Abstract
Background
Magnesium supplementation has previously shown reductions in blood pressure of up to 12 mmHg. A positive relationship between magnesium supplementation and performance gains in resistance exercise has also been seen. However, no previous studies have investigated loading strategies to optimise response. The aim of this study was to assess the effect of oral magnesium supplementation on resistance exercise and vascular response after intense exercise for an acute and chronic loading strategy on a 2-day repeat protocol.
Methods
The study was a randomised, double-blind, cross-over design, placebo controlled 2 day repeat measure protocol (n = 13). Intense exercise (40 km time trial) was followed by bench press at 80% 1RM to exhaustion, with blood pressure and total peripheral resistance (TPR) recorded. 300 mg/d elemental magnesium was supplemented for either a 1 (A) or 4 (Chr) week loading strategy. Food diaries were recorded.
Results
Dietary magnesium intake was above the Reference Nutrient Intake (RNI) for all groups. Bench press showed a significant increase of 17.7% (p = 0.031) for A on day 1. On day 2 A showed no decrease in performance whilst Chr showed a 32.1% decrease. On day 2 post-exercise systolic blood pressure (SBP) was significantly lower in both A (p = 0.0.47) and Chr (p = 0.016) groups. Diastolic blood pressure (DBP) showed significant decreases on day 2 solely for A (p = 0.047) with no changes in the Chr. TPR reduced for A on days 1 and 2 (p = 0.031) with Chr showing an increase on day 1 (p = 0.008) and no change on day 2.
Conclusion
There was no cumulative effect of Chr supplementation compared to A. A group showed improvement for bench press concurring with previous research which was not seen in Chr. On day 2 A showed a small non-significant increase but not a decrement as expected with Chr showing a decrease. DBP showed reductions in both Chr and A loading, agreeing with previous literature. This is suggestive of a different mechanism for BP reduction than for muscular strength. TPR showed greater reductions with A than Chr, which would not be expected as both interventions had reductions in BP, which is associated with TPR.
Keywords: Magnesium supplementation, Blood pressure, Bench press, Acute and chronic loading
Background
Magnesium (Mg2+) elicits significant enzymatic cellular involvement and physical regulation such as energy metabolism/production through formation of the Mg-ATP complex [1] and physiological regulation and control of neuromuscular cardiac activity, muscular contraction, vascular tone and blood pressure [2,3]. Its effect on muscular contraction and vascular tone have been shown to reduce blood pressure and subsequently vascular resistance [4].
Nutritional supplementation is a well-established method for enhancing performance in conjunction to training. Micronutrient intake has been highlighted to have gained greater prominence with athletes in relation to the importance of an adequate nutritional status [5], However, previous research highlights nutritional inadequacies and thus an impaired nutritional status (i.e. marginal nutrient deficiency) from both an athletic [5] and general population perspective [6]. This identifies physical activity as increasing the rate at which micronutrients are utilised, promoting excessive micronutrient loss via increased catabolism and excretion (sweat and urine). Magnesium is a mineral required at rest and during exercise [7]. This increase in Mg2+ turnover during exercise may lead to a state of insufficiency acting as a contributory factor towards an increase in blood pressure and a state of hypertension [8]. This, together with a decline in dietary intake below the RNI may have a negative impact on both performance and blood pressure.
Magnesium supplementation in relation to exercise has differed considerably in research opinion as to the dose and type of Mg2+ salt administered. It is influenced by the specific anion attachment with Mg2+, thus influencing supplemental solubility, elemental Mg2+ bioavailability and supplemental effectiveness [9]. Research has illustrated organic forms of Mg2+ supplementation i.e. Aspartate, citrate, lactate, pidolate, fumurate, acetate, ascorbate and gluconate to exemplify a greater solubility and bioavailability in comparison to inorganic forms i.e. oxide, sulphate, chloride and carbonate [10] When considered relative to the quantity needed to be ingested to release 300 mg of elemental Mg2+ along with the fact that certain magnesiums are unavailable in the UK, magnesium citrate was considered to be the best option for this protocol.
Research to date consists of both positive [11-13] and negative [14,15] findings. The research appears to agree that Mg2+ supplementation has no effect on physical performance when serum concentrations are within the normal range (serum Mg2+ 0.8-1.2 mmol·L−1) [12,16]. However, manipulating intakes of Mg2+ by diet or supplementation has been shown to have performance [11,17] and blood pressure enhancements [13,18]. Limitations to many of these studies is the lack of information regarding either serum magnesium or dietary intake [19]. The general consensus appears to be that Mg2+ supplementation has a greater effect when habitual dietary intake or serum levels are low.
