Abstract
Background
Total hip arthroplasty (THA) is increasingly being performed in patients with long life expectancies and active lifestyles. Newer implant bearing surfaces, with superior wear characteristics, often are used in this cohort with the goal of improving longevity of the prosthesis, but comparisons across the numerous available bearing surfaces are limited, so the surgeon and patient may have difficulty deciding which implants to use.
Questions/purposes
The purpose of this study was to answer the following question: Is there a short- to mid-term survivorship difference between common THA bearings used in patients younger than age 65 years?
Methods
We conducted a systematic review to identify randomized clinical trials (RCTs) published after 2000 that reported survivorship of ceramic-on-ceramic (CoC), ceramic-on-highly crosslinked polyethylene (CoPxl), or metal-on-highly crosslinked polyethylene (MoPxl) bearings. To qualify for our review, RCTs had to have a minimum 2-year followup and study patients were required to have an average age younger than 65 years. Direct-comparison meta-analysis and network meta-analysis were performed to combine direct and indirect evidence.
Results
Direct-comparison meta-analysis found no differences among the bearing surfaces in terms of the risk of revision; this approach demonstrated a risk ratio for revision of 0.65 (95% confidence interval [CI], 0.19–2.23; p = 0.50) between CoC and CoPxl and a risk ratio for revision of 0.40 (95% CI, 0.06–2.63; p = 0.34) between CoC and MoPxl. Network meta-analysis (with post hoc modification) likewise found no differences in survivorship across the three implant types, demonstrating the following probabilities of most effective implant with 95% credible intervals (CrI): CoC = 64.6% (0%–100%); CoPxl = 24.9% (0%–100%); and MoPxl = 9.9% (0%–100%). The CrIs ranged from 0% to 100% for all three bearing surfaces. Direct-comparison meta-analysis allowed for pooling of five RCTs, including 779 THAs, whereas network meta-analysis (before post hoc analysis) enabled pooling of 18 RCTs, including 2599 THAs.
Conclusions
Current published evidence does not support survivorship differences among commonly used bearing surfaces in patients younger than age 65 years undergoing THA at short- to mid-term followup. Long-term RCT data will be needed to determine if a survivorship benefit is realized in younger, more active patients over time.
Level of Evidence
Level I, therapeutic study.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-4065-0) contains supplementary material, which is available to authorized users.
Introduction
Although the demand for THA is driven largely by an aging population, indications are concomitantly expanding in younger, more active patients [29]. This cohort is challenging because patients are presumed to have a higher activity level and increased life expectancy—both primary risk factors for mechanical failure of the prosthesis [37]. Therefore, use of modern materials with improved wear characteristics such as ceramics, crosslinked polyethylenes, and metal-on-metal (MoM) articulations have become popular options for younger, more active patients undergoing THA [7].
One recent systematic review and meta-analysis compared survivorship among MoM, ceramic-on-ceramic (CoC), and metal-on-polyethylene (MoP) bearings, determining that MoM implants provided superior survivorship in patients younger than 55 years old [47]. However, a substantial body of evidence now suggests that MoM implants are associated with higher complication rates and premature failure than other alternatives [6, 13, 15, 23, 38, 51]. Given the disappointment with MoM bearings, along with technological advances in ceramics and polyethylenes during the last 10 to 15 years [45], we chose to investigate short- to mid-term survivorship of bearings often used today in patients younger than 65 years of age receiving THA.
To do this, we conducted a systematic review and meta-analysis of randomized clinical trials (RCTs) to compare short- to mid-term survivorship among CoC, ceramic-on-highly crosslinked polyethylene (CoPxl), and metal-on-highly crosslinked polyethylene (MoPxl) bearings. Additionally, recognizing that many RCTs have used ceramic-on-conventional polyethylene (CoPc) and metal-on-conventional polyethylene (MoPc) as comparator interventions, a network meta-analysis was performed on all RCTs that included at least one of the bearings of interest to younger, more active patients (Table 1). Traditional meta-analysis is restricted to simple, direct pairwise comparisons of interventions such as “A versus B,” or “B versus C,” or “A versus C.” However, network meta-analysis permits simultaneous comparison of “A versus B versus C.” These more complex data structures can be further strengthened by incorporating trials that examine current interventions of interest (such as CoC, CoPxl, MoPxl; or A, B, C) to historical comparators (ie, CoPc and MoPc; or D, E) in combinations such as “A versus D,” “B versus D,” “C versus D,” “A versus E,” “B versus E,” or “C versus E.” Such methodology allows for more robust analyses by permitting inferences into the comparative effectiveness of interventions that may or may not have been evaluated directly with each other [12, 26, 32, 34, 39, 44]. Network meta-analysis could prove especially valuable in orthopaedics where large RCTs are relatively rare and rapidly changing technology further limits head-to-head investigation of interventional materials.
Table 1.
Comparison of abbreviations for implant bearing surfaces
| Full nomenclature | Abbreviations used in manuscript | Alternative abbreviations in literature |
|---|---|---|
| Ceramic-on-ceramic | CoC | – |
| Ceramic-on-highly crosslinked polyethylene | CoPxl | CoXLPE |
| CoHCLPE | ||
| Metal-on-highly crosslinked polyethylene | MoPxl | MoXLPE |
| MoHCLPE | ||
| Ceramic-on-conventional polyethylene | CoPc | CoUHMWPE |
| CoPE | ||
| Metal-on-conventional polyethylene | MoPc | MoUHMWPE |
| MoPE | ||
| Metal-on-metal | MoM | – |
In this context, we asked the following question: Is there a short- to mid-term survivorship difference between common THA bearings used in patients younger than age 65 years?
Materials and Methods
The protocol for our review was established a priori and adhered to methodology guidelines regarding the conduct of systematic reviews of interventional studies and is reported following the standards proposed by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [35].
We included RCTs that compared survivorship or revision rates between THA bearing surfaces with a minimum 2-year followup. Average patient age at the time of surgery was required to be younger than 65 years. The intervention groups had to include a CoC, CoPxl, or MoPxl bearing. MoM implants were excluded because of decreasing use and a growing body of evidence for premature failure. Additional exclusion criteria were: (1) studies that only used zirconia ceramic components or uncrosslinked polyethylene liners; (2) inclusion of revision THA cases; (3) nonclinical studies (biomechanical, animal, laboratory, cadaver); and (4) reports based only on radiographic followup or component wear.
