Abstract
Objective
Obsessive compulsive and related disorders are a collection of debilitating psychiatric disorders in which the role of glutamate dysfunction in the underpinning neurobiology is becoming well established. N-acetyl cysteine (NAC) is a glutamate modulator with promising therapeutic effect. This paper presents a systematic review of clinical trials and case reports exploring the use of NAC for these disorders. A further objective was to detail the methodology of current clinical trials being conducted in the area.
Methods
PubMed, Web of Science and Cochrane Library Database were searched for human clinical trials or case reports investigating NAC in the treatment of obsessive compulsive disorder (OCD) or obsessive compulsive related disorders. Researchers with known involvement in NAC studies were contacted for any unpublished data.
Results
Four clinical trials and five case reports/series were identified. Study durations were commonly 12-weeks, using 2,400–3,000 mg/day of NAC. Overall, NAC demonstrates activity in reducing the severity of symptoms, with a good tolerability profile and minimal adverse effects. Currently there are three ongoing randomized controlled trials using NAC for OCD (two adults and one pediatric), and one for excoriation.
Conclusion
Encouraging results have been demonstrated from the few pilot studies that have been conducted. These results are detailed, in addition to a discussion of future potential research.
Keywords: Obsessive-compulsive disorder; Trichotillomania, acetylcysteine; Glutamate; Review, systematic
INTRODUCTION
Obsessive compulsive disorder (OCD) is a debilitating neuropsychiatric disorder which is suggested to affect 1–2% of the population.1,2) OCD has previously been categorised as an anxiety disorder; however, the American Psychiatric Association via the Diagnostic and Statistical Manual of Mental Disorders-version 5 (DSM-5) now assigns OCD with its own classification (American Psychiatric Association, 2013). This distinction is warranted given OCD’s unique neurobiology,3,4) clinical presentation and targeted cognitive behavioural therapies compared with other anxiety disorders.5) Although anxiety appears to be a prominent symptom of OCD, anxiety is ubiquitous amongst diverse psychopathologies, and is only one marker of OCD severity.6) Hoarding, excoriation and trichotillomania (TTM) were previously included in the OCD spectrum; however, in the DSM-5, they are now categorised as obsessive compulsive related disorders (OCRD). This segregation stems from disparities between gender distribution and age of onset, comorbidities as well as the variations of neurobiology and neuropsychology.7,8) In addition, the efficacy of pharmacotherapies used in OCD has not yielded the same results in TTM patients, further supporting differing underlying neurobiology in these disorders.9) However, OCRD and OCD share similar clinical presentations, characterised by inappropriate and excessive repetitive behaviours and dysregulation of inhibitory control processes, which suggests that some components of their pathophysiology may be similar.10,11) The commonalties in the neurobiology underlying these disorders are yet to be elucidated.
Despite extensive investigations into the neurobiology of OCD, its precise etiology remains unclear. Genetic polymorphisms,12–14) autoimmune processes,15) infections,16) inflammatory and oxidative stress17,18) and abnormalities of neurotransmission within the brain19,20) have all been suggested as underlying causes and/or contributing factors.
Selective serotonin reuptake inhibitors (SSRIs) are considered to be one of the first-line interventions for OCD.5) Despite demonstrating positive effects in several instances,21) it is estimated that 40% of patients do not achieve a clinical response from these medications, nor other augmentation strategies.22) In addition, SSRIs are often required at significantly higher doses than those used for depression to obtain clinical benefits, and complete functional recovery is rare.21,23) Such a varied response rates to SSRIs may in part be explained by the heterogeneous neurobiology associated with the disorder, but may also be due to individual variances in drug absorption and metabolism. SSRIs, particularly at the required higher doses, are associated with adverse effects such as anxiety, insomnia, nausea, diarrhea, constipation, dizziness, sedation and sexual dysfunction.21,24) Our own clinical experience has shown that the severity and nature of adverse effects associated with the use of SSRIs can often lead to treatment discontinuation, further demonstrating the need for more targeted therapeutics.
A growing body of evidence suggests that abnormalities within the cortico-striato-thalamic-cortical (CSTC) circuits are one of the key factors underlying the pathophysiology of OCD.25,26) Specifically, hyperactivity within the orbitofrontal cortex, anterior cingulate and ventromedial striatum has been associated with OCD behaviour.27,28) Glutamate is the primary neurotransmitter within the CSTC, and evidence suggests that abnormal glutamate metabolism is apparent in patients with OCD.29,30) Significantly higher levels of glutamate have been found in the cerebral spinal fluid and various regions of the brain including the right caudate and orbitofrontal cortex of treatment refractory OCD patients.15,31,32) However reduced concentrations were evident in the anterior cingulate in a sample of women with OCD, and were correlated with symptom severity.31) In addition, high levels of glutamate result in excitotoxicity and oxidative stress33) and oxidative stress has been detected in serum samples from those diagnosed with OCD, as evidenced by lipid peroxidation and alterations to antioxidant systems.17,18,34) In addition, higher levels of oxidative stress appear to correlate with symptom severity.35) Whether these findings are a cause or consequence of OCD pathophysiology, is yet to be identified. Given glutamate’s role in mediating fear related memory,36) abnormalities in this neurotransmitter’s activity may play a role in the poor cognitive processing and doubt in OCD. Glutamate’s role in the CSTC, memory and cognition as well as its pro-oxidant properties supports its suggested role in the pathophysiology of OCD. Although the role of glutamate in the neurobiology of OCRD is yet to be elucidated in brain imaging studies,37) the ability of glutamate modulating agents to regulate impulse control, a characteristic of OCRD and substance abuse,38) is becoming increasingly apparent.39–41) Thus, the use of glutamate-modulating agents is of growing interest for OCRD.
Glutamate-modulating agents which have been investigated for OCD and OCRD include riluzole, memantine, topiramate, lamotrigine and glycine; however, mixed results have been reported.42) More recently, N-acetyl cysteine (NAC), a derivate of the amino acid L-cysteine, has been explored as a potential therapy for OCD and OCRD (Fig. 1). With greater bioavailability, stability, solubility and resistance to oxidation upon consumption than L-cysteine, NAC has demonstrated neurochemical, antioxidant, antiinflammatory, mucolytic and hepatoprotective activity.43,44) An advantage of NAC in comparison to other glutamatergic pharmaceuticals, is that it is available over-the-counter without prescription, and thus represents a more affordable and accessible treatment option. Further, NAC has also demonstrated efficacy in ameliorating oxidative stress (discussed below), so could provide benefits to brain health that are in addition to normalisation of glutamatergic transmission.44)
Fig. 1.
Consort chart.
After oral administration, NAC undergoes deacetylation in the liver to form cysteine, which is used as substrate for glutathione (GSH) production.45) Unconverted cysteine enters the blood stream; however, reports on the ability of cysteine, or the parent NAC compound, to cross the blood brain barrier (BBB) are contradictory.46–48) Regardless, detection of increased GSH levels in the brain were evident after administration of NAC to rats.49) More recently, patients with major depressive disorder (MDD) supplemented with NAC were found to have increased levels of NAC metabolites (necessary for GSH production) in the anterior cingulate cortex detected by proton magnetic spectroscopy.50) These studies suggest that NAC does initiate effects in the brain. It has been postulated that cysteine may cross the BBB via a sodium-dependent transport system where it is converted into cystine, the di-sulfide derivative of cysteine.51) High levels of cystine stimulate the exchange of intracellular glutamate for cystine through the cystine-glutamate antiporter, thereby elevating non-synaptic glutamate.52,53) This process activates the metabotropic glutamate receptors (mGluR2/3) on presynaptic neurons, responsible for inhibiting the synaptic release of glutamate and thereby restoring extracellular glutamate levels in the nucleus accumbens.54,55) Regulating this exchange system has been shown to improve impulse control and reduce addictive behaviour both pre-clinically and clinically.40,41,56,57) Intracellular cystine can then be reduced back to cysteine and used for GSH production, the potent and most abundant endogenous antioxidant in the body.33,58)
A clearer understanding of the pharmacokinetics and pharmacodynamics of NAC has prompted clinical investigations of this nutraceutical as a glutamate-modulating therapeutic agent for psychiatric conditions, including addictive behaviour (such as gambling, cocaine, nicotine and marijuana use),41,59,60) bipolar disorder,61,62) schizophrenia,63,64) and autism.65) The ability of NAC to modulate factors associated with OCD and OCRD, such as the regulation of extracellular glutamate and the reduction of oxidative stress (through direct radical scavenging and increasing GSH activity), indicates that this agent may be an effective treatment for OCD and OCRD.44) Animal studies have provided some support of this hypothesis. In a mouse model of OCD involving marble burying behaviour, NAC dose-dependently decreased burying behaviour independent of locomotor activity.66)
Pilot studies and case reports of NAC in the treatment OCD and OCRD have been published.39,67,68) Despite one generalised nutraceutical69) and one complementary medicine review70) for OCD and OCRD to date, there has been no specialised review collating the current clinical evidence specifically for NAC in OCD or OCRD. This paper addresses this deficit by providing a systematic review of the evidence of published studies and current ongoing clinical trials.
