Abstract
Objectives
Emergency department (ED) visits for asthma exacerbation reflect a failure of longitudinal asthma management. However, little is known about the characteristics of patients with frequent ED visits (≥2 visits in a 1-year period). We aimed to characterise the adult patients who frequently presented to the ED for asthma exacerbation in Japan.
Design
A multicentre chart review study of 23 EDs across Japan.
Participants
Adults aged 18–54 years who presented to the ED with asthma exacerbation from 2009 to 2011.
Outcome measures
Frequency of ED visits for asthma exacerbation in a 1-year period, including the index ED visit.
Results
Of the 1002 eligible patients, 218 (22%) had frequent ED visits, accounting for 48% of total ED visits for asthma exacerbation in the 1-year period. Specifically, 12% had 2 ED visits and 10% had ≥3 visits. In these patients, guideline-recommended chronic management was suboptimal. For example, among patients with ≥3 ED visits, only 63% were treated with inhaled corticosteroids and 49% were current smokers. In a multinomial logistic regression model, markers of chronic asthma severity (history of hospitalisation for asthma and use of inhaled corticosteroids) were significantly associated with a higher frequency of ED visits (both p<0.05).
Conclusions
This multicentre study in Japan demonstrated that many patients are frequent ED users for asthma exacerbation. We also found that their asthma control management is suboptimal, most likely contributing to worse chronic severity and more frequent ED visits. Further dissemination and adoption of evidence-based guidelines are required to reduce asthma morbidity in this high-risk population.
Keywords: asthma exacerbation, emergency department, multicenter study, risk factors, inhaled corticosteroids
Strengths and limitations of this study.
This is a large multicentre study from 23 emergency departments (EDs) across different geographical regions of Japan.
This is the first study to investigate the characteristics of patients with frequent ED visits for asthma exacerbation in Japan.
Our study population mainly consisted of urban, academic EDs in Japan. Therefore, our findings may not be generalisable to rural, non-academic EDs or other healthcare settings.
Introduction
Asthma affects an estimated 300 million people worldwide, with 250 000 annual deaths attributed to this disease.1 Recent estimates indicated that approximately 4% (5 million) of Japanese adults receive a diagnosis of asthma in their lifetime,2 contributing to substantial health and economic burdens.3 4 Furthermore, asthma exacerbations account for a significant proportion of this burden, resulting in estimated annual costs of $3.4 billion in Japan.4 In this context, the Japanese government set a national goal to prevent asthma exacerbations and asthma-related mortality.5
As most of the asthma exacerbations are deemed to be preventable with high-quality prevention-oriented outpatient care, frequent (2 or more in a 1-year period) emergency department (ED) visits reflect a failure of asthma control management.6 Our previous studies in the USA investigated this high-risk population, along with risk factors of frequent ED visits for asthma exacerbations, such as non-white race/ethnicity, low socioeconomic status and higher chronic asthma severity.6–10 However, little is known about the characteristics of patients with frequent ED visits for asthma exacerbation in other industrialised nations, particularly in those with universal healthcare systems.
To address this knowledge gap in the literature, using data from a 23-centre observational study of adults presenting to the ED with asthma exacerbation, we aimed to characterise the patients with frequent ED visits for asthma exacerbation in Japan.
Methods
Study design and settings
We conducted a multicentre chart review study to characterise the clinical epidemiology of asthma exacerbations in Japanese EDs. The study setting, methods and variables have been reported previously.11 Briefly, this study was coordinated by the Japanese Emergency Medicine Network (JEMNet, http://jemnet.asia/wp) in collaboration with the US-based Emergency Medicine Network (http://www.emnet-usa.org). JEMNet is a consortium of 23 academic and community medical centres from different geographic regions across Japan. The participating institutions had a median annual ED census of 29 000 patient visits (range 12 000–67 000) and 107 visits with asthma exacerbation (range 20–200). All 23 EDs were staffed by ED-based attending physicians. The Institutional Review Board of each participating centre and Massachusetts General Hospital approved this study with a waiver of written informed consent.
