Abstract
IMPORTANCE
Suicide attempts are strong predictors of suicide, a leading cause of adolescent mortality. Suicide attempts are highly familial, although the mechanisms of familial transmission are not understood. Better delineation of these mechanisms could help frame potential targets for prevention.
OBJECTIVE
To examine the mechanisms and pathways by which suicidal behavior is transmitted from parent to child.
DESIGN, SETTING, AND PARTICIPANTS
In this prospective study conducted from July 15, 1997, through June 21, 2012, a total of 701 offspring aged 10 to 50 years (mean age, 17.7 years) of 334 clinically referred probands with mood disorders, 191 (57.2%) of whom had also made a suicide attempt, were followed up for a mean of 5.6 years.
MAIN OUTCOMES AND MEASURES
The primary outcome was a suicide attempt. Variables were examined at baseline, intermediate time points, and the time point proximal to the attempt. Participants were assessed by structured psychiatric assessments and self-report and by interview measures of domains hypothesized to be related to familial transmission (eg, mood disorder and impulsive aggression).
RESULTS
Among the 701 offspring, 44 (6.3%) had made a suicide attempt before participating in the study, and 29 (4.1%) made an attempt during study follow-up. Multivariate logistic regression revealed that proband suicide attempt was a predictor of offspring suicide attempt (odds ratio [OR], 4.79; 95% CI, 1.75–13.07), even controlling for other salient offspring variables: baseline history of mood disorder (OR, 4.20; 95% CI, 1.37–12.86), baseline history of suicide attempt (OR, 5.69; 95% CI, 1.94–16.74), and mood disorder at the time point before the attempt (OR, 11.32; 95% CI, 2.29–56.00). Path analyses were consistent with these findings, revealing a direct effect of proband attempt on offspring suicide attempt, a strong effect of offspring mood disorder at each time point, and impulsive aggression as a precursor of mood disorder.
CONCLUSIONS AND RELEVANCE
Parental history of a suicide attempt conveys a nearly 5-fold increased odds of suicide attempt in offspring at risk for mood disorder, even after adjusting for the familial transmission of mood disorder. Interventions that target mood disorder and impulsive aggression in high-risk offspring may attenuate the familial transmission of suicidal behavior.
According to a review article,1 adoption, twin, and family studies have established that suicidal behavior is familial. Moreover, the phenotype that is transmitted is a suicide attempt or suicide rather than suicidal ideation.2,3 However, few studies4–6 have addressed the pathways by which suicidal behavior is transmitted in families.
To address this gap in the literature, we began the Familial Pathways to Early-Onset Suicidal Behavior study, in which we followed up the offspring of parents with a mood disorder, with approximately half the parents in the study having a history of a suicide attempt. Previous studies7–11 have indicated that offspring of suicide attempters had a 4- to 6-fold greater risk of a suicide attempt and that possible mediators of familial transmission included the intrafamilial transmission of impulsive aggression, mood disorder, and childhood maltreatment. However, these reports were cross-sectional or covered 1 to 2 years of follow-up with relatively few suicide attempts among offspring.
In contrast, we report on offspring of parents with mood disorders who were followed up for a mean of 5.6 years. Consequently, a much larger proportion of this cohort is past the peak age at onset of mood disorder and suicidal behavior. On the basis of previous work and the extant literature, we hypothesized that proband suicide attempt would predict offspring suicide attempt, even after controlling for the familial transmission of mood disorders, and that the familial transmission of suicidal behavior would be mediated by the familial transmission of mood disorder, impulsive-aggressive traits, and childhood physical or sexual abuse.
Methods
Sample
This study was reviewed and approved by the University of Pittsburgh Institutional Review Board and the New York State Psychiatric Institute Institutional Review Board, and written informed consent or assent was obtained from all participants. The sample consisted of 701 offspring of 334 probands with mood disorders, with 191 (57.2%) of the probands having made a suicide attempt and a mean (SD) number of offspring siblings per proband of 2.1 (1.0) (Table 1). Most pro-bands were clinically referred to the Western Psychiatric Institute or the New York State Psychiatric Institute, the 2 sites of this study, from July 15, 1997, through September 6, 2005, and followed through June 21, 2012.
Table 1.
Demographic and Clinical Characteristics of Offspring and Probands at Baseline Assessmenta
| Characteristic | Proband
|
Offspring of Proband
|
||
|---|---|---|---|---|
| Suicide Nonattempter (n = 143) | Suicide Attempter (n = 191) | Suicide Nonattempter (n = 285) | Suicide Attempter (n = 416) | |
| Offspring per family, mean (SD) [range], No. | 2.0 (0.8) [1–4] | 2.2 (1.0) [1–7] | NA | NA |
|
| ||||
| Age, mean (SD) [range], y | 45.4 (9.8) [24–74] | 44.0 (10.4) [23–80] | 17.9 (8.9) [10–47] | 17.5 (8.3) [10–50] |
|
| ||||
| Age ≥18 y | 143 (100) | 191 (100) | 98 (34.4) | 156 (37.5) |
|
| ||||
| Female sex | 123 (86.0) | 161 (84.3) | 147 (51.6) | 190 (45.7) |
|
| ||||
| White race | 110 (80.3) | 126 (68.5) | 214 (79.3) | 263 (65.4) |
|
| ||||
| Hispanic ethnicityb | 20 (14.0) | 19 (9.9) | 37 (13.1) | 33 (8.0) |
|
| ||||
| Married or sustained conjugal status ≥6 mo | 75 (52.4) | 81 (42.4) | 33 (33.7) | 45 (28.7) |
|
| ||||
| Hollingshead’s Four Factor Index of Social Status score, mean (SD) [range] | 43.6 (13.1) [14–66] | 42.5 (11.3) [22–66] | 39.7 (12.9) [11–66] | 36.4 (12.9) [19–66] |
|
| ||||
| Lifetime mood disorder | 143 (100) | 191 (100) | 84 (30.0) | 143 (34.7) |
|
| ||||
| MDD | 116 (81.1) | 153 (80.1) | 76 (27.1) | 128 (31.0) |
|
| ||||
| Bipolar disorder | 28 (19.7) | 40 (21.5) | 10 (3.6) | 17 (4.1) |
|
| ||||
| Anxiety disorder | 81 (57.4) | 130 (70.7) | 60 (21.4) | 102 (24.9) |
|
| ||||
| Panic | 34 (24.1) | 70 (38.5) | 5 (5.1) | 7 (4.5) |
|
| ||||
| PTSD | 31 (22.0) | 66 (35.9) | 8 (2.9) | 36 (8.7) |
|
| ||||
| OCD | 4 (2.8) | 10 (5.3) | 5 (1.8) | 6 (1.5) |
|
| ||||
| Lifetime ADHD | Not assessed | Not assessed | 24 (13.2) | 55 (21.4) |
|
| ||||
| Lifetime conduct, antisocial, or oppositional disorder | 4 (2.9) | 8 (4.5) | 23 (8.2) | 49 (12.0) |
|
| ||||
| Lifetime alcohol or substance abuse | 52 (36.6) | 108 (58.7) | 41 (41.8) | 73 (17.7) |
|
| ||||
| Cluster B personality disorderc | 12 (8.8) | 50 (28.2) | 6 (2.1) | 18 (4.4) |
|
| ||||
| Nonsuicidal self-injurious behavior | NA | NA | 13 (6.8) | 33(12.9) |
|
| ||||
| History | ||||
|
| ||||
| Physical or sexual abuse | 80 (69.0) | 118 (83.1) | 61 (29.2) | 100 (32.4) |
|
| ||||
| Head trauma | 41 (29.3) | 58 (30.7) | 63 (23.5) | 94 (23.3) |
|
| ||||
| Suicide attempt | NA | NA | 16 (5.6) | 27 (6.5) |
|
| ||||
| Suicide-related behavior | NA | NA | 5 (1.8) | 17 (4.1) |
|
| ||||
| Follow-up, mean (SD), y | 6.3 (3.3) | 6.8 (3.8) | 5.3 (3.6) | 5.9 (3.9) |
|
| ||||
| New York site | 63 (44.1) | 67 (35.1) | 118 (41.4) | 132 (31.7) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; MDD, major depressive disorder; NA, not applicable; OCD, obsessive-compulsive disorder; PTSD, posttraumatic stress disorder.
