Abstract
Background
Measles is a highly contagious viral disease that remains an important cause of mortality among children despite the availability of a safe and effective vaccine around the world. We aimed this study to show a measles out-break occurring.
Methods
In early 2012, a report of measles outbreak was recorded on center for disease control (CDC) of Fars province, south of Iran. With this case-series study, characteristics of cases and network transition model were described.
Results
The primary case was an Afghan refugee who is likely to carry the measles virus from its country or from anywhere in Iran to Koordeh, a small village in south of Iran. Followed by the Afghan case, 6 secondary and tertiary cases including rural health worker, were occurred. Except a case of 35 year old, in which her vaccination status was unknown, all cases has had adherence to vaccination protocol.
Conclusion
More immunologic and vaccine quality investigations are needed to find the main cause of the outbreak. Nonetheless, due to the warm weather, probable bad temperature management of cold chain and technical problem in vaccination are the main suspicious reasons of the outbreak.
Keywords: Measles, Outbreak, Vaccination, Iran
Introduction
Measles is a highly contagious disease and with basic reproductive rate of 12 to 18 has more infectiousness potency than mumps, polio and even rubella. In 2008 and 2011 in worldwide, 164,000 and 118,000 people have respectively died of measles. This disease is responsible for 8% of all deaths from vaccine-preventable diseases in the world (1,2). Measles is the most lethal vaccine-preventable disease in children and it is the eighth leading cause of death in all age groups. (3) To eliminate measles, it is necessary that 95% of population to be immunized. (4) Therefore, the World Health Organization (WHO) has recommended global efforts for the reduction of measles, focusing on vaccination against measles (2).
Injection of a single dose of vaccine in around nine months to one year of age, when maternal immunity disappears, bring about 95 to 98% immunity against measles. But in some conditions in which vaccination technique is not appropriate or vaccine quality is low (5,6) and more importantly, to increase the vaccine coverage it is recommended to inject second vaccine (7). Measles vaccination program in the past four decades could fall more than 75% of measles cases and its deaths. Therefore, measles elimination program was considered to eliminate measles in America in 2000, in Europe in 2007 and in the Middle East in 2010 (8). Elimination means to be interrupted the transmission measles virus in a population of a geographic area. The ultimate goal is to eradicate the virus in worldwide over the next decades (9). Measles vaccination in combination with rubella and mumps were conducted at 12 and 18 months of life. Measles vaccination coverage in the past two decades in Iran has been become much higher than Middle East and it has improved from 72% in 1984 and 78% in 1987 to around 99% in 2011(10). Vaccination against measles was launched in 1983 and 2-doseschedule in 1985. Mass campaign vaccination of measles and rubella (MR) was done in 2003 (11). The WHO estimated that in lack of vaccination, 4.5 million people die from measles annually (12). Two-dose vaccination program has led the U.S. in 2000 very close to disease elimination. So, 90% of the 222 cases in 2012 in U.S. have been imported from other countries (13). In spite of success of having an effective vaccine, unfortunately in areas such as Africa due to poor control of the disease, case of measles has risen from 37,000 in 2008 to 172,000 in 2011(14). Even in some developed countries national statistics show an increase in cases of measles. For example, in France in 2011, numbers of 15,000 cases of measles and 1 death have been reported (13). Despite the implementation of the vaccination program, even with two doses of vaccine in 2003, new cases of measles still occur, for example, in 2012 a total of 171 confirmed cases of measles have been diagnosed (15). Despite high vaccination coverage in many areas, but sporadic cases of measles and even outbreaks occur. Several reasons express such outbreaks. First, staffs make and report factitious data on vaccines coverage. Second, the overall coverage is high, but in some places, like a small village, a part of a town or a kindergarten vaccine has not applied. In this case in which numbers of sensitive people are high and herd immunity does not work. Third, a defect impaired cold chain. A vaccine at temperature of 41°C for 2 to 3 days loses half and at 54°C for 1 day loses 80% of potency. Temperature 37◦C almost loses all throughput immunogenicity itself-causing. However, even with the stabilizers, the vaccine rapidly loses potency at temperatures above the recommended 2–8◦C (16,17). Forth, if subcutaneous or intramuscular injection of the vaccine be administered incorrectly by untrained personnel or be injected with non-standard needle and syringe could decline vaccine efficacy. Fifth, both maternal antibodies and immaturity of immune system of neonate can lower vaccine immunity (18-20). In some cases, antibodies transferred from mother are too low or weak that could multiply risk of measles infection in pre-vaccination period (21).
According to recent measles outbreak in Fars province, south of Iran, this report helps us to answer this question that “how the outbreak has occurred though vaccination coverage among a population was high?” This report aimed to describe mentioned outbreak and we also show that infection how to enter and how to disseminate.
