Abstract
Pneumoperitoneum in the neonate generally is an acute surgical emergency, which has grave implications, and immediate surgical intervention is needed to ensure survival. The most common cause is a perforated hollow viscus. However, there are causes that cannot be attributed to this etiology, constituting what has been called non-surgical, asymptomatic, benign, misleading, spontaneous or idiopathic pneumoperitoneum. Knowledge of this entity and its likely aetiological factors should improve awareness and possibly reduce the imperative to perform an unnecessary emergency laparotomy on an otherwise normal neonate with an unexplained pneumoperitoneum.
Keywords: Newborn, Spontaneous, Pneumoperitoneum, Conservative management
INTRODUCTION
Pneumoperitoneum in the neonate, generally is an acute surgical emergency which has grave implications, and immediate surgical intervention is needed to ensure survival, but it may not always be an absolute indication for surgery in neonate.[1,2] Spontaneous Pneumoperitoneum in a newborn without peritonitis, with a normal abdominal examination, is an extremely rare event which creates a dilemma for the treating surgeon regarding surgical management of the neonate. Conservative management, avoiding a laparotomy is the treatment of choice. We present herein a case of spontaneous pneumoperitoneum in a newborn who was successfully treated at our institute.
CASE REPORT
A36-week 2.1-kg preterm, female baby born to a primigravida mother by normal vaginal delivery, presented to us within first few hours of birth with respiratory distress. The mother received adequate antenatal and perinatal care and there was no history of birth asphyxia. On examination, the baby was alert but having respiratory distress in the form of grunting and subcostal recession, pulse rate-180/min, SO2-85%. The patient was stabilized and resuscitated with oropharangeal suctioning, nebulisation, oxygen therapy, intravenous fluids, antibiotics and a nasogastric tube was placed to decompress the stomach. Continuous Positive Airway Pressure (CPAP) support was given. The condition of the neonate improved. On the next day, although the general condition of the baby was stable, she developed abdominal distension and non-passage of the meconium. Abdomen was moderately distended, however, there was no erythema, tenderness or, a palpable lump [Fig.1a].The laboratory investigations were within normal range. Abdominal and chest radiographs revealed pneumoperitoneum, with free gas under both the domes of diaphragm [Fig.2a]. There was no evidence of pneumothorax or pneumomediastinum, bilateral lung fields were clear. Ultrasound showed normal domes of diaphragm.
In view of the stable general condition and without clinical evidence of necrotizing enterocolitis (NEC), pneumothorax, pneumomediastinum, and also absence of preceding event which could lead to gastrointestinal perforations, the diagnosis of spontaneous pneumoperitoneum was made. It was decided to continue with the conservative treatment. The patient was kept under close monitoring with frequent abdominal girth measurements to detect any deterioration in the condition. The abdominal distension resolved [Fig.1b]. The baby passed meconium plugs initially followed by normal meconium on administration of saline enema. Repeat abdominal radiographs showed resolution of pneumoperitoneum [Fig.2b]. A trial feed was well tolerated and was slowly graduated to full feeds by the seventh day of admission. The neonate was discharged and is doing well on follow-up.

Figure 1: (a) Clinical photographs of the neonate with abdominal distension (top). (b) Clinical photograph after resolution of spontaneous Pneumoperitoneum (bottom).
