Abstract
This update on the epidemiology and prevention of HIV in the United States is intended to provide contextual background that will help inform an understanding of recent developments in the domestic HIV epidemic. We describe the epidemiology of HIV disease in the US and the HIV continuum of care based on data collected primarily through HIV surveillance systems led by the Centers for Disease Control and Prevention including HIV incidence, prevalence, comorbidities and death. Populations and geographic regions disparately impacted by HIV are also highlighted. The HIV prevention armamentarium is also described including behavioral approaches to prevention, the emerging availability of biomedical prevention interventions such as pre-exposure prophylaxis, and structural and population-level interventions including treatment as prevention. Finally gaps in our understanding of the epidemic are underscored and suggestions for future epidemiologic research are proposed.
Keywords: HIV, epidemiology, care continuum, surveillance, prevention, biomedical, treatment as prevention
Introduction
During the past several years, there has been an upsurge of important policy initiatives for HIV epidemic control in the United States (US), epidemiologic approaches that have deepened our understanding of the dynamics of HIV prevention and treatment, and critical new research that has provided substantial additions to the HIV prevention armamentarium. On a policy level, the publication of the first-ever National HIV/AIDS Strategy (NHAS) with its three primary goals of “reducing HIV incidence”, “increasing access to care and optimizing health outcomes”, and “reducing HIV-related health disparities” was a sentinel event that has galvanized the response to the domestic HIV epidemic.1 Epidemiologically, the recognition that the epidemic has become stubbornly persistent in sub-populations such as youth and black men who have sex with men (BMSM) provides a focal point to guide HIV prevention activities.2 In addition, the conceptualization of the HIV continuum of care as a spectrum from HIV diagnosis through viral suppression3 served as the foundation for the measurement of these population-based parameters over time,4 establishment of national goals for these outcomes,5 and development of prevention programs specifically targeting these goals6,7 In addition, the visualization of geographic “hot spots” through innovative mapping programs such as AIDSVu8, and the potential to assess transmission dynamics in these hotspots using molecular epidemiology techniques,9 can be used to target the use of limited HIV prevention resources. From a research perspective, the demonstration of the efficacy of pre-exposure prophylaxis10 and treatment as prevention11 were landmark studies that solidified the central role of antiretroviral therapy in HIV prevention programs. This update on the epidemiology and prevention of HIV in the US is intended to provide contextual background that will help inform an understanding of these recent developments.
Epidemiology
Thirty-four years after AIDS was first described, there are an estimated 35 million people living with HIV globally.12 There are approximately 1.2 million people living with HIV in the US, accounting for about 3.5% of the global burden of disease.4 According to UNAIDS, the US has a concentrated epidemic as the majority of infections occur in high-risk subpopulations and less than one percent of the general population is infected.13 This section will describe the epidemiology of HIV disease in the US based on data collected primarily through HIV surveillance systems led by the Centers for Disease Control and Prevention (CDC) in collaboration with state and local public health departments. It will aim to highlight our current knowledge of the epidemic, populations disparately impacted by HIV, gaps in our understanding of the epidemic, and propose areas for additional research based on our current knowledge of the epidemic.
The HIV epidemic measured using surveillance data
In addition to cohort studies that have provided essential information on the natural history of HIV disease and the impact of treatment over the decades, surveillance data have allowed documentation of the magnitude of the epidemic. The US National HIV Surveillance system (NHSS) has characterized the epidemic in US since the initial cases in 1981; NHSS is CDC funded in 50 states, the District of Columbia (DC), and six US dependent areas.14 Initially focused on counting and describing cases of AIDS, the surveillance system evolved as the epidemic and our understanding of it unfolded. AIDS surveillance case definitions expanded to include certain opportunistic infections and laboratory tests such as CD4 counts with the most recent revision in 2014.15 As persons with HIV began to live longer due to earlier diagnosis and the availability of life-prolonging treatments, national surveillance programs expanded to capture a more complete spectrum of HIV infection and disease—from describing behaviors antecedent to HIV infection through HIV-related illness and death. CDC surveillance systems thus mirror this pathway and include behavioral surveillance, incidence surveillance, molecular epidemiology surveillance, and the morbidity monitoring project.16
Incidence
HIV incidence estimates are critical as they provide an indication of the leading edge of the epidemic. Identification of locations and populations in which the majority of new infections occur allows prevention efforts to be appropriately targeted. Use of BED assays has facilitated the detection of recently infected cases versus those who have been living with HIV disease but have only recently been diagnosed.17,18 Through the CDC’s HIV Incidence Surveillance system, recent HIV incidence estimates have shown there are 50,000 new HIV infections annually in the US.19,20 Populations with the highest proportion of incident cases include adolescents ages 13–24, young adults ages 25–35, Black persons, and men who have sex with men (MSM); the highest number of new infections was among young BMSM ages 13–24 in 2010.19 While the incidence continues to increase in these populations, new infections among persons who inject drugs (IDU) declined in recent years19, most likely due to the implementation of harm reduction programs and syringe exchange services. Despite this, the high number of continued transmissions has unfortunately been stable without evidence of decrease, highlighting the need for enhanced prevention efforts. Epidemiologic research to understand how to identify persons who are at risk for HIV and interrupt potential transmissions should therefore be a priority area.
Prevalence
The number of persons living with HIV has increased dramatically since the start of the epidemic. This is in part due to identification of new infections but also due to the increasing availability of life-prolonging antiretroviral treatments. An estimated 880,440 persons have been diagnosed and living with HIV in the US14; another 14% remain undiagnosed.4 Although the magnitude of the US epidemic is less severe than other regions of the world such as Sub Saharan Africa, there are pockets of high prevalence in which particular subpopulations are disproportionately affected including black persons and MSM. Highlighting a critical healthcare disparity, black individuals make up 13% percent of the US population21 yet account for 43% of persons living with HIV.14 Similarly, while the epidemic started among MSM and they represent a very small proportion of the underlying US population, they continue to be the most affected risk group with an increasing trend in prevalence in the last 5 years.14
Morbidity and Mortality
The epidemiology of HIV related morbidity and mortality has also shifted over the past three decades. Whereas opportunistic infections such as Pneumocystis carinii pneumonia were the most common AIDS defining illnesses in the early 1980s, opportunistic illnesses and AIDS defining cancers have declined significantly since the start of the epidemic. Expected survival for someone living with HIV is now over 20 years and 40% of persons with HIV will die from a non-HIV related cause.22 With recent HHS guidelines recommending antiretroviral therapy for all HIV-infected persons regardless of CD4 count23, these issues are likely to grow in importance as increasing numbers of patients are exposed to antiretrovirals and consequently living longer.
