Abstract
Background
Plication is an alternative tightening procedure to resection. In monkeys, plication has been shown to preserve anterior segment circulation compared with full-tendon tenotomy, but this is unconfirmed in humans.
Purpose
To evaluate anterior segment circulation by iris angiography before and after strabismus surgery in humans.
Methods
Prospective, blinded study of 14 patients (mean age (SD), 58.6 (14.3)) undergoing plication and/ or full tendon tenotomy (resection or recession) from August 2013 to March 2014. Eight patients (mean age (SD), 59.0 (13.3)) underwent plication of one muscle with or without recession of a second muscle on the same eye and six patients (mean age (SD), 58.2 (16.8)) underwent tenotomy of one to two muscles on the same eye. Preoperative and postoperative iris angiograms were compared for changes in perfusion by a masked examiner. In patients undergoing binocular surgery, one eye was chosen preoperatively to be the study eye.
Results
Postoperative iris filling defects were present in four patients (67%) after tenotomy and one patient (12.5%) after plication (p=0.09). Of the seven total vertical rectus muscles operated (three tenotomies and four plications), filling defects were present after three tenotomies and one plication (100% vs 25%; p=0.14). Of the 13 total horizontal rectus muscles operated (eight tenotomies and five plications), filling defects were present after one tenotomy and none of the plications (13% vs 0%; p=0.99).
Conclusions
Rectus muscle plication spares the ciliary vessels and may be considered a safer alternative to resection for patients at risk for anterior segment ischaemia, especially when surgery involves a vertical rectus muscle.
INTRODUCTION
Anterior segment ischaemia (ASI) is a rare but potentially serious complication of strabismus surgery. While ASI is more common after disinsertion of three or four rectus muscles,1,2 it has also been reported in surgeries involving only two rectus muscles.3–5 Risk factors for ASI include older age, atherosclerosis, previous strabismus or retinal detachment surgery, haematological disorders that increase blood viscosity, thyroid ophthalmopathy and limbal conjunctival incision.6
Plication is a tightening procedure in which the muscle is not disinserted from the globe but, rather, folded and sutured to the sclera at the muscle insertion.7 Plication has been shown to have a similar surgical effect per millimetre as resection for treatment of esotropia and exotropia.8
Advantages of plication include absence of risk of lost muscle, reversibility in the early postoperative period and potentially less disruption of the anterior ciliary arteries (ACA).9 Interest in muscle plication is increasing for these reasons, especially among those using minimally invasive techniques and topical anaesthesia.9,10 However, it is not known whether the blood supply is truly preserved compared with traditional rectus muscle resections.
Iris angiography in monkeys has shown that plication spares anterior segment circulation,11,12 but this is unconfirmed in humans. This study employed anterior segment iris angiography in patients to evaluate changes in anterior segment circulation after rectus muscle plication compared with traditional techniques requiring full tendon tenotomy (recession and resection).
METHODS
This study was approved by the University of California, Los Angeles institutional review board, and conformed to the requirements of the US Health Insurance Portability and Accountability Act. Informed consent was received from participants. Patients over the age of 18 years scheduled to undergo strabismus surgery (rectus muscle resection, recession or plication) were recruited from the clinics of two of the authors ( JLD and FGV) during preoperative visits. Surgical techniques were chosen based upon clinical factors and surgeon preference. Data were collected relating to age, sex, history of prior ocular surgery and comorbid conditions. When binocular surgery was performed, one eye was chosen preoperatively as the study eye.
Patients were analysed as a tenotomy group, which included full tendon recessions and resections, and a plication group, which included patients having plications only as well as combined plication/recession (plication of one muscle and recession of a second muscle) on the same eye. Surgery technique was standardised for resection, recession and plication among the surgeons, with the only difference being conjunctival incision type (paralimbal or fornix). Our technique for rectus muscle plication has been previously described.8,13 Briefly, the muscle is hooked and connective tissue bluntly dissected posteriorly. Two single-armed 6–0 polyglactin 910 sutures are passed in a locking fashion through about 15% of each muscle margin at the desired plication distance from the insertion as measured by callipers. The sutures are then passed partial thickness through the sclera at corresponding poles of the muscle insertion. An iris spatula is then placed between the tendon and the sutures forming a fulcrum over which the anterior tendon is folded flat between the muscle and the globe. If an adjustable technique is used, the suture ends are tied in a slipknot.
