Abstract
Aims/Introduction
We aimed to investigate the long-term trajectory of general adiposity assessed by the body mass index (BMI) before the onset of type 2 diabetes in Japanese individuals.
Materials and Methods
We retrospectively examined data on 1,553 Japanese men without diabetes. Mean BMI and incident cases of diabetes (diabetes indicated by fasting glucose concentrations ≥7.0 mmol/L, a self-reported history of clinician-diagnosed diabetes, or glycated hemoglobin ≥6.5% (≥48 mmol/mol) were assessed on an annual basis over a 10-year period after the baseline examination.
Results
Mean (standard deviation) BMI at the time of diagnosis was 24.4 kg/m2 (3.1 kg/m2) among cases of diabetes (n = 191). An increasingly high BMI was associated with the early stage of the disease development, such as an 8- to 10-year prediagnosis period; individuals who developed diabetes experienced a prolonged and stable elevated BMI of ≥24.4 kg/m2 over the 8 years before the diagnosis of diabetes. The mean BMI among the non-cases of diabetes did not exceed 23.2 kg/m2 throughout the period.
Conclusions
These results suggested that Japanese men who eventually developed diabetes during the 10-year observation period were not characterized as obese, but had stable high-normal BMIs before the onset of diabetes. Previous evidence showed that values for glycemic markers rapidly increased before the development of diabetes; however, the present study showed a slight gain in BMI in the earlier stage of the natural history of diabetes followed by a prolonged period of overweight.
Keywords: Body mass index trajectory, Prediction, Type 2 diabetes
Introduction
A large body of evidence has shown that elevated body mass index (BMI), gain in weight or BMI, and the duration of overweight or obesity were associated with an increased risk of the development of type 2 diabetes1–12. According to data on the trajectory of BMI from adolescence to young adulthood, men who eventually developed diabetes had higher BMIs during adulthood, such as around ages 30–45 years, compared with data for an entire study population13. The weight history of newly diagnosed diabetic patients was also investigated14,15, and it was reported that the highest mean BMI generally occurred at or immediately after diagnosis14. Nevertheless, the studies only included individuals with diagnosed diabetes, and the study was not designed to compare results among cases and non-cases of diabetes14,15. A few studies have investigated the long-term trajectory of BMI before the onset of diabetes in comparison with individuals free of diabetes using data from repeated clinical measurements during follow-up examinations of USA and Western adult participants16–18. In general, Asians have a higher prevalence of type 2 diabetes, although they have lower BMI levels than people of European descent19,20. A cross-sectional study that compared general obesity in treated patients with diabetes in Japan and in the UK showed a great difference in the degree of obesity between the two ethnicities, even though the two cohorts had similar characteristics regarding clinical markers other than BMI21. Longitudinal data on the trajectory of general adiposity with repeated clinical measurements before the actual onset of type 2 diabetes are sparse, especially in Asian individuals who are not predominantly overweight or obese.
Furthermore, in Japanese individuals who eventually developed type 2 diabetes, glycated hemoglobin (HbA1c) and glucose trajectories increased sharply after gradual long-term increases22. The Whitehall II study, which was a prospective study, showed changes in glucose concentrations, insulin sensitivity and insulin secretion as much as 3–6 years before the diagnosis of diabetes23. With reference to the rapid increases in levels of glycemic concentrations before the diagnosis of diabetes17,22–25, it remains unknown when in the natural history of diabetes an elevated BMI, an increasing BMI, or stable overweight or obesity could be observed among individuals who eventually develop type 2 diabetes. A better understanding of the relationships of the BMI trajectory and BMI history to the development of diabetes would help both clinicians and patients prevent deterioration of the glycemic state, which might have otherwise occurred. In the present study we investigated the trajectory of BMI and BMI histories before the development of type 2 diabetes in apparently healthy Japanese men.
