Abstract
Aim
Describe the characteristics of patients initiating human regular U-500 insulin (U-500R) and their subsequent glycemic control in a real-world setting.
Methods
US Humedica electronic health record system data (July 2007–September 2011) were used to identify patients with diabetes aged ≥18 years with ≥1 records for U-500R prescriptions, 6 months of preindex data, 12 months following first use of U-500R, and at least one glycated hemoglobin (HbA1c) value in both preindex and postindex periods. Paired t tests were used to measure the change in HbA1c from preindex to postindex periods (last or most recent values) and hypoglycemia.
Results
Among patients initiating U-500R (N=445), 96.9% had type 2 diabetes with mean age 57 years and mean body mass index 40.4 kg/m2. Postindex prescriptions were written for U-500R alone (47.0%, group A) and concomitant U-500R/U-100 insulins (53.0%, group B). Concomitant oral antihyperglycemic agents (AHAs) and non-insulin injectable AHAs were used by 43.4% and 14.6% of patients, respectively. Following initiation of U-500R, mean HbA1c improved 0.68% in all patients (p<0.0001 compared with baseline), but the decrease in HbA1c did not differ significantly between groups (A: 0.78%; B: 0.60%). Overall, hypoglycemic events, largely captured in the outpatient setting, increased in incidence from 6.7% to 11.9% (p≤0.0001) and from 0.23 to 0.39 events/patient/year, an increase of 0.16 (p=0.003), from preindex to postindex.
Conclusions
This real-world outcomes analysis demonstrates that U-500R initiation is associated with a clinically meaningful improvement in glycemic control over the subsequent 12-month period with modest increase in incidence and rate of hypoglycemia.
Keywords: Glycemic Control, Management, Hypoglycemia, Insulin Resistance
Key messages.
This study describes the characteristics of patients initiating human regular U-500 insulin (U-500R) and their subsequent glycemic control in a real-world setting.
This real-world outcomes analysis demonstrates that U-500R initiation is associated with a clinically meaningful improvement in glycemic control over the subsequent 12-month period with modest increase in incidence and rate of hypoglycemia.
Following initiation of U-500R, mean glycated hemoglobin improved 0.68% in all patients (p<0.0001 compared with baseline).
Overall, hypoglycemic events, largely captured in the outpatient setting, increased in incidence from 6.7% to 11.9% (p≤0.0001) and from 0.23 to 0.39 events/patient/year, an increase of 0.16 (p=0.003), from preindex to postindex.
This is the first study to report the frequency of concomitant use of specific non-insulin injectables with U-500R.
Introduction
Human regular U-500 insulin (U-500R; Humulin R U-500; Eli Lilly and Company, Indianapolis, Indiana) became available in the USA in 1997 for patients with diabetes requiring high doses of insulin. U-500R is five times more concentrated than human regular U-100 insulin and contains 500 units of insulin per milliliter.1 The reduced volume of dosing with the U-500 concentration allows treatment of patients with severely insulin-resistant diabetes (mainly type 2 diabetes2–11) on total daily doses >200 units or >2 units/kg1 4 5 12 with often just 2 or 3 injections daily1 4–6 8 as compared with 5 to 8 injections a day with U-100 insulins. The pharmacokinetic (PK)/pharmacodynamic (PD) profile of U-500R has similar overall exposure and effect to human regular U-100 insulin in healthy obese participants, with a longer duration of action, but slightly lower peak insulin concentration and effect.13 This unique prandial and basal activity profile allows U-500R to be used as insulin monotherapy without concomitant U-100 basal insulins.8 13–15 With the rise in obesity and insulin-resistant patients with type 2 diabetes in the USA, prescriptions for U-500R increased 97% from August 2008 to September 2010.13 Currently, U-500R is licensed and available only in the USA; outside the USA, it is available only from the manufacturer on a named-patient basis in UK and elsewhere in the world, on a compassionate use basis.
A clinical review in 2013 by Jones and Idris7 of 10 published case series showed reduction in glycated hemoglobin (HbA1c) ranging from 1.0% to 2.8% in patients treated with U-500R mainly by multiple daily injections (MDI). Sample sizes of the case series were small (9–81 patients; total 317) with an average of 3–36 months of follow-up, and severe hypoglycemic events were uncommonly reported.7 A clinical review/meta-analysis by Reutrakul et al6 reported mean HbA1c reductions of 1.59% in nine case series of U-500R by MDI.6 Only one small (N=28) randomized controlled trial (RCT) of U-500R has been published, which reported significant HbA1c reduction (from baseline 9.2% to 7.5% at 24-week end point, p=0.0001) with no reported episodes of severe hypoglycemia when combined with metformin.15 A larger RCT (N=325) is currently in progress.16
In other real-world studies, U-500R has shown to be cost-saving when compared with high-dose U-100 regimens. A recently published study showed reduction in annualized pharmacy costs and lower overall healthcare costs for patients initiating U-500R as compared with a propensity-matched group utilizing >200 units/day of U-100 regimens.9 Compared with doses ≥150 units/day of U-100 insulin regimens, U-500R demonstrated a reduction in pharmacy costs but not overall healthcare costs.10 Both of these studies showed greater medication adherence for the U-500R cohorts.9 10 In addition, both studies showed higher incidence of hypoglycemia, although rates and costs associated with the hypoglycemic events were not different; however, the databases for both of these studies did not include parameters of efficacy (HbA1c).9 10
The objectives of this study were to describe the characteristics of patients initiating U-500R and to determine their subsequent glycemic control in a real-world setting.
