Abstract
Background To achieve a measles free world, effective communication must be part of all elimination plans. The choice of communication approaches must be evidence based, locally appropriate, interactive and community owned. In this article, we document the innovative approach of using house visits supported by a web-enabled mobile phone application to create a real-time platform for adaptive management of supplemental measles immunization days in Kenya.
Methods One thousand nine hundred and fifty-two Red Cross volunteers were recruited, trained and deployed to conduct house-to-house canvassing in 11 urban districts of Kenya. Three days before the campaigns, volunteers conducted house visits with a uniform approach and package of messages. All house visits were documented using a web-enabled mobile phone application (episurveyor®) that in real-time relayed information collected to all campaign management levels. During the campaigns, volunteers reported daily immunizations to their co-ordinators. Post-campaign house visits were also conducted within 4 days, to verify immunization of eligible children, assess information sources and detect adverse events following immunization.
Results Fifty-six per cent of the 164 643 households visited said that they had heard about the planned 2012 measles vaccination campaign 1–3 days before start dates. Twenty-five per cent of households were likely to miss the measles supplemental dose if they had not been reassured by the house visit. Pre- and post-campaign reasons for refusal showed that targeted communication reduced misconceptions, fear of injections and trust in herbal remedies. Daily reporting of immunizations using mobile phones informed changes in service delivery plans for better immunization coverage. House visits were more remembered (70%) as sources of information compared with traditional mass awareness channels like megaphones (41%) and radio (37%).
Conclusions In high-density settlements, house-to-house visits are easy and more penetrative compared with traditional media approaches. Using mobile phones to document campaign processes and outputs provides real time evidence for service delivery planning to improve immunization coverage.
Keywords: House-to-house canvassing, measles campaigns, mobile phones, Kenya
KEY MESSAGES.
Using mobile phone-based technologies can create platforms for real-time evidence-based innovations in immunizations service communication and service delivery.
Mass media approaches to communication for immunization are good but house-to-house canvassing by trusted, neutral and community-based resources persons have a better reach.
National communication planning should articulate special strategies for reaching high-density and urban poor populations that are increasingly important in measles transmission.
Introduction
As we gear up to a world free of measles, rubella and congenital rubella syndrome (World Health Organization 2012), evidence-based communication planning must be an integral component of all elimination plans. Importantly, communication plans must be effectively resourced to impart the necessary impact on immunization coverage. Experience from the polio eradication programme has shown that there is a 12–20% or more increase in the absolute level of immunization coverage when communication is included as a key component of immunization strengthening (Waisborda et al. 2010). Even more important is that the channels and approaches used must be evidence-based, locally appropriate, interactive, community owned and reach all households before the vaccination days.
Africa in general and Kenya in particular, has witnessed unprecedented expansion in the numbers and coverage of mobile phones, thus connecting millions of people that previously were unconnected. The massive availability of mobile phones creates new opportunities for disease prevention programmes and implementation (Déglise et al. 2012). Secondly, Kenya, as in many African countries, cannot reach all households relying only on the traditional mass media approaches. The most recent Demographic and Health Survey in Kenya (Kenya National Bureau of Statistics (KNBS) and ICF Macro 2010) showed that there has been a dramatic increase in ownership of telephones from 13% in 2003 to at least 62% in 2008–09. During the same time period, changes in proportions of households owning television sets only increased from 18% to 28% with no change in ownership of radio that stayed at 74%. Ownership of other mass media items increased minimally. These changes in access to mobile telephones as a media platform are unprecedented and provided an opportunity to Kenya Red Cross in integrating their use to support house-to-house canvassing visits. The innovation to use mobile phones was motivated by evidence on use of mobile phones that showed that short text messaging is a potentially powerful tool for complementing behaviour change communication because it is widely available, inexpensive and instant (Cole-Lewis and Kershaw 2010).
In this article, we document the innovative and additional activity of using house-to-house inter-personal communication visits conducted by Red Cross Volunteers and documented by a web-enabled mobile phone application to create a real-time platform for linking household and immunization service providers. This additional intervention was specifically aimed at improving coverage in urban populations (Cutts 1991; Cockcroft et al. 2009).
