Abstract
Purpose of review
To provide an overview of acquired coagulopathies that can occur in various perioperative clinical settings. Also described are coagulation disturbances linked to antithrombotic medications and currently available strategies to reverse their antithrombotic effects in situations of severe hemorrhage.
Recent findings
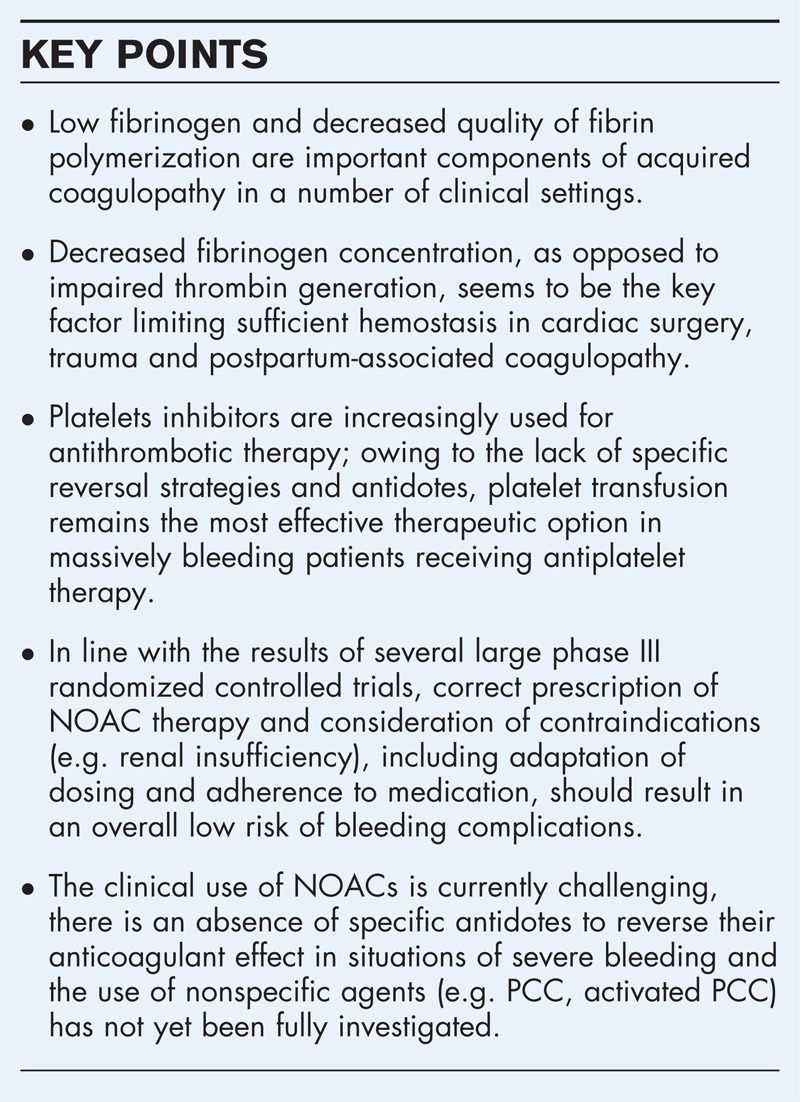
Recent studies highlight the link between low fibrinogen and decreased fibrin polymerization in the development of acquired coagulopathy. Particularly, fibrin(ogen) deficits are observable after cardiopulmonary bypass in cardiac surgery, on arrival at the emergency room in trauma patients, and with ongoing bleeding after child birth. Regarding antithrombotic therapy, although new oral anticoagulants offer the possibility of efficacy and relative safety compared with vitamin K antagonists, reversal of their anticoagulant effect with nonspecific agents, including prothrombin complex concentrate, has provided conflicting results. Specific antidotes, currently being developed, are not yet licensed for clinical use, but initial results are promising.
Summary
Targeted hemostatic therapy aims to correct coagulopathies in specific clinical settings, and reduce the need for allogeneic transfusions, thus preventing massive transfusion and its deleterious outcomes. Although there are specific guidelines for reversing anticoagulation in patients treated with antiplatelet agents or warfarin, there is currently little evidence to advocate comprehensive recommendations to treat drug-induced coagulopathy associated with new oral anticoagulants.
Keywords: anticoagulants, coagulopathy, hemorrhage, reversal
INTRODUCTION
During hemostasis, coagulation factors participate in a complex cascade culminating in the generation of thrombin, which catalyzes the conversion of fibrinogen to fibrin (Fig. 1) [1]. Fibrinogen plays a critical role in achieving and maintaining hemostasis; it serves as the precursor to fibrin, an essential component of blood clots. Subsequent polymerization forms fibrin strands, which become covalently cross-linked by activated coagulation factor XIII [2]. Fibrinogen also promotes platelet aggregation by binding glycoprotein IIb/IIIa receptors. These platelets strengthen the clot by becoming enmeshed within the fibrin strands (Fig. 2).
FIGURE 1.
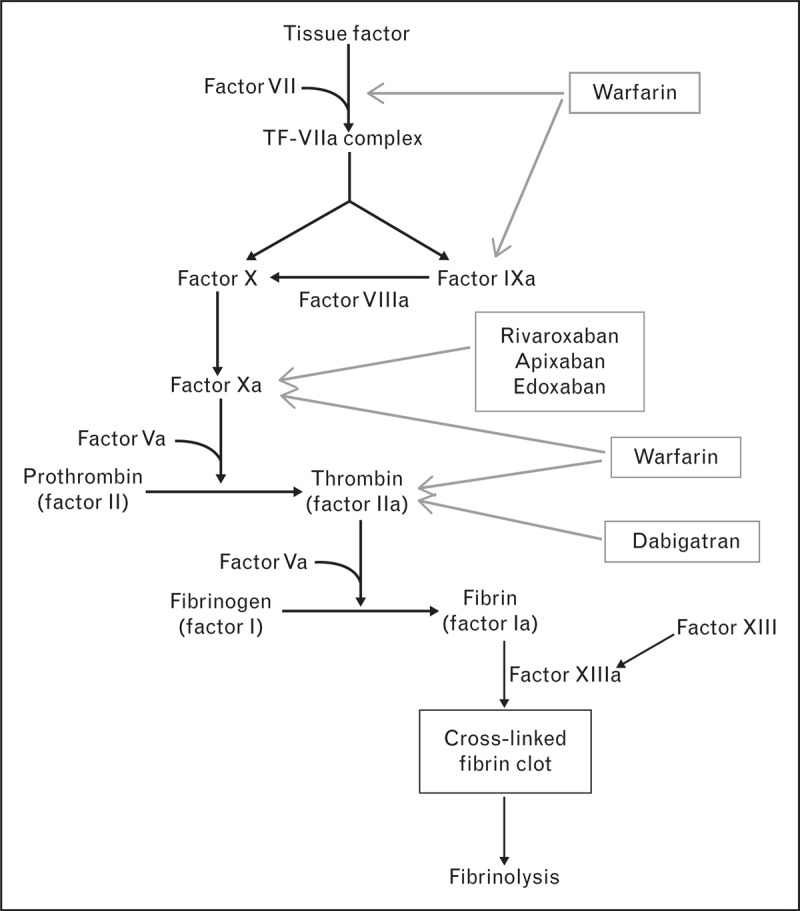
Points of action for oral anticoagulants on the coagulation cascade. Adapted with permission from [1].
