Abstract
Although hilar cholangiocarcinoma is relatively rare, it can be diagnosed on imaging by identifying its typical pattern. In most cases, the tumor appears to be centered on the right or left hepatic duct with involvement of the ipsilateral portal vein, atrophy of hepatic lobe on that side, and invasion of adjacent liver parenchyma. Multi-detector computed tomography (MDCT) and magnetic resonance cholangiopancreatography (MRCP) are commonly used imaging modalities to assess the longitudinal and horizontal spread of tumor.
Keywords: Disease spectrum, hilar cholangiocarcinoma, magnetic resonance cholangiopancreatography, multi-detector computed tomography
Introduction
Cholangiocarcinoma is a primary cancer of the bile ducts. Its incidence varies worldwide. Although it comprises only 10-15% of hepatobiliary neoplasms, its incidence is increasing.[1] However, cholangiocarcinoma remains a relatively rare disease accounting for <2% of all human malignancies.[2] Its prevalence also varies considerably from one region to another. Its prevalence is the highest in Southeast Asia. According to recent literature, the prevalence of intrahepatic cholangiocarcinoma is increasing while that of extrahepatic cholangiocarcinoma remains constant or decreasing.[3] It is more common in men than in women, occurring most frequently between the 6th and 7th decades.[4] It is classified as intrahepatic or extrahepatic cholangiocarcinoma depending on their location. Tumor that arises distal to the secondary bifurcation of the right or left hepatic duct is intrahepatic cholangiocarcinoma. Extrahepatic tumor arises from the hilar plate and common bile duct. Tumor that arises from the right or left hepatic duct or the bifurcation of common hepatic duct is hilar cholangiocarcinoma (Klatskin tumor) [Figure 1].[5,6,7] Most of the cholangiocarcinomas are ductal adenocarcinoma. Other histological types are papillary, mucinous, signet-ring cell, mucoepidermoid, squamous, adenosquamous, and cystadenocarcinoma.[8]
Figure 1.
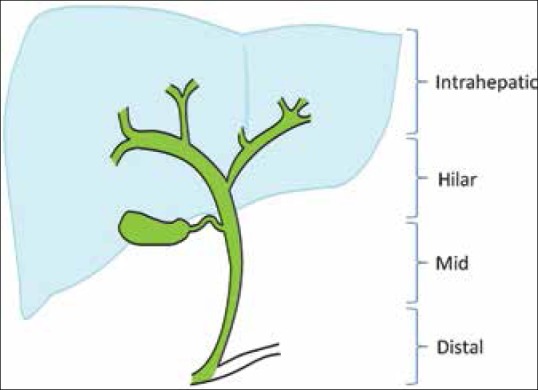
Schematic drawing showing location of intrahepatic and extrahepatic cholangiocarcinoma
Predisposing Factors
There are several predisposing factors that cause chronic inflammation of the biliary tree and subsequently increase the risk for development of cholangiocarcinoma. In endemic areas, infection with liver flukes like Opisthorchis viverrini and Clonorchis sinensis and recurrent pyogenic cholangitis are the common causes. Other predisposing factors include primary sclerosing cholangitis, viral infections like human immunodeficiency virus, hepatitis B and C virus, and Epstein-Barr virus, anomalous pancreaticobiliary junction, choledochal cyst, and fibrocystic liver disease. Liver cirrhosis, polyposis syndrome of the colon, toxins like thorotrast, dioxin, and polyvinyl chloride, biliary-enteric drainage procedure, and heavy alcohol consumption have also been reported to predispose to cholangiocarcinoma.[1,3,8]
Protocol
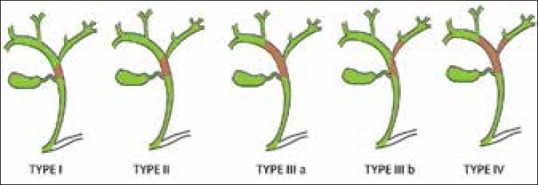
Patients were imaged using 64-slice MDCT scanner (Sensation 64slice CT; Siemens, Erlangen, Bavaria, Germany). All the patients were scanned using a standard protocol. Delayed scan were obtained after 6-10 min [Table 1].
Table 1.
MDCT protocol used for scanning patients
Patient underwent magnetic resonance imaging (MRI) on a 1.5 T system (either GE HDxT or Siemens Magnetom Symphony Maestro Class) using body array coil. Patient is instructed to fast for 12 h before examination. The unenhanced axial fast spin-echo T2W with and without fat suppression and coronal T2 single-shot fast spin-echo images are obtained using 256 × 256 matrix, 30 cm field of view (FOV), 4 mm slice thickness, 1 mm interslice gap, and 2 number of excitation (NEX). Five to six drops of gadopentetate dimeglumine are mixed with 50-100 ml of water and the patient is asked to drink this mixture to nullify the water signal in stomach. Free-breathing thin-slab three-dimensional magnetic resonance cholangiopancreatography (MRCP) is acquired with respiratory gating or triggering using 256 × 256 matrix, 32 FOV, 1.4 mm slice thickness, and 1 NEX. Dynamic gadolinium-enhanced images are useful to assess the enhancement characteristic of the lesion and the status of the surrounding vasculature.
