SUMMARY
Atherosclerosis is a common cardiovascular disease in the United States. The disease is a leading cause of illness and death in the United States. Atherosclerosis is the most common cause for heart attack and stroke. Most commonly, people develop atherosclerosis as a result of diabetes, genetic risk factors, high blood pressure, a high-fat diet, obesity, high blood cholesterol levels, and smoking. However a sizable amount of patients suffering from atherosclerosis do not harbor the classical risk factors. Ongoing infections have been suggested to play a role in this process. Periodontal disease is perhaps the most common chronic infection in adults with a wide range of clinical variability and severity. Research in the past decade has shed substantial light on both the initiating infectious agents and host immunological responses in periodontal disease. Up to 46% of the general population harbors the microorganism(s) associated with periodontal disease, although many are able to limit the progression of periodontal disease or even clear the organism(s) if infected. In the last decade, several epidemiological studies have found an association between periodontal infection and atherosclerosis. This review focuses on exploring the molecular consequences of infection by pathogen that exacerbate atherosclerosis, with focus on infection by the periodontal bacterium Porphyromonas gingivalis as a running example.
Keywords: atherosclerosis, TLRs, NOD2, Porphyromonas gingivalis, innate immunity
Introduction
Periodontal disease presents with a wide range of clinical variability and severity. Research in the past decade has shed substantial light on the initiating infectious agents and host immunological responses in periodontal disease, both of which have been shown to modify the progression of periodontal disease. Cullinan et al. have shown that up to 46% of the general population harbor the causative organism(s) of periodontal disease, but many are able to limit disease progression or even clear the organism(s) if infected (Cullinan et al., 2003). Overall, Cullinan et al. suggest a complex multifactorial etiology of periodontal disease between host ‘immune’ response and environmental factors (Cullinan, et al., 2003).
The characteristics of an individual’s immune response to infectious agents have a major effect on the severity of periodontal disease (Van Dyke & Sheilesh, 2005). Michalowicz et al. used a twin study to show that genetic hereditability appears to contribute approximately 50% to the clinical susceptibility of periodontal disease (Michalowicz et al., 2000). In addition, studies have suggested that dysregulation of innate immunity plays a key role in the progression of periodontal disease (Slots & Genco, 1984). Specifically, the host immune response is suppressed upon low-level stimulation of critical pattern recognition receptors, leading to a muted local immune response, thus enabling periodontal disease-associated bacteria such as Porphyromonas gingivalis (P. gingivalis) to evade the host immune system (Muthukuru, Jotwani, & Cutler, 2005; Tanabe & Grenier, 2008).
Epidemiologic evidence has further suggested that the long-term effects of periodontal disease can be linked to more serious systemic conditions such as cardiovascular disease, diabetes, and complications of pregnancy (Campus, Salem, Uzzau, Baldoni, & Tonolo, 2005; Chi, Messas, Levine, Graves, & Amar, 2004; Chiang, Kyritsis, Graves, & Amar, 1999; Dasanayake, Boyd, Madianos, Offenbacher, & Hills, 2001; Dasanayake et al., 2003; Nishimura et al., 2006). Bahekar et al (2007). determined a statistically significant 1.14- to 1.59-fold increase in prevalence of coronary heart disease in patients with periodontitis after adjusting for risk factors such as smoking, diabetes, alcohol intake, obesity, and blood pressure (Bahekar, Singh, Saha, Molnar, & Arora, 2007). Recently, Amar et al. have shown that the presence of a P. gingivalis bacteremia alone, a common complication in patients with periodontal disease, is not sufficient to exacerbate atherosclerosis; rather, bacteremia coupled with intra-cellular invasion of endothelial cells by P. gingivalis is required (Amar, Wu, & Madan, 2009). Upon invasion, endothelial cells activate and upregulate various adhesion molecules, thus increasing the likelihood of macrophage diapedesis and, when coupled with exposure to a high fat diet (HFD), subsequent conversion to foam cells thus furthering atheroma progression (den Dekker, Cheng, Pasterkamp, & Duckers, 2009). In addition, mature atheroma macrophages display reduced responsiveness from their pattern recognition receptors, in a fashion similar to that seen in the response to low-level stimulation of lipopolysaccharide (Muthukuru, et al., 2005; Tanabe & Grenier, 2008). Lipopolysaccharides induce a similar state of tolerance and dysregulation in endothelial cells and circulating white blood cells (Epstein, 2002). Both of these mechanisms further exacerbate the effect of periodontal disease on the progression of atherosclerosis.
Periodontal Disease’s Impact on the Immune Response
Periodontal disease results from an inflammatory response caused by deposits on the teeth of bacterial biofilm (dental plaque) and its by-products. Periodontal pathogens, such as P. gingivalis, invade and colonize periodontal sites, evading the local immune response, which ultimately leads to periodontal destruction furthering periodontal disease’s progression (Heitman, 2006; Slots & Genco, 1984). It has been shown that P. gingivalis is capable of invading both oral epithelial cells and aortic endothelial cells (Deshpande, Khan, & Genco, 1998; Njoroge, Genco, Sojar, Hamada, & Genco, 1997), and P. gingivalis has recently been detected in both oral and aortic tissues of infected mice (Velsko et al., 2014). Further, Njoroge et al. have shown that the invasive properties of P. gingivalis are dependent on the fimbriae (Fim) protein, as demonstrated by the failure of fimA- mutant DPG3 strain of P. gingivalis to adhere and invade oral epithelial cells (Njoroge, et al., 1997). Taken together, this demonstrates that in addition to colonizing periodontal sites, P. gingivalis can be found systemically within the aortic tree, and that P. gingivalis is an invasive species of bacteria with the Fim protein mediating its adherence and invasive properties.
Immune Response to Microbial Pathogens
The response of a mammalian host to microbial pathogens involves the activation of both innate and adaptive components of the immune system. An important cellular component of the innate immune response is the macrophage axis, since macrophages are often among the ‘first responders’ to a microbial pathogen. Macrophages are also involved in activating the adaptive arm of the immune response via antigen-presentation, thus linking the innate response to adaptive immunity. Therefore, macrophages play a critical role in mounting a proper immune response and it is important to understand how macrophages detect pathogens and their by-products (e.g. lipopolysaccharides) as well as the effect of pathogens on macrophages. Macrophages recognize pathogens by a variety of repetitive motifs, referred to as pathogen-associated molecular patterns, found commonly on many different pathogens. Macrophages perform this by expressing a limited number of pattern recognition receptors found on the macrophage and endothelial cells that bind to the pathogen-associated molecular patterns on the pathogen and through subsequent intracellular signaling trigger the inflammatory response (Aderem, 2003; Akira, Uematsu, & Takeuchi, 2006; Beutler et al., 2006; Medzhitov & Janeway, 2000). Some of these receptor types include toll-like receptors (TLRs), nucleotide-binding oligomerization domains (NODs), CD14, complement receptor-3, lectins, and scavenger receptors (Areschoug & Gordon, 2008).
The first major class type of pattern recognition receptor, and the one most capable in recognition and signaling in association with P. gingivalis exposure, is the TLR family. TLRs monitor the extracellular environment and phagolysosomal compartments and recognize pathogen-associated molecular patterns including lipopolysaccharides, flagella, CpG DNA, oxidized low density lipopeptide, endogenous proteins like heat shock protein 60 (Zuany-Amorim, Hastewell, & Walker, 2002) and bacterial lipoprotein (Medzhitov, 2001). More specifically, activation of TLR-2, widely known to recognize elements of gram-negative bacteria cell wall components, has been shown to lead to an increase in pro-inflammatory response (Burns, Bachrach, Shapira, & Nussbaum, 2006). Recently, Aoki et al. found that proinflammatory response to P. gingivalis Fimbria in macrophages was suppressed by the introduction of an anti-TLR-2 antibody, suggesting that TLR-2 responds to lipoproteins or lipopeptides associated with the P. gingivalis Fim proteins already implicated in macrophage invasion (Aoki, Tabeta, Murakami, Yoshimura, & Yamazaki, 2010). Thus the normal role of TLR-2 is very critical to the detection and clearance of gram-negative microbial pathogens, such as P. gingivalis.
The second major class of pattern recognition receptors includes soluble cytosolic NOD-like receptors. NOD-like receptors complement the host defense by providing a second, intracellular layer of surveillance. The NOD proteins are soluble cytosolic proteins, which recognize cell wall fragments from both gram-negative and gram-positive bacteria (Chamaillard, Girardin, Viala, & Philpott, 2003; Girardin, Hugot, & Sansonetti, 2003; Inohara, Chamaillard, McDonald, & Nunez, 2005). NOD1 recognizes a specific peptidoglycan fragment containing diaminopimelic acid, while NOD2 recognizes a muramyl dipeptide (MDP) fragment of peptidoglycan. Recently, Liu et al. found that even without TLR activity, NODs detected the presence of P. gingivalis and responded by increasing proinflammatory response, showing NODs to be an effective mechanism for triggering an immune response against P. gingivalis infection (J. Liu, Wang, & Ouyang, 2014). TLRs and NODs are found in both macrophages and endothelial cells, though how these cells initiate a threat-specific transcriptional response is poorly understood when these detection receptors are activated. NOD2 expression and unique functions have also been described in other cell types, including adipocytes, gingival, pulp and periodontal fibroblasts, oral epithelial cells, and vascular endothelial cells (Hirao et al., 2009; Hosokawa et al., 2010; Oh et al., 2005; Stroh et al., 2008; Sugawara et al., 2006; L. Tang et al., 2011). However, the precise role of NOD2 in chronic inflammatory diseases remains unclear.