FIGURE 2.
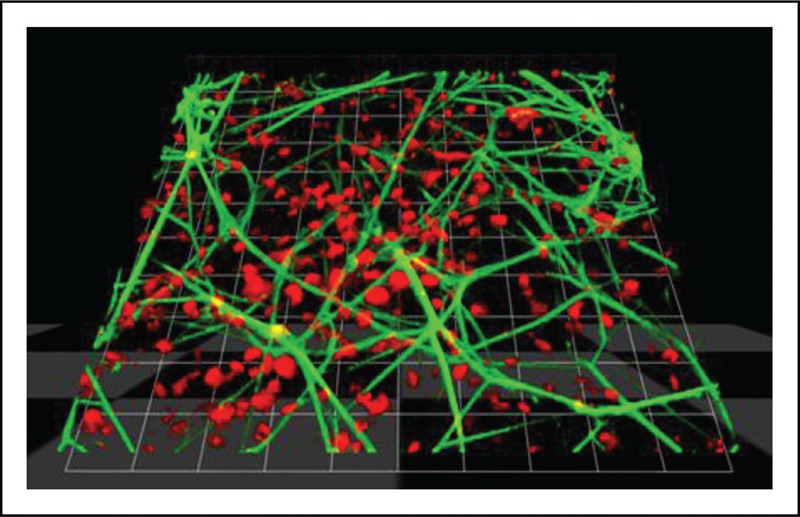
Confocal imaging of clot formation. 3D visualization of a human blood clot: fibrin (light grey) was visualized via the detection of a fluorescein isothiocyanate-conjugated antifibrinogen antibody [3] added prior to the initiation of the coagulation process (star-tem/ex-tem). Platelets (dark grey) were stained using a fluorescently labeled wheat germ agglutinin [Real-time live confocal microscopy of a human blood sample stained with TMRM (light grey) and WGA (dark grey)]. The image was acquired by live confocal microscopy using an inverted microscope (Zeiss Observer.Z1; Zeiss, Oberkochen, Germany) in combination with a spinning disc confocal system (UltraVIEW VoX; Perkin Elmer, Waltham, MA). 1 Unit = 10.21 μm; objective: 63 × oil immersion, NA 1.42.
Studies have shown that low fibrinogen concentration, that is below the normal range of 2.0–4.5 g/l [4], is associated with an increased risk of bleeding [5–7]. There is also evidence that fibrinogen supplementation can increase clot strength and reduce bleeding [8▪,9,10▪]. European guidelines published in 2013 on the management of severe bleeding in the perioperative and trauma settings both recommend fibrinogen supplementation when plasma fibrinogen concentration falls below 1.5–2.0 g/l during ongoing bleeding [11,12]. Although fibrinogen supplementation does not correct defects unrelated to fibrin-based clotting (e.g. platelet dysfunction or impaired thrombin generation), it may compensate for deficits in other parts of the hemostatic system. Indeed, experimental and prospective data have shown that fibrinogen supplementation may compensate for decreased platelet contribution to clot strength [13–15].
Physiological hemostasis is a balance between coagulation (clot formation) and fibrinolysis (clot breakdown) to protect against extreme situations such as hemorrhage and thrombosis. An imbalance in physiological hemostasis leads to coagulopathy, a condition characterized by inability of the blood to clot. Coagulopathy may be caused by a reduction or complete absence of blood-clotting proteins or as a result of dysfunction or reduced levels of platelets. This condition can lead directly to spontaneous bleeding or can exacerbate bleeding resulting from trauma, surgical procedures or medical therapy. However, in critically ill patients, activation of the coagulation system as a result of trauma, inflammation, or infection may lead to thrombosis or thromboembolic complications.
Box 1.
no caption available
ACQUIRED COAGULOPATHY IN THE PERIOPERATIVE SETTING
In the clinical settings of cardiovascular surgery, trauma and obstetrics, the primary causes of bleeding are usually anatomical rather than pathophysiological and the first step to management often involves surgical measures. The next priority is usually volume resuscitation, as maintenance of blood volume is necessary for adequate tissue perfusion and oxygenation. Acquired coagulopathy can develop secondary to blood loss, loss and consumption of coagulation factors and hemodilution owing to excessive fluid replacement and is a major risk factor for progression from initial bleeding to severe hemorrhage. Evidence suggests that restrictive fluid resuscitation strategies are associated with shorter lengths of ICU and hospital stay and decreased mortality [16,17]. However, hypovolemia results in acidosis, which is a key player in exacerbating coagulopathy. In the presence of coagulopathy, further blood loss can occur from not only ongoing surgery, but also from loss or consumption or dysfunction of coagulation factors, platelets and other blood cells involved in hemostasis. Therefore, early intervention with hemostatic therapy may be critical to prevent development of complex coagulopathies and the progression to severe, life-threatening hemorrhage. Recent clinical studies highlighting strategies to control bleeding and correct fibrin-based clot strength in various clinical settings are shown in Table 1[8▪,10▪,15,18–20,21▪].
Table 1.
