Introduction
Kidney transplantation represents the preferred treatment for ESRD. Nevertheless, the use of the essential immunosuppressive agents may be associated with various side effects. In addition to frequently encountered complications such as post-transplantation diabetes, infections or calcineurin inhibitor (CNI) nephrotoxicity, a wide variety of rare conditions have to be dealt with. Musculoskeletal pain after kidney transplantation is most often a manifestation of high-dose steroid therapy, steroid withdrawal, renal osteodystrophy or osteoporosis. Apart from these common causes, cyclosporine intake was identified for the first time as a novel reason for severe skeletal pain in 1989. It has been reported that cyclosporine may induce bone marrow oedema leading to severe and disabling bone pain mainly located in the lower limbs. Due to its relation to high CNI serum levels, the syndrome was named calcineurin inhibitor-induced pain syndrome (CIPS) by Grotz and colleagues in 2001.
Here, we report a patient who suffered from progressive disabling bilateral pain in his feet and knees due to CIPS evolving 2 months after kidney transplantation.
Case presentation
A 44-year-old patient with left-sided renal agenesis underwent kidney transplantation for ESRD. Initial routine ambulatory examinations showed stable graft function. Immunosuppressive therapy consisted of cyclosporine, mycophenolate mofetil and prednisone. Due to interaction with the patient’s anticonvulsive medication (phenobarbital), the dose of cyclosporine had to be steadily increased up to 500 mg twice daily to reach therapeutic trough levels. Two months after transplantation, the patient complained for the first time about pain in his left foot when physically active. During the following weeks, progressive pain in his feet and knees eventually forced him to walk with crutches. His medical history was negative for any trauma, rheumatologic disease or peripheral atherosclerosis.
The physical examination revealed an afebrile and normotensive patient (blood pressure 130/85 mmHg and heart rate 76 bpm). He suffered from immobilizing pain in both feet (located mainly over the toes on both sides) and on the lateral sides of both knees, which was increased by physical stress. There was some oedema at the affected sites, but no redness or trophic skin alterations. Blood tests revealed mild leucocytosis (10 790 × 103/μL, normal range 3.0–9.6 × 103/μL) and a normal C-reactive protein (5 mg/L, normal value < 5 mg/L). Creatinine level was 181 μmol/L, and eGFR (MDRD) 36 mL/min. Serum electrolyte analysis showed hypercalcaemia (albumin corrected: 2.68 mmol/L, normal range 2.1–2.54 mmol/L) and hypophosphataemia (0.75 mmol/L, normal range 0.87–1.45 mmol/L). Alkaline phosphatase level 149 U/L (normal range 40–129 U/L), parathyroid hormone level was 57 ng/L (normal range 15–65 ng/L), 25-OH vitamin D3 level 30 μg/L (normal value > 20 μg/L) and 1,25-OH vitamin D3 level 9 ng/L (normal range 18–70 ng/L; under substitution with calcium 500 mg and cholecalciferol 440 U daily).
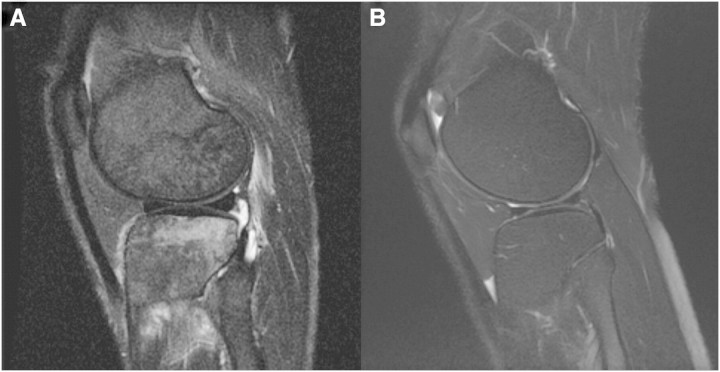
