Abstract
Purpose
Research on older children and high resource families demonstrates that maternal improvement in depression often leads to parallel changes in parenting and child adjustment. It is unclear if this association extends to younger children and low income mothers. This study examined if In-Home Cognitive Behavioral Therapy (IH-CBT), a treatment for depressed mothers participating in home visiting programs, contributes to improvements in parenting and child adjustment.
Methods
Ninety-three depressed mothers in home visiting between 2–10 months postpartum were randomly assigned to IH-CBT (n=47) plus home visiting or standard home visiting (SHV; n = 46). Mothers were identified via screening and subsequent of MDD diagnosis. Measures of depression, parenting stress, nurturing parenting, and child adjustment were administered at pre-treatment, post-treatment, and three month follow-up.
Results
Results indicated that there were no differences between IH-CBT and controls on parenting and child adjustment. Low levels of depression were associated with decreased parenting stress and increased nurturing parenting. There was no association between maternal depression and child adjustment.
Conclusions
Improvement in depression was related to changes in parenting in low income mothers participating in home visiting programs. IH-CBT was not independently associated with these improvements, although to the extent that treatment facilitated improvement there were corresponding benefits to parenting. Child adjustment was not associated with maternal depression, a finding possibly attributed to the benefits of concurrent home visiting or measurement limitations. Future research should focus on longer term follow-up, implications of relapse, and child adjustment in later years.
Keywords: depression, cognitive behavioral therapy, low income, home visiting
Depression in mothers is a major public health problem (Wisner et al. 2006). Mayberry et al. (2007) documented the persistence of depression over the first two years postpartum with between 16.1–23.1% displaying elevated symptoms on the Edinburgh Postnatal Depression Scale (Cox et al. 1987) at each of four time points. Campbell et al. (2007) found that 54.4% of mothers had trajectories reflecting moderate to high levels of depression over the first seven years of their children’s lives. Research has found that maternal depression undermines effective and nurturing parenting. Depressed mothers are less sensitive to child cues, inadequately attend to child physical and emotional needs, have fewer and more negative interactions with their children, and have negative and distorted views of children and parenting (Field 2010). Children raised by depressed mothers are at high risk for depression, insecure attachment, and emotional and behavioral dysregulation (Goodman et al. 2011).
Given the impairments emanating from maternal depression, there is considerable interest in understanding if symptom improvement facilitates emergence of more positive parenting practices and healthy child development. Research has shown that maternal recovery from depression has a positive impact on parenting and children (Logsdon et al. 2011). In their review of the literature, Gunlicks and Weissman (2008) summarized that “there is consistent evidence that reduction or remission of parental symptoms was related to reduction in child symptoms and that these effects were maintained” (p. 387). Yet, limitations in the literature and conflicting findings render the relationship between improvement or recovery and parenting and child outcomes unresolved. Much of the literature on the benefits of symptom improvement involves older children and mothers from higher SES backgrounds. It is unclear if such improvements occur in younger children, especially infants who are particularly vulnerable to the negative effects of having a depressed mother (Bagner et al. 2010). Likewise, little is known about the impact of symptom improvement in the context of poverty. Improvement in depression may have limited positive impacts against the backdrop of continual financial stressors and hardship. Furthermore, some studies (Seifer et al. 2001) have found that depressed mothers continue to display parenting deficits between episodes of major depression despite improvements in mood. For mothers who are first-time parents and inexperienced in the parenting role, improvement in depression may not lead to changes in parenting skills given that these were undeveloped prior to the episode.
Mothers participating in home visiting are an important population in which to examine depression and the impact of symptom improvement. Home visiting is a voluntary early prevention program for mothers and children designed to optimize child outcomes and prevent child abuse and neglect. There is increasing interest in home visiting models that target demographically at risk mothers, seek to enroll mothers during pregnancy or shortly after birth, and provide frequent services over the first years of the child’s life (Adirim and Supplee 2013). Acquiring nurturing parenting skills is a primary focus of home visiting. Mothers participating in home visiting have many of the risk factors for depression, including low income, young age, educational underachievement, and history of childhood trauma. Many in home visiting are first-time mothers and are inexperienced in the parenting role. Numerous studies have documented rates of depression among mothers in home visiting of up to 59% (Ammerman et al. 2010). In addition, depression mitigates the positive effects of program participation (McFarlane et al. 2013). Easterbrooks et al. (2013) found that depressed mothers failed to receive the benefits of lowered rates of abuse and neglect relative to their non-depressed counterparts. An effective intervention for perinatal depression in this population holds potential to enhance the lives of low income mothers and children, improve developmental outcomes, and protect the sizable investment made in home visiting programs.