Overview of recent studies highlighting methods to control bleeding and correct fibrin-based clot strength in various clinical settings
| Study | Design | Treatment (no. of patients) | Major findings |
| Cardiovascular surgery | |||
| Rahe-Meyer et al. [8▪] | RCT | Fibrinogen concentrate (n = 29) | Fibrinogen concentrate controls coagulopathic bleeding during aortic surgery more effectively than placebo or a standardized treatment algorithm (4 units FFP or 2 units apheresis platelets) |
| FFP/PLT (n = 32) | Fibrinogen concentrate also provides a more rapid and at least as effective control of intraoperative bleeding compared with standardized treatment (post-hoc analysis of data [18]) | ||
| Plasma fibrinogen and FIBTEM MCF were corrected by fibrinogen concentrate or fibrinogen concentrate + FFP | |||
| Fibrinogen concentrate raises plasma fibrinogen more effectively than FFP, as it allows targeting of a high normal level | |||
| The increases were short-lived; plasma fibrinogen and FIBTEM MCF were comparable in all groups by 24 h postsurgery | |||
| Tanaka et al. [15] | Prospective, randomized open-label study | Fibrinogen concentrate (n = 10) | Despite moderately decreased thrombin generation, bleeding was reduced with a single dose of 4-g fibrinogen concentrate to reach a target fibrinogen level of 2 g/l |
| PLT (n = 10) | |||
| Trauma | |||
| Khan et al. [19] | Prospective cohort study | 4 U PRBCs up to 12 U | Hemostatic resuscitation does not correct hypoperfusion or coagulopathy during the acute phase of trauma hemorrhage |
| Innerhofer et al. [20] | Post hoc analysis of data from a prospective study | Coagulation factor concentrates (fibrinogen concentrate and/or PCC; n = 66) | Coagulation factor concentrates alone corrected coagulopathy in patients with severe blunt trauma |
| Coagulation factor concentrates (fibrinogen concentrate and/or PCC) + FFP (n = 78) | |||
| Postpartum hemorrhage | |||
| Collins et al. [21▪] | Prospective, observational study | n = 356 | Fibrin-based clot formation is a rapidly available early biomarker for progression of postpartum hemorrhage |
| Mallaiah et al. [10▪] | Prospective two-phase study | Phase 1: n = 42 | Fibrinogen concentrate allows prompt correction of coagulation deficits associated with major obstetric hemorrhage |
| Phase 2: n = 51 | |||
FFP, fresh frozen plasma; MCF, maximum clot firmness; PCC, prothrombin complex concentrate; PLT, platelet; PRBCs, packed red blood cells; RCT, randomized controlled trial.
Cardiac surgery
During cardiac surgery, the primary cause of bleeding is related to surgery. Risk factors associated with increased bleeding include advanced age (>70 years), preoperative anticoagulant and/or antiplatelet therapy, preoperative coagulopathy and renal insufficiency [22]. The type of operation also impacts bleeding, for example cardiac surgery with cardiopulmonary bypass (CPB) causes widespread activation of the hemostatic system, including defects of primary hemostasis and acquired von Willebrand disease depending on the length of time on bypass. Although heparin is used to prevent blood clotting, activation of coagulation still occurs and increases as the duration of CPB increases. Furthermore, prior to surgery, the use of priming solutions such as crystalloids can lead to dilution of coagulation factors and platelets [23]. Blood components also interact with the lining of the CPB circuit causing activation, which leads to decreased levels of coagulation factors and platelets. Coagulation is grossly abnormal after discontinuation of CPB; both plasma and cellular components are affected resulting in platelet and clotting factor activation, consumption and dilution, together with activation of inflammatory cascades. Notably, plasma fibrinogen concentration has been reported to decrease by 34–42% by the end of CPB, relative to preoperative levels [5,24]. Reduced thrombin generation after CPB has also been reported and is implicated in excess postoperative bleeding [25,26]. However, immediately following cardiac surgery, the quality of the fibrin-based clot is significantly more impaired than both thrombin generation and the platelet component of the clot (decrease of 38%, 7% and 27% compared with baseline, respectively) [27].
Trauma
Coagulopathy is common in trauma and can occur very early after injury [28]. On arrival at hospital, before the administration of large amounts of fluid and prior to the onset of hypothermia and acidosis, 28–60% of patients have an identifiable coagulopathy [28–30]. This acute coagulopathy of trauma (ACT), which develops rapidly after injury in response to a combination of tissue injury and shock, is an indicator of poor prognosis [31]. ACT is associated with increased mortality, greater transfusion requirements, increased incidence of organ failure, and longer ICU and in-hospital stay [32]. In particular, a relationship between low fibrinogen concentration or decreased quality of the fibrin-based clot on arrival at the emergency room and increased transfusion requirements or mortality has recently been demonstrated [33–35].
ACT is exacerbated by subsequent medical interventions, such as massive transfusion, and contributes to trauma-associated coagulopathy [36]. The factors underlying trauma-associated coagulopathy, including hypothermia, acidosis and dilution/loss/consumption of coagulation factors, are a consequence of hemorrhage, hypoperfusion and fluid resuscitation [36]. Also in this context, the role of fibrinogen is being increasingly scrutinized; it has been shown that fibrinogen depletion in trauma occurs early and is central to trauma-associated coagulopathy [37].
Postpartum hemorrhage
During pregnancy, normal physiological changes lead to marked changes in the coagulation and fibrinolytic systems. The majority of coagulation factors increase and natural anticoagulants decrease augmenting coagulation and reducing fibrinolytic activity, thus creating a state of hypercoagulability [38]. These changes, which usually return to prepregnancy levels 3 weeks postpartum [39], may be important for minimizing blood loss at delivery.
Blood loss less than 500 ml is considered normal during delivery. Postpartum hemorrhage (PPH; defined as blood loss ≥500 ml within 24 h following delivery), and severe PPH (blood loss >1000 ml within 24 h) [40], occurs as a result of a number of obstetric complications. These complications include uterine atony, genital tract trauma (i.e. vaginal or cervical lacerations), uterine rupture, retained placental tissue or maternal bleeding disorders [40,41]. Bleeding leads to loss and consumption of coagulation factors, which may be exacerbated by dilutional coagulopathy after volume resuscitation. Therefore, hemostatic impairment may develop during PPH, which can increase bleeding and thus progression toward severe PPH [42].