A medical reference librarian (PE) experienced in searches for systematic reviews developed the search strategy with input from the study investigators. Full contents of the search strategy can be found in Appendix 1 (Supplemental materials are available with the online version of CORR®.). The search was performed using PubMed, Ovid MEDLINE, Ovid EMBASE, and the Web of Science from each database’s inception through January 24, 2014. The initial search on Ovid MEDLINE used the subject headings “hip prosthesis”, “arthroplasty”, “replacement”, and “hip” comparing different types of bearing surfaces using both subject headings and text words (“aluminum oxide” or “alumina” or “ceramic”; “metals” or “metal” or “chromium” or “chromium alloys” or “cobalt”; “polyethylene, highly crosslinked”). Other terms used were: “equipment failure”, “prosthesis failure”, “reoperation”; and specific text words: “durability”, “weightbearing”, “debris”, “wear”, “fracture”, “dislocation”, “revision”, and “stress”, particularly in relation to younger, more active patients. The search was then translated into the terms used in EMBASE or text words used in Web of Science.
Two investigators (CCW, JHJ-A) independently reviewed the titles and abstracts of the 344 articles identified by the systematic literature search. If both reviewers agreed that a study did not meet the eligibility criteria, it was excluded. Eighty-two articles received full-text review by a single investigator (CCW) with 30 of the articles randomly selected for independent review by a second author (JHJ-A). At both stages of selection, we estimated chance-adjusted agreement statistics among reviewers with a κ statistic (κ = 0.917 for abstract review; κ = 1.000 for full-text review), and all disagreements were settled by the opinion of a third senior reviewer (GAN-M). Eleven articles [2, 4, 5, 8, 14, 22, 28, 33, 40, 41, 49] were deemed eligible through this process and seven studies [9, 16–21] were added following a manual search of the bibliographies of the 11 chosen articles for a final study cohort of 18 manuscripts (Fig. 1). Further detail regarding study exclusions can be found in Appendix 2 (Supplemental materials are available with the online version of CORR®.).
Fig. 1.
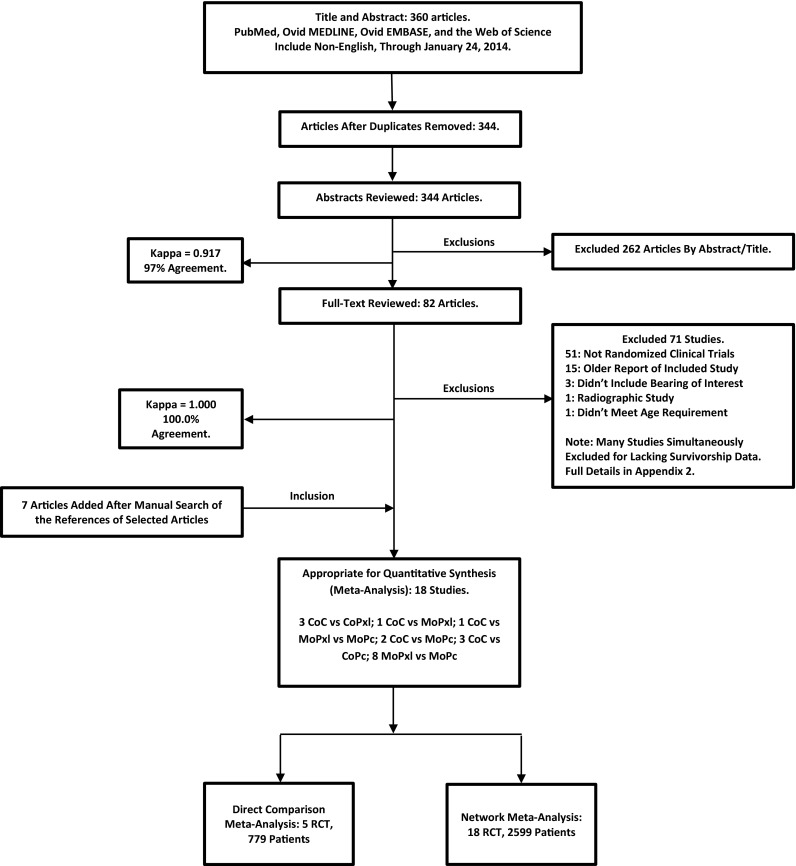
This algorithm details the process of study selection.
Data were extracted from each report and entered into a standardized data extraction spreadsheet. Data points included patient demographics and implant types, number of study participants, number of participants lost to followup, implant revision events, and length of followup period.
We contacted the corresponding author from one report that required data clarification, which was provided after the first attempt [41]. This RCT compared three implant types (CoC, MoPxl, MoPc) and had two patients revised but did not specify which treatment arm was revised. The authors confirmed both of these revision events occurred from patients in the MoPc group.
The implant survivorship or revision rate for any reason at last followup was the sole outcome measure.
The number of THAs and the number requiring revision were used for analysis. Two types of statistical analyses were used for the extracted data. The first was a pairwise direct comparison meta-analysis of three RCTs comparing CoC with CoPxl bearings and two RCTs comparing CoC with MoPxl implants. We reported the risk ratio of revision (meta-analysis metric analogous to relative risk [RR]) with 95% confidence intervals (CIs). The meta-analysis was performed with use of Review Manager (Version 5.2 [2012]; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). We decided a priori that the included studies would likely be homogeneous without accounting for variation in length of followup and thus chose the fixed-effects Mantel-Haenszel model for pooled analyses. No appreciable differences were observed when a random-effects model was tested for comparison. We used the inconsistency index (I2) statistic to assess heterogeneity. The I2 statistic estimates the percentage of variability in results across studies that are explained by true differences in patients, interventions, outcomes, and design rather than by chance; values of 25%, 50%, and 75% indicate low, moderate, and high inconsistency, respectively [24]. The number of studies, participants, and revision events was not large enough to perform a regression that would have accounted for variation in length of followup. Furthermore, as a result of the small number of included RCTs, statistical and visual evaluation of publication bias was not possible with funnel plot techniques [31].
