Abstract
How patients used Addiction-Comprehensive Health Enhancement Support System (A-CHESS)1, a mobile health intervention, while quitting drinking is worthy exploring. This study is to explore A-CHESS use patterns prior to the initial lapse reported after discharge from inpatient detoxification programs. 142 patients with alcohol addiction from two treatment agencies in the U.S. were included. A comprehensive set of A-CHESS use measures were developed based on a three-level system use framework and three A-CHESS service categories. In latent profile analyses, three A-CHESS system use patterns—inactive, passive, and active users—were found. Compared to the passive users (with the highest chance of the initial lapse), the active users (with the lowest chance of such behavior) participated more in online social activities, used more sessions, viewed more pages, and used A-CHESS longer. However, the chances of the initial lapse between A-CHESS user profiles were not statistically different. Implications of this finding were provided.
Introduction
In 2012, 7% of the U.S. population aged 12 or older were diagnosed with alcohol dependence or abuse.2 One major challenge in current addiction treatment is to extend care beyond traditional in-patient treatment.3 The emerging application of mobile communication and sensor technology in health care (called mHealth) has the potential to complement current treatment approaches in alcohol relapse prevention.4–6 Evidence shows that mHealth is well accepted by the underserved populations with chronic diseases (including addiction).7,8 Although mHealth is pervasive, highly accepted, and seemingly effective, less is known about how patients actually took advantage of it, and whether different mHealth use patterns may lead to different health outcomes.
Addiction-Comprehensive Health Enhancement Support System (A-CHESS) is a smartphone application developed to support patients with alcohol addiction after they leave residential care. A recent randomized controlled trial showed a significant reduction in the number of risky drinking days for patients who were given the access to A-CHESS.1 A-CHESS offers patients the ubiquitous access to services designed to promote the three basic needs (i.e., autonomous motivation (AM), coping competence (CC), and social relatedness (RE)) outlined in the Self-Determination Theory (SDT).7,9,10 For example, the alerts and recommendations in A-CHESS are intended to supplement the impaired cognitive functions of patients by helping them to adopt effective coping strategies when needed. A-CHESS can connect patients to the immediate support network including their addiction counselors, families, and peer patients. Motivational stories and messages from their counselors and peer patients may motivate patients to be on top of their own recovery. The continuous access to services provided in A-CHESS is not available in any existing addiction treatment program, and its use and impact on addiction outcomes is worth exploring.
A recent development of A-CHESS is a predictive feature of alcohol lapses. Using patient-reported recovery status in A-CHESS, such as the levels of urge and alcoholics anonymous (AA) meeting attendance, a Bayesian network model was developed to assess the risks of a lapse within a week of reporting.11 The model successfully predicts more than 80 percent of the cases.11 In this model, patients with recent lapse experiences were found to have a higher chance of subsequent lapses. In other words, the model can better identify potential lapsers based on whether they have lapsed recently. However, for those who did not lapse recently (i.e. the initial lapse cases), the prediction could be further explored and improved.
A-CHESS use patterns that occurred before initial alcohol lapses may inform the likelihood of such events and make early interventions possible. Studies have shown that coping activities may reduce the risks of initial lapse.12 The use of A-CHESS can be considered as a coping behavior. The patterns of A-CHESS use before the initial lapse could potentially offer valuable information to improve initial lapse prediction and prevention. The purpose of this study is to explore the A-CHESS use patterns before the initial lapse reported by the patients who have just completed residential treatment and returned to their own community.
A-CHESS System Use
A-CHESS creates electronic log files containing patients’ use of the system. Log file analyses provide rich information about how the technological systems work and how patients may gain benefits from using different components in the systems.13 In order to go beyond the traditional log file analyses where only the amount of use (e.g., page views) is analyzed, a comprehensive use-measurement framework that contains different levels of system use measures (i.e., system entry, exposure, and engagement) may help to better understand the use patterns of a multifunctional and comprehensive application, like A-CHESS.14
In mass media research, system entry is closely related to selection, meaning that people intentionally choose to allocate their time and attention to certain mass media, in this case, A-CHESS. System entry means that users choose to turn on A-CHESS and can be operationalized as a successful login or session.14 Just as a psychosocial and behavioral intervention received by alcohol addiction patients, A-CHESS system entry means that patients choose to attend (open) the treatment (the applications). Choosing to access the treatments may imply stronger motivation of alcohol addiction patients.15 Mounting evidence shows that the attendance of treatment sessions, AA meetings, religious activities, or 12-Step group meetings is significantly related to improved abstinence outcomes.16,17
System exposure refers to how much information is perceived by the users, often operationalized to be the amount (the number of pages) or the degree (the amount of time) of the exposure. As patients browse through more content in A-CHESS, they may feel more informed, more supported, and more motivated to resist the temptation to lapse. Studies showed that patients who attend more treatment sessions are more likely to achieve better outcomes.18,19
System exposure focuses on “what” contents are perceived by patients, while system engagement focuses on the patients’ interactions with the system. A-CHESS patients may not only passively receive information but also actively engage in various navigation strategies. They actively learn from and communicate with the other patients or counselors via the social networking tools. Most importantly, A-CHESS users may choose to engage in using the system for a sustained amount of time. Previous studies showed that expressing emotional support and empathy in an online environment was related to a reduction of concerns and improved quality of life.20 Patients who used the information systems more continuously (i.e. longer over-time use) reported improved health competence, social support and active participation in health care.21 Similarly, Moos and Moos (2007) found that patients with alcohol addiction who participated in AA meetings for a longer time period were more likely to be remitted at all four follow-ups22. The participation of social networks has also been found to be an important protective factor in the recovery journey of patients with addiction.23
Although system entry needs to occur before exposure or engagement can be reasonably measured, and exposure must occur for engagement to be meaningful, these three use measurement levels are not in a continuum.14 Since the tools in A-CHESS offer different functions and contents that are designed to meet the three SDT needs, the combination of three levels of system use measurement with three SDT classified A-CHESS services may offer a more comprehensive view of A-CHESS use patterns (e.g., entry to relatedness services, exposure to coping competence services, and engagement with autonomy motivation services).