Data are presented as number (percentage) of study participants unless otherwise indicated. No statistically significant differences between groups were found except for offspring race, proband Cluster B personality disorder, and proband lifetime alcohol or substance abuse (P < .001, q < .001).
On the basis of participant’s self-report.
Only assessed in those 18 years or older.
Follow-up
Offspring were followed up for a mean (SD) of 5.6 (3.8) years, with retention rates of 88.6%, 81.7%, 60.1%, 61.1%, and 58.6% of the sample from intake for years 1 through 5, respectively; probands were also followed up prospectively. No baseline differences were found between those who were retained and those who were lost to follow-up after correction for the false discovery rate (FDR) and there was no difference in the rate of follow-up of offspring of suicide attempters vs nonattempters (hazard ratio, 1.10; 95% CI, 0.66–1.82; z = 0.35; P = .73).
Site Differences
At baseline, after FDR correction, offspring in Pittsburgh, compared with offspring in New York, were younger (mean [SD], 15.4 [6.8] vs 19.1 [10] years; t210.7 = 4.09; P < .001; q < .001), less likely to be Hispanic (1.6% vs 25.6%; ; P < .001; q < .001), and followed up for a longer period of time (mean [SD], 6.1 [3.7] vs 4.9 [3.8] years; t699 = 4.06; P < .001).
Assessment
Probands and offspring were assessed by separate, masked clinical interviewers (C.B.). Baseline interviews covered lifetime occurrence of suicidal ideation and behavior, aggression, and psychiatric disorders. Subsequent annual interviews covered these domains since the last assessment. These interviews, along with self-report questionnaires, targeted known contributors to suicidal risk, namely, previous attempt and suicidal ideation; mood, anxiety, and behavioral disorders; impulsive aggression; Cluster B personality disorders (ie, borderline, antisocial, or narcissistic); family discord; history of head trauma; and history of abuse.12–14 eTable 1 in the Supplement lists all assessments, targeted domains, and periods covered.
Suicidal behavior was assessed using the Columbia History of Suicide Form and classified as suicidal ideation, suicide attempt, interrupted attempt, or aborted attempt as per the Columbia Classification Algorithm for Suicide Attempts.15,16 Interrater reliability with the Columbia History of Suicide Form is high (κ = 0.97), as was the convergent validity with the Columbia Suicide Severity Rating Scale.17,18 A suicide attempt was defined as a self-destructive act that resulted in potential or actual tissue damage with inferred or explicit intent to die.15 Suicide-related behavior included interrupted and aborted attempts and emergency referrals for suicidal ideation but not suicide attempts. Suicidal ideation was assessed by the Scale for Suicidal Ideation19 or the downward extension for youth younger than 14 years.20 Nonsuicidal self-injury (NSSI) was assessed consistent with its definition in the Columbia Classification Algorithm for Suicide Attempts.15
Aggression was measured using the Brown-Goodwin Lifetime History of Aggression in all participants.21 Axis I disorders were assessed by the Structured Clinical Interview for DSM-IV for participants 18 years and older22 and by the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present and Lifetime Version, in youth.23 The Structured Clinical Interview for DSM-IV was augmented with a module for the assessment of attention-deficit/hyperactivity disorder derived from the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present and Lifetime Version. Interrater reliability on depressive diagnoses for specific (κ = 0.96; 95% CI, 0.90–1.00) and the full range of diagnoses (κ = 0.65–0.96) was high. Personality disorders in pro-bands and offspring 18 years or older were assessed using the Structured Clinical Interview for DSM-IV Axis II disorders.24 Socioeconomic status of the head of household was assessed using Hollingshead’s Four Factor Index of Social Status.25 Race and ethnicity were based on the respondent’s self-assessment.
Self-reported Questionnaires
For those 14 years and older vs younger offspring, depressive symptoms were assessed using the Beck Depression Inventory or the Children’s Depression Inventory,26,27 hopelessness with the Beck Hopelessness Scale or the Children’s Hopelessness Scale,28,29 and impulsive aggression by the Buss Durkee Hostility Inventory or the Children’s Hostility Inventory.30,31 For those 18 years and older vs those younger than 18 years, impulsivity was assessed with the Barratt Impulsivity Scale or the impulsivity subscale of the Conners’ Teacher Rating Scale,32,33 negative life events in the previous 12 months were assessed with the shortened version of the Social Readjustment Rating Scale or the Life Events Checklist,34,35 social support was assessed with the Multidimensional Scale of Perceived Social Support36 or the Survey of Children’s Social Support,37 and reasons for staying alive were assessed with the Reasons for Living Inventory38 or the Reasons for Living Inventory for Adolescents.39 Family climate was assessed using the child-reported Family Assessment of Cohesion Evaluation Scale.40 In all participants, child maltreatment was assessed using the Abuse Dimensions Inventory41 and the Childhood Trauma Questionnaire.42 When the same domain was assessed with different instruments for different age groups, scores were z-transformed.