Classification and Staging
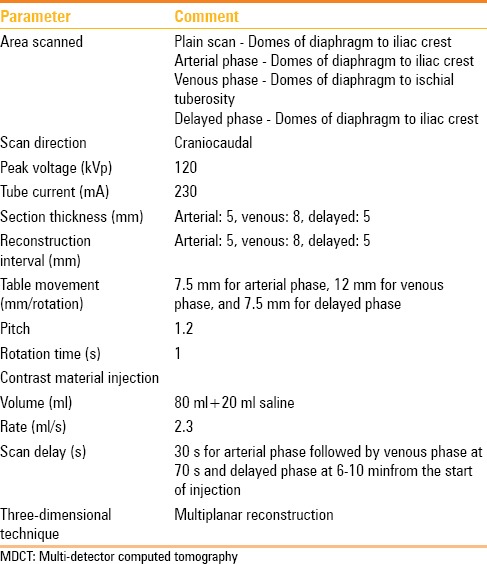
Cholangiocarcinoma can develop in any part of the extrahepatic duct, involving the upper third of the duct including the hilum in 50-75% of the reported cases, the middle third in 10-25% cases, and the lower duct in 10-25% cases.[9] Adenocarcinoma of hepatic duct at its bifurcation (hilar cholangiocarcinoma) was first described by Klatskin in 1965.[10,11] Klatskin tumor is categorized using Bismuth-Corlette classification in-to the following [Figure 2]:
Figure 2.
Schematic drawing of Bismuth-Corlette classification of ductal involvement in hilar cholangiocarcinoma
Type I: Tumors below the bifurcation of common hepatic duct;
Type II: Tumors involving the bifurcation; but not extending in-to the main right and left duct;
Type III: Tumors infiltrating the right (IIIa) or the left (IIIb) hepatic duct;
Type IV: Tumors involving both the right and left hepatic ducts.[12,13,14]
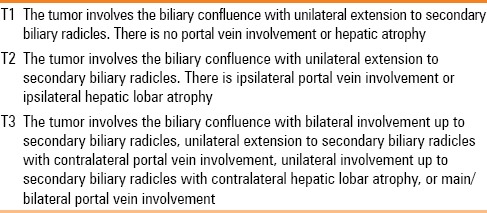
This classification system describes the longitudinal extent of the tumor, but it does not predict resectability or survival. Horizontal extension to the soft tissue and vessels can be assessed based on T staging.[15,16] Since the American Joint Commission for Cancer (AJCC) tumor-node-metastasis (TNM) staging can be determined only after resection of tumor, it has less relevance to preoperative staging [Table 2].[16] Memorial Sloan-Kettering Cancer Center proposed a preoperative staging system that correlates with resectability and outcome. It takes into account the local extent of the tumor regardless of N or M status. This staging system is based on the extent of the tumor within the biliary tree, vascular invasion, and lobar atrophy [Table 3].[6,7,16] Recently, the International Cholangiocarcinoma Group has proposed a new staging system for perihilar cholangiocarcinoma. It takes into account the anatomic, pathologic, and surgical features of the tumor. If this staging system is accepted by the international community, it will reduce most of the problems of perihilar cholangiocarcinoma.[6]
Table 2.
AJCC staging system (seventh edition) of hilar cholangiocarcinoma
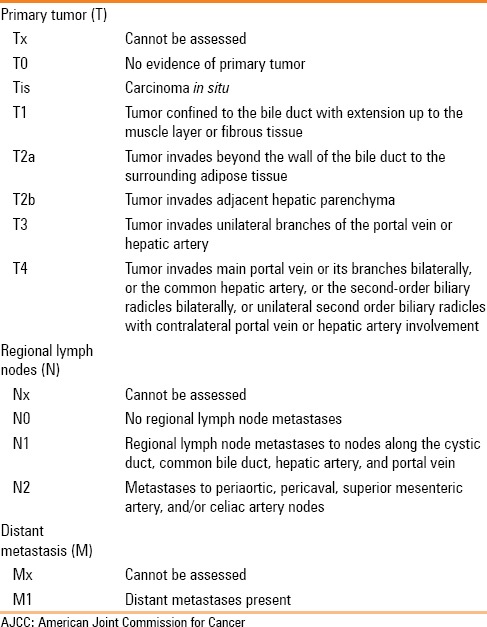
Table 3.
Preoperative tumor staging system of hilar cholangiocarcinoma
Morphological Types and Spread
The Japanese Liver Cancer Group has classified cholangiocarcinomas into three types according to macroscopic appearance of the tumor: Mass-forming, intraductal-growing, and periductal-infiltrating types. The last type is more prevalent in the hilar portion of the biliary tree [Figure 3].[17] This classification describes the gross appearance, growing characteristics, and biologic behavior of the tumor. It has prognostic implication for patients and correlates with radiological findings. Mass-forming and periductal-infiltrating tumors have bad prognosis as compared to intraductal-growing tumors after surgical resection.[9]
Figure 3 (A-C).
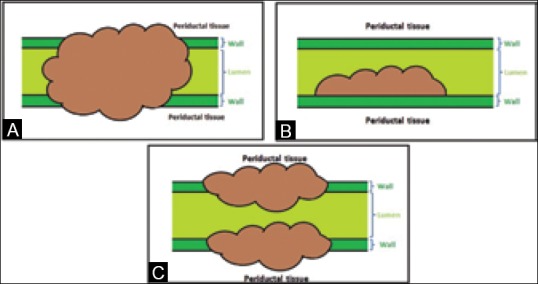
Schematic drawing showing morphological types of cholangiocarcinoma: (A) mass-forming; (B) intraductal-growing; (C) periductal-infiltrating
On imaging, hilar cholangiocarcinoma appears as irregular thickening of the bile duct wall with or without surrounding parenchymal invasion. There is usually disproportionate dilatation of intrahepatic bile ducts and segmental/lobar atrophy of the liver with or without vascular invasion. These tumors show minimal or no enhancement. Due to the fibrous nature of the tumor, enhancement in the delayed phase is observed frequently [Figures 4 and 5].[8] In patients with malignant biliary obstruction due to cholangiocarcinoma, the serum bilirubin level often reaches greater than 10 mg/dl and averages 18 mg/dl, whereas patients with obstruction from choledocholithiasis have lower bilirubin levels. The high bilirubin levels in conjunction with typical radiological findings allow a fairly confident diagnosis of cholangiocarcinoma.[16]
Figure 4 (A-D).
