Abstract
Background
Abiraterone acetate (an androgen biosynthesis inhibitor) plus prednisone is approved for treating patients with metastatic castration-resistant prostate cancer (mCRPC). Study COU-AA-302 evaluated abiraterone acetate plus prednisone versus prednisone alone in mildly symptomatic or asymptomatic patients with progressive mCRPC without prior chemotherapy.
Objective
Report the prespecified third interim analysis (IA) of efficacy and safety outcomes in study COU-AA-302.
Design, setting, and participants
Study COU-AA-302, a double-blind placebo-controlled study, enrolled patients with mCRPC from April 2009 to June 2010. A total of 1088 patients were stratified by Eastern Cooperative Oncology Group performance status (0 vs 1).
Intervention
Patients were randomised 1:1 to abiraterone 1000 mg plus prednisone 5 mg twice daily by mouth versus prednisone.
Outcome measurements and statistical analysis
Co–primary end points were radiographic progression-free survival (rPFS) and overall survival (OS). Median times to event outcomes were estimated using the Kaplan-Meier method. Hazard ratios (HRs) and 95% confidence intervals (CIs) were derived using the Cox model, and treatment comparison used the log-rank test. The O’Brien-Fleming Lan-DeMets α-spending function was used for OS. Adverse events were summarised descriptively.
Results and limitations
With a median follow-up duration of 27.1 mo, improvement in rPFS was statistically significant with abiraterone treatment versus prednisone (median: 16.5 vs 8.2 mo; HR: 0.52 [95% CI, 0.45–0.61]; p < 0.0001). Abiraterone improved OS (median: 35.3 vs 30.1 mo; HR: 0.79 [95% CI, 0.66–0.95]; p = 0.0151) but did not reach the prespecified statistical efficacy boundary (α-level: 0.0035). A post hoc multivariate analysis for OS using known prognostic factors supported the primary results (HR: 0.74 [95% CI, 0.61–0.89]; p = 0.0017), and all clinically relevant secondary end points and patient-reported outcomes improved. While the post hoc nature of the long-term safety analysis is a limitation, the safety profile with longer treatment exposure was consistent with prior reports.
Conclusions
The updated IA of study COU-AA-302 in patients with mCRPC without prior chemotherapy confirms that abiraterone delays disease progression, pain, and functional deterioration and has clinical benefit with a favourable safety profile, including in patients treated for ≥24 mo.
Trial registration
Study COU-AA-302, ClinicalTrials.gov number, NCT00887198.
Keywords: Abiraterone acetate, Chemotherapy-naive, Efficacy, Metastatic castration-resistant prostate cancer, Safety
1. Introduction
Androgen deprivation therapy is the standard of care for advanced prostate cancer (PCa), but patients invariably progress to castration-resistant disease despite castration levels of serum testosterone (<50 ng/dl) [1,2]. Metastatic castration-resistant PCa (mCRPC) represents the lethal form of the disease, with, until recently, limited treatment options and a median survival of <2 yr [3]. Chemotherapy provides an overall survival (OS) benefit for patients with mCRPC [4–7], but newer treatments with fewer side-effects are now available that may be preferable options before chemotherapy. Building on an increased understanding of the continued relevance of the androgen receptor signalling pathway in mCRPC, targeting residual androgen production offers great promise as a well-tolerated and effective alternative to standard cytotoxic therapies [8–10]. Abiraterone acetate is the prodrug of abiraterone, a specific inhibitor of CYP17 that blocks extragonadal, testicular, and tumour androgen biosynthesis [9,11,12]. In patients with mCRPC who had received prior docetaxel chemotherapy, abiraterone acetate (henceforth abiraterone) plus low-dose prednisone improved median OS by 4.6 mo (hazard ratio [HR]: 0.74; 95% confidence interval [CI], 0.64–0.86; p < 0.0001) compared with placebo plus prednisone (henceforth prednisone) [13,14].
Study COU-AA-302 is evaluating the clinical benefit of abiraterone plus prednisone versus prednisone in mildly symptomatic or asymptomatic patients with progressive mCRPC without prior chemotherapy [15]. Based on a preplanned interim analysis (IA) [15], the independent data-monitoring committee reviewed the masked efficacy and safety outcomes and recommended that the study be unblinded and patients be allowed to cross over from the prednisone group to receive abiraterone. Subsequently, in December 2012, abiraterone therapy received expanded regulatory approval in the United States and Europe [16] to also treat patients with mCRPC prior to receiving chemotherapy. We report the results of the third IA (IA3), preplanned at 55% OS events (425 of 773), for study COU-AA-302 and provide an update of efficacy and long-term safety outcomes.
2. Patients and methods
COU-AA-302 (NCT00887198) is a phase 3, multinational, randomised, double-blind, placebo-controlled study being conducted at 151 sites in 12 countries. Patients were enrolled from April 2009 to June 2010; the study is ongoing. The review boards at all participating institutions approved the study, which was conducted according to the Declaration of Helsinki, the International Conference on Harmonisation, and the Guidelines for Good Clinical Practice. All patients gave written informed consent.
2.1. Patient population
The study design and primary and secondary efficacy end points have been previously described in detail for the second IA (IA2) [15] and are summarised in this paper. The study included male patients aged ≥18 yr with chemotherapy-naive mCRPC, who were medically or surgically castrated, had tumour progression, and were asymptomatic or mildly symptomatic, as defined by the Brief Pain Inventory–Short Form (asymptomatic with scores of 0 or 1 or mildly asymptomatic with scores of 2–3). Patients with visceral metastases or patients who had received previous therapy with ketoconazole for >7 d were excluded.
2.2. Study design
Patients were stratified by Eastern Cooperative Oncology Group performance status (ECOG-PS) score (0 vs 1) and randomised 1:1 to receive abiraterone acetate 1000 mg plus prednisone 5 mg twice daily by mouth or placebo plus prednisone.
