Abstract
Introduction
This study reviews the outcomes of reverse shoulder arthroplasty (RSA) and introduces a novel method of measuring changes in the center-of-rotation (COR) of the shoulder joint post-operatively.
Methods
We performed 10 reverse shoulders in 2011. Patients were evaluated pre-operatively and post-operatively using the Constant Score. The COR of the shoulder was determined pre- and post-operatively on radiographs and the differences were analysed.
Results
There was significant improvement in Constant Scores post-operatively with reduction in pain and increase in strength. Medialisation but not distalisation of the COR was achieved.
Discussion
Longer follow-up studies and studies on survivalship are required.
Keywords: Reverse shoulder, Arthroplasty, Cuff arthropathy
1. Introduction
The modern reverse shoulder was introduced by Grammont in 1985 due to the high failure rates of conventional total shoulder arthroplasty in patients with rotator cuff arthropathy.1–3 Although widely used in Europe, it was only in 2005 that the first reverse shoulder was performed in Singapore.4 Despite the expanding indications, rotator cuff arthropathy remains the primary indication for surgery at our institute.
Most studies early and medium term studies showed excellent pain relief and recovery of function following a reverse shoulder arthroplasty (RSA) for cuff arthropathy.2,3,5–8 However, such studies are performed in predominantly Caucasian populations and there had not been any local literature examining the outcomes of patients with cuff arthropathy following a RSA. Therefore, this pilot study reviews the early functional outcomes of all patients who had RSA performed at the Singapore General Hospital in 2011 with up to 24 months follow-up.
The success of the reverse shoulder was attributed to its biomechanical principle of medialising and distalising the center-of-rotation (COR) of the shoulder joint.2,5,9 However, there are currently no standardized methods of determining the change in COR pre- and post-operatively and furthermore, most studies on RSA do not include radiological assessments. In this study, we attempt to quantify the amount of medialisation and distalisation of the COR of the shoulder after a RSA, using the acromion as the reference point. This allows us to verify the biomechanics of RSA and will hopefully provide a simple method for measuring the change in the COR.
2. Methods
In 2011, 10 RSA on 10 patients were performed by 2 senior surgeons. All shoulders were operated for cuff arthropathy. Among the 10 patients, there were 7 females and 3 males with the mean age of 70.19 years (55.9–77.4) at the time of surgery. All patients received conservative management with physiotherapy and analgesia initially. Three patients had undergone previous surgeries on the same shoulder – 2 patients had rotator cuff repairs and 1 had rotator cuff repair with an open Mumford procedure for acromioclavicular joint osteoarthritis. The other 7 patients had primary RSA with 1 patient having a RSA on the contralateral shoulder previously.
2.1. Operative technique
Superolateral approach to the shoulder and the DePuy (DePuy Orthopaedics, Inc, Warsaw, IN, USA) Delta Reverse Shoulder prosthesis were used in all cases. With the patient in a semi-upright position on a beach chair, an anterolateral incision extending from the acromioclavicular joint to 5 cm below the acromion is made and following the subcutaneous dissection, the deltoid muscle is split longitudinally. In order to prevent injury to the axillary nerve, the deltoid split is kept to a minimum. After the deltoid split, the shoulder capsule is visualised but in patients with acetabulization of the humeral head, the humeral head is seen instead. Capsulotomy and debridement of the soft tissues are performed as necessary and subsequent steps of the surgery are carried out intra-capsularly as this approach capitalises on the absence of major neurovascular bundles within the joint thus avoiding any direct neurovascular injury. The humeral head is resected to create working space and to provide exposure of the glenoid fossa. Resurfacing of the glenoid fossa is subsequently performed and the metaglene is implanted as inferiorly as possible. After preparation of the humeral canal, the trial implants are inserted and reduction is performed. If stability is satisfactory, the actual implants are inserted and the wound is closed. A cemented monobloc humeral stem was used in all cases for 2 reasons: 1) All our patients are osteopenic to a certain extent and aggressive broaching (for the press-fit stem) may result in a periprosthetic fracture and 2) The press-fit humeral stem is thicker in diameter and some of our patients are unable to accommodate it. In all cases, the cement was mixed in a bowl and hand-packed into the humeral canal. Vacuum mixing and pressurisation techniques were not used as there is currently no evidence to demonstrate their superiority.
