Abstract
Background
Congenital heart defects (CHDs) occur in approximately 8 per 1000 live births. Improvements in detection and treatment have increased survival. Few national estimates of the healthcare costs for infants, children and adolescents with CHDs are available.
Methods
We estimated hospital costs for hospitalizations using pediatric (0–20 years) hospital discharge data from the 2009 Healthcare Cost and Utilization Project Kids’ Inpatient Database (KID) for hospitalizations with CHD diagnoses. Estimates were up-weighted to be nationally representative. Mean costs were compared by demographic factors and presence of critical CHDs (CCHDs).
Results
Up-weighting of the KID generated an estimated 4,461,615 pediatric hospitalizations nationwide, excluding normal newborn births. The 163,980 (3.7%) pediatric hospitalizations with CHDs accounted for approximately $5.6 billion in hospital costs, representing 15.1% of costs for all pediatric hospitalizations in 2009. Approximately 17% of CHD hospitalizations had a CCHD, but it varied by age: approximately 14% of hospitalizations of infants, 30% of hospitalizations of patients aged 1 to 10 years, and 25% of hospitalizations of patients aged 11 to 20 years. Mean costs of CHD hospitalizations were higher in infancy ($36,601) than at older ages and were higher for hospitalizations with a CCHD diagnosis ($52,899). Hospitalizations with CCHDs accounted for 26.7% of all costs for CHD hospitalizations, with hypoplastic left heart syndrome, coarctation of the aorta, and tetralogy of Fallot having the highest total costs.
Conclusion
Hospitalizations for children with CHDs have disproportionately high hospital costs compared with other pediatric hospitalizations, and the 17% of hospitalizations with CCHD diagnoses accounted for 27% of CHD hospital costs.
Keywords: heart defects, congenital, healthcare resource use, hospital costs, Kids’ Inpatient Database
Introduction
Congenital heart defects (CHDs) are the most common birth defect and are estimated to affect almost 1% of infants born in the United States (Reller et al., 2008). Approximately 25% of newborns with CHDs have critical CHDs (CCHDs) (Botto et al., 2001; Mahle et al., 2009). CCHDs are a subset of CHDs that require surgical or trans-catheter intervention before one year of age and are amenable to detection using pulse oximetry screening (Mahle et al., 2009; Kemper et al., 2011). Improvements in CHD detection and treatment have increased life expectancy among infants and children (Williams et al., 2006; Marelli et al., 2007; Oster et al., 2013a). Many individuals with CHD of all ages will require lifelong care for these conditions. However, little is known about the healthcare needs of children and adolescents with CHDs or the impact of this population on hospital resource use.
Health services research, including costs of care, has been identified as a public health priority (Oster et al., 2013b). Rising health care costs underscore the need to provide efficient and effective care. A better understanding of the overall costs of care for CHDs and CCHDs in children and adolescents may help identify high cost surgical or medical healthcare needs in this population and identify the specific major contributors to overall CHD costs. (Oster et al., 2013b). Previous studies have identified CHDs having high cost hospitalizations. Hospitalizations among neonates discharged in 2003 with any of 35 selected birth defects showed high hospital charges for several CHDs (hypoplastic left heart syndrome, truncus arteriosus, transposition of the great arteries, and coarctation of the aorta) compared with other birth defects (Centers for Disease Control and Prevention, 2007). Reports detailing CHD hospital resource use have generally focused on the first year of life and have found high hospital costs for this population (Connor et al., 2005; Centers for Disease Control and Prevention, 2007; Peterson et al., 2013). Few studies have evaluated hospital costs after 1 year of life or into childhood and adolescence (Connor et al., 2005; Russo and Elixhauser, 2007; Opotowsky et al., 2009; O’Leary et al., 2013). Specifically, current hospital resource use for individuals with CCHDs is not well known. To address these gaps we analyzed data from the 2009 Agency for Healthcare Research and Quality (AHRQ) Kids’ Inpatient Database (KID) (Agency for Healthcare Research and Quality, 2011b) to estimate hospital costs of U.S. pediatric hospitalizations with CHD diagnoses. We quantified CHD hospital costs among children and adolescents and also examined costs by specific CCHD type.
Materials and Methods
STUDY DESIGN AND DATA SOURCE
The KID is an all-payer inpatient administrative database maintained by AHRQ’s Healthcare Cost and Utilization Project (HCUP) (Agency for Healthcare Research and Quality, 2011b,c). The 2009 KID is a stratified random sample of all hospital discharges from almost all non-Federal short-term, community-based hospitals from 44 participating states within HCUP’s sampling frame (Agency for Health-care Research and Quality, 2011c). The KID includes a 10% sample of all normal newborn discharges and an 80% sample of all other discharges of patients ≤20 years old from all sampling frame hospitals (Agency for Health-care Research and Quality, 2011c). KID data are provided at the hospital discharge level. Each observation represents one patient hospitalization; identifiable information is removed from the discharge summary by HCUP and hospitalizations cannot be linked to individual patients. Each discharge includes up to 25 International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) discharge diagnosis codes, demographic data, expected payer, hospital charges, and discharge disposition (routine, transferred, died in the hospital, etc.). Sample weights provided by HCUP allowed weighted data to be used to generate national estimates (Agency for Healthcare Research and Quality, 2011c). This study used de-identified data; this analysis was determined not to be human subjects research and exempt from IRB review.
STUDY POPULATION AND CASE INCLUSION CRITERIA
We included hospital discharges occurring January 1 to December 31, 2009 of patients ≤20 years of age with principal or secondary diagnosis codes indicating a CHD (ICD-9-CM codes 745.0–747.49). CHD hospitalizations were categorized as CCHD and noncritical CHD. CCHDs included 12 primary and secondary targets of universal screening for CHDs using pulse oximetry (Mahle et al., 2009; Kemper et al., 2011; Oster et al., 2013a). The primary targets (ICD-9-CM codes) were hypoplastic left heart syndrome (HLHS) (746.7), pulmonary atresia (746.01), tetralogy of Fallot (745.2), total anomalous pulmonary venous return (747.41), transposition of the great arteries (745.10), tricuspid atresia (746.1), and truncus arteriosus (745.0) (Mahle et al., 2009; Kemper et al., 2011). The secondary targets were double outlet right ventricle (745.11), single ventricle (745.3), Ebstein anomaly (746.2), coarctation or hypoplasia of aortic arch (747.10 [coarctation of the aorta]), and aortic interruption, atresia or hypoplasia (747.11, 747.22) (Mahle et al., 2009; Kemper et al., 2011). All discharges with principal or secondary discharge diagnosis codes for CCHDs were considered to be CCHD discharges, regardless of other noncritical CHDs present and those costs were included in the CCHD category. Hospitalizations could have multiple CHD or CCHD diagnoses, but were only counted once for overall estimates of costs. For estimates of costs of individual CCHDs, hospitalizations were counted each time an individual CCHD ICD-9-CM code appeared and could be counted more than once.