Selection of participants
Using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) code J45.xx,12 the study sites identified all ED visits with a principal ED or hospital discharge diagnosis of asthma from hospital administrative records from January 2009 until December 2011 (figure 1). The inclusion criteria of this study were asthma ED visits made by patients aged 18–54 years with a history of physician diagnosis of asthma prior to the index ED visit. We excluded ED visits made by patients with a history of physician diagnosis of chronic obstructive pulmonary disease, emphysema, or chronic bronchitis, transfer ED visits, ED visits not primarily prompted by an asthma exacerbation, or repeat ED visits by the same individual. In the case of repeat visits, only the first ED visit during the study period was included. Therefore, each ED visit in the study represented a unique patient in the ED. These criteria were the same as in our previous US-based studies on this topic.6 8
Figure 1.
The schematic of strategy used to identify emergency department (ED) visit frequency.
Data collection
Using a standardised form,6 11 13 on-site chart abstractors reviewed 60 ED charts that are randomly selected from the eligible patients identified by using the ICD-10-CM code. We collected information on patient demographics, chronic asthma history and chronic asthma medications, as well as details of the current asthma exacerbation, ED management and ED disposition.11
Sites with less than 60 charts during this period also reviewed eligible charts from the calendar years 2009 and 2010 to reach the target number of 60 charts. All chart abstractors were emergency physicians or emergency medicine residents. Abstractors were trained with a 1 h lecture, and then they completed practice charts, which were assessed versus a criterion standard. If an abstractor's accuracy was less than 80% per chart, the individual was retrained. All forms were reviewed by site investigators and submitted to a secure, web-based, electronic database. Then these data were reviewed at the JEMNet Coordinating Center, and site investigators were queried about missing data and discrepancies identified by manual data checks.
Outcome measures
The outcome measure of interest was the frequency of ED visits for asthma exacerbation in a 1-year period (ie, the number of ED visits for asthma exacerbation during the preceding 365 days including the index visit; figure 1).
Statistical analysis
For the purpose of this analysis, we classified patients into three ED-using groups based on the distribution of ED visit frequency and the literature:10 one ED visit (ie, index ED visit only), two ED visits and three or more ED visits for asthma exacerbation in the 1-year period. First, we examined unadjusted associations between the patient-level characteristics and the outcomes by using a χ2 test, a one-way analysis of variance and a Kruskal-Wallis test, where appropriate. Second, to examine independent predictors of a higher frequency of ED visits for asthma exacerbation, we constructed a multinomial logistic regression model, with one ED visit as the reference for each. The patient-level factors included in the model were age, sex, smoking, chronic asthma factors (history of hospital admission and intubation for asthma exacerbation) and chronic asthma medications (inhaled corticosteroids (ICS), oral xanthines and leukotriene modifiers).
Additionally, we performed a sensitivity analysis to assess the robustness of the association between patient-level factors and the frequency of ED visits. We fit a negative binomial regression model to account for statistical overdispersion and to avoid the use of an arbitrary cut-off point for the frequency of ED visits for asthma exacerbation. Incidence rate ratios (IRRs) are presented with 95% CIs. Two-sided p<0.05 was considered statistically significant. All analyses were performed using Stata 13.0 software (StataCorp; College Station, Texas, USA).
Results
We created a cohort of 1380 patients who presented to 1 of the 23 EDs with an asthma exacerbation during 2009–2011; 91% of the ED visits were made in 2011. Among these patients, 1002 (73%) had data on the frequency of ED visits for asthma exacerbation in the previous year, and were included in this analysis. The analytic and non-analytic cohorts were similar in age, sex, ED presentation and ED disposition (all p>0.05: data not shown).
Frequent ED visits for asthma exacerbation
Of the 1002 patients in the analytic cohort, 784 (78%; 95% CI 76% to 81%) reported one ED visit, while 117 (12%; 95% CI 10% to 14%) had two ED visits and 101 (10%; 95% CI 8% to 12%) had three or more ED visits in the 1-year period. The number of patients with asthma exacerbation and the cumulative number of ED visits for asthma exacerbation in the 1-year period by ED visit frequency are shown in figure 2. Patients with two ED visits accounted for 16% (95% CI 14% to 18%) of all ED visits for asthma exacerbation in the 1-year period, and patients with three or more ED visits accounted for 32% (95% CI 29% to 34%).