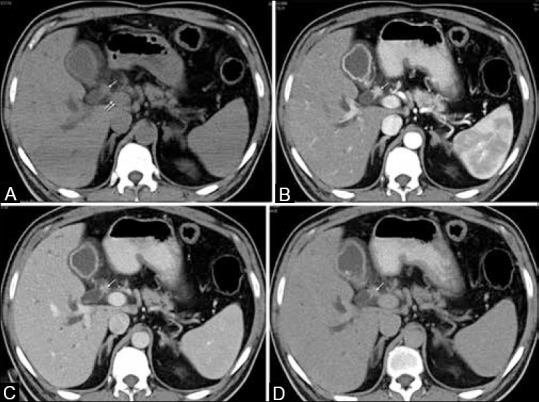
Hilar cholangiocarcinoma with early enhancement. (A) Axial unenhanced CT shows a low density mass (white single arrow) anterior to portal vein (white double arrow). (B) Axial arterial phase scan shows hyperattenuating mass at primary confluence (white single arrow). (C and D) Progressively decreased attenuation of mass on venous (white single arrow in C) and delayed phase (white single arrow in D)
Figure 5 (A-G).
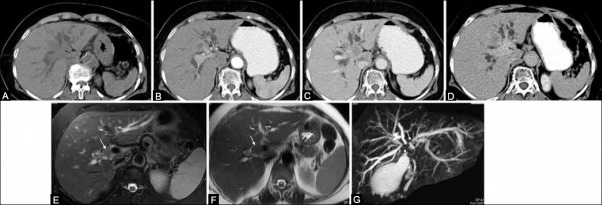
A 79-year-old female with type IV hilar cholangiocarcinoma. (A) Noncontrast CT scan shows low density mass at porta hepatis (single black arrow). (B) Transverse CT scan in arterial phase shows hypoattenuating tumor (single black arrow) encasing the hepatic artery (double black arrow). (C) Note the invasion of the adjacent liver parenchyma (single black arrow) and the small node in lesser sac (double black arrow). (D) Post-contrast delayed image shows retention of contrast material within the tumor (single black arrow). Type IV mass-forming tumor is very well detected on axial T2W images with (E) and without fat suppression (F) in different patients (single white arrow). MRCP image (G) shows isolation of bilateral sectoral ducts (single white arrow)
Mass-forming type
The tumor forms a small nodule of usually 1-2 cm in diameter with bile duct dilatation. It obstructs the bile duct lumen in early stage and causes obstructive jaundice, infiltrates the wall, and eventually invades the periductal tissue. The surface of the lumen is usually irregular. Because the size of the tumor is small, images should be very carefully assessed [Figures 6 and 7].[9]
Figure 6 (A-F).
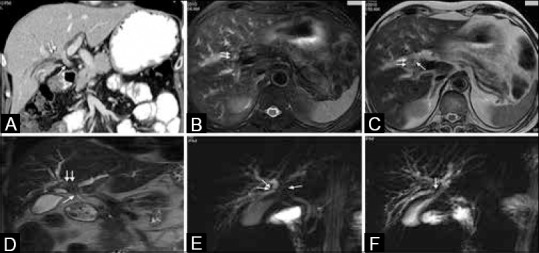
A 67-year-old male with mass-forming type IIIa hilar cholangiocarcinoma. (A) Contrast-enhanced coronal CT scan shows concentric thickening of common hepatic duct (white single arrow) and soft tissue mass (white double arrow) involving right secondary confluence. Axial T2W images with (B) and without fat suppression (C) and coronal T2W image (D) show thickening of common hepatic duct (white single arrow) with periductal mass formation (white double arrow). Thick-slab MRCP images show involvement of primary (white single arrow in E) and right secondary confluence (white double arrow in e) and isolation of segment VI duct (white single arrow in F)
Figure 7 (A-E).
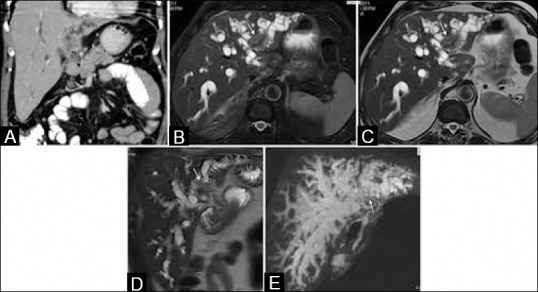
Type IIIb moderately differentiated mass-forming hilar cholangiocarcinoma. (A) Contrast-enhanced coronal CT image shows tumor mass in common hepatic duct (black single arrow) extending to the left hepatic duct (black double arrow). (B-D) Axial T2W images with and without fat suppression and coronal T2W image very well show mass-forming tumor in dilated left biliary radicles (white single arrow). (E) MRCP image show isolation of left sectoral ducts (white single arrow)
Periductal-infiltrating type
It is characterized by annular mass-like lesion or thickening along a dilated or narrowed bile duct without mass formation and manifests as an elongated, spiculated, or branch-like abnormality.[3] It usually causes complete luminal obstruction. The thickness of the wall varies from a few millimeters to 1 cm. The extent of the tumor ranges from 0.5 to 6 cm. It sometimes involves the entire extrahepatic duct, extending proximally as far as the intrahepatic ducts. Tumor can grow outside the bile ducts in the intrahepatic portion [Figures 8 and 9].[9]
Figure 8 (A-E).