Further, to the best of the authors’ knowledge research to date lacks analysis of Mg2+ from an acute (A) and chronic (Chr) viewpoint within the same study. Therefore, the aim of the current study was to assess the effect of oral Mg2+ supplementation on strength performance and vascular responses from both an A and Chr loading strategy as to establish potential differences in supplemental duration and influences of dietary status and supplemental dose on performance and vascular responses.
Methods
Subjects
A total of 13 subjects (males (m) = 7 females (f) = 6) were recruited from recreational running, cycling and triathlete clubs. Six subjects were allocated randomly to the acute intervention group (m = 3, f = 3) and 7 to the chronic intervention group (m = 4, f = 3). Subjects were recruited in accordance to meeting the inclusion/exclusion criteria, (Table 1). Informed consent and health screen were completed and ethical approval was granted by the University of Hertfordshire School of Life Sciences Ethics Committee.
Table 1.
Subject characteristics; including group sample size (n), age, height, weight, VO 2max , HR max
| Chronic | Acute | |
|---|---|---|
| N | 7 | 6 |
| Age (years) | 40.8 ± 4.4 | 35.8 ± 6.2 |
| Height (cm) | 176.2 ± 11 | 174.6 ± 12 |
| Weight (kg) | 73.2 ± 13.2 | 72.1 ± 13 |
| VO2max (ml/kg) | 51.8 ± 9.1 | 53 ± 4.8 |
| HRmax (bpm) | 176.4 ± 3.8 | 180.8 ± 7.7 |
Values are mean ± SD.
Experimental design
The study was a randomised, cross-over, double-blind, placebo controlled, 2 day repeated measure protocol. Subjects were assigned to either the acute or chronic intervention and the two trials ran parallel. Within each trial subjects undertook both the magnesium intervention and a placebo intervention with a one week washout period in a randomised order. The two interventions were a chronic (Chr) (4 weeks) and acute (A) (1 week) loading strategy, sub-divided into a supplemental and a placebo control group with a 1 week washout period. A maximal graded exercise test for determination of VO2max was conducted to ensure participant homogeneity with a cut off of 45 ml/kg−1 and 35 ml/kg−1 oxygen for males and females respectively. The study was tested across 2 consecutive days at each treatment time-point i.e. baseline and again after either 1 or 4 weeks intervention. A one week washout was then given and then a further intervention of the opposite treatment was given (placebo or magnesium) with the same loading phase.
Protocol
After familiarisation, subjects were tested for baseline measurements Anthropometric measures (height (cm), weight (kg)) and age (y)) were recorded. All subjects attended a familiarisation session on all equipment and testing protocols prior to testing. On both day 1 and recovery day 2 participants completed a 40 km time trial on bicycles owned by the subjects and set onto a rig. A set 40 km flat course with no wind setting was used on a Computrainer Pro ergometer (Computrainer, Seattle). All on-screen course data information was blinded, verbal encouragement was not given during the exercise testing. The time trial was carried out to elicit physiological stress as normally determined by training and competition. After a 30 minute rest participants completed the following tests to determine the effect of magnesium on strength and cardiovascular parameters.
Blood pressure, and augmentation index (Aix) were recorded at rest immediately and before the bench press. Subjects then performed a bench press corresponding to a 5 repetition maximum (5-RM) protocol [20]) for determination of their 1-RM. Upon completion, a 5-minutes rest period was given. Subsequently, a bench press at 80% 1-RM was performed to exhaustion. A measure of force (Newtons) was recorded during the bench press, with additional measures of blood pressure and Aix immediately upon completion of the bench press.
Supplementation
Magnesium citrate and placebo (cornflour) were capsulated into large vegetarian capsules. Capsules consisted of a total of 75 mg of elemental Mg2+ citrate, (Pioneer analytical balance. OHAUS, UK), 4 capsules per day were taken orally, equating supplemental Mg2+ to a total daily dose of 300 mg/d elemental Mg2+. Supplements were ingested evenly throughout the day on a non-testing day, or ingested 3 hours before exercise testing. Finally, the supplementation period for both placebo and Mg2+ accounted for a total ingestion period of 1 week or 4 weeks within the A and Chr groups, respectively.
Diet
A 4-day weighed food and beverage diary was recorded in relation to 3 weekdays and 1 weekend day, which was used for analysis of habitual dietary magnesium intake through use of dietary analysis software (Dietplan 6.70 Forestfield Software, UK).
Statistical analysis
Data were analysed using SPSS version 20 (IBM limited, UK) and Microsoft excel 2007 for Windows. Box-whisker plots measured normality/data distribution and showed that the data were not normally distributed. Therefore non-parametric Wilcoxon 2 related samples tests were carried out on all results to look for differences. Alpha value was set at 0.05.
