Abstract
Background and objectives
Frailty is associated with poor outcomes for patients on dialysis; however, previous studies have not taken into account the severity of frailty as a predictor of outcomes. The purpose of this study was to assess if there was an association between the degree of frailty and mortality among patients on incident dialysis.
Design, setting, participants, & measurements
A cohort study of incident chronic dialysis patients was conducted between January of 2009 and June of 2013 (last follow-up in December of 2013). On the basis of overall clinical impression, the Clinical Frailty Scale (CFS) score was determined for patients at the start of dialysis by their primary nephrologist. This simple scale allocates a single point to different states of frailty (1, very fit; 2, well; 3, managing well; 4, vulnerable; 5, mildly frail; 6, moderately frail; 7, severely frail or terminally ill) with an emphasis on function of the assessed individual. The primary outcome was time to death. Patients were censored at the time of transplantation.
Results
The cohort consisted of 390 patients with completed CFS scores (mean age of 63±15 years old). Most were Caucasian (89%) and men (67%), and 30% of patients had ESRD caused by diabetic nephropathy. The median Charlson Comorbidity Index score was 4 (interquartile range =3–6), and the median CFS score was 4 (interquartile range =2–5). There were 96 deaths over 750 patient-years at risk. In an adjusted Cox survival analysis, the hazard ratio associated with each 1-point increase in the CFS was 1.22 (95% confidence interval, 1.04 to 1.43; P=0.02).
Conclusions
A higher severity of frailty (as defined by the CFS) at dialysis initiation is associated with higher mortality.
Keywords: geriatric nephrology, ESRD, epidemiology and outcomes, dialysis, mortality
Introduction
Frailty (a loss of cognitive, functional, and health reserves leading to increased vulnerability) (1) is common in ESRD (2–5). Studies examining the effect of frailty on outcome in the general population typically include only elderly patients (6,7). However, the prevalence of frailty is high for both older and younger patients initiating dialysis (4). Furthermore, frailty is associated with a higher risk of death irrespective of age in the ESRD population (2).
Studies of frailty in dialysis populations have used different criteria that have been extrapolated from the five-item Fried frailty phenotype (2–4). These criteria are on the basis of the presence of unintentional weight loss, exhaustion, reduced grip strength, slow walking speed, or low physical activity (8). Alternative criteria have been validated and used in large ESRD databases (2,3). Although these definitions are reliable and reproducible, applying these criteria can be cumbersome in routine clinical practice. Moreover, the incremental severity of frailty is not captured using these measurement tools. It has been shown in the elderly general population that even small changes in the degree of frailty are associated with poor outcomes (1).
Therefore, the purpose of this study was to evaluate the association between the degree of frailty and mortality using a simple frailty scale in a cohort of patients with incident dialysis. We hypothesized that incremental changes in the level of frailty would be associated with death in this population.
Materials and Methods
Study Population
We conducted a cohort study of consecutive adult (age >18 years old) patients on incident dialysis who started chronic dialysis from January 1, 2009 to June 30, 2013, at a large tertiary care center. Patients on chronic dialysis were identified from a local electronic database as those for whom the treating physician felt that they had ESRD requiring dialysis and would not recover kidney function on the basis of clinical impression. We included patients who initiated dialysis after failed kidney transplant. We excluded patients who only transiently received dialysis in our center (<1 week) with the intention and eventual transfer to another regional/out-of-province dialysis unit. Patients were followed for outcomes until December 31, 2013.
Exposure Assessment
The Clinical Frailty Scale (CFS) (1) was used to measure the level of frailty for all patients initiating dialysis during the noted timeframe. This scale is on the basis of clinical judgment using available clinical information. It has been shown to have high inter-rater reliability (intraclass correlation coefficient of 0.97) and correlates well with objective measures of frailty (Pearson correlation coefficient with mathematics-based frailty index of 0.80) (1). The original version of the scale (which was used in this study) is graded from 1 to 7 (1, very fit; 2, well without active disease; 3, well with treated comorbid disease; 4, apparently vulnerable; 5, mildly frail; 6, moderately frail; 7, severely frail), with emphasis on function of the assessed individual (summarized version noted in Table 1.) All 10 nephrologists and three nephrology nurse practitioners (at this institution) were introduced to the CFS in 2008 before study initiation. Similar to the original study design, ascertainment of frailty level was on the basis of the clinician’s judgment and informed by the provided information for each level of frailty. A copy of the scale, including the descriptors of each level, was provided to the primary nephrology practitioner for each patient, who prospectively evaluated CFS scores in the week preceding or day of dialysis (when dialysis initiation was scheduled in the outpatient clinic). Among those who initiated chronic dialysis as an inpatient, CFS scores were measured during the first week of admission. The individual with the most clinical knowledge of the patient determined the CFS score; among scheduled dialysis starts, this was the patient’s primary nephrologist or nephrology nurse practitioner. Among inpatient starts without prior follow-up, this was the attending/consulting nephrologist. Characteristics and outcomes of patients who had missing frailty scale scores were captured for comparison.
Table 1.
The Canadian Society of Health and Aging CFS
| CFS Score | Interpretation |
|---|---|
| 1 | Very fit: robust, active, energetic, well motivated, and fit; fittest in their age group |
| 2 | Well: without active disease but not as fit as those in category 1 |
| 3 | Well: with treated comorbid disease |
| 4 | Apparently vulnerable: not dependent but has symptoms from comorbid disease (such as being slowed up) |
| 5 | Mildly frail: limited dependence on others for instrumental activities of daily living |
| 6 | Moderately frail: help is needed for instrumental activities of daily living and activities of daily living |
| 7 | Severely frail: completely dependent on others for instrumental activities of daily living and activities of daily living or terminally ill |
CFS, Clinical Frailty Scale.