Activation of either TLR-2 or NOD1/NOD2 receptors, common with P. gingivalis exposure, results in the activation of the NF-κb (Asai, Ohyama, Gen, & Ogawa, 2001; J. Liu, et al., 2014; Wang & Ohura, 2002). This in turn triggers the increased expression of many pro-inflammatory cytokines, including tumor necrosis factor alpha (TNF-α), Interleukin (IL)-1β, IL-6 (Geivelis, Turner, Pederson, & Lamberts, 1993; Salvi et al., 1998; Yavuzyilmaz et al., 1995); chemokines including IL-8, monocyte chemotactic protein-1 (MCP-1), chemokine (C-C motif) ligand 5 (RANTES) (Emingil, Atilla, & Huseyinov, 2004; Tsai, Ho, & Chen, 1995); C-reactive protein (CRP) (Dasanayake, 2009; Salzberg et al., 2006) and mRNA for TLRs (Ren, Leung, Darveau, & Jin, 2005). In periodontal disease, this signaling is most likely to occur in gingival epithelial cells, human gingival fibroblasts, and macrophages (Asai, et al., 2001; Wang & Ohura, 2002). However, in response to repeated bacteremias P. gingivalis has been known to trigger TLRs and NOD signaling in both aorta and cardiac endothelial cells (Deshpande, et al., 1998).
Combined, the TLRs and NODs represent two critical layers of defense to detect pathogens and modulate the immune response differentially. TLRs detect extracellular presence of P. gingivalis whereas NODs detect intracellular presence of P. gingivalis, such that activation of NOD signaling represents a breach of the outer layers of defense for a cell and hence leads to an enhanced immune response. Park et al. demonstrated that NOD signaling enhances immune response when challenging mesothelial cells, since in NOD knockout mice many common pathogen-associated molecular patterns led to slightly reduced pro-inflammatory cytokines and chemokines levels (Park et al., 2007).
Homotolerance
Lipopolysaccharide is an endotoxin found on the outer membrane of gram-negative bacteria, such as P. gingivalis, that has been shown to be a potent activator of the innate immune response, especially of macrophages. Lipopolysaccharide can also be released from dying gram-negative bacteria, which binds to a plasma lipopolysaccharide-binding protein. The combination lipopolysaccharide-lipopolysaccharide-binding protein complex transfers the lipopolysaccharides to first CD-14 and then to lymphocyte antigen 96 protein (MD-2), which ultimately activates TLR-4 signaling and triggers an inflammatory response (Cohen, 2002; Raetz, 1990) on macrophages and dendritic cells (Jerala, 2007; J. D. Johnson et al., 2002; L. L. Johnson & Sayles, 2002).
Pathogens have acquired many ways of avoiding the host immune response. Unexpectedly Tanabe et al. have recently shown that low-level pre-treatment stimulation with lipopolysaccharide, 0.01 to 0.1 μg/ml, reduces TNF-α levels in response to subsequent stronger lipopolysaccharide stimulation, 1 μg/ml, within 24 hrs. of the pre-treatment dosage of lipopolysaccharide (Tanabe & Grenier, 2008). This process ultimately leads to macrophage tolerance, as demonstrated by a decreased level of TNF-α (Tanabe & Grenier, 2008). In addition, Dobrovolskaia et al. further characterized the reduced inflammatory response as “homotolerance,” since cells pre-treated with a specific ligand to a pattern recognition receptor, e.g. P. gingivalis lipopolysaccharide: TLR-2 activation and subsequently challenged by the same pattern recognition receptors demonstrated a reduced level of TNF-α secretion (Dobrovolskaia et al., 2003). “Heterotolerance,” i.e. the overall reduced immune response, was not observed when pre-treating with a ligand for a pattern recognition receptor and subsequently challenging with a ligand for a different pattern recognition receptor, e.g. pre-treatment with P. gingivalis-lipopolysaccharide and challenge with N-palmitoyl-S-[2,3-bis(palmitoyl)-(2RS)-propyl]-(R)cysteinyl-alanyl-glycine (Pam3Cys), a synthetic lipopeptide that activates different pattern recognition receptor(s) (Dobrovolskaia, et al., 2003).
Further work by Muthukuru et al. have shown that similar pre-treatment and subsequent strong challenge by P. gingivalis lipopolysaccharide specifically demonstrated homotolerance by reduction of TLR-2 and TLR-4 mRNA levels (Muthukuru, et al., 2005) suggesting alterations in either the transcription factors present at the TLR promoters or the TLR genes themselves. The decreased secretion of a critical inflammatory mediator, TNF-α, was shown by Tanabe et al. to be the effect of a lipopolysaccharide-induced homotolerance response in macrophages (Tanabe & Grenier, 2008). However, homotolerance was not observed across the entire spectrum of pro-inflammatory cytokines; e.g. both IL-1β and matrix metalloproteinase (MMP)-9 showed increased secretion upon low-level pre-treatment stimulation and subsequent strong lipopolysaccharide stimulation (Tanabe & Grenier, 2008).
Homotolerance can possibly provide some answers regarding the immune tolerance observed in some periodontal conditions. We suggest that muting of innate immune response by P. gingivalis enables it to evade the host immune defense mechanism. Based on varying levels of tolerance across specific macrophage subsets with differential functions, this appears to be a critical evolutionary feature of P. gingivalis and provides P. gingivalis a means to avoid the host immune response, thus enabling it to survive and thrive in periodontal sites (Foey & Crean, 2013). Alternatively, this could also represent a host protective measure aimed at protection against endotoxin induced septic shock to prevent a systemic inflammatory response/cytokine release which could potentially be fatal (Biswas & Lopez-Collazo, 2009).
Impact of Periodontal Bacteria on Atherosclerosis
Atherosclerosis is now considered to be one manifestation of a state of disordered immunity in which there is dynamic interaction between endothelial dysfunction (characterized by loss of normal endothelium-dependent vasodilatation), inflammation, and repeated cycles of ‘wound healing response’ (Michelsen, Doherty, Shah, & Arditi, 2004).
Coronary heart disease is a major cause of morbidity and mortality worldwide. Traditional risk factors like hypercholesterolemia, smoking and hypertension have failed to fully explain the incidence of coronary heart disease and recently epidemiological studies have pointed to links between periodontal disease and coronary heart disease (Epstein, 2002). A possible role of infection in atherogenesis has been postulated involving multiple pathogens, with some playing a more predominant role (e.g. P. gingivalis; Chlamydophila pneumoniae), in which the risk of coronary heart disease relates to the overall aggregate pathogen load, or “pathogen burden,” that an individual carries (Epstein, 2002). Specifically, Pussinen et al. concluded that high levels of anti-P. gingivalis IgG antibodies, common in periodontal disease patients, were associated with coronary heart disease and determined an increased odds ratio (1.5) after adjusting for various common coronary heart disease risk factors (Pussinen et al., 2004). Additionally, Tang et al. found that the risk increases with the severity of periodontitis, such that patients with severe periodontal disease have an increased odds ratio of 2.0 for developing coronary heart disease (K. Tang, Lin, Wu, & Yan, 2011). In addition to contributing to the development of atherosclerosis (Epstein, 2002; Epstein, Zhou, & Zhu, 1999); infection can also trigger plaque rupture and acute thrombotic occlusion, the major factors responsible for acute myocardial infarction and for sudden death in patients with coronary heart disease (Epstein, 2002).
It has been hypothesized that a complex relationship between human periodontal disease and increased risk for acute myocardial infarction exists (Arbes, Slade, & Beck, 1999; DeStefano, Anda, Kahn, Williamson, & Russell, 1993; Joshipura et al., 1996; Mattila, 1989, 1993; Mattila, Valtonen, Nieminen, & Huttunen, 1995; Nery, Meister, Ellinger, Eslami, & McNamara, 1987; Umino & Nagao, 1993). Mechanisms are now emerging supporting this hypothesis, linking transient bacteremias, common in periodontal disease, with endothelial dysfunction, an event in atherosclerosis development (Amar et al., 2003; Tonetti et al., 2007). Periodontal infection is known to induce local inflammation, and several studies have demonstrated that patients with periodontal disease have elevated levels of systemic inflammatory mediators, such as CRP (Amar, et al., 2003). This inflammation often leads to gingival ulcerations and local vascular changes, which have the potential to increase the incidence and severity of transient bacteremias. (Amar, et al., 2003) Recently, Amar et al. have demonstrated endothelial dysfunction upon repetitive bacteremic exposure, which in turn exacerbates the development of atherosclerosis and coronary heart disease (Amar, et al., 2009). Specifically, endothelial cells upregulate cell adhesion molecule, p-selectins and inter-cellular adhesion molecules (ICAMs) (integrin ligands) in response to bacterial exposures, as from P. gingivalis, thus increasing the likelihood of monocyte transiting from the blood compartment to the local tissue compartment (Khlgatian, Nassar, Chou, Gibson, & Genco, 2002).
It has been suggested that periodontal disease can lead to persistent low-level bacteremia, an elevated white cell count, and systemic endotoxemias, which together could affect endothelial integrity, metabolism of plasma lipoproteins, blood coagulation, and platelet function (Amar, et al., 2003; Gibson et al., 2004; Hoge & Amar, 2006; J. Kim & Amar, 2006). Recent experimental studies have elucidated how repeated bacteremic exposures of P. gingivalis lead to endothelial dysfunction, after certain strains of P. gingivalis were found to have invaded human coronary artery endothelial cells and were detected within atherosclerotic plaques themselves (Deshpande, et al., 1998; Haraszthy, Zambon, Trevisan, Zeid, & Genco, 2000; Progulske-Fox et al., 1999). Specifically, P. gingivalis has been identified by PCR and fluorescence in situ hybridization in atheromatous plaques of patients suffering from atherosclerosis (Cavrini et al., 2005; Rath, Mukherjee, Kaushik, Sen, & Kumar, 2014; Velsko, et al., 2014), as well as in the bloodstream after plaque rupture (Ohki et al., 2012), suggesting that these microorganisms might be metabolically active within the atheroma.
Further, experimental studies support the hypothesis that local inflammation within the artery wall also contributes to the acceleration of atherosclerosis in response to endothelial infection, e.g. by P. gingivalis, which would result in a spectrum of systemic effects, producing alterations in circulating cytokines, acute-phase reactants, white blood cells, and responses mediated by the immune system (Epstein, 2002).
