (closer) with leader mediation competence were significant predictors of staff mediation competence.
DISCUSSION
The purpose of the study was to investigate the influence of leadership on the cultural competence of health professionals using a social network analysis. It was hypothesized that healthcare staff would be more likely to be culturally competent if their leaders were culturally competent. It was also hypothesized that the leadership effect would depend on the characteristics of the leader, including the expertise in cultural competence of the leaders.
Cultural competence of healthcare staff was positively associated with the cultural competence of the leaders, but for total cultural competence, this effect did not persist after controlling for contextual and sociodemographic variables. However, the effect did persist for paradigm and mediation competences. These findings partly support the hypothesis that healthcare staff were more likely to be culturally competent if their most central colleagues were culturally competent.
There is a considerable body of literature about organizational factors that influence cultural competence. The more the organizational environment formally and informally supports and encourages culturally responsive assessment and service delivery, the more likely health professionals are to develop cultural competence. Previous authors have recommended the development of positive leadership skills for intercultural care or a commitment toward intercultural care in order to facilitate the implementation and/or the diffusion of culturally competent attitudes (Yamada & Brekke, 2008). Champions of cultural competence or, in other words, influential leaders in cultural competence have been recommended as organizational strategies to support the development of cultural competence at the organizational level (Chrisman, 2007). Despite this acknowledgment of the importance of organizational factors, there have been very few empirical studies assessing the practical effects of such organizational factors on cultural competence (van Driel & Gabrenya, 2013). To our knowledge, our study is one of the first to assess the influence of the cultural competence of leaders on the cultural competence of the healthcare staff.
The interaction analysis helps to shed light on mechanisms by which leaders may influence healthcare staff: Leaders with expert positions had a greater positive impact on some dimensions of the cultural competence of the healthcare staff than leaders without specific expertise. “Expert” leadership would, therefore, appear to be a crucial determinant of the diffusion of cultural competence among health professionals. In other words, the findings suggest that cultural competence may be spread among health professionals through role-modeling rather than through the Pygmalion effect or formal leadership (e.g., head nurse). Role-modeling aims to help individuals to learn what cannot be taught, such as empathy, respectful attitudes toward patients, or professionalism (Warhurst, 2011). Consequently, more emphasis needs to be placed on positive role-modeling practices and, thus, on the social learning of cultural competence in the education of health professionals, as well as in lifelong learning programs. For example, mentorship has been shown to have a positive impact on the development of competences of health professionals (Gawlinski & Becker, 2012). Further studies should examine the role played by peer effects, as individual behaviors may be influenced more by homophilic peers rather than by individuals in a position of authority.
Limitations
The cross-sectional design precludes inferring causality. It is plausible that cultural competence of the leaders may be the result of the average cultural competence of the healthcare staff and not the cause. In other words, it could be that the cultural competence of the leaders represents the cultural competence needs of the service. Social desirability may have biased self-reports because of the sensitivity of ethnic questions in Belgium (Dauvrin et al., 2012). Preliminary analysis of response patterns did not show evidence of bias. However, as participation rates were lower in healthcare services identified as having a higher exposure to migration, the possibility that the data may reflect more cultural competence in health services than is actually present cannot be excluded.
Conclusions
Cultural competence among health professionals is acquired partly through role-modeling but is sensitive to contextual and individual factors. Development and implementation of cultural competence strategies require an appraisal of interprofessional relationships and a reliance on leadership role-modeling within healthcare services. Identifying the most central individuals and training them in cultural competence may constitute a new approach to lifelong learning in cultural competence. However, this approach requires caution because the most central individuals are not always the same persons as the formal leaders.
Supplementary Material
Figure.
No caption available.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.nursingresearchonline.com).
The authors acknowledge that research was funded through a research fellow grant from the Fond de la Recherche Scientifique de Belgique awarded to Marie Dauvrin (Grant FC84070 2009–2013). Marie Dauvrin is currently a postdoctoral researcher funded by the program Prospective Research for Brussels (INNOVIRIS) of the region of Brussels-Capital, Belgium. Computational resources were provided by the supercomputing facilities of the Université catholique de Louvain (CISM/UCL) and the Consortium des Equipements de Calcul Intensif en Fédération Wallonie Bruxelles (CECI) funded by the Fond de la Recherche Scientifique de Belgique.
The authors have no conflicts of interest to report.