2.3. Efficacy outcomes
The co–primary end points were radiographic progression-free survival (rPFS) and OS. OS was defined as time from randomisation to death from any cause. The term rPFS was defined as time from randomisation to radiographic progression, as previously described [15], or death. The prespecified secondary efficacy end points were time to opiate use for cancer pain, time to initiation of cytotoxic chemotherapy, time to deterioration in ECOG-PS, and time to prostate-specific antigen (PSA) progression based on Prostate Cancer Working Group 2 (PCWG2) criteria [17]. Exploratory end points included PSA response rate, defined as the proportion of patients achieving a PSA decline ≥50% according to PCWG2 criteria [17]. Patient-reported outcomes (PROs) related to pain and functional status were prespecified in the study protocol (Supplement).
2.4. Safety
Clinical assessments were conducted at prespecified visits and included medical history, vital sign measurements, body weight, physical examination, review of concomitant therapy and procedures, and review of adverse events (AEs) and serious AEs.
2.5. Statistical analyses
All randomised patients were included in the intent-to-treat population, regardless of treatment received, and were analysed according to the randomised treatment group. All patients who received study treatment were included in the safety population [18]. Three interim analyses were planned for the OS end point at approximately 15%, 40%, and 55% OS events. The data cut-off for the IA3 was 22 May 2012, and the actual analysis was conducted at 56% OS events (434 of 773 events).
Median time-to-event end points were estimated using the Kaplan-Meier product limit method, and the log-rank test was used to compare the treatment differences. The HR and associated 95% CIs were estimated by the Cox proportional hazards model [18]. A significance level of 0.04 (0.0035 for IA3) was allocated for the OS end point (three interim and a final) using the O’Brien-Fleming boundaries as implemented by the Lan-DeMets α-spending function [19]. An exploratory multivariate analysis for OS using the Cox proportional hazards model, adjusting for known baseline prognostic factors, was performed. The incidence of grade 1/2 and 3/4 AEs was descriptively reported for patients with treatment exposure of <3, 12–15, and ≥24 mo to provide a safety overview at representative time points in the disease process across short- and long-term treatment duration. The cumulative incidence of selected AEs from time to first incidence of the AE is summarised graphically.
3. Results
A total of 1088 patients were randomised 1:1 to study treatments: 546 to abiraterone plus prednisone therapy and 542 to prednisone therapy. Patients were evenly matched between treatment groups, and baseline characteristics were consistent with asymptomatic/minimally symptomatic chemotherapy-naive mCRPC (Table 1) [15]. At IA3, the median follow-up duration of OS for the intent-to-treat population was 27.1 mo. The median treatment duration at IA3 was 13.8 mo (range: 0.3–34.9) for abiraterone and 8.3 mo (range: 0.1–32.4) for prednisone. At the time of analysis, treatment was ongoing for 23% of the patients in the abiraterone group and 11% of the patients in the prednisone group, while treatment discontinuations because of AEs were low across treatment groups (8% vs 6%, respectively) (Supplemental Fig. 1). Most patients discontinued therapy because of disease progression (57% in the abiraterone group and 68% in the prednisone group); the majority went on to receive cytotoxic chemotherapy for unequivocal clinical progression, as defined per protocol. Subsequent therapy with docetaxel was common in the abiraterone group (44%) and the prednisone group (56%), while 7% and 14% of patients, respectively, received subsequent abiraterone plus prednisone treatment (Table 2).
Table 1.
Baseline patient characteristics
| Characteristic | Abiraterone plus prednisone, n = 546 | Prednisone alone, n = 542 |
|---|---|---|
| Median age, yr (IQR) | 71 (65–77) | 70 (63–76) |
| Median time from initial diagnosis to first dose, yr (IQR) | 5.5 (2.7–9.7) | 5.1 (2.8–9.1) |
| Median PSA, ng/ml (IQR) | 42.0 (16.1–116.0) | 37.7 (14.9–95.3) |
| Gleason score (≥8) at initial diagnosis, no. (%) | 263 (54) | 254 (50) |
| Extent of disease, no. (%) | ||
| Bone metastases | 452 (83) | 432 (80) |
| >10 | 264 (49) | 253 (47) |
| Soft tissue or node* | 267 (49) | 271 (50) |
| Pain at screening (BPI-SF), no. (%) | ||
| 0–1 | 353 (66) | 336 (64) |
| 2–3 | 169 (32) | 170 (33) |
| BPI-SF score, mean ± SD; median (IQR) | n = 539 | n = 534 |
| Pain intensity | 0.8 ± 1.1; 0.5 (0–1.25) | 0.8 ± 1.1; 0.5 (0–1.25) |
| Worst pain intensity | 1.2 ± 1.7; 0 (0–2) | 1.2 ± 1.6; 1 (0–2) |
| Pain interference | 0.7 ± 1.3; 0 (0–0.9) | 0.7 ± 1.2; 0.1 (0–1.0) |
| FACT-P total score | n = 527 | n = 526 |
| Mean ± SD Median (IQR) |
122.1 ± 17.0; 124.0 (112.0–134.7) | 122.6 ± 17.7; 126.0 (112.0–137.0) |
BPI-SF = Brief Pain Inventory–Short Form; FACT-P = Functional Assessment of Cancer Therapy–Prostate; IQR = interquartile range (25th and 75th quartiles); PSA = prostate-specific antigen; SD = standard deviation.
Excludes visceral metastases.
Table 2.
