Abstract
There is increasing evidence that patients who have problems with binge eating (BE) or BE disorder (BED) are quite common among the severely obese, including bariatric surgery candidates. The literature suggests that in many cases such eating behaviours improve after bariatric surgery, although this is not uniformly true. The current paper reviews the data on the development of BE, BED and loss of control (LOC) eating after bariatric surgery and the impact of these problems on long-term weight outcome. A search was made of various databases regarding evidence of BE, BED and LOC eating post-operatively in bariatric surgery patients. The data extracted from the literature suggests that 15 research studies have now examined this question. Fourteen of the available 15 studies suggest that the development of problems with BE, BED or LOC eating post-bariatric surgery is associated with less weight loss and/or more weight regain post-bariatric surgery. These data suggests that it is important to identify individuals at high risk for these problems, to follow them post-operatively, and, if appropriate interventions can be developed if such behaviours occur in order to maximize weight loss outcomes.
Keywords: binge eating disorder, obesity, outcome
Introduction
Obesity, defined as body mass index (BMI) ≥30, is increasing in prevalence in the US and globally (Moyer, 2012). It is estimated that approximately 34.4% of the US population was obese in 2007–2009 (Shields, Carol, & Ogden, 2011). Current treatments include pharmacotherapy, dietary therapy, behaviour therapy and physical activity for the obese (Recommendation on Screening; Am Fam Physician, 2012). Bariatric surgery is indicated for the morbidly obese (BMI ≥ 40) or those who are obese with a BMI ≥ 35 with at least two known associated adverse medical sequelae of obesity (Shirmer & Schauer, 2010). Depending on the type of operative procedure, both volume restriction and/or nutrient malabsorption contribute to significant excess weight loss, often accompanied by resolution of or improvement in obesity-related comorbidities. However, there is a subset of patients that either do not lose a substantial amount of weight or regain the lost weight at long-term follow-up (Frank & Crookes, 2010). Attempts to determine preoperative characteristics of the patients who have a worse outcome have been made, yet few clear predictors of such outcomes have emerged and been replicated (van Hout, 2005; Livhits et al., 2012).
A review of the extant literature reveals a dearth of longitudinal data for patients who have undergone bariatric surgery, although some long-term studies are currently underway (Belle et al., 2007; Sjöström, 2008). Several non-surgical factors have long been reported as influencing outcomes of bariatric surgery (Hsu et al., 1998; Sarwer, Wadden, & Fabricatore, 2005; van Hout, Verschure, & van Heck, 2005), and some attention has been focused on the presence of maladaptive eating patterns such as binge eating (BE) (Saunders, 1999; Green, Dymek-Valentine, Pytluk, le Grange, & Alverdy, 2004; Kalarchian et al., 2002; Wood & Ogden, 2012), BE disorder (BED) and eating with a sense of loss of control (LOC) (Burgmer et al., 2005; Colles, Dixon, & O’Brien, 2008). These have been associated with increased caloric intake, poorer outcomes and ultimately, failure of treatment (Bocchieri, Meana, & Fisher, 2002).
One of the areas of interest in the eating disorders, obesity and particularly in the bariatric surgery literature is the concept of ‘loss of control’ eating (Bocchieri et al., 2002). LOC eating is required in association with the usual criteria for BE in those with bulimia nervosa and/or BE disorder, and those problems generally requires the ingestion of an objectively large amount of food for an eating episode to constitute an eating binge. However, after bariatric surgery, the ingestion of an objectively large amount is difficult or impossible, although literature suggests that eventually, some post-bariatric patients can ingest an objectively large amount of food. The term LOC eating is now used at times instead of BE because of this limitation. Also, some authors have suggested that BE should be characterized by the sense of LOC rather than the quantity of food ingested (Hsu, Sullivan, & Benotti, 1997; Niego, Pratt, & Agras, 1997). Nonetheless, obese patients undergoing bariatric surgery and reporting LOC, even if that doesn’t include an objective large amount of food, seem to share with eating disordered patients elements of the psychopathological core of eating disorders (ED), presenting dysfunctional shape, weight and eating attitudes and high levels of psychosocial distress (de Zwaan, 2001; Hsu et al., 2002).