Methods
A retrospective analysis was conducted using data from the Humedica electronic health record (EHR) database spanning the period from July 2007 through September 2011. The Humedica EHR database contains de-identified EHRs with prescription and practice management data from partnering with large medical practices, integrated delivery networks, and hospitals in the USA. Humedica EHR normalizes, validates, and aggregates the data within this database. Patient demographics including age, race, sex, residential region, and type of insurance coverage are also specifically included in the database. Laboratory results, physician notes, radiology, pathology, procedures, and diagnosis are stored as well. This study used diagnosis (International Classification of Diseases, Ninth Revision, Clinical Modification, ICD-9-CM) and procedure codes, and records for written prescriptions from the database. The index date of the study was defined as the date when U-500R was first prescribed to specific patients. All data were de-identified to comply with Health Insurance Portability and Accountability Act Regulations.
In order to be eligible for the study, participants were required to be ≥18 years of age at index with at least one diagnosis of type 1 or type 2 diabetes (250.xx). In addition, prescription records in the 6 months prior to the index date (date of first written U-500R prescription) and 12 months postindex were necessary, along with 12 months postindex date medical service information. A minimum of two HbA1c values, one preindex or on the index date, and the second in the postindex period, were required. Patients were excluded by diagnosis of secondary diabetes (249.xx) or gestational diabetes (648.8x) in either preindex or postindex.
Statistical methods
Baseline variables of the overall study population were summarized, including preindex demographics, comorbidities, and diabetes medication history. Missing and invalid data were excluded unless otherwise specified. Age was calculated as index date year minus birth year; if birth year was 1936 or earlier, it was set to be 1936. Missing or invalid body mass index (BMI) values (≤15 or ≥60) were dropped from the data. Non-numeric HbA1c values or those with units other than percent were also excluded. The frequencies of postindex antihyperglycemic agent (AHA) use (orals and non-insulin injectables) were calculated. The dates when prescriptions were written (but not filled nor refilled) were used to identify preindex and postindex treatment patterns from the prescription records data. Preindex and postindex HbA1c values, using the latest reading in each period, were determined overall. HbA1c values were evaluated by the combinations of age groups (less than 65 vs 65 years and over), and the presence or absence of comorbid cardiovascular disease (CVD) and/or nephropathy. ICD-9-CM-captured hypoglycemic events, as flagged by the Ginde algorithm,17 were assessed, along with the medical encounter on the episode date with the highest ‘severity’ (inpatient hospitalization>emergency visit>office/clinic visit). Paired t tests were used to measure the significance of the preindex to postindex change in HbA1c values, and the changes in incidence and rates of hypoglycemic events (number of events/patient/year), both overall and within each treatment group. Least squares means (LSM) analysis, adjusting for baseline values, was also used to evaluate the change in HbA1c values. The LSM approach is commonly used to estimate treatment effects controlling for certain covariates and accounting for differing sample sizes between the treatment groups.
Results
Preindex/baseline demographics and clinical characteristics are displayed in table 1. The U-500R cohort predominantly had type 2 diabetes (96.9%) and was 60.9% Caucasian, with mean age 56.8 years and 25.6% age ≥65 years of age. This cohort also had class 3 obesity (mean BMI 40.4 kg/m2), highly prevalent comorbidities (hypertension (86.5%), neuropathy (45.2%), nephropathy (42%), and CVD (39%)), and high Charlson Comorbidity Index (mean 3.5). Care involving endocrinologists was observed in less than half of the patients (43.1%). Very few patients in this database received U-500R via off-label continuous subcutaneous insulin infusion (CSII; postindex (n=4 (0.9%)), in contrast to an earlier study showed this to be common (25.4% postindex10)). Concomitant AHA prescriptions written in the 6-month preindex period are displayed in table 1, while the 12-month postindex concomitant AHA prescriptions written are shown in table 2. During the preindex period, 38.2% of patients received written prescriptions for oral AHAs, predominantly as metformin (28.8%) with a smaller proportion of non-insulin injectable AHAs (7.6%; table 1), both of which increased during the postindex period (metformin to 33.0% and non-insulin injectable AHAs to 14.6%; table 2).
Table 1.