Given improved survival among HIV-infected persons, HIV is sometimes perceived as a chronic treatable condition, which in turn can make prevention messaging and efforts more difficult to achieve.24 Data from the CDC’s Morbidity Monitoring Project found that approximately half of HIV infected MSM engaged in unprotected anal intercourse and 33% of injection drug users shared syringes, serving as a barrier to secondary prevention efforts.16,25 The HIV chronic disease model presents an area for research including the role of treatment fatigue and secondary prevention interventions. The field of HIV and aging is also emerging. Data suggest that chronic inflammation and long term exposure to antiretrovirals may contribute to morbidity and mortality among this population, yet many questions remain as to the underlying mechanisms.26
Disparities
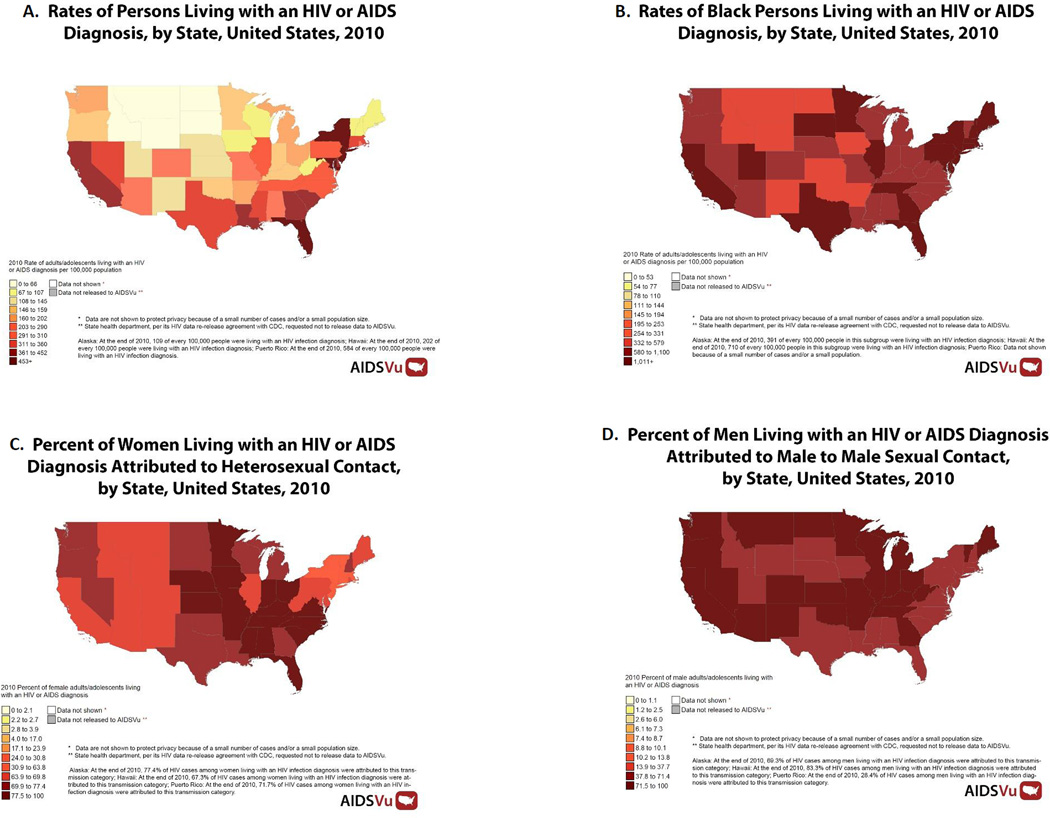
Despite progress in understanding the HIV epidemic in the US, many disparities in prevention, care, and treatment remain both geographically and demographically. Geographically, while cities such as New York, San Francisco and Washington, DC have traditionally had some of the highest HIV prevalence rates, recent declines in the number of new cases have been observed in these cities. New York City reported a decline in new HIV diagnoses among all populations form 2001 to 2013.27 San Francisco also reported a decline in new HIV cases between 2007 and 201128 and recently Washington, DC released data showing a 52% decline in the number of new cases over the past five years.29 In contrast, Southern cities in the US, including Miami, Florida and Atlanta, Georgia have seen increases in the number of persons diagnosed with HIV.30,31 This geographic disparity has been highlighted by Sullivan and colleagues who have developed the AIDSVu program which allows for visualization of the epidemic in the context of other social determinants including race, poverty, and access to care (Figure).8 The emergence of the epidemic in the Southern US has been attributed to issues such as stigma, elevated sexually transmitted disease prevalence, and treatment access.32 The ability to identify these geographic hot spots of continued transmission may be useful in describing sexual networks and transmission patterns through phylogenetic mapping, and directing prevention interventions aimed at interrupting transmission.
Figure.
Maps are from AIDSVu (www.aidsvu.org) and highlight the disproportionate impact of HIV by geographic region (Map A), by race (Map B), by mode of HIV transmission for males and females (Maps C and D, respectively).
Racial and ethnic disparities in HIV incidence and prevalence also continue to persist. Data from CDC show that BMSM ages 13–24 accounted for 58% of new infections among all MSM.33 National HIV Behavioral Surveillance data estimate that 68 to 75% of young MSM ages 18 to 24 and 59% of BMSM were unaware of their HIV infection.34 Potential explanations as to why this group is at highest risk for HIV include social determinants such as structural barriers to healthcare, stigma and homophobia, poverty, and unemployment as well as sexual network factors including high background prevalence of sexually transmitted infections, and small and intertwined sexual networks.35–39 Ongoing research to address the epidemic among this population include efforts on the part of the HIV Prevention Trials Network (www.HPTN.org) and the establishment of cohorts of both HIV negative and positive MSM36; however, additional research focusing on prevention interventions in this population is necessary.
