Summary
Introduction: Patients with obstructive sleep apnea-hypopnea syndrome (OSAHS) often have associated changes in craniofacial morphology and distribution of body fat, either alone or in combination.
Aim: To correlate cephalometric and anthropometric measures with OSAHS severity by using the apnea-hypopnea index (AHI).
Method: A retrospective cephalometry study of 93 patients with OSAHS was conducted from July 2010 to July 2012. The following measurements were evaluated: body mass index (BMI), neck circumference (NC), waist circumference (WC), hip circumference (HC), the angles formed by the cranial base and the maxilla (SNA) and the mandible (SNB), the difference between SNA and SNB (ANB), the distance from the mandibular plane to the hyoid bone (MP-H), the space between the base of the tongue and the posterior pharyngeal wall (PAS), and the distance between the posterior nasal spine and the tip of the uvula (PNS-P). Means, standard deviations, and Pearson's correlation coefficients were calculated and analyzed.
Results: AHI correlated significantly with BMI (r = 0.207, p = 0.047), NC (r = 0.365, p = 0.000), WC (r = 0.337, p = 0.001), PNS-P (r = 0.282, p = 0.006), and MP-H (r = 0.235, p = 0.023).
Conclusion: Anthropometric measurements (BMI, NC, and WC) and cephalometric measurements (MP-H and PNS-P) can be used as predictors of OSAHS severity.
Keywords: Cephalometry, Sleep Apnea, Obstructive, Anthropometry, Body Mass Index, Abdominal Circumference, Waist Circumference
Introduction
Obstructive sleep apnea-hypopnea syndrome (OSAHS) is a disorder characterized by recurrent episodes of partial or total upper airway obstruction during sleep. The apnea-hypopnea index (AHI) refers to the number of episodes of apnea and hypopnea that occur per hour of sleep1.
OSAHS affects 4–7% of the general adult population2. Owing to its current prevalence, it is considered a major public health concern, which can manifest serious physical and social consequences if not managed properly2 3. This disorder mainly affects middle-aged economically active patients, resulting in high costs and lost workdays4. Medical costs can be significantly reduced when effective diagnosis and treatment are performed early5. The diagnosis of OSAHS is based on a combination of the laboratory findings of apnea and hypopnea with clinical symptoms6.
Radiographic imaging of the upper airways allows for the study of bone and soft tissue anatomy, in addition to the determination of the site of obstruction and the choice of appropriate treatment for OSAHS patients7. Cephalometry has been used since 1983 and was initially applied in patients with sleep-related breathing disorders. It consists of cephalometric tracings obtained by teleradiography of the facial profile. The aim of the test is to study the facial, maxillary, and mandibular skeleton and any relationships with the soft tissues that may cause pharyngeal obstruction8. Cephalometry is an easy, low-cost, non-invasive, and widely available modality in the majority of hospitals. Radiation use is minimal, readily accessible to clinicians, and not uncomfortable for the patient. It has proved to be useful for the evaluation of the upper airways and bone structure in normal subjects and OSAHS patients9 10 11.
A complete cephalometric analysis should be performed in patients with OSAHS to identify associated maxillofacial abnormalities12. From this perspective, it has been used in several sleep disorder centers, with the purpose of diagnosing the site of obstruction in patients with obstructive sleep apnea. In some centers, this test is part of a service protocol that is important for the decision as to which type of surgery should be performed. Therefore, it is recommended in all patients with OSAHS undergoing surgery8 9 12 13 14 15. It is also used with mandibular advancement devices to assess therapeutic efficacy in patients with mild to moderate OSAHS15 16.
Obesity, in particular the presence of visceral fat, is considered a predictive factor for OSAHS17. Several studies have been performed using anthropometric measurements of obesity in patients with OSAHS, e.g., body mass index (BMI), neck circumference (NC), waist circumference (WC), and hip circumference (HC)18 19 20 21. These measurements may be used both to assess the need for patient referral to polysomnographic evaluation and to anticipate treatment in high-risk patients, since this disorder may cause severe consequences in untreated patients2 21. Polysomnography is not an accessible test for most individuals. It is expensive and easier, more affordable tests with less technological density, such as cephalometry9 10 11, are required17 19 22 23 to screen for OSAHS. Anthropometric measurements are easily obtained and fundamental for the preparatory study of a patient with suspected OSAHS. Therefore, the number of patients referred for polysomnography could be greatly reduced, lowering healthcare expenses, with simple measurement of cervical, waist, and hip circumferences. The use of these measurements in patients with snoring and those clinically suspected of having OSAHS would thus prioritize complementary polysomnography testing in patients with higher suspicion of disease24.