Results
There were no statistically significant difference found between anthropometric data, VO2max and HR determining a homogeneous cohort (Table 1).
Table 2 shows averaged dietary data for both the Chr and A groups. Both the Chr and A control groups showed no significant difference between macronutrient and magnesium ingestion.
Table 2.
Dietary intake, values are mean ± SD
| Chronic intervention | Acute intervention | Chronic placebo control | Acute placebo control | |
|---|---|---|---|---|
| Kcal | 2513 ± 1201 | 2686 ± 938 | 3985 ± 519 | 3785 ± 734 |
| CHO (g) | 274 ± 170 | 296 ± 118 | 397 ± 209 | 343 ± 79 |
| Fat (g) | 96 ± 58 | 115 ± 49 | 114 ± 63 | 105 ± 48 |
| Pro (g) | 119 ± 38 | 114 ± 37 | 136 ± 66 | 129 ± 16 |
| Mg2+ (mg) | 375 ± 104 | 368 ± 173 | 551 ± 347 | 378 ± 79 |
Performance
Bench press
Net strength gains as determined by 1-RM showed significant increase of 17.7% with the acute Mg2+ loading strategy compared to baseline (p = 0.031) (Figure 1). No significant strength gains were seen in the Chr intervention group (p = 0.281).
Figure 1.
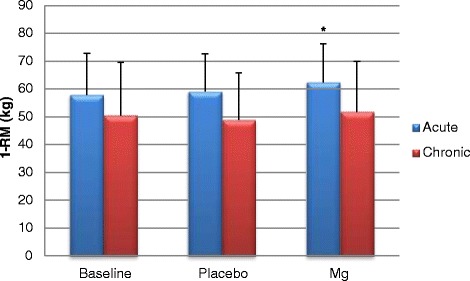
Acute and chronic bench press 1-RM scores on day 1 ± SD. * denotes significance.
Furthermore, A Mg2+ showed no decline in recovery (day 2) performance for force (N) resulting in a small day 2 (recovery day) force increase of 2.7%, showing a trend but no significnace (Figure 2). On the contrary Chr Mg2+ showed a day-to-day 32.1% performance decrement (Figure 3).
Figure 2.
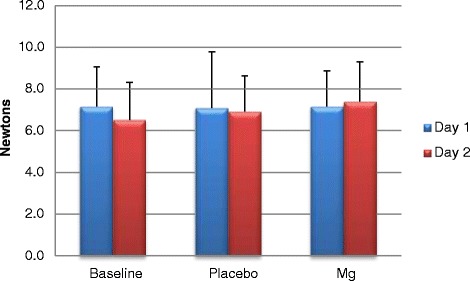
Acute force (newtons) output on day 1 and 2 (recovery) during repetitions to fatigue ± SD.
Figure 3.
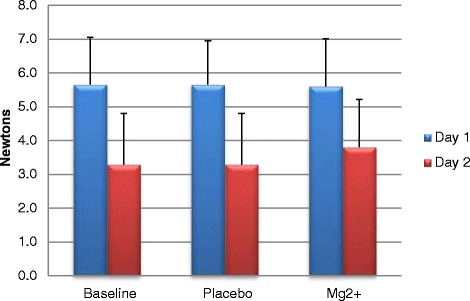
Chronic force (newtons) output on day 1 and 2 (recovery) during repetitions to fatigue ± SD.
Resting SBP measures from day 1 and 2 show a significant decrease within A Mg2+ treatment (P = 0.031), conversely placebo showed a significant increase in SBP (P = 0.047) (Table 3). Further, significant day 2 reductions in SBP were noted between A treatments of Mg2+-placebo (P = 0.016). On the contrary, Chr Mg2+ shows no significant reductions in resting SBP on day 1 or day 2.
Table 3.
Acute and chronic group mean SBP values at rest and post bench press at 80% 1-RM to fatigue on day 1 and 2 ±SD
| Physiological variable | Treatment | Group | Physiological variable | Treatment | Group | ||
|---|---|---|---|---|---|---|---|
| C Chr | A | Chr | A | ||||
| Resting SBP (mmHg) day 1 | Placebo | 119 ± 7 | 120 ± 5*1 | Post SBP (mmHg) day 1 | Placebo | 143 ± 7*3 | 136 ± 5 |
| Mg2+ | 118 ± 6 | 122 ± 4*2 | Mg2+ | 136 ± 9*3 | 137 ± 6 | ||
| Resting SBP (mmHg) day 2 | Placebo | 121 ± 8 | 125 ± 2*1, 3 | Post SBP (mmHg) day 2 | Placebo | 144 ± 9*4 | 144 ± 7*5 |
| Mg2+ | 118 ± 7 | 117 ± 7*2, 3 | Mg2+ | 137 ± 10*4 | 134 ± 5*5 | ||
*Denotes significance as paired by numbers.