Latent Profile Analysis to Study System Use
A holistic approach is needed to study the effects of A-CHESS system use patterns. By considering multiple use measures simultaneously, we can better understand the impact of the system on patient outcomes. Latent class analysis (LCA) has been increasingly used as an exploratory approach to study the underlying patterns of complex, observed response variables in either dichotomized or continuous scales.24 Compared to traditional clustering algorithm, such as k-mean, LCA is a model-based approach that offers cluster solutions that are supported by rigorous statistical tests and is based on a mixture of the underlying probability distribution, which makes the solution less arbitrary.25 Latent profile analysis (LPA), a type of LCA in which all indicators are continuous, has been used in medical research to identify relevant and valid groups in skin cancer risks26, youth risky behavior patterns27, and alcohol dependence and abuse.28 In a recent study of the system use patterns of a web-based eHealth intervention for cancer patients, LCA was proved to be a useful technique to identify subgroups of eHealth system users.29 In the present study, because the use measures are continuous, LPA will be used to explore the underlying A-CHESS use patterns based on a comprehensive set of A-CHESS use measures.
In a recent review of various effective behavior interventions for addiction patients, researchers pointed out that the real challenge is to choose the most appropriate treatments for a given patient.30 The same challenge was faced in the development of various services offered in A-CHESS. Exploring A-CHESS use patterns before the initial lapse may offer important information about which patterns of system use matter in A-CHESS. Ultimately, the understanding of effective A-CHESS use patterns may help to design more effective mHealth interventions for addiction patients.
Methods
Participants
170 patients were randomized into the intervention group in a randomized trial.7 Among them, 142 patients were included in this study because of the inclusion criteria during data cleaning (see section in Data preparation and analysis). The intervention group was given the access to A-CHESS; the control cases did not have access to A-CHESS and so are excluded from this analysis. The patients were recruited from two residential treatment organizations—one in the Midwest and the other in the Northeastern U.S.—from February 2010 to November 2011. They were at least 18 years old, met the criteria for DSM-IV31 alcohol dependence when they entered treatment, and were able to provide two backup contacts for follow-up. Patients were excluded if they had a history of suicidality, a significant developmental or cognitive impairment that would limit the ability to use A-CHESS, or vision problems.
Procedures
The study was conducted according to the Declaration of Helsinki of 1975 and approved by the Institutional Review Board at the University of Wisconsin-Madison. Patients were recruited at each clinic by project coordinators before they were discharged. Written informed consent was obtained. Before leaving the facilities, patients received training on how to use A-CHESS and the smartphones from their counselors. On the day when they were discharged (i.e. the intervention date), they each received a smartphone (either Palm Pre or HTC Evo) with a pre-installed A-CHESS program. The 3G mobile broadband connection was paid up to 8 months after the intervention dates. The patients agreed to use A-CHESS. However, using A-CHESS is not required to stay on study. The system log data were sent to a secure server at University of Wisconsin-Madison. Details about the trial can be found elsewhere.1
Intervention—SDT-Based Services Provided in A-CHESS
A-CHESS services were designed to focus on one or more SDT needs.10 Detailed information about different A-CHESS services has been reported elsewhere.7,10,32 The following is a list of services targeting each SDT construct.
Services for promoting autonomous motivation
High-Risk Locator, Notifications, Recovery Motivation, Panic Button, Weekly Check-in, Daily Check-In, Sobriety Date Counter, Our Stories, and Recovery Podcasts.
Services for improving coping competence
Notifications, Panic Button, Discussions, Ask an Expert, News, Easing Distress, Instant Library, Recovery Information, Open Expert, FAQs, Weblinks, Tutorials, Our Stories, and Recovery Podcasts.
Services for building relatedness
Panic Button, Weekly Check-in, Daily Check-In, Discussions, Ask an Expert, Events and Meeting Planner, My Friends, My Messages, My Profile, My Team, and Team Feed.