The validity of this concept has been demonstrated in a study by Zhu et al. which showed that only the combination of infection and inflammation led to a greatly increased odds ratio for coronary heart disease (Zhu, Quyyumi, Norman, Csako, & Epstein, 1999). According to the study, cytomegalovirus infection led to an increased odds ratio of 1.3 for coronary heart disease, and elevated C-reactive protein levels, indicative of an ongoing inflammatory response, led to an increased odds ratio of 2.3, while the two combined produced the increased odds ratio of 4.3 (Zhu, et al., 1999).. Zhu et al. suggest that infection alone is not sufficient for development of atherosclerosis, but the combination of both infection and an inflammatory response leaves the patient susceptible to pro-atherogenic effects (Zhu, et al., 1999). Several subsequent studies have demonstrated that patients with periodontal disease have elevated levels of systemic inflammatory mediators (Amabile et al., 2008; Nakajima et al., 2010; Sun et al., 2009; K. Tang, et al., 2011), specifically circulating C-reactive protein, a systemic marker of inflammation (Amar, et al., 2003). Still, infection plays a major role in the development of atherosclerosis. Amar et al. have recently demonstrated that P. gingivalis infected mice fed a HFD had twice as much of the aorta occupied by atherosclerotic lesions when compared to non-infected P. gingivalis mice also fed HFD (Amar, et al., 2009).
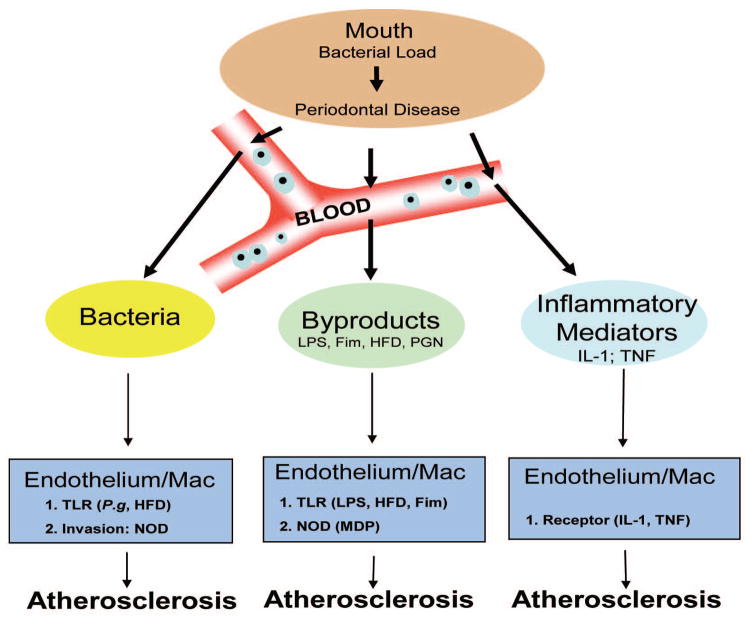
Mechanistically, TLRs and NODs, both pattern recognition receptors, are critical in the detection of various pathogens, including P. gingivalis. (Figure 1) Following detection, the host immune response provides an increase in inflammatory mediators such as IL-1, TNF-α and CRP. IL-1 signaling appears to be crucial in P. gingivalis-associated atherogenesis since IL-1R-deficient animals failed to develop atherosclerosis (Chi, et al., 2004). Studies have also demonstrated increased vascular risk in individuals with elevated levels of a wide range of molecules such as IL-6, TNF-α, ICAMs, vascular cell adhesion molecule-1 (VCAM-1) (Blake & Ridker, 2002) P-selectin, CRP, fibrinogen, and serum amyloid A (SAA) (Mahmoudi, Curzen, & Gallagher, 2007).
Figure 1. Relationship of P. gingivalis Infection and Atherosclerosis.
As the bacterial load of P. gingivalis in the oral cavity increases Periodontal Disease becomes more severe. However, damage is not just limited to the oral cavity since local vasculature enables an entry point for bacteria, bacterial by-products, or inflammatory mediators (e.g. cytokines IL-1 or TNF-α). Bacteremia, common in periodontal disease due to dental work e.g. cleaning, flossing or surgery, effect both endothelium and macrophages by inducing homotolerance along the TLR pathway. However, since P. gingivalis is an invasive bacterium, mediated by its Fim protein, it has the ability to activate the cytosolic NODs through recognition of MDP, a fragment of peptidoglycan (PGN). In addition, various bacterial by-products, e.g. Lipopolysaccharide (LPS), can also activate both the endothelium and macrophages. Further, from the oral cavity a state of local inflammation exists and immune cells are constantly releasing inflammatory mediators into the circulation, these mediators, IL-1 or TNF-α, can activate both the endothelium and macrophages. Finally, activated endothelium and macrophages have been shown to exacerbate Atherosclerosis when coupled with a HFD.
In addition, the role of TLRs has recently been advocated in periodontal disease, as evidenced by reduced bone loss in periodontal disease for TLR-2- and TLR-4-deficient mice (Costalonga, Batas, & Reich, 2009; Hou, Sasaki, & Stashenko, 2000). TLRs have also been implicated in the development of atherosclerosis based on findings that TLR-2-deficient animals are rendered less susceptible to P. gingivalis-associated atherogenesis, while application of a TLR-2 agonist, synthetic diacyl lipopeptide (FSL-1), produced similar levels of atherogenesis as P. gingivalis in wild-type TLR-2 mice (Madan & Amar, 2008). Recently, Hayashi et al. found that P. gingivalis-infected TLR-2-deficient mice exhibited lower levels of inflammatory mediators than infected mice possessing TLR-2 (Hayashi et al., 2010). This suggests that TLR-2 provides a mechanistic link between periodontal infection and arterial inflammation, the combination of which leads to a high incidence of atherosclerosis.
However, not all atherosclerosis can be explained by TLR-2 signaling (Hayashi, et al., 2010). Given that P. gingivalis is an invasive pathogen, Amar et al. evaluated the role of P. gingivalis invasion of endothelial cells has on atherosclerosis by hypothesizing that intracellular invasion of endothelial cells is required to elicit an immune response and the subsequent development of atherosclerosis (Amar, et al., 2009). Specifically, using an invasion-deficient strain of P. gingivalis DPG3 or an antibiotic Metronidazole, which prevents P. gingivalis invasiveness, Amar et al. demonstrated that either treatment ameliorated the additional atherosclerotic lesion induced by P. gingivalis infection (Amar, et al., 2009). This result suggests that endothelial invasion by P. gingivalis is required and that invasion-mediated inflammatory accounts for about half of the atherogenic process (Amar, et al., 2009).
We propose the following intergraded model of the relationship of chronic P. gingivalis infection and atherosclerosis; see Figure 1, in which repeated P. gingivalis bacteremia result in repeated endothelial/macrophage invasion leading to chronic inflammatory state and ultimately exacerbating atherosclerosis. Many potential mechanisms have been advanced in the attempt to explain the link between infection and atherosclerosis, including the modulation of lipid metabolism or infectious agents (Vercellotti, 1998). Chronic infection results in the chronic inflammation that leads to the production of pro-inflammatory cytokines which activate endothelial cells, leading to excessive induction of adhesion molecules, cytokines, growth factors and vasoconstrictors (Chi, et al., 2004).
Immune Response: Role of NOD in Infection-inflammation and Atherosclerosis
At a molecular level the finding that only invasive pathogens are sufficient to exacerbate atherosclerosis, demonstrated by Amar et al., implicates intracellular recognition molecules, e.g. NODs, as a critical drivers in the inflammatory process in both endothelial cells and macrophages (Amar, et al., 2009).
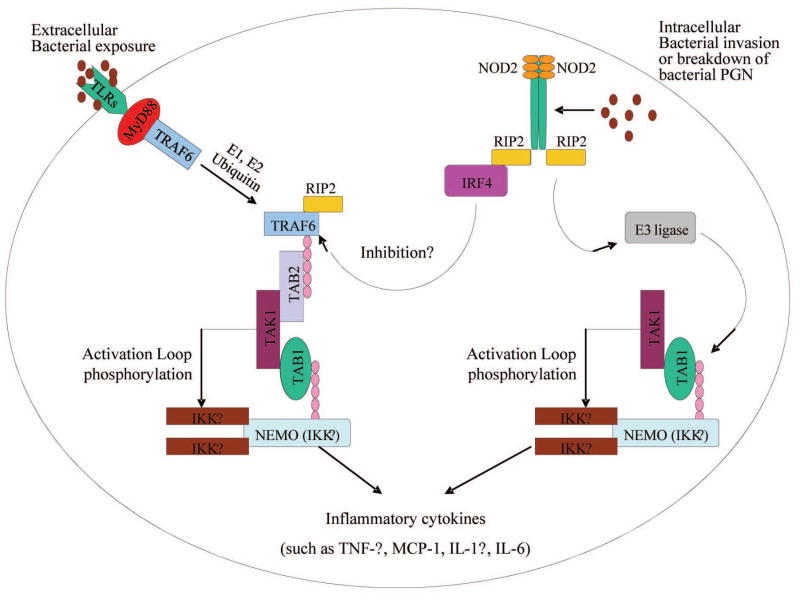
Mammals have two closely related NOD family members: NOD1 and NOD2, as shown in Figure 2. NOD1 appears to selectively recognize D-glutamyl-meso-diaminopimelic acid (iE-DAP) (Chamaillard et al., 2003; Girardin, Boneca, Carneiro, et al., 2003). NOD2 appears to selectively recognize MDP (Murray, 2005) and its expression is regulated by the pro-inflammatory cytokines TNF, IL-1β and Interferon-gamma (IFN-γ) in human endothelial cells and macrophages (H. Loppnow, Werdan, & Buerke, 2008). In addition, NOD2 has been implicated in bacterial recognition and is frequently mutated in people with familial forms of Crohn’s disease (Girardin et al., 2001; Hugot et al., 2001; N. Inohara, Ogura, Chen, Muto, & Nunez, 2001; Lesage et al., 2002; Ogura et al., 2001). However, despite similarities between NOD proteins and other pathogen-associated recognition proteins, there is little evidence that NOD proteins directly bind to pathogens or their products. This is still a point of active research.
