Abstract
Purpose/Objectives
To describe evidence-based practice (EBP) beliefs and behaviors of nurses who provide cancer pain management.
Design
Descriptive, cross-sectional with a mixed-methods approach.
Setting
Two inpatient oncology units in the Pacific Northwest.
Sample
40 RNs.
Methods
Data collected by interviews and web-based surveys.
Main Research Variables
EBP beliefs, EBP implementation, evidence-based pain management.
Findings
Nurses agreed with the positive aspects of EBP and their implementation ability, although implementation level was low. They were satisfied with their pain management practices. Oncology nursing certification was associated with innovativeness, and innovativeness was associated with EBP beliefs. Themes identified were (a) limited definition of EBP, (b) varied evidence-based pain management decision making, (c) limited identification of evidence-based pain management practices, and (d) integration of nonpharmacologic interventions into patient care.
Conclusions
Nurses' low level of EBP implementation in the context of pain management was explained by their trust that standards of care and medical orders were evidence-based.
Implications for Nursing
Nurses' EBP beliefs and behaviors should be considered when developing strategies for sustaining evidence-based pain management practices. Implementation of the EBP process by nurses may not be realistic in the inpatient setting; therefore, hospital pain management policies need to be evidence-based and reinforced with nurses.
Keywords: evidence-based practice, evidence-based practice beliefs, evidence-based practice behaviors, cancer pain management, mixed methods
Satisfactory pain management remains the single most important challenge to managing quality of life for patients with cancer (Dray, 2010). A seminal study by Cleeland et al. (1994) found that 42% of patients with cancer pain were not given adequate analgesic therapy. A systematic review confirmed that patients with cancer continued to report insufficient treatment of pain (Deandrea, Montanari, Moja, & Apolone, 2008). About 50% of patients receiving active treatment for cancer experience moderate to severe pain, as do 80%−90% of patients with advanced disease (van den Beuken-van Everdingen et al., 2007). Although evidence-based guidelines for clinical management of cancer-related pain are available from organizations such as the Agency for Health Care Policy and Research, American Pain Society, National Comprehensive Cancer Network, and Oncology Nursing Society, nurses may continue to implement traditional pain management practices rather than basing their care on the best research evidence currently available.
Evidence-based practice (EBP) involves clinical decision making based on current best research evidence, clinical expertise, and patient preferences (Sackett, Rosenberg, Gray, Haynes, & Richardson, 1996). The Institute of Medicine (2009) has set a goal that, by 2020, 90% of clinical decisions made by healthcare professionals will be evidence-based. EBP, in the context of pain management, decreases resource use and patient length of stay and improves patient outcomes, including patient satisfaction, quality of life, and symptom distress (Chang, Hwang, & Kasimis, 2002; Green et al., 2010; Samuels, 2010). Although positive outcomes are associated with EBP, nurses are not consistent about adopting evidence-based pain management practices (Bell & Duffy, 2009; Herr et al., 2012; Idell, Grant, & Kirk, 2007; Samuels, 2010).
Nurses' Evidence-Based Practice Beliefs
Beliefs about the value of EBP and the ability to implement it are associated with nurses' delivery of evidence-based care (Melnyk et al., 2004; Squires, Estabrooks, Gustavsson, & Wallin, 2011). A survey by Pravikoff, Tanner, and Pierce (2005) of 3,000 RNs from across the United States examined nurses' perceptions of their access to tools to obtain evidence and their possession of the skills to do so. Of the 1,097 respondents, 68% felt more confident about asking colleagues or peers and searching the Internet than about using bibliographic databases such as PubMed or CINAHL®. A more recent survey (Melnyk, Fineout-Overholt, Gallagher-Ford, & Kaplan, 2012) of 1,015 members of the American Nurses Association found that nurses wanted to obtain the knowledge and skills necessary to deliver evidence-based care but continued to face implementation barriers.
Nurses' top reasons for adopting EBP are having a personal interest in the change in practice, avoiding risk of negative consequences to the patient, and personally valuing the evidence (Brown, Wickline, Ecoff, & Glaser, 2009). A positive relationship exists between nurses' intentions to use research in practice and participatory management, academic degrees, education, availability of relevant research, time, positive attitudes, and mentorship. A systematic review by Squires et al. (2011) found that the only individual characteristic consistently related to the use of research in practice was nurses' attitude toward research. Little is known about the relationship between EBP beliefs and evidence-based pain management implementation among oncology nurses.