Studies suggest that fibrinogen deficit may be important for the development and severity of PPH. Fibrinogen concentration decreases progressively with increasing blood loss and was shown to be the most sensitive marker of developing hemostatic impairment in women with PPH [43]. In fact, plasma fibrinogen concentration 2 g/l or less, measured during the course of an obstetric hemorrhage, has a positive predictive value of 100% for the evolution to severe PPH [5]. Rapid replacement of fibrinogen, in addition to conventional treatments, has been shown to control bleeding in patients with obstetric hemorrhage [44]. In addition, fibrinogen concentrate corrects coagulation deficits associated with major obstetric hemorrhage and reduces the requirement for blood component therapy and the associated complications [10▪].
DRUG-INDUCED COAGULOPATHY
Coagulopathy may occur in patients receiving antithrombotic therapy. Consequently, antithrombotic agents that are used for thromboembolic prophylaxis increase a patient's risk of bleeding. An overview of these agents, including their mode of action and therapeutic indications, is shown in Table 2. If mild bleeding occurs or a patient requires an urgent invasive procedure, a decision must be made whether or not to discontinue therapy, keeping in mind that discontinuation can increase a patient's risk of ischemic events (especially in the elderly patient) [45]. In cases of major bleeding, besides several general actions such as correcting the hemodynamic compromise and/or use of endoscopic or surgical measures among others, reversal of antithrombotic therapy is also necessary. There is little evidence from clinical trials to advocate comprehensive recommendations; decisions are empirical and made on an individual patient basis. Therefore, there is a need for well defined strategies for the reversal of these agents in a number of clinical situations.
Table 2.
Overview of antiplatelet and oral anticoagulant agents, their mode of action and therapeutic indications
| Agent | Mode of action | Tmax | t1/2 | Therapeutic indications |
| Antiplatelet agents | ||||
| Aspirin | Irreversible inhibition of cyclo-oxygenase preventing the formation of thromboxane A2 | – | – | Aspirin has analgesic, antipyretic and anti-inflammatory actions and is used to treat a range of conditions, including relief of headache, migraine and neuralgia, and symptomatic relief of rheumatic pain and sciatica |
| It also has an antithrombotic action and is indicated for the: | ||||
| Treatment of patients with ACS | ||||
| Secondary prevention of cardiovascular events in patients with angina, MI, stroke and TIA, PAD, and atrial fibrillation | ||||
| NSAIDs (e.g. ibuprofen and naproxen) | Reversible inhibition of cyclo-oxygenase preventing the formation of thromboxane A2 | – | – | NSAIDs are used to treat a wide range of indications, particularly those associated with pain and inflammation, e.g. mild-to-moderate pain owing to inflammation and tissue injury, postoperative pain, osteoarthritis and rheumatoid arthritis |
| Thienopyridine derivatives (e.g. clopidogrel, ticlopidine, ticagrelor and prasugrel) | Inhibit ADP-mediated platelet activation through the irreversible blockade of P2Y12 receptors | – | – | Secondary prevention of atherothrombotic events in patients suffering from: |
| STEMI ACS, MI, ischemic stroke, established PAD | ||||
| NSTEMI ACS (in combination with aspirin) | ||||
| Prevention of atherothrombotic and thromboembolic events in patients with atrial fibrillation | ||||
| Oral anticoagulants | ||||
| Vitamin K antagonists | ||||
| Warfarin | Inhibits the ϒ carboxylation step in the synthesis of vitamin K-dependent clotting factors II, VII, IX and X | Circulating drug: 90 min | Circulating drug: 36–42 h | Primary and secondary prevention of a wide range of thromboembolic disorders |
| Common indications include: | ||||
| Therapeutic INR: ∼5–7 days | Normalization of INR: ∼5 days | Stroke prevention in patients with atrial fibrillation | ||
| Prevention of thrombus formation in patients with mechanical heart valves | ||||
| Treatment of VTE | ||||
| New/direct | ||||
| Rivaroxaban (Xarelto) | Direct inhibition of factor Xa | 2–4 h | 9–13 h | Prophylaxis of VTE following elective hip and knee replacement surgery |
| Treatment and secondary prophylaxis of VTE | ||||
| Prophylaxis of stroke and systemic embolism in patients with nonvalvular atrial fibrillation | ||||
| Prevention of atherothrombotic events in ACS (in combination with aspirin alone or aspirin plus clopidogrel or ticlopidine) | ||||
| Apixaban (Eliquis) | Direct inhibition of factor Xa | 1–3 h | 8–15 h | Prophylaxis of VTE following elective hip and knee replacement surgery |
| Prophylaxis of stroke and systemic embolism in patients with nonvalvular atrial fibrillation | ||||
| Dabigatran etexilate (Pradaxa) | Direct inhibition of thrombin | 1.25–3 h | 12–14 h | Prophylaxis of VTE following elective hip and knee replacement surgery |
| Treatment and secondary prophylaxis of VTE | ||||
| Prophylaxis of stroke and systemic embolism in patients with nonvalvular atrial fibrillation | ||||
ACS, acute coronary syndrome; INR, international normalized ratio; MI, myocardial infarction; NSTEMI, non-ST segment elevation myocardial infarction; PAD, peripheral arterial disease; STEMI, ST segment elevation myocardial infarction; t1/2, elimination half-life; TIA, transient ischemic attack; Tmax, time to maximum effect; VTE, venous thromboembolism.
Antiplatelet agents
Antiplatelet agents are effective treatments to reduce the risk of ischemic events such as myocardial infarction and stroke (Table 2). The timing of their discontinuation for surgical procedures is important, as cessation of treatment results in the recovery of platelet function, which may contribute to the occurrence of ischemic events [46]. Conversely, the most serious adverse event associated with these agents is bleeding [47]; therefore, delaying discontinuation may result in increased bleeding.
Current guidelines recommend that for surgical procedures with high-to-very-high bleeding risk, clopidogrel be discontinued 5 days before surgery to reduce bleeding and the need for transfusion, while maintaining aspirin throughout the perioperative period [45]. Conversely, in cases of serious bleeding, such as intracranial hemorrhage, the antithrombotic effect needs to be reversed immediately. The most broadly accepted method is the administration of platelet concentrate. Although based on limited evidence, it is currently recommended that platelets be administered to maintain platelet count above 50 × 109 cells/l in moderate bleeding and above 100 × 109 cells/l in patients with ongoing bleeding and/or traumatic brain injury [11]. Another approach is to administer platelets and/or desmopressin and tranexamic acid.