Materials and Methods
Study Participants
The Toranomon Hospital Health Management Center Study included a cohort consisting mainly of apparently healthy government employees who underwent annual health examinations for health screening in Tokyo, Japan. We retrospectively examined data on 1,634 men who underwent health examinations on an annual basis during a 10-year follow-up period from 1997 to 2002 at the Health Management Center, Toranomon Hospital. We excluded men who had diabetes at the baseline examination (n = 81). Subsequently, 1,553 men without diabetes aged 26–80 years were eligible for the current analysis. Female participants were not included, because the database did not contain a reasonable number of incident cases of diabetes in women to carry out meaningful analyses (33 incident cases/565 women after exclusions). Diagnosis of type 2 diabetes was made according to the American Diabetes Association criteria26 of fasting plasma glucose (FPG) level ≥7.0 mmol/L, a self-reported history of clinician-diagnosed diabetes, or HbA1c (National Glycohemoglobin Standardization Program) ≥6.5% (≥48 mmol/mol). The study protocol followed the Japanese Government's Ethical Guidelines Regarding Epidemiological Studies in accordance with the Declaration of Helsinki, and was reviewed by the institutional review board at Toranomon Hospital.
Clinical Measurements
Weight and height were measured at baseline and at each annual follow-up examination, and BMI (kg/m2) was calculated. We assessed the maximum BMI during the follow-up time before the diabetes diagnosis, and a history of excessive obesity was indicated by BMI ≥27.5 kg/m2 in the present study27. Blood samples were collected after an overnight fast and measurements made using an automatic clinical chemistry analyzer (LABOSPECT 008; Hitachi, Tokyo, Japan). Blood glucose was measured by enzymatic methods and HbA1c was assessed by high-performance liquid chromatography.
Statistical Analysis
From our retrospective examination of these data, we initially divided the participants according to whether or not they had developed diabetes during the total follow-up time. The incidence of diabetes was assessed annually after the baseline examination. We diagnosed the incidence of diabetes if an elevated fasting glucose, elevated HbA1c or a self-reported history of clinician-diagnosis was first observed at an individual's annual examination. Then we set a timeline with 0 (years) to show the year of diagnosis of diabetes (incident cases of diabetes) or the final follow-up year (non-cases). BMI trajectories before the development of diabetes were retrospectively evaluated from the year of the baseline examination until the year of diagnosis of diabetes or to the end of the follow-up period. We calculated crude mean values for BMI, and the mean (95% confidence interval) is presented in Figure1. As the time of the development of diabetes varied among these individuals over the course of the observational period, data to draw a trajectory were not available for an entire 10-year period before diagnosis for all incident cases. We assessed whether there was an association between age and BMI with the diagnosis of diabetes among individuals who developed diabetes. Analysis was carried out with IBM spss Statistics version 19 (IBM, Armonk, NY, USA).
Figure 1.
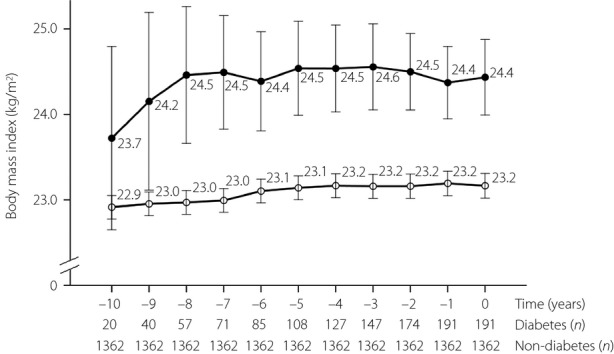
Trajectory of mean body mass index (95% confidence interval) among men who developed diabetes and who did not develop diabetes during the follow-up period of 10 years. Data are crude mean values and 95% confidence intervals. Closed circles, incident cases of diabetes; open circles, Non-diabetes cases.
Results
We documented 191 incident cases of type 2 diabetes over the 10-year follow-up period (Table1). At the baseline examination, the mean (standard deviation [SD]) BMI was 22.9 kg/m2 (2.6 kg/m2) and the mean age was 48.7 years (8.6 years) for individuals who did not develop diabetes, and the mean BMI was 24.2 kg/m2 (2.8 kg/m2) and mean age was 52.0 years (8.6 years) for those who developed diabetes.
