Abstract
As the obese population is increasing rapidly worldwide, there is more interest to study the different aspects of obesity and its impact especially on healthcare outcomes and health related issues. Targeting non-surgical times in the operating room (OR), this study focuses on the effect of obesity along with clinical factors on pre-incision times in OR. Specifically, both the individual and combined effect of clinical factors with obesity on pre-incision times is studied. Results show that with the confidence of 95%, pre-incision time in the OR of obese patients is significantly higher than those for non-obese patients by approximately five percent. Findings also show that more complex cases do not exhibit significant differences between these patient subgroups.
1. Introduction
The International Obesity Task Force estimated that 300 million people worldwide are obese and 750 million more are overweight. Thirty percent of adults in the United States are obese (Source: CDC National Center for Health Statistics), and 20.6% of U.S. healthcare expenditures are coming from additional medical spending as a result of obesity[1]. These expenditures account only for the direct costs of medical spending as a result of medical visits, and prescription drugs. The indirect and hidden costs that obesity imposes on healthcare systems need to be further analyzed and investigated. The operating room (OR) is considered to be the most expensive resource to keep open and the most profitable resource in hospitals; mainly related to the expensive staffing of these resources. Studies reveal that duration of surgery and length of stay of obese patients is longer when compared to non-obese patients ([2], [3]). However, there is less research focusing on effect of obesity on non-surgical times in the OR.
It is important to better understand the effect of obesity on non-surgical times in the OR as this helps to (re)design workflow in the OR and to accurately predict OR times for surgical scheduling. Extensive amounts of time stamp data and clinical factors are collected in the OR which provides the opportunity for understanding trends and patterns. Using this data, this research focuses on the duration of pre-incision times in the OR, and the impact of obesity along with other clinical factors on these times. Difficulties with the positioning of obese patients as well as difficulties with anesthesia process for these patients are some of the problems reported for obese patients [4],[5] by OR staff during pre-incision times. However, it is not clear whether these difficulties make a difference in the duration of pre-incision times in OR. For instance, spine surgery involves extensive amount of tasks around patient positioning. Further, the Agency for Healthcare Research and Quality reported spine surgery as the most costly operating room procedure performed in U.S. hospitals. They also ranked spine surgery sixth in terms of frequency of the surgeries that are performed in the U.S. [6]. For these reasons and to ensure a homogenous group of surgeries, this paper will focus on pre-incision times of spine surgeries. Specifically, this research will address two questions: 1) how does obesity impact pre-incision times in OR for spine surgery? and 2) how do clinical factors combined with obesity influence pre-incision times of spine surgery?
The answer to these questions allows better understating of the impact of clinical factors on workflow, and help OR managers better plan staffing and surgical scheduling, thereby reducing delayed surgical starts and overtime. This also addresses some of the indirect costs that obesity may levy on healthcare. The reason for denominating the costs of obesity is not to stigmatize obese population, rather to inform clinicians and administrators to better plan for such patients and reduce unsafe surgeries, delays and excessive cost of overtime.
The rest of the paper follows with a background section with a brief review of the literature, description of workflow during pre-incision time, and methods and results sections. Next, a discussion and conclusion follows with future research direction.
2. Background
The prevalence of the obesity epidemic is increasing worldwide along with the health problems associated with obesity. A BMI higher than 30 kg/m2 is generally regarded as obese [7]. There have been several causative factors associated with obesity such as lack of exercise, genetics, poor lifestyle choices, and poor diet [8]. Obesity is associated with several adverse clinical conditions including cardiac disease, diabetes, arrhythmias, increased all-cause mortality, high stress levels, lack of sleep, and increased cancer incidence [8]. Additionally, obese women who have early-stage breast cancer have been shown to have worse survival rates than their non-obese counterparts [9]. Complications[10], mortality[11], outcomes[12], readmissions[13], duration of surgery[14], levels of infection[14], and financial costs[13] have all been shown to be higher in obese populations undergoing surgery.