HIV Continuum of Care
The HIV continuum of care is a relatively new way of describing the epidemiology of HIV infection and identifying gaps in the ability to diagnose, care for, and successfully treat persons living with HIV. The continuum of engagement in HIV care was described by Cheever et al at HRSA in 2007,3 adapted as the HIV treatment cascade by others in the scientific literature40,41 and defined as the continuum of HIV care by the CDC in 2011.42 The care continuum begins with HIV infection, which is followed by HIV diagnosis, linkage to and retention in care, and ends with receipt of antiretroviral therapy and viral suppression, defined as a viral load less than 200 copies/ml.4 Viral suppression is the ultimate goal in the treatment of HIV disease as it results both in individual benefit to an HIV-infected patient’s health, and in public health benefit through a reduction of the risk that an infected person will transmit the virus to others.11,43
The HIV care continuum is a model that is currently being used in the US to assist with monitoring progressing in achieving the National HIV/AIDS Strategy.5 National estimates of the care continuum have shown that 86% percent of people were aware of their HIV diagnosis, 80% were linked to care within 3 months of diagnosis, 40% were engaged in care, and 30% achieved viral suppression.4 The low rates of viral suppression were attributed to the 20% of persons thought to be infected but not yet diagnosed, the 66% of persons out of care, the 4% who are in care but not on antiretroviral therapy, and the 10% who are on therapy but not suppressed.4 These gaps highlight the need for initiatives to promote non-risk based HIV testing, to develop innovative linkage, retention and re-engagement strategies, and to improve current adherence strategies. While the care continuum ends with the achievement of viral suppression, the ability to sustain lifelong suppression is necessary among persons with this chronic illness. Thus, scientific advances are needed to facilitate the maintenance of suppression and engagement in care, whether through pharmaceutical research such as the development of long acting antiretrovirals, or through behavioral research to assess (for example) the role of community health workers and treatment partners in supporting lifelong adherence.44
Gaps and future directions
While the use of surveillance data allows for greater understanding of the HIV epidemic in the US, it has several limitations. Persons captured through surveillance only include those who have been diagnosed and reported to a surveillance system. For example, CDC estimates that NHSS data are representative of 80% of all HIV cases in the US.45 Establishing cohorts that follow high risk groups such as young BMSM may allow researchers to better characterize risk behaviors, social and sexual networks, and allow for more rapid diagnosis of incident infections and thus prevent ongoing transmission.
Many initiatives are underway to address gaps in the HIV care continuum. Routine HIV testing in medical settings has been the standard recommendation from CDC since 2006, and linkage to care rates are relatively high when coupled with testing. Many high prevalence cities, including the Bronx, New York,46 Washington, DC,47 Houston, Texas,48 and Philadelphia, Pennsylvania49 have already implemented routine HIV testing programs in response to the revised CDC recommendations and have all been able to test and identify thousands of infected persons. Home-based HIV testing and internet-based HIV counseling offer new opportunities to identify persons unaware of their infection. Numerous local and federal initiatives have begun to improve linkage to and retention in care,6,7 and health information exchanges have now been shown to facilitate re-engagement in care.50
The HIV Prevention Armamentarium
HIV prevention in the US has in many ways evolved parallel to HIV surveillance: the addition of each new scientific breakthrough to prevent HIV has rapidly contributed to an expanding armamentarium of new tools to slow the epidemic.10,11,51–55 As with advances seen in medicine, demonstration that a given tool is effective does not immediately translate into adoption. Uptake of prevention methods in the US and beyond remains challenging as social norms evolve, provider and patient knowledge bases expand, and healthcare infrastructure struggles to keep pace with scientific advancement. Still, with increasing approaches to HIV prevention and availability of more modalities than ever before to prevent HIV, individual-level and populationlevel approaches are available to suit multiple situations and subpopulation needs, at nearly all points in the life course.10,54,56–62 Combination prevention efforts that enlist multiple methods to prevent HIV rather than relying on just one, and the evolving concept of a “Prevention Continuum”,4,10,11,41,43,53,54,56,58,59,62–66 now allow healthcare providers and community agencies to identify appropriate prevention methods based on the unique needs of each individual at a given point in time in concert with testing and outreach efforts. This section will describe currently available behavioral, biomedical, population-level and structural interventions that effectively prevent HIV along with relative strengths and challenges of each (Table).
Table 1.
Examples of HIV Prevention Strategies
| Individual-level |
|---|
| Behavioral |
| Abstinence |
| Serosorting, seropositioning |
| Male and female condom use |
| Individual-level counseling |
| Group counseling |
| Theoretically-based prevention programs (e.g., DEBIs, social cognitive theory, motivational interviewing) |
| Sub-population-specific prevention programs (e.g., transgender women, at risk Latina heterosexual women, black MSM) |
| Biomedical |
| Perinatal prophylaxis (including prevention of transmission via breastmilk) |
| Post-exposure prophylaxis (occupational and non-occupational) |
| Pre-Exposure prophylaxis |
| Microbicides |
| Vaginal rings |
| Combination HIV prevention/contraception interventions |
| Eventual vaccine |
| Control of sexually transmitted diseases |
| Syringe exchange programs |
| Maintenance therapies (e.g., methadone) |
| Population-level and structural |
| Expanded access to health insurance |
| Treatment as prevention |
| Routine HIV screening |
| Increased access and outreach for HIV testing (traditional and non-traditional settings) |
| Increased access to contraception |
| Culturally competent care provision |
| Condom distribution programs |
| Supervised injecting facilities |
| HIV prevention education in schools |
Behavioral approaches to HIV prevention
Early in the epidemic following identification of HIV as a sexually and parenterally transmitted disease, few prevention methods were available. Sexual transmission of HIV could be prevented largely through abstinence, fidelity and condom use; and transmission via IDU primarily through changing addiction behaviors. In response to these challenges, behavioral interventions were developed, studied, and tested in order to characterize methods that effectively reduce risk behavior.53,67–70 Among other achievements, the CDC’s Diffusion Effective Behavioral Interventions (DEBI) project allowed systematic development and review processes for evidence-based selection of behavioral approaches to HIV prevention.70 The primary goal of behavioral approaches has historically been to reduce HIV-related risk behavior, and promoting harm reduction rather than elimination has become a core tenet of behavioral interventions.68,71,72 Newer interventions have expanded beyond counseling to embrace testing, know-your-status campaigns, and outreach to sexual partners through peer-to-peer programs as well as mobile health application interventions.53,55,68,69,73–76
There are many strengths to behavioral prevention methods. Behavioral strategies that focus on individual-level behaviors in order to reduce risk of acquiring HIV are in many ways the mainstay of HIV prevention activities, and, as described below, integrate into combination prevention approaches and the prevention continuum. Less expensive and without side effects that often attend biomedical approaches, harm reduction can be highly effective to reduce risk of HIV acquisition or transmission.