Methods
The American Red Cross society in collaboration with Kenya Red Cross funded a project that conducted a house-to-house canvassing for supplemental measles immunization days implemented from 3 to 7 November 2012. By design, 1952 Red Cross volunteers were recruited, trained and deployed to conduct house-to-house canvassing and mobilization of communities 1–3 days before the supplemental immunization days. This additional social mobilization intervention was conducted in eight districts of Nairobi and three districts of Nyanza/Western provinces.
The Red Cross volunteers were selected from their respective communities to assure knowledge of households to be visited, community gatekeepers and most importantly acceptance. Recruitment was based on the fundamental principles of the Red Cross/Crescent movement, namely humanity, impartiality, neutrality, independence, voluntary service, unity and universality. However, only volunteers with Android smart phones would be recruited to conduct the house-to-house canvassing. The selected volunteers were trained for 2 days. First day of training was facilitated by District Trainers on communications for the supplemental measles immunization days (including house-to-house inter-personal strategies/skills). The second day of training was facilitated by the Kenya Red Cross Trainers specifically on the use of the mobile phone application for documenting house-to-house visits. The process of training and house-to-house canvassing (before and after the supplemental measles immunization days) was supervised by the district medical officers of health directly or through the community health extension workers and their structures.
Three days before the supplemental measles immunization days, the trained Red Cross volunteers conducted house-to-house visits. For every household head or caregiver, the volunteer would provide a standardized package of messages specifying (1) the rationale of the campaigns, (2) the targeted age-group, (3) location of the nearest vaccination point, (4) what interventions the targeted children would receive and (5) expected reactions after the vaccinations. The volunteer would then open up an inter-personal communication session in which the household head/caregiver would seek clarifications or ask questions in the comfort of their compound/home. The dialogue would end with a volunteer seeking the consent of the family to bring the targeted children for a supplemental measles dose. Basic contacts (mobile phone number), number of children in the target age-range, sources of information on the supplemental measles immunization days and consent to bringing the eligible children for vaccination were captured on an epi-surveyor real-time entry screen installed on the volunteers’ mobile phone handset.
Kenya Red Cross volunteers developed the application with technical support from DataDyne consultants hired and paid by the social mobilization project. Safaricom hosted the web-access point for all volunteer collected data as part of their corporate social responsibility programme. The web application accessible to district, provincial and national levels would provide (1) sources of information flow that are not reaching the community targets, (2) basic demographics on the numbers to expect during the supplemental immunization days, (3) households (and their contacts) of families likely to refuse supplemental doses and (4) most importantly, frequency tables for reasons given by non-consenting households.
During the supplemental measles immunization days, the Red Cross volunteers were under the supervision of the vaccination team leaders and their roles were to: (1) receive mothers and caregivers bringing children, (2) screening for age eligibility (9–59 months), (3) providing non-invasive interventions like Vitamin A supplementation and (4) making reminder telephone calls or sending short text messages targeting households visited before the supplemental immunization days. When there were no children turning up for vaccinations, the volunteers would conduct reminder visits to the households in their catchment areas. At the end of each supplemental immunization day, the volunteers would relay the numbers of measles immunizations given at each vaccination point, using mobile phones to their district coaches for presentation and discussions at the daily progress review meetings. Such daily immunization data provided catalytic information for re-engineering and re-design of the vaccination delivery strategies for subsequent days.
At the end of the supplemental immunization days, all the Red Cross volunteers embarked on post-campaign house-to-house mop-up visits in which they performed the following tasks (1) cross-checked the immunization status of all children 9–59 months by history (verbal report from mother) or checking finger markings (valid coverage), (2) documented the household sources of information on the supplemental measles immunization days, (3) collected/collated community events associated with the supplemental measles immunization days and (4) identified and referred all consenting but not immunized children to the nearest vaccinating health facility. All house-to-house visits conducted after the supplemental immunization days were also documented using the real-time mobile phone data collection tool installed on the phones of volunteers.
