Abstract
Spontaneous cerebrospinal fluid (CSF) leaks in the sphenoid sinus are an uncommon but potentially significant condition associated with thin pneumatised bone, obesity and raised intracranial pressure. Despite advances in endoscopic sinus surgery, successful repair remains problematic due to limitations in visualisation, access and management of underlying aetiological factors. Utilisation of vascularised tissue in the primary repair process of sphenoid CSF leaks is yet to be well explored in the literature. In this series, we describe our surgical approach and explore related clinical, pathological and operative factors in three cases of spontaneous sphenoid sinus CSF leaks, successfully repaired on first attempt with the use of a vascularised nasoseptal flap.
Background
Cerebrospinal fluid (CSF) leakage results from a defect compromising the duro-osteomucosal integrity of the skull base. It is of spontaneous aetiology if unrelated to trauma, surgery, malformation, tumour or radiotherapy, and may be associated with a current or previous history of benign intracranial hypertension (BIH).1 Without intervention, 10% of patients are at risk of developing meningitis annually and up to 40% in the long term.2 Accordingly, surgical repair is the preferred form of management.
Endonasal endoscopic techniques have revolutionised the management of CSF leaks, with success rates of 90% or greater reported.1 3 However, in the subset of spontaneous CSF leaks, equivalent outcomes have not been consistently demonstrated, with recurrence rates of 25–87% reported over time.4–7 Furthermore, CSF leaks of sphenoid origin, particularly if located in the lateral recess of a well-pneumatised sinus, remain technically challenging to repair due to limitations in exposure and access.8 Traditional repair techniques include fat obliteration of the sphenoid sinus, and single-layer and multilayer grafting.
The nasoseptal flap (NSF) is a mucoperiosteum and mucoperichondrium graft pedicled on the posterior nasoseptal artery and represents a significant advance in the evolution of endoscopic CSF leak repair techniques, with high success rates reported.9–12 However, the use of the NSF in the repair of spontaneous CSF leaks of the sphenoid sinus is not widely reported.8 13 In this case series, we describe our experience in managing spontaneous sphenoid CSF leaks in three patients, with deployment of the NSF as the means of primary endoscopic repair.
Case presentation
Case 1
A 48-year-old woman presented with rhinorrhoea and postnasal drip, with a positive β2-transferrin test, indicating a CSF origin. There was no history of trauma or iatrogenic insult. CT demonstrated two discrete areas of dehiscence over the right posterior and right lateral sphenoid. MRI was attempted to exclude any intracranial pathology but could not be performed due to the patient's weight and body habitus. Upright MRI was also unsuccessful.
Case 2
A 60-year-old man was referred following an episode of Haemophilus meningitis. CT had demonstrated breach of the left lateral sphenoid wall. The patient reported intermittent clear nasal discharge present for a number of years, but denied head trauma or previous surgical treatment of the skull. Repeat CT confirmed the left sphenoid bony defect and T2-weighted MRI demonstrated a meningocoele (figure 1).
Figure 1.
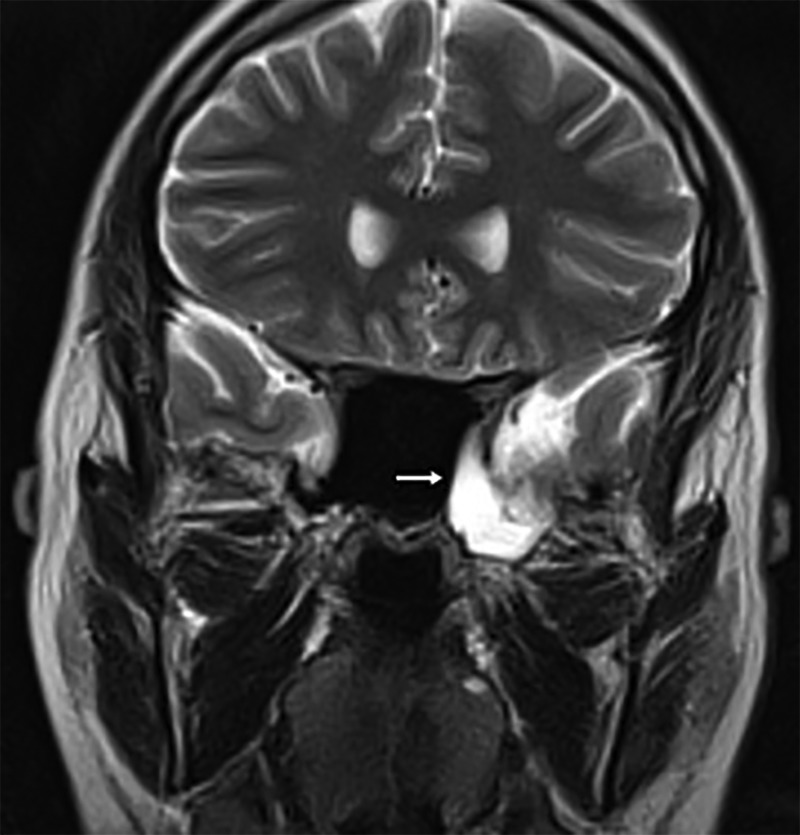
Preoperative coronal T2-weighted MRI demonstrating a left lateral sphenoid meningocoele (Case 2) (arrow).
