Abstract
AIM: To compare closure methods, closure times and medical costs between two groups of patients who had post-endoscopic resection (ER) artificial ulcer floor closures.
METHODS: Nineteen patients with duodenal adenoma, early duodenal cancer, and subepithelial tumors that received ER between September 2009 and September 2014 at Kagawa University Hospital and Ehime Rosai Hospital, an affiliated hospital of Kagawa University, were included in the study. We retrospectively compared two groups of patients who received post-ER artificial ulcer floor closure: the conventional clip group vs the over-the-scope clip (OTSC) group. Delayed bleeding, procedure time of closure, delayed perforation, total number of conventional clips and OTSCs and medical costs were analyzed.
RESULTS: Although we observed delayed bleeding in three patients in the conventional clip group, we observed no delayed bleeding in the OTSC group (P = 0.049). We did not observe perforation in either group. The mean procedure times for ulcer closure were 33.26 ± 12.57 min and 9.71 ± 2.92 min, respectively (P = 0.0001). The resection diameters were 18.8 ± 1.30 mm and 22.9 ± 1.21 mm for the conventional clip group and the OTSC group, respectively, with significant difference (P = 0.039). As for medical costs, the costs of all conventional clips were USD $1257 and the costs of OTSCs were $7850 (P = 0.005). If the post-ER ulcer is under 20 mm in diameter, a conventional clip closure may be more suitable with regard to the prevention of delayed perforation and to medical costs.
CONCLUSION: If the post-ER ulcer is over 20 mm, the OTSC closure should be selected with regard to safety and reliable closure even if there are high medical costs.
Keywords: Closure time, Endoscopic resection, Over-the-scope clip, Pancreatic juice, Bile acid
Core tip: Duodenal postoperative exposure of the artificial ulcer floor to pancreatic juice and bile acid induces delayed perforation. There are, however, no reports on comparisons of closure methods, closure times and medical costs according to the different methods for closure of artificial ulcer floors. If the post-endoscopic resection (ER) ulcer is under 20 mm in diameter, the conventional clip closure might be more suitable with regard to the prevention of delayed perforation and to medical costs. If the post-ER ulcer is over 20 mm, the over-the-scope clip closure should be selected with regard to safety and reliable closure even if there are high medical costs.
INTRODUCTION
Primary duodenal adenoma and cancer reportedly account for approximately 0.02%-0.04%[1] and 0.035%-0.12%[2,3] of all gastrointestinal neoplastic lesions, respectively, whereas the frequency of duodenal neuroendocrine tumors (e.g., carcinoid tumors) has been reported to be 0.5%[4-6]. In recent years, esophageal, gastric, and colorectal endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) have been gradually developed and are sometimes performed for duodenal tumors. Early duodenal cancers remaining inside of the mucosa with no lymph node metastasis are an indication for endoscopic resection (ER)[7]. However, because the duodenum is fixed on the retroperitoneum with two bending portions (the superior and lower duodenal angles), in many cases, it is difficult to secure the visual field for conducting endoscopy, to manipulate the endoscope, and to appropriately set the distance and angle of the knife with flexible endoscopes. In addition, it is difficult to obtain a mucosal bulge by local injection due to the presence of Brunner glands and a thin muscular layer. This procedure is associated with many operation-related complications, such as perforation. Because postoperative exposure of the artificial ulcer floor to pancreatic juice and bile acid induces delayed perforation, various closure methods for the ulcer floor have been reported[8]. However, there are currently no reports on comparisons of closure methods, closure times and medical costs according to different methods for closure of artificial ulcer floors after EMR or ESD. There have been many reports with regard to the usefulness of the over-the-scope clip (OTSC) system (Ovesco Endoscopy GmbH, Tüebingen, Germany) for perforation, bleeding and fistulas of the digestive tract. Thus, we compared the differences of two methods to close artificial ulcer floors using a conventional clip or OTSC after ER for duodenal tumors to prevent post-ER artificial ulcers from exposure to pancreatic juice and bile acid, which leads to delayed perforation.