STUDY VARIABLES
Hospital costs were the outcome of interest. Hospital charges represent what hospitals bill for services and do not include physician fees. HCUP provides hospital-specific and group-average cost-to-charge ratios (CCRs) to convert hospital charges to costs. Group-average CCRs denote a weighted average CCR estimate, banded by hospital state, urban/rural location, investor-owned/other-owned, and hospital bedsize (Agency for Healthcare Research and Quality, 2011a). Hospital costs were obtained by multiplying 2009 total hospital charges by hospital-specific 2009 CCRs. If hospital-specific CCRs were unavailable, group-average CCRs were used. For one state for which CCRs were not available for use, we used average regional hospital-specific CCRs, grouped by urban versus rural location and teaching status. Total costs were obtained by summing hospital costs for all hospitalizations. Mean costs were obtained by dividing the total cost by the total number of hospitalizations.
Hospitalizations missing age, but with an HCUP identifier denoting in-hospital birth, were set to zero years and included in the analysis as being <1 year old (Agency for Healthcare Research and Quality, 2011c). Age at admission was categorized into <1 year (birth hospitalizations and discharges occurring after the birth hospitalization but <1 year old), 1 to 10 years old, and 11 to 20 years old. Age at admission was rounded down (i.e., a 10.5-year-old would be in the 1- to 10-year-old category). Because multiple hospitalizations by the same patient cannot be tracked using HCUP data, it is possible that individuals with multiple hospitalizations may be counted in more than one age category if an individual had a birthday in between hospitalizations that placed him/her in a different age category (i.e., <1 year to 1–10 years).
Expected payer was categorized based on the primary and secondary expected payers on the discharge summary: private (including HMOs), public (Medicare or Medicaid), other (self-pay, no charge, or other), and mixed. By HCUP convention, patient race/ethnicity was categorized as non-Hispanic white, non-Hispanic black, Hispanic, or other. Discharge disposition was categorized as routine (i.e., to home), died in hospital, and other (transferred out, home health care, against medical advice, and alive, destination unknown). Presence of a major or minor operating room procedure was defined using HCUP procedure class tools (Agency for Healthcare Research and Quality, 2014). Hospitalizations with a valid operating room ICD-9-CM procedure code were categorized as having a major procedure; hospitalizations with a valid non-operating room ICD-9-CM procedure code were categorized as having a minor procedure; hospitalizations with no ICD-9-CM procedure codes were categorized as having no procedures. Hospitalizations were categorized according to the most invasive procedure code present (i.e., if a hospitalizations included a major and minor procedure code, it was counted once in the major procedure category). Preterm births were identified as <1 year olds with ICD-9-CM codes 765.0 to 765.28. Other noncardiac structural or chromosomal anomalies were defined as any ICD-9-CM code from 740.0 to 757.9 and 759.0 to 759.9, excluding minor defects (Supplementary Appendix).
For all pediatric hospitalizations, we excluded discharges with missing age, missing hospital charges, and normal newborn births. CHD hospitalizations included those with principal or secondary codes for CHD diagnoses. If an infant hospitalization had a diagnosis of preterm birth and the only CHD diagnosis was patent ductus arteriosus (ICD-9-CM 747.0), then the hospitalization was excluded. Excluded hospitalizations were retained in the final dataset but not analyzed to ensure proper weighting and estimate correct standard errors (HCUP Technical Assistance, 2013).
DATA ANALYSIS
We calculated the total number of pediatric hospitalizations, excluding normal newborns, the total number of pediatric hospitalizations with CHDs, and their costs in 2009. Cost estimates were right-skewed; we did not transform data because we wanted to compare arithmetic means (Diehr et al., 1999; McGhan et al., 2009). Mean costs per hospitalization were calculated for CHDs and stratified by variables of interest as well as age at hospitalization. Total and mean costs of hospitalizations with any CCHD were obtained and compared with costs of all hospitalizations with any noncritical CHD. Differences in means were evaluated with t tests or ANOVA tests; all p-values were two-sided. Supplemental analyses were conducted to examine factors associated with increased costs: (1) an ordinary least squares regression of the natural log of costs of all pediatric hospitalizations, controlling for CHDs; (2) an ordinary least squares regression of the natural log of costs among pediatric hospitalizations with CHDs; and (3) a quantile regression of the 10th, 25th, 50th, 75th, and 90th percentiles of the natural log of costs. Because of the log transformations, results are presented as exp(β) and should be interpreted as percentage change. Quantile regression parameters estimate the change in the quantile of costs. All models adjusted for length of stay, age group, presence of a CCHD, gender, expected payer, race, median household income, discharge disposition, and presence of a procedure on the discharge record. The quantile regression was performed in SAS version 9.3 (SAS Institute, Cary, NC), but did not account for the complex sampling design of the KID. All other analyses were performed in SAS version 9.3 (SAS Institute) using SAS survey procedures to account for the KID’s complex sampling design.
Results
The 2009 KID included 3,407,146 pediatric discharges, sampled from 4121 hospitals. There were 1685 birth hospitalizations with missing ages in which age was set to zero years. Among all pediatric hospitalizations, 14,620 were missing age, 62,699 were missing hospital charges, and 249,158 were considered normal newborn births; these hospitalizations were excluded. The 3,080,669 observations remaining after applying our exclusion criteria represented a weighted nationwide estimate of 4,461,680 pediatric hospitalizations admitted for any reason (95% confidence interval [CI]: 4,275,622–4,647,738). Among remaining hospitalizations, we excluded 12,129 pediatric hospitalizations with a diagnosis of preterm birth with only a patent ductus arteriosus diagnosis and 2,955,225 pediatric hospitalizations whose discharge record did not include a CHD ICD-9-CM code and were presumed to be admitted for a non-CHD cause. After exclusions, there were 113,315 hospitalizations with a CHD diagnosis for analysis. Weighted, this represented 163,980 nationwide hospitalizations with CHDs (95% CI: 150,664–177,295), which accounted for 3.7% of pediatric hospitalizations. Of weighted CHD hospitalizations, 27,282 (95% CI: 22,558–32,007) had a principal diagnosis of a CHD and 136,697 (95% CI: 126,942–146,453) had a secondary diagnosis of a CHD. Among infants with a CHD, 33,839 (95% CI: 31,211–36,468) or 25.9% had a diagnosis of preterm birth. Among all hospitalizations with a CHD, 46,712 (95% CI: 42,042–51,381) or 28.5% also had a diagnosis of another structural or chromosomal anomaly.