Ammerman et al. (2011) systematically adapted cognitive behavioral therapy to address the needs of depressed mothers enrolled home visiting. In-Home Cognitive Behavioral Therapy (IH-CBT) is implemented by therapists who provide treatment concurrently with ongoing home visiting. IH-CBT uses strategies that promote engagement, make content relevant to the needs of mothers in home visiting, facilitate delivery in the home, and explicitly foster a collaborative relationship between the therapist and home visitor in order to smoothly coordinate services. Empirical support for IH-CBT in treating maternal depression was obtained in a clinical trial comparing mothers who received IH-CBT and concurrent home visiting with those who received home visiting alone (Ammerman et al. 2013a; Ammerman et al. 2013b). In this study, 93 mothers participating in home visiting were first identified using a screen administered at three months postpartum. This was followed by diagnosis of Major Depressive Disorder (MDD) using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; (Spitzer et al. 1992). Following random assignment to treatment and control groups, mothers were re-assessed at post-treatment and at three month follow-up. Results indicated that mothers receiving IH-CBT experienced significant benefits in terms of depression relative to controls. Compared to those receiving home visiting alone, mothers in the IH-CBT condition were less likely to meet diagnostic criteria for MDD at post-treatment (70.7% vs. 30.2%), reported fewer depressive symptoms, and obtained lower scores on clinician ratings of depression severity. Effect sizes for these indices of depression were sizable, ranging from 0.75–0.90 at post-treatment and 0.55–0.60 at follow-up. Additional improvements were noted in social support and psychological distress. Gains were maintained through three month follow-up. While these findings demonstrate the benefits of treatment to mood and social functioning, it is unclear if there were corresponding impacts on parenting and child adjustment or how changes in depression related to these outcomes.
The purpose of this study was to examine the impact of changes in depression on parenting and child adjustment in mothers in home visiting. In the first step, we examined the efficacy of IH-CBT in improving parenting and child adjustment. Specifically, new mothers enrolled in a community-based home visiting program were identified using a two-stage process comprised of a screen and subsequent confirmation of MDD diagnosis. Mothers were 16 years of age or older and were identified at three months postpartum. They were randomly assigned to IH-CBT + home visiting or standard home visiting (in which mothers were permitted to obtain treatment in the community). Measures of parenting and child adjustment were administered at pre-treatment, post-treatment, and three month follow-up. We posited that IH-CBT and concurrent home visiting would impart benefits to depressed mothers and their children in terms of improved parenting and child adjustment. In the second step, we combined the two groups and examined the association between maternal depression and indices of parenting and child adjustment while controlling for demographic and clinical covariates. It was hypothesized that maternal depression would be related to negatively related to parenting and parenting and child adjustment across time.
Method
Sample
Subjects were 93 new mothers aged 16 or older who participated in a home visiting program and were diagnosed with Major Depressive Disorder (MDD) using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). Mothers were enrolled in Every Child Succeeds, a community-based home visiting program serving Southwestern Ohio and Northern Kentucky (USA). Two models of home visiting were used in the program: Nurse-Family Partnership (NFP; Olds 2010) and Healthy Families America (HFA; Holton and Harding 2007). Eligibility for the home visiting program required at least one of the following maternal demographic risk characteristics: unmarried, low income, ≤18 years of age, inadequate prenatal care. Mothers were enrolled in home visiting prior to 28 weeks gestation in NFP as per model parameters and from 20 weeks gestation through the child reaching three months of age for HFA. Mothers were referred from prenatal clinics, hospitals, social service agencies, and community physicians. In the NFP home visits were provided by nurses, while in HFA home visits were provided by social workers, related professionals and paraprofessionals. The goals of the home visiting program were to (1) improve pregnancy outcomes through nutrition education and substance use reduction; (2) support parents in providing children with a safe, nurturing, and stimulating home environment; (3) optimize child health and development; (4) link families to healthcare and other needed services; and (5) promote economic self-sufficiency.
Design and procedure
A randomized clinical trial design was used with assessments at pre-treatment, post-treatment, and three month follow-up. Participants were randomized to In Home-Cognitive Behavioral Therapy (IH-CBT + home visiting) or standard home visiting (SHV; home visiting alone) groups following the pre-treatment assessment. Randomization was stratified by race and home visiting model (HFA, NFP). Within the IH-CBT group a further randomization was done to assign individuals to therapists (n=2). The randomization schedule was prepared prior to the start of the study and assignments were placed in separate envelopes that were opened sequentially.