Subsequent therapy for prostate cancer
| Abiraterone plus prednisone (n = 546), no. (%) | Prednisone alone (n = 542), no. (%) | |
|---|---|---|
| Patients with selected subsequent therapy for mCRPC* | 274 (50) | 348 (64) |
| Docetaxel | 239 (44) | 304 (56) |
| Cabazitaxel | 60 (11) | 70 (13) |
| Ketoconazole | 39 (7) | 63 (12) |
| Abiraterone† | 38 (7) | 78 (14) |
| Sipuleucel-T | 33 (6) | 28 (5) |
mCRPC = metastatic castration-resistant prostate cancer.
Table reports cumulative incidence of subsequent therapy regardless of sequence after study drug discontinuation to the third interim analysis clinical cut-off date of 22 May 2012.
First patient crossover after unblinding on 7 May 2012.
Prior to unblinding and crossover from the prednisone arm to the abiraterone arm.
3.1. Efficacy outcomes
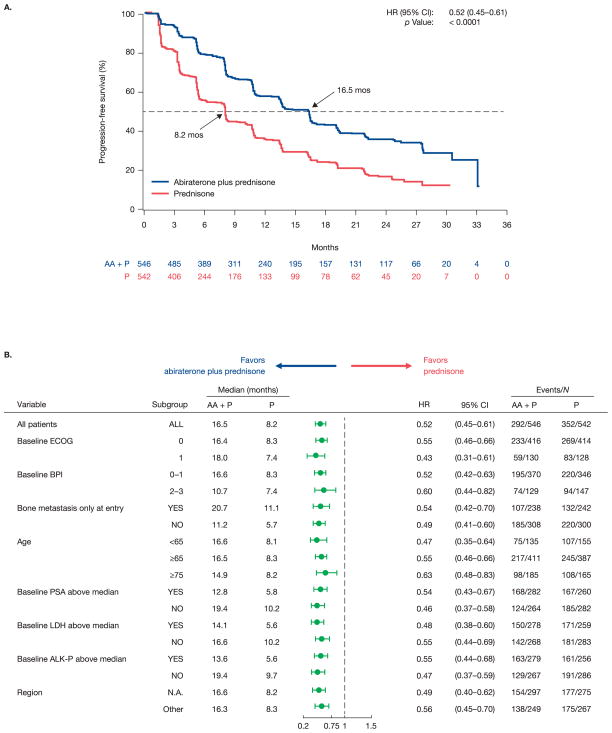
Patients receiving abiraterone compared with prednisone had statistically significant improvement in rPFS (p < 0.0001), with a median time to disease progression or death (per protocol definition) of 16.5 mo versus 8.2 mo, respectively (HR: 0.52; p <0.0001) (Fig. 1a). This improvement was observed across all patient subgroups (Fig. 1b). The OS analysis favoured abiraterone therapy over prednisone (median: 35.3 vs 30.1 mo; HR: 0.79; p = 0.0151) but did not cross the prespecified statistical boundary with an α-level of 0.0035 (Fig. 2). An exploratory multivariate analysis adjusting for baseline prognostic factors supported an OS benefit for abiraterone versus prednisone (HR: 0.74; p = 0.0017) (Table 3). Baseline serum PSA, lactate dehydrogenase, alkaline phosphatase, haemoglobin, bone metastasis, and age were significant prognostic factors (p < 0.01) (Table 3).
Fig. 1.
Co–primary end point: (a,b) radiographic progression-free survival assessed by investigator review at prespecified interim analysis. (b) The size of the circle reflects the number of patients affected. For hazard ratio (HR) <1, the result favours abiraterone. AA = abiraterone; ALK-P = alkaline phosphatase; BPI = Brief Pain Inventory; CI = confidence interval; ECOG = Eastern Cooperative Oncology Group; LDH = lactate dehydrogenase; N.A. = North America; P = prednisone; PSA = prostate-specific antigen.
Fig. 2.
Co–primary end point: (a,b) overall survival. Prespecified significance level by the O’Brien-Fleming boundary = 0.0035. (b) The size of circle reflects the number of patients affected. For hazard ratio (HR) <1, the result favours abiraterone. AA = abiraterone; ALK-P = alkaline phosphatase; BPI = Brief Pain Inventory; CI = confidence interval; ECOG = Eastern Cooperative Oncology Group; LDH = lactate dehydrogenase; N.A. = North America; NE = not estimable; P = prednisone; PSA = prostate-specific antigen.
Table 3.
Exploratory multivariate analysis of overall survival
| Parameter* | Hazard ratio (95% CI) | p value |
|---|---|---|
| Treatment (abiraterone plus prednisone vs prednisone alone) | 0.74 (0.61–0.89) | 0.002 |
| ECOG score (1 vs 0) | 1.17 (0.94–1.45) | 0.2 |
| Log (baseline serum PSA, ng/ml) | 1.18 (1.10–1.27) | <0.0001 |
| Log (baseline lactate dehydrogenase, IU/l) | 3.07 (2.11–4.48) | <0.0001 |
| Log (baseline alkaline phosphatase, IU/l) | 1.33 (1.14–1.56) | 0.0003 |
| Baseline haemoglobin, g/dl | 0.92 (0.85–0.99) | 0.02 |
| Bone metastasis only at baseline, yes vs no | 0.69 (0.57–0.85) | 0.0003 |
| Age | 1.02 (1.01–1.03) | 0.0006 |
CI = confidence interval; ECOG = Eastern Cooperative Oncology Group; PSA = prostate-specific antigen.
Patients who are not deceased at time of analysis are censored on the last date they were known to be alive or lost to follow-up.
Post hoc sensitivity analysis. Model dependent variable is overall survival, expressed as days from date of randomisation to death from any cause.
All secondary end points favoured abiraterone versus prednisone (Fig. 3). Abiraterone delayed the time to opiate use for cancer-related pain (HR: 0.71; p = 0.0002) and time to initiation of chemotherapy (HR: 0.61; p < 0.0001). Abiraterone also delayed the time to deterioration in ECOG-PS (HR: 0.83; p = 0.005) and PSA progression (HR: 0.50; p < 0.0001). The PSA response rate (≥50%) was more than doubled with abiraterone (68% [374 of 546]) compared with prednisone (29% [156 of 542]) (Fig. 4).