Statistical Analysis
We conducted univariate analyses examining the association of demographic, clinical, and psychological characteristics with suicide attempt, using logistic regression to include a cluster effect to account for sibling pairs in the sample. For the purpose of these analyses, we categorize the longitudinal data into (1) baseline clinical variables at study intake; (2) intermediate variables, which covered all time points between baseline and the one before the proximal time point; and (3) proximal, which covered the time point immediately before the onset of an actual attempt or maximum time point for suicide nonattempters. All 3 of these time points were before the assessed outcome (actual suicide attempt), thus maintaining the temporal sequence for predictive models. Self-reports of symptom severity were not included with other baseline variables to reduce the number of variables examined. Dichotomous variables, such as diagnosis, were counted as present if they occurred during at least one of the intermediate time points, and the most severe rating of suicidal ideation was reported, whereas self-report data were averaged across intermediate time points. We also examined proband lifetime diagnoses up to the time point of offspring’s suicide attempt or maximum time point. We controlled a priori for proband lifetime suicide attempts in all models.
Variables that were significant after using the FDR with the Yekutieli and Benjamini43 method to account for correlations among variables (qqvalue package in STATA statistical software, version 11.2, Stata Corp) were included in multivariate analyses to select the most salient predictors of suicide attempt at the baseline, intermediate, and proximal time points. A final multivariate model included all salient variables from these 3 time points, followed by backward stepwise regression to identify the most parsimonious set of predictors overall. All multivariate models adjusted for offspring age, sex, ethnicity, and site. Fit of the multivariate logistic regression models was evaluated using the area under the curve of the receiver operating characteristic curve of the predicted probabilities and the classification table. Similar findings emerged after conducting analogous univariate and multivariate analyses with time to onset of attempt using Cox proportional hazards regression models, so we present the former approach in this article. In this sample of 701 offspring, 25 offspring of suicide attempters and 4 offspring of suicide nonattempters made suicide attempts during follow-up, resulting in a greater than 0.99 power to detect a Cohen effect size of 0.26 for 2-sided tests with α = .05.44
Multivariate analyses were performed with actual and imputed data obtained with the Multiple Imputation by Chained Equations technique (ice command in STATA statistical software, version 11.2). Sensitivity analyses based on actual data yielded similar results. Path analyses, including the variables significant in the final multivariate analyses, were conducted using Mplus statistical software, version 7.11.45
Results
Suicide Attempts in Offspring
Of the 701 offspring, 44 (6.3%) had made a suicide attempt before participating in the study, and 29 (4.1%) made an attempt during study follow-up, of whom 19 (65.5%) made first-time attempts.
Baseline Variables
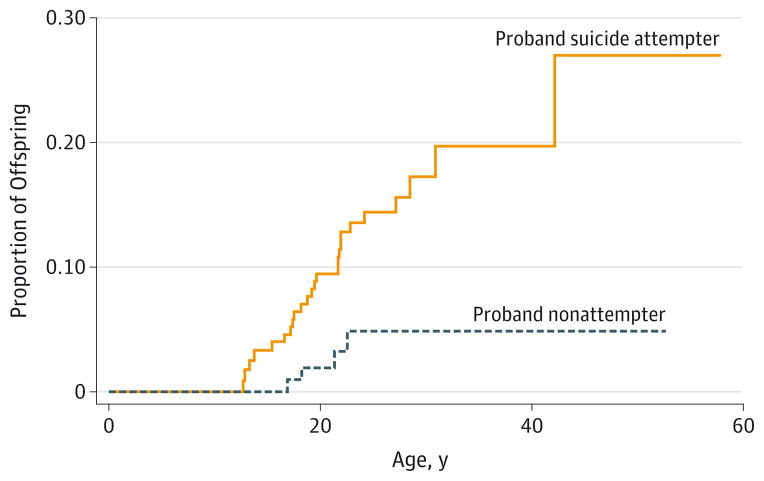
Proband suicide attempt, as an a priori hypothesis, was not subject to FDR correction but was related to risk of offspring suicide attempt (odds ratio [OR], 4.49; 95% CI, 1.56–12.90; t = 2.79; P = .005; q = 0.12). Similarly, with a survival analysis, the hazard of a suicide attempt was higher in offspring whose parent had a history of attempt (hazard ratio, 4.13; 95% CI, 1.45–11.77; z = 2.66; P = .008), with a mean (SD) age at onset of 20.1 (6.1) years (Figure 1). The risk of offspring suicide attempt was similar in the offspring of probands with unipolar depression (OR, 4.02; 95% CI, 1.39–11.65; z = 2.56; P = .01) and probands with bipolar depression (OR, 4.71; 95% CI, 0.24–93.06; z = 1.02; P = .31) but tended to be higher in the offspring of female pro-bands (OR, 5.10; 95% CI, 1.51–17.19; z = 2.63; P = .008) compared with the offspring of male probands (OR, 2.50; 95% CI, 0.30–21.19; z = 0.84; P = .40). As indicated in Table 2, offspring baseline mood disorder, history of a previous suicide attempt, impulsive aggression, and history of NSSI were related to a suicide attempt. Logistic regression revealed that the most parsimonious set of baseline variables associated with a suicide attempt was offspring mood disorder, history of NSSI, and history of a suicide attempt.
Figure 1.
Risk of Offspring Suicide Attempt by Proband History of Attempts
Wilcoxon test: , P = .008; log-rank test: , P = .004.
Table 2.