Table 1.
Characteristics of study participants according to the incidence of type 2 diabetes during the follow-up period of 10 years
| Characteristics | Non-diabetes | Diabetes | |||
|---|---|---|---|---|---|
| (n = 1362) | Total | Years before the development of diabetes | |||
| (n = 191) | <4 years (n = 64) | 4–7 years (n = 70) | ≥8 years (n = 57) | ||
| Age at time of baseline examination (years) | 48.7 ± 8.6 | 52.0 ± 8.6** | 52.3 ± 9.2 | 51.8 ± 8.1 | 51.9 ± 8.8 |
| Parental history of diabetes | 177 (13.0) | 33 (17.3) | 11 (17.2) | 14 (20.0) | 8 (14.0) |
| Fasting glucose (mmol/L) | 5.3 ± 0.4 | 5.8 ± 0.5** | 6.0 ± 0.6 | 5.9 ± 0.5 | 5.6 ± 0.5 |
| BMI at time of baseline examination (kg/m2) | 22.9 ± 2.6 | 24.2 ± 2.8** | 23.7 ± 2.7 | 24.4 ± 2.8 | 24.4 ± 3.0 |
| Age at time of final examination (years) | 58.7 ± 8.6 | 57.4 ± 9.1 | 54.4 ± 9.2 | 57.2 ± 8.4 | 61.0 ± 8.8 |
| Maximum BMI during follow-up examinations (kg/m2) | 24.0 ± 2.7 | 24.9 ± 3.0** | 24.1 ± 2.8 | 25.2 ± 3.0 | 25.5 ± 3.1 |
| History of excessive obesity (BMI ≥27.5) | 138 (10.1) | 31 (16.2)* | 6 (9.4) | 14 (20.0) | 11 (19.3) |
Data are n (%) or means ± standard deviation unless otherwise indicated. BMI, body mass index. P-value was tested by t-test or χ2-test for two groups (non-diabetes cases vs total diabetes cases).
P < 0.001;
P < 0.05.
At the time of the diagnosis of diabetes, the mean (SD) BMI was 24.4 kg/m2 (3.1 kg/m2) among cases of diabetes (Figure1). Individuals who eventually progressed to diabetes experienced increasing levels of BMI in the early stage of the disease development (during the 10- to 8-years period before the onset of diabetes). Their mean BMI was 23.7 kg/m2 (2.3 kg/m2) 10 years before diagnosis, and reached 24.5 kg/m2 (3.0 kg/m2) 8 years before diagnosis. Individuals who developed diabetes experienced a prolonged and stable elevated BMI of ≥24.4 kg/m2 (range 24.4–24.6 kg/m2) over the 8 years before the diagnosis of diabetes. In contrast, the mean BMI among individuals who did not develop diabetes did not exceed 23.2 kg/m2 throughout the 10-year follow-up period. We also assessed incident cases of diabetes using different diagnostic criteria, which were: (i) FPG ≥7.0 mmol/L or a self-reported history of clinician-diagnosis (166 incident cases); or (ii) HbA1c ≥48 mmol/mol or self-reported history of clinician-diagnosis (158 incident cases). Results did not show a progressive increase in mean BMIs in the late stages before the diagnosis of diabetes; the mean BMIs among cases of diabetes were relatively stable although elevated using these diagnostic criteria (Table S1). When we assessed the maximum BMI and the history of excessive obesity (BMI ≥27.5 kg/m2; Table1), the mean maximum BMI was higher among cases of diabetes than non-cases (24.9 kg/m2 [3.0 kg/m2] vs 24.0 kg/m2 [2.7 kg/m2]; P < 0.001 by t-test). The prevalence of individuals with a history of excessive obesity was also higher among diabetic individuals (16.2% vs 10.1%; P = 0.011 by χ2-test).
