Abstract
Outcome-driven recommendations about time intervals during which ambulatory blood pressure should be measured to diagnose white-coat or masked hypertension are lacking. We cross-classified 8237 untreated participants (mean age, 50.7 years; 48.4% women) enrolled in 12 population studies, using ≥140/≥90, ≥130/≥80, ≥135/≥85, and ≥120/≥70 mm Hg as hypertension thresholds for conventional, 24-hour, daytime, and nighttime blood pressure. White-coat hypertension was hypertension on conventional measurement with ambulatory normotension, the opposite condition being masked hypertension. Intervals used for classification of participants were daytime, nighttime, and 24 hours, first considered separately, and next combined as 24 hours plus daytime or plus nighttime, or plus both. Depending on time intervals chosen, white-coat and masked hypertension frequencies ranged from 6.3% to 12.5% and from 9.7% to 19.6%, respectively. During 91 046 person-years, 729 participants experienced a cardiovascular event. In multivariable analyses with normotension during all intervals of the day as reference, hazard ratios associated with white-coat hypertension progressively weakened considering daytime only (1.38; P=0.033), nighttime only (1.43; P=0.0074), 24 hours only (1.21; P=0.20), 24 hours plus daytime (1.24; P=0.18), 24 hours plus nighttime (1.15; P=0.39), and 24 hours plus daytime and nighttime (1.16; P=0.41). The hazard ratios comparing masked hypertension with normotension were all significant (P<0.0001), ranging from 1.76 to 2.03. In conclusion, identification of truly low-risk white-coat hypertension requires setting thresholds simultaneously to 24 hours, daytime, and nighttime blood pressure. Although any time interval suffices to diagnose masked hypertension, as proposed in current guidelines, full 24-hour recordings remain standard in clinical practice.
Keywords: ambulatory blood pressure monitoring, cardiovascular risk, masked hypertension, population science, white-coat hypertension
Ambulatory blood pressure should be offered to those with elevated conventional blood pressure.1,2 White-coat hypertension is a condition, characterized by an elevated blood pressure on conventional office measurement, but a normal ambulatory blood pressure outside the medical environment. Conversely, masked hypertension is a normal blood pressure on conventional measurement accompanied by an elevated blood pressure on ambulatory monitoring.
To define white-coat and masked hypertension, guidelines1–5 and previous studies6,7 have applied varying thresholds during different periods of the day, which have included systolic/diastolic blood pressure thresholds of ≥130/≥80 mm Hg for the 24-hour blood pressure, ≥135/≥85 mm Hg for the daytime or awake blood pressure, and ≥120/≥70 mm Hg for the nighttime or asleep blood pressure.2,4,5 There is no firm recommendation on how to maximize discrimination of risk among patients with white-coat and masked hypertension by applying the aforementioned thresholds to 24-hour, daytime, or nighttime blood pressure levels or combinations of these intervals.2 To address this issue, we did a participant-level meta-analysis among 8237 people recruited from 12 populations and enrolled in the International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes (IDACO). We determined the long-term outcome associated with white-coat hypertension and masked as defined from ambulatory blood pressure thresholds applied during varying periods of the day.
Methods
Study Population
Previous publications have described the construction of the IDACO database in detail.8 Studies qualified for inclusion if they involved a random population sample, if baseline information on the conventional and ambulatory blood pressures and cardiovascular risk factors was available, and if subsequent follow-up included both fatal and nonfatal outcomes. All studies received ethical approval and adhered to the principles of the Declaration of Helsinki, and participants gave written informed consent.
The IDACO database8 currently includes 12 752 people representing 12 randomly recruited population cohorts9–18 with validated information on outcome. Exclusion criteria were as follows: (1) age <18 years (n=303), (2) conventional blood pressure unavailable (n=248), (3) nighttime blood pressure not recorded (n=1391),10 (4) being on antihypertensive drug treatment at baseline (n=2152), and (5) ambulatory blood pressure recordings not complying with predefined8 quality standards, including <10 daytime or <5 nighttime readings (n=421). The number of participants statistically analyzed was 8237 (Figure S1 in the online-only Data Supplement).
Cross-Classification Based on Conventional and Ambulatory Blood Pressure
Previous publications19,20 and the expanded Methods available in the online-only Data Supplement provide detailed information on conventional and ambulatory blood pressure measurement and on the anthropometric and biochemical measurements performed at baseline.
Conventional hypertension was a conventional blood pressure of 140 mm Hg systolic or 90 mm Hg diastolic or more.5 Ambulatory hypertension was a 24-hour level of 130 mm Hg systolic or 80 mm Hg diastolic or more; for the daytime blood pressure these thresholds were 135 and 85 mm Hg and for the nighttime blood pressure 120 and 70 mm Hg, respectively.5 Normotension and sustained hypertension were consistently normal or elevated levels on both conventional and ambulatory blood pressures (Figure S2). White-coat hypertension was defined as conventional hypertension in the presence of a normal ambulatory blood pressure. Masked hypertension was defined as ambulatory hypertension in participants with a normal conventional blood pressure. When systolic or diastolic blood pressure was in a different category (normotensive versus hypertensive), we considered the participant as hypertensive. Table S1 lists the thresholds and intervals used for the cross-classification of participants. For ambulatory time intervals including nested periods (24 hours±daytime±nighttime), the interval with the highest blood pressure classification (normotensive versus hypertensive) determined the ambulatory blood pressure status.
Ascertainment of Events
We ascertained vital status and the incidence of fatal and nonfatal diseases from the appropriate sources in each country, as described in detail in previous publications.19,20 Outcomes were coded according to the International Classification of Diseases (ICD). Fatal and nonfatal stroke (ICD-Eighth/Ninth Revsion [8/9] 430–434 and 436, ICD-10 I60–I64 and I67–I68) did not include transient ischemic attacks. Coronary events encompassed death from ischemic heart disease (ICD-8 411–412, ICD-9 411 and 414, and ICD-10 I20, I24–I25), sudden death (ICD-8 427.2 and 795, ICD-9 427.5 and 798, and ICD-10 I46 and R96), nonfatal myocardial infarction (ICD-8/9 410 and ICD-10 I21–I22), and coronary revascularization. Cardiac events comprised coronary end points and fatal and nonfatal heart failure (ICD-8 428, 427.1, 427.2, and 429; ICD-9 429 and ICD-10 I50 and J81). The diagnosis of heart failure required admission to hospital in the 3 cohorts.9–11 In the other cohorts, heart failure was either a clinical diagnosis or the diagnosis on the death certificate. However, in all cases the event was validated against hospital files or records held by family doctors. The cardiovascular end point included all aforementioned end points plus cardiovascular mortality (ICD-8 390–448, ICD-9 390.0–459.9, and ICD-10 I00 to I79 and R96). In all outcome analyses, we only considered the first event within each category.
