Summary:
Acral melanoma is a great pretender; anything but i nfrequently, it adopts clinical faces, simulating skin conditions that make the healthcare provider diagnose it as a benign disease of the palms, soles, and ungual regions. We present a case of a hyperkeratotic acral melanoma that has been misdiagnosed and that has led to an amputation of the thumb.
Acral melanoma (ALM) was described for the first time in 1976 by Reed.1 It is the fourth variant of cutaneous melanoma, differing from it in terms of different genetic etiology, namely the presence of a mutation in the Kit gene and not in the BRAF gene. It is a rare pathology in the white population, representing only 10% of all melanomas, but its incidence increases in Asian population to 50–58% and in black-skinned population to 60–70%.2,3 From the clinical point of view, its distinctive feature is to be a great pretender; anything but infrequently, it adopts clinical faces, simulating skin conditions that make the healthcare provider diagnose it as a benign disease of the palms, soles, and ungual regions at first glance.4 On the other hand, its histological diagnosis is very clear1,3; ALM is featured by a marked acanthosis, the presence of a broadened corneum stratum, an elongation of rete ridges, and a lentiginous growth of large tumoral cells along the dermoepidermic junction. The ALM cells also present dendritic processes, atypical and hyperchromatic large nuclei, and often the absence of pigmentation probably due to the great acceleration of the cellular growth that does not allow the correct synthesis of melanin. Unfortunately, the clinical features often cause misdiagnosis of the melanoma, and the most reported misdiagnoses have been ulcers, infections, hemorrhage, and benign skin tumors. Not surprisingly, the delay in the diagnosis, and subsequent months or even years of tumoral progression, leads to a poor prognosis of the disease, which stands as a real diagnostic challenge. From the literature, it is known that efforts have been put in to spread knowledge about acral melanoma and to make clinicians aware of the clues and tips that can help prevent misdiagnosis of melanoma and improvement of prognosis. We would like to contribute to the enrichment of the reports database by sharing the case of ALM simulating acral warts.
CLINICAL CASE
A 78-year-old white woman presented at our clinic with a skin lesion of the distal phalanx of the left thumb, which was of several months of evolution (Figs. 1–3). It had been previously treated with cryotherapy based on the suspicion of a wart, showing no response to treatment but only a local progression. Physical examination revealed a hyperkeratotic plaque of 20 mm with a nondefined, asymmetric border. The lesion extended proximally to the distal third of the nail bed, causing nail detachment.
Fig. 1.

Preoperative state of the acral melanoma.
Fig. 3.
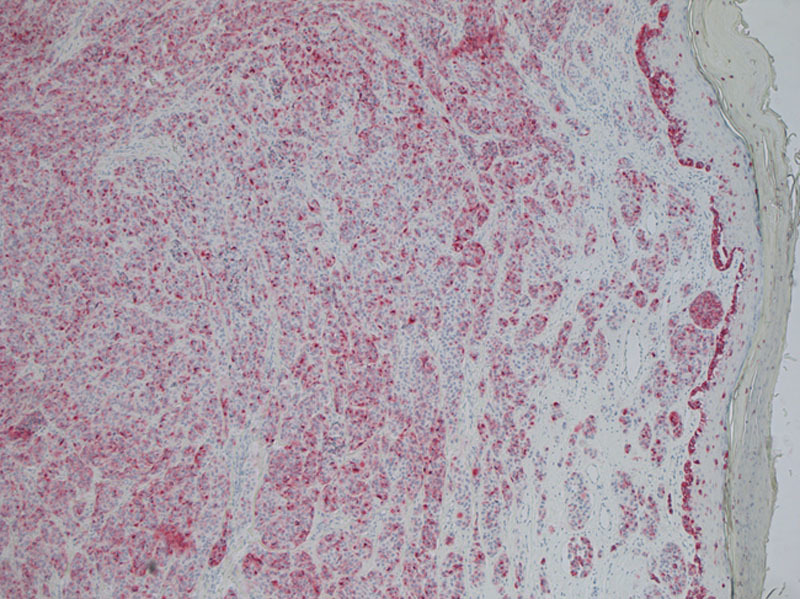
Acral melanoma positivity to monoclonal antibody hmb45.
Fig. 2.
