Case
A 58-year-old man presented to our outpatient department with a history of haematuria and fever. He was a known case of chronic renal failure (CRF). On examination, both the kidneys were palpable. Ultrasound revealed features suggestive of ADPKD with left hydronephrosis. A left-sided percutaneous nephrostomy was done. Nephrostogram revealed complete cut-off at the pelvi-ureteric junction. Abdominal magnetic resonance imaging (MRI) showed thickened ureter with some intraluminal-filling defect in all but the lower end. He was taken up for retrograde pyelography (RGP) and ureteroscopy, which showed a polypoidal growth just above the ureterovesical junction. The biopsy revealed a high-grade transitional cell carcinoma of the ureter. A left nephro-ureteroctemy was done. The entire ureter was filled with the tumour that was reaching into the renal pelvis (Figure 1A and B).
Fig. 1.
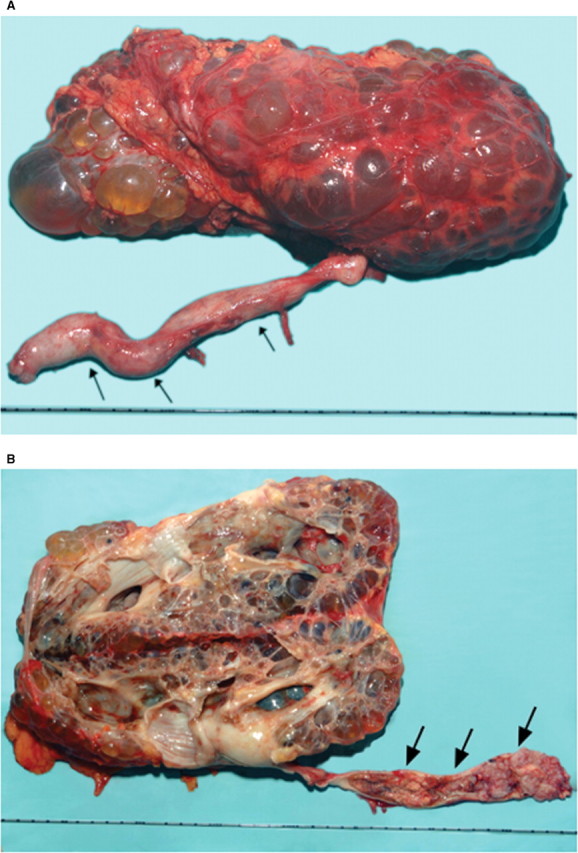
(A) Nephro-ureterectomy specimen showing polycystic kidney with dilated ureter containing tumour (arrow heads). (B) Cut-open nephro-ureterectomy specimen showing polycystic kidney with pan-ureteric TCC (arrow heads).
Comment
Hydronephrosis in ADPKD could be because of anatomical or metabolic factors that should have been picked up on routine imaging [1]. Although renal call carcinoma has been associated with ADPKD, upper tract TCC has been rarely reported [2]. The association of ADPKD with TCC of the entire ureter has never been previously reported. The diagnosis of upper tract TCC as a cause of ureteric obstruction is difficult because of non-specific symptoms, limitation of conventional imaging and the rarity of such association. In doubtful cases, RGP and ureteroscopy clinch the diagnosis. The management is further complicated due to underlying CRF in ADPKD patients.
Conflict of interest statement. None declared.
References
- 1.Grampsas SA, Chandhoke PS, Fan J, et al. Anatomic and metabolic risk factors for nephrolithiasis in patients with autosomal dominant polycystic kidney disease. Am J Kidney Dis. 2000;36:53–57. doi: 10.1053/ajkd.2000.8266. [DOI] [PubMed] [Google Scholar]
- 2.Grubb RL, III, Collyer WC, Kibel AS. Transitional cell carcinoma of the renal pelvis associated with hypercalcemia in a patient with autosomal dominant polycystic kidney disease. Urology. 2004;63:778–780. doi: 10.1016/j.urology.2003.12.005. [DOI] [PubMed] [Google Scholar]