We observed a linear association between age and BMI at the time of diagnosis of diabetes (Table2). Individuals who developed diabetes at an early age (<50 years) were more likely to have an elevated BMI (mean [SD] 25.1 kg/m2 [3.7 kg/m2] kg/m2) than those who developed diabetes at older ages (mean [SD] BMI 23.8 kg/m2 [2.7 kg/m2] for those aged 60–64 years; mean BMI 23.6 kg/m2 [3.3 kg/m2] for those aged ≥65 years). Results of our additional analysis in which participants were stratified into two groups by age at the time of diabetes diagnosis showed that men who developed diabetes at younger ages were more likely to have higher BMI levels in the late stage of the disease progression than those who developed diabetes at older ages (data not shown).
Table 2.
Body mass index according to five age groups at the time of diagnosis of diabetes among individuals who developed diabetes
| Age at the time of diagnosis of diabetes (years) | P-trend | |||||
|---|---|---|---|---|---|---|
| <50 | 50–54 | 55–59 | 60–64 | ≥65 | ||
| n | 37 | 45 | 37 | 28 | 44 | – |
| BMI at time of diagnosis of diabetes (kg/m2) | 25.1 (3.7) | 25.0 (2.9) | 24.5 (2.6) | 23.8 (2.7) | 23.6 (3.3) | 0.008 |
| BMI at time of baseline examination (kg/m2) | 25.0 (3.5) | 24.4 (2.4) | 24.1 (2.3) | 23.7 (2.6) | 23.6 (3.0) | 0.015 |
| Maximum BMI during follow-up examinations (kg/m2) | 25.6 (3.7) | 25.4 (2.7) | 25.1 (2.6) | 24.4 (2.6) | 24.2 (3.2) | 0.015 |
Data are crude mean (SD); n = 191. BMI, body mass index.
Discussion
In this cohort of apparently healthy Japanese men, the mean BMI value was 24.4 kg/m2 at the time of the diagnosis of type 2 diabetes, whereas the mean BMI did not exceed 23.2 kg/m2 among who did not develop diabetes. Considering our previous findings and those of other studies17,22–25 that the glycemic trajectory increased sharply after gradual long-term increases in individuals who progressed to diabetes, an opposite pattern was seen regarding the BMI. Specifically, a gain in the BMI was noted at an earlier stage followed by the maintenance of a high-normal mean BMI in the later stages before diagnosis, at which time glycemic indicators were shown to rapidly increase.
Although we did not observe a steady and marked mean BMI gain throughout the observational time among the individuals who developed diabetes, it was reported that there was a progressive rise in weight before the diagnosis of diabetes in Pima Indians14, and that the highest mean BMI generally occurred at or immediately after diagnosis14. In contrast, the average weight gain from 10 years before diabetes was only 1 kg among newly diagnosed Danish diabetic patients15. In a longitudinal study16 of participants from the Framingham Heart Study Offspring cohort, the mean BMI was 31.7 kg/m2 at the time of diagnosis and 30.1 kg/m2 at 10 years before the diagnosis of diabetes. Compared with findings in USA adults16, the mean BMI at the time of the diagnosis of diabetes was remarkably lower in our cohort of Japanese men, whereas the change in BMI over the 10-year follow-up period among individuals who eventually developed diabetes was of a similar degree. Adult weight gain is usually mainly fat28, and individuals with an increased BMI over 15 years had progressively worsening levels of metabolic risk profiles, including fasting glucose and fasting insulin concentrations29. According to a cross-sectional study of newly diagnosed patients with diabetes in Japan, a slight increase in BMI and waist circumference might have influenced the trend of decreases in fasting insulin concentrations over a decade30. A long duration of overweight/obesity would increase the risk of diabetes6–8,10–12, and it was reported that when the degree of adiposity persisted or became high, insulin sensitivity was impaired and glycemic deterioration occurred in lean Chinese adults31. A study of Whitehall II cohort participants was recently published; the majority of patients diagnosed with diabetes were classified as the “stable overweight” group, and it was suggested that many patients might not have a substantial weight gain in the later stage of disease development18, which is in line with our observation. The present results for Japanese individuals suggested that prolonged, elevated BMI levels even within the normal range influenced the deterioration of the glycemic state in men who subsequently progressed to diabetes.