Results
A total of 164 643 households with 161 695 children were visited by mobile phone-enabled Red Cross volunteers 3 days before the 2012 supplemental measles immunization days in eight and three districts of Nairobi and Nyanza/Western provinces, respectively. One to three days before the supplemental measles immunization days, 56% of the 164 643 households visited said that they had heard of the planned supplemental measles immunization days. Of the households visited, 75% (123 161) said that they planned to bring their children for a measles supplemental immunization dose.
In pre-campaign house-to-house visits, a total of 41 482 (25%) households with 42 041 (26%) of the targeted children had no plans to bring their children for the measles supplemental dose if they had not been reassured by the Red Cross volunteers. Post-campaign house-to-house evaluations showed that the actual number of households with un-vaccinated children was 170 only. The major reasons cited for immunization refusal in pre- and post-campaign databases (on a multiple answers question) are illustrated in Figure 1 below.
Figure 1.
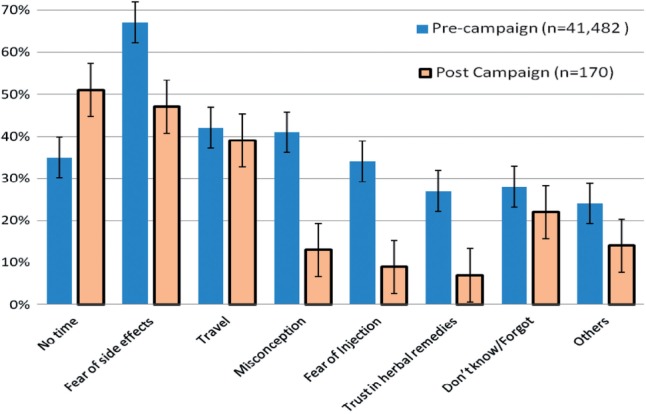
Reasons for ‘refusal’ to take a supplemental measles immunization dose in Kenya, November 2012.
Daily immunizations as documented and remitted by the Red Cross volunteers at the immunization points using mobile phones were collated and shown as illustrated in Figure 2 below:
Figure 2.
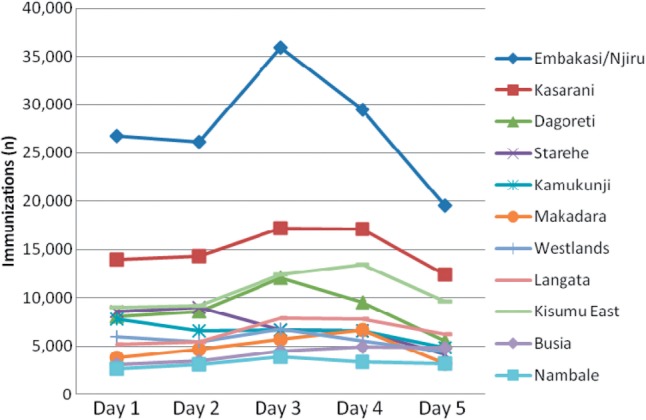
Daily monitoring of measles SIAs doses administered in selected districts of Kenya, November 2012.
After the campaign, phone-enabled Red Cross volunteers re-visited 175 617 households in which 180 493 children were counted. Of the children found in the post-campaign house visits, 96% reported to have received a measles supplemental immunization dose, although only 92% had confirmation (finger mark) of vaccination.
Sources of information on the measles campaign
Of the 17 627 households visited in post-campaign house-to-house visits, only 16 217 (response rate of 92%) were able to provide a source of information on the November measles campaign in Kenya. Table 3 outlines the frequency distribution of sources of information as provided in the post-campaign house-to-house survey.
Table 1.
