Abstract
Introduction. Guidelines advocate surveillance of vascular access to reduce incidences of thrombosis. However, the value of online vascular access flow monitoring is still under debate.
Methods. Through a systematic literature search, the effect of online access flow surveillance combined with pre-emptive intervention on thrombosis frequency is reviewed.
Results. Due to methodological differences, adequate comparison of the individual study results is not possible. Moreover, the methodological quality of most of the included studies is not suitable for an adequate statistical analysis of the results.
Conclusion. Until now, there is no conclusive evidence that online access flow evaluation has a significant effect on the rate of thrombosis. Future large-scale studies with adequate study design, adequate surveillance and intervention protocols and, possibly, better pre-emptive intervention alternative(s) are necessary.
Keywords: access survival, vascular access flow, vascular access surveillance, vascular access thrombosis, vascular access
Introduction
It has been estimated that in chronic haemodialysis patients, vascular access morbidity is responsible for 25% of all hospital admissions [1]. The main cause of dysfunction of arteriovenous grafts (AVG) and arteriovenous fistula (AVF) is stenosis (and subsequent thrombosis), which is primarily related to the vascular remodelling and adaptation to high-flow conditions. The rationale for implementing a vascular access surveillance programme is that timely detection of stenosis combined with either radiological and/or surgical pre-emptive intervention could reduce thrombotic occlusive events and may prolong access life.
The recently updated K/DOQI clinical practice guidelines for vascular access [2] and the European Best Practice Guidelines on Vascular Access [3] advocate such surveillance programmes. These guidelines state that monitoring for stenosis during dialysis treatment (online monitoring) is preferred compared to Duplex ultrasound or magnetic resonance angiography (MRA) monitoring for practical and economical reasons. Several online monitoring tools are available, of which access flow (Qa) monitoring is generally considered as the best surveillance method [2–4]. Online Qa evaluation is defined as measurement of access flow using a technique that is inherently linked to the presence of the extracorporeal circulation during haemodialysis treatment. A Qa <600 ml/min (AVG), a Qa <400 ml/min (AVF) or a Qa decline of >25% versus previous measurement (AVG) is an indication for pre-emptive intervention [2]. Whether Qa surveillance can prolong access survival is currently unproven. However, the guidelines state that thrombosis frequency is an important outcome parameter as well. Almost 60% of patients cite access thrombosis as one of the most feared complications associated with haemodialysis vascular access, ranking it second only to pain [5]. Moreover, a dysfunctional access (even before thrombosis occurs) may result in less optimal dialysis [6].
However, despite guideline recommendations, there is still discussion [7–10] on the benefits of online Qa surveillance in dialysis patients.
With the help of a systematic literature search, we provide an overview of all studies that compared online Qa surveillance combined with pre-emptive intervention to suggested [2,3] alternative or conservative surveillance tools and the effect on thrombosis frequency.
Methods
An electronic database search was carried out using Medline (Pubmed). As online vascular access flow measurement techniques were not introduced before 1995, the search was limited to the time frame between January 1995, till September 2007. Search terms were ‘Vascular access flow OR Vascular access monitoring OR Vascular access surveillance OR Preemptive intervention AND Vascular access thrombosis OR Vascular access occlusion’. Only publications in English were included. The outcome measure was the number of occlusions per patient per year. Reference lists from all relevant review articles were searched by hand. All such studies were included that compared none or different surveillance techniques for surveillance with online Qa surveillance. Included participants were male and female adult patients (age >18 years) on chronic haemodialysis for end-stage renal disease with both AVG and AVF.
Results
Description of studies
Trials identified.
In total, 524 articles were retrieved. Four hundred ninety articles were eliminated using title and abstract. The remaining 34 articles were fully assessed and 8 were finally included for the review.
Excluded studies
A total of 26 studies were excluded after reading the entire manuscript (Table 1). The reasons for excluding trials were
Table 1.
