Abstract
Efforts to study relationships between maternal airborne pollutant exposures and poor pregnancy outcomes have been frustrated by data limitations. Our objective was to report the proportion of Ohio women in 2006–2010 experiencing stillbirth whose pregnancy exposure to six criteria airborne pollutants could be approximated by applying a geospatial approach to vital records and Environmental Protection Agency air monitoring data. In addition, we characterized clinical and socio-demographic differences among women who lived within 10 km of monitoring stations compared to women who did not live within proximity of monitoring stations. For women who experienced stillbirth, 10.8% listed a residence within 10 km of each type of monitoring station. Maternal race, education, and marital status were significantly different (p<0.0001) comparing those within proximity to monitoring stations to those outside of monitoring range. No significant differences were identified in maternal age, ethnicity, smoking status, hypertension, or diabetes between groups.
Background
Despite a steady decline over the previous two decades, the United States stillbirth rate of 6.0 per 1,000 births in 2006 remained substantially higher than that of other high income countries.1–3 The national stillbirth rate (defined as fetal deaths occurring at or beyond 20 weeks of gestation) also remained 50% above the Healthy People 2010 goal of 4.1 per 1,000 leading to a revised goal for Healthy People 2020 of 5.6 per 1,000.4, 5 While, obesity, maternal age, and smoking are significant modifiable risk factors for stillbirth, other clinical, genetic, socioeconomic, and environmental factors are also important contributors to a woman’s risk of stillbirth.6, 7 Although methodological limitations in previously reported studies have yielded mixed and inconclusive results, identifying the effects of maternal exposure to airborne pollutants on fetal development and birth outcomes remains a research priority.8, 9
The Environmental Protection Agency (EPA) lists six criteria pollutants representing agents harmful to public health.10 These include carbon monoxide (CO), lead (Pb), nitrogen dioxide (NO2), ozone (O3), particle pollution, and sulfur dioxide (SO2). Pollutants are monitored at regular intervals by stations at fixed locations, though exposures of individuals residing nearby may be approximated. Exposure estimates rely on linking data representing air quality with clinical and socio-demographic measures of individuals. Previous analyses of associations between the criteria pollutants and stillbirth have been limited in analytic design as a consequence of relevant data residing in incompatible systems.11–17 Former study limitations include inadequate temporal and geographic granularity and insufficient controlling for socio-demographic risk factors. Additionally, previous efforts have typically focused on single pollutant exposures rather than considering exposures to multiple pollutants or the combined effects of multiple pollutant exposures.
A recent study utilizing a geospatial approach identified an association between stillbirth and maternal exposure to pollutants by linking vital records to data from the EPA Air Quality System.18 However, this type of analysis may also be limited by proximity of mothers to EPA monitoring stations, particularly when conducting analysis of multiple exposure types. The fixed number of monitoring stations as well as the placement of stations near urban settings may limit the coverage and representativeness of population data obtained from the EPA.
The objective of this Ohio statewide study was to describe the coverage and utility of existing air monitoring data to support investigations of maternal pollutant exposures when integrated with vital statistics. This was achieved by 1) identifying among women who experienced a live or stillbirth, the proportion who resided within proximity to an EPA air monitoring station 2) characterizing clinical and socio-demographic differences among women who lived within range of all types of monitoring stations compared to women who did not live within proximity of any air monitoring stations. This study builds upon previous efforts in developing maternal-child health data resources by integrating disparate data sets including vital statistics, hospital discharge data, geospatially-based measures from the American Communities Survey, and community-based program data.19, 20 Integration of air quality data provides an additional dimension for investigating the complex interplay of factors contributing to stillbirth and other perinatal outcomes.
Methods
The geospatial population-based cohort study incorporated data from two primary sources, vital records and air monitoring measures. Vital records including fetal death records as well as live birth records were obtained from the Ohio Department of Health representing 4,622 stillbirths and 751,123 live births occurring in Ohio during 2006–2010. The study set was reduced to singleton births with documented gestational age between 20 and 42 weeks and with documented birth weight of at least 350 grams. Additionally, infants with confirmed chromosomal anomalies were not included in the final study set. Lastly, births occurring within Ohio corresponding to mothers reporting residence outside of the state were excluded resulting in a final study set of 3,090 stillbirths and 707,110 live births (Table 1). Basic demographic and clinical measures including maternal race and ethnicity, age, marital status, level of education, smoking status, and diagnosis of hypertension or diabetes were also obtained from vital records data.