MATERIALS AND METHODS
Patients characteristics
Nineteen patients with duodenal adenoma, early duodenal cancer, and subepithelial tumors that received ER between September 2009 and September 2014 at Kagawa University Hospital and Ehime Rosai Hospital, an affiliated hospital of Kagawa University, were included in the study. The microvascular and surface patterns were examined preoperatively in all cases by magnifying narrow band imaging (NBI) using the highest magnification (approximately optical magnification × 80) for preoperative endoscopic diagnosis. In addition, a biopsy was conducted for histological diagnosis. The inclusion criteria were early duodenal cancer, adenomas with a diameter of < 20 mm or neuroendocrine tumors with a diameter of < 10 mm, and a World Health Organization (WHO) classification of up to Grade 1. The exclusion criterion was patients with suspected massive submucosal invasion detected by magnifying NBI and endosonography (EUS), in whom surgical resection was performed instead. These criteria are also recommended by the Japan Gastroenterological Society.
ER, especially ESD, was performed carefully to prevent perforation. Moreover, markings were made at the site close to the tumors after evaluating the periphery of the tumors in detail by magnifying NBI using a GIF TYPE H260Z (OLYMPUS Co., Tokyo, Japan) to minimize the postoperative ulcer floor as much as possible. Local injection with a liquid that was composed of > 50% concentrated hyaluronic acid was administered in all cases. When local injection resulted in an insufficient bulge, concentrated hyaluronic acid was used without dilution. A shallow incision was first made in the mucosa on the distal side, and the mucosa was subsequently detached from the proximal side after trimming the submucosa when possible. Because the duodenal muscular layer is very thin, the insufflation volume was adjusted so that the knife tip was parallel to the muscular layer when possible, and the electrification duration was shortened as much as possible. In addition, excessive countertraction on the muscular layer by the tip hood was avoided.
Because artificial ulcers after ER are exposed to pancreatic juice and bile acid, conventional clip closure, with or without a detainment snare, or closure with an OTSC was used for the post-ER artificial ulcer closure. Either conventional clipping or the OTSC system was selected as the closing method at the discretion of each operator (i.e., three endoscopists, each having treated > 100 cases of gastric ESD).
We retrospectively compared two groups of patients who received post-ER artificial ulcer floor closure: the conventional clip group vs the OTSC group. Delayed bleeding, procedure time of closure, delayed perforation, total number of conventional clips and OTSCs and medical costs were analyzed.
Operative devices
GIF TYPE Q260J and GIF TYPE H260Z (OLYMPUS. Co., Tokyo, Japan) endoscopes were used. A dual knife (KD-650L, OLYMPUS. Co., Tokyo, Japan) or IT knife 2 (KD-611L, OLYMPUS. Co., Tokyo, Japan) was used. A coagrasper (FD-410LR, OLYMPUS. Co., Tokyo, Japan) hemostatic forceps was used. The tip attachment employed was an Elastic Touch Attachment (TOP. Co., Tokyo, Japan). An ERBE VIO300D incisional device was used, and a UCR (OLYMPUS. Co., Tokyo, Japan) was used as the CO2 insufflation device.
Statistical analysis
All values are presented as the mean ± SD. Patient baselines statistics were analyzed using a Mann-Whitney U test. P values < 0.05 were considered statistically significant. All statistical analyses were performed using GraphPad Prism version 5 for Windows (Graph Pad Software, San Diego, CA, United States).
RESULTS
The mean age of the patients (13 men and 6 women) was 62.5 years. Table 1 shows the characteristics of the patients in both groups (i.e., conventional clip group vs OTSC group). The lesion sites were in the second portion and bulb in 10 cases and 2 cases in the conventional clip group, respectively and in 5 cases and 2 cases in the OTSC group, respectively. There were 8 cases and 4 cases in the conventional clip group that received EMR or ESD, respectively, and 4 cases and 3 cases in the OTSC group received EMR of ESD, respectively. There were no significant differences in baseline characteristic for both groups.
Table 1.
Characteristics of the patients
| Conventional clip group, n | Over-the-scope clip group, n | P value1 | |
| Patients | 12 | 7 | |
| Age (yr), mean ± SD | 62.5 ± 15.8 | 64.3 ± 13.7 | 0.20 |
| Sex, M/F | 8/4 | 5/2 | 0.42 |
| Location of lesions | |||
| 2nd portion | 10 | 5 | 0.31 |
| Bulb | 2 | 2 | 0.40 |
| Resection method (mean ± SD, min) | |||
| EMR | 8 (15.7 ± 3.68) | 4 (14.6 ± 4.57) | 0.52 (0.68) |
| ESD | 4 (45.7 ± 12.51) | 3 (55.7 ± 16.35) | 0.43 (0.43) |
Mann-Whitney U test. EMR: Endoscopic mucosal resection; ESD: Endoscopic submucosal dissection.