In relation to post SBP responses, both Chr and A Mg2+ treatment resulted in significant SBP reductions; however, such reductions can be noted on day 1 (P = 0.016) and day 2 (P = 0.016) for a Chr Mg2+ induced SBP reduction in comparison to placebo, whereas an A Mg2+ reduction can be accounted for on day 2 (P = 0.047) in comparison to placebo.
Resting DBP showed no difference for day 1 to day 2 between the placebo or Mg2+.Post DBP showed no differences between Day 1 to Day 2 for acute supplementation group (Table 4). However, chronic intervention showed a decrease in DBP for post bench press on the recovery day 2.
Table 4.
Acute and chronic group mean DBP values at rest and post bench press at 80% 1-RM to fatigue on day 1 and 2 ± SD
| Physiological variable | Treatment | Group | Physiological variable | Treatment | Group | ||
|---|---|---|---|---|---|---|---|
| Chr | A | Chr | A | ||||
| Resting DBP (mmHg) day 1 | Placebo | 85 ± 7 | 75 ± 7 | Post DBP (mmHg) day 1 | Placebo | 92 ± 8 | 85 ± 12 |
| Mg2+ | 79 ± 6 | 75 ± 4 | Mg2+ | 87 ± 7 | 82 ± 5 | ||
| Resting DBP (mmHg) day 2 | Placebo | 78 ± 8 | 79 ± 6 | Post DBP (mmHg) day 2 | Placebo | 91 ± 5*1, 2 | 86 ± 13 |
| Mg2+ | 75 ± 7*1 | 74 ± 5*2 | Mg2+ | 84 ± 8*2 | 76 ± 8*3 | ||
*Denotes significance as paired by numbers.
Although no significance was seen for Aix at rest for both A and Chr loading strategies, a significant lowering post bench press was found as highlighted in Table 5 on day 1 for A treatment and day 2 for the Chr treatment group. Day 1 Aix reductions correspond to a significant Mg2+ lowering effect compared to baseline (P = 0.016) and placebo (P = 0.031), respectively. Whereas, similar Aix reductions for the Chr Mg2+ group is noted on day 2 post bench press resulting in significant values of P = 0.039, when compared to baseline and placebo, respectively.
Table 5.
Acute and chronic group mean Aix values post bench press at 80% of 1-RM to fatigue on day 1 and 2 ± SD
| Physiological variable | Treatment | Group | |
|---|---|---|---|
| Chr | A | ||
| Post Aix day 1 (%) | Baseline | 7 ± 11 | 17 ± 5*3 |
| Placebo | 9 ± 6 | 14 ± 6*4 | |
| Mg2+ | 7 ± 5 | 10 ± 5*3 *4 | |
| Post Aix day 2 (%) | Baseline | 14 ± 7*1 | 12 ± 6 |
| Placebo | 14 ± 8*2 | 16 ± 4 | |
| Mg2+ | 8 ± 12*1, 2 | 11 ± 6 | |
*Denotes significance as paired by numbers.
Discussion
This study set out to determine whether either acute or chronic magnesium supplementation would have an effect on performance (strength and cardiovascular) and blood pressure with exercise and/or on a second bout of exercise after a 24 hr recovery period. As has been shown previously [13,21] acute magnesium supplementation has a positive effect on BP, plyometric parameters and torque, however its effect on resistance exercise has not been evident to date. Further, chronic loading strategies have not been investigated in respect to exercise as well as the effect of Mg supplementation on a second bout of exercise. It was hypothesised that as acute Mg2+ supplementation has been seen to have beneficial effects on BP, CV parameters and peak torque a longer loading strategy (4 weeks) would amplify these results, giving a more beneficial and greater response. However, this study did not find that chronic loading of Mg2+ has a cumulative effect on the effect of supplementation, perhaps due to saturation of Mg2+ within the blood or limitations to transporters.
Primary findings showed variance across treatment groups on exercise (strength and recovery) and cardiovascular responses. The Chr Mg2+ intervention showed no significance in performance gains for bench press net strength and force output (Figures 1, 2 and 3). The A Mg2+ intervention showed variance in results across all variable analysed with some improvements being seen in resting HR and blood pressure for both Chr and A treatment groups regarding strength related performance (Figures 1, 2, 3 and Tables 3, 4, 5).