In a supplemental ordinary least squares regression controlling for presence of CHD, length of stay, age, expected payer, sex, race, median income of patient zip code, discharge disposition, and presence of a major or minor operating procedure, pediatric hospitalizations with CHD still had significantly higher costs compared with pediatric patients without CHD (data not shown). Pediatric hospitalizations without a CHD diagnosis code had shorter lengths of stay per hospitalization compared with those with a CHD diagnosis code (4.3 days [95% CI, 4.2–4.4] versus 14.4 days [95% CI, 13.9–14.9]) (p <0.001). Among the 4,297,701 (95% CI, 4,122,735–4,472,667) pediatric hospitalizations without a CHD diagnosis code, 42.5% (1,827,898; 95% CI, 1,746,995–1,908,802) did not have a procedure recorded on their discharge record; 35.4% (1,520,374; 95% CI, 1,448,658–1,592,090) had a minor procedure recorded; and 22.1% (949,428; 95% CI, 907,285–991,571) had a major procedure recorded. Compared with those pediatric patients without a CHD diagnosis code, pediatric patients hospitalized with a CHD diagnosis code were more likely to have minor or major procedures recorded on their discharge record (p <0.001; Table 1). Among CHD hospitalizations in which the principal diagnosis was a CHD, the five principal procedures with the highest total costs (Million Dollars [M] [95% CI]) were: systemic to pulmonary artery shunt ($119.5 M [$90.9 M–$148.2 M]), total repair of tetralogy of Fallot ($90.9 M [$69.4 M–$112.4 M]), extracorporeal membrane oxygenation ($84.4 M [$56.7 M–$112.1 M]), creation of a conduit between the atrium and pulmonary artery ($79.0 M [$61.7 M–96.2 M]), and surgical occlusion of other thoracic vessels ($75.2 M [$58.6 M–$91.7 M]).
TABLE 1.
Weighted Estimates of Number of Hospitalizations with Congenital Heart Defects (CHD) by Age, Kids’ Inpatient Database, 2009
| All pediatric hospitalizations Na=163,980 |
<1 year Na=130,512 |
1–10 years Na=23,968 |
11–20 years Na=9,500 |
|||||
|---|---|---|---|---|---|---|---|---|
| N (%) | 95% CIb | N (%) | 95% CIb | N (%) | 95% CIb | N (%) | 95% CIb | |
| Critical CHD | ||||||||
|
| ||||||||
| No | 135,660 (82.7) | 125,702–145,618 | 111,800 (85.7) | 103,918–119,683 | 16,742 (69.9) | 14,502–18,982 | 7,117 (74.9) | 6,300–7,935 |
|
| ||||||||
| Yes | 28,320 (17.3) | 24,105–32,534 | 18,711 (14.3) | 16,115–21,308 | 7,226 (30.1) | 5,929–8,522 | 2,383 (25.1) | 1,942–2,824 |
|
| ||||||||
| Gender | ||||||||
|
| ||||||||
| Female | 76,950 (46.9) | 70,781–83,119 | 61,306 (47.0) | 56,833–65,780 | 11,121 (46.4) | 9,490–12,752 | 4,522 (47.6) | 3,964–5,080 |
|
| ||||||||
| Male | 86,900 (53.0) | 79,714–94,085 | 69,122 (53.0) | 63,939–74,305 | 12,807 (53.4) | 10,950–14,664 | 4,971 (52.3) | 4,296–5,646 |
|
| ||||||||
| Missing | 130 (0.1) | 83 (0.1) | --e | --e | ||||
|
| ||||||||
| Expected payer | ||||||||
|
| ||||||||
| Public | 76,812 (46.8) | 69,687–83,938 | 62,563 (47.9) | 57,080–68,045 | 10,841 (45.2) | 9,169–12,512 | 3,409 (35.9) | 2,961–3,856 |
|
| ||||||||
| Private | 53,473 (32.6) | 48,152–58,794 | 42,998 (32.9) | 39,065–46,931 | 6,876 (28.7) | 5,569–8,182 | 3,599 (37.9) | 3,029–4,170 |
|
| ||||||||
| Otherc | 9,748 (5.9) | 8,199–11,297 | 7,282 (5.6) | 6,324–8,240 | 1,639 (6.8) | 1,091–2,187 | 827 (8.7) | 656–998 |
|
| ||||||||
| Mixed | 23,852 (14.5) | 18,039–29,666 | 17,597 (13.5) | 13,717–21,476 | 4,599 (19.2) | 2,992–6,205 | 1,657 (17.4) | 1,125–2,188 |
|
| ||||||||
| Missing | 94 (0.6) | 72 (0.1) | --e | --e | ||||
|
| ||||||||
| Race | ||||||||
|
| ||||||||
| Non-Hispanic White | 68,071 (41.5) | 60,750–75,393 | 52,599 (40.3) | 47,686–57,513 | 10,555 (44.0) | 8,512–12,597 | 4,917 (51.8) | 4,117–5,718 |
|
| ||||||||
| Non-Hispanic Black | 23,123 (14.1) | 20,426–25,820 | 19,268 (14.8) | 17,098–21,438 | 2,779 (11.6) | 2,245–3,313 | 1,076 (11.3) | 875–1,278 |
|
| ||||||||
| Hispanic | 35,222 (21.5) | 30,010–40,435 | 28,547 (21.9) | 24,377–32,716 | 5,169 (21.6) | 3,961–6,376 | 1,507 (15.9) | 1,174–1840 |
|
| ||||||||
| Other | 14,887 (9.1) | 12,886–16,887 | 12,197 (9.3) | 10,697–13,697 | 2,086 (8.7) | 1,595–2,577 | 604 (6.4) | 465–743 |
|
| ||||||||
| Missing | 22,676 (13.8) | 17,901 (13.7) | 3,379 (14.1) | 1,396 (14.7) | ||||
|
| ||||||||
| Median household income by patient zip code | ||||||||
|
| ||||||||