A study32 of USA adults diagnosed with type 2 diabetes (∽90% were non-Hispanic white, and 10% were African American, Asian/Pacific Islander, Native American and Hispanic individuals) reported that the average BMI was 39 kg/m2 among younger participants, and that the older participants had BMI 33 kg/m2. The onset of diabetes would depend on BMI and age2,5,14,15,32, and reviews suggested that people in Asia tend to develop diabetes with a lesser degree of obesity and at younger ages19,20. Results of our longitudinal study showed that the mean BMI at the time of diagnosis of diabetes was higher among those who developed diabetes at a younger age than among those who developed diabetes when older. The weight change pattern after a new diagnosis of type 2 diabetes was reported to be predictive of glycemic and blood pressure control33, and the present results suggested that clinicians and patients should pay careful attention to an elevated BMI and weight control at the time of and after the diagnosis of diabetes, particularly in younger adults.
The strengths of the present study included a long-term follow up with repeated clinical measurements of weight, height, FPG and HbA1c to diagnose type 2 diabetes. Nevertheless, we only assessed general adiposity by BMI, and did not assess changes in waist circumference and visceral fat accumulation. It has been suggested that an accumulation of visceral fat over 5 years was independently associated with a greater risk of the development of diabetes in Japanese Americans34. We did not have available data on BMI 20 years or 30 years before the diagnosis of diabetes, so we could not determine whether individuals who eventually developed diabetes might have levels of BMI concordant with those who did not develop diabetes. Also, we did not have available data on BMI across the lifespan of individuals, and could not investigate the influence of BMI histories in childhood or in adolescence on our findings. Further extensive studies would be required with data on other obesity measures in long-term follow-up examinations. The present study only included male participants. Females were not investigated, because the number of female participants and incident cases of diabetes among women were not sufficient to draw a trajectory of BMI. An examination of sex differences in the trajectory of adiposity, including data on waist circumference, before the development of diabetes is required. Because of our study design, the time to the incidence of diabetes among cases varied over the course of the observational period, and there were differences in the time period for which the trajectory of BMI could be drawn between cases and non-cases. A small number of individuals were free from diabetes over a 9-year period after the baseline examination, but progressed to diabetes in the last 1 year after the 9-year prediabetic period. Data on oral glucose testing for the diagnosis of diabetes were not available. The lack of data on insulin and postprandial glucose concentrations during the follow-up period did not allow us to carry out detailed assessments of the pathophysiological background behind the development of diabetes. Also, we could not distinguish incident cases of type 1 diabetes during the follow-up period. As we did not calculate the risk of diabetes by BMI changes with adjustment for other factors, further investigations would be required to examine the independent role of BMI changes in the development of diabetes.
In conclusion, Japanese men who eventually developed diabetes over the 10-year period were not characterized by marked obesity, but had stable high-normal BMIs (≥24 kg/m2). Considering previous evidence of glycemic trajectories before the development of diabetes, a slight gain in BMI and a long-term stable overweight state were observed in earlier stages of the natural history of the development of diabetes than in later stages, during which rapidly increasing levels of glycemic markers could be observed.
Acknowledgments
This work is financially supported in part by the Ministry of Health, Labor and Welfare, Japan. H Sone and Y Heianza are recipients of a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science. The sponsors had no role in the design and conduct of the study. All authors sincerely thank the late Professor and Director Kinori Kosaka, MD, PhD, the Health Management Center, Toranomon Hospital, who established the foundation and framework of this project, and was always the foremost pillar of spiritual support of the Toranomon Hospital Health Management Center Study project. The authors declare no conflict of interest.
Supporting Information
Table S1 Mean body mass index (BMI) before the development of diabetes.
