Abstract
Hyponatremia affects nearly one in five of all hospitalized patients. Severe hyponatremia is associated with significant morbidity and mortality, and is therefore important to recognize. Prior reports have linked duloxetine with hyponatremia, but it is uncommon. In this case report, we describe a research subject taking duloxetine who developed severe symptomatic hyponatremia during glomerular filtration rate testing despite having undergone such testing uneventfully in the past.
Keywords: GFR, hyponatremia
Introduction
Hyponatremia (serum sodium < 135 mmol/L) is seen in 15–21% of hospitalized patients. Moderate to severe hyponatremia (serum sodium < 125 mmol/L), when it occurs, is often an iatrogenic occurrence during hospitalization with significant associated morbidity [1]. Seizures, cerebral edema and death resulting from cerebral edema have been described in some cases of water intoxication [5,6].
Hyponatremia occurs from a variety of pathogenic processes, including the use of medications which affect water metabolism. One such medication with reported hyponatremia is duloxetine, a selective serotonin reuptake inhibitor (SSRI) and selective norepinephrine reuptake inhibitor (SNRI) approved in the USA for treatment of major depressive disorder, diabetic neuropathic pain, stress urinary incontinence and fibromyalgia. We report here an instance of asymptomatic hyponatremia occurring during duloxetine treatment that became symptomatic during the course of a glomerular filtration rate (GFR) test that involved water loading the subject.
Case summary
A 48-year-old Caucasian woman with past medical history of systemic lupus erythematosus, type 2 diabetes mellitus, hypertension, migraine, gastroparesis, fibromyalgia, mitral valve prolapse, hypothyroidism and hyperprolactinemia was scheduled for an [125]I-iothalamate GFR testing as part of a research study. The participant consumed ~ 2 L of fluids at home following instructions from the staff recommending hydration before the test. She received five drops of super-saturated potassium iodide (SSKI) in 2 oz of water to block the thyroid uptake. At baseline, blood was collected for basic metabolic profile, liver function test and complete blood count. Blood and urine were collected to serve as background values to compare with the serial blood and urine tests during the iothalamate GFR testing. The participant was asked to drink additional water per the protocol based on the background urine specific gravity.
The GFR test was uneventful for the first 2 h. Then, the subject complained of acute onset of generalized headache described as ‘5–6 out of 10’ with nausea and vomiting. This was followed shortly afterwards by confusion. A Rapid Response Team procedure was activated. During this period, her heart rate was 50–60/min, blood pressure rose to 160–170 mmHg systolic and 90–108 mmHg diastolic, oxygen saturation registered 100% on room air and finger-stick blood glucose values were 99–102 mg/dL. An intravenous solution of 0.9% saline was initiated, and the subject was transferred to the Emergency Department for further management. During the GFR testing, an intake of 3300 mL of water and a urine volume of 1325 mL were recorded.
Her home medications included naratriptan, amitriptyline, cabergoline, propranolol, sitagliptin, meloxicam, hydroxychloroquine, pravastatin, lansoprazole, levothyroxine, vitamin D, azelastine, polyethylene glycol, aspirin and duloxetine. The serum sodium measured 3 months after the increase in the dose of duloxetine was 137 mmol/L.
In the Emergency Department, she had normal pupil reactivity, a supple neck, and normal pulmonary, cardiovascular and abdominal examinations. She had no peripheral edema. Neurological examination showed the patient to be responsive but confused with intact deep tendon reflexes.
Urine drug screen was negative. A chest X-ray was unremarkable. A computerized tomography (CT) scan of the brain showed diffuse cerebral edema with basal cistern effacement. No mass effect was noted.
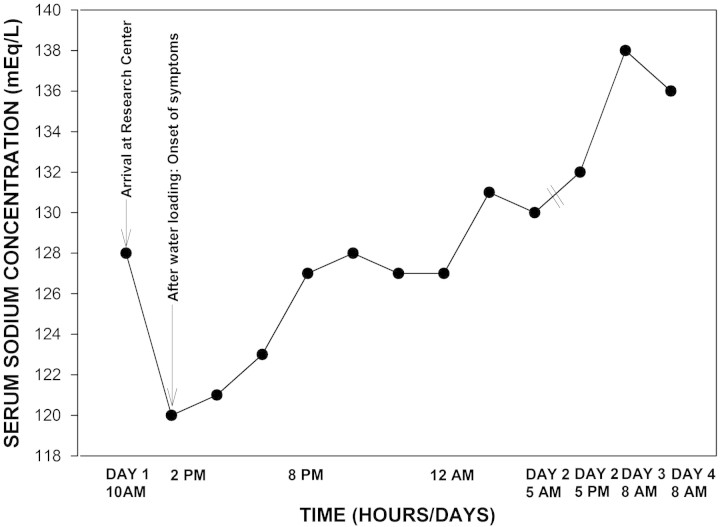
The serum sodium measured was 120 mmol/L. Her intravenous solution was altered to 3% hypertonic saline (212 mL of 3% saline = 109 mmol of sodium chloride), and she was administered furosemide 40 mg intravenously (IV), zofran 4 mg IV and lorazepam 1 mg IV. Serial serum sodium levels were checked, and the rate of hypertonic saline was adjusted accordingly. Symptoms and mental status improved with gradual increase in serum sodium (Figure 1). The serum sodium measured from the baseline blood before the GFR test was 128 mmol/L. The result was available later. She was discharged to home after 4 days with advice to taper the dose and then discontinue duloxetine. A follow-up serum sodium measurement after 2 weeks was 140 mmol/L.