METHODS
PubMed, Web of Science and the Cochrane Library Database were searched in up to March 20, 2014, using the search terms “trichotillomania” OR “hair pulling” OR “hoarding” OR “hoard” OR “excoriation” OR “skin picking” OR “nail biting” OR “impulse control disorder” OR “obsessive compulsive disorder” OR “OCD” OR “OCRD” OR “obsessions” OR “compulsions” OR “obsessive compulsive related disorder” AND “N-ace-tylcysteine” OR “n-acetyl-cysteine” OR “nacetylcysteine” OR “cystine” OR “n acetylcysteine” OR “n acetyl cysteine” OR “N-acetyl-L-cysteine”. Academics and researchers with known involvement in NAC research were also contacted in an attempt to obtain any unpublished literature. Searches of the Australian and New Zealand Clinical Trial Registrar (ANZCTR) and ClinicalTrials.gov were also included, to determine any current or upcoming NAC OCD/OCRD clinical trials.
Inclusion criteria consisted of human clinical trials or case reports - open label or controlled, involving DSM-IV or DSM-5 diagnosed OCD or OCRD in which NAC was prescribed. Conditions with very similar clinical characteristics to OCD and OCRD also warranted inclusion. While both monotherapy and adjunctive trials were open for inclusion, to date there is only data available on adjunctive studies of NAC. There was no restriction on gender, age, treatment resistance, symptom severity, dosage of NAC or study design, as very limited data in the area was suspected. OCRD studies were also included, as they are now considered to be within the obsessive compulsive paradigm in the DSM-5. Given the similarity in symptoms between the two disorders (e.g., repetitive behaviours), we wanted to explore whether efficacy of NAC would be similar across both OCD and OCRD, as well as other conditions presenting with similar features.
Analysis of the Data
Data from the clinical trials which included a control group were used to calculate an effect size as Cohen’s d by first subtracting the differences in scores between the baseline and post-treatment endpoint for the intervention (or between placebo and intervention), then dividing this by the pooled standard deviation at baseline. For data without a control group, we provide a descriptive overview of the findings. The term “significant” was used for a p value of <0.05.
RESULTS
Overview
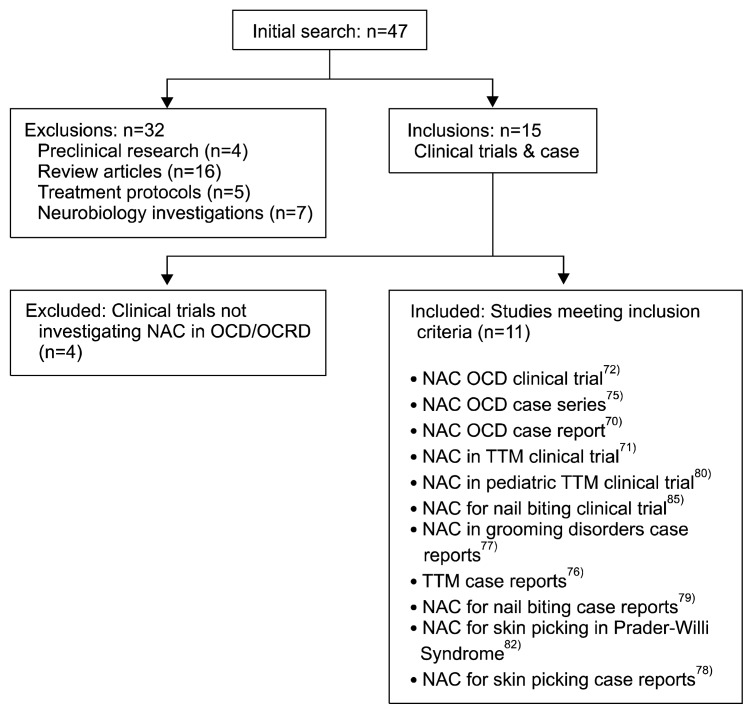
An initial search returned 47 papers, of which 11 met inclusion criteria (Fig. 2). Thirty-two papers were excluded on the basis of being either review articles (n=16), treatment protocols for OCD or OCRD (n=5), preclinical studies (n=4) or neurobiological investigations (n=7). Of the remaining 15, four clinical trials were excluded, as they did not investigate NAC for OCD, OCRD or similar conditions. This left four randomized, double blind, placebo controlled trials, one open label pilot study and six case reports. The mean trial length or length of supplementation with NAC was 13 weeks (range, 8–28 weeks) with the mean number of participants being 19 (range, 1–44) with a mean age of 30 years (range, 5–68 years). The mean of the peak NAC dose used in the studies was 1,587 mg/day (range, 800–3,000 mg/day). Sample sizes varied greatly due to the inclusion of case reports. Co-morbidities and additional treatments utilised by the participants were unspecified in some of the studies. No unpublished literature was available for inclusion.
Fig. 2.
Chemical structure of N-acetyl cysteine.
N-Acetyl Cysteine for Obsessive Compulsive Disorder
Case reports
One of the first published findings of NAC in the treatment of OCD was a case study reported by Lafleur and colleagues,67) published in 2006. A 58 year old, peri-menopausal woman was supplemented with NAC which was titrated from 600 mg to 3,000 mg daily over six weeks, and continued at the latter dose for the remaining six weeks. A dramatic drop in symptom severity was detected in the first week as determined by the Yale Brown Obsessive Compulsive Scale (Y-BOCS), with baseline 32 reduced to 24. However, this may be attributable to psychological factors associated with clinician interaction rather than pharmacological effects of NAC. A steady decrease continued from week two to week five, and despite fluctuations in symptom severity observed between weeks five and 10, there was an overall trend of improvement over the 12 weeks (Y-BOCS score of nine at endpoint). Of note, the patient’s Hamilton Rating Scale for Depression (HAM-D) score also decreased significantly over the 12 weeks, from a baseline score of 14 to an endpoint score of five. After her discharge from the hospital at the end of the 12 weeks, NAC therapy (3,000 mg/day) was maintained and a 2-month follow up demonstrated continued improvements in OCD symptoms. However, it is unclear from this case report whether symptomatic improvement at follow up was assessed based on a Y-BOCS score or self/clinician-reporting. Although the significant improvement in this patient’s OCD suggests a promising application for the use of NAC in others, great caution needs to be exercised in interpreting case reports.
In contrast, a more recent series of six retrospective case reports concluded little efficacy of NAC for OCD.71) All six patients were considered to have severe OCD (Y-BOCS score of 29.3±4.3) and were treatment-resistant (i.e., unresponsive to at least two first line pharmacotherapies). The NAC dose was titrated to 3,000 mg/day, however titration lengths for each patient were not controlled, therefore the length of time each patient received the 3,000 mg/day dose of NAC was unidentified. However, five out of six patients reported to be on 3,000 mg/day for four weeks. NAC was used adjunctively in this series and all patients were receiving pharmacotherapies (as outlined in Table 1) at doses which had been stable for a minimum of eight weeks prior to supplementation with NAC. The only patient who demonstrated a modest response to NAC in this series began with ‘moderate’ OCD severity (Y-BOCS of 26 baseline, 17 at endpoint) and MDD was the only identified comorbidity, as compared to other patients who experienced multiple co-morbidities. This response is comparable to previous studies involving cohorts of OCD patients with similar symptom severities to this patient67,68) and suggests that individuals with more severe and chronic OCD may be treatment-resistant to NAC at the 3,000 mg/day dose for this length of time. Interestingly, the two patients who were non-responsive to glutamatergic medications (topiramate and lamotrigine) did not show an improvement on NAC, but instead demonstrated a worsening in their symptom severity according to their Y-BOCS score. This highlights the increasingly accepted concept of the heterogeneous nature of OCD neurobiology and suggests that NAC may ineffective against glutamate-independent presentations of OCD. The NAC dosage and treatment regimen associated with this case report is questionable. Patients were relied upon for the purchase and consumption of the correct dose of NAC. No method was employed by researchers to monitor adherence to the correct treatment regimen. For example, remaining pills were not counted and the quality of the NAC was not assessed. Thus, the low response rate reported could be attributable to poor patient compliance, or use of potentially substandard quality NAC products. For these reasons, and the small sample size of the paper, the use of NAC cannot be discredited in a larger cohort until further clinical trials are conducted.