Strength performance
Strength related performance within the bench press showed statistical significant improvements (P = 0.031) within the A group and Chr group. Previous research has shown that Mg2+ significantly enhances bench press [22] and strength performance [11,23]. Acute Mg2+ loading showed a significant net strength increase of 5.5 kg between baseline and supplemental Mg2+ trials. Other strength related measurements of force (Newtons) illustrated A Mg2+ induced improvements. Typically, where a decrease in force would be expected on day 2 (recovery) of training as a normal physiological response to training, an A group improvement of 0.25 Newtons (2.7%) was seen with Mg2+ supplementation compared to the Chr where a 2.0 Newtons (32.1%) decrement was seen.
When examining net strength of Chr compared to A groups a notable difference between baseline scores is evident implying that subjects within the A group might well be stronger due to a 7.3 kg 1-RM difference at baseline (Figure 1). Therefore, when considering the 10.5 kg difference between Chr and A group 1-RM trials after intervention of Mg2+, inter-subject lifting capacity/ability could be a factor of concern for validating such a difference.
These performance enhancements for the strength associated tests are suggestive of physiological-regulatory functions of Mg2+ within muscle contraction and relaxation; i.e. regulating troponin expression via Ca2+ concentration gradients, Ca2+ transport, MgATP complex formation optimising energy metabolism/muscular contraction, increasing protein synthetic rate, protection against cellular damage and, greater amount of actin-mysoin crossbridges [23-26] all of which contribute to the result of increased strength and force production. Consideration must be given as to why such a contrasting difference between Chr and A groups occur specifically when regarding strength performance measures. The A Mg2+ supplemented group showed day-to-day performance improvements across 3 trials, as opposed to 3 day-to-day non-performance improved trials exhibited within the Chr Mg2+ supplemented group which may be attributed to the different loading strategies within the current study. The Mg2+ supplementation within the current research was 300 mg/d, therefore equating the Chr and A group mean daily intake for Mg2+ to 675 mg/d and 700 mg/d, respectively, when combined with dietary Mg2+ intake as analysed from food diaries. This adds a sense of greater ambiguity when considering the Mg2+ - strength performance relationship, and comparing to research highlighting observations that intakes of 500 mg/d or greater result in further increases in strength [24,25]. It could be suggested that subjects within the Chr loading group might be more susceptible to a possible reduction threshold or cell tolerance for Mg2+ absorption based upon the understanding that high Mg2+ intakes result in a lower Mg2+ absorption [27]. Additionally, Mg2+ homeostasis may be postulated to exhibit no greater benefit from the chronic perspective due to the kidney function for Mg2+ excretion as to maintain a balanced concentration of Mg2+ [27,28]; for example, could the principle of a higher Mg2+ dose, longer supplemental duration and associated proportional increase of Mg2+ excretion highlight the body’s efficiency in maintaining a state of homeostasis? Alternatively, chronic loading through providing a regular high Mg2+ intake may influence extracellular Mg2+ concentrations which coincide with manipulation of Mg2+ transporter TRPM6 function, resulting in a potential decrease in TRPM6 expression in conjunction to increasing the urinary excretion of Mg2+ [29]. Thus, an acute ingestion rate as opposed to chronic could result in a more efficient use for Mg2+.
Cardiovascular responses at rest and post bench press performance
Significant reductions in SBP and DBP are illustrated from post testing in the chronic group and rest and post testing in the acute group data across day 1 and 2 compared to baseline and placebo (Tables 3 and 4). Resting SBP was accounted for by a greater reduction in the A Mg2+ of 2 mmHg, in comparison to 0.7 mmHg with the Chr Mg2+ treatment. In addition, both resting and post DBP showed reductions with a greater day-to-day DBP reduction in the A Mg2+ in comparison to Chr Mg2+ as shown by a 69.2% and 50% (9 mmHg and 3 mmHg difference) at rest and post exercise for A and Chr groups respectively. These findings are in agreement with previous research [13,30] showing the importance of Mg2+ and its influence on blood pressure regulation. This is supported by findings within a recent meta-analysis [19] looking at Mg2+ supplementation which showed that SBP and DBP reductions of 2–3 mmHg and 3–4 mmHg, respectively. These observations oppose some previous findings which emphasise supplemental ineffectiveness of Mg2+ [31-33].