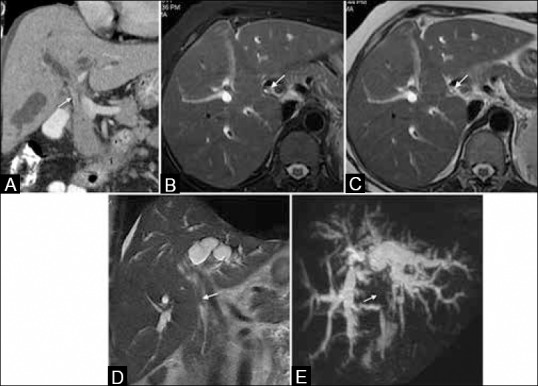
Type I periductal-infiltrating hilar cholangiocarcinoma. (A) Contrast-enhanced coronal CT image showing enhancing tumor (white single arrow) in common hepatic duct. (B-D) Axial T2W images with and without fat suppression and coronal T2W image show concentric thickening of common hepatic duct (white single arrow). (E) MRCP image reveals complete obstruction at the level of common hepatic duct (white single arrow)
Figure 9 (A-D).
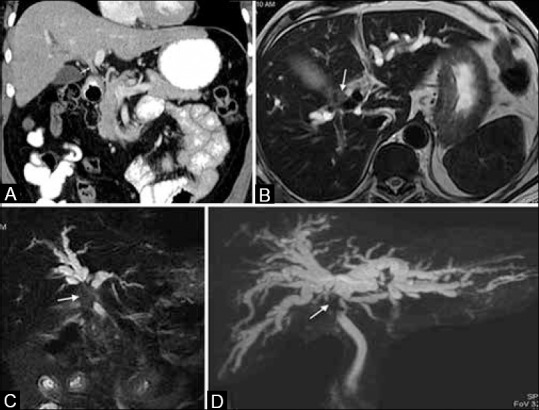
Type II periductal-infiltrating hilar cholangiocarcinoma. (A) Contrast-enhanced coronal CT image showing enhancing tumor (white single arrow) in common hepatic duct and primary confluence extending to the right and left hepatic ducts. Type II hilar tumor is well depicted on axial T2W image without fat suppression (B) coronal T2W image with fat suppression (C) and MRCP image (D) (white single arrow) in different patients
Intraductal-growing type
It may be polypoid, sessile, or superficially spreading along the mucosal layer. Generally, the tumor is confined to mucosa and does not invade deep to the submucosal layer, and the surrounding tissue is infiltrated only in late stage [Figure 10].[9] Identification of this variant is crucial because this tumor is often resectable surgically and has more favorable prognosis than the other two types.[16] Sometimes, several, discrete multiple tumors may be present along the inner surface of the bile ducts, which is called cholangiocarcinomatosis. Tumor nodules of cholangiocarcinomatosis are slender, long, and very fragile and are easily sloughed off spontaneously and during surgery, mimicking calculi.[9]
Figure 10 (A and B).
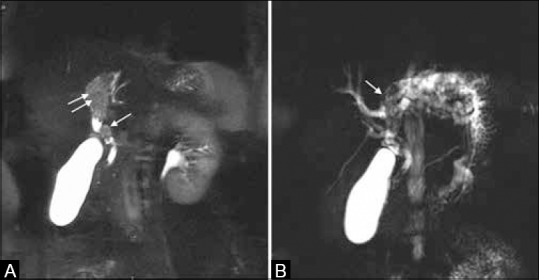
Intraductal-growing hilar cholangiocarcinoma in a 62-year-old female. (A) Coronal T2-fat-suppressed image shows mildly hyperintense tumor filling and expanding the common hepatic (white single arrow) and left hepatic duct (white double arrow). (B) MRCP image shows dilated left duct system with multiple filling defects (white single arrow)
Preoperative Assessment of Resectability
Preoperative evaluation of hilar cholangiocarcinoma is important because resection is the only effective therapy.[16] MDCT and MRCP are the best imaging techniques to diagnose the disease, delineate the extent of the tumor, and rule out liver metastasis and enlarged lymph nodes.[18] MDCT allows for faster scanning with thinner collimation and can result in an improved diagnosis and evaluation of hilar cholangiocarcinoma.[19,20] Thinner and multiplanar reconstruction of the acquired data on workstation is important to trace the biliary anatomy and assess the exact level and extent of the tumor. Crucial factors that should be assessed very carefully by the radiologist are extent of the tumor within the bile ducts, vascular involvement, hepatic atrophy, and metastatic disease.[16]
Bile duct extension
Proximal extent of the biliary tree involvement by the tumor is important in treatment planning.[21] Direct cholangiography, endoscopic retrograde cholangiopancreatcography (ERCP) or percutaneous transhepatic cholangiography (PTC) have been considered the standard of reference for evaluating the ductal extent of the tumor.[20] PTC does not depict the entire biliary system when there is segmental or ductal isolation. Moreover, inadvertent injection of contrast into isolated ducts can lead to cholangitis. 3-D MRCP is useful in such cases. MRCP is a highly accurate method of imaging the biliary tree. The reported accuracy in determining the extent of bile duct tumors ranges from 71 to 96%.[20] MRCP accurately assessed the level of bile duct involvement, according to the Bismuth-Corlette classification in 84% of patients.[22] Recent studies using MDCT have also reported high diagnostic accuracy. Choi et al. reported an approximate 80% accuracy for the diagnosis of tumor spread at the level of the secondary biliary confluences.[20] Thus, the accuracy of MRCP and MDCT in assessing the horizontal tumor spread is comparable. Sligle-slice CT often under-estimates the proximal extent of the tumor.[23] Tumor involving the hepatic duct up to secondary confluence on both sides (Bismuth type IV) is considered unresectable [Figure 5].[8]
Vascular involvement
Vascular involvement is a characteristic feature of cholangiocarcinoma in late stages. This hilar neoplasm can involve portal vein, hepatic artery, hepatic vein, and inferior vena cava [Figure 11]. The vessel is considered to be infiltrated if it is occluded, stenosed, deformed adjacent to the tumor contact, and/or more than 180° of its circumference is involved.[24] Tumor causing complete encasement or occlusion of the main portal vein and hepatic artery proximal to the bifurcation, atrophy of one hepatic lobe with encasement of contralateral vessel, and invasion of secondary biliary confluence on one side and encasement of contralateral vessel is considered unresectable.[8,24] Unilateral portal vein or hepatic artery occlusion, vascular compression, unilateral hepatic metastasis, and infiltration of fat planes adjacent to nonvascular structures are not a contraindication to surgical resection.[24] Short segment invasion of less than 20 mm in length of the main portal vein is not a contraindication for curative resection. This segment can be resected with venous graft placement.[15]
Figure 11.