Challenges with behavioral approaches to HIV prevention remain.53,54,69,72,77–79 Durability of behavioral interventions is hard to measure. Such methodological concerns mean that even in the presence of studies that characterize the impact of behavioral interventions, true estimates of effect may be elusive. Further, ongoing behavioral change is difficult for most populations. Among high risk populations, even one unprotected sexual exposure may result in a high probability of HIV transmission due to the relative prevalence of HIV in the sexual networks.80–82 Given that risk for HIV may for some subpopulations be a continuous risk, maintenance of solely behavioral harm reduction behaviors for a lifetime can be difficult. Effective behavioral counseling, one-on-one, group-level, and marketing campaigns have been shown to have relatively low population-uptake.53,69 So while behavioral strategies may present lower risks than biomedical ones on the surface, overall resources and resulting impact need to be incorporated into decision-making about adoption. Taking into account these challenges, biomedical interventions alone and in combination with behavioral interventions, represent a promising avenue for HIV prevention.
Biomedical approaches to HIV prevention
In view of the challenges outlined above and the urgent need to slow the spread of HIV, attention has turned to biomedical HIV prevention approaches. Studies on biomedical modalities to interrupt mother to child HIV transmission by providing antiretroviral therapy to pregnant and laboring women and their newborns had significant impact on the epidemic’s course.56,83–86 In high income countries, perinatal transmission has been nearly stopped; for example, the US went from a peak of 900 perinatally acquired cases in 1992 to a historical low of 53 cases in 2011.83,87,88 Cases that do occur generally do so because of lack of antenatal diagnosis or care rather than failure of the interventions.83 This remarkable success is mirrored in low- and middle-income countries as a result of collaborative global efforts including PEPFAR which have successfully supported scale of up antiretroviral treatment for pregnant women and their children. The concept of an AIDS Free Generation is now within reach.51,52,89
The concept that antiretroviral treatment can be used in preventive fashion has guided development of biomedical prevention approaches for both HIV-uninfected individuals and to HIV-infected persons to reduce risk of secondary transmission. Post-exposure prophylaxis (PEP) was first developed in response to occupational exposures to HIV, whereby antiretroviral treatment was provided to persons following HIV exposure via needlestick, surgical, or laboratory injury.59,63 Now also used following high risk sexual exposures (both consensual and non-consensual), non-occupational PEP (also known as nPEP) is a regular offering to those who may have been exposed to HIV.65 These post-exposure biomedical treatments leverage the concept that use of antiretroviral treatment prevents HIV acquisition.
Similarly, pre-exposure prophylaxis (PrEP) offers additional promise for HIV prevention. Grant et al demonstrated a 44% reduction of HIV acquisition attributable to PrEP with emtricitibine-tenofovir disproxil fumurate (TDF/FTC) among men who have sex with men (MSM) and transgender women10, with significantly elevated efficacy among persons with detectable blood levels. PrEP using TDF/FTC was approved by the FDA in 201290 and adopted by CDC with recommendations for prevention for populations at elevated risk of HIV in 2014.62 The efficacy of TDF/FTC when used as PrEP has also been demonstrated among heterosexuals in Botswana and among IDUs in Thailand.57,91,92 In the last two years, new studies have evaluated uptake of PrEP focusing in particular on BMSM who are, as discussed above, the most highly affected subpopulation in the US (www.hptn.org).
Perhaps the most critical addition to the prevention armamentarium was the recognition in the landmark HPTN 052 study published in 2011 that effective viral suppression among HIV-infected persons can significantly reduce the risk of transmission to their sexual partners by 96%.11 This study, along with observational data demonstrating population-based declines in HIV rates with increasing antiretroviral coverage,4,41,43,80,93 have fueled the incorporation of “treatment as prevention” (TasP) as a cornerstone approach of HIV prevention programs.
The future holds still further promise for biomedical interventions. Long acting injectable antiretroviral regimens (that could be used both for PrEP and TasP) are currently in clinical trials following considerable primate data that support their potential for efficacy.94 Microbicides in the form of gels (vaginal and rectal) and vaginal rings are in clinical trials currently. Future biomedical directions necessarily will include combination prevention, where behavioral, biomedical and structural interventions are integrated to provide HIV prevention approaches that suit a given person or population at a specific point in time.52,54
Research on the most effective prevention strategies and on their durability will be key towards enhancing the potential of biomedical approaches. Biomedical HIV prevention strategies are hardly challenge-free; ultimately, nearly all HIV prevention success depends on behavior, whether that behavior is getting an HIV test, using a condom, taking a daily pill, or (potentially in the future) a semi-annual injection.95 Research into determining the level of personal risk that necessitates PrEP for example is an ongoing need as is how to support adherence and how to address life course risk changes and treatment fatigue that inevitably occur. Questions surrounding cost and access to HIV testing and safety monitoring required for PrEP treatment, along with healthcare infrastructure to support such services, remain unanswered questions in the larger rollout of this lifesaving prevention mediation.
Structural and population-level approaches to HIV prevention
Several of the aforementioned barriers to provision and uptake of behavioral and biomedical prevention interventions may ultimately only be addressed through population-level and structural approaches. Reducing stigma, training and cultural competency awareness building for healthcare providers, improved access to prevention services, improved diagnosis and treatment of sexually transmitted infections, reduced cost for services and related counseling and monitoring are likely key components in changing the settings that offer HIV prevention services so that they are more likely to be used.38,39,77,78,96,97 In view of the racial, sexual, and gender disparities that exist with HIV,37,64 reduction of healthcare disparities must be prioritized.
Routine testing in emergency departments exemplifies the strength of the structural intervention with their broad reach to those who do not chose to disclose a specific risk behavior.75,98 Syringe exchange programs and supervised injection facilities decrease the spread of HIV (and Hepatitis C virus) among IDU.68,70,99 There is substantial evidence that TasP is effective and as a result TasP has been integrated into World Health Organization guidelines.80,100 Structural interventions are not without challenges as they require time and considerable resources to implement. Ultimately, modifications to existing structures may be the foundation on which the prevention continuum will work, in concert with behavioral and biomedical strategies.
Future research directions
HIV prevention research is the cornerstone on which progress in combatting the epidemic relies. Studies are critically needed to address how to best utilize combination prevention approaches for all populations, including those populations frequently excluded from research such as young BMSM.37,39,79,97 Engagement in care remains a substantial challenge; reaching persons at risk for HIV so that they may be tested and receive prevention service utilization is a further challenge. Our methods must evolve to effectively engage all populations at risk for HIV into prevention research as well as more effectively examining barriers to prevention services. Only with innovative methods that are culturally appropriate will we be able to effectively use the remarkable prevention armamentarium that has been developed.
Conclusions
Recent policy, epidemiologic and prevention advances have served to greatly inform and guide the response to the HIV epidemic in the US and beyond. Working together, public health personnel, clinical providers and impacted communities can capitalize on these developments, thereby contributing to continued national and global reductions of HIV incidence, morbidity and mortality.