The aim of this study was to correlate cephalometric and anthropometric measurements with the AHI, in order to assess if these measurements can be used as predictors of OSAHS severity.
Method
Data obtained from the medical charts of 93 male and female patients with OSAHS, ranging in age from 19 to 80 years, were studied. These patients had been examined from July 2010 to July 2012 in a specialist private clinic in Teresina. The medical charts of patients who had undergone previous surgical treatment for OSAHS, including use of continuous positive airway pressure devices or intraoral devices, in addition to patients with craniofacial deformities and upper airway tumors, were excluded from the study.
Overnight polysomnography was analyzed by a single professional, who specialized in sleep disorders. Patients were considered to have OSAHS if, in addition to clinical complaints, they had an AHI ≥ 5 upon overnight polysomnography testing1. Severity was measured by the AHI. Cephalometry was also performed by a single radiologist, who specialized in orthodontic radiographs. Each examiner was blinded to the test results obtained by the other examiner.
The following cephalometric traces were considered, since they are the most commonly used cephalometric measures: retroglossal posterior airway space (PAS), defined as the space between the base of the tongue and the posterior pharyngeal wall; the distance between the mandibular plane and the hyoid bone (MP-H); the SNA angle, formed by the junction between the sellar point (S, midpoint of the sella turcica), nasion (N, junction between the frontal and nasal bones), and point A (deepest concavity on the anterior profile of the maxilla); the SNB angle, formed by the junction between the sellar point (S), nasion (N), and point B (deepest concavity on the anterior profile of the mandibular symphysis); the distance between the posterior nasal spine and the tip of the soft palate (PNS-P); and the difference between SNA and SNB (ANB) (Figure 1)8 9 12 15.
Figure 1.
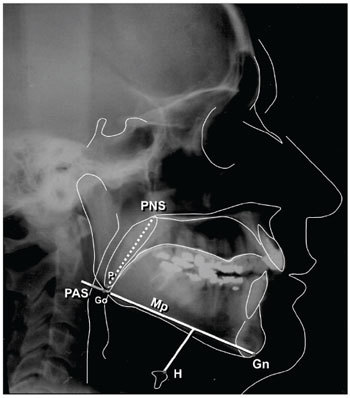
Description of cephalometric parameters (Source: the author).
Concerning anthropometric measurements, BMI, NC, WC, and HC were evaluated. BMI was calculated as the weight of the subject (in kilograms) divided by their height (in meters) squared. Obesity is defined as a BMI ≥ 30 kg/m2 25. NC was measured at the level of the crycothyroid cartilage. WC was measured between the last rib and the iliac crest and HC was measured as the maximum circumference at the level of the border of the trochanter. Anthropometric measurements were based on the World Health Organization manual 26.
Data was entered into the Statistical Package for the Social Sciences (SPSS) version 16.0 program for calculation of simple descriptive statistics, e.g., percentage distribution, mean, and standard deviation. A normality test (Kolmogorov-Smirnov) was applied and the adequate statistical test was chosen for each type of variable (parametric or nonparametric). Pearson's correlation coefficients were examined between AHI and the following variables: age, BMI, NC, WC, HC, and cephalometric measurements (SNA, SNB, ANB, MP-H, PAS, and PNS-P). Sex differences were compared by the Student's t test. Statistical significance was set at p < 0.05.
The project was approved by the Research Ethics Committee of the Universidade Federal do Piauí, under CAAE number 0047.0.045.000-10.
Results
Of the 93 patients studied, 54 (58.1%) were male. The mean BMI was 27.68 ± 3.83 kg/m2 (women, 27.41 ± 4.50 kg/m2; men, 27.88 ± 3.30 kg/m2). There were 69 (74.19%) nonobese (BMI, 25.90 ± 2.29 kg/m2) and 24 (25.81%) obese (BMI, 32.81 ± 2.50 kg/m2) patients (Table 1).
Table 1. Sample distribution according to gender and obesity.
| n | % | BMI, kg/m2 | ||
|---|---|---|---|---|
| (mean ± SD) | ||||
| Gender | Male | 54 | 58.06 | 27.88 ± 3.30 |
| Female | 39 | 41.94 | 27.41 ± 4.50 | |
| Total | 93 | 100.00 | 27.68 ± 3.83 | |
| Obesity | Nonobese | 69 | 74.19 | 25.90 ± 2.29 |
| Obese | 24 | 25.81 | 32.81 ± 2.50 | |
| Total | 93 | 100.00 | 27.68 ± 3.83 |
Note: BMI = body mass index.