Measures
Initial lapse and prediction relationship
The substance use item from the Weekly Check-in was used as the indicator of a patient’s initial lapse status. The Weekly Check-in is a self-monitoring service in A-CHESS for patients to track their recovery progress.11 Patients filled out an online questionnaire in the Weekly Check-in every 7 days in A-CHESS on smartphones. The status of their self-reported substance use behavior (i.e., drug and alcohol use) in the last 7 days was measured on a dichotomous scale (yes/no). Therefore, a lapse is defined to have occurred when a patient indicated that he/she used alcohol or took drugs in the last 7 days in their Weekly Check-in reports.11 Patients may report lapses in multiple Weekly Check-in reports during the 8-month study period. The first reported lapse cases in the Weekly Check-in after patients left the treatment facilities were identified as the initial lapse cases.
The lapse status that patients reported in the Weekly Check-in was about their substance use in the last 7 days. If the time between two consecutive Weekly Check-ins was more than 14 days, the prediction was considered invalid because it was separated by too many days from the prior report.11 Therefore, only a current Weekly Check-in with a subsequent Weekly Check-in within 14 days was considered an effective data point. If the next Weekly Check-in reported a lapse, it was taken as such; otherwise, it was considered a non-lapse. The use data that happened between the current Weekly Check-in and the previous Weekly Check-in were retrieved and used to develop measures of pre-lapse A-CHESS use (Figure 1).
Figure 1.
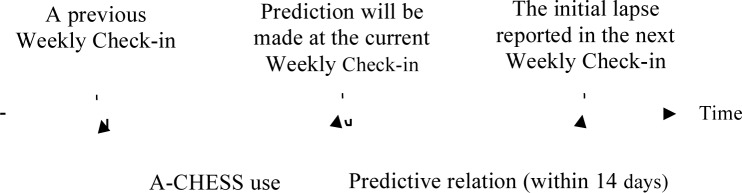
Initial lapse prediction conceptual diagram
Note: A-CHESS: Addiction-Comprehensive Health Enhancement Support System
Use measurements
A-CHESS was programmed to constantly record log files at the level of individual keystrokes or clicks of hyperlinks. The log files—with unique user identifiers and timestamps—can reveal precisely who requested what A-CHESS services and when. The log files can be used to establish activities in which the user was engaged (e.g., posting or reading) as well as the specific services that were requested (e.g., news or discussion group messages). From the log file data, A-CHESS use metrics were developed based on a combination of the SDT-focused A-CHESS service categories and the three levels of system use: entry, exposure, and engagement. SDT-based A-CHESS services were defined above. The operational meanings of the use measures are listed below.
Average daily sessions as system entry
The average number of daily sessions between the previous and current Weekly Check-in was calculated as the measurement for system entry. A new session is recorded when patients switched from using one service, such as discussion group, to another, such as easing distress. Four system entry measures were developed: Total entry (i.e. system entry measure of all A-CHESS services), AM entry (i.e. system entry measure of autonomous motivation services), CC entry (i.e. system entry measure of coping competence services), and RE entry (i.e. system entry measure of relatedness services).
Average daily pages viewed as system exposure
System exposure could be operationalized by pages viewed or time spent. Compared to those using computer-based applications, smartphone users were not restricted to a physical location, and therefore, could be more easily distracted by other tasks, like crossing the roads. This could cause time-based exposure measures to be overestimated. In addition, the contents in A-CHESS are often short and simple, and therefore may not require much time to achieve comprehension. Therefore, the duration of time between pages may not be the best measure in the context of a smartphone application. The amount of content (the number of pages viewed) may be a more useful and realistic measure of system exposure. The average number of daily pages viewed between the previous and current Weekly Check-in was calculated as the measure for system exposure. Four system exposure measures were developed: Total exposure (i.e. system exposure measure of all A-CHESS services), AM exposure (i.e. system exposure measure of autonomous motivation services), CC exposure (i.e. system exposure measure of coping competence services), and RE exposure (i.e. system exposure measure of relatedness services).
Percentage of days using A-CHESS as over-time system engagement
Over-time engagement has been used to describe the commitment and the continuous nature of system engagement in other studies.14,21 In this study, the measure of over-time system engagement was operationalized by dividing the number of days a patient used A-CHESS by the total number of available days between the patients’ previous and the current Weekly Check-in. The scale for this percentage measure is from 0% to 100%. Four over-time system engagement measures were developed: Total over-time engagement (i.e. over-time system engagement measure of all A-CHESS services), AM over-time engagement (i.e. over-time system engagement measure of autonomous motivation services), CC overtime engagement (i.e. over-time system engagement measure of coping competence services), and RE over-time engagement (i.e. over-time system engagement measure of relatedness services).
Average daily posting messages as social system engagement
The average number of daily messages posted or sent by patients between the last and the current Weekly Check-in was used to measure social system engagement. Because this measure describes the activity in online social services without a strong reference to SDT content categories, only one use measure was developed for social system engagement.