Fig. 3.
Secondary end points: (a) time to opiate use for cancer-related pain; (b) time to initiation of chemotherapy; (c) time to deterioration in the Eastern Cooperative Oncology Group (ECOG) score; (d) time to prostate-specific antigen (PSA) progression. AA = abiraterone; CI = confidence interval; HR = hazard ratio; NR = not reached; P = prednisone.
Fig. 4.

Maximal prostate-specific antigen (PSA) decline from baseline. A negative percentage indicates a decline in PSA. A positive percentage indicates that the patient never has a decline in PSA.
3.2. Patient-reported outcomes
The baseline pain scores and functional status scores (see Supplement for definitions) were well balanced between study groups (Table 1). The compliance rates across treatment groups for completion of the Brief Pain Inventory–Short Form and Functional Assessment of Cancer Therapy–Prostate (FACT-P) questionnaires were >95% each; compliance was defined as the number of completed questionnaires over the total expected. Following treatment, PRO scores showed a consistent pattern of delays in pain progression and in degradation of subscales of functional status for patients treated with abiraterone versus prednisone (Table 4). Patients receiving abiraterone had statistically significant improvement in pain interference (p = 0.005) versus prednisone, although the improvement in mean pain intensity (p = 0.061) was not significant (Table 4).
Table 4.
Patient-reported outcomes
| PRO end points | Abiraterone plus prednisone, n = 546 | Prednisone alone, n = 542 | Hazard ratio* (95% CI) | p value† |
|---|---|---|---|---|
| Median time to pain progression, mo | ||||
| Mean pain intensity‡ | 26.7 | 18.4 | 0.83 (0.68–1.01) | 0.06 |
| Pain interference### | 10.3 | 7.4 | 0.80 (0.68–0.93) | 0.005 |
| Worst pain intensity‡ (prespecified analysis) | 25.8 | 20.3 | 0.85 (0.69–1.04) | 0.1 |
| Median time to functional status degradation, mo | ||||
| FACT-P total score|| | 12.7 | 8.3 | 0.79 (0.67–0.93) | 0.005 |
| FACT general score¶ | 16.6 | 11.1 | 0.76 (0.64–0.91) | 0.002 |
| Prostate Cancer Subscale | 11.1 | 5.8 | 0.72 (0.61–0.84) | <0.0001 |
| Physical well-being | 14.8 | 11.1 | 0.76 (0.64–0.91) | 0.002 |
| Functional well-being | 13.3 | 8.4 | 0.77 (0.65–0.91) | 0.002 |
| Trial outcome index** | 13.9 | 9.3 | 0.77 (0.65–0.91) | 0.002 |
| Social/family well-being | 18.4 | 16.6 | 0.95 (0.78–1.15) | 0.6 |
| Emotional well-being | 22.5 | 14.2 | 0.73 (0.61–0.89) | 0.002 |
BPI-SF = Brief Pain Inventory–Short Form; CI = confidence interval; FACT = Functional Assessment of Cancer Therapy; FACT-P = Functional Assessment of Cancer Therapy–Prostate; PRO = patient-reported outcomes.
Obtained from stratified proportional hazards model. Hazard ratio <1 favours abiraterone plus prednisone.
Obtained from log-rank test stratified by Eastern Cooperative Oncology Group performance status (0 or 1).
Progression: ≥30% increase from baseline in BPI-SF score without decreased analgesic usage score, at two consecutive visits.
Pain interference progression: an increase at any visit in the baseline BPI-SF pain interference score of one-half the baseline standard deviation of BPI-SF.
Progression: ≥2-point increase from baseline without decreased analgesic usage score, at two consecutive visits.
Total score consists of FACT general and Prostate Cancer Subscale scores.
FACT general score consists of physical well-being, social/family well-being, emotional well-being, and functional well-being subscales.
Trial outcome index consists of physical well-being, functional well-being, and Prostate Cancer Subscale.
Using the prespecified ≥30% change from baseline in pain intensity as the minimal important difference, the worst pain intensity was not significantly different between treatment groups (p = 0.113) (Table 4). Abiraterone treatment did delay degradation in FACT-P total scores (p = 0.005) and in the PCa-specific subscale scores (p < 0.0001) versus prednisone (Table 4). All other FACT-P subscales also favoured abiraterone versus prednisone, except the social/family well-being subscale (p = 0.577).
3.3. Safety
AEs are summarised in Table 5. The most frequently reported AEs (≥15% of patients in either group) were similar to those reported previously (Table 5) [15]. The most frequently reported grade 3/4 AEs in the abiraterone or prednisone treatment groups (reported in ≥3% of patients in either group) were alanine aminotransferase (ALT) increased (6% [30 of 542] vs 1% [4 of 540]), hypertension (4% [23 of 542] vs 3% [17 of 540]), back pain (3% [15 of 542] vs 4% [21 of 542]), hyperglycaemia (3% [14 of 542] vs 2% [11 of 540]), hypokalaemia (3% [14 of 542] vs 2% [10 of 542]), aspartate aminotransferase (AST) increased (3% [17 of 542] vs 1% [5 of 540]), and dyspnoea (3% [14 of 542] vs 1% [5 of 540]), respectively.
Table 5.