Excluded articles after full assessment
| Study ID | Reason for exclusion |
|---|---|
| Besarab [7] | Review |
| Paulson [8] | Review |
| Sands [9] | Review |
| Work [10] | Review |
| Arbabzadah [11] | Evaluation of AVG that clot despite online Qa surveillance and the outcome of radiological thrombectomy |
| Bosman [12] | Study whether high dynamic venous pressure coincides with low AVG flow, measured by the ultrasound dilution technique |
| Cayco [13] | Comparison of a surveillance programme based on dynamic venous pressure with a historical group during which no surveillance was applied, in relation to AVG thrombosis incidence |
| Cinat [14] | Evaluation of the patency, complications and predictive factors of patency for AVG |
| Dember [15] | Comparison between prophylactic repair of AVG stenosis based on static venous pressure and repair at the time of thrombosis, in relation to graft survival |
| Dossabhoy [16] | Replication of data from other study [36] |
| Frinak [17] | Sensitivity and specificity of a dynamic venous access ratio test for access surveillance |
| Garland [18] | Review (Qa measurement by ultrasound dilution the standard of care for access surveillance?) |
| Goldstein [19] | Age of participants <18 years |
| Lumsden [20] | Prospective randomized trial to compare patients who underwent PTA for AVG (stenosis >50%) with a control group that received no intervention, towards AVG survival. Surveillance tool: duplex ultrasound |
| Magnesco [21] | Comparison of two online Qa measurement techniques |
| Maya [22] | Comparison of outcomes of elective angioplasty between AVF and AVG |
| Neyra [23] | Evaluation of the predictive value of the Qa decrease towards thrombosis risk |
| Plantinga [24] | Effect of clinic vascular access monitoring practices towards clinical outcomes in haemodialysis patients |
| Roberts [25] | Study towards the value of a surveillance programme based on measuring venous resistance, regarding AVG patency and survival |
| Safa [26] | To determine the value of a haemodialysis graft surveillance programme in reducing the incidence of AVG thrombosis and prolonging graft patency by means of pre-emptive intervention (PTA) of graft-related stenoses (no online Qa surveillance applied) |
| Sands [27] | Review |
| Sands [28] | Effect of pre-emptive intervention towards access survival. No online Qa surveillance used |
| Singh [29] | Comparison predictive accuracy static venous pressure, dynamic venous pressure and access flow in determining subsequent graft thrombosis |
| Tanuma [30] | Evaluation of the long-term results of vascular access, in particular the effects of PTA |
| Tessitore [31] | Predictive value of online Qa surveillance in AVF towards thrombosis, and sensitivity towards stenosis detection |
| Tonelli [32] | Review |
AVF = arteriovenous fistula; AVG = arteriovenous graft; Qa = vascular access flow.
age of participants <18 years (1) [19];
analyses focused only on sensitivity of Qa surveillance (4) [23,24,29,31];
no online Qa surveillance used (8) [13,15,17,20,22, 25,26,28];
replication of data from other studies (1) [16];
study regarding the effect of percutaneous transluminal angioplasty (PTA) (1) [30];
evaluation of AVG which thrombosed despite Qa surveillance (1) [11];
study evaluating the relation of high dynamic venous pressure and low Qa in AVG (1) [12];
prospective evaluation of AVG patency (1) [14] and
comparison of two online Qa measurement techniques (1) [21].
Included studies
The remaining eight trials and their results are presented in Table 2. A significant overall (AVF and AVG) decline in thrombosis was reported four times [33,37,38,40]. Five trials reported a thrombosis reduction in AVF [34,35,38–40], of which two were significant [38,40]. A thrombosis decline in AVG was reported four times [34,35,38,40], of which one was not significant [38]. An increase in AVG thrombosis was reported once [36]. The first choice for pre-emptive intervention was PTA in all eight trials. PTA was executed in the case of stenosis with ≥50% area reduction. Three studies [33–35] reported surgery used for pre-emptive intervention when PTA was not feasible. All studies reported an increase in radiological procedures. Despite the significant increase in radiological procedures, two studies [35,40] reported a cost reduction during the online Qa surveillance period compared to the control group(s).
Table 2.
