Abstract
Asymmetric-dimethylarginine (ADMA) competes with L-arginine for each of the three isoforms of nitric oxide synthase: endothelial; neuronal; inducible. ADMA is synthesized by protein methyltransferases followed by proteolytic degradation. ADMA is metabolized to citrulline and dimethylamine, by dimethylarginine dimethylaminohydrolase (DDAH) and enters cells through cationic amino-acid transporters extensively expressed in the liver. The liver plays a crucial role in ADMA metabolism by DDAH-1 and, as has been recently demonstrated, it is also responsible for ADMA biliary excretion. A correlation has been demonstrated between plasma ADMA levels and the degree of hepatic dysfunction in patients suffering from liver diseases with varying aetiologies: plasma ADMA levels are increased in patients with liver cirrhosis, alcoholic hepatitis and acute liver failure. The mechanism by which liver dysfunction results in raised ADMA concentrations is probably due to impaired activity of DDAH due to severe inflammation, oxidative stress, and direct damage to DDAH. High plasma ADMA levels are also relevant as they are associated with the onset of multi-organ failure (MOF). Increased plasma concentration of ADMA was identified as an independent risk factor for MOF in critically-ill patients causing enhanced Intensive Care Unit mortality: a significant reduction in nitric oxide synthesis, leading to malperfusion in various organs, eventually culminating in multi organs dysfunction.
Keywords: Liver, Asymmetric dimethylarginine, Nitric oxide, Nitric oxide-synthase, Multiple organ failure
Core tip: Nitric oxide (NO) synthesis is blocked by asymmetric dimethylarginine (ADMA) which competes with L-arginine for NO-synthase. ADMA is metabolized principally in the liver, by dimethylarginine dimethylaminohydrolase. The kidney and the liver are involved in ADMA excretion. A correlation exists between plasma ADMA levels and degree of hepatic dysfunction in patients suffering from liver cirrhosis, alcoholic hepatitis and acute liver failure. High plasma ADMA levels are relevant because they are associated with the development of multi-organ failure (MOF): increased plasma ADMA concentration was identified as a risk factor for MOF in critically-ill patients causing enhanced Intensive Care Unit mortality.
SYNTHESIS, METABOLISM AND EXCRETION OF ADMA
In the early 1990s, Vallance and colleagues, showed that nitric oxide (NO) synthesis could be inhibited by the endogenous circulating amino-acid asymmetric dimethylarginine (ADMA) by inhibition of NO-synthase (NOS)[1]. ADMA competes with L-arginine for each of the three isoforms of NOS, endothelial (eNOS), neuronal (nNOS) and inducible (iNOS) NOS[2]. ADMA is considered to be an important marker of endothelial dysfunction because of its inhibiting role in NO synthesis. In addition, ADMA is also able to inhibit NO synthesis by competing with arginine and symmetric dimethylarginine (SDMA) for cellular transport across cationic amino-acid transporters (CATs). Interestingly, the liver expresses CATs abundantly, especially CAT-2A and CAT-2B, suggesting a higher uptake of ADMA in this organ as compared with the heart, lungs and kidneys[3]. The CAT-2B are low-capacity transporters that have a high affinity for cationic amino acids and in particular present high affinity for ADMA[4]. In contrast, CAT-2A, an alternate splice variant of CAT-2B, possesses low affinity but high transport capacity.
The first step in the synthesis of methylarginines, is the methylation of protein arginine residues by intracellular enzymes termed protein methyltransferases (PRMTs). The second step relates to the proteolytic degradation of the methylated protein which produces free ADMA and SDMA, the latter not biologically active[5]. Protein synthesis and proteolysis are anabolic and catabolic counterparts of protein turnover, respectively[6].
Intracellular ADMA is metabolized to citrulline and dimethylamine, a reaction catalyzed by dimethylarginine dimethylaminohydrolase (DDAH)[7] (Figure 1). The liver and kidneys represent the main sites of ADMA metabolism: DDAH is widely distributed in rats and human subjects, in particular, in the liver, kidney and pancreas[8,9]. This enzyme is very sensitive to oxidative stress because its active site contains a critical sulfhydryl group required for its catalytic activity[10]. Two isoforms of DDAH, Types 1 and 2, have emerged as critical regulators of NO bioavailability[11]. Studies of gene silencing or deletion in rodents have led to the conclusion that plasma levels of ADMA are regulated by DDAH-1, whereas the significance of DDAH-2 lies in preserving the endothelial function[11]. Nijveldt et al[12] provide a detailed insight into the liver’s handling of ADMA, demonstrating that it plays a crucial role in ADMA metabolism, with DDAH taking up a large amount of this dimethylarginine from the circulatory system.
Figure 1.