The impact of obesity on certain aspects of spine surgery has been studied. Bederman et al., [10] studied social structure, demographics, personal, health beliefs, medical need, and community resource factors impacting rates of knee, hip, and spine surgery, and found that obese patients had higher levels of surgical complications. Kalanithi et. al., [11] studied obese patients undergoing spinal fusion and discovered that obese patients had higher rates of mortality. Fang et. al., [12] studied obese patients who had undergone spinal procedures which had become infected after surgery and identified risk factors. Fang et. al., [12] found obese patients to have worse outcomes than their non-obese counterparts. Silber et. al., [13] examined obese patients and specifically studied financial and medical outcomes that are associated with surgery and found that obese patients have higher numbers of readmission and greater financial costs than their non-obese counterparts. Mehta et. al., [14] studied the role of weight in postoperative infections and found that obese patients have longer surgical durations and higher levels of infection than non-obese patients. There are also reports for higher chance of adverse events on obese patients [8].
Obesity is becoming more prevalent among patients who are considering orthopedic surgery and spine surgery [7]. However, there is still some controversy regarding obesity’s association with failed reconstructions, complications, and reoperations after spine surgery is performed [7]. Also the relationship between obesity and the duration of nonoperative times in the OR is unknown. The aim of this study is to examine how obesity and certain clinical factors specifically affect preparation times that occur within the OR. Next, a brief background on the workflow of various activities in the OR along with a description of clinical factors for spine surgeries is provided.
2.1. Clinical Workflow during Pre-incision times
Surgery related activities on the day of surgery consist of two major set of tasks. The first set of tasks occur outside of the OR, and the second set of tasks is performed inside the OR. The OR-related times (from the time the patient enters the OR to the time the patient exits the OR) is divided into three common time periods: time to incision (TtI), skin to skin (StS), and closure to exit (CtE) (Figure 1). As the names imply, TtI is from the time the patient enters the OR until the time the incision starts; StS time is from the incision start to closure; and finally CtE is the time after closure to the time the patient is taken out of the OR. The focus of this study is on TtI in spine surgeries. There are several events that take place during TtI, some of which depend on the type of surgery and the institution where the surgery is performed (Figure 2). The order of these events however may vary based on the approach taken for the surgery (anterior or posterior or staged, to be discussed shortly) and the anatomic location of incision. As the patient is moved to the OR on the cart, the staff verifies patient’s information, discuss the procedure with the patient and answer last minute questions. The patient is then prepared for intubation. After intubation, IV (intravenous) lines, other lines (e.g. central venous catheter or CVC) are placed as needed for intraoperative administration of fluids, medications and anesthesia, as well as to draw blood. Then the patient is positioned on the OR bed for the approach of surgery to be performed (anterior, posterior, combination of anterior and posterior which is called staged) dependent upon the type of surgery and targeted levels of the spine. The most commonly used positions in spine surgery are supine, prone, and sitting. In a supine position, the patient is slid from the cart to the OR table and remains face up. This position allows the surgeon adequate access to the anterior aspects of the chest, abdomen and pelvic region. In this position, staff should ensure that the head and cervical spine are aligned along the midline. There are also guidelines for protection of the heels, elbows, and upper arms with soft padding to prevent pressure ulcers from long surgeries. The prone position is usually achieved by intubation on the patient's stretcher and movement after anesthesia onto the patient's abdomen by either manually logrolling or using a specifically made bed which rotates the patient on a table that supports the head, upper chest, hip area and legs, to leave the center of the chest without pressure. Care must be given to avoid excessive pressure on the eyes, ears, nose, breasts, and male genitalia [15]. In addition special attention must be given to the knees and ankles, head and to the arm position to avoid injury. Less commonly used position in spine surgery is the seated position. Positioning of the patient can require several members of the OR team, and require a long time to perform, contributing to high variability in TtI time.
Figure 1.
