Abstract
Leishmaniasis, an infectious disease endemic in tropical, Asian and southern European countries, is caused by obligate intramacrophage protozoa and is transmitted through the bite of infected female sandflies. More than 20 leishmanial species are responsible for four main clinical syndromes: cutaneous leishmaniasis; mucocutaneous leishmaniasis; visceral leishmaniasis, also known as kala-azar, and post-kala-azar dermal leishmaniasis. Visceral leishmaniasis can present with varying clinical features and the kidney can also be involved. Both glomerular and tubular function can be altered and patients can develop proteinuria, haematuria, abnormalities in urinary concentration and acidification and acute and chronic renal insufficiency. Not only the disease itself but also the therapy administered might be responsible for the renal involvement in kala-azar. Indeed, some of the agents with efficiency against visceral leishmaniasis, such as pentavalent antimonial drugs, amphotericin B, pentamidine, miltefosine, paromomycin and simataquine, may be associated with a high risk of renal toxicity. In this article, the literature on renal involvement in visceral leishmaniasis is reviewed.
Keywords: nephrotoxicity, renal involvement, visceral leishmaniasis
Introduction
Leishmaniasis, an infectious disease endemic in tropical, Asian and southern European countries (Figure 1), is caused by obligate intramacrophage protozoa and is transmitted through the bite of infected female sandflies (Figure 2) [1]. These vectors belong to two species: the Old World sandfly species (Phlebotomus sp.) live in desert or semi-arid ecosystems, while the New World species (Lutzomyia sp.) inhabits forest climates [2]. There are two different forms of Leishmania: the promastigote flagellar form found in the gut of the vector and the amastigote form that develops in the mammalian host. More than 20 leishmanial species are responsible for four main clinical syndromes: cutaneous leishmaniasis; mucocutaneous leishmaniasis; visceral leishmaniasis (also known as kala-azar, Hindi for black fever) and post-kala-azar dermal leishmaniasis [1].
Fig. 1.
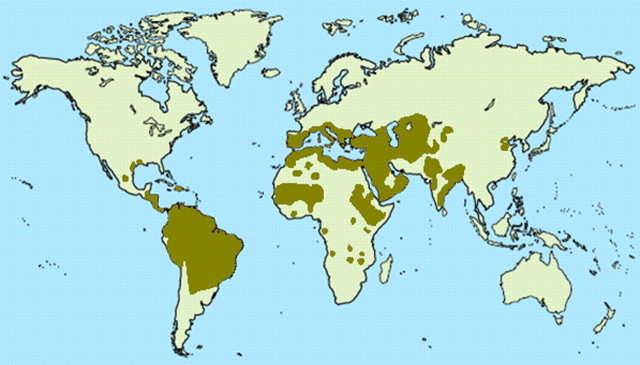
Leishmaniasis is endemic in tropical, Asian and southern European countries.
Fig. 2.
Leishmaniasis is transmitted through the bite of infected female sandflies (Phlebotomus sp. in photo). From CDC/Frank Collins.
Cutaneous and mucocutaneous leishmaniasis are usually caused by Leishmania braziliensis and present with ulcers and nodules, which involve the skin and the respiratory and oral mucosa. Visceral leishmaniasis, generally caused by Leishmania donovani and Leishmania infantum, is a systemic disease responsible for ∼500 000 new cases and 50 000 deaths worldwide each year [1]. After an incubation period that generally lasts between 2 and 6 months, the onset of symptoms is usually insidious with malaise, fever, fatigue and weight loss. Subsequently, the intense parasitism of the reticular endothelial system by the protozoa causes hepatosplenomegaly, anaemia, leukopenia and thrombocytopaenia as well as hypergammaglobulinaemia. Later symptoms include cachexia, hepatic dysfunction with jaundice, hypoalbuminemia and oedema (Table 1). They might persist for several weeks to months and, if left untreated, patients may die from bacterial co-infections, massive bleeding or severe anaemia. Immunocompromised patients, who contract the infection more frequently, may develop post-kala-azar dermal leishmaniasis, a complication of visceral leishmaniasis, which usually presents with a macular or nodular rash that develops after 6 months to 1 year after the systemic disease. Visceral leishmaniasis can present with varying clinical features and the kidney also can be involved. Both the disease itself and the therapy administered might be responsible for the renal involvement in kala-azar. Indeed, some of the agents with efficiency against visceral leishmaniasis, such as pentavalent antimonial drugs, amphotericin B, pentamidine, miltefosine, paromomycin and simataquine, may be associated with a high risk of renal toxicity. In this article, the literature on renal involvement in visceral leishmaniasis is reviewed.