Study design and online Qa surveillance results expressed in thrombosis/patient-year
| Patient numbers | Thrombosis/patient-year | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall (AVF and AVG) | AVF | AVG | ||||||||
| Author | Year | Study design | Control | Qa surveillance | Control | Qa surveillance | Control | Qa surveillance | Control | Qa surveillance |
| Houben [33] | 2003 | Prospective observational | 29 | 25 | 0.62 | 0.17 (P = 0.032) | – | – | – | – |
| Lok [34] | 2003 | Prospective sequential observational | 451 | Same as control | – | 0.12 | 0.1 (P = ns) | 0.52 | 0.35 (P = 0.034) | |
| McCarley [35] | 2001 | Prospective sequential observational | 132 | Same as control | – | – | 0.14/0.15a | 0.07 (P = ns/ P = ns) | 0.71/0.67a | 0.16 (P < 0.001/ P < 0.001) |
| Ram [36] | 2003 | Randomized controlled | 34/35a | 32 | – | – | – | – | 0.68/0.5a | 0.91 (P = unknown) |
| Sands [37] | 1999 | Randomized controlled | 40 | 63 | 1.25/0.303a | 0.059 (P < 0.01/ P < 0.05) | – | – | – | – |
| Schwab [38] | 2001 | Prospective observational, historic control | – | 42 | 0.25 | 0.16 (P < 0.05) | 0.16 | 0.07 (P < 0.05) | 0.3 | 0.22 (P = ns) |
| Shahin [39] | 2005 | Prospective observational, historic control | 146 | 76 | – | – | 0.26 | 0.21 (P = ns) | – | – |
| Wijnen [40] | 2006 | Retrospective | 119 | 117 | 0.63 | 0.25 (P = 0.000) | 0.21 | 0.09 (P = 0.022) | 1.14 | 0.45 (P = 0.000) |
AVF = arteriovenous fistula, AVG = arteriovenous graft, Qa = vascular access flow. aThree trials had two control groups: McCarley [35], no monitoring/dynamic venous pressure monitoring; Ram [36], clinical criteria/quarterly duplex ultrasound assessment; Sands [37], no monitoring/static venous pressure monitoring.
All studies used the same pre-emptive intervention(s) in the control group and the Qa surveillance group. The referral for intervention used in the control groups was either based on conservative, often not standardized, surveillance parameters (inspection, palpation, auscultation and Kt/V) [39,40] or other surveillance tools (venous (static) pressure recordings [35,37,38] and duplex ultrasound [34,36]). The only exception was the study by Hoeben et al. [33]. They compared two groups with exactly the same surveillance protocol, in which only one group had pre-emptive intervention. In the control group, no timely intervention took place after positive Qa criteria.
Methodological quality of the studies
The allocation concealment assessment using the Cochrane scoring system revealed two randomized controlled trials with a grade B score (unclear concealment) [36,37]. The remaining 6 trials [33–35,38–40] were all non-randomized controlled trials (Table 2).
Discussion
Besides the fact that the methodological quality of most of the included studies is not suitable for an adequate statistical analysis of the results presented in Table 2, there are some other important issues retrieved from the studies that illustrate that an adequate comparison is not possible.
Although seven out of eight studies reported a thrombosis decline using online Qa monitoring, not all of the results were significant. The only trial that reports a higher thrombosis frequency in AVG when compared to the control group [36] has an important caveat: referral for angiography was only indicated when Qa was <600 ml/min, neglecting the 20–25% Qa decrease. In the current guidelines, both the absolute flow and the percentual reduction compared to previous flow measurements are used as indicators for intervention [2,3]. Waiting for Qa to drop beneath an absolute flow of 600 ml/min is questionable because a drop of >25% seems to be more sensitive towards stenosis compared to an absolute flow of <600 ml/min [23,29]. Only a few papers reported the time of measurement during dialysis and none described the haemodynamic circumstances during which Qa was measured. Comparing a Qa result measured during normal blood pressure to a Qa result measured during low blood pressure may result in a false positive Qa decline (Equation (1)) [41]. The factors influencing access flow in arteriovenous graft are given in the following equation:
| (1) |
where MAP is the mean arterial pressure, RART is the resistance feeding artery, RAA is the resistance arterial anastomosis, RGRAFT is the resistance graft, RVA is the resistance venous anastomosis and RVEIN is the resistance outflow vein.