Vitamin K antagonists
Vitamin K antagonists (e.g. warfarin) are the most commonly used oral anticoagulants for the prevention and treatment of a wide range of cardiovascular diseases (Table 2). The most serious complication of therapy is bleeding; if bleeding occurs, or if a patient needs to undergo an invasive procedure, the bleeding risk needs to be balanced with the thrombotic risk. The most appropriate method to reverse the anticoagulant effect of vitamin K antagonists is dependent on the severity and urgency of the clinical situation. Options include simple dose omission, administration of vitamin K or administration of coagulation factor concentrates. Studies have suggested that oral (1.0–5.0 mg) or intravenous (0.5–2.0 mg) vitamin K can be administered to reverse the anticoagulant effects of warfarin [48,49]. Current guidelines recommend intravenous vitamin K (5 or 10 mg), as it achieves reversal more rapidly than oral administration [49,50]. In cases of serious bleeding or for patients requiring emergency surgery, complete and rapid reversal is necessary and replacement of vitamin K-dependent coagulation factors (II, VII, IX and X) may be required. Current guidelines suggest rapid reversal of anticoagulation with a four-factor prothrombin complex concentrate (PCC), which has been shown to provide a more rapid reversal of anticoagulation with fewer adverse events than fresh frozen plasma [51▪,52▪,53]. In addition, 5–10 mg intravenous vitamin K should be administered if reversal of anticoagulation is to be sustained [53,54].
In the absence of bleeding and if a patient requires surgery or an invasive procedure, it is recommended that warfarin be discontinued 5 days prior to the procedure [55]. The international normalized ratio (INR) should be monitored the day before surgery (INR 2–3, administer 3 mg intravenous vitamin K) and the day of surgery (INR >1.5 defer procedure). In patients at a high risk for thromboembolic events bridging therapy with low molecular weight or unfractionated heparin is suggested [56].
New oral anticoagulants
The new (or direct) oral anticoagulants [NOACs or direct oral anticoagulants (DOACs)] offer the possibility of efficacy, relative safety and convenience compared with warfarin. They have a rapid onset of action, shorter half-life and predictable pharmacokinetics and, therefore, they do not require routine coagulation monitoring. Their mechanism of action is the direct inhibition of specific proteins (factor Xa or thrombin) in the coagulation cascade (Table 2 and Fig. 1).
As with warfarin, bleeding is a complication of treatment with these new agents; however, bleeding management guidelines are based on limited evidence [57]. Considering the short half-lives of the NOACs and the severity of bleeding, cessation of treatment may be sufficient to reverse their anticoagulant effect in many instances. The decision to stop treatment depends on a patient's risk of bleeding versus their risk of thromboembolic complications. In hemodynamically stable patients, hemodialysis or hemofiltration may be considered for the reversal of the anticoagulant effect of dabigatran, as this method has been shown to remove 62–68% of the administered dose [58]. This reversal requires 4–6 h and may be considered when a patient presents with high dabigatran levels and compromised renal function. Conversely, hemodialysis cannot be used to reverse the effect of rivaroxaban or apixaban, as they are highly protein-bound. In cases of severe hemorrhage or when an emergency procedure requires immediate correction of coagulation, a major disadvantage of these new agents is the absence of an established reversal agent.
The potential of a number of nonspecific agents to reverse their anticoagulant effect has been assessed. In a porcine model of trauma, both activated and nonactivated PCCs but not rFVIIa were able to significantly reduce the anticoagulant activity of dabigatran compared with controls [59▪▪]. In further animal studies, PCC has been shown to broadly correct dabigatran-induced bleeding [60,61,62▪▪]. In addition, activated PCC (FEIBA) may be able to provide hemostatic support in situations in which dabigatran-induced coagulopathy exists [63]. Experimental studies have shown that both three-factor and four-factor PCCs reversed rivaroxaban effects on prothrombin time and endogenous thrombin potential [64]. However, there are no published clinical studies on the management of NOAC-induced bleeding. Despite this lack of clinical evidence, recent European guidelines on the management of perioperative bleeding recommend the use of activated and nonactivated PCC in cases of life-threatening bleeding or intracerebral hemorrhage [57]. A recent publication based on the ‘Dresden NOAC Registry’ data showed that of the 1776 patients receiving rivaroxaban therapy enrolled in the registry between October 2011 and December 2013, therapy with PCC was administered in only 9.1% of the major bleeding events [65].
In addition to the nonspecific agents, a number of specific antidotes are under clinical study and may become available in the near future. A recombinant factor Xa (andexanet alpha; PRT064445) has been developed to act as a universal antidote to a broad range of factor Xa inhibitors. Although andexanet alpha is catalytically inactive, it retains the ability to bind direct factor Xa inhibitors. It was shown to reverse the anticoagulant activity of both direct and indirect factor Xa inhibitors and to restore hemostasis in anticoagulated animals [66▪▪]. Similarly, a specific antidote for the reversal of the anticoagulant effect of dabigatran has been characterized [67▪▪]. This humanized antibody fragment (idarucizumab) shares structural similarities with thrombin in its mode of binding dabigatran, but is enzymatically inactive. It effectively reverses the anticoagulant effect of dabigatran in human plasma both in vitro and in vivo. In a porcine model of trauma, the ex-vivo addition of idarucizumab was shown to provide complete neutralization of supratherapeutic dabigatran concentrations and full reversal of its effect [58]. In addition, a synthetic small molecule (aripazine; PER977), which appears to have broad activity against a number of NOACs, including dabigatran, rivaroxaban and apixaban, is in development.