References
- Odegaard AO, Koh WP, Vazquez G, et al. BMI and diabetes risk in Singaporean Chinese. Diabetes Care. 2009;32:1104–1106. doi: 10.2337/dc08-1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasai H, Sairenchi T, Iso H, et al. Relationship between obesity and incident diabetes in middle-aged and older Japanese adults: the Ibaraki Prefectural Health Study. Mayo Clin Proc. 2010;85:36–40. doi: 10.4065/mcp.2009.0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodama S, Horikawa C, Fujihara K, et al. Quantitative relationship between body weight gain in adulthood and incident type 2 diabetes: a meta-analysis. Obes Rev. 2014;15:202–214. doi: 10.1111/obr.12129. [DOI] [PubMed] [Google Scholar]
- Chan JM, Rimm EB, Colditz GA, et al. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care. 1994;17:961–969. doi: 10.2337/diacare.17.9.961. [DOI] [PubMed] [Google Scholar]
- Schienkiewitz A, Schulze MB, Hoffmann K, et al. Body mass index history and risk of type 2 diabetes: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study. Am J Clin Nutr. 2006;84:427–433. doi: 10.1093/ajcn/84.1.427. [DOI] [PubMed] [Google Scholar]
- Everhart JE, Pettitt DJ, Bennett PH, et al. Duration of obesity increases the incidence of NIDDM. Diabetes. 1992;41:235–240. doi: 10.2337/diab.41.2.235. [DOI] [PubMed] [Google Scholar]
- Wannamethee SG, Shaper AG. Weight change and duration of overweight and obesity in the incidence of type 2 diabetes. Diabetes Care. 1999;22:1266–1272. doi: 10.2337/diacare.22.8.1266. [DOI] [PubMed] [Google Scholar]
- Jeffreys M, Lawlor DA, Galobardes B, et al. Lifecourse weight patterns and adult-onset diabetes: the Glasgow Alumni and British Women's Heart and Health studies. Int J Obes (Lond) 2006;30:507–512. doi: 10.1038/sj.ijo.0803161. [DOI] [PubMed] [Google Scholar]
- Jacobs-van der Bruggen MA, Spijkerman A, van Baal PH, et al. Weight change and incident diabetes: addressing an unresolved issue. Am J Epidemiol. 2010;172:263–270. doi: 10.1093/aje/kwq134. [DOI] [PubMed] [Google Scholar]
- Abdullah A, Wolfe R, Mannan H, et al. Epidemiologic merit of obese-years, the combination of degree and duration of obesity. Am J Epidemiol. 2012;176:99–107. doi: 10.1093/aje/kwr522. [DOI] [PubMed] [Google Scholar]
- The NS, Richardson AS, Gordon-Larsen P. Timing and duration of obesity in relation to diabetes: findings from an ethnically diverse, nationally representative sample. Diabetes Care. 2013;36:865–872. doi: 10.2337/dc12-0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchard DR, Porneala B, Janssen I, et al. Risk of type 2 diabetes and cumulative excess weight exposure in the Framingham Offspring Study. J Diabetes Complications. 2013;27:214–218. doi: 10.1016/j.jdiacomp.2012.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirosh A, Shai I, Afek A, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med. 2011;364:1315–1325. doi: 10.1056/NEJMoa1006992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Looker HC, Knowler WC, Hanson RL. Changes in BMI and weight before and after the development of type 2 diabetes. Diabetes Care. 2001;24:1917–1922. doi: 10.2337/diacare.24.11.1917. [DOI] [PubMed] [Google Scholar]
- de Fine Olivarius N, Richelsen B, Siersma V, et al. Weight history of patients with newly diagnosed Type 2 diabetes. Diabet Med. 2008;25:933–941. doi: 10.1111/j.1464-5491.2008.02472.x. [DOI] [PubMed] [Google Scholar]
- Preis SR, Pencina MJ, Mann DM, et al. Early-adulthood cardiovascular disease risk factor profiles among individuals with and without diabetes in the Framingham Heart Study. Diabetes Care. 2013;36:1590–1596. doi: 10.2337/dc12-1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faerch K, Witte DR, Tabak AG, et al. Trajectories of cardiometabolic risk factors before diagnosis of three subtypes of type 2 diabetes: a post-hoc analysis of the longitudinal Whitehall II cohort study. Lancet Diabetes Endocrinol. 2013;1:43–51. doi: 10.1016/S2213-8587(13)70008-1. [DOI] [PubMed] [Google Scholar]
