Abstract
Intramedullary schwannomas are rare spinal cord tumors. Most of these tumors have been reported as a single lesion in the spinal cord. Up until today approximately 50 cases of intramedullary shwannomas not related to neurofibromatosis have been described. We describe a rare case of thoracic intramedullary tumour in a 28 year old male patient who presented with progressive weakness of both the lower limbs and decreased sensation below D2 dermatomal level. Magnetic resonance imaging revealed an intramedullary lesion from D1 toD7. D1 to D7 laminoplasty and near total excision of the mass done. Total removal was difficult because of the infiltrative nature of the tumour. Histopathological report confirmed the diagnosis of the schwannoma. Possible site of origin and pathogenesis of intramedullary tumour have been discussed.
Keywords: Intramedullary schwannomas, neurofibromatosis, schwann cell
Introduction
Spinal canal shwannomas account for 30% of spinal tumors most of which are generally associated with neurofibromatosis, type 1 and type 2. Intramedullary shwannomas not associated with neurofibromatosis are rarely reported, which account for 0.3% of all medullary tumors and 1.1% of spinal shwannomas.[1] These lesions have appeared as intramedullary single lesions or dumbbell intra and extramedullary ones.
The authors report a case of thoracic intramedullary shwannomas and discuss the origin and pathogenesis within the spinal cord.
Case Report
A 28-year-old male patient was admitted with gradual onset weakness of both lower limbs for last three years with retention of urine, for which he was catheterized. He had no traumatic accident, no other previous disorders such as neurofibromatosis or specific skin lesions.
Neurological examination revealed that motor power of both the legs was 1/4 with flexor spasms. All modalities of sensation were absent below D2 dermatomal level. The bilateral knee jerks and ankle jerks were hyperactive and well sustained ankle clonus was observed.
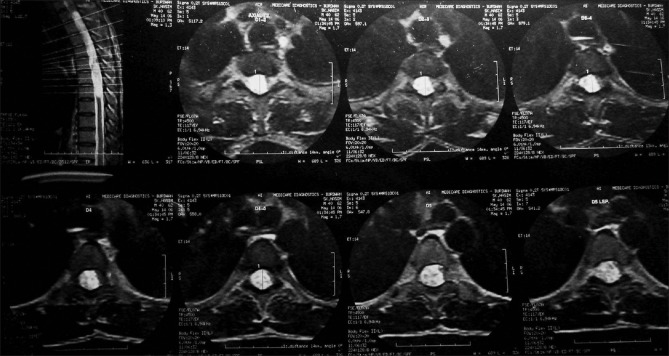
Magnetic resonance imaging shows an ill demarcated intramedullary lesion extending from D1 to D7. The lesion was hypointense on T1 weighted images and hyperintense on T2 weighted images [Figure 1]. Gadolinium contrast images shows homogeneous intense enhancement of the solid component and irregular peripheral enhancement of the cystic part [Figure 2]. Axial sections show symmetrical expansion of the spinal cord with no neural foraminal dilatations [Figure 3]. Radiological diagnosis was suggestive of ependymoma or astrocytoma. Magnetic resonance imaging (MRI) of brain was within normal limit with no known primary elsewhere decreasing the possibility of metastasis.
Figure 1.

MRI sagittal section T2 weighted image shows intramedullary hyperintense lesion extending from D1 to D7
Figure 2.

MRI sagittal section T1 weighted image with gadolinium contrast shows homogeneous intense enhancement of the solid component and irregular peripheral enhancement of the cystic part
Figure 3.
MRI axial sections shows symmetrical expansion of the spinal cord with no neural foraminal dilatations
The operation was done with standard posterior middle approach. D1 to D7 laminoplasty was performed and dura opened in the midline. After a median myelotomy, near total removal of tumor was done. The intra-operative aspect of the lesion was a grayish mass with both solid and cystic component. Infilterative nature of the mass made the total resection impossible. The nerve roots were not involved by the tumor. Histopathological analysis confirmed the diagnosis of schwannoma [Figures 4 and 5].
Figure 4.
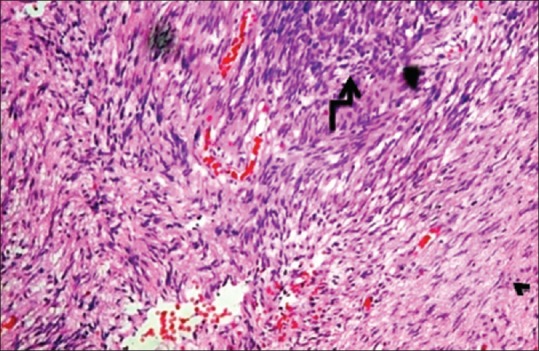
Histopathology of schwannoma with hypercellular Antony A (big arrow) and hypocellular Antony B areas (Arrow head)
Figure 5.