CONCLUSION
In the perioperative setting, coagulopathy generally occurs as a result of an injury, surgical procedure or medical anticoagulant therapy. Acquired coagulopathies are a major risk factor for progression to severe bleeding and can lead to massive blood loss and secondary complications associated with massive transfusion of allogeneic blood products, including increased mortality, morbidity, intensive care and hospital stay and costs. Therefore, early targeted intervention with hemostatic therapy may be critical to prevent development of complex coagulopathies and progression to severe, life-threatening hemorrhage. At present, there is little evidence from clinical trials to form comprehensive recommendations to treat bleeding associated or induced by the NOACs/DOACs. In particular, in cases of severe hemorrhage or when an emergency procedure requires immediate correction of coagulation, there is an absence of specific antidotes to reverse their anticoagulation effect. Specific antidotes are in development; however, further studies are required to assess these specific agents for the reversal of anticoagulation in clinical situations of bleeding.
Acknowledgements
Editorial assistance was provided by Meridian HealthComms, funded by CSL Behring.
Financial support and sponsorship
O.G. has received research funding from Novo Nordisk, Biotest, CSL Behring, Nycomed and Boehringer Ingelheim. He has also received honoraria for consultancy and/or travel support from Bayer Healthcare, Boehringer Ingelheim, CSL Behring and Portola. D.F. has received honoraria for consulting, lecture fees and sponsoring for academic studies from Astra Zeneca, AOP Orphan Baxter, Bayer, BBraun, Biotest, CSL Behring, Delta Select, Dade Behring, Edwards, Fresenius, Glaxo, Haemoscope, Hemogem, Lilly, LFB, Mitsubishi Pharma, NovoNordisk, Octapharm, Pfizer, Tem-Innovation. B.N. has received research support and speaker's honoraria from CSL Behring. We confirm that our article has not been published in its current form or a substantially similar form (in print or electronically, including on a web site), that it has not been accepted for publication elsewhere, and that it is not under consideration by another publication.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Ragni MV. The old and new: PCCs, VIIa, and long-lasting clotting factors for hemophilia and other bleeding disorders. Hematology Am Soc Hematol Educ Program 2013; 2013:44–51. [DOI] [PubMed] [Google Scholar]
- 2.Muszbek L, Yee VC, Hevessy Z. Blood coagulation factor XIII: structure and function. Thromb Res 1999; 94:271–305. [DOI] [PubMed] [Google Scholar]
- 3.Hermann M, Nussbaumer O, Knofler R, et al. Real-time live confocal fluorescence microscopy as a new tool for assessing platelet vitality. Transfus Med Hemother 2010; 37:299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solomon C, Rahe-Meyer N. In reply. Transfusion 2013; 53:1138–1140. [DOI] [PubMed] [Google Scholar]
- 5.Blome M, Isgro F, Kiessling AH, et al. Relationship between factor XIII activity, fibrinogen, haemostasis screening tests and postoperative bleeding in cardiopulmonary bypass surgery. Thromb Haemost 2005; 93:1101–1107. [DOI] [PubMed] [Google Scholar]
- 6.Charbit B, Mandelbrot L, Samain E, et al. The decrease of fibrinogen is an early predictor of the severity of postpartum hemorrhage. J Thromb Haemost 2007; 5:266–273. [DOI] [PubMed] [Google Scholar]
- 7.Karlsson M, Ternstrom L, Hyllner M, et al. Plasma fibrinogen level, bleeding, and transfusion after on-pump coronary artery bypass grafting surgery: a prospective observational study. Transfusion 2008; 48:2152–2158. [DOI] [PubMed] [Google Scholar]
- 8▪.Rahe-Meyer N, Hanke A, Schmidt DS, et al. Fibrinogen concentrate reduces intraoperative bleeding when used as first-line hemostatic therapy during major aortic replacement surgery: results from a randomized, placebo-controlled trial. J Thorac Cardiovasc Surg 2013; 145:S178–S185. [DOI] [PubMed] [Google Scholar]; The authors present findings that support the use of goal-directed, FIBTEM-guided fibrinogen concentrate as a rapid and efficacious first-line hemostatic therapy in patients with coagulopathic bleeding undergoing major aortic replacement surgery.
- 9.Rahe-Meyer N, Solomon C, Hanke A, et al. Effects of fibrinogen concentrate as first-line therapy during major aortic replacement surgery: a randomized, placebo-controlled trial. Anesthesiology 2013; 118:40–50. [DOI] [PubMed] [Google Scholar]
- 10▪.Mallaiah S, Barclay P, Harrod I, et al. Introduction of an algorithm for ROTEM-guided fibrinogen concentrate administration in major obstetric haemorrhage. Anaesthesia 2015; 70:166–175. [DOI] [PubMed] [Google Scholar]; The authors present results to show that ROTEM-guided fibrinogen concentrate allows prompt correction of coagulation deficits associated with major obstetric hemorrhage.
- 11.Spahn DR, Bouillon B, Cerny V, et al. Management of bleeding and coagulopathy following major trauma: an updated European guideline. Crit Care 2013; 17:R76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kozek-Langenecker SA, Afshari A, Albaladejo P, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol 2013; 30:270–382. [DOI] [PubMed] [Google Scholar]
- 13.Velik-Salchner C, Haas T, Innerhofer P, et al. The effect of fibrinogen concentrate on thrombocytopenia. J Thromb Haemost 2007; 5:1019–1025. [DOI] [PubMed] [Google Scholar]
- 14.Lang T, Johanning K, Metzler H, et al. The effects of fibrinogen levels on thromboelastometric variables in the presence of thrombocytopenia. Anesth Analg 2009; 108:751–758. [DOI] [PubMed] [Google Scholar]
- 15.Tanaka KA, Egan K, Szlam F, et al. Transfusion and hematologic variables after fibrinogen or platelet transfusion in valve replacement surgery: preliminary data of purified lyophilized human fibrinogen concentrate versus conventional transfusion. Transfusion 2014; 54:109–118. [DOI] [PubMed] [Google Scholar]
- 16.Silva JM, de Oliveira AM, Nogueira FA, et al. The effect of excess fluid balance on the mortality rate of surgical patients: a multicenter prospective study. Crit Care 2013; 17:R288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nisanevich V, Felsenstein I, Almogy G, et al. Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology 2005; 103:25–32. [DOI] [PubMed] [Google Scholar]
- 18.Solomon C, Hagl C, Rahe-Meyer N. Time course of haemostatic effects of fibrinogen concentrate administration in aortic surgery. Br J Anaesth 2013; 110:947–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khan S, Brohi K, Chana M, et al. Hemostatic resuscitation is neither hemostatic nor resuscitative in trauma hemorrhage. J Trauma Acute Care Surg 2014; 76:561–568. [DOI] [PubMed] [Google Scholar]
- 20.Innerhofer P, Westermann I, Tauber H, et al. The exclusive use of coagulation factor concentrates enables reversal of coagulopathy and decreases transfusion rates in patients with major blunt trauma. Injury 2013; 44:209–216. [DOI] [PubMed] [Google Scholar]
- 21▪.Collins PW, Lilley G, Bruynseels D, et al. Fibrin-based clot formation an early and rapidly available biomarker for progression of postpartum hemorrhage: a prospective cohort study. Blood 2014; 124:1727–1736. [DOI] [PubMed] [Google Scholar]; The authors present findings to show that fibrin-based clot formation is an early and rapidly available biomarker for progression of postpartum hemorrhage.