Table 1.
Clinical presentation of visceral leishmaniasis
| Early symptoms |
| • Malaise |
| • Fever |
| • Fatigue |
| • Weight loss |
| Haematological alterations |
| • Anaemia |
| • Leukopenia |
| • Thrombocytopaenia |
| • Hypergammaglobulinaemia |
| Reticuloendothelial system involvement |
| • Hepatomegaly |
| • Splenomegaly |
| Later symptoms |
| • Cachexia |
| • Hepatic dysfunction (jaundice, hypoalbuminaemia, oedema) |
Renal disease in leishmaniasis
Even though kala-azar nephropathy is still poorly understood, kidney dysfunction in this disease has been reported in several studies (Table 2).
Table 2.
Clinical features of renal involvement in visceral leishmaniasis
| Urinary abnormalities | References |
| • Proteinuria | [3, 4] |
| • Haematuria | [3, 4] |
| • Leukocyturia | [4] |
| • Pyuria | [3] |
| Tubular dysfunction | |
| • Proximal tubulopathy | [4, 5] |
| • Distal tubulopathy | [6] |
| Glomerular dysfunction | |
| • Decrease in GFR | [6] |
| • Acute glomerulonephritis | [4, 7] |
| • Nephrotic syndrome | [8, 9] |
| AKI | [7, 8, 10] |
Immune complex deposition, T cells and adhesion molecules activation have been shown to be important mechanisms of injury in the glomerulonephritis occurring in visceral leishmaniasis [11–15]. In 2007, Prianti et al. [16] observed a mesangial proliferative pattern of glomerulonephritis in Leishmania chagasi-infected mice. The presence of IgG deposits and the absence of C3b deposits in the glomeruli suggested that immunoglobulins may be involved in the pathogenesis of glomerular injury caused by kala-azar, while the complement did not seem to play an important role in the disease. However, both functional glomerular and tubular disturbances can complicate visceral leishmaniasis, particularly its chronic form [6].
One of the first human studies about renal involvement in kala-azar was a cohort study of 50 patients with visceral leishmaniasis [3]. Proteinuria and/or microscopic haematuria or pyuria were observed in 51% of patients. Urinary protein excretion was elevated in 57% of patients and in all of them this was <1 g/24 h. There was a tubulointerstitial involvement in all seven patients who underwent kidney biopsy and, in five of them, a proliferative glomerulonephritis was also detected (Table 3). Renal involvement was mild and reversed with the cure of the infection. In 2003, Salgado et al. [4] evaluated the renal function of 11 patients with visceral leishmaniasis. Five patients presented macroscopic haematuria and one developed acute nephritic syndrome. Laboratory data of urine exam showed proteinuria in 10 patients and haematuria and leukocyturia in 7 and 6 cases, respectively. Proximal tubulopathy, measured through retinol-binding protein level, was observed in five patients (Table 3). In 2007, Lima Verde et al. [6] stated that abnormalities in glomerular filtration, urinary concentration and acidification might be consistently associated to the chronic form of kala-azar. In a cross-sectional study of 50 patients with chronic visceral leishmaniasis, they reported a decreased glomerular filtration rate (GFR) in 28% of the cases. Decreased GFR was related to fluid loss, hypotension and immunological glomerular disease. Urinary concentrating capacity was abnormal in 68% of the patients after pitressin administration. Complete distal renal tubular acidosis was observed in 30% of patients and an incomplete form was found in 34% of them. In 2008, Daher et al. [10] reviewed 57 patients with visceral leishmaniasis who presented initially with fever (97%), splenomegaly (96.4%), weight loss (95.5%), pallor (93.6%), cough (89.7%), hepatomegaly (87.2%), asthenia (83.3%), anorexia (82.9%) and vomiting (73.9%). Acute kidney injury (AKI) was observed in 15 patients (26.3%); 8 of these patients had AKI before amphotericin B administration. Death occurred in three cases and in all of them serum creatinine was >114.92 μmol/L. They concluded that renal dysfunction could be an important feature of kala-azar and might be associated with increased morbidity and mortality. More