Demographic and clinical characteristics of patients at the preindex period or at index
| Patients (N) | 445 |
| Age (mean±SD) | 56.8±10.9 |
| <65 (n (%)) | 331 (74.4) |
| ≥65 (n (%)) | 114 (25.6) |
| BMI* (n (mean±SD)) | 360 (40.4±7.5) |
| Charlson Comorbidity Index† (mean±SD) | 3.5±2.3 |
| Type 1 (n (%)) | 14 (3.2) |
| Type 2 (n (%)) | 431 (96.9) |
| Gender (n (%)) | |
| Male | 234 (52.6) |
| Female | 211 (47.4) |
| Region (n (%)) | |
| Midwest | 234 (52.6) |
| Northeast | 67 (15.1) |
| South | 80 (18.0) |
| West | 64 (14.4) |
| Insurance type at index (n (%)) | |
| Commercial | 102 (22.9) |
| Dual Medicare/Medicaid | 1 (0.2) |
| Medicaid | 2 (0.5) |
| Medicare | 76 (17.1) |
| Other/unknown | 257 (57.8) |
| Uninsured | 7 (1.6) |
| Race (n (%)) | |
| Caucasian | 271 (60.9) |
| African–American | 61 (13.7) |
| Asian | 3 (0.7) |
| Other/unknown | 110 (24.7) |
| Index insulin prescriber specialty (n (%)) | |
| Endocrinology | 192 (43.1) |
| Primary care (internal medicine, family medicine, nurse practitioner) | 37 (8.3) |
| Other (pharmacy, pulmonary, nephrology) | 102 (22.9) |
| Missing | 114 (25.6) |
| Prescribed oral AHAs‡ (n (%)) | 170 (38.2) |
| Metformin | 128 (28.8) |
| Sulfonylurea | 51 (11.46) |
| DPP-4 | 16 (3.6) |
| TZD | 35 (7.9) |
| Other | 3 (0.7) |
| Prescribed insulin‡ n (%) | 322 (72.4) |
| Prescribed CSII‡ n (%) | 4 (0.9) |
| Prescribed noninsulin injectable AHAs‡ n (%) | 34 (7.6) |
| Pramlintide | 20 (4.5) |
| GLP-1 receptor agonists | 12 (2.7) |
| Unknown class | 3 (0.7) |
| Comorbidities and complications during preindex and postindex periods n (%) | |
| Hypertension | 385 (86.5) |
| Neuropathy | 201 (45.2) |
| Nephropathy | 187 (42.0) |
| Cardiovascular | 175 (39.3) |
| Depression | 98 (22.0) |
| Retinopathy | 61 (13.7) |
| Cerebrovascular | 39 (8.8) |
| Bariatric surgery | 1 (0.2) |
| Lower limb amputation | 6 (1.4) |
*Entire study period, used latest.
†Entire study period.
‡6 months preindex period.
AHA, antihyperglycemic agents; BMI, body mass index; CSII, continuous subcutaneous insulin infusion; DPP-4, dipeptidyl peptidase-4 inhibitor; GLP-1, glucagon-like peptide 1; n, number of patients; TZD, thiazolidinedione.
Table 2.
Postindex prescription information (12 months)
| Prescribed antihyperglycemic medications | n (%) |
|---|---|
| Oral AHA | 193 (43.4) |
| Metformin | 147 (33.0) |
| Sulfonylurea | 46 (10.3) |
| DPP-4 | 17 (3.8) |
| TZD | 34 (7.6) |
| Other | 3 (0.7) |
| Non-insulin injectable AHA | 65 (14.6) |
| GLP-1 receptor agonists | 15 (3.4) |
| Pramlintide | 50 (11.2) |
| Unknown | 2 (0.5) |
| Insulin (group) | |
| U-500R only (group A) | 209 (47.0) |
| U-500R with overlapping U-100 (group B) | 236 (53.0) |
AHA, antihyperglycemic agents; DPP-4, dipeptidyl peptidase-4 inhibitor; GLP-1, glucagon-like peptide 1; n, number of patients; TZD, thiazolidinedione.
Treatment groups of interest were identified by written prescriptions of U-500R in postindex (table 2) as follows: group A: U-500R was the only insulin written postindex (47.0%) and group B: overlapping U-500R and U-100 prescriptions were written during the postindex (53.0%). Of those utilizing U-500R overlapping with U-100 in the postindex, 75% of the U-100 use was prandial (rapid-acting analogs/human regular), 56% basal (glargine or detemir) or intermediate-acting (human neutral protamine Hagedorn), 12% premixed, and 18% unspecified.
Overall the mean baseline HbA1c was 9.2±1.7%. HbA1c levels during the preindex and postindex periods, stratified by overall, groups A and B, age, CVD, and nephropathy are shown in table 3. HbA1c levels adjusted for baseline HbA1c fell by 0.68±1.6% for the overall study group (p<0.0001). LSM change in HbA1c from preindex to postindex, adjusted for baseline values, was −0.78±1.5% for group A and −0.60±1.7% for group B (p<0.0001 for both compared with baseline; NS (p=0.175) between groups). Overall, the number of patients with HbA1c over 9% decreased from 207 (47%) in the preindex to 134 (30%) in the postindex period (p<0.0001). Percentage of patients reaching target values <8%, <7.5%, and <7% also significantly improved (p<0.0001 for all) from the preindex to postindex period (figure 1).
Table 3.