Such reductions in blood pressure could be speculated as being an outcome influenced by increases within the extracellular concentration of Mg2+, an effect that has been associated with reductions in the arterial tension and tone. These reductions in arterial tension and tone correspond to typical Mg2+ induced vasodilatory actions which potentiate effects of endogenous vasodilators such as adenosine, K+, nitric oxide and cyclo-oxygenase-dependent mechanisms via production of PGI2 [34]. In combination, Mg2+ acts as an antagonist to blocking Ca2+ channels [11,35,36] and further enzymatic mobilisation of Ca2+ [37]. Thus, data within the current study concur with previous research on the efficacy of Mg2+ supplementation in reducing blood pressure [13,38] and its capacity to suppress agonist vasoconstriction [4]. The above mechanisms may also be attributed to Mg2+ induced specific alterations within the vasculature, for example, Mg2+’s mediatory role within the endothelium corresponds to increased nitric oxide, PGI2 and decreases platelet aggregation, in combination to stringent down-regulation of Ca2+ voltage operated channel activity and release from the sarcoplasmic reticulum [39].
Average dietary Mg2+ intakes within the A and Chr groups corresponded to 368 mg/d and 375 mg/d, respectively. However, it must be considered that the blood pressure reduction in Chr and A loading strategies, may be attributed to the Mg2+ supplementation. With this in mind, it could be suggested that despite average dietary intakes of Mg2+ meeting the UK RNI a higher requirement for Mg2+ may be beneficial in reducing blood pressure. Further recommendations within the U.S are 420 mg/d and 320 mg/d for males, and females, respectively, in addition to Mg2+ requirements within the UK being determined many years ago [40]; Research by Geleijnse et al. [41] in a comparative study between 5 European countries which included the UK, corroborates with this study suggesting a potential increase of Mg2+ based on supplemental blood pressure enhancements, whereby the researchers highlighted a <350 mg/d of Mg2+ as suboptimal, augmenting the prevalence of hypertension. The study further accounted for an 80% insufficiency corresponding to Mg2+ intake to be evident within the UK population analysed [41].
A principle limitation within the current study concerns lack of monitoring of the subjects’ Mg2+ status via serum concentrations therefore this research is limited to infer indirect associations between Mg2+ supplementation and performance from dietary intake determined from food diaries. The study duration and the nature of a consecutive 2 day protocol both consisting of a 40 Km time trial can be seen as to limit the potential for subject recruitment and therefore final number of participants recruited. The use of males and females within groups must also be noted to account for occasional group data variance, on various parameters and a high level of standard deviation.
Conclusion
The current study showed a positive effect with A Mg2+ supplementation in relation to net strength and force gains with bench press, findings that support previous research [11,22,23,25]. Further, cardiovascular responses to the bench press were significantly enhanced by Mg2+ supplementation reducing resting SBP and DBP with the greatest effect seen with A Mg2+ supplementation for rest and post exercise. Similarly, SBP, DBP and Aix showed a significantly greater and more consistent reduction in response to the A Mg2+ loading strategy, as opposed to the minimalistic effect induced by Chr Mg2+ loading strategy.
In conclusion, it can be stated that improvements seen with the A loading strategy cannot to the same extent be observed with the Chr loading of Mg2+, thus potentially suggesting a regulatory effect within the body influenced by the duration of Mg2+ supplementation intake.
To conclude, from this study there appears to be no benefit in long term magnesium supplementation for those who have adequate dietary intake, but there are some benefits for taking an acute dose, particularly before intense exercise.
Future work may focus on the above parameters for those with low dietary Mg2+ intake and also for the optimum time that supplementation should be given to induce these positive findings.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LK conceived of the study, participated in its design and coordination, statistical analysis and writing of the manuscript. FP carried out the data collection, statistical analysis and writing of the manuscript. Both authors read and approved the final manuscript.
Contributor Information
Lindsy S Kass, Email: L.s.kass@herts.ac.uk.
Filipe Poeira, Email: Filipe_Poeira@hotmail.com.