Case 3
A 36-year-old woman presented with left CSF rhinorrhoea confirmed with a positive β2-transferrin test of nasal discharge. She denied any history of trauma to the skull or iatrogenic insults. CT scan (figure 2) and MRI demonstrated a dehiscence in the lateral wall of the left sphenoid.
Figure 2.
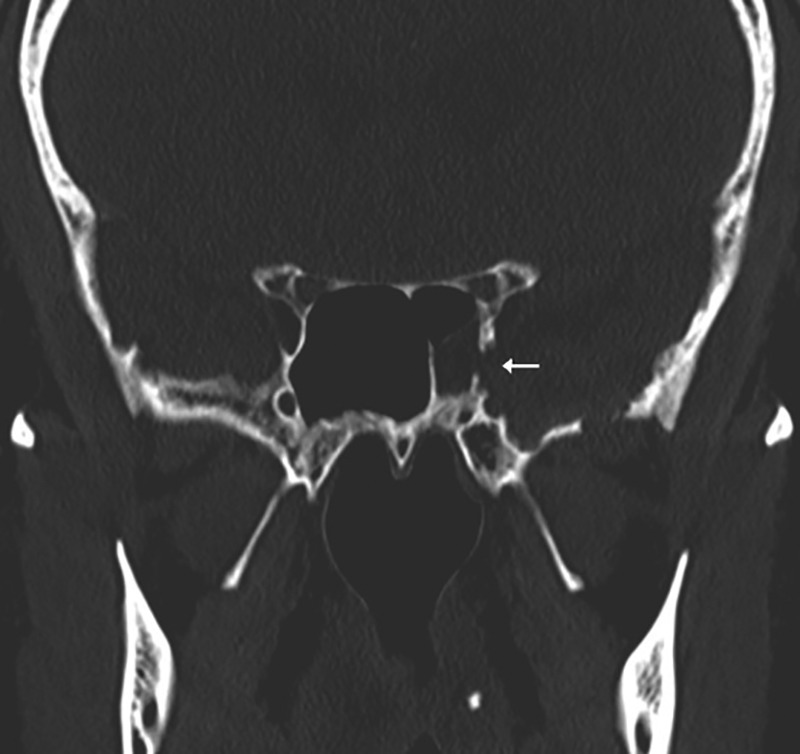
Preoperative coronal CT scan demonstrating a bony defect at the lateral extension of the left sphenoid sinus (Case 2) (arrow).
Treatment
Primary surgical repair was undertaken in all three cases. Prior to the induction of general anaesthesia, lumbar puncture was performed for measurement of ICP and a lumbar drain (Epidural Minipack System 1; Smiths Medical Australasia, Queensland, Australia) was placed. Diluted fluorescein was administered intrathecally and intravenously for defect localisation.14 A locally developed blue light filter was used intraoperatively to enhance visualisation of fluorescein-stained CSF.15 Patients were consented regarding the off-label use of fluorescein.