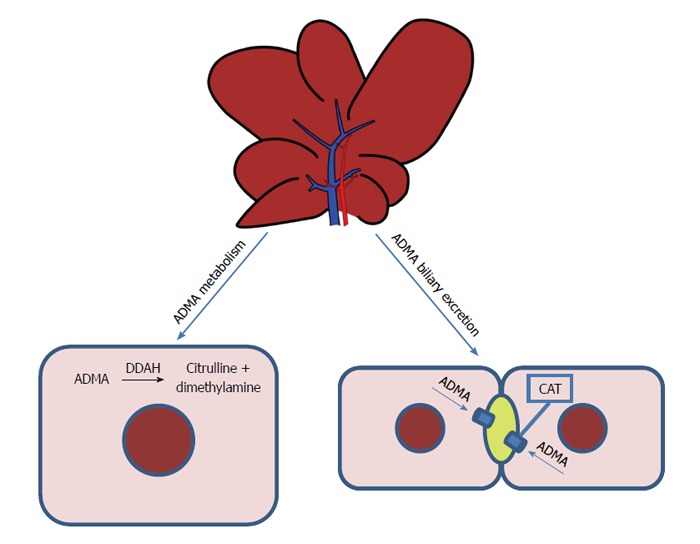
Metabolism and excretion of asymmetric dimethylarginine in the liver. Intracellular asymmetric dimethylarginine (ADMA) is metabolized to citrulline and dimethylamine, a reaction catalyzed by dimethylarginine dimethylaminohydrolase (DDAH). The liver is responsible for the biliary excretion of ADMA. CAT: Cationic amino-acid transporters.
The kidney plays an important role in ADMA excretion from the body, since ADMA is found in human urine[13]. Recently, we demonstrated that the liver, too, is responsible for the biliary excretion of ADMA (Figure 1): for the first time, this methylarginine was found in bile and a time-dependent increase in biliary excretion was shown to occur during I/R injury[14].
Understanding the mechanisms involved in ADMA synthesis, metabolism and excretion increases the possibility of understanding its modulation, which is crucial in several pathological conditions[15-17].
ADMA AND LIVER DISEASES
Although ADMA has been shown to correlate with cardiovascular risk factors[17], its plasma concentration also increases in patients suffering from end-stage kidney disease[1] and hepatic dysfunction[15]. In particular, a significant correlation has been demonstrated between plasma ADMA levels and the degree of hepatic dysfunction in patients suffering from liver diseases with varying aetiologies[18-20]. Notably, plasma ADMA levels are increased in patients with liver cirrhosis[20], alcoholic hepatitis[21] and acute liver failure[15]. Patients with decompensated cirrhosis have higher ADMA levels compared to compensated cirrhosis; these levels increase further with evolving liver failure[21]. An increase in ADMA plasma levels also occurs in patients with alcoholic cirrhosis associated with an increase in nitrate-nitrite concentrations. This event was probably caused by impaired hepatic removal and, in the cirrhotic liver, may be a prominent factor determining high intrahepatic vascular resistance and the progression of the disease[20].
The high portal pressures observed in alcoholic hepatitis patients were associated with the increased ADMA, which may result from both decreased breakdown (decreased hepatic DDAH) and/or increased production[21]. The mechanism by which liver dysfunction results in raised ADMA concentrations is probably due to impaired DDAH activity, which is highly expressed in normal livers: local processes such as severe inflammation, oxidative stress, and direct damage to DDAH protein may underlie a significant deterioration in DDAH activity in critically ill patients with hepatic dysfunction leading to elevation of ADMA concentrations[22]. High ADMA plasma concentrations may serve as important biological markers of adverse outcomes in alcoholic hepatitis[21].
In support of a crucial role for the liver as an ADMA eliminating organ, its concentration, elevated during hepatic failure, undergoes significant decline on the first postoperative day after liver transplantation, suggesting that DDAH activity is preserved during the transplantation procedure[23]. The hepatic function contributes to ADMA regulation as evidenced by an initial small increase in ADMA during the anhepatic phase of the transplant operation, consistent with complete absence of hepatic DDAH activity[15]. Following restoration of portal and hepatic arterial flow with a new graft placement, there is a significant reduction in ADMA levels, in an environment with reduced inflammatory drive[15]. Notably, in the 85% of patients who rejected the liver graft, a clear increase in ADMA concentrations preceded the onset of the first episode of rejection[23]. Correlation between methylarginine derivates and liver function and survival after liver transplantation was also observed[24].
Furthermore, Mookerjee et al[15] have reported that patients with acute liver failure showed elevated ADMA levels also related to the severity of inflammation supporting the hypothesis that proinflammatory cytokines may regulate ADMA metabolism. Recent results have demonstrated that plasma ADMA evaluation appears to be an early predictor for survival in patients with sepsis associated to acute liver failure[25].