Outcome Assessment
The primary outcome of this study was time to all-cause mortality from the date of dialysis initiation. Date of death and causes of death were ascertained through documentation in electronic records and patient charts. Patient survival was censored at transplantation or date of last follow-up. In prespecified sensitivity analyses, we also examined the association between frailty and mortality using different follow-up periods and subgroups. Specifically, we examined time to death without censoring at transplantation, time to death excluding patients with a failed renal allograft as cause of ESRD, and early mortality (death within the first 1 year of dialysis).
Baseline Characteristics
Characteristics were collected at the start of dialysis by the patient’s primary nephrologist on the basis of clinical data in electronic records. These characteristics included patient demographics, height and weight, comorbidities, cause of ESRD, type of dialysis (peritoneal, hemodialysis with central venous catheter, or hemodialysis with arteriovenous fistula or graft), and laboratory data. eGFR using the four-variable Modified Diet in Renal Disease (MDRD) equation was calculated in all patients at the start of dialysis on the basis of serum creatinine values on the day of dialysis initiation. If laboratory results were not available on the day of dialysis, the most recent values within the preceding month were used. Physicians at our center routinely document additional comorbid conditions that comprise the Charlson Comorbidity Index (CCI). This index assigns points to different medical conditions to determine an overall score of comorbidity (9). Higher CCI scores have been associated with an increased mortality risk in patients on dialysis (10,11). All comorbid conditions were documented by the patient’s primary nephrologist on the basis of clinical knowledge and notation in electronic records. Missing values were addressed by re-examination of electronic records by two nephrologists (B.A.K. and K.K.T.) and a nephrology fellow (T.A.A.).
Statistical Analyses
Descriptive statistics were reported as counts and percentages for categorical variables, means±SDs for normally distributed continuous variables, and medians and interquartile ranges for non–normally distributed continuous variables. Frailty was treated as a continuous variable with a fixed interval between each scale score. We compared the change in the likelihood ratio test treating frailty as ordinal or continuous to ensure that we could analyze the CFS in this manner. However, we also examined for a trend of the survivor function across each CFS score. Adjusted hazard ratios (HRs) and 95% confidence intervals (95% CIs) for each 1-point increase in the CFS were evaluated in sequential multivariable Cox proportional hazards models incorporating demographics, comorbid conditions, laboratory data, and dialysis factors. Variables with missing data were added to the final model to avoid excluding patients at earlier levels. Variables selected for inclusion in the models were on the basis of clinical judgment and known literature predictors of mortality in patients on dialysis. These variables included age at the start of dialysis, sex (12), race (13–15), CCI (10,11), diabetic ESRD (12,16), body mass index (17), MDRD eGFR at start of dialysis (18), serum albumin (19), location of dialysis start, and dialysis type (20,21). Proportionality was assessed with Schoenfeld's global test. The possibility of effect modification by older age (≥65 years old), comorbidity (CCI≥5), and dialysis type was explored using interaction terms for each of these variables and the CFS in the final multivariable model. In a final sensitivity analysis, we reported adjusted HRs (using those variables noted above) and 95% CIs for ordinal categories of the CFS score (scores of 4, 5, and 6/7 relative to scores of 1–3) and examined for a trend of the survivor functions across each category. Statistical analyses were performed using Stata IC, version 12 (StataCorp, College Station, TX). A two-sided P value of <0.05 was the threshold for statistical significance. Approval for this study was received from the research ethics board at Capital Health.
Results
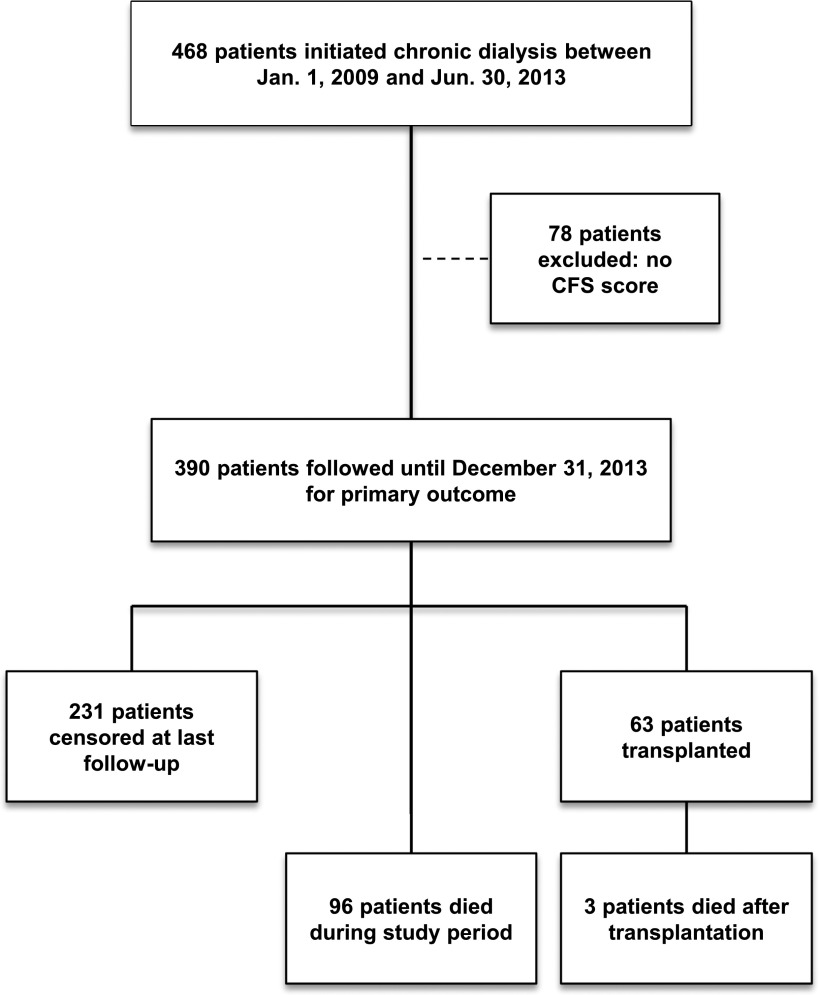
During the study period, 468 patients started chronic dialysis, of whom 390 (83%) had an assigned CFS score (Figure 1). Most of 78 patients who did not have a CFS score assigned were in the first era of the cohort (2009; n=36; 46%) (Table 2). Baseline characteristics stratified by presence and absence of an assigned CFS score are displayed in Table 2. Comparing those with scores with those without scores, there were differences in sex (67% versus 55% men), proportion with CCI scores ≥5 (44% versus 31%), and type of dialysis therapy (77% versus 65% hemodialysis).