TABLE 1.
Study exclusion criteria and final sample
| Exclusion Criteria | Stillbirths | Live births |
|---|---|---|
| Records of birth events within Ohio, 2006–2010 | 4,622 | 751,123 |
| Missing gestational age, gestational sge < 20 weeks, or gestational age > 42 weeks | 52 | 2,910 |
| Birth weight <350 grams | 954 | 366 |
| Chromosomal anomalies | 128 | 685 |
| Multiple gestation | 86 | 26,995 |
| Residence outside of Ohio | 113 | 13,057 |
|
| ||
| Final study set | 3,090 | 707,110 |
Measures of criteria pollutants were obtained from the EPA representing CO, Pb, NO2, O3, SO2 and fine particulate matter measuring less than 2.5 μm in aerodynamic diameter (PM2.5).21 Data were obtained from Ohio air monitoring stations representing pollutant level measures at time periods ranging from hourly to every few days. Data were obtained for 2005 through 2010 to correspond with the pregnancy timeframes represented by the vital records data set. Each pollutant was measured by a unique set of stations, with a range of six to 59 locations in Ohio. Although some stations measured a single pollutant, other stations obtained multiple measures. In all, measures of pollutant levels for the six criteria pollutants were captured at 126 unique geospatial coordinates across the state. Using all measures captured for each pollutant at each location, monthly average measures were calculated for every calendar month of the study period.
Linkage between vital records and air pollution data was performed using ArcGIS 10.1 (ESRI, Redlands, CA). Station locations were geocoded with a latitude-longitude coordinate pair as were maternal residences reported at the time of birth. When specific address information was missing, residence was approximated using the centroid of the residence zip code. For each live or stillbirth record, the closest monitoring station was identified for each pollutant. Additionally, the distance to the nearest monitoring station of each pollutant type was calculated.
The number of birth events listing maternal residence within five, 10, and 15 km of a monitoring station was calculated for each pollutant. We also determined the set of women residing within proximity to monitoring stations for each of the six criteria pollutants as well as the set of women who were not within the proximity of five, 10, or 15 km of any criteria pollutant monitoring stations. Additional analyses were conducted for the women within proximity to all six monitor types compared to women outside of the coverage range of any monitoring station. Consistent with methods used in previous analyses, proximity for the additional analysis was defined as 10 km.18, 22
Statistical analysis and calculations were conducted using SAS version 9.3 (SAS Institute Inc., Cary, NC) software. Bivariate χ2- or t-tests analyses were performed to identify demographic and clinical differences between populations within proximity to all six pollutant monitors and those outside the proximity of any monitoring station. Because multiple tests were performed, a Bonferroni-Holm correction was implemented to determine significance.23
Next, estimated exposures to each pollutant were calculated for each pregnancy trimester and for the entire duration of pregnancy. The initiation of the pregnancy was estimated by subtracting the clinical estimate of gestational age from the documented date of delivery. The first trimester was defined as weeks 0 through 12, the second trimester as weeks 13 through 27 and the third trimester as weeks 28 through 42. Exposures were estimated by first identifying the average monitoring station measure for the calendar month corresponding to each pregnancy month. Whole pregnancy and per trimester exposure estimates were calculated using monthly monitor measures for which the mother was pregnant for at least half of the calendar month, or for which the pregnancy trimester spanned at least half of the calendar month. For each pregnancy stage, mean population exposures for stillbirth and live birth outcomes were then calculated using exposure estimate calculations for individual mothers. The Ohio Department of Health and University of Cincinnati Institutional Review Boards approved this study.
Results
For both stillbirth and live birth sets, the mean and median distance from each residence to the nearest station monitoring each of the criteria pollutants is recorded in Table 2. For all six of the criteria pollutants, the average distances between residences and stations were inversely related to the number of monitoring stations.
TABLE 2.