recently, Agenor et al. [5] reported proximal tubular damage in a cross-sectional study of 55 patients with visceral leishmaniasis. Increased albumin excretion was observed in 44% of patients, accounting for 17% of the total urinary protein excretion. Proteinuria consisted predominantly of low-molecular weight protein fractions, such as alpha1, alpha2, beta microglobulins and especially gamma globulins. All patients presented elevated levels of urinary beta2-microglobulin. Immunoelectrophoresis showed increased urinary excretion rates of k (27%) and λ (42%) light chains. The principal blood alterations were hyponatraemia (94.6%), hypokalaemia (26%), hypochloraemia (27.2%), hypocalcaemia (32%), hypomagnesaemia (41.8%), hypouricaemia (14.3%). Increased urinary excretion fractions were: sodium (15%), potassium (26%), chloride (33.3%), calcium (32%), inorganic phosphate (27.2%), magnesium (100%) with hypermagnesiuria, uric acid (44%). Glycosuria was found in one-third of patients.
Table 3.
Reported histological patterns of renal involvement in visceral leishmaniasis
There have also been several case reports of patients with visceral leishmaniasis who developed renal involvement. In 1995, Romero Maroto et al. [17] reported the first case of renal and urinary tract leishmaniasis in a 61-year-old male patient. The patient developed granulomatous pyelonephritis, responsible for pyelocaliceal and ureteral dilatation. The ureteral involvement responded to the treatment, while the renal one required conservative surgery. In 2004, Chaigne et al. [18] reported a case of segmental necrotizing glomerulonephritis with 70% crescents on kidney biopsy in a 20-year-old man with human visceral leishmaniasis (Table 3). Treatment with liposomal amphotericin B alone did not improve the course of renal failure, while partial recovery was obtained after the administration of high-dose corticosteroids.
Renal involvement in immunocompromised patients
It is well known that kala-azar frequently affects immunocompromised individuals, such as HIV-infected patients and organ transplant recipients. There have been three reports of immunocompromised patients with visceral leishmaniasis who developed renal complications (Table 4) [7–9]. Two of these were HIV-infected patients and one a renal transplant recipient. Kidney biopsy was performed in all of them. Among HIV-infected patients, the first presented with nephrotic syndrome and irreversible AKI, likely related to the glomerular AA amyloid deposits, shown on kidney biopsy. This was the first case described in humans of secondary amyloidosis caused by visceral leishmaniasis. The second patient presented nephrotic syndrome in the absence of immune complex glomerular deposition: for the first time, the influence of the relapsing nature of leishmaniasis on the course of nephropathy was reported. The transplanted patient developed a parasitic nephritis and, subsequently, AKI. This was the first case in literature of parasitic nephritis as a cause of acute renal failure.
Table 4.
Renal involvement in immunocompromised patients with visceral leishmaniasis
| Reference | Age (years) | Sex | Immunocompromised status | Kidney biopsy | Clinical presentation of renal disease |
| [8] | 28 | Male | HIV infection | Glomerular AA amyloid deposits without mesangial hyperplasia | Nephrotic syndrome |
| AKI | |||||
| [9] | 32 | Female | HIV infection | Tubular atrophy, interstitial fibrosis, lymphocytic infiltration, mesangial hyperplasia, histiocytes with Leishmania in peritubular areas | Nephrotic syndrome |
| [7] | 69 | Male | Kidney transplant | Moderate-severe interstitial inflammation with mixed infiltrate of lymphocytes, histiocytes and plasma cells, macrophages with Leishmania | Acute nephritis |
| AKI |
Nephrotoxicity related to the treatment of the disease
Some of the agents with efficiency against visceral leishmaniasis, such as pentavalent antimonial drugs, amphotericin B, pentamidine, miltefosine, paromomycin and simataquine, might be associated with high risk of renal toxicity (Table 5).
Table 5.