Statistical Analysis
For database management and statistical analysis, we used SAS software, version 9.3 (SAS Institute Inc, Cary, NC). We compared mean values and proportions using the standard normal z test for large samples or ANOVA and the χ2-statistic, respectively. We used McNemar–Bowker test for the pairwise comparison of proportions. After stratification for cohort and sex, we interpolated missing values of body mass index (n=8) and total serum cholesterol (n=611) from the regression slope on age. In participants with unknown smoking (n=22), drinking (n=384), history of cardiovascular disease (n=1), or diabetes mellitus (n=3), we set the design variable to the cohort- and sex-specific mean of the codes (0, 1). Statistical significance was an α-level of ≤0.05 on 2-sided tests.
We calculated incidence rates in each category while standardizing by the direct method for sex and age (<40, 40–59, and ≥60 years). We used stratified Cox models to account for the heterogeneity of baseline hazards among cohorts and adjusted for sex, age, body mass index, smoking and drinking, total cholesterol, history of cardiovascular disease, and diabetes mellitus. Unless otherwise indicated, we used normotension as the reference group (hazard ratio, 1).
Results
Baseline Characteristics
Of 8237 participants, 3986 (48.4%) were women, 2438 (29.7%) were current smokers, 455 (5.5%) had diabetes mellitus, and 650 (7.9%) had a history of cardiovascular disease. Age averaged 50.7 (SD, 15.8) years. In all participants, the conventional blood pressure averaged 128.8 (21.6) mm Hg systolic and 78.6 (11.3) mm Hg diastolic. The corresponding ambulatory blood pressure levels were 122.1 (13.6) and 73.1 (8.2) mm Hg in 24-hour, 128.5 (14.5) and 78.3 (8.9) mm Hg in daytime recordings, and 111.0 (14.5) and 64.0 (9.0) mm Hg in nighttime, respectively. The median (5th–95th percentile interval) numbers of readings averaged to estimate the 24-hour, daytime, and nighttime blood pressure were 55 (35–82), 28 (15–42), and 11 (6–13), respectively.
Table 1 lists the baseline characteristics by 4 categories according to the cross-classification of conventional and 24-hour ambulatory blood pressure. The differences across the 4 categories were significant for all variables listed (P<0.0001).
Table 1.
Baseline Characteristics of 8237 Untreated Participants Cross-Classified by Conventional and 24-Hour Ambulatory Blood Pressure
| Characteristics | Normotension | White-Coat Hypertension | Masked Hypertension | Sustained Hypertension |
|---|---|---|---|---|
| No. of characteristics (%) | 4988 | 881 | 800 | 1568 |
| Women | 2767 (55.5) | 404 (45.9)* | 293 (36.6)* | 522 (33.3) |
| Current smoking | 1544 (31.0) | 168 (19.2)* | 298 (37.3)* | 428 (27.4)* |
| Drinking alcohol | 2304 (47.5) | 381 (46.6) | 458 (60.3)* | 923 (64.6)† |
| Diabetes mellitus | 182 (3.6) | 67 (7.6)* | 57 (7.1) | 149 (9.5) |
| Previous cardiovascular diseases | 237 (4.8) | 126 (14.3)* | 54 (6.8)* | 233 (14.9)* |
| Ethnicity (white) | 4171 (83.6) | 662 (75.3)* | 641 (80.1)† | 1294 (82.6) |
| Mean characteristic (SD) | ||||
| Age, y | 45.7 (15.1) | 59.3 (13.8)* | 52.8 (14.0)* | 60.8 (12.4)* |
| Body mass index, kg/m2 | 24.3 (3.8) | 26.0 (4.1)* | 25.7 (4.0) | 26.9 (4.4)* |
| Total serum cholesterol, mmol/L | 5.44 (1.15) | 5.80 (1.26)* | 5.68 (1.18)† | 5.86 (1.16)* |
| Blood pressure | ||||
| Conventional systolic, mm Hg | 117.0 (11.3) | 148.4 (15.0)* | 126.2 (8.9)* | 156.7 (20.9)* |
| Conventional diastolic, mm Hg | 73.2 (7.9) | 85.6 (9.4)* | 78.7 (7.3)* | 91.7 (10.4)* |
| 24-h systolic, mm Hg | 114.7 (7.7) | 121.4 (6.1)* | 132.7 (7.7)* | 140.8 (12.0)* |
| 24-h diastolic, mm Hg | 69.3 (5.3) | 71.7 (5.2)* | 79.9 (5.8)* | 82.6 (8.3)* |
| Daytime systolic, mm Hg | 121.0 (9.1) | 128.0 (8.3)* | 139.1 (10.0)* | 147.2 (12.9)* |
| Daytime diastolic, mm Hg | 74.5 (6.3) | 76.8 (7.0)* | 84.9 (7.0)* | 87.5 (9.4)* |
| Nighttime systolic, mm Hg | 104.1 (8.8) | 109.7 (8.8)* | 120.9 (10.7)* | 128.8 (15.3)* |
| Nighttime diastolic, mm Hg | 60.2 (6.3) | 62.8 (6.3)* | 70.5 (7.4)* | 73.4 (9.5)* |
Values are number of participants (%) or arithmetic mean (SD). Thresholds for hypertension were ≥140/≥90 and ≥130/≥80 mm Hg on conventional and 24-hour ambulatory measurement, respectively. Normotension and sustained hypertension were consistently normal or elevated blood pressure on both conventional and 24-hour ambulatory measurement. White-coat hypertension had a raised conventional blood pressure and normal 24-hour blood pressure. Masked hypertension had an elevated 24-hour ambulatory blood pressure with normal conventional blood pressure. If for a type of measurement, systolic and diastolic blood pressures were in a different category, participants were classified as hypertensive. Smoking, drinking, diabetes mellitus, history of cardiovascular disease, body mass index, and cholesterol were unavailable in 22, 384, 3, 1, 8, and 611 participants, respectively.