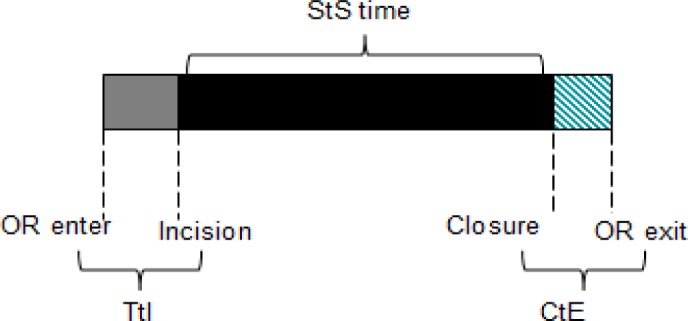
Time durations in the operating room
Figure 2.
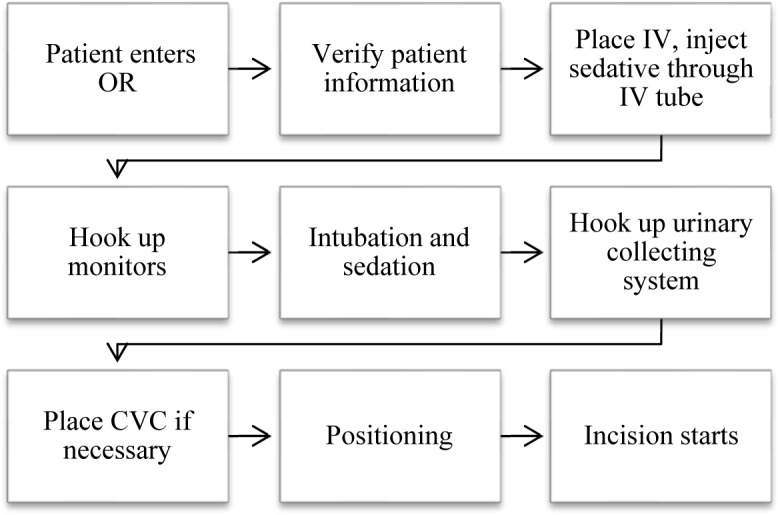
Pre-incision time workflow
3. Methods
3.1. Sample and Assumptions
This study is based on records of 3,677 adult patients aged 30 years or older (gathered from Surgical Information Recording System, SIRS) which had planned spine surgeries in a large tertiary academic medical center in the mid-west, from the start of 2010 through the end of the 2012 (3 years). This data includes a total of 2,611 procedures performed by neurosurgeons and 1,066 performed by orthopedic surgeons. Outliers were excluded where TtI was greater than 2.3 hours which was the highest one percent of the distributed times.
3.2. Measures
The primary outcome variable studied is time to incision (TtI) which is measured in minutes, and one of the independent variables is obesity measured as body mass index (BMI). The other independent variables include ASA category, number of spine levels, approach and fusion, and from here forward, these four will be referred to as clinical factors. Table 1 shows the data spread for spine patients over the four BMI categories defined by Centers for Disease Control & Prevention. As could be seen, the majority of spine surgery patients are overweight or obese.
Table 1.
Patients in BMI categories
| Underweight | Normal | Overweight | Obese | |
|---|---|---|---|---|
| % of Total | 0.8% | 19.4% | 36.1% | 42.8% |
| N | 31 | 713 | 1329 | 1574 |
Since the primary focus was on obese patients, and the underweight patients accounted for less than one percent, these underweight patients were dropped from further analyses. Further, with significance of 95% there was no difference in TtI between the normal and overweight patients based on statistical hypothesis testing (difference of less than a minute on average), hence, they were lumped together under non-obese patients and compared against obese patients. In the final sample, 43% of the patients were obese and the rest were normal or overweight.
The American Society of Anesthesiologists (ASA) adopted a five-category physical status classification system; a sixth category was later added. These are:
Healthy person.
Mild systemic disease.
Severe systemic disease.
Severe systemic disease that is a constant threat to life.