Figure 1.
Cohort selection. CFS, Clinical Frailty Scale.
Table 2.
Baseline characteristics of patients with and without assigned CFS scores
| Variable | CFS Score Available (n=390) | CFS Score Not Available (n=78) | P Value |
|---|---|---|---|
| Age (yr), mean±SD | 63±15 | 60±14 | 0.17 |
| Age >65 yr, n (%) | 196 (50) | 30 (38) | 0.06 |
| Men, n (%) | 263 (67) | 43 (55) | 0.05a |
| Caucasian, n (%) | 346 (89) | 71 (91) | 0.69 |
| ESRD cause, n (%) | 0.24 | ||
| Diabetic nephropathy | 116 (30) | 20 (26) | |
| GN | 47 (12) | 8 (10) | |
| Polycystic kidney disease | 26 (7) | 9 (12) | |
| Ischemic renal disease | 77 (20) | 12 (15) | |
| Other | 81 (21) | 14 (18) | |
| Unknown | 5 (13) | 3 (18) | |
| Comorbid conditions, n (%) | |||
| Diabetes | 188 (48) | 31 (40) | 0.21 |
| Previous myocardial infarction | 126 (32) | 18 (23) | 0.14 |
| History of stroke | 50 (13) | 8 (10) | 0.71 |
| Peripheral vascular disease | 71 (18) | 11 (14) | 0.51 |
| Congestive heart failure | 87 (22) | 12 (15) | 0.22 |
| Previous or active malignancy | 30 (8) | 7 (9) | 0.65 |
| Dementia | 8 (2) | 2 (3) | 0.68 |
| Charlson Comorbidity Index, median (interquartile range) | 4 (3–6) | 4 (2–5) | 0.01a |
| Charlson Comorbidity Index score ≥5, n (%) | 171 (44) | 24 (31) | 0.03a |
| CFS score, mean ± SD | 4±2 | — | |
| Type of dialysis, n (%) | 0.03a | ||
| Hemodialysis | 301 (77) | 51 (65) | |
| Peritoneal dialysis | 89 (23) | 27 (35) | |
| Year of start, n (%) | <0.001a | ||
| 2009 | 66 (17) | 36 (46) | |
| 2010 | 99 (25) | 14 (18) | |
| 2011 | 96 (25) | 13 (17) | |
| 2012 | 87 (22) | 6 (7) | |
| 2013 | 42 (11) | 9 (12) | |
| Body mass index, n | 372 | 60 | |
| Body mass index, median (interquartile range) | 29 (25–34) | 28 (23–32) | 0.15 |
| eGFR (MDRD; ml/min per 1.73 m2) at start, median (interquartile range) | 8 (6–10) | 8 (6–11) | 0.41 |
| Albumin (g/dl), median (interquartile range) | 3.2 (2.8–3.6) | 3.3 (2.8–3.6) | 0.85 |
CFS, Clinical Frailty Scale; MDRD, Modification of Diet in Renal Disease formula (39).
Statistically significant.