In the majority of haemodialysis patients, haemodynamics are far from stable. Rehman et al. [42] concluded that in the majority of patients, Qa measurements can be performed up to 2.5 h from the start of dialysis treatment, but in patients with a decreased mean arterial pressure (MAP) of >15%, these authors advise to perform Qa measurement in the first 90 min after starting haemodialysis or postpone it to another treatment session when MAP is more stable.
All trials used the reference technique (saline dilution) to measure Qa; however, it is important to realize that using a different and less accurate technique to measure Qa may cause severe Qa decline to be missed or unnecessary interventions. The trials that studied reproducibility of different online access flow measurement techniques identified significant differences [43,44]. Considering these differences in accuracy, it is reasonable to imagine that the use of a less accurate Qa measurement device may result in unnecessary interventions and severe Qa decline to be missed, although no study has yet addressed this issue.
An important advantage of Qa monitoring, i.e. the ability to screen the whole vascular access circuit, is often overlooked (Figure 1). Only two out of eight retrieved trials [33,39] reported the segment of the access that was screened during angiography (arterial anastomosis and venous segment). The occurrence of arterial inflow stenosis is under-recognized and may be the primary problem of 20–30% of dysfunctional grafts [9]. However, radiological evaluation often primarily focuses on outflow pathology. In a recent study [45], the value of angiographic evaluation of the whole vascular access circuit was shown. Patients were referred for angiography when Qa was <600 ml/min or Qa decreased by >25%. Overall inflow stenosis was diagnosed in 77/223 (35%) of cases (40% in arteriovenous fistula (AVF), 29% in AVG). Based on these results, the authors conclude that angiographic evaluation of access inflow should also be performed if patients are referred based on the results of Qa monitoring.
Fig. 1.
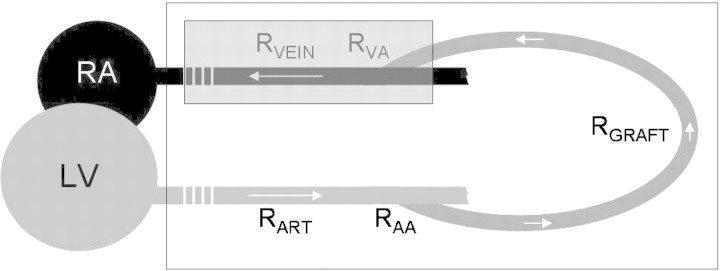
Schematic rendering of resistances in the vascular access graft circuit. RA = right atrium, LV = left ventricle, RART = resistance feeding artery, RAA = resistance arterial anastomosis, RGRAFT = resistance graft, RVA = resistance venous anastomosis, RVEIN = resistance outflow vein.  Stenosis detection span of control of vascular access flow monitoring.
Stenosis detection span of control of vascular access flow monitoring.  Stenosis detection span of control of static intra access pressure ratio monitoring.
Stenosis detection span of control of static intra access pressure ratio monitoring.
Only one study [33] reported the maximum time (8 weeks) it took to intervene after the reached cut-off value. They reported that five patients developed thrombosis before the scheduled pre-emptive intervention (total number of patients included was 86). In our own unit we schedule patients in the course of a week after positive Qa criteria. Even then, when Qa decline is severe, patients are scheduled in the course of 2 days for pre-emptive intervention. Although no study has yet addressed this issue, we advocate that intervention should take place in the course of 1 or 2 weeks after the identification of positive Qa criteria to prevent unnecessary thrombosis.