The mean age of the patients was 46.70 ± 15.46 years (range, 19 to 80 years). Table 2 describes the sample characteristics and variables studied, including their variations and means.
Table 2. Characteristics of the sample including age, anthropometric parameters, cephalometric parameters, and AHI (n = 93).
| Variable | Minimum | Maximum | Mean | Standard deviation |
|---|---|---|---|---|
| Age, years | 19.0 | 80.0 | 46.70 | 15.46 |
| BMI, kg/m2 | 19.72 | 40.18 | 27.68 | 3.83 |
| NC, cm | 30.0 | 47.0 | 38.56 | 3.92 |
| WC, cm | 73.0 | 125.0 | 97.59 | 10.10 |
| HC, cm | 87.0 | 131.0 | 104.09 | 7.39 |
| SNA° | 72.0 | 92.0 | 82.77 | 4.08 |
| SNB° | 69.0 | 92.0 | 80.96 | 4.41 |
| ANB° | −13.0 | 10.0 | 1.82 | 3.90 |
| MP-H, mm | 4.0 | 45.0 | 19.21 | 8.22 |
| PAS, mm | 3.0 | 20.0 | 10.04 | 3.80 |
| PNS-P, mm | 20.0 | 52.0 | 39.84 | 5.37 |
| AHI, events/h | 5.00 | 83.40 | 34.67 | 17.41 |
Note: AHI = apnea-hypopnea index; BMI = body mass index; NC = neck circumference; WC = waist circumference; HC = hip circumference; SNA = angle formed by the junction of the sella (S), nasion (N), and point A; SNB = angle formed by the junction of the sella (S), nasion (N), and point B; ANB = difference between SNA and SNB; MP–H = distance between the mandibular plane and the hyoid bone; PAS = space between the base of the tongue and the posterior pharyngeal wall; PNS–P = distance between the posterior nasal spine and the tip of the soft palate.
Table 3 shows an analysis of the Pearson correlation coefficients used to evaluate the relationship between AHI, age, and anthropometric/cephalometric measurements. Analyzing the relationship between age and OSAHS severity by AHI showed a positive correlation between these 2 data series, indicating that OSAHS was more severe in older patients. Similarly, there was also a positive correlation between BMI and AHI, which allowed us to infer that the higher the BMI, the greater the AHI. Regarding body circumference measurements, both NC and WC showed a statistically significant positive correlation with OSAHS severity. Concerning the relationship between cephalometric data and AHI, a statistically significant positive correlation for MP-H and PNS-P was observed (Table 3).
Table 3. Correlation of age and anthropometric/cephalometric data with AHI (n = 93).
| Age | BMI | NC | WC | HC | SNA | SNB | ANB | MP-H | PAS | PNS-P | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pearson correlation | 0.241 | 0.207 | 0.365 | 0.337 | 0.201 | −0.044 | 0.031 | −0.081 | 0.235 | −0.102 | 0.282 |
| p-value (two-tailed) | 0.020 | 0.047 | 0.000 | 0.001 | 0.053 | 0.676 | 0.769 | 0.441 | 0.023 | 0.329 | 0.006 |
Note: AHI = apnea-hypopnea index; BMI = body mass index; NC = neck circumference; WC = waist circumference; HC = hip circumference; SNA = angle formed by the junction of the sella (S), nasion (N), and point A; SNB = angle formed by the junction of the sella (S), nasion (N), and point B; ANB = difference between SNA and SNB; MP–H = distance between the mandibular plane and the hyoid bone; PAS = space between the base of the tongue and the posterior pharyngeal wall; PNS–P = distance between the posterior nasal spine and the tip of the soft palate
Comparing anthropometric parameters between men and women indicated a statistically significant difference for NC and WC, but not for HC. Regarding cephalometry, MP-H and PNS-P were significantly different between men and women (Table 4).
Table 4. Comparison between males and females for anthropometric/cephalometric data and AHI.