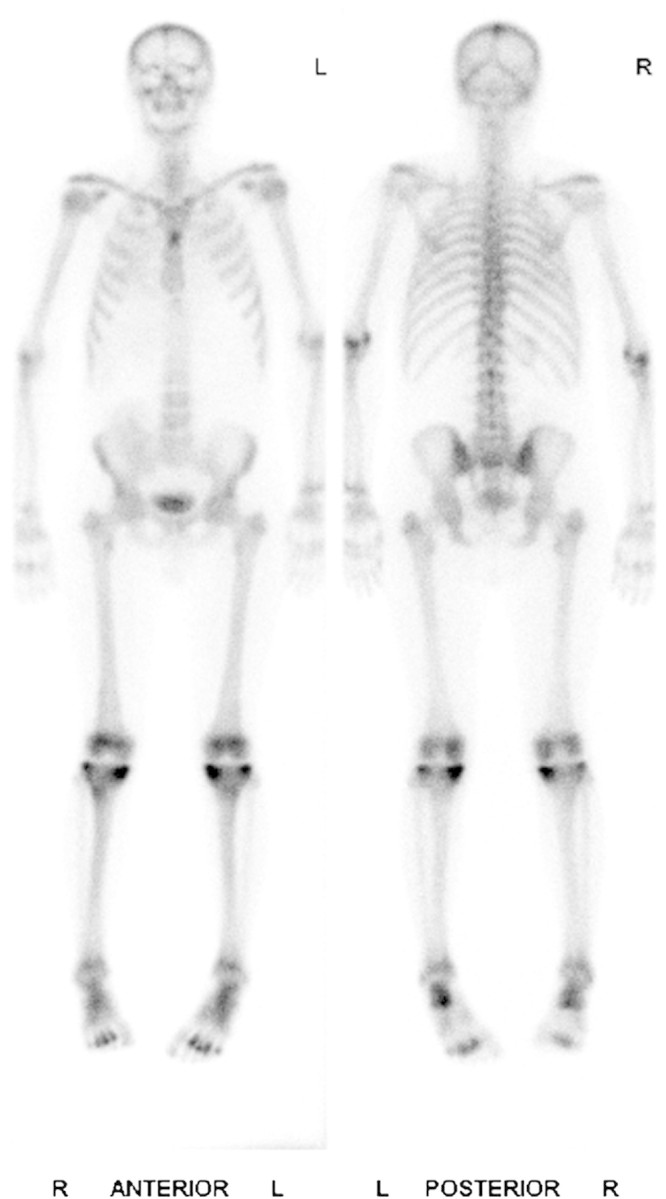
Conventional X-rays revealed signs of renal osteodystrophy but no fractures. Instead, whole-body technetium-99m dicarboxy diphosphonate (99mTc-DPD) scintigraphy (Figure 1) showed increased tracer uptake in the tibial plateau, metatarsi and elbows. The findings were confirmed by magnetic resonance imaging (MRI), where bone marrow oedema in the femur condylus and tibial plateau was demonstrated (left knee sagittal, Figure 2A)—a typical manifestation of CIPS. The tracer uptake distribution excluded osteodystrophy due to secondary hyperparathyroidism as a reason for the bone pain. Further, manifestation of osteodystrophy after transplantation with consecutive amelioration of calcium and phosphate levels as well as normalization of parathyroid hormone levels, as seen in this patient, would have been very unlikely. MRI showed no evidence of osteonecrosis, arthritis or inflammation of soft tissue, but showed the presence of bone marrow oedema confirming the clinical diagnosis of CIPS.
Fig. 1.
Increased radionuclide tracer uptake in the affected joints seen during whole-body 99mTc-DPD scintigraphy (late phase).
Fig. 2.
A. T2-weighted sagittal image of the patient’s left knee showing area of bone marrow oedema. B. Normal knee MRI.
Hence, cyclosporine was replaced by everolimus. The patient’s antihypertensive treatment with a calcium antagonist was continued, and he received an opioid analgesic. After 2 weeks, he was discharged to a rehabilitation clinic. During a follow-up visit 4 months later, an improvement of pain was noted, but the patient was still walking with crutches. Additional treatment with calcitonin was introduced, which however had no clinical benefit after 4 weeks.
Discussion
Musculoskeletal pain is a common problem after kidney transplantation. Because of the metabolic and cardiovascular burden of renal failure in addition to the impact of immunosuppressive treatment, the differential diagnosis varies from soft tissue infections, intermittent claudication or gout arthritis to avascular bone necrosis and osteoporotic fractures.
In 1989, Bouteiller and colleagues first reported a polyarticular pain syndrome in four solid-organ transplant recipients which was associated with the intake of cyclosporine [1]. The name CIPS was coined by Grotz et al. in 2001 [2]. They described nine kidney transplant recipients treated with either cyclosporine or tacrolimus and new onset of symmetrical pain in the feet and ankles, 3–18 months after transplantation. In 2002 and 2004, additional cases of CIPS after liver [3] and haematopoietic stem-cell transplantation [4] were reported. Until recently, CIPS was described only after solid-organ or stem-cell transplantation, but no such patients with immunosuppressive therapy for autoimmune disorders were reported [5]. This phenomenon was attributed to the higher dosage of CNI necessary for prevention of organ rejection after transplantation. Nevertheless, in 2008, Maeshima et al. summarized the first case of a patient suffering from adult-onset Still’s disease and development of CIPS [6].