Final reflections
There is of course some evidence and rationale supporting the recommendations of the K/DOQI guidelines and the European Best Practice Guidelines that online Qa surveillance is the preferred surveillance tool for stenosis detection when compared to the described alternatives. Although observation of clinical signs (e.g. prolonged bleeding) should not be abandoned, online Qa measurement has been shown to be more accurate in identifying significant stenosis even before clinical symptoms appear [23,29]. Static venous pressure only registers outflow stenosis (Figure 1) and has less sensitivity compared to access flow [46]. Recirculation is recognized as a very late finding of stenosis, and therefore is surely not suitable for grafts because these will not remain patent at flows lower than the extracorporeal blood pump speed [47].
However, our review identified that, to date, there is no convincing evidence that online Qa surveillance, when combined with pre-emptive intervention, has a significant effect on the rate of thrombosis.
To obtain an unambiguous answer through future research, multiple factors need to be in place. These include choice and application of available guidelines and, importantly, successful PTA and/or surgical intervention. Post-PTA Qa measurement during angiography evaluates the effect of the intervention and might improve intervention sensitivity [48]. Also, it is known that PTA causes further injury to the vessel wall and may accelerate the disease process of intimal hyperplasia [49]. Alternative therapies in the treatment of intimal hyperplasia might improve vascular access patency. Regarding Qa measurement frequency, it has recently been suggested that frequency should be increased when compared to the suggested monthly measurement [50].
Another major drawback of the identified studies is that they are statistically inadequate to account for multiple related factors that include blood pressure measurement at the time of Qa measurement, angiographic evaluation of the vascular access circuit, time till intervention after positive Qa criteria, patient vascular access prehistory, age of the graft and adequate post-PTA flow increase. Also, one must take into consideration that most of these factors differ between AVG and AVF. Each group in a randomized controlled trial should have >200 patients, so only a large multi-centre study may provide statistically adequate data.
In conclusion, our review identified that there is no convincing evidence that online Qa surveillance, when combined with pre-emptive intervention, has a significant effect on the rate of thrombosis. Future large-scale studies with adequate study design, adequate surveillance and intervention protocols and possibly better pre-emptive intervention alternative(s) are necessary.
Conflict of interest statement. None declared.
References
- 1.Rayner HC, Pisoni RL, Bommer J, et al. Mortality and hospitalization in haemodialysis patients in five European countries: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS) Nephrol Dial Transplant. 2004;19:108–120. doi: 10.1093/ndt/gfg483. [DOI] [PubMed] [Google Scholar]
- 2.NKF-K/DOQI Clinical Practice Guidelines for Vascular Access: update. Am J Kidney Dis. 2006;48(Suppl S1):S176–S2471. doi: 10.1053/j.ajkd.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 3.Tordoir J, Canaud B, Haage P, et al. EBPG on vascular access. Nephrol Dial Transplant. 2007;22(Suppl 2):ii88–ii117. doi: 10.1093/ndt/gfm021. [DOI] [PubMed] [Google Scholar]