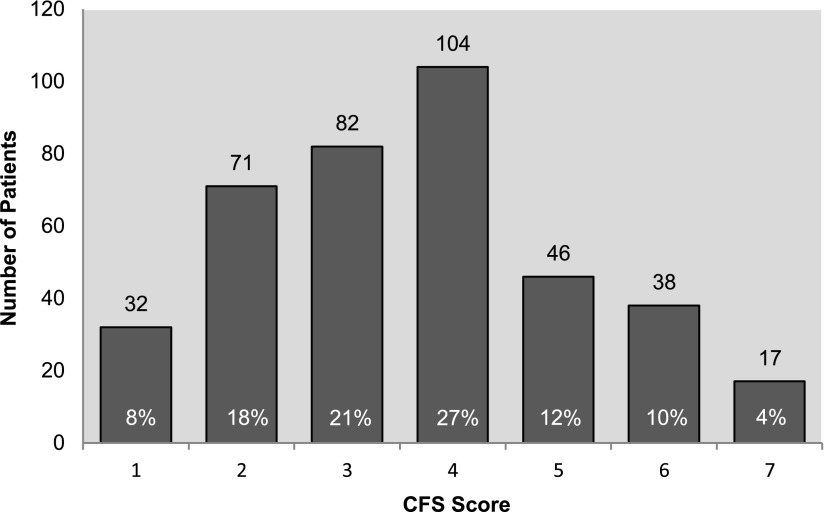
Frailty Scale Scores
The CFS scores were normally distributed (Shapiro–Wilk test, P=0.09). The distribution of patients on the basis of individual CFS scores is displayed in Figure 2. The mean CFS score was 4±2; 26% of patients were mildly to severely frail (scores of 5–7) on the basis of their CFS score, and 53% were apparently vulnerable to severely frail (scores of 4–7). Characteristics of patients at each CFS score are noted in Table 3. In general, those with higher scores had a higher proportion of individual comorbid conditions, had higher overall comorbidity (as defined by the CCI), had lower serum albumin concentration, and were older compared with those with lower scores. More patients with CFS scores of 7 received hemodialysis (versus peritoneal dialysis) and initiated dialysis as an inpatient compared with those with lower scores.
Figure 2.
Distribution of CFS scores. CFS, Clinical Frailty Scale.
Table 3.
Characteristics of patients stratified by CFS score
| Variable | CFS Score | ||||||
|---|---|---|---|---|---|---|---|
| 1 (n=31) | 2 (n=72) | 3 (n=82) | 4 (n=104) | 5 (n=46) | 6 (n=38) | 7 (n=17) | |
| Age (yr), mean ± SD | 46±17 | 57±5 | 60±13 | 67±13 | 68±13 | 72±13 | 68±11 |
| Age >65 yr, n (%) | 5 (16) | 23 (32) | 31 (38) | 65 (63) | 29 (63) | 30 (79) | 13 (76) |
| Men, n (%) | 21 (68) | 52 (72) | 65 (79) | 68 (65) | 25 (54) | 20 (53) | 12 (71) |
| Caucasian, n (%) | 29 (91) | 60 (85) | 72 (88) | 93 (89) | 43 (93) | 32 (84) | 17 (100) |
| ESRD cause, n (%) | |||||||
| Diabetic nephropathy | 0 (0) | 15 (21) | 27 (33) | 40 (38) | 18 (39) | 9 (24) | 7 (41) |
| GN | 7 (23) | 7 (10) | 11 (13) | 8 (8) | 8 (17) | 3 (8) | 3 (18) |
| Polycystic kidney disease | 6 (19) | 10 (14) | 4 (5) | 6 (6) | 0 (0) | 0 (0) | 0 (0) |
| Ischemic renal disease | 5 (16) | 11 (15) | 11 (13) | 23 (22) | 11 (24) | 15 (39) | 1 (6) |
| Other | 9 (29) | 20 (28) | 19 (23) | 18 (17) | 6 (13) | 6 (16) | 3 (18) |
| Unknown | 4 (13) | 9 (13) | 10 (12) | 9 (9) | 3 (7) | 5 (13) | 3 (18) |
| Comorbid conditions, n (%) | |||||||
| Diabetes | 5 (16) | 25 (35) | 37 (45) | 63 (61) | 26 (57) | 23 (61) | 9 (53) |
| Previous myocardial infarction | 1 (3) | 11 (15) | 23 (28) | 48 (46) | 19 (41) | 19 (50) | 5 (29) |
| History of stroke | 1 (3) | 5 (7) | 9 (11) | 15 (14) | 9 (20) | 7 (18) | 4 (24) |
| Peripheral vascular disease | 0 (0) | 6 (8) | 12 (15) | 27 (26) | 10 (22) | 11 (29) | 5 (29) |
| Congestive heart failure | 1 (3) | 6 (8) | 17 (21) | 26 (25) | 17 (37) | 14 (37) | 6 (35) |
| Previous or active malignancy | 3 (10) | 5 (7) | 5 (6) | 8 (8) | 2 (4) | 5 (13) | 2 (12) |
| Dementia | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 1 (2) | 4 (11) | 2 (12) |
| Charlson Comorbidity Index, median (interquartile range) | 2 (2–4) | 3 (2–4) | 4 (2–5) | 5 (4–6) | 5 (4–6) | 6 (4–7) | 5 (3–7) |
| Charlson Comorbidity Index score ≥5, n (%) | 3 (10) | 14 (19) | 30 (37) | 63 (61) | 27 (59) | 24 (63) | 10 (59) |
| Type of dialysis, n (%) | |||||||
| Hemodialysis | 24 (77) | 40 (58) | 65 (79) | 84 (81) | 36 (78) | 34 (89) | 16 (94) |
| Peritoneal dialysis | 7 (23) | 30 (42) | 17 (21) | 20 (19) | 10 (22) | 4 (11) | 1 (6) |
| Location of dialysis start, n (%) | |||||||
| Inpatient | 4 (13) | 14 (19) | 28 (34) | 32 (31) | 22 (48) | 27 (71) | 13 (76) |
| Outpatient | 27 (87) | 58 (81) | 54 (66) | 72 (69) | 24 (52) | 11 (29) | 4 (24) |
| Body mass index, median (interquartile range) | 28 (24–30) | 29 (25–33) | 28 (25–34) | 30 (27–36) | 29 (24–32) | 27 (23–31) | 26 (25–33) |
| eGFR (MDRD; ml/min per 1.73 m2) at start, median (interquartile range) | 7 (5–8) | 8 (6–11) | 8 (5–10) | 8 (7–10) | 9 (6–11) | 7 (6–10) | 8 (5–8) |
| Albumin (g/dl), median (interquartile range) | 3.5 (3.2–3.8) | 3.5 (3.2–3.9) | 3.3 (2.9–3.6) | 3.2 (2.9–3.6) | 3.0 (2.7–3.4) | 2.9 (2.4–3.5) | 2.5 (2.3–3.0) |
CFS, Clinical Frailty Scale; MDRD, Modification of Diet in Renal Disease formula.