All patients underwent a preoperative iris angiogram a maximum of 1 month prior to surgery, followed by a postoperative angiogram within 1 day of surgery. Pilocarpine 1% was instilled into the study eye 15 min prior to angiography. Patients with light irides had fluorescein angiograms and patients with dark irides had indocyanine green (ICG) angiograms because ICG better detects perfusion changes in darker pigmented irides.14 Trained ophthalmic photographers employed the Heidelberg Spectralis (Heidelberg Engineering, Heidelberg, Germany) camera to obtain anterior segment angiography after intravenous administration at 1 mL/s of ICG (4 mL at 12.5 mg/mL) or fluorescein (5 mL at 100 mg/mL). A 1 min video was taken after dye injection (see online supplementary video 1). Still images were then obtained at 15 s –30 s intervals over the following 4 min. Iris angiograms were analysed for filling delay or defects by one of the authors (SLP) who was unaware of the surgical procedure performed.
RESULTS
A total of 14 patients were recruited (age 58.6±14.3 years, 7 women) who underwent surgery on a total of 20 muscles. Six patients had only tenotomy (resection or recession): two lateral rectus (LR), two superior rectus (SR), one combined inferior rectus (IR) and LR, one combined medial rectus (MR) and LR. Five patients had only plications: two IR, two LR, one combined IR/LR. Three patients had combined plication of one muscle and recession of a second muscle on the same eye: two MR/LR and one IR/LR. The individual patient characteristics are presented in table 1. Plication amounts were 4–4.5 mm for the LR, 5 mm for the MR and 2.5–7 mm for the IR. All patients were operated under general anaesthesia.
Table 1.
Individual patient characteristics
| Patient number | Age | Sex | Surgery performed | Prior ocular surgery | Vascular risk factors | Incision type | Postoperative perfusion defect | |
|---|---|---|---|---|---|---|---|---|
| Plication Group | 1 | 31 | F | LR and IR plication | MR recession, SR recession | None | Fornix | None |
| 2 | 48 | M | IR plication | LR recession, MR resection, vitrectomy, scleral buckle | HCL | Fornix | None | |
| 3 | 62 | F | LR plicication | None | Rheumatoid Arthritis | Para-limbal | None | |
| 4 | 70 | M | IR plication, SO tenectomy | LR and SR recession, MR resection | None | Para-limbal | None | |
| 5 | 66 | M | LR plication | MR recession | HTN, HCL | Para-limbal | None | |
| 6 | 60 | M | MR plication, LR recession | Radioactive plaque | HTN, pre-DM | Para-limbal | None | |
| 7 | 68 | F | MR plication, LR recession | none | HCL, ischaemic stroke | Para-limbal | None | |
| 8 | 67 | M | IR plication, LR recession | MR recession, LR resection | HTN, DM, tobacco use | Para-limbal | IR defect | |
| Tenotomy Group | 9 | 69 | F | LR resection | none | HTN | Para-limbal | None |
| 10 | 36 | F | LR recession | Previous strabismus surgeries (muscles not known) | None | Para-limbal | LR defect | |
| 11 | 59 | F | IR recession, LR resection | Vitrectomy, trabeculectomy | HCL | Fornix | IR defect | |
| 12 | 78 | M | SR recession | IO recession | HTN | Para-limbal | SR defect | |
| 13 | 40 | M | LR recession, MR resection | MR recession | None | Fornix | None | |
| 14 | 67 | F | SR recession | 50% RIR tenotomy | None | Para-limbal | SR defect |
DM, diabetes mellitus; HCL, hypercholesterolaemia; HTN, hypertension; IO, inferior oblique; IR, inferior rectus; LR, lateral rectus; MR, medial rectus; RIR, right inferior rectus; SO, superior oblique; SR, superior rectus.
