Abstract
Polyneuropathy, organomegaly, endocrinopathy, monoclonal protein, skin changes (POEMS) syndrome is a systemic condition related to plasma cell dyscrasia. Increased vascular permeability is responsible for some of the hallmarks of this disorder that may include renal microangiopathy. Several lines of evidence suggest that vascular endothelial growth factor (VEGF) is central to the pathogenesis of POEMS syndrome. Thus, specifically targeting VEGF over-expression seems to be a promising treatment. Anti-VEGF therapies are yielding conflicting results. We report on a patient with POEMS syndrome treated with bevacizumab, an anti-VEGF monoclonal antibody. Sequential monitoring of serum VEGF showed sustained normalization of serum VEGF levels, without any beneficial effect on the patient's condition. Indications of this treatment should be chosen carefully.
Keywords: bevacizumab, microangiopathy, polyneuropathy organomegaly endocrinopathy monoclonal protein, skin changes syndrome, vascular endothelial growth factor
Introduction
Polyneuropathy, organomegaly, endocrinopathy, monoclonal protein, skin changes (POEMS) is a rare disease associated with plasma cell dyscrasia, which is generally lambda-chain restricted. High serum vascular endothelial growth factor (VEGF) levels have been included into the five major diagnostic criteria (polyneuropathy, monoclonal plasma cell-proliferative disorder, sclerotic bone lesions, Castleman's disease and elevated serum VEGF levels) of POEMS syndrome. Several lines of evidence suggest that VEGF is central to the pathogenesis of this paraneoplastic disorder: (i) whilst interleukin (IL) 6, tumour necrosis factor (TNF) α and IL-1β levels may or may not be elevated in POEMS syndrome, VEGF serum levels are always significantly elevated in this disease as compared to myeloma patients and control subjects [1], (ii) pathological changes in POEMS syndrome consist of microangiopathy combining neoangiogenesis and increased vascular permeability induced by excessive VEGF expression and (iii) there is a consistent relationship between serum VEGF levels and the activity of the disease before therapy, whilst a decrease or normalization of VEGF serum levels has been observed in patients experiencing remission after treatment with high-dose chemotherapy and autologous stem-cell transplantation (ASCT) [2]. Current therapeutic approaches in POEMS syndrome have mostly been aimed at the eradication of the plasma cell clone, using steroids, alkylating agents, ASCT or surgery and/or radiotherapy in the case of solitary plasmacytoma. Recent reports have highlighted that clinical improvement is better correlated with the drop in serum VEGF levels than with haematological remission [3]. Accordingly, another tempting approach to therapy in POEMS syndrome is to specifically target VEGF over-expression.
Case report
We report the case of a 57-year-old woman treated with bevacizumab, an anti-VEGF monoclonal antibody, as first line treatment for POEMS syndrome. The patient had a 24-month-long history of severe polyneuropathy, organomegaly, ascites, pleural effusion, skin pigmentation and papilloedema with a World Health Organization (WHO) status of 3. She displayed pulmonary hypertension and recent hearing loss. Cerebral magnetic resonance imaging (MRI) showed pachymeningitis. Moderate thrombocytosis (platelets count 480000/mm3) was evidenced. Serum immunoelectrophoresis revealed traces of a monoclonal IgA lambda protein. There was a 5-fold increase of free light lambda chains in the serum, without Bence-Jones proteinuria. Multiple myeloma and solitary plasmacytoma were ruled out by blood marrow smear, bone MRI and positron emission tomography (PET) scan. Renal features included hypertension, moderate renal failure (glomerular filtration rate 44 ml/min) and mild proteinuria (1 g/day). A renal biopsy showed microangiopathic lesions—endothelial cells swelling, capillary membrane double contours, widening of the subendothelial spaces and mesangiolysis—with negative immune-complex staining, which prompted the diagnosis of POEMS syndrome. Serum VEGF levels were above 4000 pg/ml (N: 62–707).