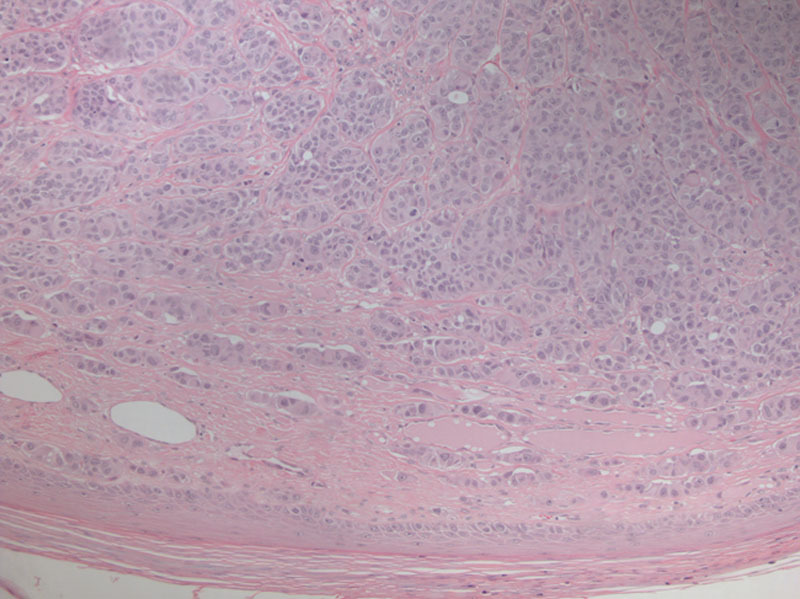
Histological analysis of acral melanoma using hematoxylin and eosin.
An incisional biopsy of the lesion was performed, and the diagnosis of ALM was established. According to Breslow depth (5.8 mm), radical excision was planned as an en bloc amputation of the distal phalanx with sentinel lymph node dissection, followed by radical axillary node dissection after 10 days. After 1 year, the oncological follow-up was negative.
DISCUSSION AND CONCLUSION
ALM may frequently adopt clinical characteristics simulating less serious skin conditions, such as benign lesions, leading, as we said earlier, to delayed and/or inadequate treatment. The knowledge of the atypical characteristics of presentation of acral lesion allows to reduce the incidence of misdiagnosis of melanoma and consequently to have a better prognosis. Recently, authors have discussed about the real benefit of the sentinel lymph node biopsy in the prognosis of the ALM, concluding that it could be really helpful only in the patients with thick melanoma (>1 mm) and that it is a very important prognostic factor if associated with ulceration in the primary tumor.5
Finally, considering ALM and its presentation as an amelanotic, hyperkeratotic lesion, which is just as rare as deceptive, it is absolutely mandatory both to document the cases as much as possible and to remember that whenever a hyperkeratotic lesion resistant to treatments for common warts is encountered, melanoma should always be ruled out.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Kuchelmeister C, Schaumburg-Lever G, Garbe C. Acral cutaneous melanoma in Caucasians: clinical features, histopathology and prognosis in 112 patients. Br J Dermatol. 2000;143:275–280. doi: 10.1046/j.1365-2133.2000.03651.x. [DOI] [PubMed] [Google Scholar]
- 2.Boriani F, O’Leary F, Tohill M, et al. Acral lentiginous melanoma—misdiagnosis, referral delay and 5 years specific survival according to site. Eur Rev Med Pharmacol Sci. 2014;18:1990–1996. [PubMed] [Google Scholar]
- 3.Phan A, Touzet S, Dalle S, et al. Acral lentiginous melanoma: histopathological prognostic features of 121 cases. Br J Dermatol. 2007;157:311–318. doi: 10.1111/j.1365-2133.2007.08031.x. [DOI] [PubMed] [Google Scholar]
- 4.Ise M, Yasuda F, Konohana I, et al. Acral melanoma with hyperkeratosis mimicking a pigmented wart. Dermatol Pract Concept. 2013;3:37–39. doi: 10.5826/dpc.0301a10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ito T, Wada M, Nagae K, et al. Acral lentiginous melanoma: who benefits from sentinel lymph node biopsy? J Am Acad Dermatol. 2015;72:71–77. doi: 10.1016/j.jaad.2014.10.008. [DOI] [PubMed] [Google Scholar]