Primary Outcome
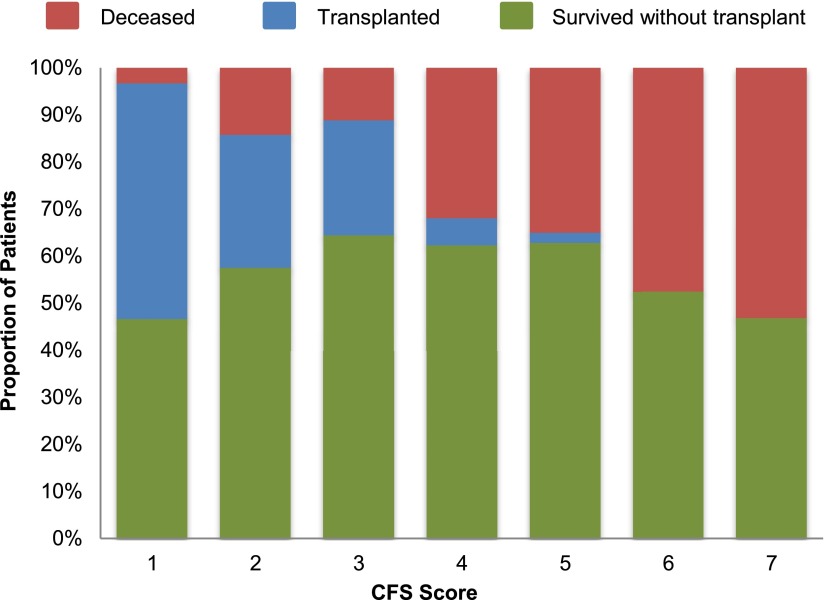
There were 96 deaths over 750 patient-years at risk (median follow-up time of 1.7 years; interquartile range =0.9–2.8 years). The proportions of patients who were deceased, alive (without transplant), and transplanted are displayed in Figure 3. Causes of death are noted in Supplemental Table 1. The majority of death was caused by withdrawal from dialysis and cardiac causes (arrythmia, myocardial infarction, congestive heart failure, or valvular heart disease) or sudden death. The proportions of patients with each cause of death were similar, regardless of CFS score (Supplemental Table 1). In an adjusted Cox survival analysis, each 1-point increase in the CFS score was associated with a relative mortality HR of 1.22 (95% CI, 1.04 to 1.43; P=0.02; model 3) (Table 4). A trend of the survivor function for each 1-point categorical increase in the CFS was also observed (P<0.001). P values for the interaction terms of the CFS with each of age ≥65 years old, CCI≥5, and dialysis modality were not significant. This suggests that advanced age, comorbidity, and dialysis modality did not modify the association between frailty and mortality in this study.
Figure 3.
Proportion of the cohort reaching end points of mortality, transplantation, or survival without transplantation stratified by CFS score. CFS, Clinical Frailty Scale.
Table 4.
Unadjusted and adjusted relative hazard for each 1-point increase in the CFS score including sensitivity analysis
| Model | N/Events | Hazard Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|---|
| Primary analyses | ||||
| Unadjusted | 390/96 | 1.42 | 1.25 to 1.61 | <0.001 |
| Model 1a | 390/96 | 1.32 | 1.15 to 1.52 | <0.001 |
| Model 2b | 390/96 | 1.30 | 1.12 to 1.51 | <0.001 |
| Model 3c | 390/96 | 1.22 | 1.04 to 1.43 | 0.02 |
| Model 4d | 372/90 | 1.21 | 1.02 to 1.43 | 0.03 |
| Sensitivity analyses | ||||
| Model 5e | 390/99 | 1.21 | 1.03 to 1.42 | 0.02 |
| Model 6f | 378/92 | 1.23 | 1.04 to 1.45 | 0.02 |
| Model 7g | 390/44 | 1.25 | 0.99 to 1.58 | 0.06 |
CFS, Clinical Frailty Scale.
Adjusted for age, race, and sex.
Adjusted for age, race, sex, Charlson Comorbidity Index ≥5, and diabetic ESRD.
Adjusted for age, race, sex, Charlson Comorbidity Index ≥5, diabetic ESRD, GFR (Modification of Diet in Renal Disease formula), albumin, dialysis modality, and location of dialysis start.
Adjusted for age, race, sex, Charlson Comorbidity Index ≥5, diabetic ESRD, GFR (Modification of Diet in Renal Disease formula), albumin, dialysis modality, location of dialysis start, and body mass index.
Model 3 including survival time after transplantation.
Model 3 excluding failed kidney allografts.
Model 3 restricted to mortality within the first 1 year.