Infiltrating mass (black single arrow) occluding the portal vein, its bifurcation and branches (black double arrows) indicate inoperable disease
Hepatic atrophy
Atrophy of the lobe is often underdiagnosed and, if present, should always be mentioned in the report as it influences therapy. Portal blood supply and bile flow are important pre-requisites to maintain the normal liver size. Segmental or lobar atrophy may result from a portal venous occlusion or biliary obstruction [Figure 12]. One or both of these findings are often present in patients with hilar cholangiocarcinoma. Long-standing biliary obstruction itself can cause parenchymal atrophy. When the portal vein branch is also obstructed, the atrophy becomes severe. Compensatory hypertrophy of contralateral uninvolved lobe occurs and results in atrophy-hypertrophy complex.[16] No liver resection should be performed that leaves an atrophic remnant.[22] Tumor that causes atrophy of hepatic lobe on one side and extension of tumor to secondary biliary confluence on the opposite side is considered unresectable.[24] Lobar atrophy is diagnosed when dilated and crowded bile ducts are present in a hypoperfused lobe.[16]
Figure 12.
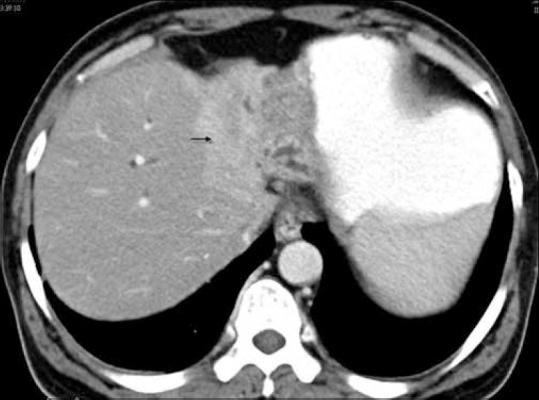
Atrophy of left lobe in type IIIb hilar cholangiocarcinoma. Note the enhancement of lateral segment in arterial phase (black single arrow) due to portal vein occlusion
Metastatic disease
Incidence of the nodal involvement is quite high in the literature, ranging from 30% to more than 50% [Figure 5C]. Its incidence increases with increasing depth of invasion of the primary tumor. Lymph nodes along the cystic duct and common bile duct in the hepatoduodenal ligament, along the hepatic artery and portal vein exhibit high incidence of metastatic involvement. It also involves retropancreatic, periaortic, pericaval, superior mesenteric artery, and/or celiac artery lymph nodes. Spread of the tumor to the nodal group beyond the hepatoduodenal ligament indicates unresectable disease. Paraaortic nodes are considered as the final nodal stations in the abdominal lymphatic system for cholangiocarcinoma.[16] Nodes greater than 10 mm in short-axis diameter, presence of necrosis, and heterogeneous appearance are considered pathological.[15] Metastasis to liver, peritoneum, and lung can occur in late stage that precludes the curative resection [Figure 13].[25,26]
Figure 13 (A-C).