| ≤39,999 | 49,334 (30.1) | 44,384–54,284 | 40,143 (30.8) | 36,183–44,104 | 6,734 (28.1) | 5,689–7,780 | 2,456 (25.9) | 2,129–2,784 |
|
| ||||||||
| 40,000–49,999 | 40,544 (24.7) | 37,047–44,042 | 32,180 (24.7) | 29,624–34,736 | 5,987 (25.0) | 5,122–6,852 | 2,378 (25.0) | 2,049–2,706 |
|
| ||||||||
| 50,000–65,999 | 38,641 (23.6) | 35,070–42,211 | 30,500 (23.4) | 27,906–33,094 | 5,851 (24.4) | 4,881–6,822 | 2,290 (24.1) | 1,957–2,623 |
|
| ||||||||
| ≥66,000 | 32,102 (19.6) | 27,865–36,340 | 25,070 (19.2) | 21,970–28,169 | 4,874 (20.3) | 3,797–5,952 | 2,158 (22.7) | 1,732–2,585 |
|
| ||||||||
| Missing | 3,358 (2.0) | 2,619 (2.0) | 521 (2.2) | 218 (2.3) | ||||
|
| ||||||||
| Discharge disposition | ||||||||
|
| ||||||||
| Routined | 133,961 (81.7) | 122,571–145,350 | 103,671 (79.4) | 95,512–111,830 | 21,718 (90.6) | 18,593–24,844 | 8,571 (90.2) | 7,462–9,681 |
|
| ||||||||
| Died | 3,952 (2.4) | 3,457–4,446 | 3,640 (2.8) | 3,186–4,094 | 205 (0.9) | 157–252 | 107 (1.1) | 83–131 |
|
| ||||||||
| Otherc | 26,018 (15.9) | 23,409–28,627 | 23,157 (17.7) | 21,041–25,273 | 2,045 (8.5) | 1,545–2,544 | 816 (8.6) | 670–962 |
|
| ||||||||
| Missing | 49 (0.0) | 44 (0.0) | -- e | -- e | ||||
|
| ||||||||
| Proceduref | ||||||||
|
| ||||||||
| No procedure | 40,075 (24.4) | 37,145–43,005 | 30,145 (23.1) | 27,970–32,319 | 7,387 (30.8) | 6,546–8,228 | 2,543 (26.8) | 2,262–2,824 |
|
| ||||||||
| Minor procedure | 66,693 (40.7) | 61,233–72,153 | 59,064 (45.3) | 54,182–63,945 | 5,098 (21.3) | 4,304–5,891 | 2,532 (26.6) | 2,213–2,850 |
|
| ||||||||
| Major procedure | 57,211 (34.9) | 50,418–64,004 | 41,303 (31.6) | 37,036–45,570 | 11,483 (47.9) | 9,407–13,559 | 4,425 (46.6) | 3,727–5,124 |
Estimates may not sum to total due to weighting and rounding.
95% confidence interval.
Other includes self-pay, no charge, other.
Routine: all hospitalizations discharged to home, self-care, or court/law enforcement; Other: all transfers, discharged to home health care, against medical advice, and alive but destination unknown.
Cells with less than 10 observations have been suppressed.
No procedure: no procedure indicated on discharge summary; Minor procedure: non-operating room diagnostic or therapeutic procedure indicated on discharge summary; Major procedure: operating room diagnostic or therapeutic procedure indicated on discharge summary.
CHD COSTS
Total weighted costs for the 4.46 million pediatric hospitalizations (excluding uncomplicated newborn hospitalizations) were estimated to be $37,067,978,726 (mean =$8308; 95% CI: $7932–$8684). Total weighted costs for the 163,980 CHD hospitalizations were $5,615,646,475 (mean =$34,246; 95% CI: $32,419–$36,073), representing 15.1% of total pediatric hospitalization costs. Costs were skewed to the right (a small number of hospitalizations had very high costs). Median costs of hospitalizations with a CHD diagnosis were $10,974 (25th–75th percentile: $2742–$36,714; 10th–90th percentile: $1311–$91,648). Excluding infants with a diagnosis of pre-term birth and CHD, total costs were estimated to be $3,384,290,957 (mean =$26,005; 95% CI: $23,874–$28,136); excluding hospitalizations that also included a diagnosis of another structural or chromosomal anomaly, total costs were estimated to be $3,363,832,004 (mean = $28,685; 95% CI: $26,988–$30,382); excluding hospitalizations with either preterm birth or another structural or chromosomal anomaly, total costs were estimated to be $1,885,688,446 (Mean =$20,350; 95% CI: $18,311–$22,405).
The majority of hospitalizations with CHDs occurred among patients <1 year old (n =130,512; 95% CI, 120,898–140,126), followed by hospitalizations of 1 to 10 years old (n =23,968; 95% CI, 20,510–27,425), and hospitalizations of 11 to 20 years old (n =9500; 95% CI, 8297–10,703) (Table 1). The majority of hospitalizations with CHDs among patients <1 and 1 to 10 years old had an expected public payer (47.9% and 45.2%, respectively) whereas, among hospitalizations with CHDs aged 11 to 20 years, the majority had an expected private payer (Table 1). Overall, approximately 41% of all hospitalizations with a CHD had a minor procedure; however, by age group, the majority of hospitalizations among patients aged 1 to 10 and 11 to 20 had a major procedure (47.9% and 46.6%, respectively) (Table 1).
