Abstract
Background
As part of a comprehensive nonsurgical approach, epidural injections often are used in the management of lumbar disc herniation. Recent guidelines and systematic reviews have reached different conclusions about the efficacy of epidural injections in managing lumbar disc herniation.
Questions/purposes
In this systematic review, we determined the efficacy (pain relief and functional improvement) of the three anatomic approaches (caudal, lumbar interlaminar, and transforaminal) for epidural injections in the treatment of disc herniation.
Methods
We performed a literature search from 1966 to June 2013 in PubMed, Cochrane library, US National Guideline Clearinghouse, previous systematic reviews, and cross-references for trials studying all types of epidural injections in managing chronic or chronic and subacute lumbar disc herniation. We wanted only randomized controlled trials (RCTs) (either placebo or active controlled) to be included in our analysis, and 66 studies found in our search fulfilled these criteria. We then assessed the methodologic quality of these 66 studies using the Cochrane review criteria for RCTs. Thirty-nine studies were excluded, leaving 23 RCTs of high and moderate methodologic quality for analysis. Evidence for the efficacy of all three approaches for epidural injection under fluoroscopy was strong for short-term (< 6 months) and moderate for long-term (≥ 6 months) based on the Cochrane rating system with five levels of evidence (best evidence synthesis), with strong evidence denoting consistent findings among multiple high-quality RCTs and moderate evidence denoting consistent findings among multiple low-quality RCTs or one high-quality RCT. The primary outcome measure was pain relief, defined as at least 50% improvement in pain or 3-point improvement in pain scores in at least 50% of the patients. The secondary outcome measure was functional improvement, defined as 50% reduction in disability or 30% reduction in the disability scores.
Results
Based on strong evidence for short-term efficacy from multiple high-quality trials and moderate evidence for long-term efficacy from at least one high quality trial, we found that fluoroscopic caudal, lumbar interlaminar, and transforaminal epidural injections were efficacious at managing lumbar disc herniation in terms of pain relief and functional improvement.
Conclusions
The available evidence suggests that epidural injections performed under fluoroscopy by trained physicians offer improvement in pain and function in well-selected patients with lumbar disc herniation.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-3490-4) contains supplementary material, which is available to authorized users.
Introduction
Epidural injections are one of the most common nonsurgical treatments for lumbar disc herniation [8, 22, 69, 71, 100, 103, 119]. Epidural injections are administered by accessing the lumbar epidural space by multiple routes—caudal, transforaminal, and interlaminar [1, 7, 8, 17, 21, 22, 69, 71, 100, 103, 119]. Even though all three modalities deliver medication into the epidural space, there are important differences among the approaches. The interlaminar entry is considered to deliver the medication close to the assumed site of pathology, but the transforaminal approach is considered the target-specific modality requiring the smallest volume to reach the primary site of pathology. In contrast, caudal epidurals are considered the safest and easiest, with minimal risk of inadvertent dural puncture, and are the preferred modality in postsurgery syndrome, even though they require relatively high volumes and have an alleged lack of specificity to the assumed site of pathology. Consequently, therapeutic effectiveness also varies among the three approaches [8, 69, 71, 100].
Numerous systematic reviews and guidelines performed by various groups of authors have reached different conclusions about the level of evidence for the effectiveness of epidural injections [5, 7, 8, 21–23, 31, 66, 69, 71, 79, 100, 103, 105, 106, 109, 113, 119]. Some authors have concluded against the effectiveness and medical necessity of epidural injections in managing pain and improving function in patients with disc herniation and radiculitis [5, 21–23, 103, 119]; however, these have been challenged [69, 76], with multiple trials showing significant improvement in pain and function [7, 8, 31, 66, 69, 71, 100, 106, 109, 113]. Some of these systematic reviews and the trials included were criticized for flaws in the assessment of trials, combining trials with variable designs, and designating active controlled trials as placebo control [22, 35, 45, 69, 70, 103, 119]. A recent systematic review by Pinto et al. [103] analyzed all epidural injection approaches compared with a placebo in patients with sciatica, offered criticism of the past reviews and guidelines [7, 8, 70, 72, 100], and criticized some reviews [5, 21, 23, 31] for summarizing the evidence from placebo-controlled trials without considering the size of the treatment effect. Pinto et al. [103] have concluded that there was high-quality evidence showing that epidural steroid injections have small, short-term effects on leg pain and disability compared with placebo in patients with sciatica but no effect in the long term. However, this systematic review by Pinto et al. [103] also had multiple deficiencies [65, 67]. Since the systematic review by Pinto et al. [103] was based on a methodologic rather than a clinical perspective [78, 80], which we find challenging, our review focused on the clinical aspects with appropriate methodologic quality assessment.
Thus, in this systematic review, we determined the short- and long-term efficacy (pain relief and functional improvement) of the three anatomic approaches (caudal, lumbar interlaminar, and transforaminal) for epidural injections in the treatment of disc herniation, considering only placebo-controlled and active-controlled trials.
Materials and Methods
Search Strategy and Criteria
We performed a literature search from 1966 to June 2013 utilizing data from PubMed, Cochrane library, US National Guideline Clearinghouse, previous systematic reviews, and cross-references. The search strategy emphasized low-back and lower-extremity pain, disc herniation, and radiculitis treated with caudal, interlaminar, or transforaminal epidural injections. Search terms included chronic low-back pain, lower-extremity pain, disc herniation, nerve root compression, radiculitis, epidural injections, caudal, interlaminar, and transforaminal.
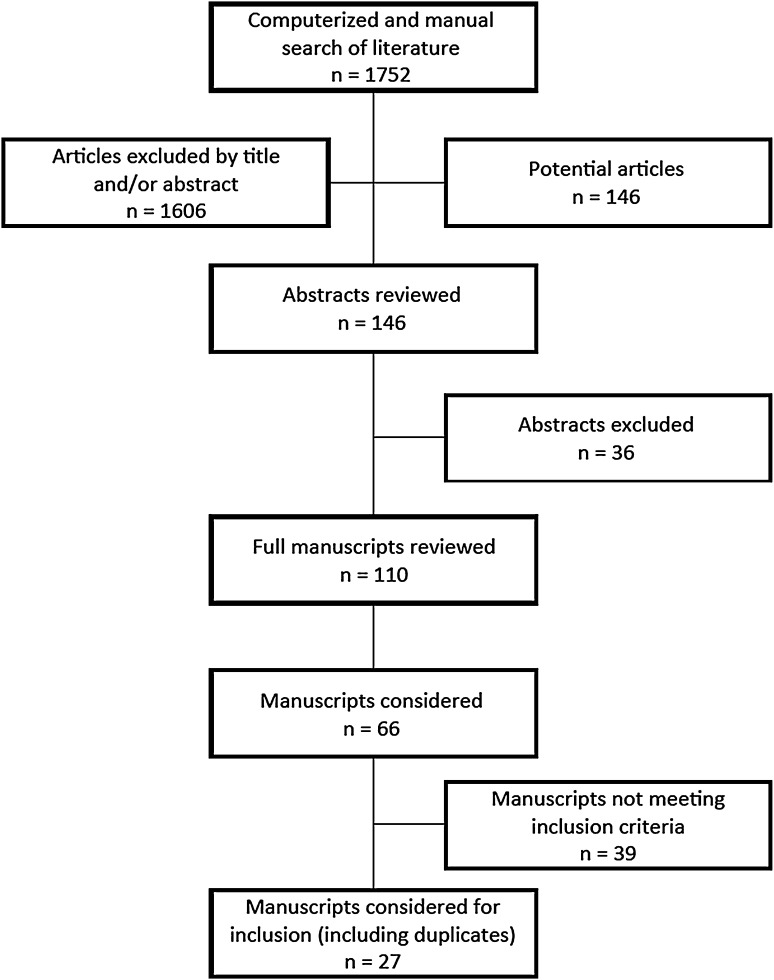
Study selection was achieved as recommended by Preferring Reporting Items for Systematic Reviews and Meta-Analyses [64] (Fig. 1). We reviewed all studies providing appropriate management and with outcome evaluations of 3 months or longer and statistical evaluations. Only randomized controlled trials (RCTs) were included for analysis, either placebo or active controlled. The true definition of placebo is to inject an inactive substance into an inactive structure; for the purposes of this review, we have utilized an injection of placebo into the epidural space or over the nerve root by any approach as placebo [48, 49, 54, 82]. The duration of symptoms of the study participants was classified as subacute (6–12 weeks) and chronic (> 12 weeks). For this evaluation, only the studies utilizing patients with chronic symptoms or patients with a mixture of subacute and chronic symptoms were considered. Studies including radiculitis secondary to spinal canal or foraminal stenosis, postsurgery syndrome, or disc herniation in postsurgery syndrome and chemical radiculitis were not included in this review. However, trials with the inclusion of multiple groups of patients were included if they had at least 25 patients with disc herniation in each group.
Fig. 1.
A flow diagram shows the study selection process.