Sensitivity Analyses
The point estimate and 95% CI for the association between each 1-point increase in the CFS and mortality were similar in sensitivity analyses (Table 4). Including survival time and outcomes of patients after transplantation did not significantly change the results (adjusted relative HR, 1.21; 95% CI, 1.03 to 1.42; P=0.02). Treating the CFS as a categorical variable (scores of 1–3, 4, 5, and 6/7), a trend of the survivor functions was noted (P<0.001). Compared with patients with a CFS score of 1–3, those with scores of 4, 5, and 6/7 had adjusted mortality HRs of 2.07 (95% CI, 1.14 to 3.74), 2.12 (95% CI, 1.05 to 4.28), and 2.38 (95% CI, 1.21 to 4.69), respectively.
Transplantation
Sixty-three (16%) patients received a renal allograft in those patients with an assigned CFS score. The proportion of patients who were transplanted declined with increasing CFS scores. None of the patients who were moderately or severely frail (CFS scores of 6 and 7, respectively) received a renal allograft during the study period.
Discussion
In this study, we identified an association between the degree of frailty (as defined by the CFS) and mortality. This association persisted after adjustment for age, CCI, and dialysis modality and persisted in sensitivity analyses. In contrast, a higher proportion of patients received kidney transplantation among those with lower CFS scores.
Although it is not surprising that frailty measured by the CFS was associated with mortality in our study, the increased risk of death with each 1-point increase in the CFS score underscores the potential prognostic significance of frailty in this population. Even in a cohort that is at a higher risk of death by virtue of having ESRD (22,23), the incremental nature of the CFS and association with mortality are preserved. Therefore, the CFS has the potential to add additional prognostic information above other known mortality predictors in dialysis (19,24).
Our findings are comparable with those by Rockwood et al. (1), who observed a similar increase in the risk of death with each 1-point increase in CFS in a cohort of community-dwelling elderly patients (>65 years old) and found that 59% of patients had CFS scores of ≥4 (versus 53% in our study). However, our population was considerably younger (average age of 63 years old). Patients with ESRD may accumulate other health issues earlier in life that contribute to frailty or ESRD itself, which can be associated with decreased physiologic reserve, characteristic of frailty (25,26). Not unexpectedly, age at the start of dialysis did not modify the association between frailty and outcome; the mortality HR was comparable whether young or old. This finding is similar to previous studies of frailty in dialysis (2–4) and suggests that there may be factors that lead to more rapid deficit accumulation and loss of reserve among patients on dialysis, regardless of age. However, these putative factors may occur well before patients initiate dialysis. Frailty scores in this cohort were normally distributed, whereas frailty in a younger population (as shown by assessment of a frailty index in an analysis of 66,589 community-dwelling individuals) tends to conform to a γ-distribution (27). This emphasizes that, even at baseline, our cohort behaves like a much older cohort of patients in the general population, with a greater proportion of scores above category 4. Therefore, initial deficit accumulation leading to frailty and subsequent mortality likely precedes need for dialysis. An assessment of changes in the CFS score and subsequent outcomes among those with CKD is planned for future study.
The association between frailty and mortality was consistent with other studies using alternative assessment tools (2–4); however, the prevalence of frailty differed. On the basis of the CFS, 26% of patients had varying degrees of frailty, and another 27% of patients were vulnerable. In contrast, prevalence of frailty in dialysis has been reported to be as high as 73% (2) and as low as 24% (28) depending on the criteria used to define it. We hypothesize that dividing frailty in two or three categories may lead to an underestimation of the mortality risk in studies with a high baseline prevalence, especially if many of those patients are not severely frail. Alternatively, the use of clinical judgment regarding factors that determined frailty score (such as cognitive status) may have led to an underestimation of frailty by clinicians in this study. Future studies will integrate other sources of information into the frailty score, including collateral report of function and objective cognitive screening (29). It remains unclear which scale is best used to measure frailty in community dwellers and dialysis cohorts (30). The CFS is a subjective measure of a patient’s overall health status as determined by the clinician’s judgment, taking into account perceived functional impairments (which are determined, in part, by mobility and cognitive function) and comorbid conditions to assign patients a level of frailty (1). Alternative frailty assessment tools use patient self-report and clinician impression (3). Finally, operational definitions developed by Fried et al. (8) emphasize the physical condition of the individual as a phenotypic manifestation of frailty (31,32). Therefore, there may be a tradeoff between the more objective definition provided by the Fried phenotype and one that is subjective but draws on clinician knowledge of other components of frailty.
Appreciating that frailty is associated with mortality, the use of categorizing the degree of frailty becomes more apparent. Longitudinal changes in frailty severity subsequent to dialysis initiation can be identified. Determining the severity of frailty can enable targeted clinical programs and support systems that address decision-making in the context of frailty (33) to better inform those who experience decisional conflict (34) or ambivalence toward initiating dialysis.
This study has a number of strengths. It is the first study to evaluate a frailty scale in patients with ESRD. The prospective acquisition of CFS scores limited the possibility of misclassification of patients (i.e., ascertainment of CFS after outcome) and improved the accuracy of data collection. The cohort was of sufficient size to allow for multivariable adjustment. There were only a few missing values in confounding variables used in the study. We had a reasonable representation of patients with completed CFS scores.