Table 1.
N-acetyl cysteine (NAC) in the treatment of obsessive compulsive disorder (OCD): clinical trials and case reports
| Authors | Year | Study design | Co-morbidities | NAC dose | Concurrent medication | Outcome measures | Baseline Y-BOCS | Endpoint Y-BOCS | Outcome/effect size |
|---|---|---|---|---|---|---|---|---|---|
| Lafleur et al.67) | 2006 | Case report (n=1) 12 weeks NAC supplementation |
MDD | 3,000 mg daily, titrated from 600 mg over 6 weeks | SSRI | Y-BOCS and HAM-D | 32 | 9 | Large reduction in OCD severity, noted improvement in quality of life |
| Van Ameringen et al.71) | 2013 | Retrospective case reports (n=6). 12 weeks NAC supplementation |
Tourette’s syndrome, MDD, dysthymia, MDE, panic disorder with agoraphobia social phobia, GAD, substance abuse, excoriation, TTM, ADHD | Mean dose=2,833.3 (±408.2) mg/day, titrated from 500 mg for 8 weeks | SSRI, benzodiazepines, hypnotic, antihistamine, anticonvulsants (glutamatergic modulating agents) | Y-BOCS, CGI-S and CGI-I | 29.3* | 28* | NAC not significant in ameliorating OCD symptoms in 5 of the 6 patients. |
| Afshar et al.68) | 2013 | 12 week RDBPCT (n=39) | None recorded | 2,400 mg daily, titrated from 600 mg over 2 weeks | SSRIs | Y-BOCS, CGI-S and CGI-I | 27.70 (Tx group); 27.62 (control group) |
16.83 (Tx group); 21.89 (control group) |
Cohen’s d=1.31 Full clinical response in 10/19 patients in treatment group |
Pooled data of patients within case series.
ADHD, attention deficit hyperactivity disorder; CGI-I, Clinical Global Impression Scale-Improvement; CGI-S, Clinical Global Impression Scale-Severity; GAD, generalised anxiety disorder; HAM-D, Hamilton Depression Scale; MMD, major depressive disorder; MDE, major depressive episode; RDBPCT, randomized, double-blind, placebo controlled trial; SSRI, selective serotonin reuptake inhibitor; TTM, trichotillomania; Tx, treatment; Y-BOCS, Yale Brown Obsessive Compulsive Scale.
Clinical trials
To our knowledge, there has been only one randomised clinical trial completed assessing the use of NAC in the treatment of OCD.68) This 12-week study was conducted in Iran where NAC was titrated from 600 mg/day and doubled weekly to reach a maximum dose of 2,400 mg/day (at week-3). This dose was maintained for the remaining nine weeks of the trial. Symptom severity was assessed by the Y-BOCS and Clinical Global Improvement (CGI) scales at four-week intervals. The mean age of study participants was 30.93 years (range, 23–44 years) and the cohort consisted predominantly of women (75%). The treatment group (n=20) demonstrated a significant effect over placebo (n=19) for ameliorating OCD symptoms according to the Y-BOCS. A gradual and continual decrease in symptom severity was evident from week-4, with the NAC showing significance over placebo from week-8 onwards.
Although a promising result, there are various limitations associated with this study. Ten participants in the treatment group recorded a full clinical response, defined as a 35% or greater reduction in their Y-BOCS score compared to baseline. The remaining nine patients’ response rates were not specified, and can be assumed to be less than 35%. This further raises the possibility that NAC may be effective only in a subset of OCD patients. Co-morbidities were not noted by the researchers, and if recorded, may have identified whether NAC was more beneficial in patients with less complex presentations, as postulated by the van Ameringen et al.’ s case series.71) The severity of this particular group of OCD participants was moderate (mean Y-BOCS=27), representing a select population of OCD patients. Additionally, a longer clinical trial may have determined if NAC efficacy would have continued, as has been shown in clinical trials involving individuals with bipolar disorder (in the depressive phase) who experienced continual improvements in their depressive symptoms occurring over a 24 week period.61)
N-Acetyl Cysteine for Obsessive Compulsive Related Disorders
Case reports
Several case reports exist for NAC in the treatment OCRD, including TTM, pathological nail biting and excoriation (Table 2). Promising results were obtained from case report of Rodrigues-Barata et al.72) involving two females (aged 23 years and 19 years) with chronic TTM, who were non-responsive to previous psychotherapy and SSRI medications. Both patients demonstrated complete regrowth of their hair within three months when supplemented with 1,200 mg/day of NAC. The authors noted that the positive results were maintained at a six-month follow up for the 23 year old, but did not specify if the NAC treatment was continued over this period. A follow up visit was not recorded for the 19 year old. Likewise, improvements were noted in another case report of a 40 year old female with TTM who was treatment-resistant to various medications and psychotherapy. Within three weeks of supplementation on NAC 1,200 mg twice daily she ceased hair pulling behaviour and noticed reductions in the urges to do so.73) Another patient, a 28 year old male with chronic TTM and nail biting demonstrated significant improvements on 1,800 mg/day NAC within two weeks. Of note, a return of symptoms was observed when the patient failed to comply with the dosing regime over a two week period. When taking the NAC consistently, he reported both the urge and thoughts to ‘indulge’ in these behaviours ameliorated, as well as the physical action of doing so.73) Excoriation symptom improvements have also been demonstrated in another case report, with picking urges decreasing by 50% within a week of NAC supplementation at 1,200 mg/day.73) Once the NAC dose was increased to 1,800 mg/day, complete abstinence was achieved within two days and was maintained at a four month follow up whilst continuing treatment at this dose. A more recent case report from Silva-Netto et al.74) further highlights NAC’s beneficial effects for excoriation. This report showed ‘major improvements’ in treatment resistant skin picking behaviours in three females who were supplemented with 1,200–1,800 mg daily of NAC. Of interest, one of the three women showed a relapse in picking behaviours when she discontinued the NAC and saw great improvements when it was reintroduced, demonstrating a direct correlation between NAC supplementation and symptom relief. Beneficial effects on nail biting were also detected in three patients participating in a clinical trial for bipolar disorder where NAC (1,000 mg twice daily) was used as an adjunctive strategy.75) A 46 year old female with bipolar disorder, episodes of psychosis and “life long” nail biting, reported a cessation of biting behaviour after two weeks of NAC supplementation. Cessation was maintained for the following seven months whilst remaining on the NAC as part of the study. A 44 year old female diagnosed with rapid cycling bipolar, also experienced “lifelong nail biting” behaviour. After four months, she noticed she was able to more consciously cease biting her nails after awareness that one nail had grown back strongly. The third in this case report series was a 46 year old male who had experienced manic and depressive episodes since 16 years of age, and obsessive thoughts concerning exercise and diet. The patient had a longstanding habit of biting his nails and chewing the surrounding skin on his fingers. By the end of the 28-week trial, he reported a reduction in his nail biting, but was unaware when he first noticed this since his participation. Of interest with this case series, two participants noted that cessation of their nail biting was autonomous, the other was able to consciously alter her behaviour after noticing an initial improvement. The participants were not taking NAC specifically to improve their nail biting behaviour, nor were they informed that NAC could do so by the researchers. This enhances the strength of the results from the case series and reduces the likelihood of a halo effect. As always, although case reports can demonstrate promising results, caution needs to be taken when applied to a larger population.
Table 2.
N-acetyl cysteine (NAC) in obsessive compulsive related disorders: case reports
| Authors | Year | Study design | Disorder | Co-morbidities | NAC dose | Concurrent medication | Outcome measures | Baseline score | Endpoint score | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| Silva-Netto et al.74) | 2014 | Case report (n=3) | Skin picking | TTM, MDE | 1,200–1,800 mg daily | Venlafaxine, lithium, quetiapine, SSRI | Self reports and clinical observation | NA | NA | Major improvements in skin picking behaviours |
| Rodrigues-Barata et al.72) | 2012 | Case report (n=2) | TTM | Not specified | 1,200 mg daily | Not specified | Clinician observation | NA | NA | Complete regrowth of hair and cessation of urges to pull hair |
| Odlaug et al.73) | 2007 | Case reports (n=3) | TTM, nail biting, excoriation | ADHD (past hx), bulimia nervosa | 1,200–2,400 mg daily | Not specified | Self reports | NA | NA | Significant reduction in urges and cessation of the behaviours |
| Berk et al.75) | 2009 | Case reports (n=3) | Chronic nail biting | Bipolar disorder | 2,000 mg daily | Lithium, mirtazapine, magnesium, fish oil, vitamin B6, valerian | Self reports | NA | NA | Cessation of nail biting and reduction in urges to perform the behaviour |
ADHD, attention deficit hyperactivity disorder; hx, history; MDE, major depressive episode; NA, not applicable; SSRI, selective serotonin reuptake inhibitor; TTM, trichotillomania.