One point of interest concerns whether problems with BE, BED or LOC prior to surgery might be associated with less weight loss or more weight regain after surgery. As a corollary, researchers have also been interested in determining if such problems as BE, BED or LOC, may emerge or re-emerge after surgery, and then compromise weight outcomes. The first question has been addressed in a number of studies and in the majority of these studies BE, BED and LOC pre-surgery do not appear to be consistently predictive of weight outcomes (see, for example, de Zwaan et al., 2010; Hsu, Betancourt, & Sullivan, 1996; Kalarchian, Wilson, Brolin, & Bradley, 1999; and Powers, Perez, Boyd, & Rosemurgy, 1999), although some studies have reported worst outcomes for pre-surgery BE patients (Green et al., 2004; Sallet et al., 2007; Scholtz et al., 2007), and other studies reported that weight loss was greatest for those with pre-surgery BE (Boan, Kolotkin, Westman, McMahon, & Grant, 2004; Latner, Wetzler, Goodman, & Glinski, 2004; Malone & Alger-Mayer, 2004). However, the literature addressing the second question concerning post-surgery eating behaviour has yielded more consistent results. In this paper, we will restrict our focus to studies addressing BE/BED/LOC eating seen post-bariatric surgery, and review the literature on the prevalence and impact of post-surgery BE/BED/LOC eating on weight loss and weight regain. This literature was previously reviewed by Niego, Kofman, Weiss, and Geliebter in 2007.
Method
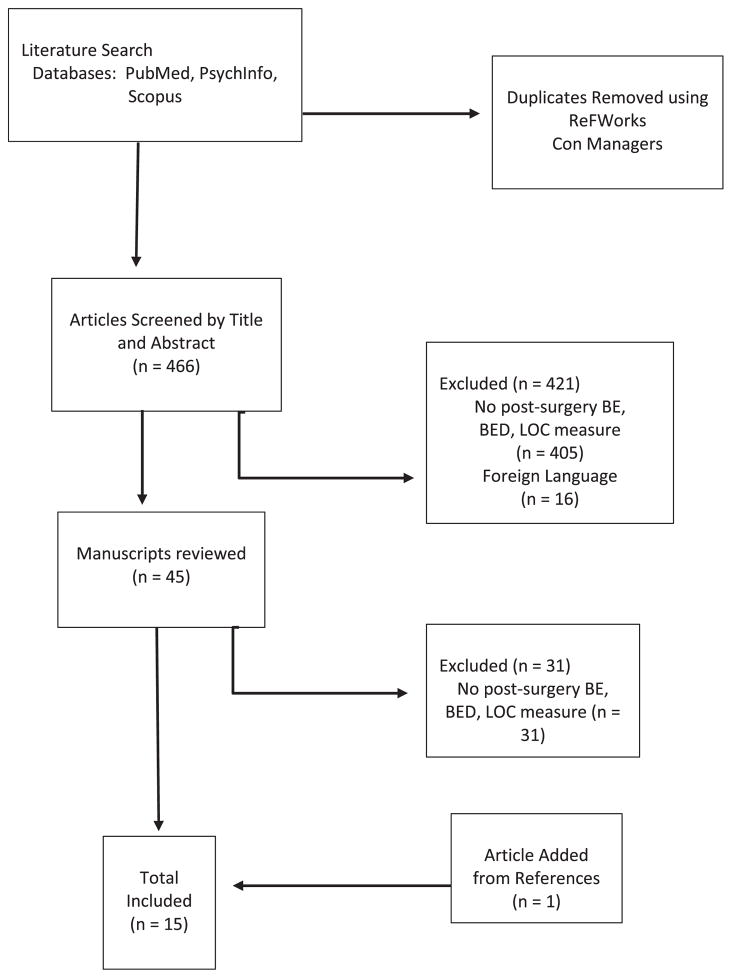
A search by Pubmed, PsycInfo and Scopus was conducted using the terms Roux-en-Y anastamosis and obesity, bariatric surgery, obesity surgery, gastric bypass, gastroplasty, jejunoileal bypass and lipectomy. We combined these terms with BED, BE, bulimia nervosa and LOC. Dates searched began in April 2013 and ranged back to 1954 for PsycInfo, 1966 for Pubmed and no limits were used for Scopus. The study selection is shown in Figure 1.