The second statistical comparison involved a network meta-analysis of all 18 RCTs meeting our study eligibility criteria. This complex statistical technique has rarely been used in the orthopaedic literature [25]; thus, we now describe it in detail. We conducted a network meta-analysis to combine direct and indirect comparisons using a random-effects model following Markov chain Monte Carlo methods, as suggested by Lu and Ades [34], which we implemented in WinBUGS 1.4.3 (MRC Biostatistics Unit, Cambridge, UK). We modeled the comparative efficacy of any two implant bearings as a function of each bearing relative to a common comparator. The approach assumes “consistency” of treatment effects across all included trials—that is, the direct and indirect estimates of effect for each pairwise comparison do not disagree beyond chance. We evaluated inconsistency by relating the estimates from the direct comparisons and those from the indirect comparisons for the magnitude and direction of the point estimates and the extent of overlap of CIs. In Bayesian analysis, one can use a prior belief (prior knowledge) that can be updated by new trial data. In this meta-analysis, we did not assume any prior probabilities and limited inference to data derived from the 18 trials (ie, used a noninformative prior distribution). We updated the Markov chain Monte Carlo model with 100,000 simulated draws after a burn in of 1000 iterations. We reported the pairwise RR and 95% credible interval (CrI) with adjustment for multiple-arm trials. We estimated the probability that each implant bearing was the most efficacious regimen (ranked first) by calculating the RR for each bearing compared with an arbitrary common comparison bearing and counting the proportion of iterations of the Markov chain in which each bearing had the largest RR in reducing revision surgery [36].
Two post hoc sensitivity analyses were performed on the network meta-analysis. The first involved exclusion of the only RCT [2] that had significant patient loss to followup over the 5-year study period (38.4%), making it at high risk of bias. The remainder of RCTs all had a loss to followup of less than 20%, suggesting a lower risk of bias as proposed by Sackett [46]. The second sensitivity analysis was performed by excluding all three CoC versus CoPc RCTs, which included the previously censored manuscript from the first sensitivity analysis. Because the original investigation aimed to compare low-wear bearings, it was hypothesized including the three studies in the comparison could potentially confound results because CoPc implants are a hybrid between high-wear conventional polyethylene and modern low-wear ceramic.
The 18 RCTs involved 2599 primary THAs with 72 subsequent revision events. Average followup was 7 years (range, 3–12 years). The investigations included several comparisons: three CoC versus CoPxl, one CoC versus MoPxl, one CoC versus MoPxl versus MoPc, two CoC versus MoPc, eight MoPxl versus MoPc, and three CoC versus CoPc (Table 2) [2, 4, 5, 8, 9, 14, 16–22, 28, 33, 40, 41, 49]. For all comparisons, there was a “Group 1” and “Group 2.” Group 1 represents the first listed cohort in the comparison with Group 2 being the second listed cohort. For example, in CoC versus CoPxl studies, Group 1 are the patients receiving CoC and Group 2 are the patients receiving CoPxl.
Table 2.
Summary of included RCTs in network meta-analysis
| RCT (first author, year of publication) | Followup (years) | Number of patients in Group 1 | Number of revisions in Group 1 | Number of patients in Group 2 | Number of revisions in Group 2 |
|---|---|---|---|---|---|
| CoC versus CoPxl | |||||
| Kim, 2013 [28] | 12 | 100 | 1 | 100 | 1 |
| Beaupre, 2013 [5] | 5 | 48 | 0 | 44 | 2 |
| Hamilton, 2010 [22] | 3 | 177 | 4 | 87 | 2 |
| CoC versus MoPxl | |||||
| Nikolaou, 2012* [41] | 5 | 34 | 0 | 32 | 0 |
| Bascarevic, 2010 [4] | 4 | 82 | 0 | 75 | 2 |
| CoC versus MoPc | |||||
| Venditolli, 2013 [49] | 12 | 71 | 1 | 69 | 8 |
| D’Antonio, 2012 [14] | 10 | 194 | 6 | 95 | 10 |
| Nikolaou, 2012* [41] | 5 | 34 | 0 | 36 | 1 |
| MoPxl versus MoPc | |||||
| Garcia-Rey, 2013 [19] | 10 | 45 | 1 | 45 | 0 |
| Geerdink, 2009 [21] | 8 | 22 | 0 | 26 | 1 |
| Engh, 2006 [18] | 6 | 116 | 0 | 114 | 2 |
| Mutimer, 2010 [40] | 6 | 55 | 0 | 55 | 3 |
| Nikolaou, 2012* [41] | 5 | 32 | 0 | 36 | 2 |
| Digas, 2007 [16] | 5 | 32 | 0 | 29 | 0 |
| Digas, 2004 [17] | 5 | 19 | 1 | 19 | 0 |
| Geerdink, 2006 [20] | 5 | 66 | 0 | 67 | 2 |
| Calvert, 2009 [9] | 3 | 59 | 0 | 60 | 0 |
| CoC versus CoPc | |||||
| Lewis, 2010 [33] | 10 | 30 | 1 | 26 | 1 |
| Amanatullah, 2011 [2] | 5 | 196 | 11 | 161 | 3 |
| Cai, 2012 [8] | 4 | 51 | 2 | 62 | 3 |
* Nikolaou investigated CoC versus MoPxl versus MoPc. Pairwise comparisons are shown; RCT = randomized, controlled trials; CoC = ceramic-on-ceramic; CoPxl = ceramic-on-highly crosslinked polyethylene; MoPxl = metal-on-highly crosslinked polyethylene; CoPc = ceramic-on-conventional polyethylene; MoPc = metal-on-highly crosslinked polyethylene; “Group 1” represents the first listed cohort in the comparison with “Group 2” being the second listed cohort. For example, in CoC versus CoPxl studies, Group 1 is the CoC patients and Group 2 is the CoPxl patients. Followup was the mean reported for each individual study.
Results
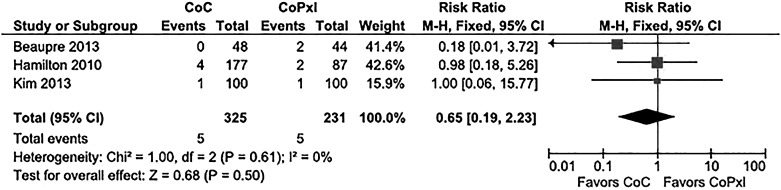
No differences in the risk of revision among bearing types were observed with direct-comparison meta-analysis. Furthermore, both direct-comparison meta-analyses demonstrated low heterogeneity among included studies. The first meta-analysis was performed for the three RCTs directly comparing CoC versus CoPxl implants. The pooled risk ratio for revision was 0.65 (95% CI, 0.19–2.23; p = 0.50). Assessment for heterogeneity was performed with a chi-square result of 1.00 (degrees of freedom [df] = 2; p = 0.61; I2 equal to 0%; Fig. 2). The second meta-analysis was performed for the two RCTs directly comparing CoC versus MoPxl implants. The pooled risk ratio for revision was 0.39 (95% CI, 0.06–2.69; p = 0.34). Assessment for heterogeneity revealed a chi square result of 0.63 (df = 1; p = 0.43; I2 equal to 0%; Fig. 3).