Challenges
Evidence-based pain management is highly complex and not easily incorporated into healthcare systems and processes (Samuels, 2010). Evidence-based pain management implementation involves comprehensive assessment of pain with a reliable and valid patient-report instrument, delivery of pharmacologic and nonpharmacologic interventions based on assessment findings, frequent reassessment of pain, and repeated delivery of interventions (Aiello-Laws & Ameringer, 2009). Based on the patient's pain experience, providers make a decision regarding maintaining the current analgesic regimen or optimizing it by changing the dose, switching medications, adding treatments for side effects, or adding other pharmacologic or nonpharmacologic therapies. Provider and organizational factors such as lack of time, heavy workload, inadequate pain assessment, underuse of pharmacologic interventions, and lack of knowledge of pain management principles have been found to influence healthcare organizations' evidence-based pain management practices (Samuels, 2010; Samuels & Fetzer, 2009; Wilson, 2007).
The culture of nursing units within the healthcare setting is an important organization-level factor in the implementation of EBP (Austin & Claassen, 2008; Estabrooks et al., 2008; Pepler et al., 2005; Scott & Pollock, 2008) and evidence-based pain management (Lauzon Clabo, 2008; Wild & Mitchell, 2000). Attitudes about pain and pain management may extend to the group or unit level, creating a type of “group-think” about pain management issues (Wild & Mitchell, 2000). An organizational culture that actively supports EBP was significantly and positively related to EBP beliefs and EBP implementation among nurses in a community hospital and a research-oriented hospital (Melnyk, Fineout-Overholt, Giggleman, & Cruz, 2010). A survey of members of the American Nurses Association by Melnyk et al. (2012) found that 54% of the 1,015 respondents agreed or strongly agreed that EBP was consistently implemented in their organization, and only 35% agreed or strongly agreed that their colleagues consistently implemented EBP with their patients. The findings support the importance of understanding the unit culture for evidence-based pain management.
Theoretical Framework
Rogers' (2003) diffusion of innovations model provides a theoretical framework for understanding why nurses adopt or reject evidence-based pain management. Diffusion is the process by which an innovation is communicated through channels within a social system. Evidence-based pain management can be considered an innovation because it requires shifting an existing idea or practice and developing a new opinion toward a new idea or practice. The hospital setting is a social system, where nurses and other healthcare providers work together on problem solving to accomplish a common goal of improving the disease state of patients. Changing current pain management practice to evidence-based pain management can be considered a diffusion of innovation process.
Adoption of an innovation often is assumed to occur automatically; however, the rate of diffusion is affected by the social system's communication strategies and individual's decision-making process (Rogers, 2003). Antecedents to an individual's decision making regarding adoption of an innovation are the individual's previous practice, perception of existing needs or problems, and innovativeness, as well as the norms of his or her social system. The purpose of the current study was to describe antecedents to evidence-based pain management decision making of nurses who provide care to patients with cancer pain. Specifically, the researchers sought to answer the following questions: (a) What are the antecedents to nurses' evidence-based pain management decision making? and (b) Do significant relationships exist between nurses' characteristics and their antecedents to evidence-based pain management decision making?
Methods
A descriptive, cross-sectional, mixed-methods design involving two inpatient oncology units—one at each of two medical centers—was used. The medical centers were a 450-bed academic medical center and a 491-bed community-based regional medical center in the Pacific Northwest. The study was approved by the University of Washington Institutional Review Board. The study sample was comprised of RNs who were employed at least part-time at one of the medical centers and who provided direct care to patients with cancer pain. The academic medical center's 28-bed medical-surgical oncology unit employed 46 RNs. The regional medical center's 34-bed medical oncology unit, which specialized in end-of-life care, employed 60 RNs.
Nurses were invited to participate in the study at shift change by the investigator, via flyers posted on the unit, and through emails sent by the nurse manager or nurse researcher at the medical center. Nurses who were interested in learning more about the study were directed to the study website, created with Catalyst Web Tools. Potential participants provided consent for study participation by completing web-based questionnaires.
Quantitative Data Collection and Measures
Questionnaires included a demographic questionnaire, the EBP Beliefs Scale (Melnyk, Fineout-Overholt, & Mays, 2008), the EBP Implementation Scale (Melnyk, et al., 2008), and Carlson's (2008) Prior Conditions Instruments. Survey data were collected from 44 RNs in May and June 2013.
The EBP Beliefs Scale measures clinicians' beliefs about the value of EBP and their ability to implement it. It consists of 16 items using a five-point Likert-type scale. The scale was treated as a one-factor scale in which items were summed and divided by 16 to yield a mean score that ranged from 1–5. Higher scores indicated stronger EBP beliefs. Examples of items include: “I believe that EBP results in the best clinical care for patients,” “I know how to implement EBP sufficiently enough to make practice changes,” and “I believe the care I deliver is evidence-based.” The scale has established face, content, and construct validity with internal consistency reliabilities typically greater than 0.85 and Cronbach alpha greater than 0.9 (Melnyk et al., 2008).