Figure 1.
Study selection flow diagram
Results
The data extracted from the available literature are summarized in Table 1 and will only be briefly reviewed here. Studies dating back to 1992 have addressed this issue. Sample sizes have varied widely, from a minimum of 16 subjects to a maximum of 497 in the report by Kofman, Lent, and Swencionis (2010). A number of the samples have focused on patients who have undergone Roux-en-Y gastric bypass with a minority focusing on gastric bands and several early reports focusing on vertical banded gastroplasty. In one of the reports, different types of procedures were utilized (de Man Lapidoth, Ghaderi, & Norring, 2011). The durations of follow-up have also varied widely and frequently have included large ranges, with the longest follow-up study having been reported at 14 years by Mitchell et al. (2001). Various assessment strategies have been employed some using self-report and/or structured instruments such as the Eating Disorder Examination and the Structured Clinical Interview for the DSM. Of critical importance, the definitions of BE, BED (because this construct evolved over the time these publications appeared) and loss of control eating have varied across these studies, making comparisons difficult. This is likely reflected in the wide disparity in the prevalence of the rates of such behaviours in these reports, even among the studies with large sample sizes.
Table 1.
Description of studies included in the review
| Year | Author(s) | Site | Procedure | N | Meana Duration F/U | Assessmentb | Behaviour measuredc
|
Post-surgeryc | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-surgery | Post-surgery | ||||||||||
|
| |||||||||||
| BE/BED | LOC | BE/BED | LOC | BE/BED/LOC predictive of ↓ weight loss | |||||||
| 1992 | Rowston et al. | University of London | BPD | 16 | 2 years | BITE | — | — | — | — | Yes |
| 1994 | Pekkarinen et al. | Helskinki | VBG | 27 | 5.4 years | BES/BITE | — | — | 37% | — | Yes |
| 1996 | Hsu et al. | Tufts | VBG | 24 | ≤3.5 years | EDE | 38% | — | — | 21% | Yes |
| 2001 | Mitchell et al. | University of North Dakota | RYGB | 78 | 14 years | Interview M-FED (SCID criteria) | 49% | — | 12% | — | Yes |
| 2002 | Kalarchian et al. | University of Pitt | RYGB | 99 | >2<7 years | EDE-Q | — | — | — | 46% | Yes |
| 2003 | Guisado & Vaz | Extremadura | VBG | 140 | 18 months | BES | — | — | 18% | — | Yes |
| 2004 | Larsen et al. | Nijmegen | Band | 157 | 34 months. | BES | 55.9% | — | 37.4% | — | Yes |
| 2007 | Scholtz et al | University of London | LAGB | 37 | 5 years. | Interview/EDE | 17% | 13% | 10% | 8% | Yes |
| 2008 | Colles et al. | Monash | Band | 129 | 12 months. | QEWP-R/Interview | 14% | 3% | — | Yes | |
| 2010 | White et al. | Yale | RYGB | 361 | 1, 2 years. | EDE-Q | — | 61% | — | 36%/39% | Yes |
| 2010 | de Zwaan et al. | University of North Dakota | RYGB | 59 | 2 years. | Interview EDE-BSV | 29% | 25% | Yes | ||
| 2010 | Koffman et al. | Yeshiva New York | RYGB | 497 | 3–10 years. | QEWP-R | — | — | 27%/18% | 50% | Yes |
| 2011 | de Man Lapidoth et al. | Sweden | Variable | 102 | 3 years. | EDE-Q | 17.6% | — | 28.4% | — | No |
| 2012 | Beck et al. | University South Denmark | RYGB | 45 | 2 years. | ‘BE Survey’ | — | — | — | — | Yes |
| 2012 | Wood et al. | University of Surrey | LAGB | 33 | 6 months | EDDS | 50% | — | 7% | — | Yes |
Duration from surgery to follow-up assessment
Assessment instrument used: BITE, Bulimia Investigatory Test, Edinburgh; BES, Binge Eating Scale; EDE, Eating Disorders Examination; M-FED, McKnight Follow-up for Eating Disorders; EDE-Q, Eating Disorders Examination-Questionnaire; Interview, clinical interview; QEWP-R, Questionnaire on Eating and Weight Patterns-Revised; ‘BE Survey’, Instrument constructed for this purpose; EDDS, Eating Disorders Diagnostic Scale.