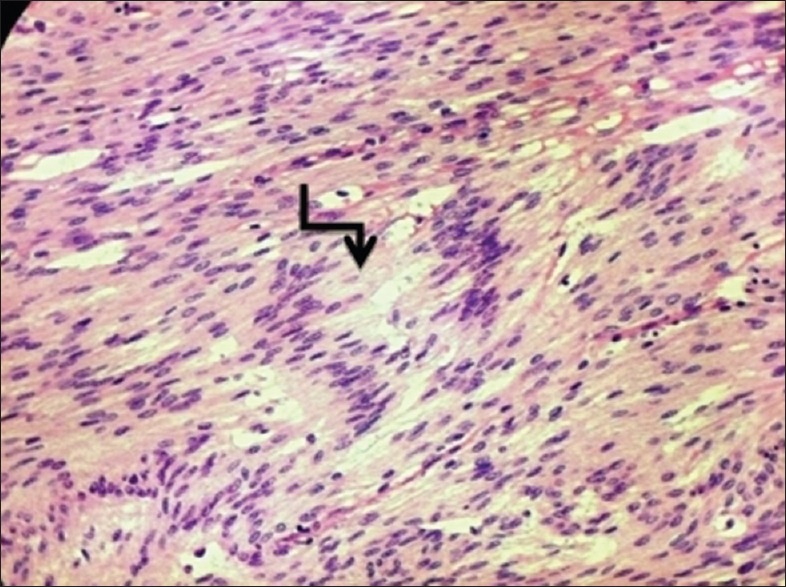
Histopathology of schwannoma with verocay body (arrow)
Post operatively, patient developed both touch and pain sensations on second postoperative day and discharged with both leg power of 3/5 on 10th postoperative day.
Discussion
Kernohan has been recognized as the first neurosurgeon to report an intramedullary schwannoma case in 1952, though Penfield had already described an intramedullary lesion with schwannomas characteristics in 1932.[2]
Conti et al.,[3] analyzed the literature from 1931 through 2002 and found only about 50 reported cases of non-neurofibromatosis related intramedullary schwannomas.
Schwannomas originate from the Schwann cells which are absent in the central nervous system; thus it can explain the rarity of intramedullary schwannomas. The pathogenesis of intramedullary schwannoma is still not clear and various hypotheses have been proposed. Probable origin of these tumors include the following:
Schwann cells along the intramedullary perivascular nervous plexus,[4]
Focal intramedullary proliferation of schwann cells in reaction to chronic diseases or trauma,
Ectopic schwann cells origination from migrating neural crest cells, and
schwann cells related to aberrant intramedullary myelin fibers.
And also, schwann cells in posterior nerve root at root entry zone are assumed to be one of the pathogenesis of intramedullary schwannomas. These areas are called as ‘critical areas’, as described by Mason,[5] where nerve root loses its sheath, could enter the subpial area in the spinal cord and appear as an intramedullary mass.
The male:female ratio for intramedullory schwannomas is 3:1 with a mean age of 40 years old. They are usually single lesions affecting the cervical spinal cord (63%), the thoracic spinal cord (26%), and the lumber spinal cord (11%). They have a slow growth pattern and because of this, the average interval between first symptom and diagnosis is 28.2 months (from 6 months through 20 years).[6]
According to new WHO classification of tumors, there are three types of shwannomas; cellular, plexiform, and melanotic. The infiltrative pattern of some intramedullary schwannomas make total resection impossible, and some authors suggest in these cases the use of radiotheraphy for residual lesions.[7]
The most described clinical manifestation is the pyramidal syndrome followed by sensitivity complaints and sphincter dysfunction. There are reports of muscular fasciculations as the first symptom.
According to Demachi,[8] there is no correlation between the classification of Antoni and the MRI findings. The Antony A-type is characterized by the presence of compact wave shaped cells rounded by a reticular net. The Anatomy B-type has large and loose cells surrounded by a collagenous web. Complete excision is the treatment of choice for spinal schwannomas, including intramedullary ones. In the present case, the plane of separation between the tumor and cord tissue was so indistinct that complete resection could not be done (Infiltrative type) and for residual tumor radiotherapy was planned.
Conclusion
Although rare, the intramedullary schwannoma should be considered as a possible diagnosis for an intramedullary lesion. Complete excision is the goal but sometime this cannot be accomplished due to infiltrative characteristic of the tumor. Better understanding of the pathogenesis will definitely guide the proper management of intramedullary schwannoma.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Brown KM, Dean A, Sharr MM. Thoracic intramedullary schwannoma. Neuropathol Appl Neurobiol. 2002;28:421–4. doi: 10.1046/j.1365-2990.2002.00415.x. [DOI] [PubMed] [Google Scholar]
- 2.Penfield W. Notes on operative technic in neurosurgery. Ann surg. 1946;124:383–5. [PubMed] [Google Scholar]
- 3.Conti P, Pansini G, Mouchaty H, Capuano C, Conti R. Spinal neurinomas: Retrospective analysis and long-term outcome of 179 consecutively operated cases and review of the literature. Surg Neurol. 2004;61:34–43. doi: 10.1016/s0090-3019(03)00537-8. [DOI] [PubMed] [Google Scholar]
- 4.Feigin I, Ogata J. Schwann cells and peripheral myelin within human central nervous tissue: The mesenchynal character of Schwann cells. J Neurophathol Exp Neurol. 1971;30:603–12. doi: 10.1097/00005072-197110000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Mason TH, Keigher HA. Intramedullary spinal neurilemmoma: Case report. J Neurosarg. 1968;29:414–6. doi: 10.3171/jns.1968.29.4.0414. [DOI] [PubMed] [Google Scholar]
- 6.Lopez J, Diaz DR, Medina YC, Jeronimo HS, Mendez AZ, Vazquez AG, et al. Schwannoma intramedullary cervical. Arch neurocien. 2004;9:55–8. [Google Scholar]
- 7.Wood WG, Rothman LM, Nussbaum BE. Intramedullary neurilemoma of the cervical spinal cord: Case report. J Neurosurg. 1975;42:465–8. doi: 10.3171/jns.1975.42.4.0465. [DOI] [PubMed] [Google Scholar]
- 8.Demachi H, Takashima T, Kadoya M, Suzuki M, Konishi H, Tomita K, et al. MR imaging of spinal neurinomas with pathological correlation. J Comput Assist Tomogr. 1990;14:250–4. doi: 10.1097/00004728-199003000-00017. [DOI] [PubMed] [Google Scholar]