Abstract
We present the case of a man with metastatic, castration-resistant prostate cancer, who had a complete prostate-specific antigen (PSA) response after 2½ doses of ipilimumab. His treatment course was complicated by diarrhea and autoimmune hepatitis, both of which resolved within 4 months. Sera and biopsy specimens were accessed, and sera from pretreatment and day 113 were analyzed. Augmented antibody responses were detected against 11 potential tumor antigens, with responses ranging from 5- to 20-fold in day 113 sera compared with baseline. Genes that were targets of a strong antibody response (arbitrarily set at 10-fold or greater increase) were analyzed by real-time PCR for expression in the tumor biopsy cDNA. Of the top 5 genes, only 3-hydroxyisobutyryl-CoA hydrolase (HIBCH) could be identified in the amplified tumor biopsy cDNA. Using an antibody to HIBCH, immunohistochemical analysis documented strong expression of the protein. Together, these data suggest that an augmented antibody response to HIBCH, an antigen that was expressed by the patient's prostate cancer, could have contributed to the clinical response. After 16 months of PSA stability, he discontinued his androgen-suppression therapy. With the return of his testosterone, his PSA increased slightly, likely originating from his intact prostate. He has been disease free for the past 6 years without any additional therapy.
Introduction
Immunotherapy affects survival in patients with prostate cancer. In 2010, the U.S. Food and Drug Administration (FDA) approved sipuleucel-T for patients with metastatic, castration- resistant, asymptomatic, or minimally symptomatic prostate cancer based on the findings of the Immunotherapy for Prostate Adenocarcinoma Treatment (IMPACT) study, which showed a survival benefit for the sipuleucel-T group, with a median survival of 25.8 versus 21.7 months (1). Sipuleucel-T is an adoptive cellular immunotherapy that is created for each patient by exposing a sample of the patient's peripheral blood mononuclear cells (PBMC) to a prostatic acid phosphatase (PAP)–granulocyte macrophage colony-stimulating factor (GM-CSF) fusion protein ex vivo and then reintroducing these modified cells into the patient. Although IMPACT showed a survival benefit for sipuleucel-T, it did not show a significant decrease in the burden of disease by Response Evaluation Criteria in Solid Tumors (RECIST) criteria or by prostate-specific antigen (PSA).
Ipilimumab is a monoclonal antibody to CTLA-4, a co-repressor molecule that plays a key role in downregulating the immune response, including the immune response to cancer. In 2011, it was approved by the FDA for advanced melanoma (2), and exploration of its benefit in patients with prostate cancer is under way. Here, we present the case of a patient with aggressive, metastatic, castration-resistant prostate cancer (CRPC), who achieved a durable complete response after treatment with ipilimumab. To the best of our knowledge, this is the first case of a truly durable complete response to an immunologic agent in prostate cancer.
Case Report
The patient was diagnosed with Gleason 4+5 adenocarcinoma of the prostate metastatic to the lymph nodes in 2001. Treatment with leuprolide acetate resulted in an incomplete PSA response, as his PSA nadir was 13.9 ng/mL. The addition of bicalutamide, 50 mg daily, brought the PSA down to 6.1 ng/mL. The dose of bicalutamide was eventually increased to 150 mg daily, but his serum PSA increased further. He had a short-lived PSA reduction following bicalutamide withdrawal. In 2004, he enrolled on a trial of an leutenizing hormone releasing hormone (LHRH) antagonist, but did not respond and had radiographic progression within a few months. He then started ketoconazole with hydrocortisone in 2005 and discontinued this treatment in early 2007 due to progression.
In 2007, he enrolled on a phase I/II study of ipilimumab. At that time, he suffered from diminished stool caliber attributed to a 9-cm prostatic tumor mass, and he had lymph node and skeletal metastases. His PSA was 654 ng/mL. After the first infusion, he experienced grade 1 fatigue and a pruritic truncal rash. After the second infusion, he developed grade 2 fatigue and grade 3 transaminitis. He had received approximately half of his third infusion when the laboratory results showing dramatic transaminase elevations became available. This infusion was aborted, and he received no further ipilimumab therapy.