Overall, there were 66 RCTs for consideration. As we wanted to include only RCTs of high or moderate quality for analysis, we assessed the methodologic quality of these 66 studies using the Cochrane review criteria for RCTs [35]. The criteria include assessment of adequate randomization, treatment allocation concealment, appropriate blinding, description of incomplete outcome data with dropouts and intent-to-treat analysis, study being free of suggestions of selective outcome reporting, and other sources of potential bias including baseline characteristics, cointerventions, compliance, and timing of the outcome measurements in all groups. The methodologic quality was graded as high if nine to 12 criteria were fulfilled, moderate if six to eight criteria were fulfilled, and low if zero to five criteria were fulfilled; trials fulfilling fewer than six criteria were excluded. Thirty-nine of the 66 trials were excluded due to multiple reasons [2, 11–17, 24, 27, 28, 30, 36–39, 41, 42, 47, 52, 53, 58, 60, 61, 68, 92–94, 98, 99, 108, 110, 114, 116, 118, 122, 124, 126, 130] (Appendix 1; supplemental materials are available with the online version of CORR®). Twenty-three trials had high or moderate methodologic quality and were included in our analysis [1, 3, 4, 18, 25, 29, 32, 40, 50, 51, 55–57, 63, 85, 86, 89, 91, 95–97, 104, 107, 111, 112, 121, 128], with four duplicate publications [55 and 56, 85 and 86, 89 and 91, 111 and 112]. Fifteen of these studies were high quality and eight were moderate quality. Ten of the 16 fluoroscopic trials (Table 1) and four of the seven nonfluoroscopic trials (Table 2) were of high quality.
Table 1.
Methodologic quality assessment of fluoroscopic randomized trials.
| Study | Randomization adequate | Concealed treatment allocation | Patient blinded | Care provider blinded | Outcome assessor blinded | Dropout rate described | All randomized participants analyzed in the group | Reports of the study free of suggestion of selective outcome reporting | Groups similar at baseline regarding most important prognostic indicators | Cointerventions avoided or similar | Compliance acceptable in all group | Time of outcome assessment in all groups similar | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Manchikanti et al. [85, 86] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | 10/12 |
| Ackerman and Ahmad [1] | N | N | N | N | N | Y | Y | Y | Y | Y | Y | Y | 7/12 |
| Dashfield et al. [29] | Y | Y | Y | N | N | Y | Y | Y | Y | N | Y | Y | 9/12 |
| Manchikanti et al. [89, 91] | Y | Y | Y | Y | N | Y | Y | Y | N | Y | Y | Y | 10/12 |
| Lee et al. [63] | Y | N | N | N | N | Y | N | Y | Y | Y | Y | Y | 7/12 |
| Rados et al. [107] | Y | N | N | N | N | Y | Y | Y | Y | Y | Y | Y | 8/12 |
| Kim and Brown [57] | Y | Y | Y | N | N | Y | N | Y | Y | Y | Y | Y | 9/12 |
| Amr [3] | Y | Y | Y | Y | N | Y | N | Y | Y | Y | Y | Y | 10/12 |
| Ghahreman et al. [40] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 11/12 |
| Karppinen et al. [55, 56] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | 11/12 |
| Riew et al. [111, 112] | U | U | Y | N | Y | N | Y | Y | Y | Y | Y | Y | 8/12 |
| Jeong et al [51] | U | U | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 9/12 |
| Park et al. [97] | N | U | Y | N | U | Y | Y | Y | Y | Y | Y | Y | 8/12 |
| Tafazal et al. [121] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | 10/12 |
| Cohen et al. [25] | Y | Y | Y | Y | Y | N | N | Y | N | Y | N | Y | 8/12 |
| Ng et al. [96] | Y | Y | Y | N | Y | Y | Y | Y | N | Y | Y | Y | 10/12 |
Y = yes; N = no; U = unclear.
Table 2.
Methodologic quality assessment of randomized trials without fluoroscopy.
| Study | Randomization adequate | Concealed treatment allocation | Patient blinded | Care provider blinded | Outcome assessor blinded | Drop-out rate described | All randomized participants analyzed in the group | Reports of the study free of suggestion of selective outcome reporting | Groups similar at baseline regarding most important prognostic indicators | Co-interventions avoided or similar | Compliance acceptable in all group | Time of outcome assessment in all groups similar | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Iversen et al. [50] | Y | Y | U | N | U | Y | N | Y | N | Y | N | Y | 6/12 |
| Murakibhavi and Khemka [95] | Y | Y | N | N | U | Y | Y | U | Y | N | Y | Y | 7/12 |
| Dilke et al. [32] | U | U | Y | N | Y | Y | U | Y | Y | Y | Y | Y | 8/12 |
| Pirbudak et al. [104] | Y | Y | Y | Y | U | Y | U | Y | Y | Y | Y | Y | 10/12 |
| Arden et al. [4] | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 11/12 |
| Carette et al. [18] | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 11/12 |
| Wilson-MacDonald et al. [128] | Y | Y | Y | N | Y | Y | Y | Y | N | Y | Y | Y | 10/12 |
Y = yes; N = no; U = unclear.
We graded the evidence for each approach using five levels of best evidence synthesis, which summarized the results according to the Cochrane rating system based on the quality and the outcome of the studies [119]. The levels of evidence were distinguished as follows: (1) strong evidence: consistent findings among multiple high-quality RCTs; (2) moderate evidence: consistent findings among multiple low-quality RCTs or one high-quality RCT; (3) limited evidence: one low-quality RCT; (4) conflicting evidence: inconsistent findings among multiple trials; and (5) no evidence: no RCTs. The evidence of all three approaches for epidural injections was strong for the short term and moderate for the long term. Further, the results were considered consistent if 60% of the trials showed results in the same direction.
At least two of the review authors (RMB, FJEF) independently, in an unblinded standardized manner, performed each search and methodologic quality assessment. The primary authors of manuscripts were not involved in the methodologic quality assessment. All searches were combined to obtain a unified strategy. Any disagreements between reviewers were resolved by a third author (JAH) and consensus.
Outcome Measures
The primary outcome measure was pain relief, defined as 50% or more reduction in pain or at least a 3-point decrease in pain scores in at least 50% of patients. The secondary outcome measure was functional improvement, defined as 50% reduction in disability or 30% reduction in the disability scores.
The injection therapy was considered effective, either with a placebo control or active control, if there was a difference in effect for the primary outcome measure in a statistically significant manner at the 5% level. Outcomes were considered at 3 months, 6 months, and 1 year and in the short term (< 6 months) and long term (≥ 6 months).
Meta-analysis was considered if more than two RCTs were homogeneous for mode of administration. However, we found that there was insufficient homogeneity for meta-analysis.
Results
Four of five total trials (three fluoroscopic, two nonfluoroscopic) and all three fluoroscopic trials showed efficacy of caudal epidural injections in managing lumbar disc herniation, with strong evidence in the short and moderate evidence for the long term (Table 3). The three fluoroscopic trials [1, 29, 86] included two high-quality trials [29, 86] and one moderate-quality trial showing mid-term efficacy [1]. Of the nonfluroroscopic trials, one moderate-quality nonfluoroscopic trial [95] showed efficacy and one moderate-quality ultrasound trial did not [50].
Table 3.
Description of study characteristics of randomized controlled epidural trials assessing the efficacy of caudal epidural injections in lumbar disc herniation.
| Study | Study characteristics | Methodologic quality score | Number of patients | Interventions | Outcome measures | Pain and function improvement | Improvement | Comment(s) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 months | 6 months | 12 months | Short term (≤ 6 months) | Long term | ||||||||
| > 6 months | ≥ 12 months | |||||||||||
| Manchikanti et al. [85, 86] (2012, 2011) | RA, AC, F | 10/12 | Total = 120 | Lidocaine vs lidocaine mixed with steroid Number of injections = 1–5 | NRS, ODI, employment status, opioid intake | 62% vs 72% | 72% vs 73% | 67% vs 72% | Y | Y | Y | Double-blind study showing improvement |
| Ackerman and Ahmad [1] (2007) | RA, AC, F | 7/12 | Total = 90 Caudal = 30 IL = 30 TF = 30 |
Methylprednisolone + saline Number of injections = 1–3 |
Numeric pain score (0–10), rating of pain relief, ODI, BDI, contrast dispersion pattern | Caudal = 57% IL = 60% TF = 283% |
Caudal = 57% IL = 60% TF = 83% |
NA | Y | Y | NA | Study showing mid-term improvement |
| Dashfield et al. [29] (2205) | RA, AC, F | 9/12 | Total = 60 Caudal = 30 Endoscopy = 30 |
Lidocaine with triamcinolone Number of injections = 1 |
Pain relief, SF-MPQ, HADS scores | SI | SI | NA | Y | Y | NA | Study showing mid-term improvement |
| Iversen et al. [50] (2011) | RA, PC, UL | 6/12 | Total = 116 | Saline or triamcinolone acetonide with saline Number of injections = 2 |
ODI, EQLS, VAS | N | N | N | U | U | U | Study with numerous deficiencies with flawed design and without local anesthetic showing lack of improvement |
| Murakibhavi and Khemka [95] (2011) | RA, AC, B | 7/12 | Group A = 50 control conservative management Group B = 52 caudal epidural steroid injections Total = 102 |
Conservative management or caudal epidural steroid injections | VAS, ODI, BDI, NPI | Group A = 32% Group B = 92% |
Group A = 24% Group B = 86% |
NA | Y | Y | NA | Moderate-quality study showing short-term improvement |
RA = randomized; AC = active control; F = fluoroscopy; PC = placebo control; UL = ultrasound; B = blinded; IL = interlaminar; TF = transforaminal; NRS = Numeric Rating Scale; ODI = Oswestry Disability Index; BDI = Beck Depression Inventory; SF-MPQ = Short-Form McGill Pain Questionnaire; HADS = Hospital Anxiety and Depression Scale; EQLS = European Quality of Life Scale; NPI = Numerical Pain Intensity; SI = significant improvement; N = no; NA = not applicable; Y = yes; U = unclear.