Figure 2. A system of pathogen recognition - TLRs and nucleotide oligomerization domain-2 (NOD2) signaling pathways.
Two primary bacterial pathogen sensors involved in P. ginigivalis recognition are the extracellular TLRs and the intracellular nucleotide oligomerization domain-2 NOD2 receptors. TLRs bind to P. ginigvalis LPS and upon ligand binding recruit a number of adaptor molecules, e.g. TNF-α Receptor Associated Factor-6 (TRAF-6) and MyD88. This in turn ultimately triggers the poly ubiquitination, via E1 and E2 ubiquitination, of NF-κB Essential Modulator (NEMO), also known as Inhibitor of NF-κB kinase-γ (IKK-γ), which in turn activates IKK-α and IKK-β subunits. IKK-α and IKK-β then phosphorylates Inhibitor of NF-κB (IκB) and promotes its degradation via the proteasome thus freeing NF-κB. The intracellular NOD2 receptor is activated upon binding to fragments of PGN, MDP, which then recruits RIP2, a serine- threonine kinase. The NOD2/RIP2 complex undergoes oligomerization itself, which enables direct binding to NEMO (IKK-γ). NOD2/RIP2/NEMO complex can then recruit E3-Ligase and promote the polyubiquination of IKK-α and, via a similar mechanism as TLR signaling, activates NF-κB. Ultimately, both TLRs and NOD2 signaling converge and result in NF-κB translocating into the nucleus and increase transcription of pro-inflammatory cytokines (e.g. TNF-α, MCP-1, IL-1β, and IL-6).
Data generated using NOD2 deficient mice show that NOD2 is involved with the response to peptidoglycan, and specifically in IL-12 production, pointing to an unexpected role of NOD2 in regulating the response to bacterial products (Watanabe, Kitani, Murray, & Strober, 2004). Peptidoglycan is often considered to be a TLR-2 agonist, raising the question of how NOD2 and TLR-2 signaling are linked. It has been demonstrated that macrophages and dendritic cells from NOD2-deficient mice are impaired in the production of pro-inflammatory cytokines and nitric oxide following intracellular infection with live, virulent Mycobacterium tuberculosis (Jo, 2008). The peptidoglycan of M. tuberculosis stimulated the release of TNF-α and IL-12p40 in a partially NOD2-dependent manner and M. tuberculosis peptidoglycan required NOD2 for the optimal induction of TNF-α (Jo, 2008; Juarez et al., 2012). This evidence shows that like TLR-2, NOD2 plays an important role in triggering the inflammatory immune response to bacterial invasion.
Both NOD2 and TLR-2 are activated by the same bacterial products (peptidoglycan derivatives) (Girardin, Boneca, Viala, et al., 2003). Recently, the effect of NOD2 activation on TLR-2-mediated cytokine responses was found to be dependent on MDP activation dose. A biphasic role of NOD2 was demonstrated in which low ligand stimulation was synergistic to the inflammatory response while high ligand levels lead to a negative regulation of the inflammatory response, with all cells remaining viable even after prolonged culture (Borm, van Bodegraven, Mulder, Kraal, & Bouma, 2008). We tested recently this hypothesis and investigated the role of NOD2 signaling in atherosclerosis and periodontal bone loss using an Apolipoprotein E(−/−) (ApoE(−/−)) mouse model based on the proposed role of NOD2 in inflammation (Yuan et al., 2013). NOD2(−/−)ApoE(−/−) and ApoE(−/−) mice fed a standard chow diet were given an oral gavage of P. gingivalis for 15 weeks. NOD2(−/−)ApoE(−/−) mice exhibited significant increases in inflammatory cytokines, alveolar bone loss, cholesterol, and atherosclerotic lesions in the aorta and the heart compared with ApoE(−/−) mice. In contrast, ApoE(−/−) mice injected i.p. with MDP to stimulate NOD2 and given an oral gavage of P. gingivalis displayed a reduction of serum inflammatory cytokines, alveolar bone loss, cholesterol, and atherosclerotic lesions in the aorta and aortic sinus compared with ApoE(−/−) mice orally challenged but injected with saline. A reduction in body weight gain was observed in ApoE(−/−) mice fed a HFD and injected with MDP compared with ApoE(−/−) mice fed a HFD but injected with saline (Yuan, et al., 2013).
Role of NOD2 in P. gingivalis detection within the endothelium and its association with Atherosclerosis
More specifically, our data indicates a role of NOD2 in P. gingivalis infection. Our data, along with published reports (Y. G. Kim et al., 2008; Moreira & Zamboni, 2012; van Beelen et al., 2007), indicate that in macrophages and endothelial cells, NOD2 acts as an intracellular sensor for bacterial infection. Macrophages and endothelial cells regulate molecules important for leukocyte recruitment in response to a NOD2 ligand, implicating a link between this innate pattern recognition receptor and immunity. Finally, since vascular endothelial cells and macrophages are critical targets for bacterial molecules (such as MDP), NOD2 may play an important role in recognizing structural patterns of bacterial pathogens in the endothelium (Oh, et al., 2005). At present we can only speculate about the source or mechanism of cell entry of MDP or related muropeptides that activate NOD2. One source might be from phagocytosed bacteria, which have undergone degradation within a phagocytic vacuole. Macrophages contain intracellular hydrolases that digest peptidoglycan of intracellular and phagocytosed bacteria, generating MDP among other products (Johannsen, Wecke, Obal, & Krueger, 1991; Vermeulen & Gray, 1984). However, it is important to recall that more than two decades ago, studies of Martin et al. (Martin, Karnovsky, Krueger, Pappenheimer, & Biemann, 1984) provided evidence for accumulation of muropeptides, which could be derived only from endogenous peptidoglycan.
Moreover, despite appealing similarities between NOD proteins and other pathogen recognition proteins with leucine-rich repeat, there is little evidence that NOD proteins directly bind to pathogens or their products. However, it can be said that NOD2 and NOD1 modify the responses of cells to MDP and iE-DAP, respectively (Murray, 2005). The best chance of understanding NOD functions seems to lie in the dissection of the cellular responses to MDP and iE-DAP to discern how these intersect the many layers of TLR signaling. It has been reported that macrophages or mice made insensitive to TLRs by previous exposure to microbial ligands remained responsive to NOD1 and NOD2 stimulation (Y. G. Kim, et al., 2008). Furthermore, NOD1- and NOD2-mediated signaling and gene expression are enhanced in TLRs ligand-tolerant macrophages (Y. G. Kim, et al., 2008). Innate immune responses induced by bacterial infection were shown to rely on NOD1 and NOD2 and their adaptor serine–threonine kinase RICK: kinase) [also known as Rip2]. Rip-2 is expressed in macrophages pretreated with TLRs ligands, but not in naïve macrophages. Thus, NOD1 and NOD2 are important for microbial recognition and host defense after TLR stimulation (Y. G. Kim, et al., 2008) (Figure 2). Indeed, MDP treatment of bone marrow-derived macrophages incubated with P. gingivalis increased mRNA expressions of NOD2, TLR- 2, Myeloid differentiation primary response gene-88 (MyD88), and receptor-interacting protein (Rip)-2 but reduced the expressions of inhibitor of NF-κB kinase-β, NF-κB, c-Jun N-terminal kinase-3, and TNF-α protein levels compared to control, highlighting pathways involved in MDP anti-inflammatory effects. (Yuan, et al., 2013)
Overall, we suggest that as endothelial cells become homotolerized by constant and/or repetitive low-level exposures of P. gingivalis bacteremias, and subsequent TLR expression levels drop, thus muting TLRs signaling. However, since P. gingivalis is an invasive bacteria, pro-inflammatory cytokines are upregulated through NOD1/NOD2 activation, which regulates the expression of ICAMs and the MCP-1, two inflammatory mediators implicated in atherosclerosis. This increases the likelihood of monocyte chemoattraction to the media-intima vessel space thus increasing the number of macrophages in atheromas and their subsequent conversion to foam cells under HFD (Harald Loppnow, 2008).
The case for a significant role of NOD2 specifically in inflammatory pathways in atherosclerosis is supported by recent findings that atherosclerosis is characterized by significantly increased levels of NOD2 in macrophages and endothelial cells (Liu et al., 2013). In addition, NOD2 has linked with the production of cytokines implicated in vascular inflammation (H. Q. Liu et al., 2013). Further, Johansson et al. found that MDP stimulation increased vascular inflammation and exacerbated atherosclerosis, showing a direct connection between NOD ligands and atherosclerotic inflammation (Johansson et al., 2014). Collectively, these data warrant more studies to elucidate further the role of NOD proteins in atherosclerosis.
Discussion
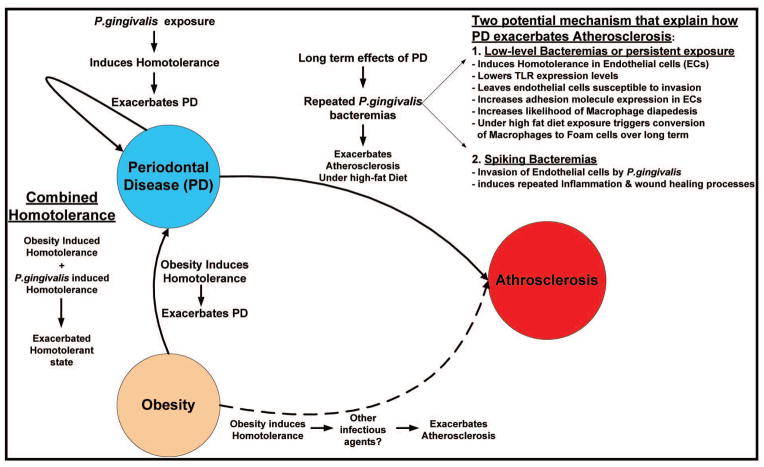
In this review we have strived to link exposure of P. gingivalis to exacerbations in periodontal disease through induction of homotolerance. Taken together, we propose an integrated model, (Figure 3), which links periodontal disease, obesity and atherosclerosis mechanistically focusing on the dysregulation in the innate immune system induced by homotolerance as a primary driver in both periodontal disease and atherosclerosis.