- 4.Lopot F, Nejedly B, Valek M. Vascular access monitoring: methods and procedures—something to standardize? Blood Purif. 2005;23:36–445. doi: 10.1159/000082009. [DOI] [PubMed] [Google Scholar]
- 5.Bay WH, Van Cleef S, Owens M. The hemodialysis access: preferences and concerns of patients, dialysis nurses and technicians, and physicians. Am J Nephrol. 1998;18:379–383. doi: 10.1159/000013380. [DOI] [PubMed] [Google Scholar]
- 6.Hakim RM, Breyer J, Ismail N, et al. Effects of dose of dialysis on morbidity and mortality. Am J Kidney Dis. 1994;23:661–669. doi: 10.1016/s0272-6386(12)70276-7. [DOI] [PubMed] [Google Scholar]
- 7.Besarab A. Access monitoring is worthwhile and valuable. Blood Purif. 2006;24:77–89. doi: 10.1159/000089442. [DOI] [PubMed] [Google Scholar]
- 8.Paulson WD. Access monitoring does not really improve outcomes. Blood Purif. 2005;23:50–56. doi: 10.1159/000082011. [DOI] [PubMed] [Google Scholar]
- 9.Sands JJ. Vascular access monitoring improves outcomes. Blood Purif. 2005;23:45–49. doi: 10.1159/000082010. [DOI] [PubMed] [Google Scholar]
- 10.Work J. Does vascular access monitoring work? Adv Ren Replace Ther. 2002;9:85–90. doi: 10.1053/jarr.2002.33520. [DOI] [PubMed] [Google Scholar]
- 11.Arbabzadeh M, Mepani B, Murray BM. Why do grafts clot despite access blood flow surveillance? Cardiovasc Intervent Radiol. 2002;25:501–505. doi: 10.1007/s00270-002-1963-4. [DOI] [PubMed] [Google Scholar]
- 12.Bosman PJ, Boereboom FT, Smits HF, et al. Pressure or flow recordings for the surveillance of hemodialysis grafts. Kidney Int. 1997;52:1084–1088. doi: 10.1038/ki.1997.432. [DOI] [PubMed] [Google Scholar]
- 13.Cayco AV, Abu-Alfa AK, Mahnensmith RL, et al. Reduction in arteriovenous graft impairment: results of a vascular access surveillance protocol. Am J Kidney Dis. 1998;32:302–308. doi: 10.1053/ajkd.1998.v32.pm9708617. [DOI] [PubMed] [Google Scholar]
- 14.Cinat ME, Hopkins J, Wilson SE. A prospective evaluation of PTFE graft patency and surveillance techniques in hemodialysis access. Ann Vasc Surg. 1999;13:191–198. doi: 10.1007/s100169900241. [DOI] [PubMed] [Google Scholar]
- 15.Dember LM, Holmberg EF, Kaufman JS. Randomized controlled trial of prophylactic repair of hemodialysis arteriovenous graft stenosis. Kidney Int. 2004;66:390–398. doi: 10.1111/j.1523-1755.2004.00743.x. [DOI] [PubMed] [Google Scholar]
- 16.Dossabhoy NR, Ram SJ, Nassar R, et al. Stenosis surveillance of hemodialysis grafts by duplex ultrasound reduces hospitalizations and cost of care. Semin Dial. 2005;18:550–557. doi: 10.1111/j.1525-139X.2005.00102.x. [DOI] [PubMed] [Google Scholar]
- 17.Frinak S, Zasuwa G, Dunfee T, et al. Dynamic venous access pressure ratio test for hemodialysis access monitoring. Am J Kidney Dis. 2002;40:760–768. doi: 10.1053/ajkd.2002.35687. [DOI] [PubMed] [Google Scholar]
- 18.Garland JS, Moist LM, Lindsay RM. Are hemodialysis access flow measurements by ultrasound dilution the standard of care for access surveillance? Adv Ren Replace Ther. 2002;9:91–98. doi: 10.1053/jarr.2002.33523. [DOI] [PubMed] [Google Scholar]
- 19.Goldstein SL, Allsteadt A, Smith CM, et al. Proactive monitoring of pediatric hemodialysis vascular access: effects of ultrasound dilution on thrombosis rates. Kidney Int. 2002;62:272–275. doi: 10.1046/j.1523-1755.2002.00414.x. [DOI] [PubMed] [Google Scholar]
- 20.Lumsden AB, MacDonald MJ, Kikeri D, et al. Prophylactic balloon angioplasty fails to prolong the patency of expanded polytetrafluoroethylene arteriovenous grafts: results of a prospective randomized study. J Vasc Surg. 1997;26:382–390. doi: 10.1016/s0741-5214(97)70031-4. [DOI] [PubMed] [Google Scholar]