Pre-campaign house visits and consent to supplemental measles immunization dose by District of Kenya; November 2012
| District | H/holds visited | Number of eligible children counted | H/holds with information prior to the visit | Number of H/holds Consenting to a supplemental measles immunization dose | % H/Hold Consenting to supplemental measles immunization |
|---|---|---|---|---|---|
| Busia/Nambale | 20 400 | 36 546 | 9106 | 14 316 | 70 |
| Dagoreti | 11 983 | 9371 | 6178 | 7855 | 66 |
| Embakasi | 25 406 | 20 066 | 14 416 | 16 395 | 65 |
| Kamukinji | 11 937 | 8728 | 8196 | 9190 | 77 |
| Kasarani | 14 283 | 12 264 | 7303 | 8218 | 58 |
| Kisumu East | 22 175 | 33 262 | 13 465 | 18 904 | 85 |
| Langata | 12 328 | 10 823 | 7335 | 11 142 | 90 |
| Makadara | 7712 | 6087 | 4219 | 6332 | 82 |
| Njiru | 13 065 | 9554 | 7413 | 8431 | 65 |
| Starehe | 14 591 | 9163 | 9266 | 12 943 | 89 |
| Westlands | 10 763 | 5831 | 6229 | 9435 | 88 |
| Total | 164 643 | 161 695 | 92 201 | 123 161 | 75 |
Table 2.
Post-campaign house Visits and Measles SIAs coverage verification by District of Kenya; November 2012
| District | H/holds visited | Number of children counted | Number of children reported vaccinated | Number of children found vaccinated and finger marked | Coverage (un weighted) |
|
|---|---|---|---|---|---|---|
| Crude (%) | Valid (%) | |||||
| Busia/Nambale | 2040 | 3646 | 3573 | 3427 | 98 | 94 |
| Dagoreti | 1085 | 1067 | 1046 | 1014 | 98 | 95 |
| Embakasi | 2757 | 2318 | 2225 | 2109 | 96 | 91 |
| Kamukinji | 1073 | 1104 | 1093 | 1027 | 99 | 93 |
| Kasarani | 1624 | 1081 | 1049 | 995 | 97 | 92 |
| Kisumu East | 2215 | 3362 | 3328 | 3295 | 99 | 98 |
| Langata | 868 | 642 | 552 | 526 | 86 | 82 |
| Makadara | 1473 | 1247 | 1023 | 985 | 82 | 79 |
| Njiru | 1538 | 1226 | 1177 | 1116 | 96 | 91 |
| Starehe | 2116 | 1636 | 1538 | 1472 | 94 | 90 |
| Westlands | 838 | 664 | 637 | 598 | 96 | 90 |
| Total | 17 627 | 17 993 | 17 241 | 16 564 | 96 | 92 |
Table 3.
Sources of information on measles SIAs from post-campaign house visit in Kenya, November 2012
| Where did you get the information on supplemental measles immunization days conducted from 3 to 7 November 2012? | Frequency of citation (multiple responses) | Proportionate contribution (%) |
|---|---|---|
| House visit | 12 098 | 75 |
| Megaphones | 6243 | 38 |
| Radio | 5280 | 33 |
| Health facility | 3229 | 20 |
| TV | 2698 | 17 |
| CHW | 2320 | 14 |
| Newspaper | 1210 | 7 |
| Others | 2104 | 13 |
Discussion and conclusions
Mobile phone platforms were used to obtain real-time data on household perceptions, attitudes and concerns (reasons for likely refusal to take a supplemental measles dose). The innovation to use mobile phones (for household data collection/transmission, short text messages and phone calls) was adapted based on reviewed evidence on providing reminders for attendance of health care appointments (Car et al. 2012). This was in addition to documented importance of mobile phones in promotion of physical activity in children and adolescents (Lau et al. 2011), adherence to malaria treatment guidelines in Kenya (Zurovac et al. 2011), testing and treatment of Tuberculosis (TB), HIV and syphilis (Horvath et al. 2010; Lester et al. 2010; Person et al. 2011; Pop-Eleches et al. 2011). Information collected using mobile phones was in real-time uploaded to a web application that was designed based on the principles of EpiCollect (Aanensen et al. 2009).
The characteristics of measles epidemiology in Kenya (unpublished surveillance reports) justified extra and focused efforts directed to the three major cities of Kenya in the November 2012 supplemental immunization days. In the three major cities of Nairobi, Nambale and Kisumu, special and additional strategies (house-to-house social mobilization by Red Cross volunteers supported by mobile phone applications) were put in place, given their size and the potential roles in sustaining measles transmission. Specifically, the high population density that is commonly associated with increased risk of measles transmission (Anderson and May 1990). Although measles transmission can be interrupted with lower immunization coverage levels in sparsely populated rural areas, the urban focus was needed to attain higher coverage rates needed for similar disease control effects (Cutts 1991; Atkinson and Cheyne 1994). Emphasis being mobile phone supported word-of-mouth communications by Kenya Red Cross volunteers over and above the community health extension workers system, established by the Ministry of Public Health and Sanitation.