Figure 2.
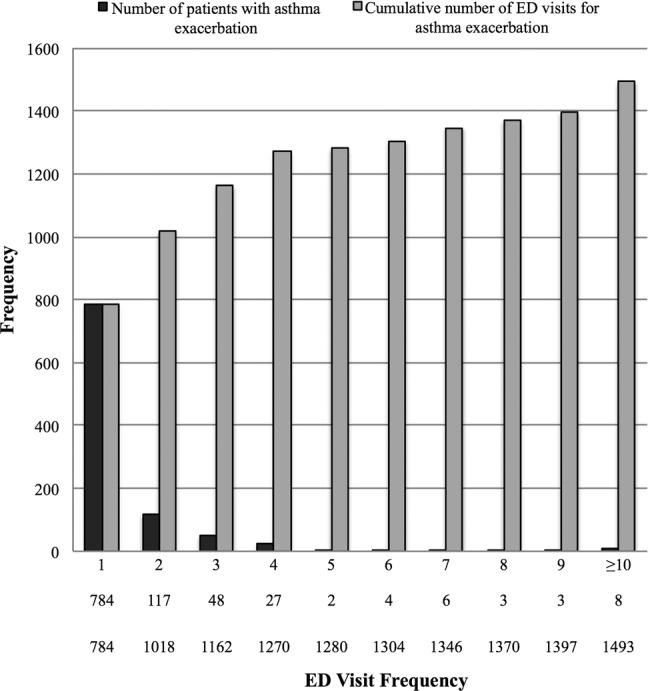
Number of patients with asthma exacerbation and cumulative number of emergency department (ED) visits for asthma exacerbation, according to ED visit frequency.
Patient characteristics by the ED visit frequency group
Chronic asthma factors, chronic asthma medications and ED management differed among the ED visit frequency groups (table 1). Patients with three or more ED visits for asthma exacerbation were more likely to be a current smoker; indeed, approximately half of them were current smokers. Likewise, patients with frequent ED visits for asthma exacerbation were more likely to have a history of oral corticosteroid use, hospital admission and intubation for asthma, and hospital admission for asthma in the past year (all p<0.001). Similarly, these patients were more likely to have been on ICS, oral xanthines and leukotriene modifiers (all p<0.001). However, the proportion of patients who had used these long-term control medications was relatively low among the frequency groups. For example, only 45% of the patients with two ED visits and 63% of the patients with three or more ED visits were currently treated with ICS.
Table 1.
Patient demographics, chronic asthma factors, acute asthma presentation and emergency department (ED) course for asthma exacerbation, according to the number of ED visits in the 1-year period
| 1 ED visit | 2 ED visits | ≥3 ED visits | ||
|---|---|---|---|---|
| Variables* | (n=784) | (n=117) | (n=101) | p Value |
| Age (years), median (IQR) | 34 (26–43) | 34 (25–42) | 37 (27–43) | 0.45 |
| Male sex | 43 (40–47) | 41 (32–50) | 39 (29–49) | 0.64 |
| Current smoker | 42 (39–46) | 32 (24–42) | 49 (38–59) | 0.045 |
| Chronic asthma factors | ||||
| History of oral corticosteroid use for asthma | 35 (31–40) | 75 (64–84) | 84 (75–91) | <0.001 |
| History of hospital admission for asthma | 23 (20–27) | 50 (39–61) | 66 (55–75) | <0.001 |
| History of intubation for asthma | 1 (1–3) | 1 (0–7) | 8 (3–16) | <0.001 |
| History of hospital admission for asthma in the past year | 2 (1–3) | 19 (12–28) | 34 (25–45) | <0.001 |
| Current use of inhaled corticosteroids | 23 (20–26) | 45 (36–55) | 63 (53–72) | <0.001 |
| Current use of oral xanthines | 10 (8–12) | 12 (7–20) | 26 (18–36) | <0.001 |
| Current use of leukotriene modifiers | 8 (6–10) | 16 (10–25) | 29 (21–39) | <0.001 |
| Acute asthma presentation | ||||
| Duration of symptoms | ||||
| <4 h before ED arrival | 16 (14–19) | 13 (7–20) | 21 (13–31) | 0.08 |
| 4–23 h | 43 (40–47) | 49 (39–58) | 53 (42–63) | |
| 1–7 days | 34 (31–38) | 36 (27–46) | 22 (14–32) | |
| >7 days | 7 (5–9) | 3 (1–8) | 4 (1–10) | |
| ED course | ||||
| Initial respiratory rate (breath/min), mean (SD) | 22±6 | 21±6 | 24±6 | 0.07 |
| Initial oxygen saturation (%), mean (SD) | 95±3 | 95±4 | 95±4 | 0.12 |
| Initial peak flow† (L/min), mean (SD) | 214±103 | 254±63 | 170±57 | 0.21 |