Figure 3. Proposed integrated model linking Periodontal Disease, Obesity, and Atherosclerosis.
We propose the following integrated model linking Periodontal Disease, Obesity and Atherosclerosis with a foundation built on a foundation of dysregulated innate immunity due to the induction of homotolerance. Homotolerance can be induced either by obesity directly or by exposure to P. gingivalis. However, when obesity is combined with P. gingivalis exposure, we speculated that exacerbates the overall homotolerant state thus having an additive effect and further exacerbating Periodontal Disease. We speculate two potential mechanisms that explain how the long-term consequence of periodontal disease exacerbates Atherosclerosis. First is the induction of homotolerance through a persistent low-level bacteremia or perhaps a transient low-level bacteremia induces a tolerant state within the endothelial cells and macrophages centered on regions of fatty-streaks/atheroma development. Specifically, this results in reduced expression of TLRs, which then leaves these cells susceptible to P. gingivalis invasion and increased adhesion receptor expression via nucleotide oligomerization domain-2 NOD2 receptor signaling. Increased adhesion receptor expression increases the likelihood of macrophages transiting from the blood compartment to the aterial intima. When coupled with a HFD macrophages will uptake cholesterol from Low-desnity lipoprotein via the scavenger receptor. Over time this has been shown to foster conversion of the macrophage to a ‘Foam’ cell and progression of Atherosclerosis. Secondly, there is a potential for a spiking bactermia during dental procedures or flossing that could actually overcome the homotolerance and result in a more traditional inflammatory response and wound healing processes which have been shown to exacerbate Atherosclerosis.
Homotolerance appears to be a mechanism designed to fine-tune the immune system to ignore a low-level stimulation of a pattern recognition receptor, certainly ideal in areas of the body with repeated exposure to such a pathogens, e.g. in the lung or colon specifically, where it can prevent repeated bouts of inflammation or perhaps even sepsis. However, in the oral cavity it appears P. gingivalis is able to take advantage of this mechanism by using it to tolerize resident and infiltrating leukocytes and effectively muting any immune response against it, thus exacerbating periodontal disease. Further understandings of the mechanisms that generate this homotolerant state are required to fully comprehend how this state is induced, what are its effects on the immune system, and what pathological conditions it affects. Findings by Muthukuru et al. showed that certain components of the innate oral mucosal immune response, most notably TLRs and inflammatory cytokines, may become tolerized during sustained exposure to bacterial structures such as LPS (Muthukuru, et al., 2005). This immune malfunction could possibly be caused by alterations of transcription factors or by epigenetic dysregulation or even by the induction of possible siRNAs to silence generated TLR mRNAs.
In addition, understanding how low-level stimulation induces tolerance while high-level stimulation does not would be critical in furthering our understanding of homotolerance. Specifically, an understanding of where the threshold exists such that too little stimulation induces tolerance versus too much stimulation induces inflammation is important. How does the cell make this decision? What is too much stimulation and what is too little stimulation? Answers to questions such as these would also be critical in our understanding of homotolerance.
Ultimately, these understandings can then be translated into better identification of rational therapeutic designs to better focus targets on key processes of disease progression. The implications are staggering when thinking of the prevalence of coronary heart disease in conjunction with our western diet. Further, treatments targeted to homotolerance would be more of a preventative measure instituted pre-clinically long before the overt debilitating and potentially fatal affects of coronary heart disease manifest itself in a patient. MDP activation of NOD2 could be the first candidate to be considered in the treatment of inflammatory processes affecting atherosclerosis, periodontal bone loss and possibly diet-induced weight gain.
Acknowledgments
This work is supported by grants from the National Institute of Heath # HL76801 and DE15989.
References
- Aderem A. Phagocytosis and the inflammatory response. J Infect Dis. 2003;187(Suppl 2):S340–345. doi: 10.1086/374747. [DOI] [PubMed] [Google Scholar]
- Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124(4):783–801. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Amabile N, Susini G, Pettenati-Soubayroux I, Bonello L, Gil JM, Arques S, Paganelli F. Severity of periodontal disease correlates to inflammatory systemic status and independently predicts the presence and angiographic extent of stable coronary artery disease. J Intern Med. 2008;263(6):644–652. doi: 10.1111/j.1365-2796.2007.01916.x. JIM1916 [pii] [DOI] [PubMed] [Google Scholar]
- Amar S, Gokce N, Morgan S, Loukideli M, Van Dyke TE, Vita JA. Periodontal disease is associated with brachial artery endothelial dysfunction and systemic inflammation. Arterioscler Thromb Vasc Biol. 2003;23(7):1245–1249. doi: 10.1161/01.ATV.0000078603.90302.4A. [DOI] [PubMed] [Google Scholar]
- Amar S, Wu SC, Madan M. Is Porphyromonas gingivalis cell invasion required for atherogenesis? Pharmacotherapeutic implications. J Immunol. 2009;182(3):1584–1592. doi: 10.4049/jimmunol.182.3.1584. 182/3/1584. [DOI] [PubMed] [Google Scholar]
- Aoki Y, Tabeta K, Murakami Y, Yoshimura F, Yamazaki K. Analysis of immunostimulatory activity of Porphyromonas gingivalis fimbriae conferred by Toll-like receptor 2. Biochem Biophys Res Commun. 2010;398(1):86–91. doi: 10.1016/j.bbrc.2010.06.040. S0006-291X(10)01150-2. [DOI] [PubMed] [Google Scholar]
- Arbes SJ, Jr, Slade GD, Beck JD. Association between extent of periodontal attachment loss and self-reported history of heart attack: an analysis of NHANES III data. J Dent Res. 1999;78(12):1777–1782. doi: 10.1177/00220345990780120301. [DOI] [PubMed] [Google Scholar]
- Areschoug T, Gordon S. Pattern recognition receptors and their role in innate immunity: focus on microbial protein ligands. Contrib Microbiol. 2008;15:45–60. doi: 10.1159/000135685. [pii] [DOI] [PubMed] [Google Scholar]
- Asai Y, Ohyama Y, Gen K, Ogawa T. Bacterial fimbriae and their peptides activate human gingival epithelial cells through Toll-like receptor 2. Infect Immun. 2001;69(12):7387–7395. doi: 10.1128/IAI.69.12.7387-7395.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahekar AA, Singh S, Saha S, Molnar J, Arora R. The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. Am Heart J. 2007;154(5):830–837. doi: 10.1016/j.ahj.2007.06.037. S0002-8703(07)00541-8 [pii] [DOI] [PubMed] [Google Scholar]
- Beutler B, Jiang Z, Georgel P, Crozat K, Croker B, Rutschmann S, Hoebe K. Genetic analysis of host resistance: Toll-like receptor signaling and immunity at large. Annu Rev Immunol. 2006;24:353–389. doi: 10.1146/annurev.immunol.24.021605.090552. [DOI] [PubMed] [Google Scholar]
- Biswas SK, Lopez-Collazo E. Endotoxin tolerance: new mechanisms, molecules and clinical significance. Trends Immunol. 2009;30(10):475–487. doi: 10.1016/j.it.2009.07.009. S1471-4906(09)00154-9 [pii] [DOI] [PubMed] [Google Scholar]
- Blake GJ, Ridker PM. Inflammatory bio-markers and cardiovascular risk prediction. J Intern Med. 2002;252(4):283–294. doi: 10.1046/j.1365-2796.2002.01019.x. 1019. [DOI] [PubMed] [Google Scholar]
- Borm ME, van Bodegraven AA, Mulder CJ, Kraal G, Bouma G. The effect of NOD2 activation on TLR2-mediated cytokine responses is dependent on activation dose and NOD2 genotype. Genes Immun. 2008;9(3):274–278. doi: 10.1038/gene.2008.9. [DOI] [PubMed] [Google Scholar]
- Burns E, Bachrach G, Shapira L, Nussbaum G. Cutting Edge: TLR2 is required for the innate response to Porphyromonas gingivalis: activation leads to bacterial persistence and TLR2 deficiency attenuates induced alveolar bone resorption. J Immunol. 2006;177(12):8296–8300. doi: 10.4049/jimmunol.177.12.8296. 177/12/8296. [DOI] [PubMed] [Google Scholar]
- Campus G, Salem A, Uzzau S, Baldoni E, Tonolo G. Diabetes and periodontal disease: a case-control study. J Periodontol. 2005;76(3):418–425. doi: 10.1902/jop.2005.76.3.418. [DOI] [PubMed] [Google Scholar]