Data from the house-to-house visits that spread information by word-of-mouth and conducted dialogue at household level show that the large majority (75%) of urban households in selected Kenya cities would accept supplemental measles immunizations with or without additional information. The 25% likely refusals in these cities compare well with what is published on individual and contextual factors associated with low immunization coverage in Sub-Saharan Africa (Wiysonge et al. 2012). Although house-to-house canvassing strategy for social mobilization was conducted in previous supplemental immunization activities (SIAs), no similar data had ever been collected and made available in Kenya. This mobile phone application enabled a cross-sectional status of awareness on supplemental measles immunization days at least a day before the start date.
As Red Cross Volunteers spread information by word-of-mouth and held dialogue sessions on immunization at household level, they also collected data on sources of information, education and awareness. This data would then trigger the shifting of communication strategies from information, education and awareness to wider but yet specific ecological complexities that influence household choices and capacity to choose. This shift in social mobilization was informed by the documented experiences from the Polio Eradication Initiative that emphasizes use of data to guide actions in behaviour change communication (Taylor and Shimp 2010). In the house-to-house canvassing visits by Red Cross volunteers, emphasis would not be on a top-down information delivery approach but rather a hybrid strategy that combined informed activism supported by programme rationalization and key messages (Obregón and Waisbord 2010). Comparing pre- and post-campaign reasons for refusal shows that targeted communication significantly reduced fear of injections, misconceptions, trust in herbs, fear of side effects and lack of time. Lack of knowledge/forgetting and travel did not improve with house-to-house canvassing visit, underscoring the importance of good service delivery micro-planning in supplemental measles immunization days specifically and immunization in general (Shefer et al. 1999; Ward et al. 2012).
With daily immunization targets provided to all districts and provinces, we were able to document the slow start on Day 1 and 2 (Saturday and Sunday) of the supplemental measles immunization days, when most vaccinations were expected and allowed the campaign managers to take timely corrective actions. Major reasons for the slow start (unpublished monitoring and daily review reports) were heavy rains, parents’ expectation of house-to-house vaccination as had been the practice with supplemental polio immunization days, inadequacies in vaccination teams (numbers and distribution) and late start of sessions. Armed with evidence of slow starts, innovations in the campaign delivery strategy and plan were put in place on Day 3 and 4 (Monday/Tuesday) that included (1) the creation of additional teams (by splitting vaccinators from the standard two, to one vaccinator), (2) creation of more temporary fixed points, (3) village-to-village vaccination services and (4) targeting Early Childhood Development Centers. This adaptive planning and management of supplemental measles immunization activities was always feasible but was more evidence based due to information available on real-time numbers of children immunized relayed by mobile phones on a daily basis.
Post-campaign house-to-house coverage verification data show that 9 out of 11 districts supported by Kenya Red Cross attained ≥90% supplemental measles immunization coverage. Even when 90% measles coverage was not attained, the changes in attained rates (comparing 2009 and 2012 administrative data on follow-up campaigns) were increased from 57% and 53% to 73% and 86% in Langata and Makadara districts, respectively. These findings are collaborated by the administrative reports (unpublished) by districts. Most importantly, the data show that despite several other confounding factors across board, the changes in coverage are more pronounced in districts that were introducing house-to-house strategy for the first time compared with those implementing the phone-documented house-to-house visits (unpublished 2009 and 2012 administrative coverage reports) for the second time.