A moribund person who is not expected to survive without the operation.
A declared brain-dead person whose organs are being removed for donor purposes.
The ASA physical status classification is used for assessing the clinical condition of patients before surgery. Only patients from ASA categories one through four were present in the sample.
The number of levels as the name implies refers to the number of spine levels in the procedure. Level 0 is used to represent cases where no spines are worked on, rather the procedure involves just a washout. As the number of levels of spine increases from one through five, TtI increases rapidly. Then for levels six through eight, TtI flattens and again starts to increase slowly for levels greater than nine through 19. However, these cases are very rare. Specifically, there are only 57 cases with spine levels greater than eight. Based on these facts, the sample includes levels 0 through five, 6–8 and 9+, thus a total of seven groups.
Spine surgeries are performed using three different approaches, anterior, posterior, and staged. Anterior approach is applied when spine is accessed from an anterior position whereas in posterior approach, spine is accessed from a posterior position. Staged approach is the combination of anterior and posterior where both of these approaches are used in one surgery and with separate incisions. The patient is usually positioned supine for anterior approach and prone or rarely seated for posterior approach. In staged approach, the positioning is done based on the order in which anterior and posterior approaches are used, and the patient is repositioned after the first incision is closed. Thus the variable approach can be one of anterior, posterior or staged.
The spinal column is made of individual vertebrae separated by discs. Fusion surgery removes much or the entire disc, replacing it with bone grafts or hardware (screws and rods). Hardware keeps the spine stabilized while the bones grow together or fuse. This variable is binary in nature representing the presence or absence of fusion.
3.3. Analysis
Two types of analyses were conducted, 1) regression analysis to study the effect of the five factors on TtI, and 2) t-tests to study the combined effect of the factors (obesity and ASA category, obesity and spine levels, obesity and approach, and obesity and fusion). TtI is normally distributed, and hence the student t-test was selected. We also studied the individual effect of each of the factors on TtI. The results of this analysis are described in the next section.
4. Results
4.1. Regression and Individual Effects
Based on the regression analysis, all five factors have highly significant effect on TtI. This could be seen in Table 2.
Table 2.
Regression analysis test results
| Factor | Sum of Squares | F Ratio | P-Value |
|---|---|---|---|
| Obesity | 6578.75 | 11.1679 | <.0001 |
| ASA category | 22996.32 | 26.0253 | <.0001 |
| Number of levels | 105712.6 | 21.1123 | <.0001 |
| Approach | 12426.1 | 21.0942 | <.0001 |
| Fusion | 96427.46 | 327.3851 | <.0001 |
When TtI is compared for obese and non-obese patients, the time is significantly different (slightly higher for obese patients by three minutes on average). Among cases with ASA categories of one through four, as the ASA category increases, TtI also increases. Figure 3 shows how TtI is changing for different ASA categories. As for approach, staged surgeries have on average the longest TtI among the three approaches, taking 3.5 minutes longer than those surgeries with an anterior approach, which in turn takes on average 15 minutes longer than those with posterior approach. The sample includes 80% of cases with posterior approach, 12% anterior, and only 8% of cases with staged approach. With the fusion, the sample includes 47% of spine cases with fusion. Cases with fusion have TtI which on average is 20 minutes longer than cases without fusion.
Figure 3.
