Abstract
The purpose of this study was to test an intervention to increase mammography screening in women ages 51 to 75 who had not received a mammogram in the last 15 months. A total of 1681 women were randomized to: 1) a mailed tailored interactive DVD, 2) a computer-tailored telephone counseling, or 3) usual care. Women with incomes below $75,000 who were in the interactive DVD group had significantly more mammograms than women in usual care. Women with incomes above $75,000 had significantly fewer mammograms than women with incomes less than $75,000 regardless of group. Further investigation is needed to understand why women with incomes above $75,000 did not show the same benefit of the intervention.
Clinical Trials number: NCT00287040
Keywords: Breast Cancer, Randomized Trials, Cancer Screening, Health Promotion
Introduction
Although deaths from breast cancer have steadily decreased over the last decade, up to 40,000 women in the United States die from breast cancer each year. For many of these women, death could have been averted if their cancer been discovered at an earlier stage (Siegel et al., 2011). Although the best age and interval for mammography screening remains controversial, there is no debate about benefits of routine screening. Unfortunately, since 2006, the proportion of women ages 50–64 who had a mammogram in the past two years has declined by 8% demonstrating the need for an effective and easily delivered intervention to maintain routine screening (Breen et al., 2007).
For nearly two decades, research has demonstrated that tailored communication interventions have greater efficacy than targeted or non-tailored interventions regardless of media delivery (print, telephone, or in person) (Noar et al., 2007; Skinner et al., 1999). However, with the advent of new technology, we now have the opportunity to test a tailored program using widely available media such as the DVD. If tailoring to increase mammography adherence can be delivered via DVD, the potential for cost savings is apparent. We selected telephone counseling as a comparison group because studies have shown it more effective than print and it is not as labor intensive as in-person counseling.
Tailored interventions for mammography have included messages based on the constructs of perceived susceptibility, benefits and barriers to screening and self-efficacy. Although demographic variables have been considered as covariates in prior tailoring studies, few researchers have actually conducted analyses to determine if these covariates moderate the intervention effect (i.e. Does the intervention effect differ for subgroups of women) (Skinner et al., 1994; Sohl and Moyer, 2007; Bodurtha et al., 2009; Costanza et al., 2000; Rimer et al., 2002).
With rapidly evolving technology, tailored communications can be delivered with new technology media including the Web or interactive DVD’s mailed to the home; however, we lack research to identify the effect of the media type or potential moderator effects on intervention efficacy (Resnicow et al., 2010). We tested a prospective randomized intervention to determine differences in mammography adherence by type of media delivery and to determine any moderation effect of demographic variables with the intervention for women 51 to75 years of age.
Eligibility criteria included being a woman who had not had a mammogram in the past 15 months, being between 51 and 75 years of age, and being a member of a large health maintenance organization or a statewide insurance plan. Women were not eligible if they had been diagnosed with breast cancer. Eligible and consenting women were randomly assigned to receive a: 1) tailored interactive DVD, 2) computer-tailored telephone counseling, or 3) usual care. Media for delivery (DVD and Telephone) were selected because over 95% of household had either a phone or DVD,(Gruenwedel, 2010) and DVD programs could be easily developed for tailored messaging.
Specific research questions were:
At six-month follow-up, what were the differences in mammography adherence among women who received a tailored telephone counseling intervention, a mailed tailored DVD intervention, or usual care?
Did demographic characteristics of income, age, and education moderate the intervention effects for mammography adherence?
Materials and Methods
Participants were recruited from a large health maintenance organization in the Midwest and a large insurance plan in North Carolina. Mammography cost was covered with no out-of-pocket costs to members. IRB approval was obtained at both sites. First, eligible women were sent a letter explaining the study and provided an opportunity to call a toll-free number within two weeks if they did not want to be contacted. If a woman did not opt out, they were called by research assistants (RAs) using standard protocol and a computerized tracking system. RA’s explained the study and determined their interest in participating. If participants were willing to enter the study, a verbal consent was obtained and T1 data collected either immediately or during another scheduled phone call. All data were collected by trained interviewers on the phone. Consented women were mailed the written HIPPA form, which was signed and returned so that their 6 month data could be accessed from medical records. After consent, women were randomized to one of the three groups: 1) telephone, 2) mailed tailored interactive DVD, or 3) usual care. Data were collected at baseline (T1), 4 weeks (T2), and six months (T3). The T2 data included belief variables, and knowledge to determine if the intervention changed these mediators. Additionally, at T2, women in the intervention group were asked questions about satisfaction with method of intervention delivery (Skinner et al., 2011a). Although only the intervention groups were asked about satisfaction with the intervention, these questions were embedded in T2 which was completed by women in all groups. Data were collected by phone using trained interviewers at an established survey center. The usual care group completed surveys but did not receive a tailored intervention. Usual care varied depending on location but ranged from nothing to a post-card reminder when it was time to schedule a mammogram.