| Number of inhaled β-agonists in first hour, median (IQR) | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.33 |
| Number of inhaled β-agonists over ED stay, median (IQR) | 1 (1–2) | 1 (1–2) | 2 (1–2) | 0.17 |
| Received systemic corticosteroid treatment | 41 (37–44) | 44 (34–53) | 62 (52–72) | <0.001 |
| ED disposition | 0.62 | |||
| Sent home | 89 (86–91) | 86 (79–92) | 89 (81–94) | |
| Hospital admission | 11 (9–13) | 12 (7–19) | 11 (6–19) | |
| Other (eg, left against medical advice) | 1 (0–1) | 2 (0–6) | 0 | |
| Sent home with systemic corticosteroids | 35 (32–39) | 29 (20–39) | 32 (23–43) | 0.42 |
*Data were expressed as % (95% CI) unless otherwise specified.
†Analysed for 56 patients (6%) with initial peak flow available.
Although there were no significant between-group differences in the markers of acute severity (eg, respiratory rates and peak flow measurement at the ED presentation), patients with a higher frequency of ED visits were more likely to be treated with systemic corticosteroids during their index ED visit (p<0.001). In contrast, there was no significant difference in ED disposition among the three groups (p=0.62).
Factors associated with frequent ED visits for asthma exacerbation
In the multinomial logistic regression model, history of hospital admission for asthma and current use of ICS remained significant as independent predictors of a higher frequency of ED visits across the frequency groups (table 2). Likewise, with the use of a negative binomial regression model (table 3), history of hospital admission for asthma (IRR 3.07; 95% CI 2.07 to 4.56; p<0.001), current use of ICS (IRR 2.06; 95% CI 1.36 to 3.14; p=0.001) and current use of oral xanthines (IRR 1.72; 95% CI 1.02 to 2.91; p=0.04) were independently associated with a higher frequency of ED visits for asthma exacerbation.
Table 2.
Multinomial models of factors associated with frequent emergency department (ED) visits for asthma exacerbation
| 2 (vs 1) ED visits |
≥3 (vs 1) ED visits |
|||
|---|---|---|---|---|
| Variables | Risk ratio (95% CI) | p Value | Risk ratio (95% CI) | p Value |
| Age, years | ||||
| 18–29 | 1 (reference) | 1 (reference) | ||
| 30–39 | 0.76 (0.39 to 1.48) | 0.43 | 0.81 (0.41 to 1.60) | 0.55 |
| 40–54 | 0.73 (0.39 to 1.39) | 0.34 | 0.86 (0.46 to 1.61) | 0.64 |
| Male sex | 0.67 (0.38 to 1.19) | 0.17 | 0.74 (0.43 to 1.29) | 0.29 |
| Current smoker | 1.91 (1.01 to 3.58) | 0.04 | 1.86 (0.97 to 3.57) | 0.06 |
| History of hospital admission for asthma | 3.06 (1.72 to 5.45) | <0.001 | 4.77 (2.73 to 8.32) | <0.001 |
| History of intubation for asthma | 0.36 (0.04 to 3.15) | 0.36 | 1.19 (0.37 to 3.84) | 0.29 |
| Current use of inhaled corticosteroids | 2.03 (1.10 to 3.74) | 0.02 | 2.10 (1.17 to 3.79) | 0.01 |
| Current use of oral xanthines | 0.79 (0.30 to 2.06) | 0.63 | 1.75 (0.85 to 3.56) | 0.13 |
| Current use of leukotriene modifiers | 1.39 (0.57 to 3.37) | 0.47 | 2.63 (1.31 to 5.28) | 0.01 |
Bold results are statistically significant.