Table 2 shows the results for the two groups. The lesion diameters obtained by pathologic examination were 12.5 ± 1.60 mm for the conventional clip group and 13.3 ± 1.74 mm for the OTSC group, with no significant difference (P = 0.14). The resection diameters were 18.8 ± 1.30 mm and 22.9 ± 1.21 mm for the conventional clip group and the OTSC group, respectively, with significant difference (P = 0.039).
Table 2.
Results for the two groups
| Conventional clip (n = 12) | Over-the-scope clip (n = 7) | P value1 | |
| Lesion diameter (mm), mean ± SD | 12.5 ± 1.60 | 13.3 ± 1.74 | 0.140 |
| Resection diameter (mm), mean ± SD | 18.8 ± 1.30 | 22.9 ± 1.21 | 0.039 |
| Delayed bleeding (POD 1-7) | 3 | 0 | 0.049 |
| Treatment measure for delayed bleeding | hemostatic forceps | - | - |
| Delayed perforation (POD 1-7) | 0 | 0 | - |
| Procedure time of ulcer closure (min), mean ± SD | 33.26 ± 12.57 | 9.71 ± 2.92 | 0.0001 |
| Clips, mean | 9.8 | 1.25 | 0.015 |
| Total clips | 121 | 10 | 0.002 |
| Cost of one clip (¥/$/€)2 | 975/9.56/7.01 | 80000/785/576 | 0.008 |
| Cost of all clips (¥/$/€)2 | 117975/1257/847 | 800000/7850/5760 | 0.005 |
| Pathological diagnosis | |||
| Adenoma | 7 | 4 | 0.410 |
| Tubular adenocarcinoma | 4 | 2 | 0.390 |
| Leiomyoma | 1 | 0 | 0.810 |
| Carcinoid | 0 | 1 | 0.810 |
Mann-Whitney U test;
Average exchange rate at September, 2014.
Although we observed delayed bleeding until day 7 after ER in 3 patients in the conventional clip group, we observed no delayed bleeding in the OTSC group (P = 0.049). We controlled the bleeding using hemostatic forceps, and we observed no subsequent bleeding. We did not observe perforation in either group. The mean procedure time for ulcer closure was 33.26 ± 12.57 min in the conventional clip group and 9.71 ± 2.92 min in the OTSC group, which showed a significant difference (P = 0.0001; Table 2).
As for medical costs, one clip costs ¥975, USD $9.56, or €7.01, and complete closure of an artificial ulcer required an average of 9.8 clips in the conventional clip group; one OTSC costs ¥80000, $US 785, or €576, and complete closure of an artificial ulcer required an average of 1.25 OTSCs in the OTSC group (P = 0.008; Table 2). The total of 121 conventional clips were used in the conventional clip group, and 10 OTSCs were used in the OTSC group. Therefore, the costs of all conventional clips were ¥117975, $1257, and €847, and the costs of all OTSCs were ¥800000, $7850, €5760, resulting a significant difference (P = 0.005; Table 2). In the histopathological examinations, we observed no significant differences between the groups in the proportions of adenoma, tubular adenocarcinomas, leiomyoma and carcinoids.
Figure 1 shows representative white light magnified endoscopic images with an irregular microsurface pattern (Figure 1A), and magnifying NBI images with an irregular microvascular pattern (Figure 1B), and an ulcer floor closure with a detainment snare and conventional clips (Figure 1C).
Figure 1.
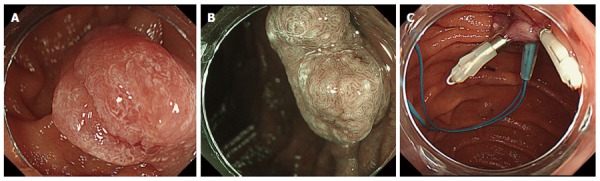
White light endoscopic image, magnifying narrow band image, closure method of Case 2 (conventional clip). A: White light magnified endoscopic images with an irregular microsurface pattern in the second portion; B: Magnifying narrow band imaging images with an irregular microvascular pattern indicated focal cancer; C: Ulcer floor closure with a detainment snare and conventional clips.