BE, Binge eating; BED, Binge eating disorders; LOC, Loss of control eating.
The prior review by Niego et al. published in 2007 included literature through 2006; therefore, approximately half of the studies cited in our current review would have been included. In this review, they found that the literature supported the notion that significant BE was related to poorer surgical outcome, and if such a behaviour was retained after surgery, the result was poorer weight loss outcomes.
In the only negative study reported to date, de Man Lapidoth et al. (2011) collected data from 4 surgery centres in Sweden. Various bariatric procedures were employed. One hundred two provided follow-up data, which revealed that 29 (28.4%) reported post-operative BE. This group did not differ from those not reporting this symptom on a three-year BMI outcome. BE after weight loss surgery was associated with psychopathology and lower self-reported health-related quality of life. The authors stressed that the occurrence of such problems suggests a need for surgical teams to be observant about the occurrence of these behaviours.
Discussion
A review of these data show several important points: first, the disappearance of pre-surgery BE with surgery in a significant percentage of patients has been frequently described. About one-half of the studies evaluated pre-operative eating-disordered behaviour, with two studies examining what was labelled pre-operative LOC rather than BE, although LOC would have been assessed in other studies given that subjects satisfied criteria for BE. LOC eating episodes that were not BE episodes might have been underreported in the studies reporting only BE or BED. Second, all but one study suggest that the presence of BE/BED/LOC eating post-operatively is associated with less weight loss or more weight regain. Additionally, we see that of the studies that did evaluate post-operative BE/BED/LOC eating, rates varied widely from 0% in Latner et al. (2004) to 46% in the Kalarchian et al. paper (2002). Possible contributors to this wide variance include the different types of surgery employed (e.g. LAGB vs Roux-en-Y gastric bypass vs vertical banded gastroplasty), and the type of assessment (e.g. self-report measures vs face-to-face interview; QEWP-R vs EDE-Q), as well as length of time to follow-up. Additionally, in obesity, BE episodes are known to be difficult to assess because they are not as distinctive as such episodes in bulimia nervosa, where they are often terminated with some type of compensatory behaviour such as vomiting (de Zwaan et al., 2004; Marcus, Smith, Santelli, & Kaye, 1992). There are other potential problems with the LOC construct that require further clarification. For example, there are concerns that this label may be applied retrospectively by patients who assess that an eating episode was problematic. There also may be gradations of LOC, as opposed to viewing this characteristic as a dichotomous variable (Mitchell et al., 2012).
A possible interactive effect between of LOC and time has also been highlighted. Hsu and colleagues (1997) found that the initial improvement in pre-surgery ED status erodes after 2 years, significantly predicting poorer outcomes, and Sallet et al. (2007) noted that at two years’ post-surgery, the association between pre-surgery BE status and weight outcomes becomes more clearly manifested. These findings suggest that data collected with less than two years of follow-up may be misread. However, other work suggests value in having LOC assessed fairly early in follow-up. The prospective value of LOC eating was described by White and colleagues (2010). These authors found that LOC at 6 months significantly predicted weight loss at latter assessment times, and LOC at 12 months significantly predicted weight loss at 24 months.