Clinically, CIPS is characterized by symmetrical pain located primarily in the lower limbs (ankles, feet and knees), while the hip and spine are typically spared. The symptoms evolve 3–18 months after initiation of either cyclosporine or tacrolimus treatment [2]. Pain worsens in an upright position, during movement and while resting the legs in a position below the heart level.
The pathophysiological mechanism leading to CIPS is unknown. Grotz and colleagues proposed the hypothesis that CNI-induced vascular disturbance leads to an increased permeability of bone marrow vessels with consecutive bone marrow oedema [2,7]. Experimental data suggest CNI-induced perfusion alterations such as an endothelin-mediated vasoconstriction of the microvasculature [8]. The hypothesis of a CNI-dependent disturbance of bone marrow vessels is supported by radiological findings of increased radionuclide tracer uptake as a sign of hypervascularization, hyperperfusion and hypermetabolism. The fact that the lower limbs are affected preferentially may be the result of higher venous pressure in the upright position and underscores the hypothesis of altered vascular permeability [2,9]. An alternative hypothesis was suggested by O’Neill who proposed an inhibition of the calcineurin-dependent Na/K-ATPase by cyclosporine leading to an overall decrease of Na/K pump activity with subsequent rise of intracellular Ca2 + concentration. High levels of intracellular Ca2 + activate calpain, a Ca2 +-dependent proteolytic enzyme, which in turn would lead to cell death [10]. Due to the massive doses of cyclosporine (14 mg/kg/day) because of the interaction with the phenobarbital therapy, we speculate that unmeasured metabolites of cyclosporine could have accumulated and contributed to the side effects.
CIPS is a diagnosis of exclusion. Although the clinical presentation with bilateral pain in the lower extremities is typical and seen in the majority of cases, additional studies are necessary to distinguish CIPS from polyneuropathy, osteoporosis, hyperparathyroidism, reflex sympathetic dystrophy or avascular bone necrosis. Cyclosporine can cause both large- and small-fibre neuropathy; thus, a careful physical examination including thermal stimulation and nerve conduction studies may be necessary for evaluation. Osteoporosis is a common cause of bone pain after transplantation. In contrast to CIPS, patients suffering from osteoporosis mainly complain about lower back pain. Persisting secondary hyperparathyroidism leads to calcifications in soft tissue and cartilage and to subperiosteal resorption zones. The latter are typically located on the radial side of the middle phalanx of digit II and III, and tuft erosions occur at the finger tips. In hyperparathyroidism, scintigraphic analysis shows tracer uptake in various joints as well as in the tips of the ribs and the clavicles, whereas in CIPS, the uptake is located preferentially in the foot bones. Probably, the most difficult disorder to distinguish from CIPS is reflex sympathetic dystrophy since it is characterized by a similar radiological picture (nearly normal conventional X-ray, comparable radionuclide tracer uptake, and bone marrow oedema on MRI). Nevertheless, it has an asymmetrical distribution and is characterized by trophic skin lesions, allodynia and dysaesthesia. Avascular bone necrosis after transplantation is a complication of high corticosteroid levels. In contrast to CIPS, it is mainly, if not exclusively, localized in the hip. Since the introduction of cyclosporine as an immunosuppressive agent, lower corticosteroid doses are used after transplantation, and the incidence of avascular bone necrosis has decreased [11]. Eventually, diffuse arthralgias and fatigue are often encountered after transplantation due to steroid withdrawal [12], but should not display a diagnostic challenge. The cornerstone of treatment in CIPS patients is reduction or replacement of CNI treatment, although discomfort can persist for months [2]. In addition, a calcium-channel blocker, especially extended-release nifedipine in the range of 30–60 mg per day, can be applied [13]. Patients should be encouraged to elevate their legs while lying down to minimize venous pressure and therefore bone marrow oedema. Apart from calcium-channel blockers, calcitonin may help to attenuate pain by inhibiting osteolysis. Analgesics, with the exception of non-steroidal antiphlogistics, can be applied but are in most cases of minor benefit.
Conclusions
In conclusion, musculoskeletal pain is a common symptom after solid-organ transplantation. In the case of disabling pain, preferentially located in the lower extremities, in a patient with a CNI-containing immunosuppressive regimen, one should consider the differential diagnosis of CIPS. Reduction or replacement of CNI therapy and administration of calcium-channel blockers help to ameliorate symptoms and improve quality of life.
Teaching points
In the case of symmetrical bone pain of the lower limbs aggravated during physical stress and a CNI-containing immunosuppressive regimen, one should consider CIPS as a rare but possible explanation for symptoms, especially—but not exclusively—in a transplant recipient.