Significance of the difference with the left adjacent column:
P<0.001 and
P<0.05.
Prevalence of White-Coat, Masked, and Sustained Hypertension
Based on the cross-classification between conventional and 24-hour ambulatory blood pressure (Table 1), 4988 participants (60.6%) were normotensive and 881 (10.7%), 800 (9.7%), and 1568 (19.0%) had white-coat, masked, and sustained hypertension, respectively. Using different time intervals during which ambulatory blood pressure thresholds were applied substantially affected the estimates of prevalence (Table 2). They ranged from 50.7% to 60.6% for normotension, from 6.3% to 12.5% for white-coat hypertension, from 9.7% to 19.6% for masked hypertension, and from 17.3% to 23.5% for sustained hypertension. The prevalence of normotension and white-coat hypertension was lowest and the prevalence of masked and sustained hypertension was highest based on thresholds set simultaneously to the 24-hour and the daytime and nighttime blood pressures (Table 2). Table 3 summarizes reclassification rates of participants with white-coat and masked hypertension from the commonly used definitions based on daytime, nighttime, or 24-hour ambulatory blood pressure to one of the other definitions.
Table 2.
Prevalence of Blood Pressure Categories According to Intervals of Ambulatory Monitoring
| Intervals Used to Categorize the Ambulatory Blood Pressure | Normotension | White-coat Hypertension | Masked Hypertension | Sustained Hypertension |
|---|---|---|---|---|
| Daytime only | 4683 (56.9) | 747 (9.1) | 1105 (13.4) | 1702 (20.7) |
| Nighttime only | 4806 (58.3) | 1027 (12.5) | 982 (11.9) | 1422 (17.3) |
| 24 h only | 4988 (60.6) | 881 (10.7) | 800 (9.7) | 1568 (19.0) |
| 24 h plus daytime | 4551 (55.3) | 642 (7.8) | 1237 (15.0) | 1807 (21.9) |
| 24 h plus nighttime | 4572 (55.5) | 724 (8.8) | 1216 (14.8) | 1725 (20.9) |
| 24 h plus daytime and nighttime | 4176 (50.7) | 515 (6.3) | 1612 (19.6) | 1934 (23.5) |
Values are number of participants (%). Normotension and sustained hypertension had consistently normal or elevated blood pressure levels on both conventional and ambulatory measurement. White-coat hypertension was defined as conventional hypertension in the presence of a normal ambulatory blood pressure. Masked hypertension was defined as ambulatory hypertension in participants with a normal conventional blood pressure. When systolic or diastolic blood pressure was in a different category (normotensive vs hypertensive), participant were classified as hypertensive. For ambulatory time intervals including nested periods (24 hours±daytime±nighttime), the interval with the highest blood pressure classification (normotensive vs hypertensive) determined the ambulatory blood pressure status.
Table 3.
Reclassification of White-Coat and Masked Hypertensive Participants
| Time Intervals Used for Reclassification | White-Coat Hypertension
|
Masked Hypertension
|
||||
|---|---|---|---|---|---|---|
| Original Intervals | Maintaining White-Coat Hypertension | Reclassified to Sustained Hypertension | Original Intervals | Maintaining Masked Hypertension | Reclassified to Normotension | |
| From daytime to 24 h | 747 | 642 (85.9) | 105 (14.1) | 1105 | 668 (60.5) | 437 (39.5) |
| From nighttime to 24 h | 1027 | 724 (70.5) | 303 (29.5) | 982 | 566 (57.6) | 416 (42.4) |
| From daytime to 24 h plus daytime and nighttime | 747 | 515 (68.9) | 232 (31.1) | 1105 | 1105 (100) | 0 |
| From nighttime to 24 h plus daytime and nighttime | 1027 | 515 (50.1) | 512 (49.9) | 982 | 982 (100) | 0 |
| From 24 h to 24 h plus daytime and nighttime | 881 | 515 (58.5) | 366 (41.5) | 800 | 800 (100) | 0 |
Values are number of participants (reclassification rates, %) of white-coat and masked hypertensive participants from the commonly used definitions based on daytime, nighttime, or 24-hour ambulatory blood pressure to one of the other definitions. The McNemar–Bowker test for symmetry along the diagonal of the matrix was significant for all rows (P<0.0001).
Incidence of Events
In the overall study population, median follow-up was 11.1 years (5th–95th percentile interval, 2.5–18.2 years). During 91 046 person-years of follow-up, 906 participants died (10.0 per 1000 person-years) and 729 participants experienced a fatal or nonfatal cardiovascular event (8.2 per 1000 person-years). Considering cause-specific first cardiovascular events, the incidence of cardiac events and stroke amounted to 473 and 242, respectively. More details on the incidence of end points are available in the Results in the online-only Data Supplement.
Risk of a Cardiovascular Event Associated With White-Coat Hypertension
Table 4 provides risk estimates by varying time intervals during which the ambulatory blood pressure thresholds were applied. Although accounting for cohort, sex, age, body mass index, smoking, drinking, total serum cholesterol, history of cardiovascular disease, and diabetes mellitus (Table 4), white-coat hypertension based on daytime blood pressure compared with daytime normotension as well as that based on nighttime blood pressure compared with nighttime normotension carried significantly elevated risks of 30% (P≤0.048). Defining white-coat hypertension based on the 24-hour blood pressure with or without accounting for the daytime or nighttime blood pressure or both weakened the risk compared with normotension during the same periods to a nonsignificant level ranging from 27% (P=0.097) for 24-hour plus daytime blood pressure to 9% (P=0.55) for 24-hour plus nighttime blood pressure. Irrespective of the ambulatory blood pressure time intervals used to cross-classify participants, the linear trend in the hazard ratios from normotension over white-coat and masked hypertension to sustained hypertension was consistently significant (P<0.0001).
Table 4.