| Females (n = 39) | Males (n = 54) | p-value | |
|---|---|---|---|
| Age, years | 49.77 ± 14.32 | 44.48 ± 15.99 | p > 0.05 |
| BMI, kg/m2 | 27.41 ± 4.50 | 27.88 ± 3.30 | p > 0.05 |
| NC, cm | 35.31 ± 2.27 | 40.91 ± 3.09 | **p < 0.01 |
| WC, cm | 94.41 ± 10.79 | 99.89 ± 8.99 | **p < 0.01 |
| HC, cm | 102.56 ± 8.65 | 105.19 ± 6.18 | p > 0.05 |
| SNA° | 82.74 ± 3.38 | 82.80 ± 4.56 | p > 0.05 |
| SNB° | 80.41 ± 4.35 | 81.35 ± 4.44 | p > 0.05 |
| ANB° | 2.33 ± 3.98 | 1.44 ± 3.83 | p > 0.05 |
| MP-H, mm | 15.04 ± 6.62 | 22.22 ± 8.00 | **p < 0.01 |
| PAS, mm | 9.28 ± 3.44 | 10.59 ± 3.98 | p > 0.05 |
| PNS-P, mm | 37.82 ± 5.10 | 41.30 ± 5.12 | **p < 0.01 |
| AHI, events/h | 31.02 ± 15.20 | 37.30 ± 18.53 | p > 0.05 |
Note: AHI = apnea-hypopnea index; BMI = body mass index; NC = neck circumference; WC = waist circumference; HC = hip circumference; SNA = angle formed by the junction of the sella (S), nasion (N), and point A; SNB = angle formed by the junction of the sella (S), nasion (N), and point B; ANB = difference between SNA and SNB; MP–H = distance between the mandibular plane and the hyoid bone; PAS = space between the base of the tongue and the posterior pharyngeal wall; PNS–P = distance between the posterior nasal spine and the tip of the soft palate
Tables 5 and 6 show an analysis of the Pearson correlation coefficients used to assess the relationship between AHI and age as well as anthropometric/cephalometric measurements for males and females.
Table 5. Pearson correlation of AHI with age and anthropometric data for males and females.
| Age | BMI | NC | WC | HC | ||
|---|---|---|---|---|---|---|
| M | Pearson correlation | 0.358 | 0.273 | 0.349 | 0.395 | 0.156 |
| p-value (two-tailed) | 0.008** | 0.046* | 0.010** | 0.003** | 0.259 | |
| n | 54 | 54 | 54 | 54 | 54 | |
| F | Pearson correlation | 0.131 | 0.123 | 0.329 | 0.192 | 0.212 |
| p-value (two-tailed) | 0.426 | 0.457 | 0.041* | 0.242 | 0.195 | |
| n | 39 | 39 | 39 | 39 | 39 |
Note: AHI = apnea-hypopnea index; M = males; F = females; BMI = body mass index; NC = neck circumference; WC = waist circumference; HC = hip circumference; ** p < 0.01; * p < 0.05.
Table 6. Pearson correlation between AHI and cephalometric data for males and females.
| SNA | SNB | ANB | MP-H | PAS | PNS-P | ||
|---|---|---|---|---|---|---|---|
| M | Pearson correlation | −0.075 | 0.031 | −0.125 | 0.229 | −0.212 | 0.305 |
| p-value (two-tailed) | 0.592 | 0.822 | 0.368 | 0.096 | 0.124 | 0.025* | |
| n | 54 | 54 | 54 | 54 | 54 | 54 | |
| F | Pearson correlation | 0.020 | −0.021 | 0.040 | 0.073 | 0.010 | 0.135 |
| p-value (two-tailed) | 0.904 | 0.898 | 0.809 | 0.660 | 0.951 | 0.412 | |
| n | 39 | 39 | 39 | 39 | 39 | 39 |
Note: AHI = apnea-hypopnea index; M = males; F = females; SNA = angle formed by the junction of the sella (S), nasion (N), and point A; SNB = angle formed by the junction of the sella (S), nasion (N), and point B; ANB = difference between SNA and SNB; MP–H = distance between the mandibular plane and the hyoid bone; PAS = space between the base of the tongue and the posterior pharyngeal wall; PNS–P = distance between the posterior nasal spine and the tip of the soft palate; * p < 0.05.
For anthropometric measurements, AHI showed a statistically significant correlation with age, BMI, NC, and WC in males. Only NC showed a significant correlation in females. In both genders, the most significant correlation was with NC (Table 5). Regarding cephalometric measurements, the only correlation found was that of AHI with PNS-P measurement in males (Table 6).
Discussion
Obesity may increase susceptibility to OSAHS by causing fat deposition in the upper airway tissues, narrowing the nasopharyngeal caliber and/or leading to hypoventilation in association with reduced wall complacency27. Assessment of craniofacial morphology in OSAHS patients not only aids specialists concerned with recognizing morphologic changes induced by altered sleep patterns, but also provides the patient with adequate treatment11.
There is a vast amount of scientific literature on cephalometric and anthropometric measures, which compares control groups and snorers to OSAHS patients and aims at using these measurements as predictors of this condition7 9 10 11 13 15 18 20 22 28 29 30 31 32. Some studies have been performed to assess appropriate treatments, surgical treatment plans, and the indications of intraoral devices11 16 27 33 34 35 36 37 38 39 40, while others were performed to evaluate the relationship between these measurements and OSAHS severity17 18 19 20 22 23 24 32 40 41 42 43 44 45.