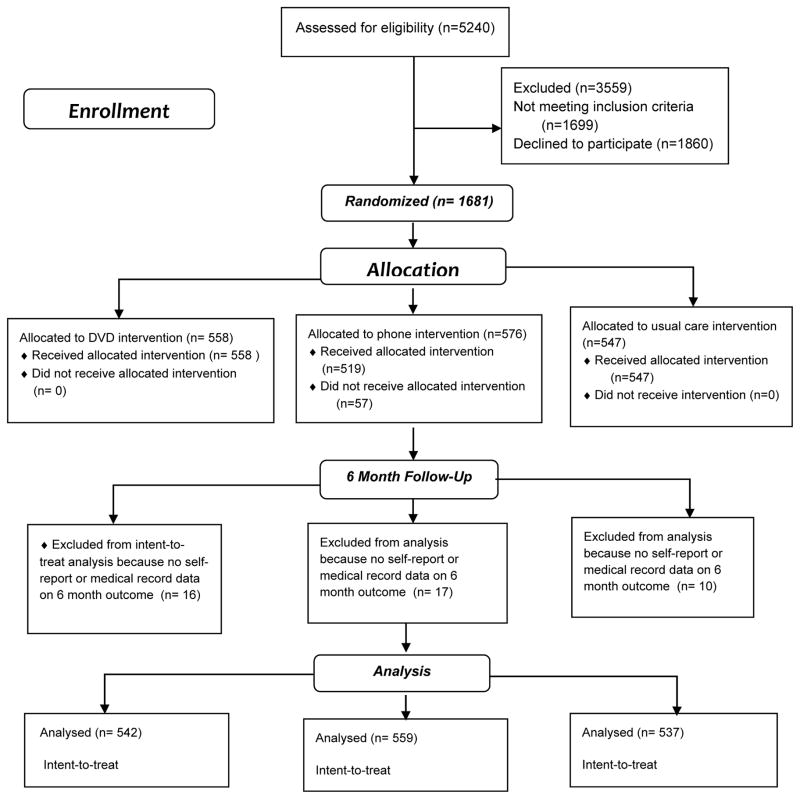
Demographic, beliefs, and self-reported screening activities were collected at T1. Beliefs and self-reported screening were collected at T3. A twenty dollar incentive was given for each of the three surveys to all three groups. Medical record claims data were used to identify mammography adherence post-intervention. Disposition of sample participants is illustrated in the Consort Diagram (Figure 1).
Figure 1.
CONSORT FLOW DIAGRAM
Statistical Strategy
The three groups were compared for distributional properties on baseline characteristics using the Kruskal-Wallis test for continuous and ordinal variables and the two-sided Fisher’s exact test for nominal categorical variables. Binary logistic regression was used to analyze the intervention effect. Demographic and other theoretically justified variables were entered as potential confounders of the relationship between the interventions and mammography adherence (Senn, 1994). Wald chi-square tests, adjusted odds ratios, and 95% confidence intervals were used to test independent variables in the logistic regression models. Interactions between the intervention and baseline covariates were tested for potential moderating effects. The study was designed to achieve a sample size of at least 534 in each of the three groups at six months, considering attrition, in order to insure at least 80% power to detect 10% differences (phone 40%, DVD 30%, usual care 20%) in six months screening between any pair of randomized groups (the omnibus test between all three groups exceeded 80% power) and 80% power to detect intervention moderation (i.e., interaction) effects that were two times stronger (i.e., 2.0 odds ratio) for one demographic category versus another category. An intent-to-treat analysis was used.
Measurement
Demographics and family history were assessed using standard questions. Belief scales included perceived risk, perceived benefits, perceived barriers, self-efficacy, breast cancer fear, and fatalism. All scales had been previously tested and found to be both reliable and valid (Champion et al., 2008)
Mammography adherence was computed with both six-month self-report interview data and medical records claim data. If either self-report or medical records indicated that women had a mammogram between baseline and six months, the mammography adherence outcome variable was scored “yes”. Of the 1,681 women with baseline interviews, 25.8% were missing the six-month interview, 9.6% were missing medical record data, and only 2.6% were missing both pieces of information. Use of both self-report and medical record data served to decrease potential bias due to missing data in either interview or medical record information. The Kappa coefficient of agreement for adherence between self-report and medical records was .82 in our sample among women with both sources of data.