He was diagnosed with autoimmune hepatitis and treated with prednisone, 120 mg/day, and mycophenolate for 6 weeks, until resolution of his hepatitis. His thyroid function tests showed a thyroid stimulating hormone value of <0.01 (normal range, 0.28–5 µIU/mL) with a total T4 301 (normal range, 68–200 ng/dL). A nuclear medicine I-123 thyroid scan showed very faint uptake by the thyroid, which argued against Graves disease and was consistent with a medication or viral-mediated thyroiditis. He also developed progressively worsening diarrhea that started with 7 stools per day and eventually worsened to 15 bloody stools per day. Evaluation for infectious etiologies was negative. A colonoscopy showed two lesions in the colon, which were biopsied and revealed colitis. Prednisone and mycophenolate did not control the diarrhea, and he received a single dose of infliximab, 5 mg/kg. The diarrhea slowly improved over a period of 4 months, and his immuno-suppressants were tapered successfully without return of the diarrhea. Nearly 3 years later, in 2010, he presented with an episode of immunoglobulin A (IgA) nephropathy, presenting with hematuria and renal failure. The diagnosis was made by kidney biopsy. He was treated with prednisone, 60 mg/day for 2 weeks, and his renal function returned to 1.2 to 1.3 mg/dL, with no further recurrence without immunosuppression. It is unclear whether IgA nephropathy was related to his ipilimumab exposure.
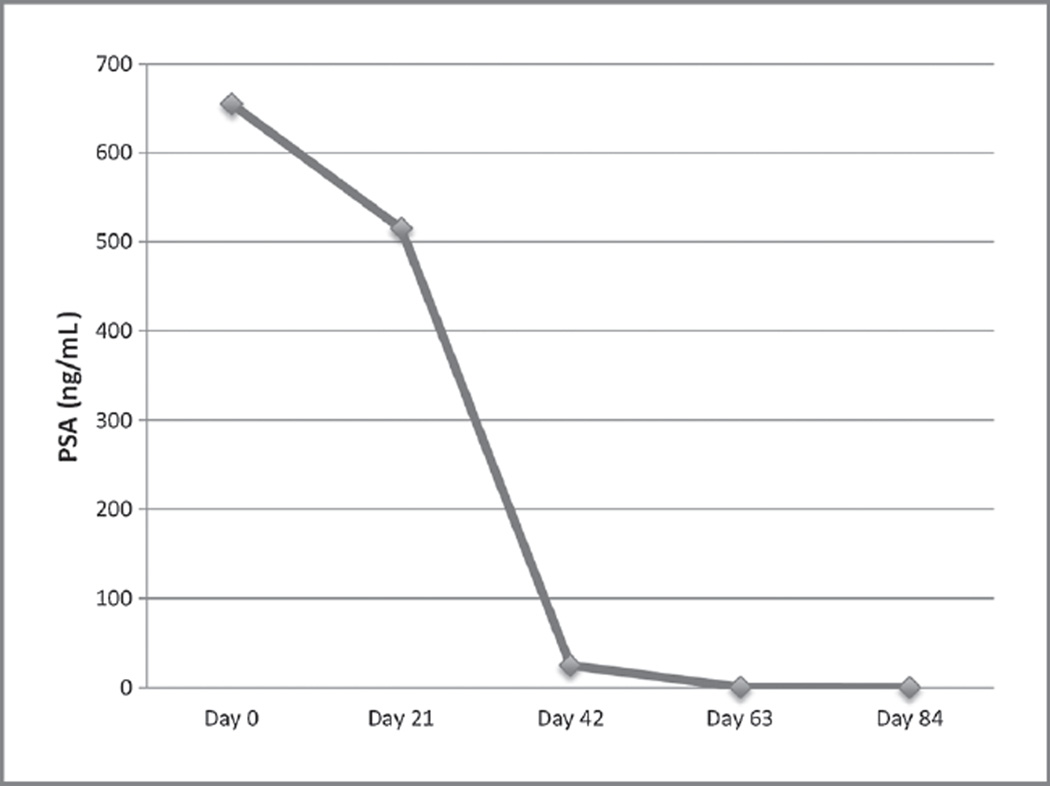
His serum PSA was 515 ng/mL after 3 weeks of therapy, 25 ng/mL after 6 weeks, 0.3 ng/mL after 9 weeks, and reached undetectable levels by 3 months (Fig. 1). Serial imaging studies revealed complete resolution of adenopathy, bone abnormalities, and the prostate mass, with a normal 3-cm prostate gland remaining.
Figure 1.