Change in HbA1c by treatment group, age, cardiovascular disease and nephropathy
| Treatment group | n | Pre-HbA1c (mean±SD) | Post-HbA1c (mean±SD) | Change*† |
|---|---|---|---|---|
| U-500R only (group A) | 209 | 9.2±1.6 | 8.4±1.4 | −0.78±1.50 |
| U-500R with overlapping U-100 (group B) | 236 | 9.2±1.9 | 8.6±1.9 | −0.60±1.74 |
| Overall | 445 | 9.2±1.7 | 8.5±1.7 | −0.68±1.63 |
| Age group (years) | ||||
| <65 | 331 | 9.4±1.7 | 8.7±1.8 | −0.67±1.66 |
| ≥65 | 114 | 8.6±1.6 | 7.9±1.3 | −0.71±1.56 |
| Cardiovascular disease | ||||
| Yes | 175 | 9.1±1.7 | 8.4±1.7 | −0.68±1.63 |
| No | 270 | 9.2±1.8 | 8.5±1.7 | −0.68±1.64 |
| Nephropathy | ||||
| Yes | 187 | 9.1±1.6 | 8.5±1.8 | −0.55±1.62 |
| No | 258 | 9.3±1.8 | 8.5±1.6 | −0.78±1.64 |
*Unadjusted p values are all p<0.0001, compares endpoint HbA1c with baseline HbA1c values.
†LS mean changes±SE, adjusted for baseline HbA1c values.
Group A, −0.78±0.10; group B, −0.60±0.09 (p=0.175).
<65 years, −0.58±0.08; ≥65 years, −0.98±0.13 (p=0.011).
Cardiovascular disease=yes, −0.72±0.10; no, −0.66±0.09 (p=0.665).
Nephropathy=yes, −0.60±0.10; no, −0.74±0.09 (p=0.322).
HbA1c, glycated hemoglobin; LS, least squares; n, number of patients.
Figure 1.
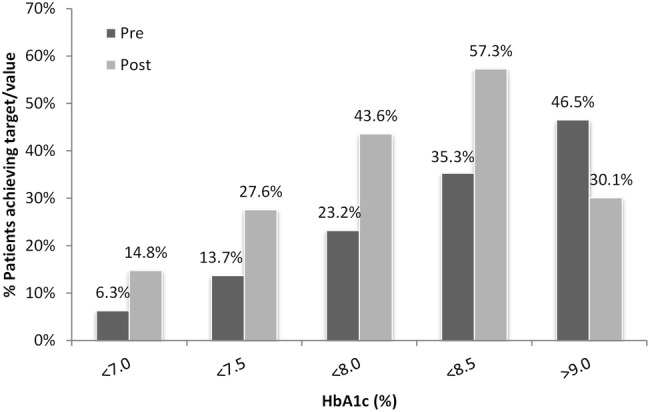
Attainment of glycated hemoglobin (HbA1c) targets/values preindex and postindex in overall study population (N=445, all p<0.0001).
The incidence and rates of hypoglycemic events are displayed in table 4. Overall, there were more hypoglycemic events in the postperiod (175 events in 53 patients over 12 months) than in the 6-month preindex (52 events in 30 patients). The incidence of patients having at least one hypoglycemic event postindex in group A versus group B was similar (12.4% vs 11.4%; p=0.745), while the incidence at baseline was somewhat lower in group A versus group B (4.8% vs 8.5%; p=0.121). Hypoglycemic events did not appear significantly different between the first 6 months postindex versus the last 6 months between cohorts. The annualized rate of hypoglycemic events per patient per year was 0.23 in the preindex period and 0.39 in the postindex period, an overall increase of 0.16 events per patient per year (p=0.003). In the two treatment groups, the hypoglycemia rate (events per patient per year) increased by 0.15 (p=0.021) and 0.17 (p=0.051), in groups A and B, respectively, from preindex to postindex.
Table 4.
Hypoglycemic events
| Hypoglycemic events and rates preindex and postindex by treatment group*† |
||||||||
|---|---|---|---|---|---|---|---|---|
| Treatment | Preindex rate‡ n (mean±SD) | 0–6 month postindex rate‡ n (mean±SD) | 0–6 month postindex versus preindex | 7–12 month postindex rate‡ n (mean±SD) | 7–12 month postindex versus preindex | 0–12 month postindex rate‡ n (mean±SD) | Change in annual rate (mean±SD) | 0–12 month postindex versus preindex |
| U-500R only (group A) | 16 (0.15±0.77) | 34 (0.33±1.23) | p=0.026 | 30 (0.29±1.00) | p=0.071 | 64 (0.31±0.99) | 0.15±0.95 | p=0.021 |
| U-500R with overlapping U-100 (group B) | 36 (0.31±1.23) | 57 (0.48±2.23) | p=0.062 | 54 (0.46±2.28) | p=0.199 | 111 (0.47±2.0) | 0.17±1.29 | p=0.051 |
| Total | 52 (0.23±1.04) | 91 (0.41±1.83) | p=0.005 | 84 (0.38±1.80) | p=0.045 | 175 (0.39±1.61) | 0.16±1.14 | p=0.003 |
| Group A versus group B | p=0.124 | p=0.364 | NA | p=0.318 | NA | p=0.284 | p=0.911 | NA |
| Patients with at least 1 hypoglycemic event in preindex or postindex |
|||||||
|---|---|---|---|---|---|---|---|
| Treatment | preindex n (%) | 0–6 month postindex n (%) | 0–6 month postindex versus preindex | 7–12 month postindex n (%) | 7–12 month postindex versus preindex | 0–12 month postindex n (%) | 0–12 month postindex versus preindex |
| U-500R only (group A) | 10 (4.8) | 19 (9.1) | p=0.0005 | 19 (9.1) | p=0.0005 | 26 (12.4) | p=0.007 |
| U-500R with overlapping U-100 (group B) | 20 (8.5) | 23 (9.8) | p<0.0001 | 17 (7.2) | p<0.0001 | 27 (11.4) | p<0.0001 |
| Total | 30 (6.7) | 42 (9.4) | p<0.0001 | 36 (8.1) | p<0.0001 | 53 (11.9) | p<0.0001 |
| Group A versus group B | p=0.121 | p=0.814 | NA | p=0.466 | NA | p=0.745 | NA |
| Hypoglycemic events in preindex or postindex by visit type/setting |
||||
|---|---|---|---|---|
| Visit type | Preindex n (%) | 0–6 month postindex n (%) | 7–12 month postindex n (%) | 0–12 month postindex n (%) |
| Office or clinic | 40 (76.9) | 80 (87.9) | 72 (85.7) | 152 (86.9) |
| Emergency | 3 (5.8) | 1 (1.1) | 2 (2.4) | 3 (1.7) |
| Inpatient | 5 (9.6) | 7 (7.7) | 7 (8.3) | 14 (8.0) |