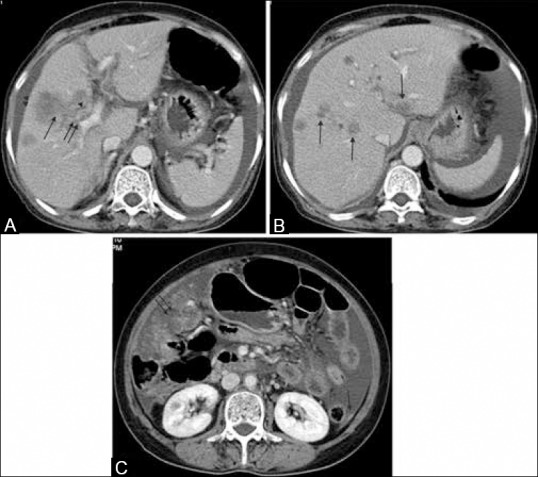
A 62-year-old female with type IIIa hilar cholangiocarcinoma. (A) Axial contrast-enhanced image shows infiltrating mass in the right lobe (black single arrow) with occlusion of anterior branch of right portal vein (black double arrow), concentric thickening of right hepatic duct (black single arrow-head), and ascites (black double arrow-head). (B and C) Axial contrast-enhanced image shows several hypodense metastatic deposits in liver parenchyma (black single arrow in B) and peritoneum (black single arrow in C) and omentum (black double arrow in C)
Treatment Options
Majority of the patient of advanced hilar cholangiocarcinoma die within 6-12 months of the diagnosis usually due to hepatic failure or secondary infections because of biliary obstruction. The prognosis has been considered worse for lesions affecting the confluence of the bile ducts and better for lesions close to the papilla. The yield of percutaneous needle biopsy or biliary brush cytology is poor and one may miss the opportunity to resect an early cancer. Histologic confirmation of malignancy is not mandatory before exploration. Combination of presence of focal obstructive hilar lesion and appropriate clinical and laboratory finding in the absence of previous biliary tract surgery is sufficient to make the diagnosis of Klatskin tumor which is correct in most of the cases.[16] Hence, the mainstay of preoperative diagnosis in hilar cholangiocarcinoma is imaging.[20] To determine the operability and in order to select the appropriate surgical procedure, an accurate preoperative evaluation of both longitudinal spread and horizontal invasion is a prerequisite.[19] Complete tumor excision with negative tumor margins and restoration and biliary-enteric continuity from liver remnant are the main goals of the surgical treatment.[16] Type I and II tumors are treated with en-bloc resection of the extrahepatic bile ducts, gall bladder, and regional lymph nodes with 5-10 mm of bile duct margins. In type III tumors, hilar resection with right or left hepatectomy or trisegmentectomy is considered. Right or left trisegmentectomy is offered to patients with type IV tumors. In type III and IV tumors, caudate lobectomy is necessary because bile duct to this segment frequently joins the bile duct bifurcation. Roux-en-Y hepaticojejunostomy is required after resection of the hilar tumor.[11,27] Preoperative portal vein embolization (PVE) is required in patients with locally advanced perihilar tumor to increase the liver mass, shift in liver function to future liver remnant (FLR), and preoperative adjustment to portal pressure changes. PVE is indicated when the FLR is ≤20%, ≤30%, and ≤40% in patients with normal underlying liver, intermediate liver disease, and cirrhosis, respectively.[28] Embolization is achieved with polyvinyl alcohol particles or coils. Hepatocyte growth factor and epidermal growth factor are released in response to PVE, and hepatocyte regeneration occurs with resultant hypertrophy of contralateral liver. Maximum liver regeneration occurs within the first 2 weeks of PVE. FLR is reassessed at 4 weeks after PVE and if the FLR is adequate, the resection can be performed at that time.[6] Patients with unresectable tumor are candidates for palliative therapy [Table 4].[16,24] Main aim of the palliation therapy is to decompress the biliary system for relief of jaundice. Drainage of only 25-30% of functional liver tissue is sufficient for the resolution of jaundice. Percutaneous transhepatic biliary drainage and subsequent placement of the self-expandable metallic wall stent is preferred over endoscopically placed stent. Metallic wall stents are cost-effective, have longer duration of patency, and are associated with short hospital stay. Percutaneous drainage through an atrophic lobe does not relieve the jaundice and should be avoided. Jaundice due to portal vein occlusion without biliary dilatation is also not corrected with stenting. Patients who are found to have unresectable tumor at the time of surgery are candidates for palliative bilio-enteric bypass or hepaticojejunostomy, if feasible technically. Roux-en-Y hepaticojejunostomy is preferred when the tumor is low placed and the hilar bile duct is not obstructed. Longmire's operation may be performed in obstructed hilum. In this operation, the second bile duct of left hepatic lobe and the jejunum are anastomosed with each other after resection of the lateral left hepatic lobe. The right hepatic duct could be decompressed if it is dilated and the left hepatic duct is obstructed. When the right hepatic duct is short, decompression can be done using segment V duct.[14,16,25,27] Palliative radiation therapy can be offered to those patients who have unresectable, locally advanced tumor without widespread disease. Combined external beam radiation and intraluminal iridium-192 is commonly used. It improves pain control, maintains biliary patency, and increases survival. Stereotactic body radiotherapy has less treatment-related complications. High dose of radiation to the tumor and a margin is delivered using multiple beams over 3-5 days. It limits the dose to the adjacent normal tissue and does not require concurrent chemotherapy.[6,16] Palliative systemic chemotherapeutic agents like cisplatin followed by gemcitabine or gemcitabine alone for 6 months have shown an improvement in median survival rate.[16] Photodynamic therapy causes destruction of the tumor cells limited to superficial 4-4.5 mm depth. In photodynamic therapy, the injected photosensitizer (sodium porfimer) accumulates in the malignant cells. Direct cholangioscopic illumination activates this compound and causes malignant cell death. It is well tolerated and improves survival and quality of life.[16,29] Complete resection of tumor can be achieved with orthotopic liver transplant (OLT). Recurrence rate with OLT is high and the 5-year survival rate is only 10%. Combination of neoadjuvant therapy, intra-operative staging for regional metastases, and liver transplantation is superior to OLT, radical resection, and adjuvant therapy alone in selected patients. The 5-year survival rate with this combined therapy is 73% in highly selected patients.[6,30]
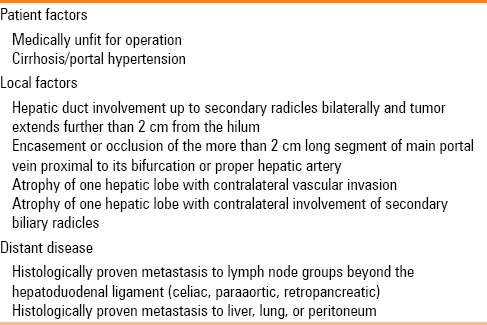
Table 4.