PSA trend for patient. Day 0 is the first treatment with ipilimumab. Day 21 is the second treatment. Day 42 is the half-dose third treatment after which no subsequent doses were given. PSA remained undetectable for 16 months, and once hormone suppression was withdrawn, became detectable at low levels compatible with an intact prostate gland and has remained stable for 5 years since the initiation of therapy.
After he remained in complete remission for 16 months, at his request, leuprolide acetate was discontinued. As his testosterone recovered, his PSA became detectable at low levels (highest reached was 0.51 ng/mL). PSA levels have remained stable since testosterone recovery (testosterone 270 ng/dL) and are thought to represent PSA production by his native, untreated prostate gland. Repeated imaging studies have revealed no evidence of local or distant progression.
The patient remains entirely disease free 6 years after he experienced a dramatic response to treatment with ipilimumab. Although the first several months of treatment were complicated by serious immune-related adverse events and an episode of IgA nephropathy was seen 3 years after therapy, these complications have resolved. To the best of our knowledge, this is the first case of a durable complete remission in advanced CRPC induced by an immunotherapeutic agent.
Discussion
Before the approval of sipuleucel-T in 2010, treatment for incurable prostate cancer consisted of androgen-suppression therapy (AST) and chemotherapy. Although AST can result in dramatic responses, it is not curative, and prostate cancer eventually becomes resistant to it. The results of chemotherapy are typically less dramatic and reserved for symptomatic, castration-resistant disease. The case presented represents a unique complete response in this patient for whom chemotherapy is usually recommended. Furthermore, the response has been durable in that the patient has not received any treatment, even hormonal, for the past 5 years.
The response to ipilimumab in prostate cancer is varied. A pilot study using one to two doses of ipilimumab, 3 mg/kg, resulted in a 50% PSA decrease in 2 of 12 patients (17%) treated (3). Another phase I study that combined ipilimumab with PSA-TRICOM vaccine and GM-CSF showed a greater response in chemotherapy-naïve patients (6 of 24 had ≥50% PSA decline) than in those who had previously received chemotherapy (0 of 6 had ≥50% PSA decline; ref, 4). In addition, the combination of ipilimumab with prostate GVAX vaccination resulted in PSA declines in a majority of patients, with evidence of tumor regression in 2 patients (5). Recently, the results of the phase III study of ipilimumab, 10 mg/kg plus 8 Gy of bone-directed radiation, versus placebo plus 8 Gy bone-directed radiation in 799 men with metastatic CRPC previously treated with chemotherapy were presented. There was a trend toward improved overall survival in the group that received ipilimumab (HR, 0.85; 95% confidence interval, 0.72–1.00; P = 0.053; ref. 6).
Investigations of ipilimumab show a correlation of immune adverse events (iAE) and efficacy. The patient in this discussion had autoimmune hepatitis, autoimmune colitis, and thyroiditis. Attia and colleagues reported in 2005 that in patients with melanoma treated with ipilimumab, the response rate was 36% for those with iAEs versus 5% in those without iAEs (P = 0.008; ref. 7). These associations have been suggested in patients with prostate cancer as well (8).
There is also a correlation between rising absolute lymphocyte counts and response to ipilimumab in patients with melanoma (9). Our patient's absolute lymphocyte count was 810/mm3 before starting ipilimumab treatment. It peaked at 1,430/mm3 6 months after the first treatment and came down to 760/mm3 11 months after treatment.
A clinical response to a treatment that is antigen agnostic and acts by interfering with an immune response inhibitor is exciting. This observation is consistent with preclinical evidence that shows that elimination of checkpoint blockade can augment an ongoing immune response and induce regression of "immunogenic" tumors. Because this patient did not receive a vaccine, we hypothesize that he developed a tumor-specific immune response that was insufficient to control cancer growth secondary to inhibitory signals provided by the tumor microenvironment. Following the administration of ipilimumab, his immune response was released from checkpoint blockade and tumor regression ensued. This hypothesis is consistent with the three "E" model (elimination, equilibrium, and escape) of Schreiber and colleagues (10), and clinical studies suggesting a pre- existing immune response is prognostic of a beneficial outcome (11) and can be predictive of response to immunotherapy (12).