The hepatic I/R injury induced changes on the ADMA/DDAH pathway; consequently, this pathway should be considered as a point of interest potentially capable of reducing the effects of I/R. In particular, the decrease in DDAH-1 activity observed after hepatic I/R is associated with a reduction in mRNA and protein expression and an increase in serum ADMA levels in the early reperfusion period (1 h)[14]. Recent data in rat liver subjected to I/R has confirmed a decrease in DDAH activity[26]. Lanteri et al[27] observed an increase in DDAH-1 expression when the tissue DDAH-1 was evaluated after three hours’ reperfusion.
The serum concentration of ADMA is negatively associated with DDAH activity in the liver[28]. In addition, we observed a decrease in intracellular ADMA levels during reperfusion, together with ADMA release both in the circulation and bile[14].
Increases in serum ADMA levels were also detected two weeks after experimental BDL[29,30], while on the contrary in a period close to BDL-induced damage, no increase in serum ADMA levels was found, even though a tissue increase in ADMA occurred in the days immediately after BDL[31]. In addition, ADMA is significantly higher in the right and median lobes as compared with the left lobe; this heterogeneity is probably associated with a decrease in CAT-2 transporters, particularly evident in RL and ML when compared with the respective sham-operated group[31]. In addition, a decrease in CAT-2 transporters associated with an increase in tissue ADMA was also described 2 wk after BDL[29].
The mechanism by which ADMA causes increased risk of adverse outcome in critically ill patients is probably by inhibition of endothelial nitric oxide elaboration. High ADMA concentrations block NOS[1] and inhibit endothelium-dependent vasodilation in both animals[32] and human beings[33]. The crucial role of the liver can be explained by the high expression of the ADMA-degrading enzyme DDAH, which makes the liver a prime organ in the clearing of ADMA[22]. Interestingly, liver abundantly also express CATs, especially CAT-2A and CAT-2B, and the extensive hepatic expression of CAT-2A mRNA suggests a higher uptake of ADMA in this organ as compared with the heart, lungs and kidneys[3]. Accordingly, the occurrence of liver dysfunction in critical illness places other organs at risk, especially organs that are strongly dependent on basal nitric oxide production[22].
MULTIPLE ORGAN FAILURE AND ADMA
Multi organ failure (MOF) is the concurrent dysfunction of several organs. It is considered the most challenging problem in Intensive Care Unit (ICU) patients: in patients with MOF, the mortality becomes higher, ranging from 30%-80% depending on the number of failed organs[34]. Sepsis and severe trauma are considered the main predisposing factors for the development of MOF. A pivotal role is traditionally attributed to the kidneys and liver in MOF development; however a unifying mechanism has been recently proposed by Nijveldt et al[18], currently known as the ADMA-MOF hypothesis. The hypothesis came into being after a Phase III trial, when the unspecific NOS inhibitor NG-monomethylarginine was shown to increase mortality rates in patients with septic shock[35]. In this trial, the use of the NOS inhibitor was mainly intended to reduce the production of excessive amounts of NO: due to the physiopathological roles of this molecule, NO was assumed to have a role in the deterioration of septic patients, raising the suggestion that NOS inhibitors may have a therapeutic potential.
The three known isoforms of NOS are iNOS, nNOS and eNOS. iNOS expression can be induced by bacterial lipopolysaccharide, cytokines, and other agents. When induced in macrophages, iNOS produces large amounts of NO, which represents these cells’ major weapon due to its cytostatic and cytotoxic effects against parasitic micro-organisms and certain tumours[36]. The overproduction of NO in response to septic shock may harm healthy cells when NO is released in the wrong site. This is because cell and tissue damage is attributable to the NO radical itself or to the peroxynitrite ONOO-, whose production arises from the interaction between NO and O2-•[36]. nNOS is constitutively expressed in central and peripheral neurons; its functions include central regulation of blood pressure, smooth muscle relaxation and vasodilatation via peripheral nitrergic nerves[37] (Figure 2). eNOS, due to its localization, is a homeostatic regulator of blood pressure and blood flow, vascular smooth-muscle proliferation, platelet aggregation and leukocyte adhesion[38].
Figure 2.
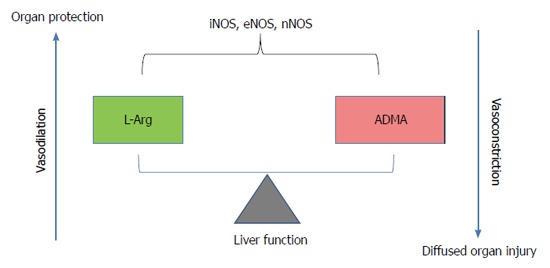
Role of arginine/asymmetric dimethylarginine ratio. Asymmetric dimethylarginine accumulation blocks nitric oxide synthase (NOS) and induces consequent endothelial dysfunction in the vasculature. On the contrary, high arginine levels as substrate for NOS induces vasodilatation. ADMA: Asymmetric dimethylarginine; iNOS: Inducible nitric oxide-synthase; eNOS: Endothelial nitric oxide-synthase; nNOS: Neuronal nitric oxide-synthase.