In the current study, there was a significant correlation between age and AHI (Table 3), indicating that OSAHS is more severe in older patients. This is in agreement with the majority of previous studies17 22 23 24 45 46, with the exception of those by Mayer et al42 and Schellenberg, Maisline, and Schwab37.
It was observed that BMI was correlated with AHI, allowing us to infer that more severe OSAHS occurs in subjects with a higher BMI, which is concordant with most published studies17 19 21 22 23 31 32 37 39 42 45 46 47. Nevertheless, this fact was not observed by Yucel et al41 and Martinez-Rivera et al24.
NC is a simple measurement that is easily performed. Findings in the present study point to a positive correlation between NC and AHI, which is in agreement with other studies19 20 22 24 31 32 37 38 39 41 46. A correlation with BMI was also observed previously17 18 19 23 32 44, suggesting that obesity affects patients with OSAHS through fat deposition in the neck20 23 30. In contrast to the majority of studies, Ogretmenoglu et al17 stated that NC was more weakly correlated with AHI than BMI.
WC also showed a positive correlation with AHI, in agreement with other studies19 23 24 32 38 39 46.This correlation was weaker than that observed with NC, supporting the existing literature19 23 39. The present study is also consistent with others 19 32 showing that the correlation of AHI with WC is greater than that with BMI. However, Davidson and Patel32 observed that WC was more predictive than BMI as well as NC.
Analyzing the relationship between cephalometric data and AHI showed a statistically significant correlation for MP-H and PNS-P, indicating an increased palatal length and an increased distance between the hyoid bone and the mandibular plane, which was consistent with other studies29 42 43 46 48. According to Yucel et al41, only MP-H measurement is related to AHI. The position of the hyoid bone, which has an impact on the shape and position of the tongue, affects hypopharyngeal airway patency41.
A study by Bharadwaj, Ravikumar, and Krishnaswamy conducted in India compared 10 OSAHS patients to a control group of 10 healthy subjects (mean age, 34.9 years). These authors concluded that upright cephalometry demonstrated mandibular retrognathism, increased ANB angle, increased PNS-P length and increased soft palate thickness, increased tongue length, and decreased PAS in the group of OSAHS patients when compared to the control group11. Other studies have shown that PNS-P and MP-H measurements are increased, while PAS is decreased, in patients with OSAHS, and these measurements were considered predictive of OSAHS7 9 15. PAS measurement was correlated with severity of OSAHS assessed using the AHI7 9. A study conducted in Strasbourg (France) in 1990, comparing 43 OSAHS patients to a control group of 40 asymptomatic individuals, showed that PNS-P measurement was increased in patients with OSAHS, while SNA, SNB, and ANB measurements did not demonstrate any alterations in either group28. Other studies have shown increased MP-H measurement and decreased PAS measurement in comparisons between OSAHS groups and control groups13 40. However, Mayer et al42 found no correlation between PAS measurement and AHI.
In a comparison between male and female patients in the present study, BMI and HC were similar. NC and WC were significantly higher in males than in females. These results are partially in agreement with findings by Millman et al49, who described a higher NC for males, but no difference between the genders for BMI and WC. Another study demonstrated a significantly increased BMI in females41. This fact reflects well-known characteristics concerning body fat distribution in men and women49.
In the current study, NC was more closely correlated with AHI than WC and BMI, both in the overall population and in male and female subjects, indicating that NC is the best anthropometric measurement for prediction of OSAHS severity, especially in males18 19 23 39 41 44. Comparing cephalometry between male and female subjects showed a statistically significant difference in MP-H and PNS-P measurements, which were higher in male subjects. PNS-P measurement was correlated with AHI in males, while there were no significant correlations in females.
In conclusion, the results of this study show a correlation of anthropometric (BMI, NC, and WC) and cephalometric (MP-H and PNS-P) measurements with the AHI, reinforcing their preparatory role and use as predictors of OSAHS.