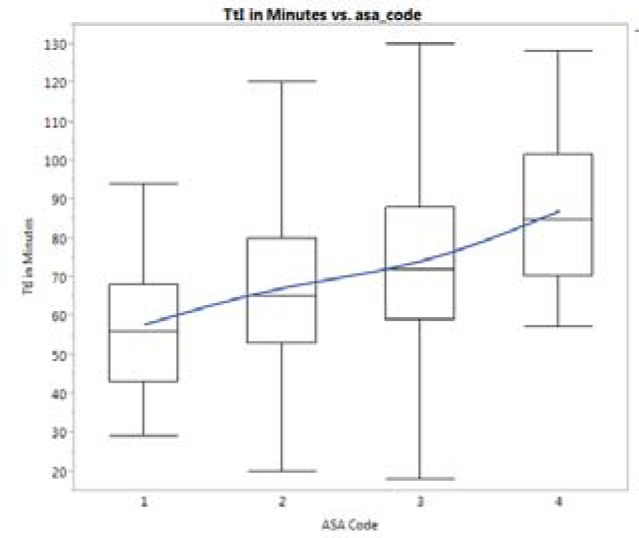
ASA categories and time to incision
4.2. Combined effect
When the combined effect of obesity and the clinical factors were studied, some of the factors were significant. Table 3 shows the results of the statistical results from ANOVA for effect of four clinical factors combined with obesity on TtI. These results indicate that TtI of obese and non-obese patients for any given ASA category is not statistically different. As for the effect of spine levels combined with obesity on TtI, surgeries done on one or two levels of spine, there is a significant difference between TtI of obese and non-obese patients (that is for 68% of cases). For single spine level surgery, TtI of obese patients is on average four minutes longer than non-obese patients. For two levels, this difference is three minutes on average. For higher number of levels of spine, the difference between obese and non-obese patients is not significant. The comparison of averages of TtI for obese and non-obese patients with different number of levels of spine are shown in Figure 4.
Table 3.
ANOVA results for combinational effect of factors with obesity
| Factor | Factor Value | P-Value |
|---|---|---|
| ASA category | 1 | 0.3647 |
| 2 | 0.3362 | |
| 3 | 0.0781 | |
| 4 | 0.2465 | |
| Spine levels | 0 | 0.8095 |
| 1 | <0.0001 | |
| 2 | 0.0183 | |
| 3 | 0.4752 | |
| 4 | 0.3819 | |
| 5 | 0.4567 | |
| 6–8 | 0.7371 | |
| 9+ | 0.8456 | |
| Approach | Posterior | <0.0001 |
| Anterior | 0.0271 | |
| Staged | 0.3985 | |
| Fusion | Yes | <0.0001 |
| No | <0.0001 |
Figure 4.
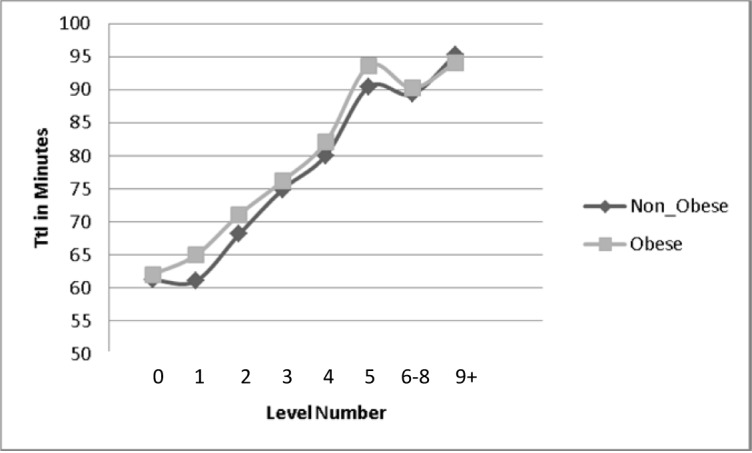
Average time to incision by level
The statistical results show that TtI for obese patients with posterior and anterior approach is significantly different from TtI for non-obese patients for the same type of approach. With the staged approach however, there is no significant difference between TtI of the two groups of obese and non-obese patients. Our analysis indicates that TtI of obese patients within each approach takes few minutes longer than non-obese patients (four minutes for posterior and anterior approaches, and three minutes for staged approach). Based on the results of ANOVA shown in Table 3, fusion has a significant effect on TtI of obese and non-obese patients. Obese patients with fusion have on average TtI which is two minutes longer than TtI on non-obese patients. This difference for patients without fusion tends to be five minutes on average.