Among all ages, CCHD hospitalizations had higher mean costs per hospitalization than did those with noncritical CHDs ($52,899 vs. $30,351, respectively). Patients that died while hospitalized had the highest mean costs per hospitalization (Table 2). Hospitalizations among patients <1 year old had the highest mean costs ($36,601) whereas, hospitalizations of 1- to 10-year-olds and 11- to 20-year-olds had similar mean costs ($25,498 and $24,961, respectively) (Table 2). The mean costs per hospitalization among those <1 year old whose discharge was routine ($30,595) were significantly higher compared with 1- to 10-year-olds ($22,907) and 11- to 20-year-olds ($21,957) that were routinely discharged. Hospitalizations with a CCHD had significantly higher mean costs than hospitalizations without critical CHDs for patients <1 year old, 1 to 10 years old, and 11 to 20 years old. However, the difference between mean costs per hospitalization of CCHD and noncritical CHD hospitalizations decreased with increasing age (Table 2). At all ages, mean costs per hospitalization were significantly higher with the presence of a major procedure (Table 2).
TABLE 2.
Weighted Mean Costs (U.S. Dollars) by Age of Hospitalizations with a Congenital Heart Defect, Kids’ Inpatient Database, 2009
| All Ages
|
<1year old
|
1–10 years old
|
11–20 years old
|
|||||
|---|---|---|---|---|---|---|---|---|
| Mean (U.S. $) (SEa) | pb | Mean (U.S. $) (SEa) | pb | Mean (U.S. $) (SEa) | pb | Mean (U.S. $) (SEa) | pb | |
| Any congenital heart defect | 34,246 (932) | 36,601 (1,103) | 25,498 (1,079) | 23,961 (873) | ||||
|
| ||||||||
| Critical congenital heart defect | ||||||||
|
| ||||||||
| No | 30,352 (753) | <0.001 | 32,352 (898) | < 0.001 | 20,521 (787) | < 0.001 | 22,066 (804) | <0.001 |
|
| ||||||||
| Yes | 52,899 (1,990) | 61,990 (2,416) | 37,032 (1,927) | 29,622 (1,567) | ||||
|
| ||||||||
| Gender | ||||||||
|
| ||||||||
| Female | 33,196 (931) | <0.001 | 35,449 (1,114) | < 0.001 | 25,393 (1,074) | 0.79 | 21,850 (965) | <0.001 |
|
| ||||||||
| Male | 35,200 (970) | 37,645 (1,133) | 25,624 (1,239) | 25,883 (1,113) | ||||
|
| ||||||||
| Expected payer | ||||||||
|
| ||||||||
| Public | 34,773 (1,102) | 37,291 (1,319) | 23,968 (1,002) | 22,925 (1,011) | ||||
|
| ||||||||
| Private | 31,308 (1,210) | <0.001 | 32,520 (1,330) | < 0.001 | 26,794 (1,794) | 0.11 | 25,452 (1,222) | 0.08 |
|
| ||||||||
| Otherc | 31,090 (2,015) | 32,517 (2,467) | 29,588 (2,342) | 21,495 (1,722) | ||||
|
| ||||||||
| Mixed | 40,467 (2,105) | 45,868 (2,778) | 25,712 (1,575) | 24,068 (1,778) | ||||
|
| ||||||||
| Race | ||||||||
|
| ||||||||
| Non-Hispanic White | 33,094 (1,080) | 35,554 (1,262) | 24,971 (1,424) | 24,223 (1,179) | ||||
|
| ||||||||
| Non-Hispanic Black | 36,019 (1,383) | <0.001 | 38,246 (1,597) | < 0.01 | 25,860 (1,530) | 0.32 | 22,387 (1,729) | 0.60 |
|
| ||||||||
| Hispanic | 32,455 (1,540) | 33,909 (1,874) | 26,921 (1,495) | 23,907 (1,386) | ||||
|
| ||||||||
| Other | 37,345 (1,583) | 39,572 (1,862) | 27,351 (1,456) | 26,893 (2,809) | ||||
|
| ||||||||
| Median household income by patient zip code | ||||||||
|
| ||||||||
| <=39,999 | 35,336 (1,260) | 37,999 (1,507) | 24,469 (1,204) | 21,617 (1,152) | ||||
|
| ||||||||
| 40,000–49,999 | 34,576 (1,043) | 0.39 | 37,075 (1,259) | 0.31 | 25,221 (1,084) | 0.57 | 24,314 (1,162) | 0.01 |
|
| ||||||||
| 50,000–65,999 | 33,560 (953) | 35,858 (1,163) | 25,609 (1,114) | 23,280 (1,119) | ||||
|
| ||||||||
| >= 66,000 | 33,109 (1,265) | 34,886 (1,480) | 26,585 (1,738) | 27,204 (1,573) | ||||
|
| ||||||||
| Discharge disposition | ||||||||
|
| ||||||||
| Routined | 28,796 (916) | 30,595 (1,091) | 22,907 (930) | 21,957 (833) | ||||
|
| ||||||||
| Died | 97,720 (4,273) | <0.001 | 96,655 (4,379) | < 0.001 | 123,321 (12,542) | < 0.001 | 84,997 (11,507) | <0.001 |
|
| ||||||||
| Otherd | 52,632 (1,740) | 54,015 (1,867) | 43,225 (3,121) | 36,961 (3,117) | ||||
|
| ||||||||
| Proceduree | ||||||||
|
| ||||||||
| No procedure | 5,964 (267) | 5,994 (336) | 5,765 (189) | 6,178 (276) | ||||
|
| ||||||||
| Minor procedure | 30,825 (821) | <0.001 | 32,184 (919) | < 0.001 | 21,240 (962) | < 0.001 | 18,416 (911) | <0.001 |
|
| ||||||||
| Major procedure | 58,046 (1,478) | 65,256 (1,895) | 40,084 (1,687) | 37,353 (1,354) | ||||
SE: Standard error.
p-value for difference between means; t-test, or ANOVA test.
Other includes self-pay, no charge, other.
Routine: all hospitalizations discharged to home, self-care, or court/law enforcement; Other: all transfers, discharged to home health care, against medical advice, and alive but destination unknown.
No procedure: no procedure indicated on discharge summary; Minor procedure: non-operating room diagnostic or therapeutic procedure indicated on discharge summary; Major procedure: operating room diagnostic or therapeutic procedure indicated on discharge summary.
Supplemental analyses assessed factors associated with increased hospital costs among pediatric hospitalizations with a CHD diagnosis code. In an adjusted linear regression, length of stay, presence of a CCHD, death while hospitalized, and presence of a minor or major procedure was significantly associated with increased hospital costs. However, younger ages were associated with significantly decreased costs (Supplementary Table S1, which is available online). Quantile regression analysis allowed a comparison of the impact of regression coefficients at different cost quantiles. Again, length of stay, presence of a CCHD, death while hospitalized, and presence of a minor or major procedure were strongly associated with increased costs (Supplementary Table S1). However, these factors were most strongly associated with increased costs in the 25th, 50th, and 75th percentiles (Supplementary Table S1).