Acknowledgements
This publication was supported in part by the District of Columbia Developmental Center for AIDS Research (DC D-CFAR), an NIH-funded program (P30AI087714).The authors would like to acknowledge Dr. Patrick Sullivan and Ms. Alexandra Ricca, from Emory University, who assisted with the AIDSVu maps.
Conflict of Interest
AD Castel has received research support from National Institutes of Health and District of Columbia Department of Health; speaker honorarium from DC Care Consortium; and travel reimbursement from American Academy of Pediatrics and National Institute of Health.
M Magnus has received research support from NIH, CMS, and CDC; and royalties from Jones & Bartlett Learning, Inc.
AE Greenberg has received research support from DC DOH, NIH, CDC, and EGPAF; and a speaker honorarium from CIENI.
Footnotes
Human and Animal Rights and Informed Consent
All studies by M Magnus and AE Greenberg involving animal and/or human subjects were performed after approval by the appropriate institutional review boards. When required, written informed consent was obtained from all participants.
References
Papers of particular interest, published recently, have been highlighted as:
* Of importance ** Of major importance
- 1. United States. National HIV/AIDS Strategy: Federal Implementation Plan. 2010. Washington, D.C.: White House Office of National AIDS Policy; 2010. Office of National AIDS Policy. This document outlines the implementaiton strategy for the first national HIV AIDS Strategy for the United States.
- 2.Centers for Disease Control and Prevention. High-Impact HIV Prevention: CDC’s Approach to Reducing HIV Infections in the United States. Atlanta, GA: 2011. [Google Scholar]
- 3. Cheever Laura. Outreach: Engaging People in HIV Care: Summary of a HRSA/HAB 2005 Consultation on Linking PLWH Into Care. 2006 This is the first documentation of the HIV care continuum and laid the foundation for current approaches to monitoring HIV care and treatment outcomes.
- 4.Centers for Disease Control and Prevention. Vital Signs: HIV Diagnosis, Care, and Treatment Among Persons Living with HIV – United States, 2011. MMWR Morb Mortal Wkly Rep. 2014 Nov 28;63(47):1113–1117. [PMC free article] [PubMed] [Google Scholar]
- 5.Executive Order--HIV Care Continuum Initiative [press release] Vol. 2013. Washington, DC: 2013. Jul 15, [Google Scholar]
- 6.Centers for Disease Control and Prevention. The Care and Prevention in the United States (CAPUS) Demonstration Project. [Accessed January 28, 2015];2012 http://www.cdc.gov/hiv/prevention/demonstration/capus/.
- 7.Centers for Disease Control and Prevention. Enhanced Comprehensive HIV Prevention Planning and Implementation for Metropolitan Statistical Areas Most Affected by HIV/AIDS. 2013. [Accessed August 24, 2014];2014 http://www.cdc.gov/hiv/prevention/demonstration/echpp/tools.html.
- 8.AIDSVu. [Accessed February 4, 2015];( www.aidsvu.org) Emory University, Rollins School of Public Health. 2015 [Google Scholar]
- 9.Grabowski MK, Redd AD. Molecular tools for studying HIV transmission in sexual networks. Current opinion in HIV and AIDS. 2014 Mar;9(2):126–133. doi: 10.1097/COH.0000000000000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. Dec 30;363(27):2587–2599. doi: 10.1056/NEJMoa1011205. This paper presents the results of a Phase III study to characterize use and efficacy of pre-expsoure prophylaxis for HIV using Truvada in the prevention of HIV among men who have sex with men and among transgender women.
- 11. Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011 Aug 11;365(6):493–505. doi: 10.1056/NEJMoa1105243. This paper presents the results of a Phase III study to characterize use and efficacy of antiretroviral treatment of an HIV-infected indivdiual in the prevention of HIV acquisition among sexual partners. These results from HPTN 052 present the foundation and evidence for treatment as prevention interventions on the population level.
- 12.UNAIDS. [Accessed January 30, 2015];World AIDS Day 2014 Report - Fact sheet. 2014 http://www.unaids.org/en/resources/campaigns/World-AIDS-Day-Report-2014/factsheet. [Google Scholar]
- 13.Joint United Nations Programme on HIV/AIDS (UNAIDS)/World Health Organization (WHO). Guideline for second generation HIV surveillance. 2000 [Google Scholar]
- 14.Centers for Disease Control and Prevention. [Atlanta, GA];Diagnoses of HIV Infection and AIDS in the United States and Dependent Areas, 2012. 2012 [Google Scholar]
- 15. Centers for Disease Control and Prevention. Revised surveillance case definition for HIV infection--United States, 2014. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. 2014 Apr 11;63(RR-03):1–10. This is the most recent surveillance case definition for HIV/AIDS in the United States, representing the last major case defintion revision.
- 16.Lansky A, Brooks JT, DiNenno E, Heffelfinger J, Hall HI, Mermin J. Epidemiology of HIV in the United States. Journal of acquired immune deficiency syndromes (1999) 2010 Dec;55(Suppl 2):S64–S68. doi: 10.1097/QAI.0b013e3181fbbe15. [DOI] [PubMed] [Google Scholar]
- 17.Barnighausen T, McWalter TA, Rosner Z, Newell ML, Welte A. HIV incidence estimation using the BED capture enzyme immunoassay: systematic review and sensitivity analysis. Epidemiology (Cambridge, Mass.) 2010 Sep;21(5):685–697. doi: 10.1097/EDE.0b013e3181e9e978. [DOI] [PubMed] [Google Scholar]
- 18.Laeyendecker O, Brookmeyer R, Cousins MM, et al. HIV incidence determination in the United States: a multiassay approach. The Journal of infectious diseases. 2013 Jan 15;207(2):232–239. doi: 10.1093/infdis/jis659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Estimated HIV Incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report. 2012 Dec;17(4) 2012. [Google Scholar]
- 20.Prejean J, Song R, Hernandez A, et al. Estimated HIV incidence in the United States, 2006–2009. PloS one. 2011;6(8):e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Census Bureau. USA Quick Facts from the US Census Bureau. [Accessed January 19, 2015];2013 http://quickfacts.census.gov/qfd/states/00000.html.