Nephrotoxicity of anti-leishmanial drugs
| References | Drugs | Nephrotoxicity |
| [19] | Antimonial compounds | Possible interaction with antidiuretic hormone |
| [19, 20] | Antimonial compounds | Acute tubular necrosis |
| [21] | Conventional amphotericin B | Distal tubular acidosis |
| Nephrogenic diabetes insipidus | ||
| Potassium wasting | ||
| [22, 23] | Conventional amphotericin B | Potassium wasting |
| [24] | Conventional amphotericin B | AKI |
| [25] | Pentamidine | AKI |
| Hyperkalaemia | ||
| [26] | Pentamidine | Hypocalcaemia |
| Hypomagnesaemia |
Pentavalent antimonial compounds
These drugs have been the first-line treatment for visceral leishmaniasis in different countries since 1940s [1]. Sodium stibogluconate and meglumine antimoniate remain the most widely used anti-leishmanial agents [27]. The most serious adverse effects, usually related to the cumulative dose, are cardiotoxicity and clinical pancreatitis. Less common side effects include myalgia, arthralgia, nausea, vomiting, abdominal pain and elevated liver function tests. Very few trials have reported renal effects of antimonial compounds. One of the first studies aimed to evaluate their nephrotoxicity was performed by Veiga et.al. [19] in 1990. They observed disturbances in urine concentrating capacity in rats treated with both meglumine antimoniate and sodium stibogluconate, expressed by significantly low levels of urine osmolality after the administration of the two drugs. The decrease in urine osmolality was associated to an important increase in urinary flow, while fractional excretion of sodium was normal. A likely interference of the drugs in the action of the antidiuretic hormone was supposed. Functional and histopathological alterations of the acute tubular necrosis were found at higher doses of the drugs. In 1999, Rodrigues et al. [20] reported a case of AKI due to acute tubular necrosis, demonstrated on kidney biopsy, in a 50-year-old male patient with generalized cutaneous leishmaniaisis after meglumine antimoniate administration.
Because of the increasing resistance to antimonial compounds in several countries, such as India (Bihar State) and Nepal, these agents have been progressively replaced by other drugs.
Amphotericin B and its new formulations
Conventional amphotericin B deoxycholate has progressively substituted for pentavalent antimonial compounds in several countries due to increasing treatment failure rates [28]. This drug possesses high anti-leishmanial efficacy but it is associated with a high risk of renal toxicity in addition to other side effects (rigour, fever, malaise, anorexia, trombophlebitis and bone marrow suppression) [1]. Conventional amphotericin B may cause dose-dependent renal abnormalities, such as AKI, distal renal tubular acidosis and nephrogenic diabetes insipidus [21], and renal potassium wasting [21–23]. These effects may revert with discontinuation of the therapy, although, in the case of AKI, renal dysfunction might progress and be incompletely reversible. In addition to the poor selectivity of amphotericin B between human cholesterol and fungal ergosterol, other mechanisms seem to be involved in the pathogenesis of the renal toxicity of the drug [29]. Vasoconstriction and direct interaction with epithelial cell membranes might, indeed, be responsible for the decrease in glomerular filtration and tubular dysfunction [30]. Oliveira et al. [24] have recently investigated the factors associated with AKI in two hundred and 27 patients with visceral leishmaniasis. AKI was observed in 33.9% of cases and risk factors were male gender [odds ratio (OR) = 2.2; P = 0.03], advanced age (OR = 1.05; P < 0.001) and jaundice (OR = 2.9; P = 0.002). There was a strong association between amphotericin B use and AKI (OR = 18.4; P < 0.0001), whereas glucantime use was associated with lower incidence of AKI compared with amphotericin B use (OR = 0.05; P < 0.0001). Mortality was 13.3%, and it was higher in patients with AKI (30.2%).