Materials & Methods
Recent measles outbreak occurred in the spring of 2012 in Koordeh, a district in south of Fars province with an area of nearly 500 square kilometers and a population of 1800. The trend of annual number of measles case and vaccination coverage in Koordeh is showed in Fig.1. So, according to world health organization (WHO) definition, criteria of a measles outbreak are satisfied (22,23). In this case-series study, after case detection and confirmation, we gathered all documents of 7 measles cases in this outbreak. Data were derived from any medical recording in health center, physician's notes, laboratory results, hospital files, and also by patient history. To be confirmed suspected and probable cases, blood samples were taken and sent to the reference laboratory. Presence of measles-specific IgM antibodies calls for definite measles diagnosis (22). Data that collected in this report were demographic, date (s) of rash appearance, case finding and lab result, and vaccination history.
Fig. 1.
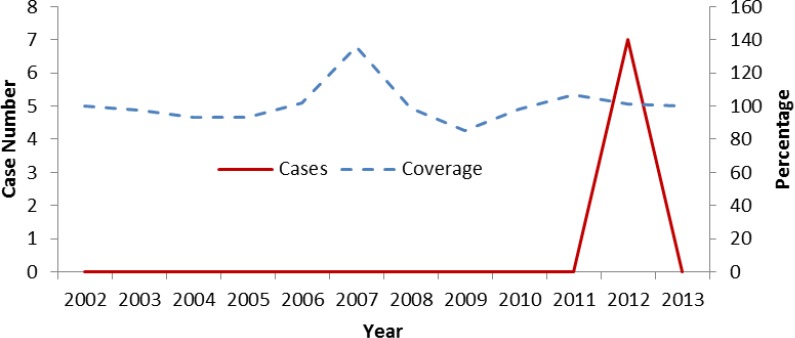
Trend of measles cases and vaccine coverage in South of Iran, 2002-13
Results
In this outbreak total of 7 confirmed measles cases were diagnosed, Table 1. Primary case (case 1) was a16 year's old Afghani refugee (imported case) that referred to the health center with flu-like symptoms and Coryza on May 11th, 2012. With diagnosis of a common cold, the patient was discharged with anti-fever and anti-rhinorrhea drugs. He developed typical symptoms of measles after 2 days. The first secondary case (case 2) was an11-month female infant (index case) who showed typical measles symptoms such as fever, rash, conjunctivitis and involvement of respiratory air ways on May 19th, 2012. After this, 3 secondary cases (cases No. 3, 4 and 5) have developed typical measles symptoms. More than 1 incubation period (7-21 days) after detection of case 1, 2 tertiary cases referred to health center with marked measles symptoms, Fig.2. Blood sample were obtained for the rest of cases and immune assay investigations were positive for measles. In response to the outbreak, all eligible residents, 856 people, were vaccinated against measles. To decrease both the severity of disease and the case fatality rate for all patients oral vitamin A were administrated according to WHO schedule (22).
Table 1.
Demographic characteristics and measles-related symptoms of measles cases in the outbreak of south of Iran, 2012
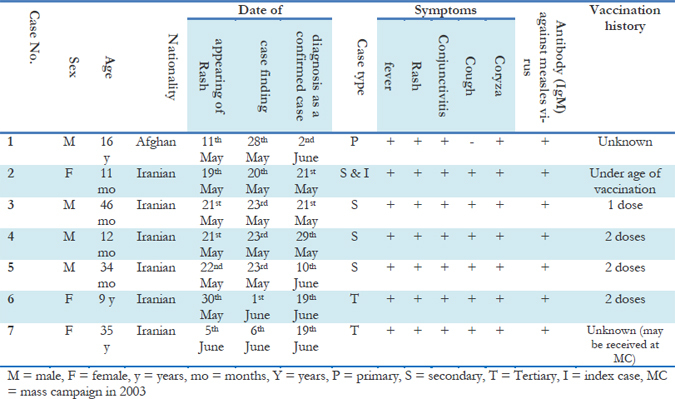
Fig. 2.
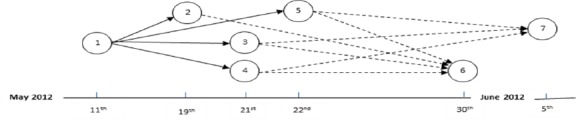
Epidemic network of a measles outbreak in south of Iran, 2012.