Demographic and Clinical Characteristics of Offspring and Proband and Risk of Suicide Attempt in Offspring
| Characteristic | Baseline
|
Time Points
|
||||
|---|---|---|---|---|---|---|
| Intermediate
|
Proximala
|
|||||
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Offspring | ||||||
|
| ||||||
| Age | 0.99 (0.96–1.02) | .37 | NA | NA | NA | |
|
| ||||||
| Sex | 1.56 (0.74–3.27) | .24 | NA | NA | NA | |
|
| ||||||
| White | 0.77 (0.34–1.72) | .52 | NA | NA | NA | |
|
| ||||||
| Hispanic | 1.46 (0.51–4.16) | .48 | NA | NA | NA | |
|
| ||||||
| Site | 0.90 (0.42–1.92) | .79 | NA | NA | NA | |
|
| ||||||
| Mood disorder | 8.68 (3.41–22.11) | <.001b | 5.88 (2.55–13.57) | <.001b | 16.77 (3.59–78.33) | <.001b |
|
| ||||||
| ADHD | 2.76 (0.99–7.64) | .05 | 2.90 (1.28–6.57) | .01 | 7.03 (1.65–29.91) | .008 |
|
| ||||||
| PTSD | 3.36 (1.34–8.45) | .01 | 3.81 (1.45–10.03) | .007 | 6.87 (1.73–27.27) | .006 |
|
| ||||||
| Anxiety disorder | 1.51 (0.69–3.26) | .30 | 3.36 (1.63–6.93) | .001c | 1.61 (0.41–6.27) | .49 |
|
| ||||||
| Eating disorder | 4.94 (1.33–18.37) | .02 | NA | NA | NA | NA |
|
| ||||||
| Alcohol or substance abuse | 2.40 (1.04–5.52) | .04 | 2.59 (1.18–5.71) | .02 | 0.47 (0.06–3.77) | .48 |
|
| ||||||
| Behavioral or antisocial disorder | 2.91 (1.26–6.71) | .01 | 3.19 (1.38–7.35) | .007 | 5.28 (1.36–20.44) | .02 |
|
| ||||||
| Depression, self-report | NA | NA | 1.89 (1.43–2.51) | <.001b | 1.72 (1.12–2.63) | .01 |
|
| ||||||
| Hopelessness | NA | NA | 1.45 (1.07–1.98) | .02 | 1.68 (1.10–2.58) | .02 |
|
| ||||||
| Impulsivity | 1.95 (1.31–2.90) | .001c | 2.61 (1.77–3.84) | <.001b | 1.82 (0.94–3.50) | .07 |
|
| ||||||
| Impulsive aggression | 2.16 (1.35–3.44) | .001c | 2.40 (1.47–3.91) | <.001b | 2.65 (0.97–7.24) | .06 |
|
| ||||||
| Aggression | 2.01 (1.43–2.83) | <.001b | 1.45 (1.03–2.04) | .04 | 1.81 (1.38–2.37) | <.001b |
|
| ||||||
| Negative life events | NA | NA | 2.00 (1.51–2.65) | <.001b | 2.61 (1.50–4.52) | .001c |
|
| ||||||
| Reasons for living | NA | NA | 0.92 (0.54–1.56) | .76 | 0.56 (0.24–1.29) | .17 |
|
| ||||||
| Social support | NA | NA | 0.74 (0.50–1.11) | .15 | 0.73 (0.36–1.50) | .39 |
|
| ||||||
| Family adaptability or cohesion | NA | NA | 0.93 (0.87–0.99) | .02 | 0.96 (0.90–1.2) | .20 |
|
| ||||||
| Nonsuicidal self-injurious behavior | 6.98 (2.41–20.24) | <.001b | 7.67 (2.02–29.15) | .003c | 11.02 (3.03–40.11) | <.001b |
|
| ||||||
| Lifetime history of physical or sexual abuse | 2.12 (0.97–4.62) | .06 | NA | NA | NA | NA |
|
| ||||||
| History of suicide attemptd | 11.03 (4.87–24.99) | <.001b | NA | NA | NA | NA |
|
| ||||||
| History of suicide-related behaviorsd | 3.64 (0.88–15.04) | .07 | NA | NA | NA | NA |
|
| ||||||
| Suicidal ideation | 1.18 (1.05–1.33) | .007 | 1.27 (1.16–1.39) | <.001b | 0.98 (0.76–1.26) | .87 |
|
| ||||||
| Suicide-related behaviors | NA | NA | 5.88 (2.09–16.56) | .001c | 7.96 (0.80–79.46) | .08 |
|
| ||||||
| Proband | ||||||
|
| ||||||
| Mood | 1.05 (0.31–3.56) | .94 | 1.41 (0.49–4.04) | .52 | 1.68 (0.69–4.10) | .25 |
|
| ||||||
| Alcohol or substance abuse | 1.88 (0.86–4.14) | .12 | 1.25 (0.54–2.89) | .60 | 0.38 (0.09–1.66) | .20 |
|
| ||||||
| PTSD | 1.33 (0.57–3.16) | .51 | 1.49 (0.70–3.20) | .30 | 2.17 (0.91–5.16) | .08 |
|
| ||||||
| Anxiety | 1.26 (0.59–2.85) | .58 | 0.74 (0.36–1.51) | .40 | 0.76 (0.35–1.67) | .50 |
|
| ||||||
| Cluster B personality disorder | 2.19 (0.98–4.91) | .06 | NA | NA | NA | NA |
|
| ||||||
| Lifetime history of physical or sexual abuse | 0.83 (0.29–2.39) | .73 | NA | NA | NA | NA |
|
| ||||||
| Lifetime history of suicide | 4.49 (1.56–12.90) | .005 | NA | NA | NA | NA |
|
| ||||||
| Impulsivity | 1.02 (0.99–1.04) | .18 | 1.01 (.99–1.03) | .44 | 1.01 (0.97–1.05) | .70 |
|
| ||||||
| Impulsive aggression | 1.02 (0.99–1.06) | .24 | 1.02 (0.98–1.07) | .29 | 1.05 (0.97–1.14) | .26 |
|
| ||||||
| Aggression | 1.26 (0.92–1.74) | .15 | 1.11 (0.73–1.70) | .62 | 1.06 (0.78–1.44) | .71 |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; NA, not applicable; OR, odds ratio; PTSD, posttraumatic stress disorder.
Time point immediately before the onset of an actual suicide attempt or maximum time point for suicide nonattempters.
q < .001.
q < .05.
Compared with no event.
Intermediate Time Points
At the intermediate time points, offspring mood disorder, post-traumatic stress disorder, anxiety, behavioral or antisocial disorder, self-reported depressive symptoms, impulsivity, impulsive aggression, negative life events, NSSI, suicidal ideation, and suicide-related behavior were all related to an outcome of a suicide attempt. Logistic regression found that the most parsimonious set of variables at intermediate time points associated with suicide attempt were offspring negative life events and suicidal ideation (Table 2).
Proximal Time Point
At the proximal time point (ie, the one immediately before the attempt), offspring mood disorder, negative life events, aggression, and NSSI were associated with suicide attempt. Logistic regression identified offspring mood disorder and aggression at the proximal time as being the most parsimonious variables associated with suicide attempt (Table 2).