Data Preparation and Analysis
The use data retrieval was based on the submission date/time of the selected Weekly Check-in reports. Initial lapse cases were retrieved from the Weekly Check-in database as described in the process flow chart (Figure 2). In August 2011, a new intervention component was added to provide additional, automatic alerts sent out to both patients and counselors about patients’ risk of upcoming lapses.11 To avoid the impact of the new intervention on the predictive relationship studied here, four patients were excluded because all of their Weekly Check-in reports were submitted after this new intervention feature. Of the remaining patients, six did not have effective initial prediction data points: that is, a Weekly Check-in followed by a subsequent Weekly Check-in submitted within 14 days (Figure 1). Among 152 patients with effective prediction cases, 58 reported a lapse in at least one report, but 7 of them were excluded because their initial lapse was reported during their first Weekly Check-in—no prior Weekly Check-in can be used together as a prediction point. Because the 51 initial lapse cases occurred in different weeks of the 8-month study period, a matching process was performed to select compatible non-lapse cases. The process selected a number of non-lapse reports at a particular time point (e.g., 4th week after intervention) to match to the same proportion of lapse cases reported on the same week. Because all the initial lapse cases happened after the 2nd week of the intervention, 3 patients who only have non-lapse reports at the 2nd week were excluded as not matched non-lapse cases. The final dataset contains 51 lapse cases and 91 non-lapse cases.
Figure 2.
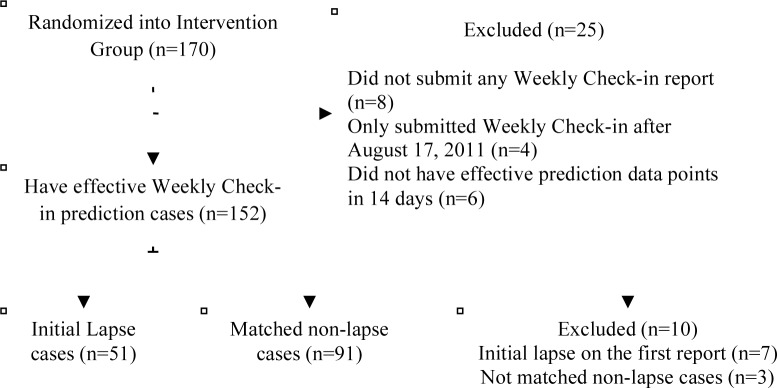
Initial lapse data process flow chart
After selecting these 142 cases (i.e. 51 lapse and 91 non-lapse cases), A-CHESS log data between reports (Figure 1) were retrieved. Usage measures were calculated for each case. Outliers (with a z-score over 3 or below -3) were recoded to the next most extreme values to minimize the impact of outliers.33 A LPA was conducted to identify the underlying A-CHESS use patterns. For some variables with high proportion of extreme boundary values (e.g. 38% of non-users for coping competence services and 33% of patients had a 100% in total over-time engagement), a censored normal distribution was used in LPA using Mplus v7.11.34,35
This LPA identified the underlying use patterns (i.e. latent profiles) based on the comprehensive A-CHESS use measures. The number of latent profiles was increased until the most parsimonious model solution was found. The most parsimonious model was determined by minimizing Bayesian Information Criteria (BIC), statistically significant results in Lo-Mendell-Rubin likelihood ratio test (LMR-LRT), and entropy (over 0.9).36 During each latent class modeling procedure, a three-step process was adopted to test the predictive relationship between latent profile groups and the distal outcome variable (i.e. the subsequently-reported initial lapse in the following Weekly Check-in). The three-step procedure can avoid the impact of the distal outcome variable on the latent profile groups when they are in the same model.37 The three-step model, implemented in Mplus v7.11, was used to offer the pairwise chi-square test of the probabilities of the initial lapse among the latent profiles.37
Results
142 patients (51 initial lapse cases or lapsers; and 91 non-lapse cases or non-lapsers), had a mean age of 37.93 years old (from 20 to 64), mostly Caucasians (82%) and mostly male (60.6%). About 40% of patients have received some college education or higher. Only 19% of patients are currently employed. About 60% of patients have abused drugs. Table 1 shows the descriptive statistics of demographic characteristics and A-CHESS use measures. Less than 4% outliers (z > 3) were found in all A-CHESS use measures except the Total, CC, and RE over-time engagement measures. The results of t-tests (for continuous variables) and chi-square tests (for categorical variables) showed that lapsers and non-lapses were not statistically different on most demographics and use measures. However, compared to non-lapsers, lapsers are more likely to be female (p=0.005) and currently unemployed (p=0.036).
Table 1.