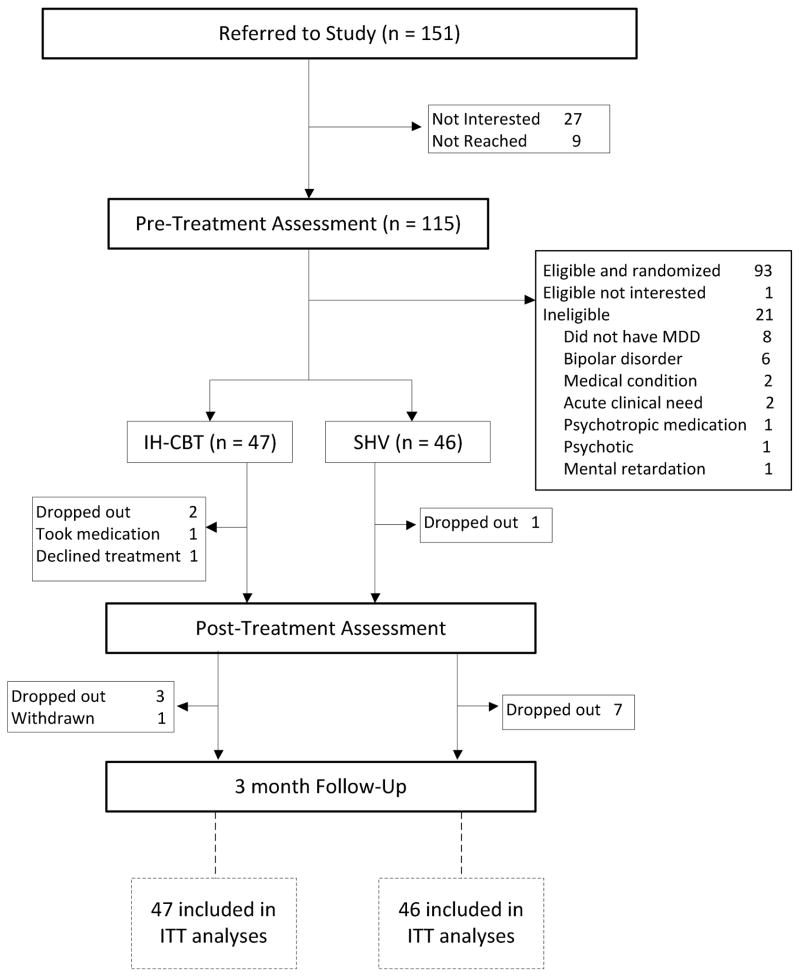
Figure 1 shows the Consort diagram through the study starting at referral. Of the 151 referred mothers (who were referred by 48 home visitors), 115 subsequently received a pre-treatment assessment. Twenty-seven referred mothers were not interested in participating, and 9 were unable to be reached. There were no differences between assessed and non-assessed participants on mother age, mother race, household income, baby age, or home visiting model (all p > .05). Ninety-four of 115 participants were found to be eligible. Reasons for ineligibility were not having MDD, having bipolar disorder, medical condition contributing to psychiatric presentation, acute clinical need, taking psychotropic medication, psychotic, and mental retardation. One mother was disinterested in participating following the assessment but prior to randomization. The remaining 93 mothers were randomized to IH-CBT (n=47) or SHV (n=46) and comprised the intent to treat sample. Between pre-treatment and post-treatment assessments, 1 mother in IH-CBT started medication following the 1st treatment session and another declined treatment after randomization. Thirteen mothers dropped out of the study between pre-treatment and follow-up. There were no differences in dropout rate between conditions, and dropout was unrelated to initial MDD severity, recurrent vs. single episode MDD, or psychiatric comorbidity (p > .05). Overall, 93.5% of participants received at least one of the post-treatment and follow-up assessments.
Figure 1.
Flow of participants through study. Randomization was stratified by race, home visiting model, and therapist.
In Home-Cognitive Behavioral Therapy
Mothers in the IH-CBT condition received IH-CBT + home visiting (see SHV condition for description). IH-CBT was delivered in the home by two licensed master’s level social workers. Treatment consisted of 15 sessions that were scheduled weekly and lasted 60 minutes plus a booster session one month post-treatment. The focus and content of treatment followed the directives of CBT (Beck 2011). The primary focus of treatment was depression reduction (parenting skills and child functioning were not directly targeted in the treatment, although these were addressed in home visiting). Adaptations to CBT were made to address setting, population, and context in order to maximize engagement and outcomes. First, IH-CBT was delivered in the home. The second adaptation involved addressing the primary concerns of young, low income, new mothers who were socially isolated (Levy and O’Hara 2010). The third adaptation sought to facilitate close collaboration with home visitors. Collaboration occurred through regular communication and the home visitor attending the 15th session.
Standard Home Visiting
In standard home visiting (SHV), mothers received services from home visitors as per the HFA and NFP model directives. Both models call for regular home visits during the intervals covered during the trial, and home visitors are given discretion to increase frequency of visits if needed. Curricula for both models are distinct but emphasize child health and development, nurturing mother-child relationship, maternal health and self-sufficiency, and linkage to other community services. Consistent with standard of care, mothers in the SHV condition were permitted to receive treatment for depression in the community.
Measures
Edinburgh Postnatal Depression Scale
The Edinburgh Postnatal Depression Scale (EPDS; Cox et al. 1987) is a 10 item self-report measure of depressive symptoms. Items consist of depressive symptoms that are endorsed on a four point scale indicating occurrence and severity over the past week, yielding a total score. The EPDS was used to screen mothers for eligibility using a cutoff of ≥11.
