It is estimated that more than 2.1 million adolescents (10–19 years of age) live with human immunodeficiency virus (HIV) in low-income and middle-income countries.1 When compared with both adults and younger children, HIV-infected adolescents have higher rates of nonadherence, virologic failure, and death.2,3 As they age, adolescents generally increase their health care–related autonomy. Adolescents may attend a clinic with or without an adult caregiver (parent). The relationship between parental attendance at clinic visits and adolescent chronic disease outcomes is unknown. We hypothesized that routine clinic attendance without a parent would be associated with the risk of HIV treatment failure, particularly in younger adolescents.
Methods
Three hundred predominantly perinatally HIV-infected adolescents (10–19 years of age) receiving HIV treatment at the Botswana-Baylor Children’s Clinical Centre of Excellence were followed up at their quarterly clinic visits in a longitudinal adherence study beginning in 2012. Enrollment was stratified to include 50 adolescents with detectable viral loads (VLs) at entry, approximating the proportion of patients in the underlying population with detectable VLs. Human immunodeficiency virus RNA levels (VLs) were obtained at each visit. Institutional review board approval was obtained from the Botswana Health Research Development Committee, the University of Pennsylvania Institutional Review Board, and the Baylor College of Medicine Institutional Review Board. A parent or guardian was present at the study entry visit to consent to each adolescent’s participation. Written informed consent was obtained from the parents and written assent was obtained from the adolescents. After the initial visit, parents were present only if they would otherwise attend routine clinic visits. The relative risk of virologic failure (VL ≥ 400 copies/mL) at 3 months or 6 months of follow-up was calculated for adolescents with and without a parent present at the 3-month study visit. Multivariable logistic regression was used to assess for confounding by age, sex, time receiving treatment, and orphan status. Linear regression was used to evaluate the likelihood of virologic failure with increasing age for those with and without a parent present.
Results
For the 300 enrolled participants, the median age was 13.4 years (interquartile range, 11.8–15.6 years) with a median time of receiving HIV treatment of 7.5 years (interquartile range, 5.3–8.8 years). Of the participants, 158 were female (52.7%). There were 85 maternal orphans (28.3%), 70 paternal orphans (23.3%), and 50 double orphans (16.7%). Two hundred thirty-eight participants (79%) were World Health Organization clinical stage 3 or 4 (advanced or severe disease) at the treatment baseline and 199 participants (66%) had advanced or severe immunologic suppression. However, at study entry, 267 participants (89%) had been asymptomatic for at least 6 months. The Table shows the number (percentage) of patients with and without a parent present at 3 months and 6 months of follow-up who had a detectable HIV VL. One participant was excluded because he ran away from home and did not come to the 3-month and 6-month study visits.
Table.
HIV VLs and Missing Parents for 299 Adolescents
| Variable | Parent, No. (%) | P Value for χ2a | |
|---|---|---|---|
| Present | Absent | ||
| VLs detectable at month 3 | |||
| Yes | 10 (5.0) | 22 (21.8) | |
| No | 152 (76.8) | 58 (57.4) | <.001 |
| Missing | 36 (18.2) | 21 (20.8) | |
| VLs detectable at month 3 or month 6 | |||
| Yes | 12 (7.6) | 36 (25.5) | |
| No | 141 (89.2) | 105 (74.5) | <.001 |
| Missing | 5 (3.2) | 0 | |
Abbreviation: HIV, human immunodeficiency virus; VLs, viral loads.
Based on the comparison between virologic failure (missing values excluded) in the groups with and without a parent present at the specified visit times.
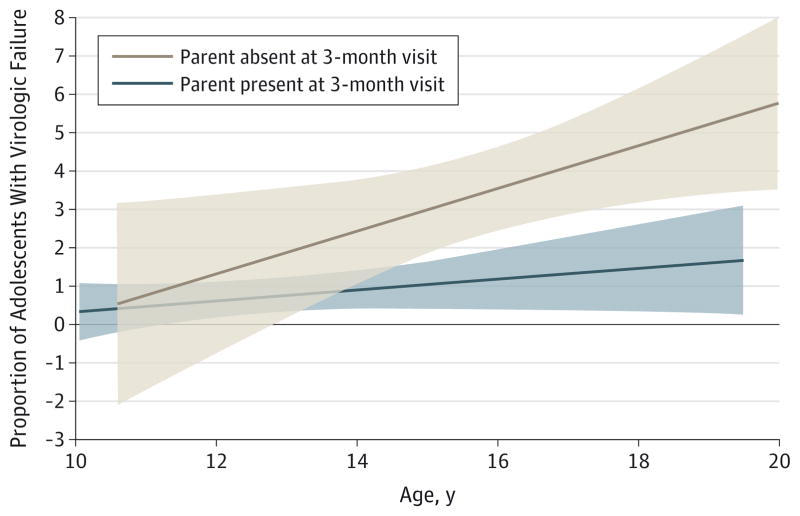
The odds of failure at the 3-month visit if a parent was not present were 4.5 (95% CI, 1.5–4.1) compared with those with a parent present at 3 months. There was no confounding by sex, time receiving treatment, or orphan status. Controlling for age decreased the odds of virologic failure from 4.5 to 3.6 (95% CI, 1.5–8.4) for those without vs with a parent present at 3 months. The Figure illustrates the difference in proportion of patients with virologic failure by age stratified by the presence/absence of a parent in the clinic at the 3-month visit.
Figure.
Proportion of Patients With Virologic Failure by Age Stratified by Parental Absence
The shaded areas indicate 95% CI bands.
Discussion
Absence of a parent from an adolescent’s clinic visit was strongly associated with HIV virologic failure. These results suggest that interventions to identify potentially supportive caregivers and strengthen adolescent/parent dyads might lower adolescents’ risk of treatment failure. In settings where psychosocial support resources are limited, targeting adolescents who attend clinics alone might help the most vulnerable youth with HIV and other chronic diseases.
Acknowledgments
Funding/Support: Dr Lowenthal is supported through career development award K23 MH095669 from the National Institute of Mental Health. Dr Gross receives support from grant P30 A1 045008 from the Penn Center for AIDS Research.
Footnotes
Conflict of Interest Disclosures: None reported.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We thank the adolescents and families at the Botswana-Baylor Children’s Clinical Centre of Excellence who shared their experiences as part of the adolescent Ba Nana Adherence Study as well as the Botswana-Baylor staff and, in particular, the Ba Nana Adherence Study staff.
Author Contributions: Dr Lowenthal and Ms Chapman had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Lowenthal, Nachega, Gross.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Lowenthal, Marukutira.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Lowenthal, Nachega, Gross.
Obtained funding: Lowenthal.
Administrative, technical, or material support: Tshume, Anabwani, Gross.
Study supervision: Lowenthal, Marukutira, Chapman.
References
- 1.Joint United Nations Programme on HIV/AIDS. Report on the Global AIDS Epidemic. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 2.Lowenthal ED, Bakeera-Kitaka S, Marukutira T, Chapman J, Goldrath K, Ferrand RA. Perinatally acquired HIV infection in adolescents from sub-Saharan Africa: a review of emerging challenges. Lancet Infect Dis. 2014;14(7):627–639. doi: 10.1016/S1473-3099(13)70363-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Health for the World’s Adolescents: A Second Chance in the Second Decade. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]