Figures 2 and 3 show representative white light endoscopic images (Figures 2A and 3A), magnifying NBI images (Figure 2B), resection by EMR (Figure 2C), resection by ESD (Figure 3B), and post-ER artificial ulcer closure by OTSC (Figures 2D, E and 3C). The OTSC was not visible on the ulcer floor, which had recovered within the mucosa with chorioepithelium 6 mo later without stricture (Figure 2F).
Figure 2.
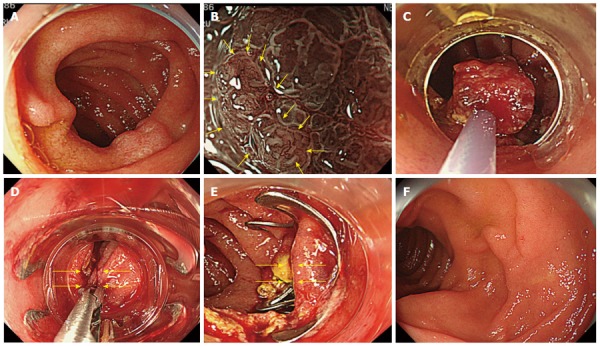
White light endoscopic image, magnifying narrow band image, resection method, closure method of case 6 (over-the-scope clip). A: An approximately 13-mm depressed lesion is observed in the posterior wall side of the slightly anal side of the major duodenal papilla in the descending portion of the duodenum; B: The magnifying narrow band image shows a clear boundary between the tumor and normal mucosa, and a mildly irregular surface structure of the tumor. The microvascular pattern (yellow arrows) shows expansion, winding, and caliber variation, which we evaluated as an inflammatory change caused by pancreatic juice and bile acid rather than malignant findings; C: After circumferential resection, en bloc resection was conducted by hybrid endoscopic submucosal dissection using a snare resection when two-thirds of the submucosal trimming was finished; D: As the artificial ulcer floor occupied half of the circumference and was close to the major duodenal papilla, closure in the minor axial direction toward the intestinal tract was attempted by grasping the mucosa in the anal and mouth sides with a twin Grasper® (yellow arrows); E: Complete suture closure was performed in the minor axial direction using an over-the-scope clip (OTSC) (yellow arrows); F: The OTSC was not visible on the ulcer floor, which had recovered within the mucosa with chorioepithelium 6 mo later.
Figure 3.
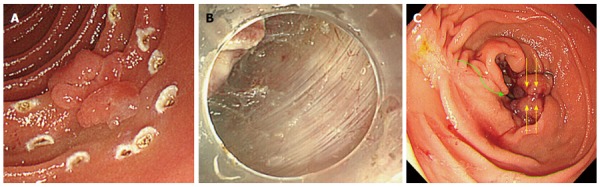
White right endoscopic image, muscular layer surface and longitudinal closure method of the artificial ulcer after resection in case 13 (over-the-scope clip). A: An approximately 20-mm irregularly protruding lesion is observed in the posterior wall side of the slightly anal side of the major duodenal papilla in the descending portion of the duodenum. Duodenal cancer was diagnosed based on the magnifying narrow band imaging results; B: The detached thin myenteric parts could be observed by applying only mild countertraction using the tip hood; C: The largest artificial ulcer floor is approximately 30 mm, occupying half of the circumference of the duodenal lumen. Bile juice directly flowed onto the artificial ulcer floor from the major duodenal papilla (green curved arrow). Reefing closure using an over-the-scope clip (OTSC) was conducted as rapidly as possible while cleaning the ulcer floor. Because closure using the OTSC in the minor axial direction was technically difficult, longitudinal reefing was used; however, no postoperative stenosis was observed (yellow arrows).