Risk of Cardiovascular End Point by Intervals of Ambulatory Monitoring
| Blood Pressure Cross-Classification | E/R, n | Rate (SE) | Hazard Ratio (95% CI) | P Value |
|---|---|---|---|---|
| Daytime | ||||
| Normotension | 203/4683 | 6.0 (0.4) | 1.00 | … |
| White-coat hypertension | 92/747 | 9.7 (1.2) | 1.30 (1.00–1.69) | 0.048 |
| Masked hypertension | 105/1105 | 8.8 (0.9) | 1.61 (1.27–2.05) | 0.0001 |
| Sustained hypertension | 329/1702 | 13.7 (0.8) | 2.14 (1.76–2.60) | <0.0001 |
| Nighttime | ||||
| Normotension | 209/4806 | 5.9 (0.4) | 1.00 | … |
| White-coat hypertension | 121/1027 | 8.7 (0.9) | 1.30 (1.03–1.64) | 0.031 |
| Masked hypertension | 99/982 | 9.6 (1.0) | 1.71 (1.34–2.18) | <0.0001 |
| Sustained hypertension | 300/1422 | 15.4 (0.9) | 2.40 (1.97–2.93) | <0.0001 |
| 24 h | ||||
| Normotension | 219/4988 | 5.9 (0.4) | 1.00 | … |
| White-coat hypertension | 98/881 | 8.3 (1.0) | 1.20 (0.93–1.54) | 0.16 |
| Masked hypertension | 89/800 | 10.1 (1.1) | 1.81 (1.41–2.32) | <0.0001 |
| Sustained hypertension | 323/1568 | 15.0 (0.9) | 2.31 (1.91–2.80) | <0.0001 |
| 24 h plus daytime | ||||
| Normotension | 187/4551 | 5.7 (0.4) | 1.00 | … |
| White-coat hypertension | 74/642 | 9.0 (1.2) | 1.27 (0.96–1.69) | 0.097 |
| Masked hypertension | 121/1237 | 9.1 (0.8) | 1.72 (1.36–2.17) | <0.0001 |
| Sustained hypertension | 347/1807 | 13.7 (0.8) | 2.23 (1.83–2.72) | <0.0001 |
| 24 h plus nighttime | ||||
| Normotension | 189/4572 | 5.7 (0.4) | 1.00 | … |
| White-coat hypertension | 70/724 | 7.3 (1.1) | 1.09 (0.82–1.45) | 0.55 |
| Masked hypertension | 119/1216 | 9.2 (0.9) | 1.67 (1.32–2.11) | <0.0001 |
| Sustained hypertension | 351/1725 | 14.8 (0.8) | 2.35 (1.93–2.87) | <0.0001 |
| 24 h plus daytime and nighttime | ||||
| Normotension | 159/4176 | 5.5 (0.5) | 1.00 | … |
| White-coat hypertension | 50/515 | 7.7 (1.3) | 1.13 (0.81–1.57) | 0.47 |
| Masked hypertension | 149/1612 | 8.8 (0.7) | 1.70 (1.35–2.14) | <0.0001 |
| Sustained hypertension | 371/1934 | 13.8 (0.8) | 2.34 (1.90–2.88) | <0.0001 |
Definition of the blood pressure cross-classifications is given in the Methods and in the footnote to Table 2. Rates (SE) of events per 1000 person-year were standardized by the direct method for sex and age. Hazard ratios (95% CI) express the risk compared with normotension and were adjusted for sex, age, body mass index, smoking, drinking, total cholesterol, diabetes mellitus, history of cardiovascular disease, and cohort. CI indicates confidence interval; and E/R, events/participants at risk.
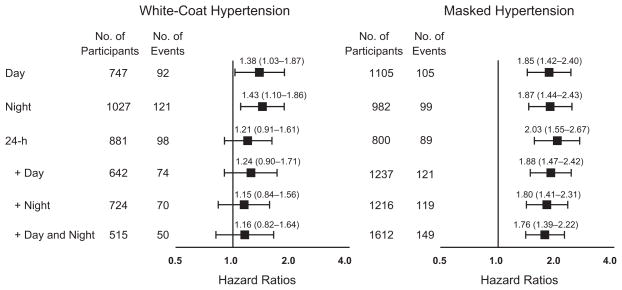
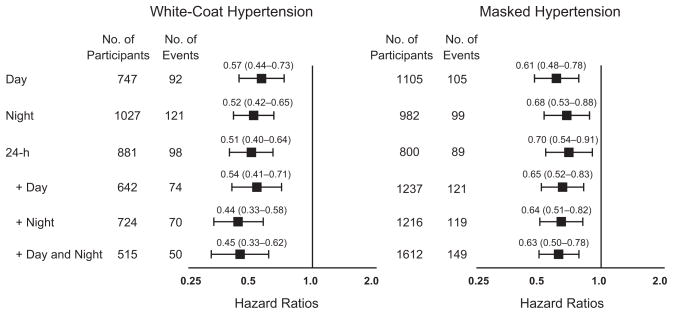
In Table 4, the normotensive reference group differed according to the time intervals considered. In a further step of the analysis, we applied the most stringent definition of normotension as unique reference (Figure 1). This definition required that the conventional blood pressure was normal and that the 24-hour, daytime, and nighttime ambulatory blood pressures were within normal limits. The hazard ratios for white-coat hypertension versus normotension weakened from 1.38 for daytime only to 1.16 for 24 hours plus daytime and nighttime. Conversely, applying the most stringent definition of hypertension (Figure 2) showed that the risk of white-coat hypertension was consistently lower than that of sustained hypertension (P<0.0001) with hazard ratios decreasing from 0.57 for daytime to 0.45 for 24 hours plus daytime and nighttime.
Figure 1.
Risk of a cardiovascular end point associated with white-coat and masked hypertension vs stringently defined normotension defined by various intervals of ambulatory monitoring. Definition of the blood pressure cross-classifications is given in the Methods and in the footnote to Table 2. In this analysis, we applied the most stringent definition of normotension as unique reference in which the conventional blood pressure was normal and that the ambulatory blood pressure was within normal limits for 24 hours plus daytime and nighttime. Hazard ratios express the risk compared with normotension and were adjusted for sex, age, body mass index, smoking, drinking, total cholesterol, diabetes mellitus, history of cardiovascular disease, and cohort. Horizontal bars denote the 95% confidence interval of the hazard ratios.
Figure 2.