Safety overview and adverse events of special interest
| Abiraterone plus prednisone (n = 542), no. (%) | Prednisone alone (n = 540), no. (%) | |||
|---|---|---|---|---|
| AEs (grade 1–4) | 538 (99) | 524 (97) | ||
| Grade 3/4 AE | 267 (49) | 235 (44) | ||
| Any serious AE | 188 (35) | 146 (27) | ||
| AE leading to treatment discontinuation | 58 (11) | 53 (10) | ||
| AE leading to death | 21 (4) | 16 (3) | ||
| Common AEs (≥15% patients in either group) | Grade 1–4, no. (%) | Grade 1–4, no. (%) | ||
| Fatigue | 215 (40) | 187 (35) | ||
| Back pain | 180 (33) | 179 (33) | ||
| Arthralgia | 159 (29) | 132 (24) | ||
| Peripheral oedema | 141 (26) | 113 (21) | ||
| Nausea | 130 (24) | 124 (23) | ||
| Constipation | 128 (24) | 110 (20) | ||
| Hot flush | 123 (23) | 99 (18) | ||
| Diarrhoea | 127 (23) | 98 (18) | ||
| Hypertension | 118 (22) | 73 (14) | ||
| Bone pain | 113 (21) | 103 (19) | ||
| Cough | 98 (18) | 74 (14) | ||
| Hypokalaemia | 93 (17) | 69 (13) | ||
| Pain in extremity | 93 (17) | 87 (16) | ||
| Musculoskeletal pain | 88 (16) | 81 (15) | ||
| Insomnia | 79 (15) | 62 (12) | ||
| Muscle spasm | 77 (14) | 111 (21) | ||
| AEs of special interest | Grade 1–4, no. (%) | Grades 3/4, no. (%) | Grade 1–4, no. (%) | Grades 3/4, no. (%) |
| Fatigue | 215 (40) | 13 (2) | 187 (35) | 10 (2) |
| Fluid retention | 159 (29) | 5 (1) | 130 (24) | 9 (2) |
| Hypertension | 118 (22) | 23 (4) | 73 (14) | 17 (3) |
| Cardiac disorders | 110 (20) | 36 (7) | 92 (17) | 19 (4) |
| Hypokalaemia | 93 (17) | 14 (3) | 69 (13) | 10 (2) |
| ALT increased | 65 (12) | 30 (6) | 27 (5) | 4 (1) |
| AST increased | 60 (11) | 17 (3) | 26 (5) | 5 (1) |
| Hyperglycaemia | 47 (9) | 14 (3) | 43 () | 11 (2) |
| Weight gain | 28 (5) | 0 | 39 (7) | 0 |
AE = adverse event; ALT = alanine aminotransferase; AST = aspartate aminotransferase.
AEs leading to dose modifications or interruption of treatment occurred in 21% of patients receiving abiraterone (112 of 542) and in 12% of patients in the prednisone group (65 of 540) and included ALT increased, AST increased, hypertension, and vomiting. AEs leading to death occurred in 4% of patients in the abiraterone group (21 of 542) and 3% of patients in the prednisone group (16 of 540). Drug-related treatment-emergent AEs leading to death occurred in 1% of patients in each treatment group (6 patients each).
AEs of special interest included events related to mineralocorticoid excess (hypertension, hypokalaemia, fluid retention) based on the known mechanism of action of abiraterone. Grade 3 or 4 mineralocorticoid-related AEs and increases in ALT and AST were more common with abiraterone (Table 5). The grade 3 or 4 AEs of increased ALT and AST remained higher in the abiraterone group (6% [30 of 542] and 3% [17 of 542]) versus the prednisone group (1% [4 of 540] and 1% [5 of 540]), respectively. Grade 3 or 4 cardiac disorder AEs in the abiraterone versus the prednisone group were rare: arrhythmias (4% [21 of 542] vs 2% [11 of 540]), ischaemic heart disease (2% [11 of 542] vs 1% [8 of 540]), cardiac failure (1% [6 of 542] vs 0), and cardiac disorders of other causes (<1% each), respectively. Cardiac disorders that led to treatment discontinuation were also extremely rare and were reported in <1% of patients in each treatment group. In a post hoc analysis, the incidence of selected grade 3 or 4 AEs was low, despite longer abiraterone treatment exposure (Supplemental Fig. 2). The cumulative incidence of selected AEs (all grades) from the time of first event was similar across treatment groups (Supplemental Fig. 3).
4. Discussion
We present the updated efficacy and safety outcomes from the prespecified IA3, with longer treatment exposure and a greater number of death events—434 compared with 333 in the previous analysis [15]. With a longer follow-up of 27.1 mo, the current results confirm the clinical benefits of abiraterone versus prednisone in chemotherapy-naive patients with mCRPC, including significantly delayed time to disease progression (16.5 mo vs 8.2 mo; HR: 0.52; p < 0.0001). Abiraterone therapy improved OS compared with prednisone (median: 35.3 mo vs 30.1 mo; HR: 0.79; p = 0.0151), but this result did not cross the prespecified efficacy boundary for statistical significance, as defined by the O’Brian-Fleming boundary implemented by the Lan-DeMets α-spending function.
This study also used two primary end points and several clinically relevant secondary end points to establish efficacy and clinical benefit. Previous findings at IA2 of this study showed that rPFS, when assessed by investigator review, was consistently and robustly associated with OS, with a Spearman correlation coefficient of 0.72 between the two end points [15,20]. All secondary end points (time to opiate use for cancer-related pain, time to cytotoxic chemotherapy, time to ECOG-PS deterioration by at least one grade, time to PSA progression) remained consistent with the results of previous analyses [15] and demonstrated statistically significant differences in favour of treatment with abiraterone compared with prednisone.
Additionally, this study incorporated and reported prespecified, validated PRO measures to show that abiraterone treatment delayed pain progression and deterioration of functional status compared with prednisone, consistent with our previous IA2 report [21]. Along with previous explorations of PROs in patients with mCRPC following chemotherapy [22–24], the current data further confirm the value of addressing the concerns of patients and clinicians related to improvements in how the patient feels and functions during treatment.