Table 3.
Negative binomial regression models of factors associated with frequent emergency department visits for asthma exacerbation
| Variables | Incident rate ratio (95% CI) | p Value |
|---|---|---|
| Age, years | ||
| 18–29 | 1 (reference) | |
| 30–39 | 0.83 (0.52 to 1.31) | 0.42 |
| 40–54 | 0.89 (0.58 to 1.37) | 0.60 |
| Male sex | 0.78 (0.53 to 1.13) | 0.19 |
| Current smoker | 1.19 (0.78 to 1.82) | 0.42 |
| History of hospital admission for asthma | 3.07 (2.07 to 4.56) | <0.001 |
| History of intubation for asthma | 1.51 (0.58 to 3.93) | 0.40 |
| Current use of inhaled corticosteroids | 2.06 (1.36 to 3.14) | 0.001 |
| Current use of oral xanthines | 1.72 (1.02 to 2.91) | 0.04 |
| Current use of leukotriene modifiers | 1.73 (0.99 to 3.00) | 0.05 |
Bold results are statistically significant.
Discussion
This multicentre study is the first to characterise patients with frequent ED visits for asthma exacerbation in Japan. Among 1002 patients presenting with asthma exacerbation to 1 of the 23 Japanese EDs, we found that 22% had frequent ED visits, accounting for 48% of total ED visits for asthma exacerbation in the 1-year period. We also found that the frequent ED users received suboptimal asthma control management. Indeed, more than one-third of patients with three and more ED visits were not treated with ICS and half were current smokers, most likely contributing to worse chronic severity and more frequent ED visits for asthma exacerbation.
Results in context
Previous studies in the USA reported many patients with frequent ED visits for asthma exacerbation. In the 1990s, 73–82% of patients in the ED with asthma exacerbation had frequent ED visits in the previous year,7 8 while the number was 46% in the 2010s.6 In contrast, our study in Japan demonstrated that 22% of patients in the ED with asthma exacerbation had frequent ED visits in the 1-year period. The reasons for this apparent difference between the US and Japanese studies are most likely multifactorial. Potential explanations include differences in study design, setting and population, although our recent multicentre observational study of US adults for 2011–2012 used the same design as the current study.6 Differences in healthcare systems may also partly explain the differences. The Japanese healthcare system provides universal healthcare.14 15 Additionally, most primary care offices in Japan do not require an appointment to see physicians,15 and primary care offices frequently serve as urgent care clinics. Accordingly, Japanese patients with asthma may have chosen to visit their primary care office instead of the ED when they had asthma exacerbations, thereby reducing the number of frequent ED visits in this study.
Suboptimal longitudinal management in frequent ED users
In agreement with the previous studies,6–9 we found that patients with frequent ED visits for asthma exacerbation were more likely to have markers of severe chronic asthma—for example, history of hospital admission for asthma, and current use of ICS. It is clinically plausible that patients with more severe asthma have more frequent ED visits for asthma exacerbation.16 However, we were struck by the finding that long-term asthma treatment in this high-risk population was suboptimal. Indeed, our data demonstrated that only 45% of the patients with two ED visits and 63% of the patients with three or more ED visits for asthma exacerbation were treated with ICS. This observation was consistent with the literature demonstrating that the ICS use in patients with asthma remains low in Japan compared with that in other developed nations, although its rate has been increasing (12% in 2001 to 18% in 2005).17
We also found that approximately half of the patients with three or more ED visits for asthma exacerbation in the 1-year period were current smokers. It is well documented that cigarette smoke exposure is a risk factor for asthma exacerbation.18–21 Accordingly, international and national guidelines for asthma recommend smoking cessation and avoiding smoke exposure.22–24 Our findings collectively suggest that only a subset of these high-risk patients in Japan received optimal long-term asthma control treatment and education, most likely contributing to worse chronic asthma severity and more frequent ED visits for asthma exacerbation. Therefore, further dissemination and adoption of evidence-based guidelines are required to reduce the large burden of asthma morbidity in Japan.