The EBP Implementation Scale measures the extent to which clinicians perceive themselves as having implemented EBP in the past eight weeks. It consists of 18 items using a five-point Likert-type scale. The scale was treated as a one-factor scale in which items were summed and divided by 18 to yield a mean score that ranged from 1–5. Higher scores indicated higher levels of performance of EBP activities. Activities addressed by the items included: “Critically appraised evidence from a research study,” “Used an EBP guideline or systematic review to change clinical practice where I work,” and “Promoted the use of EBP to my colleagues.” The scale has established face, content, and construct validity with internal consistency reliabilities and Cronbach alpha greater than 0.9 (Melnyk et al., 2008).
Carlson's (2008) Prior Conditions Instruments were designed to measure constructs in Rogers' (2003) Diffusion of Innovations model. These constructs, termed “prior conditions,” include previous practices, perceived existing needs or problems, innovativeness, and social system norms. They influence nurses' decisions to use evidence-based pain management practices. The subscales include 11 items on nurses' perceptions of how often they perform evidence-based pain management (previous practices), 6 items on nurses' beliefs about pain and perceptions of pain management (perceived existing needs or problems), 6 items on nurses' ability to initiate or adapt to change (innovativeness), and 7 items on nurses' perceptions about colleagues' pain management behaviors (social system norms). All items use a five-point Likert-type scale. Each instrument was treated as a one-factor scale. Items were summed and divided by the number of subscale items to yield a mean score that ranged from 1–5. Higher scores indicated more support for the conditions for the adoption of evidence-based pain management practices. The subscales have established construct validity and a Cronbach alpha range of 0.73–0.83 (Carlson, 2008).
Qualitative Data Collection
From August to October 2013, a subgroup of 12 nurses participated in individual semistructured interviews to share their perceptions of EBP in the context of evidence-based pain management. Nurses were selected for an individual interview based on their level of evidence-based pain management documentation in the patient medical record, which was examined as part of a larger study on barriers and facilitators to evidence-based pain management in the inpatient oncology setting. Three nurses with low scores and three nurses with high scores for evidence-based pain management documentation from each medical center were selected for the interview. Nurses were invited by email and in person by the investigator. Two nurses who were invited chose not to participate because of lack of time. Twelve nurses—six from each medical center—participated in a telephone or in-person interview with the investigator. The interview questions had been pilot tested with two RNs who provide pain management at other healthcare organizations. Their feedback on the clarity and validity of the questions was used to develop the interview guide (see Figure 1). All interviews were digitally recorded, with consent, and lasted from 30–45 minutes. Interview responses were transcribed verbatim by an experienced transcriptionist. These transcriptions provided the narrative data for qualitative analysis.
Figure 1. Nurse Semistructured Interview Guide.
Data Analysis
Quantitative data from the study questionnaires were entered into SPSS®, version 21.0, for statistical analysis. Descriptive statistics were used to examine the demographic data and to answer the study questions. T tests and chi-square tests were performed to compare nurse characteristics and questionnaire scores between the two groups of nurses. Spearman's rho correlations were calculated to test relationships between nurse characteristics and the questionnaire scores. A significance level of 0.05 was set for all analyses.
The transcribed qualitative data were entered into ATLAS.ti. Content analysis and thematic description (Hsieh & Shannon, 2005; Sandelowski, 2000) were used to identify and understand the meaning of EBP, show how EBP is operationalized, and show how EBP influences pain management on the inpatient unit. The investigator and a member of the research team read each transcript for the set of general themes generated by the nurses. Ideas and concepts were coded as they were communicated through passages or whole responses. A reflexive journal was kept to record the researchers' reactions to the data and examine biases. The emerging set of themes was discussed and used to develop a formal coding framework. Codes were generated from categories that arose from the data and were based on relevant literature and Rogers' (2003) diffusion of innovations model. Quotations exemplifying key themes were identified. The researchers compared individually assigned codes until agreement was obtained.
Results
Demographics
The final sample included 22 academic medical center nurses and 18 nurses from the community-based regional medical center (see Table 1). Four regional medical center nurses who completed questionnaires did not care for the patients whose medical records were reviewed as part of the larger study on barriers and facilitators to cancer-related, evidence-based pain management; these four nurses were not included in the final sample. Nurse demographics did not differ significantly by medical center except for (a) academic degree (p = 0.013), with more nurses with an associate degree in nursing at the regional medical center, and (b) part-time versus full-time employment (p = 0.033), with more nurses working part-time at the regional medical center.