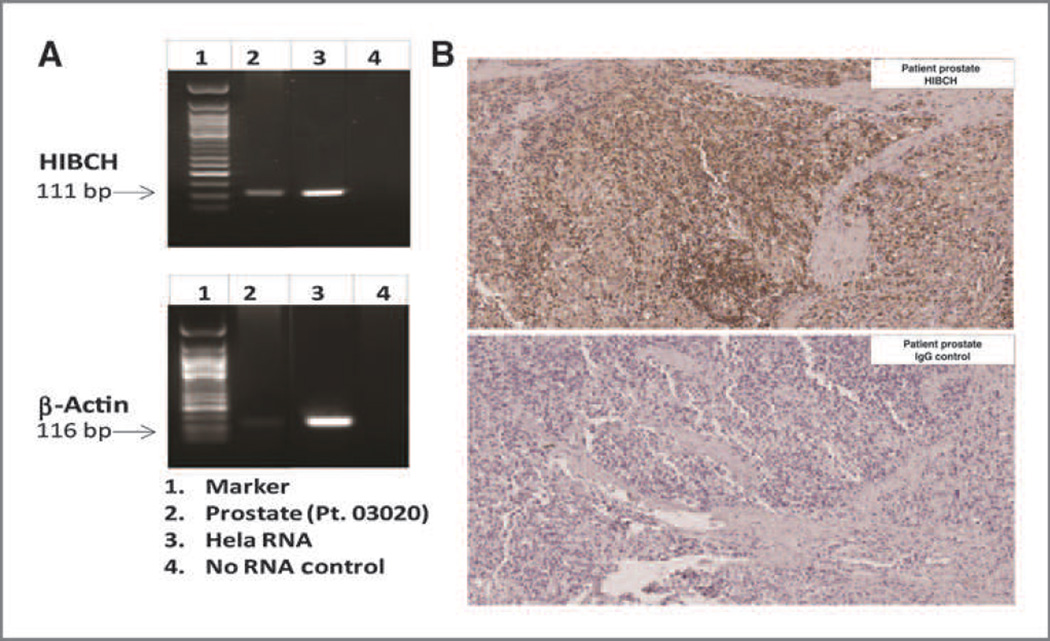
To investigate whether the administration of ipilimumab was associated with an augmentation of anticancer immunity in this patient, ProtoArrays (Invitrogen) were used to assess increases in antibody responses following the initiation of immunotherapy. After obtaining informed consent, sera and biopsy specimens were accessed, and sera from pretreatment and day 113 after first treatment were analyzed. Augmented antibody responses were detected against 11 potential tumor antigens, with responses ranging from 5-to 20-fold in day 113 sera compared with baseline (Table 1). To assess whether these antibody responses were directed against antigens that were potentially relevant to this patient, RNA was isolated from 5-µm sections of an archived biopsy specimen taken before the initiation of ipilimumab treatment, and cDNA was amplified and used for real-time PCR (RT-PCR). Genes that were targets of a strong antibody response (arbitrarily set at 10-fold or greater increase) were analyzed by RT-PCR for expression in the tumor biopsy cDNA. Of the top 5 genes, only HIBCH (3-hydroxyisobutyryl-CoA hydrolase) could be identified in the amplified tumor biopsy cDNA (Fig. 2A). Next, we sought to identify whether HIBCH protein could be detected in the patient's biopsy specimen. Using an antibody to HIBCH, immunohistochemical (IHC) analysis documented strong expression of the protein (Fig. 2B). Together, these data suggest that an augmented antibody response to HIBCH, an antigen that was expressed by the patient's prostate cancer, could have contributed to the clinical response.
Table 1.