CCHD COSTS
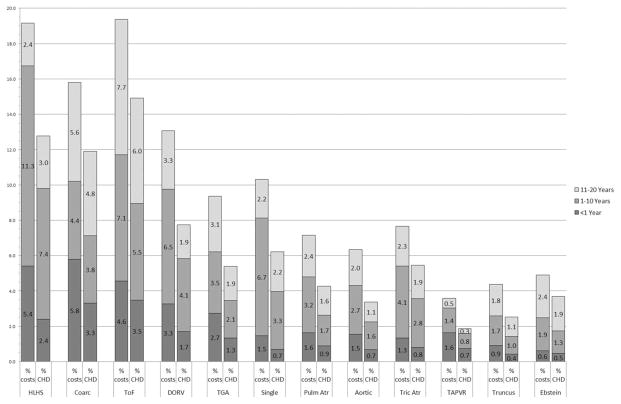
The 28,320 hospitalizations with a CCHD accounted for 17.3% of all CHD hospitalizations and 26.7% of hospital costs (Table 3). Among all ages, hospitalizations with total anomalous pulmonary venous return had the highest mean cost per hospitalization ($73,033), but hospitalizations with HLHS had the highest total cost ($333.1 M) (Table 3), representing 5.9% of the total costs for pediatric CHD hospitalizations. The five most costly CCHD hospitalizations (by total cost in millions of dollars) were: HLHS ($333.1 M), coarctation of the aorta ($316.3 M), tetralogy of Fallot ($279.0 M), double outlet right ventricle ($202.9 M), and transposition of the great arteries ($159.2 M). Among CCHD hospitalizations, those for Ebstein anomaly had the lowest mean costs ($42,565); mean costs per hospitalization for Ebstein anomaly remained significantly higher than mean costs per hospitalization for noncritical CHDs ($30,352, Table 2) (p <0.001). At all ages, hospitalizations with a CCHD diagnosis accounted for a disproportionately larger percentage of hospital costs than represented in the total number of hospitalizations with any CHD (Fig. 1). For example, hospitalizations among those aged <1 year old with HLHS represented 2.4% of all hospitalizations with CHD, but accounted for 5.4% of total hospital costs in that age group; for hospitalizations 1 to 10 years old, HLHS hospitalizations represented 7.4% of all hospitalizations with CHD, but accounted for 11.3% of all costs in that age group (Fig. 1).
TABLE 3.
Weighed Estimated Number, Mean Cost, and Total Cost of Critical Congenital Heart Defects, 2009 Kids’ Inpatient Database
| Na | 95% CIb | % of all CHDsc | Mean Cost (U.S. $) | 95% CIb Mean Cost | Total Cost (Million U.S. $) | 95% CIb Total Cost (Million U.S. $) | |
|---|---|---|---|---|---|---|---|
| Hypoplastic left heart syndrome | 5,175 | 4,211–6,139 | 3.2 | 64,368 | 57,941–70,796 | 333.1 | 252.0–414.2 |
| Coarctation of the aorta | 5,684 | 4,848–6,520 | 3.5 | 55,645 | 51,355–59,936 | 316.3 | 255.8–376.8 |
| Tetralogy of Fallot | 6,415 | 5,519–7,311 | 3.9 | 43,490 | 39,625–47,356 | 279.0 | 227.1–330.9 |
| Double outlet right ventricle | 3,380 | 2,748–4,013 | 2.1 | 60,022 | 55,553–64,490 | 202.9 | 161.1–244.7 |
| Transposition of the great arteries | 2,444 | 2,036–2,852 | 1.5 | 65,133 | 58,523–71,742 | 159.2 | 124.7–193.7 |
| Single ventricle | 1,904 | 1,513–2,296 | 1.2 | 60,557 | 53,353–67,760 | 115.3 | 85.8–144.8 |
| Pulmonary atresia | 1,739 | 1,417–2,061 | 1.1 | 59,124 | 53,030–65,218 | 102.8 | 78.8–126.8 |
| Interruption/hypoplasia of the aortic arch | 1,375 | 1,150–1,599 | 0.8 | 69,415 | 60,957–77,872 | 95.4 | 72.9–117.9 |
| Tricuspid atresia | 1,899 | 1,566–2,233 | 1.2 | 49,337 | 44,315–54,359 | 93.7 | 72.0–115.4 |
| Total anomalous pulmonary venous return | 1,198 | 954–1,442 | 0.7 | 73,033 | 65,783–80,282 | 87.5 | 66.5–108.5 |
| Truncus arteriosus | 899 | 741–1,057 | 0.5 | 64,394 | 55,878–72,909 | 57.9 | 44.2–71.6 |
| Ebstein anomaly | 1,093 | 910–1,276 | 0.7 | 42,565 | 36,259–48,870 | 46.5 | 35.7–57.3 |
| All critical CHD | 28,320 | 24,105–32,534 | 17.3 | 52,899 | 48,997–56,801 | 1,498.1 | 1,209.4–1,786.7 |
| All CHD (including critical CHD) | 163,980 | 150,664–177,295 | 34,246 | 32,419–36,073 | 5,615.6 | 4,960.9–6,270.3 |
Hospitalizations with critical congenital heart defects could be counted in more than one category if more than one critical congenital heart defect was present on the discharge summary.
95% confidence interval.
Congenital heart defects.
FIGURE 1.