Table 1. Sample Characteristics (N = 40).
| Characteristic | ¯X | Median | SD | Range |
|---|---|---|---|---|
|
| ||||
| Years in nursing practice | 6.8 | 4.6 | 5.9 | 1–30 |
|
| ||||
| Characteristic | n | |||
|
| ||||
| Gender | ||||
| Male | 3 | |||
| Female | 37 | |||
| Age (years) | ||||
| 20–40 | 25 | |||
| 41–50 | 9 | |||
| 51–60 | 6 | |||
| Ethnicity | ||||
| Caucasian | 35 | |||
| Asian | 3 | |||
| African American | 1 | |||
| Other | 1 | |||
| Years employed at workplace | ||||
| 1–2 | 8 | |||
| 3–5 | 19 | |||
| 6–10 | 12 | |||
| Longer than 10 | 1 | |||
| Employment status | ||||
| Full-time | 25 | |||
| Part-time | 15 | |||
| Oncology certified nurse | ||||
| Yes | 10 | |||
| No | 30 | |||
| Highest nursing degree | ||||
| Associate degree | 18 | |||
| Bachelor's degree | 22 | |||
Antecedents
The two groups' average scores were not significantly different for the EBP Beliefs Scale (t[38] = –0.43, p = 0.75), the EBP Implementation Scale (t[38] = 0.91, p = 0.37), or Carlson's Prior Conditions Instruments subscales–previous practices (t[38] = 0.06, p = 0.96); perceived existing needs or problems (t[38] = −0.29, p = 0.31), innovativeness (t[38] = 0.62, p = 0.49), and norms of the social system (t[38] = 0.56, p = 0.75) (see Table 2).
Table 2. Mean and Range of Scores for Quantitative Measures.
| Measure | AMC | CRMC | Combined | Range | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| ¯X | SD | ¯X | SD | ¯X | SD | ||
| EBP Beliefs Scale | 3.73 | 0.46 | 3.79 | 0.48 | 3.76 | 0.46 | 2.94-4.88 |
| EBP Implementation Scale | 1.74 | 0.83 | 1.55 | 0.45 | 1.65 | 0.68 | 1.11-5 |
| Carlson's Prior Conditions Instruments | |||||||
| Previous practices | 4.19 | 0.41 | 4.18 | 0.4 | 4.19 | 0.4 | 2.27-4.82 |
| Existing needs and problems | 3.4 | 0.72 | 3.27 | 0.7 | 3.34 | 0.71 | 1.86-4.57 |
| Innovativeness | 3.47 | 0.57 | 3.36 | 0.54 | 3.42 | 0.55 | 2.17-4.67 |
| Social system norms | 3.36 | 0.61 | 3.41 | 0.48 | 3.39 | 0.55 | 2.29-4.71 |
AMC—academic medical center; CRMC—community-based regional medical center; EBP—evidence-based practice
Both groups of nurses agreed with the positive aspects of EBP and their ability to implement it (¯X = 3.76, SD = 0.46), although their perceived level of EBP implementation was low (¯X = 1.65, SD = 0.68). The nurses supported adopting evidence-based pain management (¯X = 4.19, SD = 0.40) and were satisfied with their own pain management practices and that of others in their practice setting (¯X = 3.34, SD = 0.71). The nurses were sometimes or often innovative (¯X = 3.42, SD = 0.55) and were neutral about their social system being supportive of adopting evidence-based pain management practices (¯X = 3.39, SD = 0.55).
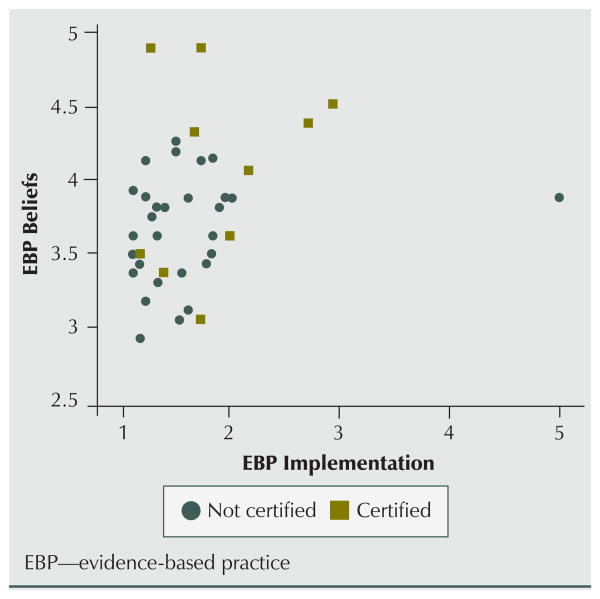
A significant association was found between Oncology Nursing Certification Corporation certification and innovativeness (r = 0.46, p = 0.003). Innovativeness also was associated with EBP beliefs (r = 0.48, p = 0.002). EBP beliefs were associated with nurses' perceived level of EBP implementation (r = 0.36, p = 0.02). Figure 2 shows the trend for more positive EBP beliefs and higher perceived EBP implementation among oncology certified nurses.
Figure 2. Scatter Plot of EBP Beliefs and Implementation Scores by Certification.
Themes
Four key themes emerged from the interviews related to EBP and evidence-based pain management.