Fig. 2.
This is a direct-comparison meta-analysis with a forest plot of the RRs for revision of CoC versus CoPxl bearings. The horizontal bars represent the CIs for individual studies, and the black diamond represents the cumulative risk ratio of the set of studies. The black diamond crosses the vertical line, indicating no statistical difference in risk of bearing failure between the groups. M-H = Mantel-Haenszel.
Fig. 3.
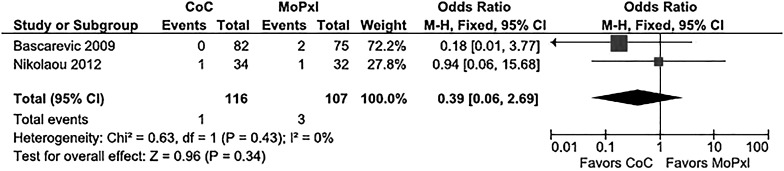
This is a direct-comparison meta-analysis with a forest plot of the RRs for revision of CoC versus MoPxl bearings. The horizontal bars represent the CIs for individual studies, and the black diamond represents the cumulative RR for the set of studies. The black diamond crosses the vertical line, indicating no statistical difference in risk of bearing failure between the groups. M-H = Mantel-Haenszel.
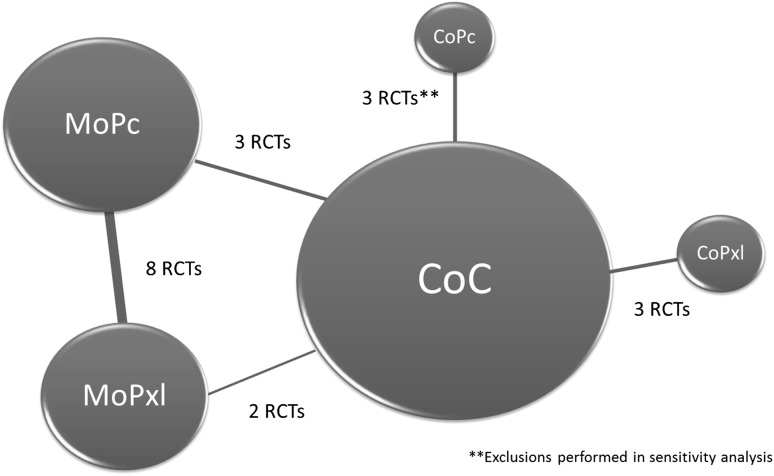
A network meta-analysis was performed after developing a linkage system of direct and indirect comparisons for all 18 RCTs (Fig. 4). No difference in performance was observed among CoC, CoPxl, MoPxl, and CoPc implants with all being superior to MoPc (metal-on-conventional polyethylene) implants. Network meta-analyses aim to test if superiority exists for one of the comparator interventions. The statistical outcome of this metric is a “probability of being the most efficacious intervention” with 95% CrIs [12, 26, 32, 34, 39, 44]. Interventions can then be ranked by their probabilities; however, overlapping CrIs indicate that a statistical difference was not detected. Analysis from our network meta-analysis showed the following probabilities of being ranked the most effective intervention with 95% CrIs: CoC = 18.8% (0%–100%), CoPxl = 13.2% (0%–100%), MoPxl = 4.9% (0%–100%), CoPc = 63.0% (0%–100%), MoPc = 0% (0%–0%). The RRs of revision surgery with lower level and upper level 95% CrIs were also calculated for each pairwise comparison (Table 3).
Fig. 4.
This is a schematic of the constructed linkage system enabling a network meta-analysis to be performed on all 18 RCTs. The CoPc studies were excluded for the sensitivity analyses. Circle size is proportional to the number of hips receiving each implant type and line thickness is proportional to the number of RCTs.
Table 3.
Network meta-analysis of 18 RCTs
| Bearing surface | Probability of being ranked most effective (%) | Lower level 95% credible interval (%) | Upper level 95% credible interval (%) |
|---|---|---|---|
| CoC | 18.8 | 0 | 100 |
| CoPxl | 13.2 | 0 | 100 |
| MoPxl | 4.9 | 0 | 100 |
| CoPc | 63.0 | 0 | 100 |
| MoPc | 0 | 0 | 0 |
| Bearing surface comparison | Relative risk of revision surgery | Lower level 95% credible interval (%) | Upper level 95% credible interval (%) |
|---|---|---|---|
| CoC versus CoPxl | 1.97 | 0.19 | 44.87 |
| CoC versus MoPxl | 3.82 | 0.40 | 148.80 |
| CoC versus CoPc | 0.61 | 0.07 | 7.55 |
| CoC versus MoPc | 9.33 | 1.78 | 285.2 |
| CoPxl versus MoPxl | 4.88 | 0.05 | 134.7 |
| CoPxl versus CoPc | 0.31 | 0.01 | 8.59 |
| CoPxl versus MoPc | 4.88 | 0.20 | 281.3 |
| MoPxl versus CoPc | 0.16 | 0.01 | 3.69 |
| MoPxl versus MoPc | 2.49 | 0.40 | 21.54 |
| MoPc versus CoPc | 0.06 | 0.01 | 0.10 |
RCT = randomized clinical trial; CoC = ceramic-on-ceramic; CoPxl = ceramic-on-highly crosslinked polyethylene; MoPxl = metal-on-highly crosslinked polyethylene; CoPc = ceramic-on-conventional polyethylene; MoPc = metal-on-conventional polyethylene.
Two sensitivity analyses were performed by recalculating the network results after study exclusions. Both confirmed the findings that performance was no different among CoC, CoPxl, MoPxl, and CoPc implants with all being superior to MoPc. The first analysis was executed after exclusion of one study with significant patient loss to followup with the following probabilities of being ranked the most effective intervention: CoC = 36.7% (0%–100%), CoPxl = 18% (0%–100%), MoPxl = 6.8% (0%–100%), CoPc = 38.3% (0%–100%), MoPc = 0% (0%–0%). The RRs of revision surgery with lower level and upper level 95% CrIs were also calculated for each pairwise comparison (Table 4). The second sensitivity analysis was conducted after removing all three studies comparing CoC versus CoPc, and the probabilities of being ranked the most effective intervention were: CoC = 64.6% (0%–100%), CoPxl = 24.9% (0%–100%), MoPxl = 9.9% (0%–100%), MoPc = 0% (0%–0%). The RRs of revision surgery with lower level and upper level 95% CrIs were also calculated for each pairwise comparison (Table 5). Like with the first sensitivity analysis, no statistically significant changes were observed from the primary analysis.