Five fluoroscopic trials [1, 3, 63, 89, 107] showed efficacy of lumbar interlaminar epidural injections in managing lumbar disc herniation, with strong evidence for the short term and moderate evidence [3, 89] for the long term. Two of these trials were high quality [3, 89] and three moderate quality [1, 63, 107] (Table 4). Of the four nonfluoroscopic studies (all high quality), two showed efficacy [104, 128] and two did not [4, 18]. However, the level of evidence was strong and moderate based on fluoroscopic trials only, whereas a combination of fluoroscopic and nonfluoroscopic trials yielded moderate evidence, and when only nonfluoroscopic or blind trials were considered, the evidence was conflicting, with inconsistent findings among multiple trials.
Table 4.
Description of study characteristics of randomized controlled epidural trials assessing the efficacy of lumbar interlaminar epidural injections in lumbar disc herniation.
| Study | Study characteristics | Methodologic quality score | Number of patients | Interventions | Outcome measures | Pain and function improvement | Improvement | Comment(s) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 months | 6 months | 12 months | Short term | Long term | ||||||||
| (≤ 6 months) | > 6 months | ≥ 12 months | ||||||||||
| Manchikanti et al. [89, 91] (2012, 2010) | RA, AC, F | 10/12 | Total = 120 Local anesthetic = 60 Local anesthetic and steroids = 60 |
Xylocaine® or Xylocaine® with nonparticulate Celestone®
Number of injections = 1–5 |
NRS, ODI, employment status, opioid intake, SI ≥ 50% of NRS scores and ODI scores | 72% vs 82% | 63% vs 85% | 67% vs 85% or 80% vs 86% in successful group | Y | Y | Y | Study with long-term followup showing improvement |
| Lee et al. [63] (2009) | RA, AC, F | 7/12 | Total = 93 IL = 34 TF = 59 |
Lidocaine with triamcinolone Number of injections = 1–3 |
NRS, PSI | SI in both groups | SI in both groups | SI in both groups | Y | NA | NA | Study with short-term followup showing improvement |
| Rados et al. [107] (2011) | RA, AC, F | 8/12 | Total = 64 IL = 32 TF = 32 |
Lidocaine with methylprednisolone Number of injections = 1–3 |
VAS, ODI | 53% vs 63% | 53% vs 63% | NA | Y | Y | NA | Study with short followup showing improvement |
| Kimand Brown [57] (2011) | RA, AC, F | 9/12 | Total = 60 Methylprednisolone = 30 Dexamethasone = 30 |
Depo-medrol® or dexamethasone with bupivacaine Number of injections = 1–2 |
VAS, pain medication intake, emergency room visits | NA | NA | U | NA | NA | NA | Relatively small study with undetermined results |
| Amr [3] (2011) | RA, AC, F | 10/12 | Total = 200 Steroid = 100 Steroid + ketamine = 100 |
Triamcinolone plus preservative-free ketamine and 0.9% saline Number of injections = 1 |
Pain scores, Oswestry Low Back Pain Disability Questionnaire | SI in ketamine group | SI in ketamine group | SI in ketamine group | Y | Y | Y | Study with long-term followup showing improvement |
| Ackerman and Ahmad [1] (2007) | RA, AC, F | 7/12 | Total = 90 Caudal = 30 IL = 30 TF = 30 |
Steroid and saline with local anesthetic Number of injections = 1–3 |
Pain relief | Y | Y | NA | Y | Y | NA | Study showing mid-term improvement |
| Dilke et al. [32] (1973) | RA, PC, B | 8/12 | Total = 100 Epidural = 50 Interspinous = 50 |
Methylprednisolone in normal saline or interspinous ligament Number of injections = 1–2 |
Pain relief, analgesic consumption, changes in straight leg raising, or neurologic signs | Y | NA | NA | Y | NA | NA | Study showing improvement |
| Pirbudak et al. [104] (2003) | RA, AC, B | 10/12 | Total = 92 Epidural = 46 Epidural + amitriptyline = 46 |
Betamethasone and bupivacaine or with addition of amitriptyline Number of injections = 1–3 |
VAS, ODI | SI in both groups | SI in both groups | SI in both groups | Y | Y | Y | Study showing improvement |
| Arden et al. [4] (2005) | RA, PC, B | 11/12 | Total = 228 Steroid group = 120 Placebo group = 108 |
Triamcinolone and bupivacaine or normal saline into interspinous ligament Number of injections = 3 |
ODQ, pain relief, VAS, SF-36 | NSI | NSI | NSI | N | N | N | Study showing lack of improvement |
| Carette et al. [18] (1997) | RA, PC, B | 11/12 | Total = 158 Methylprednisolone = 78 Placebo = 80 |
Normal saline vs Depo-medrol® and procaine Number of injections = 1 to 3 |
VAS, ODI | NSI | NSI | NSI | N | N | N | Inappropriate blinded placebo study showing lack of improvement |
| Wilson-MacDonald et al. [128] (2005) | RA, AC, B | 10/12 | Total = 60 Intramuscular = 34 Epidural = 26 |
Intramuscular injection or epidural bupivacaine with methylprednisolone Number of injections = 1–2 |
Oxford Pain Chart, ODI | SI in the treatment group | U | U | Y | U | U | Small study showing short-term improvement |
RA = randomized; AC = active control; F = fluoroscopy; PC = placebo control; B = blinded; IL = interlaminar; TF = transforaminal; NRS = Numeric Rating Scale; ODI = Oswestry Disability Index; SI = significant improvement; PSI = Patient Satisfaction Index; ODQ = Oswestry Disability Questionnaire; NA = not applicable; Y = yes; NSI = no significant improvement; U = unclear; N = no.
Seven fluoroscopic trials showed efficacy of transforaminal epidural injections in managing lumbar disc herniation, with strong evidence for the short term and moderate evidence for the long term (Table 5). Three of these were high-quality trials [40, 51, 121] and four moderate-quality trials [1, 97, 107, 112]. Two high-quality fluoroscopic trials showed lack of efficacy [25, 55].
Table 5.
Description of study characteristics of randomized controlled epidural trials assessing the efficacy of lumbar transforaminal epidural injections in lumbar disc herniation.
| Study | Study characteristics | Methodologic quality score | Number of patients | Interventions | Outcome measures | Pain and function improvement | Improvement | Comment(s) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 months | 6 months | 12 months | Short term | Long term | ||||||||
| (≤ 6 months) | > 6 months | ≥ 12 months | ||||||||||
| Cohen et al. [25] (2012) | RA, PC, F | 10/12 | Total = 84 Saline = 30 Corticosteroid = 28 Etanercept = 26 |
Steroids, etanercept, or saline Number of injections = 1–2 |
Pain relief, ODI, global perceived effect | Steroids = 50% Etanercept = 42% Saline = 43% |
Steroids = 29% Etanercept = 38% Saline = 40% |
Steroids = NA Etanercept = NA Saline = NA |
N | N | NA | Although this was a well-conducted study, it was not a true placebo study. Even though there was no significant difference, the authors concluded epidural steroid injections may provide short-term pain relief for some. The included patients had subacute sciatica. |
| Ghahreman et al. [40] (2010) | RA, PC, F | 12/12 | Total = 150 5 groups with 28, 37, 27, 28, 30 |
Steroids with saline vs local anesthetic vs intramuscular steroids vs Intramuscular saline Number of injections = 1–3 |
At least 50% pain relief | TF saline = 19% TF local anesthetic = 7% TF epidural = 54% |
NA | NA | Steroids = Y Local anesthetic and saline = N |
NA | NA | First study of its nature with a true placebo evaluation showing short-term improvement |
| Karppinen et al. [55, 56] (2001) | RA, PC, F | 11/12 | Total = 160 Methylprednisolone-bupivacaine = 80 Saline = 80 |
Sodium chloride solution or methylprednisolone (40 mg) and bupivacaine (5 mg) Number of injections = 1 |
VAS, ODI, Nottingham Health Profile, cost, physical examination | NA | SI in both groups | SI in both groups | U | U | U | An ineffective or inappropriate placebo design, without applicable results |
| Jeong et al. [51] (2007) | RA, AC, F | 9/12 | Total = 193 G = 104 PG = 89 |
0.5 mL bupivacaine hydrochloride and 40 mg 1 mL triamcinolone Number of injections = 1 |
VAS | PG = 88.4% G = 70.9% |
PG = 60.4% G = 67.2% |
NA | Y | Y | NA | Moderate-quality study showing mid-term improvement |
| Riew et al. [111, 112] (2006, 2006) | RA, AC, F | 8/12 | Total = 55 Bupivacaine = 27 Bupivacaine + steroid = 28 |
Bupivacaine 0.25% or bupivacaine with 6 mg betamethasone Number of injections = 1–4 |
North American Spine Society Outcome Instrument, operative treatment considered as failure of injection treatment | NA | NA | 33% vs 71% (avoided surgery) | Steroids = Y Local anesthetic = U |
Steroids = Y Local anesthetic = U |
Steroids = Y Local anesthetic = N |
Surgery avoided in 33% of bupivacaine group and 71% in steroid group |
| Ng et al. [96] (2005) | RA, AC, F | 11/12 | Total = 86 Bupivacaine = 43 Bupivacaine + steroid = 43 |
Bupivacaine only or bupivacaine with methylprednisolone Number of injections = 1 |
VAS, ODI, change in walking distance, claudication, satisfaction of the outcome | Bupivacaine = 47.5% Bupivacaine + steroid = 41.5% |
NA | NA | Steroids = Y Local anesthetic = N |
NA | NA | Small study with short-term followup showing improvement |
| Lee et al. [63] (2009) | RA, AC, F | 7/12 | Total = 93 IL = 34 TF = 59 |
Interlaminar vs transforaminal epidural injections 4 mL (TF) Number of injections = 1–3 |
NRS, PSI | Roland Pain Score: TF = 3.34–1.59 IL = 3.25–1.57 |
NA | NA | Y | NA | NA | Study with short-term followup showing improvement |
| Ackerman and Ahmad [1] (2007) | RA, AC, F | 7/12 | Total = 90 Caudal = 30 IL = 30 TF = 30 |
Steroid and saline with local anesthetic Number of injections = 1–3 |
Pain relief | Caudal = 57% IL = 60% TF = 83% |
Caudal = 57% IL = 60% TF = 83% |
NA | Y | P | NA | Study showing mid-term improvement |
| Park et al. [97] (2010) | RA, AC, F | 7/12 | Total = 106 Dexamethasone = 53 Triamcinolone acetate = 53 |
Dexamethasone or triamcinolone acetate with lidocaine Number of injections = 1 |
VAS, Short MPQ, ODI | Dexamethasone = 40% Triamcinolone = 71% |
NA | NA | Y | NA | NA | Short-term improvement with triamcinolone compared to dexamethasone |
| Rados et al. [107] (2011) | RA, AC, F | 8/12 | Total = 64 IL = 32 TF = 32 |
IL vs TF Number of injections = 1–3 |
VAS, ODI, disability scores | TF = 53% IL = 75% |
TF = 53% IL = 75% |
NA | Y | Y | NA | Study showing mid-term improvement |
| Tafazal et al. [121] (2009) | RA, AC, F | 10/12 | Total = 76 Bupivacaine = 34 Bupivacaine + steroid = 42 |
Bupivacaine with methylprednisolone Number of injections = 1–3 |
VAS, ODI, LBOS, Modified Somatic Perception Questionnaire, MZD | VAS and ODI changes: Bupivacaine = 24.3 and 13.8 Bupivacaine + steroid = 27.4 and 13.6 |
Y | NA | Y | Y | Y | Study showing long-term improvement |
RA = randomized; PC = placebo control; F = fluoroscopy; AC = active control; G = ganglionic; PG = preganglionic; IL = interlaminar; TF = transforaminal; ODI = Oswestry Disability Index; NRS = Numeric Rating Scale; PSI = Patient Satisfaction Index; MPQ = McGill Pain Questionnaire; LBOS = Low Back Outcome Score; MZD = Modified Zung Depression; NA = not applicable; SI = significant improvement; Y = yes; N = no; U = unclear.