- Cavrini F, Sambri V, Moter A, Servidio D, Marangoni A, Montebugnoli L, Cevenini R. Molecular detection of Treponema denticola and Porphyromonas gingivalis in carotid and aortic atheromatous plaques by FISH: report of two cases. J Med Microbiol. 2005;54(Pt 1):93–96. doi: 10.1099/jmm.0.45845-0. [DOI] [PubMed] [Google Scholar]
- Chamaillard M, Girardin SE, Viala J, Philpott DJ. Nods, Nalps and Naip: intracellular regulators of bacterial-induced inflammation. Cell Microbiol. 2003;5(9):581–592. doi: 10.1046/j.1462-5822.2003.00304.x. [DOI] [PubMed] [Google Scholar]
- Chamaillard M, Hashimoto M, Horie Y, Masumoto J, Qiu S, Saab L, Inohara N. An essential role for NOD1 in host recognition of bacterial peptidoglycan containing diaminopimelic acid. Nat Immunol. 2003;4(7):702–707. doi: 10.1038/ni945ni945. [DOI] [PubMed] [Google Scholar]
- Chi H, Messas E, Levine RA, Graves DT, Amar S. Interleukin-1 receptor signaling mediates atherosclerosis associated with bacterial exposure and/or a high-fat diet in a murine apolipoprotein E heterozygote model: pharmacotherapeutic implications. Circulation. 2004;110(12):1678–1685. doi: 10.1161/01.CIR.0000142085.39015.31. [DOI] [PubMed] [Google Scholar]
- Chiang CY, Kyritsis G, Graves DT, Amar S. Interleukin-1 and tumor necrosis factor activities partially account for calvarial bone resorption induced by local injection of lipopolysaccharide. Infect Immun. 1999;67(8):4231–4236. doi: 10.1128/iai.67.8.4231-4236.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. The immunopathogenesis of sepsis. Nature. 2002;420(6917):885–891. doi: 10.1038/nature01326. [DOI] [PubMed] [Google Scholar]
- Costalonga M, Batas L, Reich BJ. Effects of Toll-like receptor 4 on Porphyromonas gingivalis-induced bone loss in mice. J Periodontal Res. 2009;44(4):537–542. doi: 10.1111/j.1600-0765.2008.01152.x. JRE1152 [pii] [DOI] [PubMed] [Google Scholar]
- Cullinan MP, Hamlet SM, Westerman B, Palmer JE, Faddy MJ, Seymour GJ. Acquisition and loss of Porphyromonas gingivalis, Actinobacillus actinomycetemcomitans and Prevotella intermedia over a 5-year period: effect of a triclosan/copolymer dentifrice. J Clin Periodontol. 2003;30(6):532–541. doi: 10.1034/j.1600-051x.2003.00292.x. 292. [DOI] [PubMed] [Google Scholar]
- Dasanayake AP. C-reactive protein levels are elevated in patients with periodontitis and their CRP levels may go down after periodontal therapy. J Evid Based Dent Pract. 2009;9(1):21–22. doi: 10.1016/j.jebdp.2008.12.010. S1532-3382(08)00222-4 [pii] [DOI] [PubMed] [Google Scholar]
- Dasanayake AP, Boyd D, Madianos PN, Offenbacher S, Hills E. The association between Porphyromonas gingivalis-specific maternal serum IgG and low birth weight. J Periodontol. 2001;72(11):1491–1497. doi: 10.1902/jop.2001.72.11.1491. [DOI] [PubMed] [Google Scholar]
- Dasanayake AP, Russell S, Boyd D, Madianos PN, Forster T, Hill E. Preterm low birth weight and periodontal disease among African Americans. Dent Clin North Am. 2003;47(1):115–125. x–xi. doi: 10.1016/s0011-8532(02)00056-3. [DOI] [PubMed] [Google Scholar]
- den Dekker WK, Cheng C, Pasterkamp G, Duckers HJ. Toll like receptor 4 in atherosclerosis and plaque destabilization. Atherosclerosis. 2009 doi: 10.1016/j.atherosclerosis.2009.09.075. S0021-9150(09)00833-8 [pii] [DOI] [PubMed] [Google Scholar]
- Deshpande RG, Khan MB, Genco CA. Invasion of aortic and heart endothelial cells by Porphyromonas gingivalis. Infect Immun. 1998;66(11):5337–5343. doi: 10.1128/iai.66.11.5337-5343.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeStefano F, Anda RF, Kahn HS, Williamson DF, Russell CM. Dental disease and risk of coronary heart disease and mortality. Bmj. 1993;306(6879):688–691. doi: 10.1136/bmj.306.6879.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobrovolskaia MA, Medvedev AE, Thomas KE, Cuesta N, Toshchakov V, Ren T, Vogel SN. Induction of in vitro reprogramming by Toll-like receptor (TLR)2 and TLR4 agonists in murine macrophages: effects of TLR “homotolerance” versus “heterotolerance” on NF-kappa B signaling pathway components. J Immunol. 2003;170(1):508–519. doi: 10.4049/jimmunol.170.1.508. [DOI] [PubMed] [Google Scholar]
- Emingil G, Atilla G, Huseyinov A. Gingival crevicular fluid monocyte chemoattractant protein-1 and RANTES levels in patients with generalized aggressive periodontitis. J Clin Periodontol. 2004;31(10):829–834. doi: 10.1111/j.1600-051X.2004.00584.xCPE584. [DOI] [PubMed] [Google Scholar]
- Epstein SE. The multiple mechanisms by which infection may contribute to atherosclerosis development and course. Circ Res. 2002;90(1):2–4. [PubMed] [Google Scholar]
- Epstein SE, Zhou YF, Zhu J. Infection and atherosclerosis: emerging mechanistic paradigms. Circulation. 1999;100(4):e20–28. doi: 10.1161/01.cir.100.4.e20. [DOI] [PubMed] [Google Scholar]
- Foey AD, Crean S. Macrophage subset sensitivity to endotoxin tolerisation by Porphyromonas gingivalis. PLoS One. 2013;8(7):e67955. doi: 10.1371/journal.pone.0067955. PONE-D-13-13563 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geivelis M, Turner DW, Pederson ED, Lamberts BL. Measurements of interleukin-6 in gingival crevicular fluid from adults with destructive periodontal disease. J Periodontol. 1993;64(10):980–983. doi: 10.1902/jop.1993.64.10.980. [DOI] [PubMed] [Google Scholar]
- Gibson FC, 3rd, Hong C, Chou HH, Yumoto H, Chen J, Lien E, Genco CA. Innate immune recognition of invasive bacteria accelerates atherosclerosis in apolipoprotein E-deficient mice. Circulation. 2004;109(22):2801–2806. doi: 10.1161/01.CIR.0000129769.17895.F0. [DOI] [PubMed] [Google Scholar]
- Girardin SE, Boneca IG, Carneiro LA, Antignac A, Jehanno M, Viala J, Philpott DJ. Nod1 detects a unique muropeptide from gram-negative bacterial peptidoglycan. Science. 2003;300(5625):1584–1587. doi: 10.1126/science.1084677300/5625/1584. [DOI] [PubMed] [Google Scholar]
- Girardin SE, Boneca IG, Viala J, Chamaillard M, Labigne A, Thomas G, Sansonetti PJ. Nod2 is a general sensor of peptidoglycan through muramyl dipeptide (MDP) detection. J Biol Chem. 2003;278(11):8869–8872. doi: 10.1074/jbc.C200651200. [DOI] [PubMed] [Google Scholar]
- Girardin SE, Hugot JP, Sansonetti PJ. Lessons from Nod2 studies: towards a link between Crohn’s disease and bacterial sensing. Trends Immunol. 2003;24(12):652–658. doi: 10.1016/j.it.2003.10.007. [DOI] [PubMed] [Google Scholar]
- Girardin SE, Tournebize R, Mavris M, Page AL, Li X, Stark GR, Philpott DJ. CARD4/Nod1 mediates NF-kappaB and JNK activation by invasive Shigella flexneri. EMBO Rep. 2001;2(8):736–742. doi: 10.1093/embo-reports/kve155kve155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haraszthy VI, Zambon JJ, Trevisan M, Zeid M, Genco RJ. Identification of periodontal pathogens in atheromatous plaques. J Periodontol. 2000;71(10):1554–1560. doi: 10.1902/jop.2000.71.10.1554. [DOI] [PubMed] [Google Scholar]
- Hayashi C, Madrigal AG, Liu X, Ukai T, Goswami S, Gudino CV, Genco CA. Pathogen-mediated inflammatory atherosclerosis is mediated in part via Toll-like receptor 2-induced inflammatory responses. J Innate Immun. 2010;2(4):334–343. doi: 10.1159/000314686000314686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heitman J. Sexual reproduction and the evolution of microbial pathogens. Curr Biol. 2006;16(17):R711–725. doi: 10.1016/j.cub.2006.07.064. S0960-9822(06)01919-1 [pii] [DOI] [PubMed] [Google Scholar]
- Hirao K, Yumoto H, Takahashi K, Mukai K, Nakanishi T, Matsuo T. Roles of TLR2, TLR4, NOD2, and NOD1 in pulp fibroblasts. J Dent Res. 2009;88(8):762–767. doi: 10.1177/0022034509341779. [DOI] [PubMed] [Google Scholar]
- Hoge M, Amar S. Role of interleukin-1 in bacterial atherogenesis. Drugs Today (Barc) 2006;42(10):683–688. doi: 10.1358/dot.2006.42.10.1003543. [DOI] [PubMed] [Google Scholar]
- Hosokawa I, Hosokawa Y, Ozaki K, Yumoto H, Nakae H, Matsuo T. Proinflammatory effects of muramyldipeptide on human gingival fibroblasts. J Periodontal Res. 2010;45(2):193–199. doi: 10.1111/j.1600-0765.2009.01217.xJRE1217. [DOI] [PubMed] [Google Scholar]
- Hou L, Sasaki H, Stashenko P. Toll-like receptor 4-deficient mice have reduced bone destruction following mixed anaerobic infection. Infect Immun. 2000;68(8):4681–4687. doi: 10.1128/iai.68.8.4681-4687.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hugot JP, Chamaillard M, Zouali H, Lesage S, Cezard JP, Belaiche J, Thomas G. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn’s disease. Nature. 2001;411(6837):599–603. doi: 10.1038/35079107. [DOI] [PubMed] [Google Scholar]