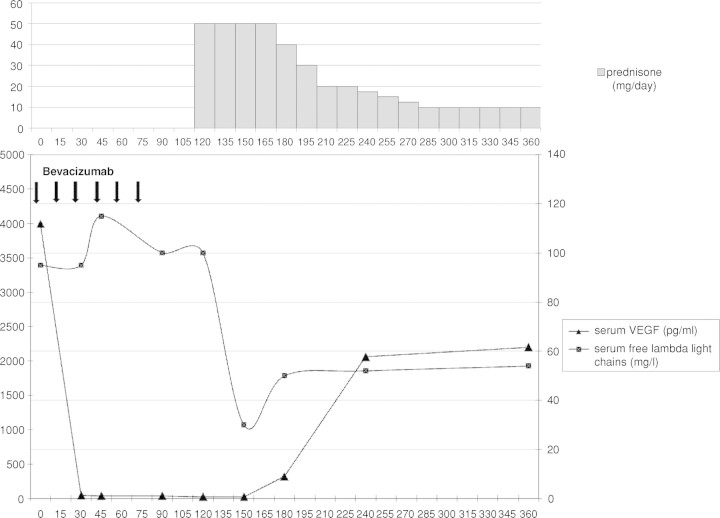
The patient received six courses of bevacizumab (5 mg/kg, q 14 days) with good tolerance. Serum VEGF levels dropped rapidly to a nadir of 40 pg/ml (Figure 1), but her clinical condition worsened unremittingly: 4 months after bevacizumab therapy, the patient displayed high output cardiac failure, severe pulmonary hypertension and bilateral pleural effusions culminating in acute respiratory distress syndrome. The patient received 1 mg/kg/day of prednisone along with intensive support care. The clinical course dramatically improved within 1 week. Steroids were tapered over a 6-month period and maintained at 10 mg/day. Over that period, clinical status improved steadily: complete clearance of pleural effusions (Figure 2), significant diminution of pulmonary hypertension and objective improvement in polyneuropathy. In parallel, free serum lambda chain levels fell from 118 to 38 mg/l and then stabilized at about 50 mg/l for up to 1 year on low-dose prednisone therapy. In sharp contrast, serum VEGF levels increased progressively to 2000 pg/ml (Figure 1).
Fig. 1.
Evolution of serum VEGF levels and free serum lambda light chains during bevacizumab and steroid therapy.
Fig. 2.
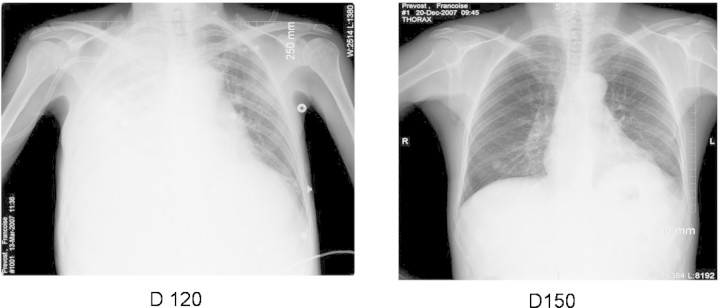
Complete resolution of pleural effusions 1 month after steroid therapy.
Discussion
We here report the case of a patient with POEMS syndrome treated with bevacizumab. In spite of complete VEGF blockade, normalization of serum VEGF levels failed to induce remission. So far, only seven reports are available to evaluate treatment with bevacizumab in POEMS syndrome. Two patients had previously been unsuccessfully treated by alkylating agents [4,5], one had relapsed after conventional chemotherapy [6] and one after bone marrow transplantation [7]. Another patient received both bevacizumab and cyclophosphamide simultaneously [8] and two were treated with bevacizumab before ASCT [9,10].
In all patients, VEGF blood levels dropped significantly with conflicting clinical outcomes: clinical condition worsened rapidly in three patients, leading to death in a few weeks, whilst the other four patients experienced clinical improvement, although long-term information is missing. Although VEGF is a likely pathogenic factor in POEMS syndrome, the discrepancy in response to serum VEGF blockade raises the question of the pathophysiological impact of the inhibition of this cytokine in this disease. Other cytokines such as IL-1β, IL-6 and TNF-α may contribute to the pathogenesis of POEMS syndrome, explaining that targeting VEGF alone can be ineffective, while prednisone—given its non-specific effect on cytokine release—can be effective. Alternatively, the contradictory effects of bevacizumab in these eight patients may depend on the duration of the disease. Indeed, the four patients who responded to bevacizumab therapy had a short duration of disease compared to the other four patients. It has been hypothesized that aberrant angiogenesis due to high VEGF levels could lead to abnormal vessels no longer sensitive to anti-VEFG therapy. Thus, a non-return point in the reversibility of blood vessel damage may explain different outcomes.