An endonasal endoscopic technique with image guidance (StealthStation S7, Medtronic, Minnesota, USA) was utilised in all cases. NSFs were harvested as described by Hadad et al9 and stored within the nasopharynx.10 This technique involves parallel horizontal incisions of the nasal septum, inferiorly over the maxillary crest and superiorly 1–2 cm below the superior most aspect of the septum. A vertical incision joins these anteriorly. Posteriorly, the superior horizontal incision is extended inferolaterally over the sphenoid rostrum and the inferior incision is extended superolaterally to cross the posterior choana. Dimensions of the NSF should match those of the anticipated defect with slight overestimation. The NSF is elevated in an anterior to posterior manner with careful preservation of the posterolateral neurovascular pedicle.
Complete sphenoethmoidectomy was then performed for wide skull base exposure. A transpterygoid approach as described by Bolger and Osenbach16 was undertaken for defects located within the lateral recess of a well-pneumatised sinus; however, our technique did not involve sphenopalatine artery ligation. This approach entails formation and posterior extension of the middle meatal antrostomy. The posterior wall of the maxillary sinus is removed to expose the pterygopalatine fossa. This anatomic region is carefully dissected, and traversed with preservation and retraction of the internal maxillary artery and its sphenopalatine artery branch. The anterior wall of the well-pneumatised sphenoid sinus is then removed to expose the sphenoid sinus leak site laterally.
Following CSF leak site identification, adjacent mucosa was stripped to expose the osseous defect. Gentle pressure was applied in an attempt to reduce herniated tissue. For large volume or irreducible sacs, bipolar diathermy (Stammberger suction-bipolar, Karl Storz, Tutulingen, Germany) was used for excision. Repair was performed with collagen matrix (DuraGen) subdurally and middle turbinate bone or septal bone/cartilage extradurally (underlay); NSF (overlay); 3–10 mL of fibrin sealant (Tisseel, Baxter, Illinois, USA) and oxidised cellulose polymer (Surgicel Fibrillar, Ethicon, New Jersey, USA). A 0.5 mm silastic splint (Medtronic, North Ryde, New South Wales, Australia) was sutured over the denuded septal cartilage and bone, and left in place for 6 weeks. A Foley catheter balloon was not used to support the NSF.
Postoperatively, the lumbar drain was left in situ for 5 days, clamped for 24 h, and then removed. Strict bed rest, 30° head-up positioning and avoidance of straining was advised for 1 week with a further 6 weeks of no lifting or straining. Patients were reviewed endoscopically at 2, 6 and 12 weeks postoperatively and variably thereafter.
Outcome and follow-up
Patients’ clinical, pathological and operative data are outlined in table 1. In case 1, bilateral NSFs were raised to ensure complete coverage of the dual defects. In case 3, the CSF leak was situated in the lateral recess of a well-pneumatised cavity and required a transpterygoid approach (figure 3).
Table 1.
Patients’ clinical, pathological and operative data
| Case/sex | Age (year) | BMI (kg/m2) | Clinical presentation | ICP (cm H2O) | Leak site and size | Approach | Repair | Pathology | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1/F | 49 | 66.5 | Rhinorrhoea | 15 | R posterior (3 mm) | TS | DuraGen, septal cartilage, bilateral NSF | Encephalocoele | 40 |
| R lateral (4 mm) | Encephalocoele | ||||||||
| 2/M | 59 | 28.4 | Meningitis | 15 | L lateral (15 mm) | TS | DuraGen, septal cartilage, NSF | Meningocoele | 27 |
| 3/F | 34 | 29.3 | Rhinorrhoea | 8 | L lateral Recess (5 mm) | TP | DuraGen, middle turbinate bone, NSF | Encephalocoele | 23 |
F, female; ICP, intracranial pressure; L, left; M, male; NSF, nasoseptal flap; R, right; TP, transpterygoid approach; TS, transethmoidal–sphenoidal approach.
Figure 3.