Descriptive statistics of patient characteristics and A-CHESS use
| Lapsers (n=51, 36%) | Non-lapsers (n=91, 64%) | p-value | |
|---|---|---|---|
| Demographics | |||
| Age, M(SD) | 38.01(9.60) | 37.86(9.12) | 0.901 |
| Female, N(%) | 28(54.9) | 28(30.8) | 0.005 |
| Race, N(%) | 0.895 | ||
| Caucasian | 41(80.4) | 73(80.2) | |
| African American | 7(13.7) | 11(12.1) | |
| Other | 3(5.9) | 7(7.7) | |
| Education, N(%) | 0.248 | ||
| High school and lower | 25(49) | 57(62.6) | |
| Some College | 17(33.3) | 25(27.5) | |
| 2 and 4 year College degree | 8(15.7) | 9(9.9) | |
| Other | 1(2) | 0(0) | |
| Drug use, N(%) | 33(64.7) | 57(62.6) | 0.806 |
| Unemployed, N(%) | 46(90.2) | 69(75.8) | 0.036 |
| Use measures | |||
| System entry (Average daily sessions), M(SD) | |||
| Total Entry | 4.01(4.41) | 4.30(5.02) | 0.731 |
| AM entry | 0.29(0.30) | 0.27(0.30) | 0.746 |
| CC entry | 0.73(1.36) | 0.70(1.46) | 0.919 |
| RE entry | 1.72(1.62) | 1.83(1.88) | 0.719 |
| System exposure (Average daily pages viewed), M(SD) | |||
| Total exposure | 13.47(10.17) | 14.99(12.93) | 0.472 |
| AM exposure | 1.93(1.45) | 1.77(1.26) | 0.499 |
| CC exposure | 1.96(2.93) | 1.53(2.60) | 0.370 |
| RE exposure | 9.42(7.32) | 9.73(8.96) | 0.831 |
| Over-time system engagement (% of days using A-CHESS), M(SD) | |||
| Total over-time engagement | 75.37(26.26) | 72.86(30.92) | 0.625 |
| AM over-time engagement | 35.46(16.84) | 30.75(14.55) | 0.083 |
| CC over-time engagement | 26.66(29.59) | 23.02(28.59) | 0.474 |
| RE over-time engagement | 68.38(27.46) | 64.70(30.64) | 0.477 |
| Social system engagement (Average daily posting messages), M(SD) | |||
| 0.32(0.43) | 0.27(0.43) | 0.451 | |
Abbreviations: A-CHESS: Addiction-Comprehensive Health Enhancement Support System; AM: Autonomous motivation; CC: Coping competence; RE: Relatedness
A latent profile model was developed and estimated. The model contains all use measures outlined in the Measures section. Model fits indices based on different numbers of profile solutions were listed in Table 2. Among these indices, BIC keeps decreasing when models become more complicated, and all models have good delineation of profiles with high entropy over 0.9. However, by examining LMR test result, the 3-profile solution was selected because the LMR test showed that the four-level model does not significantly improve the model fit (p=0.3849).
Table 2.
Fit statistics of latent profile models
| Full model | Decision | |||
|---|---|---|---|---|
| Number of Profiles | BIC | Entropy | LMR(p) | |
| 2 | 9286 | 0.971 | 0.0452 | |
| 3 | 8943 | 0.968 | 0.0244 | Selected |
| 4 | 8760 | 0.976 | 0.3849 | |
Abbreviations: BIC: Bayesian Information Criteria, LMR: Lo-Mendell-Rubin likelihood ratio test.
In Table 3, model estimated profile means were listed to provide an overview of the latent profiles’ characteristics. Based on the profile means of the use measures, three profiles can be named as inactive (35.9%), passive (49.3%), and active users (14.8%). The inactive users have the lowest A-CHESS use with lower than one service session per day, and about 40% over-time system engagement. The passive users have modest A-CHESS use, but their use in several over-time system engagement measures (except for CC over-time engagement) approached to the active users. Compared to the passive users, the active users have used more sessions, viewed more pages, and used A-CHESS longer especially in coping competence and relatedness services. The active users also more actively posted messages (almost one message a day) via online discussion groups or personal messages, than the passive users (about one message every three days). The active users have the lowest percentage of initial lapsers (28.6%) while the passive users have the highest chance (40.2%) for an initial lapse. However, the probabilities of the initial lapse between these three groups were not statistically different (p=0.315 to 0.691) at the present study.
Table 3.