Clinical trials
Promising results were obtained from Grant and colleagues’ pilot research,39) published in 2009 (Table 3). This randomized, double blind, placebo controlled trial demonstrated that 2,400 mg of NAC per day was superior to placebo for reducing TTM symptoms in 44 adults, displaying significance from week-9. Significant improvements across all TTM scales, including self-reported (Massachusetts General Hospital Hair Pulling Scale) and clinician-rated scales (Psychiatric Institute Trichotillomania Scales), were demonstrated in the NAC group. Of note, the treatment group recorded no adverse effects throughout the duration of the trial, highlighting that NAC has a good tolerability profile and appears safe as an adjunctive therapy. However, despite noticeable improvements reported by both patients and clinicians regarding TTM symptoms, Quality of Life Inventory, HAM-D and Hamilton Anxiety scales (HAM-A) did not record a significant improvement over placebo. In addition, the Sheehan Disability self reported scale, showed only a mild effect size (Cohen’s d=0.42). However, only low-mild functional impairment and mood was detected at baseline in both groups. For example, HAM-D mean scores were 3.68 in both, and HAM-A mean scores were 3.72 and 3.4 in the control and treatment groups respectively. Despite NAC demonstrating promising results over placebo for improving TTM in this study, it is important to note that 44% (n=11) of patients in the treatment group did not respond to NAC. This varied response rate may be due differences in disorder neurobiology or drug pharmacokinetics and/or pharmacodynamics between patients. As suggested by Grant et al.,39) future investigations involving NAC for TTM should explore the various subtypes of TTM (e.g., autonomous versus conscious hair pulling as well as the presentations of co-morbidities) to identify patient subgroups likely to be most responsive to NAC, enabling a ‘tailored’ treatment approach for each patient.
Table 3.
N-acetyl cysteine (NAC) in obsessive compulsive related disorders: clinical trials
| Authors | Year | Study design | Disorder | Co-morbidities | NAC dose | Concurrent medication | Outcome measures | Baseline score | Endpoint score | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| Grant et al.39) | 2009 | 12 Week, RDBPCT trial (n=50) | Adult TTM | MDD, PTSD, GAD, OCD, bulimia nervosa, excoriation | 1,200 mg for the first 6 weeks, increased to 2,400 mg for the remaining 6 weeks | Stable doses for at least 6 months of SSRIs, SNRIs and/or stimulants | MGH-HPS, PITS, CGI, HAM-A, HAM-D, SDS and QLI | 17.6 tx group; 16.7 control group (MGH-HPS) | 10.4 tx group; 16 control group (MGH-HPS) | Cohen’s d=1.27 NAC significant over placebo for improving TTM symptoms in 56% (n=14) of patients in treatment group |
| Bloch et al.76) | 2013 | 12 Week, RDBPCT (n=39) | Paediatric TTM | ADHD, autism, PTSD, MDD, OCD, SAD, MR, enuresis, borderline IQ | 2,400 mg, titrated from 600 mg for up to 4 weeks | SSRI, anti psychotics, atomoxetine | MGH-HPS, TSC-C/P, NIMH-TSS, IST-C, MASC, CDI, CGI, PAERS | 13.15 tx group; 16.58 control group (MGH-HPS) | 10.70 tx group; 13.53 control group (MGH-HPS) | Cohen’s d=0.41 Modest decrease in symptoms detected in both placebo and NAC group; However, NAC not significant over placebo |
| Ghanizadeh et al.81) | 2013 | 12 Week, RDBPCT (n=25) | Children and adolescents with nail biting | OCD, eepression, anxiety disorder, tic disorder, ADHD, excoriation | 800 mg daily, titrated from 200 mg daily over a week | SSRIs, psychostimulant, antipsychotics, TCAs, NRI | Nail length | 62 mm tx group; 72.5 mm control group | 70.5 mm tx group; 75.5 mm control group | Cohen’s d: NA NAC showed significant effects over placebo for increasing nail length after first month (p<0.04), but not by the second |
| Miller and Angulo78) | 2014 | 12 Week, open label pilot study (n=35) | Paediatric and adults with skin icking in Prader Willi syndrome | Not specified | 450–1,200 mg daily | VPA, GH, MEF, QPE, RSP, SPR, TES, THY, SSRI, PRV | Counting and measuring lesions pre and post treatment | Lesion size ranging from 0.3×0.2 cm to 2.5×3 cm and 1–25 in lesion numbers | All participants with reduced size and number of lesions | Cohen’s d: NA All 35 participants had improvements in skin picking behaviour; 71% had complete resolution, 29% a significant reduction in number of active lesions |
ADHD, attention deficit hyperactivity disorder; CDI, Children’s Depression Inventory; CGI, Clinical Global Impression Scale; VPA, valproic acid; GAD, generalised anxiety disorder; GH, growth hormone; HAM-A, Hamilton Anxiety Rating Scale; HAM-D, Hamilton Depression Scale; IQ, intelligence quotient; MASC, Multidimensional Anxiety Scale for Children; MEF, metformin; MIST-C, Milwaukee Inventory for Styles of Trichotillomania-Child; MGH-HPS, Massachusetts General Hospital Hair Pulling Scale; MDD, major depressive disorder; NA, not applicable; NIMH-TSS, National Institute of Mental Health Trichotillomania Severity Scale; NRI, noradrenalin reuptake inhibitors; OCD, obsessive compulsive disorder; PAERS, Pediatric Adverse Events Rating Scale; PITS, Psychiatric Institute Trichotillomania Scale; PTSD, post traumatic stress disorder; PRV, modafinil; QLI, Quality of Life Inventory; QPE, quetiapine; RDBPCT, randomized, double blind, placebo controlled trial; RSP, risperdone; SAD, separation anxiety disorder; SDS, Sheehan Disability Scale; SSRI, selective serotonin reuptake inhibitor; SNRI, selective serotonin noradrenaline reuptake inhibitor; SPR, spironolactone; TCA, tricyclic antidepressants; TES, testosterone; THY, levothyroxine; TTM, trichotillomania; TSC-P, Trichotillomania Scale for Children, Child and Parent; tx, treatment.
More recently, NAC, titrated to a maximum dose of 2,400 mg over four weeks, failed to show significance over placebo in 35 pediatric TTM patients (aged 8–17 years).76) The authors noted that given that an improvement was seen in both groups, particularly in the first few weeks of treatment, the regular supportive assessments by the clinicians (every two weeks) and adjunctive psycho-education could have been responsible for strengthening the placebo effect. Differing pathophysiologies have also been suggested in pediatric TTM compared to adult TTM.77) The severity of the urge, the associated anxiety and frequency of these thoughts appears to increase in adults, and perhaps NAC is more specific for this population as shown by Grant et al.39)
NAC has demonstrated significant improvements in relieving skin picking behaviours in an open label pilot study involving 35 children and adults (aged 5–39 years old) with Prader-Willi Syndrome (PWS).78) PWS is a neurodevelopmental disorder caused by chromosome abnormalities and presents with obsessive-compulsive behaviours.79) Although not considered an OCRD as per the DSM-5, skin picking is apparent in 80–95% of individuals with the syndrome80) and its similarities with OCD and OCRD warrants inclusion in this review. After 12 weeks of NAC supplementation, ranging from 450–1,200 mg, all participants showed a significant improvement in skin picking behaviours determined by lesion size, frequency and the presence of scarring versus open wounds. Seventy-one percent of participants had complete resolution of self-mutilating behaviours, the remaining 29% had lesions that were smaller in size and number and with signs of wound healing present, e.g., the presence of scabs and reduction in the number of open lesions. The NAC was tolerated extremely well amongst all participants and used adjunctively to various medications without negative interactions (Table 3). Only mild gastrointestinal upsets were reported, such as cramping, flatulence and diarrhea. These symptoms dissipated after the first few weeks of NAC supplementation.