2.2. Assessment
All patients were assessed pre- and post-operatively according to the 100-point modified Constant–Murley shoulder score.10 The Constant Score was further analysed according to its subcomponents of pain, abduction strength and range of motion. All assessments were performed by physiotherapists thus allowing for independent assessment of the patients without bias from the operating surgeon.
In order to determine the change in COR, plain AP radiographs of the shoulder were taken pre- and post-operatively. The radiographs were taken with the patients in a supine position and the beam centred over the shoulder. On the radiographs, a “circle of best fit” is drawn over the humeral head (pre-op) and glenosphere (post-op) (Figs. 1 and 2) and the center of the circle is designated as the COR.9 A line is drawn from the COR to the most lateral tip of the acromion and subsequently divided into its horizontal and vertical components (Figs. 1 and 2). The difference between the pre- and post-operative horizontal components represents the amount of medialisation achieved and the difference between the vertical components represents the amount of distalisation achieved. This allows for verification of the biomechanical changes after a reverse shoulder replacement and to establish a simple method for measuring the change in the COR.
Fig. 1.
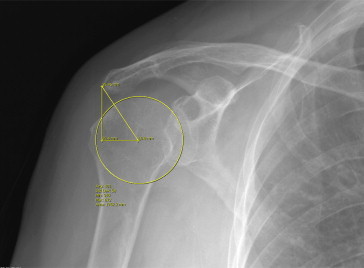
A “circle of best fit” is drawn over the native humeral head and the centre of the circle is determined. A line is then drawn from the centre of the circle to the lateral tip of the acromion and the line is divided into its vertical and horizontal components.
Fig. 2.
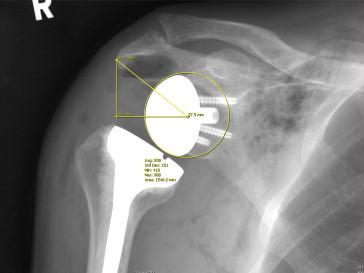
The “circle of best fit” is now drawn over the glenoid component instead. The horizontal and vertical components are determined and compared with the original COR.
2.3. Statistical analysis
A paired, 2-tailed Student T test was used for all analyses. p-Values of less than 0.05 are considered significant. All statistical analyses were carried out using Statistical Package for the Social Sciences (SPSS) version 17.0.
3. Results
All patients attended the pre-operative assessment and returned for all the follow-ups, except for 2 patients who did not attend the follow-up at 24 months. One patient developed wrist drop from traction injury to the posterior cord of the brachial plexus and although the wrist drop resolved after 12 months, she still has decreased shoulder mobility. At the time of writing, all implants remained stable and none of the shoulders required revision. There was no radiological evidence of scapula notching.
The average pre-operative Constant Score was 24.7 points. Post-operatively, there was progressive improvement and at 24 months the Constant Score was 52.5 points (p = 0.002) (Table 1). Significant improvements in flexion and abduction were observed as well. Prior to surgery, the range of flexion and abduction were 59.8 and 47.5°, respectively. At 24 months post-surgery, the average flexion increased to 106° (p = 0.001) and mean abduction of 95.8° (p = 0.001) was achieved (Table 2).
Table 1.