Discussion
Measles is a contagious, but preventable disease. The incidence has significant decline in our country over recent years due to expanding administration of national vaccination program throughout country among susceptible children and at risk population (1-3). In the country until 1971, less than 40% of at risk population had been vaccinated against measles. After Islamic revolution, with the integration of the EPI program into the well-developed infrastructure of primary health care (PHC) in 1984, coverage of expanded program of immunization (EPI), including measles vaccine, increased to 90% by the early 1990s. Nationally, the coverage for first and second doses of measles vaccine has been 95% at national level since 1992 and 1996, respectively (24). Also conducting a nationwide measles immunization campaign in 2003, using a combined measles and rubella vaccine for all people aged 5 to 25 years, a target population representing approximately 50% of the total population of Iran (11). In this effort, 2189 urban health care centers, 1238 urban health care stations, 2305 rural health care centers, 16,293 health houses in rural areas, 761 hospitals, and 1159 private clinics had involved in active vaccination program. The campaign was done with excellent cooperation from the private sector and military organs. During one month, 33.5 million persons aged 5-25 years were vaccinated with a combined measles- rubella vaccine, and 99% coverage of the target population was achieved. A post-campaign serologic survey conducted in 2007 and result demonstrated that 97.4% of the population aged 5–40 years had acceptable immunity against measles and rubella (25) but with respect to of this coverage and vaccination programs, several reports of infection outbreak in older age groups also have been documented (26-28).
The mentioned outbreak was the largest documented outbreak in nearly a decade in Fars province, created substantial health risks, and required a vigorous and rapid public health response. Why it happened? This outbreak of measles in the Fars province was caused by the importation of measles from abroad into a susceptible population. Despite this, the spread of disease outside at risk population was minimal due to high level of vaccination among community. It is clear that the main reason underlying of occurrence of the outbreaks, or at least their initiation, is the formation of susceptible foci among target population. Although the highest cumulative incidence was in those aged under the 5 years, we also had infection among the adult person in this outbreak. One of the reasons for these children and the adult becoming susceptible to infection, despite having been immunized against measles at young ages or at campaign programs, may be attenuation of their immunity over the years since their vaccination time. Otherwise, it should be considered that exaggerated and forceful immunization programs against measles maybe prevent the immune-enhancing influence of repeated exposure of vaccinated children to the wild-type measles virus and producing susceptible population among immunized communities (29). Also we should consider other causes for this vaccine failure. Any shortage of cold chain system in national and local levels for affording effective vaccine, appropriate handling of vaccine in health houses in rural area, proper administration of vaccine for target group, nutritional situation of community might be responsible for this or same epidemic. As a limitation, although Koplik's spot is an important sign to recognize measles, however, it does not use as a routine clinical tool in our surveillance system (30). Another limitation was lack of standard forms and sheets for recording of appropriate data. We also haven't enough data about vaccination and source of infection of primary case who was an afghan refugee, this limitation could deactivate further disease control tasks.
To be successful measles control, we needs to do community immunity levels measuring, careful cold chain assessment, accurate measles surveillance monitoring and evaluation and Mass “catch-up” measles immunization (31). We must investigate immunologic and vaccine quality to find main cause of the outbreak. We also advise that all steps of surveillance system of measles should be integrated in all health service levels especially at peripheral level.
Conclusion
Finally, we could conclude that some complex situations triggered this epidemic. Primary case was a trafficking refugee and our surveillance system couldn't exactly observe and check vaccination status of each refugee. Accumulation of unvaccinated refugees in a place leads to an epidemic event and herd immunity cannot do anything. On the other hand, spreading of measles among vaccinated (but questionable immunized) persons could come from a defect in cold chain system or a technological fault in vaccination and needs to conduct an immunoassay survey.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgements
We thank CDC of communicable diseases for surveillance data sharing. We also thank the deputy of health affairs for financial support. The authors declare that there is no conflict of interests.
References
- Moss WJ, Griffin DE (2012). Measles. Lancet, 379: 153–64. [DOI] [PubMed] [Google Scholar]
- WHO (2013). Global Immunization Data. Available at http://www.who.int/immunization_monitoring/Global_Immunization_Data.pdf Access date: 4-April-2013.