- 21.Magnasco A, Bacchini G, Cappello A, et al. Clinical validation of glucose pump test (GPT) compared with ultrasound dilution technology in arteriovenous graft surveillance. Nephrol Dial Transplant. 2004;19:1835–1841. doi: 10.1093/ndt/gfh292. [DOI] [PubMed] [Google Scholar]
- 22.Maya ID, Oser R, Saddekni S, et al. Vascular access stenosis: comparison of arteriovenous grafts and fistulas. Am J Kidney Dis. 2004;44:859–865. [PubMed] [Google Scholar]
- 23.Neyra NR, Ikizler TA, May RE, et al. Change in access blood flow over time predicts vascular access thrombosis. Kidney Int. 1998;54:1714–1719. doi: 10.1046/j.1523-1755.1998.00145.x. [DOI] [PubMed] [Google Scholar]
- 24.Plantinga LC, Jaar BG, Astor B, et al. Association of clinic vascular access monitoring practices with clinical outcomes in hemodialysis patients. Nephron Clin Pract. 2006;104:c151–c159. doi: 10.1159/000094961. [DOI] [PubMed] [Google Scholar]
- 25.Roberts AB, Kahn MB, Bradford S, et al. Graft surveillance and angioplasty prolongs dialysis graft patency. J Am Coll Surg. 1996;183:486–492. [PubMed] [Google Scholar]
- 26.Safa AA, Valji K, Roberts AC, et al. Detection and treatment of dysfunctional hemodialysis access grafts: effect of a surveillance program on graft patency and the incidence of thrombosis. Radiology. 1996;199:653–657. doi: 10.1148/radiology.199.3.8637982. [DOI] [PubMed] [Google Scholar]
- 27.Sands JJ. A review of vascular access monitoring techniques: what works best? Nephrol News Issues. 2003;17:86–87. [PubMed] [Google Scholar]
- 28.Sands J, Miranda CL. Prolongation of hemodialysis access survival with elective revision. Clin Nephrol. 1995;44:329–333. [PubMed] [Google Scholar]
- 29.Singh N, Ahmad S, Wienckowski JR, et al. Comparison of access blood flow and venous pressure measurements as predictors of arteriovenous graft thrombosis. J Vasc Access. 2006;7:66–73. doi: 10.1177/112972980600700205. [DOI] [PubMed] [Google Scholar]
- 30.Tanuma Y. Efficacy of percutaneous transluminal angioplasty in the management of chronic hemodialysis patients. Hinyokika Kiyo. 2002;48:593–597. [PubMed] [Google Scholar]
- 31.Tessitore N, Bedogna V, Gammaro L, et al. Diagnostic accuracy of ultrasound dilution access blood flow measurement in detecting stenosis and predicting thrombosis in native forearm arteriovenous fistulae for hemodialysis. Am J Kidney Dis. 2003;42:331–341. doi: 10.1016/s0272-6386(03)00659-0. [DOI] [PubMed] [Google Scholar]
- 32.Tonelli M. Monitoring and maintenance of arteriovenous fistulae and graft function in haemodialysis patients. Curr Opin Nephrol Hypertens. 2004;13:655–660. doi: 10.1097/00041552-200411000-00012. [DOI] [PubMed] [Google Scholar]
- 33.Hoeben H, Abu-Alfa AK, Reilly RF, et al. Vascular access surveillance: evaluation of combining dynamic venous pressure and vascular access blood flow measurements. Am J Nephrol. 2003;23:403–408. doi: 10.1159/000074297. [DOI] [PubMed] [Google Scholar]
- 34.Lok CE, Bhola C, Croxford R, et al. Reducing vascular access morbidity: a comparative trial of two vascular access monitoring strategies. Nephrol Dial Transplant. 2003;18:1174–1180. doi: 10.1093/ndt/gfg122. [DOI] [PubMed] [Google Scholar]
- 35.McCarley P, Wingard RL, Shyr Y, et al. Vascular access blood flow monitoring reduces access morbidity and costs. Kidney Int. 2001;60:1164–1172. doi: 10.1046/j.1523-1755.2001.0600031164.x. [DOI] [PubMed] [Google Scholar]