Multivariate Model
The most salient variables predicting offspring suicide attempt at each time block were entered into a logistic regression model along with offspring age, sex, Hispanic ethnicity, site, and proband suicide attempt. Using backward stepwise regression, the most parsimonious set of variables associated with offspring suicide attempt were offspring mood disorder at baseline, a history of an offspring suicide attempt before entry into the study, offspring mood disorder at the time point before the suicide attempt, and proband suicide attempt. There were no main effects of offspring age, offspring or proband sex, or offspring or proband polarity of mood disorder on offspring suicide attempt and no significant interactions of any variables with proband attempt (Table 3).
Table 3.
Multivariate Model for Onset of Suicide Attemptsa
| Characteristic | OR (95% CI) | t-Test | P Value |
|---|---|---|---|
| Baseline mood disorder | 4.20 (1.37–12.86) | 2.51 | .01 |
| Historyb | |||
| Suicide attempt | 5.69 (1.94–16.74) | 3.16 | .002 |
| Suicide-related behavior | 0.97 (0.21–4.49) | −0.04 | .97 |
| Mood disorder at proximal time pointc | 11.32 (2.29–56.00) | 3.04 | .004 |
| Proband lifetime history of suicide | 4.79 (1.75–13.07) | 3.06 | .002 |
| Offspring | |||
| Age at baseline | 0.94 (0.87–1.01) | −1.68 | .09 |
| Sex | 0.80 (0.33–1.96) | −0.49 | .62 |
| Hispanic | 1.06 (0.29–3.93) | 0.09 | .93 |
| Sited | 0.81 (0.30–2.14) | −0.43 | .67 |
Abbreviation: OR, odds ratio.
Goodness-of-fit statistics: area under the curve = 0.89 (95% CI, 0.81–0.96); 96.3% were correctly classified.
Compared with no event.
Time point immediately before the onset of an actual suicide attempt or maximum time point for suicide nonattempters.
New York is the reference site.
Predictors of Mood Disorder at the Proximal Time Point
Because offspring mood disorder at the proximal time point to the attempt was among the strongest predictors of a suicide attempt, we tried to deconstruct this variable by identifying those baseline and intermediate variables most closely associated with it (eTable 2 in the Supplement), which were baseline proband Cluster B disorder and offspring age, as well as the following offspring variables assessed at intermediate time points: mood disorder, anxiety disorder, eating disorder, and impulsive aggression.
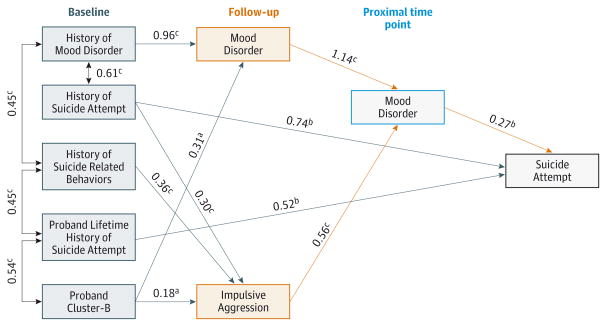
Path Model
Path analyses were conducted that included predictors of offspring mood disorder at a proximal time point (eTable 1 in the Supplement) and predictors of offspring suicide attempt (Table 3 and Figure 2). We report the path coefficients and statistical significance for the entire path being described. Proband suicide attempt had a direct effect on offspring attempt (β = 0.52, SE = 0.20, z = 2.64, P = .008). However, the indirect pathway from proband attempt via proband Cluster B, offspring impulsive aggression, and mood disorder before the attempt was not statistically significant (β = 0.03, SE = 0.02, P = .08). Offspring history of a previous suicide attempt had a direct path to offspring suicide attempt (β = 0.74, SE = 0.26, z = 2.87, P = .004). The effects of previous attempts and previous suicide-related behavior in offspring were also mediated via offspring impulsive aggression and mood disorder (β = 0.05, SE = 0.02, z = 2.20, P = .03, and β = 0.05, SE = 0.03, z = 1.95, P = .05, respectively). A final pathway was a consistent effect of offspring mood disorder at baseline and each follow-up point on offspring suicide attempt (β = 0.30, SE = 0.10, z = 2.86, P = .004).
Figure 2.
Path Analysis Including Predictors of Suicide Attempt and Mood Disorder at the Prior Time Point
Black line indicates baseline variables; red line, follow-up variables; and blue line, variables at proximal time points. Numbers are path coefficients. All paths are statistically significant. The root mean square error of approximation = 0.04, the weighted root mean square residual = 0.77, the comparative fit index = 0.97, and R2 = 0.62.
aP < .05.
bP < .01.
cP < .001.
Discussion
In this longitudinal study of the familial transmission of suicidal behavior, parental suicide attempt conveyed a nearly 5-fold increased odds of suicide attempts in offspring, even after accounting for a history of previous suicide attempt in offspring and the familial transmission of mood disorder. In addition, impulsive aggression was an important precursor of mood disorder in offspring, which in turn increased the risk of an offspring suicide attempt.
We hypothesized that suicidal behavior would be familially transmitted via the transmission of impulsive aggression.3,5,6,8 However, the pathway from proband to offspring attempt via proband Cluster B disorder, offspring impulsive aggression, and mood disorder to offspring attempt was not statistically significant (P = .08). One possible explanation for the difference between previous and current findings in this study is that as participants aged, the incidence of depression in offspring increased, from 29.6% after a 1- to 2-year follow-up11 to 48.2% in the current study. In fact, impulsive aggression played an important role in increasing the likelihood of an offspring suicide attempt, but it did so by increasing the risk of the subsequent development of a mood disorder, which in turn increased the risk of an attempt. This link between impulsive aggression and onset of mood disorder is consistent with longitudinal studies46–49 of youth with attention-deficit/hyperactivity disorder, oppositional defiant disorder, or high irritability scores, in which impulsive aggression and the related constructs (eg, irritability) predicted the onset of depression and suicide attempts. The transition from impulsive aggression to mood disorder may be particularly salient to understanding recurrent suicidal behavior because this pathway from offspring suicide attempt at baseline to an attempt at follow-up was mediated by offspring impulsive aggression and mood disorder.