Risk of a cardiovascular end point associated with white-coat and masked hypertension vs stringently defined hypertension defined by various intervals of ambulatory monitoring. Definition of the blood pressure cross-classifications is given in the Methods and in the footnote to Table 2. In this analysis, we applied the most stringent definition of hypertension as unique reference in which the conventional blood pressure was over the threshold and that the ambulatory blood pressure was over the thresholds for 24 hours plus daytime and nighttime. Hazard ratios express the risk compared with hypertension and were adjusted for sex, age, body mass index, smoking, drinking, total cholesterol, diabetes mellitus, history of cardiovascular disease, and cohort. Horizontal bars denote the 95% confidence interval of the hazard ratios.
Risk of a Cardiovascular Event Associated With Masked Hypertension
In multivariable-adjusted analyses (Table 4), the risk associated with masked hypertension compared with normotension was always highly significant (P≤0.0001) with estimates of excess risk ranging from 61% to 81%. Applying the most stringent definition of normotension (Figure 1) confirmed that the hazard ratios comparing masked hypertension with normotension were all significant (P<0.0001), between 1.76 and 2.03. Conversely, applying the most stringent definition of hypertension (Figure 2) showed that the risk of masked hypertension was lower than that of sustained hypertension (P≤0.0074). The hazard ratios were essentially similar, from 0.61 to 0.70.
Risk of Other End Points Associated With White-Coat and Masked Hypertension
Results for total and cardiovascular mortality, fatal and non-fatal cardiac events, and stroke—equivalent to those given for the composite cardiovascular end point in Table 4—are provided in Table S2. In analyses with normotension as reference and adjusted as before, white-coat hypertension did not confer a formally significantly elevated risk (P≥0.051) except for the risk of stroke based on a nighttime-derived definition of white-coat hypertension (P=0.0065).
Masked hypertension was a significant predictor (P≤0.023) of all end points with the exception of all-cause mortality if the diagnosis was derived from the daytime blood pressure, 24-hour blood pressure, or 24-hour plus daytime blood pressure (P≥0.059).
Discussion
Current guidelines for ambulatory blood pressure monitoring or for the management of hypertension do not provide outcome-driven evidence for defining the time windows during which the ambulatory blood pressure should be measured to define white-coat and masked hypertension in an accurate manner. Depending on the definition, frequencies of white-coat and masked hypertension ranged from 6.3% to 12.5% and from 9.7% to 19.6%, respectively. Furthermore, the risk associated with white-coat hypertension decreased when a more stringent definition of ambulatory normotension was used. Finally, ambulatory hypertension during any time interval predicted an ≈2-fold higher cardiovascular risk in patients with masked hypertension.
During the past decade, European guidelines5,21,22 have proposed changing or twin thresholds for ambulatory hypertension without providing any solid justification in terms of outcome data. The 2003 guideline only recommended a threshold for the 24-hour ambulatory blood pressure of ≥125/≥80 mm Hg.21 The 2007 guideline proposed as thresholds for the 24-hour, daytime, and nighttime blood pressure levels of ≥125 to 130/≥80, ≥130 to 135/≥85, and ≥120/≥70 mm Hg, respectively.22 The 2013 guideline5 removed the ambiguity in the thresholds for the 24-hour and daytime blood pressure, recommending ≥130/≥80 and ≥135/≥85 mm Hg, respectively, whereas keeping the nighttime threshold at ≥120/≥70 mm Hg. In a 2007 analysis of the IDACO database,6 we determined thresholds for the ambulatory blood pressure, which yielded 10-year cardiovascular risks similar to those associated with optimal (120/80 mm Hg), normal (130/85 mm Hg), and high (140/90 mm Hg) blood pressure on conventional measurement. After rounding, approximate thresholds for an optimal ambulatory blood pressure amounted to 115/75 mm Hg for 24 hours, 120/80 mm Hg for daytime, and 100/65 mm Hg for nighttime. Rounded thresholds for a normal ambulatory blood pressure were 125/75, 130/85, and 110/70 mm Hg, respectively, and those for ambulatory hypertension were 130/80, 140/85, and 120/70 mm Hg.
Whether white-coat hypertension substantially elevates cardiovascular risk continues to divide expert opinion. In a meta-analysis of summary statistics from 4 prospective cohorts, the pooled hazard ratio for stroke associated with white-coat hypertension defined by a daytime blood pressure threshold of 130/80 mm Hg became comparable with that in ambulatory hypertension group by the ninth year of follow-up.23 However, the median follow-up of the 4 cohorts was only 5.4 years, and the pooled hazard ratio was not adjusted.23 The risk in white-coat hypertension was not significantly different from that in normotension when multivariable-adjusted models were applied.12,24,25 In the meta-analysis by Pierdomenico and Cuccurullo,25 5 of the 7 eligible studies applied a daytime blood pressure threshold of 135/85 mm Hg, whereas 2 other studies either applied a daytime threshold ranging from 131 to 136 mm Hg26 or a 24-hour blood pressure cut off of 130/80 mm Hg.27 In a previous IDACO publication,28 we included both treated and untreated participants. In this analysis, we classified treated people according to the achieved ambulatory blood pressure.28 Compared with normotension, the risk of all cardiovascular and cause-specific cardiovascular complications was not increased, irrespective of whether we used 130/80 or 135/85 mm Hg as cutoff threshold for the daytime blood pressure (0.63≥P≥0.09).28 Subsequently, Franklin et al,24 using the IDACO database, reported that in treated subjects with isolated systolic hypertension, the cardiovascular risk was similar in elevated conventional and normal daytime systolic blood pressure as compared with those with normal conventional and normal daytime blood pressure (P=0.57). However, both treated patients with isolated systolic hypertension and white-coat hypertension and treated participants with normal blood pressure had an ≈2-fold increased cardiovascular risk when compared with untreated normotensive people.24 Summarizing the evidence of previous studies,26 it is clear that the long-term white-coat hypertension carries an increased risk and that the prognostic meaning of white-coat hypertension differs among treated and untreated subjects. What our current study adds to the knowledge on white-coat hypertension26 is that to identify the low-risk subjects among untreated people with white-coat hypertension, full 24-hour ambulatory recordings are required and the most stringent definition of ambulatory normotension, with thresholds applied to the whole ambulatory recording including daytime and nighttime, has to be applied. Although in our study the risk of white-coat hypertension, as defined using the most stringent definition, was not significantly different from the risk in sustained normotension, we cannot definitely exclude that this definition of white-coat hypertension is not associated with increased risk. Further analyses in large population cohorts applying the same stringent definition of white-coat hypertension are needed to confirm our findings.