Total costs of hospitalizations with critical congenital heart defects as a percentage of total costs of all hospitalizations with any congenital heart defect; total hospitalizations with a critical congenital heart defect as a percentage of total hospitalizations with any congenital heart defect, by age. CHD, congenital heart defect; HLHS, hypo-plastic left heart syndrome; Coarc, coarctation of the aorta; ToF, tetralogy of Fallot; DORV, double outlet right ventricle; TGA, transposition of the great arteries; Single, single ventricle; Pulm Atr, pulmonary atresia; Aortic, interruption or hypoplasia of aortic arch; Tric Atr, tricuspid atresia; TAPVR, total anomalous pulmonary venous return; Truncus, truncus arteriosus; Ebstein, Ebstein anomaly
Discussion
Our analysis of 2009 KID data revealed that the costs for hospitalizations of pediatric patients (<20 years old) with CHDs surpassed $5.6 billion. Costs were highest for hospitalizations of patients less than one year of age, for hospitalizations of patients with a CCHD, or for hospitalizations in which the patient died in the hospital. However, high resource use was not limited to infancy; 14.6% of hospitalizations with CHD occurred in 1- to 10- year-olds and 5.8% occurred in children aged 11 to 20. The cost per hospitalization among 1- to 10- and 11- to 20-year-olds averaged roughly $25,000. Previous work has observed CHD hospitalizations of infants and neonates to be associated with high hospital charges (Centers for Disease Control and Prevention, 2007), as well as identified factors associated with high hospital costs, including increased surgical risk, complications during hospitalizations, late detection of a CCHD, and type of CCHD (Connor et al., 2005; Benavidez et al., 2007; Russo and Elixhauser, 2007; Peterson et al., 2013). Our results add to the literature by estimating the high costs of CHD hospitalizations and the specific CCHD contribution to costs after infancy, as well as identifying CCHDs associated with high hospital costs. Hospitalizations with CCHDs had disproportionately higher costs in comparison to total CHD hospitalizations. Among CCHDs, costs for those with HLHS surpassed $333 million, and accounted for 6% of the total cost of all hospitalizations with any CHD.
This study had several limitations. First, because the KID is an administrative database, we used ICD-9-CM codes to identify CHD hospitalizations, which are imperfect identifiers of CHDs (Frohnert et al., 2005; Strickland et al., 2008). Misclassification of patient hospitalizations with or without CHDs could bias estimates of cost in either direction. Additionally, we lacked patient-level data, preventing us from analyzing individual patient costs, re-admissions, hospital transfers, or the impact of individual patients with multiple CHD diagnoses on hospital costs. However, our goal was to examine total and mean hospital costs, as opposed to patient-level costs. Second, the accuracy of cost estimates is affected by variation of CCRs across and within each hospital (Rogowski, 1999). Hospital-specific CCRs may not be appropriate for cost estimates of specialized procedures and diagnoses; however, as we did not have department-specific CCRs, these ratios were the best available. Third, in our analysis, cost estimates were right-skewed. A comparison of mean estimates can be problematic if some patients (e.g., because of complications or co-morbidities) have higher costs (Diehr et al., 1999; McGhan et al., 2009). However, we chose to examine arithmetic means, which better characterize overall healthcare resource use than do medians (Diehr et al., 1999; McGhan et al., 2009). Fourth, our estimates of the costs of hospitalizations with CHD may be impacted by our exclusion criteria. We included CHD hospitalizations of preterm births, as well as CHD hospitalizations with noncardiac structural and chromosomal anomalies. These observations likely inflate the cost of hospitalizations with CHD beyond what should be expected for a CHD alone. In fact, removing those hospitalizations with either a preterm birth or additional congenital or chromosomal anomaly reduced total cost estimates by approximately 66%. However, we sought to obtain an overall estimate of all CHD hospitalizations and excluding preterm births or other congenital anomalies would have excluded a large subset of those hospitalized with a CHD. Finally, while we provide race/ethnicity as coded in the KID, hospitals vary in how they report race/ethnicity. Moreover, race/ethnicity is likely not missing at random when not coded (Agency for Healthcare Research and Quality, 2011c). AHRQ generates disparity files restricted to 40% of HCUP discharges from states and hospitals with race/ethnicity data meeting specific criteria for accuracy (Coffey et al., 2010). While these patient exclusion criteria have been used in studies of healthcare disparities (Barocas et al., 2012), their application here would have precluded generating nationwide estimates.
CHDs are of public health importance due to their prevalence and severity. CCHDs are severe, require early interventions, and often require lifelong care and treatment (Warnes et al., 2001; Williams et al., 2006; Marelli et al., 2007; Oster et al., 2013a). Overall, 17.3% of all hospitalizations with a CHD had a CCHD; additionally, a greater percentage of hospitalizations with CCHD occurred for 1 to 10 and 11 to 20 year olds than for <1 year olds, indicating that these patients continue to receive inpatient care beyond infancy. Many individuals with CHDs surviving past infancy have CHDs of mid to high complexity and require lifelong care (Warnes et al., 2001; Williams et al., 2006). As the population of children and adolescents living with CHDs ages, the costs to hospitals for care incurred for individuals hospitalized for CHDs can be expected to increase. Research investigating factors associated with hospital costs for children and adolescents with CHDs and what types of inpatient hospital resources are consumed at these older ages is needed to plan for the future needs of this growing population.
Supplementary Material
Acknowledgments
We acknowledge the HCUP partner organizations that provided 2009 data from the following states: Arizona, Arkansas, California, Colorado, Connecticut, Florida, Georgia, Hawaii, Illinois, Iowa, Indiana, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Missouri, Montana, Nebraska, New Hampshire, New Mexico, New Jersey, Nevada, New York, North Carolina, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Vermont, Washington, Wisconsin, West Virginia, and Wyoming. We gratefully acknowledge the thoughtful comments on an earlier version of this manuscript provided by Jane Baumblatt, MD, and Anne Elixhauser, PhD, of AHRQ, as well as the thorough data replication by Ms. Abbey Jones, MPH, of CDC.
Regina M. Simeone was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education (ORISE) through an interagency agreement between the U.S. Department of Energy and the Centers for Disease Control and Prevention.
Footnotes
The authors have no conflicts of interest to disclose. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Agency for Healthcare Research and Quality
Additional Supporting Information may be found in the online version of this article.
References
- Agency for Healthcare Research and Quality. [Accessed March 14, 2013];Cost-to-charge ratio files: 2009 Kids’ Inpatient Database (KID) user guide. 2011a Available at: http://www.hcup-us.ahrq.gov/db/state/CCR2009KIDUserGuide.pdf.
- Agency for Healthcare Research and Quality. HCUP Kids’ Inpatient Database (KID) [Accessed January 2, 2013];Healthcare Cost and Utilization Project (HCUP) 2009. 2011b Available at: http://www.hcup-us.ahrq.gov/kido-verview.jsp.
- Agency for Healthcare Research and Quality. [Accessed March 14, 2013];Introduction to the HCUP KIDS’ Inpatient Database (KID) 2009. 2011c Available at: http://www.hcup-us.ahrq.gov/db/nation/kid/KID_2009_Introduction.pdf.