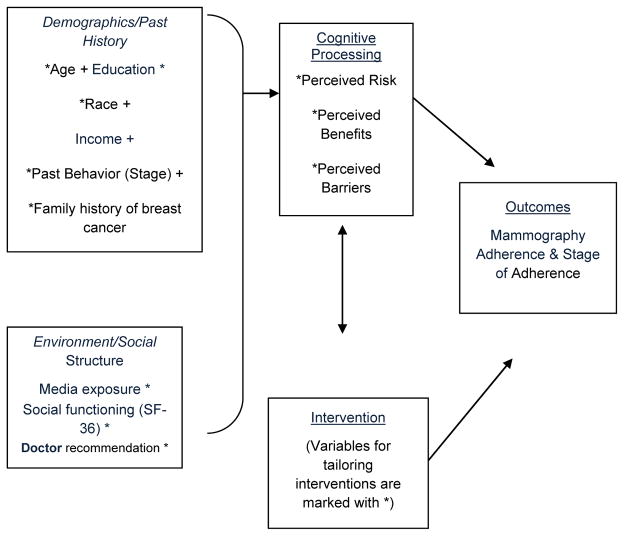
Theoretical Development of Intervention
The theoretical frameworks supporting the development of tailored interventions included the Health Belief and Transtheoretical Model previously associated with mammography use (Champion et al., 2008; Prochaska et al., 2008; Champion and Huster, 1995; Champion et al., 2000; Champion and Skinner, 2003; King et al., 1994; Skinner et al., 1998; Champion, 1991; Vernon et al., 1990; Schechter et al., 1990; Lierman et al., 1991; Rimer et al., 1988; Taplin and Montano, 1993; Rimer et al., 2002; Champion et al., 2006; Avis et al., 2004). Perceived and actual risk, perceived benefits, barriers, self-efficacy, and knowledge constructs were used for tailoring both the DVD and telephone interventions. Although intervention content has been explained in detail elsewhere, we provide the basic methodology below (Skinner et al., 2011a).
First tailored messages were developed for the theoretical constructs of perceived and actual risk, benefits, self-efficacy, and barriers as well as age and race. Tailoring was done by first asking participants to respond to a question about each belief. Participants responded to the belief questions using the arrows on the DVD remote. Message responses were selected based on algorithms built into the DVD program. Fatalism, which was assessed with its own scale for the baseline and follow-up assessments, was considered to be a barrier for the purpose of tailoring. By answering simple questions with the remote control throughout the program, messages specific to the individual woman’s beliefs were delivered. For instance, if a woman did not perceive herself to be at risk for breast cancer and had a family history, the message delivered included information that 3 out of 4 women who get breast cancer have no family history. There were 36 or more combinations of messaging. The number of message possibilities varied depending on the woman’s responses to queries. A woman could select none or up to seven barriers and for each barrier selected, a message was delivered. If a barrier was not selected, no message was delivered. The DVD allowed us to use video and other visual representations when delivering the message. The programmed DVD began with a narrator introducing the program. Four women representing different demographic profiles were selected to deliver intervention messages. An animation of breast cancer developing and metastasizing was shown. Women who had not had a previous mammogram viewed a video of the mammography process. Finally, women were queried about barriers that would prevent them from receiving a mammogram and messages to address these barriers provided through tailored programming. Fatalism and fear were measured with separate scales during interview assessments, but were considered as part of the barriers construct for the purpose of tailoring. For instance, one barrier was “I am afraid of finding out that I might have breast cancer”. The DVD program ended with the narrator encouraging viewers to make a mammography appointment.
The telephone intervention was developed using the same tailoring variables and messages used in the interactive DVD, keeping the message content consistent so that intervention arms varied only by media delivery. Telephone counselors were graduate students trained to deliver a standardized message that reflected each woman’s responses to questions, and sessions were recorded for quality control. Evaluation of phone interventions reflected a high degree of consistency. Interveners were trained to politely terminate attempts at extra dialogue to keep both content and time consistent for each participant. The average length of time spent using the interactive DVD was 10 minutes and the telephone intervention took, on average, 11.3 minutes.