In contrast to white-coat hypertension,12,26,27,29–31 the current literature by and large supports the view that masked hypertension carries a risk only slightly lower than or equal to sustained hypertension,28,32 irrespective of treatment status. The Finn-Home Study Investigators33 are in agreement with IDACO findings,28 demonstrating that high-normal systolic and diastolic conventional blood pressure, older age, greater body mass index, current smoking, and diabetes mellitus are independent determinants of masked hypertension. Similarly, Franklin et al32 reported that among people not being treated for hypertension, the prevalence of masked hypertension, using a daytime ambulatory threshold of 135/85 mm Hg, was higher in diabetic than in nondiabetic participants (18.1% versus 13.8%). Moreover, we previously reported that masked hypertension, as diagnosed by ambulatory34 or home35 blood pressure monitoring, leads to an ≈2-fold increase in the risk of cardiovascular events or stroke in people with an optimal or normal conventional blood pressure. What our current study adds to the knowledge on blood pressure is that ambulatory hypertension during any part of the day reliably identifies this high-risk condition.
Our current study must be interpreted within the context of some potential limitations. First, conventional blood pressure was the average of only 2 readings obtained at a single examination, which might not have been sufficient to remove the white-coat effect. Second, we have no information on anti-hypertensive drug treatment after the baseline visit at enrolment. Third, the current IDACO participants were recruited from 12 geographically areas with different life styles and healthcare delivery systems. Study protocols and definition of events were cohort specific. However, we accounted for these differences in methodology among cohorts by including center as stratification variable in the Cox proportional hazard models. Finally, ambulatory blood pressure monitoring was not standardized in terms of device type and intervals between readings. However, using a single SAS macro ensured that the time-weighted mean values during all periods of the day were calculated identically across cohorts.
Our current study has important clinical implications and may inform future guidelines. From a clinical point of view, our findings highlight that to identify individuals at low risk of cardiovascular complications among untreated participants with white-coat hypertension, full 24-hour ambulatory recordings are necessary with thresholds set during the whole recording period including daytime and nighttime. Conversely, to diagnose masked hypertension, ambulatory hypertension during any period of the day might be sufficient with a slight difference in the predictive accuracy. Furthermore, among 8237 untreated IDACO participants, 747 (9.1%) and 881 (10.7%) had white-coat hypertension based on the 24-hour or daytime blood pressure according to the current guidelines,2,5 but only 515 (6.3%) had the low-risk variant as defined in our current report.
Perspectives
To identify patients with white-coat hypertension with a cardiovascular risk similar to that of normotensive people, one needs full 24-hour ambulatory recordings with thresholds set to all recording intervals, including daytime and nighttime. The definition in current guidelines of truly low-risk white-coat hypertension is therefore not precise enough. To diagnose masked hypertension, ambulatory hypertension during any period of the day is sufficient with a slight difference in predictive accuracy. Current guidelines therefore accurately cover the definition of masked hypertension. The difference between white-coat and masked hypertension in terms of time intervals during which blood pressure must be monitored is unexpected and novel. Our findings might inform expert committees writing guidelines so that arbitrary definitions are replaced by outcome-driven standards.
Supplementary Material
Figure S1. Flow chart of the study participants. BP denotes blood pressure.
Figure S2. Cross-classification of office and ambulatory blood pressure categories.
Office hypertension was a blood pressure at least 140 mm Hg systolic and/or 90 mm Hg diastolic. Ambulatory hypertension was a 24-h level of 130 mm Hg systolic and/or 80 mm Hg diastolic or more; for the daytime blood pressure these thresholds were 135 mm Hg and 85 mm Hg and for the nighttime blood pressure 120 mm Hg and 70 mm Hg, respectively. If for a type of blood pressure measurement, systolic and diastolic blood pressure were in different categories, participants were classified as hypertensive.
Table S1. Thresholds and Intervals Used for Cross-Classification of Participants
Table S2. Risk of Fatal Endpoints and Cardiac and Cerebrovascular Events by Intervals of Ambulatory Monitoring (Starts)
Table S3. Risk of Cardiovascular Endpoint by Intervals of Ambulatory Monitoring Applying the Markov Single-Chain Monte Carlo Imputation Method.
Novelty and Significance.
What Is New?
In 8237 untreated participants, we generated outcome-driven proposals about the time intervals during which the ambulatory blood pressure should be measured to diagnose truly low-risk white-coat hypertension and masked hypertension. White-coat hypertension was hypertension on conventional measurement with ambulatory normotension, the opposite condition being masked hypertension. Intervals used for classification of participants were daytime, nighttime, and 24 hours, first considered separately, and next combined as 24 hours plus daytime or plus nighttime or plus both.
What Is Relevant?
To identify patients with white-coat hypertension who have a cardiovascular risk similar to that of normotensive people, one needs full 24-hour ambulatory recordings with thresholds set to all recording intervals, including daytime and nighttime. To diagnose masked hypertension, ambulatory hypertension during any period of the day is sufficient with only a slight increase in predictive accuracy, if the ambulatory blood pressure is consistently elevated for most of the day.
Summary
The difference between white-coat and masked hypertension in terms of time intervals during which blood pressure must be monitored was unexpected. These findings might inform guidelines so that outcome-driven standards replace arbitrary definitions and so that the management of white-coat hypertension is differentiated, based on the time interval of blood pressure monitoring used for its diagnosis.
Acknowledgments
We gratefully acknowledge the expert clerical assistance of Sandra Covens and Annick De Soete (Studies Coordinating Centre, Leuven, Belgium).