Fig. 1.
Symptoms and mental status improved with gradual increase in serum sodium.
Discussion
GFR is considered the best measure of kidney function in health and disease [7]. In large clinical studies, [125]I-iothalamate has often been used to estimate GFR. The test requires water loading, multiple blood draws and 6–8 h of time [8]. Despite the significant water loading recommended to achieve the most accurate GFR results, hyponatremia has not been reported previously during GFR testing.
Renal capacity for free water excretion is up to 28 L/day [9]. As a result, under normal physiological conditions, hyponatremia rarely develops solely as a result of excess water intake. Our subject developed a precipitous drop of serum sodium to a hazardous level of 120 mEq/L during the GFR test.
Of note, our subject had undergone uneventful [125]I-iothalamate testing in the past without complications prior to receiving duloxetine. In previously reported cases of duloxetine-related hyponatremia, the time course of developing hyponatremia was acute as compared with our subject whose serum sodium was normal even after 6 months of duloxetine usage [2,10]. It is likely that the pre-admission water load specified in the GFR protocol provoked hyponatremia in our subject, which was worsened by the added water ingestion during the GFR procedure. Our patient illustrates the need for vigilance during water loading, even when well tolerated previously, especially when medications such as antidepressant and antipsychotic are in use. A stat serum sodium blood test could be performed prior to exposing the subject to water loading when such a situation like ours occurs in a clinical research setting.
Our case illustrates the value of a detailed medication history when performing water loads and supports the need for vigilance when studying subjects who take an antidepressant or antipsychotic medication despite a documented history of eunatremia on such therapies.
Conflict of interest statement. None declared.
References
- 1.Donal OD, Trehan A. SIADH and hyponatremia: foreword. NDT Plus. 2009;2:iii1–iii4. doi: 10.1093/ndtplus/sfp152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Safdieh JE, Rudominer R. A case of hyponatremia induced by duloxetine. J Clin Psychopharmacol. 2006;26:675–676. doi: 10.1097/01.jcp.0000246207.73034.96. [DOI] [PubMed] [Google Scholar]
- 3.Dirks AC, van Hyfte DM. Recurrent hyponatremia after substitution of citalopram with duloxetine. J Clin Psychopharmacol. 2007;27:313. doi: 10.1097/01.jcp.0000270086.22877.78. [DOI] [PubMed] [Google Scholar]
- 4.Maramattom BV. Duloxetine-induced syndrome of inappropriate antidiuretic hormone secretion and seizures. Neurology. 2006;66:773–774. doi: 10.1212/01.wnl.0000200993.33730.95. [DOI] [PubMed] [Google Scholar]
- 5.Jacquin P, Ouvry O, Alvin P. Fatal water intoxication in a young patient with anorexia nervosa. J Adolesc Health. 1992;13:631–633. doi: 10.1016/1054-139x(92)90379-p. [DOI] [PubMed] [Google Scholar]
- 6.Cuesta MJ, Juan JA, Peralta V. Secondary seizures from water intoxication in anorexia nervosa. Gen Hosp Psychiatry. 1992;14:212–213. doi: 10.1016/0163-8343(92)90087-q. [DOI] [PubMed] [Google Scholar]
- 7.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lewis J, Greene T, Appel L, et al. AASK Study Group A comparison of iothalamate-GFR and serum creatinine-based outcomes: acceleration in the rate of GFR decline in the African American Study of Kidney Disease and Hypertension. J Am Soc Nephrol. 2004;15:3175–3183. doi: 10.1097/01.ASN.0000146688.74084.A3. [DOI] [PubMed] [Google Scholar]
- 9.Bahia A, Chu ES, Mehler PS. Polydipsia and hyponatremia in a woman with anorexia nervosa. Int J Eat Disord. 2010 doi: 10.1002/eat.20792. In press. [DOI] [PubMed] [Google Scholar]
- 10.Krüger S, Lindstaedt M. Duloxetine and hyponatremia: a report of 5 cases. J Clin Psychopharmacol. 2007;27:101–104. doi: 10.1097/JCP.0b013e31802e688a. [DOI] [PubMed] [Google Scholar]