As has been already clarified, ADMA inhibits NO synthesis by competing with L-arginine for cellular transport across CATs, and for binding with the three isoforms of NOS. Already in 1995, Huang et al[39] had observed that the pharmacological blockade of NO production with arginine analogues, could simultaneously affect multiple isoforms of NOS; more importantly, they showed that mutant mice lacking the eNOS gene were hypertensive due to the absence of endothelium-derived relaxing factor activity, a mechanism independent of non-endothelial isoforms of NOS. In another ex vivo experiment on isolated rat hearts from endotoxin-treated animals, coronary flow was elevated compared with control hearts; the addition of an NO-synthesis inhibitor to the perfusion medium decreased coronary flow, but local ischemic events still occurred. This local ischemia was reverted by the infusion of L-arginine, so increasing the arginine/ADMA ratio[40].
These results suggest that, in critical illness, the regulation of organ perfusion by NO is of vital importance. Not surprisingly, worsening conditions in critically ill patients are often associated with increased serum ADMA. Nijveldt et al[22] showed that critically ill patients are exposed to elevated ADMA plasma levels, and, importantly, that plasma ADMA concentration was independently related to the presence of hepatic failure. Furthermore, plasma ADMA ranked as the first and strongest predictor for outcome, with an increased risk for patients who were in the highest quartile for ADMA. Recently, it has been shown that the arginine/ADMA ratio is a more powerful predictor of organ failure with respect to ADMA alone. The arginine/ADMA ratio in ICU patients is associated with circulatory failure, organ failure and mortality in septic patients[41,42].
WHAT MIGHT BE THE MECHANISM BEHIND RAISED ADMA LEVELS IN CRITICALLY ILL PATIENTS?
Up-regulation of iNOS occurring in sepsis leads to the release of huge amounts of oxidants. Kupffer cells play a major role in this process as they can release large amounts of inflammatory mediators; the leukocytes activated by the Kupffer cells are an important local source of free radicals, which cause oxidative damage to DNA, membrane lipids and proteins. DDAH, the enzyme responsible for ADMA degradation, is a potential target of reactive species: S-nitrosylation of DDAH-2 has been shown to reduce this enzyme’s activity, leading to the accumulation of ADMA[43]. Many cardiovascular risk factors lead to oxidative stress too, contributing to eNOS uncoupling, ADMA accumulation with consequent endothelial dysfunction in the vasculature[37]. This local increase in ADMA could be the initial cause of liver malperfusion, leading to compromised liver function. Due to the main role of liver in ADMA metabolization, a worsening of the liver function causes a further increase in ADMA in serum, further compromising the perfusion flow of the liver and other organs. For this reason, the liver is considered as playing a crucial role in MOF[44]. Alternatively, pre-existent liver failure or a change causing reduced clearance capability for serum ADMA, could be a decisive contributing factor in MOF development. In septic patients with an acute liver failure, plasma levels of ADMA were significantly increased with respect to patients with an intact hepatic function[25]. Furthermore, it has been shown that defective DDAH, along with the removal of liver tissue and prolonged hepatic injury, influences the liver’s capacity to eliminate ADMA, resulting in higher systemic levels of ADMA and a lower arginine/ADMA ratio[45,46]. In a prospective study, a positive correlation between raised ADMA levels and severity of organ failure, inflammation and presence of early shock in severe sepsis was observed. Furthermore, higher ADMA levels were associated to the occurrence of a genetic polymorphism in the DDAH-2 gene, so a correlation between a defective DDAH-2 gene and the extent of MOF has been proposed by the authors[47]. These studies confirm the pivotal role of the liver, and more specifically, of hepatic DDAH enzymatic activity, in the insurgence of MOF.
The increased circulatory ADMA and MOF have been recently reviewed in a model of cholestasis: the ADMA and NO dysregulation were particularly evaluated into extrahepatic organs such as kidney, brain and heart[48]. The understanding of the role and regulation of ADMA could have clinical implications to treat not only cholestatic liver disease but also ADMA-related disorders.
Other studies suggest that, secondarily to the liver, the kidney, too, plays a role in ADMA accumulation. Patients suffering from renal failure exhibit impaired urinary excretion, reduced arginine synthesis and impaired DDAH activity, all factors leading to increased serum ADMA concentrations[49]. Increased serum levels of ADMA predict the progression to dialysis and death in patients with chronic kidney disease. A randomized, double-blind, placebo-controlled study on cardiovascular and renal outcomes in 2102 renal transplant recipients found ADMA to be a significant risk factor for graft failure, major cardiac events, cerebrovascular events, and all-cause mortality[50]. Other factors contributing to an imbalance in the arginine/ADMA ratio and potentially with a role in MOF are: a higher amount of protein methylation and an increased rate of protein turnover[45]. In a recent study, critically ill patients and healthy volunteers were given isotopically labelled amino acids in order to assess whole protein turnover. In this study, critically ill patients’ whole body protein turnover was significantly higher than that of healthy volunteers during parenteral nutrition delivery[51]. The mechanism by which protein turnover increases in critically ill patients has yet to be elucidated.