Structured Clinical Interview for DSM-IV Axis I Disorders
The Structured Clinical Interview for DSM-IV (SCID-I, January 2007 version; Spitzer et al. 1992) is a semi-structured psychiatric interview that is widely used in research and clinical practice. Interviews were audio-recorded and 25% were rated by a second rater yielding a kappa coefficient = .89. The full SCID was administered at pre-treatment to determine MDD diagnosis.
Hamilton Depression Rating Scale
The first 17 items of the Hamilton Depression Rating Scale (HDRS; Hamilton 1960) were used as part of the psychiatric interview. The HDRS is clinician rated and consists of depressive symptoms which are recorded using 5- or 3-point scales reflecting presence and severity over the past week. Interviews were audio-recorded and 25% were rated by a second rater yielding an intraclass correlation coefficient of .93. The HDRS was administered at pre-treatment and by independent evaluators at post-treatment and follow-up.
Parenting Stress Index-Short-Form
The Parenting Stress Index-Short-Form (PSI-SF; Abidin 1995) is a 36-item parent report measure of child and parent functioning/coping. This widely used measure yields a standardized score for Total Stress and scale scores for Parental Distress, Parent-Child Dysfunctional Interaction, and Difficult Child. The PSI-SF has excellent psychometric properties and is widely used in research.
HOME Inventory
The HOME Inventory (HOME; Caldwell and Bradley 1984) is a standardized observational measure of features in the home consistent with a stimulating, nurturing, and safe environment. In addition to a Total Score, scores are derived for Responsivity, Acceptance, Organization, Learning Materials, Involvement, and Variety. Internal (α = .84) and test-retest (r = .62–.74) reliabilities are strong (Bradley et al. 2001).
Ages and Stages Questionnaire: Social-Emotional
The Ages and Stages Questionnaire: Social-Emotional (ASQ:SE; Squires et al. 2002) is a measure of social and emotional adaptive functioning in children aged 6–60 months. There are 8 versions reflecting 6 month intervals between 6–60 months of age, and number and content of items changes across versions to reflect developmental relevance. Items are organized around seven domains of social and emotional development: self-regulation, compliance, communication, adaptive functioning, autonomy, affect, and interaction with people. A total standardized score is derived reflecting overall social and emotional functioning with a high score indicating greater maladjustment. In this study, the 6 and 12 month versions of the ASQ: SE were used. Scores from each version are not comparable, so we used the normative sample to transform the value into Z-scores by subtracting the group mean from the value and dividing it with the group standard deviation.
Procedures and the consent form were approved by the Institutional Review Board of Cincinnati Children’s Hospital Medical Center. The study is registered with ClinicalTrials.gov (Identifier: NCT01221701, http://www.clinicaltrials.gov/ct2/show/NCT01221701).
Results
Overview of analytic strategy
We first examined the difference between the treatment (IH-CBT) and control (SHV) groups across the three time points on the PSI-SF total, HOME total and ASQ:SE. The purpose of this analysis was to determine if our depression-focused treatment had an impact on parenting and child outcomes. A mixed effect regression model was fitted where the outcomes were modeled as a function of group assignment (IH-CBT or SHV), time (pre-treatment, post-treatment and follow-up) and the interaction between group and time. Reported p-values for the main analysis were adjusted using a false discovery rate (FDR) methodology that determines the expected proportion of false positives among the declared significant results (Benjamini and Hochberg 2000). This was followed by investigating the relationship between scores on the Hamilton Depression Rating Scale (HDRS) and PSI-SF, HOME and ASQ:SE. The primary analysis used a linear mixed effect regression model with restricted maximum likelihood estimation. This approach accounts for missing data and permits examination of depression and its relation to parenting and child adjustment across time. The basic model includes terms for HDRS, time, and the interaction between the HDRS and time. Different correlation structures for the repeated measurements were explored and compared using a goodness of fit test. In addition we divided the data on the level of the interaction variables and report the corresponding regression coefficients for each time point separately. The following covariates were tested in the model and found not to be significant: condition, mother’s age, mother’s race, marital status, family income, psychiatric comorbidity, home visit model, therapist, and intensity of home visits. As a result, these are not shown in the tables.
Sample characteristics
Table 1 shows the demographics of the two groups. No differences were found between treatment and control groups on these variables. There were no differences between groups on the risk variables (unmarried, low income, ≤18 years, inadequate prenatal care) used to determine eligibility for the home visiting program. In terms of home visitation model, 81 mothers were in the HFA model and 12 in the NFP model. Eighty-five mothers were primiparous and 8 had more than one child (all of these were in the HFA model). Mothers received a mean of 13.9 (SD= 9.2) home visits prior to assessment. No differences were found on one vs. multiple children or number of home visits received (p > .05). Groups were equivalent on home visitor training and education.
Table 1.