5. Discussion
Obesity is considered as a factor that influences tasks that take place during TtI. The primary goal was to study the individual and combined effect of obesity and clinical factors on TtI. As for individual effect, all five clinical factors are significant. Obesity makes for a low difference of just three minutes, however the clinical factors account for much higher differences (19 minutes for approach, 20 minutes for fusion and up to 30 minutes for ASA category). This increase might be because patients with higher ASA category need more prep time in the OR. This is partly due to the complexity added as a result of the existing condition of the patient which may require additional equipment to be attached to the patient. With patients having higher ASA categories, there also may be difficulties with patient positioning due to increased frailty caused by illness. Results show that surgeries using an anterior approach have an average TtI which is 15 minutes longer than that for the posterior approach, despite the prone and seated positioning used in the posterior approach typically being more complex and taking longer time. Input from the OR team suggests that increased time is not patient-related, but OR staffing related; for the surgery done using anterior positioning (in lower levels of spine), the presence of a non-orthopedic surgeon (usually a vascular surgeon) is often required for incision to start. This is mainly due to the fact that accessing spine from anterior position requires a second surgeon to prepare the abdomen for the greatest access as possible to the front of the spine while keeping the large vessels safe, leading to extra preparation time. Also, since the presence of a second surgeon is required, the orthopedic team may need to wait until the second surgeon arrives from their primary surgery or other tasks. This factor seems to be the main reason for TtI of anterior cases to be significantly longer than posterior cases. However, it is noted that posterior approach is more common among the spine surgeries in our data. The effect of obesity could be explained due to the difficulty with intubation and positioning of obese patients. Obesity and some other factors such as limited neck mobility and poor mouth opening accounts for two thirds of all contributing factors for difficulty in intubation [16]. Obesity is also related to other contributing factors for difficult intubation such as short and fleshy necks. Obesity may also be related to difficulty in line placement, due to difficulty palpating landmarks for central lines, or peripheral lines [17]. Other difficulties as a result of patient obesity during preoperative tasks in the OR include problems with positioning of obese patients including difficulty lifting the patient, size of the bed and ensuring patient safety by requiring extra personnel. These difficulties are often assumed to require extra time to get resolved.
As for the combined effect, there is a significant difference for surgeries with one or two levels, but not for higher levels. When effect of approach is combined with obesity, for approaches anterior and posterior, there is a significant difference between obese and non-obese patients in terms of TtI, but for staged approach the difference is not significant. Overall, obesity is shown to be a significant factor affecting TtI. However, when the cases are more complex, obesity does not make a significant difference in TtI of patients. For instance, surgeries, with higher ASA category, higher number of spine levels, staged-approach, do not exhibit significant differences between obese and non-obese groups of patients. This might be due to the fact these complex surgeries are uncommon and the sample size is extremely small. To increase sample size, multi-year surgery data can be combined to better study multivariate effect of factors. Such an approach also poses the problem of changes in culture, practice and technology over time. Hence, multi-institution data need to be warehoused in registries to address this lack of sufficient sample size for more complex cases.
6. Conclusion and Future Work
This study focused on the effect of obesity and clinical factors on TtI of spine surgery. Both, individual effects and combined effects (of clinical factors with obesity) were studied. Obesity shows to be significantly affecting TtI as an individual factor and in combination with the factors such as fusion, number of levels and approach. With more common surgeries such as one or two levels of spine, and anterior or posterior approaches, and for both fusion and non-fusion cases, obese patients have longer TtI. For less common cases such as those with higher ASA categories, higher levels of spine, and a staged approach, there is no significant difference between obese and non-obese patients. However, complex cases need to be further studied. As for obesity, our study was based on BMI and does not focus on extremely tall patients. Height is also a factor that affects positioning of patients, including challenges with instruments, bed size, etc. The next phase is to focus on including height and weight as separate factors and study the effect on TtI.