Number of monitoring stations for each pollutant and the average distance between stations and maternal residence at the time of live or stillbirth event.
| Pollutant | Number of stations | Distance from stillbirth residence to nearest station (km) (mean, median) | Distance from live birth residence to nearest station (km) (mean, median) | ||
|---|---|---|---|---|---|
| CO | 17 | 36.1, | 17.6 | 40.7, | 19.8 |
| Pb | 20 | 24.8, | 16.5 | 29.5, | 17.7 |
| NO2 | 6 | 68.1, | 49.1 | 72.3, | 66.2 |
| O3 | 59 | 14.4, | 14.8 | 18.3, | 9.9 |
| PM2.5 | 57 | 16.3, | 8.6 | 20.7, | 10.0 |
| SO2 | 39 | 20.5, | 14.4 | 24.4, | 15.9 |
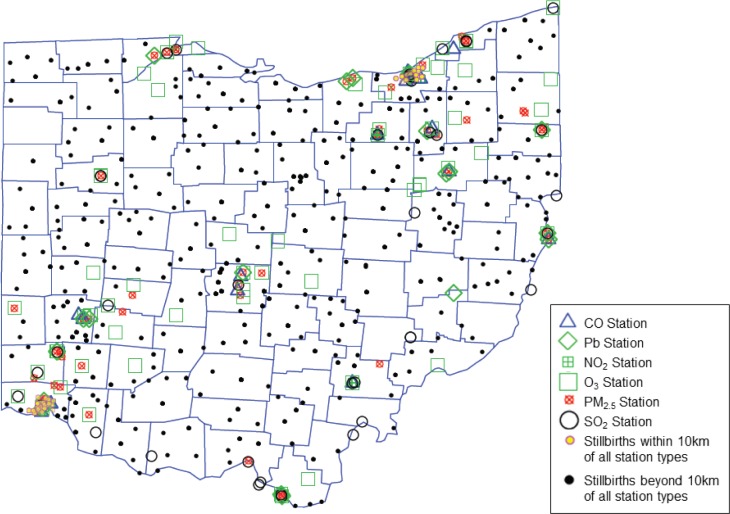
Table 3 lists the number of stillbirth and live birth events listing a residence within a 5, 10, and 15 km radius from each monitoring station. The proportion of the 3,090 stillbirths and 707,110 live births covered by each radius is also reported. Additionally, the number and proportion of births with residence within range of all six criteria pollutant monitoring station types is listed. Ozone and PM2.5 monitoring stations had the best coverage with over 55% of stillbirths and nearly 50% of live births having a corresponding maternal residence within 10 km from a station. Just 10.8% of the stillbirth and 8.1% of the live birth population listed a residence within 10 km of each of the six monitoring station types. On the other hand, 33.6% of the stillbirth and 39.1% of the live birth population listed a residence that was more than 10 km from any of the six monitoring station types (Figure 1).
TABLE 3.
Number and percentage of 3,090 stillbirths and 707,110 live births within range of pollution monitoring stations.
| Pollutant | Stillbirths within 5 km |
Stillbirths within 10 km |
Stillbirths within 15 km |
Live births within 5 km |
Live births within 10 km |
Live births within 15 km |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CO | 611 | 19.8% | 1,061 | 34.3% | 1,428 | 46.2% | 93,658 | 13.2% | 200,399 | 28.3% | 288,023 | 40.7% |
| Pb | 527 | 17.1% | 1,107 | 35.8% | 1,451 | 47.0% | 81,601 | 11.5% | 202,609 | 28.7% | 299,932 | 42.4% |
| NO2 | 237 | 7.7% | 446 | 14.4% | 574 | 18.6% | 34,487 | 4.9% | 80,334 | 11.4% | 114,228 | 16.2% |
| O3 | 728 | 23.6% | 1,741 | 56.3% | 2,198 | 71.1% | 137,521 | 19.4% | 350,055 | 49.5% | 474,048 | 67.0% |
| PM2.5 | 1,004 | 32.5% | 1,782 | 57.7% | 2,095 | 67.8% | 173,391 | 24.5% | 345,782 | 48.9% | 447,803 | 63.3% |
| SO2 | 516 | 16.7% | 1,104 | 35.7% | 1,583 | 51.2% | 88,784 | 12.6% | 219,416 | 31.0% | 329,355 | 46.6% |
|
| ||||||||||||
| All | 104 | 3.4% | 335 | 10.8% | 505 | 16.3% | 14,632 | 2.1% | 57,271 | 8.1% | 96,676 | 13.7% |
| None | 1,809 | 58.5% | 1,037 | 33.6% | 738 | 23.9% | 457,085 | 64.6% | 276,543 | 39.1% | 182,622 | 25.8% |
FIGURE 1.