Unmet needs for chemotherapy-naive patients with progressive mCRPC are low toxicity and effective treatments that can prolong life, delay disease progression, and maintain quality of life [25]. Second-line antiandrogens, nonspecific adrenal androgen inhibitors, and oestrogen-based therapies are associated with PSA responses in some patients, but the effects of these agents on survival are unknown [25–27]. Sipuleucel-T, an immunotherapeutic drug, has demonstrated significant survival benefit over placebo for patients with mCRPC (median OS: 25.8 mo vs 21.7 mo; p = 0.03) [28], with no impact on disease progression (median: 3.7 mo vs 3.6 mo; p = 0.63) or post-therapy changes in PSA. Enzalutamide is approved in the United States and the European Union based on survival benefits in patients with mCRPC following chemotherapy [29], and positive results for chemotherapy-naive mCRPC were recently announced [30]. Radium 223 chloride is approved in the United States and Europe for patients with symptomatic bone mCRPC without visceral metastasis [31].
The most common subsequent therapy for patients who terminated the study was docetaxel in both study groups (44% for abiraterone; 56% for prednisone). As the data cut-off date for the current analysis (22 May 2012) was in proximity to the date of unblinding of the study, as recommended by the independent data-monitoring committee (7 May 2012), only three patients had crossed over from the prednisone group to receive abiraterone. Hence, the unblinding of the study is unlikely to have had a significant impact on the study results presented in this paper. The safety findings of the updated results with longer follow-up are similar to those of the previous report [15], with mostly grade 1 or 2 AEs. Among AEs of special interest, only increased ALT or AST remained higher in the abiraterone group than in the prednisone group, similar to the previous observation [15]. Post hoc analyses of long-term safety did not reveal any new safety findings in patients with ≥24 mo of treatment exposure with abiraterone or with prednisone. Despite the limitation of a post hoc analysis, these results are particularly reassuring for clinicians who may be concerned about long-term side-effects of prolonged prednisone exposure.
5. Conclusions
In patients with asymptomatic and mildly symptomatic mCRPC without prior chemotherapy, treatment with abiraterone plus prednisone significantly delayed disease progression, time to opiate use, and initiation of chemotherapy, and it was associated with an increase in OS. Abiraterone also delayed functional decline and progression of pain interference compared with prednisone alone. No new safety signals were observed with ≥24 mo of treatment with abiraterone or with prednisone. With the follow-up duration now exceeding 27 mo, this ongoing study in patients with mCRPC provides more mature efficacy and safety follow-up outcomes. The observed continued benefits of prolonged rPFS, coupled with the improved maintenance of quality of life, are particularly important for chemotherapy-naive patients with mCRPC.
Supplementary Material
Take-home message.
The updated analysis of study COU-AA-302 confirms the continued clinical benefit of abiraterone acetate and prednisone in the treatment of chemotherapy-naive patients with metastatic castration-resistant prostate cancer. Long-term use of abiraterone and prednisone for ≥24 mo was not associated with any new safety concerns.
Patient summary.
The updated results of this ongoing study showed that disease progression was delayed in patients with advanced prostate cancer who were treated with abiraterone acetate and prednisone, and there was a continued trend in prolongation of life compared with patients treated with prednisone alone. Treatment with abiraterone acetate and prednisone was well tolerated by patients who were treated for >2 yr.
Acknowledgments
Funding/Support and role of the sponsor: All aspects of the study, including design and conduct, data collection, management, and analysis, were sponsored by Janssen Research and Development (formerly Ortho Biotech Oncology Research and Development, unit of Cougar Biotechnology), Raritan, NJ, USA, and conducted on behalf of the Study 302 Investigators. Writing assistance was funded by Janssen Global Services, LLC.
Writing assistance was provided by Hajira Koeller, of PAREXEL.
Footnotes
Presented at the Genitourinary Cancers Symposium (ASCO GU), 14–16 February 2013, Orlando, FL, USA, and the American Society of Clinical Oncology 2013 Annual Meeting, 31 May to 4 June 2013, Chicago, IL, USA.
Author contributions: Dana E. Rathkopf had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Ryan, Griffin, Kheoh, Molina.
Acquisition of data: Rathkopf, Smith, de Bono, Logothetis, Shore, de Souza, Fizazi, Mulders, Mainwaring, Hainsworth, Beer, North, Fradet, Van Poppel, Carles, Flaig, Efstathiou, E. Yu, Higano, Taplin, Small, Scher, Ryan, Saad.
Analysis and interpretation of data: Rathkopf, Ryan, Griffin, Todd, Park, M. Yu, Kheoh, Molina.
Drafting of the manuscript: Rathkopf, Smith, de Bono, Logothetis, Shore, de Souza, Fizazi, Mulders, Mainwaring, Hainsworth, Beer, North, Fradet, Van Poppel, Carles, Flaig, Efstathiou, E. Yu, Higano, Taplin, Small, Scher, Ryan, Saad, Griffin, Todd, Park, M. Yu, Kheoh, Molina.
Critical revision of the manuscript for important intellectual content: Rathkopf, Smith, de Bono, Logothetis, Shore, de Souza, Fizazi, Mulders, Mainwaring, Hainsworth, Beer, North, Fradet, Van Poppel, Carles, Flaig, Efstathiou, E. Yu, Higano, Taplin, Griffin, Todd, M. Yu, Park, Kheoh, Small, Scher, Molina, Ryan, Saad.
Statistical analysis: Park, Kheoh.
Obtaining funding: Molina and Griffin.
Administrative, technical, or material support: Molina, Griffin.
Supervision: Molina, Griffin.
Other (specify): None.