- Inohara Chamaillard, McDonald C, Nunez G. NOD-LRR proteins: role in host-microbial interactions and inflammatory disease. Annu Rev Biochem. 2005;74:355–383. doi: 10.1146/annurev.biochem.74.082803.133347. [DOI] [PubMed] [Google Scholar]
- Inohara N, Ogura Y, Chen FF, Muto A, Nunez G. Human Nod1 confers responsiveness to bacterial lipopolysaccharides. J Biol Chem. 2001;276(4):2551–2554. doi: 10.1074/jbc.M009728200. [DOI] [PubMed] [Google Scholar]
- Jerala R. Structural biology of the LPS recognition. Int J Med Microbiol. 2007;297(5):353–363. doi: 10.1016/j.ijmm.2007.04.001. S1438-4221(07)00068-9 [pii] [DOI] [PubMed] [Google Scholar]
- Jo EK. Mycobacterial interaction with innate receptors: TLRs, C-type lectins, and NLRs. Curr Opin Infect Dis. 2008;21(3):279–286. doi: 10.1097/QCO.0b013e3282f88b5d00001432-200806000-00011. [DOI] [PubMed] [Google Scholar]
- Johannsen L, Wecke J, Obal F, Jr, Krueger JM. Macrophages produce somnogenic and pyrogenic muramyl peptides during digestion of staphylococci. Am J Physiol. 1991;260(1 Pt 2):R126–133. doi: 10.1152/ajpregu.1991.260.1.R126. [DOI] [PubMed] [Google Scholar]
- Johansson ME, Zhang XY, Edfeldt K, Lundberg AM, Levin MC, Boren J, Yan ZQ. Innate immune receptor NOD2 promotes vascular inflammation and formation of lipid-rich necrotic cores in hypercholesterolemic mice. Eur J Immunol. 2014 doi: 10.1002/eji.201444755. [DOI] [PubMed] [Google Scholar]
- Johnson JD, O’Connor KA, Deak T, Stark M, Watkins LR, Maier SF. Prior stressor exposure sensitizes LPS-induced cytokine production. Brain Behav Immun. 2002;16(4):461–476. doi: 10.1006/brbi.2001.0638. S0889159101906385. [DOI] [PubMed] [Google Scholar]
- Johnson LL, Sayles PC. Deficient humoral responses underlie susceptibility to Toxoplasma gondii in CD4-deficient mice. Infect Immun. 2002;70(1):185–191. doi: 10.1128/IAI.70.1.185-191.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshipura KJ, Rimm EB, Douglas CW, Trichopoulos D, Ascherio A, Willett WC. Poor oral health and coronary heart disease. Journal of Dental Research. 1996;75:1631–1636. doi: 10.1177/00220345960750090301. [DOI] [PubMed] [Google Scholar]
- Juarez E, Carranza C, Hernandez-Sanchez F, Leon-Contreras JC, Hernandez-Pando R, Escobedo D, Sada E. NOD2 enhances the innate response of alveolar macrophages to Mycobacterium tuberculosis in humans. Eur J Immunol. 2012;42(4):880–889. doi: 10.1002/eji.201142105. [DOI] [PubMed] [Google Scholar]
- Khlgatian M, Nassar H, Chou HH, Gibson FC, 3rd, Genco CA. Fimbria-dependent activation of cell adhesion molecule expression in Porphyromonas gingivalis-infected endothelial cells. Infect Immun. 2002;70(1):257–267. doi: 10.1128/IAI.70.1.257-267.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Amar S. Periodontal disease and systemic conditions: a bidirectional relationship. Odontology. 2006;94(1):10–21. doi: 10.1007/s10266-006-0060-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YG, Park JH, Shaw MH, Franchi L, Inohara N, Nunez G. The cytosolic sensors Nod1 and Nod2 are critical for bacterial recognition and host defense after exposure to Toll-like receptor ligands. Immunity. 2008;28(2):246–257. doi: 10.1016/j.immuni.2007.12.012. [DOI] [PubMed] [Google Scholar]
- Lesage S, Zouali H, Cezard JP, Colombel JF, Belaiche J, Almer S, Hugot JP. CARD15/NOD2 mutational analysis and genotype-phenotype correlation in 612 patients with inflammatory bowel disease. Am J Hum Genet. 2002;70(4):845–857. doi: 10.1086/339432. S0002-9297(07)60292-4 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu HQ, Zhang XY, Edfeldt K, Nijhuis MO, Idborg H, Back M, Yan ZQ. NOD2-mediated innate immune signaling regulates the eicosanoids in atherosclerosis. Arterioscler Thromb Vasc Biol. 2013;33(9):2193–2201. doi: 10.1161/ATVBAHA.113.301715. [DOI] [PubMed] [Google Scholar]
- Liu J, Wang Y, Ouyang X. Beyond toll-like receptors: Porphyromonas gingivalis induces IL-6, IL-8, and VCAM-1 expression through NOD-mediated NF-kappaB and ERK signaling pathways in periodontal fibroblasts. Inflammation. 2014;37(2):522–533. doi: 10.1007/s10753-013-9766-0. [DOI] [PubMed] [Google Scholar]
- Loppnow H. Intited review: Vascular cells control atherosclerosis by cytokine- and innate immunity-related inflammatory mechanisms. Innate Immunity. 2008;14(2):63–68. doi: 10.1177/1753425908091246. [DOI] [PubMed] [Google Scholar]
- Loppnow H, Werdan K, Buerke M. Vascular cells contribute to atherosclerosis by cytokine- and innate-immunity-related inflammatory mechanisms. Innate Immun. 2008;14(2):63–87. doi: 10.1177/1753425908091246. 14/2/63 [pii] [DOI] [PubMed] [Google Scholar]
- Madan M, Amar S. Toll-like receptor-2 mediates diet and/or pathogen associated atherosclerosis: proteomic findings. PLoS One. 2008;3(9):e3204. doi: 10.1371/journal.pone.0003204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmoudi M, Curzen N, Gallagher PJ. Atherogenesis: the role of inflammation and infection. Histopathology. 2007;50(5):535–546. doi: 10.1111/j.1365-2559.2006.02503.x. HIS2503 [pii] [DOI] [PubMed] [Google Scholar]
- Martin SA, Karnovsky ML, Krueger JM, Pappenheimer JR, Biemann K. Peptidoglycans as promoters of slow-wave sleep. I. Structure of the sleep-promoting factor isolated from human urine. J Biol Chem. 1984;259(20):12652–12658. [PubMed] [Google Scholar]
- Mattila KJ. Viral and bacterial infections in patients with acute myocardial infarction. J Intern Med. 1989;225(5):293–296. doi: 10.1111/j.1365-2796.1989.tb00084.x. [DOI] [PubMed] [Google Scholar]
- Mattila KJ. Dental infections as a risk factor for acute myocardial infarction. Eur Heart J. 1993;14(Suppl K):51–53. [PubMed] [Google Scholar]
- Mattila KJ, Valtonen VV, Nieminen M, Huttunen JK. Dental infection and the risk of new coronary events: prospective study of patients with documented coronary artery disease. PG - 588–92. Clin Infect Dis. 1995;20(3) doi: 10.1093/clinids/20.3.588. [DOI] [PubMed] [Google Scholar]
- Medzhitov R. Toll-like receptors and innate immunity. Nat Rev Immunol. 2001;1(2):135–145. doi: 10.1038/35100529. [DOI] [PubMed] [Google Scholar]
- Medzhitov R, Janeway C., Jr Innate immune recognition: mechanisms and pathways. Immunol Rev. 2000;173:89–97. doi: 10.1034/j.1600-065x.2000.917309.x. [DOI] [PubMed] [Google Scholar]
- Michalowicz BS, Diehl SR, Gunsolley JC, Sparks BS, Brooks CN, Koertge TE, Schenkein HA. Evidence of a substantial genetic basis for risk of adult periodontitis. J Periodontol. 2000;71(11):1699–1707. doi: 10.1902/jop.2000.71.11.1699. [DOI] [PubMed] [Google Scholar]
- Michelsen KS, Doherty TM, Shah PK, Arditi M. TLR signaling: an emerging bridge from innate immunity to atherogenesis. J Immunol. 2004;173(10):5901–5907. doi: 10.4049/jimmunol.173.10.5901. 173/10/5901. [DOI] [PubMed] [Google Scholar]
- Moreira LO, Zamboni DS. NOD1 and NOD2 Signaling in Infection and Inflammation. Front Immunol. 2012;3:328. doi: 10.3389/fimmu.2012.00328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray PJ. NOD proteins: an intracellular pathogen-recognition system or signal transduction modifiers? Curr Opin Immunol. 2005;17(4):352–358. doi: 10.1016/j.coi.2005.05.006. S0952-7915(05)00080-4 [pii] [DOI] [PubMed] [Google Scholar]
- Muthukuru M, Jotwani R, Cutler CW. Oral mucosal endotoxin tolerance induction in chronic periodontitis. Infect Immun. 2005;73(2):687–694. doi: 10.1128/IAI.73.2.687-694.2005. 73/2/687 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakajima T, Honda T, Domon H, Okui T, Kajita K, Ito H, Yamazaki K. Periodontitis-associated up-regulation of systemic inflammatory mediator level may increase the risk of coronary heart disease. J Periodontal Res. 2010;45(1):116–122. doi: 10.1111/j.1600-0765.2009.01209.xJRE1209. [DOI] [PubMed] [Google Scholar]
- Nery EB, Meister F, Jr, Ellinger RF, Eslami A, McNamara TJ. Prevalence of medical problems in periodontal patients obtained from three different populations. J Periodontol. 1987;58(8):564–568. doi: 10.1902/jop.1987.58.8.564. [DOI] [PubMed] [Google Scholar]
- Nishimura F, Taniguchi A, Yamaguchi-Morimoto M, Soga Y, Iwamoto Y, Kokeguchi S, Seino Y. Periodontal infection and dyslipidemia in type 2 diabetics: association with increased HMG-CoA reductase expression. Horm Metab Res. 2006;38(8):530–535. doi: 10.1055/s-2006-949525. [DOI] [PubMed] [Google Scholar]