Model details
| Profiles | Inactive Users | Passive Users | Active Users | |
|---|---|---|---|---|
| % of profile membership counts1 | 35.9 | 49.3 | 14.8 | |
| % of the initial lapse | 33.3 | 40.2 | 28.6 | |
| Model estimated profile means | System Entry (Average daily sessions) | |||
| Total Entry | 0.82 | 3.98 | 13.14 | |
| CC Entry | 0.21 | 0.65 | 3.00 | |
| RE Entry | 0.39 | 1.83 | 5.09 | |
| AM Entry | 0.14 | 0.32 | 0.49 | |
| System exposure (Average daily pages viewed) | ||||
| Total exposure | 4.22 | 15.26 | 36.70 | |
| CC exposure | 0.37 | 1.45 | 6.49 | |
| RE exposure | 3.01 | 9.70 | 25.51 | |
| AM exposure | 1.26 | 2.08 | 2.39 | |
| Over-time system engagement (% of days using A-CHESS) | ||||
| Total over-time engagement | 41.90 | 90.54 | 95.46 | |
| CC over-time engagement | 6.17 | 24.12 | 68.22 | |
| RE over-time engagement | 33.57 | 81.71 | 93.58 | |
| AM over-time engagement | 23.87 | 35.37 | 43.72 | |
| Social system engagement (Average daily posting messages) | ||||
| Total | 0.05 | 0.30 | 0.89 | |
Note: 1. The percentages of user counts in profiles were based on the most likely latent profile membership. 2. Abbreviations: A-CHESS: Addiction-Comprehensive Health Enhancement Support System; AM: Autonomous motivation; CC: Coping competence; RE: Relatedness
Discussion
The purpose of this study is to explore the underlying use patterns of a mobile health application, A-CHESS, before the initial lapse after a period of inpatient alcohol detoxification. A-CHESS use measures were developed based on three-level system use framework (i.e., system entry, exposure, and engagement), as well as three SDT service categories (i.e., autonomous motivation, coping competence, and relatedness services). In LPA, three profiles and their unique use patterns were found (Table 3). The inactive users really did not use A-CHESS much. Although the inactive users turned on A-CHESS on average in 4 days out of a 10-day period, they utilized very few (like one or two pages) coping competence and autonomous motivation services. In this case, they may just read the “daily thought” (i.e. an encouragement message sent out each day) or use the Weekly or Daily Check-in, which A-CHESS showed a reminder message on the phone screen. Compared to the inactive users, the passive users used the “social network (relatedness)” services more frequently. However, this use pattern may also be due to the “daily thoughts” message sent to them daily. The passive users did not post or read as many messages as the active users. Therefore, the inactive users did not use A-CHESS regularly even with the daily alerts. The passive users turned on A-CHESS (probably because of the daily prompts) but were not very engaged in using A-CHESS. The active users truly used A-CHESS regularly and actively. The passive users have the highest probability (40.2%) of the initial lapse in the following week while the active users have the lowest probability (28.6%) of such events. However, the probabilities of the initial lapse between these three user profiles were not different.
The non-statistically different likelihoods of the initial lapse between A-CHESS use profiles do not allow for further inferential conclusion to be drawn. However, the different A-CHESS use patterns and their relative chances of lapses—seemingly matching to the literature—showed the potential to explore further and worth mentioning. Compared to the passive users with the highest likelihood of the initial lapse, the active users who have the lowest likelihood of the initial lapse used more service sessions, viewed much more content about coping competence, and especially actively reached out to others by posting or sending messages. This observation is similar to what was found in the addiction literature where patients who participated more treatment sessions, improved their coping skills, and built stronger support network usually experienced better recovery outcomes.22,23,38,39 Therefore, the active users’ A-CHESS use patterns may be worth promoting, especially for those who consumed fewer coping competence services and less actively participated online social network. The inactive users may be a mix of those who have smooth recovery and did not feel the need of using A-CHESS, and those who really needed helps but just did not want to use A-CHESS for some reasons. Therefore, their chance of the initial lapse (33.3%) fell in between the other two user groups.
This study has several strengths in both system science and addiction recovery research. The analysis of system use behavior in this study was based on the actual log files, which are the objective observation of each activity that patients have with the intervention system, A-CHESS. Therefore, the results in this study have provided a different perspective of user behaviors other than the self-reported system use. Future studies that examine both the log files and the self-reported system use may offer a more complete picture of user behaviors. In addition, a comprehensive set of A-CHESS use measures were developed and analyzed together, which offered rich information about the different A-CHESS use patterns before the initial lapse. The LPA results, although non-conclusive, seemingly match well with the existing addiction literature regarding treatment effects on the alcohol lapse. The findings from this study may benefit to the design of A-CHESS-like technological interventions. The method used to study the system use mHealth interventions.
Several limitations were related to the data used in this study. First, the data used in this analysis were based on patients’ Weekly Check-in. If patients did not fill out Weekly Check-in in a way as described in the Methods section, their data would not be included in the analyses. Patients who did not fill out Weekly Check-in may have some valid and non-ignorable reasons that could be related to their substance use status. For example, some patients who drank might not want to disclose their drinking status in A-CHESS but would tell their counselors at a different setting. This kind of non-random missingness may limit the generalizability of the results. The latent use profiles found in this study may not be applied to all patients but only to those who would use A-CHESS and Weekly Check-in. Besides, the overlapped SDT categories may lead to potentially high correlations between the A-CHESS use measure indicators. A more complex model with a higher number of profiles may be needed in order to fit a complex correlation structure in our data. However, the relatively small sample size in this study precluded the construction of a more complex model and may not offer enough power to detect the group differences. Besides, patients from two treatment agencies may not be representative to the general alcohol addiction population. Therefore, future studies should acquire more participants from more sites in order to confirm and further understand the results of the present study. According to a recent PEW research report, adult smartphone owners in the U.S.A. increased from 30% to 50% in early 2013.40 As mobile communication technology becomes more common, it is more likely to run population-based trial on A-CHESS or similar systems at a lower cost.
Patients who suffer from alcohol addiction need continuous support in order to recover from their addiction. In this case, ubiquitous mobile technology, like a smartphone, can be useful to deliver such interventions. This study offered an understanding of the patients’ A-CHESS system use patterns, and how these patterns were related to the chances of patients’ initial lapse after the residential detoxification programs. Future research in this area to test and extend these findings is needed in order to develop and refine effective mHealth interventions for addiction patients.