- 22.Braithwaite RS, Justice AC, Chang CC, et al. Estimating the proportion of patients infected with HIV who will die of comorbid diseases. The American journal of medicine. 2005 Aug;118(8):890–898. doi: 10.1016/j.amjmed.2004.12.034. [DOI] [PubMed] [Google Scholar]
- 23.US Department of Health and Human Services. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. Washington, DC: 2014. [Google Scholar]
- 24.Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. Lancet. 2013 Nov 2;382(9903):1525–1533. doi: 10.1016/S0140-6736(13)61809-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blair JM, McNaghten AD, Frazier EL, Skarbinski J, Huang P, Heffelfinger JD. Clinical and behavioral characteristics of adults receiving medical care for HIV infection --- Medical Monitoring Project, United States, 2007. Morbidity and mortality weekly report. Surveillance summaries. 2011 Sep 2;60(11):1–20. [PubMed] [Google Scholar]
- 26.Hunt PW. HIV and aging: emerging research issues. Current opinion in HIV and AIDS. 2014 Jul;9(4):302–308. doi: 10.1097/COH.0000000000000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.New York City HIV Surveillance Annual Report 2013. New York, NY: 2014. Dec, New York City Department of Health and Mental Hygiene. [Google Scholar]
- 28.San Franscisco Deartment of Public Health. San Francisco Department of Public Health, HIV Epidemiology Section. HIV/AIDS Epidemiology Annual Report 2013. 2014 Aug [Google Scholar]
- 29.DC Department of Health HIV/AIDS, Hepatitis, STD, TB Administration. Interim HIV/AIDS Surveillance Report: Preliminary 2013 Data. 2015 Jan [Google Scholar]
- 30.Miami-Dade County Department of Health. Number of Reported AIDS and HIV cases in 2011, 2012 and 2013. Miami, FL: 2014. Miami Dade County. [Google Scholar]
- 31.Rane D, Kelly J. Georgia Department of Public Health HIV Surveillance Update. Atlanta, GA: [Google Scholar]
- 32.Reif SS, Whetten K, Wilson ER, et al. HIV/AIDS in the Southern USA: a disproportionate epidemic. AIDS care. 2014;26(3):351–359. doi: 10.1080/09540121.2013.824535. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. HIV surveillance in men who have sex with men (MSM) Slide Set. 2012 [Google Scholar]
- 34.Centers for Disease Control and Prevention. Prevalence and awareness of HIV Infection among men who have sex with men—21 cities, United States, 2008. Morbidity Mortality Weekly Report. 2010;59(37):1201–1207. [PubMed] [Google Scholar]
- 35. Mayer KH, Wang L, Koblin B, et al. Concomitant socioeconomic, behavioral, and biological factors associated with the disproportionate HIV infection burden among Black men who have sex with men in 6 U.S. cities. PloS one. 2014;9(1):e87298. doi: 10.1371/journal.pone.0087298. This study describes findings from one of the largest cohorts of Black men who have sex with men to date.
- 36.Sullivan PS, Peterson J, Rosenberg ES, et al. Understanding racial HIV/STI disparities in black and white men who have sex with men: a multilevel approach. PloS one. 2014;9(3):e90514. doi: 10.1371/journal.pone.0090514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rosenberg ES, Millett GA, Sullivan PS, Del Rio C, Curran JW. Understanding the HIV disparities between black and white men who have sex with men in the USA using the HIV care continuum: a modeling study. The lancet. HIV. 2014 Dec;1(3):e112–e118. doi: 10.1016/S2352-3018(14)00011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jeffries WLt, Marks G, Lauby J, Murrill CS, Millett GA. Homophobia is associated with sexual behavior that increases risk of acquiring and transmitting HIV infection among black men who have sex with men. AIDS and behavior. 2013 May;17(4):1442–1453. doi: 10.1007/s10461-012-0189-y. [DOI] [PubMed] [Google Scholar]
- 39.Bogart LM, Wagner GJ, Galvan FH, Klein DJ. Longitudinal relationships between antiretroviral treatment adherence and discrimination due to HIV-serostatus, race, and sexual orientation among African-American men with HIV. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2010 Oct;40(2):184–190. doi: 10.1007/s12160-010-9200-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Greenberg AE. Fighting HIV/AIDS In Washington, DC. Health affairs (Millwood, Va.) 2009;28(6):1677–1687. doi: 10.1377/hlthaff.28.6.1677. [DOI] [PubMed] [Google Scholar]
- 41.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2011 Mar;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. Vital signs: HIV Prevention through care and treatment-United States. MMWR Morb Mortal Wkly Rep. 2011;60(47):1618–1623. [PubMed] [Google Scholar]
- 43. Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009 Jan 3;373(9657):48–57. doi: 10.1016/S0140-6736(08)61697-9. This article was the first to describe a mathematical model asserting that the scale up of HIV testing and immediate treatment with antiretroviral therapy could result in significant declines in HIV incidence (i.e., test and treat approach).
- 44.Sherer R. The future of HIV care in the USA. Sexually transmitted infections. 2012 Mar;88(2):106–111. doi: 10.1136/sextrans-2011-050160. [DOI] [PubMed] [Google Scholar]
- 45.Hall HI, Song R, Gerstle JE, 3rd, Lee LM Group HARSE. Assessing the completeness of reporting of human immunodeficiency virus diagnoses in 2002–2003: capture-recapture methods. American journal of epidemiology. 2006 Aug 15;164(4):391–397. doi: 10.1093/aje/kwj216. [DOI] [PubMed] [Google Scholar]
- 46.Myers JE, Braunstein SL, Shepard CW, et al. Assessing the impact of a community-wide HIV testing scale-up initiative in a major urban epidemic. Journal of acquired immune deficiency syndromes (1999) 2012 Sep 1;61(1):23–31. doi: 10.1097/QAI.0b013e3182632960. [DOI] [PubMed] [Google Scholar]
- 47.Castel AD, Magnus M, Peterson J, et al. Implementing a novel citywide rapid HIV testing campaign in Washington, D.C.: findings and lessons learned. Public health reports (Washington, D.C.: 1974) 2012 Jul-Aug;127(4):422–431. doi: 10.1177/003335491212700410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hallmark CJ, Skillicorn J, Giordano TP, et al. HIV testing implementation in two urban cities: practice, policy, and perceived barriers. PloS one. 2014;9(10):e110010. doi: 10.1371/journal.pone.0110010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Momplaisir F, Yehia BR, Harhay MO, Fetzer B, Brady KA, Long JA. HIV testing trends: Southeastern Pennsylvania, 2002–2010. AIDS patient care and STDs. 2014 Jun;28(6):303–310. doi: 10.1089/apc.2014.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Magnus M, Herwehe J, Gruber D, et al. Improved HIV-related outcomes associated with implementation of a novel public health information exchange. International journal of medical informatics. 2012 Oct;81(10):e30–e38. doi: 10.1016/j.ijmedinf.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 51.Millett GA, Crowley JS, Koh H, et al. A way forward: the National HIV/AIDS Strategy and reducing HIV incidence in the United States. Journal of acquired immune deficiency syndromes (1999) 2010 Dec;55(Suppl 2):S144–S147. doi: 10.1097/QAI.0b013e3181fbcb04. [DOI] [PubMed] [Google Scholar]
- 52. Dieffenbach CW, Fauci AS. Thirty years of HIV and AIDS: future challenges and opportunities. Annals of internal medicine. 2011 Jun 7;154(11):766–771. doi: 10.7326/0003-4819-154-11-201106070-00345. This landpark paper characterizes the past and the future of HIV treatment and preveniton, laying out a foundation for future research and innovation.