- Njoroge T, Genco RJ, Sojar HT, Hamada N, Genco CA. A role for fimbriae in Porphyromonas gingivalis invasion of oral epithelial cells. Infect Immun. 1997;65(5):1980–1984. doi: 10.1128/iai.65.5.1980-1984.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogura Y, Bonen DK, Inohara N, Nicolae DL, Chen FF, Ramos R, Cho JH. A frameshift mutation in NOD2 associated with susceptibility to Crohn’s disease. Nature. 2001;411(6837):603–606. doi: 10.1038/35079114. [DOI] [PubMed] [Google Scholar]
- Oh HM, Lee HJ, Seo GS, Choi EY, Kweon SH, Chun CH, Jun CD. Induction and localization of NOD2 protein in human endothelial cells. Cell Immunol. 2005;237(1):37–44. doi: 10.1016/j.cellimm.2005.09.006. [DOI] [PubMed] [Google Scholar]
- Ohki T, Itabashi Y, Kohno T, Yoshizawa A, Nishikubo S, Watanabe S, Ishihara K. Detection of periodontal bacteria in thrombi of patients with acute myocardial infarction by polymerase chain reaction. Am Heart J. 2012;163(2):164–167. doi: 10.1016/j.ahj.2011.10.012. S0002-8703(11)00772-1. [DOI] [PubMed] [Google Scholar]
- Park JH, Kim YG, Shaw M, Kanneganti TD, Fujimoto Y, Fukase K, Nunez G. Nod1/RICK and TLR signaling regulate chemokine and antimicrobial innate immune responses in mesothelial cells. J Immunol. 2007;179(1):514–521. doi: 10.4049/jimmunol.179.1.514. 179/1/514. [DOI] [PubMed] [Google Scholar]
- Progulske-Fox A, Kozarov E, Dorn B, Dunn W, Jr, Burks J, Wu Y. Porphyromonas gingivalis virulence factors and invasion of cells of the cardiovascular system. J Periodontal Res. 1999;34(7):393–399. doi: 10.1111/j.1600-0765.1999.tb02272.x. [DOI] [PubMed] [Google Scholar]
- Pussinen PJ, Vilkuna-Rautiainen T, Alfthan G, Palosuo T, Jauhiainen M, Sundvall J, Asikainen S. Severe periodontitis enhances macrophage activation via increased serum lipopolysaccharide. Arterioscler Thromb Vasc Biol. 2004;24(11):2174–2180. doi: 10.1161/01.ATV.0000145979.82184.9f. [DOI] [PubMed] [Google Scholar]
- Raetz CR. Biochemistry of endotoxins. Annu Rev Biochem. 1990;59:129–170. doi: 10.1146/annurev.bi.59.070190.001021. [DOI] [PubMed] [Google Scholar]
- Rath SK, Mukherjee M, Kaushik R, Sen S, Kumar M. Periodontal pathogens in atheromatous plaque. Indian J Pathol Microbiol. 2014;57(2):259–264. doi: 10.4103/0377-4929.13470. IndianJPatholMicrobiol_2014_57_2_259_134704. [DOI] [PubMed] [Google Scholar]
- Ren L, Leung WK, Darveau RP, Jin L. The expression profile of lipopolysaccharide-binding protein, membrane-bound CD14, and toll-like receptors 2 and 4 in chronic periodontitis. J Periodontol. 2005;76(11):1950–1959. doi: 10.1902/jop.2005.76.11.1950. [DOI] [PubMed] [Google Scholar]
- Salvi GE, Brown CE, Fujihashi K, Kiyono H, Smith FW, Beck JD, Offenbacher S. Inflammatory mediators of the terminal dentition in adult and early onset periodontitis. J Periodontal Res. 1998;33(4):212–225. doi: 10.1111/j.1600-0765.1998.tb02193.x. [DOI] [PubMed] [Google Scholar]
- Salzberg TN, Overstreet BT, Rogers JD, Califano JV, Best AM, Schenkein HA. C-reactive protein levels in patients with aggressive periodontitis. J Periodontol. 2006;77(6):933–939. doi: 10.1902/jop.2006.050165. [DOI] [PubMed] [Google Scholar]
- Slots J, Genco RJ. Black-pigmented Bacteroides species, Capnocytophaga species, and Actinobacillus actinomycetemcomitans in human periodontal disease: virulence factors in colonization, survival, and tissue destruction. J Dent Res. 1984;63(3):412–421. doi: 10.1177/00220345840630031101. [DOI] [PubMed] [Google Scholar]
- Stroh T, Batra A, Glauben R, Fedke I, Erben U, Kroesen A, Siegmund B. Nucleotide oligomerization domains 1 and 2: regulation of expression and function in preadipocytes. J Immunol. 2008;181(5):3620–3627. doi: 10.4049/jimmunol.181.5.3620. 181/5/3620. [DOI] [PubMed] [Google Scholar]
- Sugawara Y, Uehara A, Fujimoto Y, Kusumoto S, Fukase K, Shibata K, Takada H. Toll-like receptors, NOD1, and NOD2 in oral epithelial cells. J Dent Res. 2006;85(6):524–529. doi: 10.1177/154405910608500609. 85/6/524. [DOI] [PubMed] [Google Scholar]
- Sun XJ, Meng HX, Shi D, Xu L, Zhang L, Chen ZB, Ren XY. Elevation of C-reactive protein and interleukin-6 in plasma of patients with aggressive periodontitis. J Periodontal Res. 2009;44(3):311–316. doi: 10.1111/j.1600-0765.2008.01131.x. JRE1131 [pii] [DOI] [PubMed] [Google Scholar]
- Tanabe SI, Grenier D. Macrophage tolerance response to Aggregatibacter actinomycetemcomitans lipopolysaccharide induces differential regulation of tumor necrosis factor-alpha, interleukin-1 beta and matrix metalloproteinase 9 secretion. J Periodontal Res. 2008;43(3):372–377. doi: 10.1111/j.1600-0765.2007.01049.x. JRE1049 [pii] [DOI] [PubMed] [Google Scholar]
- Tang K, Lin M, Wu Y, Yan F. Alterations of serum lipid and inflammatory cytokine profiles in patients with coronary heart disease and chronic periodontitis: a pilot study. J Int Med Res. 2011;39(1):238–248. doi: 10.1177/147323001103900126. [DOI] [PubMed] [Google Scholar]
- Tang L, Zhou XD, Wang Q, Zhang L, Wang Y, Li XY, Huang DM. Expression of TRAF6 and pro-inflammatory cytokines through activation of TLR2, TLR4, NOD1, and NOD2 in human periodontal ligament fibroblasts. Arch Oral Biol. 2011;56(10):1064–1072. doi: 10.1016/j.archoralbio.2011.02.020. S0003-9969(11)00068-9. [DOI] [PubMed] [Google Scholar]
- Tonetti MS, D’Aiuto F, Nibali L, Donald A, Storry C, Parkar M, Deanfield J. Treatment of periodontitis and endothelial function. N Engl J Med. 2007;356(9):911–920. doi: 10.1056/NEJMoa063186. [DOI] [PubMed] [Google Scholar]
- Tsai CC, Ho YP, Chen CC. Levels of interleukin-1 beta and interleukin-8 in gingival crevicular fluids in adult periodontitis. J Periodontol. 1995;66(10):852–859. doi: 10.1902/jop.1995.66.10.852. [DOI] [PubMed] [Google Scholar]
- Umino M, Nagao M. Systemic diseases in elderly dental patients. Int Dent J. 1993;43(3):213–218. [PubMed] [Google Scholar]
- van Beelen AJ, Zelinkova Z, Taanman-Kueter EW, Muller FJ, Hommes DW, Zaat SA, de Jong EC. Stimulation of the intracellular bacterial sensor NOD2 programs dendritic cells to promote interleukin-17 production in human memory T cells. Immunity. 2007;27(4):660–669. doi: 10.1016/j.immuni.2007.08.013. S1074-7613(07)00443-8 [pii] [DOI] [PubMed] [Google Scholar]
- Van Dyke TE, Sheilesh D. Risk factors for periodontitis. J Int Acad Periodontol. 2005;7(1):3–7. [PMC free article] [PubMed] [Google Scholar]
- Velsko IM, Chukkapalli SS, Rivera MF, Lee JY, Chen H, Zheng D, Kesavalu L. Active invasion of oral and aortic tissues by Porphyromonas gingivalis in mice causally links periodontitis and atherosclerosis. PLoS One. 2014;9(5):e97811. doi: 10.1371/journal.pone.0097811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vercellotti GM. Effects of viral activation of the vessel wall on inflammation and thrombosis. Blood Coagul Fibrinolysis. 1998;9(Suppl 2):S3–6. [PubMed] [Google Scholar]
- Vermeulen MW, Gray GR. Processing of Bacillus subtilis peptidoglycan by a mouse macrophage cell line. Infect Immun. 1984;46(2):476–483. doi: 10.1128/iai.46.2.476-483.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PL, Ohura K. Porphyromonas gingivalis lipopolysaccharide signaling in gingival fibroblasts-CD14 and Toll-like receptors. Crit Rev Oral Biol Med. 2002;13(2):132–142. doi: 10.1177/154411130201300204. [DOI] [PubMed] [Google Scholar]
- Watanabe T, Kitani A, Murray PJ, Strober W. NOD2 is a negative regulator of Toll-like receptor 2-mediated T helper type 1 responses. Nat Immunol. 2004;5(8):800–808. doi: 10.1038/ni1092. [DOI] [PubMed] [Google Scholar]
- Yavuzyilmaz E, Yamalik N, Bulut S, Ozen S, Ersoy F, Saatci U. The gingival crevicular fluid interleukin-1 beta and tumour necrosis factor-alpha levels in patients with rapidly progressive periodontitis. Aust Dent J. 1995;40(1):46–49. doi: 10.1111/j.1834-7819.1995.tb05614.x. [DOI] [PubMed] [Google Scholar]
- Yuan H, Zelka S, Burkatovskaya M, Gupte R, Leeman SE, Amar S. Pivotal role of NOD2 in inflammatory processes affecting atherosclerosis and periodontal bone loss. Proc Natl Acad Sci U S A. 2013;110(52):E5059–5068. doi: 10.1073/pnas.1320862110. 1320862110 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J, Quyyumi AA, Norman JE, Csako G, Epstein SE. Cytomegalovirus in the pathogenesis of atherosclerosis: the role of inflammation as reflected by elevated C-reactive protein levels. J Am Coll Cardiol. 1999;34(6):1738–1743. doi: 10.1016/s0735-1097(99)00410-6. S0735-1097(99)00410-6. [DOI] [PubMed] [Google Scholar]
- Zuany-Amorim C, Hastewell J, Walker C. Toll-like receptors as potential therapeutic targets for multiple diseases. Nat Rev Drug Discov. 2002;1(10):797–807. doi: 10.1038/nrd914. [DOI] [PubMed] [Google Scholar]