Pre- and post-operative Constant Score.
| Patient | Constant score (pre-op) | Constant score (3 months) | Constant score (6 months) | Constant score (1 year) | Constant score (2years) |
|---|---|---|---|---|---|
| 1 | 15.5 | 48 | 72 | 69 | 31 |
| 2 | 28 | 67 | 80 | 79 | 74 |
| 3 | 22.5 | 57 | 57.5 | 61 | 44 |
| 4 | 7 | 31 | 25 | 25 | 43 |
| 5 | 14.5 | 24 | 32.5 | 57 | 63 |
| 6 | 40 | 24 | 45 | 39.5 | Lost to f/u |
| 7 | 16.5 | 53 | 72 | 72 | 83 |
| 8 | 43 | 30.5 | 66 | 71 | Lost to f/u |
| 9 | 16.5 | 8 | 11.5 | 25 | 27.5 |
| 10 | 43.5 | 12.5 | 38 | 40.5 | 54.5 |
| Mean | 24.7 | 35.5 | 49.95 | 53.9 | 52.5 |
| p-Valuea | 0.22 | 0.008 | 0.003 | 0.002b | |
p-Values are derived after comparison of post-operative scores with pre-operative scores.
Paired T-test used for statistical analysis.
Table 2.
Subcomponents of Constant Score.
| Pre-op | Post-op (3 months)a | Post-op (6 months) | Post-op (1 year) | Post-op (2 year)b | |
|---|---|---|---|---|---|
| Flexion (°) | 59.8 | 88 (p = 0.127) | 110.4 (p = 0.002) | 114.5 (p = 0.001) | 106 (p = 0.001) |
| Abduction (°) | 47.5 | 69.2 (p = 0.161) | 95.1 (p = 0.003) | 101.7 (p = 0.001) | 95.8 (p = 0.001) |
| Internal rotation (points) | 3.6 | 1.6 (p = 0.128) | 3.2 (p = 0.726) | 4.2 (p = 0.604) | 4.8 (p = 0.262) |
| External rotation (points) | 3.6 | 5.2 (p = 0.335) | 6.4 (p = 0.089) | 7.2 (p = 0.038) | 6.5 (p = 0.012) |
| Abduction strength (lbs) | 0.9 | 2.1 (p = 0.427) | 5.7 (p = 0.015) | 6.4 (p = 0.012) | 5.4 (p = 0.026) |
| Pain score (points) | 5.4 | 9 (p = 0.035) | 10.95 (p = 0.007) | 10.5 (p = 0.006) | 11.3 (p = 0.005) |
p-Values are derived after comparison of post-operative scores with pre-operative scores.
Paired T-test used for statistical analysis.
Subcomponents of the Constant Score were further analysed and with the exception of internal rotation, significant improvements were achieved for all other components at 24 months. There was a drastic reduction in shoulder pain after the surgery with pain control improving from 5.4 points pre-operatively to 11.3 points (p = 0.005) at the end of follow-up (Table 2). Similarly, the abduction strength had increased from 0.9 lbs to 5.4 lbs (p = 0.012) and the external rotation score improved to 6.5 points (p = 0.038) post-operatively (Table 2).
Radiological measurements indicated that the COR had been medialised by 20.17 mm (p = 0.001) after the surgery but no significant distalisation was achieved (Table 3).
Table 3.
Pre- and post-operative distance between the COR and the acromion (mm).
| Patient | Pre-op medial-lateral | Post-op medial-lateral | Pre-op cranial-caudal | Post-op cranial-caudal |
|---|---|---|---|---|
| 1 | 16.5 | 37.5 | 28.5 | 29.7 |
| 2 | 10.2 | 31.2 | 33.2 | 46.8 |
| 3 | 11.9 | 31.4 | 22.5 | 26.4 |
| 4 | 19.8 | 42.9 | 30.9 | 29.5 |
| 5 | 29.3 | 40.7 | 22.5 | 24.5 |
| 6 | 16.4 | 38.9 | 26.5 | 29.5 |
| 7 | 20.3 | 44 | 25 | 21.2 |
| 8 | 6.7 | 37.7 | 40.8 | 32.3 |
| 9 | 21.4 | 28.2 | 23.1 | 33.8 |
| 10 | 9.7 | 31.4 | 37.6 | 36.8 |
| Mean | 16.22 | 36.39 | 29.06 | 31.05 |
| p-Valuea | 0.001 | 0.357 | ||
p-Values are derived after comparison of post-operative scores with pre-operative scores.
4. Discussion
Reverse shoulder replacement is a relatively new procedure locally and since its introduction in 2005,4 it has become increasingly popular due to its expanding indications. This study examines the functional outcomes of an Asian population after RSA and in addition, it introduces a novel method of measuring changes in the COR through the use of radiographs.