CONCLUSION
MOF is the concurrent dysfunction of several organs. Higher morbidity and mortality has been observed in patients with higher serum ADMA[22,41,42]; currently ADMA is considered to be not merely an asymptomatic index but, additionally, a risk factor. The ADMA-MOF hypothesis holds that the liver plays a pivotal role. Liver is the main organ devoted to ADMA clearance; this hepatic capability can be compromised by various factors, such as: severe organ injury, free radical release compromising DDAH activity, genetic polymorphism for hepatic DDAH[25,45-47]. These conditions, with the exception of congenital polymorphism, occur especially in sepsis, but other forms of trauma, as tumours or ischemic injury, can also produce the same result. In all these cases, the loss of liver function causes an imbalance in the arginine/ADMA ratio and the subsequent inhibition of eNOS, resulting in a significant reduction in NO synthesis and leading to malperfusion in various organs, eventually culminating in multi-organ failure. It has been observed that the arginine/ADMA ratio is a better predictor of morbidity and mortality than ADMA alone, suggesting that the restoration of this ratio, for example by means of the administration of L-arginine, should be considered a suitable option when attempting to improve a patient’s condition[45].
ACKNOWLEDGMENTS
We thank Professor Anthony Baldry for revising the English and Mrs. Nicoletta Breda for editing assistance.
Footnotes
Supported by Fondazione Cariplo, Grant No. 2011-0439.
Conflict-of-interest: Authors declare no conflict of interest.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: January 28, 2015
First decision: February 10, 2015
Article in press: March 31, 2015
P- Reviewer: Dirchwolf M, Eid NAS, Elalfy H S- Editor: Qi Y L- Editor: A E- Editor: Ma S
References
- 1.Vallance P, Leone A, Calver A, Collier J, Moncada S. Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet. 1992;339:572–575. doi: 10.1016/0140-6736(92)90865-z. [DOI] [PubMed] [Google Scholar]
- 2.Förstermann U, Schmidt HH, Pollock JS, Sheng H, Mitchell JA, Warner TD, Nakane M, Murad F. Isoforms of nitric oxide synthase. Characterization and purification from different cell types. Biochem Pharmacol. 1991;42:1849–1857. doi: 10.1016/0006-2952(91)90581-o. [DOI] [PubMed] [Google Scholar]
- 3.Hattori Y, Kasai K, Gross SS. Cationic amino acid transporter gene expression in cultured vascular smooth muscle cells and in rats. Am J Physiol. 1999;276:H2020–H2028. doi: 10.1152/ajpheart.1999.276.6.H2020. [DOI] [PubMed] [Google Scholar]
- 4.Closs EI, Gräf P, Habermeier A, Cunningham JM, Förstermann U. Human cationic amino acid transporters hCAT-1, hCAT-2A, and hCAT-2B: three related carriers with distinct transport properties. Biochemistry. 1997;36:6462–6468. doi: 10.1021/bi962829p. [DOI] [PubMed] [Google Scholar]
- 5.Zakrzewicz D, Eickelberg O. From arginine methylation to ADMA: a novel mechanism with therapeutic potential in chronic lung diseases. BMC Pulm Med. 2009;9:5. doi: 10.1186/1471-2466-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teerlink T. ADMA metabolism and clearance. Vasc Med. 2005;10 Suppl 1:S73–S81. doi: 10.1191/1358863x05vm597oa. [DOI] [PubMed] [Google Scholar]
- 7.MacAllister RJ, Parry H, Kimoto M, Ogawa T, Russell RJ, Hodson H, Whitley GS, Vallance P. Regulation of nitric oxide synthesis by dimethylarginine dimethylaminohydrolase. Br J Pharmacol. 1996;119:1533–1540. doi: 10.1111/j.1476-5381.1996.tb16069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kimoto M, Tsuji H, Ogawa T, Sasaoka K. Detection of NG,NG-dimethylarginine dimethylaminohydrolase in the nitric oxide-generating systems of rats using monoclonal antibody. Arch Biochem Biophys. 1993;300:657–662. doi: 10.1006/abbi.1993.1091. [DOI] [PubMed] [Google Scholar]
- 9.Kimoto M, Whitley GS, Tsuji H, Ogawa T. Detection of NG,NG-dimethylarginine dimethylaminohydrolase in human tissues using a monoclonal antibody. J Biochem. 1995;117:237–238. doi: 10.1093/jb/117.2.237. [DOI] [PubMed] [Google Scholar]