Financial disclosures: Dana E. Rathkopf certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: Dana E. Rathkopf has received research funding from Cougar Biotechnology, Janssen Biotech, and Medivation. Matthew R. Smith has served as a consultant/advisor for, and received research funding from, Janssen. Johann S. de Bono is an employee of The Institute of Cancer Research and has served as a consultant/advisor for and received honoraria from Astellas, Medivation, and Johnson & Johnson. Christopher J. Logothetis has served as a consultant/advisor for, and received honoraria and research funding from, Astellas, Novartis, BMS, Johnson & Johnson, and Sanofi. Neal D. Shore served as a consultant/advisor for Amgen, Astellas, Algeta, Bayer, Ferring, Dendreon, Janssen, Millennium, Sanofi, and BNI. Paul de Souza has served as a consultant/advisor for, and has received honoraria from, Janssen Australia Pty Ltd. Karim Fizazi has served as a consultant/advisor for, and received honoraria from, Janssen. Paul Mainwaring has served as a consultant/advisor for, and received honoraria from, Roche, Sanofi, and Janssen. Tomasz M. Beer has received research funding from Cougar Biotechnology, Janssen Biotech, Astellas Pharma Global, and Medivation. Scott North has served as a consultant/advisor for Janssen and Astellas and has received honoraria from Janssen, Astellas, Pfizer, Novartis, and GSK. Yves Fradet has received honoraria and research funding from Janssen Ortho. Joan Carles has served as a consultant/advisor for Janssen, Novartis, Sanofi, Pfizer, and Astellas and has received honoraria from Janssen, Astellas, Pfizer, Novartis, and GSK. Thomas W. Flaig is an employee of, and has intellectual property interests in, Aurora Oncology; has served as a consultant/advisor for GTx and Sanofi; and has received honoraria from Amgen and research funding from Amgen, Bayer/Onyx, BN ImmunoTherapeutics, Cougar Biotechnology, Dendreon, Genentech, GlaxoSmithKline, GTx, Janssen Oncology, Medivation, Novartis, Pfizer, Sanofi, Veridex, and Zymogenetics. Eleni Efstathiou has received honoraria from, and served on an ad board and steering committee for, Johnson & Johnson, Millennium, and Sanofi. Evan Y. Yu has served as a consultant/advisor for, and received research funding from, Janssen. Celestia S. Higano has served as a consultant for Amgen, AstraZeneca, Bayer, Centocor Ortho Biotech, Dendreon, Genentech, GTx, Inc., Medivation, Millennium, Pfizer, Bristol-Myers Squibb, Sanofi-Aventis, Teva Pharmaceuticals, Abbott Laboratories, Endo, Fresenius Kabi, Cougar Biotechnology, and Novartis and has received institutional research funding from Amgen, Aragon, Bristol-Myers Squibb, Dendreon, Exelixis, ImClone, Medarex, Medivation, Millennium, OncoGenex, GlaxoSmithKline, Nerviano, Novartis, Cougar Biotechnology, Algeta, and Genentech. Mary-Ellen Taplin has served as a consultant/advisor for, and received honoraria and research funding from, Janssen. Thomas W. Griffin is an employee of Janssen Research and Development and owns stock in Johnson & Johnson. Mary Todd is an employee of Janssen Global Services and owns stock in Johnson & Johnson. Margaret Yu is an employee of, and owns stock in, Janssen Research and Development. Youn C. Park is an employee of Janssen Research and Development and owns stock in Johnson & Johnson. Thian Kheoh is an employee of Janssen Research and Development and owns stock in Johnson & Johnson. Howard I. Scher has served as a consultant (uncompensated) for Aragon Pharmaceuticals, Bristol-Myers Squibb, Celgene, Johnson & Johnson Pharmaceutical Development, Medivation, and Veridex (now Janssen Research and Development); has served as a consultant (compensated) for ODEON, Enzon, Millennium, Novartis, and Ortho Biotech Oncology Research and Development; and has received research funding (paid to institution) from Aragon Pharmaceuticals, Exelixis, Janssen Research and Development, Medivation, and Veridex (now Janssen Research and Development). Arturo Molina is an employee of Janssen Research and Development and owns stock in Johnson & Johnson. Charles J. Ryan has received honoraria from Janssen. Fred Saad has served as a consultant for, and received honoraria and research funding from, Janssen and Astellas.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Heidenreich A, Bastian PJ, Bellmunt J, et al. EAU guidelines on prostate cancer, II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 2014;65:467–79. doi: 10.1016/j.eururo.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 2.National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN guidelines) [Accessed May 28, 2013];Prostate cancer v. 2.2013. National Comprehensive Cancer Network Web site. http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf.