Criteria of unresectability of hilar cholangiocarcinoma
Common Mimics
Correct diagnosis of hilar cholangiocarcinoma is challenging on imaging and many neoplastic and non-neoplastic conditions can be misdiagnosed as hilar cholangiocarcinoma. Its common mimics are primary sclerosing cholangitis, recurrent pyogenic cholangitis, Mirizzi syndrome, gall bladder cancer, inflammatory pseudotumor, lymphoma, melanoma deposits, sarcoidosis, carcinoid tumor, and metastasis. Typical features of primary sclerosing cholangitis are multifocal strictures, duct wall thickening, and irregular beading of intrahepatic and extrahepatic bile ducts with peripheral pruning of the ducts. Recurrent pyogenic cholangitis manifests as biliary strictures, duct wall thickening, and pigmented intraductal calculi. Predominant involvement of the left lateral and right posterior segmental biliary duct system is typical of recurrent primary cholangitis. Mirizzi syndrome shows extrinsic narrowing of the common hepatic duct due to impacted calculus in the neck of the gall bladder or abnormally inserted cystic duct. Gall bladder carcinoma in the neck often infiltrates the common hepatic duct and simulates hilar cholangiocarcinoma. Nonvisualization or partial visualization of gall bladder, mass engulfing the calculi, and contiguous infiltration of liver parenchyma around the gall bladder fossa often differentiate these two conditions. Melanoma of the biliary tract is hyperintense on T1-weighted images and hypointense on T2-weighted images due to melanin content. Carcinoid tumors occur relatively in early age group and are less aggressive. Biliary inflammatory pseudotumor, lymphoma, metastasis, and sarcoidosis may be indistinguishable from cholangiocarcinoma.[8,31]
Conclusion
MDCT and MRCP are used to stage the hilar cholangiocarcinoma. The common feature of hilar cholangiocarcinoma is dilatation of intrahepatic biliary radicles, involvement of primary and one or both of the secondary confluence with invasion of ipsilateral portal vein, adjacent liver parenchymal infiltration, and lobar atrophy. Awareness of these common findings will aid the prospective imaging diagnosis of this rare disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lazaridis KN, Gores GJ. Cholangiocarcinoma. Gastroenterology. 2005;128:1655–67. doi: 10.1053/j.gastro.2005.03.040. [DOI] [PubMed] [Google Scholar]
- 2.Slattery JM, Sahani DV. What is the current state-of-the-art imaging for detection and staging of cholangiocarcinoma. Oncologist. 2006;11:913–22. doi: 10.1634/theoncologist.11-8-913. [DOI] [PubMed] [Google Scholar]
- 3.Chung YE, Kim MJ, Park YN, Choi JY, Pyo JY, Kim YC, et al. Varying appearances of cholangiocarcinoma: Radiologic-pathologic correlation. Radiographics. 2009;29:683–700. doi: 10.1148/rg.293085729. [DOI] [PubMed] [Google Scholar]
- 4.Vanderveen KA, Hussain HK. Magnetic resonance imaging of cholangiocarcinoma. Cancer Imaging. 2004;4:104–15. doi: 10.1102/1470-7330.2004.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Han JK, Choi BI, Kim AY, An SK, Lee JW, Kim TK, et al. Cholangiocarcinoma: Pictorial essay of CT and cholangiographic findings. Radiographics. 2002;22:173–87. doi: 10.1148/radiographics.22.1.g02ja15173. [DOI] [PubMed] [Google Scholar]
- 6.Valero V, 3rd, Cosgrove D, Herman JM, Pawlik TM. Management of perihilar cholangiocarcinoma in the era of multimodal therapy. Expert Rev Gastroenterol Hepatol. 2012;6:481–95. doi: 10.1586/egh.12.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suarez-Munoz MA, Fernandez-Aguilar JL, Sanchez-Perez B, Perez-Daga JA, Garcia-Albiach B, Pulido-Roa Y, et al. Risk factors and classifications of hilar cholangiocarcinoma. World J Gastrointest Oncol. 2013;5:132–8. doi: 10.4251/wjgo.v5.i7.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ashkar L, Maheshwari S, Pressacco J, Nakai A, Edelman RR, Reinhold C, et al. MR Cholangiopancreatography. In: Edelman RR, Hesselink J, Zlatkin M, editors. Clinical Magnetic Resonance Imaging. 3rd ed. Philadelphia: Saunders; 2005. pp. 4695–4711. [Google Scholar]
- 9.Lim JH. Cholangiocarcinoma: Morphologic classification according to growth pattern and imaging findings. AJRAm J Roentgenol. 2003;181:819–27. doi: 10.2214/ajr.181.3.1810819. [DOI] [PubMed] [Google Scholar]
- 10.Klatskin G. Adenocarcinoma of the hepatic duct at its bifurcation within the porta hepatis. An unusual tumor with distinctive clinical and pathological features. Am J Med. 1965;38:241–56. doi: 10.1016/0002-9343(65)90178-6. [DOI] [PubMed] [Google Scholar]
- 11.Papoulas M, Lubezky N, Goykhman Y, Kori I, Santo E, Nakache R, et al. Contemporary surgical approach to hilar cholangiocarcinoma. Isr Med Assoc J. 2011;13:99–103. [PubMed] [Google Scholar]