The major sources of information on the 2012 supplemental measles immunization days in Kenya were documented as house visits, megaphones and radio in descending order. This data show that house-to-house visits can be very penetrative compared with traditional mass media approaches. The observed importance of interpersonal communication was confirmed by a survey in three coast region districts in which exit interviews with 104 mothers/caretakers of measles vaccine recipients showed that the major sources of information were health workers (health facility at 24%), house visits by community health extension workers at 17% and radio at 14%. Although radio and other mass media approaches to communication for immunization remain relevant, these results show that a house visit, by an independent and neutral but trusted community resource person like Red Cross volunteers contributes to an array of factors that parents need in decision making to vaccinate or not to vaccinate (Jackson et al. 2008). The trust and confidence Kenya Red Cross enjoys as a brand seemed to be more effective than all other sources of information, which is in line with what has been documented elsewhere (Brownlie and Howson 2005; Hobson-West 2007).
In conclusion, this article articulates the targeted use of a trusted, neutral and community-based support by Red Cross volunteers in attaining high measles coverage rates in selected urban populations of Kenya. The use of house-to-house strategy supported by real-time documentation using mobile phones to conduct dialogue and seek consent to immunization is a shift from awareness, education and information giving approaches that have dominated planning and execution of SIAs for decades. Second, documentation of house-to-house visits showed that this approach combined with giving information and education as well as seeking consent and creating a feedback loop between households and service delivery planners had a pronounced improvement in vaccination uptake. In turn, individualized and focused dialogue is documented to convince immunization sceptics while illustrating that good and adaptive operational micro-plans are an essential element to attainment of high vaccination coverage. Last, we document that a house visit in which dialogue is held is more remembered and cited as a source of information on supplemental immunization. We recommend the use of household dialogue by trained house-to-house volunteers in promotion of immunization service utilization in future immunization promotional campaigns. Where access to mobile communication technologies is high, it is also recommended that documentation of house visit findings be used to create a real time platform for adaptive communication strategy.
Acknowledgements
The authors are indebted to Schyns N. Bahati, systems design and developer, who developed the web-enabled mobile phone application, Benson Simba and Bibi Mbete as regional health officers who supervised the field data collection, quality assurance and adherence to the project guidelines and Patrick Gitahi, Kenya Red Cross Monitoring and Evaluation officer, who co-ordinated, collated and analysed all the data presented in this study. Special thanks to all the Kenya Red Cross Volunteers and co-ordinators that conducted and documented the house visits with the web-enabled mobile phone application. This was an operations study funded by American Red Cross and implemented by Kenya Red Cross Society, as part of the national social mobilization and communication plan for the 2012 supplemental measles immunization campaign in Kenya. The findings in this article have been presented to the National Steering and Coordination committee for measles supplemental immunization activities in Kenya.
Conflict of interest statement. None declared.
References
- Aanensen DM, Huntley DM, Feil EJ, et al. EpiCollect: linking smart phones to web applications for epidemiology, ecology and community data collection. PLoS One. 2009;4:e6968. doi: 10.1371/journal.pone.0006968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson RM, May RM. Immunization and herd immunity. The Lancet. 1990;335:641–5. doi: 10.1016/0140-6736(90)90420-a. [DOI] [PubMed] [Google Scholar]
- Atkinson SJ, Cheyne J. Immunization in urban areas: issues and strategies. Bulletin of the World Health Organization. 1994;72:183–94. [PMC free article] [PubMed] [Google Scholar]
- Brownlie J, Howson A. ‘Leaps of faith’ and MMR: an empirical study of trust. Sociology. 2005;39:221–39. [Google Scholar]
- Car J, Gurol-Urganci I, De Jongh T, et al. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Systematic Reviews. 2012;7:CD007458. doi: 10.1002/14651858.CD007458.pub2. [DOI] [PubMed] [Google Scholar]