The new lipid formulations of amphoterin B (liposomal derivative and lipid complex formulations) have shown a reduced nefrotoxicity when compared to the conventional form of the drug. In these formulations, deoxycholate has been replaced by other lipids that possess higher stability and higher affinity for fungal ergosterol, thus improving efficacy while reducing toxicity [22]. Among the different derivatives of the drug, the liposomal amphotericin B has shown the highest therapeutic efficacy and the most safety profile [31–33]. Although transient increases in the creatinine level may occur, acute and chronic toxicity is rare, even with high doses of the drug [31]. In India, liposomal amphotericin B showed lower rates of toxicity than conventional amphotericin B or amphotericin B lipid complex [33–36]. Three randomized comparative trials for the treatment of fungal infections in neutropenic patients also confirmed reduced renal toxicity for liposomal amphotericin B than for the conventional form of the drug or amphotericin B lipid complex [30]. In 2004, Aguado et al. [37] assessed the risk of haematological, renal and hepatic toxicity associated with amphotericin B lipid complex in a multicentre open-label study of 93 patients with suspected systemic fungal infection or leishmaniasis. They did not observe any difference between serum creatinine concentration before and after the study. No significant correlation between the dose of the drug administered and the level of serum creatinine was found. The drug showed low nephrotoxicity even when administered to patients with preexisting renal insufficiency.
Pentamidine
Pentamidine was previously a second-line alternative treatment, but nowadays it is rarely used because of low efficacy and high toxicity [38]. Both reversible AKI and electrolyte abnormalities have been associated to the use of this agent [25]. A direct nephrotoxic effect may be involved in the mechanism by which pentamidine causes AKI, leading to tubular necrosis, which is more likely in presence of volume depletion and co-administration of other nephrotoxic drugs. Tubular nephrotoxicity seems to be also responsible for electrolyte abnormalities, such as hyperkalaemia [25], hypomagnesaemia and hypocalcaemia [26]. Even though there are several studies showing the nephrotoxicity of pentamidine during prevention and treatment of Pneumocystis carinii pneumonia [39,40], only few studies have been performed in patients with visceral leishmaniasis to test its safety. Pentamidine was tested in six published and one unpublished trial carried out between 1980 and 1990s. Irreversible insulin-dependent diabetes mellitus was reported in 4–12% of patients and few cases of shock and myocarditis and fatal outcomes were rarely observed; no specific renal toxicity was reported [23].
Miltefosine
This is the only oral agent currently in use for treatment of visceral leishmaniasis. This agent was tested in six-dose finding studies and one comparative study performed between 1998 and 2000, involving 665 patients. Moderate to severe nephrotoxicity was reported in 2 and 1% of patients, respectively, and this was dose related [23].
Paromomycin
This is an aminoglycoside antibiotic with efficiency against leishmania and rare adverse effects. In 2007, Sundar et al. [41] conducted a randomized, controlled open-label study comparing paromomycin with amphotericin B in 667 patients with visceral leishmaniasis. Paromomycin was shown to be efficient as amphotericin B and mortality rates for the two drugs were <1%. Adverse events, which were more common among patients receiving paromomycin than among those receiving amphotericin B (6 versus 2%, P = 0.02), included transient elevation of aspartate aminotransferase levels (>3 times the upper limit of the normal range); transient reversible ototoxicity (2 versus 0%, P = 0.20) and injection-site pain (55 versus 0%, P < 0.001).
In contrast, amphotericin B was associated with greater nephrotoxicity (4 versus 0%, P < 0.001), fevers (57 versus 3%), rigours (24 versus 0%, P < 0.001) and vomiting (10 versus <1%, P < 0.001) compared to paromomycin.
Sitamaquine
This is another alternative for oral treatment for visceral leishmaniasis, although it is no longer commercially available. In 2001, Dietze et al. performed a phase 2, open-label, dose-escalating safety and efficacy study in patients with kala-azar. Nephrotoxicity, that was not anticipated from preclinical animal studies or from phase 1 studies, was seen at higher doses of the drug in three of the 22 enrolled patients [42].
There is a wide consensus among experts that anti-leishmanial therapy in endemic countries should include combination drug regimens to avoid the development of acquired resistance and perform shorter treatment courses with higher efficacy and lower toxicity. At this time, guidelines for specific combination regimens do not yet exist.
Conclusions
Renal involvement in human visceral leishmaniasis might be characterized by complex and varying clinical features. Both glomerular and tubular function can be altered and patients can develop proteinuria, hematuria, abnormalities in urinary concentration and acidification, acute and chronic renal insufficiency. They might be caused both by the disease itself as well as by the drugs administered to treat the infection. Data on renal prognosis is limited. AKI may contribute to poor patient outcomes. However, glomerular lesions may respond to therapy for kala-azar. In immunocompromised patients, a relapsing course has been reported.