- 10.Murray-Rust J, Leiper J, McAlister M, Phelan J, Tilley S, Santa Maria J, Vallance P, McDonald N. Structural insights into the hydrolysis of cellular nitric oxide synthase inhibitors by dimethylarginine dimethylaminohydrolase. Nat Struct Biol. 2001;8:679–683. doi: 10.1038/90387. [DOI] [PubMed] [Google Scholar]
- 11.Palm F, Onozato ML, Luo Z, Wilcox CS. Dimethylarginine dimethylaminohydrolase (DDAH): expression, regulation, and function in the cardiovascular and renal systems. Am J Physiol Heart Circ Physiol. 2007;293:H3227–H3245. doi: 10.1152/ajpheart.00998.2007. [DOI] [PubMed] [Google Scholar]
- 12.Nijveldt RJ, Teerlink T, Siroen MP, van Lambalgen AA, Rauwerda JA, van Leeuwen PA. The liver is an important organ in the metabolism of asymmetrical dimethylarginine (ADMA) Clin Nutr. 2003;22:17–22. doi: 10.1054/clnu.2002.0612. [DOI] [PubMed] [Google Scholar]
- 13.Zoccali C. Asymmetric dimethylarginine in end-stage renal disease patients: a biomarker modifiable by calcium blockade and angiotensin II antagonism? Kidney Int. 2006;70:2053–2055. doi: 10.1038/sj.ki.5001898. [DOI] [PubMed] [Google Scholar]
- 14.Ferrigno A, Rizzo V, Bianchi A, Di Pasqua LG, Berardo C, Richelmi P, Vairetti M. Changes in ADMA/DDAH pathway after hepatic ischemia/reperfusion injury in rats: the role of bile. Biomed Res Int. 2014;2014:627434. doi: 10.1155/2014/627434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mookerjee RP, Dalton RN, Davies NA, Hodges SJ, Turner C, Williams R, Jalan R. Inflammation is an important determinant of levels of the endogenous nitric oxide synthase inhibitor asymmetric dimethylarginine (ADMA) in acute liver failure. Liver Transpl. 2007;13:400–405. doi: 10.1002/lt.21053. [DOI] [PubMed] [Google Scholar]
- 16.Kielstein JT, Zoccali C. Asymmetric dimethylarginine: a cardiovascular risk factor and a uremic toxin coming of age? Am J Kidney Dis. 2005;46:186–202. doi: 10.1053/j.ajkd.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 17.He H, Wang S, Li X, Wang H, Zhang W, Yuan L, Liu X. A novel metabolic balance model for describing the metabolic disruption of and interactions between cardiovascular-related markers during acute myocardial infarction. Metabolism. 2013;62:1357–1366. doi: 10.1016/j.metabol.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 18.Nijveldt RJ, Teerlink T, van Leeuwen PA. The asymmetrical dimethylarginine (ADMA)-multiple organ failure hypothesis. Clin Nutr. 2003;22:99–104. doi: 10.1054/clnu.2002.0614. [DOI] [PubMed] [Google Scholar]
- 19.Davis JS, Darcy CJ, Yeo TW, Jones C, McNeil YR, Stephens DP, Celermajer DS, Anstey NM. Asymmetric dimethylarginine, endothelial nitric oxide bioavailability and mortality in sepsis. PLoS One. 2011;6:e17260. doi: 10.1371/journal.pone.0017260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lluch P, Torondel B, Medina P, Segarra G, Del Olmo JA, Serra MA, Rodrigo JM. Plasma concentrations of nitric oxide and asymmetric dimethylarginine in human alcoholic cirrhosis. J Hepatol. 2004;41:55–59. doi: 10.1016/j.jhep.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 21.Mookerjee RP, Malaki M, Davies NA, Hodges SJ, Dalton RN, Turner C, Sen S, Williams R, Leiper J, Vallance P, et al. Increasing dimethylarginine levels are associated with adverse clinical outcome in severe alcoholic hepatitis. Hepatology. 2007;45:62–71. doi: 10.1002/hep.21491. [DOI] [PubMed] [Google Scholar]
- 22.Nijveldt RJ, Teerlink T, Van Der Hoven B, Siroen MP, Kuik DJ, Rauwerda JA, van Leeuwen PA. Asymmetrical dimethylarginine (ADMA) in critically ill patients: high plasma ADMA concentration is an independent risk factor of ICU mortality. Clin Nutr. 2003;22:23–30. doi: 10.1054/clnu.2002.0613. [DOI] [PubMed] [Google Scholar]
- 23.Siroen MP, Warlé MC, Teerlink T, Nijveldt RJ, Kuipers EJ, Metselaar HJ, Tilanus HW, Kuik DJ, van der Sijp JR, Meijer S, et al. The transplanted liver graft is capable of clearing asymmetric dimethylarginine. Liver Transpl. 2004;10:1524–1530. doi: 10.1002/lt.20286. [DOI] [PubMed] [Google Scholar]
