Abstract
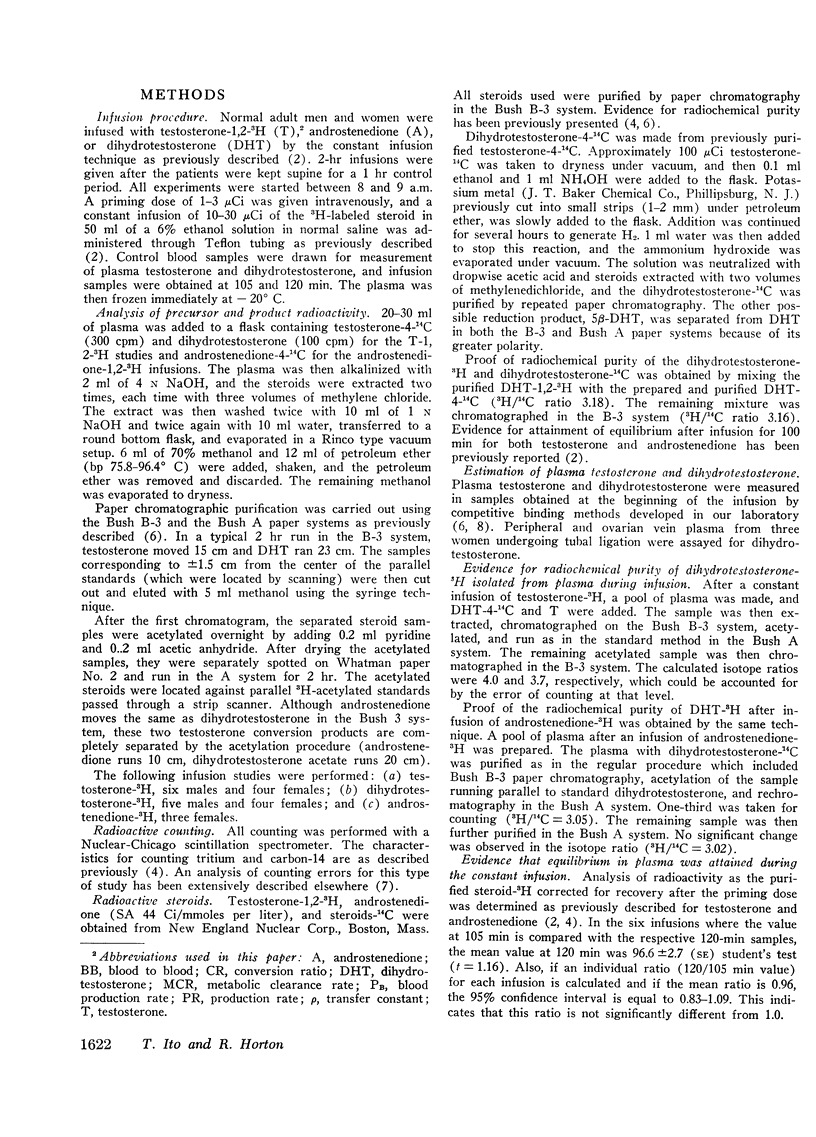
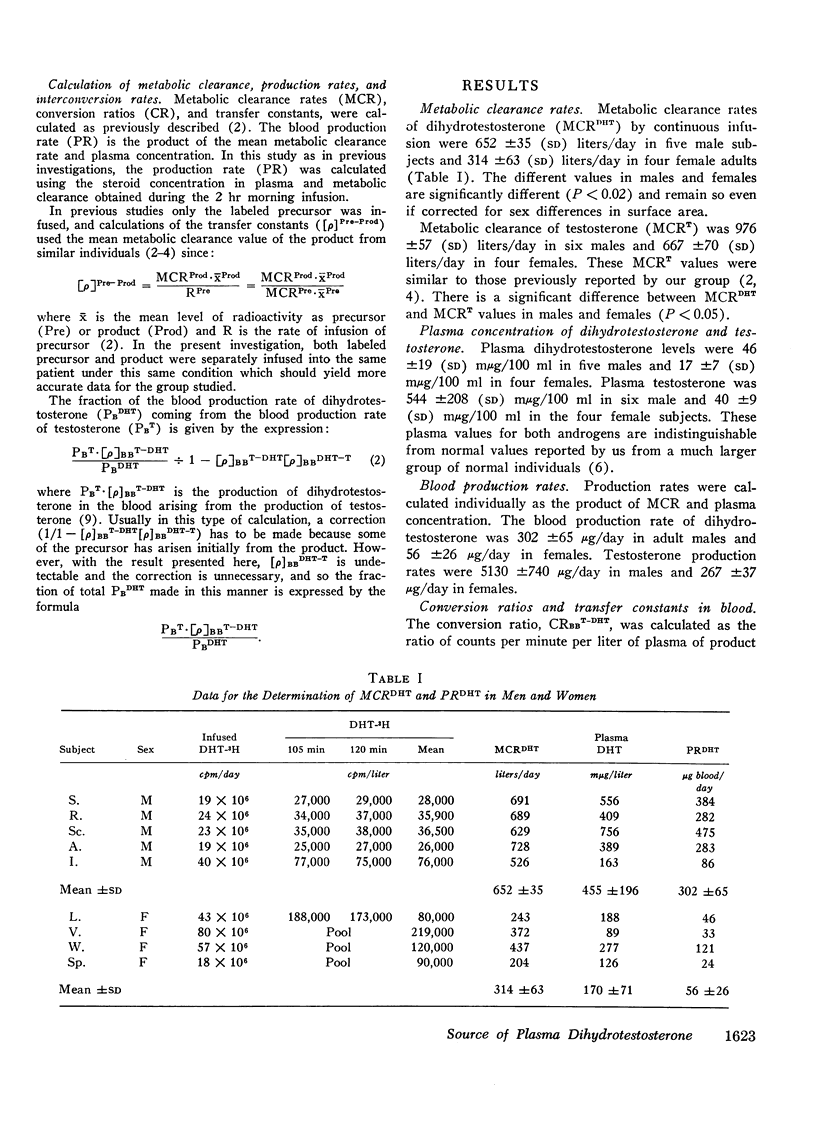
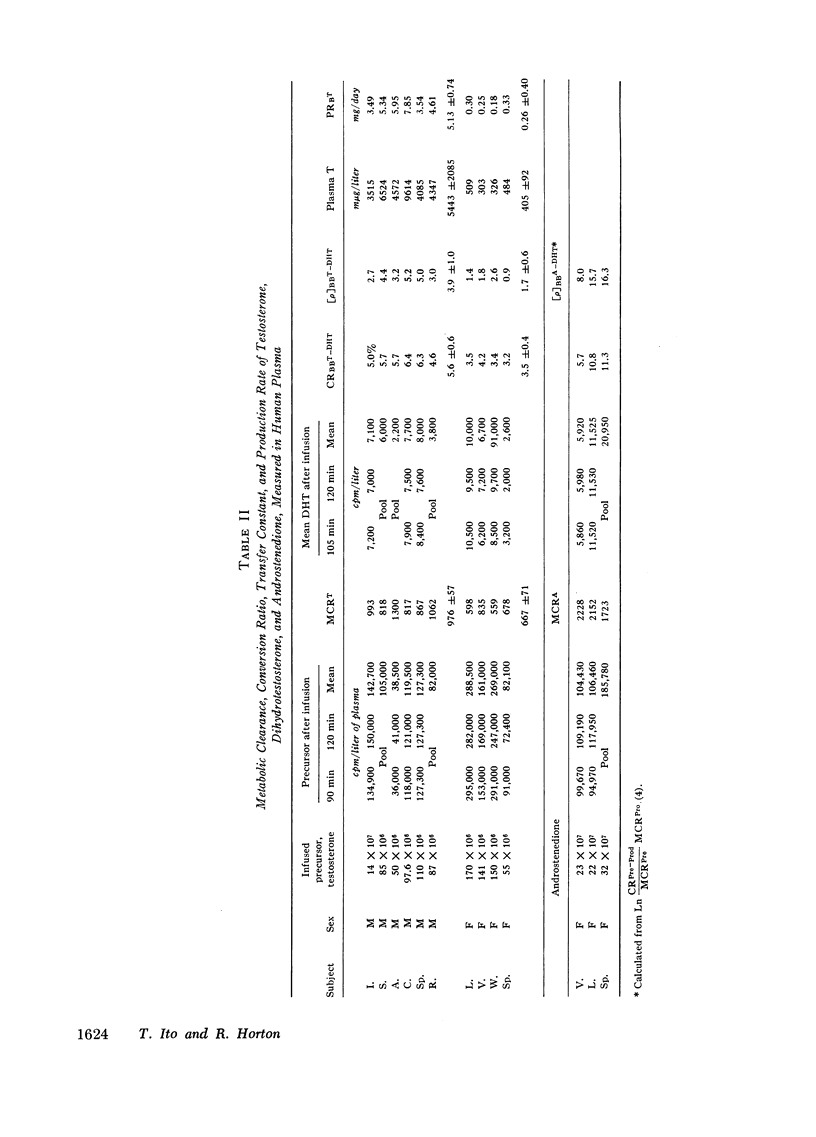
The source of plasma dihydrotestosterone (DHT) (17β-hydroxy-5α-androstan-3-one) in humans has been investigated by infusing two potential peripheral precursors, testosterone (T) and androstenedione (A). Metabolic clearance rates (MCR), conversion ratios (CR), transfer constants (ρ), and blood production rates (PB) were calculated. Plasma testosterone and dihydrotestosterone were measured by competitive binding techniques. The MCRDHT was 652 ±35 (SD) liters/day in five males and 314 ±63 (SD) liters/day in four adult females. In each individual, the MCRDHT was significantly lower than MCRT as predicted by testosterone-binding protein affinity studies. The PBDHT was 302 ±65 (SD) μg/day in males and 56 ±26 μg/day in females. Testosterone and androstenedione are precursors (prehormones) for plasma dihydrotestosterone. The conversion ratio CRBBT-DHT, calculated as the ratio of counts per minute per liter of plasma of product to precursor after infusion of labeled precursor, was 5.6 ±0.6 (SD)% (six subjects) in the male and 3.5 ±0.4 (SD)% (four subjects) in the female. CRBBA-DHT after androstenedione infusion to three female subjects averaged 9.2%. No dihydrotestosterone back conversion was detected (< 0.2%). The transfer constants were [ρ]BBT-DHT, 3.9 ±1.0% (male) and 1.7 ±0.6% (female), and [ρ]BBA-DHT average was 13.3% in three female subjects. Using either plasma testosterone and dihydrotestosterone values from our subjects and mean androstenedione values as reported in the literature, approximate contributions can be calculated. Testosterone conversion accounts for at least 70% of plasma DHT in the male, but less than 20% in the normal female. Androstenedione appears to be a major prehormone of