Discussion
Lumbar disc herniation is readily diagnosed and the most common indication for surgical intervention in the lumbar spine [43, 127]. While it is generally believed that the course and prognosis of acute sciatica secondary to disc herniation are favorable [59, 125], some patients continue to have persistent and disabling symptoms for 2 years or longer [34, 123] and many undergo surgery [43, 117, 127]. Therapeutic epidural injections utilized as a nonsurgical management for chronic persistent disabling disc herniation and radiculitis have become increasingly popular [46, 81, 83, 84]. In fact, Manchikanti et al. [83], in an assessment of utilization characteristics of epidural injections in the fee-for-service Medicare population, found a 130% growth per 100,000 Medicare patients from 2000 to 2011 [81, 83, 84]. The lumbar transforaminal approach had a breathtaking increase of 665% in that same period. In this systematic review, we determined the efficacy of the three anatomic approaches to epidural injections—caudal, lumbar interlaminar, and transforaminal—in the treatment of disc herniation and radiculitis with placebo-controlled and active-controlled interventions.
The limitations of this review include the paucity of high-quality literature for each modality, despite 23 trials meeting inclusion criteria in lumbar disc herniation for three modes of administration. In addition, we were unable to perform a meta-analysis due to a lack of homogeneity among the RCTs for mode of administration. Further, the majority of the evidence was obtained from active-controlled trials, specifically for long-term improvement with all three approaches. Active-controlled trials compare two different procedures or drugs. Thus, some may consider this as a weakness. The majority of the analytical flaws arrive as methodologists consider one of the drugs as placebo and compare between the two groups rather than baseline to followup periods. Thus, the strengths of active-controlled trials include their comparative evaluation, which has become pivotal in modern evidence-based medicine [77]. These studies provide insight into the effectiveness of local anesthetic with or without steroids and various methods such as interlaminar, caudal, and transforaminal. Placebo-controlled trials are also extremely important and constitute a limitation to our analysis. Specifically, it is desirable to have studies with their placebo group designed with appropriate inclusion of injection of placebo solution into a nonactive structure, which has not been included in the majority of the studies and is a debated issue [9, 10, 18–20, 40, 50, 55, 69, 70, 78, 103]. Further, placebo interventions have been misinterpreted based on the solution injected and the location of the injection. This has reached such proportions that methodologists have continued to consider even a local anesthetic injection or any solution injected into an active structure as placebo even though these invariably result in a multitude of effects, with some of the effects being therapeutic [6, 8–10, 18, 19, 33, 40, 48, 50, 54, 55, 62, 70, 71, 73–75, 78, 80, 86–91, 100–103, 115, 120]. In designing the studies, apart from active-controlled design, the reviewers must be cognizant of the multiple effects of placebo; nocebo; Hawthorne effect; natural course of the disease, which is not applicable in these chronic patients; and regression to the mean, which has been extensively discussed in reference to placebo, nocebo, and pure and impure placebos [48, 54]. Thus, this may be considered as a weakness but not a flaw unless active-controlled trials are misinterpreted. Some may also consider not utilizing all RCTs irrespective of their size and quality as a deficiency; however, we believe that is one of the strengths of this systematic review.
We found high-quality evidence showing that epidural injections have short-term benefits in terms of alleviating pain and disability of lumbar disc herniation and moderate long-term effects for all three approaches. The evidence was stronger for short-term effects compared to long-term effects. The results of our systematic review are similar to those of some previous reviews [8, 69, 71, 76, 100]. Of importance is the systematic review by Pinto et al. [103], which partially agreed with our review in reference to short-term but not long-term improvement. Pinto et al. [103] concluded epidural steroid injections have a small, short-term effect on leg pain and disability compared to placebo in patients with sciatica, but without significant effect in the long term. Our review differs from that of Pinto et al. [103], which has been criticized for its deficiencies [65, 67]. Pinto et al. [103] utilized methodologic quality assessment criteria, based on an instrument developed for physiotherapy, which has not been validated for interventional techniques [65, 67] and differs substantially from criteria developed by the Cochrane review group [35, 119]. Additional deficiencies of that systematic review include the inclusion of a multitude of heterogeneous studies that were labeled homogeneous. The authors indicated that the studies were homogeneous based on the fact that reviewers have decided that local anesthetic injection was a placebo. We believe that such a methodology invalidates the entire concept of meta-analysis of homogeneous studies. Pinto et al. [103] also did not take into consideration the varying effects of placebo and nocebo, impure placebo, and the effects of injecting not only various active solutions but also inactive solutions into active structures [20, 48, 49, 54, 69–71, 78, 82].
The evidence appears to be somewhat stronger for caudal epidural injections. Only one placebo-controlled trial by Iversen et al. [50] utilizing ultrasound imaging showed a lack of efficacy. However, this trial has numerous deficiencies, including flawed design, poor selection criteria, poor inclusion criteria, and no injection of local anesthetic, leading to only moderate quality in methodologic quality assessment. The only study assessing long-term improvement of 2 years, including 120 patients with local anesthetic with or without steroids, was an active-controlled trial that showed sustained improvement over a 2-year period, with repeat procedures as medically necessary and indicated, both in reducing low-back and lower-extremity pain and improving function [79, 85, 86].
For lumbar interlaminar epidural injections, there were two fluoroscopic studies [3, 89] and one blind trial [104] assessing long-term effectiveness that showed improvement. A major study by Carette et al. [18], published in 1997, showed no efficacy with a blind approach. In this assessment, the authors utilized sodium chloride solution in the epidural space, which may have significant effects beyond the placebo effect [8, 9, 44, 71, 82, 85, 86, 89, 91, 100, 129]. Of the trials showing improvement, all were actively controlled [3, 89, 104]. However, true placebo studies with injection into the intraspinous ligament showed contradicting results. Efficacy was shown by Dilke et al. [32] in 1973 and lack of efficacy was shown by Arden et al. [4] in 2005.
In reference to lumbar transforaminal epidural injections, there was only one long-term study with 1-year followup in a relatively small number of patients (total 55) with an active-controlled design. There were multiple well-performed studies showing no efficacy. Among the placebo studies [25, 40, 55], Ghahreman et al. [40] used a true placebo design injecting sodium chloride solution into a muscle and over the nerve root, whereas Cohen et al. [25] and Karppinen et al. [55] utilized a rather impure placebo design injecting sodium chloride solution into the neural space over the nerve root.
There was only one trial, that of Ackerman and Ahmad [1], comparing all three approaches; however, this was only of moderate quality and reported improvement with a 6-month followup, with superior results for the transforaminal approach compared to the interlaminar and caudal approaches. One additional trial by Lee et al. [63] compared interlaminar versus transforaminal epidural injection with a short-term followup and showed basically similar results with both approaches.
In this analysis, utilizing appropriate methodology, based on Cochrane review criteria for quality of evidence for RCTs [119], we found strong evidence for epidural injections in managing chronic pain of disc herniation in the short term and moderate evidence in the long term. This may be in contrast to some of the previous reviews while in agreement with others. Previous authors have concluded lack of efficacy of epidural injections over the long term, inappropriately utilized local anesthetic as placebo, and performed meta-analysis that often yielded misleading results because local anesthetics have yielded results that were similar to steroids [22, 69, 78, 86, 91, 103, 119]. While the strength of our review is that it provided qualitative evidence, we were unable to provide quantitative information (as might be done through pooling data in meta-analysis) because of excessive heterogeneity among the trials identified by the systematic review. Thus, to facilitate meta-analysis, future RCTs should focus on study design with long-term followup and appropriate outcome parameters, which will make it more likely that their results will be suitable for pooling and make them more likely to be included in a meta-analysis. These results can guide shared decision making in which patients are informed about up-to-date evidence and probable outcomes in a balanced manner [26].