Although the familial transmission of attempts occurs independently of the transmission of mood disorder, the transmission of mood disorder was also a significant pathway to early-onset suicidal behavior. Mood disorders are prominent among adolescents who attempt or die by suicide.50–52 Therefore, the prevention and treatment of mood disorders in youth are logical approaches for reducing the incidence of suicide attempts. The sequencing of risk factors over time is consistent with the stress-diathesis model of suicidal risk, with the diathesis being parental history of suicidal attempt and more proximal stressors that contribute to imminent suicidal risk, such as negative life events and mood disorder, at the time point immediately before the suicide attempt.13
We failed to find a role for child maltreatment in the intrafamilial transmission of suicidal behavior, in contradistinction to earlier reports.9–11 Offspring abuse was related to onset of mood disorder and suicidal behavior, but after correction for multiple comparisons, this association was not statistically significant. Differences between this and previous reports might be because previous reports were cross-sectional or covered relatively short periods, had relatively few suicide attempts among offspring, or because of the increased cumulative risk of depression in offspring.
This study, to our knowledge, is one of the few prospective studies to examine the familial transmission of suicidal behavior, with a large, well-characterized sample. Limitations include the lack of data on most biological coparents and participant attrition. Fortunately, no baseline characteristics are associated with attrition, and the results using Cox proportional hazards regression analyses were similar to those obtained by logistic regression, suggesting that our findings are not accounted for by differential retention. Probands are mostly female, so we lack power to detect whether the effect of maternal suicide attempt is greater than the effect of paternal suicide attempt, as is suggested by some studies.53,54 One-third of our probands had bipolar disorder. However, our risk models were similar regardless of offspring or proband polarity, consistent with other studies55–57 that found similar risk factors for suicidal behavior in individuals with unipolar and bipolar disorders.
Clinical implications of these results include the importance of assessment and early intervention in the families of parents with mood disorders and a history of a suicide attempt. The prevention of the onset of depression may attenuate the familial transmission of suicidal behavior, which could be tested with efficacious preventive interventions to reduce the risk of onset of depression in high-risk youth.58,59 Given that many of the parental suicide attempters had Cluster B disorder, efficacious interventions for this condition may also have beneficial effects on the parent-child relationship and offspring functional outcome.60 Because impulsive aggression can be a precursor to mood disorder, which in turn elevates suicidal risk, helping youth with prominent irritability and impulsive aggression to achieve better emotion regulation may reduce suicidal risk by diminishing the risk for mood disorder and the likelihood of acting on suicidal impulses.52,61 The primary school classroom-based preventive intervention, the Good Behavior Game, has promise in reducing the risk of adolescent-onset suicidal ideation and behavior.62
Conclusions
In this high-risk longitudinal study, we found that parental suicide attempt conveyed a nearly 5-fold increased risk of offspring attempt, even controlling for the familial transmission of mood disorder. Impulsive aggression was an important precursor of mood disorder and could be targeted in interventions designed to prevent youth at high familial risk from making a suicide attempt. Future work should focus on the deconstruction of suicidal behavior into intermediate biobehavioral phenotypes to further elucidate mechanisms by which suicidal behavior is transmitted from parent to child.63 Promising intermediate phenotypes include impaired decision making and executive function, difficulty with emotion regulation, and alterations in the hypothalamic-pituitary-adrenal axis at baseline and in response to social stress.63
Supplementary Material
Acknowledgments
Funding/Support: This study was supported by grants MH056612 (Dr Brent), MH056390 (Dr Mann), and MH077930 (Dr Melhem) from the National Institute of Mental Health and a Young Investigator Award from the American Foundation for Suicide Prevention (Dr Melhem).
Footnotes
Supplemental content at jamapsychiatry.com
Additional Contributions: The following project staff from the University of Pittsburgh provided outstanding work on this project: Joseph Park, MA, who participated in manuscript preparation; Monica Walker Payne, MA, who provided leadership with project coordination; Thomas Hahner, MS, and Emily Hogan, MSCP, LPC, NCC, who worked as clinical interviewers; Irina Puchkareva, MS, who assisted with database management; and Dana Kaufman, BFA, who assisted with database entry.
Author Contributions: Dr Brent has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Brent, Melhem, Oquendo, Birmaher, Keilp, Stanley, Mann.
Acquisition, analysis, or interpretation of data: Brent, Melhem, Oquendo, Burke, Birmaher, Stanley, Biernesser, Kolko, Ellis, Porta, Zelazny, Iyengar, Mann.
Drafting of the manuscript: Brent, Oquendo, Birmaher.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Brent, Melhem, Oquendo, Birmaher, Ellis, Porta, Iyengar.
Obtained funding: Brent, Melhem, Oquendo, Birmaher, Keilp, Iyengar, Mann.
Administrative, technical, or material support: Brent, Oquendo, Stanley, Biernesser, Kolko, Mann.
Study supervision: Brent, Melhem, Burke, Biernesser, Keilp, Zelazny, Mann.