REFERENCES
- Anderson L. M., Scrimshaw S. C., Fullilove M. T., Fielding J. E., Normand J. (2003). Culturally competent healthcare systems: A systematic review. American Journal of Preventive Medicine, 24, 68– 79 doi:10.1016/S0749-3797(02)00657-8 [DOI] [PubMed] [Google Scholar]
- Anderson R. A., Crabtree B. F., Steele D. J., McDaniel R. R., Jr. (2005). Case study research: The view from complexity science. Qualitative Health Research, 15, 669– 685 doi:10.1177/1049732305275208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes E., Bullock A. D., Bailey S. E. R., Cowpe J. G., Karaharju-Suvanto T. (2013). A review of continuing professional development for dentists in Europe. European Journal of Dental Education, 17, 5– 17 doi:10.1111/eje.12045 [DOI] [PubMed] [Google Scholar]
- Barrow M., McKimm J., Gasquoine S. (2011). The policy and the practice: Early-career doctors and nurses as leaders and followers in the delivery of health care. Advances in Health Sciences Education, 16, 17– 29 doi:10.1007/s10459-010-9239-2 [DOI] [PubMed] [Google Scholar]
- Beach M. C., Gary T. L., Price E. G., Robinson K., Gozu A., Palacio A., … Cooper L. A. (2006). Improving health care quality for racial/ethnic minorities: A systematic review of the best evidence regarding provider and organization interventions. BMC Public Health , 6, 104 doi:10.1186/1471-2458-6-104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach M. C., Price E. G., Gary T. L., Robinson K. A., Gozu A., Palacio A., Cooper L. A. (2005). Cultural competence: A systematic review of health care provider educational interventions. Medical Care, 43, 356.– 373 doi:10.1097/01.mlr.0000156861.58905.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt J. R., Green A. R. (2010). Commentary: Linking cultural competence training to improved health outcomes: Perspectives from the field. Academic Medicine, 85, 583– 585 doi:10.1097/ACM.0b013e3181d2b2f3 [DOI] [PubMed] [Google Scholar]
- Betancourt J. R., Green A. R., Carrillo J. E., Ananeh-Firempong O., II (2003). Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Reports , 118, 293– 302 Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1497553/pdf/12815076.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgatti S. P., Everett M. G., Freeman L. C. (2002). Ucinet for Windows: Software for social network analysis (version 6.416). Harvard, MA: Analytic Technologies. [Google Scholar]
- Brach C., Fraserirector I. (2000). Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Medical Care Research and Review, 57, 181– 217 doi:10.1177/1077558700574009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron I. D., Fairhall N., Langron C., Lockwood K., Monaghan N., Aggar C., … Kurrle S. E. (2013). A multifactorial interdisciplinary intervention reduces frailty in older people: Randomized trial. BMC Medicine , 11, 65 doi:10.1186/1741-7015-11-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campinha-Bacote J. (2002). The process of cultural competence in the delivery of healthcare services: A model of care. Journal of Transcultural Nursing, 13, 181– 184 doi:10.1177/10459602013003003 [DOI] [PubMed] [Google Scholar]
- Chrisman N. J. (2007). Extending cultural competence through systems change: Academic, hospital, and community partnerships. Journal of Transcultural Nursing, 18, 68S– 76S doi:10.1177/1043659606295692 [DOI] [PubMed] [Google Scholar]
- Creswick N., Westbrook J. I., Braithwaite J. (2009). Understanding communication networks in the emergency department. BMC Health Services Research, 9, 247 doi:10.1186/1472-6963-9-247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry S. E., Cortland C. I., Graham M. J. (2011). Role-modelling in the operating room: Medical student observations of exemplary behaviour. Medical Education, 45, 946– 957 doi:10.1111/j.1365-2923.2011.04014.x [DOI] [PubMed] [Google Scholar]
- Dauvrin M., Derluyn I., Coune I., Verrept H., Lorant V. (2012). Towards fair health policies for migrants and ethnic minorities: the case-study of ETHEALTH in Belgium. BMC Public Health, 12, 726 doi: 10.1186/1471-2458-12-726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMaggio P., Garip F. (2012). Network effects and social inequality. Annual Review of Sociology, 38, 93– 118 doi:10.1146/annurev.soc.012809.102545 [Google Scholar]