The plication and tenotomy groups had similar age, sex, history of prior ocular surgery, vascular risk factors and conjunctival incision type. Past ocular surgeries that were considered significant were those with potential to alter anterior segment circulation and included vitrectomy, radioactive plaque placement, trabeculectomy and prior rectus muscle surgery. A history of prior clear corneal incision cataract surgery or isolated oblique muscle surgery was not considered significant. Vascular risk factors included hypertension, hypercholesterolaemia, diabetes and rheumatoid arthritis. Preoperative angiograms demonstrated no evidence of iris-filling defects or delays.
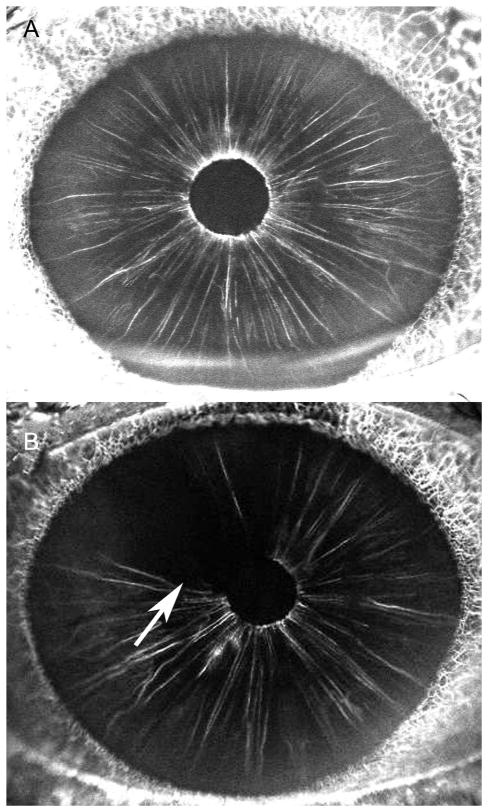
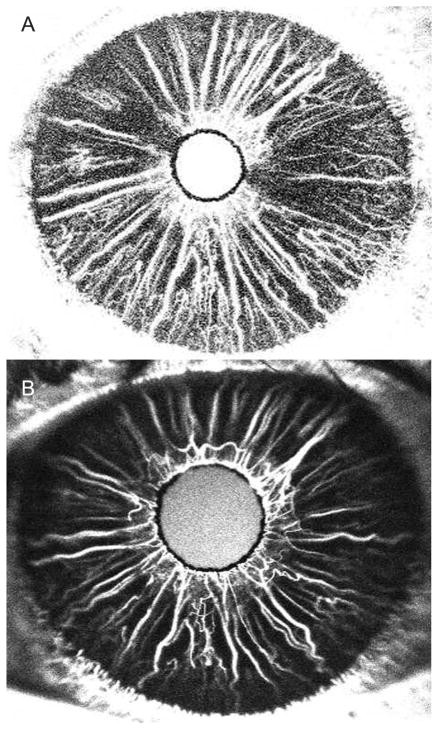
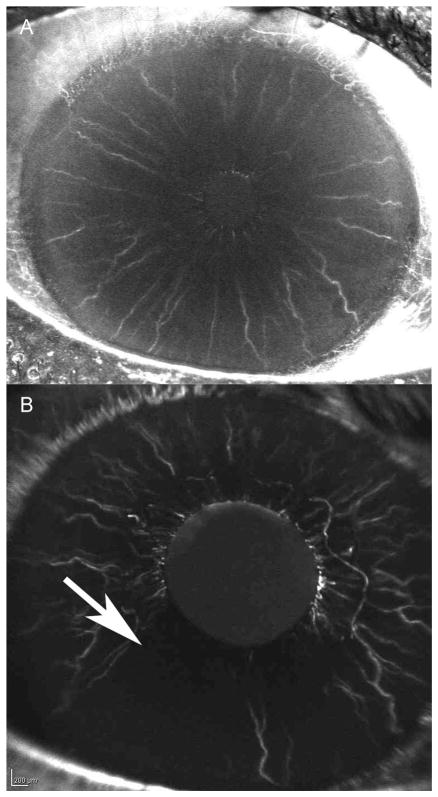
There were postoperative iris-filling defects in four of six patients in the tenotomy-only group, and in one of eight patients in the plication group (p=0.09, Fisher Exact test, table 2). Figure 1 for Patient 14 shows a normal preoperative iris angiogram, but a filling defect in the distribution of the SR following SR recession. Figure 2 shows Patient 4 who had normal iris perfusion following IR plication. The single patient (Patient 8) in the plication group with a filling defect had an IR plication and LR recession with no obvious damage to the ciliary vessels observed during surgery (figure 3).