| Other | 1 (1.9) | 1 (1.1) | 2 (2.4) | 3 (1.7) |
| Not recorded/missing | 3 (5.8) | 2 (2.2) | 1 (1.2) | 3 (1.7) |
*Total: N=445; group A: n=209; group B: n=236.
†No hypoglycemic coma events were captured.
‡Annualized rate=hypoglycemic events per patient per year.
NA, not applicable; N/n, number of patients.
Discussion
Limited real-world data exist on the efficacy and safety of U-500R therapy in patients in a large-scale naturalistic setting. Two recent studies focused on healthcare resource utilization,9 costs and adherence9 10 with propensity-matched high-dose U-100 insulin-treated cohorts compared with U-500R-treated cohorts. Both studies reported higher incidence of ICD-9-CM-coded hypoglycemic events with U-500R, although the rate and costs associated with the hypoglycemic events were no different between U-500R and U-100 insulin use.9 10 Since the respective databases for those studies did not include HbA1c values, comparison of postindex glycemic control between the U-500R and U-100 cohorts was not possible, and this information is needed to interpret the comparative hypoglycemia data.
The current real-world study of U-500R use is the first to analyze HbA1c data over time in addition to detailed baseline prescription and hypoglycemia data. The Humedica EHR database was able to capture 445 unique patients meeting entry criteria for preindex and postindex periods. Although this number is smaller than the number of propensity-matched pairs from the two previous real-world studies (6849 and 1039,10 respectively), it is close to the total number of U-500R-treated patients reported in the world's literature of published case series (N=524; most retrospective; combining MDI series4 6 7 18 with off-label CSII use4 6 7 19 20 and use in pregnancy21). The overall HbA1c reduction of 0.68% in this cohort is statistically and clinically significant, but is less than that reported in the clinical case series (1.0–3.5%4 6 7 18–20) and from the single RCT (1.0–1.7%).15 However, this is not surprising since the prior clinical reports were conducted by investigators/institutions with particular clinical experience with use and titration of U-500R over time, thus likely representing more expert use than that captured by the Humedica EHR database for all U-500R use during the study period, within the prespecified study parameters. In addition, mean baseline HbA1c values for this study population were lower (9.1±1.7%) than in the reported case series (weighted mean HbA1c 10.0%4).
The challenges of treating severely insulin-resistant patients with diabetes are well recognized by the American Diabetes Association and the European Association for the Study of Diabetes (EASD) which recommend individualized HbA1c goals of 7.5–8.0% or even higher when intensive self-management education, repeated counseling and effective doses of multiple antihyperglycemic medications are ineffective, particularly in patients with multiple comorbidities22 and patients requiring U-500R for high-dose therapy.23 In this study, the percentage of patients achieving HbA1c <7.5% significantly increased from 13.7% to 27.6% and <8.0% rose from 23.2% to 43.6% (figure 1; p<0.0001 for both from preindex to postindex).
Although U-500R therapy with concomitant use of basal or prandial U-100 insulin has been advocated for by some,3 18 24 most case series have reported use of U-500R by itself2 4–6 consistent with reported PK/PD prandial and basal characteristics of U-500R.13 The two RCTs of U-500R also had algorithms using U-500R as insulin monotherapy.15 16 This study is unique in being able to differentiate reduction in HbA1c postindex between those with U-500R use alone (group A; 0.78%) as compared with concomitant U-500R and U-100 therapy (group B; 0.60%) although groups A and B were not statistically different (table 3). U-500R insulin monotherapy may also reduce the risk of dosing errors and confusion that might arise from concomitant use of non-dedicated U-100 insulin syringes or volumetric syringes for U-500R and U-100 insulins.1 4 5 7 8 Owing to the limitations in the database, this analysis was unable to evaluate the total daily dose and frequency of dosing for the insulins prescribed to help shed light into these prescribing patterns. Additionally, this database does not contain all of the patients’ clinical information (eg, self-monitoring blood glucose diary entries) that physicians would use when determining the choice of medications to prescribe.