- Vistisen D, Witte DR, Tabak AG, et al. Patterns of obesity development before the diagnosis of type 2 diabetes: the Whitehall II cohort study. PLoS Med. 2014;11:e1001602. doi: 10.1371/journal.pmed.1001602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon KH, Lee JH, Kim JW, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–1688. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009;301:2129–2140. doi: 10.1001/jama.2009.726. [DOI] [PubMed] [Google Scholar]
- Sone H, Ito H, Ohashi Y, et al. Obesity and type 2 diabetes in Japanese patients. Lancet. 2003;361:85. doi: 10.1016/S0140-6736(03)12151-4. [DOI] [PubMed] [Google Scholar]
- Heianza Y, Arase Y, Fujihara K, et al. Longitudinal trajectories of HbA1c and fasting plasma glucose levels during the development of type 2 diabetes: the Toranomon Hospital Health Management Center Study 7 (TOPICS 7) Diabetes Care. 2012;35:1050–1052. doi: 10.2337/dc11-1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabak AG, Jokela M, Akbaraly TN, et al. Trajectories of glycaemia, insulin sensitivity, and insulin secretion before diagnosis of type 2 diabetes: an analysis from the Whitehall II study. Lancet. 2009;373:2215–2221. doi: 10.1016/S0140-6736(09)60619-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vistisen D, Witte DR, Tabak AG, et al. Sex differences in glucose and insulin trajectories prior to diabetes diagnosis: the Whitehall II study. Acta Diabetol. 2014;51:315–319. doi: 10.1007/s00592-012-0429-7. [DOI] [PubMed] [Google Scholar]
- Sattar N, McConnachie A, Ford I, et al. Serial metabolic measurements and conversion to type 2 diabetes in the west of Scotland coronary prevention study: specific elevations in alanine aminotransferase and triglycerides suggest hepatic fat accumulation as a potential contributing factor. Diabetes. 2007;56:984–991. doi: 10.2337/db06-1256. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- Lean M. Health consequences of overweight and obesity in adults. In: Crawford D, Jeffery RW, Ball K, Brug J, editors. Obesity Epidemiology from Aetiology to Public Health. 2nd edn. New York: Oxford University Press Inc; 2010. pp. 43–58. [Google Scholar]
- Lloyd-Jones DM, Liu K, Colangelo LA, et al. Consistently stable or decreased body mass index in young adulthood and longitudinal changes in metabolic syndrome components: the Coronary Artery Risk Development in Young Adults Study. Circulation. 2007;115:1004–1011. doi: 10.1161/CIRCULATIONAHA.106.648642. [DOI] [PubMed] [Google Scholar]
- Matsuba I, Saito K, Takai M, et al. Fasting insulin levels and metabolic risk factors in type 2 diabetic patients at the first visit in Japan: a 10-year, nationwide, observational study (JDDM 28) Diabetes Care. 2012;35:1853–1857. doi: 10.2337/dc12-0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R, Brickman WJ, Christoffel KK, et al. Association of adiposity trajectories with insulin sensitivity and glycemic deterioration: a longitudinal study of rural Chinese twin adults. Diabetes Care. 2012;35:1506–1512. doi: 10.2337/dc11-2060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillier TA, Pedula KL. Characteristics of an adult population with newly diagnosed type 2 diabetes: the relation of obesity and age of onset. Diabetes Care. 2001;24:1522–1527. doi: 10.2337/diacare.24.9.1522. [DOI] [PubMed] [Google Scholar]
- Feldstein AC, Nichols GA, Smith DH, et al. Weight change in diabetes and glycemic and blood pressure control. Diabetes Care. 2008;31:1960–1965. doi: 10.2337/dc08-0426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wander PL, Boyko EJ, Leonetti DL, et al. Change in visceral adiposity independently predicts a greater risk of developing type 2 diabetes over 10 years in Japanese Americans. Diabetes Care. 2013;36:289–293. doi: 10.2337/dc12-0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Mean body mass index (BMI) before the development of diabetes.