- 53.Kaufman MR, Cornish F, Zimmerman RS, Johnson BT. Health behavior change models for HIV prevention and AIDS care: practical recommendations for a multi-level approach. Journal of acquired immune deficiency syndromes (1999) 2014 Aug 15;66(Suppl 3):S250–S258. doi: 10.1097/QAI.0000000000000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kurth AE, Celum C, Baeten JM, Vermund SH, Wasserheit JN. Combination HIV prevention: significance, challenges, and opportunities. Current HIV/AIDS reports. 2011 Mar;8(1):62–72. doi: 10.1007/s11904-010-0063-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Muessig KE, Nekkanti M, Bauermeister J, Bull S, Hightow-Weidman LB. A Systematic Review of Recent Smartphone, Internet and Web 2.0 Interventions to Address the HIV Continuum of Care. Current HIV/AIDS reports. 2015 Jan 28; doi: 10.1007/s11904-014-0239-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chi BH, Adler MR, Bolu O, et al. Progress, challenges, and new opportunities for the prevention of mother-to-child transmission of HIV under the US President's Emergency Plan for AIDS Relief. Journal of acquired immune deficiency syndromes (1999) 2012 Aug 15;60(Suppl 3):S78–S87. doi: 10.1097/QAI.0b013e31825f3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Escudero DJ, Lurie MN, Kerr T, Howe CJ, Marshall BD. HIV pre-exposure prophylaxis for people who inject drugs: a review of current results and an agenda for future research. Journal of the International AIDS Society. 2014;17:18899. doi: 10.7448/IAS.17.1.18899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McMahon JM, Myers JE, Kurth AE, et al. Oral pre-exposure prophylaxis (PrEP) for prevention of HIV in serodiscordant heterosexual couples in the United States: opportunities and challenges. AIDS patient care and STDs. 2014 Sep;28(9):462–474. doi: 10.1089/apc.2013.0302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kuhar DT, Henderson DK, Struble KA, et al. Updated US Public Health Service guidelines for the management of occupational exposures to human immunodeficiency virus and recommendations for postexposure prophylaxis. Infection control and hospital epidemiology. 2013 Sep;34(9):875–892. doi: 10.1086/672271. [DOI] [PubMed] [Google Scholar]
- 60.Johnson BT, Michie S, Snyder LB. Effects of behavioral intervention content on HIV prevention outcomes: a meta-review of meta-analyses. Journal of acquired immune deficiency syndromes (1999) 2014 Aug 15;66(Suppl 3):S259–S270. doi: 10.1097/QAI.0000000000000235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Poteat T, Wirtz AL, Radix A, et al. HIV risk and preventive interventions in transgender women sex workers. Lancet. 2014 Jul 21; doi: 10.1016/S0140-6736(14)60833-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Preexposure prophylaxis for the prevention of HIV infection in the United States-2014, A Clinical Practice Guideline. Atlanta, GA: 2014. United States Public Health Service. [Google Scholar]
- 63.Beekmann SE, Henderson DK. Prevention of human immunodeficiency virus and AIDS: postexposure prophylaxis (including health care workers) Infectious disease clinics of North America. 2014 Dec;28(4):601–613. doi: 10.1016/j.idc.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008 Aug 30;372(9640):764–775. doi: 10.1016/S0140-6736(08)60887-9. [DOI] [PubMed] [Google Scholar]
- 65.Smith DK, Grohskopf LA, Black RJ, et al. Antiretroviral postexposure prophylaxis after sexual, injection-drug use, or other nonoccupational exposure to HIV in the United States: recommendations from the U.S. Department of Health and Human Services. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. 2005 Jan 21;54(RR-2):1–20. [PubMed] [Google Scholar]
- 66.Herbst JH, Beeker C, Mathew A, et al. The effectiveness of individual-, group-, and community-level HIV behavioral risk-reduction interventions for adult men who have sex with men: a systematic review. American journal of preventive medicine. 2007 Apr;32(4 Suppl):S38–S67. doi: 10.1016/j.amepre.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 67.Maulsby C, Millett G, Lindsey K, et al. A systematic review of HIV interventions for black men who have sex with men (MSM) BMC public health. 2013;13:625. doi: 10.1186/1471-2458-13-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Copenhaver MM, Johnson BT, Lee IC, Harman JJ, Carey MP, Team SR. Behavioral HIV risk reduction among people who inject drugs: meta-analytic evidence of efficacy. Journal of substance abuse treatment. 2006 Sep;31(2):163–171. doi: 10.1016/j.jsat.2006.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lyles CM, Kay LS, Crepaz N, et al. Best-evidence interventions: findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000–2004. American journal of public health. 2007 Jan;97(1):133–143. doi: 10.2105/AJPH.2005.076182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Centers for Disease Control and Prevention. CDC Compendium and Prevention Research Synthesis. [Accessed January 25, 2015]; http://www.cdc.gov/hiv/prevention/research/compendium/.
- 71.Marks G, Millett GA, Bingham T, Lauby J, Murrill CS, Stueve A. Prevalence and protective value of serosorting and strategic positioning among Black and Latino men who have sex with men. Sexually transmitted diseases. 2010 May;37(5):325–327. doi: 10.1097/OLQ.0b013e3181c95dac. [DOI] [PubMed] [Google Scholar]
- 72.Moreno R, Nababan HY, Ota E, et al. Structural and community-level interventions for increasing condom use to prevent the transmission of HIV and other sexually transmitted infections. The Cochrane database of systematic reviews. 2014;7:CD003363. doi: 10.1002/14651858.CD003363.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Johnson BT, Scott-Sheldon LA, Smoak ND, Lacroix JM, Anderson JR, Carey MP. Behavioral interventions for African Americans to reduce sexual risk of HIV: a meta-analysis of randomized controlled trials. Journal of acquired immune deficiency syndromes (1999) 2009 Aug 1;51(4):492–501. doi: 10.1097/QAI.0b013e3181a28121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schnall R, Travers J, Rojas M, Carballo-Dieguez A. eHealth interventions for HIV prevention in high-risk men who have sex with men: a systematic review. Journal of medical Internet research. 2014;16(5):e134. doi: 10.2196/jmir.3393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. 2006 Sep 22;55(RR-14):1–17. quiz CE11-14. These are recommendations for routine HIV screening in the US, a major shift in the domestic approach to HIV testing on the population level.