The American Diabetes Association, EASD, American Association of Clinical Endocrinologists, and The Endocrine Society position statements and publications22 23 25 26 emphasize the importance of avoidance of hypoglycemia, particularly severe hypoglycemia, in insulin-treated patients with type 2 diabetes. Although the incidence and rate of hypoglycemic events did increase in our U-500R cohorts postindex, the clinical setting of these events was predominately outpatient, and may have been mild or moderate in severity. Certainly, improved glycemic control (to postindex mean HbA1c values of 8.4% and 8.6%, respectively, in groups A and B) would be expected to increase the occurrence of hypoglycemia. The glycemic efficacy in our cohort, although novel, does not help to provide understanding of the higher incidence of hypoglycemia (setting not specified) observed in the propensity-matched U-500R versus U-100 insulin cohorts of the recent naturalistic studies9 10 since we were not able to assess a matched cohort treated only with U-100 insulins in this database. Severe hypoglycemia has occasionally been reported in clinical case series11 19 21 24 with no reports in others18 27–29 and no severe hypoglycemia in the recent U-500R RCT.15 One case series (N=53) reported eight episodes of severe hypoglycemia occurring in six patients.11 Severe hypoglycemia rate was reported as 0.1 episode per patient-year in one case series of U-500R by CSII (20; N=59). A recent case series reported an increase in mild hypoglycemia from 13.0% prior to U-500R to 42.0% after initiation of U-500R therapy.27 Some studies have reported more episodes of mild hypoglycemia in the early period after initiation of U-500R;15 28 however, our analysis did not show any difference between the early and later postindex period (table 4). In the current study, there were no episodes of severe hypoglycemia accompanied by hypoglycemic coma. Higher adherence observed with U-500R therapy compared with high-dose U-100 insulin could contribute to more hypoglycemia.9 10 Combining oral secretagogues (sulfonylureas or glinides) with insulin is known to increase hypoglycemia,22 25 26 and it is important to note that 11% of the U-500R cohort from this study were also co-treated with sulfonylureas in addition to U-500R therapy (still over 9% postindex) which may also reflect a lack of experience by prescribers in this database.
This study adds to the clinical understanding of U-500R-treated patient characteristics and demographics previously reported in clinical and naturalistic studies.2–10 This is the first study to differentiate between concomitantly used non-insulin injectable AHAs with U-500R, with the finding of more preindex and postindex concomitant use of the amylin agonist, pramlintide, than use of glucagon-like peptide-1 receptor agonists (GLP-1 RAs; tables 1 and 2). Off-label combined use of pramlintide with U-500R has rarely been discussed in the literature,30 although concomitant use of U-500R with GLP-1 RAs has been reported.15 29 31 32 A retrospective observational study by Lane et al29 showed a decrease in HbA1c by 1.4%, total daily insulin dose by 28%, and weight loss of 5.1 kg after 12 weeks of liraglutide added to U-500R therapy in patients with insulin-resistant type 2 diabetes. Combined use of U-500R and GLP-1 RAs is also not FDA-approved in the USA.
Some limitations apply to this study. As mentioned earlier, this analysis could not use propensity matching to comparably dosed U-100 insulin patients due to inability to verify total daily insulin dose. This study was unable to determine if the patient actually took U-500R; the data extracted from the EHR only confirm that the prescription was written, and as such, even though our data revealed that 28% of the patients did not have U-100 insulin prescriptions written in the pre-period, we do not believe it meant that concentrated insulin was the first insulin for all of those patients. It is possible that patients had prescriptions written prior to our data collection window with refills that would extend into our pre-period, or that patients did not obtain prescriptions for U-100 insulins prior to U-500R initiation. In addition, insulin prescription refill and dosage information records were inconsistent and often missing within these EHR data. Accordingly, the adherence or persistence of patients to treatment could not be accurately determined. The index periods were not the same duration, preindex; 6 months and postindex; 12 months, possibly falsely elevating the assessment of comorbidities and prescriptions written in the postperiod. In previous studies using the Truven MarketScan database, patients were identified using ICD-9-CM codes associated with hypoglycemia (likely representing major hypoglycemia) or diabetes with specified manifestations, thus there was a greater incidence of hypoglycemia in U-500R than with U-100 insulins, but neither study included assessment of glycemic efficacy.9 10 The current study using Humedica EHR database identified hypoglycemic events used the Ginde algorithm, which has only been validated for use with claims databases and not EHR databases.17 Additionally these events could not be confirmed with blood glucose values within the Humedica EHR database, and capture of hypoglycemia by ICD-9-CM codes is likely to under-report the true incidence. As aforementioned, the Humedica EHR database could not differentiate clearly between patients who took concomitant U-500R/U-100 insulins and those who might have switched back to U-100 insulins from U-500R during the postindex period, a practice that has been reported in prior case series.3 4 In the future, efficacy and safety analyses of these further subgroups would be of clinical interest.