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
The authors thank Vidyasagar Pampati MSc for statistical assistance, Alvaro F. Gómez MA and Laurie Swick BS for manuscript review, and Tonie M. Hatton and Diane E. Neihoff, transcriptionists, for their assistance in preparation of this manuscript.
Footnotes
One of the authors (RMB) certifies that he or she, or a member of his or her immediate family, has received or may receive payments or benefits, during the study period, an amount of less than USD 10,000 from Boston Scientific (Natick, MA, USA) and Kimberly Clark (Dallas, TX, USA). One of the authors (FJEF) certifies that he or she, or a member of his or her immediate family, has received or may receive payments or benefits, during the study period, an amount of less than USD 10,000, from St Jude Medical, Inc (St Paul, MN, USA) and Joimax Inc (Irvine, CA, USA). One of the authors (ADK) certifies that he or she, or a member of his or her immediate family, has received or may receive payments or benefits, during the study period, an amount of less than USD 10,000, from Depomed, Inc (Newark, CA, USA).
Each of the remaining authors certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
This work was performed at Pain Management Center of Paducah, KY (Paducah, KY, USA).
References
- 1.Ackerman WE, 3rd, Ahmad M. The efficacy of lumbar epidural steroid injections in patients with lumbar disc herniations. Anesth Analg. 2007;104:1217–1222. doi: 10.1213/01.ane.0000260307.16555.7f. [DOI] [PubMed] [Google Scholar]
- 2.Ahadian FM, McGreevy K, Schulteis G. Lumbar transforaminal epidural dexamethasone: a prospective, randomized, double-blind, dose-response trial. Reg Anesth Pain Med. 2011;36:572–578. doi: 10.1097/AAP.0b013e318232e843. [DOI] [PubMed] [Google Scholar]
- 3.Amr YM. Effect of addition of epidural ketamine to steroid in lumbar radiculitis: one-year follow-up. Pain Physician. 2011;14:475–481. [PubMed] [Google Scholar]
- 4.Arden NK, Price C, Reading I, Stubbing J, Hazelgrove J, Dunne C, Michel M, Rogers P, Cooper C; WEST Study Group. A multicentre randomized controlled trial of epidural corticosteroid injections for sciatica: The WEST study. Rheumatology (Oxford). 2005;44:1399–1406. [DOI] [PubMed]
- 5.Armon C, Argoff CE, Samuels J, Backonja M. Assessment: use of epidural steroid injections to treat radicular lumbosacral pain: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2007;68:723–729. doi: 10.1212/01.wnl.0000256734.34238.e7. [DOI] [PubMed] [Google Scholar]
- 6.Arner S, Lindblom U, Meyerson BA, Molander C. Prolonged relief of neuralgia after regional anesthetic block: a call for further experimental and systematic clinical studies. Pain. 1990;43:287–297. doi: 10.1016/0304-3959(90)90026-A. [DOI] [PubMed] [Google Scholar]
- 7.Benny B, Azari P. The efficacy of lumbosacral transforaminal epidural steroid injections: a comprehensive literature review. J Back Musculoskelet Rehabil. 2011;24:67–76. doi: 10.3233/BMR-2011-0279. [DOI] [PubMed] [Google Scholar]
- 8.Benyamin RM, Manchikanti L, Parr AT, Diwan SA, Singh V, Falco FJ, Datta S, Abdi S, Hirsch JA. The effectiveness of lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain. Pain Physician. 2012;15:E363–E404. [PubMed] [Google Scholar]
- 9.Bhatia MT, Parikh LC. Epidural saline therapy in lumbo-sciatic syndrome. J Indian Med Assoc. 1966;47:537–542. [PubMed] [Google Scholar]
- 10.Bisby MA. Inhibition of axonal transport in nerves chronically treated with local anesthetics. Exp Neurol. 1975;47:481–489. doi: 10.1016/0014-4886(75)90080-1. [DOI] [PubMed] [Google Scholar]
- 11.Breivik H, Hesla PE, Molnar I, Lind B. Treatment of chronic low back pain and sciatica: comparison of caudal epidural injections of bupivacaine and methylprednisolone with bupivacaine followed by saline. In: Bonica JJ, Albe-Fesard D, editors. Advances in Pain Research and Therapy. New York, NY: Raven Press; 1976. pp. 927–932. [Google Scholar]
- 12.Bronfort G, Evans RL, Maiers M, Anderson AV. Spinal manipulation, epidural injections, and self-care for sciatica: a pilot study for a randomized clinical trial. J Manipulative Physiol Ther. 2004;27:503–508. doi: 10.1016/j.jmpt.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Buchner M, Zeifang F, Brocai DR, Schiltenwolf M. Epidural corticosteroid injection in the conservative management of sciatica. Clin Orthop Relat Res. 2000;375:149–156. doi: 10.1097/00003086-200006000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Burgher AH, Hoelzer BC, Schroeder DR, Wilson GA, Huntoon MA. Transforaminal epidural clonidine versus corticosteroid for acute lumbosacral radiculopathy due to intervertebral disc herniation. Spine (Phila Pa 1976). 2011;36:E293–E300. [DOI] [PMC free article] [PubMed]
- 15.Bush K, Hillier S. A controlled study of caudal epidural injections of triamcinolone plus procaine for the management of intractable sciatica. Spine (Phila Pa 1976). 1991;16:572–575. [DOI] [PubMed]
- 16.Buttermann GR. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy: a prospective, randomized study. J Bone Joint Surg Am. 2004;86:670–679. [PubMed] [Google Scholar]
- 17.Candido KD, Raghavendra MS, Chinthagada M, Badiee S, Trepashko DW. A prospective evaluation of iodinated contrast flow patterns with fluoroscopically guided lumbar epidural steroid injections: the lateral parasagittal interlaminar epidural approach versus the transforaminal epidural approach. Anesth Analg. 2008;106:638–644. doi: 10.1213/ane.0b013e3181605e9b. [DOI] [PubMed] [Google Scholar]
- 18.Carette S, Leclaire R, Marcoux S, Morin F, Blaise GA, St-Pierre A, Truchon R, Parent F, Levesque J, Bergeron V, Montminy P, Blanchette C. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med. 1997;336:1634–1640. doi: 10.1056/NEJM199706053362303. [DOI] [PubMed] [Google Scholar]
- 19.Cassuto J, Sinclair R, Bonderovic M. Anti-inflammatory properties of local anesthetics and their present and potential clinical implications. Acta Anaesthesiol Scand. 2006;50:265–282. doi: 10.1111/j.1399-6576.2006.00936.x. [DOI] [PubMed] [Google Scholar]
- 20.Chou R, Atlas SJ, Loeser JD, Rosenquist RW, Stanos SP. Guideline warfare over interventional therapies for low back pain: can we raise the level of discourse? J Pain. 2011;12:833–839. doi: 10.1016/j.jpain.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 21.Chou R, Atlas SJ, Stanos SP, Rosenquist RW. Nonsurgical interventional therapies for low back pain: a review of the evidence for an American Pain Society clinical practice guideline. Spine (Phila Pa 1976). 2009;34:1078–1093. [DOI] [PubMed]
- 22.Chou R, Huffman L. Guideline for theEvaluation and Management of Low Back Pain: Evidence Review. Glenview, IL: American Pain Society, 2009. Available at: http://www.americanpainsociety.org/uploads/pdfs/LBPEvidRev.pdf. Accessed July 26, 2013.
- 23.Chou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, Baisden J, Carragee EJ, Grabois M, Murphy DR, Resnick DK, Stanos SP, Shaffer WO, Wall EM; American Pain Society Low Back Pain Guideline Panel. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society. Spine (Phila Pa 1976). 2009;34:1066–1077. [DOI] [PubMed]
- 24.Cohen SP, Bogduk N, Dragovich A, Buckenmaier CC, 3rd, Griffith S, Kurihara C, Raymond J, Richter PJ, Williams N, Yaksh TL. Randomized, double-blind, placebo-controlled, dose-response, and preclinical safety study of transforaminal epidural etanercept for the treatment of sciatica. Anesthesiology. 2009;110:1116–1126. doi: 10.1097/ALN.0b013e3181a05aa0. [DOI] [PubMed] [Google Scholar]
- 25.Cohen SP, White RL, Kurihara C, Larkin TM, Chang A, Griffith SR, Gilligan C, Larkin R, Morlando B, Pasquina PF, Yaksh TL, Nguyen C. Epidural steroids, etanercept, or saline in subacute sciatica: a multicenter, randomized trial. Ann Intern Med. 2012;156:551–559. doi: 10.7326/0003-4819-156-8-201204170-00397. [DOI] [PubMed] [Google Scholar]
- 26.Could truly informed consent transform spine care? The Back Letter. 2013;28:61–69.