Another factor that may account for the contradictory data is that different studies use different weight outcomes (BMI, BMI loss, % excess weight loss, weight regain), and that only a small group of studies assessed concomitant depressive symptoms and other potentially maladaptive eating behaviours such as grazing, nibbling, sweet eating or night eating syndrome. Although BE may be physically impossible for many patients due to surgical restriction of gastric volume, a different form of compulsive eating may emerge after surgery, and new maladaptive eating behaviours, like grazing (Saunders, 2001), rumination (chewing food, then spitting it out) as well as LOC (White, Kalarchian, Masheb, Marcus, & Grilo, 2010). These might appear to serve the same function as the previous BE (Saunders, 2004), resulting in excessive caloric intake and ultimately weight regain (van Hout et al., 2005).
The importance of considering the presence of LOC eating postoperatively seems to be clear in order to better understand weight loss and weight regain after bariatric surgery. However, important questions on different dimensions of this behaviour remain unanswered. Regarding the (re) emergence of BE/BED/LOC: why do some people experience BE/BED/LOC eating at times (re)emerging of this after surgery, whereas others do not? Is there a critical follow-up time for the emergence of these problems post-operatively? What are the predictive factors for the emergence or reemergence of these problems? Can clinicians distinguish, before surgery patients that will maintain their BE/BED/LOC status after surgery from those who will remit? Regarding the association with other dysfunctional eating behaviours or eating psychopathology: does pre-operative BE/BED/LOC eating develop into other eating behaviours (e.g. grazing) that also have an important impact on weight outcomes after surgery? Do such problems overlap with other maladaptive eating behaviours resulting in greater impact on weight loss/regain? Regarding treatment and health services: can clinicians prevent or treat the (re)emergence of BE/BED/LOC eating post-operatively? To our knowledge, no systematic work has been reported in this area.
In conclusion, the variability in weight outcomes after bariatric surgery is considerable, particularly at long-term follow-up, and dysfunctional eating appears to be associated with weight regain. However, the factors contributing to successful outcomes after surgery are complex, multiple and probably time-related, and the importance of single-predictive variables should not be over emphasized.
Because eating behaviours post-operatively are associated with weight loss and/or regain, attention should be focused on the follow-up period. Considering the prospective value of BE/BED/LOC eating, a preventive attitude based or early detection appear to be sensitive strategies to help prevent poor outcomes, and there is a clear need for studies focusing on prevention and treatment.
In summary, our findings agree with conclusions offered by Niego, Pratt and Agras in an earlier review (2007) suggesting that the emergence or re-emergence of BE/BED/LOC after bariatric surgery results in less weight loss and/or more weight regain. The available literature, with the exception of the study by de Man Lapidoth et al. (2011), support such an association.
Acknowledgments
Supported by RO1 DK 84979 (JEM) from the National Institute of Diabetes, Digestive and Kidney Diseases in the National Institutes of Health.