- Agency for Healthcare Research and Quality. [Accessed April 17, 2014];HCUP procedure classes. 2014 Available at: https://www.hcup-us.ahrq.gov/tools-software/procedure/procedure.jsp.
- Barocas D, Gray D, Fowke J, et al. Racial variation in the quality of surgical care for prostate cancer. J Urol. 2012;188:1279–1285. doi: 10.1016/j.juro.2012.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benavidez OJ, Connor JA, Gauvreau K, et al. The contribution of complications to high resource utilization during congenital heart surgery admissions. Congenit Heart Dis. 2007;2:319–326. doi: 10.1111/j.1747-0803.2007.00119.x. [DOI] [PubMed] [Google Scholar]
- Botto LD, Correa A, Erickson JD. Racial and temporal variations in the prevalence of heart defects. Pediatrics. 2001;107:E32. doi: 10.1542/peds.107.3.e32. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Hospital stays, hospital charges, and in-hospital deaths among infants with selected birth defects - United States, 2003. MMWR Morb Mortal Wkly Rep. 2007;56:25–29. [PubMed] [Google Scholar]
- Coffey R, Barrett M, Houchens R, et al. Methods applying AHRQ quality indicators fo Healthcare Cost and Utilization Project (HCUP) data for the eighth (2010) National Healthcare Quality Report (NHQR) and National Healthcare Disparities Report (NHDR) [Accessed June 13, 2013];HCUP Methods Series Report # 2010-06. 2010 Available at: http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp.
- Connor JA, Gauvreau K, Jenkins KJ. Factors associated with increased resource utilization for congenital heart disease. Pediatrics. 2005;116:689–695. doi: 10.1542/peds.2004-2071. [DOI] [PubMed] [Google Scholar]
- Diehr P, Yanez D, Ash A, et al. Methods for analyzing health care utilization and costs. Annu Rev Public Health. 1999;20:125–144. doi: 10.1146/annurev.publhealth.20.1.125. [DOI] [PubMed] [Google Scholar]
- Frohnert BK, Lussky RC, Alms MA, et al. Validity of hospital discharge data for identifying infants with cardiac defects. J Perinatol. 2005;25:737–742. doi: 10.1038/sj.jp.7211382. [DOI] [PubMed] [Google Scholar]
- HCUP Technical Assistance. [Accessed January 2, 2013];HCUP calculating standard errors tutorial. 2013 Available at: http://www.hcup-us.ahrq.gov/tech_assist/tutorials.jsp.
- Kemper AR, Mahle WT, Martin GR, et al. Strategies for implementing screening for critical congenital heart disease. Pediatrics. 2011;128:e1259–e1267. doi: 10.1542/peds.2011-1317. [DOI] [PubMed] [Google Scholar]
- Mahle WT, Newburger JW, Matherne GP, et al. Role of pulse oximetry in examining newborns for congenital heart disease: a scientific statement from the AHA and APA. Circulation. 2009;120:447–458. doi: 10.1161/CIRCULATIONAHA.109.192576. [DOI] [PubMed] [Google Scholar]
- Marelli AJ, Mackie AS, Ionescu-Ittu R, et al. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation. 2007;115:163–172. doi: 10.1161/CIRCULATIONAHA.106.627224. [DOI] [PubMed] [Google Scholar]
- McGhan WF, Al M, Doshi JA, et al. The ISPOR good practices for quality improvement of cost-effectiveness research task force report. Value Health. 2009;12:1086–1099. doi: 10.1111/j.1524-4733.2009.00605.x. [DOI] [PubMed] [Google Scholar]
- O’Leary JM, Siddiqi OK, de Ferranti S, et al. The changing demographics of congenital heart disease hospitalizations in the United States, 1998 through 2010. JAMA. 2013;309:984–986. doi: 10.1001/jama.2013.564. [DOI] [PubMed] [Google Scholar]
- Opotowsky AR, Siddiqi OK, Webb GD. Trends in hospitalizations for adults with congenital heart disease in the U.S. J Am Coll Cardiol. 2009;54:460–467. doi: 10.1016/j.jacc.2009.04.037. [DOI] [PubMed] [Google Scholar]
- Oster M, Lee KA, Honein MA, et al. Temporal trends in survival among infants with critical congenital heart defects. Pediatrics. 2013a;131:e1502–e1508. doi: 10.1542/peds.2012-3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oster ME, Riehle-Colarusso T, Simeone RM, et al. Public health science agenda for congenital heart defects: report from a Centers for Disease Control and Prevention Experts Meeting. J Am Heart Assoc. 2013b;2:e000256. doi: 10.1161/JAHA.113.000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C, Dawson A, Grosse SD, et al. Hospitalizations, costs, and mortality among infants with critical congenital heart disease: How important is timely detection? Birth Defects Res A Clin Mol Teratol. 2013;97:664–672. doi: 10.1002/bdra.23165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reller MD, Strickland MJ, Riehle-Colarusso T, et al. Prevalence of congenital heart defects in metropolitan Atlanta, 1998–2005. J Pediatr. 2008;153:807–813. doi: 10.1016/j.jpeds.2008.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogowski J. Measuring the cost of neonatal and perinatal care. Pediatrics. 1999;103(Suppl E):329–335. [PubMed] [Google Scholar]
- Russo CA, Elixhauser A. HCUP Statistical Brief #24. Rockville, MD: U.S. Agency for Healthcare Research and Quality; 2007. Hospitalizations for birth defects, 2004. [PubMed] [Google Scholar]
- Strickland MJ, Riehle-Colarusso TJ, Jacobs JP, et al. The importance of nomenclature for congenital cardiac disease: implications for research and evaluation. Cardiol Young. 2008;18(Suppl 2):92–100. doi: 10.1017/S1047951108002515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warnes CA, Liberthson R, Danielson GK, et al. Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. 2001;37:1170–1175. doi: 10.1016/s0735-1097(01)01272-4. [DOI] [PubMed] [Google Scholar]
- Williams RG, Pearson GD, Barst RJ, et al. Report of the National Heart, Lung, and Blood Institute Working Group on research in adult congenital heart disease. J Am Coll Cardiol. 2006;47:701–707. doi: 10.1016/j.jacc.2005.08.074. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.