NAC (800 mg/day) has been studied versus a placebo comparator for treating nail biting in a double blind, randomized trial of 25 children and adolescents, aged 6–18 years old.81) The primary outcome was measured nail length and participants were seen before treatment, one month after baseline and two months thereafter. A statistically significant difference in nail length between the two groups occurred after the first month of treatment (p≤0.04). However, no between-group differences were seen after two months. While methodologically limited, the trial provides preliminary support of the efficacy of NAC in decreasing nail biting behaviour in children and adolescents.
Current NAC in OCD and OCRD Clinical Trials
Several clinical trials are currently underway investigating NAC for the treatment of OCD and OCRD (Table 4). Results from these studies may clarify the efficacy of NAC for these disorders. Studies are being conducted in several regions around the world, with trials in progress in Australia, the USA, the UK and Brazil. These, coupled with a previous clinical trial conducted in Iran,68) highlight the global interest in the potential use of NAC for OCD and OCRD. Longer treatment phases (16 weeks) are planned for the Sarris and Shavitt trials, which will be advantageous in identifying the therapeutic efficacy of NAC (as results may be found after 8–10 weeks of use), and determining if these effects are long lasting. In addition, current trials are better powered. The new trials will involve both pediatric and adult patient groups and may allow for determination of differences in NAC efficacy between patient subpopulations. Shavitt et al. will explore the symptom dimensions within their OCD participants (e.g., somatic obsessions and compulsions, aggressive obsessions and compulsions) using the Dimensional Yale-Brown Obsessive Compulsive Scale. This will potentially reveal if NAC is beneficial for particular presentations of OCD, as suggested from previous research where some patients appear treatment-resistant to NAC over others.71) The maximum dose of NAC used across these studies is 3,000 mg/day, which may consolidate previous research involving this dose, however, will not explore if a higher dose may be more effective in severe and chronic presentations of OCD or OCRD. The study of Sarris et al. attempts to recruit a wider patient demographic, which may incorporate a range of treatment histories, including treatment naïve patients. This may provide the first insight into NAC efficacy as a monotherapy. Unfortunately, one study (Pittenger et al.) has been terminated due to lack of participants and funding for the trial.
Table 4.
Current N-acetyl cysteine (NAC) in Obsessive Compulsive Disorders (OCD) and Obsessive Compulsive Related Disorders: Clinical Trials
| Study | Participants | Study design | Expected completion | NAC dose (mg) | Outcome measure | Status |
|---|---|---|---|---|---|---|
| Pittenger et al. (Yale University) NCT00539513 |
Treatment refractory OCD patients | 12 Week RDBPCT | NA | 3,000 | Y-BOCS, HAM-D | Terminated due to limited participants and funding |
| Bloch et al. (Yale University) NCT01172275 |
Pediatric OCD patients (8–17 years of age) | 12 Week RDBPCT | 2014 | 2,700 | CY-BOCS, DY-BOCS, CGI, PAERS | Currently recruiting |
| Shavitt et al. (University of Sao Paulo) NCT01555970 |
Treatment refractory OCD patients | 16 Week RDBPCT | 2016 | 3,000 | Y-BOCS, DY-BOCS, CGI-I, CGI-S, BDI, BAI | Currently recruiting |
| Sarris et al. (University of Melbourne) ACTRN12613000310763l |
Adult OCD patients | 16 Week RDBPCT | 2014 | 3,000 | Y-BOCS, CGI-S, CGI-I, HAM-A, MADRS | Currently recruiting |
| Grant et al. (University of Chicago) NCT01063348 |
Excoriation | 12 Week RDBPCT | 2014 | 3,000 | Y-BOCS modified for PSP, SP-SAS | Currently recruiting |
ACTRN, Australian New Zealand Clinical Trials Registry; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; CGI-I, Clinical Global Impression Scale-Improvement; CGI-S, Clinical Global Impression Scale-Severity; CY-BOCS, Children’s Yale Brown Obsessive Compulsive Scale; DY-BOCS, Dimensional Yale Brown Obsessive Compulsive Scale; HAM-A, Hamilton Anxiety Rating Scale; HAM-D, Hamilton Depression Scale; MADRS, Montgomery Asberg Depression Rating Scale; NA, not applicable; NCT, National Clinical Trial; PAERS, Pediatric Adverse Events Rating Scale; PSP, pathological skin picking; RDBPCT, randomised, double-blind, placebo controlled trial; SP-SAS, Skin Picking Symptom Assessment Scale; Y-BOCS, Yale Brown Obsessive Compulsive Scale.
DISCUSSION
To our knowledge, this is the first review specifically exploring the use of NAC in the treatment of OCD and OCRD. With an increase in the amount of clinical trials and case reports published since 2006, and more ongoing research, this indicates NAC to be a relatively new potential therapy for these conditions, and one of growing interest. However, of the few studies in the area (n=11) over half are case reports and results are promising but inconsistent. This highlights the need for further rigorous clinical research. Of note, NAC has been used adjunctively with various pharmacotherapies, particularly SSRI medication, without negative interactions and appears to show benefit in some treatment refractory patients. Promising new research highlights the potential of NAC to potentiate the antidepressant activity of certain SSRIs and tricyclic antidepressants.82) However, NAC is yet to be investigated as a monotherapy for OCD or OCRD and thus, its ability to exert therapeutic effects when administrated on its own is yet to be identified.
From the reviewed literature, the preliminary evidence supports the use of NAC in presentations of moderate-severity OCD and OCRD. Doses of 2,400–3,000 mg/day for a minimum of eight weeks (preferably 12 weeks) may be adequate for exerting an initial therapeutic effect. However, even this treatment regime in moderate presentations of OCD and OCRD showed varied response rates as demonstrated in the trials of Grant et al.39) and Afshar et al.68), where almost half of the participants within the treatment group did not display a full clinical response. In addition, two other studies failed to demonstrate a therapeutic effect of NAC.71,76) However, the severity of OCD symptoms in patients in the case series of Van Ameringen et al.71) was of greater degree than Afshar et al.68) Additionally, they were an older patient group with a high lifetime prevalence of OCD and various co-morbidities including tourettes, MDD, substance abuse, TTM, attention deficit hyperactivity disorder, and excoriation. This case series also lacked rigorous clinician oversight. Furthermore, NAC was not administered for a time frame that has been necessary to achieve therapeutic effects in other psychiatric trials.39,61,68) Insignificant effects of NAC over placebo have been identified in a pediatric TTM clinical trial.76) However, the pediatric population may have been heavily influenced by clinical interventions and psychoeducation regarding TTM, as suggested by improvements in both the treatment and control group. Due to various methodological limitations associated with the case series and pediatric clinical trial, the potential of NAC for OCD and OCRD cannot be discounted. Differences in disease severity, chronicity, co-morbidities, as well as neurobiological heterogeneity may account for varied treatment response rates amongst these studies. It is imperative that future research explores NAC’s efficacy in larger clinical trials, which include a varied cohort of symptom severity and age. Dose escalation studies and trials with longer durations (i.e., more than 12 weeks), would be beneficial to determine if more severe and complex presentations, particularly of OCD, would respond to NAC.
Continued, comprehensive investigations into the neurobiology of obsessive-compulsive and related disorders, as well as a clearer understanding of the pharmacokinetics of NAC may help to elucidate more specific therapeutic indications for NAC within clinical presentations of OCD and OCRD. Knowledge of the in vivo mechanisms of action of NAC in OCD and OCRD are also lacking. Given what is known about NAC’s ability to modulate glutamate, it may be patients with glutamate abnormalities who are responsive to NAC. If so, the therapeutic efficacy for NAC in both of these disorders suggests that the parallels between OCD and OCRD clinical presentations may be, in some cases, the result of underlying glutamate dysregulation, as well as oxidative stress, the latter either as a causative factor or consequence of the disease process. However, from the reviewed literature, the role of glutamate in the pathophysiology of patients responsive to NAC cannot be determined. Future clinical trials which incorporate measures to determine glutamate abnormalities, such as magnetic resonance imaging (MRI) or functional MRI brain imaging would be of great utility in addressing whether NAC has the ability to directly modulate activity in the regions most heavily implicated in the pathogenesis of these disorders.