DISCUSSION
Improvement in the ESD technique and the development of safe devices have allowed conventional resections by EMR and en bloc resections by ESD of duodenal neoplastic lesions. However, intraoperative perforation has been reported to occur with very high frequency compared with that in esophageal, gastric, and colorectal ESDs, indicating a high degree of difficulty in duodenal ESD[9-11]. Moreover, the incidence of delayed perforation has been reported to be as high as 6%-7%. For the prevention of delayed perforation, it is necessary to close and reef the ulcer floor because artificial ulcer floors are exposed to digestive juices, such as pancreatic juice and bile acid, after resection[12]. The placement of endoscopic nasobiliary drainage (ENBD) and endoscopic nasopancreatic drainage (ENPD) and the administration of pancreatic enzyme inhibitors have been reported to be effective[13]. However, it is difficult to postoperatively insert ENBD or ENPD in every case due to the high risk of detachment of the thin myenteric parts because of overstressing the artificial ulcer floor after ESD. In addition, insertion before ESD is also likely to be difficult because of the drainage tube, which acts as an additional obstacle to endoscopic manipulation during ESD.
In a report by Ono et al at the Conference of Japan Gastroenterological Endosocpy Society on a multicenter questionnaire survey conducted in 13 facilities in Japan, the intraoperative and delayed perforation rates were 9.3% and 3.1%, respectively, resulting in a 12% total perforation rate. Intraoperative perforation occurred in 3.9% and 24% of EMR and ESD cases, respectively, whereas delayed perforation occurred in 1.2% and 6% of EMR and ESD cases, respectively.
In terms of delayed bleeding and procedure times, the conventional clip closure was significantly inferior to the OTSC closure. With close follow-up observation, delayed bleeding is certainly controllable with a hemostatic forceps, and the procedure time of the conventional clip is within a tolerable time. Therefore, both methods are suitable for post-ER prophylactic treatment.
With regard to delayed perforation, because the conventional clip closure and the OTSC closure showed no significant difference, both methods are suitable for post-ER closure. When closing 20-mm or larger artificial ulcer floors with normal clips and a detainment snare, a gap is generated between the clips, leading to exposure to digestive juices. The OTSC system is considered very effective and safe for the closure of artificial ulcer floors because single reefing strongly closes the floor in the system. However, there is a notable disadvantage with the OTSC closure. The costs of all OTSCs were 6- to 7-times more expensive than that of conventional clips. In terms of medical costs, this difference cannot be ignored.
In conclusion, if the post-ER ulcer is under 20 mm in diameter, the conventional clip closure might be more suitable with regard to the prevention of delayed perforation and to medical costs. However, if the post-ER ulcer is over 20 mm in diameter, the OTSC closure should be selected with regard to safety and reliable closure even if there are high medical costs.
ACKNOWLEDGMENTS
We would like to thank Dr. Makoto Oryu for technical and editorial assistance.
COMMENTS
Background
Duodenal postoperative exposure of the artificial ulcer floor to pancreatic juice and bile acid induces delayed perforation. Because the indication for endoscopic resection (ER) for duodenal tumors has been controversial, in recent years, ER has been performed gradually. As postoperative exposure of the artificial ulcer floor to pancreatic juice and bile acid induces delayed perforation, there are currently no reports on comparisons of closure methods, closure times and medical costs.
Research frontiers
There are no reports on comparisons of closure methods, closure times and medical costs according to the different methods for closure of artificial ulcer floors of post-Endoscopic resection.
Innovations and breakthroughs
There have been many reports with regard to the usefulness of the over-the-scope clip (OTSC) system for perforation, bleeding and fistulas of the digestive tract. Thus, the authors compared the differences of two methods to close artificial ulcer floors using a conventional clip or OTSC after ER for duodenal tumors to prevent post-ER artificial ulcers from exposure to pancreatic juice and bile acid, which leads to delayed perforation.
Applications
If the post-ER ulcer is over 20 mm, the OTSC closure should be selected with regard to safety and reliable closure even if there are high medical costs.
Terminology
The over-the-scope clip system is used for perforation, bleeding and fistulas of the digestive tract.
Peer-review
This report compares the closure methods, i.e., conventional clip vs OTSC, following ER for duodenal tumors. Based on the results obtained with 19 patients, the authors concluded that if post-ER ulcer is under 20 mm diameter, a conventional closure may be more suitable. However, with ulcer > 20 mm, the OTSC closure should be selected. The manuscript is informative, well written, and supported by the tables and pictures. Hence, in my opinion, it deserves priority publishing.