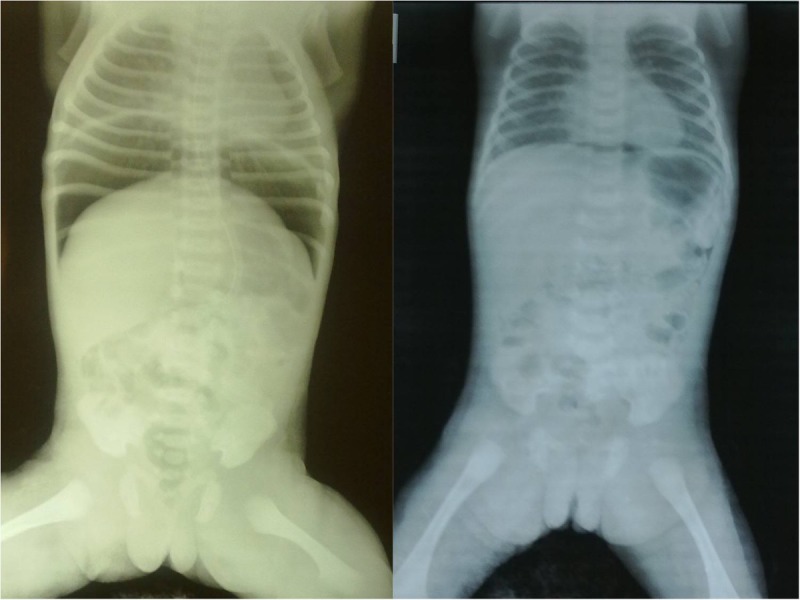
Figure 2: (a) Radiographs revealing the pneumoperitoneum (left). (b) Radiographs revealing resolution of spontaneous pneumoperitoneum after conservative management (right).
DISCUSSION
Besides NEC which is the most common cause of pneumoperitoneum in a neonate, there are numerous other surgical causes of pneumoperitoneum and these include gastric and duodenal perforations, isolated colonic perforations, caecal perforations, perforated pouch colon, idiopathic gastric necrosis, and necrosis of small intestine or colon secondary to intestinal atresia, volvulus, meconium ileus, Hirschsprung's disease or Meckel's diverticulum.[3] Other rare causes of neonatal intestinal perforation could be mechanical injury from the gavage tubes, rectal thermometers, rectal tubes used for rectal washes, resuscitation with oxygen under pressure in patients with distal pyloric or duodenal obstruction, congenital defects of the musculature and diverticula.[3,4] The usual accepted mode of treatment of neonates with pneumoperitoneum and necrotizing enterocolitis (NEC) with pneumoperitoneum is operative management.
Since 1966, when an article had concluded that every newborn infant with pneumoperitoneum must undergo laparotomy, a lot of paradigm shift in the management has occurred over the over last few decades.[5] It is the result of increasing awareness regarding the entity called spontaneous pneumoperitoneum, among experienced paediatric surgeons. It is also known as non-surgical, asymptomatic, benign, misleading, spontaneous or idiopathic pneumoperitoneum.[1,6,7]
As spontaneous pneumoperitoneum has been earlier reported in premature infants who are on mechanical ventilation for pulmonary or cardiac diseases.[1,8] In the index case, all of the earlier mentioned causes were absent and pneumoperitoneum was the result of oxygen therapy in the form of CPAP. The pathophysiology of the appearance of pneumoperitoneum could possibly be extension of free air under tension in the mediastinum along the vascular planes through the normal diaphragmatic openings, retrograde path through the pulmonary lymphatics, congenital diaphragmatic hernia or from a pleuroperitoneal fistula.[1,2,6-10]
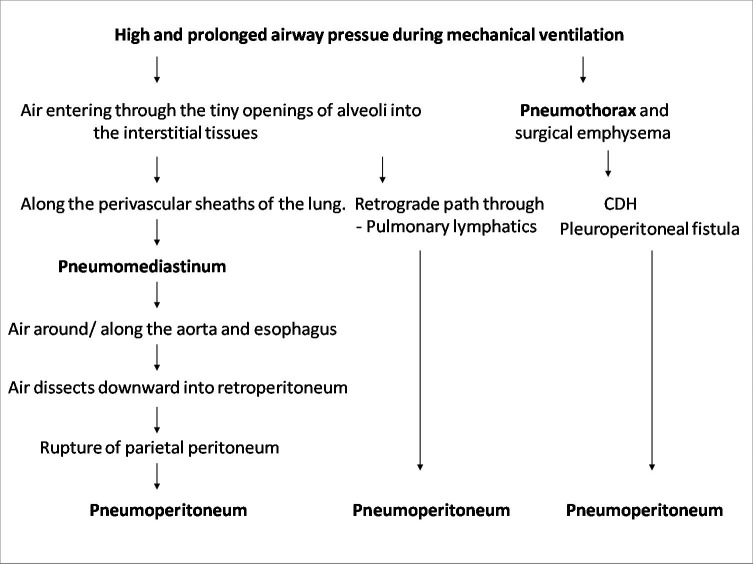
A flow chart [Fig. 3] to explain the mechanism in the development of spontaneous pneumoperitoneum is proposed after imbibing the ideas from the works of Macklin and Williams.[1,10]
Figure 3: A flow chart to explain the mechanism in the development of spontaneous pneumoperitoneum.