Table 2.
Postoperative iris angiography results
| Filling defect (%) | p Value | |
|---|---|---|
| By patient | ||
| Plication (n=8) | 1 (12.5) | 0.09* |
| Recess/resect (n=6) | 4 (67) | |
| By muscle | ||
| Vertical plication (n=4) | 1 (25) | 0.14* |
| Vertical recess/resect (n=3) | 3 (100) | |
| Horizontal plication (n=5) | 0 | 0.99* |
| Horizontal recess/resect (n=8) | 1 (13) | |
Fisher Exact Test.
Figure 1.
Patient 14, superior rectus recession. (A) Preoperative iris angiogram at 45 s showing a normal perfusion. (B) Postoperative iris angiogram at 37 s showing a filling defect superiorly (arrow).
Figure 2.
Patient 4, inferior rectus plication. (A) Preoperative iris angiogram at 37 s showing normal perfusion. (B) Postoperative iris angiogram at 35 s. No filling defect after inferior rectus plication.
Figure 3.
Patient 8, inferior rectus plication and lateral rectus recession, right eye. (A) Preoperative iris angiogram at 35 s showing a normal perfusion. (B) Postoperative iris angiogram at 44 s showing a filling defect inferiorly (arrow).
There were 20 individual muscles operated, including three vertical tenotomies, four vertical plications, eight horizontal tenotomies and five horizontal rectus plications. There were filling defects in the distribution of all three vertical tenotomies and in one of the four vertical plications (p=0.14, Fisher Exact test). There were filling defects in distribution of one of the eight horizontal tenotomies and in none of the horizontal plications (p=0.99, Fisher Exact test, table 2). The single patient (Patient 10) with a filling defect after horizontal tenotomy was a 36-year-old woman with a history of prior strabismus surgery (unknown muscle combinations) who had an isolated LR recession.
There were no significant differences in age, sex, history of prior ocular surgery, vascular risk factors or conjunctival incision between the patients with filling defects and those without filling defects. No patients showed postoperative flare, corneal oedema, iridoplegia or hypotony that would have been interpreted as clinical signs of ASI.
DISCUSSION
To the best knowledge of the authors, this study is the first to confirm preservation of anterior segment circulation after rectus plication in humans. Similar to prior iris angiography studies after strabismus surgery, we found more postoperative iris-filling defects after vertical rectus than horizontal rectus tenotomy, emphasising the important role of the two long posterior ciliary arteries (LPCA) that run in the horizontal midline. There were postoperative iris-filling defects after all vertical rectus muscle tenotomies and only one after vertical rectus plication. The patient in the plication group (Patient 8) who showed a postoperative iris-filling defect adjacent to the plicated IR also had LR recession (figure 3). The surgery was uneventful and there was no obvious damage to the ciliary vessels during the plication. This filling defect might have been from unobserved damage to the ciliary vessels during either muscle suturing or folding, or possibly in combination with the adjacent LR tenotomy.
Postoperative iris-filling defects were rare after horizontal tenotomy with only one patient having a filling defect after LR recession (Patient 10). This patient was a 36-year-old woman with no vascular risk factors but with a history of prior strabismus surgeries who underwent isolated LR muscle recession. This highlights the fact that while blood flow changes after horizontal rectus muscle tenotomy are uncommon, they may occur.