In concurrence with previous studies, significant relief of pain and improvements in function and strength are achieved post-operatively.2,3,5–8 This is reflected by the progressive increase in the Constant Scores after the procedure. Ideally, our outcomes should be comparable to other published studies but in comparison with the results of Wall et al and Sirveaux et al, the post-operative Constant Scores in this study are significantly lower despite similar patient demographics.3,8 A closer comparison revealed that the results of this study were lower than anticipated across all segments of the Constant Score rather than a particular segment. One patient had a low Constant Score due to brachial plexus injury (Patient 9). Another patient has cognitive impairment secondary to dementia (Patient 4) and therefore the low scores may not be reflective of her shoulder function. Given our small sample size, the inclusion of both patients is likely to have a more significant adverse effect on our scores. There is a slight decrease in the Constant Scores at 24 months which is due to 3 patients (Patients 1, 2 and 3) who had early deterioration in their scores at the latest follow-up. The first patient (Patient 1) had more than 50% decline in his shoulder function due to pain resulting from cervical radiculopathy. He also developed iatrogenic peripheral neuropathy secondary to chemotherapy for the treatment of multiple myeloma. There were no signs and symptoms suggestive of infection and no radiological evidence of fracture, implant loosening or metastatic disease. The Constant Score of the second patient (Patient 2) decreased by 5 points at 24 months but it may not be clinically important.11 The last patient returned for functional assessment of her shoulder at 24 months but did not attend the follow-up appointment with her surgeon.
Several studies have shown that internal rotation of the shoulder remains poor despite reverse shoulder replacement.5,12 The exact causes remain unknown but it may be due to alterations in the biomechanics of the deltoid, changes in rotational moment arm of the subscapularis and the design of the prosthesis.5,12 Hence, the outcome for this study is consistent with the existing literature. On the other hand, several authors have found that restoration of shoulder external rotation post-surgery is dependent on the quality and integrity of the teres minor.3,5,13 Given the importance of teres minor, it is necessary to assess it properly and identify any pathology prior to surgery since better outcomes may be achieved with a combined RSA and latissimus dorsi and teres major tendon transfer.14 Unfortunately, there was no documentation regarding the condition of the teres minor in this study. Hence, despite an improvement in shoulder external rotation post-surgery, we are unable to associate the improvement to the condition of the teres minor.
The success of the reverse shoulder is attributed to its biomechanical principle of medialising and distalising the center-of-rotation (COR) of the shoulder joint.2,5,9 Saltzman et al have shown in their series that the Delta III reverse shoulder prosthesis significantly medialises and distalises the COR post-operatively.9 However, there are currently no standardized methods of determining the change in COR pre- and post-operatively and furthermore, most studies on RSA do not include radiological assessments.
The COR was determined using Saltzman's “circle of best fit” technique but the lateral edge of acromion was used as our reference point instead.9 This was because we found the most lateral edge of the acromion to be a highly consistent reference point that is easy to determine with low inter-observer variability and the method described by Saltzman et al required a standardised template.9 Since both the pre-operative and post-operative radiographs are magnified to a similar extent this method of measurement avoids errors due to magnification. However, the differences in projection of the acromion may result in variability of the reference point. Hence, multiple post-operative radiographs can be used to improve the accuracy of the measurements.
Using our method of measurement, we showed that there is significant medialisation of the shoulder center for all patients after surgery. However, this method also showed that there was inadequate distalisation of the COR in our patients. To achieve maximal distalisation, the metaglene needs to be positioned as inferiorly as possible on the glenoid surface but this may not be achievable due to poor bone stock or bone loss from the disease process. In addition, due to the smaller glenoid size of Asian females, the metaglene may have to be positioned more superiorly than ideal, in order to prevent extraosseous placement of the inferior baseplate screw.15 Secondly, the amount of post-operative distalisation attainable is also influenced by the chronicity and the severity of pre-operative humeral head migration. Therefore, in patients with severe and chronic superior migration of the humeral head, distalisation of the prosthesis may not be possible. Although, distalisation of the prosthesis theoretically increases the tension of the deltoid muscle and improves stability, the clinical significance is uncertain and the current literature has yet examined this issue.2,5,9
5. Conclusion
Due to our ageing population, there will be increasing numbers of reverse shoulders being performed here and with experience, indications will be expanded to include revision arthroplasty, proximal humerus fractures and irreparable cuff tears. This study serves as a pilot for future studies with longer follow-ups and larger patient population. Further studies on survivalship and RSA performed for other indications are required as well.