List of strong antibody responses by at least 5-fold and validation of selected genes by RT-PCR
| Rank | Database ID | Ultimate ORF ID |
Description | Fold increase Aba |
RT-PCRb |
|---|---|---|---|---|---|
| 1 | BC004292.1 | IOH22899 | PHD finger protein 15 (PHF15) | 20.9 | − |
| 2 | BC067822.1 | IOH40096 | 3-hydroxyisobutyryl-coenzyme A hydrolase (HIBCH) | 20.1 | + |
| 3 | BC047870.1 | IOH26949 | Src kinase-associated phosphoprotein 1 (SKAP1) | 14.5 | − |
| 4 | NM_004202.1 | IOH11127 | Thymosin β-4, Y-chromosomal | 10.4 | − |
| 5 | BC020942.1 | IOH11137 | Transmembrane protein 140 (TMEM140) | 10.1 | − |
| 6 | NM_001283.2 | IOH42182 | Adaptor-related protein complex 1, sigma 1 subunit (AP1S1), transcript variant 1 | 7.1 | ND |
| 7 | BC005382.1 | IOH7371 | SPANX family, member E (SPANXE) | 6.9 | ND |
| 8 | NM_024294.1 | IOH5168 | Chromosome 6 open reading frame 106 (C6orf106), transcript variant 1 | 6.3 | ND |
| 9 | NM_152435.1 | IOH22648 | Amidohydrolase domain containing 1 (AMDHD1) | 6.3 | ND |
| 10 | NM_000430.2 | IOH39940 | Platelet-activating factor acetylhydrolase, isoform Ib, a subunit 45 kDa (PAFAH1B1) | 6 | ND |
| 11 | NM_020235.2 | IOH44025 | Bobby sox homolog (Drosophila; BBX) | 5 | ND |
Abbreviations: ND, not done; ORF, open reading frame; +, increased; −, decreased.
Fold increase antibody response at day 113.
RT-PCR detection of specified gene in tumor biopsy specimen.
Figure 2.
Expression and localization of HIBCH in our patient. A, RT-PCR from amplified RNA using formalin-fixed paraffin-embedded tissue of autologous tumor shows the 111-bp size specific for the HIBCH gene. β-Actin served as a positive control. Lane 1, marker; lane 2, prostate cancer; lane 3, Hela control; and lane 4, no RNA control. B, IHC staining of autologous prostate tumor biopsy with anti-HIBCH antibody (Abcam; rabbit polyclonal to HIBCH; cat no. AB101672) and with control rabbit immunoglobulin G (Vector Laboratories; ImmPRESS Reagent kit; cat no. MP-7401). Scale bar, ×20.
Previous studies have examined the humoral response to antigens expressed by the prostate cancer cell lines used to produce prostate GVAX. In a recent article, responses to two of these antigens, prostate-specific membrane antigen (PSMA) and Filamin B, were evaluated in patients receiving prostate GVAX and ipilimumab. Patients with low-level increases in antibody responses (2- to <4-fold) to PSMA had significantly increased (P = 0.028) survival, whereas patients with increased responses to Filamin B did not exhibit an increase in survival (4). A potential limitation of this analysis was the focus on only two proteins. Another study evaluated posttreatment antibody responses using ProtoArrays in patients receiving ipilimumab and GM-CSF (13). Five patients with decreases in PSA (responders) as well as 5 patients with rising PSA were evaluated. Responder patients had a larger number of strong antibody responses, and in 2 patients, T cells reactive with one of these antigens, PAK6, were identified. Supporting an important role for PAK6, IHC studies documented PAK6 expression on prostate cancer cells from one of the patients with a coordinated antibody and T-cell response.
HIBCH is a mitochondrial protein that is critical in valine catabolism (14, 15). Deficiency of this protein leads to neurologic deficits that are identifiable in infancy (16). It is found in many tissues, including prostate. Less than 10 publications have referred to HIBCH, and none have identified HIBCH as a potential tumor/tumor-associated antigen. Mutations in the HIBCH gene (substitution, nonsense, and missense mutation) are present at low levels (0.5%–6%) in many cancers (Supplementary Fig. S1). However, in prostate cancer, one study reported 50% of patients (5 of 10) with a simple somatic mutation (single-base substitution) and 10.5% (2 of 19) with a copy-number alteration. An analysis of HIBCH in a larger cohort of prostate cancers reported 5% (3 of 56) with an amplification of copy number and 4% (11 of 248) with mRNA upregulation or a homozygous deletion (17–19).
The IHC data presented above suggest that there is strong expression of HIBCH protein by the tumor of the patient being studied, raising the possibility that the "overexpressed" protein may serve as a tumor-associated antigen. In addition, given the frequency of mutations reported in the HIBCH gene, it is possible that the HIBCH gene in this patient's prostate cancer was mutated and represented a novel neoantigen against which the patient had not been tolerized. However, we have not been able to sequence the HIBCH gene in this patient and do not have access to substantial numbers of PBMC from the first 5 years this patient was in response, limiting our ability to detect a T-cell response against a mutated HIBCH epitope. Nevertheless, in support of this possibility, a recent report documented the development of a strong T-cell response against a mutated tumor-expressed protein in a patient with melanoma who experienced tumor regression following treatment with ipilimumab (20). Similarly, evidence is increasing that patients with melanoma who are treated with adoptive immunotherapy and experience long-term tumor regression have developed immune responses against mutated gene products present in the tumor (21). These findings support the concept that strong immune responses develop against mutated antigens, which are unique to the tumor and of which the patient is not tolerant. If these findings can be extended, they provide a possible mechanism of action to explain objective responses of patients treated with agents that interfere with an immune checkpoint or other immunotherapies and provide insights into what may be required to increase response rates.