Demographic characteristics of IH-CBT (n=47) and SHV (n=46) participants
| Variable | IH-CBT Condition | SHV Condition | t or x2 | p-value |
|---|---|---|---|---|
| M (SD) or N (%) | M (SD) or N (%) | |||
| Mother age (years) | 22.4 (5.2) | 21.5 (3.9) | 0.9 | ns |
| Mother Race | ||||
| White | 30 (63.8%) | 28 (60.8%) | 1.2 | ns |
| African American | 14 (29.9%) | 16 (34.8%) | ||
| Native American | 1 (2.1%) | 0 (0.0%) | ||
| Native Hawaiian or other Pacific Islander | 1 (2.1%) | 1 (2.2%) | ||
| Bi-racial | 1 (2.1%) | 1 (2.2%) | ||
| Mother Ethnicity | ||||
| Latina | 3 (6.4%) | 4 (8.7%) | 0.5 | ns |
| None | 44 (93.6%) | 42 (91.3%) | ||
| Marital Status | ||||
| Single, Never Married | 41 (87.2%) | 39 (84.8%) | 1.0 | ns |
| Married | 6 (12.8%) | 6 (13.0%) | ||
| Separated | 0 (0.0%) | 1 (2.2%) | ||
| Education (years) | 11.6 (2.0) | 11.3 (1.7) | 1.0 | ns |
| Income | ||||
| US$0–9, 999 | 27 (58.7%) | 25 (54.3%) | 7.5 | ns |
| US$10, 000–19,999 | 6 (13.0%) | 13 (28.3%) | ||
| US$20, 000–29, 999 | 10 (21.7%) | 5 (10.9%) | ||
| US$30, 000–39, 999 | 2 (4.3%) | 1 (2.2%) | ||
| US$40, 000–49, 999 | 0 (0.0%) | 2 (4.3%) | ||
| >US$50, 000 | 1 (2.2%) | 1 (2.2%) | ||
| Child’s age (days) | 159.8 (73.7) | 146.1 (74.4) | 0.9 | ns |
Group comparisons
Table 2 presents the means and standard deviations for both groups (IH-CBT and SHV) at each time point (pre-assessment, post-assessment, and follow-up) for the PSI-SF, HOME, and ASQ:SE. F-values are shown reflecting group by time interactions and effect size (d) are presented for group comparisons at each time point. Results show no group differences over time for these measures. Effect sizes at each assessment point revealed no differences although the comparison between IH-CBT and SHV groups on the HOME approached but did not reach statistical significance (p = .053). As a result, groups were combined for subsequent analyses examining maternal depression and parenting and child measures over time.
Table 2.
Comparisons between IH-CBT (N=47) and SHV (N=46) groups on parenting and child measures at each time point
| Measure | Assessment | Group | d | F (Group x Time) | |||
|---|---|---|---|---|---|---|---|
| IH-CBT | SHV | ||||||
| Mean | SD | Mean | SD | ||||
| PSI-SF | Pre | 83.49 | 18.93 | 87.31 | 20.07 | 0.20 | 1.57 |
| Post | 73.34 | 23.65 | 79.56 | 18.47 | 0.29 | ||
| Follow-up | 64.58 | 31.00 | 75.92 | 27.27 | 0.39 | ||
| HOME | Pre | 31.36 | 5.75 | 31.32 | 6.41 | −0.01 | 0.98 |
| Post | 34.58 | 5.73 | 31.88 | 6.61 | −0.44† | ||
| Follow-up | 34.45 | 5.88 | 33.59 | 4.87 | −0.16 | ||
| ASQ:SE | Pre | 0.06 | 0.57 | 0.20 | 0.64 | 0.23 | 2.16 |
| Post | −0.08 | 0.56 | −0.01 | 0.53 | 0.13 | ||
| Follow-up | 0.01 | 0.71 | −0.04 | 0.42 | −0.09 | ||
Note.
PSI-SF = Parenting Stress Index-Short Form Total, HOME = Home Inventory Total, ASQ:SE = Ages and Stages: Social Emotional, transformed into Z Scores.
p = .053
Maternal depression and parenting and child adjustment
Table 3 shows the relation between maternal depression (as indicated by HDRS scores) and the measures of parenting and child adjustment over time. Results show a strong association between the HDRS and the PSI-SF and this differed depending on the time. Specifically, the significant depression by time interaction (F=9.48, p>0.001) indicates that the strength of the relationship between the HDRS and PSI-SF increased over time. The depression by time interactions were non-significant for the HOME and ASQ:SE.
Table 3.