Conflict of Interest Disclosures: In the 3 years before submission, Dr Oquendo reported receiving unrestricted educational grants from AstraZeneca, Janssen, Bristol Myers Squibb, Pfizer, Eli Lilly, and Shire, receiving royalties from the Columbia Suicide Severity Rating Scale (C-SSRS), and receiving royalties from the electronic self-rated version of the C-SSRS from ERT Inc. Her family owns stock in Bristol Myers Squibb. Dr Stanley reported receiving royalties from the C-SSRS, receiving royalties from the electronic self-rated version of the C-SSRS from ERT Inc, and receiving support from grants from the National Institutes of Health and the American Foundation for Suicide Prevention. Dr Birmaher reported receiving research support from the National Institute of Mental Health and receiving royalties from Random House Inc, Lippincott Williams & Williams, and Up To Date. Dr Burke reported receiving royalties from the C-SSRS. Dr Mann reported receiving royalties for commercial use of the C-SSRS from the Research Foundation for Mental Hygiene and having stock options in Qualitas Health, a start-up company developing an eicosapentaenoic acid food supplement. Dr Kolko reported receiving funding for federal research grants from the National Institute of Mental Health and the Substance Abuse and Mental Health Services Administration. Dr Brent reported receiving royalties from Guilford Press, receiving royalties from the electronic self-rated version of the C-SSRS from ERT Inc, and serving on the editorial board of UpToDate. No other disclosures were reported.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
References
- 1.Brent DA, Melhem N. Familial transmission of suicidal behavior. Psychiatr Clin North Am. 2008;31 (2):157–177. doi: 10.1016/j.psc.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brent DA, Bridge J, Johnson BA, Connolly J. Suicidal behavior runs in families: a controlled family study of adolescent suicide victims. Arch Gen Psychiatry. 1996;53(12):1145–1152. doi: 10.1001/archpsyc.1996.01830120085015. [DOI] [PubMed] [Google Scholar]
- 3.Lieb R, Bronisch T, Höfler M, Schreier A, Wittchen HU. Maternal suicidality and risk of suicidality in offspring: findings from a community study. Am J Psychiatry. 2005;162(9):1665–1671. doi: 10.1176/appi.ajp.162.9.1665. [DOI] [PubMed] [Google Scholar]
- 4.Mann JJ, Bortinger J, Oquendo MA, Currier D, Li S, Brent DA. Family history of suicidal behavior and mood disorders in probands with mood disorders. Am J Psychiatry. 2005;162(9):1672–1679. doi: 10.1176/appi.ajp.162.9.1672. [DOI] [PubMed] [Google Scholar]
- 5.Kim CD, Seguin M, Therrien N, et al. Familial aggregation of suicidal behavior: a family study of male suicide completers from the general population. Am J Psychiatry. 2005;162(5):1017–1019. doi: 10.1176/appi.ajp.162.5.1017. [DOI] [PubMed] [Google Scholar]
- 6.McGirr A, Alda M, Séguin M, Cabot S, Lesage A, Turecki G. Familial aggregation of suicide explained by cluster B traits: a three-group family study of suicide controlling for major depressive disorder. Am J Psychiatry. 2009;166(10):1124–1134. doi: 10.1176/appi.ajp.2009.08111744. [DOI] [PubMed] [Google Scholar]
- 7.Brent DA, Oquendo M, Birmaher B, et al. Familial transmission of mood disorders: convergence and divergence with transmission of suicidal behavior. J Am Acad Child Adolesc Psychiatry. 2004;43(10):1259–1266. doi: 10.1097/01.chi.0000135619.38392.78. [DOI] [PubMed] [Google Scholar]
- 8.Brent DA, Oquendo M, Birmaher B, et al. Peripubertal suicide attempts in offspring of suicide attempters with siblings concordant for suicidal behavior. Am J Psychiatry. 2003;160(8):1486–1493. doi: 10.1176/appi.ajp.160.8.1486. [DOI] [PubMed] [Google Scholar]
- 9.Brent DA, Oquendo M, Birmaher B, et al. Familial pathways to early-onset suicide attempt: risk for suicidal behavior in offspring of mood-disordered suicide attempters. Arch Gen Psychiatry. 2002;59 (9):801–807. doi: 10.1001/archpsyc.59.9.801. [DOI] [PubMed] [Google Scholar]
- 10.Brodsky BS, Mann JJ, Stanley B, et al. Familial transmission of suicidal behavior: factors mediating the relationship between childhood abuse and offspring suicide attempts. J Clin Psychiatry. 2008;69(4):584–596. doi: 10.4088/jcp.v69n0410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melhem NM, Brent DA, Ziegler M, et al. Familial pathways to early-onset suicidal behavior: familial and individual antecedents of suicidal behavior. Am J Psychiatry. 2007;164(9):1364–1370. doi: 10.1176/appi.ajp.2007.06091522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47(3–4):372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- 13.Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156(2):181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 14.Fazel S, Wolf A, Pillas D, Lichtenstein P, Långström N. Suicide, fatal injuries, and other causes of premature mortality in patients with traumatic brain injury: a 41-year Swedish population study. JAMA Psychiatry. 2014;71(3):326–333. doi: 10.1001/jamapsychiatry.2013.3935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Posner K, Oquendo MA, Gould M, Stanley B, Davies M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164(7):1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mann JJ, McBride PA, Brown RP, et al. Relationship between central and peripheral serotonin indexes in depressed and suicidal psychiatric inpatients. Arch Gen Psychiatry. 1992;49 (6):442–446. doi: 10.1001/archpsyc.1992.01820060022003. [DOI] [PubMed] [Google Scholar]
- 17.Oquendo MA, Halberstam B, Mann JJ. Risk factors for suicidal behavior: the utility and limitations of research instruments. In: First MB, editor. Standardized Evaluation in Clinical Practice. Washington, DC: American Psychiatric Publishing; 2003. pp. 103–129. [Google Scholar]
- 18.Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–1277. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47(2):343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 20.Kazdin AE, French NH, Unis AS, Esveldt-Dawson K, Sherick RB. Hopelessness, depression, and suicidal intent among psychiatrically disturbed inpatient children. J Consult Clin Psychol. 1983;51(4):504–510. doi: 10.1037//0022-006x.51.4.504. [DOI] [PubMed] [Google Scholar]
- 21.Brown GL, Goodwin FK. Human aggression and suicide. Suicide Life Threat Behav. 1986;16(2):223–243. doi: 10.1111/j.1943-278x.1986.tb00353.x. [DOI] [PubMed] [Google Scholar]
- 22.Spitzer R, Williams J, Gibbon M, First M. Structured Clinical Interview for DSM-IV (SCID) New York: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- 23.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 24.First M, Spitzer R, Gibbon M, Williams J, Benjamin L. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) (Version 2.0) New York: Biometrics Research Department, New York Psychiatric Institute; 1996. [Google Scholar]
- 25.Hollingshead A. Four Factor Index of Social Status. New Haven, CT: Yale University; 1975. [Google Scholar]
- 26.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 27.Kovacs M. The Children’s Depression, Inventory (CDI) Psychopharmacol Bull. 1985;21(4):995–998. [PubMed] [Google Scholar]
- 28.Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42(6):861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 29.Kazdin AE, Rodgers A, Colbus D. The hopelessness scale for children: psychometric characteristics and concurrent validity. J Consult Clin Psychol. 1986;54(2):241–245. doi: 10.1037//0022-006x.54.2.241. [DOI] [PubMed] [Google Scholar]