Potential limitations
Our study has several potential limitations. First, our study population mainly consisted of urban, academic EDs in Japan. Therefore, our findings may not be representative of patients with asthma in rural, non-academic EDs or generalisable to the other developed nations. Second, 27% of patients were excluded owing to a lack of information on the frequency of ED visits for asthma exacerbation in the previous year. However, the analytic and non-analytic cohorts were similar in the patient demographics, ED presentation and ED disposition. These similarities argue against a significant selection bias. Third, this is a chart review study; therefore, the quality of information could be deficient owing to misclassification. However, a prior ED-based study reported high agreement in the patient characteristics between chart review and directly observed care in the patients presenting to the ED for asthma exacerbation, with the κ-statistics from 0.50 to 0.82.25 Furthermore, in this multicentre study, the inter-rater agreement was moderate to perfect (κ-statistics, 0.56–1.00).11 Fourth, as with any observational studies, the observed associations with frequent ED visits do not necessarily prove causality and might be explained, at least partly, by unmeasured confounders, such as the amount of inhaled β-agonist or ICS use before the ED visit and time-variant covariates (eg, ICS use over time). Finally, as described above, patients with asthma exacerbation might have presented to their primary care office rather than the ED, thereby leading to an underestimation of the burden of patients with frequent asthma exacerbations. However, since our focus was on the burden of the frequent ED utilisation, our findings are of direct relevance to optimise asthma management in this high-risk population.
Conclusions
In this 23-centre observational study of ED adult patients with asthma exacerbation in Japan, we found that many patients had two or more ED visits for asthma exacerbation, accounting for approximately half of the total ED visits for asthma exacerbation in the 1-year period. Our data also demonstrated that asthma control management in this high-risk population is suboptimal, most likely contributing to worse chronic severity and more frequent ED visits for asthma exacerbation. For researchers, our observations should facilitate further investigation into the quality of the longitudinal asthma control care and research on barriers to the delivery of evidence-based asthma care in Japan. For clinicians and professional organisations, continuous efforts to promote dissemination and adoption of evidence-based guidelines—for example, development of a nationwide asthma programme focusing on early intervention and disease control26 27—are required to reduce asthma morbidity in this high-risk population.
Acknowledgments
We thank the participating investigators for their ongoing dedication to emergency medicine research.
Footnotes
JEMNet study members: The site principal investigators were: Yukikazu Awaya, MD (Yahata Municipal Hospital, Kitakyushu, Fukuoka); Tadahiro Goto, MD (Fukui University Hospital, Eiheiji, Fukui); Nao Hanaki, MD (Japanese Redcross Nagoya Second Hospital, Nagoya, Aichi); Takuro Hayashi, MD (Kobe City Medical Center General Hospital, Kobe, Hyogo); Taichi Imamura, MD (Shonan Kamakura General Hospital); Yusuke Kodama, MD (Kyoritsu General Hospital, Nagoya, Aichi); Takahiro Kondo, MD (Ekisaikai General Hospital, Nagoya, Aichi); Yasuhiro Koyama, MD (St. Marianna University Hospital, Kawasaki, Kawasaki); Tomomichi Matsuda, MD (Sapporo East Tokushukai Hospital, Sappro, Hokkaido); Nobuhiro Miyamae, MD (Rakuwakai Otowa Hospital, Kyoto, Kyoto); Miki Morikawa, MD (Juntendo University Urayasu Hospital, Urayasu, Chiba); Hideya Nagai, MD (Fukui Prefectural Hospital, Fukui, Fukui); Masahumi Ohta, MD (Kensei Hospital, Tsugaru, Aomori); Hiroshi Okamoto, MD (Kurashiki Central Hospital, Kurashiki, Okayama); Yuichi Okano, MD (Japanese Redcross Kumamoto Hospital, Kumamoto, Kumamoto); Masashi Okubo, MD (Okinawa Prefectural Chubu Hospital, Uruma, Okinawa); Yutaka Saito, MD (Kawasaki City Hospital Kawasaki, Kawasaki); Hiroyuki Suzuki, MD (Fukuoka Tokushukai Hospital, Kasuga, Fukuoka); Sei Takahashi, MD (Kinikyo Chuo Hospital, Sappro, Hokkaido); Kotaro Takebe, MD (Kyoto Prefectural University Hospital, Kyoto, Kyoto); Kenzo Tanaka, MD, MPH (Kameda Medical Center, Kamogawa, Chiba); Yuki Sato, MD (Nigata City General Hospital, Nigata, Nigata); and Hideto Yasuda, MD (Japanese Redcross Musashino Hospital, Musashino, Tokyo).