- 24.Martín-Sanz P, Olmedilla L, Dulin E, Casado M, Callejas NA, Pérez-Peña J, Garutti I, Sanz J, Calleja J, Barrigón S, et al. Presence of methylated arginine derivatives in orthotopic human liver transplantation: relevance for liver function. Liver Transpl. 2003;9:40–48. doi: 10.1053/jlts.2003.50008. [DOI] [PubMed] [Google Scholar]
- 25.Brenner T, Fleming TH, Rosenhagen C, Krauser U, Mieth M, Bruckner T, Martin E, Nawroth PP, Weigand MA, Bierhaus A, et al. L-arginine and asymmetric dimethylarginine are early predictors for survival in septic patients with acute liver failure. Mediators Inflamm. 2012;2012:210454. doi: 10.1155/2012/210454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trocha M, Merwid-Ląd A, Chlebda-Sieragowska E, Szuba A, Pieśniewska M, Fereniec-Gołębiewska L, Kwiatkowska J, Szeląg A, Sozański T. Age-related changes in ADMA-DDAH-NO pathway in rat liver subjected to partial ischemia followed by global reperfusion. Exp Gerontol. 2014;50:45–51. doi: 10.1016/j.exger.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 27.Lanteri R, Acquaviva R, Di Giacomo C, Sorrenti V, Li Destri G, Santangelo M, Vanella L, Di Cataldo A. Rutin in rat liver ischemia/reperfusion injury: effect on DDAH/NOS pathway. Microsurgery. 2007;27:245–251. doi: 10.1002/micr.20345. [DOI] [PubMed] [Google Scholar]
- 28.Davids M, Richir MC, Visser M, Ellger B, van den Berghe G, van Leeuwen PA, Teerlink T. Role of dimethylarginine dimethylaminohydrolase activity in regulation of tissue and plasma concentrations of asymmetric dimethylarginine in an animal model of prolonged critical illness. Metabolism. 2012;61:482–490. doi: 10.1016/j.metabol.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 29.Chang KA, Lin IC, Sheen JM, Chen YC, Chen CC, Tain YL, Hsieh CS, Huang LT. Sex differences of oxidative stress to cholestatic liver and kidney injury in young rats. Pediatr Neonatol. 2013;54:95–101. doi: 10.1016/j.pedneo.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 30.Yang YY, Lee TY, Huang YT, Chan CC, Yeh YC, Lee FY, Lee SD, Lin HC. Asymmetric dimethylarginine (ADMA) determines the improvement of hepatic endothelial dysfunction by vitamin E in cirrhotic rats. Liver Int. 2012;32:48–57. doi: 10.1111/j.1478-3231.2011.02651.x. [DOI] [PubMed] [Google Scholar]
- 31.Ferrigno A, Palladini G, Bianchi A, Rizzo V, Di Pasqua LG, Perlini S, Richelmi P, Vairetti M. Lobe-specific heterogeneity in asymmetric dimethylarginine and matrix metalloproteinase levels in a rat model of obstructive cholestasis. Biomed Res Int. 2014;2014:327537. doi: 10.1155/2014/327537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Böger RH, Bode-Böger SM, Sydow K, Heistad DD, Lentz SR. Plasma concentration of asymmetric dimethylarginine, an endogenous inhibitor of nitric oxide synthase, is elevated in monkeys with hyperhomocyst(e)inemia or hypercholesterolemia. Arterioscler Thromb Vasc Biol. 2000;20:1557–1564. doi: 10.1161/01.atv.20.6.1557. [DOI] [PubMed] [Google Scholar]
- 33.Böger RH, Bode-Böger SM, Szuba A, Tsao PS, Chan JR, Tangphao O, Blaschke TF, Cooke JP. Asymmetric dimethylarginine (ADMA): a novel risk factor for endothelial dysfunction: its role in hypercholesterolemia. Circulation. 1998;98:1842–1847. doi: 10.1161/01.cir.98.18.1842. [DOI] [PubMed] [Google Scholar]
- 34.Baue AE, Durham R, Faist E. Systemic inflammatory response syndrome (SIRS), multiple organ dysfunction syndrome (MODS), multiple organ failure (MOF): are we winning the battle? Shock. 1998;10:79–89. doi: 10.1097/00024382-199808000-00001. [DOI] [PubMed] [Google Scholar]
- 35.López A, Lorente JA, Steingrub J, Bakker J, McLuckie A, Willatts S, Brockway M, Anzueto A, Holzapfel L, Breen D, et al. Multiple-center, randomized, placebo-controlled, double-blind study of the nitric oxide synthase inhibitor 546C88: effect on survival in patients with septic shock. Crit Care Med. 2004;32:21–30. doi: 10.1097/01.CCM.0000105581.01815.C6. [DOI] [PubMed] [Google Scholar]