Results
Sample
A total of 3,541 women were eligible for the study, and 1,860 refused to participate, yielding 1,681 consented participants for a participation rate of 1681 / 3541 or 47.5% (See Figure 2). Participants had baseline data collected after verbal telephone consent and were mailed a written informed consent and HIPPA authorization form to allow the research team to access medical records claims data. Attrition for the T2 self-report survey was 271 (16%) and for T3 was 433 (26%). Before the study ended, the Indiana medical insurance company aligned with this study was split into different groups, thus medical claims data for women if the Midwest was more difficult to obtain. In order to reduce missing data, both medical record and interview data for determining six-month mammography adherence combined both medical records and self-report allowing inclusion of 1,638 women. Demographic characteristics of the 1,638 women are included in Table 1. Most participants were Caucasian and about 15% of women reported their race as African American. Despite random assignment, the groups differed significantly on binary education (4 year college degree or less) and marginally on baseline stage (pre-contemplation vs. contemplation). These and other theoretically important covariates were adjusted for in the models.
Figure 2.
Theoretical Framework
* = Intervention/Tailoring Variables
Table 1.
Participant Characteristics and Baseline Beliefs by Group (N=1,638)
| Characteristics/Beliefs | DVD Group (N = 542) | Telephone Group (N = 559) | Usual Care Group (N = 537) | P value |
|---|---|---|---|---|
| Age, mean (SD) | 51.5 (7.9) | 51.7 (8.1) | 52.3 (8.0) | 0.1149 |
| Years of education, mean (SD) | 14.4 (2.4) | 14.2 (2.3) | 14.6 (2.6) | 0.0830 |
| Number of media sources from which heard about mammograms in the last six months | 2.9 (1.7) | 2.9 (1.8) | 3.0 (1.7) | 0.3609 |
| Education: ≥4 year college degree | 175 (32.3) | 171 (30.6) | 204 (38.0) | 0.0263 |
| Race | ||||
| Black or African American | 83 (15.3) | 83 (14.9) | 71 (13.3) | 0.4083 |
| White | 443 (81.7) | 466 (83.7) | 451 (84.5) | |
| Other | 16 (3.0) | 8 (1.4) | 12 (2.3) | |
| Married or living with a partner, n (%) yes | 406 (74.9) | 433 (77.5) | 390 (72.3) | 0.1822 |
| Currently working for pay, n (%) yes | 442 (81.6) | 437 (78.2) | 421 (78.4) | 0.3027 |
| Household income | ||||
| <$30,000 | 91 (17.2) | 84 (15.5) | 86 (16.3) | 0.9662 |
| $30,001 – $75,000 | 234 (44.2) | 245 (45.2) | 237 (44.8) | |
| >75,001 | 204 (38.6) | 213 (39.3) | 206 (38.9) | |
| Mammography stage (baseline) | ||||
| Pre-contemplation | 166 (30.6) | 162 (29.0) | 133 (24.8) | 0.0851 |
| Contemplation | 376 (69.4) | 397 (71.0) | 404 (75.2) | |
| Site | ||||
| North Carolina | 319 (58.9) | 341 (61.0) | 312 (58.1) | 0.5967 |
| Indiana University | 223 (41.1) | 218 (39.0) | 225 (41.9) | |
Note. For continuous variables and ordinal income, the Kruskall Wallis test was used. For categorical variables, the two-sided Fisher’s exact test was used.
Research Question 1
Mammography adherence did not differ by group after adjusting for covariates (See Table 2) when comparing DVD or phone versus usual care. We also tested DVD versus phone using this model and this main effect was not significant (p = 0.89). However, other variables including age, knowledge, perceived susceptibility, perceived barriers, and baseline stage significantly predicted adherence. Older women who were contemplating a mammogram at baseline and had fewer perceived barriers and were more likely to obtain a mammogram, after adjusting for other variables in the model. Greater perceived susceptibility marginally (p = .051) predicted mammography screening.
Table 2.