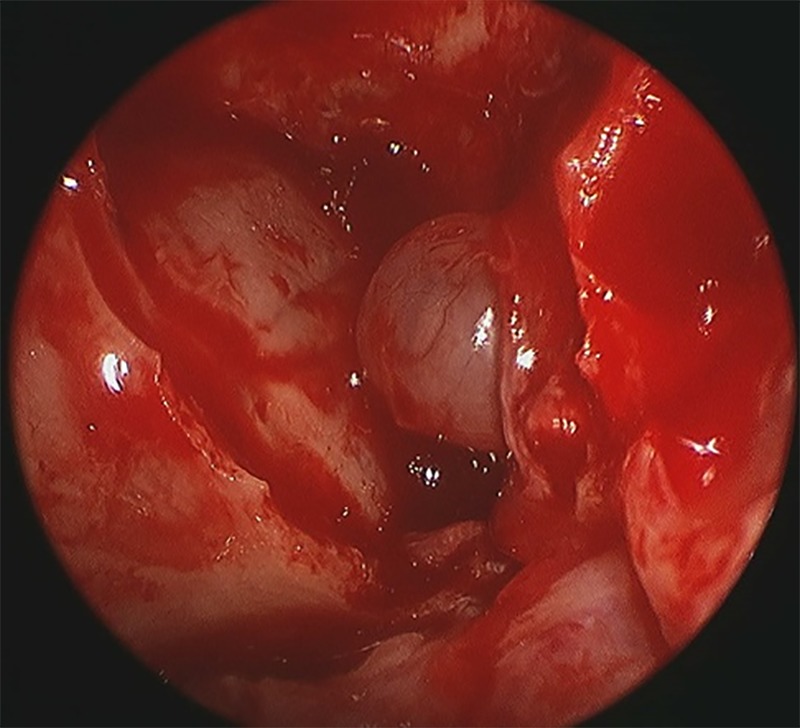
Transpterygoid endoscopic view of a meningocoele protruding from the lateral recess of the left sphenoid sinus (Case 2).
Case 1 had a prolonged postoperative course as sequelae of her morbid obesity. This included admission to the intensive care unit and reintubation for respiratory failure, surgical tracheostomy, continuous positive airway pressure for obstructive sleep apnoea, pacemaker insertion for arrhythmia and intravenous antibiotics for a methicillin-resistant Staphylococcus aureus chest infection. She ultimately made a good recovery and was decannulated and returned home. The postoperative courses of cases 2 and 3 were unremarkable.
CSF leaks in all three cases of this series were treated successfully on first attempt, without subsequent recurrence (100% success rate). The mean duration of follow-up was 30 months (range of follow-up 23–40 months).
Discussion
Endonasal endoscopic techniques have increasingly replaced transcranial and open extracranial approaches in the management of spontaneous sphenoid sinus CSF leaks. Advantages include minimal invasiveness and superior cosmesis, improved visualisation and access, shortened operative time, length of stay and recovery period, and avoidance of frontal or temporal lobe retraction and associated anosmia, cerebral contusion and memory deficit.2
Despite disappointing early outcomes, recent series have reported closure rates of 88.9–93.3%, comparable to those of non-spontaneous CSF leaks.5 17 18 These accomplishments reflect superior understanding and management of underlying aetiological factors, and innovations in endoscopic surgery. However, these authors detail the use of only multilayer grafting with autologous and synthetic materials, or fat obliteration of the sphenoid sinus for laterally located and inaccessible CSF leaks. Fat obliteration may compromise postoperative radiographic surveillance and has been associated with delayed mucocoele formation.19 Recurrence of CSF leaks in these series were attributed to inadequate management of underlying BIH,5 lateral sphenoid recess locality17 and multiple previous attempts at repair.18
The NSF was originally described in the reconstruction of large dural defects following skull base surgery,9 but has proven useful in other settings.10–12 Its vascular pedicle clearly defines the arterial supply, providing reliability, versatility and mobility of the flap in multiple planes. The NSF provides a base of healthy mucosa that is expected to remucosalise over a non-vascularised graft through epithelial cell migration.12 Despite its increasing popularity and success in endoscopic skull base surgery, no series has detailed exclusive employment of the NSF as a primary surgical means of managing spontaneous CSF leaks of the sphenoid sinus. Vaezi et al13 described successful NSF repair of three spontaneous sphenoid pseudomeningocoeles in two patients, one of whom had undergone prior unsuccessful attempts at repair with non-vascularised grafts through intracranial and endonasal endoscopic approaches.14 Alexander et al8 reported successful NSF use as a salvage technique following failed initial multilayer graft closure for a defect occupying the lateral recess. As such, our series is the first to focus on primary NSF repair in spontaneous sphenoid sinus CSF leaks. Some concerns have been expressed regarding olfactory impairment following high-septal NSF harvest;12 however, this has been demonstrated to be uncommon and no such complications were noted in our series.