References
- 1.Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. Journal of health economics. 31(1):11. doi: 10.1016/j.jhealeco.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Gu GF, H, SS, Ding Y, Jia JB, Zhou X. The effect of body mass index on the outcome of minimally invasive surgery for lumbar spinal stenosis complicated with lumbar instability. Chin J Spine Spinal Cord. 2012;22:4. [Google Scholar]
- 3.Hardesty CK, P-KC, Son-Hing JP, Thompson GH. Obesity negatively affects spinal surgery in idiopathic scoliosis. Clin Orthop Relat Res. 2013;471:5. doi: 10.1007/s11999-012-2696-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nielsen KC, GU, Steele SM, et al. Influence of obesity on surgical regional anesthesia in the ambulatory setting: an analysis of 9,038 blocks. Anesthesiology. 2005;102:6. doi: 10.1097/00000542-200501000-00027. [DOI] [PubMed] [Google Scholar]
- 5.Rocke DA, MW, Rout CC, Gouws E. Relative risk analysis of factors associated with difficult intubation in obstetric anesthesia. Anesthesiology. 1992;77:6. doi: 10.1097/00000542-199207000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Weiss A and others. 2014. Healthcare Cost and Utilization Project, statistical brief. [Google Scholar]
- 7.Jiang J, et al. Does Obesity Affect the Surgical Outcome and Complication Rates of Spinal Surgery? A Meta-analysis. Clinical orthopaedics and related research. 2014;472(3):968–75. doi: 10.1007/s11999-013-3346-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramsay MA. The chronic inflammation of obesity and its effects on surgery and anesthesia. International anesthesiology clinics. 2013;51(3):1–12. doi: 10.1097/AIA.0b013e3182981219. [DOI] [PubMed] [Google Scholar]
- 9.Ampil F, et al. Morbid obesity does not disadvantage patients with in situ or early-stage carcinoma undergoing breast-conserving surgery. Anticancer research. 2013;33(9):3867–9. [PubMed] [Google Scholar]
- 10.Bederman SS, et al. Drivers of surgery for the degenerative hip, knee, and spine: a systematic review. Clinical Orthopaedics and Related Research®. 2012;470(4):1090–1105. doi: 10.1007/s11999-011-2004-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalanithi PA, Arrigo R, Boakye M. Morbid obesity increases cost and complication rates in spinal arthrodesis. Spine. 2012;37(11):982–988. doi: 10.1097/BRS.0b013e31823bbeef. [DOI] [PubMed] [Google Scholar]
- 12.Fang A, et al. Risk factors for infection after spinal surgery. Spine. 2005;30(12):1460–1465. doi: 10.1097/01.brs.0000166532.58227.4f. [DOI] [PubMed] [Google Scholar]
- 13.Silber JH, et al. Medical and financial risks associated with surgery in the elderly obese. Annals of surgery. 2012;256(1):79–86. doi: 10.1097/SLA.0b013e31825375ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehta AI, et al. 2012 Young Investigator Award winner: The distribution of body mass as a significant risk factor for lumbar spinal fusion postoperative infections. Spine. 2012;37(19):1652–1656. doi: 10.1097/BRS.0b013e318241b186. [DOI] [PubMed] [Google Scholar]
- 15.MC VLDIR. Positioning of patients for operation. Stiefel RH, Electricity, electrical safety, and instrumentation in the operating room. 1993:43. [Google Scholar]
- 16.Williamson JA, WR, Szekely S, Gillies ER, Dreosti AV. The Australian Incident Monitoring Study. Difficult intubation: an analysis of 2000 incident reports. Anaesth Intensive Care. 1993;21:5. doi: 10.1177/0310057X9302100518. [DOI] [PubMed] [Google Scholar]
- 17.Juvin PM, PhD, Blarel Anne, Bruno Fabienne, Desmonts Jean-Marie MD. Is Peripheral Line Placement More Difficult in Obese Than in Lean Patients? Anesthesia & Anangesia. 2003;96(4) doi: 10.1213/01.ANE.0000050570.85195.29. [DOI] [PubMed] [Google Scholar]