Logistic Regression Model for Mammography Screening
| N = 1599 | Regression Coefficient | Standard Error | Wald Chi-square | DF | Value | Adjusted Odds Ratio (95 % CI) |
|---|---|---|---|---|---|---|
| Covariates | ||||||
| Baseline Stage (Contemplation vs. Pre-Contemplation) | 1.373 | .143 | 92.16 | 1 | <.0001 | 3.95 (2.98, 5.23) |
| Age | .030 | .008 | 15.33 | 1 | <.0001 | 1.03 (1.02, 1.05) |
| Education 4 yrs. college or more | .23 | .130 | 3.31 | 1 | .0690 | 1.27 (0.98, 1.63) |
| Married | .039 | .141 | 0.08 | 1 | .7828 | 1.04 (0.79, 1.37) |
| Number of media sources | .043 | .032 | 1.74 | 1 | .1877 | 1.05 (0.98, 1.11) |
| Site (North Carolina vs. Indiana) | −.114 | .114 | 0.99 | 1 | .3190 | 0.89 (0.71, 1.12) |
| Income, Omnibus Wald Chi-square | 6.14 | 2 | .0465 | |||
| Income (>75K vs. <30K) | .753 | .311 | 5.88 | 1 | .0153 | |
| Income (30–75K vs. <30K) | .432 | .291 | 2.21 | 1 | .1374 | |
| Beliefs | ||||||
| Barrier | −.020 | .006 | 9.70 | 1 | .0018 | 0.98 (0.97, 0.99) |
| Benefit | .012 | .027 | 0.21 | 1 | .6496 | 1.01 (0.96, 1.07) |
| Self-Efficacy | −.010 | .014 | 0.49 | 1 | .4832 | 0.99 (0.96, 1.02) |
| Susceptibility | .033 | .017 | 3.81 | 1 | .0510 | 1.03 (1.00, 1.07) |
| Fear | .007 | .009 | 0.57 | 1 | .4515 | 1.01 (0.99, 1.03) |
| Fatalism | −.013 | .010 | 1.72 | 1 | .1898 | 0.99 (0.97, 1.01) |
| Knowledge | −.009 | .054 | 0.03 | 1 | .8739 | 0.99 (0.89, 1.10) |
| Intervention effect | ||||||
| Omnibus Wald Chi-square | 1.26 | 2 | .5336 | |||
| DVD vs. control | .353 | .337 | 1.10 | 1 | .2951 | |
| Phone vs. control | .304 | .347 | 0.77 | 1 | .3811 | |
| Interaction between intervention and income | ||||||
| Omnibus Wald Chi-square | 11.03 | 4 | .0262 | |||
Note: Odds ratios were not reported for income or intervention effects because there was an interaction between those two variables. The interaction is described in the next table. DF indicates degrees of freedom for Wald Chi-square test.
Research Question 2
The interaction between income and the intervention on mammography adherence was significant (omnibus test, p = .026; Table 2) indicating a moderation effect. Income was originally categorized into three groups: 1) low (below $30,000), 2) medium ($30,000 to $75,000) and 3) high (above $75,000). To understand this interaction, we ran a binary logistic regression separately for the three income groups, testing the DVD versus control within each income group while adjusting for the same covariates. The DVD-versus-control effect size (i.e., adjusted odds ratio) was similar for lower (1.42) and middle (1.59) income groups; therefore, these two groups were combined when reporting the findings in Table 3. Table 3 shows results for the intervention effect of DVD versus control, and phone versus control, using two binary logistic regressions, one for the combined low and middle income groups and another regression for the higher income group. We also re-ran the models using phone as the reference category so that we could obtain the effect for DVD versus phone. For women with incomes less than $75,000, the DVD intervention did not significantly differ in mammograms obtained compared to the telephone. In comparison, the DVD was significantly less effective than usual care (adjusted odds ratio = 0.63), and significantly less effective than phone (adjusted odds ratio = 0.57), in producing mammography adherence for the highest income group (Table 3).
Table 3.
Effect of Interaction Between Intervention and Income on Mammography Screening
| Regression Coefficient | Standard Error | Wald Chi-square | p-value | Adjusted Odds Ratio (95 % CI) | |
|---|---|---|---|---|---|
| High Income (>+75K) (n = 623) | |||||
| DVD (35.3%) vs. control (47.1%) | −.457 | .219 | 4.38 | .0364 | 0.63 (0.41, 0.97) |
| Phone (45.5%) vs. control (47.1%) | .100 | .214 | 0.22 | .6393 | 1.11 (0.73, 1.68) |
| DVD (35.3%) vs. Phone (45.5%) | −.558 | .218 | 6.52 | .0106 | 0.57 (0.37, 0.88) |
| Low and Middle Income (<75K) (n = 976) | |||||
| DVD (41.2%) vs. control (35.6%) | .414 | .174 | 5.70 | .0170 | 1.51 (1.08, 2.13) |
| Telephone (40.4%) vs. control (35.6%) | .285 | .172 | 2.74 | .0977 | 1.33 (0.95, 1.86) |
| DVD (35.3%) vs. Phone (45.5%) | .129 | .170 | 0.58 | .4471 | 1.14 (0.82, 1.59) |
Note. The intervention effects in Table 3 are adjusted for the same covariates as in the final model shown in Table 2, except the models used for Table 3 are estimated separately for two income levels instead of adjusted for income. The percentage in parentheses after the labels for DVD, phone, and control are the rates of mammography screening (from medical records and interview data) unadjusted for covariates. Each Wald chi-square test was based upon 1 degree of freedom.