Table 4.
Network meta-analysis excluding RCT with significant loss to followup
| Bearing surface | Probability of being ranked most effective (%) | Lower level 95% credible interval (%) | Upper level 95% credible interval (%) |
|---|---|---|---|
| CoC | 36.7 | 0 | 100 |
| CoPxl | 18 | 0 | 100 |
| MoPxl | 6.8 | 0 | 100 |
| CoPc | 38.3 | 0 | 100 |
| MoPc | 0 | 0 | 0 |
| Bearing surface comparison | Relative risk of revision surgery | Lower level 95% credible interval (%) | Upper level 95% credible interval (%) |
|---|---|---|---|
| CoC versus CoPxl | 2.1 | 0.2 | 75.3 |
| CoC versus MoPxl | 4.1 | 0.4 | 294.0 |
| CoC versus CoPc | 1.2 | 0.0 | 43.2 |
| CoC versus MoPc | 10.1 | 1.5 | 552.1 |
| CoPxl versus MoPxl | 2.0 | 0.0 | 257.4 |
| CoPxl versus CoPc | 0.6 | 0.0 | 40.7 |
| CoPxl versus MoPc | 5.0 | 0.1 | 545.2 |
| MoPxl versus CoPc | 0.3 | 0.0 | 16.6 |
| MoPxl versus MoPc | 2.5 | 0.3 | 26.8 |
| MoPc versus CoPc | 0.1 | 0.0 | 4.5 |
RCT = randomized clinical trial; CoC = ceramic-on-ceramic; CoPxl = ceramic-on-highly crosslinked polyethylene; MoPxl = metal-on-highly crosslinked polyethylene; CoPc = ceramic-on-conventional polyethylene; MoPc = metal-on-highly crosslinked polyethylene.
Table 5.
Network meta-analysis excluding all CoPc RCTs*
| Bearing surface | Probability of being ranked most effective (%) | Lower level 95% credible interval (%) | Upper level 95% credible interval (%) |
|---|---|---|---|
| CoC | 64.6 | 0 | 100 |
| CoPxl | 24.9 | 0 | 100 |
| MoPxl | 9.9 | 0 | 100 |
| MoPc | 0 | 0 | 0 |
| Bearing surface comparison | Relative risk of revision surgery | Lower level 95% credible interval (%) | Upper level 95% credible interval (%) |
|---|---|---|---|
| CoC versus CoPxl | 2.3 | 0.1 | 179.7 |
| CoC versus MoPxl | 5.2 | 0.3 | 780.2 |
| CoC versus MoPc | 13.3 | 1.3 | 1562 |
| CoPxl versus MoPxl | 2.3 | 0.0 | 748.7 |
| CoPxl versus MoPc | 5.9 | 0.1 | 1720 |
| MoPxl versus MoPc | 2.6 | 0.2 | 48.4 |
* Excludes three trials; CoPc = ceramic-on-conventional polyethylene; RCT = randomized clinical trial; CoC = ceramic-on-ceramic; CoPxl = ceramic-on-highly crosslinked polyethylene; MoPxl = metal-on-highly crosslinked polyethylene; MoPc = metal-on-highly crosslinked polyethylene.
Discussion
As more patients undergo THA each year [29], and the average age of patients undergoing THA gets younger [30], our specialty will need to continue to focus on improving the durability of the implants we use. Modern implants with improved wear characteristics include CoC, CoPxl, MoPxl, and MoM. One recent systematic review and meta-analysis determined that MoM was the superior bearing for younger, more active patients based on survivorship [47]. However, with the substantial body of evidence suggesting poor performance of MoM implants, and with advances in contemporary ceramics and crosslinked polyethylenes, survivorship of implants with improved wear characteristics deserves a fresh examination of the published evidence. The optimal methodological tool for this question is network meta-analysis because it enables pooling of data from both direct and indirect comparisons [12, 26, 32, 34, 39, 44]. This is an especially important consideration in the orthopaedic literature because RCTs are rare, relatively small, and infrequently compare all interventions of interest simultaneously. Therefore, the aim of our investigation was to perform a systematic review and network meta-analysis of RCTs to compare short- with mid-term survivorship among CoC, CoPxl, and MoPxl bearings in patients younger than age 65 years.
Our findings must be taken in light of several limitations. First, there was heterogeneity in the length of followup among the RCTs in our study. To maximize the number of eligible RCTs, a cutoff was set in the study protocol for a minimum 2-year followup, which resulted in a mean followup of 7 years (range, 3–12 years). Second, the small number of events (only 72 revisions) created a level of imprecision for the point estimates. Although network meta-analysis allowed for an increase of RCTs and patients (from five to 18 and from 799 to 2599, respectively), the persistently wide confidence and credible intervals indicate that the possibility of a Type II statistical error remains. Furthermore, because of the lack of revision events, we could not adequately subclassify by reason for revision, leaving revision resulting from any cause as our primary endpoint. Other important outcomes such as patient pain, functionality, and implant-specific issues (like squeaking or corrosion) were not assessed and require future study, optimally in large RCTs. Lastly, our data represent short- to mid-term survivorship among bearings that were designed for longevity. Long-term RCT data and subsequent systematic reviews will be needed to assess if differences in survivorship among bearings present over time.
The limitations of our study highlight important deficits within the current standard of orthopaedic evidence. Our systematic review demonstrated a scarcity of large RCTs comparing implant bearings. Furthermore, many of the RCTs already have significant loss to followup, which will decrease their ability to make useful comments about long-term outcomes in the future. These RCTs also lacked depth of reporting in many cases. In particular, more uniform inclusion of time-to-event, safety, functional scores, and patient reported outcome data will be mandatory moving forward to provide consistently useful information. As a specialty, orthopaedics can derive greater understanding about new devices, implants, and technologies with the initiation of large, well-designed RCTs; otherwise, decisions for patient care will be driven by forms of evidence with higher potential for bias and heterogeneity such as retrospective reviews and registry data. Both forms of evidence are still extremely important sources of information and should be scrutinized in conjunction with results from RCTs and meta-analyses. For example, the Australian Orthopaedic Association National Joint Replacement Registry has acquired data on more than 165,000 THAs, including the bearing surfaces evaluated in our review, with more than 10 years of followup. The Australian Registry data show a 10-year revision rate of 4.8% for CoC bearings, 5.1% for CoPxl, and 4.5% for MoPxl [3]. There is no significant difference between survivorship of any bearing couple at 10 years, which corroborates the results of our study.