References
- Beck NN, Mehlsen M, Støving RK, Alverdy C, le Grange D. Psychological characteristics and associations with weight outcomes two years after gastric bypass surgery: postoperative eating disorder symptoms are associated with weight loss outcomes. Eating Behaviors. 2012;13:394–397. doi: 10.1016/j.eatbeh.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Belle S, Berk P, Courcoulas A, Flum D, Miles C, Mitchell J, et al. Longitudinal assessment of bariatric surgery consortium writing group. Safety and efficacy of bariatric surgery: longitudinal assessment of bariatric surgery. Surgery for Obesity and Related Disorders. 2007;3:116–126. doi: 10.1016/j.soard.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boan J, Kolotkin RL, Westman EC, McMahon RL, Grant JP. Binge eating, quality of life and physical activity improve after Roux-en-Y gastric bypass for morbid obesity. Obesity Surgery. 2004;14:341–348. doi: 10.1381/096089204322917864. [DOI] [PubMed] [Google Scholar]
- Bocchieri LE, Meana M, Fisher BL. A review of psychosocial outcomes of surgery for morbid obesity. Journal of Psychosomatic Research. 2002;52:155–165. doi: 10.1016/s0022-3999(01)00241-0. [DOI] [PubMed] [Google Scholar]
- Burgmer R, Grigutsch K, Zipfel S, Wolf AM, de Zwaan M, Husemann B, et al. The influence of eating behavior and eating pathology on weight loss after gastric restriction operations. Obesity Surgery. 2005;15:684–691. doi: 10.1381/0960892053923798. [DOI] [PubMed] [Google Scholar]
- Colles SL, Dixon JB, O’Brien PE. Grazing and loss of control related to eating: two high-risk factors following bariatric surgery. Obesity. 2008;16:615–622. doi: 10.1038/oby.2007.101. [DOI] [PubMed] [Google Scholar]
- Frank P, Crookes P. Short- and long-term surgical follow-up of the post-bariatric surgery patient. Gastroenterology Clinics of North America. 2010;39:135–146. doi: 10.1016/j.gtc.2009.12.011. [DOI] [PubMed] [Google Scholar]
- Green AEC, Dymek-Valentine M, Pytluk S, Le Grange Dl, Alverdy J. Psychosocial outcome of gastric bypass surgery for patients with and without binge eating. Obesity Surgery. 2004;14:975–985. doi: 10.1381/0960892041719590. [DOI] [PubMed] [Google Scholar]
- Guisado Macias J, Vaz Leal F. Psychopathological differences between morbidly obese binge eaters and non-binge eaters after bariatric surgery. Eating and Weight Disorders. 2003;8:315–318. doi: 10.1007/BF03325032. [DOI] [PubMed] [Google Scholar]
- van Hout G. Psychosocial effects of bariatric surgery. Acta chirurgica Belgica. 2005;105:40–43. [PubMed] [Google Scholar]
- van Hout GCM, Verschure SKM, van Heck GL. Psychosocial predictors of success following bariatric surgery. Obesity Surgery. 2005;15:552–560. doi: 10.1381/0960892053723484. [DOI] [PubMed] [Google Scholar]
- Hsu L, Benotti PN, Dwyer J, Roberts SB, Saltzman E, Shikora S, et al. Non-surgical factors that influence the outcome of bariatric surgery: a review. Psychosomatic Medicine. 1998;60:338–346. doi: 10.1097/00006842-199805000-00021. [DOI] [PubMed] [Google Scholar]
- Hsu LKG, Betancourt S, Sullivan SP. Eating disturbances before and after vertical banded gastroplasty: a pilot study. International Journal of Eating Disorders. 1996;19:23–34. doi: 10.1002/(SICI)1098-108X(199601)19:1<23::AID-EAT4>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- Hsu LKG, Mulliken B, McDonagh B, Krupa Das S, Rand W, Fairburn CG, et al. Binge eating disorder in extreme obesity. International Journal of Obesity. 2002;26:1398–1403. doi: 10.1038/sj.ijo.0802081. [DOI] [PubMed] [Google Scholar]