References
- 1.Maguire ME. Magnesium transporters: properties, regulation and structure. Front Biosci. 2006;11:3149–3163. doi: 10.2741/2039. [DOI] [PubMed] [Google Scholar]
- 2.Bohl CH, Volpe SL. Magnesium and exercise. Crit Rev Food Sci Nutr. 2002;42(6):533–63. doi: 10.1080/20024091054247. [DOI] [PubMed] [Google Scholar]
- 3.Fawcett WJ, Haxby EJ, Male D a. Magnesium: physiology and pharmacology. Br J Anaesth. 1999;83:302–20. doi: 10.1093/bja/83.2.302. [DOI] [PubMed] [Google Scholar]
- 4.Touyz RM. Role of magnesium in the pathogenesis of hypertension. Mol Aspects Med. 2003;24:107–36. doi: 10.1016/S0098-2997(02)00094-8. [DOI] [PubMed] [Google Scholar]
- 5.Lukaski HC. Micronutrients (magnesium, zinc, and copper): are mineral supplements need for athletes? Int J Sport Nutr. 1995;5suppl:S74–S83. [PubMed] [Google Scholar]
- 6.Ford ES, Mokdad AH. Dietary magnesium intake in a national sample of U.S. adults. J Nutr. 2003;133:2879–2882. doi: 10.1093/jn/133.9.2879. [DOI] [PubMed] [Google Scholar]
- 7.Uzun A. The acute effect of maximal strength, power endurance and interval run training on levels of some elements in elite basketball players. Life Sci J. 2013;10:2697–2701. [Google Scholar]
- 8.Kass LS, Skinner P, Poeira F. A pilot study on the effects of magnesium supplementation with high and low habitual dietary magnesium intake on resting and recovery from aerobic and resistance exercise and systolic blood pressure. J Sports Sci Med. 2013;12:144–150. [PMC free article] [PubMed] [Google Scholar]
- 9.Ranadel VV, Somberg JC. Bioavailability and pharmacokinetics of magnesium after administration of magnesium salts to humans. Am J Ther. 2001;8:345–357. doi: 10.1097/00045391-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Newhouse IJ, Finstad EW. The effects of magnesium supplementation on exercise performance. Clin J Sport Med. 2000;10:195–200. doi: 10.1097/00042752-200007000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Santos DA, Matias CN, Monteiro CP, Silva AM, Rocha PM, Minderico CS, Bettencourt Sardinha L, Laires MJ. Magnesium intake is associated with strength performance in elite basketball, handball and volleyball players. Magnes Res. 2011;24:215–9. doi: 10.1684/mrh.2011.0290. [DOI] [PubMed] [Google Scholar]
- 12.Lukaski HC, Nielsen FH. Dietary magnesium depletion affects metabolic responses during submaximal exercise in postmenopausal women. Hum Nutr Metab. 2002;132:930–935. doi: 10.1093/jn/132.5.930. [DOI] [PubMed] [Google Scholar]
- 13.Itoh K, Kawasaka T, Nakamura M. The effects of high oral magnesium supplementation on blood pressure, serum lipids and related variables in apparently healthy Japanese subjects. Br J Nutr. 1997;78:737–50. doi: 10.1079/BJN19970191. [DOI] [PubMed] [Google Scholar]
- 14.Finstad EW, Newhouse IJ. The effects of magnesium supplementation on exercise performance. Clin J Sport Med. 2001;33:493–498. doi: 10.1097/00005768-200103000-00024. [DOI] [PubMed] [Google Scholar]
- 15.Terblanche S, Noakes TD, Dennis SC, Marais D, Eckert M. Failure of magnesium supplementation to influence marathon running performance or recovery in magnesium-replete subjects. Int J Sport Nutr. 1992;2:154–64. doi: 10.1123/ijsn.2.2.154. [DOI] [PubMed] [Google Scholar]
- 16.Williams M. Dietary supplements and sports performance: amino acids. J Int Soc Sports Nutr. 2005;2:63–7. doi: 10.1186/1550-2783-2-2-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Golf SW, Bender S, Gruttner J. On the significance of magnesium in extreme physical stress. Cardiovasc Drugs Ther. 1998;12(2):197–202. doi: 10.1023/A:1007708918683. [DOI] [PubMed] [Google Scholar]
- 18.Jee SH, Miller ER, Guallar E, Singh VK, Appel LJ, Klag MJ. The effect of magnesium supplementation on blood pressure: a meta-analysis of randomized clinical trials. Am J Hypertens. 2002;15:691–6. doi: 10.1016/S0895-7061(02)02964-3. [DOI] [PubMed] [Google Scholar]
- 19.Kass L, Weekes J, Carpenter L. Effect of magnesium supplementation on blood pressure: a meta-analysis. Eur J Clin Nutr. 2012;66:411–8. doi: 10.1038/ejcn.2012.4. [DOI] [PubMed] [Google Scholar]
- 20.Baechle T, Earle R. Essentials of Strength Training and Conditioning. 3. Human Kinetics: Illonois; 2008. [Google Scholar]
- 21.Setaro L, Santos-Silva P, Nakano E, Sales C, Nune N, Greve J, Colli C. Magnesium status and the physical performance of volleyball players: effects of magnesium supplemenatation. J Sport Sci. 2014;32:438–435. doi: 10.1080/02640414.2013.828847. [DOI] [PubMed] [Google Scholar]