Locations of 126 monitoring station locations throughout Ohio along with points indicating stillbirths with residence within 10 km of all six criteria pollutants monitoring stations and with residence beyond 10 km from any monitoring station.
Characteristics of the stillbirth and live birth populations are listed in Table 4. Also in the table, clinical and demographic characteristics are further stratified into categories of women who reported a residence within 10 km of each of the six types of monitoring stations and women whose residence was more than 10 km from any station type. Among women who experienced a stillbirth, race, education, and marital status had significant differences between groups. However, no significant differences were identified in age, ethnicity, smoking status, hypertension, or diabetes between groups. Among the large live birth set, all comparisons yielded significance in comparisons between groups.
TABLE 4.
Clinical and demographic characteristics of the stillbirth and live birth study populations including a comparison of women with a residence within 10 km of all six monitoring station types and women with a residence more than 10 km from every monitoring station type.
| All stillbirths (N=3,090) | Stillbirths (N=3,090) | All live births (N=707,110) | Live births (N=707,110) | |||||
|---|---|---|---|---|---|---|---|---|
| Residence near 0 station types (n=1,037) | Residence near all 6 stations types (n=335) | p-value | Residence near 0 station types (n=276,543) | Residence near all 6 stations types (n=57,271) | p-value | |||
| Age (mean) | 27.1 | 27.1 | 26.4 | 0.2 | 26.7 | 27.1 | 25.5 | < 0.0001* |
| Race (%) | < 0.0001* | < 0.0001* | ||||||
| White | 66.2 | 89.7 | 22.4 | 79.7 | 93.9 | 41.8 | ||
| Black | 29.6 | 6.0 | 74.0 | 17.2 | 4.1 | 55.7 | ||
| Other | 4.2 | 4.3 | 3.6 | 3.2 | 2.0 | 2.5 | ||
| Hispanic ethnicity (%) | 5.8 | 4.5 | 6.6 | 0.1 | 4.6 | 3.4 | 7.7 | < 0.0001* |
| Maternal education (%) | < 0.0001* | < 0.0001* | ||||||
| No high school degree | 20.4 | 16.8 | 27.9 | 17.6 | 15.1 | 30.7 | ||
| High school degree | 40.3 | 43.6 | 43.5 | 26.6 | 28.4 | 27.5 | ||
| Any college | 39.3 | 39.6 | 28.6 | 55.8 | 56.5 | 41.8 | ||
| Married (%) | 48.0 | 63.8 | 27.6 | < 0.0001* | 57.3 | 65.5 | 30.3 | < 0.0001* |
| Smoker (%) | 23.7 | 25.1 | 22.4 | 0.3 | 19.7 | 20.6 | 19.5 | < 0.0001* |
| Hypertension (%) | 9.5 | 9.3 | 13.7 | 0.08 | 6.2 | 6.2 | 6.9 | < 0.0001* |
| Diabetes (%) | 7.3 | 6.9 | 8.4 | 0.7 | 5.8 | 5.7 | 5.1 | < 0.0001* |
statistical significance
Exposures to each of the six pollutants are presented in Table 5 for both stillbirth and live birth data sets. Mean exposures are listed for each pregnancy trimester and for the pregnancy duration representing all estimated exposures having a residence within 10 km of the relevant station type. Only exposures to PM2.5 exceeded EPA standards; however the high exposure rates affected both stillbirth and live birth populations.
TABLE 5.
Calculated trimester and pregnancy exposure estimates of within 10 km of a pollution monitoring station compared to Environmental Protection Agency (EPA) standard.