Acknowledgments
Conflict of interest statement. None declared.
References
- 1.Chappuis F, Sundar S, Hailu A, et al. Visceral leishmaniasis: what are the needs for diagnosis, treatment and control? Nat Rev Microbiol. 2007;5:873–882. doi: 10.1038/nrmicro1748. [DOI] [PubMed] [Google Scholar]
- 2.Sharma U, Singh S. Insect vectors of Leishmania: distribution, physiology and their control. J Vector Borne Dis. 2008;45:255–272. Review. [PubMed] [Google Scholar]
- 3.Dutra M, Martinelli R, de Carvalho EM, et al. Renal involvement in visceral leishmaniasis. Am J Kidney Dis. 1985;6:22–27. doi: 10.1016/s0272-6386(85)80034-2. [DOI] [PubMed] [Google Scholar]
- 4.Salgado Filho N, Ferreira TM, Costa JM. Involvement of the renal function in patients with visceral leishmaniasis (kala-azar) Rev Soc Bras Med Trop. 2003;36:217–221. doi: 10.1590/s0037-86822003000200004. [DOI] [PubMed] [Google Scholar]
- 5.Agenor Araújo Lima Verde F, Agenor Araújo Lima Verde F, De Francesco Daher E, et al. Renal tubular dysfunction in human visceral leishmaniasis (kala-azar) Clin Nephrol. 2009;71:492–500. doi: 10.5414/cnp71492. [DOI] [PubMed] [Google Scholar]
- 6.Lima Verde FA, Lima Verde FA, Lima Verde IA, et al. Evaluation of renal function in human visceral leishmaniasis (kala-azar): a prospective study on 50 patients from Brazil. J Nephrol. 2007;20:430–436. [PubMed] [Google Scholar]
- 7.Dettwiler S, McKee T, Hadaya K, et al. Visceral leishmaniasis in a kidney transplant recipient: parasitic interstitial nephritis, a cause of renal dysfunction. Am J Transplant. 2010;10:1486–1489. doi: 10.1111/j.1600-6143.2010.03125.x. [DOI] [PubMed] [Google Scholar]
- 8.Navarro M, Bonet J, Bonal J, et al. Secondary amyloidosis with irreversible acute renal failure caused by visceral leishmaniasis in a patient with AIDS. Nefrologia. 2006;26:745–746. [PubMed] [Google Scholar]
- 9.Alex S, Criado C, Fernández-Guerrero ML, et al. Nephrotic syndrome complicating chronic visceral leishmaniasis: re-emergence in patients with AIDS. Clin Nephrol. 2008;70:65–68. doi: 10.5414/cnp70065. [DOI] [PubMed] [Google Scholar]
- 10.Daher EF, Evangelista LF, Silva Júnior GB, et al. Clinical presentation and renal evaluation of human visceral leishmaniasis (kala-azar): a retrospective study of 57 patients in Brazil. Braz J Infect Dis. 2008;12:329–332. doi: 10.1590/s1413-86702008000400015. [DOI] [PubMed] [Google Scholar]
- 11.Sartori A, De Oliveira AV, Roque-Barreira MC, et al. Immune complex glomerulonephritis in experimental kala-azar. Parasite Immunol. 1987;9:93–103. doi: 10.1111/j.1365-3024.1987.tb00491.x. [DOI] [PubMed] [Google Scholar]
- 12.de Brito T, Hoshino-Shimizu S, Neto VA, et al. Glomerular involvement in human kala-azar. A light, immunofluorescent, and electron microscopic study based on kidney biopsies. Am J Trop Med Hyg. 1975;24:9–18. [PubMed] [Google Scholar]
- 13.Poli A, Abramo F, Mancianti F, et al. Renal involvement in canine leishmaniasis. A light-microscopic, immunohistochemical and electron-microscopic study. Nephron. 1991;57:444–452. doi: 10.1159/000186348. [DOI] [PubMed] [Google Scholar]
- 14.Weisinger JR, Pinto A, Velazquez GA, et al. Clinical and histological kidney involvement in human kala-azar. Am J Trop Med Hyg. 1978;27(s Pt 1):357–359. doi: 10.4269/ajtmh.1978.27.357. [DOI] [PubMed] [Google Scholar]