Footnotes
Ethics approval: The study was reviewed and approved by the Ethics Committee of Ehime Rosai Hospital, No. 40.
Informed consent: All study participants, or their legal guardian, provided informed written consent prior to study enrolment.
Conflict-of-interest: The authors declare no conflicts of interest, and no corporate financing was received.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: October 18, 2014
First decision: November 14, 2014
Article in press: March 19, 2015
P- Reviewer: Slomiany BL S- Editor: Yu J L- Editor: A E- Editor: Ma S
References
- 1.Morrison WA, Donath D. Tumors of the Small Intestine. Cal West Med. 1941;55:235–237. [PMC free article] [PubMed] [Google Scholar]
- 2.Burgerman A, Baggenstoss AH, Cain JC. [Primary malignant neoplasms of the duodenum, exclusing the papilla of vater; a clinicopathologic study of 31 cases] Gastroenterology. 1956;30:421–431. [PubMed] [Google Scholar]
- 3.Hung FC, Kuo CM, Chuah SK, Kuo CH, Chen YS, Lu SN, Chang Chien CS. Clinical analysis of primary duodenal adenocarcinoma: an 11-year experience. J Gastroenterol Hepatol. 2007;22:724–728. doi: 10.1111/j.1440-1746.2007.04935.x. [DOI] [PubMed] [Google Scholar]
- 4.Mullen JT, Wang H, Yao JC, Lee JH, Perrier ND, Pisters PW, Lee JE, Evans DB. Carcinoid tumors of the duodenum. Surgery. 2005;138:971–97; discussion 977-978. doi: 10.1016/j.surg.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 5.Soga J. Carcinoids and their variant endocrinomas. An analysis of 11842 reported cases. J Exp Clin Cancer Res. 2003;22:517–530. [PubMed] [Google Scholar]
- 6.Modlin IM, Kidd M, Latich I, Zikusoka MN, Shapiro MD. Current status of gastrointestinal carcinoids. Gastroenterology. 2005;128:1717–1751. doi: 10.1053/j.gastro.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 7.Alexander S, Bourke MJ, Williams SJ, Bailey A, Co J. EMR of large, sessile, sporadic nonampullary duodenal adenomas: technical aspects and long-term outcome (with videos) Gastrointest Endosc. 2009;69:66–73. doi: 10.1016/j.gie.2008.04.061. [DOI] [PubMed] [Google Scholar]
- 8.Mori H, Shintaro F, Kobara H, Nishiyama N, Rafiq K, Kobayashi M, Nakatsu T, Miichi N, Suzuki Y, Masaki T. Successful closing of duodenal ulcer after endoscopic submucosal dissection with over-the-scope clip to prevent delayed perforation. Dig Endosc. 2013;25:459–461. doi: 10.1111/j.1443-1661.2012.01363.x. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto H, Miura Y. Duodenal ESD: conquering difficulties. Gastrointest Endosc Clin N Am. 2014;24:235–244. doi: 10.1016/j.giec.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 10.Inoue T, Uedo N, Yamashina T, Yamamoto S, Hanaoka N, Takeuchi Y, Higashino K, Ishihara R, Iishi H, Tatsuta M, et al. Delayed perforation: a hazardous complication of endoscopic resection for non-ampullary duodenal neoplasm. Dig Endosc. 2014;26:220–227. doi: 10.1111/den.12104. [DOI] [PubMed] [Google Scholar]
- 11.Jung JH, Choi KD, Ahn JY, Lee JH, Jung HY, Choi KS, Lee GH, Song HJ, Kim DH, Kim MY, et al. Endoscopic submucosal dissection for sessile, nonampullary duodenal adenomas. Endoscopy. 2013;45:133–135. doi: 10.1055/s-0032-1326178. [DOI] [PubMed] [Google Scholar]
- 12.Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, Oryu M, Masaki T. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19:2752–2760. doi: 10.3748/wjg.v19.i18.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fedorov ED, Plakhov RV, Mikhaleva LM, Ivanova EV, Galkova ZV, Buntseva OA. [The results of endoscopic mucosal resection and submucosal layer endoscopic dissection in patients with superficial epithelial neoplasms of stomach and duodenum] Eksp Klin Gastroenterol. 2011;(10):65–72. [PubMed] [Google Scholar]