| Stillbirths | Live births | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pollutant | EPA Standard10 | Stillbirths within 10 km | First trimester exposure (mean±sd) | Second trimester exposure (mean±sd) | Third trimester exposure (mean±sd) | Whole pregnancy exposure (mean±sd) | Live births within 10 km | First trimester exposure (mean±sd) | Second trimester exposure (mean±sd) | Third trimester exposure (mean±sd) | Whole pregnancy exposure (mean±sd) |
| CO (ppm) | 9 (8-hour average) | 1,061 | 0.38±0.12 | 0.37±0.12 | 0.37±0.13 | 0.37±0.11 | 200,399 | 0.39±0.13 | 0.39±0.13 | 0.38±0.14 | 0.39±0.11 |
| Pb (μg/m3) | 0.15 (rolling 3 month average) | 1,107 | 0.1±0.0 | 0.1±0.0 | 0.0±0.0 | 0.1±0.0 | 202,609 | 0.1±0.0 | 0.1±0.0 | 0.1±0.0 | 0.1±0.0 |
| NO2 (ppb) | 100 (1-hour average) | 446 | 16.5±2.9 | 16.5±3.6 | 16.0±3.0 | 16.4±2.7 | 80,334 | 16.9±3.5 | 16.6±3.6 | 16.3±3.6 | 16.7±3.3 |
| O3(ppm) | 0.075 (8-hour average) | 1,741 | 0.03±0.01 | 0.03±0.01 | 0.03±0.01 | 0.03±0.01 | 350,055 | 0.03±0.01 | 0.03±0.01 | 0.03±0.01 | 0.03±0.01 |
| PM2.5 (μg/m3) | 12 (annual average) | 1,782 | 13.6±2.8 | 13.2±2.3 | 13.3±2.8 | 13.3±1.8 | 345,782 | 13.7±2.9 | 13.3±2.4 | 13.0±2.3 | 13.3±1.8 |
| SO2 (ppb) | 75 (1-hour average) | 1,104 | 3.5±1.9 | 3.4±2.0 | 3.5±2.3 | 3.4±1.8 | 219,416 | 3.8±2.1 | 3.6±2.1 | 3.5±2.1 | 3.6±1.9 |
sd= standard deviation
ppm = parts per million
ppb = parts per billion
Discussion
The linkage approach described in this manuscript has potential to enable powerful analyses of pollution effects on stillbirth as well as other pregnancy related outcomes. The final linked study data set joined measures from the EPA and vital record sets providing a data set containing socio-demographic measures at the individual person level along with pollution exposure approximations customized both temporally and spatially to each individual pregnancy. Exposure approximations for each trimester of pregnancy enable additional analyses about the stages of fetal development that may be most susceptible to high levels of pollutant exposure. This approach has already provided insight into the impact of high PM2.5 exposure levels on stillbirth. In a previous analysis we found a 42% increase in stillbirth risk associated with increased PM2.5 exposure during the third trimester of pregnancy.24 Further, we estimated that up to 2.2 per 1,000 Ohio stillbirths are potentially attributable to high levels of PM2.5 exposure.
Efforts to use this approach to estimate pregnancy exposures to all six criteria pollutants using a maximum of 10 km distance between residence and monitoring stations would be limited to less than 11% of the Ohio stillbirth and about 8% of the live birth populations. Also the analysis would be restricted to residents of the urban Cincinnati and Cleveland regions. Although this geospatial approach for approximating exposure may be sufficient for single particulate analysis, reliance of residence in close proximity to air monitoring stations is a considerable limitation to the analysis of the effects of multiple pollutants. Having just six monitoring stations in the state of Ohio, NO2 approximations are the most sparsely represented in the data set. Although it may be difficult to conduct representative analyses of simultaneous exposures to all six criteria pollutants, this geospatial approach could potentially support meaningful analyses of a subset of the criteria pollutants.
In the current analysis, although we found that coverage for estimating exposures to all six criteria pollutants was limited to urban populations, there were no significant difference in the prevalence of important stillbirth risk factors including maternal age, smoking status, hypertension, and diabetes between the rural and urban groups. While the distribution of clinical risk factors was consistent among those in close proximity to all monitoring stations as well as those outside the proximity of any monitoring station, there were significant differences in the socio-demographic makeup of the two groups. Women residing near all six types of monitoring stations were more likely to be black, unmarried, and to have attained a lower level of education than women listing a residence beyond the range of any monitoring station. Because many of these characteristics are associated with the stillbirth outcome, any study using our data management approach would need to make proper adjustment for these coexisting risk factors when conducting analyses and in reporting results.
The described approach has generalizability beyond analyses related to stillbirth. Other studies have focused on the effects of maternal exposure to pollutants on preterm birth25–27 and autism.28 Our approach would provide the same improvements to temporal and spatial granularity in the analyses of these and other clinical outcomes associated with maternal exposures. A separate investigation using our approach has identified an association between high levels of PM2.5 exposure and preterm birth.29 As all pregnant women are potentially at risk for negative outcomes resulting from pollution exposures, our methods have broad applicability and relevance in better understanding the true risks to fetal and infant health associated with in-utero exposures.