- 15.Costa FA, Guerra JL, Silva SM, et al. CD4(+) T cells participate in the nephropathy of canine visceral leishmaniasis. Braz J Med Biol Res. 2000;33:1455–1458. doi: 10.1590/s0100-879x2000001200009. [DOI] [PubMed] [Google Scholar]
- 16.Prianti MG, Yokoo M, Saldanha LC, et al. Leishmania (Leishmania) chagasi-infected mice as a model for the study of glomerular lesions in visceral leishmaniasis. Braz J Med Biol Res. 2007;40:819–823. doi: 10.1590/s0100-879x2007000600011. [DOI] [PubMed] [Google Scholar]
- 17.Romero Maroto J, López López C, Mayol MJ, et al. Renal and urinary tract leishmaniasis. A disease to keep in mind. Actas Urol Esp. 1995;19:789–794. [PubMed] [Google Scholar]
- 18.Chaigne V, Knefati Y, Lafarge R, et al. A patient with visceral leishmaniasis and acute renal failure in necrotizing glomerulonephritis. Nephrologie. 2004;25:179–183. [PubMed] [Google Scholar]
- 19.Veiga JP, Khanam R, Rosa TT, et al. Pentavalent antimonial nephrotoxicity in the rat. Rev Inst Med Trop Sao Paulo. 1990;32:304–309. doi: 10.1590/s0036-46651990000400012. [DOI] [PubMed] [Google Scholar]
- 20.Rodrigues ML, Costa RS, Souza CS, et al. Nephrotoxicity attributed to meglumine antimoniate (Glucantime) in the treatment of generalized cutaneous leishmaniasis. Rev Inst Med Trop Sao Paulo. 1999;41:33–37. doi: 10.1590/s0036-46651999000100007. [DOI] [PubMed] [Google Scholar]
- 21.Goldman RD, Koren G. Amphotericin B nephrotoxicity in children. J Pediatr Hematol Oncol. 2004;26:421–426. doi: 10.1097/00043426-200407000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Sundar S, Chatterjee M. Visceral leishmaniasis—current therapeutic modalities. Indian J Med Res. 2006;123:345–352. [PubMed] [Google Scholar]
- 23.Olliaro PL, Guerin PJ, Gerstl S, et al. Treatment options for visceral leishmaniasis: a systematic review of clinical studies done in India, 1980-2004. Lancet Infect Dis. 2005;5:763–774. doi: 10.1016/S1473-3099(05)70296-6. [DOI] [PubMed] [Google Scholar]
- 24.Oliveira MJ, Silva Júnior GB, Abreu KL, et al. Risk factors for acute kidney injury in visceral leishmaniasis (Kala-Azar) Am J Trop Med Hyg. 2010;82:449–453. doi: 10.4269/ajtmh.2010.09-0571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lachaal M, Venuto RC. Nephrotoxicity and hyperkalaemia in patients with acquired immunodeficiency syndrome treated with pentamidine. Am J Med. 1989;87:260–263. doi: 10.1016/s0002-9343(89)80147-0. [DOI] [PubMed] [Google Scholar]
- 26.Shah GM, Alvarado P, Kirschenbaum MA. Symptomatic hypocalcemia and hypomagnesemia with renal magnesium wasting associated with pentamidine therapy in a patient with AIDS. Am J Med. 1990;89:380–382. doi: 10.1016/0002-9343(90)90354-g. [DOI] [PubMed] [Google Scholar]
- 27.Den Boer M, Davidson RN. Treatment options for visceral leishmaniasis. Expert Rev Anti Infect Ther. 2006;4:187–197. doi: 10.1586/14787210.4.2.187. . Review. [DOI] [PubMed] [Google Scholar]
- 28.Sundar S, More DK, Singh MK, et al. Failure of pentavalent antimony in visceral leishmaniasis in India: report from the center of the Indian epidemic. Clin Infect Dis. 2000;31:1104–1107. doi: 10.1086/318121. [DOI] [PubMed] [Google Scholar]