- 36.Nathan CF, Hibbs JB. Role of nitric oxide synthesis in macrophage antimicrobial activity. Curr Opin Immunol. 1991;3:65–70. doi: 10.1016/0952-7915(91)90079-g. [DOI] [PubMed] [Google Scholar]
- 37.Förstermann U, Sessa WC. Nitric oxide synthases: regulation and function. Eur Heart J. 2012;33:829–837, 837a-837d. doi: 10.1093/eurheartj/ehr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moncada S, Higgs A. The L-arginine-nitric oxide pathway. N Engl J Med. 1993;329:2002–2012. doi: 10.1056/NEJM199312303292706. [DOI] [PubMed] [Google Scholar]
- 39.Huang PL, Huang Z, Mashimo H, Bloch KD, Moskowitz MA, Bevan JA, Fishman MC. Hypertension in mice lacking the gene for endothelial nitric oxide synthase. Nature. 1995;377:239–242. doi: 10.1038/377239a0. [DOI] [PubMed] [Google Scholar]
- 40.Avontuur JA, Bruining HA, Ince C. Inhibition of nitric oxide synthesis causes myocardial ischemia in endotoxemic rats. Circ Res. 1995;76:418–425. doi: 10.1161/01.res.76.3.418. [DOI] [PubMed] [Google Scholar]
- 41.Visser M, Paulus WJ, Vermeulen MA, Richir MC, Davids M, Wisselink W, de Mol BA, van Leeuwen PA. The role of asymmetric dimethylarginine and arginine in the failing heart and its vasculature. Eur J Heart Fail. 2010;12:1274–1281. doi: 10.1093/eurjhf/hfq158. [DOI] [PubMed] [Google Scholar]
- 42.Böger RH. Live and let die: asymmetric dimethylarginine and septic shock. Crit Care. 2006;10:169. doi: 10.1186/cc5076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leiper J, Murray-Rust J, McDonald N, Vallance P. S-nitrosylation of dimethylarginine dimethylaminohydrolase regulates enzyme activity: further interactions between nitric oxide synthase and dimethylarginine dimethylaminohydrolase. Proc Natl Acad Sci USA. 2002;99:13527–13532. doi: 10.1073/pnas.212269799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harbrecht BG, Doyle HR, Clancy KD, Townsend RN, Billiar TR, Peitzman AB. The impact of liver dysfunction on outcome in patients with multiple injuries. Am Surg. 2001;67:122–126. [PubMed] [Google Scholar]
- 45.Brinkmann SJ, de Boer MC, Buijs N, van Leeuwen PA. Asymmetric dimethylarginine and critical illness. Curr Opin Clin Nutr Metab Care. 2014;17:90–97. doi: 10.1097/MCO.0000000000000020. [DOI] [PubMed] [Google Scholar]
- 46.Nijveldt RJ, Teerlink T, Siroen MP, van der Hoven B, Prins HA, Wiezer MJ, Meijer C, van der Sijp JR, Cuesta MA, Meijer S, et al. Elevation of asymmetric dimethylarginine (ADMA) in patients developing hepatic failure after major hepatectomy. JPEN J Parenter Enteral Nutr. 2004;28:382–387. doi: 10.1177/0148607104028006382. [DOI] [PubMed] [Google Scholar]
- 47.O’Dwyer MJ, Dempsey F, Crowley V, Kelleher DP, McManus R, Ryan T. Septic shock is correlated with asymmetrical dimethyl arginine levels, which may be influenced by a polymorphism in the dimethylarginine dimethylaminohydrolase II gene: a prospective observational study. Crit Care. 2006;10:R139. doi: 10.1186/cc5053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sheen JM, Chen YC, Tain YL, Huang LT. Increased circulatory asymmetric dimethylarginine and multiple organ failure: bile duct ligation in rat as a model. Int J Mol Sci. 2014;15:3989–4006. doi: 10.3390/ijms15033989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang DL, Liu J, Liu S, Zhang Y, Liu WH. The differences of asymmetric dimethylarginine removal by different dialysis treatments. Ren Fail. 2010;32:935–940. doi: 10.3109/0886022X.2010.502281. [DOI] [PubMed] [Google Scholar]
- 50.Abedini S, Meinitzer A, Holme I, März W, Weihrauch G, Fellstrøm B, Jardine A, Holdaas H. Asymmetrical dimethylarginine is associated with renal and cardiovascular outcomes and all-cause mortality in renal transplant recipients. Kidney Int. 2010;77:44–50. doi: 10.1038/ki.2009.382. [DOI] [PubMed] [Google Scholar]
- 51.Rooyackers O, Kouchek-Zadeh R, Tjäder I, Norberg Å, Klaude M, Wernerman J. Whole body protein turnover in critically ill patients with multiple organ failure. Clin Nutr. 2015;34:95–100. doi: 10.1016/j.clnu.2014.01.020. [DOI] [PubMed] [Google Scholar]