Linear relationship between HDRS scores and parenting and child measures across time for the full sample (N = 93)
| Measure | Assessment | Coef | SE | DF | t | F (HDRS x Time) |
|---|---|---|---|---|---|---|
| PSI-SF | Pre | 0.91 | 0.43 | 90 | 2.11 | 9.48*** |
| Post | 1.29 | 0.23 | 82 | 5.57*** | ||
| Follow-up | 2.17 | 0.36 | 73 | 5.97*** | ||
| HOME | Pre | −0.12 | 0.14 | 87 | −0.84 | 1.57 |
| Post | −0.30 | 0.07 | 80 | −4.06*** | ||
| Follow-up | −0.29 | 0.07 | 73 | −3.95*** | ||
| ASQ:SE | Pre | 0.01 | 0.01 | 90 | 0.88 | 1.25 |
| Post | 0.02 | 0.01 | 80 | 2.50* | ||
| Follow-up | 0.01 | 0.01 | 75 | 1.34 |
Note.
PSI-SF = Parenting Stress Index-Short Form Total, HOME = Home Inventory Total, ASQ:SE = Ages and Stages: Social Emotional, transformed into Z Score.
p<0.05 (p-values are FDR adjusted)
Examination of the coefficients at each time point shows a strong relationship between HDRS scores and the PSI-SF and HOME across time points. There is a significant positive relationship between the HDRS and PSI-SF at post and follow-up and a trend at pre-treatment (FDR corrected p=0.056) such that changes in severity of depression is associated with resutant shifts in parenting stress. Subsequent analyses with the subscales of the PSI-SF revealed an identical pattern of a positive association between depression and stress for Parental Distress, Parent-Child Dysfunctional Interaction, and Difficult Child (p < .05). For the HOME, a negative relationship was found between depression and nurturing and stimulating parenting at post-treatment and follow-up (but not at pre-treatment). Subsequent analyses with the subscales of the HOME revealed an identical pattern of a negative association between depression and nurturing and stimulating parenting for Responsivity, Acceptance, Organization, Learning Materials, Involvement, and Variety (p < .05). Taken together, these results show that as depression improved, there were parallel changes in parenting. For the ASQ:SE, a negative association between depression and child adjustment was found only at post-treatment.
Discussion
In the first step of this study, we contrasted IH-CBT and SHV groups on measures of parenting and child adjustment. No significant differences were found, and the hypothesis that IH-CBT would be superior to controls was not supported. The general trend was in the direction of improved parenting and child adjustment in IH-CBT group relative to controls. It is possible that statistical power was insufficient to detect group differences, particularly for the PSI-SF in which the patterns of means over time favored the IH-CBT condition. However, it is important to note that IH-CBT is focused on reducing depressive symptoms (for which effect sizes are moderate), and there are no treatment elements that directly address parenting challenges or child behavior problems. Consequently, it is not surprising that IH-CBT treatment by itself did not benefit parenting and child behavior in this population of low income mothers in home visiting programs. It is possible that benefits to parenting and child adjustment might emerge after a longer period of maternal recovery from depression. To this end, it is important to note that improvement in depression occurs in both the treatment and control groups, as is typical of clinical trials. Some (7.0%-Ammerman et al. 2013a) in the control condition received treatment in the community that was minimally adequate which may have led to improvement, and it is the natural course of MDD for episodes to end and for mood to return to previous levels.
In the second step of the study we examined the association between maternal improvement in depression and parenting and child adjustment. Results indicated a strong relationship between maternal depression and parenting stress and nurturing parenting. Consistent with our hypothesis, lower levels of depression were consistently related to decreased stress and more nurturing parenting behaviors. This relationship strengthened in post-treatment and follow-up in parenting stress. Examination of the subscales of each of the instruments used to measure these constructs confirmed the extent of this relationship in that decreased depression was associated with healthy levels of different aspects of parenting stress and nurturing parenting. These findings add to the growing literature that improvement in depression is associated with corresponding improvements in parenting (Garber et al. 2011). Given that home visiting was provided to all mothers during this time, it is impossible to disaggregate the contributions of this co-occurring service. However, it is possible that concurrent home visiting acted synergistically with recovery processes to accelerate emergence or acquisition of parenting skills during the interval between pre-treatment and follow-up.
Depression was not associated with child social and emotional adjustment. It is possible that this was attributable to the young age of the children, who were an average of five months old at pre-treatment. The emergence of a more clearly evident maladjustment in later toddlerhood may have revealed a stronger link between maternal depression and child functioning. In contrast, there is a sizable literature documenting impaired behavior in the offspring of depressed mothers (Field 2010) and such a relationship would be expected in the current study. Perhaps the ASQ: SE was less sensitive to the kinds of child maladjustment that is linked to maternal depression. The measure is a widely used screen, but a more in-depth or independent observational measure of child behavior may have revealed more subtle aspects of maladjustment that may subsequently be related to maternal depression. It is also possible that concurrent home visiting, with its emphasis on promoting healthy infant development, may have offset the effects of maternal depression on child behavior, at least during these first 18 months of life. Further research is needed to investigate the relation between maternal depression and child adjustment in this population.