This real-world outcome analysis demonstrates that initiation of U-500R is associated with a clinically meaningful improvement in glycemic control among all study patients (0.68% decrease in HbA1c) over the subsequent 12-month period. Future studies are planned using databases that hopefully will allow detailed assessment of glycemic efficacy along with dosing information (total daily doses and frequency of administration and dosing regimens), safety parameters of hypoglycemia and changes in weight and BMI, and patient adherence over time to address remaining gaps in better understanding clinical use of U-500R.
Acknowledgments
The authors thank Karen Sprague, MPH for assistance with the preparation of the manuscript.
Footnotes
Contributors: ELE, BHC, and JAJ researched data and wrote manuscript. SCG performed statistical analysis and contributed to manuscript. RCH, II, ALP, and RMB contributed to discussion and reviewed manuscript.
Competing interests: This work was sponsored by Eli Lilly and Company. BHC, SCG, and JAJ are full-time employees and are minor stockholders of Eli Lilly and Company. ELE is a former employee of Eli Lilly and Company. II has received research support from Eli Lilly and Company and has served as a consultant for and is on the speakers’ bureaus of Eli Lilly and Company and Merck Sharpe Dohme. ALP has served as a consultant and speaker for Eli Lilly and Company, Novo Nordisk, Sanofi-Aventis, Bristol-Myers Squibb, and AstraZeneca. RCH has served as a consultant for and received research support from Eli Lilly and Company and Novo Nordisk, serves on the advisory boards for Eli Lilly and Takeada and is on the speakers’ bureaus of Eli Lilly and Company, Novo Nordisk, AstraZeneca, Boehringer Ingelheim, Glaxco Smith Kline, Janssen, and Takeda. RMB has served on a scientific advisory board, consulted or performed clinical research with Abbott Diabetes Care, Amylin, Bayer, Becton Dickinson, Intuity, Calibra, DexCom, Eli Lilly, Halozyme, Helmsley Trust, Hygieia, Johnson & Johnson, Medtronic, Merck, the National Institute of Health, Novo Nordisk, ResMed, Roche, Sanofi, and Takeda. His employer, Park Nicollet Health Services, has contracts with the listed companies for his services. RMB has inherited Merck stock, and has been a volunteer officer of the American Diabetes Association.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All analysis results in support of this submission, whether explicitly included in the submission or not, will be retained by Eli Lily and Company.
References
- 1. Humulin® R regular U-500 [package insert]. Indianapolis, IN: Eli Lilly and Company, 2014. http://pi.lilly.com/us/humulin-r-u500-pi.pdf.
- 2.Cochran E, Musso C, Gorden P. The use of U-500 in patients with extreme insulin resistance. Diabetes Care 2005;28:1240–4. 10.2337/diacare.28.5.1240 [DOI] [PubMed] [Google Scholar]
- 3.Garg R, Johnston V, McNally PG et al. U-500 insulin: why, when and how to use in clinical practice. Diabetes Metab Res Rev 2007;23:265–8. 10.1002/dmrr.709 [DOI] [PubMed] [Google Scholar]
- 4.Lane WS, Cochran EK, Jackson JA et al. High-dose insulin therapy: is it time for U-500 insulin? Endocr Pract 2009;15:71–9. 10.4158/EP.15.1.71 [DOI] [PubMed] [Google Scholar]
- 5.Segal AR, Brunner JE, Burch FT et al. Use of concentrated insulin human regular (U-500) for patients with diabetes. Am J Health Syst Pharm 2010;67:1526–35. 10.2146/ajhp090554 [DOI] [PubMed] [Google Scholar]
- 6.Reutrakul S, Wroblewski K, Brown RL. Clinical use of U-500 regular insulin: review and meta-analysis. J Diabetes Sci Technol 2012;6:412–20. 10.1177/193229681200600229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones P, Idris I. The use of U-500 regular insulin in the management of patients with obesity and insulin resistance. Diabetes Obes Metab 2013;15:882–7. 10.1111/dom.12094 [DOI] [PubMed] [Google Scholar]
- 8.Cochran EK, Valentine V, Samaan KH et al. Practice tips and tools for the successful use of U-500 regular human insulin: the diabetes educator is key. Diabetes Educ 2014;40:153–65. 10.1177/0145721713508822 [DOI] [PubMed] [Google Scholar]
- 9.Eby EL, Wang P, Curtis BH et al. Cost, healthcare resource utilization, and adherence of individuals with diabetes using U-500 or U-100 insulin: a retrospective database analysis. J Med Econ 2013;16:529–38. 10.3111/13696998.2013.772059 [DOI] [PubMed] [Google Scholar]
- 10.Eby EL, Zagar AJ, Wang P et al. Healthcare costs and adherence associated with human regular U-500 versus high-dose U-100 Insulin in patients with diabetes. Endocr Pract 2014;20:663–70. 10.4158/EP13407.OR [DOI] [PubMed] [Google Scholar]
- 11.Ziesmer AE, Kelly KC, Guerra PA et al. U-500 regular insulin use in insulin resistant type 2 diabetic veteran patients. Endocr Pract 2012;18:34–8. 10.4158/EP11043.OR [DOI] [PubMed] [Google Scholar]
- 12.Ovalle F. Clinical approach to the patient with diabetes mellitus and very high insulin requirements. Diabetes Res Clin Pract 2010;90:231–42. 10.1016/j.diabres.2010.06.025 [DOI] [PubMed] [Google Scholar]
- 13.de la Peña A, Riddle M, Morrow LA et al. Pharmacokinetics and pharmacodynamics of high-dose human regular U-500 insulin versus human regular U-100 insulin in healthy obese subjects. Diabetes Care 2011;34:2496–501. 10.2337/dc11-0721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de la Peña A, Ma X, Reddy S et al. Application of PK/PD modeling and simulation to dosing regimen optimization of high-dose human regular U-500 insulin. J Diabetes Sci Technol 2014;8:821–9. 10.1177/1932296814532326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Distiller LA, Nortje H, Wellmann H et al. A 24-week, prospective, randomized, open-label, treat-to-target pilot study of obese type 2 diabetes patients with severe insulin resistance to assess the addition of exenatide on the efficacy of u-500 regular insulin plus metformin. Endocr Pract 2014;20:1143–50. 10.4158/EP14067.OR [DOI] [PubMed] [Google Scholar]
- 16.NIH Clinical Trials Study Record Detail. US National Institutes of Health website: http://clinicaltrials.gov/show/NCT01774968 (accessed 3 Mar 2014).