- 36.Ram SJ, Work J, Caldito GC, et al. A randomized controlled trial of blood flow and stenosis surveillance of hemodialysis grafts. Kidney Int. 2003;64:272–280. doi: 10.1046/j.1523-1755.2003.00070.x. [DOI] [PubMed] [Google Scholar]
- 37.Sands JJ, Jabyac PA, Miranda CL, et al. Intervention based on monthly monitoring decreases hemodialysis access thrombosis. ASAIO J. 1999;45:147–150. doi: 10.1097/00002480-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Schwab SJ, Oliver MJ, Suhocki P, et al. Hemodialysis arteriovenous access: detection of stenosis and response to treatment by vascular access blood flow. Kidney Int. 2001;59:358–362. doi: 10.1046/j.1523-1755.2001.00498.x. [DOI] [PubMed] [Google Scholar]
- 39.Shahin H, Reddy G, Sharafuddin M, et al. Monthly access flow monitoring with increased prophylactic angioplasty did not improve fistula patency. Kidney Int. 2005;68:2352–2361. doi: 10.1111/j.1523-1755.2005.00697.x. [DOI] [PubMed] [Google Scholar]
- 40.Wijnen E, Planken N, Keuter X, et al. Impact of a quality improvement programme based on vascular access flow monitoring on costs, access occlusion and access failure. Nephrol Dial Transplant. 2006;21:3514–3519. doi: 10.1093/ndt/gfl424. [DOI] [PubMed] [Google Scholar]
- 41.Schneditz D, Fan Z, Kaufman A, et al. Stability of access resistance during haemodialysis. Nephrol Dial Transplant. 1998;13:739–744. doi: 10.1093/ndt/13.3.739. [DOI] [PubMed] [Google Scholar]
- 42.Rehman SU, Pupim LB, Shyr Y, et al. Intradialytic serial vascular access flow measurements. Am J Kidney Dis. 1999;34:471–477. doi: 10.1016/s0272-6386(99)70074-0. [DOI] [PubMed] [Google Scholar]
- 43.Lopot F, Nejedly B, Sulkova S, et al. Comparison of different techniques of hemodialysis vascular access flow evaluation. Int J Artif Organs. 2003;26:1056–1063. doi: 10.1177/039139880302601203. [DOI] [PubMed] [Google Scholar]
- 44.Wijnen E, Essers S, van Meijel G, et al. Comparison between two on-line reversed line position hemodialysis vascular access flow measurement techniques: saline dilution and thermodilution. ASAIO J. 2006;52:410–415. doi: 10.1097/01.mat.0000227680.67901.01. [DOI] [PubMed] [Google Scholar]
- 45.Asif A, Gadalean FN, Merrill D, et al. Inflow stenosis in arteriovenous fistulas and grafts: a multicenter, prospective study. Kidney Int. 2005;67:1986–1992. doi: 10.1111/j.1523-1755.2005.00299.x. [DOI] [PubMed] [Google Scholar]
- 46.Spergel, Holland J, Fadem S, et al. Static intra-access pressure ratio does not correlate with access blood flow. Kidney Int. 2004;66:1512–1516. doi: 10.1111/j.1523-1755.2004.00946.x. [DOI] [PubMed] [Google Scholar]
- 47.Wijnen E, Van Der Sande FM, Kooman JP, et al. Vascular access recirculation: setting a new detection method in the context of the overall utility of detection. Nat Clin Pract Nephrol. 2007;3:252–253. doi: 10.1038/ncpneph0453. [DOI] [PubMed] [Google Scholar]
- 48.Krivitski NM. Access flow measurement during surveillance and percutaneous transluminal angioplasty intervention. Semin Dial. 2003;16:304–308. doi: 10.1046/j.1525-139x.2003.16067.x. [DOI] [PubMed] [Google Scholar]
- 49.Ikizler TA, Himmelfarb J. Trials and trade-offs in haemodialysis vascular access monitoring. Nephrol Dial Transplant. 2006;21:3362–3363. doi: 10.1093/ndt/gfl562. [DOI] [PubMed] [Google Scholar]
- 50.White JJ, Ram SJ, Jones SA, et al. Influence of luminal diameters on flow surveillance of hemodialysis grafts: insights from a mathematical model. Clin J Am Soc Nephrol. 2006;1:972–978. doi: 10.2215/CJN.00580206. [DOI] [PubMed] [Google Scholar]