While ASI is a rare complication of strabismus surgery, its significant consequences force surgeons to be cautious when operating on several rectus muscles or in patients with vascular risk factors. Reported complications range from mild, self-limited iritis to severe ischaemic changes, such as iris atrophy, keratopathy, posterior synechiae, cataract and even phthisis bulbi.6
Anterior segment perfusion comes from a combination of the ACA and the LPCAs. The ACAs run along the rectus muscles and have been estimated to provide 70%–80% of the blood supply to the anterior segment.15 The two LPCAs supply the remainder of the anterior segment blood supply and have an intrascleral course beneath the medial and LR muscles.16 Careful surgical dissection of the ACAs during muscle surgery has been shown to preserve anterior segment circulation.17
The first in vivo study of anterior segment circulation in human subjects, after strabismus surgery, was done by Hayreh and Scott in 1978.16 Using fluorescein angiography, they investigated the effect on anterior segment circulation after tenotomy of one or more rectus muscles and found no changes in iris perfusion with tenotomy of the horizontal rectus muscles, but significant changes after vertical rectus surgery. The authors hypothesised that their results were due to absence of superior or inferior LPCAs.
Similar results were found by Chan et al14 by ICG angiography after strabismus surgery in 45 patients. There was a 57% prevalence of immediate postoperative filling defects after primary vertical or combined vertical/horizontal muscle surgery, but no filling defects after horizontal surgery. Other studies also confirmed the increased incidence of ischaemia after vertical rectus surgery.1,18,19 In rabbits, Bagheri et al2 found no composition of rectus muscle surgeries that increased risk of ASI in the two-muscle group, though all two-muscle cases with ASI involved surgery on adjacent muscles. Iris angiography was not used in this study to look for subclinical changes in anterior segment circulation.
It is evident from prior studies that both patient susceptibility as well as the combination and total number of muscles disinserted from the globe are major variables in the incidence of ASI.2,6 Conjunctival incision location may also be a variable with higher rates of ischaemia seen after limbal incision compared with fornix incision in an animal model.20 Our study did not reveal a significant increase in postoperative perfusion defects after limbal incision compared with fornix incision, though it was not powered to study this relationship.
This study is limited by its relatively small sample size and that it does not include all possible combinations of muscle surgery. Another limitation is that the study examined only the immediate effects of surgery on anterior segment circulation. There is a theoretical question, that changes to blood flow may arise later when folded muscles begin to scar. This question was addressed in a monkey study by Park et al11 that showed no hypoperfusion in the distribution of plicated muscles on serial angiograms up to 16 weeks postoperatively. Future studies could include serial iris angiograms after plication to detect possible late perfusion changes. However, late clinical evidence of ASI has not been reported.
In conclusion, rectus muscle plication preserves anterior segment circulation. This procedure may be considered a safer alternative to resection in patients at risk for ASI.
Supplementary Material
Acknowledgments
Funding NIH/NEI K23EY021762 (SLP), Knights Templar Eye Foundation (SLP), Oppenheimer Family Foundation (SLP), Research to Prevent Blindness unrestricted grant (FGV).
Footnotes
Competing interests None.
Ethics approval UCLA Institutional Review Board.
Provenance and peer review Not commissioned; externally peer reviewed.
Contributors EZO, SLP and FGV contributed to the study concept and design. Acquisition of the data was performed by SLP, JLD and FGV and data analysis was performed by EZO and AVQ. The manuscript was drafted by EZO and critical revisions were performed by SLP, JLD and FGV. Funding was obtained by SLP and FGV.