Discussion
Neither the DVD nor Phone intervention was effective for the group as a whole. However, income significantly moderated the intervention effect. Women randomized to the tailored DVD group who had incomes at $75,000 or below demonstrated greater mammography adherence compared to usual care. Since over 60% of women in this study had household incomes of $75,000 or less, this finding has significant translational potential. For these women, an inexpensive DVD mailed to their home may be all that is needed to increase mammography adherence.
Surprisingly, women with higher incomes actually received fewer mammograms if they were randomized to receive a DVD as compared to the control or to the telephone intervention group. It should be noted that women with higher incomes had more mammograms than women with the lowest incomes, regardless of group assignment; however, further investigation is needed to understand why the intervention was less effective with women who had incomes above $75,000. Understanding the negative impact of DVD on women whose household income was greater than $75,000 is challenging. One hypothesis would be that women with higher incomes did not take the time to view the DVD. However, previous analysis reported that regardless of income, the majority of women (91%) reported viewing the entire DVD across all groups (Skinner et al., 2011b). Although these results are based on self-report, there is no reason to think that the women with higher incomes would over-report viewing compared to other women. Perhaps there was something about the DVD that negatively impacted women with higher incomes. Three of the four female actors were cast as women with lower incomes. Only one character was a professional woman. Communication research supports actors being similar to recipients for greatest effect. Additionally, women with higher incomes may have been more accustomed to gaining health information from the Internet. Income has been shown to be a strong predictor of Internet use, with 95% of people making over $75,000 using internet services versus only 57% internet use for those in households making less than $30,000.(Fox, 2011) If women with higher incomes seek most of their health information on the Internet, a mailed DVD may not be as effective as it is for women with middle or lower incomes.
The usual care group had a significantly larger percentage of women who reported a college education or greater and were more likely to be in contemplation as compared to the women assigned to the DVD or telephone counseling group. It is possible that these factors created a greater testing effect in the high income group (although the fact that we adjusted for education and baseline stage in the models should have ameliorated these potential influences on the efficacy results). A similar result was reported by other investigators who discussed the probable impact that data collection had on colon cancer screening regardless of intervention (Vernon et al., 2011; Saywell et al., 2004).
The telephone intervention did not significantly alter mammography adherence regardless of income, results that differ from past research (Champion et al., 2003; Champion et al., 2002; Champion et al., 2007). In retrospect, the delivery of telephone messages for this study diverged from our previous work. The current telephone intervention was tightly scripted so that content could be held constant for comparison of media delivery. The interveners were trained to discuss only the messages that were to be tailored. When the conversations were reviewed for quality assurance, evaluators found the intervention was more stilted and less interactive than the less-scripted interventions we have tested previously. Our intent in developing a tightly scripted telephone intervention was to keep content as similar as possible, while varying only the delivery medium. In so doing, we may have inadvertently limited the ability of the intervener to respond to cues from the participant. Fidelity was determined by recording each session and evaluating content using standard checklists. Intervention concerns were discussed at weekly meetings.
Limitations
Generalization of results of this study are limited to women who agreed to participate. In addition, although participants were randomized to groups, the usual care group had a significantly higher education and marginally higher stage of contemplation at baseline, perhaps allowing issues such as testing effects to differentially influence this group. Finally, approximately 10% of the sample was missing medical record data and self-report data were substituted raising the possibility of social desirability influencing participant responses.
Conclusion
Our results provide significant insight as to the importance of intervention media across income groups. The DVD intervention significantly increased mammography adherence for women whose household income was $75,000 or under. As internet and DVD usage changes over time, we need to continue to assess which media are effective for which groups (e g. would DVD be more effective for certain income levels and are there other demographic variables that could act as moderators). Personalized medicine has become an area of focus in pharmacological studies; and there is no reason why behavioral interventions should not also be investigated to determine the type of media delivery best suited to subgroups of women. More research and statistical modeling is needed to determine the moderation effects of various demographic variables. In the meantime, for lower and middle-income women, the DVD may be an inexpensive method for delivering health education.