Sources of Funding
The European Union (grants IC15-CT98-0329-EPOGH, LSHM-CT-2006-037093 InGenious HyperCare, HEALTH-F4-2007-201550 HyperGenes, HEALTH-F7-2011-278249 EU-MASCARA, HEALTH- F7-305507 HOMAGE and the European Research Council Advanced Research Grant 294713 EPLORE) and the Fonds voor Wetenschappelijk Onderzoek Vlaanderen, Ministry of the Flemish Community, Brussels, Belgium (G.0734.09, G.0881.13, and G.0880.13 N) supported the Studies Coordinating Centre (Leuven, Belgium). The European Union (grants LSHM-CT-2006-037093 and HEALTH-F4-2007-201550) also supported the research groups in Shanghai, Kraków, Padova, and Novosibirsk. The Danish Heart Foundation (grant 01-2-9-9A-22914) and the Lundbeck Fonden (grant R32-A2740) supported the studies in Copenhagen. The Ohasama study received support via Grant-in-Aid for Scientific Research (23249036, 23390171, 23790242, 24591060, 24390084, 24591060, 24790654, 25461205, 25461083, and 25860156) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan; Health Labour Sciences Research Grant (H23-Junkankitou [Seishuu]-Ippan-005) from the Ministry of Health, Labour, and Welfare, Japan; Japan Arteriosclerosis Prevention Fund; and a grant from the Daiwa Securities Health Foundation. The National Natural Science Foundation of China (grants 30871360, 30871081, 81170245, and 81270373), Beijing, China, and the Shanghai Commissions of Science and Technology (grant 07JC14047 and the Rising Star program 06QA14043 and 11QH1402000) and Education (grant 07ZZ32 and the Dawn project 08SG20) supported the JingNing study in China. The Comisión Sectorial de Investigación Científica de la Universidad de la República (Grant I+D GEFA-HT-UY) and the Agencia Nacional de Innovación e Investigación supported research in Uruguay. The research in Czech Republic was supported by the Charles University Research Fund (project number P36). Grant 1-R01AG036469 A1 from the National Institute of Aging and Fogarty International center, grant G-97000726 from FONACIT and grant LOCTI/008 to 2008 from FundaConCiencia supported the Maracaibo Aging Study.
Footnotes
Disclosures
None.
This paper was sent to David Calhoun, Guest editor, for review by expert referees, editorial decision, and final disposition.
References
- 1.National Institute for Health and Clinical Excellence (NICE) The Clinical Management of Primary Hypertension in Adults. UK: National Clinical Guideline Centre; 2011. [Google Scholar]
- 2.O’Brien E, Parati G, Stergiou G, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–1767. doi: 10.1097/HJH.0b013e328363e964. [DOI] [PubMed] [Google Scholar]
- 3.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 4.Ogihara T, Kikuchi K, Matsuoka H, et al. Japanese Society of Hypertension Committee. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009) Hypertens Res. 2009;32:3–107. [PubMed] [Google Scholar]
- 5.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 6.Kikuya M, Hansen TW, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Staessen JA International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes Investigators. Diagnostic thresholds for ambulatory blood pressure monitoring based on 10-year cardiovascular risk. Circulation. 2007;115:2145–2152. doi: 10.1161/CIRCULATIONAHA.106.662254. [DOI] [PubMed] [Google Scholar]
- 7.Ohkubo T, Imai Y, Tsuji I, Nagai K, Ito S, Satoh H, Hisamichi S. Reference values for 24-hour ambulatory blood pressure monitoring based on a prognostic criterion: the Ohasama Study. Hypertension. 1998;32:255–259. doi: 10.1161/01.hyp.32.2.255. [DOI] [PubMed] [Google Scholar]
- 8.Thijs L, Hansen TW, Kikuya M, et al. IDACO Investigators. The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO): protocol and research perspectives. Blood Press Monit. 2007;12:255–262. doi: 10.1097/mbp.0b013e3280f813bc. [DOI] [PubMed] [Google Scholar]
- 9.Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure and mortality: a population-based study. Hypertension. 2005;45:499–504. doi: 10.1161/01.HYP.0000160402.39597.3b. [DOI] [PubMed] [Google Scholar]
- 10.Staessen JA, Bieniaszewski L, O’Brien ET, Imai Y, Fagard R. An epidemiological approach to ambulatory blood pressure monitoring: the Belgian Population Study. Blood Press Monit. 1996;1:13–26. [PubMed] [Google Scholar]
- 11.Ingelsson E, Björklund-Bodegård K, Lind L, Arnlöv J, Sundström J. Diurnal blood pressure pattern and risk of congestive heart failure. JAMA. 2006;295:2859–2866. doi: 10.1001/jama.295.24.2859. [DOI] [PubMed] [Google Scholar]
- 12.Ohkubo T, Kikuya M, Metoki H, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005;46:508–515. doi: 10.1016/j.jacc.2005.03.070. [DOI] [PubMed] [Google Scholar]
- 13.Schettini C, Bianchi M, Nieto F, Sandoya E, Senra H. Ambulatory blood pressure: normality and comparison with other measurements. Hypertension Working Group. Hypertension. 1999;34(4 Pt 2):818–825. doi: 10.1161/01.hyp.34.4.818. [DOI] [PubMed] [Google Scholar]
- 14.Li Y, Wang JG, Gao P, Guo H, Nawrot T, Wang G, Qian Y, Staessen JA, Zhu D. Are published characteristics of the ambulatory blood pressure generalizable to rural Chinese? The JingNing population study. Blood Press Monit. 2005;10:125–134. doi: 10.1097/00126097-200506000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Kuznetsova T, Malyutina S, Pello E, Thijs L, Nikitin Y, Staessen JA. Ambulatory blood pressure of adults in Novosibirsk, Russia: interim report on a population study. Blood Press Monit. 2000;5:291–296. doi: 10.1097/00126097-200010000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Kuznetsova T, Staessen JA, Kawecka-Jaszcz K, Babeanu S, Casiglia E, Filipovsky J, Nachev C, Nikitin Y, Peleskã J, O’Brien E. Quality control of the blood pressure phenotype in the European Project on Genes in Hypertension. Blood Press Monit. 2002;7:215–224. doi: 10.1097/00126097-200208000-00003. [DOI] [PubMed] [Google Scholar]