Collectively, our study results suggest that all three commonly used bearings perform similarly in younger, more active patients at short- to mid-term followup and that all likely have superior longevity compared with historical MoPc bearings. Our results showed no differences among CoC, CoPxl, MoPxl, and CoPc based on the credible intervals for all of these ranging from 0% to 100% (Tables 3–5). However, the credible interval for MoPc in all analyses was from 0% to 0%, suggesting inferiority in comparison to the other four bearing surfaces. Both pairwise, direct-comparison meta-analysis and network meta-analysis demonstrated no statistically significant differences in mid-term survivorship among CoC, CoPxl, and MoPxl implants. Network meta-analysis also showed no difference in survivorship of CoPc implants compared with CoC, CoPxl, and MoPxl; however, the inferiority of MoPc implants compared with all other types was demonstrated. Given the hybrid nature of CoPc bearings (low-wear ceramic coupled with high-wear conventional polyethylene), a sensitivity analysis was conducted by recalculation after excluding studies that examined CoPc implants. No statistical differences were seen from baseline results. A second sensitivity analysis was conducted after excluding one study, which had substantial loss to followup [2], and the results of our analyses did not change.
Our study represents the most comprehensive synthesis of short- to mid-term, level I survivorship data in the literature on commonly used bearings in younger, more active patients undergoing THA. To our knowledge, no other study has performed a meta-analysis comparing survivorship of modern CoC, CoPxl, and MoPxl implants in patients younger than 65 years of age. One recent meta-analysis investigated MoM, CoC, and MoPc implants, concluding superior survivorship of MoM implants in patients younger than 55 years of age [45]. However, that study did not apply rigorous PRISMA and Cochrane guidelines for meta-analyses and further did not compare the most common bearing surfaces being used in current practice. Therefore, a new synthesis of the data was needed of published RCTs on this topic for comparison with outcomes in the peer-reviewed literature from other sources of evidence such as registries and retrospective reviews. A traditional systematic review and meta-analysis would have only allowed for pooling of the three identified RCTs comparing CoC versus CoPxl and the two identified RCTs comparing CoC versus MoPxl. These evaluations were important to our investigation, yet a much more comprehensive and precise set of data synthesis was achieved through the use of network meta-analysis. This challenging technique is rarely described in the orthopaedic literature [25], but could certainly supplement evidence-based studies in the field [12, 26, 32, 34, 39, 44]. From the network approach, we were able to increase the number of included RCTs from five to 18 and the number of included THAs from 779 to 2599 by a series of direct and indirect statistical comparisons. We believe this strengthens the interpretation of our data for surgeons making evidence-based decisions on which bearing surface to use in their younger, more active patients.
With minimal if any differences observed in survivorship among CoC, CoPxl, and MoPxl bearings, it may be prudent to place greater emphasis on other factors in the decision-making process, namely cost and implant-specific complications. Implant costs vary widely among countries and individual healthcare facilities; however, the relationship is consistent with the price of CoC being higher than the price of CoPxl, which is higher than the price of MoPxl [7]. The economic impact of these decisions on the individual patient, provider, and hospital, up to the level of payers and societies, will be important to consider moving forward. There are also complications specific to some implants. Squeaking has been well documented in CoC components; however, specific risk factors remain in debate [27, 42, 48]. Ceramic liners can also fracture during surgical implantation, which leads to a wasted expensive implant [50]. Postoperative fracture of ceramics, although rare with recent material advancements, has been reported with CoC being at greatest risk [1]. Finally, MoPxl may be the most important group to monitor over the coming decade. Adverse reactions to metal debris were once thought to be a phenomenon limited to MoM implants; however, recent reports have raised concern in MoPxl bearings for taper junction trunnionosis [10, 11, 43]. Increased awareness of trunnionosis may necessitate monitoring of serum metal levels in addition to ultrasound or metal artifact reduction sequencing MRI in the painful MoPxl THA according to a contemporary consensus statement algorithm from multiple orthopaedic specialty societies [30].
In conclusion, our systematic review and network meta-analysis has demonstrated similar short- to mid-term survivorship among CoC, CoPxl, and MoPxl bearings in patients younger than 65 years of age. Attributable in large part to the network meta-analysis technique, this represents the most comprehensive summary of the available evidence of which we are aware. Although surgeons should remain cautious until long-term RCT data become available, the short- to mid-term experience supports comparable performance among the implants. In light of this information, decision-makers may choose to focus on other factors such as cost and implant-specific complications when debating which implant to use in younger, more active patients undergoing THA. Furthermore, because large RCT data with long-term followup are relatively limited in orthopaedics, the network meta-analysis technique could provide an important tool for raising the quality of evidence derived from systematic reviews moving forward.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
We thank Dr Victor Montori and Dr Colin West for their contributions to the methodology used in our investigation; Ms Patricia Erwin for her assistance in defining the search strategy for the systematic review; and Ms Karen Fasbender for her support in manuscript preparation.
Footnotes
The authors received funding from CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences, a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH. The institution of one or more of the authors (RJS, RTT) has received, during the study period, funding from DePuy Orthopaedics, Inc (Warsaw, IN, USA), Wright Medical Technology, Inc (Arlington, TN, USA), MAKO Surgical Corp (Ft Lauderdale, FL, USA), and Biomet Inc (Warsaw, IN, USA). One of the authors certifies that he (RTT), or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of less than USD 10,000 from MAKO Surgical Corp, USD 10,000 to USD 100,000 from DePuy Orthopaedics, Inc, and less than USD 10,000 from Wright Medical Technology, Inc. One of the authors certifies that he (RJS), or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Biomet Inc.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
References
- 1.Abdel MP, Heyse TJ, Elpers ME, Mayman DJ, Su EP, Pellicci PM, Wright TM, Padgett DE. Ceramic liner fractures presenting as squeaking after primary total hip arthroplasty. J Bone Joint Surg Am. 2014;96:27–31. doi: 10.2106/JBJS.M.00737. [DOI] [PubMed] [Google Scholar]
- 2.Amanatullah DF, Landa J, Strauss EJ, Garino JP, Kim SH, Di Cesare PE. Comparison of surgical outcomes and implant wear between ceramic-ceramic and ceramic-polyethylene articulations in total hip arthroplasty. J Arthroplasty. 2011;26:72–77. doi: 10.1016/j.arth.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 3.AOANJR–Australian Orthopaedic Association National Joint Registry. Annual Report 2013. 2013. Available at: https://aoanjrr.dmac.adelaide.edu.au/en/annual-reports-2013. Accessed July 15, 2014.