- Hsu LKG, Sullivan SP, Benotti PN. Eating disturbances and outcome of gastric bypass surgery: a pilot study. International Journal of Eating Disorders. 1997;21:385–390. doi: 10.1002/(sici)1098-108x(1997)21:4<385::aid-eat12>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Kalarchian MA, Marcus MD, Wilson GT, Labouvie EW, Brolin RE, LaMarca LB. Binge eating among gastric bypass patients at long-term follow-up. Obesity Surgery. 2002;12:270–275. doi: 10.1381/096089202762552494. [DOI] [PubMed] [Google Scholar]
- Kalarchian M, Wilson G, Brolin R, Bradley L. Effects of bariatric surgery on binge eating and related psychopathology. Eating and Weight Disorders. 1999;4:1–5. doi: 10.1007/BF03376581. [DOI] [PubMed] [Google Scholar]
- Kofman MD, Lent MR, Swencionis C. Maladaptive eating patterns, quality of life, and weight outcomes following gastric bypass: Results of an internet survey. Obesity. 2010;18:1938–1943. doi: 10.1038/oby.2010.27. [DOI] [PubMed] [Google Scholar]
- Larsen JK, van Ramshorst B, Geenen R, Brand N, Stroebe W, van Doornen LJP. Binge eating and its relationship to outcome after laparoscopic adjustable gastric banding. Obesity Surgery. 2004;14:1111–1117. doi: 10.1381/0960892041975587. [DOI] [PubMed] [Google Scholar]
- Latner JD, Wetzler S, Goodman ER, Glinski J. Gastric bypass in a low-income, inner-city population: eating disturbances and weight loss. Obesity Research. 2004;12(6):956–961. doi: 10.1038/oby.2004.117. [DOI] [PubMed] [Google Scholar]
- Livhits M, Mercado C, Yermilov I, Parikh JA, Dutson E, Mehran A, et al. Pre-operative predictors of weight loss following bariatric surgery: systematic review. Obesity Surgery. 2012;22:70–89. doi: 10.1007/s11695-011-0472-4. [DOI] [PubMed] [Google Scholar]
- Malone M, Alger-Mayer S. Binge status and quality of life after gastric bypass surgery: a one-year study. Obesity Research. 2004;12 doi: 10.1038/oby.2004.53. [DOI] [PubMed] [Google Scholar]
- de Man Lapidoth L, Ghaderi A, Norring C. Binge eating in surgical weight-loss treatments: long-term associations with weight loss, health related quality of life (HRQL), and psychopatholoty. Eating and Weight Disorders. 2011;16:263–269. doi: 10.1007/BF03327470. [DOI] [PubMed] [Google Scholar]
- Marcus M, Smith D, Santelli R, Kaye W. Characterization of eating disordered behavior in obese binge eaters. International Journal of Eating Disorders. 1992;12:249–256. [Google Scholar]
- Mitchell JE, Karr TM, Peat C, Wonderlich S, Crosby RD, Engel S, et al. A fine-grained analysis of eating behavior in women with bulimia nervosa. International Journal of Eating Disorders. 2012;3:400–406. doi: 10.1002/eat.20961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JE, Lancaster KL, Burgard MA, Howell LM, Krahn DD, Crosby RD, et al. Long-term follow-up of patients’ status after gastric bypass. Obesity Surgery. 2001;11:464–468. doi: 10.1381/096089201321209341. [DOI] [PubMed] [Google Scholar]
- Moyer V. US preventive services task force. Screening for and management of obesity in adults: US preventive services task force recommendation statement. Annals of Internal Medicine. 2012;157:373–378. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- Niego SH, Kofman MD, Weiss JJ, Geliebter A. Binge eating in the bariatric surgery population: a review of the literature. International Journal of Eating Disorders. 2007;40:349–359. doi: 10.1002/eat.20376. [DOI] [PubMed] [Google Scholar]
- Niego SH, Pratt EM, Agras WS. Subjective or objective binge: is the distinction valid? International Journal of Eating Disorders. 1997;22:291–298. doi: 10.1002/(sici)1098-108x(199711)22:3<291::aid-eat8>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Pekkarinen T, Koskela K, Huikuri K, Mustajoki P. Long-term results of gastroplasty for morbid obesity: binge-eating as a predictor of poor outcome. Obesity Surgery. 1994;4:248–255. doi: 10.1381/096089294765558467. [DOI] [PubMed] [Google Scholar]