NAC appears to be extremely well tolerated, with minimal adverse effects reported. Mild gastrointestinal effects appear to be the most common symptom-flatulence (which ceased after two weeks of NAC supplementation), headache, skin rash, diarrhea and nausea and vomiting of mild-moderate intensity.67,73,76,78,81) However, nausea and vomiting was also experienced in the placebo group of one particular trial, and was not evident in others.68) Other clinical trials have demonstrated no adverse effects, and NAC has shown to be very well tolerated in doses up to 8,000 mg/day in other areas of research.39,71,83) This suggests there may be scope for a higher dose of NAC to be investigated in OCD and OCRD patients who appear resistant to doses of 3,000 mg/day used in the discussed research.
In summation, although NAC appears effective in the majority of the published research, data is inconclusive, and it is yet to be rigorously investigated. Factors such as larger cohorts, higher doses and longer treatment may provide more definitive answers regarding the benefits of NAC for OCD and OCRD. The chronic and debilitating nature of these disorders, coupled with the current lack of reliable pharmacotherapies, strongly justifies the need for treatment alternatives. The emergence of promising, yet preliminary NAC research highlights this nutraceutical as a potential treatment option that warrants further investigation.
REFERENCES
- 1.Slade T, Johnston A, Oakley Browne MA, Andrews G, Whiteford H. 2007 National Survey of Mental Health and Wellbeing: methods and key findings. Aust N Z J Psychiatry. 2009;43:594–605. doi: 10.1080/00048670902970882. [DOI] [PubMed] [Google Scholar]
- 2.Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:53–63. doi: 10.1038/mp.2008.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piras F, Piras F, Chiapponi C, Girardi P, Caltagirone C, Spalletta G. Widespread structural brain changes in OCD: A systematic review of voxel-based morphometry studies. Cortex. 2013 doi: 10.1016/j.cortex.2013.01.016. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Milad MR, Rauch SL. Obsessive-compulsive disorder: beyond segregated cortico-striatal pathways. Trends Cogn Sci. 2012;16:43–51. doi: 10.1016/j.tics.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Franklin ME, Foa EB. Treatment of obsessive compulsive disorder. Annu Rev Clin Psychol. 2011;7:229–243. doi: 10.1146/annurev-clinpsy-032210-104533. [DOI] [PubMed] [Google Scholar]
- 6.Stein DJ, Fineberg NA, Bienvenu OJ, Denys D, Lochner C, Nestadt G, et al. Should OCD be classified as an anxiety disorder in DSM-V? Depress Anxiety. 2010;27:495–506. doi: 10.1002/da.20699. [DOI] [PubMed] [Google Scholar]
- 7.Chamberlain SR, Fineberg NA, Blackwell AD, Clark L, Robbins TW, Sahakian BJ. A neuropsychological comparison of obsessive-compulsive disorder and trichotillomania. Neuropsychologia. 2007;45:654–662. doi: 10.1016/j.neuropsychologia.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 8.Stein DJ, Grant JE, Franklin ME, Keuthen N, Lochner C, Singer HS, et al. Trichotillomania (hair pulling disorder), skin picking disorder, and stereotypic movement disorder: toward DSM-V. Depress Anxiety. 2010;27:611–626. doi: 10.1002/da.20700. [DOI] [PubMed] [Google Scholar]
- 9.Chamberlain SR, Menzies L, Sahakian BJ, Fineberg NA. Lifting the veil on trichotillomania. Am J Psychiatry. 2007;164:568–574. doi: 10.1176/ajp.2007.164.4.568. [DOI] [PubMed] [Google Scholar]
- 10.Chamberlain SR, Blackwell AD, Fineberg NA, Robbins TW, Sahakian BJ. The neuropsychology of obsessive compulsive disorder: the importance of failures in cognitive and behavioural inhibition as candidate endophenotypic markers. Neurosci Biobehav Rev. 2005;29:399–419. doi: 10.1016/j.neubiorev.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Chamberlain SR, Fineberg NA, Blackwell AD, Robbins TW, Sahakian BJ. Motor inhibition and cognitive flexibility in obsessive-compulsive disorder and trichotillomania. Am J Psychiatry. 2006;163:1282–1284. doi: 10.1176/ajp.2006.163.7.1282. [DOI] [PubMed] [Google Scholar]
- 12.Arnold PD, Sicard T, Burroughs E, Richter MA, Kennedy JL. Glutamate transporter gene SLC1A1 associated with obsessive-compulsive disorder. Arch Gen Psychiatry. 2006;63:769–776. doi: 10.1001/archpsyc.63.7.769. [DOI] [PubMed] [Google Scholar]
- 13.Dickel DE, Veenstra-VanderWeele J, Cox NJ, Wu X, Fischer DJ, Van Etten-Lee M, et al. Association testing of the positional and functional candidate gene SLC1A1/ EAAC1 in early-onset obsessive-compulsive disorder. Arch Gen Psychiatry. 2006;63:778–785. doi: 10.1001/archpsyc.63.7.778. [DOI] [PubMed] [Google Scholar]
- 14.Goddard AW, Shekhar A, Whiteman AF, McDougle CJ. Serotoninergic mechanisms in the treatment of obsessive-compulsive disorder. Drug Discov Today. 2008;13:325–332. doi: 10.1016/j.drudis.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 15.Bhattacharyya S, Khanna S, Chakrabarty K, Mahadevan A, Christopher R, Shankar SK. Anti-brain autoantibodies and altered excitatory neurotransmitters in obsessive-compulsive disorder. Neuropsychopharmacology. 2009;34:2489–2496. doi: 10.1038/npp.2009.77. [DOI] [PubMed] [Google Scholar]
- 16.Swedo SE, Schrag A, Gilbert R, Giovannoni G, Robertson MM, Metcalfe C, et al. Streptococcal infection, Tourette syndrome, and OCD: is there a connection? PANDAS: horse or zebra? Neurology. 2010;74:1397–1398. doi: 10.1212/WNL.0b013e3181d8a638. author reply 1398–1399. [DOI] [PubMed] [Google Scholar]
- 17.Ersan S, Bakir S, Erdal Ersan E, Dogan O. Examination of free radical metabolism and antioxidant defence system elements in patients with obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:1039–1042. doi: 10.1016/j.pnpbp.2006.03.034. [DOI] [PubMed] [Google Scholar]
- 18.Ozdemir E, Cetinkaya S, Ersan S, Kucukosman S, Ersan EE. Serum selenium and plasma malondialdehyde levels and antioxidant enzyme activities in patients with obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33:62–65. doi: 10.1016/j.pnpbp.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Menzies L, Chamberlain SR, Laird AR, Thelen SM, Sahakian BJ, Bullmore ET. Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: the orbitofronto-striatal model revisited. Neurosci Biobehav Rev. 2008;32:525–549. doi: 10.1016/j.neubiorev.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brennan BP, Rauch SL, Jensen JE, Pope HG., Jr A critical review of magnetic resonance spectroscopy studies of obsessive-compulsive disorder. Biol Psychiatry. 2013;73:24–31. doi: 10.1016/j.biopsych.2012.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bloch MH, McGuire J, Landeros-Weisenberger A, Leckman JF, Pittenger C. Meta-analysis of the dose-response relationship of SSRI in obsessive-compulsive disorder. Mol Psychiatry. 2010;15:850–855. doi: 10.1038/mp.2009.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pallanti S, Grassi G, Cantisani A. Emerging drugs to treat obsessive-compulsive disorder. Expert Opin Emerg Drugs. 2014;19:67–77. doi: 10.1517/14728214.2014.875157. [DOI] [PubMed] [Google Scholar]
- 23.Bandelow B. The medical treatment of obsessive-compulsive disorder and anxiety. CNS Spectr. 2008;13(9 Suppl 14):37–46. doi: 10.1017/s1092852900026924. [DOI] [PubMed] [Google Scholar]
- 24.Papakostas GI. Tolerability of modern antidepressants. J Clin Psychiatry. 2008;69(Suppl E1):8–13. [PubMed] [Google Scholar]