Acknowledgments
Disclosure and Acknowledgement
The author reports on a part of his dissertation and his involvement in a clinical trial testing A-CHESS. The reason that the author is listed as the only author in this paper is because the author has the solo responsibility to the integrity and quality of his dissertation. The author appreciates the support from his mentor, Dr. David H. Gustafson and all the committee members, as well as the dedicated and talented project team behind this trial.
References
- 1.Gustafson DH, McTavish FM, Chih M-Y, et al. A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA psychiatry. 2014;71:566–72. doi: 10.1001/jamapsychiatry.2013.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration, Results from the 2012 National Survey on Drug Use and Health: Mental Health Findings, NSDUH Series H-47, HHS Publication No. (SMA) 13-4805. Rockville, MD: 2013. Substance Abuse and Mental Health Services Administration. [Google Scholar]
- 3.McKay JR. Continuing care research: what we have learned and where we are going. J Subst Abuse Treat. 2009 Mar;36(2):131–45. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gustafson DH, Palesh TE, Picard RW, Plsek PE, Maher L, Capoccia VA. Automating addiction treatment: enhancing the human experience and creating a fix for the future. In: Bushko RG, editor. Future of Intelligent and Extelligent Health Environment. Birmingham, Alabama: IOS Press; 2005. pp. 186–206. [PubMed] [Google Scholar]
- 5.Marsch La, Ben-Zeev D. Technology-Based Assessments and Interventions Targeting Psychiatric and Substance Use Disorders: Innovations and Opportunities. J Dual Diagn. 2012 Nov;8(4):259–61. [Google Scholar]
- 6.Cohn AM, Hunter-Reel D, Hagman BT, Mitchell J. Promoting behavior change from alcohol use through mobile technology: the future of ecological momentary assessment. Alcohol Clin Exp Res. 2011 Dec;35(12):2209–15. doi: 10.1111/j.1530-0277.2011.01571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McTavish FM, Chih M-Y, Shah D, Gustafson DH. How patients recovering from alcoholism use a smartphone intervention. J Dual Diagn. 2012 Nov 10;8(4):294–304. doi: 10.1080/15504263.2012.723312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rajput Za, Mbugua S, Amadi D, Chepng’eno V, Saleem JJ, Anokwa Y, et al. Evaluation of an Android-based mHealth system for population surveillance in developing countries. J Am Med Inform Assoc. 2012 Feb 24;19(4):655–9. doi: 10.1136/amiajnl-2011-000476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000 Jan;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 10.Gustafson DH, Shaw BR, Isham A, Baker T, Boyle MG, Levy M. Explicating an evidence-based, theoretically informed, mobile technology-based system to improve outcomes for people in recovery for alcohol dependence. Subst Use Misuse. 2011 Jan;46(1):96–111. doi: 10.3109/10826084.2011.521413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chih M, Patton T, McTavish FM, Isham AJ, Judkins-Fisher CL, Atwood AK, et al. Predictive modeling of addiction lapses in a mobile health application. J Subst Abuse Treat. 2014 Jan 10;46(1):29–35. doi: 10.1016/j.jsat.2013.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Witkiewitz K, Masyn KE. Drinking trajectories following an initial lapse. Psychol Addict Behav. 2008 Jun;22(2):157–67. doi: 10.1037/0893-164X.22.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han JY. Transaction logfile analysis in health communication research: challenges and opportunities. Patient Educ Couns. Elsevier Ireland Ltd. 2011 Mar;82(3):307–12. doi: 10.1016/j.pec.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 14.Shah D, Namkoong K, Moon TJ, Chih M-Y, Han JY. Explicating Use of ICTs in Health Contexts: Entry, Exposure, and Engagement; Association for Education in Journalism and Mass Communication 2011 Annual Conference; St. Louis, MO. [Google Scholar]
- 15.Cunningham Ja, McCambridge J. Is alcohol dependence best viewed as a chronic relapsing disorder? Addiction. 2012 Jan;107(1):6–12. doi: 10.1111/j.1360-0443.2011.03583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bonn-Miller M, Zvolensky MJ, Moos RH. 12-Step Self-Help Group Participation as a Predictor of Marijuana Abstinence. Addict Res Theory. 2011;19(1):76–84. [Google Scholar]
- 17.Robinson EAR, Krentzman AR, Webb JR, Brower KJ. Six-month changes in spirituality and religiousness in alcoholics predict drinking outcomes at nine months. J Stud Alcohol Drugs. 2011 Jul;72(4):660–8. doi: 10.15288/jsad.2011.72.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lash SJ. Increasing participation in substance abuse aftercare treatment. Am J Drug Alcohol Abuse. 1998 Feb;24(1):31–6. doi: 10.3109/00952999809001697. [DOI] [PubMed] [Google Scholar]