- Powers PS, Perez A, Boyd F, Rosemurgy A. Eating pathology before and after bariatric surgery: a prospective study. International Journal of Eating Disorders. 1999;25:293–300. doi: 10.1002/(sici)1098-108x(199904)25:3<293::aid-eat7>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Rowston W, McCluskey S, Gazet J, Lacey J, Franks G, Lynch D. Eating behavior, physical symptoms and psychosocial factors associated with weight reduction following the Scopinaro operation as modified by Gazet. Obesity Surgery. 1992;2:335–360. doi: 10.1381/096089292765559954. [DOI] [PubMed] [Google Scholar]
- Sallet PC, Sallet JA, Dixon JB, Collis E, Pisani CE, Levy A, et al. Eating behavior as a prognostic factor for weight loss after gastric bypass. Obesity Surgery. 2007;17:445–451. doi: 10.1007/s11695-007-9077-3. [DOI] [PubMed] [Google Scholar]
- Sarwer DB, Wadden TA, Fabricatore AN. Psychosocial and behavioral aspects of bariatric surgery. Obesity Research. 2005;13:639–648. doi: 10.1038/oby.2005.71. [DOI] [PubMed] [Google Scholar]
- Saunders R. Binge eating in gastric bypass patients before surgery. Obesity Surgery. 1999;9:72–76. doi: 10.1381/096089299765553845. [DOI] [PubMed] [Google Scholar]
- Saunders R. Compulsive eating and gastric bypass surgery: what does hunger have to do with it? Obesity Surgery. 2001;11:757–761. doi: 10.1381/09608920160558731. [DOI] [PubMed] [Google Scholar]
- Saunders R. “Grazing”: a high-risk behavior. Obesity Surgery. 2004;14:98–102. doi: 10.1381/096089204772787374. [DOI] [PubMed] [Google Scholar]
- Scholtz S, Bidlake L, Morgan J, Fiennes A, El-Etar A, Lacey JH, et al. Long-term outcomes following laparoscopic adjustable gastric banding: post-operative psychological sequelae predict outcome at 5-year follow-up. Obesity Surgery. 2007;17:1220–1225. doi: 10.1007/s11695-007-9212-1. [DOI] [PubMed] [Google Scholar]
- Screening for and management of obesity in adults. Recommendation statement. American Family Physician. 2012;86:1–3. [PubMed] [Google Scholar]
- Shields M, Carol M, Ogden C. Adult obesity prevalence in Canada & the United States. NCNS Data Briefs. 2011;56 [PubMed] [Google Scholar]
- Shirmer B, Schauer P. Schwartz’s Principles of Surgery. Chapter 27. New York, NY: McGraw Hill; 2010. Surgical management of obesity. [Google Scholar]
- Sjöström L. Bariatric surgery and reduction in morbidity and mortality: experiences from the SOS study. International Journal of Obesity. 2008;32:93–97. doi: 10.1038/ijo.2008.244. [DOI] [PubMed] [Google Scholar]
- White MA, Kalarchian MA, Masheb RM, Marcus MD, Grilo CM. Loss of control over eating predicts outcomes in bariatric surgery patients: a prospective, 24-month follow-up study. Journal of Clinical Psychiatry. 2010;71:175–184. doi: 10.4088/JCP.08m04328blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood KV, Ogden J. Explaining the role of binge eating behavior in weight loss post-bariatric surgery. Appetite. 2012;59:177–180. doi: 10.1016/j.appet.2012.04.019. [DOI] [PubMed] [Google Scholar]
- de Zwaan M. Binge eating disorder and obesity. International Journal of Obesity. 2001;25:s51–s55. doi: 10.1038/sj.ijo.0801699. [DOI] [PubMed] [Google Scholar]
- de Zwaan M, Hilbert A, Swan-Kremeier L, Simonich H, Lancaster K, Howell LM, et al. Comprehensive interview assessment of eating behavior 18–35 months after gastric bypass surgery for morbid obesity. Surgery for Obesity and Related Diseases. 2010;6:79–85. doi: 10.1016/j.soard.2009.08.011. [DOI] [PubMed] [Google Scholar]
- de Zwaan M, Mitchell JE, Swan-Kremeier L, McGregor T, Howell ML, Roerig JL, et al. A comparison of different methods of assessing the features of eating disorders in post-gastric bypass patients: a pilot study. European Eating Disorders Review. 2004;12:380–386. [Google Scholar]