- 27.Cuckler JM, Bernini PA, Wiesel SW, Booth RE, Jr, Rothman RH, Pickens GT. The use of epidural steroid in the treatment of radicular pain. J Bone Joint Surg. 1985;67:63–66. [PubMed] [Google Scholar]
- 28.Czarski Z. Treatment of sciatica with hydrocortisone and Novocaine injections into the sacral hiatus [in Polish] Przegl Lek. 1965;21:511–513. [PubMed] [Google Scholar]
- 29.Dashfield A, Taylor M, Cleaver J, Farrow D. Comparison of caudal steroid epidural with targeted steroid placement during spinal endoscopy for chronic sciatica: a prospective, randomized, double-blind trial. Br J Anaesth. 2005;94:514–519. doi: 10.1093/bja/aei084. [DOI] [PubMed] [Google Scholar]
- 30.Debi R, Halperin N, Mirovsky Y. Local application of steroids following lumbar discectomy. J Spinal Disord Tech. 2002;15:273–276. doi: 10.1097/00024720-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 31.DePalma MJ, Bhargava A, Slipman CW. A critical appraisal of the evidence for selective nerve root injection in the treatment of lumbosacral radiculopathy. Arch Phys Med Rehabil. 2005;86:1477–1483. doi: 10.1016/j.apmr.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 32.Dilke TF, Burry HC, Grahame R. Extradural corticosteroid injection in the management of lumbar nerve root compression. Br Med J. 1973;2:635–637. doi: 10.1136/bmj.2.5867.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Falco FJ, Manchikanti L, Datta S, Sehgal N, Geffert S, Onyewu O, Zhu J, Coubarous S, Hameed M, Ward SP, Sharma ML, Hameed H, Singh V, Boswell MV. An update of the effectiveness of therapeutic lumbar facet joint interventions. Pain Physician. 2012;15:E909–E953. [PubMed] [Google Scholar]
- 34.Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, Castel LD, Kalsbeek WD, Carey TS. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169:251–258. doi: 10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Furlan AD, Pennick V, Bombardier C, van Tulder M; Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009;34:1929–1941. [DOI] [PubMed]
- 36.Gallucci M, Limbucci N, Zugaro L, Barile A, Stavroulis E, Ricci A, Galzio R, Masciocchi C. Sciatica: treatment with intradiscal and intraforaminal injections of steroid and oxygen-ozone versus steroid only. Radiology. 2007;242:907–913. doi: 10.1148/radiol.2423051934. [DOI] [PubMed] [Google Scholar]
- 37.Gelalis ID, Arnaoutoglou E, Pakos EE, Politis AN, Rapti M, Xenakis TA, Papadopoulos G. Effect of interlaminar epidural steroid injection in acute and subacute pain due to lumbar disk herniation: a randomized comparison of 2 different protocols. Open Orthop J. 2009;3:121–124. doi: 10.2174/1874325000903010121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gerszten PC, Smuck M, Rathmell JP, Simopoulos TT, Bhagia SM, Mocek CK, Crabtree T. Bloch DA; SPINE Study Group. Plasma disc decompression compared with fluoroscopy-guided transforaminal epidural steroid injections for symptomatic contained lumbar disc herniation: a prospective, randomized, controlled trial. J Neurosurg Spine. 2010;12:357–371. doi: 10.3171/2009.10.SPINE09208. [DOI] [PubMed] [Google Scholar]
- 39.Ghahreman A, Bogduk N. Predictors of a favorable response to transforaminal injection of steroids in patients with lumbar radicular pain due to disc herniation. Pain Med. 2011;12:871–879. doi: 10.1111/j.1526-4637.2011.01116.x. [DOI] [PubMed] [Google Scholar]
- 40.Ghahreman A, Ferch R, Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. 2010;11:1149–1168. doi: 10.1111/j.1526-4637.2010.00908.x. [DOI] [PubMed] [Google Scholar]
- 41.Ghai B, Vadaje KS, Wig J, Dhillon MS. Lateral parasagittal versus midline interlaminar lumbar epidural steroid injection for management of low back pain with lumbosacral radicular pain: a double-blind, randomized study. Anesth Analg. 2013;117:219–227. doi: 10.1213/ANE.0b013e3182910a15. [DOI] [PubMed] [Google Scholar]
- 42.Gharibo C, Varlotta G, Rhame E, Liu EC, Bendo J, Perloff M. Interlaminar versus transforaminal epidural steroids for the treatment of sub-acute lumbar radicular pain: a randomized, blinded, prospective outcome study. Pain Physician. 2011;14:499–511. [PubMed] [Google Scholar]
- 43.Gibson JN, Waddell G. Surgical interventions for lumbar disc prolapse. Cochrane Database Syst Rev. 2007;1:CD001350. [DOI] [PMC free article] [PubMed]
- 44.Gupta AK, Mital VK, Azmi RU. Observations of the management of lumbosciatic syndromes (sciatica) by epidural saline. J Indian Med Assoc. 1970;54:194–196. [PubMed] [Google Scholar]
- 45.Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D; Methods Work Group, Third US Preventive Services Task Force. Current methods of the US Preventive Services Task Force. Am J Prevent Med. 2001;20:21–35.
- 46.Health and Social Care Information Centre. Hospital Episodes Statistics (HESonline). Available at: www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=210. Accessed July 26, 2013.
- 47.Hesla PE, Breivik H. Epidural analgesia and epidural steroid injection for treatment of chronic low back pain and sciatica [in Norwegian] Tidsskr Nor Laegeforen. 1979;99:936–939. [PubMed] [Google Scholar]
- 48.Howick J, Bishop FL. Heneghan, Wolstenholme J, Stevens S, Hobbs FD, Lewith G. Placebo use in the United Kingdom: results from a national survey of primary care practitioners. PLOS One. 2013;8:e58247. doi: 10.1371/journal.pone.0058247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hróbjartsson A, Gøtzsche PC. Placebo interventions for all clinical conditions. Cochrane Database Syst Rev. 2010;1:CD003974. [DOI] [PMC free article] [PubMed]
- 50.Iversen T, Solberg TK, Romner B, Wilsgaard T, Twisk J, Anke A, Nygaard O, Hasvold T, Ingebrigtsen T. Effect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: multicentre, blinded, randomised controlled trial. BMJ. 2011;343:d5278. doi: 10.1136/bmj.d5278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jeong HS, Lee JW, Kim SH, Myung JS, Kim JH, Kang HS. Effectiveness of transforaminal epidural steroid injection by using a preganglionic approach: a prospective randomized controlled study. Radiology. 2007;245:584–590. doi: 10.1148/radiol.2452062007. [DOI] [PubMed] [Google Scholar]
- 52.Jirarattanaphochai K, Jung S, Thienthong S, Krisanaprakornkit W, Sumananont C. Peridural methylprednisolone and wound infiltration with bupivacaine for postoperative pain control after posterior lumbar spine surgery: a randomized double-blinded placebo-controlled trial. Spine (Phila Pa 1976). 2007;32:609–616. [DOI] [PubMed]
- 53.Kang SS, Hwang BM, Son HJ, Cheong IY, Lee SJ, Lee SH, Chung TY. The dosages of corticosteroid in transforaminal epidural steroid injections for lumbar radicular pain due to a herniated disc. Pain Physician. 2011;14:361–370. [PubMed] [Google Scholar]
- 54.Kaptchuk TJ, Friedlander E, Kelley JM, Sanchez MN, Kokkotou E, Singer JP, Kowalczykowski M, Miller FG, Kirsch I, Lembo AJ. Placebos without deception: a randomized controlled trial in irritable bowel syndrome. PLoS One. 2010;5:e15591. doi: 10.1371/journal.pone.0015591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Karppinen J, Malmivaara A, Kurunlahti M, Kyllönen E, Pienimäki T, Nieminen P, Ohinmaa A, Tervonen O, Vanharanta H. Periradicular infiltration for sciatica: a randomized controlled trial. Spine (Phila Pa 1976). 2001;26:1059–1067. [DOI] [PubMed]
- 56.Karppinen J, Ohinmaa A, Malmivaara A, Kurunlahti M, Kyllönen E, Pienimäki T, Nieminen P, Tervonen O, Vanharanta H. Cost effectiveness of periradicular infiltration for sciatica: subgroup analysis of a randomized controlled trial. Spine (Phila Pa 1976). 2001;26:2587–2595. [DOI] [PubMed]
- 57.Kim D, Brown J. Efficacy and safety of lumbar epidural dexamethasone versus methylprednisolone in the treatment of lumbar radiculopathy: a comparison of soluble versus particulate steroids. Clin J Pain. 2011;27:518–522. doi: 10.1097/AJP.0b013e31820c53e0. [DOI] [PubMed] [Google Scholar]
- 58.Klenerman L, Greenwood R, Davenport HT, White DC, Peskett S. Lumbar epidural injections in the treatment of sciatica. Br J Rheumatol. 1984;23:35–38. doi: 10.1093/rheumatology/23.1.35. [DOI] [PubMed] [Google Scholar]
- 59.Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ. 2007;334:1313–1317. doi: 10.1136/bmj.39223.428495.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kraemer J, Ludwig J, Bickert U, Owczarek V, Traupe M. Lumbar epidural perineural injection: a new technique. Eur Spine J. 1997;6:357–361. doi: 10.1007/BF01142687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Laiq N, Khan MN, Iqbal MJ, Khan S. Comparison of epidural steroid injections with conservative management in patients with lumbar radiculopathy. J Coll Physicians Surg Pak. 2009;19:539–543. [PubMed] [Google Scholar]
- 62.Lavoie PA, Khazen T, Filion PR. Mechanisms of the inhibition of fast axonal transport by local anesthetics. Neuropharmacology. 1989;28:175–181. doi: 10.1016/0028-3908(89)90054-3. [DOI] [PubMed] [Google Scholar]