Limited definition of evidence-based practice
The nurses' understood meaning of EBP reflected the definition of research utilization: the use of research findings in clinical practice (Melnyk & Fineout-Overholt, 2010). What was not included in their description of EBP was the integration of the best available research evidence with clinical expertise and patient values and preferences. The following response highlights the collective perception that the use of research improves patient outcomes.
So I guess that's something I haven't thought much about since school, but it just means to me that there have been a lot of studies done on a subject to find the … um I guess the most helpful way to do things and prevent bad outcomes like death and infection.
Varied evidence-based pain management decision making
Some nurses were unsure if they were delivering evidence-based pain management. Most did not describe a process that included integrating the best scientific evidence with clinical expertise and the patient's values and preferences. Interventions were not typically identified from published guidelines or research findings. The following responses explain the variety of evidence-based pain management decision-making processes.
Well, as a floor nurse, I think we rely heavily on our policies and what information is brought to me on education days by clinical nurse specialists. Um, I don't really individually seek out evidence-based practices to try to implement on my own.
So I guess when I am in a situation that I've been in before, I try whatever worked previously, which isn't necessarily completely evidence-based. If I've never been in the situation before, I would go to one of the more experienced nurses.
I'm choosing [evidence-based interventions] based on my experience more than anything else, primarily, and then the patient's experience secondary.
Limited identification of evidence-based pain management practices
A range of responses was elicited regarding identification of evidence-based pain management practices. Some nurses were unclear if a pain management policy and procedure existed. However, nurses were knowledgeable about policies and procedures for medication delivery systems. Pain management was commonly related to doctors' orders. Nurses at both medical centers were not clear if doctors' orders were always evidence-based, as described by the following responses.
Um, personally, I don't really know like what, like what I do that is evidence-based like as a nurse because I am just carrying out the doctor's notes.
Whether what we are doing is evidence-based when I'm there, I go off of orders. I don't go off and look it up, you know, but maybe I will go home later and look it up. You know, like was this a good thing to do?
Evidence-based pain management implementation requires nurses to rely on, ask, or collaborate with a doctor to order evidence-based pain management pharmacologic interventions or to adapt a pain management pharmacologic protocol. Evidence of collaboration existed, but most nurses relied on doctors' orders for implementing evidence-based pain management practices. The following response is an example of successful doctor-nurse collaboration after a nurse at the regional medical center learned about a new medication at a pharmaceutical-sponsored dinner.
Typically, [doctors] are well ahead of us on that. So if I bring it up they will address why they aren't doing it or they will do it, but they won't blow us off. So the constipation med I was telling you about, the medical team went to that and they started researching it and we started using that drug and it has been good for constipation secondary to narcotic use. They had been researching it on their own separately, so we ended up coming to the same conclusion.
Integration of nonpharmacologic interventions into patient care
The nurses described different processes for integrating nonpharmacologic interventions into patient care. Because most nonpharmacologic interventions do not require a doctor's order, nurses would independently implement them with patients.
I know that there are other ways to relieve pain than just, you know, for example narcotic pain medication, and to offer hot packs or cold packs or try to distract a patient sometimes works just as well, or can help narcotics work better and so I try to offer those things, especially if their current pain management system, what they're doing for pain management isn't working as well as it could.
Another implementation process involved collaboration with nurse colleagues to use the intervention with other patients on the unit.
If it was nonpharmacologic and something I could do without a doctor's orders, you know, I would, after reading the article or, you know, looking into it, I would probably consult with my fellow nurses, just to see or get their input and say, you know, “I found this and I thought it would work really well with our patient population, you know, would you like to help me try it or implement it?” and see how well it works for them.
Communication strategies were important in diffusing nonpharmacologic interventions on the nursing unit and throughout the regional medical center.
Um, usually I would bring it to the charge nurse first or the supervisors if it is something new that I am feeling like that would change, and then we kinda talk about it to see if it is something we can trial … and then if it is something more complex, we will send out an email to all the staff, um, and then we talk about it in huddle at the beginning of each shift. We'll talk about what it is we are trialing, or what it is we are wanting to, you know, kinda put it into plan and we will put it, make notes on the board as well. Um, and then we usually give it at least a week, and if it is going bad then we kinda cut it off, but if it seems to be working … then our manager usually presents that to the other managers, and I know we have adopted things that other floors have started.”
Discussion
The current study provides an understanding of nurses' perspectives regarding the antecedents to evidence-based pain management decision making through quantitative results illustrated with qualitative findings. The interview responses supported the quantitative findings and provided a richer understanding.
The nurses' understood meaning of EBP described research utilization. Although EBP often is considered to be synonymous with research utilization, the definition of EBP is broader because clinical decision making is based on the best available research evidence integrated with clinical expertise and patient values and preferences (Sackett et al., 1996). The nurses' understanding of EBP was not surprising because the focus of EBP initiatives is often on adopting practices based on the best scientific evidence rather than on the more nebulous integration of patient preferences and values with clinician expertise. When probed, the nurses stated that they considered patient preferences and clinical experience when making clinical decisions.