- 12.Bismuth H, Corlette MB. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet. 1975;140:170–8. [PubMed] [Google Scholar]
- 13.Bismuth H, Nakache R, Diamond T. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 1992;215:31–8. doi: 10.1097/00000658-199201000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mansfield SD, Barakat O, Charnley RM, Jaques BC, O’“Suilleabhain CB, Atherton PJ, et al. Management of hilar cholangiocarcinoma in the North of England: Pathology, treatment and outcome. World J Gastroenterol. 2005;11:7625–30. doi: 10.3748/wjg.v11.i48.7625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chung YE, Kim MJ, Park YN, Lee YH, Choi JY. Staging of extrahepatic cholangiocarcinoma. Eur Radiol. 2008;18:2182–95. doi: 10.1007/s00330-008-1006-x. [DOI] [PubMed] [Google Scholar]
- 16.House MG, Angelica MD, Jarnagin WR, Jarnagin WR, Blumgart LH. Cancer of the bile ducts: Extrahepatic biliary tumors. In: Jarnagin WR, editor. Blumgart: Surgery of the Liver, Biliary Tract and Pancreas. 5th ed. Philadelphia: Saunders; 2012. pp. 771–88. [Google Scholar]
- 17.4th ed. Tokyo, Japan: Kanehara and Co. Ltd; 2000. Liver Cancer Study Group of Japan. The General Rules for the Clinical and Pathological Study of Primary Liver Cancer. [Google Scholar]
- 18.Figueras J, Llado L, Valls C, Serrano T, Ramos E, Fabregat J, et al. Changing strategies in diagnosis and management of hilar cholangiocarcinoma. Liver Transpl. 2000;6:786–94. doi: 10.1053/jlts.2000.18507. [DOI] [PubMed] [Google Scholar]
- 19.Akamatsu N, Sugawara Y, Osada H, Okada T, Itoyama S, Komagome M, et al. Diagnostic accuracy of multidetector-row computed tomography for hilar cholangiocarcinoma. J Gastroenterol Hepatol. 2010;25:731–7. doi: 10.1111/j.1440-1746.2009.06113.x. [DOI] [PubMed] [Google Scholar]
- 20.Choi JY, Kim MJ, Lee JM, Kim KW, Lee JY, Han JK, et al. Hilar cholangiocarcinoma: Role of preoperative imaging with sonography, MDCT, MRI, and direct cholangiography. AJR Am J Roentgenol. 2008;191:1448–57. doi: 10.2214/AJR.07.3992. [DOI] [PubMed] [Google Scholar]
- 21.Feydy A, Vilgrain V, Denys A, Sibert A, Belghiti J, Vullierme MP, et al. Helical CT assessment in hilar cholangiocarcinoma: Correlation with surgical and pathological findings. AJR Am J Roentgenol. 1999;172:73–7. doi: 10.2214/ajr.172.1.9888743. [DOI] [PubMed] [Google Scholar]
- 22.Manfredi R, Masselli G, Maresca G, Brizi MG, Marona P. MR imaging and MRCP of hilar cholangiocarcinoma. Abdom Imaging. 2003;28:319–25. doi: 10.1007/s00261-002-0047-x. [DOI] [PubMed] [Google Scholar]
- 23.Valls C, Ruiz S, Martinez L, Leiva D. Radiological diagnosis and staging of hilar cholangiocarcinoma. World J Gastrointest Oncol. 2013;5:115–26. doi: 10.4251/wjgo.v5.i7.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee HY, Kim SH, Lee JM, Kim SW, Jang JY, Han JK, et al. Preoperative assessment of resectibility of hepatic hilar cholangiocarcinoma: Combined CT and cholangiography with revised criteria. Radiology. 2006;239:113–21. doi: 10.1148/radiol.2383050419. [DOI] [PubMed] [Google Scholar]
- 25.Bold RJ, Goodnight JE., Jr Hilar cholangiocarcinoma: Surgical and endoscopic approaches. Surg Clin North Am. 2004;84:525–42. doi: 10.1016/S0039-6109(03)00232-9. [DOI] [PubMed] [Google Scholar]
- 26.Burke EC, Jarnagin WR, Hochwald SN, Pisters PW, Fong Y, Blumgart LH. Hilar Cholangiocarcinoma: Patterns of spread, the importance of hepatic resection for curative operation, and a presurgical clinical staging system. Ann Surg. 1998;228:385–94. doi: 10.1097/00000658-199809000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang WL, Zhang XC, Zhang DW, Tong BF. Diagnosis and surgical treatment of hepatic hilar cholangiocarcinoma. Hepatobiliary Pancreat Dis Int. 2007;6:631–5. [PubMed] [Google Scholar]
- 28.Anaya DA, Blazer DG, Abdalla EK. Strategies for resection using portal vein embolization: Hepatocellular carcinoma and hilar cholangiocarcinoma. Semin Intervent Radiol. 2008;25:110–22. doi: 10.1055/s-2008-1076684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee TY, Cheon YK, Chim CS. Current status of photodynamic therapy for bile duct cancer. Clin Endosc. 2013;46:38–44. doi: 10.5946/ce.2013.46.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosen CB, Heimbach JK, Gores GJ. Liver transplantation for cholangiocarcinoma. Transpl Int. 2010;23:692–7. doi: 10.1111/j.1432-2277.2010.01108.x. [DOI] [PubMed] [Google Scholar]
- 31.Menias CO, Surabhi VR, Prasad SR, Wang HL, Narra VR, Chintapalli KN. Mimics of cholangiocarcinoma: Spectrum of disease. Radiographics. 2008;28:1115–29. doi: 10.1148/rg.284075148. [DOI] [PubMed] [Google Scholar]