Although the use of maternal residence enables additional spatial granularity over cruder county- or state-wide exposure approximations, our approach does not capture spatial mobility throughout the course of pregnancy. Our approach utilized a residence provided at the time of birth; however, a more detailed residence history would enable further customization of individual exposure approximations throughout the pregnancy period. In addition, our approach was unable to adjust to variations in pollutant levels within the 10 km radius of each monitoring station. The described variations introduce the limitation of underestimated risk attributed to maternal exposure.
Conclusions
Using a spatial approach to linking measures of air quality to vital records, we were able to identify characteristics of women residing within the coverage range of EPA monitoring stations. Although women residing within range of stations were significantly different in regards to socio-demographic characteristics than women residing outside the coverage range of monitoring stations, groups expressed similar clinical risk factors for stillbirth. While the spatial approach supports analysis of single particulate exposures, the inclusion of additional pollutants in an analysis of combined exposure effects may be prohibitively restrictive of eligible populations. Although, researchers should consider potential limitations associated with populations in close proximity to air monitoring stations, the described approach has generalizability to support the study of the effects of pollutant exposures on various pregnancy and birth related outcomes.
Acknowledgments
This study included data provided by the Ohio Department of Health, which should not be considered an endorsement of this study or its conclusions.
References
- 1.MacDorman MF, Kirmeyer S, Wilson EC. Fetal and Perinatal Mortality, United States, 2006. National Vital Statistics Reports. 2012 Aug 28;60(8) [PubMed] [Google Scholar]
- 2.Lawn JE, Gravett MG, Nunes TM, Rubens CE, Stanton C. Global report on preterm birth and stillbirth (1 of 7): definitions, description of the burden and opportunities to improve data. BMC Pregnancy Childbirth. 2010;10(Suppl 1):S1. doi: 10.1186/1471-2393-10-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stanton C, Lawn JE, Rahman H, Wilczynska-Ketende K, Hill K. Stillbirth rates: delivering estimates in 190 countries. Lancet. 2006 May 6;367(9521):1487–94. doi: 10.1016/S0140-6736(06)68586-3. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services . Healthy People 2010. Washington, DC: 2000. [Google Scholar]
- 5.Healthy People 2020 Healthy People 2020 Summary of Objectives. Accessed January 16, 2014; http://www.healthypeople.gov/2020/topicsobjectives/objectiveslist.aspx?topicId=26]
- 6.Flenady V, Koopmans L, Middleton P, Froen JF, Smith GC, Gibbons K, et al. Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. Lancet. 2011 Apr 16;377(9774):1331–40. doi: 10.1016/S0140-6736(10)62233-7. [DOI] [PubMed] [Google Scholar]
- 7.Fretts RC. Etiology and prevention of stillbirth. Am J Obstet Gynecol. 2005 Dec;193(6):1923–35. doi: 10.1016/j.ajog.2005.03.074. [DOI] [PubMed] [Google Scholar]
- 8.Maisonet M, Correa A, Misra D, Jaakkola JJ. A review of the literature on the effects of ambient air pollution on fetal growth. Environ Res. 2004 May;95(1):106–15. doi: 10.1016/j.envres.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 9.Shah PS, Balkhair T. Air pollution and birth outcomes: a systematic review. Environ Int. 2011 Feb;37(2):498–516. doi: 10.1016/j.envint.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 10.United States Environmental Protection Agency National Ambient Air Quality Standards (NAAQS) Accessed November 21, 2013; http://www.epa.gov/air/criteria.html]
- 11.Bobak M, Leon DA. Pregnancy outcomes and outdoor air pollution: an ecological study in districts of the Czech Republic 1986–8. Occup Environ Med. 1999 Aug;56(8):539–43. doi: 10.1136/oem.56.8.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glinianaia SV, Rankin J, Bell R, Pless-Mulloli T, Howel D. Particulate air pollution and fetal health: a systematic review of the epidemiologic evidence. Epidemiology. 2004 Jan;15(1):36–45. doi: 10.1097/01.ede.0000101023.41844.ac. [DOI] [PubMed] [Google Scholar]