The nurses agreed with the positive aspects of EBP and their ability to implement it, although their perceived level of EBP implementation was low in the context of evidence-based pain management. Qualitative inquiry showed that the nurses let searching for and identifying evidence-based pain management strategies be the responsibility of others, including physicians and those responsible for developing the hospital's pain management policies and procedures. Because the mainstay of pain management is analgesic therapy, nurses relied on the medical team to ensure that the best practice was in place. Therefore, nurses did not critically appraise the scientific evidence or access evidence-based guidelines to find best practices for pharmacologic therapies for pain management. In addition, nurses trusted the unit's standards of care to be evidence-based.
Both hospitals had evidence-based policies and procedures, which nurses learn about at orientation and are expected to follow. Unfortunately, at the time of the interviews, some of the nurses were not clear whether a pain management policy and procedure existed or that these policies and procedures were indeed evidence-based. Nurses' knowledge of their healthcare organization's pain management policy has been reported to be significantly related to the individual nurse's knowledge of pain management and perceived accountability for pain management (Alley, 2001). This would be an important issue to explore further at both medical centers.
When pain management interventions were not successful in relieving pain, many nurses in the current study reported that they would seek another nurse to determine other interventions rather than considering an evidence-based clinical practice guideline or searching the literature. This has been previously supported in the literature (Pravikoff et al., 2005) and demonstrates the importance of unit culture in the practice of evidence-based pain management by nurses. This finding also illustrates the importance of the social system's communication strategies in diffusing pain management practices in the hospital setting.
The nurses independently integrated nonpharmacologic treatments into patient care. The qualitative findings indicated a difference between the two groups in collaborating with other healthcare professionals to integrate new pain management approaches. The academic medical center nurses did not describe sharing new treatments learned from journals or continuing education programs with their medical team. These nurses were employed by an EBP-focused organization, as evidenced by its Magnet® recognition status, where processes were in place to ensure best practice implementation (Stimpfel, Rosen, & McHugh, 2014). This may result in nurses not actively collaborating with the medical team when integrating new approaches into care.
As described by Rogers' (2003) diffusion of innovations model, innovations first are adopted by innovators; therefore, finding that perceived innovation was positively related to EBP beliefs was not unexpected. What was not expected was the trend for nurses with oncology certification to have more positive EBP beliefs and higher perceived EBP implementation than other nurses in the study. Although this finding needs further exploration through large-scale studies, the involvement of oncology certified nurses in the planning and implementation of evidence-based pain management initiatives in the inpatient oncology setting is worth considering.
Nursing Implications
Findings from the current study have important implications for nurse leaders in clinical and academic settings. Nurses value EBP and its importance to patient care, but their level of EBP implementation is low. In a busy clinical setting, finding and critically appraising the scientific evidence for best practices often is not practical. Evidence-based clinical practice guidelines and other resources are readily available for nurses on the Internet; however, to ensure evidence-based pain management practices among nurses, the best scientific evidence needs to be embedded in hospital pain management policies and procedures. Clinical nurse specialists and nurse educators are key people to develop these policies and procedures because of their training and expertise in EBP.
Although bedside nurses are not responsible for writing orders for pharmacologic interventions, they need to use critical thinking to ensure that the analgesic protocol is evidence-based. In addition, nurses need to collaborate with the healthcare team to identify other evidence-based interventions when current interventions are not successful in providing pain relief. Nurses also need to learn how to incorporate best scientific evidence with clinical expertise and patient values and preferences. These skills should be taught in nursing schools and reinforced in the clinical setting by clinical nurse specialists and educators through consultation, education, and mentorship.
Because nurses integrate nonpharmacologic pain management interventions into patient care, scientific evidence for many of these interventions needs to be further established through well-designed studies. This is an important realm of nursing care because nurses can independently implement these interventions for improving cancer pain management.
Limitations
Because of the small self-selected sample, caution should be taken in generalizing the findings of the current study to other healthcare settings or nurses. The use of self-reported data is an additional limitation. Because diffusion of an innovation takes place over time, a longitudinal study design will be required to describe the innovation diffusion process.
Conclusion
Through a mixed-methods approach, the current study provided a rich description of the antecedents to EBP decision making among two groups of nurses caring for patients with cancer pain. The current study allowed a detailed understanding of oncology nurses' perspectives regarding EBP. Insights gained should be considered when evaluating evidence-based pain management behaviors in healthcare organizations. The antecedents to EBP decision making need to be considered when developing a plan for improving evidence-based pain management. Making sustained evidence-based pain management a reality in the healthcare setting is essential for quality cancer care.
Knowledge Translation.