- 22.Matias CN, Santos DA, Monteiro CP, Silva AM, Raposo MDF, Martins F, Sardinha LB, Bicho M, Laires MJ. Magnesium and strength in elite judo athletes according to intracellular water changes. Magnes Res. 2010;23:138–41. doi: 10.1684/mrh.2010.0217. [DOI] [PubMed] [Google Scholar]
- 23.Dominguez LJ, Barbagallo M, Lauretani F, Bandinelli S, Bos A, Corsi AM, Simonsick EM, Ferrucci L. Magnesium and muscle performance in older persons: the InCHIANTI study. Am J Clin Nutr. 2006;84:419–426. doi: 10.1093/ajcn/84.1.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lukaski HC. Vitamin and mineral status: effects on physical performance. Nutrition. 2004;20:632–44. doi: 10.1016/j.nut.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Brilla LR, Haley TF. Effect of magnesium supplementation on strength training in humans. J Am Coll Nutr. 1992;11:326–329. doi: 10.1080/07315724.1992.10718233. [DOI] [PubMed] [Google Scholar]
- 26.Carvil P, Cronin J. Magnesium and implications on muscle function. Strength Cond J. 2010;32:48–54. doi: 10.1519/SSC.0b013e3181c16cdc. [DOI] [Google Scholar]
- 27.Jahnen-Dechent W, Ketteler M. Magnesium basics. Clin Kidney J. 2012;5(Suppl 1):i3–i14. doi: 10.1093/ndtplus/sfr163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.De Baaij JHF, Hoenderop JGJ, Bindels RJM. Regulation of magnesium balance: lessons learned from human genetic disease. Clin Kidney J. 2012;5(Suppl 1):i15–i24. doi: 10.1093/ndtplus/sfr164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alexander RT, Hoenderop JG, Bindels RJ. Molecular determinants of magnesium homeostasis: insights from human disease. J Am Soc Nephrol. 2008;19:1451–8. doi: 10.1681/ASN.2008010098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Motoyama T, Sano H, Fukuzaki H. Oral magnesium supplementation in patients with essential hypertension. Hypertension. 1989;13:227–232. doi: 10.1161/01.HYP.13.3.227. [DOI] [PubMed] [Google Scholar]
- 31.Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, Williams B, Ford G a. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–33. doi: 10.1097/01.hjh.0000199800.72563.26. [DOI] [PubMed] [Google Scholar]
- 32.Cappuccio FP. Lack of effect of oral magnesium double blind study. Br Med J. 1985;291:235–238. doi: 10.1136/bmj.291.6490.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Doyle L, Flynn a, Cashman K. The effect of magnesium supplementation on biochemical markers of bone metabolism or blood pressure in healthy young adult females. Eur J Clin Nutr. 1999;53:255–61. doi: 10.1038/sj.ejcn.1600714. [DOI] [PubMed] [Google Scholar]
- 34.Pokan R, Hofmann P, von Duvillard SP, Smekal G, Wonisch M, Lettner K, Schmid P, Shechter M, Silver B, Bachl N. Oral magnesium therapy, exercise heart rate, exercise tolerance, and myocardial function in coronary artery disease patients. Br J Sports Med. 2006;40:773–8. doi: 10.1136/bjsm.2006.027250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Laires MJ. Biochemistry Laboratory, Faculty of Human Kinetics, Technical University of Lisbon, Portugal, 2 Genetics Laboratory, Faculty of Medicine, University of Lisbon, Portugal. Front Biosci. 2004;9:262–276. doi: 10.2741/1223. [DOI] [PubMed] [Google Scholar]
- 36.O’Rourke B, Backx PH, Marban E. Phosphorylation-independent modulation of L-type calcium channels by magnesium-nucleotide complexes. Science. 1992;257:245–8. doi: 10.1126/science.1321495. [DOI] [PubMed] [Google Scholar]
- 37.Laurant P, Touyz RM. Physiological and pathophysiological role of magnesium in the cardiovascular system: implications in hypertension. J Hypertens. 2000;18:1177–91. doi: 10.1097/00004872-200018090-00003. [DOI] [PubMed] [Google Scholar]
- 38.Guerrero-Romero F, Rodríguez-Morán M. Low serum magnesium levels and metabolic syndrome. Acta Diabetol. 2002;39:209–13. doi: 10.1007/s005920200036. [DOI] [PubMed] [Google Scholar]
- 39.Geiger H, Wanner C. Magnesium in disease. Clin Kidney J. 2012;5(Suppl 1):i25–i38. doi: 10.1093/ndtplus/sfr165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nielsen FH, Lukaski HC. Update on the relationship between magnesium and exercise. Magnes Res. 2006;19:180–9. [PubMed] [Google Scholar]
- 41.Geleijnse JM, Grobbee DE, Kok FJ. Impact of dietary and lifestyle factors on the prevalence of hypertension in Western populations. J Hum Hypertens. 2005;19(Suppl 3):S1–4. doi: 10.1038/sj.jhh.1001953. [DOI] [PubMed] [Google Scholar]