Conflicts of interest
All authors have none to declare.
References
- 1.Grammont P.M., Trouilloud P., Laffay J.P., Deries X. Etude et réalisation d’une nouvelle prothèse d’épaule. Rhumatologie. 1987;10:407–418. [Google Scholar]
- 2.Smithers C.J., Young A.A., Walch G. Reverse shoulder arthroplasty. Curr Rev Musculoskelet Med. 2011 Dec;4:183–190. doi: 10.1007/s12178-011-9097-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sirveaux F., Favard L., Oudet D., Huquet D., Walch G., Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86:388–395. doi: 10.1302/0301-620x.86b3.14024. [DOI] [PubMed] [Google Scholar]
- 4.National University Hospital . 2005. Asia First’s Delta Reversed Shoulder Joint Replacement.http://www.nhgiplc.com/files/medicalResearch/Shoulder%20Joint%20Replacement.pdf [Google Scholar]
- 5.Boileau P., Watkinson D.J., Hatzidakis A.M., Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14:147S–161S. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Cuff D., Pupello D., Virani N., Levy J., Frankle M. Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency. J Bone Joint Surg Am. 2008 Jun;90:1244–1251. doi: 10.2106/JBJS.G.00775. [DOI] [PubMed] [Google Scholar]
- 7.Werner C.M., Steinmann P.A., Gilbart M., Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005 Jul;87:1476–1486. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]
- 8.Wall B., Nové-Josserand L., O'Connor D.P., Edwards T.B., Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007 Jul;89:1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 9.Saltzman M.D., Mercer D.M., Warme W.J., Bertelsen A.L., Matsen F.A., 3rd A method for documenting the change in center of rotation with reverse total shoulder arthroplasty and its application to a consecutive series of 68 shoulders having reconstruction with one of two different reverse prostheses. J Shoulder Elbow Surg. 2010 Oct;19:1028–1033. doi: 10.1016/j.jse.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 10.Constant C.R., Gerber C., Emery R.J., Søjbjerg J.O., Gohlke F., Boileau P. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg. 2008 Mar–Apr;17:355–361. doi: 10.1016/j.jse.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 11.Kukkonen J., Kauko T., Vahlberg T., Joukainen A., Aärimaa V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elbow Surg. 2013 Dec;22:1650–1655. doi: 10.1016/j.jse.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 12.Herrmann S., König C., Heller M., Perka C., Greiner S. Reverse shoulder arthroplasty leads to significant biomechanical changes in the remaining rotator cuff. J Orthop Surg Res. 2011 Aug 16;6:42. doi: 10.1186/1749-799X-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simovitch R.W., Helmy N., Zumstein M.A., Gerber C. Impact of fatty infiltration of the teres minor muscle on the outcome of reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2007 May;89:934–939. doi: 10.2106/JBJS.F.01075. [DOI] [PubMed] [Google Scholar]
- 14.Boileau P., Rumian A.P., Zumstein M.A. Reversed shoulder arthroplasty with modified L'Episcopo for combined loss of active elevation and external rotation. J Shoulder Elbow Surg. 2010 Mar;19:20–30. doi: 10.1016/j.jse.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 15.Ji J.H., Jeong J.Y., Song H.S. Early clinical results of reverse total shoulder arthroplasty in the Korean population. J Shoulder Elbow Surg. 2013 Aug;22:1102–1107. doi: 10.1016/j.jse.2012.07.019. [DOI] [PubMed] [Google Scholar]