Although recent success with cancer immunotherapy has led to substantial enthusiasm for its application in cancers previously considered refractory to this therapy, continued progress is not guaranteed. A comprehensive understanding of the mechanisms behind the immune system's ability to eradicate advanced cancers and the development and validation of approaches to monitor those mechanisms will be essential to the application of precision medicine that will allow fine-tuning of immune responses, elimination of metastases, and life-long anticancer immunity. The arsenal of immunotherapeutics is increasing rapidly. Similarly, novel vaccine strategies with a number of advantages over previous approaches are in clinical trials and hold potential to prime tumor-reactive T cells against antigens of which the host is not tolerant. Our case represents an unusual example of a striking result. Although much work needs to be done before such results become routine and not rare, this case provides the proof-of-concept of what is possible.
Supplementary Material
Acknowledgment
Disclosure of Potential Conflicts of Interest
C.B. Bifulco is a consultant/advisory board member for EMD/Serono. J.N. Graff, B.A. Fox, and T.M. Beer have received commercial research support from Bristol-Myers Squibb.
Footnotes
Note: Supplementary data for this article are available at Cancer Immunology Research Online (http://cancerimmunolres.aacrjournals.org/).
Authors' Contributions
Conception and design: J.N. Graff, S. Puri, B.A. Fox, T.M. Beer
Development of methodology: S. Puri, T.M. Beer
Acquisition of data (provided animals, acquired and managed patients, provided facilities, etc.): J.N. Graff, S. Puri, C.B. Bifulco, B.A. Fox, T.M. Beer
Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): J.N. Graff, S. Puri, C.B. Bifulco, B.A. Fox
Writing, review, and/or revision of the manuscript: J.N. Graff, S. Puri, C.B. Bifulco, B.A. Fox, T.M. Beer
Administrative, technical, or material support (i.e., reporting or organizing data, constructing databases): J.N. Graff, T.M. Beer
Study supervision: T.M. Beer
References
- 1.Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–422. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- 2.Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Small EJ, Tchekmedyian NS, Rini BI, Fong L, Lowy I, Allison JP. A pilot trial of CTLA-4 blockade with human anti-CTLA-4 in patients with hormone-refractory prostate cancer. Clin Cancer Res. 2007;13:1810–1815. doi: 10.1158/1078-0432.CCR-06-2318. [DOI] [PubMed] [Google Scholar]
- 4.Madan RA, Mohebtash M, Arlen PM, Vergati M, Rauckhorst M, Steinberg SM, et al. Ipilimumab and a poxviral vaccine targeting prostate-specific antigen in metastatic castration-resistant prostate cancer: a phase 1 dose-escalation trial. Lancet Oncol. 2012;13:501–508. doi: 10.1016/S1470-2045(12)70006-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van den Eertwegh AJ, Versluis J, van den Berg HP, Santegoets SJ, van Moorselaar RJ, van der Sluis TM, et al. Combined immunotherapy with granulocyte-macrophage colony-stimulating factor-transduced allogeneic prostate cancer cells and ipilimumab in patients with metastatic castration-resistant prostate cancer: a phase 1 dose-escalation trial. Lancet Oncol. 2012;13:509–517. doi: 10.1016/S1470-2045(12)70007-4. [DOI] [PubMed] [Google Scholar]
- 6.Gerritsen WR, Kwon ED, Fizazi K, et al. CA184-043: A randomized, multicenter, double-blind phase 3 trial comparing overall survival (OS) in patients (pts) with post-docetaxel castration-resistant prostate cancer (CRPC) and bone metastases treated with ipilimumab (ipi) vs placebo (pbo), each following a single-dose radiotherapy (RT) European Cancer Congress. 2013 abstr 2850. [Google Scholar]