Spontaneous CSF fistulae are associated with the highest rate of encephalocoele formation (50–100%).5 20 In our series, 75% of defects occurred concurrently with encephalocoeles. Although early literature documented only isolated case reports and small case series of encephalocoeles occupying the lateral recess of a well-pneumatised sphenoid,18 more recent data has demonstrated this locality to be the most commonly encountered and associated with spontaneous encephalocoele formation.5 17 The lateral sphenoid constituted 75% of our repair sites, however, only one defect was situated within a well-pneumatised lateral recess. The transpterygoid approach permitted access to and repair of the CSF fistula in this locality.
Obesity and raised ICP have been associated with the development of spontaneous CSF fistulae. In our series, all patients were overweight and one was morbidly obese, consistent with BMI findings of other authors.5 18 20 Excess weight increases intra-abdominal and intrathoracic pressure and is suspected to impair circulation in cranial venous collectors potentiating permanent BIH.17 21 22 Over time, constant pulsatile pressure applied to the skull base ultimately results in erosion, especially in regions of thin pneumatised bone such as that which occupies the lateral recess of the sphenoid.20 Quantification of ICP can be ascertained through measurement of opening pressure on lumbar puncture (normal 5–15 cm H2O),20 or through continuous monitoring via a lumbar drain in the postoperative period.5 In our series, opening pressure remained within normal parameters in all cases and ranged from 8 to 15 cm H2O, as expected, in the setting of concurrent CSF leak. In contrast, Illing et al20 reported an elevated ICP in 95% of their 59 patients with spontaneous CSF leaks of the lateral sphenoid recess (mean ICP 27.7±8.2 cm H2O). However, their data combined preoperative and postoperative measurements, which may account for the variation in their results from our own. Failure to address underlying BIH through medical and surgical intervention may result in recurrence of CSF leaks at the location of repair and additional distant sites.5
In conclusion, the NSF is an effective and reliable technique for the primary closure of spontaneous sphenoid sinus CSF leaks and compares favourably with traditional techniques including multilayer grafting and free fat graft obliteration.
Learning points.
Repair of spontaneous cerebrospinal fluid (CSF) leaks of the sphenoid sinus can be technically challenging due to difficulties with visualisation and access.
Traditional techniques of endoscopic repair with free fat obliteration, and single and multilayer grafting, have produced mixed results.
The NSF represents an effective alternative with utility in primary and salvage surgical therapy of spontaneous sphenoid sinus CSF leaks.
Footnotes
Contributors: DAG was responsible for data collection and manuscript preparation. NPS was responsible for manuscript preparation.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hegazy HM, Carrau RL, Snyderman CH et al. Transnasal endoscopic repair of cerebrospinal fluid rhinorrhea: a meta-analysis. Laryngoscope 2000;110:1166–72. 10.1097/00005537-200007000-00019 [DOI] [PubMed] [Google Scholar]
- 2.Alonso RC, de la Pena MJ, Caicoya AG et al. Spontaneous skull base meningoencephaloceles and cerebrospinal fluid fistulas. Radiographics 2013;33:553–70. 10.1148/rg.332125028 [DOI] [PubMed] [Google Scholar]
- 3.Schick B, Ibing R, Brors D et al. Long-term study of endonasal duraplasty and review of the literature. Ann Oto Rhinol Laryngol 2001;110:142–7. 10.1177/000348940111000209 [DOI] [PubMed] [Google Scholar]
- 4.Hubbard JL, McDonald TJ, Pearson BW et al. Spontaneous cerebrospinal fluid rhinorrhea: evolving concepts in diagnosis and surgical management based on the Mayo Clinic experience from 1970 through 1981. Neurosurgery 1985;16:314–21. 10.1227/00006123-198503000-00006 [DOI] [PubMed] [Google Scholar]