- 25.Ting JT, Feng G. Neurobiology of obsessive-compulsive disorder: insights into neural circuitry dysfunction through mouse genetics. Curr Opin Neurobiol. 2011;21:842–848. doi: 10.1016/j.conb.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harrison BJ, Pujol J, Cardoner N, Deus J, Alonso P, López-Solà M, et al. Brain corticostriatal systems and the major clinical symptom dimensions of obsessive-compulsive disorder. Biol Psychiatry. 2013;73:321–328. doi: 10.1016/j.biopsych.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 27.Ahmari SE, Spellman T, Douglass NL, Kheirbek MA, Simpson HB, Deisseroth K, et al. Repeated cortico-striatal stimulation generates persistent OCD-like behavior. Science. 2013;340:1234–1239. doi: 10.1126/science.1234733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adler CM, McDonough-Ryan P, Sax KW, Holland SK, Arndt S, Strakowski SM. fMRI of neuronal activation with symptom provocation in unmedicated patients with obsessive compulsive disorder. J Psychiatr Res. 2000;34:317–324. doi: 10.1016/S0022-3956(00)00022-4. [DOI] [PubMed] [Google Scholar]
- 29.Pittenger C, Bloch MH, Williams K. Glutamate abnormalities in obsessive compulsive disorder: neurobiology, pathophysiology, and treatment. Pharmacol Ther. 2011;132:314–332. doi: 10.1016/j.pharmthera.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu K, Hanna GL, Rosenberg DR, Arnold PD. The role of glutamate signaling in the pathogenesis and treatment of obsessive-compulsive disorder. Pharmacol Biochem Behav. 2012;100:726–735. doi: 10.1016/j.pbb.2011.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yücel M, Wood SJ, Wellard RM, Harrison BJ, Fornito A, Pujol J, et al. Anterior cingulate glutamate-glutamine levels predict symptom severity in women with obsessive-compulsive disorder. Aust N Z J Psychiatry. 2008;42:467–477. doi: 10.1080/00048670802050546. [DOI] [PubMed] [Google Scholar]
- 32.Chakrabarty K, Bhattacharyya S, Christopher R, Khanna S. Glutamatergic dysfunction in OCD. Neuropsychopharmacology. 2005;30:1735–1740. doi: 10.1038/sj.npp.1300733. [DOI] [PubMed] [Google Scholar]
- 33.Burdo J, Dargusch R, Schubert D. Distribution of the cystine/glutamate antiporter system xc- in the brain, kidney, and duodenum. J Histochem Cytochem. 2006;54:549–557. doi: 10.1369/jhc.5A6840.2006. [DOI] [PubMed] [Google Scholar]
- 34.Behl A, Swami G, Sircar SS, Bhatia MS, Banerjee BD. Relationship of possible stress-related biochemical markers to oxidative/antioxidative status in obsessive-compulsive disorder. Neuropsychobiology. 2010;61:210–214. doi: 10.1159/000306591. [DOI] [PubMed] [Google Scholar]
- 35.Chakraborty S, Singh OP, Dasgupta A, Mandal N, Nath Das H. Correlation between lipid peroxidation-induced TBARS level and disease severity in obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33:363–366. doi: 10.1016/j.pnpbp.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 36.Riaza Bermudo-Soriano C, Perez-Rodriguez MM, Vaquero-Lorenzo C, Baca-Garcia E. New perspectives in glutamate and anxiety. Pharmacol Biochem Behav. 2012;100:752–774. doi: 10.1016/j.pbb.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 37.Flessner CA, Knopik VS, McGeary J. Hair pulling disorder (trichotillomania): genes, neurobiology, and a model for understanding impulsivity and compulsivity. Psychiatry Res. 2012;199:151–158. doi: 10.1016/j.psychres.2012.03.039. [DOI] [PubMed] [Google Scholar]
- 38.Fontenelle LF, Oostermeijer S, Harrison BJ, Pantelis C, Yücel M. Obsessive-compulsive disorder, impulse control disorders and drug addiction: common features and potential treatments. Drugs. 2011;71:827–840. doi: 10.2165/11591790-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 39.Grant JE, Odlaug BL, Kim SW. N-acetylcysteine, a glutamate modulator, in the treatment of trichotillomania: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2009;66:756–763. doi: 10.1001/archgenpsychiatry.2009.60. [DOI] [PubMed] [Google Scholar]
- 40.Bauer J, Pedersen A, Scherbaum N, Bening J, Patschke J, Kugel H, et al. Craving in alcohol-dependent patients after detoxification is related to glutamatergic dysfunction in the nucleus accumbens and the anterior cingulate cortex. Neuropsychopharmacology. 2013;38:1401–1408. doi: 10.1038/npp.2013.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schmaal L, Veltman DJ, Nederveen A, van den Brink W, Goudriaan AE. N-acetylcysteine normalizes glutamate levels in cocaine-dependent patients: a randomized crossover magnetic resonance spectroscopy study. Neuropsychopharmacology. 2012;37:2143–2152. doi: 10.1038/npp.2012.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grados MA, Specht MW, Sung HM, Fortune D. Glutamate drugs and pharmacogenetics of OCD: a pathway-based exploratory approach. Expert Opin Drug Discov. 2013;8:1515–1527. doi: 10.1517/17460441.2013.845553. [DOI] [PubMed] [Google Scholar]
- 43.Bonanomi L, Gazzaniga A. Toxicological, pharmacokinetic and metabolic studies on acetylcysteine. Eur J Respir Dis Suppl. 1980;111:45–51. [PubMed] [Google Scholar]
- 44.Berk M, Malhi GS, Gray LJ, Dean OM. The promise of N-acetylcysteine in neuropsychiatry. Trends Pharmacol Sci. 2013;34:167–177. doi: 10.1016/j.tips.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 45.Atkuri KR, Mantovani JJ, Herzenberg LA, Herzenberg LA. N-Acetylcysteine--a safe antidote for cysteine/glutathione deficiency. Curr Opin Pharmacol. 2007;7:355–359. doi: 10.1016/j.coph.2007.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Erickson MA, Hansen K, Banks WA. Inflammation-induced dysfunction of the low-density lipoprotein receptor-related protein-1 at the blood-brain barrier: protection by the antioxidant N-acetylcysteine. Brain Behav Immun. 2012;26:1085–1094. doi: 10.1016/j.bbi.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arfsten DP, Johnson EW, Wilfong ER, Jung AE, Bobb AJ. Distribution of radio-labeled N-Acetyl-L-Cysteine in Sprague-Dawley rats and its effect on glutathione metabolism following single and repeat dosing by oral gavage. Cutan Ocul Toxicol. 2007;26:113–134. doi: 10.1080/15569520701212233. [DOI] [PubMed] [Google Scholar]
- 48.Sheffner AL, Medler EM, Bailey KR, Gallo DG, Mueller AJ, Sarett HP. Metabolic studies with acetylcysteine. Biochem Pharmacol. 1966;15:1523–1535. doi: 10.1016/0006-2952(66)90197-3. [DOI] [PubMed] [Google Scholar]
- 49.Dean OM, van den Buuse M, Berk M, Copolov DL, Mavros C, Bush AI. N-acetyl cysteine restores brain glutathione loss in combined 2-cyclohexene-1-one and d-amphetamine-treated rats: relevance to schizophrenia and bipolar disorder. Neurosci Lett. 2011;499:149–153. doi: 10.1016/j.neulet.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 50.Das P, Tanious M, Fritz K, Dodd S, Dean OM, Berk M, et al. Metabolite profiles in the anterior cingulate cortex of depressed patients differentiate those taking N-acetyl-cysteine versus placebo. Aust N Z J Psychiatry. 2013;47:347–354. doi: 10.1177/0004867412474074. [DOI] [PubMed] [Google Scholar]
- 51.Smith QR. Transport of glutamate and other amino acids at the blood-brain barrier. J Nutr. 2000;130(4S Suppl):1016S–1022S. doi: 10.1093/jn/130.4.1016S. [DOI] [PubMed] [Google Scholar]
- 52.Kau KS, Madayag A, Mantsch JR, Grier MD, Abdulhameed O, Baker DA. Blunted cystine-glutamate antiporter function in the nucleus accumbens promotes cocaine-induced drug seeking. Neuroscience. 2008;155:530–537. doi: 10.1016/j.neuroscience.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kalivas PW. The glutamate homeostasis hypothesis of addiction. Nat Rev Neurosci. 2009;10:561–572. doi: 10.1038/nrn2515. [DOI] [PubMed] [Google Scholar]
- 54.Baker DA, Shen H, Kalivas PW. Cystine/glutamate exchange serves as the source for extracellular glutamate: modifications by repeated cocaine administration. Amino Acids. 2002;23:161–162. doi: 10.1007/s00726-001-0122-6. [DOI] [PubMed] [Google Scholar]