plasma dihydrotestosterone accounting for at least two-thirds plasma dihydrotestosterone by peripheral conversion in adult females. In three normal women undergoing tubal ligation, there was an unimpressive gradient between ovarian vein and peripheral plasma dihydrotestosterone. It is suggested that dihydrotestosterone in the blood does not arise from direct secretion but may reflect events occurring in peripheral androgen target tissues.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baird D. T., Horton R., Longcope C., Tait J. F. Steroid dynamics under steady-state conditions. Recent Prog Horm Res. 1969;25:611–664. doi: 10.1016/b978-0-12-571125-8.50017-x. [DOI] [PubMed] [Google Scholar]
- Baird D., Horton R., Longcope C., Tait J. F. Steroid prehormones. Perspect Biol Med. 1968 Spring;11(3):384–421. doi: 10.1353/pbm.1968.0053. [DOI] [PubMed] [Google Scholar]
- Bruchovsky N., Wilson J. D. The conversion of testosterone to 5-alpha-androstan-17-beta-ol-3-one by rat prostate in vivo and in vitro. J Biol Chem. 1968 Apr 25;243(8):2012–2021. [PubMed] [Google Scholar]
- Gloyna R. E., Wilson J. D. A comparative study of the conversion of testosterone to 17-beta-hydroxy-5-alpha-androstan-3-one (Dihydrotestosterone) by prostate and epididymis. J Clin Endocrinol Metab. 1969 Jul;29(7):970–977. doi: 10.1210/jcem-29-7-970. [DOI] [PubMed] [Google Scholar]
- Herman T. S., Fimognari G. M., Edelman I. S. Studies on renal aldosterone-binding proteins. J Biol Chem. 1968 Jul 25;243(14):3849–3856. [PubMed] [Google Scholar]
- Horton R., Tait J. F. Androstenedione production and interconversion rates measured in peripheral blood and studies on the possible site of its conversion to testosterone. J Clin Invest. 1966 Mar;45(3):301–313. doi: 10.1172/JCI105344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton R., Tait J. F. In vivo conversion of dehydroisoandrosterone to plasma androstenedione and testosterone in man. J Clin Endocrinol Metab. 1967 Jan;27(1):79–88. doi: 10.1210/jcem-27-1-79. [DOI] [PubMed] [Google Scholar]