- Edmondson A. C. (2003). Speaking up in the operating room: How team leaders promote learning in interdisciplinary action teams. Journal of Management Studies, 40, 1419– 1452 doi:10.1111/1467-6486.00386 [Google Scholar]
- Eekhout I., de Boer R. M., Twisk J. W. R., de Vet H. C. W., Heymans M. W. (2012). Missing data: A systematic review of how they are reported and handled. Epidemiology, 23, 729– 732 doi:10.1097/EDE.0b013e3182576cdb [DOI] [PubMed] [Google Scholar]
- Fattore G., Frosini F., Salvatore D., Tozzi V. (2009). Social network analysis in primary care: The impact of interactions on prescribing behaviour. Health Policy, 92, 141– 148 doi:10.1016/j.healthpol.2009.03.005 [DOI] [PubMed] [Google Scholar]
- Ferguson J. K. (2009). Preventing healthcare-associated infection: Risks, healthcare systems and behaviour. Internal Medicine Journal, 39, 574– 581 doi:10.1111/j.1445-5994.2009.02004.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien, M. A., Flodgren G., Parmelli E., Doumit G., Gattellari M., Grimshaw J., Eccles M. P. (2011). Local opinion leaders: Effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews , 8 doi:10.1002/14651858.CD000125.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossion P., Ledoux Y., Valente F., Servais L., Staner L., Pelc I., Minner P. (2002). Psychiatric disorders and social characteristics among second-generation Moroccan migrants in Belgium: An age-and gender-controlled study conducted in a psychiatric emergency department. European Psychiatry, 17, 443– 450 doi:10.1016/S0924-9338(02)00707-1 [DOI] [PubMed] [Google Scholar]
- Freedman D. A. (2006). On the so-called “Huber sandwich estimator” and “robust standard errors.” American Statistician, 60, 299– 302 doi:10.1198/000313006X152207 [Google Scholar]
- Friedkin N. E. (2001). Norm formation in social influence networks. Social Networks, 23, 167– 189 doi:10.1016/S0378-8733(01)00036-3 [Google Scholar]
- Fuller J. B., Hester K., Barnett T., Relyea L. F. C. (2006). Perceived organizational support and perceived external prestige: Predicting organizational attachment for university faculty, staff, and administrators. Journal of Social Psychology, 146, 327– 347 doi:10.3200/SOCP.146.3.327-347 [DOI] [PubMed] [Google Scholar]
- Gawlinski A., Becker E. (2012). Infusing research into practice: A staff nurse evidence-based practice fellowship program. Journal for Nurses in Staff Development, 28, 69– 73 doi:10.1097/NND.0b013e31824b418c [DOI] [PubMed] [Google Scholar]
- Ingleby J. D. (2011). Memorandum of understanding For the implementation of a European Concerted Research Action designated as COST Action IS1103 ADAPTING EUROPEAN HEALTH SYSTEMS TO DIVERSITY (ADAPT). Brussels, Belgium: COST Network. [Google Scholar]
- Jabobs D., Rea A. (2005). Construction et importation des classements ethniques. Allochtones et immigrés aux Pays-Bas et en Belgique. [Construction and importation of ethnic classifications. Foreigners and immigrants in the Netherlands and Belgium]. Revue Européenne des Migrations Internationales, 21, 35– 59. [Google Scholar]
- Jirwe M., Gerrish K., Keeney S., Emami A. (2009). Identifying the core components of cultural competence: Findings from a Delphi study. Journal of Clinical Nursing, 18, 2622– 2634 doi:10.1111/j.1365-2702.2008.02734.x [DOI] [PubMed] [Google Scholar]
- Johnstone M.-J., Kanitsaki O. (2008). The politics of resistance to workplace cultural diversity education for health service providers: An Australian study. Race Ethnicity and Education, 11, 133– 154 doi:10.1080/13613320802110258 [Google Scholar]
- Kaplan H. C., Brady P. W., Dritz M. C., Hooper D. K., Linam W. M., Froehle C. M., Margolis P. (2010). The influence of context on quality improvement success in health care: A systematic review of the literature. Milbank Quarterly, 88, 500– 559 doi:10.1111/j.1468-0009.2010.00611.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krajic K., Straßmayar C., Karl-Trummer U., Novak-Zezula S., Pelikan J. M. (2005). Improving ethnocultural competence of hospital staff by training: Experiences from the European ‘Migrant-Friendly Hospitals’ project. Diversity in Health and Social Care, 2, 279– 290. [Google Scholar]