- Murray CJL, Lopez AD (1997). Mortality case for eight regions of the world: global burden of disease study. Lancet, 349: 1269–76. [DOI] [PubMed] [Google Scholar]
- Fine PEM (1993). Herd immunity: history, theory, practice. Epidemiologic Reviews, 15: 265–302. [DOI] [PubMed] [Google Scholar]
- Halsey NA (1983). The Optimal Age for Administering Measles Vaccine in Developing Countries In: Halsey NA, de Quadros CA, editors. Recent Advances in Immunization. Washington, DC: PAHO, 4–13. [Google Scholar]
- Van den Ent M, Gupta SK, Hoekstra E (2009). Two doses of measles vaccine reduce death. Indian Pediatrics, 17: 933–38. [PubMed] [Google Scholar]
- American Academy of Pediatrics, Committee on Infectious Diseases (1989). Measles: Reassessment of the current immunization policy. Pediatrics, 84: 1110–13. [PubMed] [Google Scholar]
- Cutts FT, Henao-Restrepo AM, Olive JM (1999). Measles elimination: progress and challenges. Vaccine, 17: S47–S52. [DOI] [PubMed] [Google Scholar]
- EPI (1996). Meeting on advances in measles elimination: conclusions and recommendations. Weekly Epidemiological Record, 71: 305–12. [PubMed] [Google Scholar]
- WHO (2012). Measles immunization coverage by country. Available at http://apps.who.int/gho/da-ta/view.main.230 Access date: 4-April-2013
- Esteghamati A, Gouya MM, Zahraei SM, Dadras MN, Rashidi A, Mahoney F (2007). Progress in measles and rubella elimination in Iran. Pediatr Infect Dis J, 26 (12): 1137–1141. [DOI] [PubMed] [Google Scholar]
- World Health Organization (1999). The World Health report, 1999—making a difference Geneva: World Health Organization, 98: 104. [Google Scholar]
- Mulholland EK, Griffiths UK, Biellik R (2012). Measles in the 21st Century. N Engl J Med, 366: 1755–7. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2011). Measles outbreaks and progress towards meeting measles pre-elimination goals: WHO African Region, 2009–2010. Wkly Epidemiol Rec, 86: 129–40. [PubMed] [Google Scholar]
- WHO (2013). Reported measles cases and incidence rates by WHO Member States 2012. Available at http://www.who.int/immunization_monitoring/diseases/measlesreportedcasesbycountry.pdf Access date: 4-April-2013.
- Colinet G, Rossignol J, Peetermans J (1982). A study of the stability of a bivalent measles-mumps vaccine. J Biol Stand, 10: 341–346. [DOI] [PubMed] [Google Scholar]
- Galazka A, Milstien J, Zaffran M (1998). Thermostability of vaccines. Geneva: World Health Organization. (WHOdocumentWHO/GPV/98.07). [Google Scholar]
- Moss WJ, Griffin DE (2006). Global measles elimination. Nat Rev Microbiol, 4: 900–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gans HA, Arvin AM, Galinus J, Logan L, DeHovitz R, Maldonado Y (1998). Deficiency of the humoral immune response to measles vaccine in infants immunized at age 6 months. J Am Med Assoc, 280 (6): 527–32. [DOI] [PubMed] [Google Scholar]
- Angel JB, Walpita P, Lerch RA, Sidhu MS, Masuredar M, DeLellis RA et al. (1998). Vaccine-associated measles pneumonitis in an adult with AIDS. Ann Intern Med, 129: 104–6. [DOI] [PubMed] [Google Scholar]
- Mulholland K (1995). Measles and Pertussis in developing countries with good vaccine coverage. Lancet, 345: 305–7. [DOI] [PubMed] [Google Scholar]
- WHO (2009). Guidelines for epidemic preparedness and response to measles outbreaks Geneva: (WHO/IVB/09.03). Available from: http://whqlibdoc.who.int/hq/2009/who_ivb_09.03_eng.pdf (Accessed on 7-April-2013).
- Al Wahaibi S, El-Bushra HE, Al-Sulaiman MA (1997). Measles outbreak in Riyadh City, 1997. Saudi Epidemiology Bulletin, 4 (2): 4–5. [Google Scholar]
- Zahraei SM, Gouya MM, Mokhtari Azad T, Soltanshahi R, et al. (2011). Successful Control and Impending Elimination of Measles in the Islamic Republic of Iran. JID, 204: 305–311. [DOI] [PubMed] [Google Scholar]
- Majdzadeh R, Moradi A, Zeraati H, GhajariehSepanlou S, Zamani G, Zonobi V (2008). Evaluation of the measles-rubella mass vaccination campaign in the population covered by Tehran University of Medical Sciences. East Mediterr Health J, 14: 810–7. [PubMed] [Google Scholar]
- Ministry of Health and Medical Education of IRI (1998). Study of measles epidemiology in Iran during 1991 to 1998. Annual report of the Minister of Health and Medical Education, Tehran. [Google Scholar]
- Ministry of Health and Medical Education of IRI (2002). Health picture. Annual report of the Minister of Health and Medical Education, Tehran. [Google Scholar]
- Izadi S, Zahraie SM, Sartipi M (2012). An Investigation into a Measles Outbreak in Southeast Iran. Jpn J Infect Dis, 65: 45–51. [PubMed] [Google Scholar]
- Paunio M, Peltola H, Valle M, et al (1998). Explosive school-based measles outbreak: intense exposure may have resulted in high risk, even among revaccinees. Am J Epidemiol, 148: 1103. [DOI] [PubMed] [Google Scholar]
- Zenner D, Nacul L (2012). Predictive power of Koplik's spots for the diagnosis of measles. J Infect Dev Ctries, 6: 271–5. [DOI] [PubMed] [Google Scholar]
- Clements C J (1994). Global programme for vaccines of the World Health Organization. Role of mass campaigns in global measles control. Lancet, 344: 174–5. [PubMed] [Google Scholar]