- 63.Lee JH, An JH, Lee SH. Comparison of the effectiveness of interlaminar and bilateral transforaminal epidural steroid injections in treatment of patients with lumbosacral disc herniation and spinal stenosis. Clin J Pain. 2009;25:206–210. doi: 10.1097/AJP.0b013e3181878f9e. [DOI] [PubMed] [Google Scholar]
- 64.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151:W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 65.Macedo LG, Elkins MR, Maher CG, Moseley AM, Herbert RD, Sherrington C. There was evidence of convergent and construct validity of Physiotherapy Evidence Database quality scale for physiotherapy trials. J Clin Epidemiol. 2010;63:920–925. doi: 10.1016/j.jclinepi.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 66.MacVicar J, King W, Landers MH, Bogduk N. The effectiveness of lumbar transforaminal injection of steroids: a comprehensive review with systematic analysis of the published data. Pain Med. 2013;14:14–28. doi: 10.1111/j.1526-4637.2012.01508.x. [DOI] [PubMed] [Google Scholar]
- 67.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- 68.Makki D, Nawabi DH, Francis R, Hamed AR, Hussein AA. Is the outcome of caudal epidural injections affected by patient positioning? Spine (Phila Pa 1976). 2010;35:E687–E690. [DOI] [PubMed]
- 69.Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, Buenaventura RM, Bryce DA, Burks PA, Caraway DL, Calodney AK, Christo PJ, Cohen SP, Colson J, Conn A, Cordner HJ, Coubarous S, Datta S, Deer TR, Diwan SA, Falco FJ, Fellows B, Geffert SC, Grider JS, Gupta S, Hameed H, Hameed M, Hansen H, Helm S 2nd, Janata JW, Justiz R, Kaye AD, Lee M, Manchikanti KN, McManus CD, Onyewu O, Parr AT, Patel V, Racz GB, Sehgal N, Sharma M, Simopoulos TT, Singh V, Smith HS, Snook LT, Swicegood J, Vallejo R, Ward SP, Wargo BW, Zhu J, Hirsch JA. An update of comprehensive evidence-based guidelines for interventional techniques of chronic spinal pain. Part II. Guidance and recommendations. Pain Physician. 2013;16:S49–S283. [PubMed]
- 70.Manchikanti L, Benyamin RM, Falco FJ, Caraway DL, Datta S, Hirsch JA. Guidelines warfare over interventional techniques: is there a lack of discourse or straw man? Pain Physician. 2012;15:E1–E26. [PubMed] [Google Scholar]
- 71.Manchikanti L, Buenaventura RM, Manchikanti KN, Ruan X, Gupta S, Smith HS, Christo PJ, Ward SP. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician. 2012;15:E199–E245. [PubMed] [Google Scholar]
- 72.Manchikanti L, Cash KA, McManus CD, Damron KS, Pampati V, Falco FJ. Lumbar interlaminar epidural injections in central spinal stenosis: preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012;15:51–63. [PubMed] [Google Scholar]
- 73.Manchikanti L, Cash KA, McManus CD, Pampati V. Fluoroscopic caudal epidural injections in managing chronic axial low back pain without disc herniation, radiculitis or facet joint pain. J Pain Res. 2012;5:381–390. doi: 10.2147/JPR.S35924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Manchikanti L, Cash KA, McManus CD, Pampati V, Benyamin R. Fluoroscopic lumbar interlaminar epidural injections in managing chronic lumbar axial or discogenic pain. J Pain Res. 2012;5:301–311. doi: 10.2147/JPR.S32699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Manchikanti L, Cash KA, McManus CD, Pampati V, Fellows B. Results of 2-year follow-up of a randomized, double-blind, controlled trial of fluoroscopic caudal epidural injections in central spinal stenosis. Pain Physician. 2012;15:371–384. [PubMed] [Google Scholar]
- 76.Manchikanti L, Datta S, Gupta S, Munglani R. Bryce DA, Ward SP, Benyamin RM, Sharma ML, Helm S 2nd, Fellows B, Hirsch JA. A critical review of the American Pain Society clinical practice guidelines for interventional techniques. Part 2. Therapeutic interventions. Pain Physician. 2010;13:E215–E264. [PubMed] [Google Scholar]
- 77.Manchikanti L, Falco FJ, Benyamin RM, Helm S, 2nd, Singh V, Hirsch JA. Value-based interventional pain management: a review of Medicare national and local coverage determination policies. Pain Physician. 2013;16:E145–E180. [PubMed] [Google Scholar]
- 78.Manchikanti L, Falco FJ, Hirsch JA. Epidural corticosteroid injections in the management of sciatica. Ann Intern Med. 2012;157:865–877; online comment posted March 29, 2013. [DOI] [PubMed]
- 79.Manchikanti L, Falco FJ, Pampati V, Cash KA, Benyamin RM, Hirsch JA. Cost utility analysis of caudal epidural injections in the treatment of lumbar disc herniation, central spinal stenosis, post lumbar surgery syndrome, and axial or discogenic low back pain. Pain Physician. 2013;16:E129–E143. [PubMed] [Google Scholar]
- 80.Manchikanti L, Falco FJ, Singh V, Benyamin RM, Racz GB, Helm S, II, Caraway DL, Calodney AK, Snook LT, Smith HS, Gupta S, Ward SP, Grider JS, Hirsch JA. An update of comprehensive evidence-based guidelines for interventional techniques of chronic spinal pain. Part I. Introduction and general considerations. Pain Physician. 2013;16:S1–S48. [PubMed] [Google Scholar]
- 81.Manchikanti L, Falco FJ, Singh V, Pampati V, Parr AT, Benyamin RM, Fellows B, Hirsch JA. Utilization of interventional techniques in managing chronic pain in the Medicare population: analysis of growth patterns from 2000 to 2011. Pain Physician. 2012;15:E969–E982. [PubMed] [Google Scholar]
- 82.Manchikanti L, Giordano J, Fellows B, Hirsch JA. Placebo and nocebo in interventional pain management: a friend or a foe—or simply foes? Pain Physician. 2011;14:E157–E175. [PubMed] [Google Scholar]
- 83.Manchikanti L, Pampati V, Falco FJ, Hirsch JA. A critical analysis of the growth of epidural injections in the Medicare population from 2000 to 2011. Pain Physician. 2013;16:E349–E364. [PubMed] [Google Scholar]
- 84.Manchikanti L, Pampati V, Falco FJ, Hirsch JA. Growth of spinal interventional pain management techniques: analysis of utilization trends and Medicare expenditures 2000 to 2008. Spine (Phila Pa 1976). 2013;38:157–168. [DOI] [PubMed]
- 85.Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. A randomized, controlled, double-blind trial of fluoroscopic caudal epidural injections in the treatment of lumbar disc herniation and radiculitis. Spine (Phila Pa 1976). 2011;36:1897–1905. [DOI] [PubMed]
- 86.Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Effect of fluoroscopically guided caudal epidural steroid or local anesthetic injections in the treatment of lumbar disc herniation and radiculitis: a randomized, controlled, double blind trial with a two-year follow-up. Pain Physician. 2012;15:273–286. [PubMed] [Google Scholar]
- 87.Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Assessment of effectiveness of percutaneous adhesiolysis and caudal epidural injections in managing lumbar post surgery syndrome: a 2-year follow-up of randomized, controlled trial. J Pain Res. 2012;5:597–608. doi: 10.2147/JPR.S38999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Fluoroscopic caudal epidural injections in managing post lumbar surgery syndrome: two-year results of a randomized, double-blind, active-control trial. Int J Med Sci. 2012;9:582–591. doi: 10.7150/ijms.4672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Manchikanti L, Singh V, Cash KA, Pampati V, Falco FJ. The role of fluoroscopic interlaminar epidural injections in managing chronic pain of lumbar disc herniation or radiculitis: a randomized, double-blind trial. Pain Pract. 2013;13:547–558. doi: 10.1111/papr.12023. [DOI] [PubMed] [Google Scholar]
- 90.Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Evaluation of lumbar facet joint nerve blocks in managing chronic low back pain: a randomized, double-blind, controlled trial with a 2-year follow-up. Int J Med Sci. 2010;7:124–135. doi: 10.7150/ijms.7.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Evaluation of the effectiveness of lumbar interlaminar epidural injections in managing chronic pain of lumbar disc herniation or radiculitis: a randomized, double-blind, controlled trial. Pain Physician. 2010;13:343–355. [PubMed] [Google Scholar]
- 92.Mathews JA, Mills SB, Jenkins VM, Grimes SM, Morkel MJ, Mathews W, Scott CM, Sittampalam Y. Back pain and sciatica: controlled trials of manipulation, traction, sclerosant and epidural injection. Br J Rheumatol. 1987;26:416–423. doi: 10.1093/rheumatology/26.6.416. [DOI] [PubMed] [Google Scholar]
- 93.McCahon RA, Ravenscroft A, Hodgkinson V, Evley R, Hardman J. A pilot study of the dose-response of caudal methylprednisolone with levobupivacaine in chronic lower back pain. Anaesthesia. 2011;66:595–603. doi: 10.1111/j.1365-2044.2011.06764.x. [DOI] [PubMed] [Google Scholar]