Presence of pneumothorax or pneumomediastinum immediately before or simultaneously with pneumoperitoneum is a pointer towards spontaneous pneumoperitoneum, although it may be absent in few cases, which happened in our case.[6-10]
A neonate with radiographs showing pneumoperitoneum requires a thorough clinical (abdominal and pulmonary signs) and laboratory correlation (blood parameters and blood gases) to establish the aetiology of perforation to direct further management. The indications for surgical intervention in pneumoperitoneum are the features of peritonitis, pain, cardiovascular instability, leucocytosis, evidence of leakage from gastrointestinal tract and failure of conservative management.[1]
Footnotes
Source of Support: Nil
Conflict of Interest: None
References
- 1. doi: 10.1136/pgmj.73.863.531. Williams NM, Watkin DF. Spontaneous pneumoperitoneum and other nonsurgical causes of intraperitoneal free gas. Postgrad Med J. 1997; 73:531-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zerella JT, James V, McCullough JV: Pneumoperitoneum in infants without gastrointestinal perforation. Surgery. 1981;89:163-7. [PubMed] [Google Scholar]
- 3. doi: 10.1007/s00383-009-2488-6. Khan TR, Rawat JD, Ahmed I, Rashid KA, Maletha M, Wakhlu A, et al. Neonatal pneumoperitoneum: a critical appraisal of its causes and subsequent management from a developing country. PediatrSurg Int. 2009; 25:1093-7. [DOI] [PubMed] [Google Scholar]
- 4. doi: 10.4103/0189-6725.86076. Khan RA, Mahajan JK, Rao KN. Spontaneous intestinal perforation in neonates: Is surgery always indicated? Afr J Paediatr Surg 2011;8:249-51. [DOI] [PubMed] [Google Scholar]
- 5. Miller JA: The ‘Football sign’ in neonatal perforation. Am J Dis Child.1962; 104:311-2 . [Google Scholar]
- 6. Agrawal D,Taneja S, Avasthi S. Spontaneous idiopathic pneumoperitoneum in a newborn. Pediatric Oncall [serial online] 2012;9:4. [Google Scholar]
- 7. Shah R S, Patel M P, Pikale H S, Kulkarni B K, Borwankar S S. Benign neonatal pneumoperitoneum--an enigma. J Postgrad Med. 1992; 38:84-5 . [PubMed] [Google Scholar]
- 8. doi: 10.1001/archpedi.1974.02110300087011. Leonidas JC. Hall RT, Rhodas PG, Amourv RA. Pneumoperitoneutm in ventilated newborns. Am J Dis Child. 1974;128:677-8. [DOI] [PubMed] [Google Scholar]
- 9. doi: 10.1016/s0022-3476(74)80121-6. Brown DR, Keenan WJ: Pneumoperitoneum without gastrointestinal perforation in a neonate. J PediatrSurg. 1974;85:377-8 . [DOI] [PubMed] [Google Scholar]
- 10. Macklin CC. Transport of air along sheaths of pulmonic blood vessels to mediastinum: clinical implications. Arch Intern Med.1939;64:913-6. [Google Scholar]