- 17.Ginde AA, Blanc PG, Lieberman RM et al. Validation of ICD-9-CM coding algorithm for improved identification of hypoglycemia visits. BMC Endocr Disord 2008;8:4 10.1186/1472-6823-8-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lowery JB, Donihi AC, Korytkowski MT. U-500 insulin as a component of basal bolus insulin therapy in type 2 diabetes. Diabetes Technol Ther 2012;14:505–7. 10.1089/dia.2011.0248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lane WS, Weinrib SL, Rappaport JM et al. A prospective trial of U500 insulin delivered by OmniPod in patients with type 2 diabetes mellitus and severe insulin resistance. Endocr Pract 2010;16:778–84. Erratum in: Endocr Prac. 2010;16:1082 10.4158/EP10014.OR [DOI] [PubMed] [Google Scholar]
- 20.Lane WS, Weinrib SL, Rappaport JM et al. The effect of long-term use of U-500 insulin via continuous subcutaneous infusion on durability of glycemic control and weight in obese, insulin-resistant patients with type 2 diabetes. Endocr Pract 2013;19:196–201. 10.4158/EP12226.OR [DOI] [PubMed] [Google Scholar]
- 21.Mendez-Figueroa H, Maggio L, Dahlke JD et al. Treatment of severe insulin resistance in pregnancy with 500 units per milliliter of concentrated insulin. Obstet Gynecol 2013;122:99–104. 10.1097/AOG.0b013e3182978a11 [DOI] [PubMed] [Google Scholar]
- 22.Inzucchi SE, Bergenstal RM, Buse JB et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012;35:1364–79. 10.2337/dc12-0413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Inzucchi SE, Bergenstal RM, Buse JB et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2015;38:140–9. 10.2337/dc14-2441 [DOI] [PubMed] [Google Scholar]
- 24.Davidson MB, Navar MD, Echeverry D et al. U-500 regular insulin:clinical experience and pharmacokinetics in obese, severely insulin-resistant type 2 diabetic patients. Diabetes Care 2010;33:281–3. 10.2337/dc09-1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garber AJ, Abrahamson MJ, Barzilay JI et al. American Association of Clinical Endocrinologists’ comprehensive diabetes management algorithm 2013 consensus statement: executive summary. Endocr Pract 2013;15:540–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seaquist ER, Anderson J, Childs B et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care 2013;36:1384–95. 10.2337/dc12-2480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boldo A, Comi RJ. Clinical experience with U500: risks and benefits. Endocr Pract 2012;18:56–61. 10.4158/EP11163.OR [DOI] [PubMed] [Google Scholar]
- 28.Dailey AM, Gibert JA, Tannock LR. Durability of glycemic control using U-500 insulin. Diabetes Res Clin Pract 2012; 95:340–4. 10.1016/j.diabres.2011.10.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lane W, Weinrib S, Rappaport J. The effect of liraglutide added to U-500 insulin in patients with type 2 diabetes and high insulin requirements. Diabetes Technol Ther 2011;13:592–5. 10.1089/dia.2010.0221 [DOI] [PubMed] [Google Scholar]
- 30.Valentine V. Don't resist using U-500 insulin and pramlintide for severe insulin resistance. Clin Diabetes 2012;30:80–4. 10.2337/diaclin.30.2.80 [DOI] [Google Scholar]
- 31.Balena R, Hensley IE, Miller S et al. Combination therapy with GLP-1 receptor agonists and basal insulin: a systematic review of the literature. Diabetes Obes Metab 2012;15: 485–502. 10.1111/dom.12025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pantalone KM, Faiman C. Liraglutide effective in the severely insulin-resistant patient with type 2 diabetes requiring U-500 insulin: a case report. Diabetes Technol Ther 2013;15:1–2. 10.1089/dia.2012.0328 [DOI] [PubMed] [Google Scholar]