- 76.Darbes L, Crepaz N, Lyles C, Kennedy G, Rutherford G. The efficacy of behavioral interventions in reducing HIV risk behaviors and incident sexually transmitted diseases in heterosexual African Americans. AIDS (London, England) 2008 Jun 19;22(10):1177–1194. doi: 10.1097/QAD.0b013e3282ff624e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Levy ME, Wilton L, Phillips G, 2nd, et al. Understanding structural barriers to accessing HIV testing and prevention services among black men who have sex with men (BMSM) in the United States. AIDS and behavior. 2014 May;18(5):972–996. doi: 10.1007/s10461-014-0719-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mahajan AP, Sayles JN, Patel VA, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS (London, England) 2008 Aug;22(Suppl 2):S67–S79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ayala G, Bingham T, Kim J, Wheeler DP, Millett GA. Modeling the impact of social discrimination and financial hardship on the sexual risk of HIV among Latino and Black men who have sex with men. American journal of public health. 2012 May;102(Suppl 2):S242–S249. doi: 10.2105/AJPH.2011.300641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Das M, Chu PL, Santos GM, et al. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PloS one. 2010;5(6):e11068. doi: 10.1371/journal.pone.0011068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Terzian AS, Bodach SD, Wiewel EW, et al. Novel use of surveillance data to detect HIV-infected persons with sustained high viral load and durable virologic suppression in New York City. PloS one. 2012;7(1):e29679. doi: 10.1371/journal.pone.0029679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Castel AD, Befus M, Willis S, et al. Use of the community viral load as a population-based biomarker of HIV burden. AIDS (London, England) 2012 Jan 28;26(3):345–353. doi: 10.1097/QAD.0b013e32834de5fe. [DOI] [PubMed] [Google Scholar]
- 83.Nesheim S, Taylor A, Lampe MA, et al. A framework for elimination of perinatal transmission of HIV in the United States. Pediatrics. 2012 Oct;130(4):738–744. doi: 10.1542/peds.2012-0194. [DOI] [PubMed] [Google Scholar]
- 84.Connor EM, Sperling RS, Gelber R, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. Pediatric AIDS Clinical Trials Group Protocol 076 Study Group. N Engl J Med. 1994 Nov 3;331(18):1173–1180. doi: 10.1056/NEJM199411033311801. [DOI] [PubMed] [Google Scholar]
- 85.Siegfried N, van der Merwe L, Brocklehurst P, Sint TT. Antiretrovirals for reducing the risk of mother-to-child transmission of HIV infection. The Cochrane database of systematic reviews. 2011;7:CD003510. doi: 10.1002/14651858.CD003510.pub3. [DOI] [PubMed] [Google Scholar]
- 86.Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. Recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States [Google Scholar]
- 87.Nesheim S, Harris LF, Lampe M. Elimination of perinatal HIV infection in the USA and other high-income countries: achievements and challenges. Current opinion in HIV and AIDS. 2013 Sep;8(5):447–456. doi: 10.1097/COH.0b013e3283636ccb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Centers for Disease Control and Prevention. Pediatric HIV Surveillance Slides (through 2011) 2014 [Google Scholar]
- 89.Fauci AS, Folkers GK. Toward an AIDS-free generation. Jama. 2012 Jul 25;308(4):343–344. doi: 10.1001/jama.2012.8142. [DOI] [PubMed] [Google Scholar]
- 90.FDA approves first drug for reducing the risk of sexually acquired HIV infection [press release] 2012 Jul 16; [Google Scholar]
- 91.Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013 Jun;381(9883):2083–2090. doi: 10.1016/S0140-6736(13)61127-7. [DOI] [PubMed] [Google Scholar]
- 92.Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012 Aug;367(5):423–434. doi: 10.1056/NEJMoa1110711. [DOI] [PubMed] [Google Scholar]
- 93.Hoffmann CJ, Gallant JE. Rationale and evidence for human immunodeficiency virus treatment as prevention at the individual and population levels. Infectious disease clinics of North America. 2014 Dec;28(4):549–561. doi: 10.1016/j.idc.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 94. Spreen WR, Margolis DA, Pottage JC., Jr Long-acting injectable antiretrovirals for HIV treatment and prevention. Current opinion in HIV and AIDS. Nov 8;(6):565–571. doi: 10.1097/COH.0000000000000002. This paper highlights novel prevention interventions in injectable, long acting PrEP.
- 95.Marcus JL, Buisker T, Horvath T, et al. Helping our patients take HIV pre-exposure prophylaxis (PrEP): a systematic review of adherence interventions. HIV medicine. 2014 Aug;15(7):385–395. doi: 10.1111/hiv.12132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Latkin C, Weeks MR, Glasman L, Galletly C, Albarracin D. A dynamic social systems model for considering structural factors in HIV prevention and detection. AIDS and behavior. 2010 Dec;14(Suppl 2):222–238. doi: 10.1007/s10461-010-9804-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hightow-Weidman LB, Phillips G, 2nd, Jones KC, et al. Racial and sexual identity-related maltreatment among minority YMSM: prevalence, perceptions, and the association with emotional distress. AIDS patient care and STDs. 2011 Aug;25(Suppl 1):S39–S45. doi: 10.1089/apc.2011.9877. [DOI] [PubMed] [Google Scholar]
- 98.Brown J, Shesser R, Simon G, et al. Routine HIV screening in the emergency department using the new US Centers for Disease Control and Prevention Guidelines: results from a high-prevalence area. Journal of acquired immune deficiency syndromes (1999) 2007 Dec 1;46(4):395–401. doi: 10.1097/qai.0b013e3181582d82. [DOI] [PubMed] [Google Scholar]
- 99.Hagan H, Pouget ER, Des Jarlais DC. A systematic review and meta-analysis of interventions to prevent hepatitis C virus infection in people who inject drugs. The Journal of infectious diseases. 2011 Jul 1;204(1):74–83. doi: 10.1093/infdis/jir196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.WHO Guidelines Approved by the Guidelines Review Committee. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach. Geneva: 2013. [PubMed] [Google Scholar]