These findings have implications for mothers in home visiting in particular, and low income new mothers in general. For mothers in home visiting, improvement in depression is accompanied by changes in parenting stress and nurturing caregiving, both of which are key foci of home visiting programs. Treatments that are effective in reducing depression in this population, such as IH-CBT (Ammerman et al. 2013a), can facilitate improvement and hold promise to prevent the negative consequences of depression that have been documented in home visiting (Duggan et al. 2009; Easterbrooks et al. 2013; McFarlane et al. 2013). Mothers in home visiting exhibit most of the demographic and clinical factors that are associated with depression. It is imperative that home visiting programs consider this issue a priority in order to fully address the needs of this high risk population and to optimize outcomes sought by these services. Mothers in home visiting are also at least in part representative of low income mothers generally. They share with other low income mothers the challenges of violence, financial hardship, social isolation, and risk for depression (Garner 2013). Treatments targeting depression in low income mothers (e.g., O’Mahen et al. 2013) hold considerable promise to secondarily benefit parenting.
The study had a number of strengths. First, the study focused on depression in new, low income mothers, a population heretofore understudied and underrepresented in the perinatal depression literature. Second, the RCT design provided a rigorous framework within which to examine IH-CBT. Third, the diagnosis of MDD was confirmed using a semi-structured psychiatric interview and depression was characterized by independent clinician ratings. This is in contrast to the sole reliance on self-reported depression that is typical of research on perinatal depression generally and in home visiting in particular. Fourth, HDRS assessments were blinded at post-treatment and follow-up. Fifth, an intent-to-treat strategy was used and retention of the sample was good. Sixth, two widely disseminated and evidence-based models of home visiting were represented in the sample. Findings are generalizable to low income, socially isolated mothers, who in turn reflect the largest population enrolled in home visiting programs. Seventh, a number demographic and clinical covariates were considered.
The study also has several limitations that warrant caution in interpreting findings. First, the sample size was relatively small, limiting power. Second, there was no long term follow-up. It is not known if impacts of improvement were sustained or emerged beyond the three month follow-up time point, a period in which risk for relapse is high (Hollon and Dimidjian 2009). Third, child functioning was measured by maternal report, and it is possible that more objective indices (e.g., Forman et al. 2007) or reports from others would have yielded different findings. Fourth, findings may not be generalizable to mothers with higher levels of social resources.
Conclusion
A treatment focused on depression reduction in low income mothers in home visiting did not result in changes in parenting stress, nurturing parenting, or child adjustment. However, depression was strongly related to parenting stress and nurturing parenting such that improvements in depression resulted in corresponding changes in these variables. Maternal depression was unrelated to child adjustment, possible attributable to child age, sensitivity of measurement, or compensating effects of home visiting. Treatments that are effective in reducing depression in this population can lead to corresponding benefits to parenting that in turn boost home visiting outcomes.
Acknowledgments
Supported by Grant R34MH073867 from the National Institute of Mental Health. The authors acknowledge the participation and support of The Health Foundation of Greater Cincinnati, United Way of Greater Cincinnati, Kentucky H.A.N.D.S., Ohio Help Me Grow, and www.OhioCanDo4Kids.org.
Footnotes
Conflict of Interest: The authors have no conflict of interest to report.
References
- Abidin RR. The Parenting Stress Index professional manual. Psychological Assessment Resources; Odessa, FL: 1995. [Google Scholar]
- Adirim T, Supplee L. Overview of the federal home visiting program. Pediatrics. 2013;132(Suppl 2):S59–64. doi: 10.1542/peds.2013-1021C. [DOI] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Altaye M, Stevens J, Teeters AR, Van Ginkel JB. A clinical trial of in-home CBT for depressed mothers in home visitation. Behavior therapy. 2013a;44:359–372. doi: 10.1016/j.beth.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Altaye M, Teeters AR, Stevens J, Van Ginkel JB. Treatment of depressed mothers in home visiting: impact on psychological distress and social functioning. Child Abuse Negl. 2013b;37:544–554. doi: 10.1016/j.chiabu.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Bosse NR, Teeters AR, Van Ginkel JB. Maternal depression in home visitation: A systematic review. Aggression and Violent Behavior. 2010;15:191–200. doi: 10.1016/j.avb.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Stevens J, Bosse NR, Short JA, Bodley AL, Van Ginkel JB. An open trial of In-Home CBT for depressed mothers in home visitation. Maternal and Child Health Journal. 2011;15:1333–1341. doi: 10.1007/s10995-010-0691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR. Effect of maternal depression on child behavior: A sensitive period? J Am Acad Child Adolesc Psychiatry. 2010;49:699–707. doi: 10.1016/j.jaac.2010.03.012. S0890-8567(10)00293-5 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck JS. Cognitive behavior therapy: Basics and beyond. 2. Guilford; New York: 2011. [Google Scholar]