- 29.Varlam DE, Siddiq MM, Parton LA, et al. Apoptosis contributes to amphotericin B-induced nephrotoxicity. Antimicrob Agents Chemother. 2001;45:679–685. doi: 10.1128/AAC.45.3.679-685.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Deray G. Amphotericin B nephrotoxicity. J Antimicrob Chemother. 2002;49(Suppl 1):37–41. doi: 10.1093/jac/49.suppl_1.37. . Review. [DOI] [PubMed] [Google Scholar]
- 31.Bern C, Adler-Moore J, Berenguer J, et al. Liposomal amphotericin B for the treatment of visceral leishmaniasis. Clin Infect Dis. 2006;43:917–924. doi: 10.1086/507530. [DOI] [PubMed] [Google Scholar]
- 32.Alvar J, Croft S, Olliaro P. Chemotherapy in the treatment and control of leishmaniasis. Adv Parasitol. 2006;61:223–274. doi: 10.1016/S0065-308X(05)61006-8. Review. [DOI] [PubMed] [Google Scholar]
- 33.Sundar S, Mehta H, Suresh AV, et al. Amphotericin B treatment for Indian visceral leishmaniasis: conventional versus lipid formulations. Clin Infect Dis. 2004;38:377–383. doi: 10.1086/380971. [DOI] [PubMed] [Google Scholar]
- 34.Sundar S, Jha TK, Thakur CP, et al. Single-dose liposomal amphotericin B in the treatment of visceral leishmaniasis in India: a multicenter study. Clin Infect Dis. 2003;37:800–804. doi: 10.1086/377542. [DOI] [PubMed] [Google Scholar]
- 35.Sundar S, Jha TK, Thakur CP, et al. Low-dose liposomal amphotericin B in refractory Indian visceral leishmaniasis: a multicenter study. Am J Trop Med Hyg. 2002;66:143–146. doi: 10.4269/ajtmh.2002.66.143. [DOI] [PubMed] [Google Scholar]
- 36.Sundar S, Agrawal G, Rai M, et al. Treatment of Indian visceral leishmaniasis with single or daily infusions of low dose liposomal amphotericin B: randomised trial. BMJ. 2001;323:419–422. doi: 10.1136/bmj.323.7310.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aguado JM, Lumbreras C, González-Vidal D, et al. Assessment of nephrotoxicity in patients receiving amphotericin B lipid complex: a pharmacosurveillance study in Spain. Clin Microbiol Infect. 2004;10:785–790. doi: 10.1111/j.1198-743X.2004.00963.x. [DOI] [PubMed] [Google Scholar]
- 38.Das VN, Siddiqui NA, Pandey K, et al. A controlled, randomized nonblinded clinical trial to assess the efficacy of amphotericin B deoxycholate as compared to pentamidine for the treatment of antimony unresponsive visceral leishmaniasis cases in Bihar, India. Ther Clin Risk Manag. 2009;5:117–124. [PMC free article] [PubMed] [Google Scholar]
- 39.Schwarz A, Perez-Canto A. Nephrotoxicity of antiinfective drugs. Int J Clin Pharmacol Ther. 1998;36:164–167. [PubMed] [Google Scholar]
- 40.O'Brien JG, Dong BJ, Coleman RL, et al. A 5-year retrospective review of adverse drug reactions and their risk factors in human immunodeficiency virus-infected patients who were receiving intravenous pentamidine therapy for Pneumocystis carinii pneumonia. Clin Infect Dis. 1997;24:854–859. doi: 10.1093/clinids/24.5.854. [DOI] [PubMed] [Google Scholar]
- 41.Sundar S, Jha TK, Thakur CP, et al. Injectable paromomycin for visceral leishmaniasis in India. N Engl J Med. 2007;356:2571–2581. doi: 10.1056/NEJMoa066536. [DOI] [PubMed] [Google Scholar]
- 42.Dietze R, Carvalho SF, Valli LC, et al. Phase 2 trial of WR6026, an orally administered 8-aminoquinoline, in the treatment of visceral leishmaniasis caused by Leishmania chagasi. Am J Trop Med Hyg. 2001;65:685–689. doi: 10.4269/ajtmh.2001.65.685. [DOI] [PubMed] [Google Scholar]