Nurses value evidence-based practice but often rely on physicians and advanced practice nurses to identify evidence-based pain management interventions.
To ensure evidence-based pain management practice by nurses, the best scientific evidence needs to be embedded in hospital pain management policies and procedures.
Additional scientific evidence for nonpharmacologic cancer pain management interventions is needed.
Acknowledgments
This study was supported, in part, by scholarships from the American Cancer Society (DSCN-12-201-01-SCN), the ONS Foundation, and the University of Washington. This study was also supported, in part, by an award from the National Institute of Nursing Research of the National Institutes of Health (R01NR012450, K24NR015340, and T32NR013456). Eaton can be reached at linda.eaton@nurs.utah.edu, with copy to editor at ONFEditor @ons.org.
Contributor Information
Linda H. Eaton, School of Nursing at the University of Washington in Seattle and a postdoctoral research fellow in the College of Nursing at the University of Utah in Salt Lake City.
Alexa R. Meins, School of Nursing at the University of Washington in Seattle.
Pamela H. Mitchell, School of Nursing at the University of Washington in Seattle.
Joachim Voss, School of Nursing at the University of Washington in Seattle.
Ardith Z. Doorenbos, School of Nursing at the University of Washington in Seattle.
References
- Aiello-Laws LB, Ameringer SW. Oncology Nursing Society Putting Evidence Into Practice resource: Pain. In: Eaton L, Tip-ton J, editors. Putting Evidence Into Practice: Improving oncology patient outcomes. Pittsburgh, PA: Oncology Nursing Society; 2009. pp. 215–230. [Google Scholar]
- Alley LG. The influence of an organizational pain management policy on nurses' pain management practices. Oncology Nursing Forum. 2001;28:867–874. [PubMed] [Google Scholar]
- Austin MJ, Claassen J. Implementing evidence-based practice in human service organizations: Preliminary lessons from the frontlines. Journal of Evidence-Based Social Work. 2008;5:271–293. doi: 10.1300/J394v05n01_10. [DOI] [PubMed] [Google Scholar]
- Bell L, Duffy A. Pain assessment and management in surgical nursing: A literature review. British Journal of Nursing. 2009;18:153–156. doi: 10.12968/bjon.2009.18.3.39042. [DOI] [PubMed] [Google Scholar]
- Brown CE, Wickline MA, Ecoff L, Glaser D. Nursing practice, knowledge, attitudes and perceived barriers to evidence based practice at an academic medical center. Journal of Advanced Nursing. 2009;65:371–381. doi: 10.1111/j.1365-2648.2008.04878.x. [DOI] [PubMed] [Google Scholar]
- Carlson C. Development and testing of four instruments to assess prior conditions that influence nurses' adoption of evidence based pain management practices. Journal of Advanced Nursing. 2008;64:632–643. doi: 10.1111/j.1365-2648.2008.04833.x. [DOI] [PubMed] [Google Scholar]
- Chang VT, Hwang SS, Kasimis B. Longitudinal documentation of cancer pain management outcomes: A pilot study at a VA medical center. Journal of Pain and Symptom Management. 2002;24:494–505. doi: 10.1016/S0885-3924(02)00516-X. [DOI] [PubMed] [Google Scholar]
- Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH, Stewart JA, Pandya KJ. Pain and its treatment in outpatients with metastatic cancer. New England Journal of Medicine. 1994;330:592–596. doi: 10.1056/NEJM199403033300902. [DOI] [PubMed] [Google Scholar]
- Deandrea S, Montanari M, Moja L, Apolone G. Prevalence of undertreatment in cancer pain. A review of published literature. Annals of Oncology. 2008;19:1985–1991. doi: 10.1093/annonc/mdn419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dray A. New drugs for cancer pain relief. In: Paice JA, Bell RF, Kalso EA, Soyannwo OA, editors. Cancer pain: From molecules to suffering. Seattle, WA: International Association for the Study of Pain; 2010. pp. 173–188. [Google Scholar]
- Estabrooks CA, Scott S, Squires JE, Stevens B, O'Brien-Pallas L, Watt-Watson J, Williams J. Patterns of research utilization on patient care units. Implementation Science. 2008;3:31. doi: 10.1186/1748-5908-3-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green E, Zwaal C, Beals C, Fitzgerald B, Harle I, Jones J, Wiernikowski J. Cancer-related pain management: A report of evidence-based recommendations to guide practice. Clinical Journal of Pain. 2010;26:449–462. doi: 10.1097/AJP.0b013e3181dacd62. [DOI] [PubMed] [Google Scholar]