- Ito T., Horton R. Dihydrotestosterone in human peripheral plasma. J Clin Endocrinol Metab. 1970 Oct;31(4):362–368. doi: 10.1210/jcem-31-4-362. [DOI] [PubMed] [Google Scholar]
- Kato T., Horton R. A rapid method for the estimation of testosterone in female plasma. Steroids. 1968 Nov;12(5):631–650. doi: 10.1016/s0039-128x(68)80039-x. [DOI] [PubMed] [Google Scholar]
- Kato T., Horton R. Studies of testosterone binding globulin. J Clin Endocrinol Metab. 1968 Aug;28(8):1160–1168. doi: 10.1210/jcem-28-8-1160. [DOI] [PubMed] [Google Scholar]
- Korenman S. G. Comparative binding affinity of estrogens and its relation to estrogenic potency. Steroids. 1969 Feb;13(2):163–177. doi: 10.1016/0039-128x(69)90004-x. [DOI] [PubMed] [Google Scholar]
- Longcope C., Kato T., Horton R. Conversion of blood androgens to estrogens in normal adult men and women. J Clin Invest. 1969 Dec;48(12):2191–2201. doi: 10.1172/JCI106185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longcope C., Layne D. S., Tait J. F. Metabolic clearance rates and interconversions of estrone and 17beta-estradiol in normal males and females. J Clin Invest. 1968 Jan;47(1):93–106. doi: 10.1172/JCI105718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermeulen A., Verdonck L. Testosterone assays by competitive protein binding. Acta Endocrinol Suppl (Copenh) 1970;147:239–256. doi: 10.1530/acta.0.065s239. [DOI] [PubMed] [Google Scholar]
- Wilson J. D., Walker J. D. The conversion of testosterone to 5 alpha-androstan-17 beta-ol-3-one (dihydrotestosterone) by skin slices of man. J Clin Invest. 1969 Feb;48(2):371–379. doi: 10.1172/JCI105994. [DOI] [PMC free article] [PubMed] [Google Scholar]