- 5.Woodworth BA, Prince A, Chiu AG et al. Spontaneous CSF leaks: a paradigm for definitive repair and management of intracranial hypertension. Otolaryngol Head Neck Surg 2008;138:715–20. 10.1016/j.otohns.2008.02.010 [DOI] [PubMed] [Google Scholar]
- 6.Schlosser RJ, Bolger WE. Significance of empty sella in cerebrospinal fluid leaks. Otolaryngol Head Neck Surg 2003;128:32–8. 10.1067/mhn.2003.43 [DOI] [PubMed] [Google Scholar]
- 7.Schlosser RJ, Wilensky EM, Grady MS et al. Elevated intracranial pressures in spontaneous cerebrospinal fluid leaks. Am J Rhinol 2003;17:191–5. [PubMed] [Google Scholar]
- 8.Alexander NS, Chaaban MR, Riley KO et al. Treatment strategies for lateral sphenoid sinus recess cerebrospinal fluid leaks. Arch Otolaryngol Head Neck Surg 2012;138:471–8. 10.1001/archoto.2012.614 [DOI] [PubMed] [Google Scholar]
- 9.Hadad G, Bassagasteguy L, Carrau RL et al. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope 2006;116:1882–6. 10.1097/01.mlg.0000234933.37779.e4 [DOI] [PubMed] [Google Scholar]
- 10.Kassam AB, Thomas A, Carrau RL et al. Endoscopic reconstruction of the cranial base using a pedicled nasoseptal flap. Neurosurgery 2008;63(1 Suppl 1):ONS44–52; discussion ONS52–43 10.1227/01.NEU.0000297074.13423.F5 [DOI] [PubMed] [Google Scholar]
- 11.Wheless SA, McKinney KA, Carrau RL et al. Nasoseptal flap closure of traumatic cerebrospinal fluid leaks. Skull Base 2011;21:93–8. 10.1055/s-0030-1266763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El-Sayed IH, Roediger FC, Goldberg AN et al. Endoscopic reconstruction of skull base defects with the nasal septal flap. Skull Base 2008;18:385–94. 10.1055/s-0028-1096202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vaezi A, Snyderman CH, Saleh HA et al. Pseudomeningoceles of the sphenoid sinus masquerading as sinus pathology. Laryngoscope 2011;121:2507–13. 10.1002/lary.21876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seth R, Rajasekaran K, Benninger MS et al. The utility of intrathecal fluorescein in cerebrospinal fluid leak repair. Otolaryngol Head Neck Surg 2010;143:626–32. 10.1016/j.otohns.2010.07.011 [DOI] [PubMed] [Google Scholar]
- 15.Singh NP, Roberts DN. An inexpensive blue filter for fluorescein-assisted repair of cerebrospinal fluid rhinorrhea. Laryngoscope 2014;124:1103–5. 10.1002/lary.24502 [DOI] [PubMed] [Google Scholar]
- 16.Bolger W, Osenbach R. Endoscopic transpterygoid approach to the lateral sphenoid recess. Ear Nose Throat J 1999;78:36–46. [Google Scholar]
- 17.Lopatin AS, Kapitanov DN, Potapov AA. Endonasal endoscopic repair of spontaneous cerebrospinal fluid leaks. Arch Otolaryngol Head Neck Surg 2003;129:859–63. 10.1001/archotol.129.8.859 [DOI] [PubMed] [Google Scholar]
- 18.Lai SY, Kennedy DW, Bolger WE. Sphenoid encephaloceles: disease management and identification of lesions within the lateral recess of the sphenoid sinus. Laryngoscope 2002;112:1800–5. 10.1097/00005537-200210000-00018 [DOI] [PubMed] [Google Scholar]
- 19.Citardi MJ, Cox AJ III, Bucholz RD. Acellular dermal allograft for sellar reconstruction after transsphenoidal hypophysectomy. Am J Rhinol 2000;14:69–73. 10.2500/105065800781602920 [DOI] [PubMed] [Google Scholar]
- 20.Illing E, Schlosser RJ, Palmer JN et al. Spontaneous sphenoid lateral recess cerebrospinal fluid leaks arise from intracranial hypertension, not Sternberg's canal. Int Forum Allergy Rhinol 2014;4:246–50. 10.1002/alr.21262 [DOI] [PubMed] [Google Scholar]
- 21.Badia L, Loughran S, Lund V. Primary spontaneous cerebrospinal fluid rhinorrhea and obesity. Am J Rhinol 2001;15:117–19. 10.2500/105065801781543736 [DOI] [PubMed] [Google Scholar]
- 22.Clark D, Bullock P, Hui T et al. Benign intracranial hypertension: a cause of CSF rhinorrhoea. J Neurol Neurosurg Psychiatry 1994;57:847–9. 10.1136/jnnp.57.7.847 [DOI] [PMC free article] [PubMed] [Google Scholar]