- Kreuter M. W., Lukwago S. N., Bucholtz D. C., Clark E. M., Sanders-Thompson V. (2003). Achieving cultural appropriateness in health promotion programs: Targeted and tailored approaches. Health Education & Behavior, 30, 133– 146 doi:10.1177/10901798102251021 [DOI] [PubMed] [Google Scholar]
- Laczko F., Appave G. (Eds.) (2013). World migration report 2013. Migrant well-being and development. Geneva, Switzerland: International Organization of Migration; Retrieved from http://publications.iom.int/bookstore/free/WMR2013_EN.pdf [Google Scholar]
- Laveault D., Grégoire J. (2002). Introduction aux théories des tests en psychologie et en sciences de l’éducation [Introduction to theories of tests in psychology and in educational sciences] (2nd ed.). Brussels, Belgium: De Boeck. [Google Scholar]
- Levecque K., Lodewyckx I., Vranken J. (2007). Depression and generalised anxiety in the general population in Belgium: A comparison between native and immigrant groups. Journal of Affective Disorders, 97, 229– 239 doi:10.1016/j.jad.2006.06.022 [DOI] [PubMed] [Google Scholar]
- Livingston J. S. (1988). Pygmalion in management. Harvard Business Review , 81, 1– 12 Retrieved from http://www.iwolm.com/wp-content/downloads/pygmalion.pdf [PubMed] [Google Scholar]
- Lorant V., Van Oyen H., Thomas I. (2008). Contextual factors and immigrants’ health status: Double jeopardy. Health & Place, 14, 678– 692 doi:10.1016/j.healthplace.2007.10.012 [DOI] [PubMed] [Google Scholar]
- Marsick V. J., Watkins K. E. (2007). Les tensions de l’apprentissage informel sur le lieu de travail [Tensions surrounding informal learning in the workplace]. Revue Française de Pédagogie, 160, 29– 38 doi:10.4000/rfp.586 [Google Scholar]
- Mascia D., Cicchetti A., Damiani G. (2013). “Us and them”: A social network analysis of physicians’ professional networks and their attitudes towards EBM. BMC Health Service Research, 13, 429 doi:10.1186/1472-6963-13-429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mostow C., Crosson J., Gordon S., Chapman S., Gonzalez P., Hardt E., … David M. (2010). Treating and precepting with RESPECT: A relational model addressing race, ethnicity, and culture in medical training. Journal of General Internal Medicine , 25, 146– 154 doi:10.1007/s11606-010-1274-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen S. S., Krasnik A. (2010). Poorer self-perceived health among migrants and ethnic minorities versus the majority population in Europe: A systematic review. International Journal of Public Health, 55, 357– 371 doi:10.1007/s00038-010-0145-4 [DOI] [PubMed] [Google Scholar]
- Northouse P. G. (2009). Leadership: Theories and practices (5th ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Ochieng B. M. N. (2013). Black African migrants: The barriers with accessing and utilizing health promotion services in the UK. European Journal of Public Health, 23, 265– 269 doi:10.1093/eurpub/cks063 [DOI] [PubMed] [Google Scholar]
- Paez K. A., Allen J. K., Beach M. C., Carson K. A., Cooper L. A. (2009). Physician cultural competence and patient ratings of the patient-physician relationship. Journal of General Internal Medicine, 24, 495– 498 doi:10.1007/s11606-009-0919-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perloff R. M., Bonder B., Ray G. B., Ray E. B., Siminoff L. A. (2006). Doctor-patient communication, cultural competence, and minority health: Theoretical and empirical perspectives. American Behavioral Scientist, 49, 835– 852 doi:10.1177/0002764205283804 [Google Scholar]
- Purnell L. (2002). The Purnell model for cultural competence. Journal of Transcultural Nursing, 13, 193– 196 doi:10.1177/10459602013003006 [DOI] [PubMed] [Google Scholar]
- Qureshi A., Collazos F., Ramos M., Casas M. (2008). Cultural competency training in psychiatry. European Psychiatry, 23, 49– 58. doi:10.1016/S0924-9338(08)70062-2 [DOI] [PubMed] [Google Scholar]
- Renzaho A. M. N., Romios P., Crock C., Sønderlund A. L. (2013). The effectiveness of cultural competence programs in ethnic minority patient-centered health care—A systematic review of the literature. International Journal for Quality in Health Care, 25, 261– 269 doi:10.1093/intqhc/mzt006 [DOI] [PubMed] [Google Scholar]
- Roberts S. A., Sieczkowski C., Campbell T., Balla G., Keenan A. (2012). Implementing and sustaining a hand hygiene culture change programme at Auckland District Health Board. New Zealand Medical Journal, 125, 75– 85. [PubMed] [Google Scholar]