References
- 1.Force AAoSMT . Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22(5):667–89. [PubMed] [Google Scholar]
- 2.Racionero Casero M A, Garcia Rio F, Pino Garcia J M, Prados Sanchez C, Diaz Lobato S, Villamor Leon J. [The sleep apnea syndrome as a health problem An estimation of its prevalence and morbimortality] An Med Interna. 1999;16(2):97–102. [PubMed] [Google Scholar]
- 3.Barthel S W, Strome M. Snoring, obstructive sleep apnea, and surgery. Med Clin North Am. 1999;83(1):85–96. doi: 10.1016/s0025-7125(05)70089-4. [DOI] [PubMed] [Google Scholar]
- 4.Pieters T, Rodenstein D O. Therapeutic options in obstructive sleep apnoea: have we made enough progress? Sleep medicine reviews. 2001;5(1):3–6. doi: 10.1053/smrv.2000.0148. [DOI] [PubMed] [Google Scholar]
- 5.Kapur V, Blough D K, Sandblom R E, Hert R, de Maine J B, Sullivan S D. et al. The medical cost of undiagnosed sleep apnea. Sleep. 1999;22(6):749–55. doi: 10.1093/sleep/22.6.749. [DOI] [PubMed] [Google Scholar]
- 6.Lindberg E, Gislason T. Epidemiology of sleep-related obstructive breathing. Sleep medicine reviews. 2000;4(5):411–33. doi: 10.1053/smrv.2000.0118. [DOI] [PubMed] [Google Scholar]
- 7.Powell N B, Riley R W, Robinson A. Surgical management of obstructive sleep apnea syndrome. Clin Chest Med. 1998;19(1):77–86. doi: 10.1016/s0272-5231(05)70433-0. [DOI] [PubMed] [Google Scholar]
- 8.Riley R, Guilleminault C, Herran J, Powell N. Cephalometric analyses and flow-volume loops in obstructive sleep apnea patients. Sleep. 1983;6(4):303–11. doi: 10.1093/sleep/6.4.303. [DOI] [PubMed] [Google Scholar]
- 9.Olszewska E, Sieskiewicz A, Rozycki J, Rogalewski M, Tarasow E, Rogowski M. et al. A comparison of cephalometric analysis using radiographs and craniofacial computed tomography in patients with obstructive sleep apnea syndrome: preliminary report. Eur Arch Otorhinolaryngol. 2009;266:535–42. doi: 10.1007/s00405-008-0826-2. [DOI] [PubMed] [Google Scholar]
- 10.Julià-Serdà G, Pérez-Peñate G, Saavedra-Santana P, Ponce-González M, Valencia-Gallardo J M, Rodríguez-Delgado R. et al. Usefulness of cephalometry in sparing polysomnography of patients with suspected obstructive sleep apnea. Sleep Breath. 2006;10(4):181–7. doi: 10.1007/s11325-006-0073-y. [DOI] [PubMed] [Google Scholar]
- 11.Bharadwaj R, Ravikumar A, Krishnaswamy N R. Evaluation of craniofacial morphology in patients with obstructive sleep apnea using lateral cephalometry and dynamic MRI. Indian J Dent Res. 2011;22(6):739–48. doi: 10.4103/0970-9290.94566. [DOI] [PubMed] [Google Scholar]
- 12.Alvarez C M, Lessin M E, Gross P D. Mandibular advancement combined with horizontal advancement genioplasty for the treatment of obstructive sleep apnea in an edentulous patient. A case report. Oral Surg Oral Med Oral Pathol. 1987;64(4):402–6. doi: 10.1016/0030-4220(87)90139-3. [DOI] [PubMed] [Google Scholar]
- 13.Guilleminault C, Riley R, Powell N. Obstructive sleep apnea and abnormal cephalometric measurements. Implications for treatment. Chest. 1984;86(5):793–4. doi: 10.1378/chest.86.5.793. [DOI] [PubMed] [Google Scholar]
- 14.Safaya A, Suri J C. The protocol for the diagnosis of obstructive sleep apnea syndrome. IJO & HNS. 1998;50(1):46–51. doi: 10.1007/BF02996770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akpinar M E, Celikoyar M M, Altundag A, Kocak I. The comparison of cephalometric characteristics in nonobese obstructive sleep apnea subjects and primary snorers cephalometric measures in nonobese OSA and primary snorers. Eur Arch Otorhinolaryngol. 2011;268(7):1053–9. doi: 10.1007/s00405-010-1448-z. [DOI] [PubMed] [Google Scholar]
- 16.Rose E, Lehner M, Staats R, Jonas I E. Cephalometric analysis in patients with obstructive sleep apnea. J Orofac Orthop. 2002;63(4):315–24. doi: 10.1007/s00056-002-0058-9. [DOI] [PubMed] [Google Scholar]