- Herr K, Titler M, Fine PG, Sanders S, Cavanaugh JE, Swegle J, Forcucci C. The effect of a translating research into practice (TRIP)—Cancer intervention on cancer pain management in older adults in hospice. Pain Medicine. 2012;13:1004–1017. doi: 10.1111/j.1526-4637.2012.01405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Idell CS, Grant M, Kirk C. Alignment of pain reassessment practices and National Comprehensive Cancer Network guidelines. Oncology Nursing Forum. 2007;34:661–671. doi: 10.1188/07.ONF.661-671. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Leadership commitments to improve value in healthcare: Finding common ground: Workshop summary. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- Lauzon Clabo LM. An ethnography of pain assessment and the role of social context on two postoperative units. Journal of Advanced Nursing. 2008;61:531–539. doi: 10.1111/j.1365-2648.2007.04550.x. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Fineout-Overholt E. Evidence-based practice in nursing and healthcare: A guide to best practice. 2nd. Philadelphia, PA: Lippincott Williams and Wilkins; 2010. [Google Scholar]
- Melnyk BM, Fineout-Overholt E, Fischbeck Feinstein N, Li H, Small L, Wilcox L, Kraus R. Nurses' perceived knowledge, beliefs, skills, and needs regarding evidence based practice: Implications for accelerating the paradigm shift. World views on Evidence-Based Nursing. 2004;1:185–193. doi: 10.1111/j.1524-475X.2004.04024.x. doi:10.1111/j.1524 -475X.2004.04024.x. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Fineout-Overholt E, Gallagher-Ford L, Kaplan L. The state of evidence-based practice in US nurses: Critical implications for nurse leaders and educators. Journal of Nursing Administration. 2012;42:410–417. doi: 10.1097/NNA.0b013e3182664e0a. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Fineout-Overholt E, Giggleman M, Cruz R. Correlates among cognitive beliefs, EBP implementation, organizational culture, cohesion and job satisfaction in evidence-based practice mentors from a community hospital system. Nursing Outlook. 2010;58:301–308. doi: 10.1016/j.outlook.2010.06.002. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Fineout-Overholt E, Mays MZ. The Evidence-Based Practice Beliefs and Implementation Scales: Psychometric properties of two new instruments [published erratum appears in Worldviews on Evidence-Based Nursing, 6, 49] Worldviews on Evidence-Based Nursing. 2008;5:208–216. doi: 10.1111/j.1741-6787.2008.00126.x. doi:10.1111/j.1741 -6787.2008.00126.x. [DOI] [PubMed] [Google Scholar]
- Pepler CJ, Edgar L, Frisch S, Rennick J, Swidzinski M, White C, Gross J. Unit culture and research-based nursing practice in acute care. Canadian Journal of Nursing Research. 2005;37:66–85. [PubMed] [Google Scholar]
- Pravikoff DS, Tanner AB, Pierce ST. Readiness of U.S. nurses for evidence-based practice. American Journal of Nursing. 2005;105(9):40–51. doi: 10.1097/00000446-200509000-00025. [DOI] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of innovations. 5th. New York, NY: Free Press; 2003. [Google Scholar]
- Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: What it is and what it isn't. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuels JG. The application of high-reliability theory to promote pain management. Journal of Nursing Administation. 2010;40:471–476. doi: 10.1097/NNA.0b013e3181f88a41. [DOI] [PubMed] [Google Scholar]
- Samuels JG, Fetzer S. Pain management documentation quality as a reflection of nursing judgment. Journal of Nursing Care Quality. 2009;24:223–231. doi: 10.1097/NCQ.0b013e318194fcec. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Focus on research methods: Whatever happened to qualitative description? Research in Nursing and Health. 2000;23:334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. doi:10.1002/1098-240X(200008)23:4<334::AID -NUR9>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Scott SD, Pollock C. The role of nursing unit culture in shaping research utilization behaviors. Research in Nursing and Health. 2008;31:298–309. doi: 10.1002/nur.20264. [DOI] [PubMed] [Google Scholar]
- Squires JE, Estabrooks CA, Gustavsson P, Wallin L. Individual determinants of research utilization by nurses: A systematic review update. Implementation Science. 2011;6:1. doi: 10.1186/1748-5908-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stimpfel AW, Rosen JE, McHugh MD. Understanding the role of the professional practice environment on quality of care in Magnet® and non-Magnet hospitals. Journal of Nursing Administration. 2014;44:10–16. doi: 10.1097/NNA.0000000000000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. Prevalence of pain in patients with cancer: A systematic review of the past 40 years. Annals of Oncology. 2007;18:1437–1449. doi: 10.1093/annonc/mdm056. [DOI] [PubMed] [Google Scholar]
- Wild LR, Mitchell PH. Quality pain management outcomes: The power of place. Outcomes Management for Nursing Practice. 2000;4:136–143. [PubMed] [Google Scholar]
- Wilson B. Nurses' knowledge of pain. Journal of Clinical Nursing. 2007;16:1012–1020. doi: 10.1111/j.1365-2702.2007.01692.x. [DOI] [PubMed] [Google Scholar]