Diagnosis is one of exclusion; other reasons for limb pain such as infections, gout arthritis, avascular bone necrosis or osteoporotic fractures need to be excluded.
While physical examination is often unspectacular, an increased tracer uptake in scintigraphy studies and bone marrow oedema in MRI are typically seen.
The cornerstone of amelioration of symptoms is reduction or replacement of CNI treatment, although discomfort can persist for months. Additionally, calcium-channel blockers like nifedipine or otherwise calcitonin exert some beneficial effects.
Prior to transplantation, in the case of expected relevant interactions of established medication with immunosuppressive treatment, it seems to be advisable to think of switching to alternative drugs if suitable.
Conflict of interest statement. None declared.
References
- 1.Bouteiller G, Lloveras JJ, Condouret J, et al. Painful polyarticular syndrome probably induced by cyclosporin in three patients with a kidney transplant and one with a heart transplant. Rev Rhum Mal Osteoartic. 1989;56:753–755. [PubMed] [Google Scholar]
- 2.Grotz WH, Breitenfeldt MK, Braune SW, et al. Calcineurin-inhibitor induced pain syndrome (CIPS): a severe disabling complication after organ transplantation. Transpl Int. 2001;14:16–23. doi: 10.1007/s001470000285. [DOI] [PubMed] [Google Scholar]
- 3.Malat GE, Dupuis RE, Kassman B, et al. Tacrolimus-induced pain syndrome in a pediatric orthotopic liver transplant patient. Pediatr Transplant. 2002;6:435–438. doi: 10.1034/j.1399-3046.2002.02030.x. [DOI] [PubMed] [Google Scholar]
- 4.Kida A, Ohashi K, Tanaka C, et al. Calcineurin-inhibitor pain syndrome following haematopoietic stem cell transplantation. Br J Haematol. 2004;126:288. doi: 10.1111/j.1365-2141.2004.05066.x. [DOI] [PubMed] [Google Scholar]
- 5.Elder GJ. From marrow oedema to osteonecrosis: common paths in the development of post-transplant bone pain. Nephrology (Carlton) 2006;11:560–567. doi: 10.1111/j.1440-1797.2006.00708.x. [DOI] [PubMed] [Google Scholar]
- 6.Maeshima K, Ishii K, Horita M, et al. Calcineurin-inhibitor induced pain syndrome (CIPS) in an adult-onset Still's disease patient. Nippon Naika Gakkai Zasshi. 2008;97:2782–2784. doi: 10.2169/naika.97.2782. [DOI] [PubMed] [Google Scholar]
- 7.Villaverde V, Cantalejo M, Balsa A, et al. Leg bone pain syndrome in a kidney transplant patient treated with tacrolimus (FK506) Ann Rheum Dis. 1999;58:653–654. doi: 10.1136/ard.58.10.653a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kirk AD, Jacobson LM, Heisey DM, et al. Posttransplant diastolic hypertension: associations with intragraft transforming growth factor-beta, endothelin, and renin transcription. Transplantation. 1997;64:1716–1720. doi: 10.1097/00007890-199712270-00015. [DOI] [PubMed] [Google Scholar]
- 9.Collini A, De Bartolomeis C, Barni R, et al. Calcineurin-inhibitor induced pain syndrome after organ transplantation. Kidney Int. 2006;70:1367–1370. doi: 10.1038/sj.ki.5001833. [DOI] [PubMed] [Google Scholar]
- 10.O’Neill EA, Sloan VS. A potential mechanism of cyclosporine-associated bone pain: comment on the radiologic vignette by Stone et al. Arthritis Rheum. 1998;41:565–566. doi: 10.1002/1529-0131(199803)41:3<565::AID-ART29>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 11.Le Parc JM, Andre T, Helenon O, et al. Osteonecrosis of the hip in renal transplant recipients. Changes in functional status and magnetic resonance imaging findings over three years in three hundred five patients. Rev Rhum Engl Ed. 1996;63:413–420. [PubMed] [Google Scholar]
- 12.Miozzari M, Ambuhl PM. Steroid withdrawal after long-term medication for immunosuppressive therapy in renal transplant patients: adrenal response and clinical implications. Nephrol Dial Transplant. 2004;19:2615–2621. doi: 10.1093/ndt/gfh421. [DOI] [PubMed] [Google Scholar]
- 13.Gauthier VJ, Barbosa LM. Bone pain in transplant recipients responsive to calcium channel blockers. Ann Intern Med. 1994;121:863–865. doi: 10.7326/0003-4819-121-11-199412010-00007. [DOI] [PubMed] [Google Scholar]