- 17.Ogretmenoglu O, Suslu A E, Yucel O T, Onerci T M, Sahin A. Body fat composition: a predictive factor for obstructive sleep apnea. Laryngoscope. 2005;115(8):1493–8. doi: 10.1097/01.mlg.0000172204.82314.c3. [DOI] [PubMed] [Google Scholar]
- 18.Davies R J, Ali N J, Stradling J R. Neck circumference and other clinical features in the diagnosis of the obstructive syndrome. Thorax . 1992;47:101–5. doi: 10.1136/thx.47.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pinto J A, Godoy L BM, Marquis V WPB, Sonego T B, Leal C FA, Ártico M S. Anthropometric data as predictors of obstructive sleep apnea severity. Braz J Otorhinolaryngol. 2011;77(4):516–21. doi: 10.1590/S1808-86942011000400017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferguson K A, Ono T, Lowe A A, Ryan C F, Fleetham J A. The relationship between obesity and craniofacial structure in obstructive sleep apnea. Chest. 1995;108(2):375–81. doi: 10.1378/chest.108.2.375. [DOI] [PubMed] [Google Scholar]
- 21.Schafer H, Pauleit D, Sudhop T, Gouni-Berthold I, Ewig S, Berthold H K. Body fat distribution, serum leptin, and cardiovascular risk factors in men with obstructive sleep apnea. Chest. 2002;122(3):829–39. doi: 10.1378/chest.122.3.829. [DOI] [PubMed] [Google Scholar]
- 22.Montoya F S, Bedialauneta J RI, Larracoechea U A, Ibarguen A M, Del Rey A S, Fernandez J MS. The predictive value of clinical and epidemiological parameters in the identification of patients with obstructive sleep apnoea (OSA): a clinical prediction algorithm in the evaluation of OSA. Eur Arch Otorhinolaryngol. 2007;264(6):637–43. doi: 10.1007/s00405-006-0241-5. [DOI] [PubMed] [Google Scholar]
- 23.Dixon J B, Schachter L M, O'Brien P E. Predicting sleep apnea and excessive day sleepiness in the severely obese: indicators for polysomnography. Chest. 2003;123:1134–41. doi: 10.1378/chest.123.4.1134. [DOI] [PubMed] [Google Scholar]
- 24.Martinez-Rivera C, Abad J, Fiz J A, Rios J, Morera J. Usefulness of truncal obesity indices as predictive factors for obstructive sleep apnea syndrome. Obesity (Silver Spring) 2008;16(1):113–8. doi: 10.1038/oby.2007.20. [DOI] [PubMed] [Google Scholar]
- 25.WHO Obesity: preventing and managing the global epidemic Report of a WHO consultation. World Health Organization technical report series. 2000894i–xii., 1-253 [PubMed] [Google Scholar]
- 26.WHO Physical status: the use and interpretation of anthropometry Report of a WHO Expert Committee. World Health Organization technical report series. 19958541–452. [PubMed] [Google Scholar]
- 27.Redline S, Tishler P V. The genetics of sleep apnea. Sleep Med Rev. 2000;4(6):583–602. doi: 10.1053/smrv.2000.0120. [DOI] [PubMed] [Google Scholar]
- 28.Bacon W H, Turlot J C, Krieger J, Stierle J L. Cephalometric evaluation of pharyngeal obstructive factors in patients with sleep apneas syndrome. Angle Orthod. 1990;60(2):115–22. doi: 10.1043/0003-3219(1990)060<0115:CEOPOF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Maltais F, Carrier G, Cormier Y, Sériès F. Cephalometric measurements in snorers, non-snorers, and patients with sleep apnoea. Thorax. 1991;46:419–23. doi: 10.1136/thx.46.6.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barvaux V A, Aubert G, Rodenstein D O. Weight loss as a treatment for obstructive sleep apnoea. Sleep medicine reviews. 2000;4(5):435–52. doi: 10.1053/smrv.2000.0114. [DOI] [PubMed] [Google Scholar]
- 31.Sharma S K, Malik V, Vasudev C, Banga A, Mohan A, Handa K K. et al. Prediction of obstructive sleep apnea in patients presenting to a tertiary care center. Sleep Breath. 2006;10(3):147–54. doi: 10.1007/s11325-006-0062-1. [DOI] [PubMed] [Google Scholar]
- 32.Davidson T M, Patel M R. Waist circumference and sleep disordered breathing. Laryngoscope. 2008;118(2):339–47. doi: 10.1097/MLG.0b013e3181587d7c. [DOI] [PubMed] [Google Scholar]
- 33.Doghramji K Jabourian Z H Pilla M Farole A Lindholm R N Predictors of outcome for uvulopalatopharyngoplasty Laryngoscope 1995105(3 Pt 1):311–4. [DOI] [PubMed] [Google Scholar]