Some authors have suggested that the rapid decrease of VEGF levels after chronic VEGF over-expression could be deleterious. Straume et al. suggested that a sudden drop in VEGF may accelerate neurological damage and endothelial apoptosis, explaining the rapid decline of clinical condition in their patient [5]. In this journal, a French group [11] reported findings of thrombotic microangiopathy on renal biopsy in six patients treated with bevacizumab for cancer, suggesting a potential endothelial toxicity of bevacizumab. Thus, an abrupt drop in VEGF levels may aggravate endothelial lesions, explaining a potential worsening in patients with POEMS syndrome treated with bevacizumab.
Our case, along with the seven patients previously reported, sheds light on the complexity of the pathophysiology of POEMS syndrome. The beneficial impact of bevacizumab in four POEMS patients provides a proof of concept for VEGF blockade. This case report, which documents clinical worsening despite complete serum VEGF blockade, but dramatic improvement on steroids, clearly establishes that VEGF blockade should not be considered a panacea for treatment nor a reliable marker to predict remission in POEMS syndrome.
Acknowledgments
The authors would like to thank Dr Francis Gaches and Dr Françoise Rigal-Huguet for significant help to patient's diagnosis, and Mrs Félicie Pastore for editorial assistance.
Conflict of interest statement. MS contributed vital reagents and performed serum VEGF dosages. AM contributed to pathological analysis of the patient's renal biopsy. JG and AP contributed equally to the redaction of this report, under the supervision of DC.
References
- 1.Watanabe O, Arimura K, Kitajima I, et al. Greatly raised vascular endothelial growth factor (VEGF) in POEMS syndrome. Lancet. 1996;347:702. doi: 10.1016/s0140-6736(96)91261-1. [DOI] [PubMed] [Google Scholar]
- 2.Imai N, Kitamura E, Tachibana T, et al. Efficacy of autologous peripheral blood stem cell transplantation in POEMS syndrome with polyneuropathy. Intern Med. 2007;46:135–138. doi: 10.2169/internalmedicine.46.1713. [DOI] [PubMed] [Google Scholar]
- 3.Dispenzieri A, Lacy MQ, Hayman SR, et al. Peripheral blood stem cell transplant for POEMS syndrome is associated with high rates of engraftment syndrome. Eur J Haematol. 2008;80:397–406. doi: 10.1111/j.1600-0609.2008.01037.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Badros A, Porter N, Zimrin A. Bevacizumab therapy for POEMS syndrome. Blood. 2005;106:1135. doi: 10.1182/blood-2005-03-0910. [DOI] [PubMed] [Google Scholar]
- 5.Straume O, Bergheim J, Ernst P. Bevacizumab therapy for POEMS syndrome. Blood. 2006;107:4972–4973. doi: 10.1182/blood-2005-12-5045. author reply 4973–4974. [DOI] [PubMed] [Google Scholar]
- 6.Kanai K, Kuwabara S, Misawa S, et al. Failure of treatment with anti-VEGF monoclonal antibody for long-standing POEMS syndrome. Intern Med. 2007;46:311–313. doi: 10.2169/internalmedicine.46.6246. [DOI] [PubMed] [Google Scholar]
- 7.Samaras P, Bauer S, Stenner-Liewen F, et al. Treatment of POEMS syndrome with bevacizumab. Haematologica. 2007;92:1438–1439. doi: 10.3324/haematol.11315. [DOI] [PubMed] [Google Scholar]
- 8.Doffoel-Hantz V, Jaccard A, Sparsa A, et al. Bevacizumab therapy for Poems syndrome. Ann Dermatol Venereol. 2008;135:320–321. doi: 10.1016/j.annder.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 9.Dietrich PY, Duchosal MA. Bevacizumab therapy before autologous stem-cell transplantation for POEMS syndrome. Ann Oncol. 2008;19:595. doi: 10.1093/annonc/mdm602. [DOI] [PubMed] [Google Scholar]
- 10.Ohwada C, Nakaseko C, Sakai S, et al. Successful combination treatment with bevacizumab, thalidomide and autologous PBSC for severe POEMS syndrome. Bone Marrow Transplant. 2009;43:730–740. doi: 10.1038/bmt.2008.381. [DOI] [PubMed] [Google Scholar]
- 11.Izzedine H, Brocheriou I, Deray G, et al. Thrombotic microangiopathy and anti-VEGF agents. Nephrol Dial Transplant. 2007;22:1481–1482. doi: 10.1093/ndt/gfl565. [DOI] [PubMed] [Google Scholar]