- 55.Moran MM, McFarland K, Melendez RI, Kalivas PW, Seamans JK. Cystine/glutamate exchange regulates metabotropic glutamate receptor presynaptic inhibition of excitatory transmission and vulnerability to cocaine seeking. J Neurosci. 2005;25:6389–6393. doi: 10.1523/JNEUROSCI.1007-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Baker DA, McFarland K, Lake RW, Shen H, Toda S, Kalivas PW. N-acetyl cysteine-induced blockade of cocaine-induced reinstatement. Ann N Y Acad Sci. 2003;1003:349–351. doi: 10.1196/annals.1300.023. [DOI] [PubMed] [Google Scholar]
- 57.Kupchik YM, Moussawi K, Tang XC, Wang X, Kalivas BC, Kolokithas R, et al. The effect of N-acetylcysteine in the nucleus accumbens on neurotransmission and relapse to cocaine. Biol Psychiatry. 2012;71:978–986. doi: 10.1016/j.biopsych.2011.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lushchak VI. Glutathione homeostasis and functions: potential targets for medical interventions. J Amino Acids. 2012;2012:736837. doi: 10.1155/2012/736837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gray KM, Watson NL, Carpenter MJ, Larowe SD. N-acetylcysteine (NAC) in young marijuana users: an open-label pilot study. Am J Addict. 2010;19:187–189. doi: 10.1111/j.1521-0391.2009.00027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Grant JE, Kim SW, Odlaug BL. N-acetyl cysteine, a glutamate-modulating agent, in the treatment of pathological gambling: a pilot study. Biol Psychiatry. 2007;62:652–657. doi: 10.1016/j.biopsych.2006.11.021. [DOI] [PubMed] [Google Scholar]
- 61.Berk M, Copolov DL, Dean O, Lu K, Jeavons S, Schapkaitz I, et al. N-acetyl cysteine for depressive symptoms in bipolar disorder--a double-blind randomized placebo-controlled trial. Biol Psychiatry. 2008;64:468–475. doi: 10.1016/j.biopsych.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 62.Berk M, Dean O, Cotton SM, Gama CS, Kapczinski F, Fernandes BS, et al. The efficacy of N-acetylcysteine as an adjunctive treatment in bipolar depression: an open label trial. J Affect Disord. 2011;135:389–394. doi: 10.1016/j.jad.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 63.Lavoie S, Murray MM, Deppen P, Knyazeva MG, Berk M, Boulat O, et al. Glutathione precursor, N-acetyl-cysteine, improves mismatch negativity in schizophrenia patients. Neuropsychopharmacology. 2008;33:2187–2199. doi: 10.1038/sj.npp.1301624. [DOI] [PubMed] [Google Scholar]
- 64.Bulut M, Savas HA, Altindag A, Virit O, Dalkilic A. Beneficial effects of N-acetylcysteine in treatment resistant schizophrenia. World J Biol Psychiatry. 2009;10:626–628. doi: 10.1080/15622970903144004. [DOI] [PubMed] [Google Scholar]
- 65.Hardan AY, Fung LK, Libove RA, Obukhanych TV, Nair S, Herzenberg LA, et al. A randomized controlled pilot trial of oral N-acetylcysteine in children with autism. Biol Psychiatry. 2012;71:956–961. doi: 10.1016/j.biopsych.2012.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Egashira N, Shirakawa A, Abe M, Niki T, Mishima K, Iwasaki K, et al. N-acetyl-L-cysteine inhibits marble- burying behavior in mice. J Pharmacol Sci. 2012;119:97–101. doi: 10.1254/jphs.11228SC. [DOI] [PubMed] [Google Scholar]
- 67.Lafleur DL, Pittenger C, Kelmendi B, Gardner T, Wasylink S, Malison RT, et al. N-acetylcysteine augmentation in serotonin reuptake inhibitor refractory obsessive-compulsive disorder. Psychopharmacology (Berl) 2006;184:254–256. doi: 10.1007/s00213-005-0246-6. [DOI] [PubMed] [Google Scholar]
- 68.Afshar H, Roohafza H, Mohammad-Beigi H, Haghighi M, Jahangard L, Shokouh P, et al. N-acetylcysteine add-on treatment in refractory obsessive-compulsive disorder: a randomized, double-blind, placebo-controlled trial. J Clin Psychopharmacol. 2012;32:797–803. doi: 10.1097/JCP.0b013e318272677d. [DOI] [PubMed] [Google Scholar]
- 69.Camfield DA, Sarris J, Berk M. Nutraceuticals in the treatment of obsessive compulsive disorder (OCD): a review of mechanistic and clinical evidence. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:887–895. doi: 10.1016/j.pnpbp.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 70.Sarris J, Camfield D, Berk M. Complementary medicine, self-help, and lifestyle interventions for obsessive compulsive disorder (OCD) and the OCD spectrum: a systematic review. J Affect Disord. 2012;138:213–221. doi: 10.1016/j.jad.2011.04.051. [DOI] [PubMed] [Google Scholar]
- 71.Van Ameringen M, Patterson B, Simpson W, Turna J. N-acetylcysteine augmentation in treatment resistant obsessive compulsive disorder: A case series. J Obesessive-Compuls Relat Disord. 2013;2:48–52. doi: 10.1016/j.jocrd.2012.10.003. [DOI] [Google Scholar]
- 72.Rodrigues-Barata AR, Tosti A, Rodríguez-Pichardo A, Camacho-Martínez F. N-acetylcysteine in the treatment of trichotillomania. Int J Trichology. 2012;4:176–178. doi: 10.4103/0974-7753.100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Odlaug BL, Grant JE. N-acetyl cysteine in the treatment of grooming disorders. J Clin Psychopharmacol. 2007;27:227–229. doi: 10.1097/01.jcp.0000264976.86990.00. [DOI] [PubMed] [Google Scholar]
- 74.Silva-Netto R, Jesus G, Nogueira M, Tavares H. N-acetyl-cysteine in the treatment of skin-picking disorder. Rev Bras Psiquiatr. 2014;36:101. doi: 10.1590/1516-4446-2013-1154. [DOI] [PubMed] [Google Scholar]
- 75.Berk M, Jeavons S, Dean OM, Dodd S, Moss K, Gama CS, et al. Nail-biting stuff? The effect of N-acetyl cysteine on nail-biting. CNS Spectr. 2009;14:357–360. doi: 10.1017/s1092852900023002. [DOI] [PubMed] [Google Scholar]
- 76.Bloch MH, Panza KE, Grant JE, Pittenger C, Leckman JF. N-Acetylcysteine in the treatment of pediatric trichotillomania: a randomized, double-blind, placebo-controlled add-on trial. J Am Acad Child Adolesc Psychiatry. 2013;52:231–240. doi: 10.1016/j.jaac.2012.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Panza KE, Pittenger C, Bloch MH. Age and gender correlates of pulling in pediatric trichotillomania. J Am Acad Child Adolesc Psychiatry. 2013;52:241–249. doi: 10.1016/j.jaac.2012.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Miller JL, Angulo M. An open-label pilot study of N-acetylcysteine for skin-picking in Prader-Willi syndrome. Am J Med Genet A. 2014;164A:421–424. doi: 10.1002/ajmg.a.36306. [DOI] [PubMed] [Google Scholar]
- 79.Clarke DJ, Boer H, Whittington J, Holland A, Butler J, Webb T. Prader-Willi syndrome, compulsive and ritualistic behaviours: the first population-based survey. Br J Psychiatry. 2002;180:358–362. doi: 10.1192/bjp.180.4.358. [DOI] [PubMed] [Google Scholar]
- 80.Morgan JR, Storch EA, Woods DW, Bodzin D, Lewin AB, Murphy TK. A preliminary analysis of the phenomenology of skin-picking in Prader-Willi syndrome. Child Psychiatry Hum Dev. 2010;41:448–463. doi: 10.1007/s10578-010-0180-7. [DOI] [PubMed] [Google Scholar]
- 81.Ghanizadeh A, Derakhshan N, Berk M. N-acetylcysteine versus placebo for treating nail biting, a double blind randomized placebo controlled clinical trial. Antiinflamm Antiallergy Agents Med Chem. 2013;12:223–228. doi: 10.2174/1871523011312030003. [DOI] [PubMed] [Google Scholar]
- 82.Costa-Campos L, Herrmann AP, Pilz LK, Michels M, Noetzold G, Elisabetsky E. Interactive effects of N-acetyl-cysteine and antidepressants. Prog Neuropsychopharmacol Biol Psychiatry. 2013;44:125–130. doi: 10.1016/j.pnpbp.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 83.De Rosa SC, Zaretsky MD, Dubs JG, Roederer M, Anderson M, Green A, et al. N-acetylcysteine replenishes glutathione in HIV infection. Eur J Clin Invest. 2000;30:915–929. doi: 10.1046/j.1365-2362.2000.00736.x. [DOI] [PubMed] [Google Scholar]