Although 91% of women in the DVD group reported receiving and viewing the DVD, women may have varied as to attention to the program (Skinner et al., 2011b). Research is needed to determine how acceptability of media varies by individual characteristics and by intervention content. Scientists are beginning to use complex methodological designs to identify the interplay of content, methods for message delivery, and actual technology delivery intervention effectiveness (Resnicow et al., 2010). It will be important for future studies to consider the impact of demographic moderators on intervention effectiveness to increase the impact of tailored media.
Acknowledgments
Source of Support: Institute for Nursing Research at the National Institutes of Health under Award Number R01 NR008434 and by the National Cancer Institute of the National Institutes of Health under Award Number R25CA117865
Research reported in this publication was funded by Institute for Nursing Research at the National Institutes of Health Award Number R01 NR008434 and supported by the National Cancer Institute of the National Institutes of Health under Award Number R25CA117865. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Reprints are not available from the authors
Conflict of Interest Statement:
The authors declare that there are no conflicts of interest.
References
- Avis NE, Smith KW, Link CL, et al. Increasing mammography screening among women over age 50 with a videotape intervention. Preventive Medicine. 2004;39:498–506. doi: 10.1016/j.ypmed.2004.05.024. [DOI] [PubMed] [Google Scholar]
- Bodurtha J, Quillin JM, Tracy KA, et al. Mammography screening after risk-tailored messages: the women improving screening through education and risk assessment (WISER) randomized, controlled trial. Journal of Women’s Health. 2009;18:41–47. doi: 10.1089/jwh.2007.0703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breen N, Cronin KA, Meissner HI, et al. Reported drop in mammography: Is this cause for concern? Cancer Online. 2007 doi: 10.1002/cncr.22723. [DOI] [PubMed] [Google Scholar]
- Champion V, Maraj M, Hui S, et al. Comparison of tailored interventions to increase mammography screening in nonadherent older women. Preventive Medicine. 2003;36:150–158. doi: 10.1016/s0091-7435(02)00038-5. [DOI] [PubMed] [Google Scholar]
- Champion V, Skinner CS, Hui S, et al. The effect of telephone versus print tailoring for mammography adherence. Patient Education and Counseling. 2007;65:416–423. doi: 10.1016/j.pec.2006.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Champion VL. The relationship of selected variables to breast cancer detection behaviors in women 35 and older. Oncology Nursing Forum. 1991;18:733–739. [PubMed] [Google Scholar]
- Champion VL, Huster G. Effect of interventions on stage of mammography adoption. Journal of Behavioral Medicine. 1995;18:169–187. doi: 10.1007/BF01857868. [DOI] [PubMed] [Google Scholar]
- Champion VL, Monahan PO, Springston JK, et al. Measuring mammography and breast cancer beliefs in African American Women. Journal of Health Psychology. 2008;13:827–837. doi: 10.1177/1359105308093867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Champion VL, Ray DW, Heilman DK, et al. A tailored intervention for mammography among low-income African-American women. Journal of Psychosocial Oncology. 2000;18:1–13. [Google Scholar]
- Champion VL, Skinner CS. Differences in perceptions of risk, benefits, and barriers by stage of mammography adoption. Journal of Women’s Health. 2003;12:277–286. doi: 10.1089/154099903321667618. [DOI] [PubMed] [Google Scholar]
- Champion VL, Skinner CS, Menon U, et al. Comparison of tailored mammography interventions at two months post intervention. Annals of Behavioral Medicine. 2002;24:211–218. doi: 10.1207/S15324796ABM2403_06. [DOI] [PubMed] [Google Scholar]
- Champion VL, Springston JK, Zollinger TW, et al. Comparison of three interventions to increase mammography screening in low income African American women. Cancer Detectection and Prevention. 2006;30:535–544. doi: 10.1016/j.cdp.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Costanza ME, Stoddard AM, Luckmann R, et al. Promoting mammography: results of a randomized trial of telephone counseling and a medical practice intervention. American Journal of Preventive Medicine. 2000;19:39–46. doi: 10.1016/s0749-3797(00)00150-1. [DOI] [PubMed] [Google Scholar]
- Fox S. Profiles of health information seekers. Pew Internet and American Life Project 2011 [Google Scholar]
- Gruenwedel E. [accessed March 23, 2011];Home Media Magazine. 2010 [Google Scholar]