- 19.Lash SJ, Stephens RS, Burden JL, Grambow SC, DeMarce JM, Jones ME, et al. Contracting, prompting, and reinforcing substance use disorder continuing care: a randomized clinical trial. Psychol Addict Behav. 2007 Sep;21(3):387–97. doi: 10.1037/0893-164X.21.3.387. [DOI] [PubMed] [Google Scholar]
- 20.Namkoong K, Shah DV, Han JY, Kim SC, Yoo W, Fan D, et al. Expression and reception of treatment information in breast cancer support groups: how health self-efficacy moderates effects on emotional well-being. Patient Educ Couns. 2010 Dec;81(Suppl):S41–7. doi: 10.1016/j.pec.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han JY, Hawkins RP, Shaw BR, Pingree S, McTavish F, Gustafson DH. Unraveling uses and effects of an interactive health communication system. J Broadcast Electron Media. 2009 Feb 27;53(1):112–33. doi: 10.1080/08838150802643787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moos RH, Moos BS. Treated and untreated alcohol-use disorders: Course and predictors of remission and relapse. Eval Rev. 2007 Dec 1;31(6):564–84. doi: 10.1177/0193841X07306749. [DOI] [PubMed] [Google Scholar]
- 23.Hunter-Reel D, McCrady BS, Hildebrandt T, Epstein EE. Indirect Effect of Social Support for Drinking on Drinking Outcomes: The Role of Motivation. J Stud Alcohol Drugs. 2010;71(6):930–7. doi: 10.15288/jsad.2010.71.930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Finch WH, Bronk KC. Conducting Confirmatory Latent Class Analysis Using M plus. Struct Equ Model A Multidiscip J. 2011 Jan 13;18(1):132–51. [Google Scholar]
- 25.Magidson J, Vermunt JK. Latent class models for clustering: A comparison with K-means. Can J Mark Res. 2002 Jan 1;20(1):36–43. [Google Scholar]
- 26.Steffen AD, Glanz K, Wilkens LR. Identifying latent classes of adults at risk for skin cancer based on constitutional risk and sun protection behavior. Cancer Epidemiol biomarkers prev. 2007 Jul;16(7):1422–7. doi: 10.1158/1055-9965.EPI-06-0959. [DOI] [PubMed] [Google Scholar]
- 27.Cole M, Stanton B, Deveaux L, Harris C, Cottrell L, Clemens R, et al. Latent class analysis of risk behaviors among bahamian young adolescents: relatoinship between values prioritizatio and latent class. Soc Behav Personal an Int J. 2007 Jan 1;35(8):1061–76. [Google Scholar]
- 28.Muthén B. Should substance use disorders be considered as categorical or dimensional? Addiction. 2006 Sep;101(Suppl):6–16. doi: 10.1111/j.1360-0443.2006.01583.x. [DOI] [PubMed] [Google Scholar]
- 29.Børøsund E, Cvancarova M, Ekstedt M, Moore SM, Ruland CM. How user characteristics affect use patterns in web-based illness management support for patients with breast and prostate cancer. J Med Internet Res. 2013 Jan;15(3):e34. doi: 10.2196/jmir.2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Witkiewitz K, Marlatt GA. Behavioral Therapy Across the Spectrum. Alcohol Res Heal. 2011;33(4):313–9. [PMC free article] [PubMed] [Google Scholar]
- 31.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) Arlington, VA: American Psychiatric Association; 2000. [Google Scholar]
- 32.Gustafson DH, Boyle MG, Shaw BR, Isham A, McTavish F, Richards S, et al. An e-health solution for people with alcohol problems. Alcohol Res Health. 2011 Jan;33(4):327–37. [PMC free article] [PubMed] [Google Scholar]
- 33.Osborne JW, Overbay A. The power of outliers (and why researchers should always check for them) Pract Assessment, Res Eval. 2004;9(6):1–12. [Google Scholar]
- 34.Tobin J. Estimation of Relationships for Limited Dependent Variables. Econometrica. 1958 Jan;26(1):24. [Google Scholar]
- 35.Muthén LK, Muthén BO. Mplus User ’s Guide, ver 7. 7th ed. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- 36.Nylund KL, Asparouhov T, Muthén BO. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct Equ Model A Multidiscip J. 2007 Oct 23;14(4):535–69. [Google Scholar]
- 37.Asparouhov T, Muthen B. Auxiliary Variables in Mixture Modeling : A 3-Step Approach Using Mplus, version 6. Mplus Web Notes No 15. 2013;(15) [Google Scholar]
- 38.Witkiewitz K, Marlatt GA. Emphasis on Interpersonal Factors in a Dynamic Model of Relapse. Am Psychol. 2005;60(4):341–2. doi: 10.1037/0003-066X.60.4.341. [DOI] [PubMed] [Google Scholar]
- 39.Litt MD, Kadden RM, Cooney NL, Kabela E. Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. J Consult Clin Psychol. 2003;71(1):118–28. doi: 10.1037//0022-006x.71.1.118. [DOI] [PubMed] [Google Scholar]
- 40.Fox S, Duggan M. Mobile Health 2012. Pew Internet & American Life Project. 2012 [Google Scholar]