- 13.Landgren O. Environmental pollution and delivery outcome in southern Sweden: a study with central registries. Acta paediatrica. 1996 Nov;85(11):1361–4. doi: 10.1111/j.1651-2227.1996.tb13926.x. [DOI] [PubMed] [Google Scholar]
- 14.Pereira LA, Loomis D, Conceicao GM, Braga AL, Arcas RM, Kishi HS, et al. Association between air pollution and intrauterine mortality in Sao Paulo, Brazil. Environ Health Perspect. 1998 Jun;106(6):325–9. doi: 10.1289/ehp.98106325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vassilev ZP, Robson MG, Klotz JB. Outdoor exposure to airborne polycyclic organic matter and adverse reproductive outcomes: a pilot study. Am J Ind Med. 2001 Sep;40(3):255–62. doi: 10.1002/ajim.1096. [DOI] [PubMed] [Google Scholar]
- 16.Hwang BF, Lee YL, Jaakkola JJ. Air pollution and stillbirth: a population-based case-control study in Taiwan. Environ Health Perspect. 2011 Sep;119(9):1345–9. doi: 10.1289/ehp.1003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pearce MS, Glinianaia SV, Rankin J, Rushton S, Charlton M, Parker L, et al. No association between ambient particulate matter exposure during pregnancy and stillbirth risk in the north of England, 1962–1992. Environ Res. 2010 Jan;110(1):118–22. doi: 10.1016/j.envres.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Faiz AS, Rhoads GG, Demissie K, Kruse L, Lin Y, Rich DQ. Ambient air pollution and the risk of stillbirth. American journal of epidemiology. 2012 Aug 15;176(4):308–16. doi: 10.1093/aje/kws029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hall ES, Goyal NK, Ammerman RT, Miller MM, Jones DE, Short JA, et al. Development of a linked perinatal data resource from state administrative and community-based program data. Matern Child Health J. 2014 Jan;18(1):316–25. doi: 10.1007/s10995-013-1236-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.South AP, Jones DE, Hall ES, Huo S, Meinzen-Derr J, Liu L, et al. Spatial analysis of preterm birth demonstrates opportunities for targeted intervention. Maternal and Child Health Journal. 2012 Feb;16(2):470–8. doi: 10.1007/s10995-011-0748-2. [DOI] [PubMed] [Google Scholar]
- 21.United States Environmental Protection Agency AirData. Jan 15, 2013. Available from: http://www.epa.gov/airdata/
- 22.Faiz AS, Rhoads GG, Demissie K, Lin Y, Kruse L, Rich DQ. Does ambient air pollution trigger stillbirth? Epidemiology. 2013 Jul;24(4):538–44. doi: 10.1097/EDE.0b013e3182949ce5. [DOI] [PubMed] [Google Scholar]
- 23.Holm S. A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics. 1979;6:65–70. [Google Scholar]
- 24.DeFranco E, Hall E, Hossain M, Chen A, Haynes E, Jones D, et al. Air pollution and stillbirth risk: exposure to airborne particulate matter during pregnancy is associated with fetal death. 2013. Unpublished results. [DOI] [PMC free article] [PubMed]
- 25.Pereira G, Belanger K, Ebisu K, Bell ML. Fine Particulate Matter and Risk of Preterm Birth in Connecticut in 2000–2006: A Longitudinal Study. American journal of epidemiology. 2013 Sep 25; doi: 10.1093/aje/kwt216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ritz B, Yu F, Chapa G, Fruin S. Effect of air pollution on preterm birth among children born in Southern California between 1989 and 1993. Epidemiology. 2000 Sep;11(5):502–11. doi: 10.1097/00001648-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Sram RJ, Binkova B, Dejmek J, Bobak M. Ambient air pollution and pregnancy outcomes: a review of the literature. Environ Health Perspect. 2005 Apr;113(4):375–82. doi: 10.1289/ehp.6362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Becerra TA, Wilhelm M, Olsen J, Cockburn M, Ritz B. Ambient air pollution and autism in Los Angeles county, California. Environ Health Perspect. 2013 Mar;121(3):380–6. doi: 10.1289/ehp.1205827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeFranco E, Chen A, Xu F, Hall E, Hossain M, Haynes E, et al. Air pollution and risk of prematurity: exposure to airborne particulate matter during pregnancy is associated with preterm birth risk. Am J Obstet Gynecol. 2014;210(1):S346. [Google Scholar]