- 22.Ferraris VA, Ferraris SP, et al. Society of Thoracic Surgeons Blood Conservation Guideline Task Force,. Perioperative blood transfusion and blood conservation in cardiac surgery: the Society of Thoracic Surgeons and The Society of Cardiovascular Anesthesiologists clinical practice guideline. Ann Thorac Surg 2007; 83:S27–86. [DOI] [PubMed] [Google Scholar]
- 23.Besser MW, Klein AA. The coagulopathy of cardiopulmonary bypass. Crit Rev Clin Lab Sci 2010; 47:197–212. [DOI] [PubMed] [Google Scholar]
- 24.Solomon C, Pichlmaier U, Schoechl H, et al. Recovery of fibrinogen after administration of fibrinogen concentrate to patients with severe bleeding after cardiopulmonary bypass surgery. Br J Anaesth 2010; 104:555–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coakley M, Hall JE, Evans C, et al. Assessment of thrombin generation measured before and after cardiopulmonary bypass surgery and its association with postoperative bleeding. J Thromb Haemost 2011; 9:282–292. [DOI] [PubMed] [Google Scholar]
- 26.Bosch YP, Al Dieri R, ten Cate H, et al. Measurement of thrombin generation intra-operatively and its association with bleeding tendency after cardiac surgery. Thromb Res 2014; 133:488–494. [DOI] [PubMed] [Google Scholar]
- 27.Solomon C, Rahe-Meyer N, Sorensen B. Fibrin formation is more impaired than thrombin generation and platelets immediately following cardiac surgery. Thromb Res 2011; 128:277–282. [DOI] [PubMed] [Google Scholar]
- 28.Floccard B, Rugeri L, Faure A, et al. Early coagulopathy in trauma patients: an on-scene and hospital admission study. Injury 2012; 43:26–32. [DOI] [PubMed] [Google Scholar]
- 29.Rugeri L, Levrat A, David JS, et al. Diagnosis of early coagulation abnormalities in trauma patients by rotation thrombelastography. J Thromb Haemost 2007; 5:289–295. [DOI] [PubMed] [Google Scholar]
- 30.Maegele M, Lefering R, Yucel N, et al. Early coagulopathy in multiple injury: an analysis from the German Trauma Registry on 8724 patients. Injury 2007; 38:298–304. [DOI] [PubMed] [Google Scholar]
- 31.Frith D, Goslings JC, Gaarder C, et al. Definition and drivers of acute traumatic coagulopathy: clinical and experimental investigations. J Thromb Haemost 2010; 8:1919–1925. [DOI] [PubMed] [Google Scholar]
- 32.Brohi K, Cohen MJ, Davenport RA. Acute coagulopathy of trauma: mechanism, identification and effect. Curr Opin Crit Care 2007; 13:680–685. [DOI] [PubMed] [Google Scholar]
- 33.Schöchl H, Cotton B, Inaba K, et al. FIBTEM provides early prediction of massive transfusion in trauma. Crit Care 2011; 15:R265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meyer AS, Meyer MA, Sorensen AM, et al. Thrombelastography and rotational thromboelastometry early amplitudes in 182 trauma patients with clinical suspicion of severe injury. J Trauma Acute Care Surg 2014; 76:682–690. [DOI] [PubMed] [Google Scholar]
- 35.Rourke C, Curry N, Khan S, et al. Fibrinogen levels during trauma hemorrhage, response to replacement therapy, and association with patient outcomes. J Thromb Haemost 2012; 10:1342–1351. [DOI] [PubMed] [Google Scholar]
- 36.Frith D, Davenport R, Brohi K. Acute traumatic coagulopathy. Curr Opin Anaesthesiol 2012; 25:229–234. [DOI] [PubMed] [Google Scholar]
- 37.Davenport R, Brohi K. Fibrinogen depletion in trauma: early, easy to estimate and central to trauma-induced coagulopathy. Crit Care 2013; 17:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prisco D, Ciuti G, Falciani M. Hemostatic changes during normal pregnancy. Haematologica Reports 2005; 1:1–5. [Google Scholar]
- 39.Saha P, Stott D, Atalla R. Haemostatic changes in the puerperium ‘6 weeks postpartum’ (HIP Study) - implication for maternal thromboembolism. BJOG 2009; 116:1602–1612. [DOI] [PubMed] [Google Scholar]
- 40.WHO Guidelines for the Management of Postpartum Haemorrhage and Retained Placenta Geneva, 2009. http://whqlibdoc.who.int/publications/2009/9789241598514_eng.pdf [Accessed 17 October 2014]. [PubMed] [Google Scholar]
- 41.Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control study. BMJ 2001; 322:1089–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Solomon C, Collis RE, Collins PW. Haemostatic monitoring during postpartum haemorrhage and implications for management. Br J Anaesth 2012; 109:851–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Lloyd L, Bovington R, Kaye A, et al. Standard haemostatic tests following major obstetric haemorrhage. Int J Obstet Anesth 2011; 20:135–141. [DOI] [PubMed] [Google Scholar]
- 44.Bell SF, Rayment R, Collins PW, Collis RE. The use of fibrinogen concentrate to correct hypofibrinogenaemia rapidly during obstetric haemorrhage. Int J Obstet Anesth 2010; 19:218–223. [DOI] [PubMed] [Google Scholar]
- 45.Windecker S, Kolh P, Alfonso F, et al. ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014; 35:2541–2619. [DOI] [PubMed] [Google Scholar]
- 46.Bertrand ME. When and how to discontinue antiplatelet therapy. Eur Heart J Suppl 2008; 10:A35–A41. [Google Scholar]
- 47.McQuaid KR, Laine L. Systematic review and meta-analysis of adverse events of low-dose aspirin and clopidogrel in randomized controlled trials. Am J Med 2006; 119:624–638. [DOI] [PubMed] [Google Scholar]
- 48.Hung A, Singh S, Tait RC. A prospective randomized study to determine the optimal dose of intravenous vitamin K in reversal of over-warfarinization. Br J Haematol 2000; 109:537–539. [DOI] [PubMed] [Google Scholar]
- 49.Watson HG, Baglin T, Laidlaw SL, et al. A comparison of the efficacy and rate of response to oral and intravenous Vitamin K in reversal of over-anticoagulation with warfarin. Br J Haematol 2001; 115:145–149. [DOI] [PubMed] [Google Scholar]
- 50.Baglin TP, Keeling DM, Watson HG. British Committee for Standards in Haematology Guidelines on oral anticoagulation (warfarin): third edition – 2005 update. Br J Haematol 2006; 132:277–285. [DOI] [PubMed] [Google Scholar]
- 51▪.Hickey M, Gatien M, Taljaard M, et al. Outcomes of urgent warfarin reversal with frozen plasma versus prothrombin complex concentrate in the emergency department. Circulation 2013; 128:360–364. [DOI] [PubMed] [Google Scholar]; The authors show that four-factor PCC for the emergency reversal of warfarin was faster and associated with fewer adverse events than fresh frozen plasma.