Contributors: HW contributed in the study concept and design, analysis and interpretation of the data, and drafting of the manuscript. YH and TC contributed in the study concept and design, acquisition of the data, and critical revision of the manuscript for important intellectual content. CAC contributed in the study concept and design, analysis and interpretation of the data, and critical revision of the manuscript for important intellectual content. KH contributed in the study concept and design, interpretation of the data, and critical revision of the manuscript for important intellectual content.
Funding: This study was supported by a grant from St. Luke's Life Science Institute (Tokyo, Japan).
Competing interests: CAC has provided asthma-related consultation for GlaxoSmithKline, Merck, Novartis and Teva.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Centers for Disease Control and Prevention. Asthma. http://www.cdc.gov/asthma/ (accessed 10 Mar 2015).
- 2.Fukutomi Y, Nakamura H, Kobayashi F et al. . Nationwide cross-sectional population-based study on the prevalences of asthma and asthma symptoms among Japanese adults. Int Arch Allergy Immunol 2010;153:280–7. 10.1159/000314369 [DOI] [PubMed] [Google Scholar]
- 3.Weiss KB, Sullivan SD, Lyttle CS. Trends in the cost of illness for asthma in the United States, 1985–1994. J Allergy Clin Immunol 2000;106:493–9. 10.1067/mai.2000.109426 [DOI] [PubMed] [Google Scholar]
- 4.Adachi M, Fukuda T, Morikawa A et al. . [Asthma mortality and burden of asthma in Japan]. Allergology & Immunology 2005;12:1438–47. [Google Scholar]
- 5.Ministry of Health, Labor and Welfare. http://www.mhlw.go.jp/new-info/kobetu/kenkou/ryumachi/jititai.html (accessed 10 Mar 2015).
- 6.Hasegawa K, Sullivan AF, Hirashima ET et al. . A multicenter observational study of US adults with acute asthma: who are the frequent users of the emergency department? J Allergy Clin Immunol Pract 2014;2:733–40. 10.1016/j.jaip.2014.06.012 [DOI] [PubMed] [Google Scholar]
- 7.Ford JG, Meyer IH, Sternfels P et al. . Patterns and predictors of asthma-related emergency department use in Harlem. Chest 2001;120:1129–35. 10.1378/chest.120.4.1129 [DOI] [PubMed] [Google Scholar]
- 8.Griswold SK, Nordstrom CR, Clark S et al. . Asthma exacerbations in North American adults: who are the “frequent fliers” in the emergency department? Chest 2005;127:1579–86. 10.1378/chest.127.5.1579 [DOI] [PubMed] [Google Scholar]
- 9.Pines JM, Buford K. Predictors of frequent emergency department utilization in Southeastern Pennsylvania. J Asthma 2006;43:219–23. 10.1080/02770900600567015 [DOI] [PubMed] [Google Scholar]
- 10.Hasegawa K, Tsugawa Y, Brown DF et al. . A population-based study of adults who frequently visit the emergency department for acute asthma. California and Florida, 2009–2010. Ann Am Thorac Soc 2014;11:158–66. 10.1513/AnnalsATS.201306-166OC [DOI] [PubMed] [Google Scholar]
- 11.Hasegawa K, Chiba T, Hagiwara Y et al. . Quality of care for acute asthma in emergency departments in Japan: a multicenter observational study. J Allergy Clin Immunol Pract 2013;1:509–15.e1-3. 10.1016/j.jaip.2013.05.001 [DOI] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). http://www.cdc.gov/nchs/icd/icd10cm.htm (accessed 10 Mar 2015).