Despite these strengths, there are limitations. Being an observational study, there may have been unknown or unmeasured confounders that affected the association between frailty and mortality. Nevertheless, we were able to adjust for several important variables that have been shown to be associated with mortality in other studies of patients on dialysis. Although most factors were similar comparing those with and without CFS scores, there were differences in sex, modality, and overall comorbidity. There is a small possibility that inclusion of these patients if their CFS scores were available would have modified the results of our study. We acknowledge that, although the CFS has been validated in other cohorts (1,35,36), this is the first application in patients on dialysis. Identifying a similar mortality association in another dialysis cohort would be important along with identifying how well it agrees with other frailty assessment tools used in dialysis. In addition, examining other outcomes (including hospitalization, use of homecare resources, and need for institutionalization) would be important to determine if frailty defined by the CFS affects morbidity. Another limitation is the fact that the CFS is subjective and that different clinicians may grade severity differently or misclassify patients on the basis of limited availability. However, although this scale is subjective, it is a more realistic reflection of routine clinical practice, which often requires overall clinical impression. It is likely that many patients who were severely frail may not have been considered for dialysis, and this group of patients would not have been included in this analysis. However, it is unlikely that inclusion of this group of patients would have changed the results of our study. Furthermore, although severely frail patients are not always initiated on dialysis, it is informative to see that 14% of patients in this study had CFS scores of 6/7, suggesting that frailty was not a contraindication to dialysis initiation at our center. Finally, we appreciate that dementia was likely under-recognized in our cohort and that a more accurate identification of dementia may have increased the proportion of patients classified as frail. This is not surprising, because other studies have shown that dementia and cognitive impairment are under-recognized in dialysis (37,38). Furthermore, we suspect that a more accurate capture of those who had dementia would have led to an even stronger association between frailty and mortality.
In summary, we identified that the higher levels of frailty as defined by the CFS are associated with an increased mortality risk in patients on incident dialysis. Future studies are needed to evaluate the usefulness of the CFS in other dialysis populations.
Disclosures
None.
Supplementary Material
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.07760814/-/DCSupplemental.
References
- 1.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A: A global clinical measure of fitness and frailty in elderly people. CMAJ 173: 489–495, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bao Y, Dalrymple L, Chertow GM, Kaysen GA, Johansen KL: Frailty, dialysis initiation, and mortality in end-stage renal disease. Arch Intern Med 172: 1071–1077, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johansen KL, Chertow GM, Jin C, Kutner NG: Significance of frailty among dialysis patients. J Am Soc Nephrol 18: 2960–2967, 2007 [DOI] [PubMed] [Google Scholar]
- 4.McAdams-DeMarco MA, Law A, Salter ML, Boyarsky B, Gimenez L, Jaar BG, Walston JD, Segev DL: Frailty as a novel predictor of mortality and hospitalization in individuals of all ages undergoing hemodialysis. J Am Geriatr Soc 61: 896–901, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McAdams-DeMarco MA, Suresh S, Law A, Salter ML, Gimenez LF, Jaar BG, Walston JD, Segev DL: Frailty and falls among adult patients undergoing chronic hemodialysis: A prospective cohort study. BMC Nephrol 14: 224, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Conroy S, Dowsing T: The ability of frailty to predict outcomes in older people attending an acute medical unit. Acute Med 12: 74–76, 2013 [PubMed] [Google Scholar]
- 7.Ekerstad N, Swahn E, Janzon M, Alfredsson J, Löfmark R, Lindenberger M, Carlsson P: Frailty is independently associated with short-term outcomes for elderly patients with non-ST-segment elevation myocardial infarction. Circulation 124: 2397–2404, 2011 [DOI] [PubMed] [Google Scholar]
- 8.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research Group : Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56: M146–M156, 2001 [DOI] [PubMed] [Google Scholar]
- 9.Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40: 373–383, 1987 [DOI] [PubMed] [Google Scholar]
- 10.Fried L, Bernardini J, Piraino B: Charlson comorbidity index as a predictor of outcomes in incident peritoneal dialysis patients. Am J Kidney Dis 37: 337–342, 2001 [DOI] [PubMed] [Google Scholar]
- 11.Di Iorio B, Cillo N, Cirillo M, De Santo NG: Charlson Comorbidity Index is a predictor of outcomes in incident hemodialysis patients and correlates with phase angle and hospitalization. Int J Artif Organs 27: 330–336, 2004 [DOI] [PubMed] [Google Scholar]
- 12.Villar E, Remontet L, Labeeuw M, Ecochard R: Effect of age, gender, and diabetes on excess death in end-stage renal failure. J Am Soc Nephrol 18: 2125–2134, 2007 [DOI] [PubMed] [Google Scholar]
- 13.Bleyer AJ, Tell GS, Evans GW, Ettinger WH, Jr., Burkart JM: Survival of patients undergoing renal replacement therapy in one center with special emphasis on racial differences. Am J Kidney Dis 28: 72–81, 1996 [DOI] [PubMed] [Google Scholar]