- Cockcroft A, Anderson N, Omer K, et al. One size does not fit all: local determinants of measles vaccination in four districts of Pakistan. BMC International Health and Human Rights. 2009;9(Suppl 1):S4. doi: 10.1186/1472-698X-9-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiologic Reviews. 2010;32:56–69. doi: 10.1093/epirev/mxq004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutts FT. Strategies to improve immunization services in urban Africa. Bulletin of the World Health Organization. 1991;69:407–14. [PMC free article] [PubMed] [Google Scholar]
- Déglise C, Suggs LS, Odermatt P. Short message service (SMS) applications for disease prevention in developing countries. Journal of Medical Internet Research. 2012;14:e3. doi: 10.2196/jmir.1823. doi:10.2196/jmir.1823. http://www.jmir.org/2012/1/e3/, accessed 8 November 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobson-West P. ‘Trusting blindly can be the biggest risk of all’: organised resistance to childhood vaccination in the UK. Sociology of Health & Illness. 2007;29:198–215. doi: 10.1111/j.1467-9566.2007.00544.x. [DOI] [PubMed] [Google Scholar]
- Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. The Lancet. 2010;376:1838–45. doi: 10.1002/14651858.CD009756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson C, Cheater FM, Reid I. A systematic review of decision support needs of parents making child health decisions. Health Expectations. 2008;11:232–51. doi: 10.1111/j.1369-7625.2008.00496.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenya National Bureau of Statistics (KNBS) and ICF Macro. 2010. Kenya Demographic and Health Survey 2008-09. Calverton, Maryland: KNBS and ICF Macro. http://www.measuredhs.com/pubs/pdf/FR229/FR229.pdf, accessed 30 October 2012. [Google Scholar]
- Lau PWC, Lau EY, Wong DP, Ransdell L. A systematic review of information and communication technology–based interventions for promoting physical activity behavior change in children and adolescents. Journal of Medical Internet Research. 2011;13:e48. doi: 10.2196/jmir.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester RT, Ritvo P, Mills EJ, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. The Lancet. 2010;376:1838–45. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- Obregón R, Waisbord S. The complexity of social mobilization in health communication: top-down and bottom-up experiences in polio eradication. Journal of Health Communication. 2010;15(Suppl 1):25–47. doi: 10.1080/10810731003695367. [DOI] [PubMed] [Google Scholar]
- Person AK, Blain MLM, Jiang H, et al. Text messaging for enhancement of testing and treatment for tuberculosis, human immunodeficiency virus, and syphilis: a survey of attitudes toward cellular phones and healthcare. Telemedicine Journal and e-health. 2011;17:189–95. doi: 10.1089/tmj.2010.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pop-Eleches C, Thirumurthy H, Habyarimana JP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25:825–34. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shefer A, Briss P, Rodewald L, et al. Improving immunization coverage rates: an evidence-based review of the literature. Epidemiologic Reviews. 1999;21:96–142. doi: 10.1093/oxfordjournals.epirev.a017992. [DOI] [PubMed] [Google Scholar]
- Taylor S, Shimp L. Using data to guide action in polio health communications: experience from the Polio Eradication Initiative (PEI) Journal of Health Communication. 2010;15(Suppl 1):48–65. doi: 10.1080/10810731003698585. [DOI] [PubMed] [Google Scholar]
- Waisborda S, Shimp L, Ogden EW, Morry C. Communication for polio eradication: improving the quality of communication programming through real-time monitoring and evaluation. Journal of Health Communication. 2010;15(Suppl 1):9–24. doi: 10.1080/10810731003695375. [DOI] [PubMed] [Google Scholar]
- Ward K, Chow MYK, King C, Leask J. Strategies to improve vaccination uptake in Australia, a systematic review of types and effectiveness. The Australian and New Zealand Journal of Public Health. 2012;6:369–77. [Google Scholar]
- Wiysonge CS, Uthman OA, Ndumbe PM, Hussey GD. Individual and contextual factors associated with low childhood immunisation coverage in sub-Saharan Africa: a multilevel analysis. PLoS One. 2012;7:e37905. doi: 10.1371/journal.pone.0037905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) Global Measles and Rubella Strategic Plan 2012-2020. 2012. http://www.who.int/immunization/newsroom/Measles_Rubella_StrategicPlan_2012_2020.pdf, accessed 20 November 2012. [Google Scholar]
- Zurovac D, Sudoi RK, Akhwale WS, et al. The effect of mobile phone text-message reminders on Kenyan health workers' adherence to malaria treatment guidelines: a cluster randomised trial. The Lancet. 2011;378:795–803. doi: 10.1016/S0140-6736(11)60783-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