- 7.Attia P, Phan GQ, Maker AV, Robinson MR, Quezado MM, Yang JC, et al. Autoimmunity correlates with tumor regression in patients with metastatic melanoma treated with anti-cytotoxic T-lymphocyte antigen-4. J Clin Oncol. 2005;23:6043–6053. doi: 10.1200/JCO.2005.06.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beer TM, Slovin SF, Higano CS, Tejwani S, Dorff TB, Stankevich E, et al. Phase I trial of ipilimumab (IPI) alone and in combination with radiotherapy (XRT) in patients with metastatic castration resistant prostate cancer (mCRPC) J Clin Oncol 26; 15s. 2008 suppl; abstr 5004. [Google Scholar]
- 9.Berman DM, Wolchok J, Weber J, Hamid O, O'Day S, Chasalow SD. Association of peripheral blood absolute lymphocyte count (ALC) and clinical activity in patients (pts) with advanced melanoma treated with ipilimumab. J Clin Oncol 27:15s. 2009 (suppl; abstr 3020. [Google Scholar]
- 10.Schreiber RD, Old LJ, Smyth MJ. Cancer immunoediting: integrating immunity's roles in cancer suppression and promotion. Science. 2011;331:1565–1570. doi: 10.1126/science.1203486. [DOI] [PubMed] [Google Scholar]
- 11.Fridman WH, Pages F, Sautes-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer. 2012;12:298–306. doi: 10.1038/nrc3245. [DOI] [PubMed] [Google Scholar]
- 12.Ulloa-Montoya F, Louahed J, Dizier B, Gruselle O, Spiessens B, Lehmann FF, et al. Predictive gene signature in MAGE-A3 antigen-specific cancer immunotherapy. J Clin Oncol. 2013;31:2388–2395. doi: 10.1200/JCO.2012.44.3762. [DOI] [PubMed] [Google Scholar]
- 13.Kwek SS, Dao V, Roy R, Hou Y, Alajajian D, Simko JP, et al. Diversity of antigen-specific responses induced in vivo with CTLA-4 blockade in prostate cancer patients. J Immunol. 2012;189:3759–3766. doi: 10.4049/jimmunol.1201529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rendina G, Coon MJ. Enzymatic hydrolysis of the coenzyme a thiol esters of beta-hydroxypropionic and beta-hydroxyisobutyric acids. J Biol Chem. 1957;225:523–534. [PubMed] [Google Scholar]
- 15.Shimomura Y, Murakami T, Fujitsuka N, Nakai N, Sato Y, Sugiyama S, et al. Purification and partial characterization of 3-hydroxyisobutyryl-coenzyme A hydrolase of rat liver. J Biol Chem. 1994;269:14248–14253. [PubMed] [Google Scholar]
- 16.Loupatty FJ, Clayton PT, Ruiter JP, Ofman P, Ijlst L, Brown GK, et al. Mutations in the gene encoding 3-hydroxyisobutyryl-CoA hydrolase results in progressive infantile neurodegeneration. Am J Hum Genet. 2007;80:195–199. doi: 10.1086/510725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baca SC, Prandi D, Lawrence MS, Mosquera JM, Romanel A, Drier Y, et al. Punctuated evolution of prostate cancer genomes. Cell. 2013;153:666–677. doi: 10.1016/j.cell.2013.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barbieri CE, Baca SC, Lawrence MS, Demichelis F, Blattner M, Theurillat JP, et al. Exome sequencing identifies recurrent SPOP, FOXA1 and MED12 mutations in prostate cancer. Nat Genet. 2012;44:685–689. doi: 10.1038/ng.2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grasso CS, Wu YM, Robinson DR, Cao X, Dhanasekaran SM, Khan AP, et al. The mutational landscape of lethal castration-resistant prostate cancer. Nature. 2012;487:239–243. doi: 10.1038/nature11125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Rooij N, van Buuren MM, Philips D, Velds A, Toebes M, Heemskerk B, et al. Tumor exome analysis reveals neoantigen-specific T-cell reactivity in an ipilimumab-responsive melanoma. J Clin Oncol. 2013;31:e439–e442. doi: 10.1200/JCO.2012.47.7521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hinrichs CS, Rosenberg SA. Exploiting the curative potential of adoptive T-cell therapy for cancer. Immunol Rev. 2014;257:56–71. doi: 10.1111/imr.12132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.