References
- 1.Saunders RA, Phillips MS. Anterior segment ischemia after three rectus muscle surgery. Ophthalmology. 1988;95:533–7. doi: 10.1016/s0161-6420(88)33154-4. [DOI] [PubMed] [Google Scholar]
- 2.Bagheri A, Tavakoli M, Torbati P, et al. Natural course of anterior segment ischemia after disinsertion of extraocular rectus muscles in an animal model. J AAPOS. 2013;17:395–401. doi: 10.1016/j.jaapos.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Jacobs DS, Vastine DW, Urist MJ. Anterior segment ischemia and sector iris atrophy: after strabismus surgery in a patient with chronic lymphocytic leukemia. Ophthalmic Surg. 1976;7:42–8. [PubMed] [Google Scholar]
- 4.Raizman M, Beck RW. Iris ischemia following surgery on two rectus muscles (letter) Arch Ophthalmol. 1985;103:1783–7. doi: 10.1001/archopht.1985.01050120013005. [DOI] [PubMed] [Google Scholar]
- 5.Simon JW, Grajny A. Anterior segment ischemia following augmented 2-muscle transposition surgery. J AAPOS. 2004;8:586–7. doi: 10.1016/j.jaapos.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 6.Saunders RA, Bluestein EC, Wilson E, et al. Anterior segment ischemia after strabismus surgery. Surv Ophthalmol. 1994;38:456–66. doi: 10.1016/0039-6257(94)90175-9. [DOI] [PubMed] [Google Scholar]
- 7.Wright KW. Color atlas of strabismus surgery. 3. New York: Springer; 2007. pp. 149–52. [Google Scholar]
- 8.Chaudhuri Z, Demer JL. Surgical outcomes following rectus muscle plication. JAMA Ophthalmol. 2014;132:579–85. doi: 10.1001/jamaophthalmol.2013.8188. [DOI] [PubMed] [Google Scholar]
- 9.Leenheer RS, Wright KW. Miniplication to treat small-angle strabismus: a minimally invasive procedure. J AAPOS. 2012;16:327–30. doi: 10.1016/j.jaapos.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Mojon DS. A modified technique for rectus muscle plication in minimally invasive strabismus surgery. Ophthalmologica. 2010;224:236–42. doi: 10.1159/000260230. [DOI] [PubMed] [Google Scholar]
- 11.Park C, Min BM, Wright KW. Effect of a modified rectus tuck on anterior ciliary artery perfusion. Korean J Ophthalmol. 1991;5:15–25. doi: 10.3341/kjo.1991.5.1.15. [DOI] [PubMed] [Google Scholar]
- 12.Wright KW, Lanier AB. Effect of a modified rectus tuck on anterior segment circulation in monkeys. J Pediatr Ophthalmol Strabismus. 1991;28:77–81. doi: 10.3928/0191-3913-19910301-06. [DOI] [PubMed] [Google Scholar]
- 13.Velez FG, Demer JL, Pihlblad MS, et al. Rectus muscle plication using an adjustable suture technique. J AAPOS. 2013;17:480–3. doi: 10.1016/j.jaapos.2013.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan TK, Rosenbaum AL, Rao R, et al. Indocyanine green angiography of the anterior segment in patients undergoing strabismus surgery. Br J Ophthalmol. 2001;86:214–18. doi: 10.1136/bjo.85.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilcox LM, Keough EM, Connally RJ, et al. The contribution of blood flow by the anterior ciliary arteries to the anterior segment in the primate eye. Exp Eye Res. 1980;30:167–74. doi: 10.1016/0014-4835(80)90110-4. [DOI] [PubMed] [Google Scholar]
- 16.Hayreh SS, Scott WE. Flourescein Iris Angiography. II. Disturbances in iris circulation following strabismus operation on the various recti. Arch Ophthalmol. 1978;96:1390–400. doi: 10.1001/archopht.1978.03910060144010. [DOI] [PubMed] [Google Scholar]
- 17.McKeown CA, Lambert HM, Shore JW. Preservation of the anterior ciliary vessels during extraocular muscle surgery. Ophthalmology. 1989;96:498–506. doi: 10.1016/s0161-6420(89)32867-3. [DOI] [PubMed] [Google Scholar]
- 18.Virdi PS, Hayreh SS. Anteiror segment ischemia after recession of various recti. An experimental study. Ophthalmology. 1987;94:1258–71. doi: 10.1016/s0161-6420(87)80009-x. [DOI] [PubMed] [Google Scholar]
- 19.Olver JM, Lee JP. Recovery of anterior segment circulation after strabismus surgery in adult patients. Ophthalmology. 1992;99:305–15. doi: 10.1016/s0161-6420(92)31971-2. [DOI] [PubMed] [Google Scholar]
- 20.Fishman PH, Repka MX, Green R, et al. A primate model of anterior segment ischemia after strabismus surgery. The role of conjunctival circulation. Ophthalmology. 1990;97:456–61. doi: 10.1016/s0161-6420(90)32561-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.