- 17.O’Brien E, Murphy J, Tyndall A, Atkins N, Mee F, McCarthy G, Staessen J, Cox J, O’Malley K. Twenty-four-hour ambulatory blood pressure in men and women aged 17 to 80 years: the Allied Irish Bank Study. J Hypertens. 1991;9:355–360. doi: 10.1097/00004872-199104000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Maestre GE, Pino-Ramírez G, Molero AE, Silva ER, Zambrano R, Falque L, Gamero MP, Sulbarán TA. The Maracaibo Aging Study: population and methodological issues. Neuroepidemiology. 2002;21:194–201. doi: 10.1159/000059524. [DOI] [PubMed] [Google Scholar]
- 19.Boggia J, Thijs L, Hansen TW, et al. International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes Investigators. Ambulatory blood pressure monitoring in 9357 subjects from 11 populations highlights missed opportunities for cardiovascular prevention in women. Hypertension. 2011;57:397–405. doi: 10.1161/HYPERTENSIONAHA.110.156828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Y, Thijs L, Boggia J, et al. International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes (IDACO) Investigators. Blood pressure load does not add to ambulatory blood pressure level for cardiovascular risk stratification. Hypertension. 2014;63:925–933. doi: 10.1161/HYPERTENSIONAHA.113.02780. [DOI] [PubMed] [Google Scholar]
- 21.European Society of Hypertension/European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension/European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–1053. doi: 10.1097/00004872-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2007;28:1462–1536. doi: 10.1093/eurheartj/ehm236. [DOI] [PubMed] [Google Scholar]
- 23.Verdecchia P, Reboldi GP, Angeli F, Schillaci G, Schwartz JE, Pickering TG, Imai Y, Ohkubo T, Kario K. Short- and long-term incidence of stroke in white-coat hypertension. Hypertension. 2005;45:203–208. doi: 10.1161/01.HYP.0000151623.49780.89. [DOI] [PubMed] [Google Scholar]
- 24.Franklin SS, Thijs L, Hansen TW, et al. International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators. Significance of white-coat hypertension in older persons with isolated systolic hypertension: a meta-analysis using the International Database on Ambulatory Blood Pressure Monitoring in Relation to Cardiovascular Outcomes population. Hypertension. 2012;59:564–571. doi: 10.1161/HYPERTENSIONAHA.111.180653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens. 2011;24:52–58. doi: 10.1038/ajh.2010.203. [DOI] [PubMed] [Google Scholar]
- 26.Verdecchia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistelli M, Guerrieri M, Gatteschi C, Zampi I, Santucci A, Santucci C, Reboldi G. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793–801. doi: 10.1161/01.hyp.24.6.793. [DOI] [PubMed] [Google Scholar]
- 27.Kario K, Shimada K, Schwartz JE, Matsuo T, Hoshide S, Pickering TG. Silent and clinically overt stroke in older Japanese subjects with white-coat and sustained hypertension. J Am Coll Cardiol. 2001;38:238–245. doi: 10.1016/s0735-1097(01)01325-0. [DOI] [PubMed] [Google Scholar]
- 28.Hansen TW, Kikuya M, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Jeppesen J, Ibsen H, Imai Y, Staessen JA IDACO Investigators. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens. 2007;25:1554–1564. doi: 10.1097/HJH.0b013e3281c49da5. [DOI] [PubMed] [Google Scholar]
- 29.Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens. 2005;19:801–807. doi: 10.1038/sj.jhh.1001903. [DOI] [PubMed] [Google Scholar]
- 30.Pierdomenico SD, Pannarale G, Rabbia F, Lapenna D, Licitra R, Zito M, Campanella M, Gaudio C, Veglio F, Cuccurullo F. Prognostic relevance of masked hypertension in subjects with prehypertension. Am J Hypertens. 2008;21:879–883. doi: 10.1038/ajh.2008.196. [DOI] [PubMed] [Google Scholar]
- 31.Björklund K, Lind L, Zethelius B, Andrén B, Lithell H. Isolated ambulatory hypertension predicts cardiovascular morbidity in elderly men. Circulation. 2003;107:1297–1302. doi: 10.1161/01.cir.0000054622.45012.12. [DOI] [PubMed] [Google Scholar]
- 32.Franklin SS, Thijs L, Li Y, et al. International Database on Ambulatory blood pressure in Relation to Cardiovascular Outcomes Investigators. Masked hypertension in diabetes mellitus: treatment implications for clinical practice. Hypertension. 2013;61:964–971. doi: 10.1161/HYPERTENSIONAHA.111.00289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hänninen MR, Niiranen TJ, Puukka PJ, Johansson J, Jula AM. Prognostic significance of masked and white-coat hypertension in the general population: the Finn-Home Study. J Hypertens. 2012;30:705–712. doi: 10.1097/HJH.0b013e328350a69b. [DOI] [PubMed] [Google Scholar]
- 34.Brguljan-Hitij J, Thijs L, Li Y, et al. International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcome Investigators. Risk stratification by ambulatory blood pressure monitoring across JNC classes of conventional blood pressure. Am J Hypertens. 2014;27:956–965. doi: 10.1093/ajh/hpu002. [DOI] [PubMed] [Google Scholar]
- 35.Asayama K, Thijs L, Brguljan-Hitij J, et al. International Database of Home Blood Pressure in Relation to Cardiovascular Outcome (IDHOCO) Investigators. Risk stratification by self-measured home blood pressure across categories of conventional blood pressure: a participant-level meta-analysis. PLoS Med. 2014;11:e1001591. doi: 10.1371/journal.pmed.1001591. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Flow chart of the study participants. BP denotes blood pressure.
Figure S2. Cross-classification of office and ambulatory blood pressure categories.
Office hypertension was a blood pressure at least 140 mm Hg systolic and/or 90 mm Hg diastolic. Ambulatory hypertension was a 24-h level of 130 mm Hg systolic and/or 80 mm Hg diastolic or more; for the daytime blood pressure these thresholds were 135 mm Hg and 85 mm Hg and for the nighttime blood pressure 120 mm Hg and 70 mm Hg, respectively. If for a type of blood pressure measurement, systolic and diastolic blood pressure were in different categories, participants were classified as hypertensive.
Table S1. Thresholds and Intervals Used for Cross-Classification of Participants
Table S2. Risk of Fatal Endpoints and Cardiac and Cerebrovascular Events by Intervals of Ambulatory Monitoring (Starts)
Table S3. Risk of Cardiovascular Endpoint by Intervals of Ambulatory Monitoring Applying the Markov Single-Chain Monte Carlo Imputation Method.