- 13.Hasegawa K, Sullivan AF, Tsugawa Y et al. . Comparison of US emergency department acute asthma care quality: 1997–2001 and 2001–2012. J Allergy Clin Immunol 2014;135:73–80 10.1016/j.jaci.2014.08.028. [DOI] [PubMed] [Google Scholar]
- 14.OECD. Health at a Glance 2013. http://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2013_health_glance-2013-en (accessed 10 Mar 2015).
- 15.Ikegami N, Campbell JC. Japan's health care system: containing costs and attempting reform. Health Aff (Millwood) 2004;23:26–36. 10.1377/hlthaff.23.3.26 [DOI] [PubMed] [Google Scholar]
- 16.Chipps BE, Zeiger RS, Borish L et al. . Key findings and clinical implications from The Epidemiology and Natural History of Asthma: Outcomes and Treatment Regimens (TENOR) study. J Allergy Clin Immunol 2012;130:332–42.e10. 10.1016/j.jaci.2012.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adachi M, Ohta K, Morikawa A et al. . [Changes in asthma insights and reality in Japan (AIRJ) in 2005 since 2000]. Arerugi 2008;57:107–20. [PubMed] [Google Scholar]
- 18.Osborne ML, Pedula KL, O'Hollaren M et al. . Assessing future need for acute care in adult asthmatics: the Profile of Asthma Risk Study: a prospective health maintenance organization-based study. Chest 2007;132:1151–61. 10.1378/chest.05-3084 [DOI] [PubMed] [Google Scholar]
- 19.Silverman RA, Boudreaux ED, Woodruff PG et al. . Cigarette smoking among asthmatic adults presenting to 64 emergency departments. Chest 2003;123:1472–9. 10.1378/chest.123.5.1472 [DOI] [PubMed] [Google Scholar]
- 20.Siroux V, Pin I, Oryszczyn MP et al. . Relationships of active smoking to asthma and asthma severity in the EGEA study. Epidemiological study on the genetics and environment of asthma. Eur Respir J 2000;15:470–7. 10.1034/j.1399-3003.2000.15.08.x [DOI] [PubMed] [Google Scholar]
- 21.Marquette CH, Saulnier F, Leroy O et al. . Long-term prognosis of near-fatal asthma. A 6-year follow-up study of 145 asthmatic patients who underwent mechanical ventilation for a near-fatal attack of asthma. Am Rev Respir Dis 1992;146:76–81. 10.1164/ajrccm/146.1.76 [DOI] [PubMed] [Google Scholar]
- 22.Global Initiative for Asthma (GINA). http://www.ginasthma.org/ (accessed 10 Mar 2015). [Google Scholar]
- 23.National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): guidelines for the diagnosis and management of asthma-summary report 2007. J Allergy Clin Immunol 2007;120:S94–138. 10.1016/j.jaci.2007.09.029 [DOI] [PubMed] [Google Scholar]
- 24.Ohta K, Ichinose M, Nagase H et al. . Japanese guideline for adult asthma 2014. Allergol Int 2014;63:293–333. 10.2332/allergolint.14-RAI-0766 [DOI] [PubMed] [Google Scholar]
- 25.McDermott MF, Lenhardt RO, Catrambone CD et al. . Adequacy of medical chart review to characterize emergency care for asthma: findings from the Illinois Emergency Department Asthma Collaborative. Acad Emerg Med 2006;13:345–8. 10.1111/j.1553-2712.2006.tb01705.x [DOI] [PubMed] [Google Scholar]
- 26.Haahtela T, Valovirta E, Kauppi P et al. . The Finnish Allergy Programme 2008–2018—scientific rationale and practical implementation. Asia Pacific Allergy 2012;2:275–9. 10.5415/apallergy.2012.2.4.275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kauppi P, Linna M, Martikainen J et al. . Follow-up of the Finnish Asthma Programme 2000–2010: reduction of hospital burden needs risk group rethinking. Thorax 2013;68:292–3. 10.1136/thoraxjnl-2011-201028 [DOI] [PubMed] [Google Scholar]