- 34.Series F, St Pierre S, Carrier G. Surgical correction of nasal obstruction in the treatment of mild sleep apnoea: importance of cephalometry in predicting outcome. Thorax. 1993;48(4):360–3. doi: 10.1136/thx.48.4.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Woodson B T. Structural effectiveness of pharyngeal sleep apnea surgery. Sleep medicine reviews. 2008;12(6):463–79. doi: 10.1016/j.smrv.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 36.Hora F, Napolis L M, Daltro C, Kodaira S K, Tufik S, Togeiro S M. et al. Clinical, anthropometric and upper airway anatomic characteristics of obese patients with obstructive sleep apnea syndrome. Respiration. 2007;74(5):517–24. doi: 10.1159/000097790. [DOI] [PubMed] [Google Scholar]
- 37.Schellenberg J B, Maislin G, Schwab R J. Physical findings and risk for obstructive sleep apnea. The importance of oropharyngeal structures. Am J Respir Crit Care Med. 2000;162:740–8. doi: 10.1164/ajrccm.162.2.9908123. [DOI] [PubMed] [Google Scholar]
- 38.Onat A Hergenc G Yuksel H Can G Ayhan E Kaya Z et al. Neck circumference as a measure of central obesity: associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference Clin Nutr 200928146–51.. Epub 2008/11/18 [DOI] [PubMed] [Google Scholar]
- 39.Hoffstein V, Mateika S. Differences in abdominal and neck circumferences in patients with and without obstructive sleep apnoea. Eur Respir J. 1992;5(4):377–81. [PubMed] [Google Scholar]
- 40.Partinen M, Guilleminault C, Quera-Salva M, Jamieson A. Obstructive sleep apnea and cephalometric roentgenograms. The role of anatomic upper airway abnormalities in the definition of abnormal breathing during sleep. Chest. 1988;93(6):1199–205. doi: 10.1378/chest.93.6.1199. [DOI] [PubMed] [Google Scholar]
- 41.Yucel A, Unlu M, Haktanir A, Acar M, Fidan F. Evaluation of the upper airway cross-sectional area changes in different degrees of severity of obstructive sleep apnea syndrome: cephalometric and dynamic CT study. AJNR Am J Neuroradiol. 2005;26(10):2624–9. [PMC free article] [PubMed] [Google Scholar]
- 42.Mayer P, Pépin J L, Bettega G, Veale D, Ferretti G, Deschaux C. et al. Relationship between body mass index, age and upper airway measurements in snorers and sleep apnoea patients. Eur Respir J. 1996;9(9):1801–9. doi: 10.1183/09031936.96.09091801. [DOI] [PubMed] [Google Scholar]
- 43.Davies R. Stradling. The relationship between neck circumference, radiographic pharyngeal anatomy, and the obstructive sleep apnoea syndrome. Eur Respir J. 1990;3(5):509–14. [PubMed] [Google Scholar]
- 44.Katz I Stradling J Sljutsky A S Zamel N Hoffstein V Do patients with obstructive sleep apnea have thick necks? Am Rev Respir Dis 1990141(5 Pt 1):1228–31. [DOI] [PubMed] [Google Scholar]
- 45.Young T, Peppard P E, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol . 2005;99:1592–9. doi: 10.1152/japplphysiol.00587.2005. [DOI] [PubMed] [Google Scholar]
- 46.Julia-Serda G, Perez-Penate G, Saavedra-Santana P, Ponce-Gonzalez M, Valencia-Gallardo J M, Rodriguez-Delgado R. et al. Usefulness of cephalometry in sparing polysomnography of patients with suspected obstructive sleep apnea. Sleep Breath. 2006;10(4):181–7. doi: 10.1007/s11325-006-0073-y. [DOI] [PubMed] [Google Scholar]
- 47.Katz I Stradling J Slutsky A S Zamel N Hoffstein V Do patients with obstructive sleep apnea have thick necks? The American review of respiratory disease 1990141(5 Pt 1):1228–31. [DOI] [PubMed] [Google Scholar]
- 48.de Tarso Moura Borges P, Paschoal J R. Initial indication of treatment in 60 patients with sleep obstructive ventilatory disturbance. Braz J Otorhinolaryngol. 2005;71(6):740–6. doi: 10.1016/S1808-8694(15)31242-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Millman R P, Carlisle C C, Eveloff S E, McGarvey S T, Levinson P D. Body fat distribution and sleep apnea severity in women. Chest. 1995;107(2):362–6. doi: 10.1378/chest.107.2.362. [DOI] [PubMed] [Google Scholar]