- King ES, Rimer BK, Seay J, et al. Promoting mammography use through progressive interventions: Is it effective? American Journal of Public Health. 1994;84:104–106. doi: 10.2105/ajph.84.1.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lierman LM, Kasprzyk D, Benoliel JQ. Understanding adherence to breast self-examination in older women. Western Journal of Nursing Research. 1991;13:46–66. doi: 10.1177/019394599101300104. [DOI] [PubMed] [Google Scholar]
- Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin. 2007;133:673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Spring B, Nigg CR. Multiple health behavior change research: an introduction and overview. Preventive Medicine. 2008;46:281–285. doi: 10.1016/j.ypmed.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnicow K, Strecher V, Couper M, et al. Methodologic and design issues in patient-centered e-health research. American Journal of Preventive Medicine. 2010;38:98–102. doi: 10.1016/j.amepre.2009.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimer BK, Davis SW, Engstrom PF, et al. Some reasons for compliance and noncompliance in a health maintenance organization breast cancer screening program. Journal of Compliance in Health Care. 1988;3:103–114. [PubMed] [Google Scholar]
- Rimer BK, Halabi S, Sugg Skinner C, et al. Effects of a mammography decision-making intervention at 12 and 24 months. American Journal of Preventive Medicine. 2002;22:247–257. doi: 10.1016/s0749-3797(02)00417-8. [DOI] [PubMed] [Google Scholar]
- Saywell RM, Jr, Champion VL, Skinner CS, et al. A cost-effectiveness comparison of three tailored interventions to increase mammography screening. Journal of Women’s Health. 2004;13:909–918. doi: 10.1089/jwh.2004.13.909. [DOI] [PubMed] [Google Scholar]
- Schechter C, Vanchieri CF, Crofton C. Evaluating women’s attitudes and perceptions in developing mammography promotion messages. Public Health Reports. 1990;105:253–257. [PMC free article] [PubMed] [Google Scholar]
- Senn S. Testing for baseline balance in clinical trials. Statistics in Medicine. 1994;13:1715–1726. doi: 10.1002/sim.4780131703. [DOI] [PubMed] [Google Scholar]
- Siegel R, Ward E, Brawley O, et al. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA: A Cancer Journal for Clinicians. 2011;61:212–236. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- Skinner CS, Arfken CL, Sykes RK. Knowledge, perceptions, and mammography stage of adoption among older urban women. American Journal of Preventive Medicine. 1998;14:54–63. doi: 10.1016/s0749-3797(97)00008-1. [DOI] [PubMed] [Google Scholar]
- Skinner CS, Buchanan A, Champion V, et al. Process outcomes from a randomized controlled trial comparing tailored mammography interventions delivered via telephone vs. DVD. Patient Education and Counseling. 2011a;85:308–312. doi: 10.1016/j.pec.2010.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner CS, Buchanan AH, Champion V, et al. Process outcomes from a randomized controll trial comparing tailored mammography interventions delivered via telephone vs. DVD. Patient Education and Counseling. 2011b;85:308–312. doi: 10.1016/j.pec.2010.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner CS, Campbell MK, Rimer BK, et al. How effective is tailored print communication? Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 1999;21:290–298. doi: 10.1007/BF02895960. [DOI] [PubMed] [Google Scholar]
- Skinner CS, Strecher VJ, Hospers H. Physicians’ recommendations for mammography: Do tailored messages make a difference? American Journal of Public Health. 1994;84:43–49. doi: 10.2105/ajph.84.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohl SJ, Moyer A. Tailored interventions to promote mammography screening: a meta-analytic review. Preventive Medicine. 2007;45:252–261. doi: 10.1016/j.ypmed.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taplin SH, Montano DE. Attitudes, age, and participation in mammographic screening: a prospective analysis. Journal of the American Board of Family Practice. 1993;6:13–23. [PubMed] [Google Scholar]
- Vernon SW, Bartholomew LK, McQueen A, et al. A randomized controlled trial of a tailored interactive computer-delivered intervention to promote colorectal cancer screening: sometimes more is just the same. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2011;41:284–299. doi: 10.1007/s12160-010-9258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernon SW, Laville EA, Jackson GL. Participation in breast screening programs: a review. Social Science & Medicine. 1990;30:1107–1118. doi: 10.1016/0277-9536(90)90297-6. [DOI] [PubMed] [Google Scholar]