- 94.McGregor AH, Anjarwalla NK, Stambach T. Does the method of injection alter the outcome of epidural injections? J Spinal Disord. 2001;14:507–510. doi: 10.1097/00002517-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 95.Murakibhavi VG, Khemka AG. Caudal epidural steroid injection: a randomized controlled trial. Evid Based Spine Care J. 2011;2:19–26. doi: 10.1055/s-0031-1274753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ng L, Chaudhary N, Sell P. The efficacy of corticosteroids in periradicular infiltration for chronic radicular pain: a randomized, double-blind, controlled trial. Spine (Phila Pa 1976). 2005;30:857–862. [DOI] [PubMed]
- 97.Park CH, Lee SH, Kim BI. Comparison of the effectiveness of lumbar transforaminal epidural injection with particulate and nonparticulate corticosteroids in lumbar radiating pain. Pain Med. 2010;11:1654–1658. doi: 10.1111/j.1526-4637.2010.00941.x. [DOI] [PubMed] [Google Scholar]
- 98.Park CH, Lee SH, Park HS. Lumbar retrodiscal versus post-ganglionic transforaminal epidural steroid injection for the treatment of lumbar intervertebral disc herniations. Pain Physician. 2011;14:353–360. [PubMed] [Google Scholar]
- 99.Park KD, Lee J, Jee H, Park Y. Kambin triangle versus the supraneural approach for the treatment of lumbar radicular pain. Am J Phys Med Rehabil. 2012;91:1039–1050. doi: 10.1097/PHM.0b013e318264573a. [DOI] [PubMed] [Google Scholar]
- 100.Parr AT, Manchikanti L, Hameed H, Conn A, Manchikanti KN, Benyamin RM, Diwan S, Singh V, Abdi S. Caudal epidural injections in the management of chronic low back pain: a systematic appraisal of the literature. Pain Physician. 2012;15:E159–E198. [PubMed] [Google Scholar]
- 101.Pasqualucci A. Experimental and clinical studies about the preemptive analgesia with local anesthetics: possible reasons of the failure. Minerva Anestesiol. 1998;64:445–457. [PubMed] [Google Scholar]
- 102.Pasqualucci A, Varrassi G, Braschi A, Peduto VA, Brunelli A, Marinangeli F, Gori F, Colò F, Paladín A, Mojoli F. Epidural local anesthetic plus corticosteroid for the treatment of cervical brachial radicular pain: single injection versus continuous infusion. Clin J Pain. 2007;23:551–557. doi: 10.1097/AJP.0b013e318074c95c. [DOI] [PubMed] [Google Scholar]
- 103.Pinto RZ, Maher CG, Ferreira ML, Hancock M, Oliveira VC, McLachlan AJ, Koes B, Ferreira PH. Epidural corticosteroid injections in the management of sciatica: a systematic review and meta-analysis. Ann Intern Med. 2012;157:865–877. doi: 10.7326/0003-4819-157-12-201212180-00564. [DOI] [PubMed] [Google Scholar]
- 104.Pirbudak L, Karakurum G, Oner U, Gulec A, Karadasli H. Epidural corticosteroid injection and amitriptyline for the treatment of chronic low back pain associated with radiculopathy. Pain Clinic. 2003;15:247–253. [Google Scholar]
- 105.Price C, Arden N, Coglan L, Rogers P. Cost-effectiveness and safety of epidural steroids in the management of sciatica. Health Technol Assess. 2005;9:1–58, iii. [DOI] [PubMed]
- 106.Quraishi NA. Transforaminal injection of corticosteroids for lumbar radiculopathy: systematic review and meta-analysis. Eur Spine J. 2012;21:214–219. doi: 10.1007/s00586-011-2008-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rados I, Sakic K, Fingler M, Kapural L. Efficacy of interlaminar vs transforaminal epidural steroid injection for the treatment of chronic unilateral radicular pain: prospective, randomized study. Pain Med. 2011;12:1316–1321. doi: 10.1111/j.1526-4637.2011.01213.x. [DOI] [PubMed] [Google Scholar]
- 108.Rasmussen S, Krum-Møller DS, Lauridsen LR, Jensen SE, Mandøe H, Gerlif C, Kehlet H. Epidural steroid following discectomy for herniated lumbar disc reduces neurological impairment and enhances recovery: a randomized study with two-year follow-up. Spine (Phila Pa 1976). 2008;33:2028–2033. [DOI] [PubMed]
- 109.Rho ME, Tang CT. The efficacy of lumbar epidural steroid injections: transforaminal, interlaminar, and caudal approaches. Phys Med Rehabil Clin N Am. 2011;22:139–148. doi: 10.1016/j.pmr.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 110.Ridley MG, Kingsley GH, Gibson T, Grahame R. Outpatient lumbar epidural corticosteroid injection in the management of sciatica. Br J Rheumatol. 1988;27:295–299. doi: 10.1093/rheumatology/27.4.295. [DOI] [PubMed] [Google Scholar]
- 111.Riew KD, Park JB, Cho YS, Gilula L, Patel A, Lente LG, Bridwell KH. Nerve root blocks in the treatment of lumbar radicular pain: a minimum five-year follow-up. J Bone Joint Surg Am. 2006;88:1722–1725. doi: 10.2106/JBJS.E.00278. [DOI] [PubMed] [Google Scholar]
- 112.Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C, Goette K. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain: a prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am. 2000;82:1589–1593. doi: 10.2106/00004623-200011000-00012. [DOI] [PubMed] [Google Scholar]
- 113.Roberts ST, Willick SE, Rho ME, Rittenberg JD. Efficacy of lumbosacral transforaminal epidural steroid injections: a systematic review. PM R. 2009;1:657–668. doi: 10.1016/j.pmrj.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 114.Rogers P, Nash T, Schiller D, Norman J. Epidural steroids for sciatica. Pain Clinic. 1992;5:67–72. [Google Scholar]
- 115.Sato C, Sakai A, Ikeda Y, Suzuki H, Sakamoto A. The prolonged analgesic effect of epidural ropivacaine in a rat model of neuropathic pain. Anesth Analg. 2008;106:313–320. doi: 10.1213/01.ane.0000296460.91012.51. [DOI] [PubMed] [Google Scholar]
- 116.Sayegh FE, Kenanidis EI, Papavasiliou KA, Potoupnis ME, Kirkos JM, Kapetanos GA. Efficacy of steroid and nonsteroid caudal epidural injections for low back pain and sciatica: a prospective, randomized, double-blind clinical trial. Spine (Phila Pa 1976). 2009;34:1441–1447. [DOI] [PubMed]
- 117.Selim AJ, Ren XS, Fincke G, Deyo RA, Rogers W, Miller D, Linzer M, Kazis L. The importance of radiating leg pain in assessing health outcomes among patients with low back pain: results from the Veterans Health Study. Spine (Phila Pa 1976). 1998;23:470–474. [DOI] [PubMed]
- 118.Snoek W, Weber H, Jorgensen B. Double-blind evaluation of extradural methylprednisolone for herniated lumbar disc. Acta Orthop Scand. 1977;48:635–641. doi: 10.3109/17453677708994810. [DOI] [PubMed] [Google Scholar]
- 119.Staal JB, de Bie RA, de Vet HC, Hildebrandt J, Nelemans P. Injection therapy for subacute and chronic low back pain: an updated Cochrane review. Spine (Phila Pa 1976). 2009;34:49–59. [DOI] [PubMed]
- 120.Tachihara H, Sekiguchi M, Kikuchi S, Konno S. Do corticosteroids produce additional benefit in nerve root infiltration for lumbar disc herniation. Spine (Phila Pa 1976). 2008;33:743–747. [DOI] [PubMed]
- 121.Tafazal S, Ng L, Chaudhary N, Sell P. Corticosteroids in peri-radicular infiltration for radicular pain: a randomised double blind controlled trial: one year results and subgroup analysis. Eur Spine J. 2009;18:1220–1225. doi: 10.1007/s00586-009-1000-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Thomas E, Cyteval C, Abiad L, Picot MC, Taourel P, Blotman F. Efficacy of transforaminal versus interspinous corticosteroid injection in discal radiculalgia—a prospective, randomised, double-blind study. Clin Rheumatol. 2003;22:299–304. doi: 10.1007/s10067-003-0736-z. [DOI] [PubMed] [Google Scholar]
- 123.Tubach F, Beauté J, Leclerc A. Natural history and prognostic indicators of sciatica. J Clin Epidemiol. 2004;57:174–179. doi: 10.1016/S0895-4356(03)00257-9. [DOI] [PubMed] [Google Scholar]
- 124.Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine(Phila Pa 1976). 2002;27:11–16. [DOI] [PubMed]
- 125.Valat JP, Genevay S, Marty M, Rozenberg S, Koes B. Sciatica. Best Pract Res Clin Rheumatol. 2010;24:241–252. doi: 10.1016/j.berh.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 126.Valat JP, Giraudeau B, Rozenberg S, Goupille P, Bourgeois P, Micheau-Beaugendre V, Soubrier M, Richard S, Thomas E. Epidural corticosteroid injections for sciatica: a randomised, double blind, controlled clinical trial. Ann Rheum Dis. 2003;62:639–643. doi: 10.1136/ard.62.7.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, Abdu WA, Hilibrand AS, Boden SD, Deyo RA. Surgical vs nonoperative treatment for lumbar disk herniation: The Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441–2450. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wilson-MacDonald J, Burt G, Griffin D, Glynn C. Epidural steroid injection for nerve root compression: a randomized, controlled trial. J Bone Joint Surg Br. 2005;87:352–355. doi: 10.1302/0301-620x.87b3.15338. [DOI] [PubMed] [Google Scholar]
- 129.Wittenberg RH, Greskötter KR, Steffen R, Schoenfeld BL. Is epidural injection treatment with hypertonic saline solution in intervertebral disk displacement useful? (The effect of NaCl solution on intervertebral disk tissue) [in German] Z Orthop Ihre Grenzgeb. 1990;128:223–226. doi: 10.1055/s-2008-1039504. [DOI] [PubMed] [Google Scholar]
- 130.Zahaar MS. The value of caudal epidural steroids in the treatment of lumbar neural compression syndromes. J Neurol Orthop Med Surg. 1991;12:181–184. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.