- 3.Halabi S, Small EJ, Kantoff PW, et al. Prognostic model for predicting survival in men with hormone-refractory metastatic prostate cancer. J Clin Oncol. 2003;21:1232–7. doi: 10.1200/JCO.2003.06.100. [DOI] [PubMed] [Google Scholar]
- 4.Tannock IF, de WR, Berry WR, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–12. doi: 10.1056/NEJMoa040720. [DOI] [PubMed] [Google Scholar]
- 5.Petrylak DP, Tangen CM, Hussain MH, et al. Docetaxel and estramustine compared with mioxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004;351:1513–20. doi: 10.1056/NEJMoa041318. [DOI] [PubMed] [Google Scholar]
- 6.Berthold DR, Pond GR, Soban F, de Witt R, Eisenberger M, Tannock IF. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer: updated survival in the TAX 327 study. J Clin Oncol. 2008;26:242–5. doi: 10.1200/JCO.2007.12.4008. [DOI] [PubMed] [Google Scholar]
- 7.de Bono JS, Oudard S, Ozguroglu M, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376:1147–54. doi: 10.1016/S0140-6736(10)61389-X. [DOI] [PubMed] [Google Scholar]
- 8.Attard G, Belldegrun AS, de Bono JS. Selective blockade of androgenic steroid synthesis by novel lyase inhibitors as a therapeutic strategy for treating metastatic prostate cancer. BJU Int. 2005;96:1241–6. doi: 10.1111/j.1464-410X.2005.05821.x. [DOI] [PubMed] [Google Scholar]
- 9.Molina A, Belldegrun A. Novel therapeutic strategies for castration resistant prostate cancer: inhibition of persistent androgen production and androgen receptor mediated signaling. J Urol. 2011;185:787–94. doi: 10.1016/j.juro.2010.10.042. [DOI] [PubMed] [Google Scholar]
- 10.Agarwal N, Sonpavde G, Sternberg CN. Novel molecular targets for the therapy of castration-resistant prostate cancer. Eur Urol. 2012;61:950–60. doi: 10.1016/j.eururo.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 11.Attard G, Reid AH, A’Hern R, et al. Selective inhibition of CYP17 with abiraterone acetate is highly active in the treatment of castration-resistant prostate cancer. J Clin Oncol. 2009;27:3742–8. doi: 10.1200/JCO.2008.20.0642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ryan CJ, Cheng ML. Abiraterone acetate for the treatment of prostate cancer. Expert Opin Pharmacother. 2013;14:91–6. doi: 10.1517/14656566.2013.745852. [DOI] [PubMed] [Google Scholar]
- 13.Fizazi K, Scher HI, Molina A, et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2012;13:983–92. doi: 10.1016/S1470-2045(12)70379-0. [DOI] [PubMed] [Google Scholar]
- 14.de Bono JS, Logothetis CJ, Molina A, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364:1995–2005. doi: 10.1056/NEJMoa1014618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ryan CJ, Smith MR, de Bono JS, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368:138–48. doi: 10.1056/NEJMoa1209096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zytiga (abiraterone acetate) [prescribing information] Horsham, PA: Janssen Biotech Inc; 2012. [Google Scholar]
- 17.Scher HI, Halabi S, Tannock I, et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol. 2008;26:1148–59. doi: 10.1200/JCO.2007.12.4487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cox DR. Regression models and life-tables (with discussion) J Royal Stat Soc. 1972;B:187–220. [Google Scholar]
- 19.Kalbfleisch JD, Prentice RL. The statistical analysis of failure time data. 2. New York, NY: John Wiley & Sons; 2002. [Google Scholar]
- 20.Ryan CJ, Molina A, Piulats JR, et al. Association of radiographic progression-free survival (rPFS) adapted from Prostate Cancer Working Group 2 (PCWG2) consensus criteria with overall survival in patients with metastatic castration-resistant prostate cancer (mCRPC): results from COU-AA-302; Presented at: European Society for Medical Oncology annual congress; 28 September to 2 October, 2012; Vienna, Austria. [Google Scholar]
- 21.Basch E, Autio K, Ryan CJ, et al. Abiraterone acetate plus prednisone versus prednisone alone in chemotherapy-naive men with metastatic castration-resistant prostate cancer: patient-reported outcome results of a randomised phase 3 trial. Lancet Oncol. 2013;14:1193–9. doi: 10.1016/S1470-2045(13)70424-8. [DOI] [PubMed] [Google Scholar]
- 22.Logothetis CJ, Basch E, Molina A, et al. Effect of abiraterone acetate and prednisone compared with placebo and prednisone on pain control and skeletal-related events in patients with metastatic castration-resistant prostate cancer: exploratory analysis of data from the COU-AA-301 randomised trial. Lancet Oncol. 2012;13:1210–7. doi: 10.1016/S1470-2045(12)70473-4. [DOI] [PubMed] [Google Scholar]
- 23.Sternberg CN, Molina A, North S, et al. Effect of abiraterone acetate on fatigue in patients with metastatic castration-resistant prostate cancer after docetaxel chemotherapy. Ann Oncol. 2013;24:1017–25. doi: 10.1093/annonc/mds585. [DOI] [PubMed] [Google Scholar]
- 24.Harland S, Staffurth J, Molina A, et al. Effect of abiraterone acetate treatment on the quality of life of patients with metastatic castration-resistant prostate cancer after failure of docetaxel chemotherapy. Eur J Cancer. 2013;49:3648–57. doi: 10.1016/j.ejca.2013.07.144. [DOI] [PubMed] [Google Scholar]
- 25.Garcia JA, Rini BI. Castration-resistant prostate cancer: many treatments, many options, many challenges ahead. Cancer. 2012;118:2583–93. doi: 10.1002/cncr.26582. [DOI] [PubMed] [Google Scholar]
- 26.Small EJ, Vogelzang NJ. Second-line hormonal therapy for advanced prostate cancer: a shifting paradigm. J Clin Oncol. 1997;15:382–8. doi: 10.1200/JCO.1997.15.1.382. [DOI] [PubMed] [Google Scholar]
- 27.Rathkopf D, Scher HI. Androgen receptor antagonists in castration-resistant prostate cancer. Cancer J. 2013;19:43–9. doi: 10.1097/PPO.0b013e318282635a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kantoff PW, Higano CS, Shore ND, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–22. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- 29.Scher HI, Fizazi K, Saad F, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–97. doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 30.Medivation and Astellas announce the phase 3 PREVAIL trial of enzalutamide meets both co-primary endpoints of overall survival and radiographic progression-free survival in chemotherapy-naive patients with advanced prostate cancer. [Accessed November 13, 2013];Medivation Web site. http://files.shareholder.com/downloads/MDV/2789073008x0x698626/7aa6cc0f-13e0-46fd-add8-516e8d7cad8a/MDVN_News_2013_10_22_General_Releases.pdf.
- 31.Parker C, Nilsson S, Heinrich D, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369:213–23. doi: 10.1056/NEJMoa1213755. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.