- 52▪.Sarode R, Milling TJ, Jr, Refaai MA, et al. Efficacy and safety of a 4-factor prothrombin complex concentrate in patients on vitamin K antagonists presenting with major bleeding: a randomized, plasma-controlled, phase IIIb study. Circulation 2013; 128:1234–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors present findings to show that 4-factor PCC is an effective alternative to plasma for the urgent reversal of vitamin K antagonists in major bleeding events.
- 53.Guyatt GH, Akl EA, Crowther M, et al. Executive summary: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141:7S–47S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yasaka M, Sakata T, Minematsu K, Naritomi H. Correction of INR by prothrombin complex concentrate and vitamin K in patients with warfarin related hemorrhagic complication. Thromb Res 2002; 108:25–30. [DOI] [PubMed] [Google Scholar]
- 55.Tran HA, Chunilal SD, Harper PL, et al. An update of consensus guidelines for warfarin reversal. Med J Aust 2013; 198:198–199. [DOI] [PubMed] [Google Scholar]
- 56.Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed.: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141:e326S–350S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Heidbuchel H, Verhamme P, Alings M, et al. European Heart Rhythm Association Practical Guide on the use of new oral anticoagulants in patients with nonvalvular atrial fibrillation. Europace 2013; 15:625–651. [DOI] [PubMed] [Google Scholar]
- 58.Stangier J, Rathgen K, Stahle H, Mazur D. Influence of renal impairment on the pharmacokinetics and pharmacodynamics of oral dabigatran etexilate: an open-label, parallel-group, single-centre study. Clin Pharmacokinet 2010; 49:259–268. [DOI] [PubMed] [Google Scholar]
- 59▪▪.Grottke O, van Ryn J, Spronk HM, Rossaint R. Prothrombin complex concentrates and a specific antidote to dabigatran are effective ex-vivo in reversing the effects of dabigatran in an anticoagulation/liver trauma experimental model. Crit Care 2014; 18:R27. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is the first experimental animal trial to show in vitro that PCC, activated PCC and the specific antidote aDabi-Fab are effective for the reversal of coagulopathy induced by the new oral anticoagulant dabigatran.
- 60.Zhou W, Schwarting S, Illanes S, et al. Hemostatic therapy in experimental intracerebral hemorrhage associated with the direct thrombin inhibitor dabigatran. Stroke 2011; 42:3594–3599. [DOI] [PubMed] [Google Scholar]
- 61.Pragst I, Zeitler SH, Doerr B, et al. Reversal of dabigatran anticoagulation by prothrombin complex concentrate (Beriplex P/N) in a rabbit model. J Thromb Haemost 2012; 10:1841–1848. [DOI] [PubMed] [Google Scholar]
- 62▪▪.Herzog E, Kaspereit FJ, Krege W, et al. Thrombotic safety of prothrombin complex concentrate (Beriplex P/N) for dabigatran reversal in a rabbit model. Thromb Res 2014; 134:729–736. [DOI] [PubMed] [Google Scholar]; The authors present findings from a rabbit model study to confirm that PCC can reverse dabigatran overdose. In addition, they show that thrombosis after the administration of PCC could be prevented in the presence of dabigatran.
- 63.Khoo TL, Weatherburn C, Kershaw G, et al. The use of FEIBA in the correction of coagulation abnormalities induced by dabigatran. Int J Lab Hematol 2013; 35:222–224. [DOI] [PubMed] [Google Scholar]
- 64.Levi M, Moore KT, Castillejos CF, et al. Comparison of three-factor and four-factor prothrombin complex concentrates regarding reversal of the anticoagulant effects of rivaroxaban in healthy volunteers. J Thromb Haemost 2014; 12:1428–1436. [DOI] [PubMed] [Google Scholar]
- 65.Beyer-Westendorf J, Forster K, Pannach S, et al. Rates, management, and outcome of rivaroxaban bleeding in daily care: results from the Dresden NOAC registry. Blood 2014; 124:955–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66▪▪.Lu G, DeGuzman FR, Hollenbach SJ, et al. A specific antidote for reversal of anticoagulation by direct and indirect inhibitors of coagulation factor Xa. Nat Med 2013; 19:446–451. [DOI] [PubMed] [Google Scholar]; The authors present proof-of-concept results showing the potential of a universal antidote to reverse the anticoagulant effects of a broad range of factor Xa inhibitors.
- 67▪▪.Schiele F, van Ryn J, Canada K, et al. A specific antidote for dabigatran: functional and structural characterization. Blood 2013; 121:3554–3562. [DOI] [PubMed] [Google Scholar]; The authors present the characterization of an antidote that effectively reverses the anticoagulant effect of dabigatran in human plasma and in vivo in rats.