- 4.Bascarevic Z, Vukasinovic Z, Slavkovic N, Dulic B, Trajkovic G, Bascarevic V, Timotijevic S. Alumina-on-alumina ceramic versus metal-on-highly cross-linked polyethylene bearings in total hip arthroplasty: a comparative study. Int Orthop. 2010;34:1129–1135. doi: 10.1007/s00264-009-0899-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beaupre LA, Manolescu A, Johnston DW. A randomized trial of ceramic-on-ceramic bearing versus ceramic-on-crossfire-polyethylene bearing in total hip arthroplasty: five-year outcomes. J Arthroplasty. 2013;28:485–489. doi: 10.1016/j.arth.2012.07.027. [DOI] [PubMed] [Google Scholar]
- 6.Bozic KJ, Lau EC, Ong KL, Vail TP, Rubash HE, Berry DJ. Comparative effectiveness of metal-on-metal and metal-on-polyethylene bearings in Medicare total hip arthroplasty patients. J Arthroplasty. 2012;27:37–40. doi: 10.1016/j.arth.2012.03.031. [DOI] [PubMed] [Google Scholar]
- 7.Bozic KJ, Morshed S, Silverstein MD, Rubash HE, Kahn JG. Use of cost-effectiveness analysis to evaluate new technologies in orthopaedics. The case of alternative bearing surfaces in total hip arthroplasty. J Bone Joint Surg Am. 2006;88:706–714. doi: 10.2106/JBJS.E.00614. [DOI] [PubMed] [Google Scholar]
- 8.Cai P, Hu Y, Xie J. Large-diameter Delta ceramic-on-ceramic versus common-sized ceramic-on-polyethylene bearings in THA. Orthopedics. 2012;35:e1307–e1313. doi: 10.3928/01477447-20120822-14. [DOI] [PubMed] [Google Scholar]
- 9.Calvert GT, Devane PA, Fielden J, Adams K, Horne JG. A double-blind, prospective, randomized controlled trial comparing highly cross-linked and conventional polyethylene in primary total hip arthroplasty. J Arthroplasty. 2009;24:505–510. doi: 10.1016/j.arth.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 10.Cooper HJ. Della Valle CJ, Berger RA, Tetreault M, Paprosky WG, Sporer SM, Jacobs JJ. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94:1655–1661. doi: 10.2106/JBJS.K.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper HJ, Urban RM, Wixson RL, Meneghini RM, Jacobs JJ. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am. 2013;95:865–872. doi: 10.2106/JBJS.L.01042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cope S, Jansen JP. Quantitative summaries of treatment effect estimates obtained with network meta-analysis of survival curves to inform decision-making. BMC Med Res Methodol. 2013;13:147. doi: 10.1186/1471-2288-13-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cuckler JM. Metal-on-metal surface replacement: a triumph of hope over reason: affirms. Orthopedics. 2011;34:e439–e441. doi: 10.3928/01477447-20110714-21. [DOI] [PubMed] [Google Scholar]
- 14.D’Antonio JA, Capello WN, Naughton M. Ceramic bearings for total hip arthroplasty have high survivorship at 10 years. Clin Orthop Relat Res. 2012;470:373–381. doi: 10.1007/s11999-011-2076-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Steiger RN, Hang JR, Miller LN, Graves SE, Davidson DC. Five-year results of the ASR XL Acetabular System and the ASR Hip Resurfacing System: an analysis from the Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg Am. 2011;93:2287–2293. doi: 10.2106/JBJS.J.01727. [DOI] [PubMed] [Google Scholar]
- 16.Digas G, Karrholm J, Thanner J, Herberts P. 5-year experience of highly cross-linked polyethylene in cemented and uncemented sockets: two randomized studies using radiostereometric analysis. Acta Orthop. 2007;78:746–754. doi: 10.1080/17453670710014518. [DOI] [PubMed] [Google Scholar]
- 17.Digas G, Karrholm J, Thanner J, Malchau H, Herberts P. The Otto Aufranc Award. Highly cross-linked polyethylene in total hip arthroplasty: randomized evaluation of penetration rate in cemented and uncemented sockets using radiostereometric analysis. Clin Orthop Relat Res. 2004;429:6–16. doi: 10.1097/01.blo.0000150314.70919.e3. [DOI] [PubMed] [Google Scholar]
- 18.Engh CA, Jr, Stepniewski AS, Ginn SD, Beykirch SE, Sychterz-Terefenko CJ, Hopper RH, Jr, Engh CA. A randomized prospective evaluation of outcomes after total hip arthroplasty using cross-linked marathon and non-cross-linked Enduron polyethylene liners. J Arthroplasty. 2006;21:17–25. doi: 10.1016/j.arth.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Garcia-Rey E, Garcia-Cimbrelo E, Cruz-Pardos A. New polyethylenes in total hip replacement. J Bone Joint Surg Br. 2013;95:326–332. doi: 10.1302/0301-620X.95B3.29456. [DOI] [PubMed] [Google Scholar]
- 20.Geerdink CH, Grimm B, Ramakrishnan R, Rondhuis J, Verburg AJ, Tonino AJ. Crosslinked polyethylene compared to conventional polyethylene in total hip replacement: pre-clinical evaluation, in-vitro testing and prospective clinical follow-up study. Acta Orthop. 2006;77:719–725. doi: 10.1080/17453670610012890. [DOI] [PubMed] [Google Scholar]
- 21.Geerdink CH, Grimm B, Vencken W, Heyligers IC, Tonino AJ. Cross-linked compared with historical polyethylene in THA: an 8-year clinical study. Clin Orthop Relat Res. 2009;467:979–984. doi: 10.1007/s11999-008-0628-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hamilton WG, McAuley JP, Dennis DA, Murphy JA, Blumenfeld TJ, Politi J. THA with Delta ceramic on ceramic: results of a multicenter investigational device exemption trial [Erratum in Clin Orthop Relat Res. 2010;468:909] Clin Orthop Relat Res. 2010;468:358–366. doi: 10.1007/s11999-009-1091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hasegawa M, Yoshida K, Wakabayashi H, Sudo A. Prevalence of adverse reactions to metal debris following metal-on-metal THA. Orthopedics. 2013;36:e606–e612. doi: 10.3928/01477447-20130426-23. [DOI] [PubMed] [Google Scholar]
- 24.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ibrahim T, Qureshi A, Sutton AJ, Dias JJ. Surgical versus nonsurgical treatment of acute minimally displaced and undisplaced scaphoid waist fractures: pairwise and network meta-analyses of randomized controlled trials. J Hand Surg Am. 2011;36(1759–1768):e1751. doi: 10.1016/j.jhsa.2011.08.033. [DOI] [PubMed] [Google Scholar]