- Benjamini Y, Hochberg Y. On the adaptive control of the false discovery rate in multiple testing with independent statistics. Journal of Educational and Behavioral Statistics. 2000;25:60–83. [Google Scholar]
- Bradley RH, Corwyn RF, McAdoo HP, Coll CG. The home environments of children in the United States part I: Variations by age, ethnicity, and poverty status. Child Dev. 2001;72:1844–1867. doi: 10.1111/1467-8624.t01-1-00382. [DOI] [PubMed] [Google Scholar]
- Caldwell BM, Bradley RH. Home Observations for Measurement of the Environment Administration Manual Revised edn. Home Inventory; Little Rock, AK: 1984. [Google Scholar]
- Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T. Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Dev Psychol. 2007;43:1202–1215. doi: 10.1037/0012-1649.43.5.1202. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Duggan AK, Berlin LJ, Cassidy J, Burrell L, Tandon SD. Examining maternal depression and attachment insecurity as moderators of the impacts of home visiting for at-risk mothers and infants. J Consult Clin Psychol. 2009;77:788–799. doi: 10.1037/a0015709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easterbrooks MA, et al. Limiting home visiting effects: maternal depression as a moderator of child maltreatment. Pediatrics. 2013;132(Suppl 2):S126–133. doi: 10.1542/peds.2013-1021K. [DOI] [PubMed] [Google Scholar]
- Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev. 2010;33:1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman DR, O’Hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Dev Psychopathol. 2007;19:585–602. doi: 10.1017/S0954579407070289. [DOI] [PubMed] [Google Scholar]
- Garber J, Ciesla JA, McCauley E, Diamond G, Schloredt KA. Remission of depression in parents: links to healthy functioning in their children. Child Dev. 2011;82:226–243. doi: 10.1111/j.1467-8624.2010.01552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner AS. Home visiting and the biology of toxic stress: opportunities to address early childhood adversity. Pediatrics. 2013;132(Suppl 2):S65–73. doi: 10.1542/peds.2013-1021D. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Gunlicks ML, Weissman MM. Change in child psychopathology with improvement in parental depression: A systematic review. Journal of American Academy Child Adolescent Psychiatry. 2008;47:379–389. doi: 10.1097/CHI.0b013e3181640805. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollon SD, Dimidjian S. Cognitive and behavioral treatment of depression. In: Gotlib IH, Hammen CL, editors. Handbook of Depression. 2. Guilford Press; New York: 2009. [Google Scholar]
- Holton JK, Harding K. Healthy Families America: Ruminations on implementing a home visitation program to prevent child maltreatment. Journal of Prevention and Intervention in the Community. 2007;34:13–38. doi: 10.1300/J005v34n01_02. [DOI] [PubMed] [Google Scholar]
- Levy LB, O’Hara MW. Psychotherapeutic interventions for depressed, low-income women: A review of the literature. Clin Psychol Rev. 2010;30:934–950. doi: 10.1016/j.cpr.2010.06.006. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Wisner K, Sit D, Luther JF, Wisniewski SR. Depression treatment and maternal functioning. Depress Anxiety. 2011;28:1020–1026. doi: 10.1002/da.20892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayberry LJ, Horowitz JA, Declercq E. Depression symptom prevalence and demographic risk factors among U.S. women during the first 2 years postpartum. J Obstet Gynecol Neonatal Nurs. 2007;36:542–549. doi: 10.1111/j.1552-6909.2007.00191.x. [DOI] [PubMed] [Google Scholar]
- McFarlane E, Burrell L, Crowne S, Cluxton-Keller F, Fuddy L, Leaf PJ, Duggan A. Maternal relationship security as a moderator of home visiting impacts on maternal psychosocial functioning. Prev Sci. 2013;14:25–39. doi: 10.1007/s11121-012-0297-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL. The Nurse-Family Partnership: From trials to practice. In: Reynolds AJ, Rolnick AJ, Englund MM, Temple JA, editors. Childhood programs and practices in the first decade of life: A human capital integration. Cambridge University Press; New York: 2010. pp. 49–75. [Google Scholar]
- O’Mahen H, Himle JA, Fedock G, Henshaw E, Flynn H. A pilot randomized controlled trial of cognitive behavioral therapy for perinatal depression adapted for women with low incomes. Depress Anxiety. 2013;30:679–687. doi: 10.1002/da.22050. [DOI] [PubMed] [Google Scholar]
- Seifer R, Dickstein S, Sameroff AJ, Magee KD, Hayden LC. Infant mental health and variability of parental depression symptoms. J Am Acad Child Adolesc Psychiatry. 2001;40:1375–1382. doi: 10.1097/00004583-200112000-00007. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Squires J, Bricker D, Twombly E. Ages and Stages Questionnaires: Social-emotional user’s manual. Paul H. Brookes; Baltimore: 2002. [Google Scholar]
- Wisner KL, Chambers C, Sit DK. Postpartum depression: a major public health problem. JAMA. 2006;296:2616–2618. doi: 10.1001/jama.296.21.2616. [DOI] [PubMed] [Google Scholar]