- 30.Buss AH, Durkee A. An inventory for assessing different kinds of hostility. J Consult Psychol. 1957;21(4):343–349. doi: 10.1037/h0046900. [DOI] [PubMed] [Google Scholar]
- 31.Kazdin AE, Rodgers A, Colbus D, Siegel T. Children’s Hostility Inventory: measurement of aggression and hostility in psychiatric inpatient children. J Clin Child Psychol. 1987;16(4):320–328. [Google Scholar]
- 32.Barratt ES. Factor analysis of some psychometric measures of impulsiveness and anxiety. Psychol Rep. 1965;16:547–554. doi: 10.2466/pr0.1965.16.2.547. [DOI] [PubMed] [Google Scholar]
- 33.Pelham WE, Jr, Milich R, Murphy DA, Murphy HA. Normative data on the IOWA Conners teacher rating scale. J Clin Child Psychol. 1989;18(3):259–262. [Google Scholar]
- 34.Lewinsohn PM, Rohde P, Seeley JR, Fischer SA. Age and depression: unique and shared effects. Psychol Aging. 1991;6(2):247–260. doi: 10.1037//0882-7974.6.2.247. [DOI] [PubMed] [Google Scholar]
- 35.Brand AH, Johnson JH. Note on reliability of the Life Events Checklist. Psychol Rep. 1982;50:1274. [Google Scholar]
- 36.Zimet G, Dahlem N, Zimet S, Farley G. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52:30–41. [Google Scholar]
- 37.Dubow E, Ullman D. Assessing social support in elementary school children: The Survey of Children’s Social Support. J Clin Child Psychol. 1989;18(1):52–64. [Google Scholar]
- 38.Ivanoff A, Jang S, Smyth N, Linehan M. Fewer reasons for staying alive when you are thinking of killing yourself: The Brief Reasons for Living Inventory. J Psychopathol Behav Assess. 1994;16(1):1–13. [Google Scholar]
- 39.Osman A, Downs WR, Kopper BA, et al. The Reasons for Living Inventory for Adolescents (RFL-A): development and psychometric properties. J Clin Psychol. 1998;54(8):1063–1078. doi: 10.1002/(sici)1097-4679(199812)54:8<1063::aid-jclp6>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 40.Olsen D, Portner J, Bell R. Family Adaptability and Cohension Evaluation Scales (FACES-II) Minneapolis: University of Minnesota Press; 1982. [Google Scholar]
- 41.Chaffin M, Wherry J, Newlin C, Crutchfield A, Dykman R. The Abuse Dimensions Inventory: initial data on a research measure of abuse severity. J Interpers Violence. 1997;12(4):569–589. [Google Scholar]
- 42.Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151(8):1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 43.Yekutieli D, Benjamini Y. Resampling-based false discovery rate controlling multiple test procedures for correlated test statistics. J Stat Plan Inference. 1999;82(1):171–196. [Google Scholar]
- 44.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Academic Press; 1977. Rev. [Google Scholar]
- 45.Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- 46.Burke JD. An affective dimension within oppositional defiant disorder symptoms among boys: personality and psychopathology outcomes into early adulthood. J Child Psychol Psychiatry. 2012;53(11):1176–1183. doi: 10.1111/j.1469-7610.2012.02598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hipwell AE, Stepp S, Feng X, et al. Impact of oppositional defiant disorder dimensions on the temporal ordering of conduct problems and depression across childhood and adolescence in girls. J Child Psychol Psychiatry. 2011;52(10):1099–1108. doi: 10.1111/j.1469-7610.2011.02448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chronis-Tuscano A, Molina BS, Pelham WE, et al. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2010;67(10):1044–1051. doi: 10.1001/archgenpsychiatry.2010.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stringaris A, Zavos H, Leibenluft E, Maughan B, Eley TC. Adolescent irritability: phenotypic associations and genetic links with depressed mood. Am J Psychiatry. 2012;169(1):47–54. doi: 10.1176/appi.ajp.2011.10101549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brent DA, Perper JA, Goldstein CE, et al. Risk factors for adolescent suicide: a comparison of adolescent suicide victims with suicidal inpatients. Arch Gen Psychiatry. 1988;45(6):581–588. doi: 10.1001/archpsyc.1988.01800300079011. [DOI] [PubMed] [Google Scholar]
- 51.Shaffer D, Gould MS, Fisher P, et al. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry. 1996;53(4):339–348. doi: 10.1001/archpsyc.1996.01830040075012. [DOI] [PubMed] [Google Scholar]
- 52.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70 (3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuramoto SJ, Stuart EA, Runeson B, Lichtenstein P, Långström N, Wilcox HC. Maternal or paternal suicide and offspring’s psychiatric and suicide-attempt hospitalization risk. Pediatrics. 2010;126(5):e1026–e1032. doi: 10.1542/peds.2010-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Agerbo E, Nordentoft M, Mortensen PB. Familial, psychiatric, and socioeconomic risk factors for suicide in young people: nested case-control study. BMJ. 2002;325(7355):74–77. doi: 10.1136/bmj.325.7355.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Goldstein TR, Ha W, Axelson DA, et al. Predictors of prospectively examined suicide attempts among youth with bipolar disorder. Arch Gen Psychiatry. 2012;69(11):1113–1122. doi: 10.1001/archgenpsychiatry.2012.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Abreu LN, Lafer B, Baca-Garcia E, Oquendo MA. Suicidal ideation and suicide attempts in bipolar disorder type I: an update for the clinician. Rev Bras Psiquiatr. 2009;31(3):271–280. doi: 10.1590/s1516-44462009005000003. [DOI] [PubMed] [Google Scholar]
- 57.Halfon N, Labelle R, Cohen D, Guilé JM, Breton JJ. Juvenile bipolar disorder and suicidality: a review of the last 10 years of literature. Eur Child Adolesc Psychiatry. 2013;22(3):139–151. doi: 10.1007/s00787-012-0328-z. [DOI] [PubMed] [Google Scholar]
- 58.Garber J, Clarke GN, Weersing VR, et al. Prevention of depression in at-risk adolescents: a randomized controlled trial. JAMA. 2009;301(21):2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Compas BE, Forehand R, Thigpen JC, et al. Family group cognitive-behavioral preventive intervention for families of depressed parents: 18-and 24-month outcomes. J Consult Clin Psychol. 2011;79(4):488–499. doi: 10.1037/a0024254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lynch TR, Trost WT, Salsman N, Linehan MM. Dialectical behavior therapy for borderline personality disorder. Annu Rev Clin Psychol. 2007;3:181–205. doi: 10.1146/annurev.clinpsy.2.022305.095229. [DOI] [PubMed] [Google Scholar]
- 61.Nock MK, Stein MB, Heeringa SG, et al. Army STARRS Collaborators. Prevalence and correlates of suicidal behavior among soldiers: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) JAMA Psychiatry. 2014;71(5):514–522. doi: 10.1001/jamapsychiatry.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wilcox HC, Kellam SG, Brown CH, et al. The impact of two universal randomized first- and second-grade classroom interventions on young adult suicide ideation and attempts. Drug Alcohol Depend. 2008;95(suppl 1):S60–S73. doi: 10.1016/j.drugalcdep.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mann JJ, Arango VA, Avenevoli S, et al. Candidate endophenotypes for genetic studies of suicidal behavior. Biol Psychiatry. 2009;65(7):556–563. doi: 10.1016/j.biopsych.2008.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.