- 14.Pei YP, Greenwood CM, Chery AL, Wu GG: Racial differences in survival of patients on dialysis. Kidney Int 58: 1293–1299, 2000 [DOI] [PubMed] [Google Scholar]
- 15.Wong JS, Port FK, Hulbert-Shearon TE, Carroll CE, Wolfe RA, Agodoa LY, Daugirdas JT: Survival advantage in Asian American end-stage renal disease patients. Kidney Int 55: 2515–2523, 1999 [DOI] [PubMed] [Google Scholar]
- 16.Mailloux LU, Bellucci AG, Mossey RT, Napolitano B, Moore T, Wilkes BM, Bluestone PA: Predictors of survival in patients undergoing dialysis. Am J Med 84: 855–862, 1988 [DOI] [PubMed] [Google Scholar]
- 17.Molnar MZ, Streja E, Kovesdy CP, Bunnapradist S, Sampaio MS, Jing J, Krishnan M, Nissenson AR, Danovitch GM, Kalantar-Zadeh K: Associations of body mass index and weight loss with mortality in transplant-waitlisted maintenance hemodialysis patients. Am J Transplant 11: 725–736, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beddhu S, Samore MH, Roberts MS, Stoddard GJ, Ramkumar N, Pappas LM, Cheung AK: Impact of timing of initiation of dialysis on mortality. J Am Soc Nephrol 14: 2305–2312, 2003 [DOI] [PubMed] [Google Scholar]
- 19.Owen WF, Jr., Lew NL, Liu Y, Lowrie EG, Lazarus JM: The urea reduction ratio and serum albumin concentration as predictors of mortality in patients undergoing hemodialysis. N Engl J Med 329: 1001–1006, 1993 [DOI] [PubMed] [Google Scholar]
- 20.Fenton SS, Schaubel DE, Desmeules M, Morrison HI, Mao Y, Copleston P, Jeffery JR, Kjellstrand CM: Hemodialysis versus peritoneal dialysis: A comparison of adjusted mortality rates. Am J Kidney Dis 30: 334–342, 1997 [DOI] [PubMed] [Google Scholar]
- 21.Ganesh SK, Hulbert-Shearon T, Port FK, Eagle K, Stack AG: Mortality differences by dialysis modality among incident ESRD patients with and without coronary artery disease. J Am Soc Nephrol 14: 415–424, 2003 [DOI] [PubMed] [Google Scholar]
- 22.Foley RN, Parfrey PS, Sarnak MJ: Epidemiology of cardiovascular disease in chronic renal disease. J Am Soc Nephrol 9[Suppl]: S16–S23, 1998 [PubMed] [Google Scholar]
- 23.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY: Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351: 1296–1305, 2004 [DOI] [PubMed] [Google Scholar]
- 24.Zoccali C, Tripepi G, Mallamaci F: Predictors of cardiovascular death in ESRD. Semin Nephrol 25: 358–362, 2005 [DOI] [PubMed] [Google Scholar]
- 25.Kuro-o M: A potential link between phosphate and aging—lessons from Klotho-deficient mice. Mech Ageing Dev 131: 270–275, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stenvinkel P, Larsson TE: Chronic kidney disease: A clinical model of premature aging. Am J Kidney Dis 62: 339–351, 2013 [DOI] [PubMed] [Google Scholar]
- 27.Rockwood K, Mogilner A, Mitnitski A: Changes with age in the distribution of a frailty index. Mech Ageing Dev 125: 517–519, 2004 [DOI] [PubMed] [Google Scholar]
- 28.Painter P, Kuskowski M: A closer look at frailty in ESRD: Getting the measure right. Hemodial Int 17: 41–49, 2013 [DOI] [PubMed] [Google Scholar]
- 29.Mallery LH, Allen M, Fleming I, Kelly K, Bowles S, Duncan J, Moorhouse P: Promoting higher blood pressure targets for frail older adults: A consensus guideline from Canada. Cleve Clin J Med 81: 427–437, 2014 [DOI] [PubMed] [Google Scholar]
- 30.Bergman H, Ferrucci L, Guralnik J, Hogan DB, Hummel S, Karunananthan S, Wolfson C: Frailty: An emerging research and clinical paradigm—issues and controversies. J Gerontol A Biol Sci Med Sci 62: 731–737, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bouillon K, Kivimaki M, Hamer M, Sabia S, Fransson EI, Singh-Manoux A, Gale CR, Batty GD: Measures of frailty in population-based studies: An overview. BMC Geriatr 13: 64, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rothman MD, Leo-Summers L, Gill TM: Prognostic significance of potential frailty criteria. J Am Geriatr Soc 56: 2211–2216, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moorhouse P, Mallery LH: Palliative and therapeutic harmonization: A model for appropriate decision-making in frail older adults. J Am Geriatr Soc 60: 2326–2332, 2012 [DOI] [PubMed] [Google Scholar]
- 34.Renal Physicians Association : Shared Decision-Making in the Appropriate Initiation of and Withdrawal from Dialysis, 2nd Ed., Rockville, MD, Renal Physicians Association, 2010 [Google Scholar]
- 35.Bagshaw SM, Stelfox HT, McDermid RC, Rolfson DB, Tsuyuki RT, Baig N, Artiuch B, Ibrahim Q, Stollery DE, Rokosh E, Majumdar SR: Association between frailty and short- and long-term outcomes among critically ill patients: A multicentre prospective cohort study. CMAJ 186: E95–E102, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chan DC, Tsou HH, Chen CY, Chen CY: Validation of the Chinese-Canadian study of health and aging clinical frailty scale (CSHA-CFS) telephone version. Arch Gerontol Geriatr 50: e74–e80, 2010 [DOI] [PubMed] [Google Scholar]
- 37.Murray AM, Tupper DE, Knopman DS, Gilbertson DT, Pederson SL, Li S, Smith GE, Hochhalter AK, Collins AJ, Kane RL: Cognitive impairment in hemodialysis patients is common. Neurology 67: 216–223, 2006 [DOI] [PubMed] [Google Scholar]
- 38.Sehgal AR, Grey SF, DeOreo PB, Whitehouse PJ: Prevalence, recognition, and implications of mental impairment among hemodialysis patients. Am J Kidney Dis 30: 41–49, 1997 [DOI] [PubMed] [Google Scholar]
- 39.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D, Modification of Diet in Renal Disease Study Group : A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Ann Intern Med 130: 461–470, 1999 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.