- Sandhu S., Bjerre N. V., Dauvrin M., Dias S., Gaddini A., Greacen T., … Priebe S. (2013). Experiences with treating immigrants: A qualitative study in mental health services across 16 European countries. Social Psychiatry and Psychiatric Epidemiology , 48, 105– 116 doi:10.1007/s00127-012-0528-3 [DOI] [PubMed] [Google Scholar]
- Sasse A., Deblonde J., Van Beckhoven D. (2013). Epidémiologie du SIDA et de l’infection à VIH en Belgique [Epidemiology of AIDS and HIV-related infections in Belgium] (p. 75). Brussels, Belgium: Institut Scientifique de Santé Publique ISP; Retrieved from https://www.wiv-isp.be/News/Documents/Rapport_VIH-SIDA_2013_Print_Press.pdf [Google Scholar]
- Seeleman C., Suurmond J., Stronks K. (2009). Cultural competence: A conceptual framework for teaching and learning. Medical Education, 43, 229– 237 doi:10.1111/j.1365-2923.2008.03269.x [DOI] [PubMed] [Google Scholar]
- Service Public Fédéral Economie, P.M.E (2010). Population par nationalité par commune 01.01.2010 [Population by nationality by municipality 01.01.2010]. Brussels, Belgium: Service Public Fédéral, Economie P. M. E. Classes Moyennes et Energie. [Google Scholar]
- Stansbury J. P., Jia H., Williams L. S., Vogel W. B., Duncan P. W. (2005). Ethnic disparities in stroke: Epidemiology, acute care, and postacute outcomes. Stroke , 36, 374– 386 doi:10.1161/01.STR.0000153065.39325.fd [DOI] [PubMed] [Google Scholar]
- Taylor S. L., Dy S., Foy R., Hempel S., McDonald K. M., Øÿvretveit J., … Shekelle P. G. (2011). What context features might be important determinants of the effectiveness of patient safety practice interventions? BMJ Quality & Safety , 20, 611– 617 doi:10.1136/bmjqs.2010.049379 [DOI] [PubMed] [Google Scholar]
- Ujcic-Voortman J. K., Baan C. A., Seidell J. C., Verhoeff A. P. (2012). Obesity and cardiovascular disease risk among Turkish and Moroccan migrant groups in Europe: A systematic review. Obesity Reviews, 13, 2– 16 doi:10.1111/j.1467-789X.2011.00932.x [DOI] [PubMed] [Google Scholar]
- Valente T. W. (2010). Social networks and health: Models, methods and applications. (pp. 81– 99). Oxford, UK: Oxford University Press. [Google Scholar]
- van Driel M., Gabrenya W. K., Jr. (2013). Organizational cross-cultural competence: Approaches to measurement. Journal of Cross-Cultural Psychology, 44, 874– 899 doi:10.1177/0022022112466944 [Google Scholar]
- van Heurck R., Payen M. C., De Wit S., Clumeck N. (2013). Epidemiology of MDR-TB in a Belgian infectious diseases unit: A 15 years review. Acta Clinica Belgica, 68, 321– 324 doi:10.2143/acb.3269 [DOI] [PubMed] [Google Scholar]
- Vandenheede H., Deboosere P. (2009). Type 2 diabetes in Belgians of Turkish and Moroccan origin. Archives of Public Health, 67, 62– 87 doi:10.1186/0778-7367-67-2-62 [Google Scholar]
- Warhurst R. (2011). Role modelling in manager development: Learning that which cannot be taught. Journal of European Industrial Training, 35, 874– 891 doi:10.1108/03090591111185565 [Google Scholar]
- Wells M. I. (2000). Beyond cultural competence: A model for individual and institutional cultural development. Journal of Community Health Nursing, 17, 189– 199 doi:10.1207/S15327655JCHN1704_1 [DOI] [PubMed] [Google Scholar]
- Wilson C., Alam R., Latif S., Knighting K., Williamson S., Beaver K. (2012). Patient access to healthcare services and optimisation of self-management for ethnic minority populations living with diabetes: A systematic review. Health and Social Care in the Community, 20, 1– 19 doi:10.1111/j.1365-2524.2011.01017.x [DOI] [PubMed] [Google Scholar]
- Yamada A.-M., Brekke J. S. (2008). Addressing mental health disparities through clinical competence not just cultural competence: The need for assessment of sociocultural issues in the delivery of evidence-based psychosocial rehabilitation services. Clinical Psychology Review, 28, 1386– 1399 doi:10.1016/j.cpr.2008.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwarenstein M., Goldman J., Reeves S. (2009). Interprofessional collaboration: Effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews, Issue 3, Art. No. CD000072. doi:10.1002/14651858.CD000072.pub [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