- 26.Jansen JP, Naci H. Is network meta-analysis as valid as standard pairwise meta-analysis? It all depends on the distribution of effect modifiers. BMC Med. 2013;11:159. doi: 10.1186/1741-7015-11-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jarrett CA, Ranawat AS, Bruzzone M, Blum YC, Rodriguez JA, Ranawat CS. The squeaking hip: a phenomenon of ceramic-on-ceramic total hip arthroplasty. J Bone Joint Surg Am. 2009;91:1344–1349. doi: 10.2106/JBJS.F.00970. [DOI] [PubMed] [Google Scholar]
- 28.Kim YH, Park JW, Kulkarni SS, Kim YH. A randomised prospective evaluation of ceramic-on-ceramic and ceramic-on-highly cross-linked polyethylene bearings in the same patients with primary cementless total hip arthroplasty. Int Orthop. 2013;37:2131–2137. doi: 10.1007/s00264-013-2036-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kwon YM, Lombardi AV, Jacobs JJ, Fehring TK, Lewis CG, Cabanela ME. Risk stratification algorithm for management of patients with metal-on-metal hip arthroplasty: consensus statement of the American Association of Hip and Knee Surgeons, the American Academy of Orthopaedic Surgeons, and the Hip Society. J Bone Joint Surg Am. 2014;96:e4. doi: 10.2106/JBJS.M.00160. [DOI] [PubMed] [Google Scholar]
- 31.Lau J, Ioannidis JP, Terrin N, Schmid CH, Olkin I. The case of the misleading funnel plot. BMJ. 2006;333:597–600. doi: 10.1136/bmj.333.7568.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laws A, Kendall R, Hawkins N. A comparison of national guidelines for network meta-analysis. Value Health. 2014;17:642–654. doi: 10.1016/j.jval.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 33.Lewis PM, Al-Belooshi A, Olsen M, Schemitch EH, Waddell JP. Prospective randomized trial comparing alumina ceramic-on-ceramic with ceramic-on-conventional polyethylene bearings in total hip arthroplasty. J Arthroplasty. 2010;25:392–397. doi: 10.1016/j.arth.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 34.Li T, Puhan MA, Vedula SS, Singh S, Dickersin K. Network meta-analysis-highly attractive but more methodological research is needed. BMC Med. 2011;9:79. doi: 10.1186/1741-7015-9-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151:W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 36.Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23:3105–3124. doi: 10.1002/sim.1875. [DOI] [PubMed] [Google Scholar]
- 37.Malchau H, Herberts P, Eisler T, Garellick G, Soderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am. 2002;84(Suppl 2):2–20. doi: 10.2106/00004623-200200002-00002. [DOI] [PubMed] [Google Scholar]
- 38.Melvin JS, Karthikeyan T, Cope R, Fehring TK. Early failures in total hip arthroplasty–a changing paradigm. J Arthroplasty. 2014;29:1285–1288. doi: 10.1016/j.arth.2013.12.024. [DOI] [PubMed] [Google Scholar]
- 39.Mills EJ, Thorlund K, Ioannidis JP. Demystifying trial networks and network meta-analysis. BMJ. 2013;346:f2914. doi: 10.1136/bmj.f2914. [DOI] [PubMed] [Google Scholar]
- 40.Mutimer J, Devane PA, Adams K, Horne JG. Highly crosslinked polyethylene reduces wear in total hip arthroplasty at 5 years. Clin Orthop Relat Res. 2010;468:3228–3233. doi: 10.1007/s11999-010-1379-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nikolaou VS, Edwards MR, Bogoch E, Schemitsch EH, Waddell JP. A prospective randomised controlled trial comparing three alternative bearing surfaces in primary total hip replacement. J Bone Joint Surg Br. 2012;94:459–465. doi: 10.1302/0301-620X.94B4.27735. [DOI] [PubMed] [Google Scholar]
- 42.Owen DH, Russell NC, Smith PN, Walter WL. An estimation of the incidence of squeaking and revision surgery for squeaking in ceramic-on-ceramic total hip replacement: a meta-analysis and report from the Australian Orthopaedic Association National Joint Registry. Bone Joint J. 2014;96:181–187. doi: 10.1302/0301-620X.96B2.32784. [DOI] [PubMed] [Google Scholar]
- 43.Pastides PS, Dodd M, Sarraf KM, Willis-Owen CA. Trunnionosis: a pain in the neck. World J Orthop. 2013;4:161–166. doi: 10.5312/wjo.v4.i4.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Puhan MA, Schunemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, Kessels AG, Guyatt GH. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630. doi: 10.1136/bmj.g5630. [DOI] [PubMed] [Google Scholar]
- 45.Rajpura A, Kendoff D, Board TN. The current state of bearing surfaces in total hip replacement. Bone Joint J. 2014;96:147–156. doi: 10.1302/0301-620X.96B2.31920. [DOI] [PubMed] [Google Scholar]
- 46.Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shetty V, Shitole B, Shetty G, Thakur H, Bhandari M. Optimal bearing surfaces for total hip replacement in the young patient: a meta-analysis. Int Orthop. 2011;35:1281–1287. doi: 10.1007/s00264-010-1104-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Su EP. Ceramic-ceramic bearing: too unpredictable to use it regularly. HSS J. 2012;8:287–290. doi: 10.1007/s11420-012-9289-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vendittoli PA, Riviere C, Lavigne M, Lavoie P, Alghamdi A, Duval N. Alumina on alumina versus metal on conventional polyethylene: a randomized clinical trial with 9 to 15 years follow-up. Acta Orthop Belg. 2013;79:181–190. [PubMed] [Google Scholar]
- 50.Viste A, Chouteau J, Desmarchelier R, Fessy MH. Fractures of a sandwich ceramic liner at ten year follow-up. Int Orthop. 2012;36:955–960. doi: 10.1007/s00264-011-1375-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wyles CC, Van Demark RE 3rd, Sierra RJ, Trousdale RT. High rate of infection after aseptic revision of failed metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2014;472:509–516. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.